PULP PERIAPICAL PATHOSIS INTRODUCTION Inflammation of pulp and


![CLASSIFICATION OF PULPAL DISEASES According to Grossman I] PULPITIS a) REVERSIBLE 1. Acute (symptomatic) CLASSIFICATION OF PULPAL DISEASES According to Grossman I] PULPITIS a) REVERSIBLE 1. Acute (symptomatic)](https://slidetodoc.com/presentation_image_h/b72453dd07ce656f37ac8bc5f3ea13b0/image-11.jpg)
![II] PULP DEGENERATION Calcific (Radiographic diagnosis) Others (Histopathologic diagnosis) III] PULP NECROSIS II] PULP DEGENERATION Calcific (Radiographic diagnosis) Others (Histopathologic diagnosis) III] PULP NECROSIS](https://slidetodoc.com/presentation_image_h/b72453dd07ce656f37ac8bc5f3ea13b0/image-12.jpg)










![WEINE’S CLASSIFICATION PULPOPERIAPICAL DISEASE: 1] PAINFUL PULPOPERIAPICAL PATHOSES a) Incipient acute periapical periodontitis b) WEINE’S CLASSIFICATION PULPOPERIAPICAL DISEASE: 1] PAINFUL PULPOPERIAPICAL PATHOSES a) Incipient acute periapical periodontitis b)](https://slidetodoc.com/presentation_image_h/b72453dd07ce656f37ac8bc5f3ea13b0/image-58.jpg)













- Slides: 101
PULP & PERIAPICAL PATHOSIS
INTRODUCTION Inflammation of pulp and periapical tissue is one of the most common diseases encountered in our day to day practice. To give proper and effective treatment one has to diagnose correctly. Arriving at a correct diagnosis requires knowledge, skill, art and experience; knowledge of the diseases and their symptoms, skill to apply proper test procedures, the art to correlate the facts and experiences to reach proper conclusions.
PULPAL PATHOSIS “ The pulp lives for the dentin and the dentin lives by the grace of the pulp. Few marriages in nature are marked by a greater affinity. ” Alfred L. Ogilvie -

ETIOLOGY OF PULPAL DISEASES According to Ingle, I. BACTERIAL a) CORONAL INGRESS 1. Caries 2. Fracture 3. Non fracture trauma 4. Developmental Anomalies b) RADICULAR INGRESS 1. Caries 2. Retrogenic infection – periodontal pocket & abscess 3. Hematogenic
2. TRAUMATIC a) ACUTE 1. Coronal fracture 2. Radicular fracture 3. Vascular stasis 4. Luxation 5. Avulsion b) CHRONIC 1. Adolescent female bruxism 2. Traumatism 3. Attrition or abrasion 4. Erosion
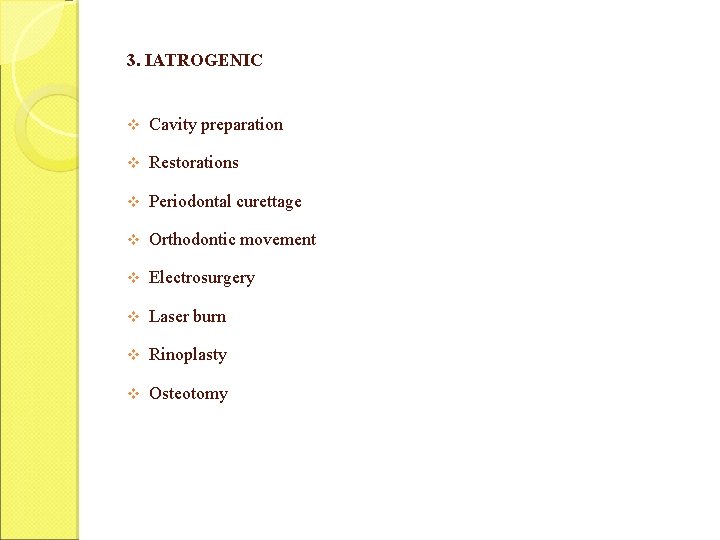
3. IATROGENIC v Cavity preparation v Restorations v Periodontal curettage v Orthodontic movement v Electrosurgery v Laser burn v Rinoplasty v Osteotomy
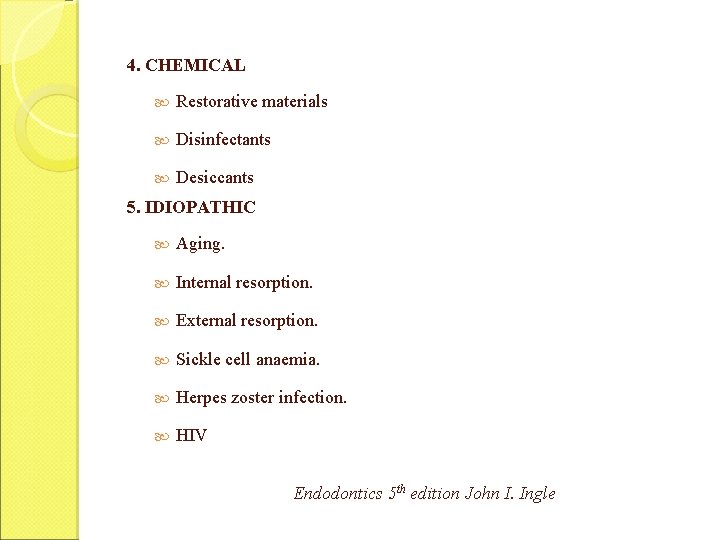
4. CHEMICAL Restorative materials Disinfectants Desiccants 5. IDIOPATHIC Aging. Internal resorption. External resorption. Sickle cell anaemia. Herpes zoster infection. HIV Endodontics 5 th edition John I. Ingle

According to Grossman PHYSICAL a) MECHANICAL a) Trauma b) Pathological wear c) Cracked tooth syndrome d) Barometric changes b) THERMAL a) Heat from cavity preparation b) Exothermic heat from the setting of cement c) Conduction of temperature through deep fillings d) Frictional heat caused by polishing of restoration
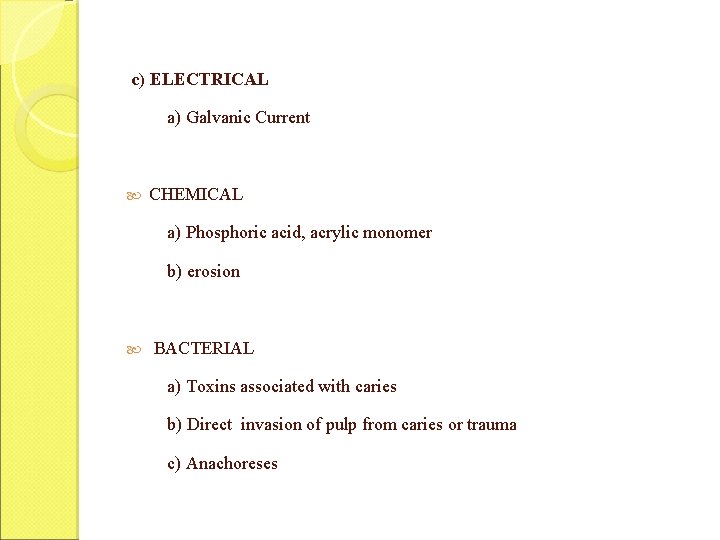
c) ELECTRICAL a) Galvanic Current CHEMICAL a) Phosphoric acid, acrylic monomer b) erosion BACTERIAL a) Toxins associated with caries b) Direct invasion of pulp from caries or trauma c) Anachoreses
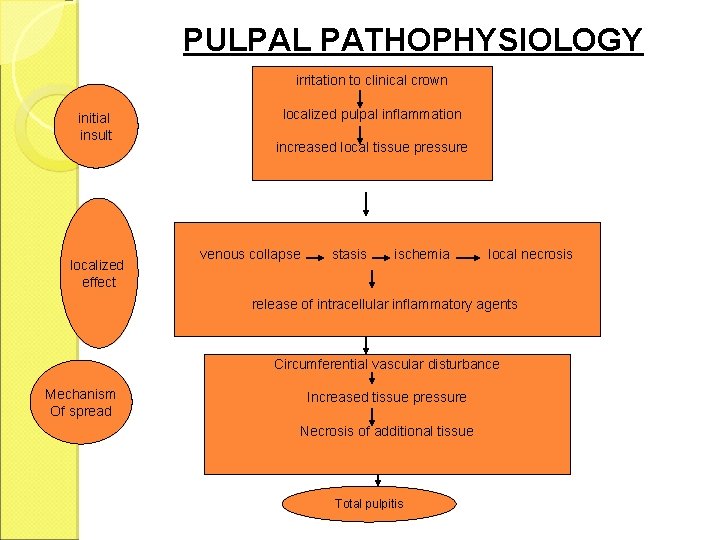
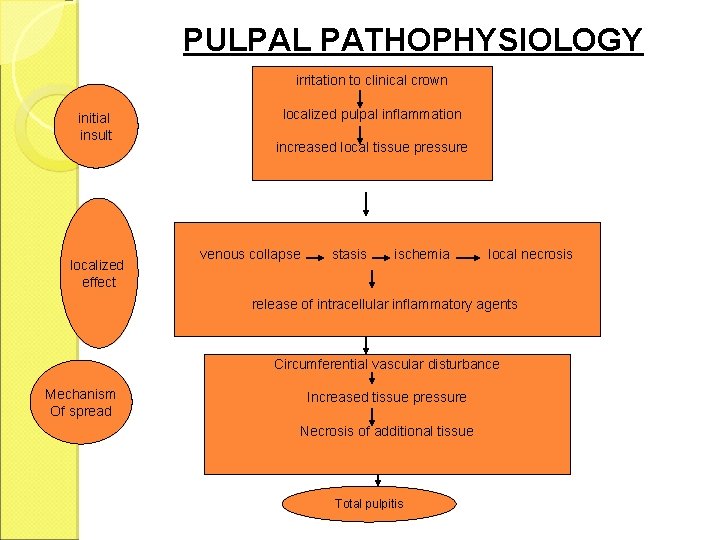
PULPAL PATHOPHYSIOLOGY irritation to clinical crown initial insult localized effect localized pulpal inflammation increased local tissue pressure venous collapse stasis ischemia local necrosis release of intracellular inflammatory agents Circumferential vascular disturbance Mechanism Of spread Increased tissue pressure Necrosis of additional tissue Total pulpitis
![CLASSIFICATION OF PULPAL DISEASES According to Grossman I PULPITIS a REVERSIBLE 1 Acute symptomatic CLASSIFICATION OF PULPAL DISEASES According to Grossman I] PULPITIS a) REVERSIBLE 1. Acute (symptomatic)](https://slidetodoc.com/presentation_image_h/b72453dd07ce656f37ac8bc5f3ea13b0/image-11.jpg)
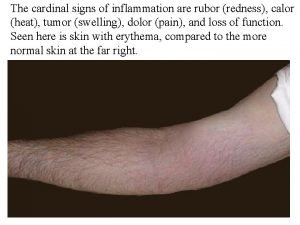
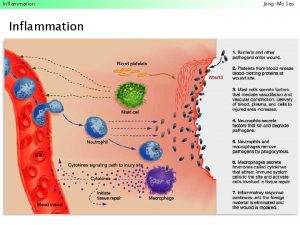
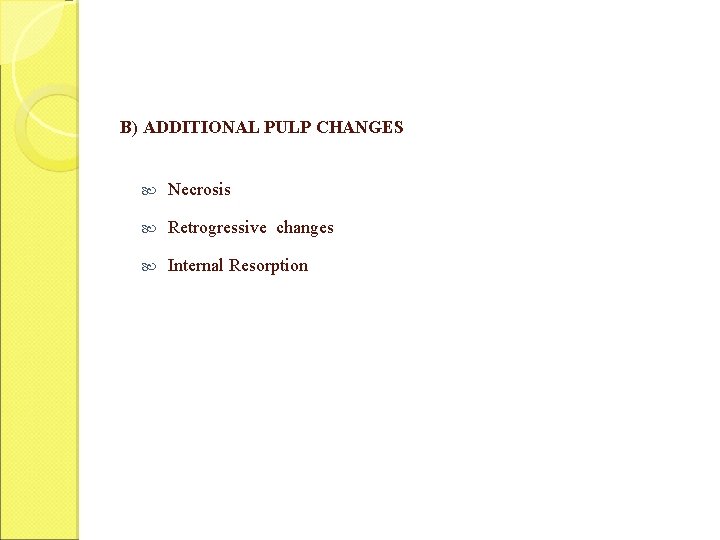
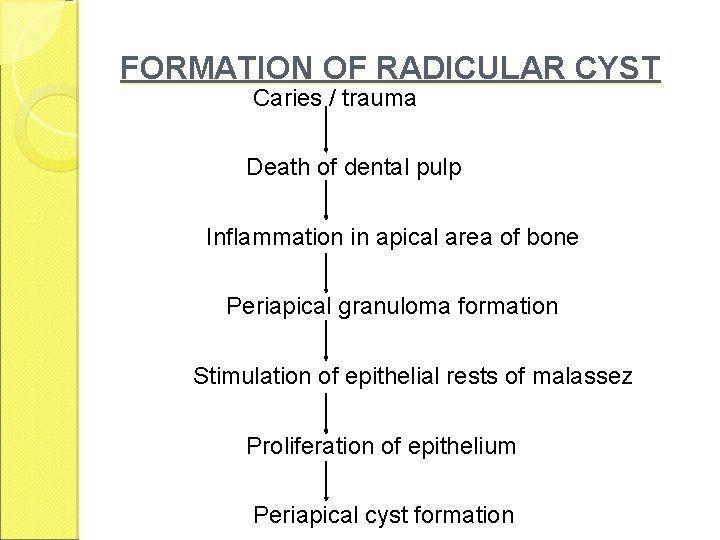
CLASSIFICATION OF PULPAL DISEASES According to Grossman I] PULPITIS a) REVERSIBLE 1. Acute (symptomatic) 2. Chronic (asymptomatic) b) IRREVERSIBLE 1. Acute - Abnormally responsive to cold - Abnormally responsive to heat 2. Chronic - Asymptomatic with pulp exposure - Hyperplastic pulpitis - Internal resorption
![II PULP DEGENERATION Calcific Radiographic diagnosis Others Histopathologic diagnosis III PULP NECROSIS II] PULP DEGENERATION Calcific (Radiographic diagnosis) Others (Histopathologic diagnosis) III] PULP NECROSIS](https://slidetodoc.com/presentation_image_h/b72453dd07ce656f37ac8bc5f3ea13b0/image-12.jpg)
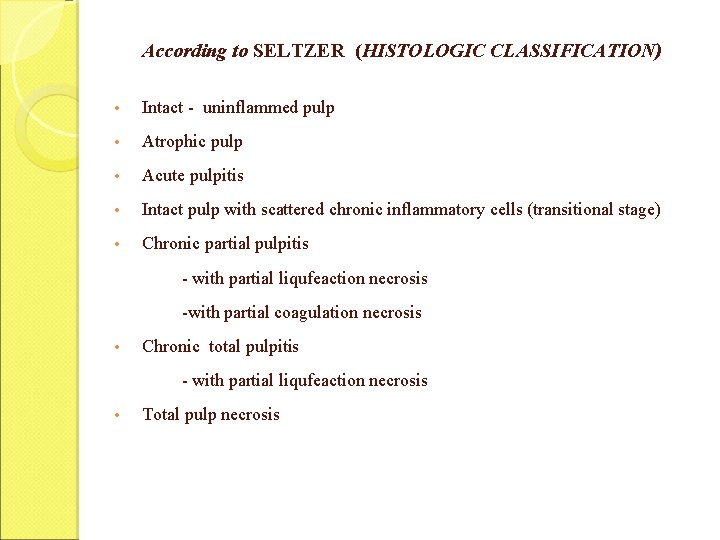
II] PULP DEGENERATION Calcific (Radiographic diagnosis) Others (Histopathologic diagnosis) III] PULP NECROSIS
According to Cohen: Reversible pulpitis Irreversible pulpitis Asymptomatic Irreversible pulpitis Symptomatic irreversible Hyperplastic pulpitis Internal resorption Pulp necrosis

According to. Weine A) INFLAMMATORY CHANGES HYPERALGIA Hypersensitive dentin. Hyperemia. PAINFUL PULPITIS Acute pulpalgia (acute pulpitis) Chronic pulpalgia (subacute pulpitis) NON PAINFUL PULPITIS Cronic Ulcerative Pulpitis Chronic Pulpitis Hyperplastic pulpitis.
B) ADDITIONAL PULP CHANGES Necrosis Retrogressive changes Internal Resorption
According to SELTZER (HISTOLOGIC CLASSIFICATION) • Intact - uninflammed pulp • Atrophic pulp • Acute pulpitis • Intact pulp with scattered chronic inflammatory cells (transitional stage) • Chronic partial pulpitis - with partial liqufeaction necrosis -with partial coagulation necrosis • Chronic total pulpitis - with partial liqufeaction necrosis • Total pulp necrosis
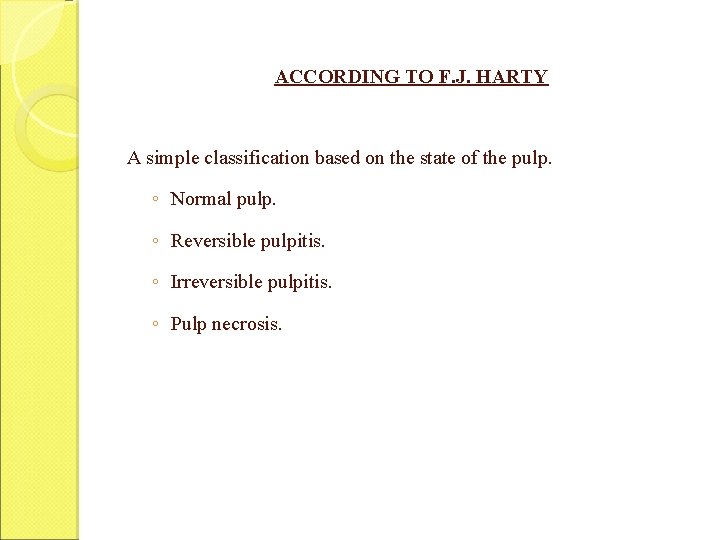
ACCORDING TO F. J. HARTY A simple classification based on the state of the pulp. ◦ Normal pulp. ◦ Reversible pulpitis. ◦ Irreversible pulpitis. ◦ Pulp necrosis.
SHAFER’S Classification 1. According to involvement a) Partial b) Total 2. According to severity a) Acute b) Chronic 3. According to presence or absence of direct communication between the dental pulp and oral environment a) Pulpitis aperta b) Pulpitis Clausa
REVERSIBLE PULPITIS A mild to moderate inflammatory condition of pulp caused by noxious stimuli in which pulp is capable of returning to the uninflamed state following removal of the stimuli. Also, referred as “PULP HYPERAEMIA”.

