COMMON SURGICAL DISEASES OF THE STOMACH AND DUODENUM




- Slides: 71
COMMON SURGICAL DISEASES OF THE STOMACH AND DUODENUM • Dr. Babiker Ali Babiker Mohammed • MBBS, FRCSEd, Diploma in Laparoscopy • Consultant General & GI Surgeon • Prince Mohammed bin Abdulaziz Hospital
COMPONENTS • PEPTIC ULCER • GASTRIC TUMOURS • DUODENAL TUMOURS
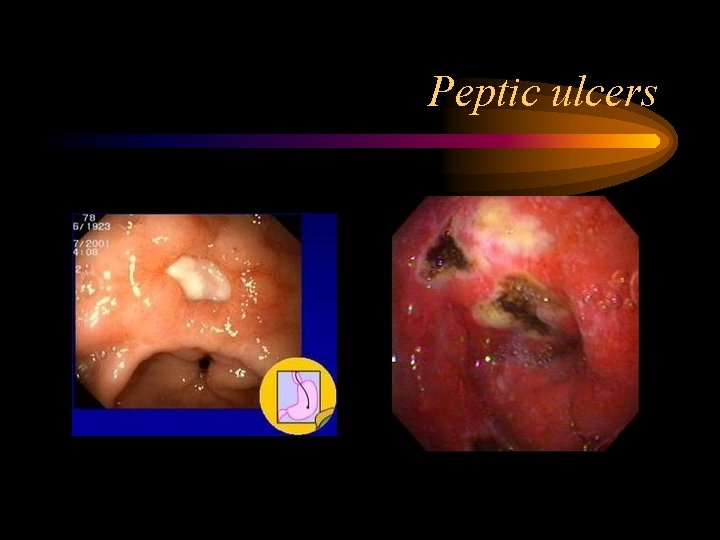
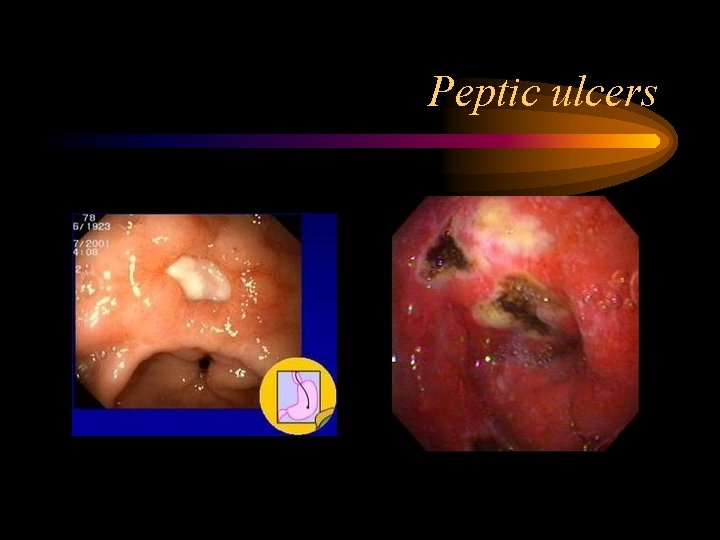
Peptic ulcers
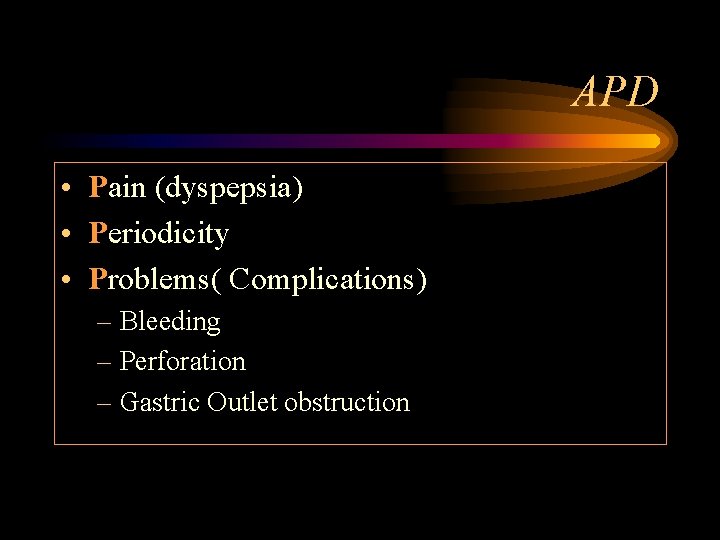
APD • Pain (dyspepsia) • Periodicity • Problems( Complications) – Bleeding – Perforation – Gastric Outlet obstruction
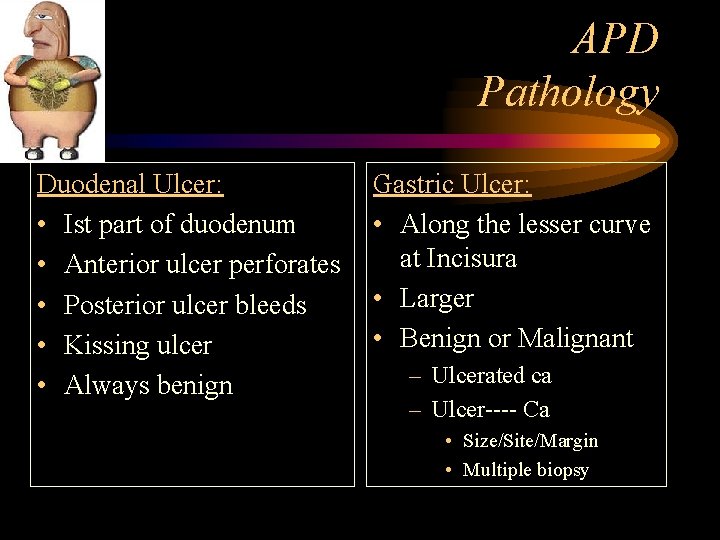
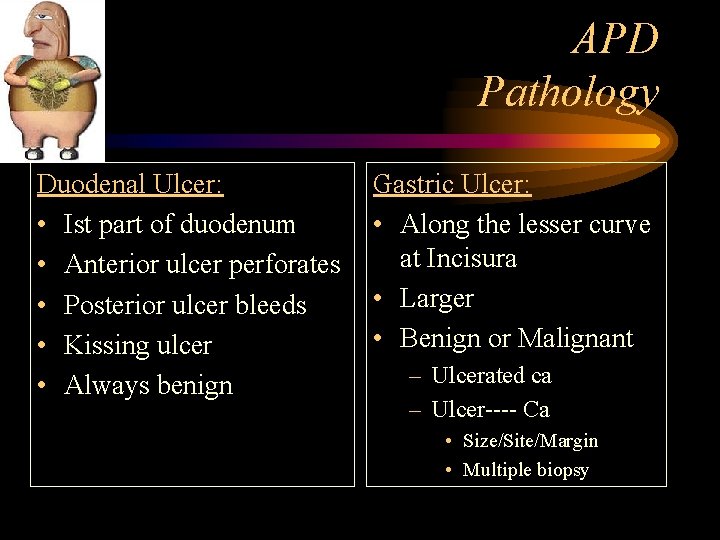
APD Pathology Duodenal Ulcer: • Ist part of duodenum • Anterior ulcer perforates • Posterior ulcer bleeds • Kissing ulcer • Always benign Gastric Ulcer: • Along the lesser curve at Incisura • Larger • Benign or Malignant – Ulcerated ca – Ulcer---- Ca • Size/Site/Margin • Multiple biopsy
Peptic ulcer – cause……………. .
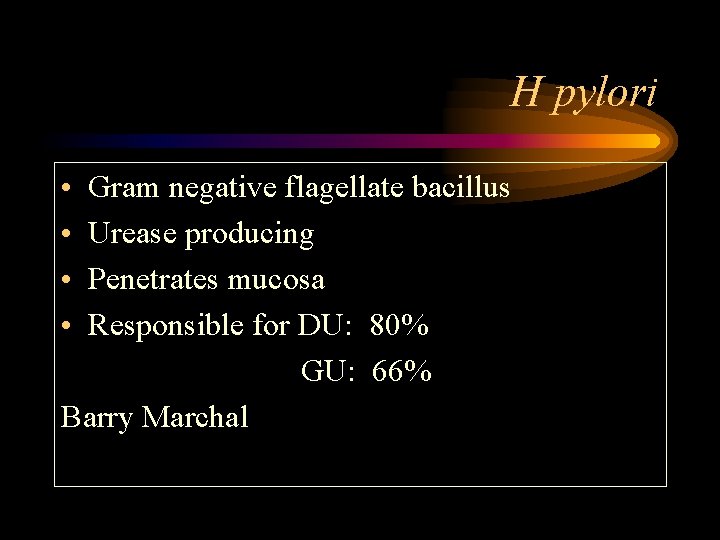
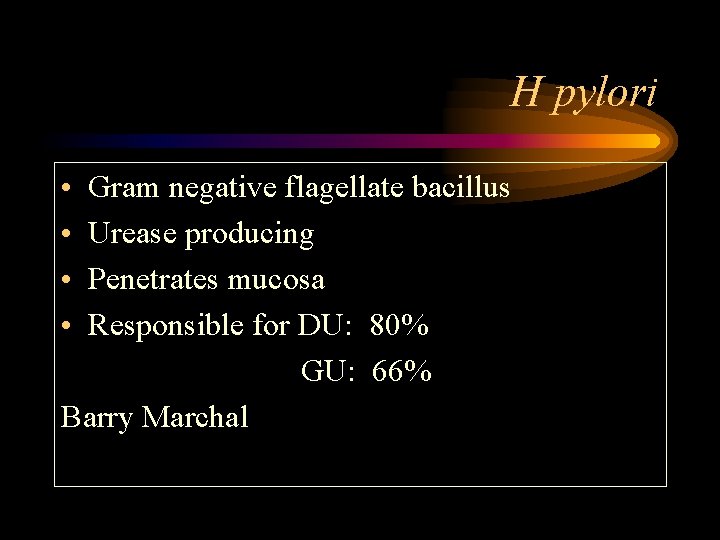
H pylori • • Gram negative flagellate bacillus Urease producing Penetrates mucosa Responsible for DU: 80% GU: 66% Barry Marchal
H pylori

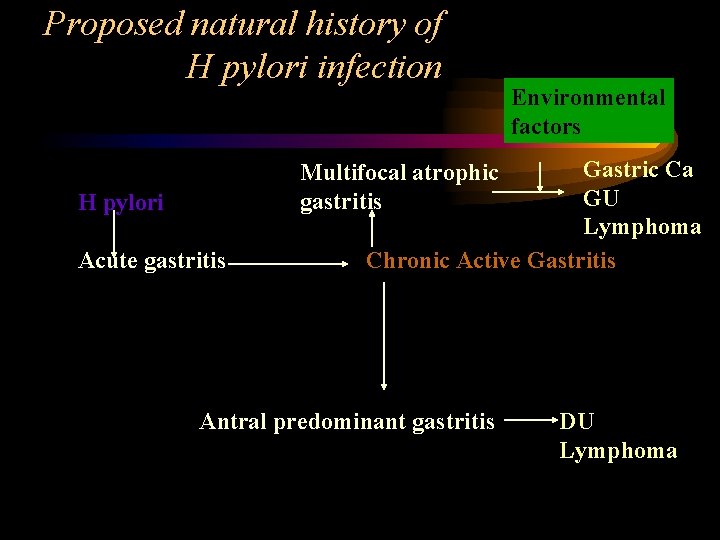
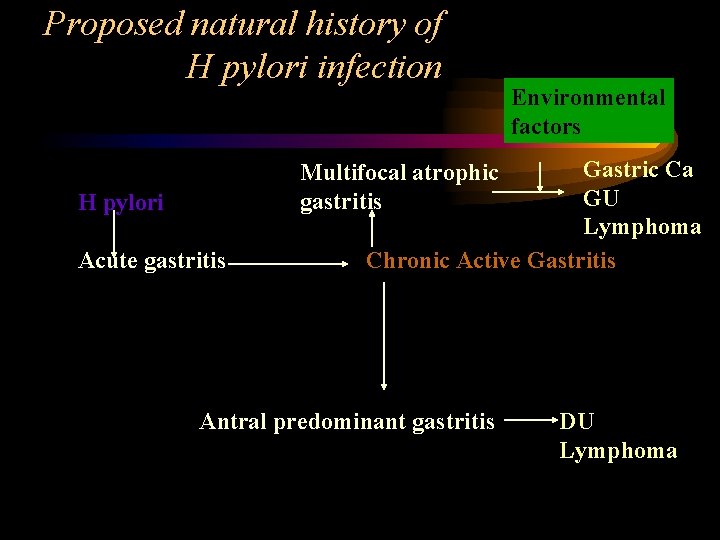
