Purulentinflammatory diseases of the lung and pleura Injury




- Slides: 26

Purulent-inflammatory diseases of the lung and pleura. Injury of the thoracic cavity and damage of the esophagus. Emergency medical aid of emergencies.
A brief tour of embryonic development of anatomical structures and organs of the chest: a) the formation of structures and organs of the chest begins almost identically: 3 - 6 weeks of pregnancy; b) their quantitative formation finishes almost at the same - at five years old; c) it determines the best term for radical surgery on the organs of the thorax (5 -7 years), to obtain a good functional and cosmetic long-term outcome in children. * Although the volume of the muscles of the chest reaches the age norm only in 12 -15 years; * Cartilage tissue is preserved in the ribs up to 20 -25 years; * Lungs and blood vessels pass certain stages of theirs formation in age: 6 months - 5 -7 years - 14 years - 29 -32 years. * The development of the thymus also goes through five age periods with the most intensive development in the first five years of life and during puberty.
The syndrome of intrathoracic voltage (SITV) in children is a difficult complex of the symptoms, that manifests a mono- or combination increasing of intrapleural, intrapulmonary or mediastinal pressure resulting from the accession of complications with different surgical (BDL, trauma of chest, lobar emphysema, diaphragmatic hernia, which is complicated by pulmonary bulla and cyst ) and somatic (spontaneous pneumothorax in bronchial asthma, tense pleuritis in glomerulonephritis, diseases of the spleen) diseases.
The main pathophysiological changes in SITV : • rapid deterioration in lung ventilation on the affected side and healthy side; • displacement of the heart and mediastinal vessels, along with a healthy side; • hypertension of small pulmonary circulation; • abnormal shunting of blood from the right (normally up to 5%) - in to the left; • formation of an acute or chronic hypoxia, central nervous system and entire body; • development of the pleuropulmonary shock; • risk of sudden cardiac arrest and breathing. - The frequency of SITV is determined during the life by frequency of complications, by the spread of the underlying disease, by the age of the child. - In the case of a unilateral lesion by SITV of child's body - the main objective diagnostic criterion (chest X-Ray, ultrasound, cardiogram) is the suddenness and speed of dislocation of the lateral borders of the heart and mediastinum to the healthy side against the background, mainly severe acute respiratory failure, and cardiovascular failure.
In bilateral SITV (often against a background of mechanical ventilation) is dominated symptoms bilateral increasing of intrathoracic pressure and compression of chest organs, but not the shift of the mediastinum. It is noted: - decreasing of saturation blood by oxygen; - increasing of tachycardia; - The emergence of reaction on pain in the chest; - The appearance and progression of pallor and marbling of the skin, mucosal tunics; - Cold clammy sweat; pained face; tense, a paradoxical pulse (disappears on inspiration); - The appearance or progression of pathological changes in the examination, percussion, auscultation and palpation of the chest; - Increased blood pressure, central venous pressure; - Change in the overall analysis of blood.
Originating mainly suddenly it difficult medical condition requires urgent and adequate rapid response a surgeon, and resident too. - Pleural puncture. - Drainage of the pleural cavity (thoracentesis). - Drainage of the mediastinum. - Puncture and drainage of the cavity of tense cyst of a lung. - Therapeutic bronchoscopy and temporary occlusion of the bronchus. - Urgent radical surgery.