ETIOLOGY 1. Trauma 2. Thermal shock 3. Excessive dehydration 4. Galvanism 5. Chemical stimulus 6. Bacteria 7. Circulatory disturbances 8. Local vascular congestion
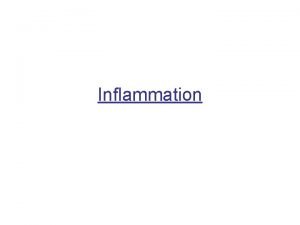
Symptoms Sharp pain lasting for a moment More often brought on by cold than hot food Does not occur spontaneously Does not continue when stimulus has been removed Teeth are not tender on percussion Histopathology Hyperaemia - mild to moderate inflammatory changes are limited to the area of involved dentinal tubules Reparative dentin, dilated blood vessels, disruption of odontoblast layer Extravasation of edema fluid Immunologically competent chronic inflammatory cells Presence of acute inflammatory cells
DIAGNOSIS 1. Pain: Sharp pain, lasts for a few seconds Cold, sweet or sour causes pain 2. Visual examination & history: Examine for caries, restorations, fractures or traumatic occlusion History of past dental treatment 3. Clinical tests: Cold test is excellent way to locate pain Normal to percussion, palpation and mobility 4. Radiographically : No changes 5. Vitality test: More readily response to cold stimulation than normal teeth EPT requires minimal current to initiate positive response
Treatment - Prevention - Removal of the noxious stimuli - Check for vitality - Periodic care to prevent caries - Proper insulation of the restoration - Desensitization Prognosis Good - if irritant is removed earlier Otherwise condition may develop to Irreversible pulpitis

IRREVERSIBLE PULPITIS A persistent inflammatory condition of the pulp, symptomatic or asymptomatic, caused by noxious stimulus. May be Acute or chronic q ETIOLOGY Caries Chemical, Sequelae thermal and mechanical injuries of reversible pulpitis

HISTOPATHOLOGY Both acute and chronic inflammatory stages are seen dentin Chronic inflammatory response Caries not removed inflammatory changes will increase in severity Post capillary venules become congested Attract PMNL’s Affect circulation - Necrosis Phagocytosis by PMNL ‘s Chronic ulcerative pulpitis Carious process continues PMNL ‘s Die & release lysosomal enzymes microabscess Acute Inflammatory reaction lysis pus
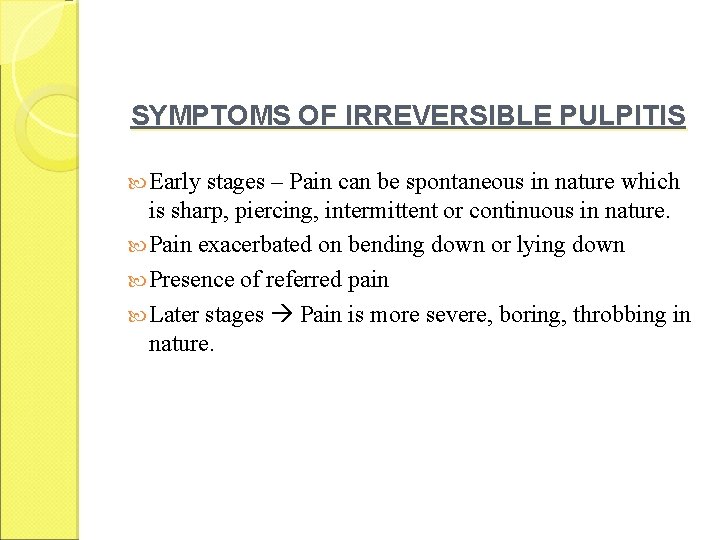
SYMPTOMS OF IRREVERSIBLE PULPITIS Early stages – Pain can be spontaneous in nature which is sharp, piercing, intermittent or continuous in nature. Pain exacerbated on bending down or lying down Presence of referred pain Later stages Pain is more severe, boring, throbbing in nature.
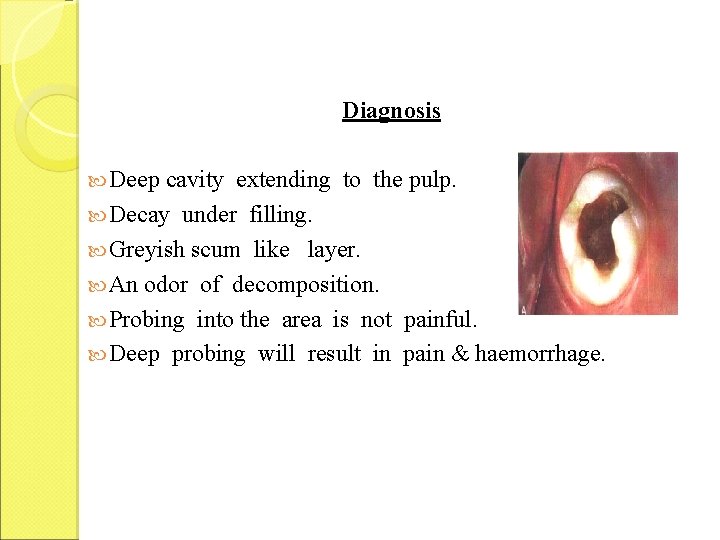
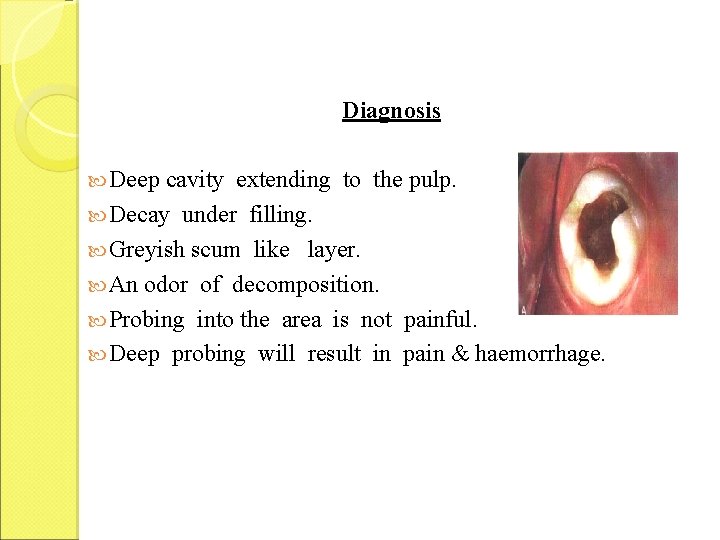
Diagnosis Deep cavity extending to the pulp. Decay under filling. Greyish scum like layer. An odor of decomposition. Probing into the area is not painful. Deep probing will result in pain & haemorrhage.
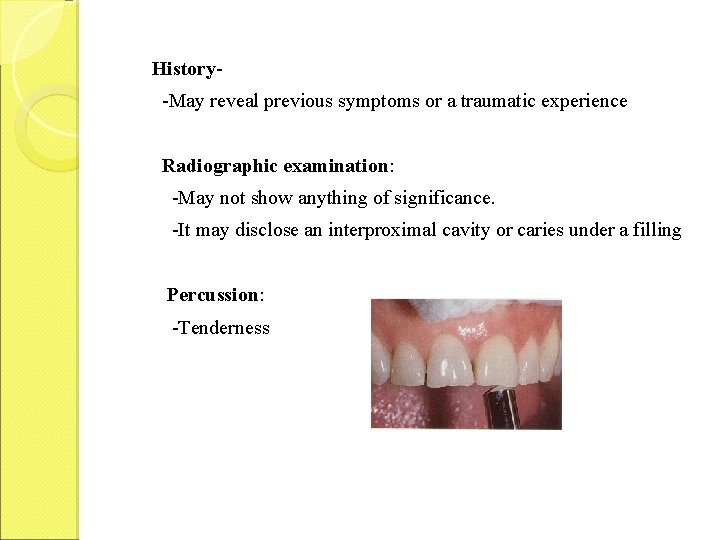
History-May reveal previous symptoms or a traumatic experience Radiographic examination: -May not show anything of significance. -It may disclose an interproximal cavity or caries under a filling Percussion: -Tenderness

Vitality test: Thermal test: As pulpal inflammation progresses, heat will intensify the responses. Cold will tend to relieve the pain in advanced stages of pulpits. Electric test: Early stages – response to less current. Later (Necrotic tissue)- more current is required. Treatment: Pulpectomy. Surgical removal should be considered if the tooth is unrestorable.
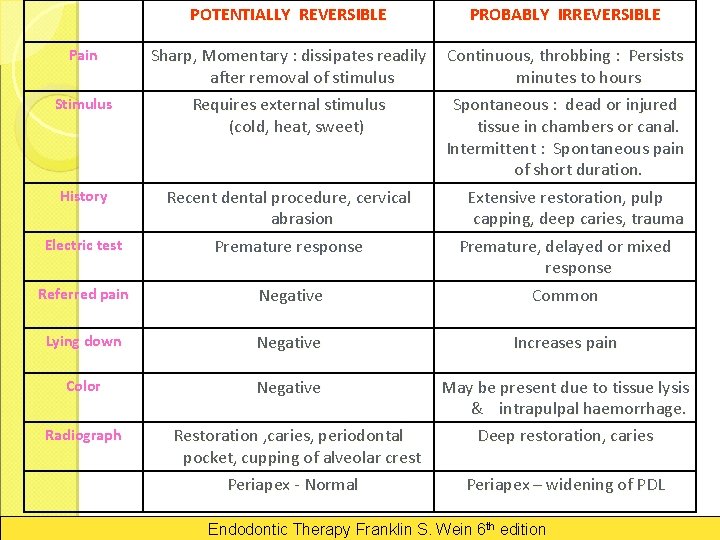
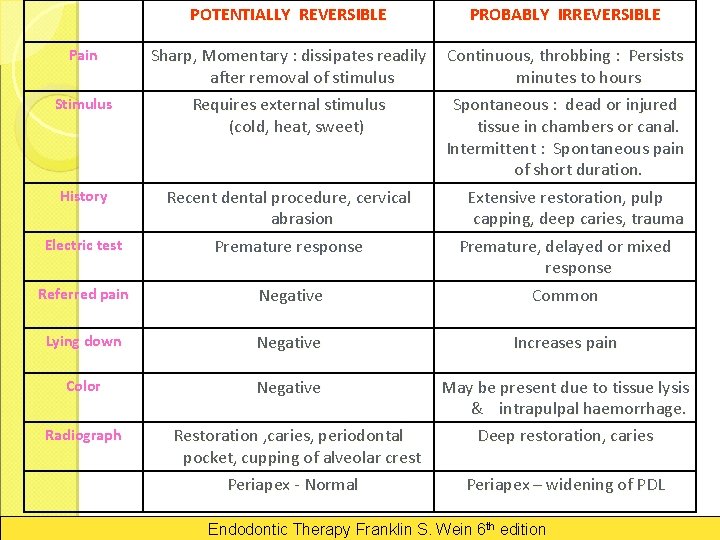
POTENTIALLY REVERSIBLE PROBABLY IRREVERSIBLE Sharp, Momentary : dissipates readily after removal of stimulus Requires external stimulus (cold, heat, sweet) Electric test Recent dental procedure, cervical abrasion Premature response Referred pain Negative Continuous, throbbing : Persists minutes to hours Spontaneous : dead or injured tissue in chambers or canal. Intermittent : Spontaneous pain of short duration. Extensive restoration, pulp capping, deep caries, trauma Premature, delayed or mixed response Common Lying down Negative Increases pain Color Negative May be present due to tissue lysis & intrapulpal haemorrhage. Deep restoration, caries Pain Stimulus History Radiograph Restoration , caries, periodontal pocket, cupping of alveolar crest Periapex - Normal Periapex – widening of PDL Endodontic Therapy Franklin S. Wein 6 th edition

CHRONIC HYPERPLASTIC PULPITIS (Pulp Polyp) Chronic hyperplastic pulpitis is a productive pulpal inflammation due to an extensive carious exposure of a young pulp. Characterized by - development of granulation tissue, covered at times with epithelium and resulting from long standing, low grade irritation .
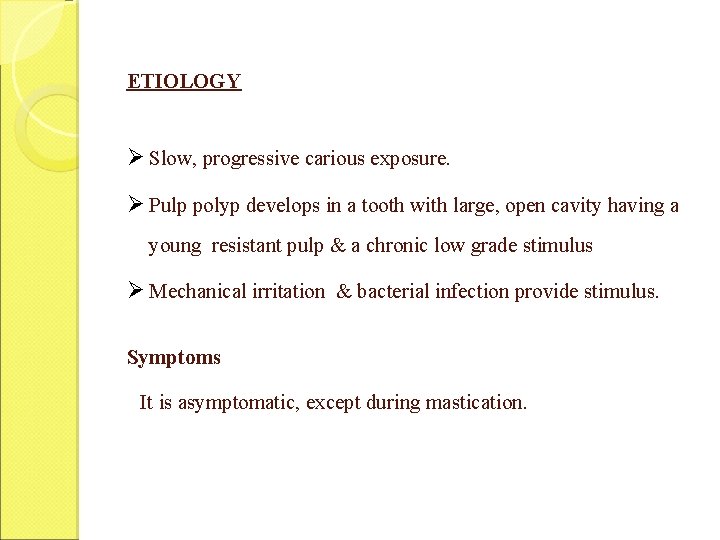
ETIOLOGY Ø Slow, progressive carious exposure. Ø Pulp polyp develops in a tooth with large, open cavity having a young resistant pulp & a chronic low grade stimulus Ø Mechanical irritation & bacterial infection provide stimulus. Symptoms It is asymptomatic, except during mastication.