Proposed natural history of H pylori infection Environmental factors Gastric Ca GU Lymphoma Chronic Active Gastritis Multifocal atrophic gastritis H pylori Acute gastritis Antral predominant gastritis DU Lymphoma

• Haemotology • Biochemistry – Serology for H pylori/Urea Breath test • Radiology – Barium meal • Special – Endoscopy and biopsy – CLO test Investigations
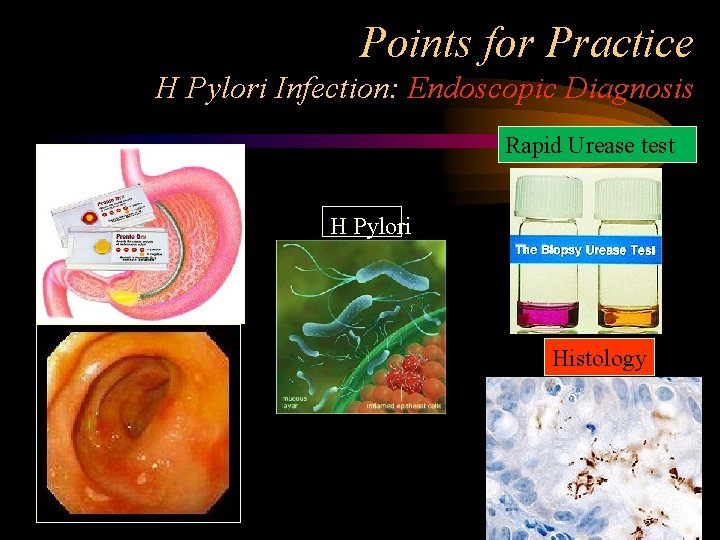
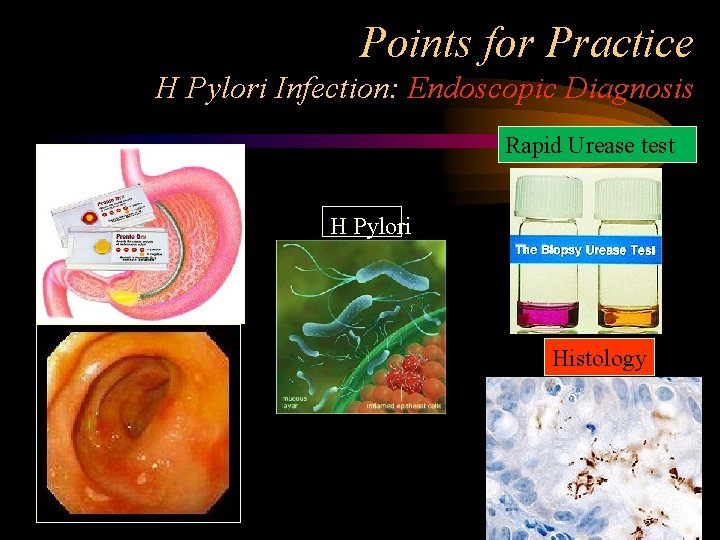
Points for Practice H Pylori Infection: Endoscopic Diagnosis Rapid Urease test H Pylori Histology
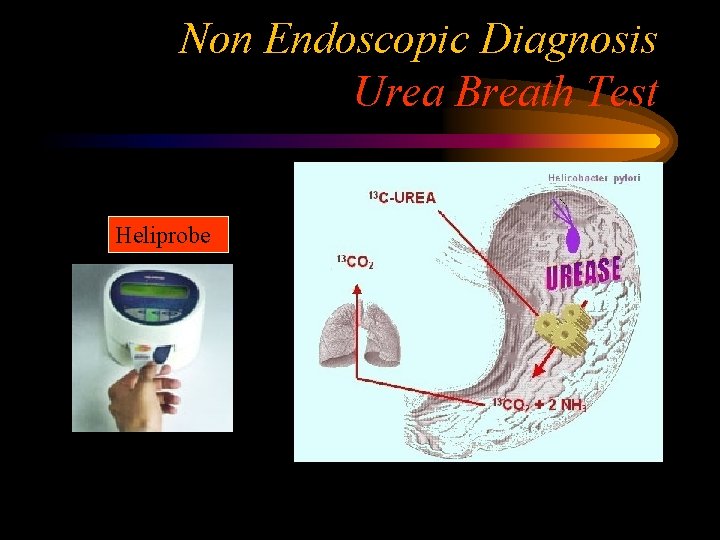
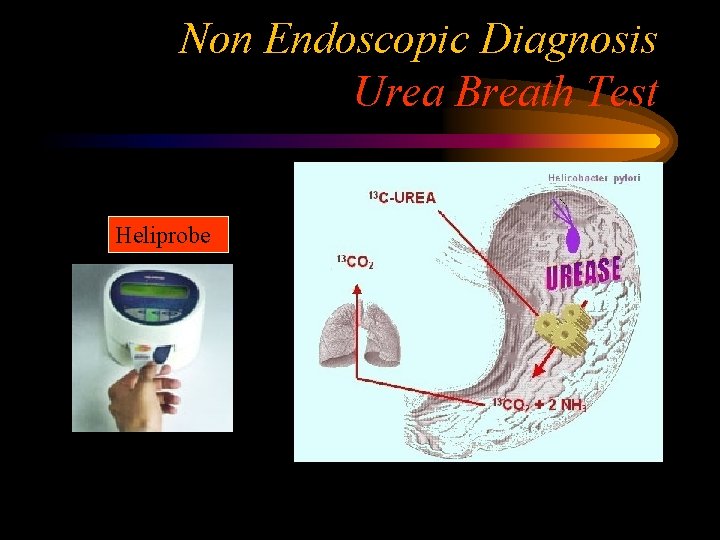
Non Endoscopic Diagnosis Urea Breath Test Heliprobe
Uncomplicated Duodenal ulcer Needs only Medical Managemen
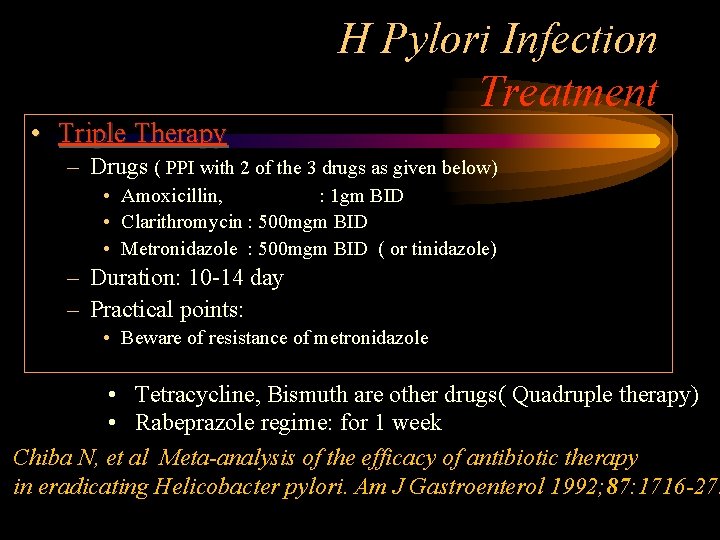
H Pylori Infection Treatment • Triple Therapy – Drugs ( PPI with 2 of the 3 drugs as given below) • Amoxicillin, : 1 gm BID • Clarithromycin : 500 mgm BID • Metronidazole : 500 mgm BID ( or tinidazole) – Duration: 10 -14 day – Practical points: • Beware of resistance of metronidazole • Tetracycline, Bismuth are other drugs( Quadruple therapy) • Rabeprazole regime: for 1 week Chiba N, et al Meta-analysis of the efficacy of antibiotic therapy in eradicating Helicobacter pylori. Am J Gastroenterol 1992; 87: 1716 -27.