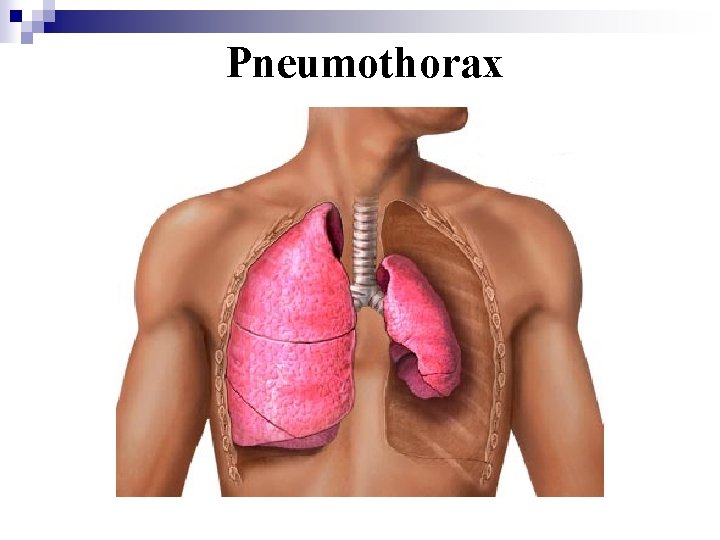
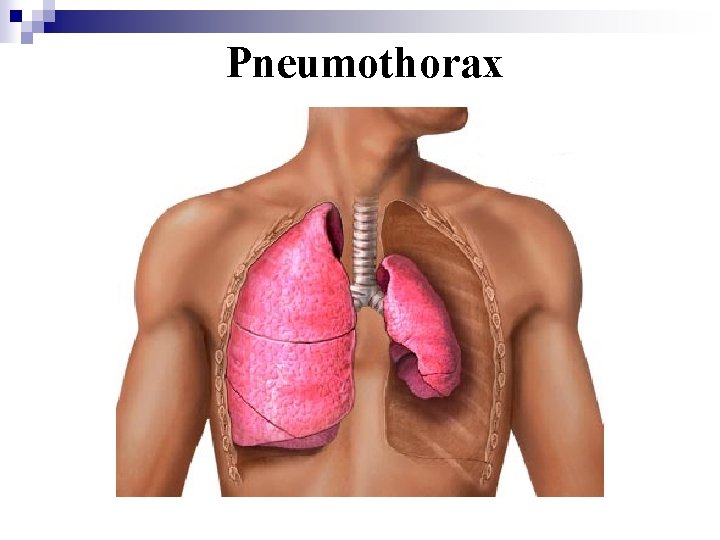
Pneumothorax
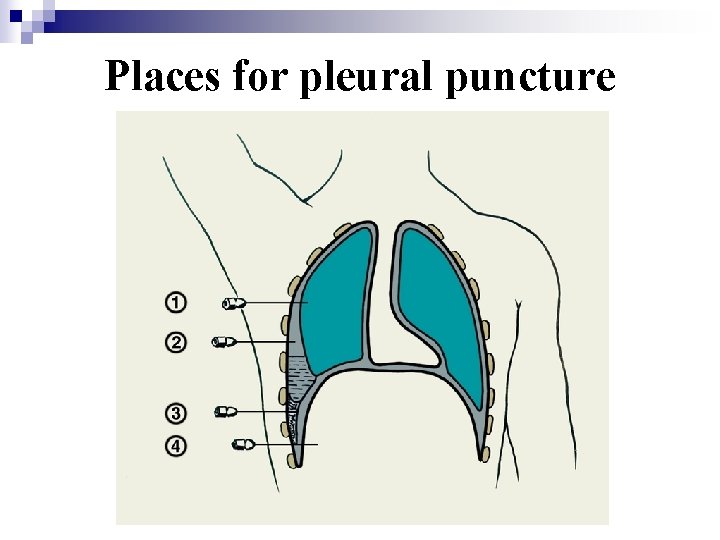
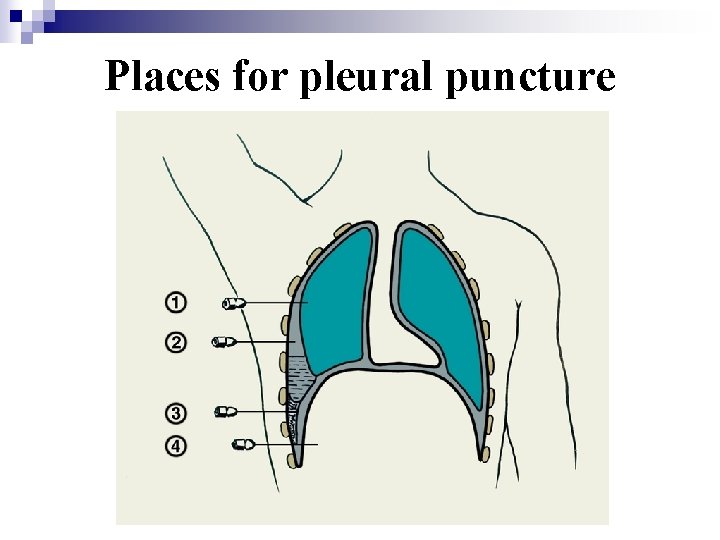
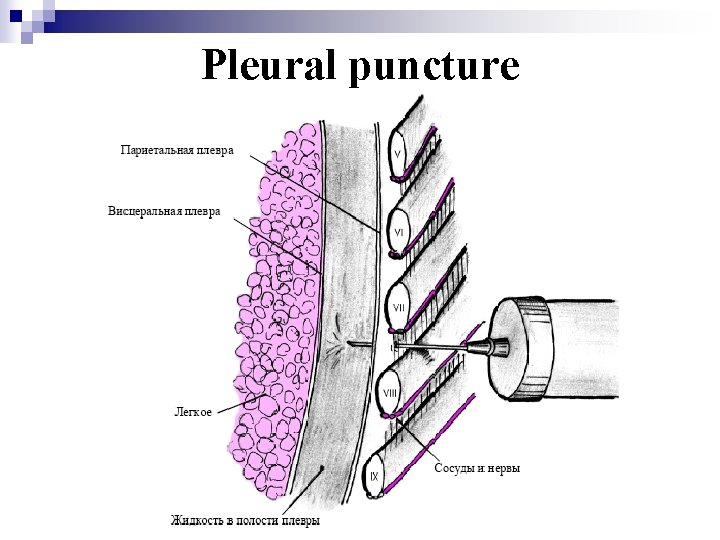
Places for pleural puncture
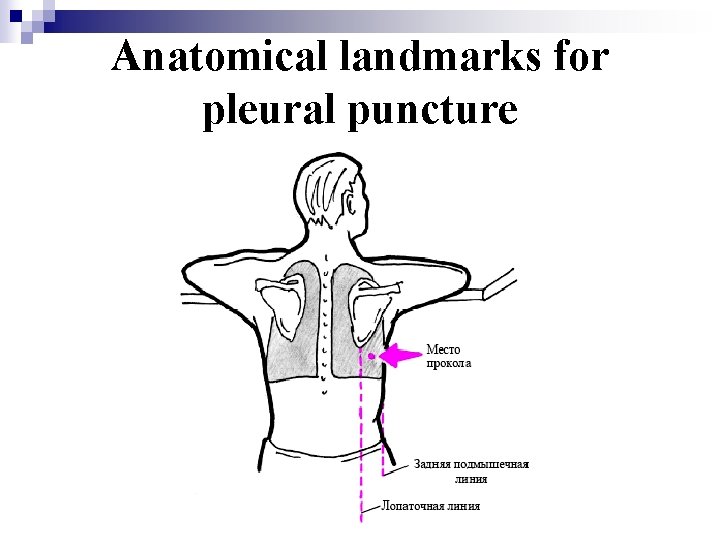
