Lung abscess Pleural empyema Tuberculosis Janusz Kowalewski MD
Lung abscess Pleural empyema Tuberculosis Janusz Kowalewski, MD, Ph. D. Department and Clinic of Thoracic Surgery Faculty of Medicine Nicolaus Copernicus University in Toruń
Lung abscess DEFINITION: Lung abscess (Latin: abscessus) is a collection of pus that has built up within the lung tissue. This is usually caused by a bacterial infection.
Lung absces: predisposing factors: - Diabetes - Neoplastic disease Alcohol abuse - Malnutrition - Narcotics abuse - Immunosupression - HIV infection - Older age
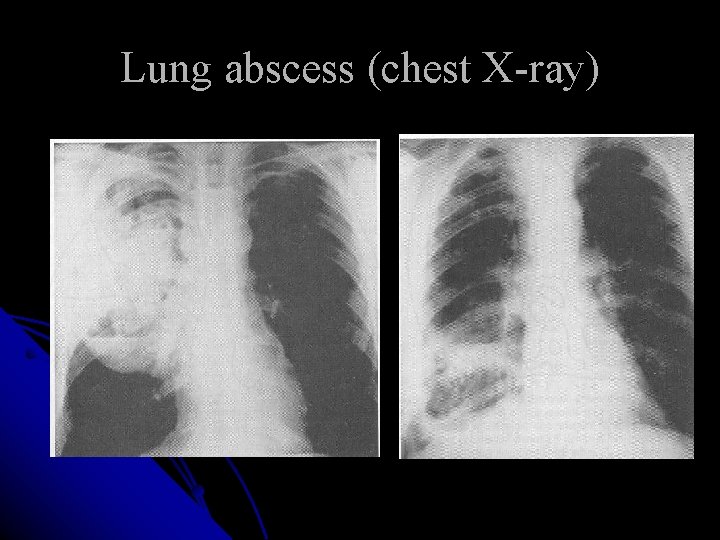
Lung abscess (chest X-ray)
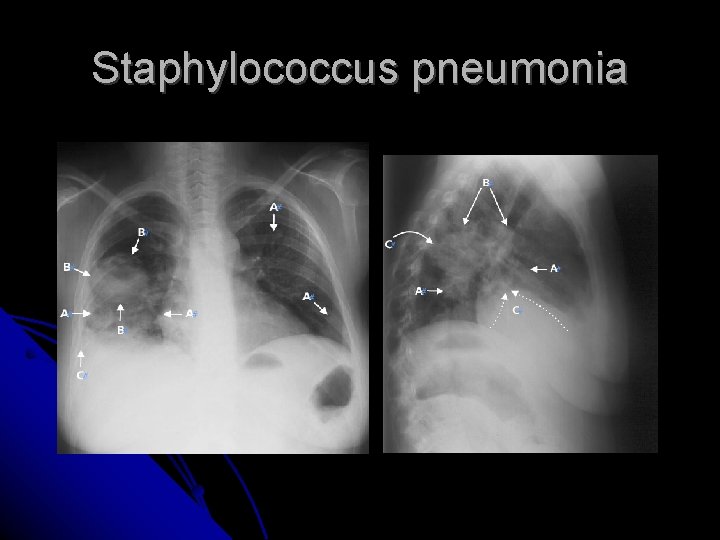
Staphylococcus pneumonia
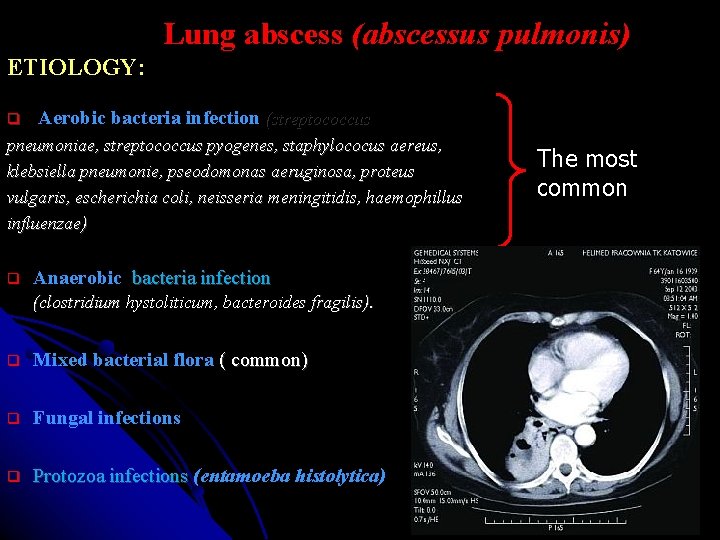
Lung abscess (abscessus pulmonis) ETIOLOGY: Aerobic bacteria infection (streptococcus pneumoniae, streptococcus pyogenes, staphylococus aereus, klebsiella pneumonie, pseodomonas aeruginosa, proteus vulgaris, escherichia coli, neisseria meningitidis, haemophillus influenzae) Anaerobic bacteria infection (clostridium hystoliticum, bacteroides fragilis). Mixed bacterial flora ( common) Fungal infections Protozoa infections (entamoeba histolytica) Protozoa infections The most common
Streptococcus pneumoniae
Staphylococcus aureus
Classification: Lung abscess (abscessus pulmonis) PRIMARY ABSCESS: In healthy lung parenchyma (anaerobic aspiration, specific pneumonia) SECONDARY ABSCESS: In lung tissue affected by: existing lung disease, metastatic tumors, lung carcinoma, foreign body, infarction, emphysema.
Lung abscess • Clinical signs ?
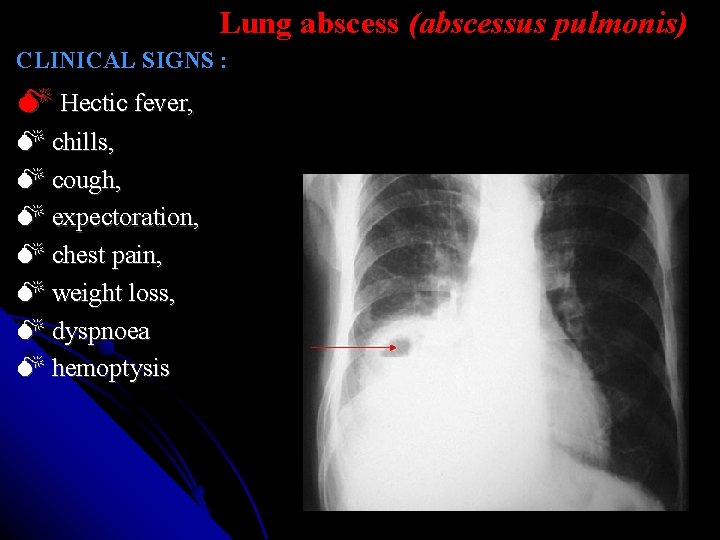
Lung abscess (abscessus pulmonis) CLINICAL SIGNS : Hectic fever, chills, cough, expectoration, chest pain, weight loss, dyspnoea hemoptysis
Lung absces (diagnosis) ?