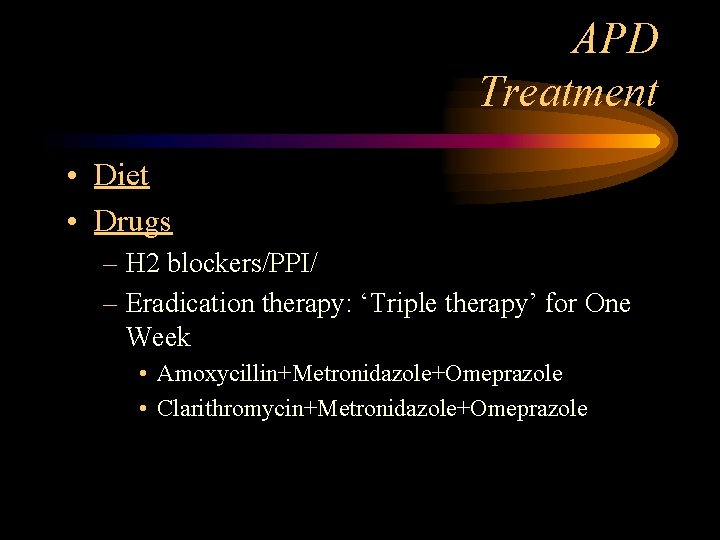
APD Treatment • Diet • Drugs – H 2 blockers/PPI/ – Eradication therapy: ‘Triple therapy’ for One Week • Amoxycillin+Metronidazole+Omeprazole • Clarithromycin+Metronidazole+Omeprazole
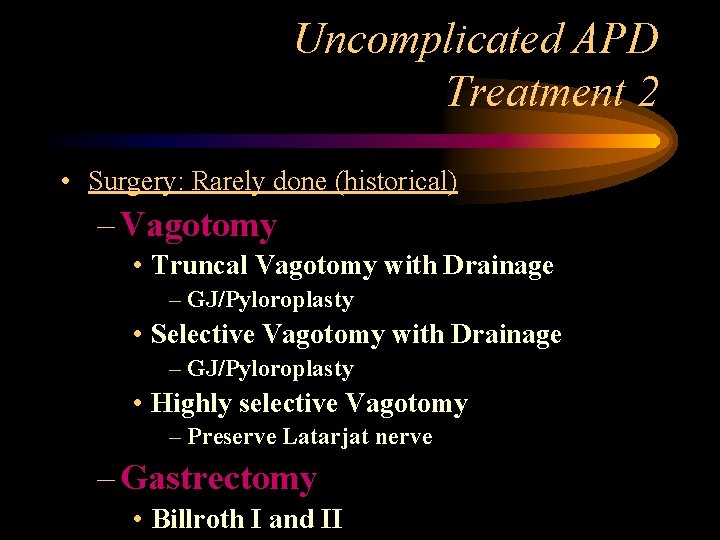
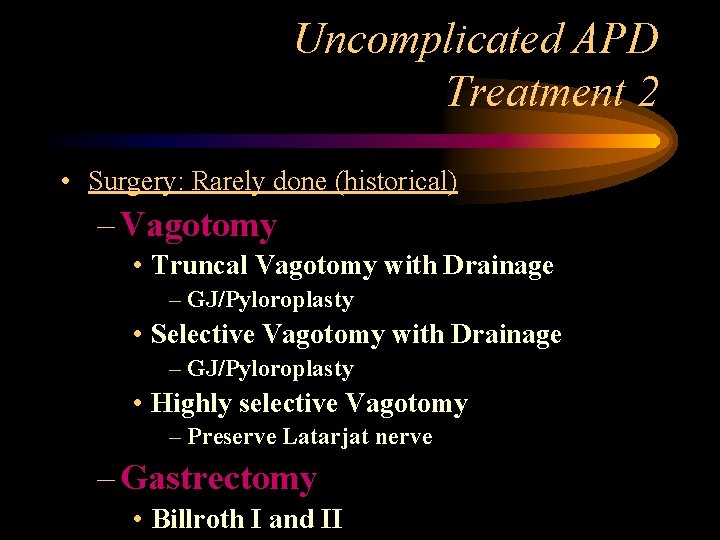
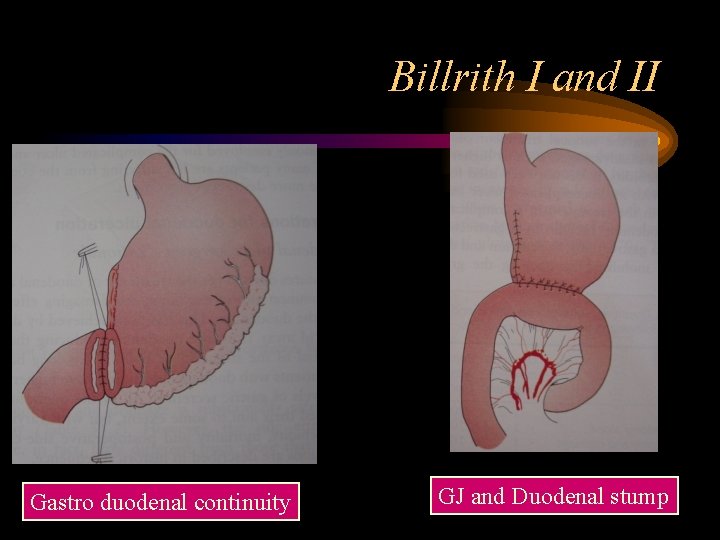
Uncomplicated APD Treatment 2 • Surgery: Rarely done (historical) – Vagotomy • Truncal Vagotomy with Drainage – GJ/Pyloroplasty • Selective Vagotomy with Drainage – GJ/Pyloroplasty • Highly selective Vagotomy – Preserve Latarjat nerve – Gastrectomy • Billroth I and II
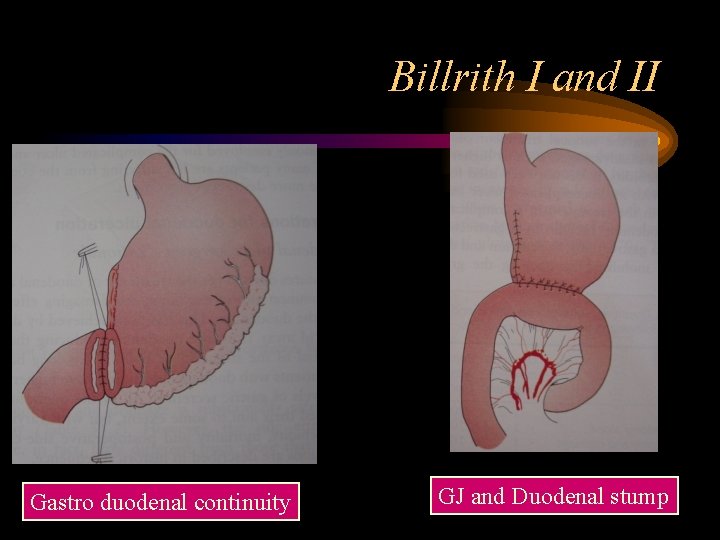
Billrith I and II Gastro duodenal continuity GJ and Duodenal stump
APD Complications • Bleeding • Perforation • Gastric Outlet obstruction

Minimally Invasive Surgery
Complicated Duodenal Ulcer Needs Minimal access/Surgical management -Bleeding DU -Stricture -Perforation
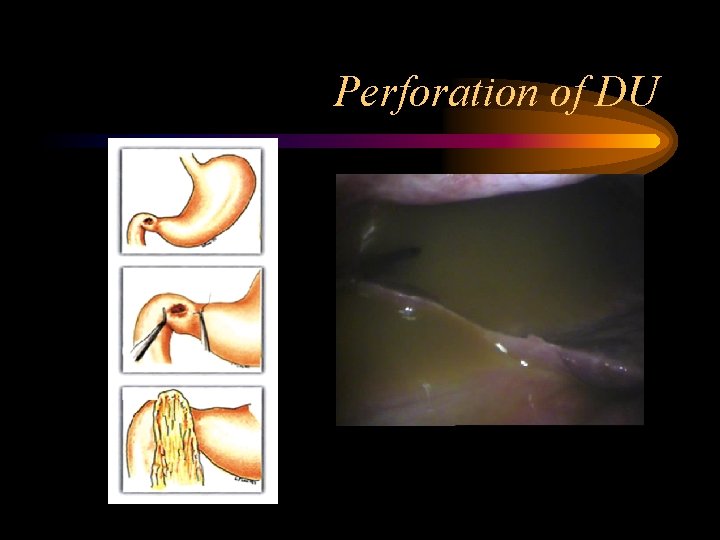
Perforated DU/GU • Etiology – refer • Pathology – refer • • Clinical Presentation Investigation DD Treatment
Perforated Ulcer • As ‘Acute Abdomen’ • Hypovolumic shock/ Board like abdomen • DD – Pancreatitis – Cholecystitis – AAA – Medical cause • MI/Pleurisy/Pulmonary embolism etc
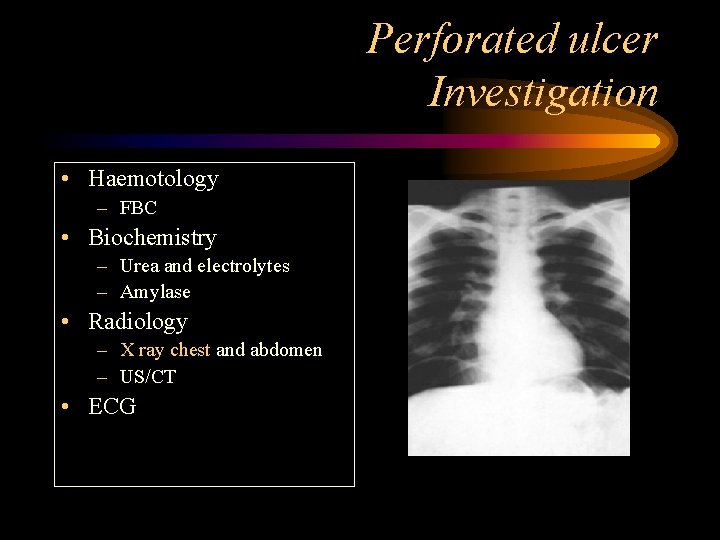
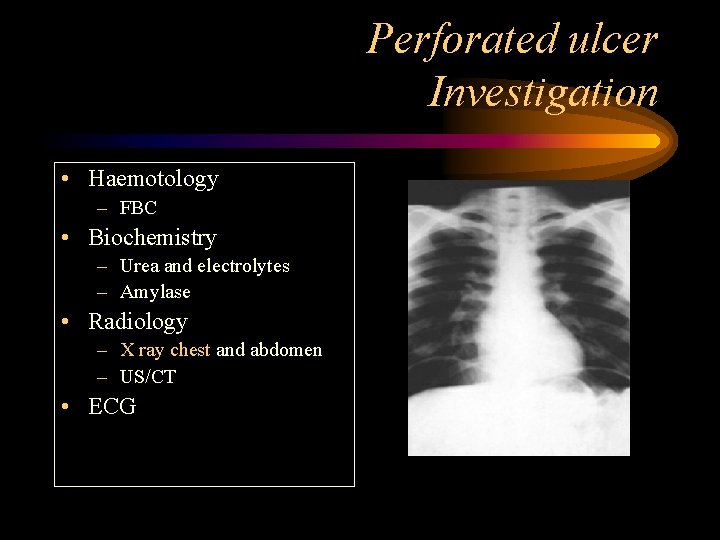
Perforated ulcer Investigation • Haemotology – FBC • Biochemistry – Urea and electrolytes – Amylase • Radiology – X ray chest and abdomen – US/CT • ECG
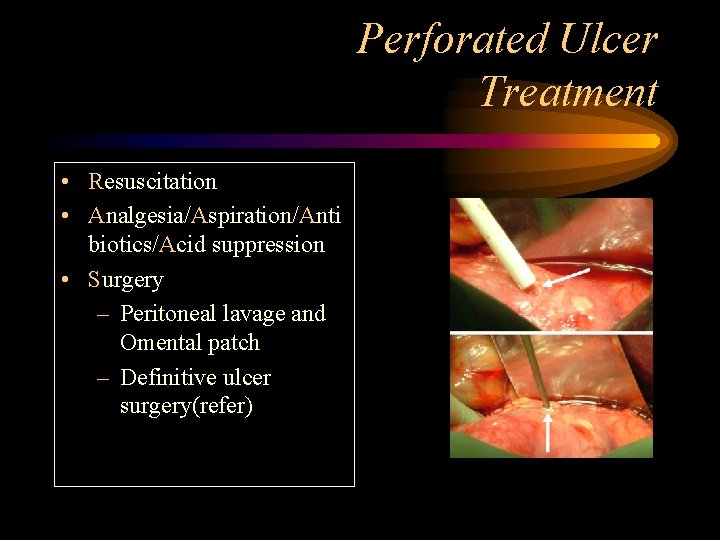
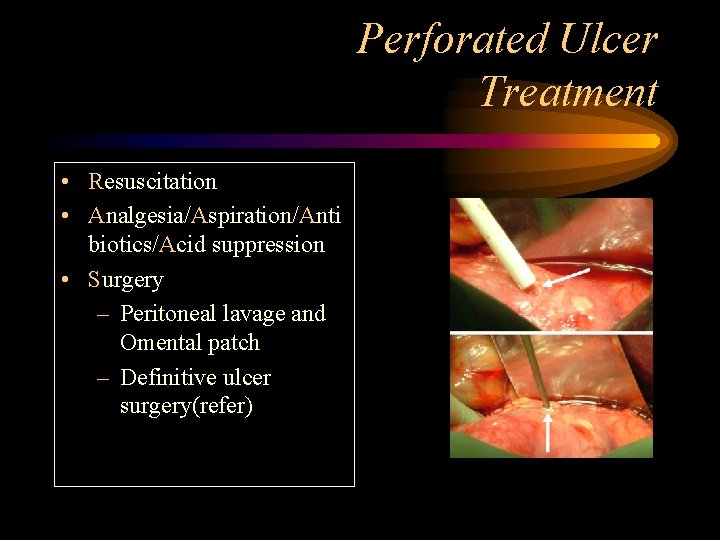
Perforated Ulcer Treatment • Resuscitation • Analgesia/Aspiration/Anti biotics/Acid suppression • Surgery – Peritoneal lavage and Omental patch – Definitive ulcer surgery(refer)
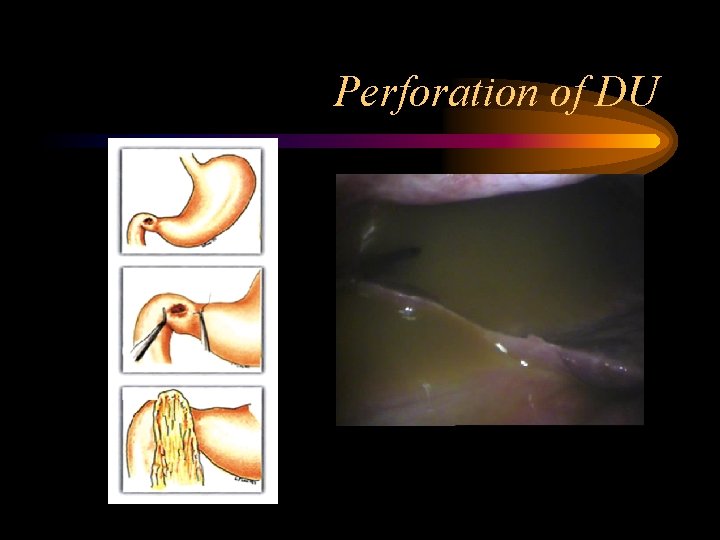
Perforation of DU
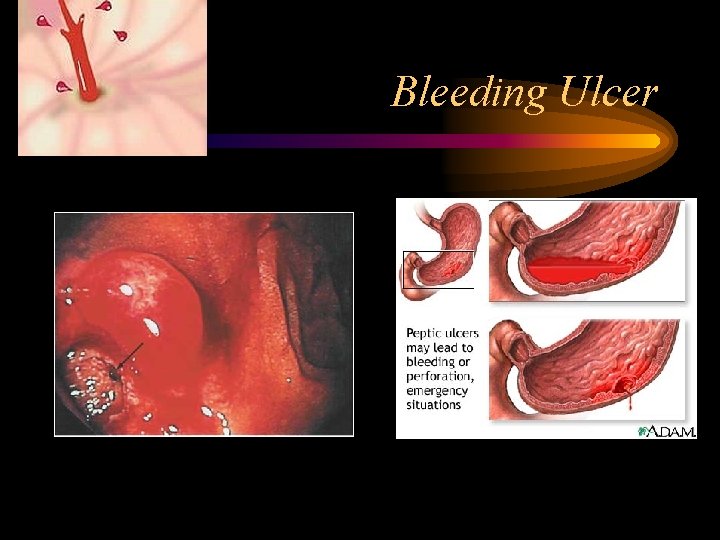
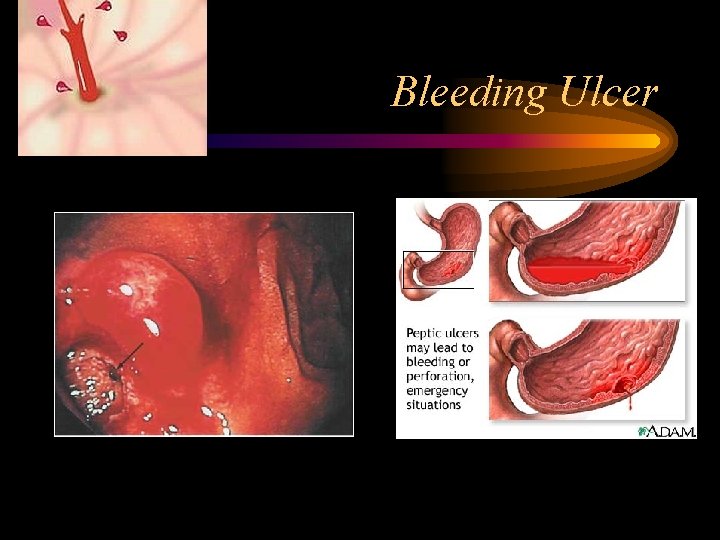
Bleeding Ulcer
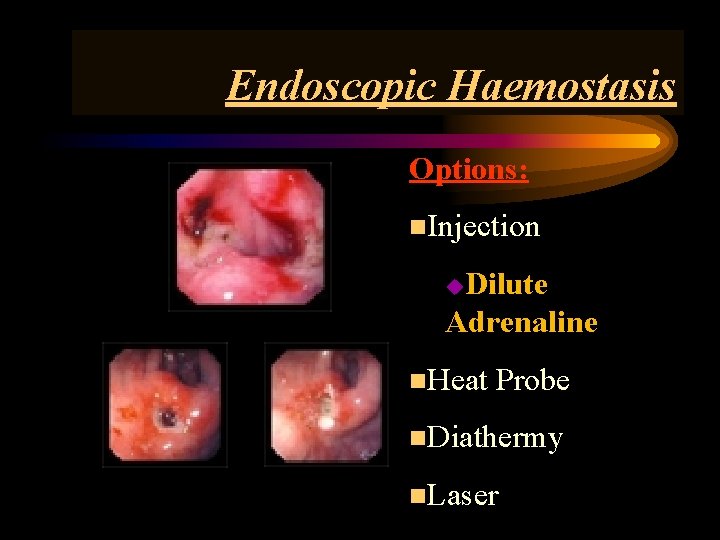
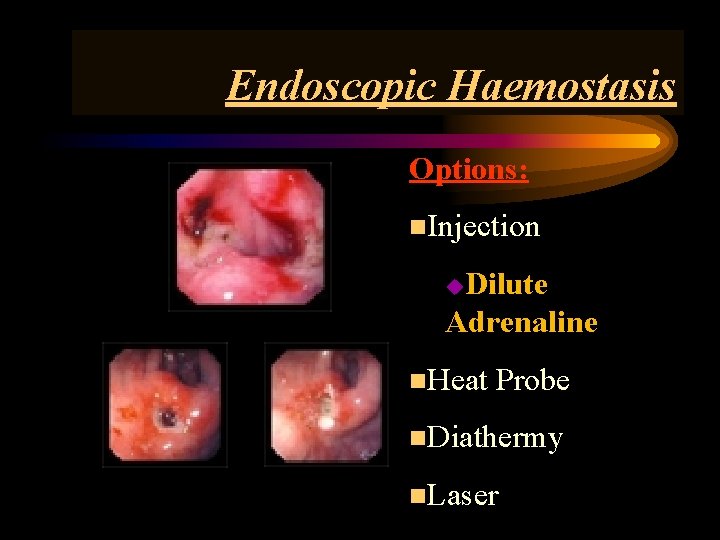
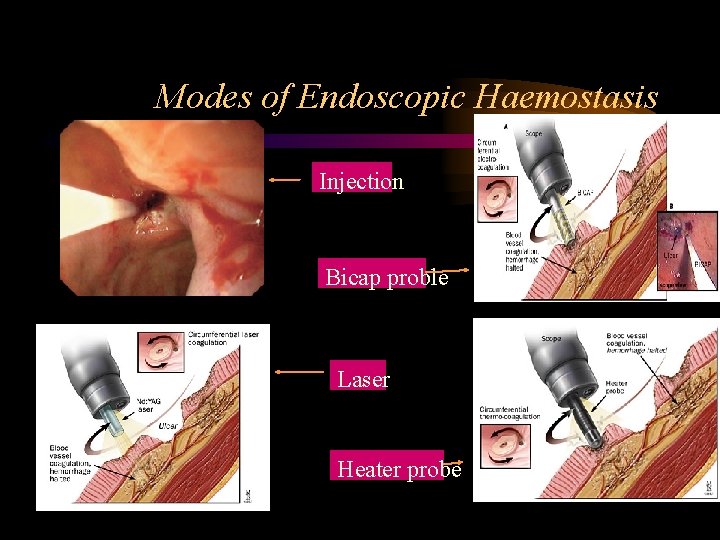
Endoscopic Haemostasis Options: n. Injection Dilute Adrenaline u n. Heat Probe n. Diathermy n. Laser
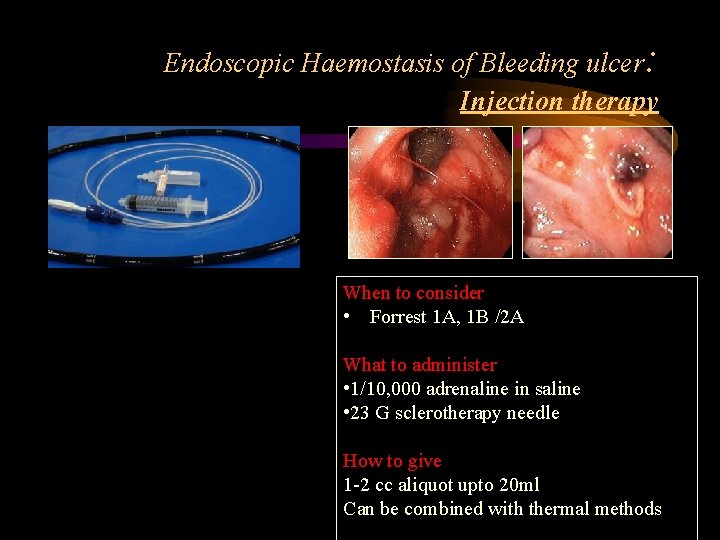
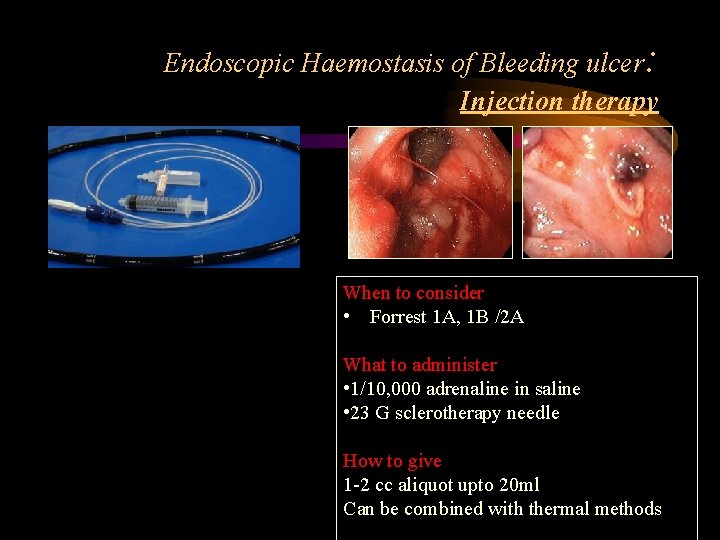
Endoscopic Haemostasis of Bleeding ulcer: Injection therapy When to consider • Forrest 1 A, 1 B /2 A What to administer • 1/10, 000 adrenaline in saline • 23 G sclerotherapy needle How to give 1 -2 cc aliquot upto 20 ml Can be combined with thermal methods
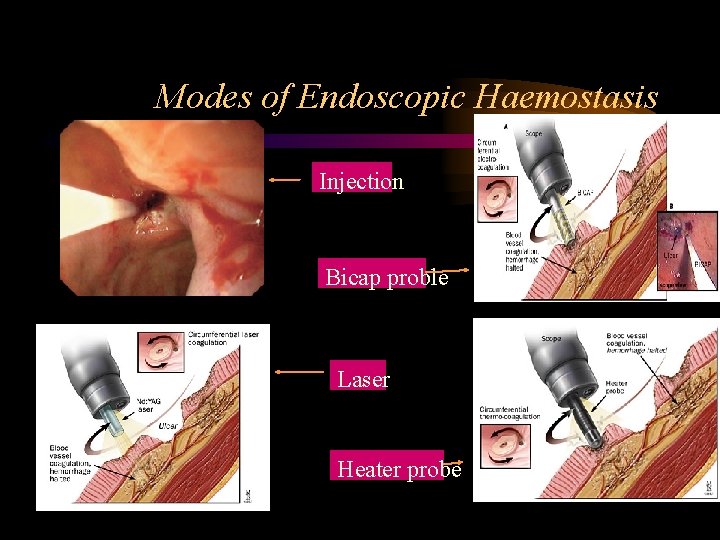
Modes of Endoscopic Haemostasis Injection Bicap proble Laser Heater probe
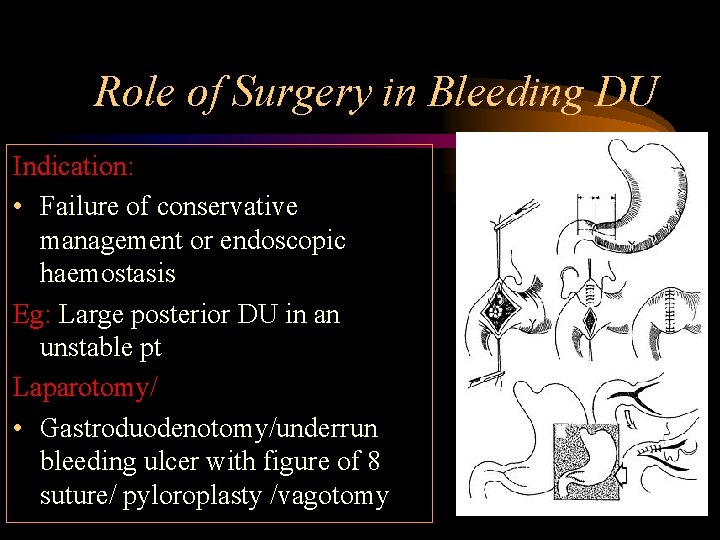
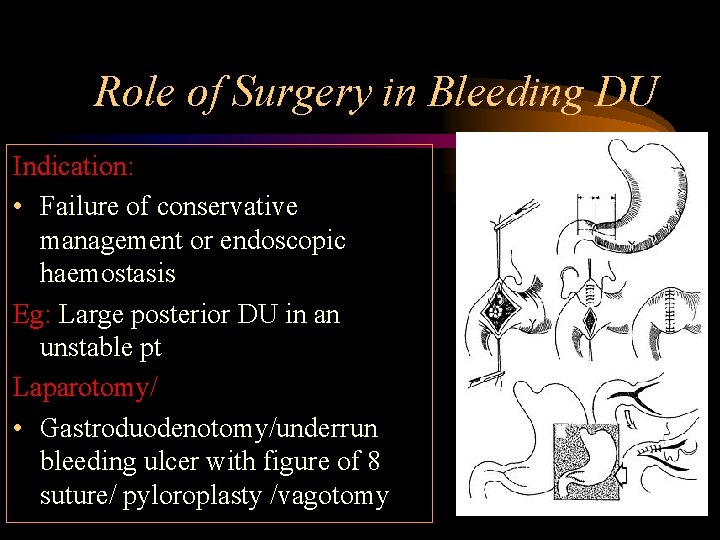