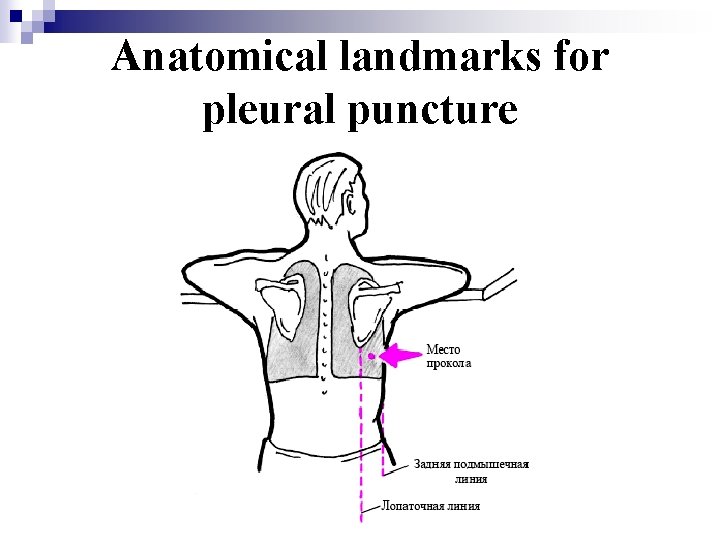
Anatomical landmarks for pleural puncture
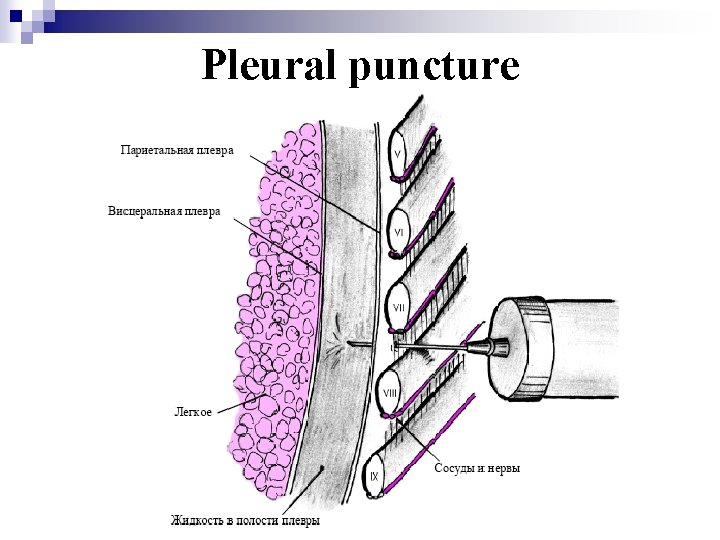
Pleural puncture
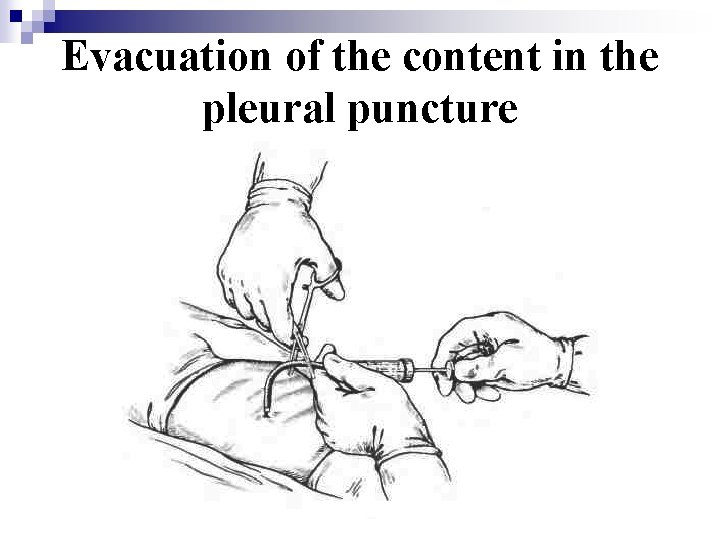
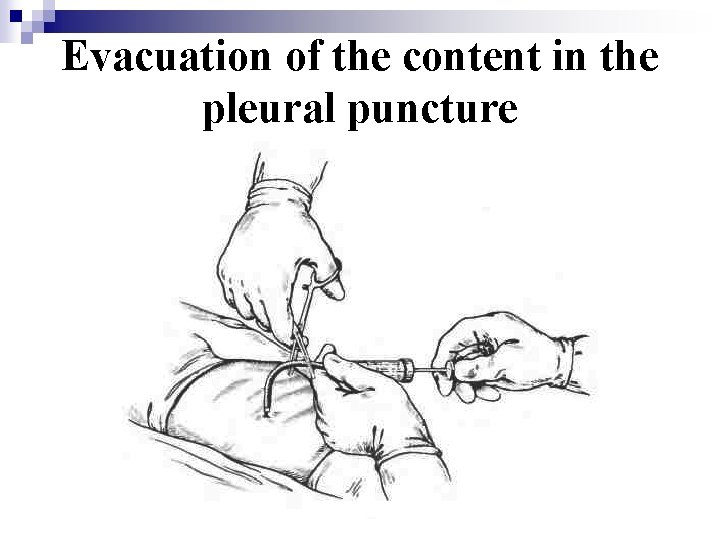
Evacuation of the content in the pleural puncture
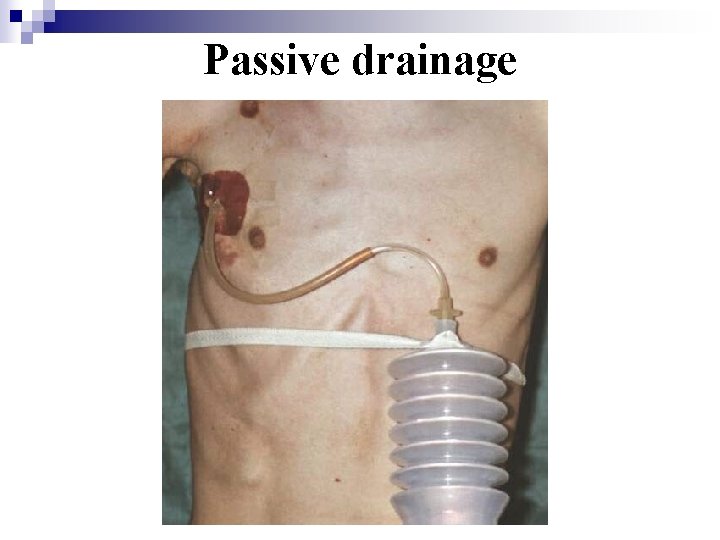
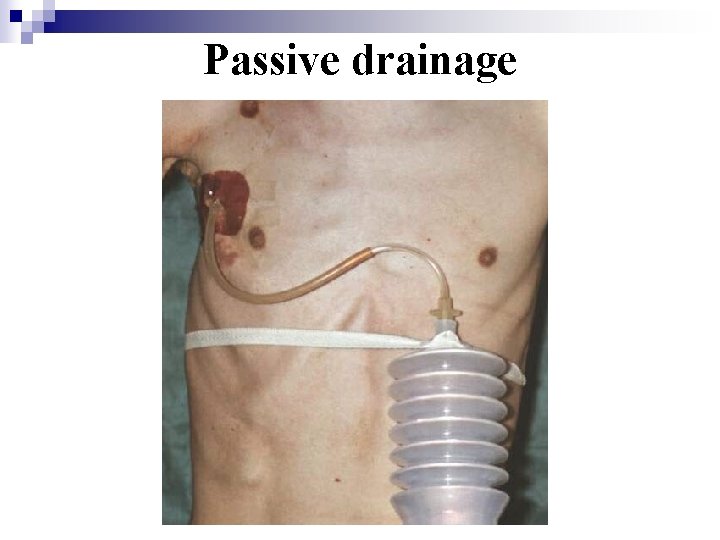
Passive drainage
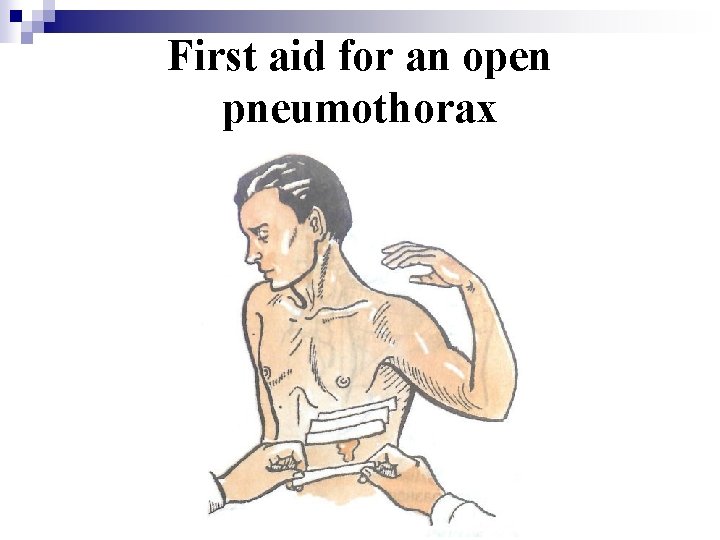
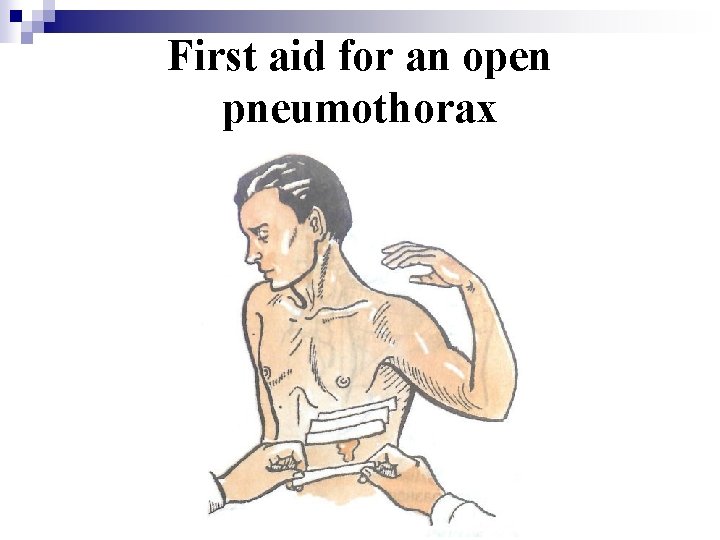
First aid for an open pneumothorax
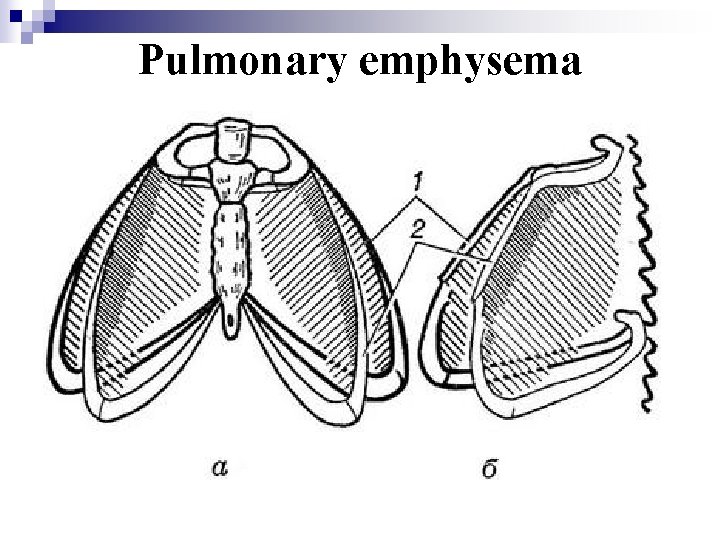
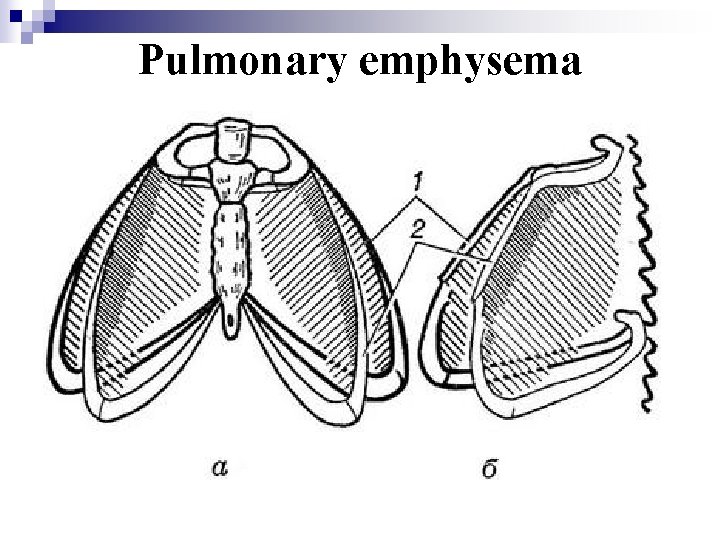
Pulmonary emphysema

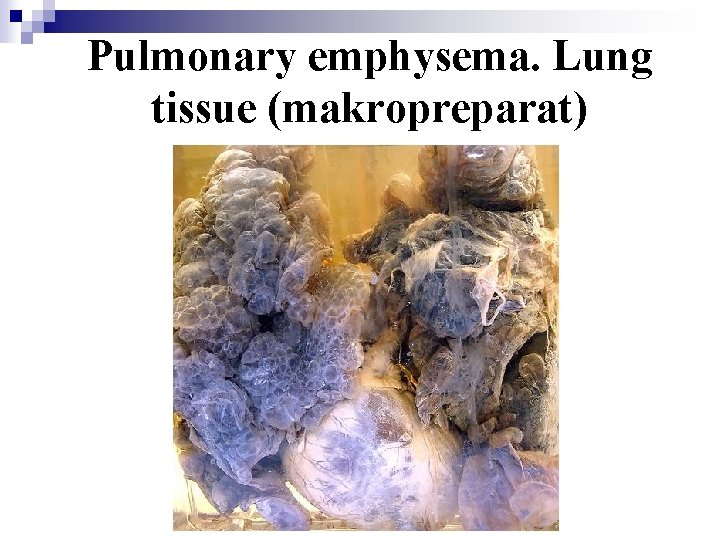
Pulmonary emphysema (makropreparat)
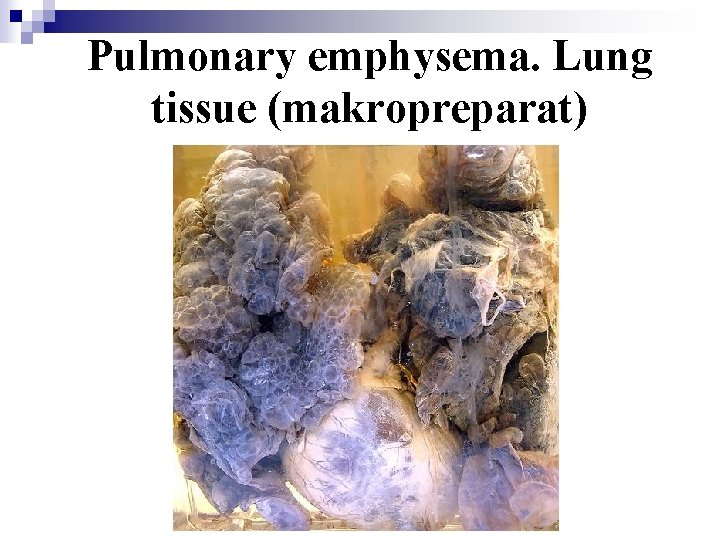
Pulmonary emphysema. Lung tissue (makropreparat)
Depending on the frequency, causes and place of increasing intrathoracic pressure we classify four forms of SITV: - pleural, - intrapulmonary, - mediastinal, - combined. In newborns SITV often occurs as a complication of catheterization of the subclavian veins, aspiration of mucus from the bronchi and esophagus, as well as in spontaneous chylothorax and chylopericardium.
Differential diagnosis is carried out with: - atelectasis of the lungs, - congenital heart disease, - abnormalities of the aorta and the pulmonary veins, - volvulus of the stomach in newborns and children during the first months of life, - perforation of the digestive tract in newborns with ulcerative necrotizing enterocolitis (UNEC), - pericarditis, - volumetric processes of the brain (cysts and different tumors).

Treatment SITV: Emergency is in care is accurate and quick X-ray diagnostics and conducting of etiologic algorithm: - pleural puncture and drainage of the pleural cavity, mediastinum; - percutaneous puncture, drainage by Monaldi, Seldinger of cavity of a complicated cyst (bulla); - bronchoscopy, removal of foreign body, a temporary occlusion of main bronchus by foam rubber sponge; - radical surgery. Parallel to the intensive therapy in the amount of 80 -100% of the physiological needs according to age and presence of shock in a patient: - anesthetics; - haemostatics; - sedatives; - oxygen therapy; - alcohol-polyglukin-procaine (novocaine) (0. 25%) - 0. 5% for local blockade in the ratio 1: 1: 3 vagosympathetic, retrosternal and paravertebral blockades and also blockades of locations of fractures - antibiotic therapy; - cardio- and hepatoprotectors; - improvement of microcirculation.
Congenital lobar emphysema (CLE) - is a process often emphysematous of 3 -5 segment left upper lobe. It arises as a result of insufficiency or functional immaturity of the elastic fibers in the lungs and main or segmental bronchi. By clinical course and pathological and morphological mechanisms distinguish diffuse and local forms of the disease. Congenital lobar emphysema (CLE) is divided on the three forms: - uncompensated (is showed of the first days of life); - subcompensated (is provoked by acute respiratory viral infection of upper respiratory tract in the first months of life); - compensated (can be detected after a year of life and has all clinical symptoms of obstructive disease of respiratory tract). Late diagnosis is often the result of errors of clinicians and radiologists.
Clinical symptoms The chest (usually the left side) is swollen, lags behind in the act of breathing. There are dyspnea, cyanosis, dry and recrudescent cough on the background of normal or subfebrile body temperature, a pathological emphysema of a lung on the affected side with the displacement of the heart in a healthy side and atelectasis of the lower parts of the lungs on the affected side. Treatment Intravenous infusion therapy, antispasmodics, analgesic inhalation; Urgent or planned thoracotomy (lobectomy or segmentectomy).
Cysts of the lungs (intrapulmonary cavity with air or liquid) Classification: - Unilateral, bilateral; - congenital, acquired; - single-chamber, multi-chamber; - complicated, uncomplicated; Complications (mostly by valve mechanism) occurs in a place of dichotomous division of the bronchi. Often preliminary infection of the cyst helps it (acute respiratory infections, bronchitis, pneumonia). Cliniciscausedofacutepneumonia, suppuration, bleedingandgapof the cyst. - Breakthrough of the cyst into the pleural cavity: a sudden paroxysmal cough, the child is concerned, there is shortness of breath, fever and tachycardia. Lag of the chest in the act of breathing and increasing an affected half of its. There is a clinical picture of pneumothorax, anemia and SITV. - The X-ray pictures of organs of the chest show thin sharp contours of cyst. - Tomogram, X-Rays in 2 projections help to distinguish it from the bula; bronchography, CT, MRI, - from the lung abscess and other diseases. - Angiography and scintigraphy fix an avascular area on the periphery; in 16% of cases with bronchography the contrast enters the cyst.

The differential diagnosis is carried out with: - staphylococcal bullae (the walls of it are there seldom); - secondary (acquired, parasitic and nonparasitic cysts); - diaphragmatic hernia; - limited pneumothorax of different genesis (BDL usually); - complications of helminthic infestation; - congenital lobar emphysema; - abscess of the lungs with a level; - anomalies of the diaphragm; - tumors of the mediastinum; - doubling of the digestive tract. Treatment: Urgent or elective (planned) surgery (segmentectomy, lobectomy). Puncture, the cyst micro drainage must be done in cases of contraindications to radical surgical treatment, They are as the stage of diagnosis and conservative treatment (if are danger of gap or of internal bleeding).
Bacterial degradation of lungs (BDL) in children - acute or chronic suppurative destructive inflammation of the lungs (the bronchi, parenchyma, pleura, vessels). Synonyms: empyema, staphylococcal pneumonia. The transition of acute pneumonia in the BDL is from 5 -8 to 26. 2% of cases The disguising syndromes: - abdominal (stomach pain, vomiting, constipation, diarrhea, ketoacidosis); - asthmatic (laryngitis, cases of obstruction, foreign body of airway); - Neurotoxic (hyperthermia, convulsions, cerebral edema) - Cardiovascular (hepato-splenomegaly, rash on the face, edema of the eyelids). Leading syndromes: - progressive endogenous intoxication, - progressive respiratory failure. Aetiology: viral, viral and bacterial gram (+), gram (-) and mixed aerobicanaerobic infections. Aerogenic route of infection is the main way.
The reasons for the transition to the destruction: - reduction of local and general immunity; - high virulence of the infection; - uncropped causes of secondary inflammation: subatelectasis, trauma, foreign bodies, parasitic cyst, lung abnormality; - a combination of obstruction + infection; - undrained foci of infection. Mostly are affected fourth-order bronchi (subpleural, rare can be the central abscess). Microscopic and clinical-radiological picture are determined by the abilities of viruses to generate exo-and endotoxins, by difference of structure of microfoci, by child's age, by shape and localization of lesions and the overall response of the body in response to aggression.
Treatment: a) intensive, conservative and symptomatic therapy; b) pleural puncture; c) drainage and micro drainage of pleural cavity, of abscess cavity and of complicated cysts; d) medical diagnostic broncho-thoracoscopy (dividing of adhesives occlusion of bronchi, intrabronchial drainage of abscess and bougienage of bronchi, electrocoagulation of the cyst); e) urgent radical (in case of bleeding), and elective surgery (decortication, perikardektomiya, removal of bronchiectasis, opening and drainage of abscess, removal of the abscess). s Dispensary care, rehabilitation: for at least three years and even more.
 Purulent diseases of lungs and pleura
Purulent diseases of lungs and pleura Pulmonary ligament
Pulmonary ligament Battering intentional or unintentional
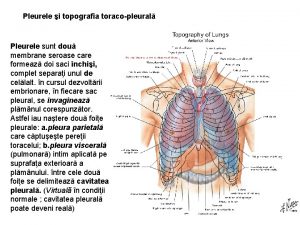
Battering intentional or unintentional Visceral and parietal pleura
Visceral and parietal pleura Pericardium pleura and peritoneum
Pericardium pleura and peritoneum Pericardium pleura and peritoneum
Pericardium pleura and peritoneum Costomediastinal pleura
Costomediastinal pleura Endothoracic fascia
Endothoracic fascia Segmental bronchus
Segmental bronchus Pleural adhesions
Pleural adhesions Surface anatomy of pleura
Surface anatomy of pleura Ligamento interpleural de morosow
Ligamento interpleural de morosow Parede membranacea traqueia
Parede membranacea traqueia Dewy pleura
Dewy pleura Primary secondary and tertiary bronchi
Primary secondary and tertiary bronchi Suprapleural membrane
Suprapleural membrane Aortic impression lung
Aortic impression lung Hypersonor
Hypersonor Surface marking of pleura
Surface marking of pleura Serous membranes
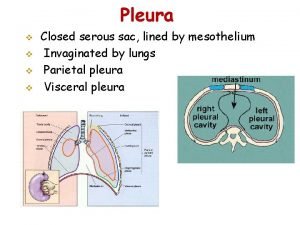
Serous membranes Pleura
Pleura Pleura polmonare
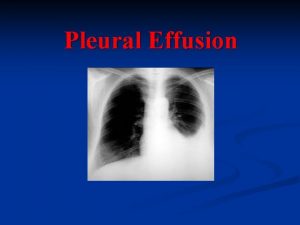
Pleura polmonare Foto rontgen efusi pleura
Foto rontgen efusi pleura Analisis cairan pleura
Analisis cairan pleura Tenziós ptx
Tenziós ptx Pleura
Pleura Visceral pleura
Visceral pleura