Lung absces (abscessus pulmonis) Diagnosis: clinical signs, chest X-ray, CT scan, bronchoscopy, sputum analysis (BAL) CRP, OB, WBC elevation
Lung abscess (abscessus pulmonis) Bad prognostic factors: big abscess, right lower lobe, bad general condition (anemia, hipoproteinemia, alcohol abuse, narcotics abuse), pathogenic bacteria: - Pseudomonas aeruginosa – mortality rate: app. 83%, - Staphylococus aureus – mortality rate: app. 50%. - Klebsiella pneumoniae -44%). (Boaz Hirshberg, Miri Sklair-Levi, Ran Nir-Paz, Liat Ben-Sira, et al. Factors predicting mortality of patients with lung abscess Chest. Chicago: Mar 1999. Vol. 115, Iss. 3; pg. 746, 5 pgs)
Lung abscess (abscessus pulmonis) LOCAL COMPLICATIONS: Spread to the healthy lung tissue, Pleural empyema, Broncho-pleural fistula, Phlegmon of the chest wall, Major hemoptysis, Aspergilloma.
Lung abscess (abscessus pulmonis) General complicatons: bacterial endocarditis, multifocal liver abscess, multifocal brain abscess, nephritis, amyloidosis, sepsis, multi-organ failure Mortality rate: 15%-20% (Bartlett JG. Lung abscess. In: Baum GL, Wolinsky E, eds. Textbook of pulmonary diseases. 5 th ed. Boston, MA: Little, Brown and Company, 2007; 607 -620. )

Lung abscess (abscessus pulmonis) Conservative treatment ? ? ? : Antibiotics based on drug sensitivity 6 -8 weeks Supported by chest physiotherapy and bronchoscopic aspiration
Lung abscess (abscessus pulmonis) THERAPY: It is thought that lung abscess in its early stage can regress spontaneously in approximately 20 -30% of cases. If conservative treatment is ineffective or complications are observed adequate invasive or surgical treatment should be initiated. It is estimated that invasive treatment by intercostal tube drainage or surgery is indispensable in 11 -12% of patients in whom antibiotic therapy was ineffective. (Estrera AS, Platt MR, Mills LJ, et al. Primary lung abscess. J Thorac Cardiovasc Surg 1980; 79: 275 -282).
Lung abscess (abscessus pulmonis) INVASIVE THERAPY: INJECTION OF THERAPEUTIC AGENTS DIRECTLY INTO AN ABSCESS CAVITY: The abscess is punctured through the chest wall and antibiotics are injected directly into its cavity. This method is suitable for large peripheral abscesses where the visceral and parietal pleura are accreted. The method is burdened with a risk of pneumothorax or empyema formation. ENDOSCOPIC ABSCESS EVACUATION: If lung abscess is a result of pathology of the bronchial tree with its obstruction and retention of septic debris within bronchi distally to the level of obstruction bronchoscopy is an effective technique for abscess evacuation. The abscess evacuation can be completed by the injection of antibiotic into the abscess cavity.
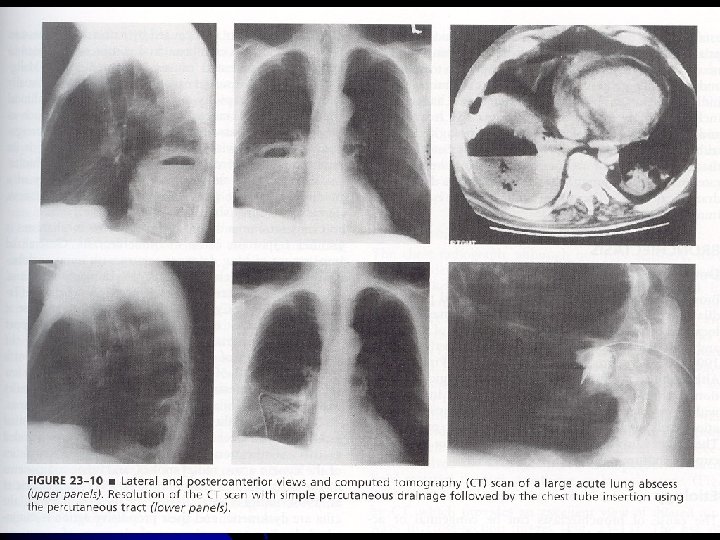
Lung abscess (abscessus pulmonis) INVASIVE MANAGEMENT: CAVERNOSTOMY: A method used in selected cases of lung abscess (Monaldi procedure). Obliteration of the pleural cavity is an indispensable condition to perform this procedure. Short fragments of two or three ribs are resected over a place where the distance between an abscess capsule and the chest wall is the shortest. The surface of the lung is visualized and the abscess cavity is opened. Then the abscess cavity is packed with gauze saturated with an antiseptic solution. The gauze is changed regularly for several weeks until the process of healing and contraction of a lung defect is obtained. PERCUTANEOUS CATHETER DRAINAGE Percutaneous catheter drainage of lung abscess under fluoroscopic or computed tomography guidance is a technique introduced into medical practice during last three decades and brings relatively good results in selected cases. The limitation of this method is a localization of an abscess near important anatomical structures that makes an introduction of a catheter hazardous. The technique is burdened with some serious complications such as pneumothorax accompanied by a brocho-pleural fistula, pleural empyema, hemorrhage and cardiac arrest.
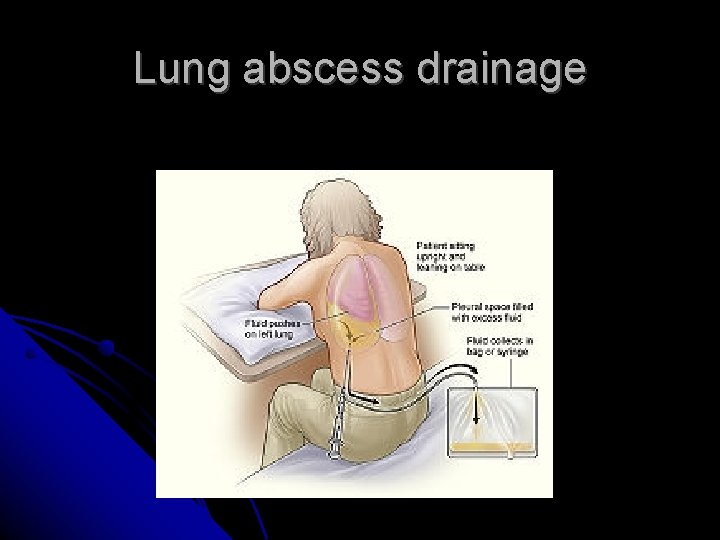
Lung abscess drainage
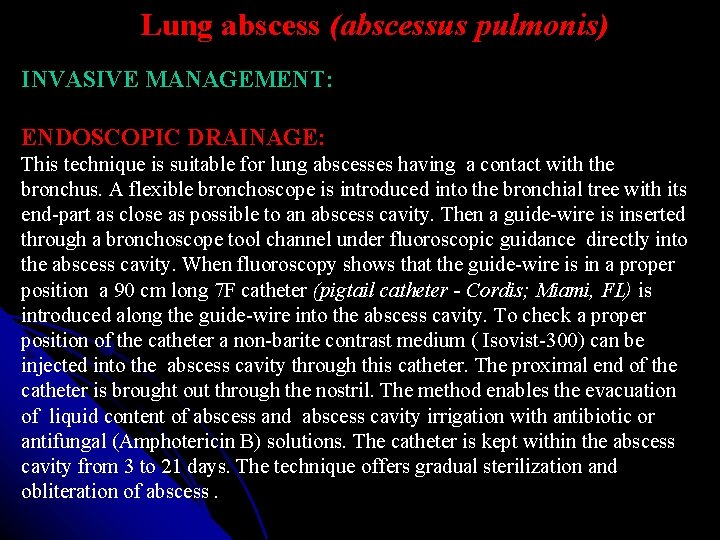
Lung abscess (abscessus pulmonis) INVASIVE MANAGEMENT: ENDOSCOPIC DRAINAGE: This technique is suitable for lung abscesses having a contact with the bronchus. A flexible bronchoscope is introduced into the bronchial tree with its end-part as close as possible to an abscess cavity. Then a guide-wire is inserted through a bronchoscope tool channel under fluoroscopic guidance directly into the abscess cavity. When fluoroscopy shows that the guide-wire is in a proper position a 90 cm long 7 F catheter (pigtail catheter - Cordis; Miami, FL) is introduced along the guide-wire into the abscess cavity. To check a proper position of the catheter a non-barite contrast medium ( Isovist-300) can be injected into the abscess cavity through this catheter. The proximal end of the catheter is brought out through the nostril. The method enables the evacuation of liquid content of abscess and abscess cavity irrigation with antibiotic or antifungal (Amphotericin B) solutions. The catheter is kept within the abscess cavity from 3 to 21 days. The technique offers gradual sterilization and obliteration of abscess.