Role of Surgery in Bleeding DU Indication: • Failure of conservative management or endoscopic haemostasis Eg: Large posterior DU in an unstable pt Laparotomy/ • Gastroduodenotomy/underrun bleeding ulcer with figure of 8 suture/ pyloroplasty /vagotomy
Gastric Outlet Obstruction Etiology • Congenital • Inflammatory: Chronic DU • Neoplastic – Ca distal stomach – Ca head of pancreas
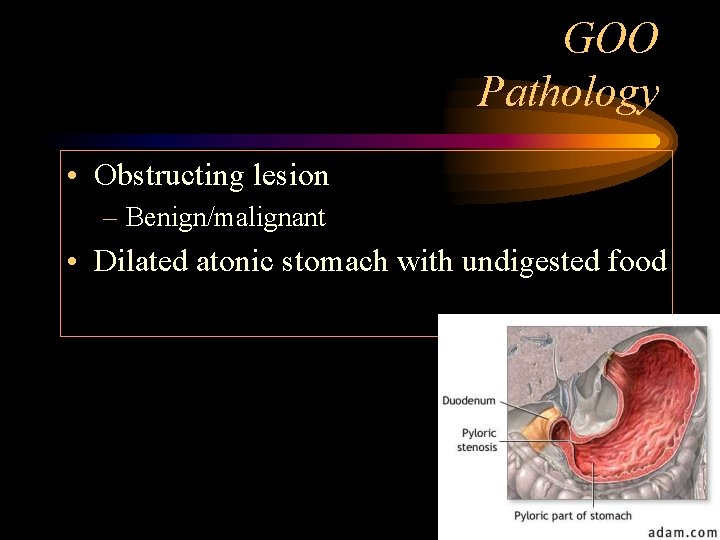
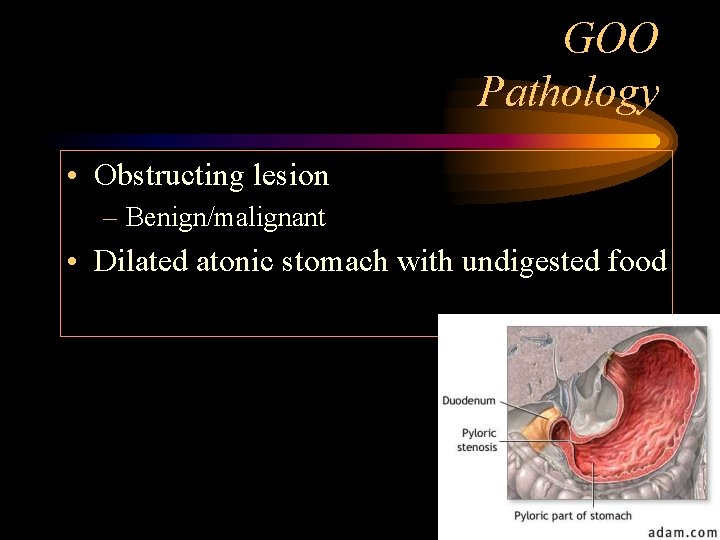
GOO Pathology • Obstructing lesion – Benign/malignant • Dilated atonic stomach with undigested food
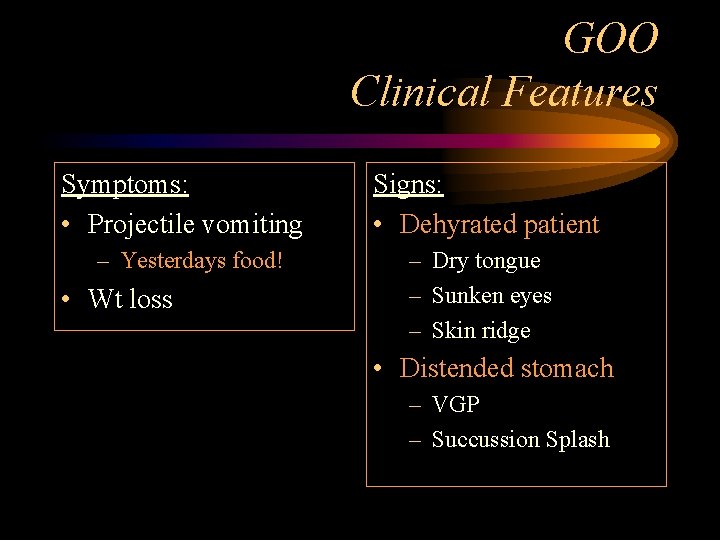
GOO Clinical Features Symptoms: • Projectile vomiting – Yesterdays food! • Wt loss Signs: • Dehyrated patient – Dry tongue – Sunken eyes – Skin ridge • Distended stomach – VGP – Succussion Splash
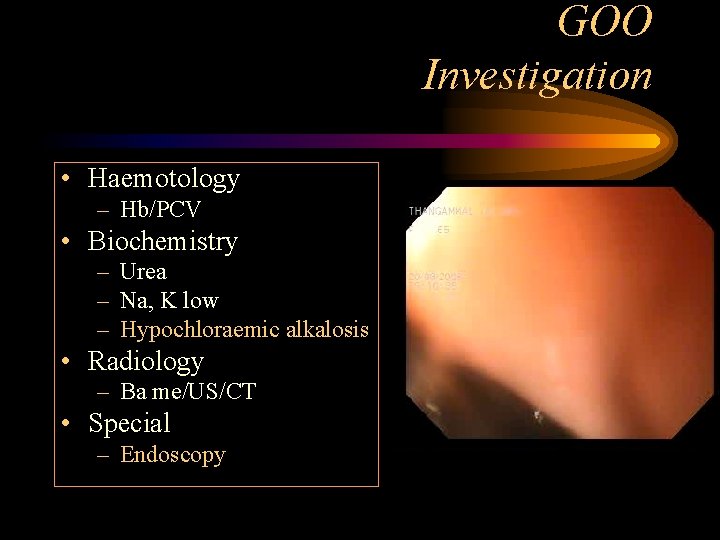
GOO Investigation • Haemotology – Hb/PCV • Biochemistry – Urea – Na, K low – Hypochloraemic alkalosis • Radiology – Ba me/US/CT • Special – Endoscopy
GOO Treatment • Rehydrate the dehydrated patient – Saline • Empty the distended stomach – Wide bore Ryle’s tube • Drain the obstructed stomach – Gastrojejunostomy
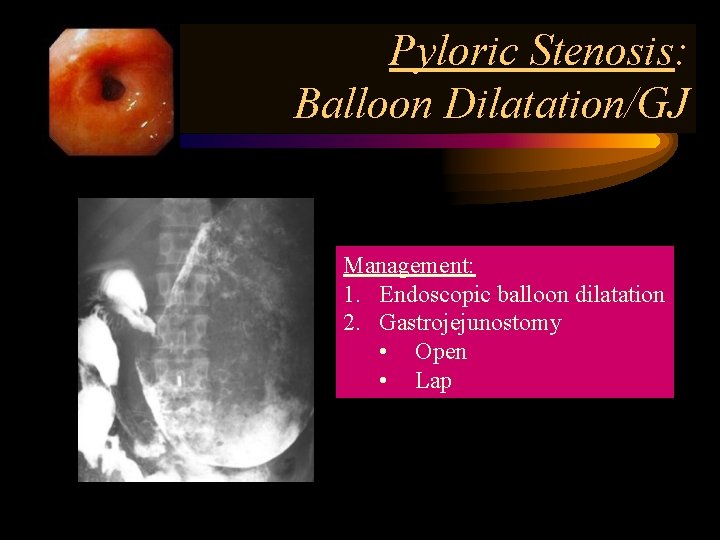
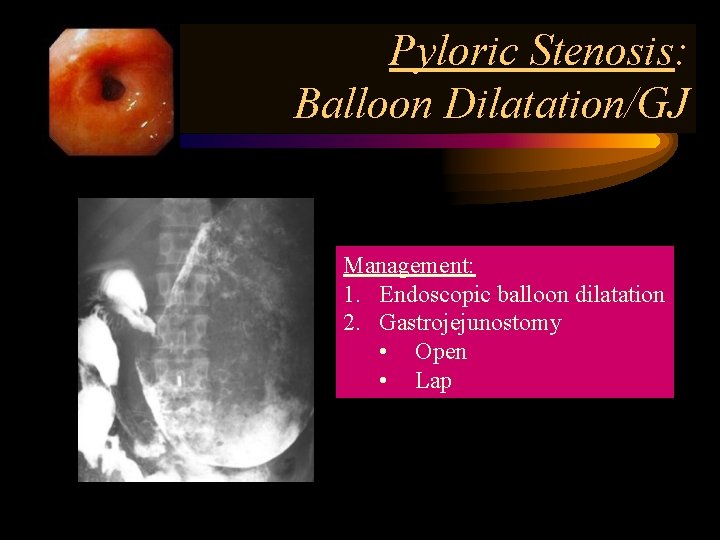
Pyloric Stenosis: Balloon Dilatation/GJ Management: 1. Endoscopic balloon dilatation 2. Gastrojejunostomy • Open • Lap
Tumors of the stomach and duodenum These are : Polyps Tumours : benign malignant
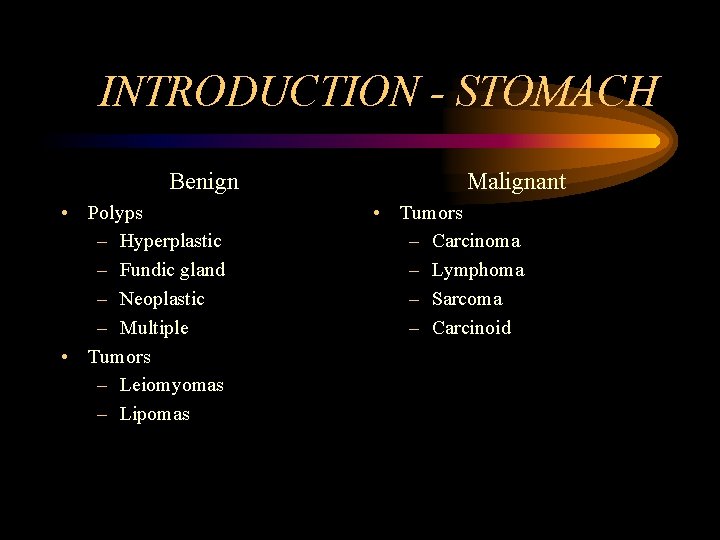
INTRODUCTION - STOMACH Benign • Polyps – Hyperplastic – Fundic gland – Neoplastic – Multiple • Tumors – Leiomyomas – Lipomas Malignant • Tumors – Carcinoma – Lymphoma – Sarcoma – Carcinoid
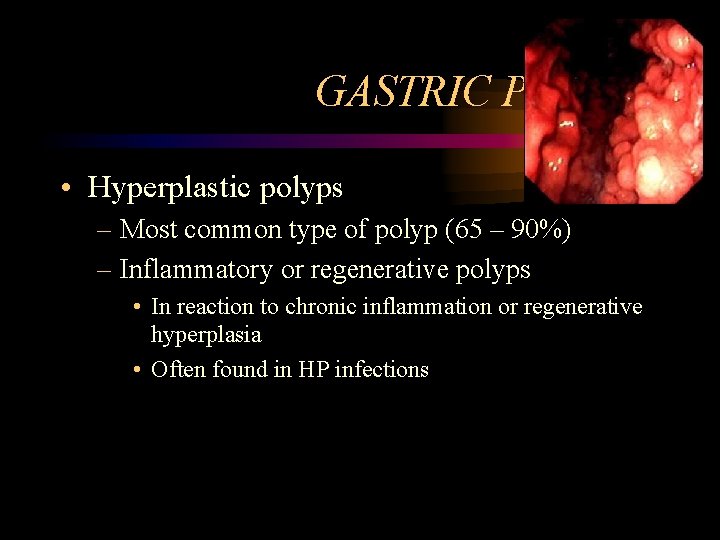
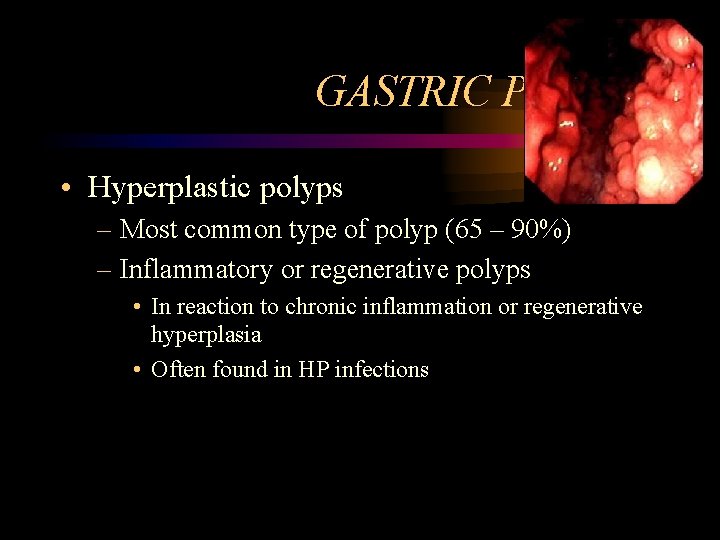
GASTRIC POLYPS • Hyperplastic polyps – Most common type of polyp (65 – 90%) – Inflammatory or regenerative polyps • In reaction to chronic inflammation or regenerative hyperplasia • Often found in HP infections
GASTRIC POLYPS – Sessile and seldom pedunculated • Mostly in the antrum • Multiple in 50% of cases • Varying in size but seldom < 2 cm – Rate of malignant transformation 1 – 3% • Usually larger than 2 cm
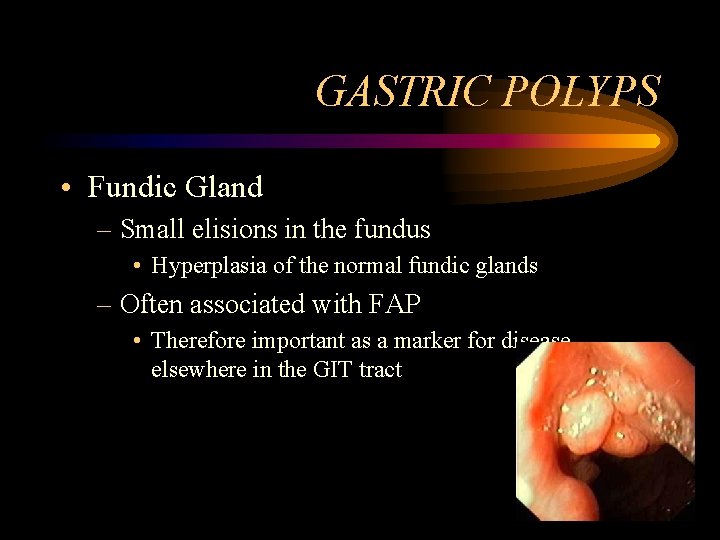
GASTRIC POLYPS • Fundic Gland – Small elisions in the fundus • Hyperplasia of the normal fundic glands – Often associated with FAP • Therefore important as a marker for disease elsewhere in the GIT tract
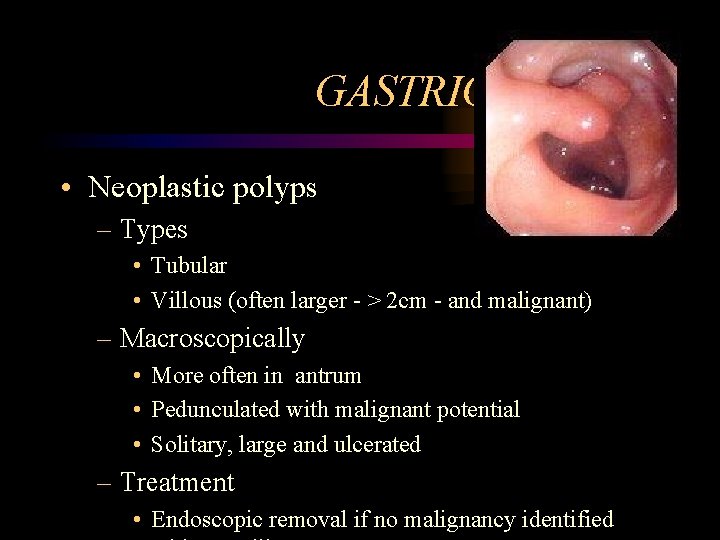
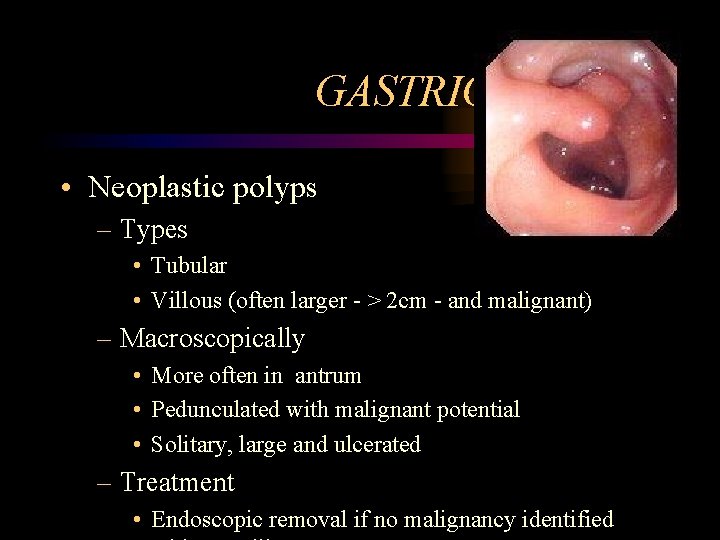
GASTRIC POLYPS • Neoplastic polyps – Types • Tubular • Villous (often larger - > 2 cm - and malignant) – Macroscopically • More often in antrum • Pedunculated with malignant potential • Solitary, large and ulcerated – Treatment • Endoscopic removal if no malignancy identified