HISTOPATHOLOGY Budding capillaries, proliferating fibroblasts & inflammatory cells are seen. Presence of granulation tissue – which is young vascular connective tissue containing PMNL’s, lymphocytes & plasma cells. Collagenous fibres -rooted in deeper tissue of pulp chamber. Sensory nerve fibres are almost absent near surface. Surface is usually covered by stratified squamous epithelium.
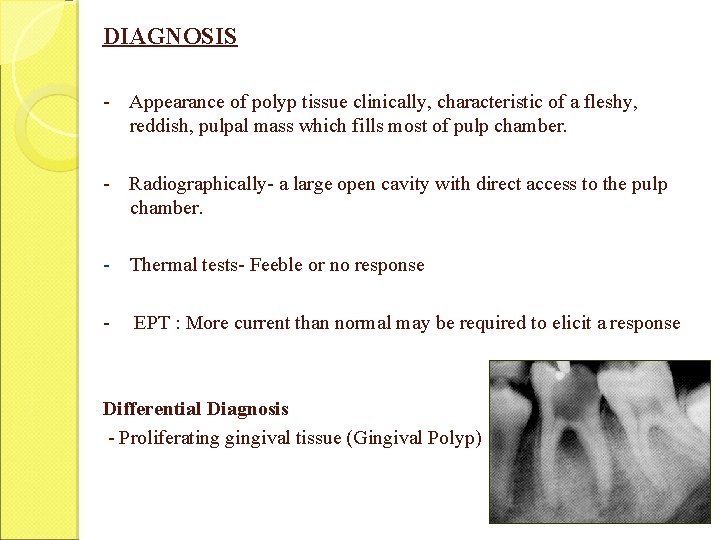
DIAGNOSIS - Appearance of polyp tissue clinically, characteristic of a fleshy, reddish, pulpal mass which fills most of pulp chamber. - Radiographically- a large open cavity with direct access to the pulp chamber. - Thermal tests- Feeble or no response - EPT : More current than normal may be required to elicit a response Differential Diagnosis - Proliferating gingival tissue (Gingival Polyp)

TREATMENT • Elimination of polyp tissue with a sharp curette or spoon excavator, followed by extirpation of the pulp, provided the tooth can be restored. • • Bleeding can be controlled with pressure. pulpectomy can be completed in a single visit.
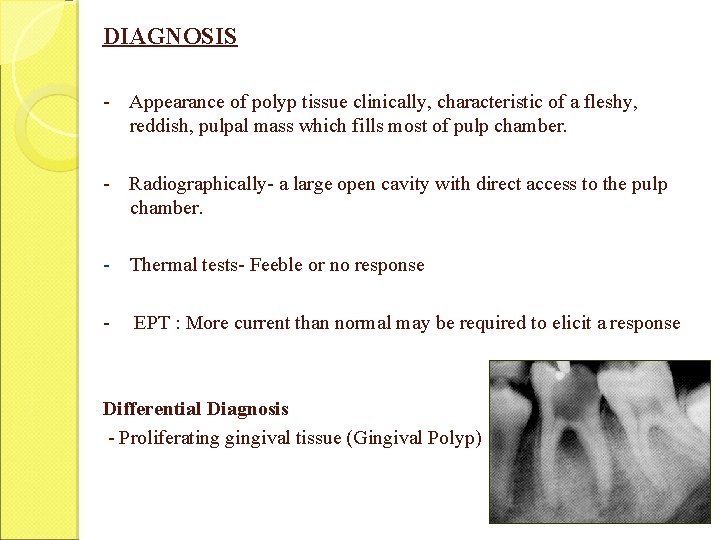
CHRONIC PULPITIS (CLOSED FORM) Occur from operative procedures, trauma or periodontal lesions extending apically to the foramina of lateral canals Excessive orthodontic movement may affect the vascular supply to the pulp producing localized areas of necrosis Depending on the strength and duration of the inciting irritant, pulpitis may be chronic from onset or become chronic after the acute responses have subsided Exacerbation – additional operative procedures Minimal pulpal damage – resolution may occur
CHRONIC PULPITIS (ULCERATIVE OR OPEN FORM) Is a chronic inflammation of the cariously exposed pulp characterized by the formation of an abscess at the point of exposure (ulcer). Terms used are - Pulpal chronic abscess or pulpal granuloma. The abscess is surrounded by granulomatous tissue Can be partial or total.
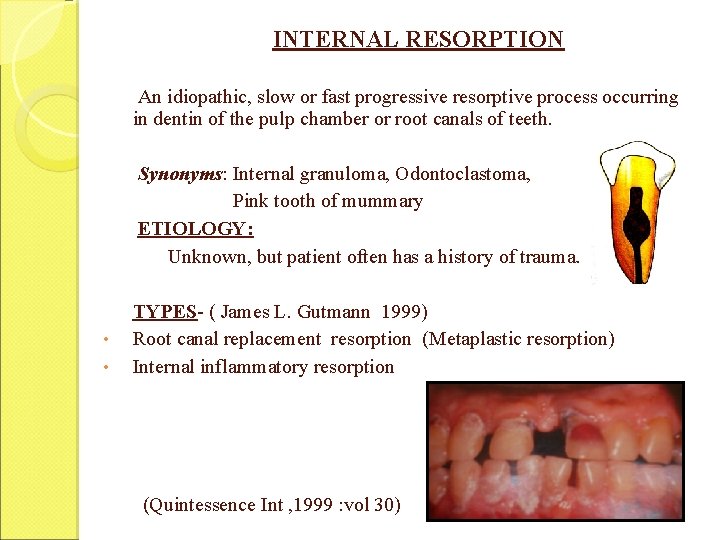
INTERNAL RESORPTION An idiopathic, slow or fast progressive resorptive process occurring in dentin of the pulp chamber or root canals of teeth. Synonyms: Internal granuloma, Odontoclastoma, Pink tooth of mummary ETIOLOGY: Unknown, but patient often has a history of trauma. • • TYPES- ( James L. Gutmann 1999) Root canal replacement resorption (Metaplastic resorption) Internal inflammatory resorption (Quintessence Int , 1999 : vol 30)
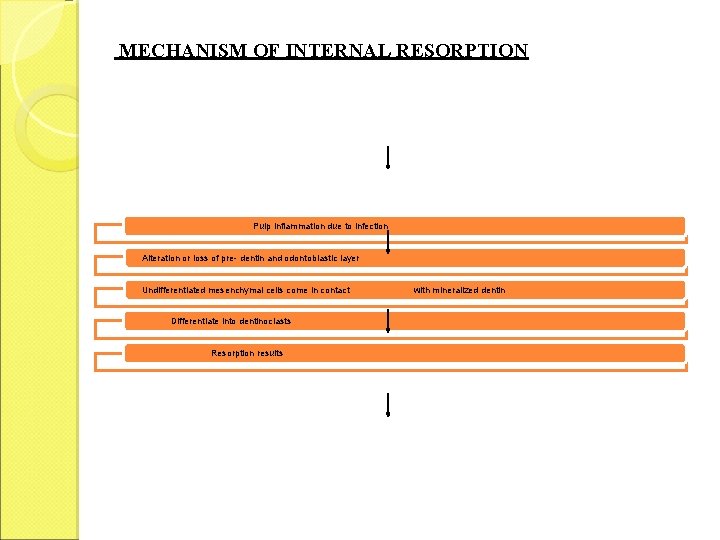
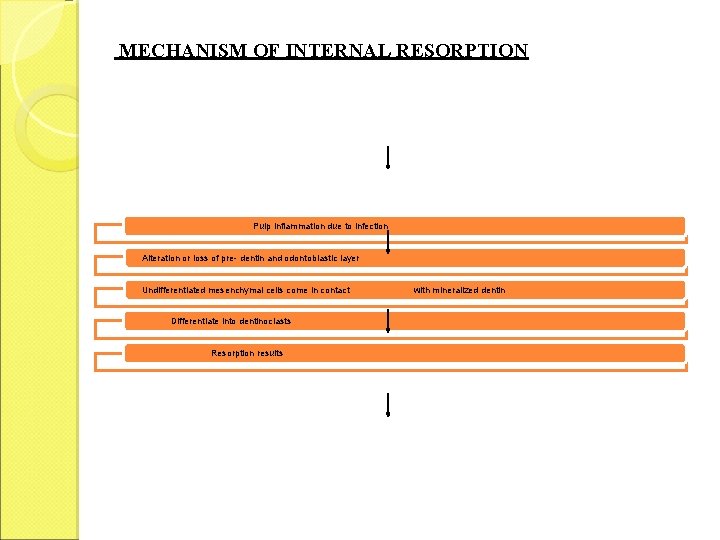
MECHANISM OF INTERNAL RESORPTION Pulp inflammation due to infection Alteration or loss of pre- dentin and odontoblastic layer Undifferentiated mesenchymal cells come in contact Differentiate into dentinoclasts Resorption results with mineralized dentin
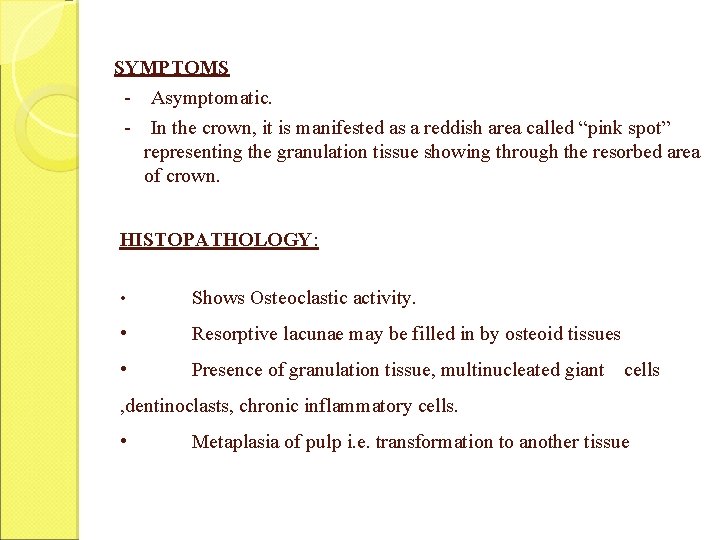
SYMPTOMS - Asymptomatic. - In the crown, it is manifested as a reddish area called “pink spot” representing the granulation tissue showing through the resorbed area of crown. HISTOPATHOLOGY: • Shows Osteoclastic activity. • Resorptive lacunae may be filled in by osteoid tissues • Presence of granulation tissue, multinucleated giant cells , dentinoclasts, chronic inflammatory cells. • Metaplasia of pulp i. e. transformation to another tissue
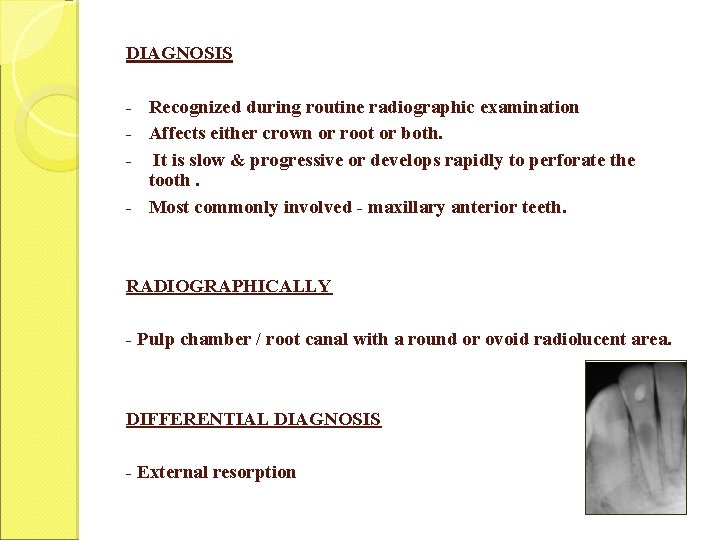
DIAGNOSIS - Recognized during routine radiographic examination - Affects either crown or root or both. - It is slow & progressive or develops rapidly to perforate the tooth. - Most commonly involved - maxillary anterior teeth. RADIOGRAPHICALLY - Pulp chamber / root canal with a round or ovoid radiolucent area. DIFFERENTIAL DIAGNOSIS - External resorption