Lung abscess (abscessus pulmonis) Surgical treatment: Method: RESECTION. Indications: ? ? ? Mortality rate: 11%-28%.
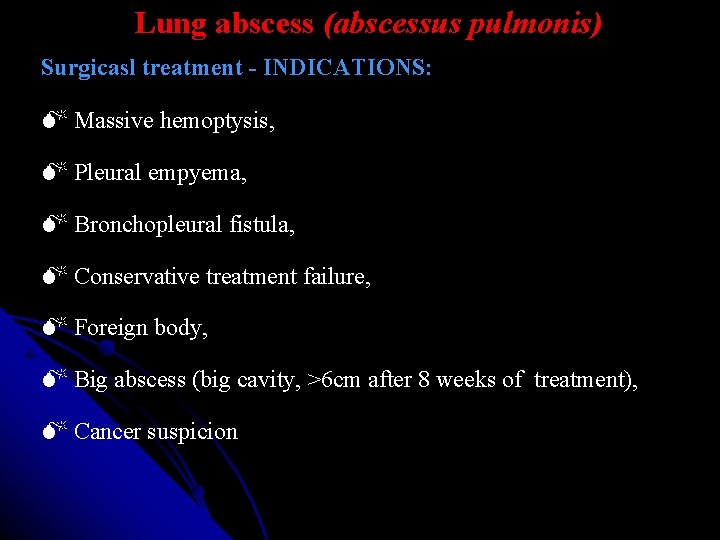
Lung abscess (abscessus pulmonis) Surgicasl treatment - INDICATIONS: Massive hemoptysis, Pleural empyema, Bronchopleural fistula, Conservative treatment failure, Foreign body, Big abscess (big cavity, >6 cm after 8 weeks of treatment), Cancer suspicion.
Lung cancer (abscessus pulmonis) Surgical treatment: METHODS: Wedge resection: Anatomical resections: (segmentectomy, lobectomy, pneumonectomy)
Lung abscess (abscessus pulmonis) METHODS OF SURGICAL TREATMENT: A type of resection of pulmonary parenchyma is dependent on localization and size of abscess and a patient’s general state. NON-ANATOMICAL LUNG RESECTION Marginal or wedge pulmonary parenchyma resection for abscesses using linear staplers: TA and GIA type is effective for small lesions localized peripherally. ANATOMICAL LUNG RESECTION Large lung abscesses, abscesses localized deeply in pulmonary parenchyma and multiple lung abscesses are all indications for anatomical resections. The most frequent procedures are resections of a pulmonary lobe (lobectomy) or resection of two pulmonary lobes of the right lung (bilobectomy). In the cases of solitary abscess or multiple abscesses with vast destruction of the lung the resection of the whole lung (pneumonectomy) is sometimes necessary. Local conditions rarely enable less extensive surgical procedures such as semisegmentectomy or bisegmentectomy.
Lung abscess (abscessus pulmonis) METHODS OF SURGICAL TREATMENT : VATS (Video Assisted Thoracic Surgery) A method that is a combination of minithoracotomy and videothoracoscopic technique (video telescope and endoscopic instruments). It enables resection of some small, peripherally localized abscesses. DECORTICATION + LUNG RESECTION A method used for the treatment of lung abscesses accompanied by pleural empyema. Decortication consists in the removal of a thick fibrinopurulent coat from the lung surface. Besides it the part of a pleural empyema capsule that covers the internal surface of the chest wall is also resected along with the parietal pleura. The procedure is completed by resection of pulmonary parenchyma with abscess. LUNG RESECTION + IRRIGATING DRAINAGE A procedure used in the cases of lung abscess coexisting with acute pleural empyema. When pulmonary parenchyma with lung abscess is resected two or three tubes are introduced into the pleural cavity and continuous irrigating drainage with antibiotic or antiseptic solution is carried out.
PLEURAL EMPYEMA (empyema pleurae) Pleural empyema is a kind of exudative pleuritis caused by Microorganisms (bacteria, fungi, some protozoa) that infected the pleural cavity. Inflammation of organs or anatomical structures localized within the chest and out of its anatomical borders can caused a retention of effusion in the pleural space (hydrothorax) A reason for pleural effusions are also systemic diseases. Initially sterile exudate can be resorbed by the pleura if a primary disease is treated effectively. The infection of the exudate causes its transformation into purulent liquid that fills the pleural cavity and forms pleural empyema (empyema pleurae).
PLEURAL EMPYEMA (empyema pleurae) Pleural effusion infected by: bacteria, fungi, protozoa.
PLEURAL EMPYEMA (empyema pleurae) CLINICAL CONDITIONS CAUSING LIQUID RETENTION IN THE PLEURAL CAVITY : TRANSUDATE - circulatory insufficiency, hepatic cirrhosis, nephrotic syndrome, superior vena caval obstruction. EXUDATE – malignancy, infection, pulmonary embolism, esophageal perforation, pancreatitis, sarcoidosis, systemic diseases. LYMPH (chylothorax) – trauma, surgery, malignancy, subclavian vein thrombosis. BLOOD (haemothorax) - trauma, malignancy In a case when a liquid collected in the pleural space becomes infected by virulent microorganisms it transforms into pus. Pleural empyema can develop in any individual but it seems to be more frequent in younger people in whom immune system is weakened.