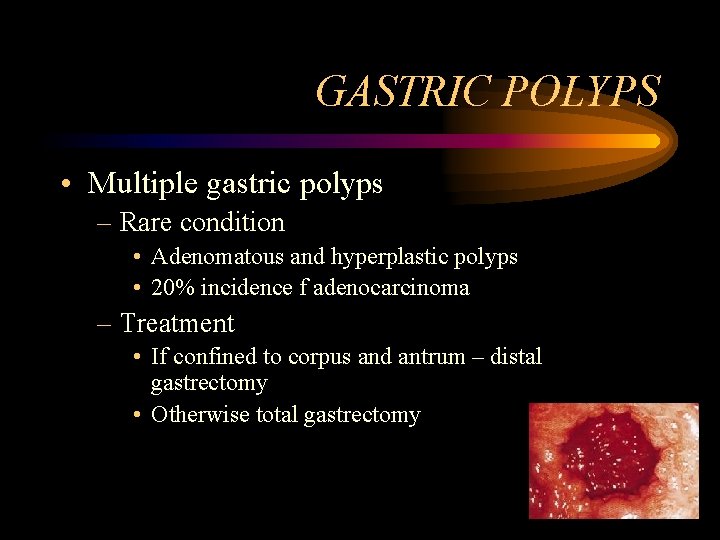
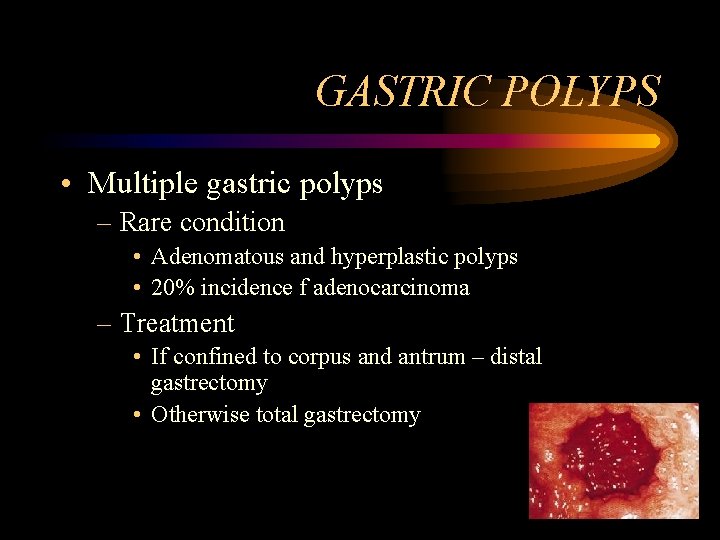
GASTRIC POLYPS • Multiple gastric polyps – Rare condition • Adenomatous and hyperplastic polyps • 20% incidence f adenocarcinoma – Treatment • If confined to corpus and antrum – distal gastrectomy • Otherwise total gastrectomy
GASTRIC POLYPS – Sometimes associated with Polyposis syndromes • • • FAP Gardner Peutz-Jeghers Cowden Cronkhite Canada

GASTRIC LEIOMYOMA • Incidence of 16% at autopsy • Pathology – Arise from smooth muscle of the GIT tract • Difficult to distinguish from GIST – 75% benign • Differentiation only on mitotic index – Large protruding elisions with central ulcer
GASTRIC LEIOMYOMA • Usually presents with bleeding if at all • Treatment is local excision with 2 – 3 cm margin
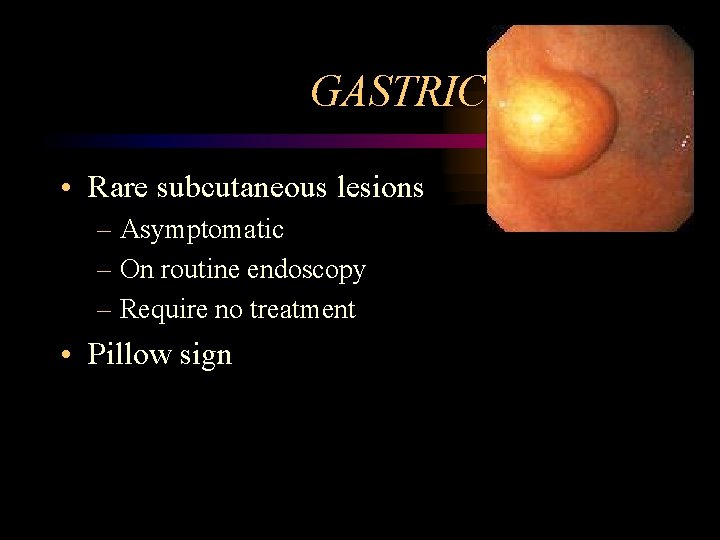
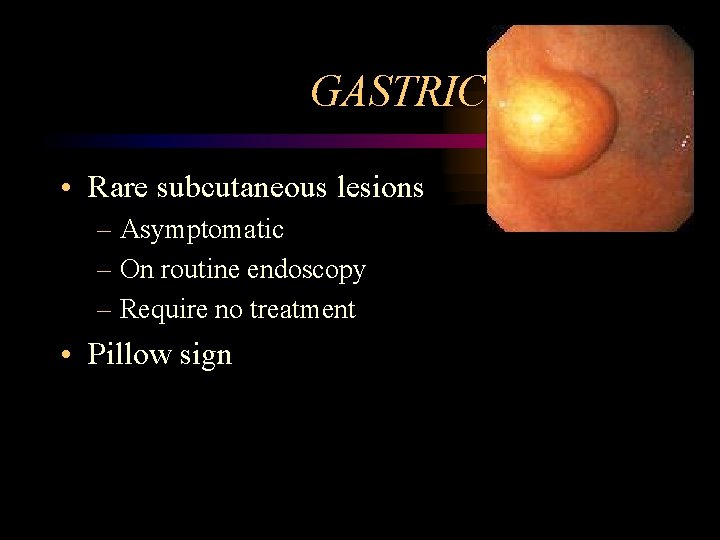
GASTRIC LIPOMA • Rare subcutaneous lesions – Asymptomatic – On routine endoscopy – Require no treatment • Pillow sign
ADENOCARCINOMA OF THE STOMACH • Declining incidence in western world – HP associated due to chronic atrophic gastritis – Also related to • Low dietary intake vegetables and fruit • High dietary intake of starches • More common in males ( 3 : 1 )
ADENOCARCINOMA OF THE STOMACH • Histology – Invariably adeno-carcinoma – Squamous cell carcinoma from oesophagus • Involves fundus and cardia
ADENOCARCINOMA OF THE STOMACH • Histological typing – Ulcerated carcinoma (25%) • Deep penetrated ulcer with shallow edges • Usually through all layers of the stomach – Polipoid carcinoma (25%) • Intraluminal tumors, large in size • Late metastasis
Adenocarcinoma of the stomach – Superficial spreading carcinomas (15%) • Confinement to mucosa and sub-mucosa • Metastasis 30% at time of diagnosis • Better prognosis stage for stage
ADENOCARCINOMA OF THE STOMACH • Histological typing – Linitis plastica (10%) • Varity of SS but involves all layers of the stomach • Early spread with poor prognosis – Advanced carcinoma (35%) • Partly within and outside the stomach • Represents advanced stage of most of the fore mentioned carcinomas
ADENOCARCINOMA OF THE STOMACH • Symptoms and signs – Vague discomfort difficult to distinguish from dyspepsia – Anorexia • Meat aversion • Pronounced weight loss
Adenocarcinoma of the stomach • At late stage – Epigastric mass – Haematemesis usually coffee ground seldom severe – Metastasis • Vircho node in neck • Blumer shelf in rectum
ADENOCARCINOMA OF THE STOMACH • Surgical resection only cure – Late presentation makes sugary often futile – Palliation controversial for • Haemorrhage • Gastric outlet