TREATMENT - Extirpation of pulp, stops the internal resorptive process. - Routine endodontic treatment is indicated, but in advanced cases -calcium hydroxide paste dressing - Repair is completed when calcific barrier is present. - Later the canal with its defect is obturated with plasticized gutta percha. PROGNOSIS Is favourable, before perforation occurs.
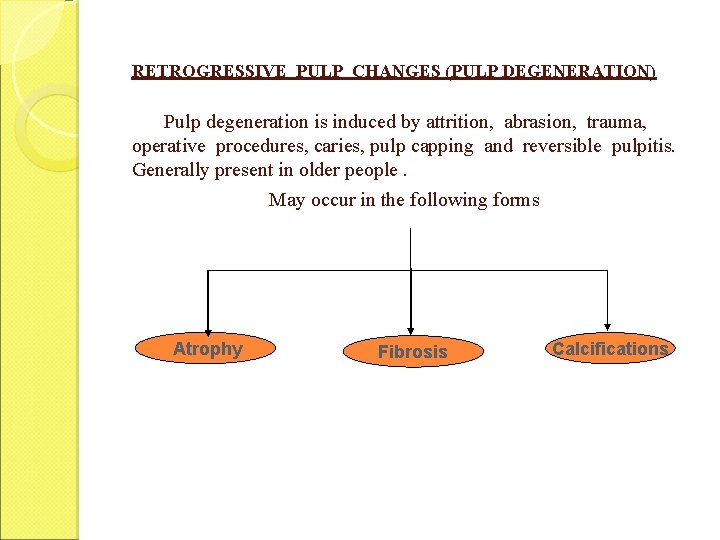
RETROGRESSIVE PULP CHANGES (PULP DEGENERATION) Pulp degeneration is induced by attrition, abrasion, trauma, operative procedures, caries, pulp capping and reversible pulpitis. Generally present in older people. May occur in the following forms Atrophy Fibrosis Calcifications
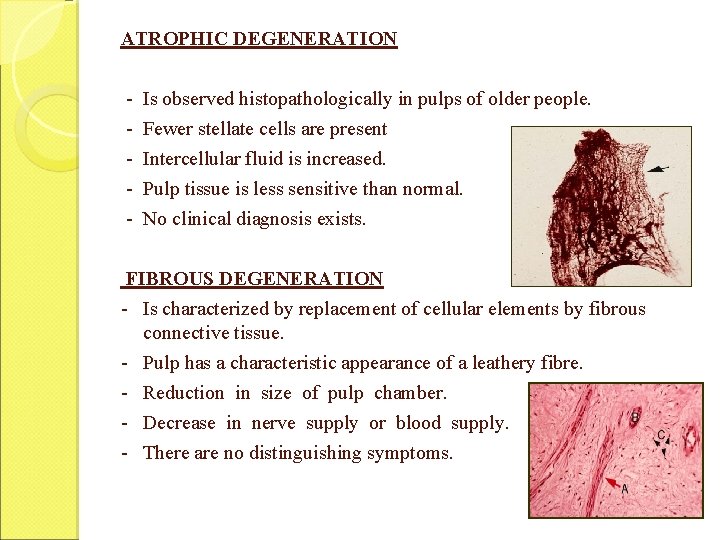
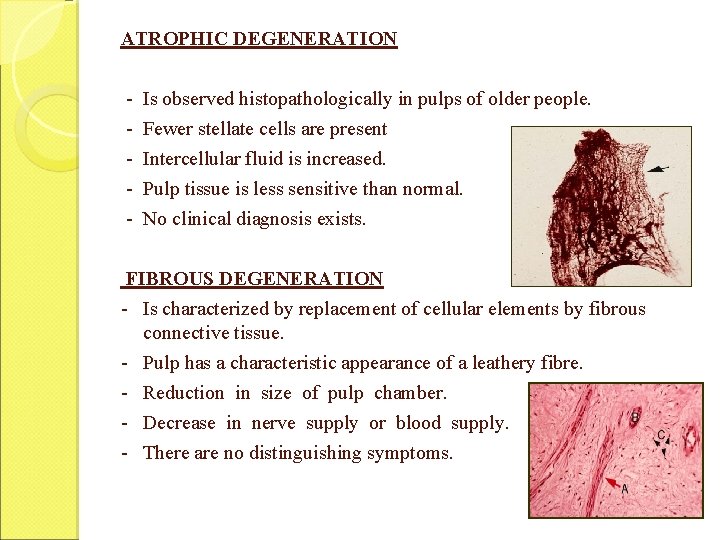
ATROPHIC DEGENERATION - Is observed histopathologically in pulps of older people. - Fewer stellate cells are present - Intercellular fluid is increased. - Pulp tissue is less sensitive than normal. - No clinical diagnosis exists. FIBROUS DEGENERATION - Is characterized by replacement of cellular elements by fibrous connective tissue. - Pulp has a characteristic appearance of a leathery fibre. - Reduction in size of pulp chamber. - Decrease in nerve supply or blood supply. - There are no distinguishing symptoms.
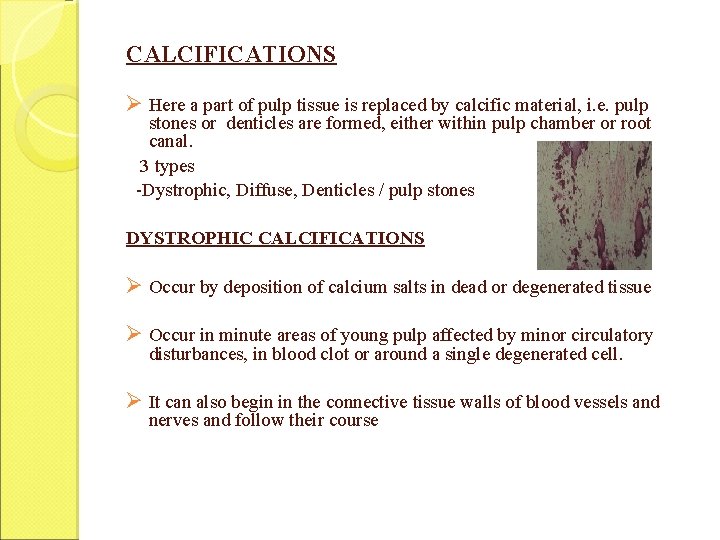
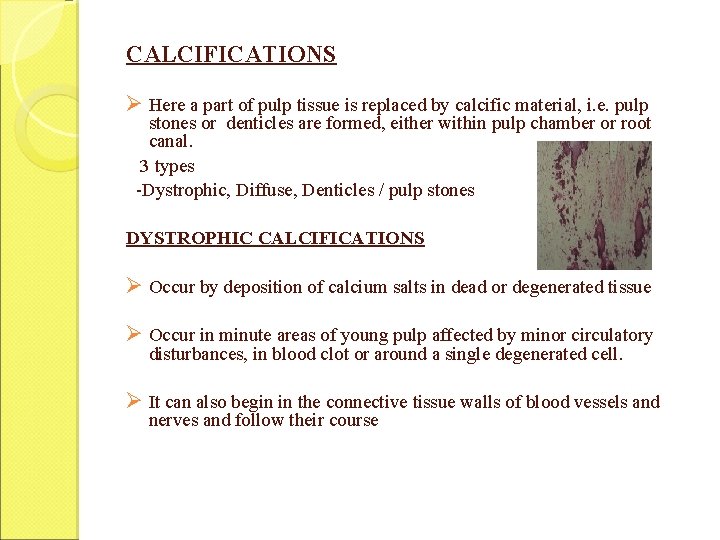
CALCIFICATIONS Ø Here a part of pulp tissue is replaced by calcific material, i. e. pulp stones or denticles are formed, either within pulp chamber or root canal. 3 types -Dystrophic, Diffuse, Denticles / pulp stones DYSTROPHIC CALCIFICATIONS Ø Occur by deposition of calcium salts in dead or degenerated tissue Ø Occur in minute areas of young pulp affected by minor circulatory disturbances, in blood clot or around a single degenerated cell. Ø It can also begin in the connective tissue walls of blood vessels and nerves and follow their course
DIFFUSE CALCIFICATIONS Ø Generally observed in root canals Ø The deposits become long, thin and fibrillar on fusing
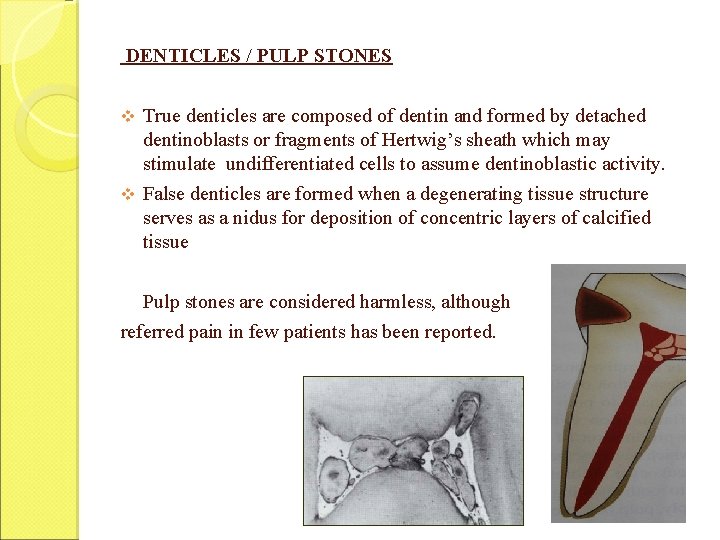
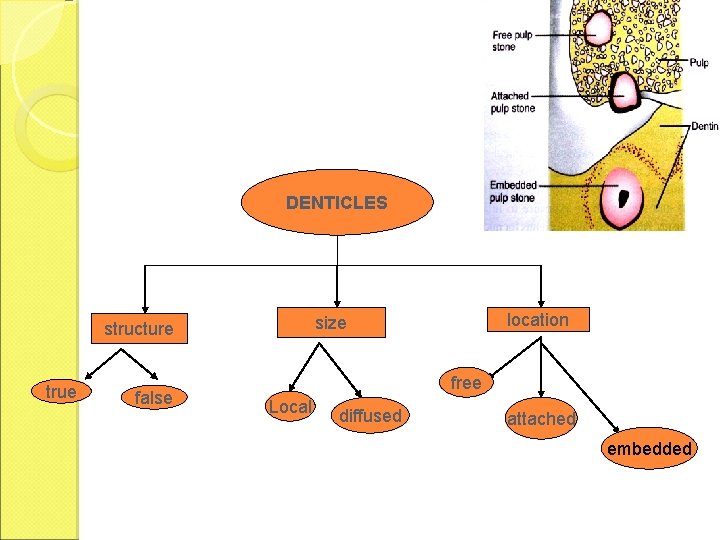
DENTICLES / PULP STONES v True denticles are composed of dentin and formed by detached dentinoblasts or fragments of Hertwig’s sheath which may stimulate undifferentiated cells to assume dentinoblastic activity. v False denticles are formed when a degenerating tissue structure serves as a nidus for deposition of concentric layers of calcified tissue Pulp stones are considered harmless, although referred pain in few patients has been reported.
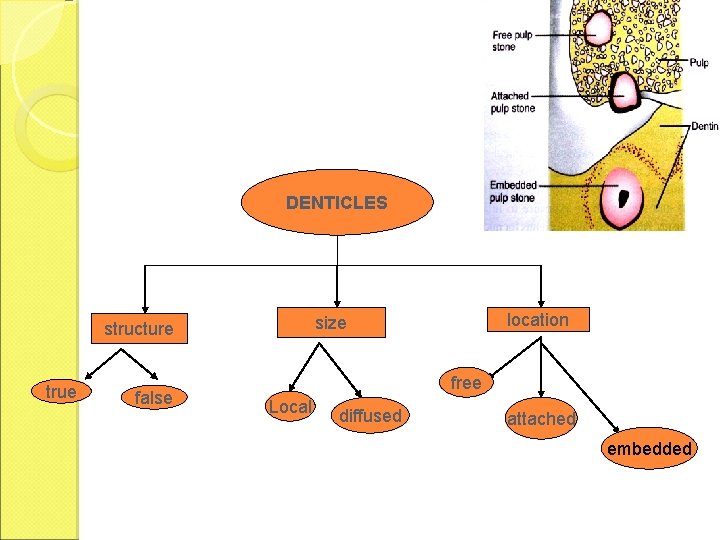
DENTICLES true false location size structure free Local diffused attached embedded
NECROSIS OF PULP Necrosis or death of the pulp tissue is a sequela of acute and chronic inflammation of the pulp or an immediate arrest of circulation by traumatic injury. - It may be partial or total. ETIOLOGY 1) As a Sequelae to inflammation 2) Bacteria, trauma and chemical irritation. : causing an ischaemic infarction & resulting in dry gangrenous necrotic pulp.
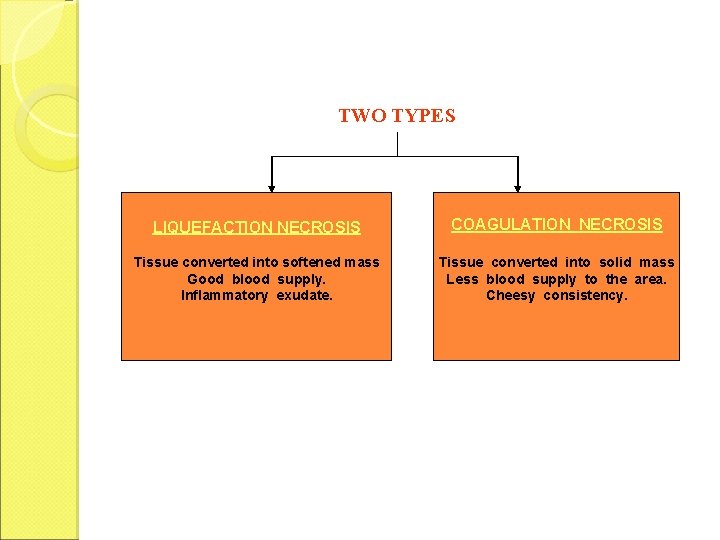
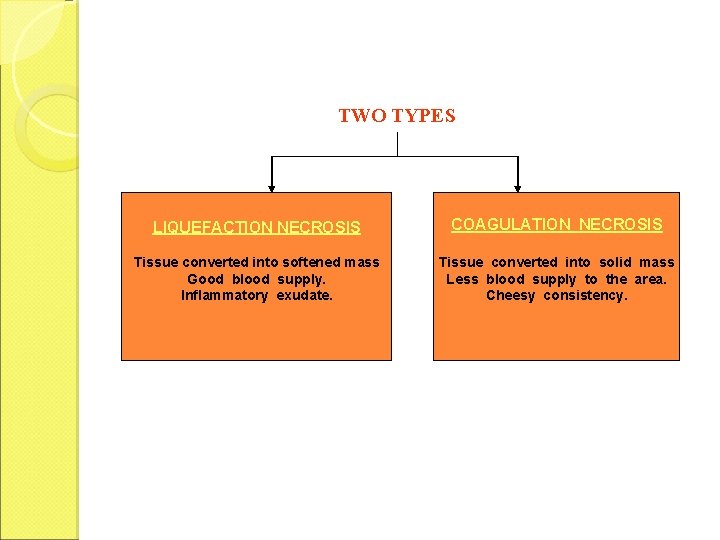
TWO TYPES LIQUEFACTION NECROSIS COAGULATION NECROSIS Tissue converted into softened mass Good blood supply. Inflammatory exudate. Tissue converted into solid mass Less blood supply to the area. Cheesy consistency.
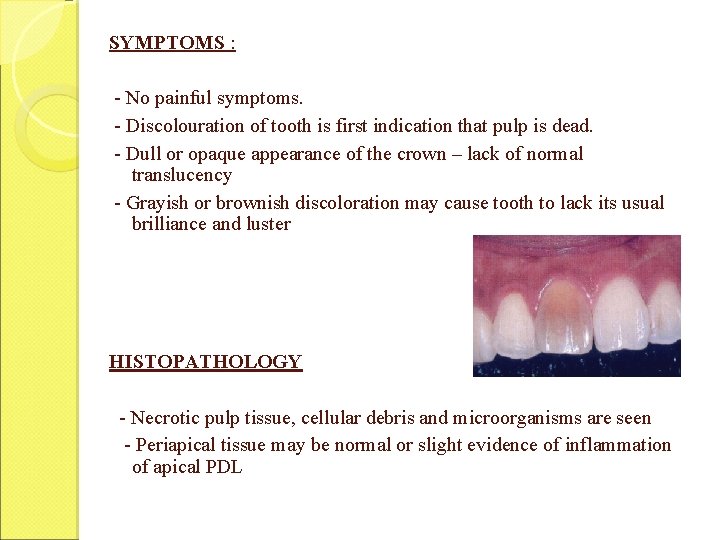
SYMPTOMS : - No painful symptoms. - Discolouration of tooth is first indication that pulp is dead. - Dull or opaque appearance of the crown – lack of normal translucency - Grayish or brownish discoloration may cause tooth to lack its usual brilliance and luster HISTOPATHOLOGY - Necrotic pulp tissue, cellular debris and microorganisms are seen - Periapical tissue may be normal or slight evidence of inflammation of apical PDL