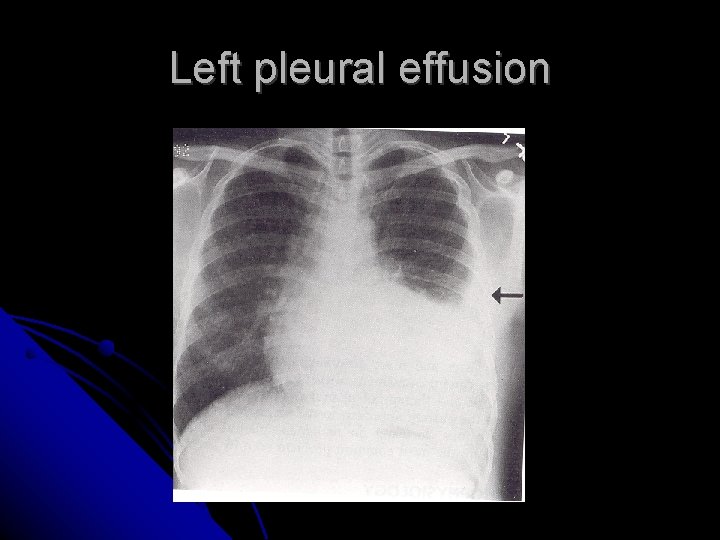
Left pleural effusion
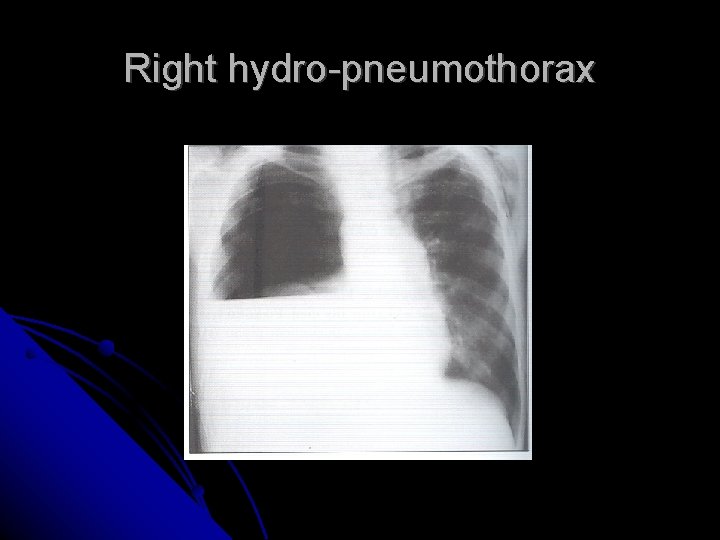
Right hydro-pneumothorax
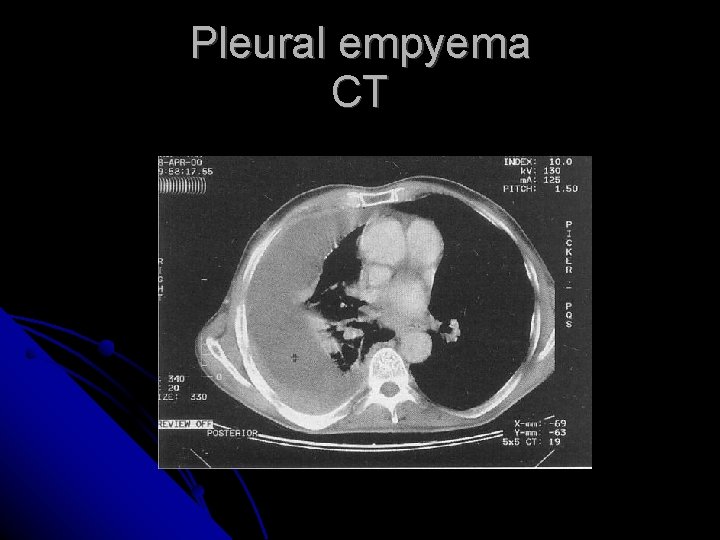
Pleural empyema CT
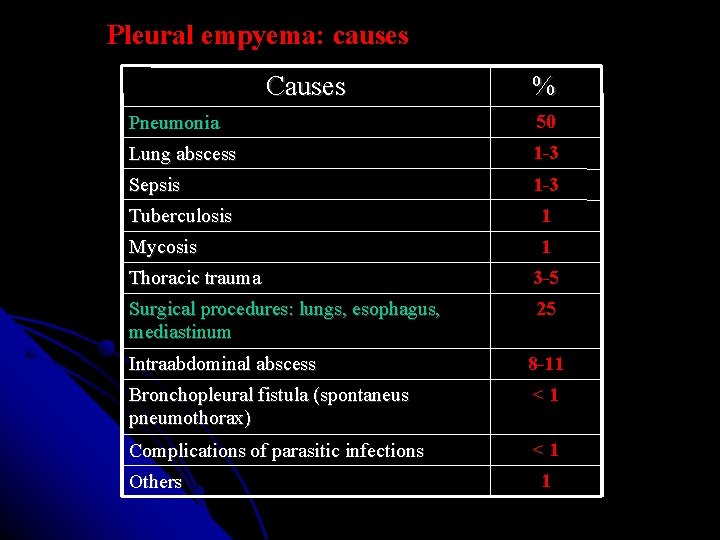
Pleural empyema: causes Causes % Pneumonia 50 Lung abscess 1 -3 Sepsis 1 -3 Tuberculosis 1 Mycosis 1 Thoracic trauma 3 -5 Surgical procedures: lungs, esophagus, mediastinum 25 Intraabdominal abscess 8 -11 Bronchopleural fistula (spontaneus pneumothorax) <1 Complications of parasitic infections <1 Others 1
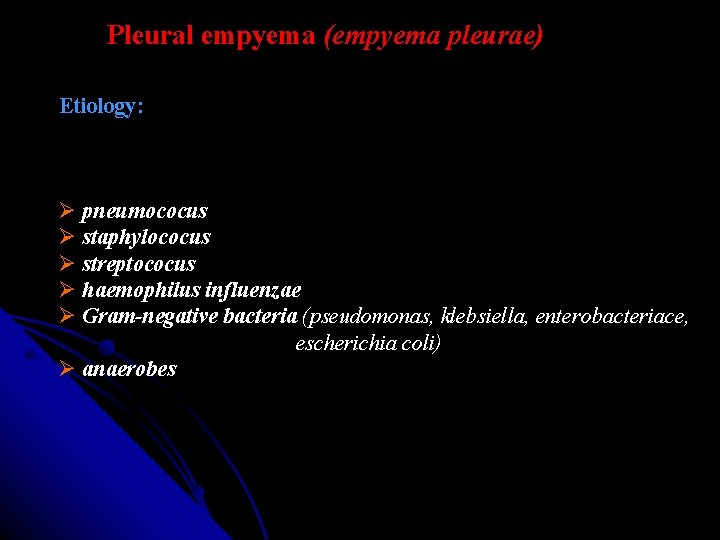
Pleural empyema (empyema pleurae) Etiology: pneumococus staphylococus streptococus haemophilus influenzae Gram-negative bacteria (pseudomonas, klebsiella, enterobacteriace, escherichia coli) anaerobes
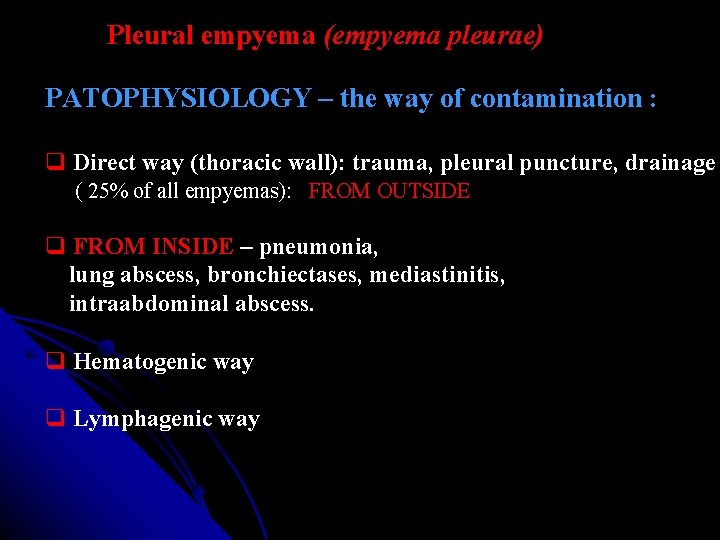
Pleural empyema (empyema pleurae) PATOPHYSIOLOGY – the way of contamination : Direct way (thoracic wall): trauma, pleural puncture, drainage ( 25% of all empyemas): FROM OUTSIDE FROM INSIDE – pneumonia, lung abscess, bronchiectases, mediastinitis, intraabdominal abscess. Hematogenic way Lymphagenic way
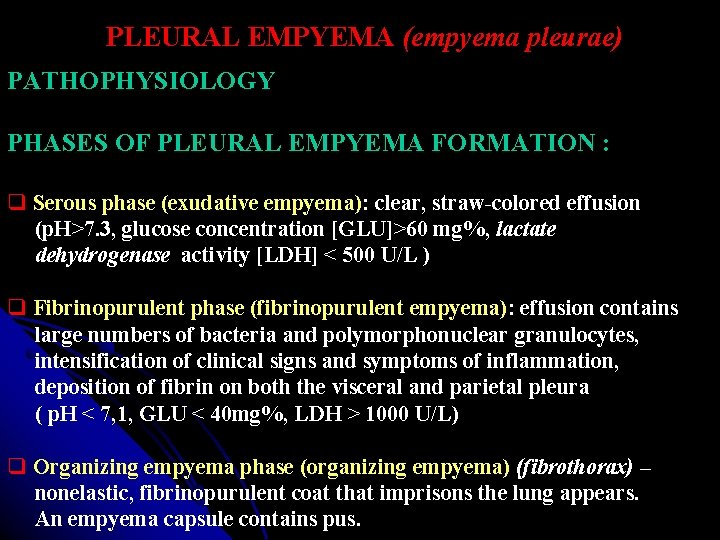
PLEURAL EMPYEMA (empyema pleurae) PATHOPHYSIOLOGY PHASES OF PLEURAL EMPYEMA FORMATION : Serous phase (exudative empyema): clear, straw-colored effusion (p. H>7. 3, glucose concentration [GLU]>60 mg%, lactate dehydrogenase activity [LDH] < 500 U/L ) Fibrinopurulent phase (fibrinopurulent empyema): effusion contains large numbers of bacteria and polymorphonuclear granulocytes, intensification of clinical signs and symptoms of inflammation, deposition of fibrin on both the visceral and parietal pleura ( p. H < 7, 1, GLU < 40 mg%, LDH > 1000 U/L) Organizing empyema phase (organizing empyema) (fibrothorax) – nonelastic, fibrinopurulent coat that imprisons the lung appears. An empyema capsule contains pus.
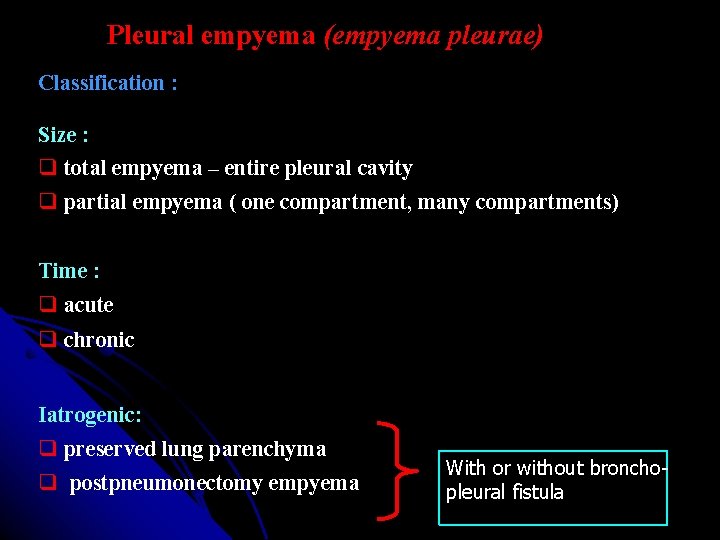
Pleural empyema (empyema pleurae) Classification : Size : total empyema – entire pleural cavity partial empyema ( one compartment, many compartments) Time : acute chronic Iatrogenic: preserved lung parenchyma postpneumonectomy empyema With or without bronchopleural fistula
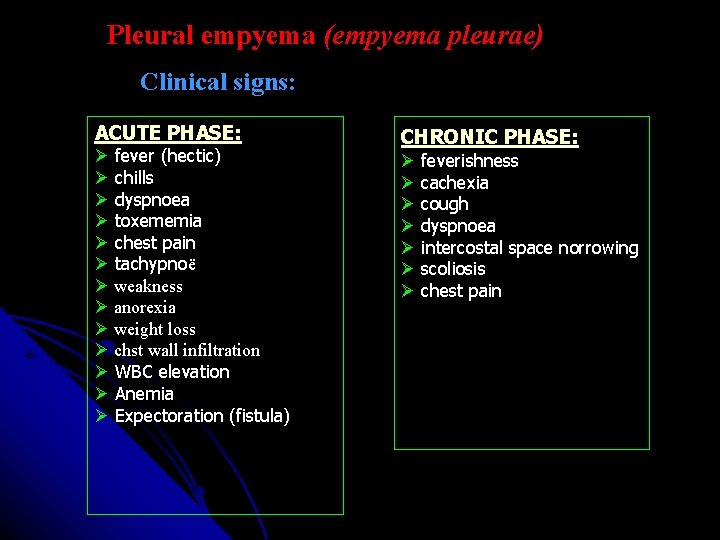
Pleural empyema (empyema pleurae) Clinical signs: ACUTE PHASE: fever (hectic) chills dyspnoea toxememia chest pain tachypnoë weakness anorexia weight loss chst wall infiltration WBC elevation Anemia Expectoration (fistula) CHRONIC PHASE: feverishness cachexia cough dyspnoea intercostal space norrowing scoliosis chest pain
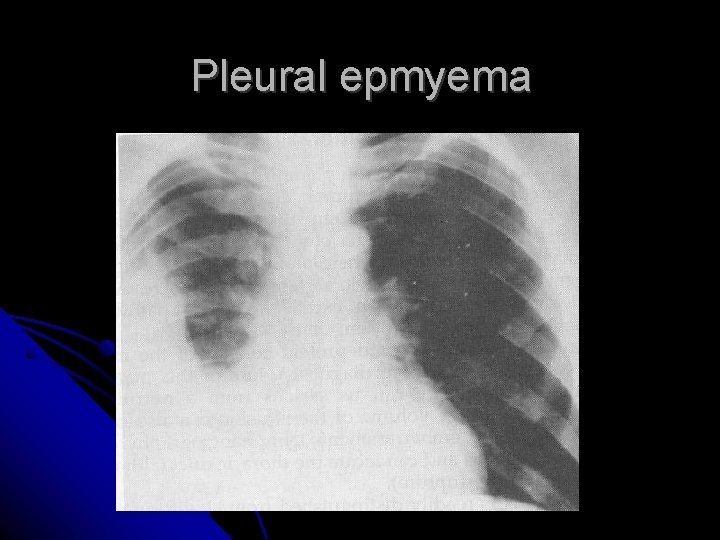
Pleural epmyema
Pleural empyema (empyema pleurae) TREATMENT : ACUTE PHASE: Antibiotics (IV), Pleural pucture, Pleural drainage, Antibiotics (inside the pleura).
PLEURAL EMPYEMA (empyema pleurae) TREATMENT : CHRONIC PHASE: Pleural drainage + antibiotics to the pleural cavity. Drainage flow Open drainage (chest window) after 14 days. Fibrinolitics ( streptokinase, streptodornase): local PE. VATS (debridement).
PLEURAL EMPYEMA (empyema pleurae) SURGICAL TREATMENT: Thoracotomy and decortication of the lung - Decortication of the lung + lung resection Thoracostomy (fenestration) – chest window.
PLEURAL EMPYEMA (empyema pleurae) COMPLICATIONS : atelectasis and respiratory insufficiency broncho-pleural fistula pleuro-cutaneous fistula esophageo-pleural fistula sepsis peritonitis metastatic abscesses in liver, kidneys, spleen and other organs. chest wall inflamatory infiltration progressing respiratory insufficiency
PLEURAL EMPYEMA (empyema pleurae) PROGNOSIS : Mortality rate in acute phase: app. 1 -19%. (sepsis). Chronic phase : Mortality rate in patients with diabetes, cancer, alcohol abuse is app. 40%. (respiratory insufficiency, MOF).
Bronchiectasis Definition: abnormal permanent dilatation of subsegmental airways. The first description: Laënnec in 1819. Term bronchiectasis: Hasse in 1846. The first successful surgical procedure for bronchiectasis (partial resection of the lung lobe)Krause 1898.
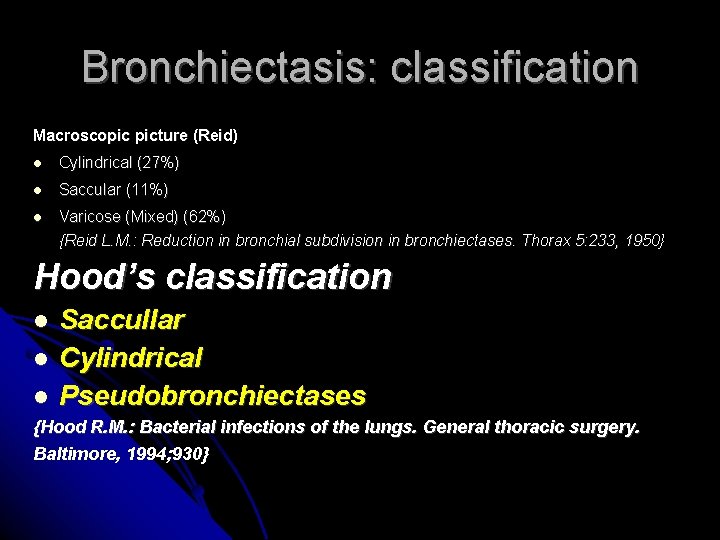
Bronchiectasis: classification Macroscopic picture (Reid) Cylindrical (27%) Saccular (11%) Varicose (Mixed) (62%) {Reid L. M. : Reduction in bronchial subdivision in bronchiectases. Thorax 5: 233, 1950} Hood’s classification Saccullar Cylindrical Pseudobronchiectases {Hood R. M. : Bacterial infections of the lungs. General thoracic surgery. Baltimore, 1994; 930}
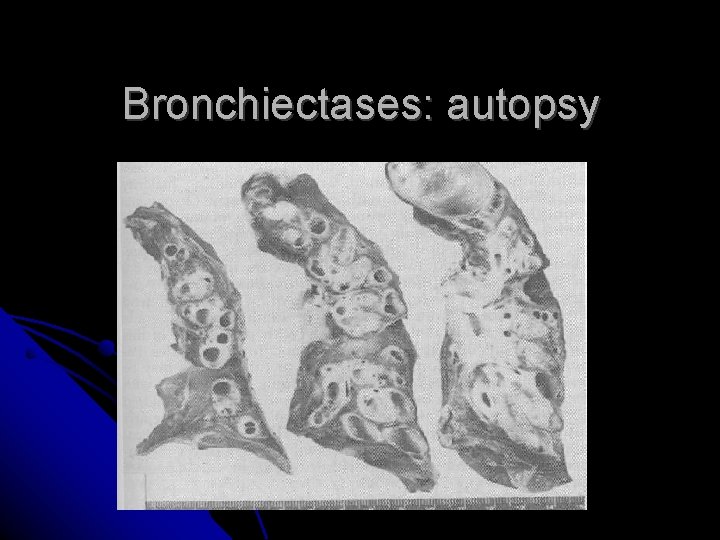
Bronchiectases: autopsy
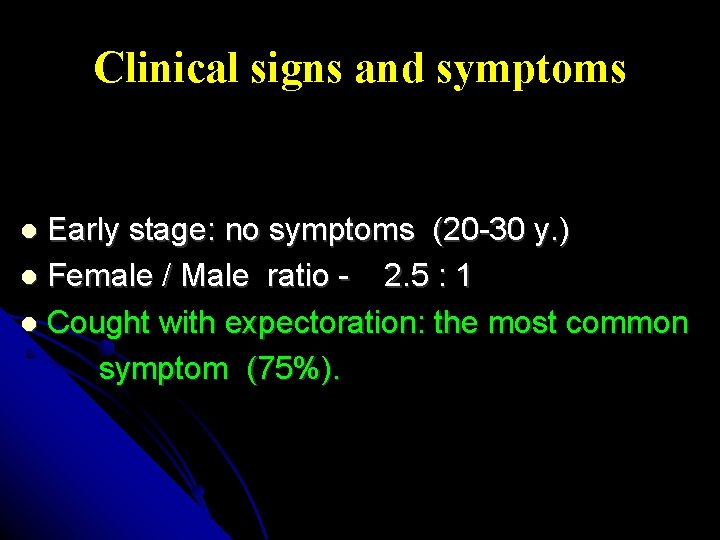
Clinical signs and symptoms Early stage: no symptoms (20 -30 y. ) Female / Male ratio - 2. 5 : 1 Cought with expectoration: the most common symptom (75%).
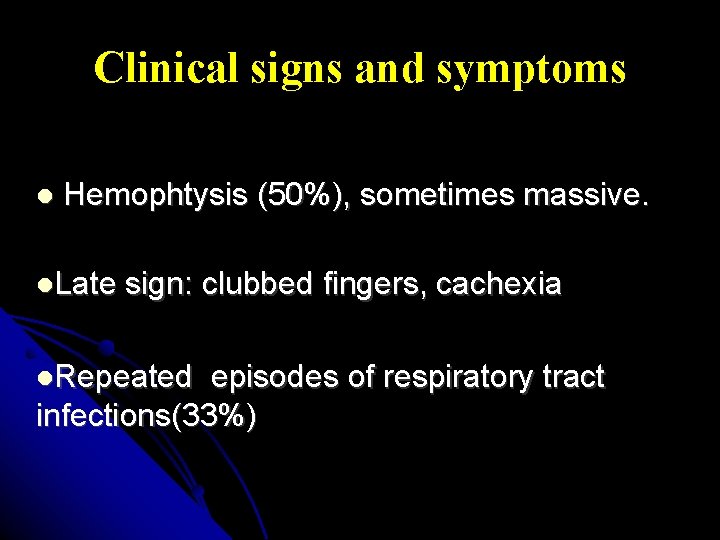
Clinical signs and symptoms Hemophtysis (50%), sometimes massive. Late sign: clubbed fingers, cachexia Repeated episodes of respiratory tract infections(33%)
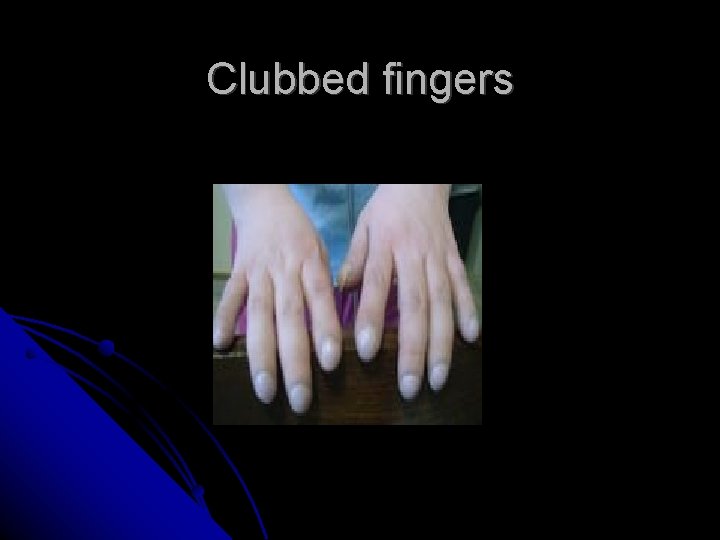
Clubbed fingers
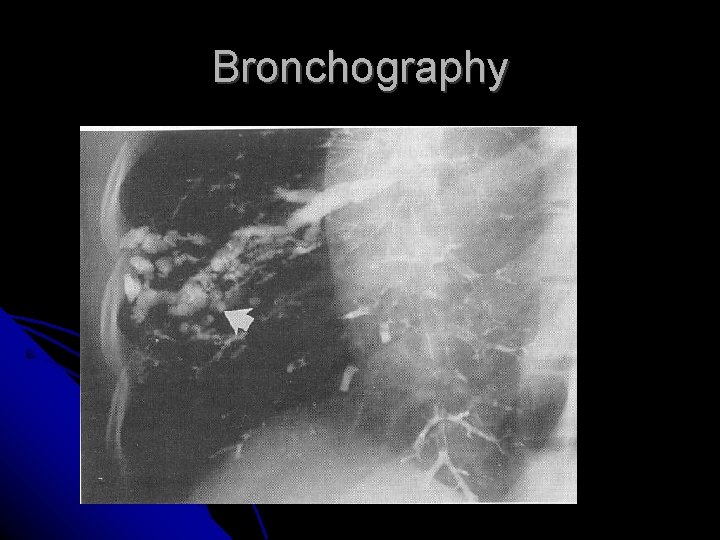
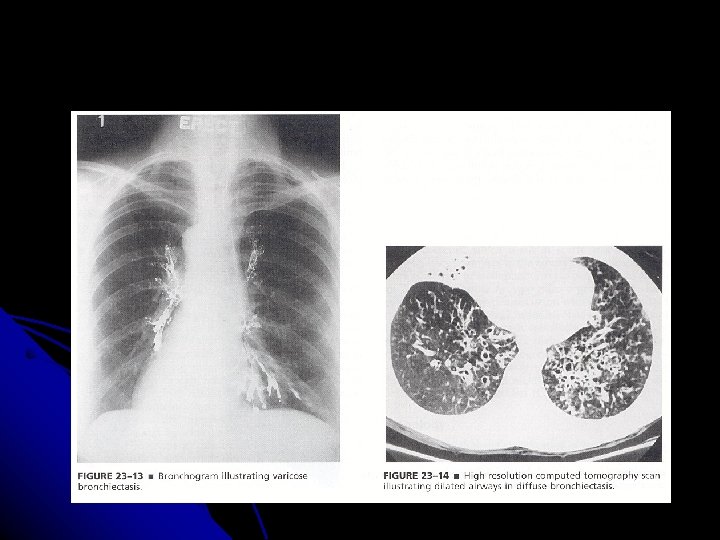
Bronchography
Diagnosis CT: the gold standard
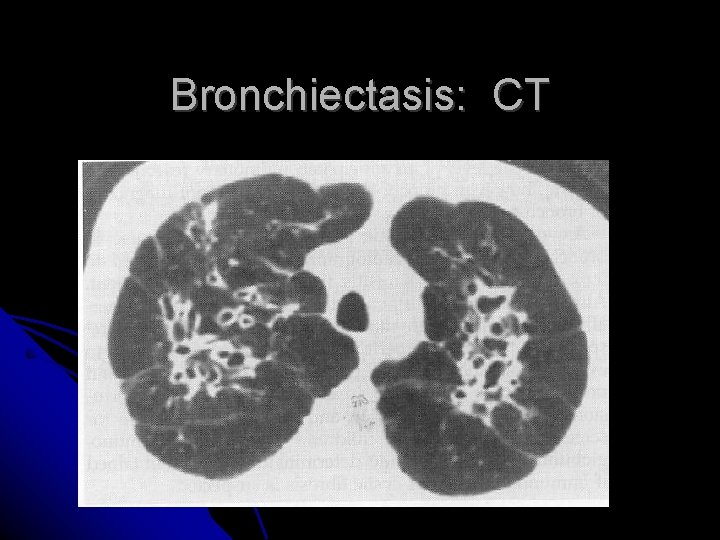
Bronchiectasis: CT

Bronchiectasis: treatment Conservative: FIRST LINE TREATMENT!!! - Antibiotics - Mucolitic agents - Postural drainage - Breathing exercises
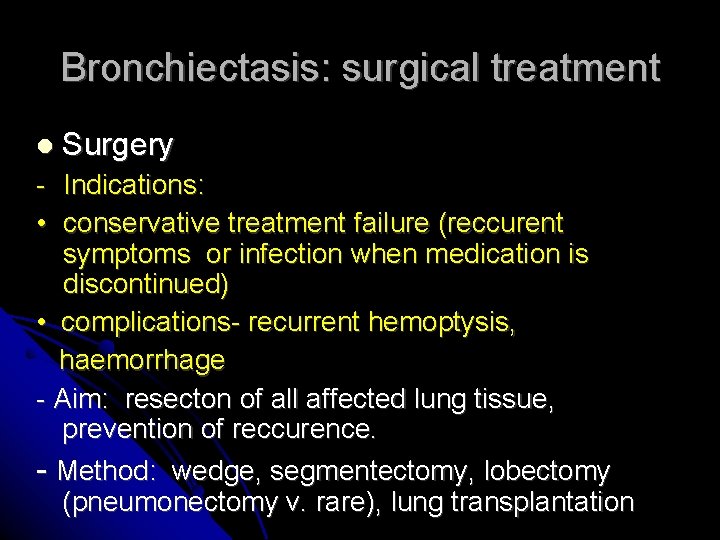
Bronchiectasis: surgical treatment Surgery - Indications: • conservative treatment failure (reccurent symptoms or infection when medication is discontinued) • complications- recurrent hemoptysis, haemorrhage - Aim: resecton of all affected lung tissue, prevention of reccurence. - Method: wedge, segmentectomy, lobectomy (pneumonectomy v. rare), lung transplantation
Mycobacterium Tuberculosis
1882 ROBERT KOCH
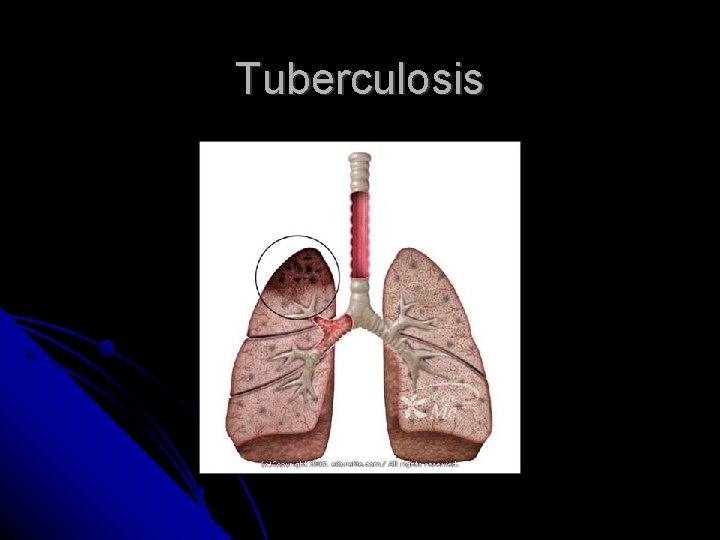
Tuberculosis
TBC infection
Clinical picture Non-characteristic Purulent cough Malaise Weight loss Haemoptysis Fever Night sweats very often
Diagnosis Tuberculin skin testing Sputum smear (Ziehl- Neelsen) Sputum (bronchoalveolar lavage) cultures X-ray examination Nucleic acid assay (NAA) PCR IFN-Ɣ
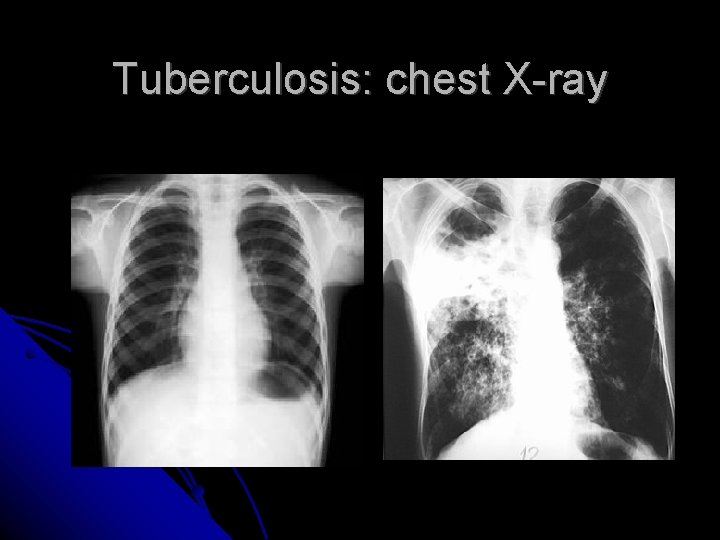
Tuberculosis: chest X-ray
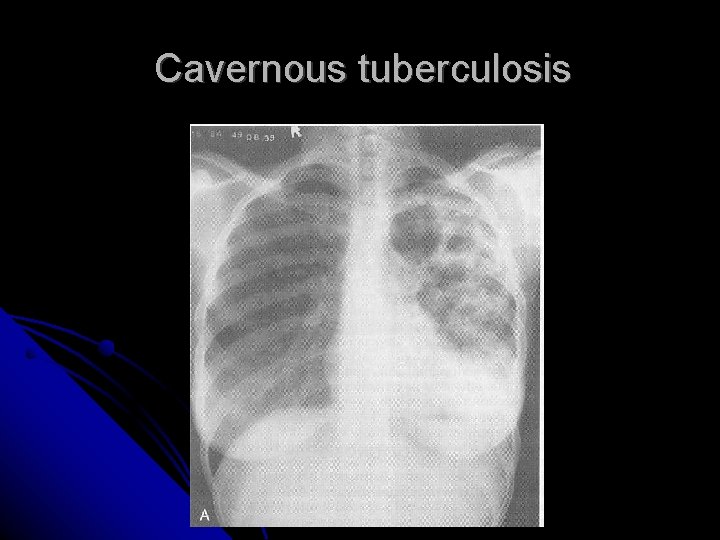
Cavernous tuberculosis
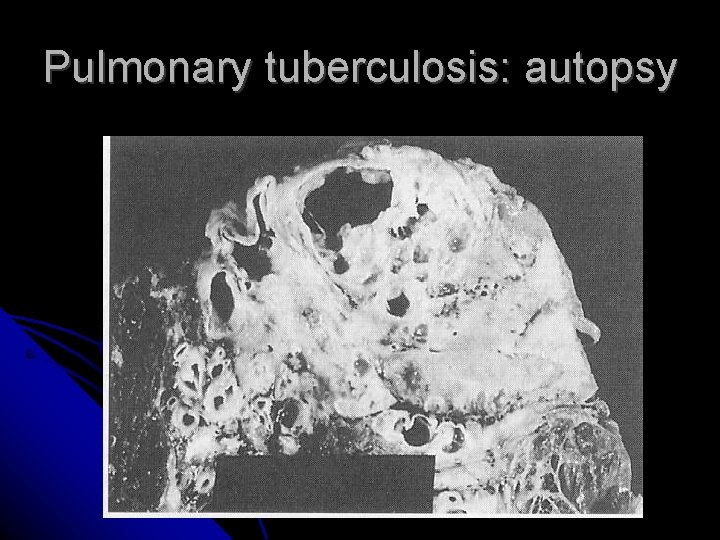
Pulmonary tuberculosis: autopsy
TREATMENT Conservative treatment with antitubercuolus drugs Surgical treatment approx. 2% of cases 2 million deaths annually worldwide
PHARMACOLOGY Isoniazid Rifampin Pyrazinamide Streptomicin Ethambutol Time: 6 -9 months Resistance for first line drugs (Isoniazid, Rifampin, Ethambutol) is a serious problem.
SURGICAL TREATMENT INDICATIONS UNEFFECTIVE PHARMACOLOGICAL TREATMENT FOR 12 MONTHS COMPLICATIONS OF TUBERCULOSIS
SURGICAL TREATMENT OF COMPLICATIONS ABSOLUTE INDICATIONS - Haemorrhage - Pleural empyema with bronchopleural fistula - Aspergilloma in posttuberculous cavity - Lymph node compression of the bronchi
SURGICAL TREATMENT OF COMPLICATIONS RELATIVE INDICATIONS - Posttuberculous cavity - Tuberculoma (carcinoma suspicion, potential source of tuberculosis reactivation) - Lung completely destroyed by tuberculosis
- Slides: 72