ADENOCARCINOMA OF THE STOMACH – Simple gastrectomy as effective as abdominal block • Splenectomy often added due to direct involvement • Only for the very distal partial gestrectomy • Rest total gastrectomy • Prognosis overall 12% 5 year survival – 90% for stage I disease
GASTRIC LYMPHOMA • 5% of all primary gastric neoplasm's • 2 different types of lymphoma – Part of systemic lymphoma with gastric involvement (32%) – Part of primary involvement of the GIT (MALT Tumors) • 10 – 20% of all lymphomas occur in the abdomen • 50% of those are gastric in nature
GASTRIC LYMPHOMA • Risk factors – HP due to chronic stimulation of the MALT – In early stages of disease Rx of HP leads to regression of the disease
GASTRIC LYMPHOMA Primary MALT • Early stages also referred to as pseudolymphoma – Indolent for long periods – Low incidence of • Spread to lymph nodes • Involvement of bone marrow – Therefore much better prognosis
GASTRIC LYMPHOMA Primary MALT • Mostly involves the antrum • 5 different types according to appearance – Infiltrative – Nodular – Combination - Ulcerative - Polypoid
GASTRIC LYMPHOMA Primary MALT • At time of presentation – Larger than 10 cm (50%) – More than 1 focus (25%) – Ulcerated (30 – 50%) • Pattern of metastasis similar to gastric carcinoma • Signs and symptoms – Occur late and are vague – Relieved by anti-secretory drugs
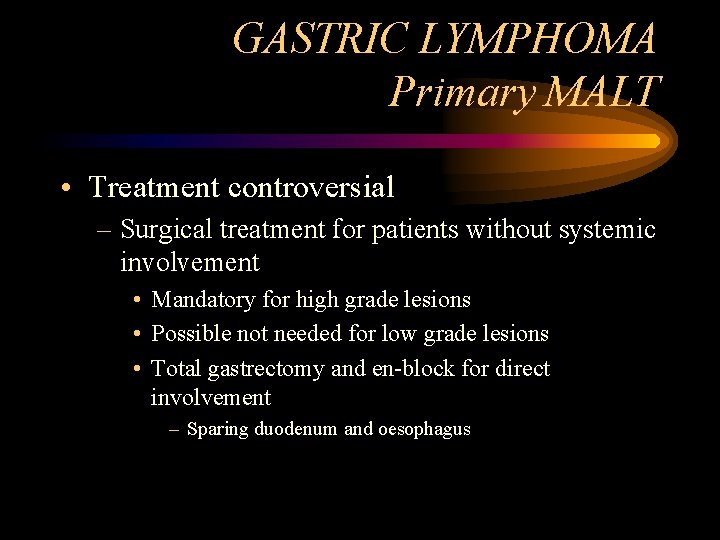
GASTRIC LYMPHOMA Primary MALT • Treatment controversial – Surgical treatment for patients without systemic involvement • Mandatory for high grade lesions • Possible not needed for low grade lesions • Total gastrectomy and en-block for direct involvement – Sparing duodenum and oesophagus
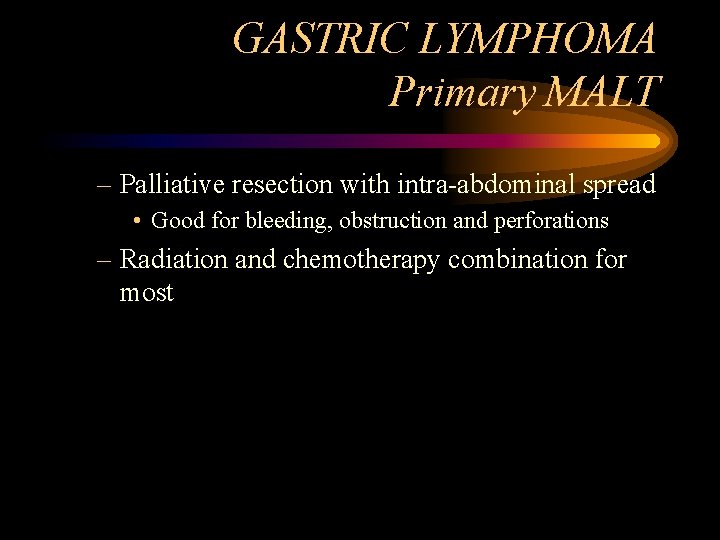
GASTRIC LYMPHOMA Primary MALT – Palliative resection with intra-abdominal spread • Good for bleeding, obstruction and perforations – Radiation and chemotherapy combination for most
GASTRIC SARCOMA • 1 – 3 % of gastric malignancies • Include a wide variety of tumors – Leiomyosarcoma – Leiomyoblastoma – GIST
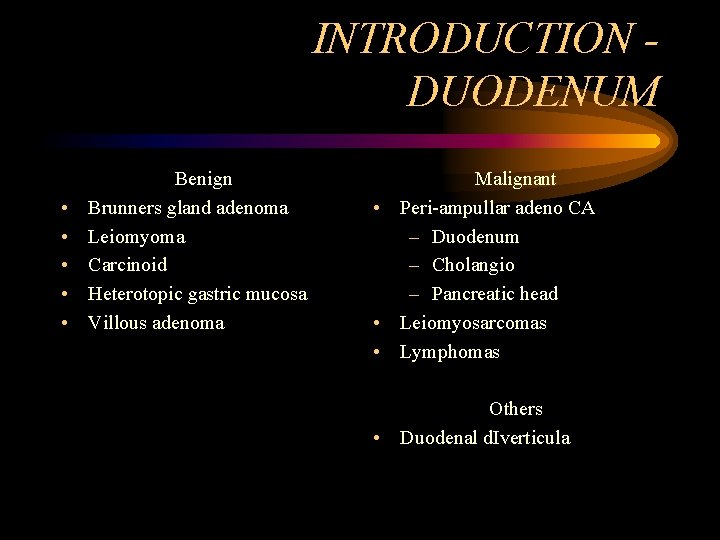
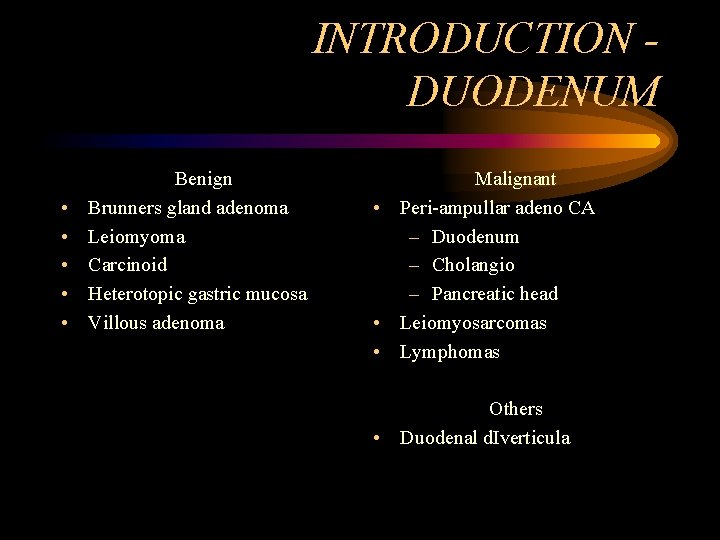
INTRODUCTION DUODENUM • • • Benign Brunners gland adenoma Leiomyoma Carcinoid Heterotopic gastric mucosa Villous adenoma Malignant • Peri-ampullar adeno CA – Duodenum – Cholangio – Pancreatic head • Leiomyosarcomas • Lymphomas Others • Duodenal d. Iverticula
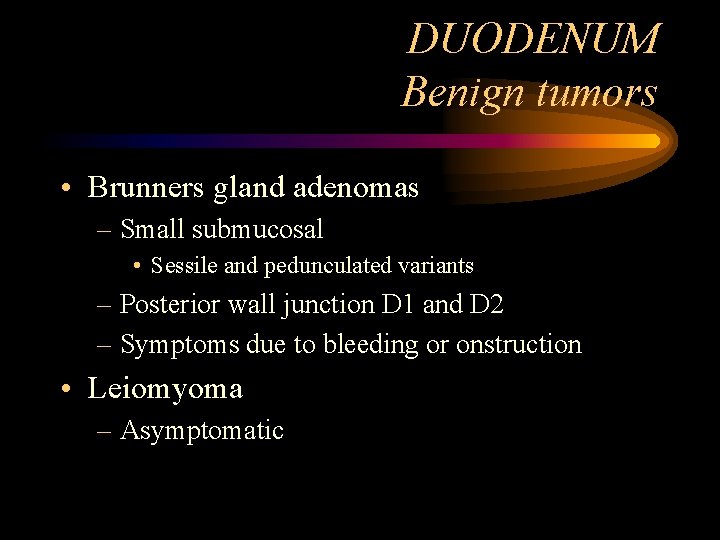
DUODENUM Benign tumors • Brunners gland adenomas – Small submucosal • Sessile and pedunculated variants – Posterior wall junction D 1 and D 2 – Symptoms due to bleeding or onstruction • Leiomyoma – Asymptomatic