POISONOUS INTERMEDIATE & END PRODUCTS FOUND IN NECROSIS 1. Intermediate proteolytic products that emit foul odour a. Indole and Skatole b. Putriscine and Cadaverine c. Indican 2. End products Hydrogen sulphide, ammonia, water, carbon dioxide & fatty acids 3. Exotoxins 4. Endotoxins 5. Foreign bacterial protein
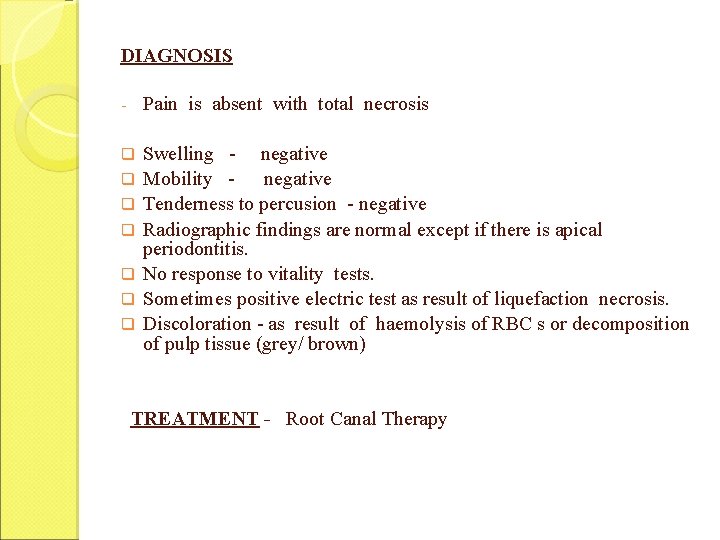
DIAGNOSIS - Pain is absent with total necrosis q Swelling - negative Mobility negative Tenderness to percusion - negative Radiographic findings are normal except if there is apical periodontitis. No response to vitality tests. Sometimes positive electric test as result of liquefaction necrosis. Discoloration - as result of haemolysis of RBC s or decomposition of pulp tissue (grey/ brown) q q q TREATMENT - Root Canal Therapy
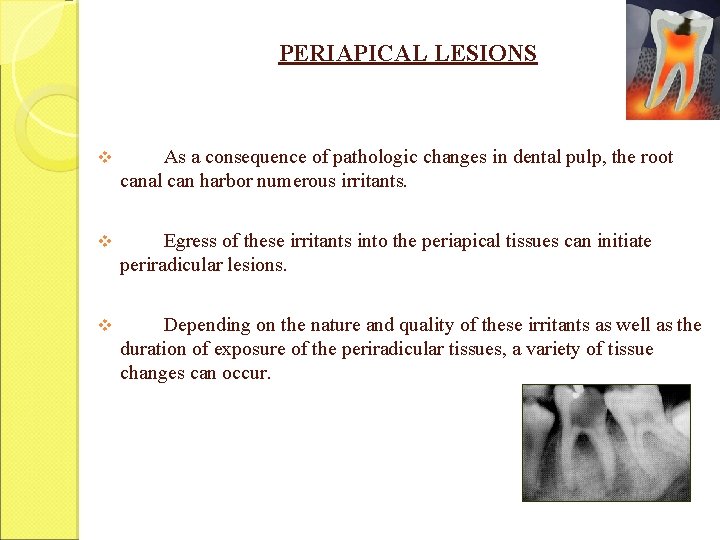
PERIAPICAL LESIONS v As a consequence of pathologic changes in dental pulp, the root canal can harbor numerous irritants. v Egress of these irritants into the periapical tissues can initiate periradicular lesions. v Depending on the nature and quality of these irritants as well as the duration of exposure of the periradicular tissues, a variety of tissue changes can occur.
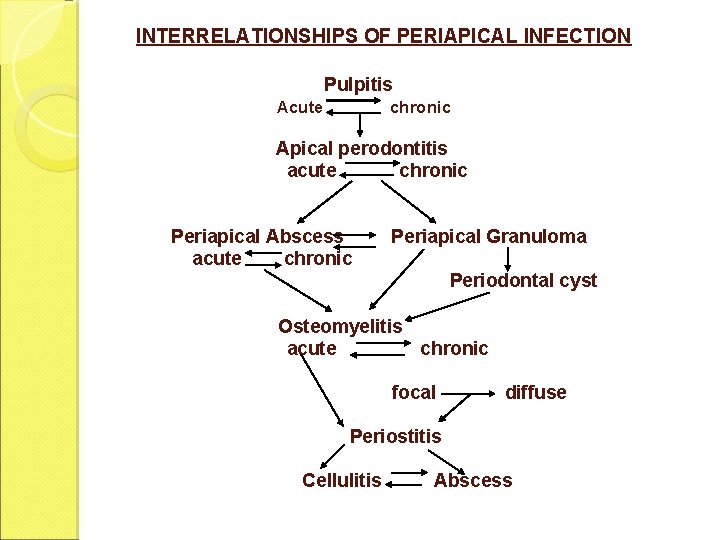
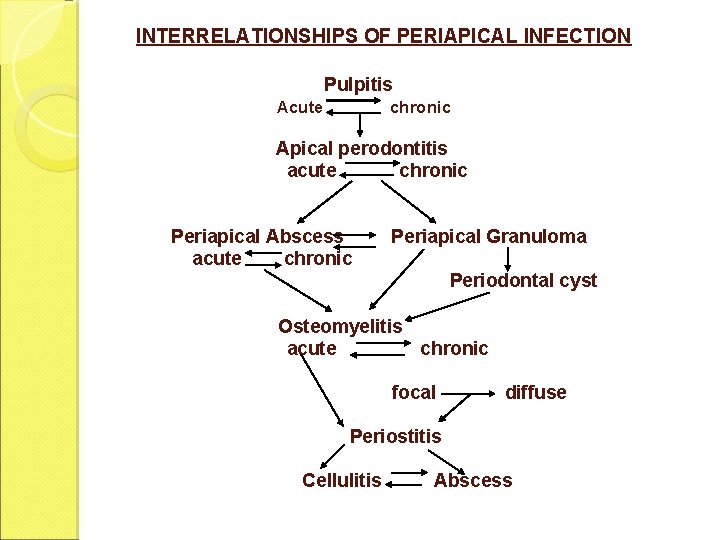
INTERRELATIONSHIPS OF PERIAPICAL INFECTION Pulpitis Acute chronic Apical perodontitis acute chronic Periapical Abscess acute chronic Periapical Granuloma Periodontal cyst Osteomyelitis acute chronic focal diffuse Periostitis Cellulitis Abscess
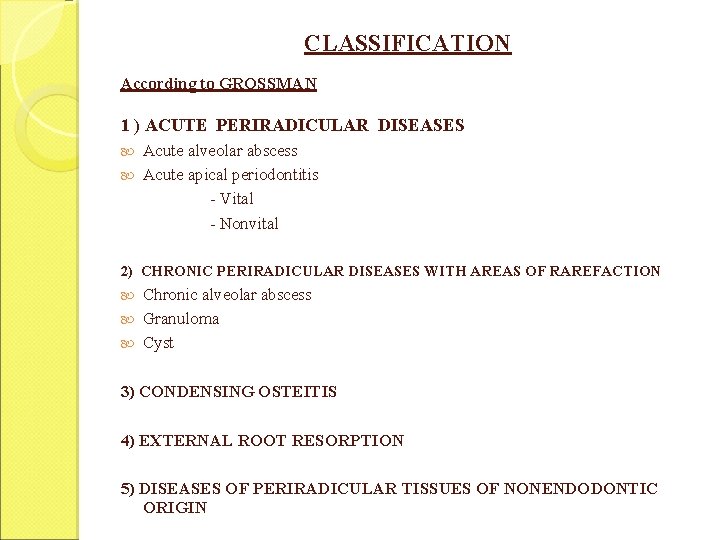
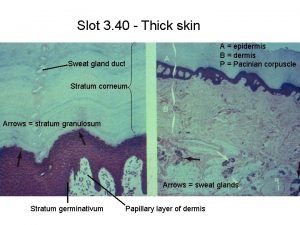
CLASSIFICATION According to GROSSMAN 1 ) ACUTE PERIRADICULAR DISEASES Acute alveolar abscess Acute apical periodontitis - Vital - Nonvital 2) CHRONIC PERIRADICULAR DISEASES WITH AREAS OF RAREFACTION Chronic alveolar abscess Granuloma Cyst 3) CONDENSING OSTEITIS 4) EXTERNAL ROOT RESORPTION 5) DISEASES OF PERIRADICULAR TISSUES OF NONENDODONTIC ORIGIN
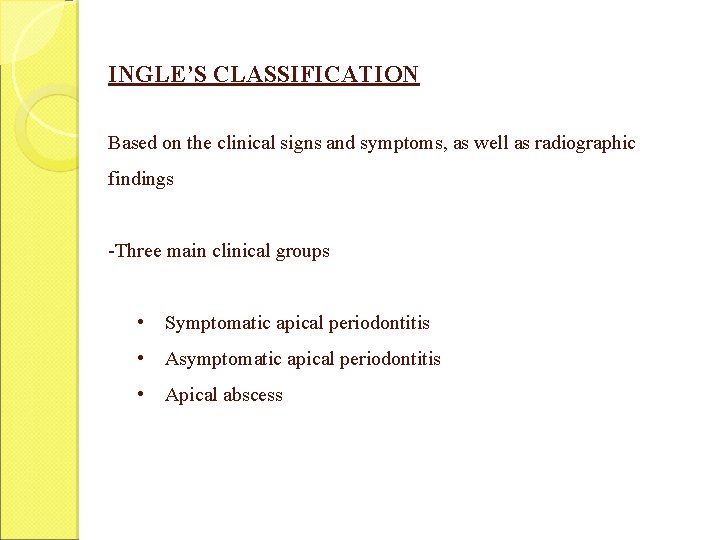
INGLE’S CLASSIFICATION Based on the clinical signs and symptoms, as well as radiographic findings -Three main clinical groups • Symptomatic apical periodontitis • Asymptomatic apical periodontitis • Apical abscess
![WEINES CLASSIFICATION PULPOPERIAPICAL DISEASE 1 PAINFUL PULPOPERIAPICAL PATHOSES a Incipient acute periapical periodontitis b WEINE’S CLASSIFICATION PULPOPERIAPICAL DISEASE: 1] PAINFUL PULPOPERIAPICAL PATHOSES a) Incipient acute periapical periodontitis b)](https://slidetodoc.com/presentation_image_h/b72453dd07ce656f37ac8bc5f3ea13b0/image-58.jpg)
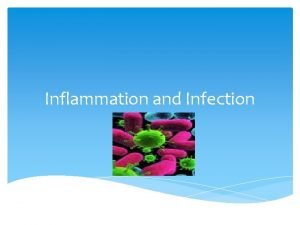
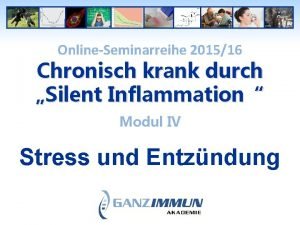
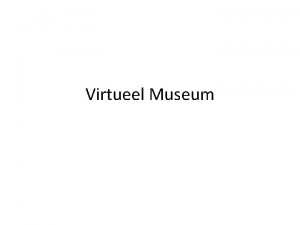
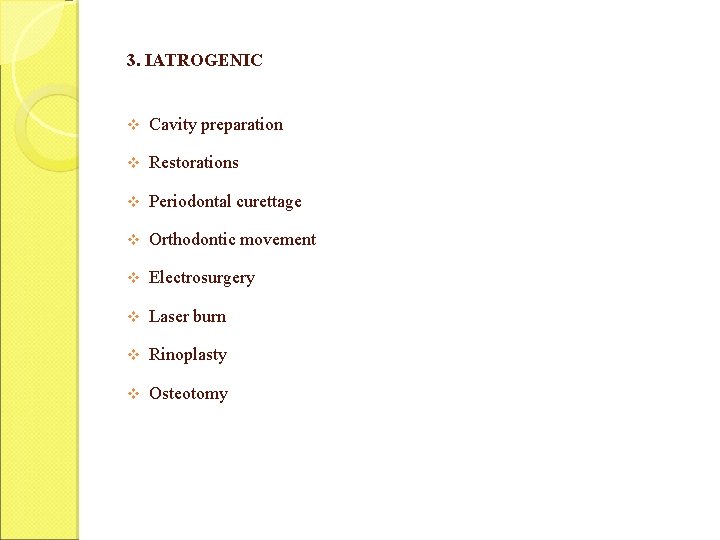
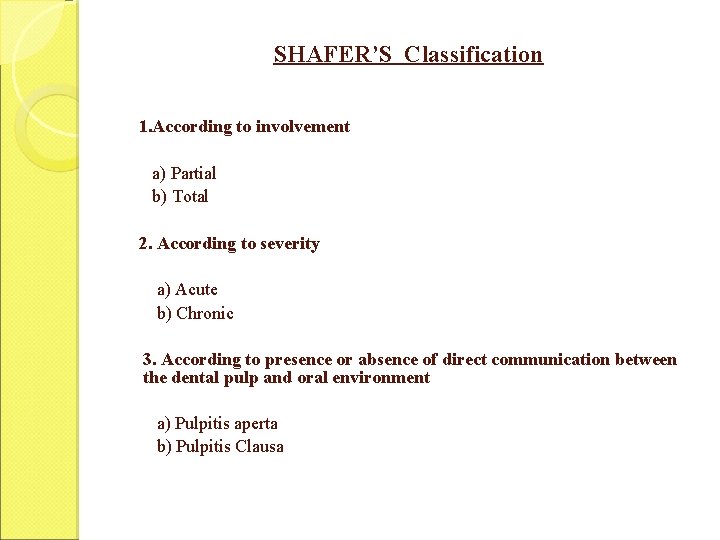
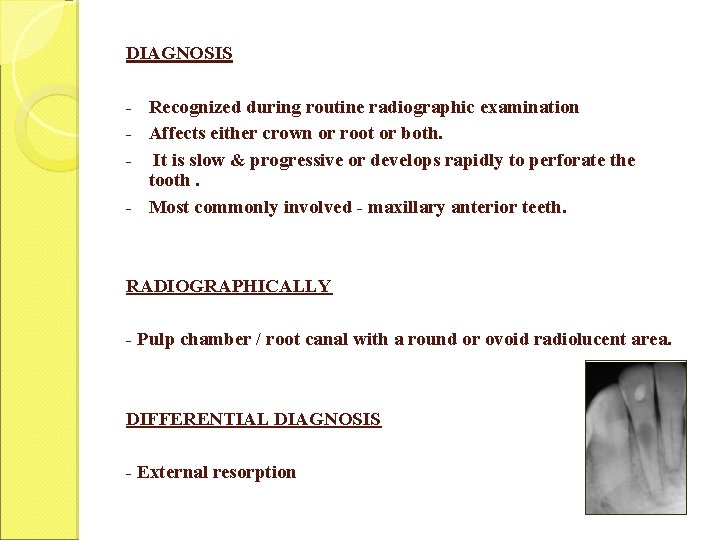
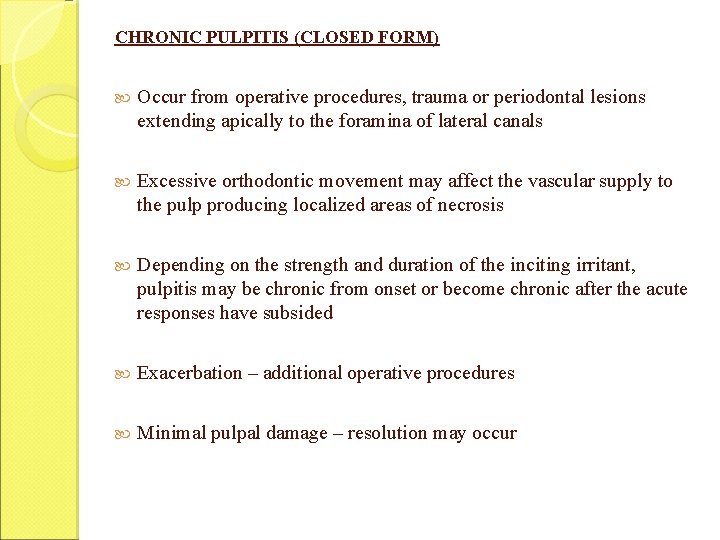
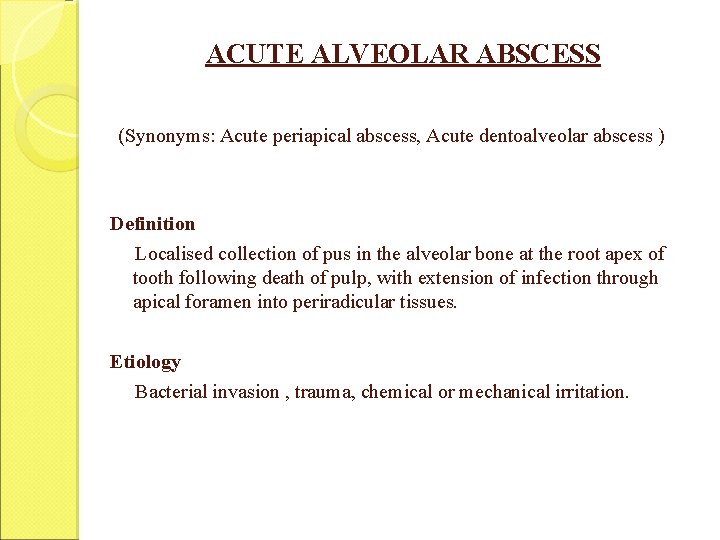
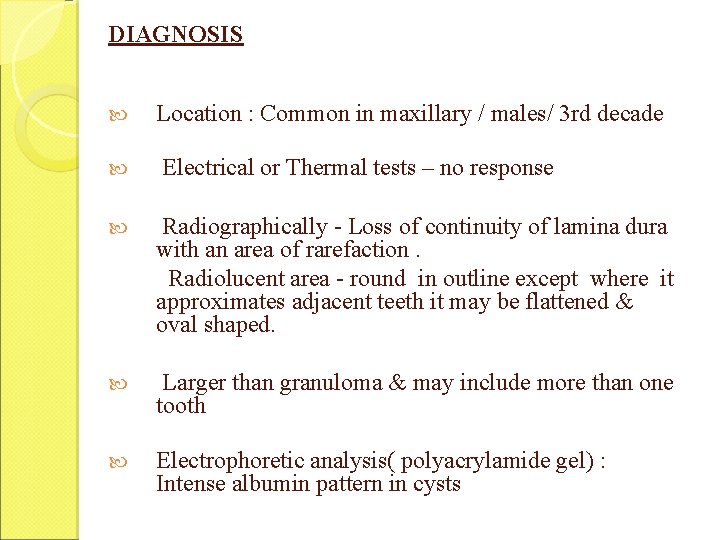
WEINE’S CLASSIFICATION PULPOPERIAPICAL DISEASE: 1] PAINFUL PULPOPERIAPICAL PATHOSES a) Incipient acute periapical periodontitis b) Advanced acute periapical periodontitis i. Acute periapical abscess ii. Recrudescent abscess iii. Subacute periapical abscess 2] NON PAINFUL PULPOPERIAPICAL PATHOSES a) Pulpoperiapical osteosclerosis b) Incipient chronic periapical periodontitis c) Advanced chronic periapical periodontitis i. Periapical granuloma ii. Chronic periapical abscess iii. Periapical cyst

WHO (1995) Classification: K 04. 4 -Acute apical periodontitis K 04. 5 -Chronic apical periodontitis (Apical granuloma) K 04. 6 -Periapical abscess with sinus K 04. 60 -Periapical abscess with sinus to maxillary antrum K 04. 61 -Periapical abscess with sinus to nasal cavity K 04. 62 -Periapical abscess with sinus to oral cavity K 04. 63 -Periapical abscess with sinus to skin K 04. 7 -Periapical abscess without sinus K 04. 8 -Radicular cyst (Apical periodontal cyst, Periapical cyst) K 04. 80 -Apical and lateral cyst K 04. 81 -Residual cyst K 04. 82 -Inflammatory paradental cyst
ACUTE ALVEOLAR ABSCESS (Synonyms: Acute periapical abscess, Acute dentoalveolar abscess ) Definition Localised collection of pus in the alveolar bone at the root apex of tooth following death of pulp, with extension of infection through apical foramen into periradicular tissues. Etiology Bacterial invasion , trauma, chemical or mechanical irritation.

HISTOPATHOLOGY PMN’S infiltration Accumulation of inflammatory exudates Distention of PDL Prosses continues, PDL separates Mobile tooth Bone resorption at apex Liquefaction necrosis containing PMN’S , debris, cell remnants & purulent exudates

SYMPTOMS First symptom - tenderness Later - patient has severe throbbing pain with swelling of the overlying soft tissue As the infection progresses, swelling becomes more pronounced and extends beyond the original site Tooth becomes more painful, elongated and mobile If untreated - progresses to osteitis, periostitis, cellulitis or osteomyelitis Sinus tract - opens to buccal mucosa
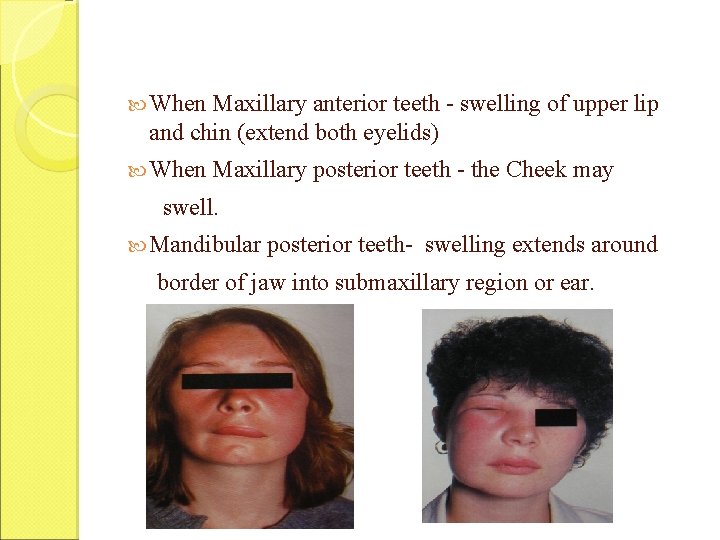
When Maxillary anterior teeth - swelling of upper lip and chin (extend both eyelids) When Maxillary posterior teeth - the Cheek may swell. Mandibular posterior teeth- swelling extends around border of jaw into submaxillary region or ear.
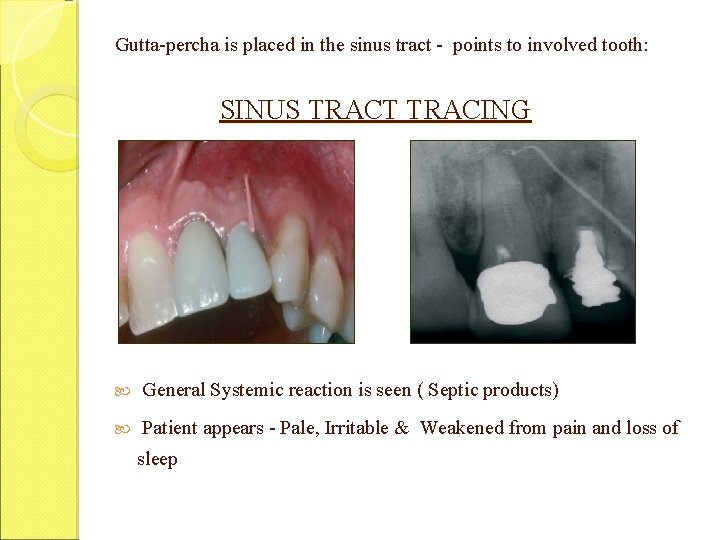
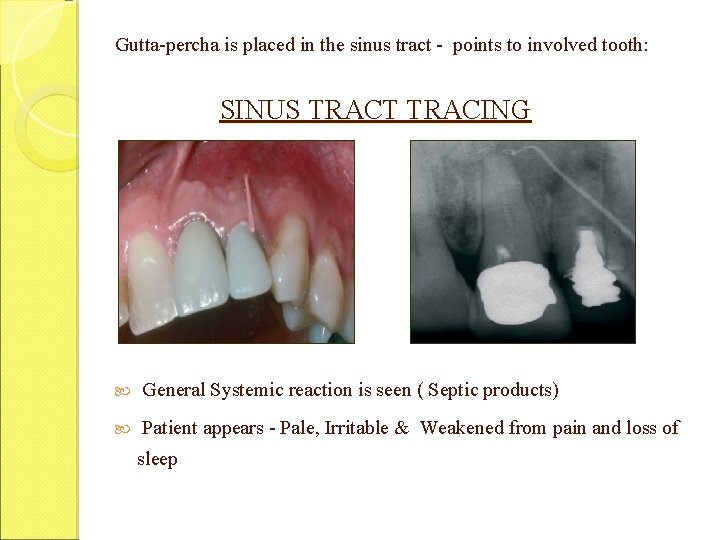
Gutta-percha is placed in the sinus tract - points to involved tooth: SINUS TRACT TRACING General Systemic reaction is seen ( Septic products) Patient appears - Pale, Irritable & Weakened from pain and loss of sleep

DIAGNOSIS § Early stage - difficult to locate tooth. § Once infection progresses to process of periodontitis & extrusion, a radiographic evaluation shows thickening of periodontal ligament space & breakdown of bone § Electric test & thermal tests: No response § Tooth is tender on percussion § Apical mucosa is tender on palpation § Tooth may be mobile & extruded. DIFFERENTIAL DIAGNOSIS Periodontal abscess & Irreversible pulpitis
Treatment: Establish drainage & control systemic infection. ON FIRST VISIT : Tooth is left open for drainage. Thorough instrumentation & irrigation before medicating and sealing. Once the swelling and pain subsides endodontic treatment is done. If diffuse swelling : Antibiotic coverage is prescribed along with hot mouth rinse, Once area is localised, incision and drainage is instituted
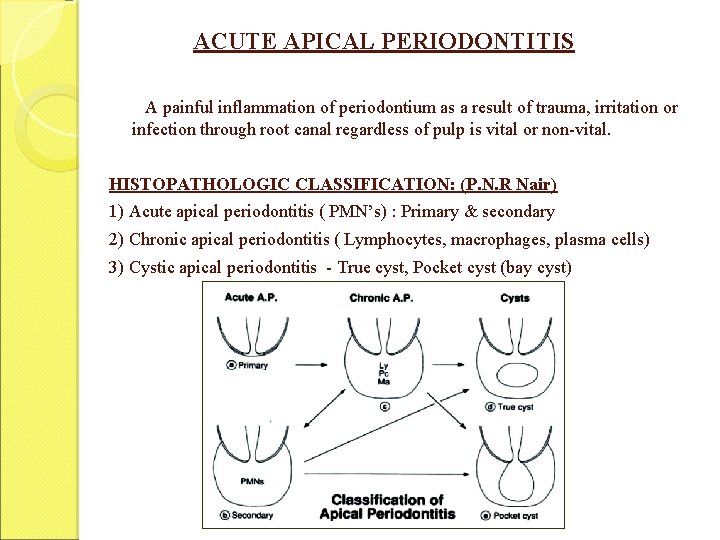
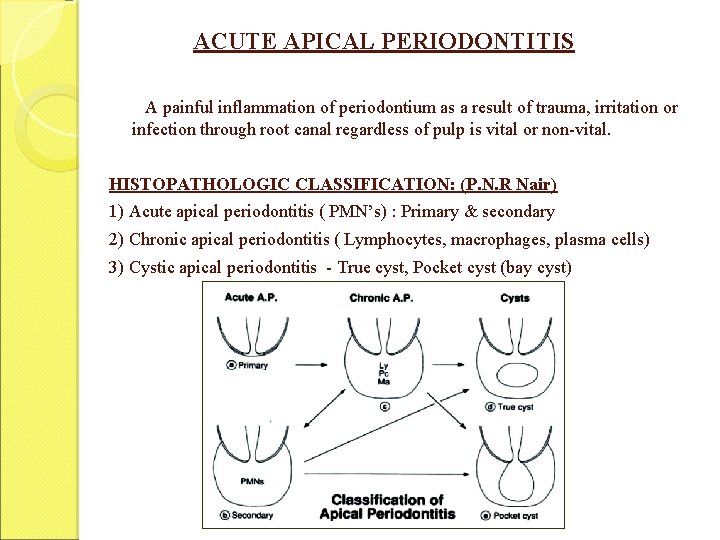
ACUTE APICAL PERIODONTITIS A painful inflammation of periodontium as a result of trauma, irritation or infection through root canal regardless of pulp is vital or non-vital. HISTOPATHOLOGIC CLASSIFICATION: (P. N. R Nair) 1) Acute apical periodontitis ( PMN’s) : Primary & secondary 2) Chronic apical periodontitis ( Lymphocytes, macrophages, plasma cells) 3) Cystic apical periodontitis - True cyst, Pocket cyst (bay cyst)

APICAL PERIODONTITIS:
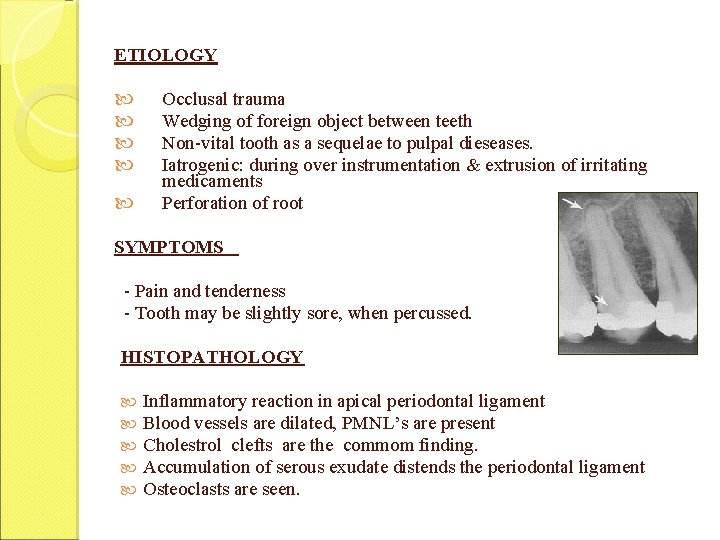
ETIOLOGY Occlusal trauma Wedging of foreign object between teeth Non-vital tooth as a sequelae to pulpal dieseases. Iatrogenic: during over instrumentation & extrusion of irritating medicaments Perforation of root SYMPTOMS - Pain and tenderness - Tooth may be slightly sore, when percussed. HISTOPATHOLOGY Inflammatory reaction in apical periodontal ligament Blood vessels are dilated, PMNL’s are present Cholestrol clefts are the commom finding. Accumulation of serous exudate distends the periodontal ligament Osteoclasts are seen.
DIAGNOSIS Tooth is tender to percussion Symptoms are due to Overinstrumentation, Irritating medicament or Overfilling Radiographically: thickened periodontal ligament or small area of rarefaction TREATMENT Endodontic therapy v Postoperative pain is controlled analgesics & antibiotics v Hyper-occlusion relieve the occlusion. v
ACUTE EXACERBATION OF A CHRONIC LESION (PHOENIX ABSCESS) An acute inflammatory reaction superimposed on an existing chronic lesion, such as a cyst or granuloma ETIOLOGY 1. 2. 3. 4. Noxious stimuli from a diseased pulp with chronic periradicular disease. Because of influx of necrotic products or bacteria and their toxins, the dormant lesions may become reactive & cause an acute inflammatory response. Lowering of the body's defenses in the presence of bacteria - may also trigger an acute inflammatory response. Mechanical irritation during root canal instrumentation SYMPTOMS Tooth - tender to touch & elevated in its socket Mucosa - sensitive to palpation & appears red & swollen
HISTOPATHOLOGY : Liquefaction necrosis with disintegrating PMNL & cellular debris (pus), surrounded by infiltration of macrophages, lymphocytes & plasma cells DIAGNOSIS History of patient vitality tests Lack of response RADIOGRAPHICALLY : - Large area of radiolucency at the apex.
DIFFERENTIAL DIAGNOSIS : Acute alveolar abscess, Acute irreversible pulpitis TREATMENT Establishment of drainage Once symptoms subside - RCT
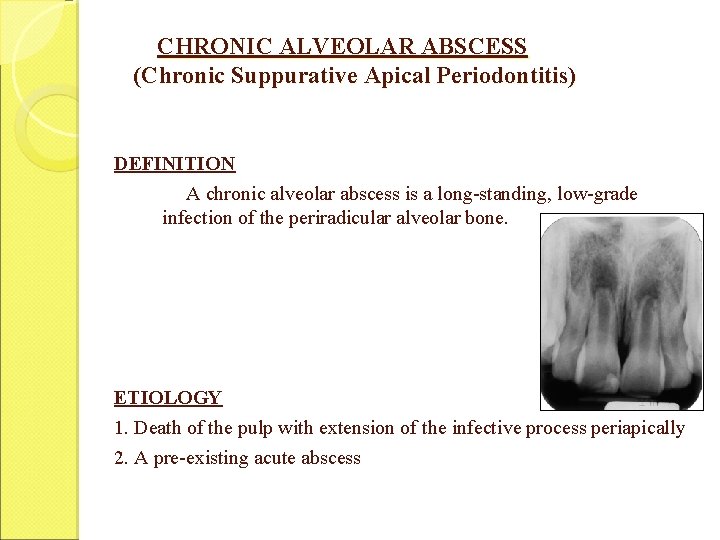
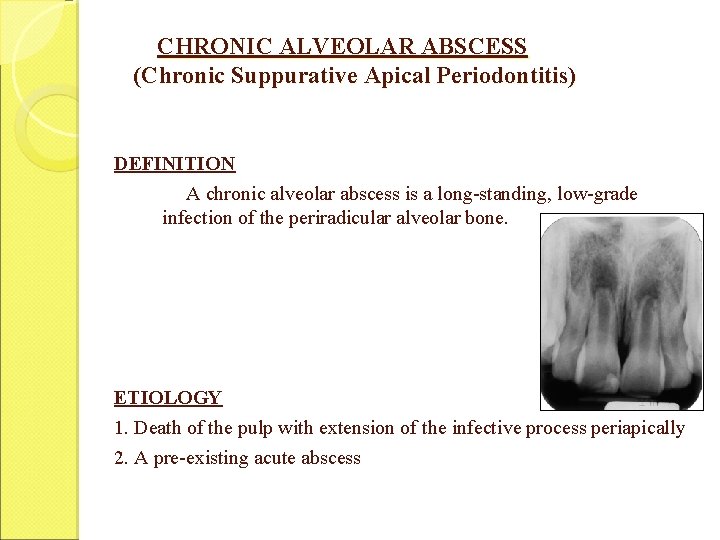
CHRONIC ALVEOLAR ABSCESS (Chronic Suppurative Apical Periodontitis) DEFINITION A chronic alveolar abscess is a long-standing, low-grade infection of the periradicular alveolar bone. ETIOLOGY 1. Death of the pulp with extension of the infective process periapically 2. A pre-existing acute abscess
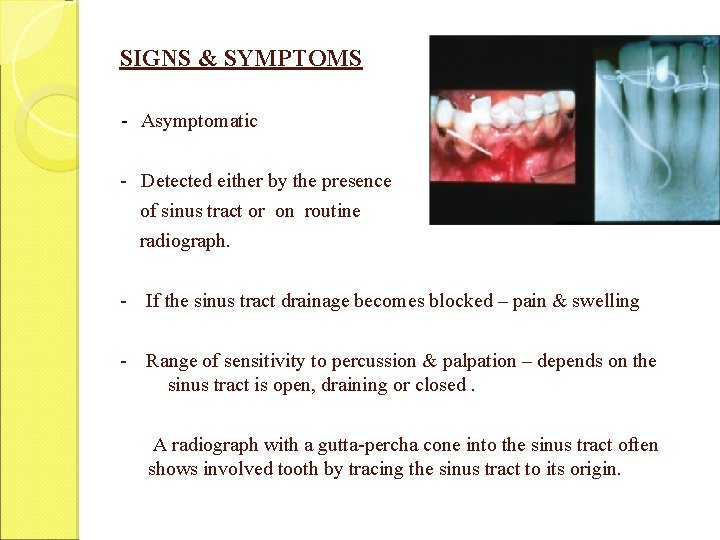
SIGNS & SYMPTOMS - Asymptomatic - Detected either by the presence of sinus tract or on routine radiograph. - If the sinus tract drainage becomes blocked – pain & swelling - Range of sensitivity to percussion & palpation – depends on the sinus tract is open, draining or closed. A radiograph with a gutta-percha cone into the sinus tract often shows involved tooth by tracing the sinus tract to its origin.

DIAGNOSIS Chronic abscess may be painless or mildly painful. First sign - osseous breakdown (radiographically) seen during routine examination. Patient may give the history of sudden sharp pain which subsided & has not reoccurred. Clinically -A large carious exposure, composite, acrylic or metallic restoration or discolouration of crown of tooth. RADIOGRAPHICALLY A diffuse area of bone rarefaction Periodontal ligament is thickened. Vitality tests – Negative

HISTOPATHOLOGY Periodontal fibers at root apex are detached / lost. Apical cementum may be affected. Lymphocytes , plasma cells at the periphery & PMNL’s at the center Fibroblasts - form a capsule at periphery. TREATMENT Endodontic thearpy. The sinus tract ultimately heals by granulation When sinus tract does not heal while the tooth is under endodontic treatment, it is curetted with a small spoon excavator.
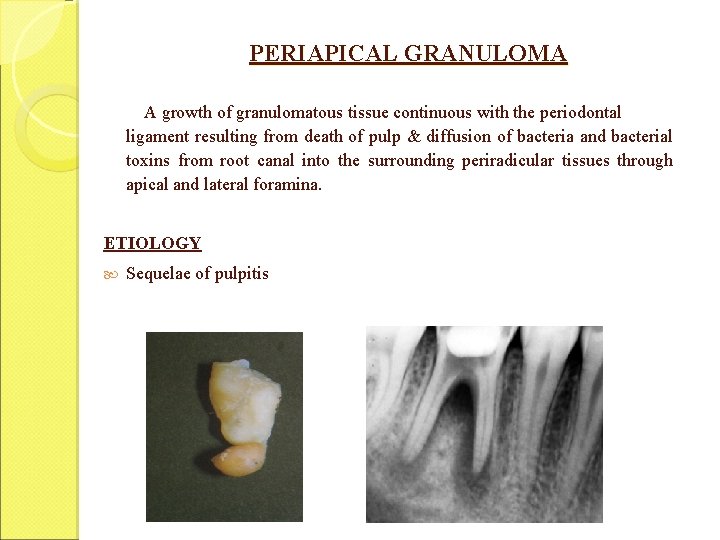
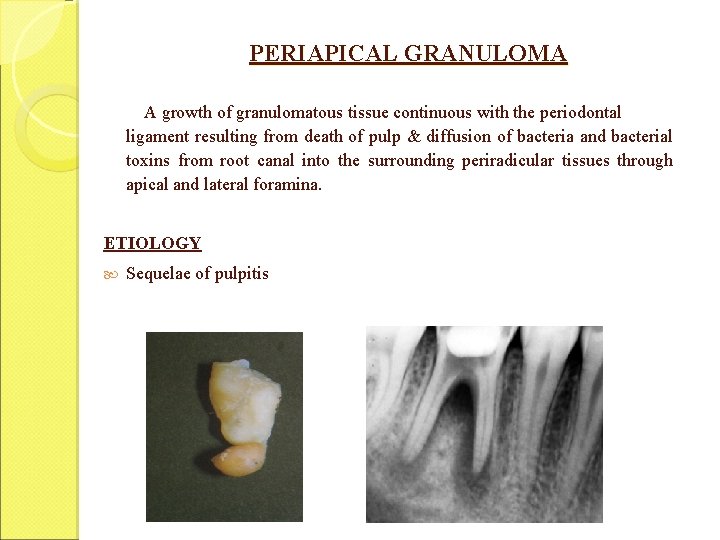
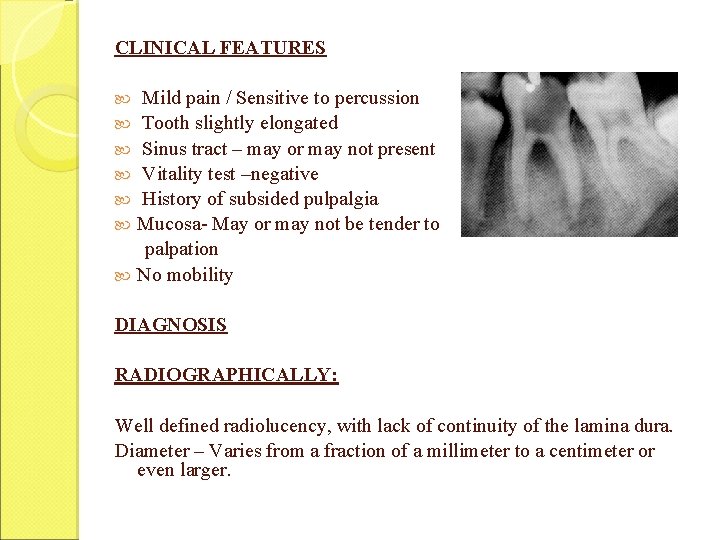
PERIAPICAL GRANULOMA A growth of granulomatous tissue continuous with the periodontal ligament resulting from death of pulp & diffusion of bacteria and bacterial toxins from root canal into the surrounding periradicular tissues through apical and lateral foramina. ETIOLOGY Sequelae of pulpitis
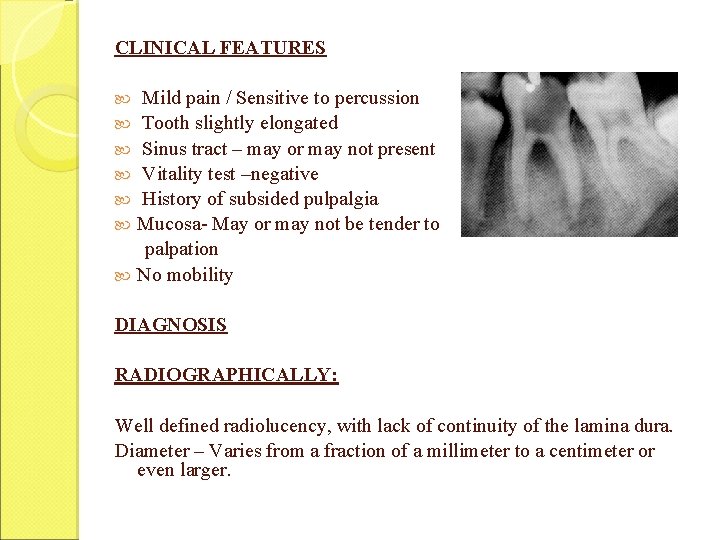
CLINICAL FEATURES Mild pain / Sensitive to percussion Tooth slightly elongated Sinus tract – may or may not present Vitality test –negative History of subsided pulpalgia Mucosa- May or may not be tender to palpation No mobility DIAGNOSIS RADIOGRAPHICALLY: Well defined radiolucency, with lack of continuity of the lamina dura. Diameter – Varies from a fraction of a millimeter to a centimeter or even larger.
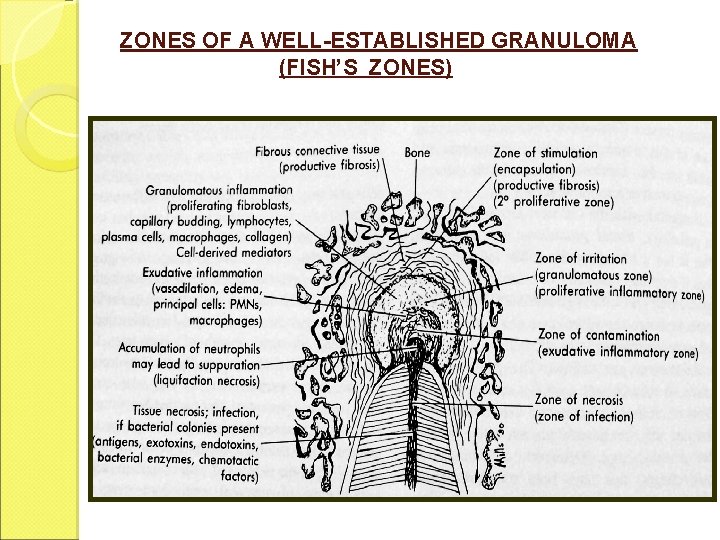
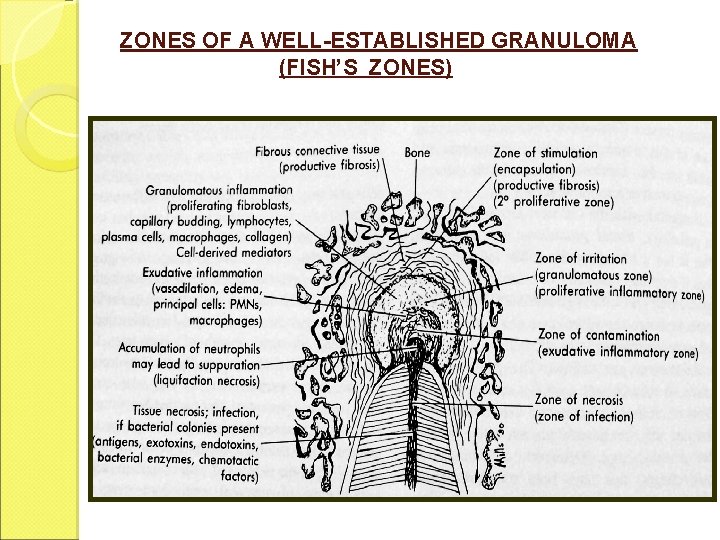
ZONES OF A WELL-ESTABLISHED GRANULOMA (FISH’S ZONES)

KRONFELD’S MOUNTAIN PASS CONCEPT Kronfeld : Granuloma is not an environment in which bacteria live but one in which they are destroyed. Bacteria (zone I) – compares bacteria in the root canals with an army entrenched behind high and inaccessible mountains Foramina : Mountain passes. Granulomatous (proliferative) tissue : mobilized army defending plains (periapex) from invaders. Major battle (b/w invaders + WBC’s) - acute inflammation (zone II) Local destruction created by battle is repaired (granulation tissue - zone III) and the environment returns to the normal pattern.
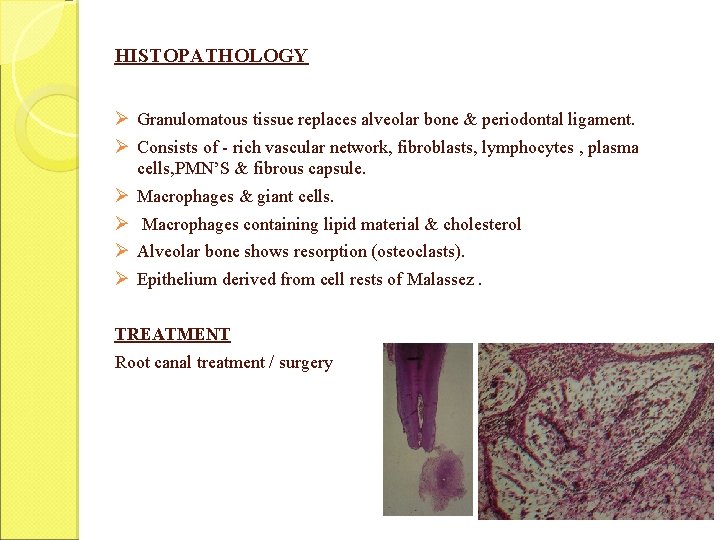
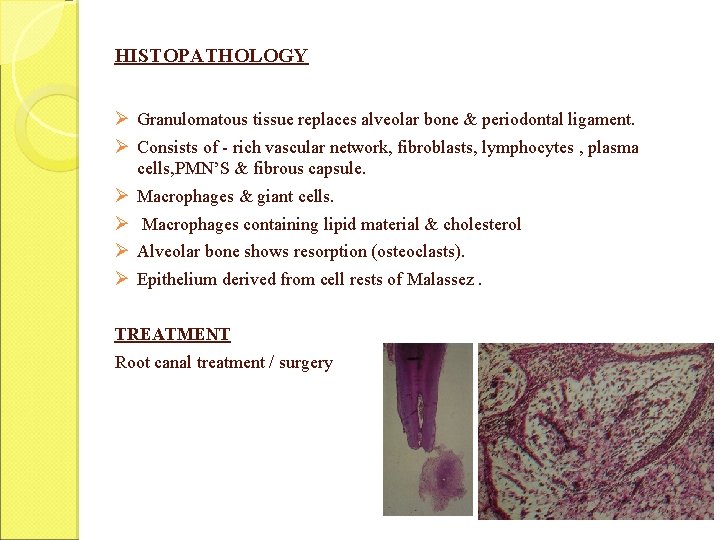
HISTOPATHOLOGY Ø Granulomatous tissue replaces alveolar bone & periodontal ligament. Ø Consists of - rich vascular network, fibroblasts, lymphocytes , plasma cells, PMN’S & fibrous capsule. Ø Ø Macrophages & giant cells. Macrophages containing lipid material & cholesterol Alveolar bone shows resorption (osteoclasts). Epithelium derived from cell rests of Malassez. TREATMENT Root canal treatment / surgery
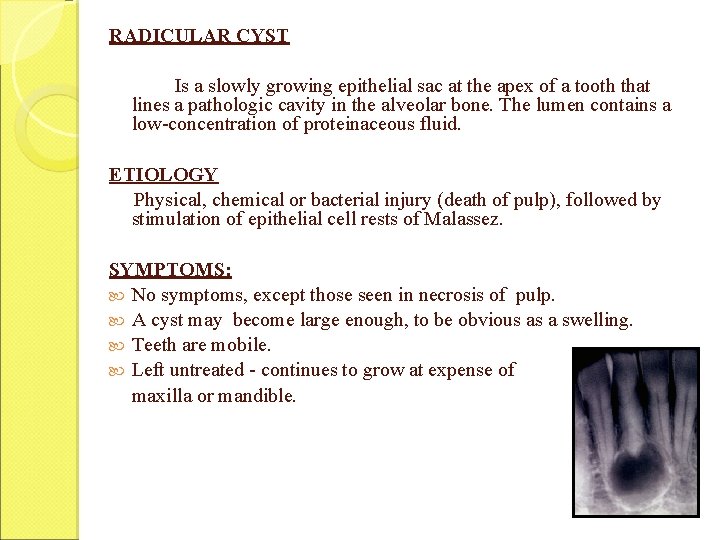
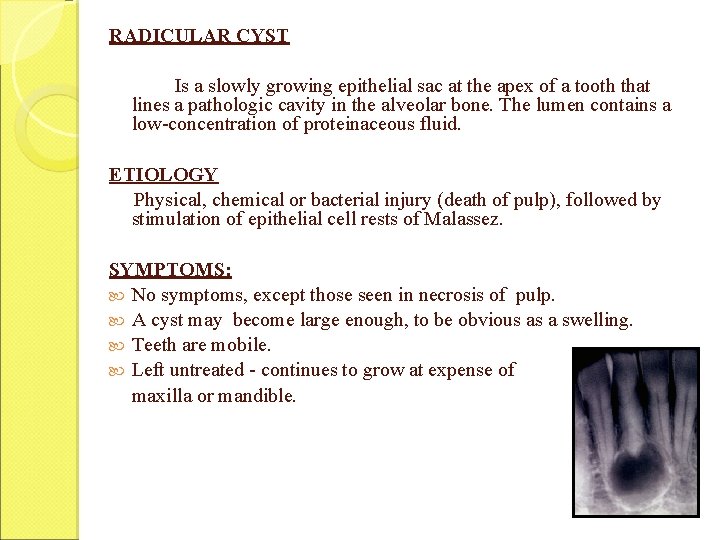
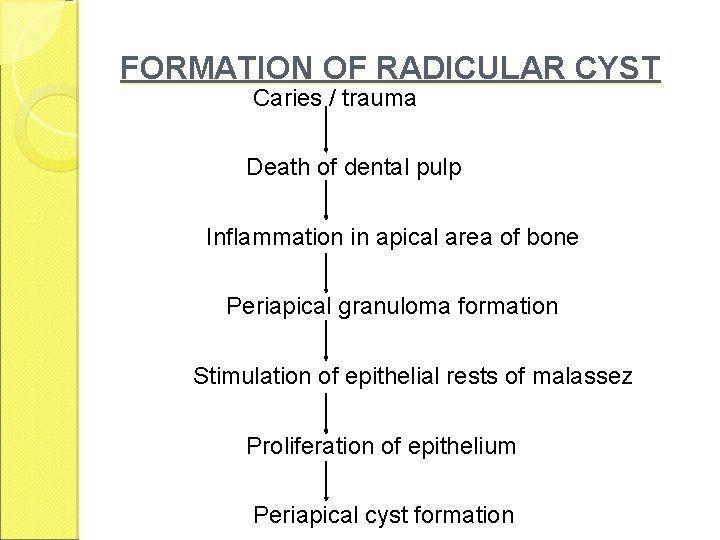
RADICULAR CYST Is a slowly growing epithelial sac at the apex of a tooth that lines a pathologic cavity in the alveolar bone. The lumen contains a low-concentration of proteinaceous fluid. ETIOLOGY Physical, chemical or bacterial injury (death of pulp), followed by stimulation of epithelial cell rests of Malassez. SYMPTOMS: No symptoms, except those seen in necrosis of pulp. A cyst may become large enough, to be obvious as a swelling. Teeth are mobile. Left untreated - continues to grow at expense of maxilla or mandible.
FORMATION OF RADICULAR CYST Caries / trauma Death of dental pulp Inflammation in apical area of bone Periapical granuloma formation Stimulation of epithelial rests of malassez Proliferation of epithelium Periapical cyst formation
DIAGNOSIS Location : Common in maxillary / males/ 3 rd decade Electrical or Thermal tests – no response Radiographically - Loss of continuity of lamina dura with an area of rarefaction. Radiolucent area - round in outline except where it approximates adjacent teeth it may be flattened & oval shaped. Larger than granuloma & may include more than one tooth Electrophoretic analysis( polyacrylamide gel) : Intense albumin pattern in cysts
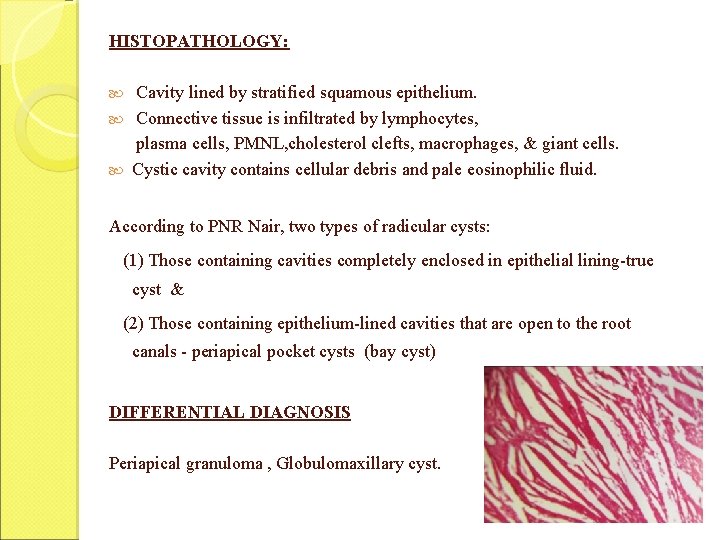
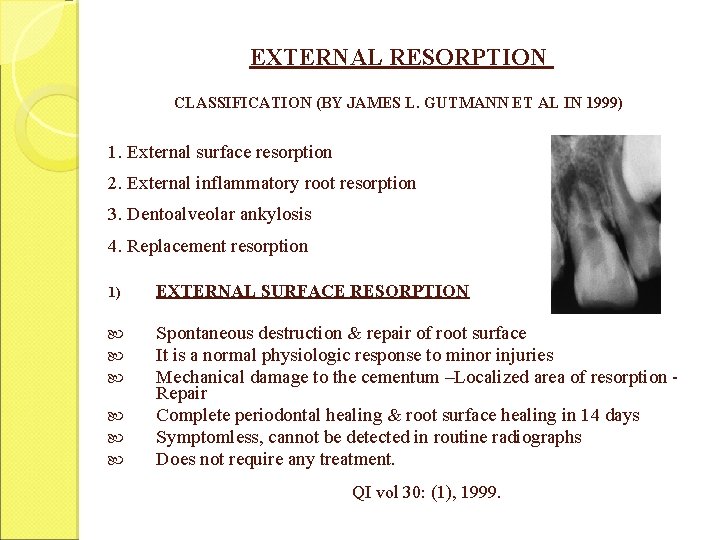
HISTOPATHOLOGY: Cavity lined by stratified squamous epithelium. Connective tissue is infiltrated by lymphocytes, plasma cells, PMNL, cholesterol clefts, macrophages, & giant cells. Cystic cavity contains cellular debris and pale eosinophilic fluid. According to PNR Nair, two types of radicular cysts: (1) Those containing cavities completely enclosed in epithelial lining-true cyst & (2) Those containing epithelium-lined cavities that are open to the root canals - periapical pocket cysts (bay cyst) DIFFERENTIAL DIAGNOSIS Periapical granuloma , Globulomaxillary cyst.

TRUE CYST POCKET

TREATMENT True cyst : Root canal treatment of the affected tooth, together with surgical enucleation may be attempted. Pocket cyst : Conventional RCT, followed by periodic observation.

CHRONIC PERIRADICULAR DISEASE WITH AREA OF CONDENSATION CONDENSING OSTEITIS Condensing osteitis is the response to a low-grade, chronic inflammation of periradicular area as a result of a mild irritation through the root canal. Characterized as a localized overproduction of apical bone. ETIOLOGY Mild irritation from pulpal disease - stimulates osteoblastic activity SYMPTOMS Usually asymptomatic , discovered during routine radiographic examination.
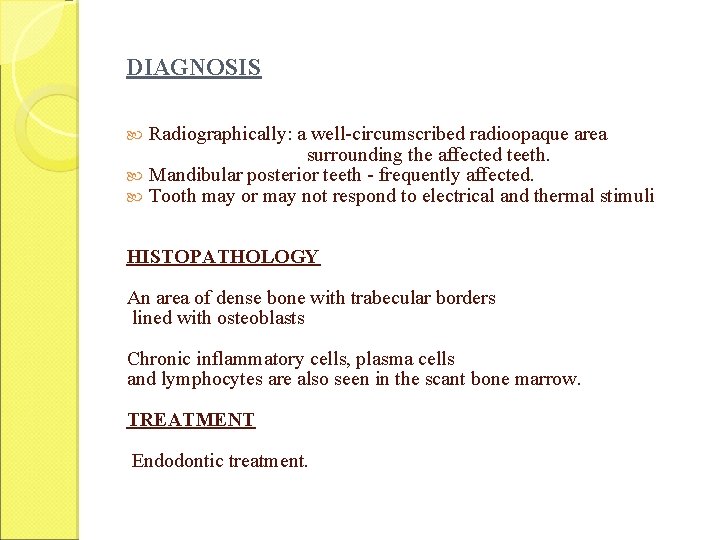
DIAGNOSIS Radiographically: a well-circumscribed radioopaque area surrounding the affected teeth. Mandibular posterior teeth - frequently affected. Tooth may or may not respond to electrical and thermal stimuli HISTOPATHOLOGY An area of dense bone with trabecular borders lined with osteoblasts Chronic inflammatory cells, plasma cells and lymphocytes are also seen in the scant bone marrow. TREATMENT Endodontic treatment.
EXTERNAL RESORPTION CLASSIFICATION (BY JAMES L. GUTMANN ET AL IN 1999) 1. External surface resorption 2. External inflammatory root resorption 3. Dentoalveolar ankylosis 4. Replacement resorption 1) EXTERNAL SURFACE RESORPTION Spontaneous destruction & repair of root surface It is a normal physiologic response to minor injuries Mechanical damage to the cementum –Localized area of resorption Repair Complete periodontal healing & root surface healing in 14 days Symptomless, cannot be detected in routine radiographs Does not require any treatment. QI vol 30: (1), 1999.
2) EXTERNAL INFLAMMATORY ROOT RESORPTION Injury or irritation to periodontal tissues where inflammation is beyond repair. ETIOLOGY Trauma Orthodontic tooth movement - excessive forces. Trauma from occlusion Periodontal pathology Avulsion & Luxation injuries CLINICAL FEATURES H/o trauma Necrotic pulp / irreversible pulpitis Tooth mobility Percussion sensitivity If resorption communicates with gingival sulcus- leads to pocket formation
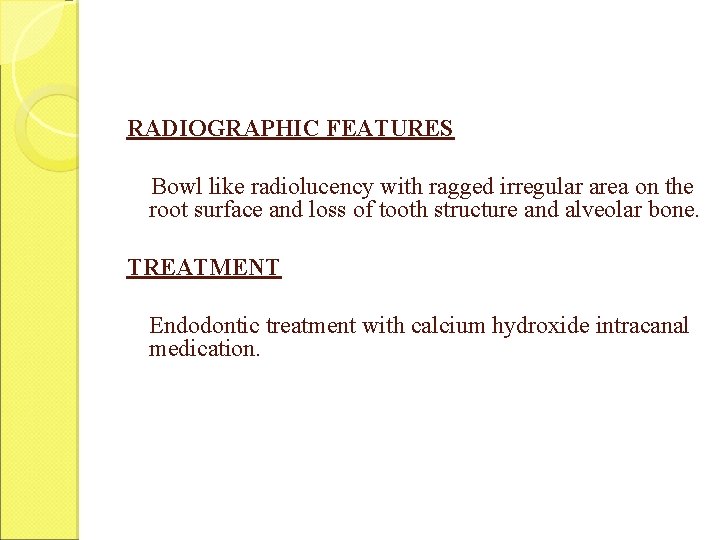
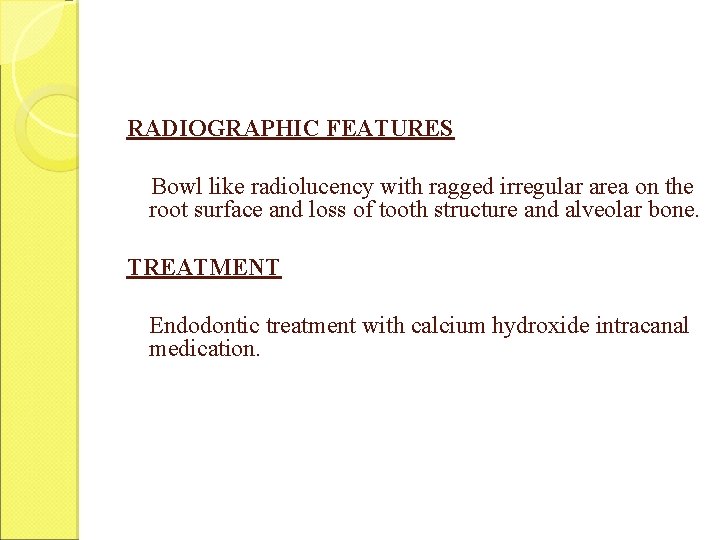
RADIOGRAPHIC FEATURES Bowl like radiolucency with ragged irregular area on the root surface and loss of tooth structure and alveolar bone. TREATMENT Endodontic treatment with calcium hydroxide intracanal medication.
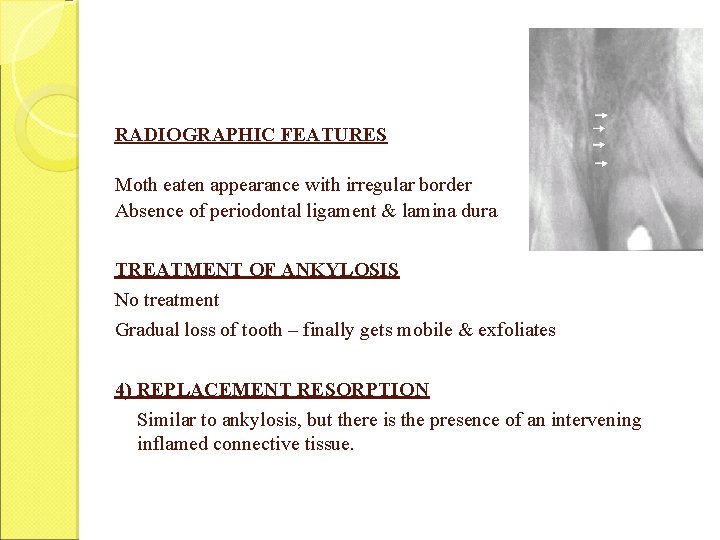
3) DENTOALVEOLAR ANKYLOSIS Union of tooth & bone with no intervening periodontal ligament & connective tissue ETIOLOGY Trauma, Intrusive luxation, Reimplantation of avulsed tooth (damage to PL cells & cementum) CLINICAL FEATURES Lack of mobility , Lack of mesial drift Dull metallic sound on percussion Infraocclusion
RADIOGRAPHIC FEATURES Moth eaten appearance with irregular border Absence of periodontal ligament & lamina dura TREATMENT OF ANKYLOSIS No treatment Gradual loss of tooth – finally gets mobile & exfoliates 4) REPLACEMENT RESORPTION Similar to ankylosis, but there is the presence of an intervening inflamed connective tissue.
NONENDODONTIC PERIRADICULAR LESIONS ODONTOGENIC CYSTS Dentigerous cyst Lateral periodontal cyst Odontogenic keratocyst Residual apical cyst NON- ODONTOGENIC LESIONS Central giant cell granuloma Nasopalatine duct cyst Simple bone cyst Globulomaxillary cyst Enostosis

BONY PATHOLOGY Fibro-osseous lesions Osteoblastoma & cementoma Cementifying & ossifying fibroma ODONTOGENIC TUMOURS Ameloblastoma MALIGNANCIES • Sarcoma • Carcinoma
Conclusion: Periapical shadows are the daily bread of the general dentist. The clinician should possess a thorough working knowledge and skill necessary to establish a suitable working diagnosis in each case. It requires practice to gain skill and so the clinician must approach each periapical shadow in a logical fashion and follow it through, step by step, until the end point is reached.
References: 1. Endodontics (4 th & 5 th edition) – John I. Ingle 2. Pathways of pulp (9 th edition)- S Cohen and Burns 3. Shafers - A text book of oral pathology (4 th edition) 4. Endodontic Practice (11 th Edition) – Louis I. Grossman 5. Endodontic Therapy (4 th & 5 th edition) – Franklin S. Weine 6. Endodontics in clinical practice (4 rd edition) – F. J. Harty 7. Endodontics (3 rd edition) – K Gulabivala
8. Colour atlas & Text of Endodontics (2 nd edition) – 9. Problem solving in Endodontics – James L Gutman 10. The Dental pulp (3 rd edition) – Seltzer 11. Oral & Maxillofacial Pathology- Brad W Neville Christopher J K Stock

HANK YOU
 Periapical granuloma vs abscess
Periapical granuloma vs abscess Non corticated
Non corticated Emulsion peel x ray
Emulsion peel x ray Periapical
Periapical Lesiones radiopacas
Lesiones radiopacas Lateral periodontal cyst
Lateral periodontal cyst Periapical radiograph indications
Periapical radiograph indications Periapical granuloma
Periapical granuloma Periapical
Periapical What are periradicular tissues?
What are periradicular tissues? Cellular events of acute inflammation
Cellular events of acute inflammation Cellular events of acute inflammation
Cellular events of acute inflammation Morphological pattern of inflammation
Morphological pattern of inflammation Cell injury and inflammation
Cell injury and inflammation Dry vs wet gangrene
Dry vs wet gangrene Cavity liners and bases
Cavity liners and bases Liners and bases in dentistry
Liners and bases in dentistry Nervus trigeminus inflammation
Nervus trigeminus inflammation Swellingo
Swellingo What are cardinal signs of inflammation
What are cardinal signs of inflammation Morphological patterns of inflammation
Morphological patterns of inflammation Acute inflammation
Acute inflammation Tromboflibitis
Tromboflibitis Stages of inflammation
Stages of inflammation Mediators of inflammation
Mediators of inflammation Acute inflammation definition
Acute inflammation definition Cellular events of acute inflammation
Cellular events of acute inflammation 5 cardinal signs of inflammation
5 cardinal signs of inflammation Acute inflammation
Acute inflammation Types of inflammation
Types of inflammation Vascular response in acute inflammation
Vascular response in acute inflammation übergewicht vla
übergewicht vla Redha meaning
Redha meaning Inflammation greek
Inflammation greek Pharyngeal tonsils
Pharyngeal tonsils Cortisol tagesprofil ganzimmun
Cortisol tagesprofil ganzimmun Morphologic patterns of acute inflammation
Morphologic patterns of acute inflammation Catarrhal inflammation
Catarrhal inflammation Mediators of inflammation
Mediators of inflammation Periportal inflammation
Periportal inflammation Acute inflammation
Acute inflammation Carcinomatous epulis
Carcinomatous epulis Morphological pattern of acute inflammation
Morphological pattern of acute inflammation Chemical mediators of inflammation
Chemical mediators of inflammation Serous inflammation examples
Serous inflammation examples Chronic inflammation
Chronic inflammation Wet gangrene
Wet gangrene Itis inflammation
Itis inflammation Acute inflammation
Acute inflammation Bệnh gì
Bệnh gì Phagocytosis definition
Phagocytosis definition Dlc in physiology
Dlc in physiology Morphological patterns of acute inflammation
Morphological patterns of acute inflammation Systemic effect of inflammation
Systemic effect of inflammation Schema intestin
Schema intestin Middle meatus
Middle meatus Types of inflammation
Types of inflammation Granuloma
Granuloma Fluid on elbow
Fluid on elbow Zones of pulp
Zones of pulp Pitkyaranta pulp mill
Pitkyaranta pulp mill Dorsal subcutaneous space
Dorsal subcutaneous space Functions of the pulp
Functions of the pulp Definition of cavity preparation
Definition of cavity preparation Dora mali
Dora mali Pulp fiction
Pulp fiction Pulp fiction three act structure
Pulp fiction three act structure Polish jokes
Polish jokes Pulp diagnosis
Pulp diagnosis White pulp
White pulp Type of pulp
Type of pulp Enamel pulp
Enamel pulp Pulp oximeter
Pulp oximeter Chronic hyperplastic pulpitis
Chronic hyperplastic pulpitis Nerve fibers
Nerve fibers Rcp pulp
Rcp pulp Indirect pulp capping
Indirect pulp capping Rsidead
Rsidead Arkansas state mammal
Arkansas state mammal Celesa pulp
Celesa pulp Boundaries of thenar space
Boundaries of thenar space Coffee pulp as fertilizer
Coffee pulp as fertilizer Body paragraph structure
Body paragraph structure Module 5 supply and demand introduction and demand
Module 5 supply and demand introduction and demand Benvolio quotes act 1, scene 1
Benvolio quotes act 1, scene 1 Example of advantages and disadvantages essay
Example of advantages and disadvantages essay Introduction to acids and bases webquest
Introduction to acids and bases webquest Epic poem the odyssey
Epic poem the odyssey Introduction to computer organization and architecture
Introduction to computer organization and architecture How does tragic love affect teenagers today?
How does tragic love affect teenagers today? The odyssey and epic poetry: an introduction, part 1
The odyssey and epic poetry: an introduction, part 1 Body paragraph structure
Body paragraph structure Introduction to systems analysis and design
Introduction to systems analysis and design San y nas
San y nas What rules must an epic follow?
What rules must an epic follow? Romeo and juliet essay
Romeo and juliet essay Romeo and juliet introduction
Romeo and juliet introduction Romeo juliet introduction
Romeo juliet introduction Difference between recruitment and selection
Difference between recruitment and selection Executive project report
Executive project report Introduction to operations and supply chain management
Introduction to operations and supply chain management Introduction to oil and gas industry ppt
Introduction to oil and gas industry ppt