DUODENUM Benign tumors • Carcinoid – Mostly active (gastrin, SS and serotonin) – Simple excision
DUODENUM Benign tumors • Hetrotopic gastric mucosa – Multiple small mucosal lesions – No clinical significance • Villous adenoma – Intestinal bleeding – Obstruction of ampulla with jaundice – Risk of malignancy high (50%) – Endoscopic snaring or local excision
DUODENUM Malignant tumors • Located in the descending part of the duodenum • Symptoms – Pain, obstruction bleeding and jaundice – Earlier than pancreas head
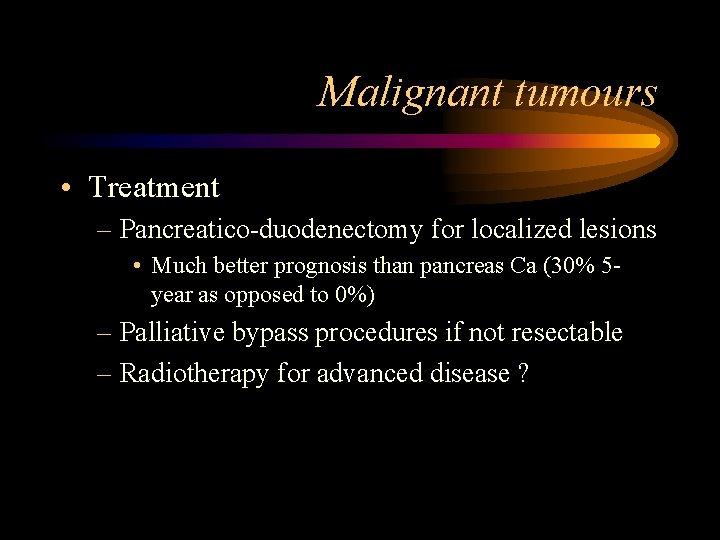
Malignant tumours • Treatment – Pancreatico-duodenectomy for localized lesions • Much better prognosis than pancreas Ca (30% 5 year as opposed to 0%) – Palliative bypass procedures if not resectable – Radiotherapy for advanced disease ?
 Sarophytes
Sarophytes Non common communicable diseases
Non common communicable diseases Difference between duodenum and jejunum
Difference between duodenum and jejunum Transpyloric plane mnemonic
Transpyloric plane mnemonic L
L Abdomen
Abdomen M cells
M cells Plica semicircularis
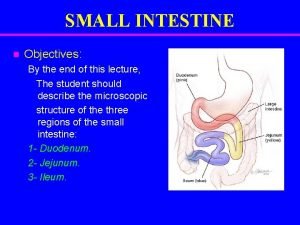
Plica semicircularis Small bowel
Small bowel Eutonic stomach
Eutonic stomach Hour glass contracture
Hour glass contracture C-loop of the duodenum
C-loop of the duodenum Duodenum cow
Duodenum cow Pancreatic tissue
Pancreatic tissue Cow digestive system diagram
Cow digestive system diagram Le duodeno-pancreas
Le duodeno-pancreas Treitz ligament
Treitz ligament What does bile digest in a frog
What does bile digest in a frog Back of mouth diagram
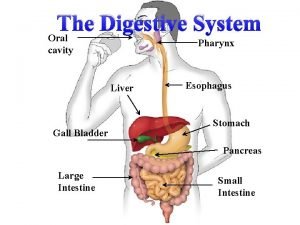
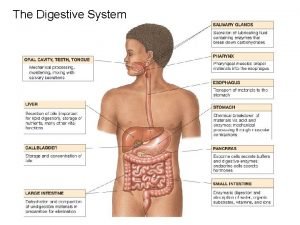
Back of mouth diagram 13.2 structures of the digestive system
13.2 structures of the digestive system Duodenum 4 parts
Duodenum 4 parts Loop of duodenum
Loop of duodenum Small intestine relations
Small intestine relations Duodenum jejunum ileum
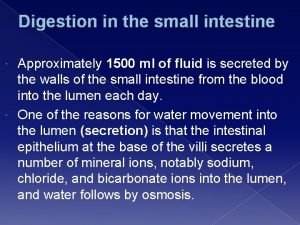
Duodenum jejunum ileum Digestion in the duodenum
Digestion in the duodenum Valve github
Valve github Duct of wirsung
Duct of wirsung Lig duodenorenale
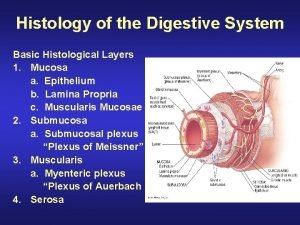
Lig duodenorenale Digestive histology
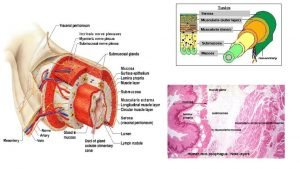
Digestive histology Digestive system
Digestive system Synaptic integration
Synaptic integration Duodenum cell
Duodenum cell Duodenum arterial supply
Duodenum arterial supply Rugae of mucosa
Rugae of mucosa Teeth formula
Teeth formula Kode icd 10 hepatoma
Kode icd 10 hepatoma Common factors of 36 and 48
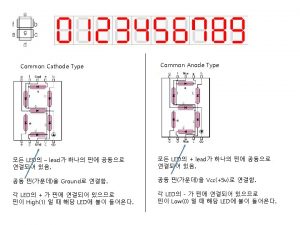
Common factors of 36 and 48 Common anode and common cathode
Common anode and common cathode Factors of 60 and 72
Factors of 60 and 72 Factors of 54
Factors of 54 Lcm of 10 and 18
Lcm of 10 and 18 Highest common factors and lowest common multiples
Highest common factors and lowest common multiples Lifestyle modern
Lifestyle modern Venn diagram of communicable and non-communicable diseases
Venn diagram of communicable and non-communicable diseases Section 19-3 diseases caused by bacteria and viruses
Section 19-3 diseases caused by bacteria and viruses Define a primary skin lesion and list three types
Define a primary skin lesion and list three types Chapter 6 musculoskeletal system
Chapter 6 musculoskeletal system Chapter 24 sexually transmitted diseases and hiv/aids
Chapter 24 sexually transmitted diseases and hiv/aids Chapter 22 genetics and genetically linked diseases
Chapter 22 genetics and genetically linked diseases Chapter 21 mental health diseases and disorders
Chapter 21 mental health diseases and disorders Chapter 17 reproductive system diseases and disorders
Chapter 17 reproductive system diseases and disorders Chapter 15 nervous system diseases and disorders
Chapter 15 nervous system diseases and disorders What conditions do fungal organisms favor for growth
What conditions do fungal organisms favor for growth Seborrheic keratoses
Seborrheic keratoses In what situation should a nail service not be performed?
In what situation should a nail service not be performed? Certain infectious and parasitic diseases
Certain infectious and parasitic diseases Chapter 8 cardiovascular system
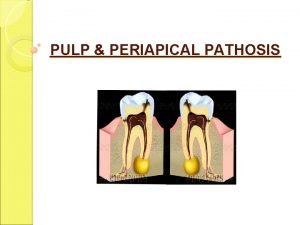
Chapter 8 cardiovascular system Pulpitis classification
Pulpitis classification Milady chapter 8 skin disorders and diseases
Milady chapter 8 skin disorders and diseases Venn diagram of communicable and non-communicable diseases
Venn diagram of communicable and non-communicable diseases Purulent diseases of lungs and pleura
Purulent diseases of lungs and pleura Tronsmo plant pathology and plant diseases download
Tronsmo plant pathology and plant diseases download Tronsmo plant pathology and plant diseases download
Tronsmo plant pathology and plant diseases download Albugo eye
Albugo eye Venn diagram of communicable and non-communicable diseases
Venn diagram of communicable and non-communicable diseases Vitamin name list
Vitamin name list Myth and fallacies about non-communicable diseases
Myth and fallacies about non-communicable diseases 10 diseases of lymphatic system
10 diseases of lymphatic system Roles and responsibilities of healthcare team
Roles and responsibilities of healthcare team Inet wellspan
Inet wellspan What is medical asepsis
What is medical asepsis Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể