Duodenal Injuries Taichiro Tsunoyama Introduction Duodenal injuries are









- Slides: 54
Duodenal Injuries Taichiro Tsunoyama
Introduction • • • Duodenal injuries are uncommon Incidence of blunt duodenal injury; 0. 2% Penetrating(78%) wounds are more common than blunt(22%) • Duodenal injuries are both difficult to diagnose and repair due to its retroperitoneal location
Duodenal Anatomy • First portion of the small intestine • From the plyoric ring to the Treitz ligament • 25 -30 cm in length, Latin word duodeni (twelve each) • Divided into 4 portions
Divided into 4 portions 1 st: Superior Pass backword and upward toword the neck of the gallbladder Most of portion is intraperitoneal 2 nd: Descending Contain the bile and panceatic duct(Ampulaa of Vater) Entirely retroperitoneal 3 rd: Transverse SMA runs downward over the 3 rd portion 4 th: Ascending Short distance(2 -3 cm), suspensory ligament of Treitz

Blood Supply Derived from the pancreatioduodenal artery Superior branch; from hepatic artery Inferior branch; from SMA Drain into the portal vain and SMV


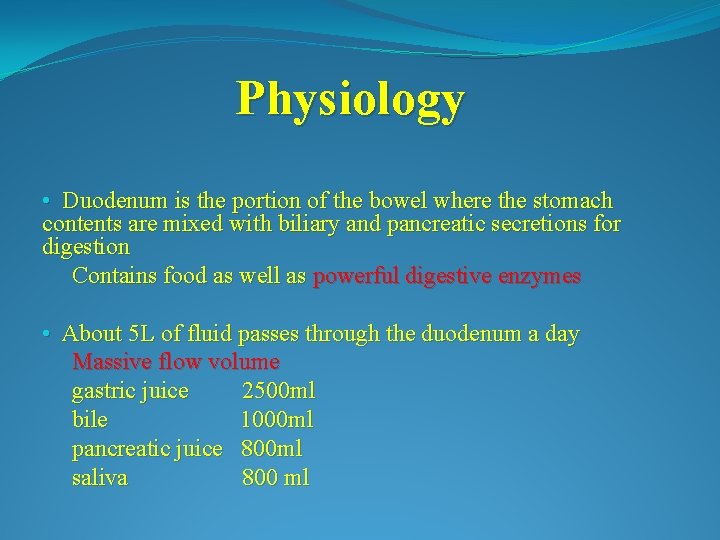
Physiology • Duodenum is the portion of the bowel where the stomach contents are mixed with biliary and pancreatic secretions for digestion Contains food as well as powerful digestive enzymes • About 5 L of fluid passes through the duodenum a day Massive flow volume gastric juice 2500 ml bile 1000 ml pancreatic juice 800 ml saliva 800 ml
Mechanism of Injury • Most injuries are penetrating in nature • Blunt injuries account for approx 25%
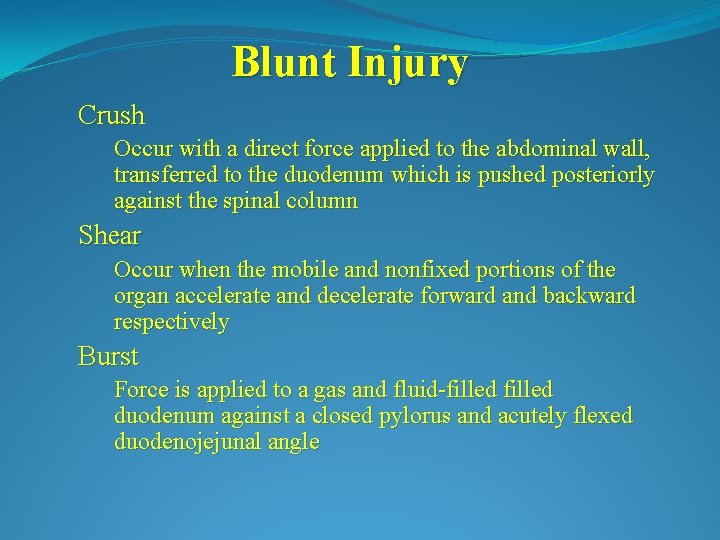
Blunt Injury Crush Occur with a direct force applied to the abdominal wall, transferred to the duodenum which is pushed posteriorly against the spinal column Shear Occur when the mobile and nonfixed portions of the organ accelerate and decelerate forward and backward respectively Burst Force is applied to a gas and fluid-filled duodenum against a closed pylorus and acutely flexed duodenojejunal angle
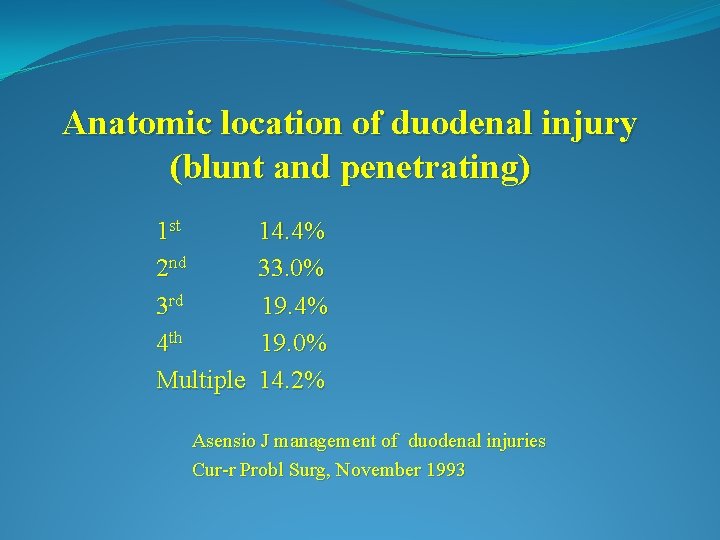
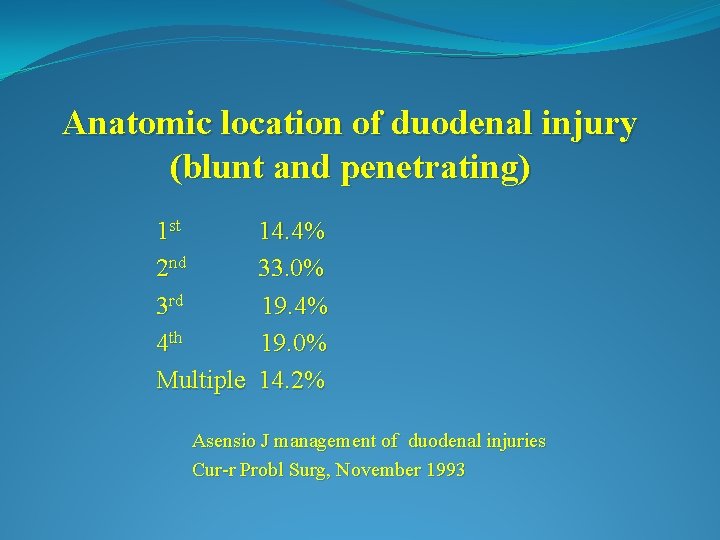
Anatomic location of duodenal injury (blunt and penetrating) 1 st 2 nd 3 rd 4 th Multiple 14. 4% 33. 0% 19. 4% 19. 0% 14. 2% Asensio J management of duodenal injuries Cur-r Probl Surg, November 1993
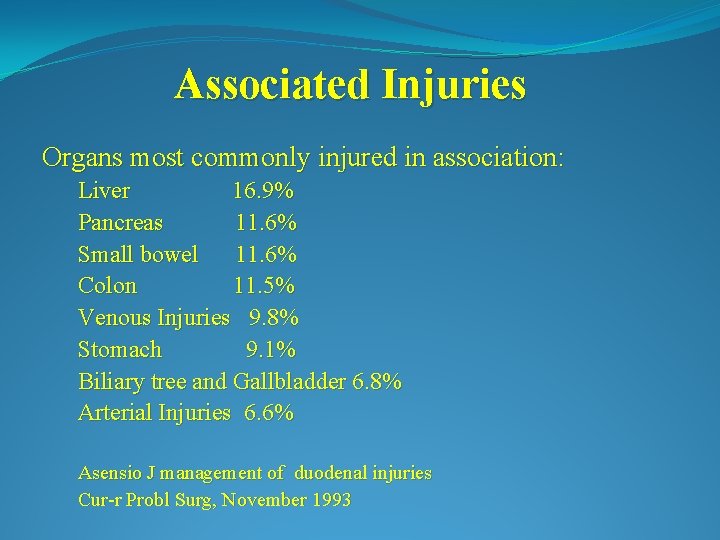
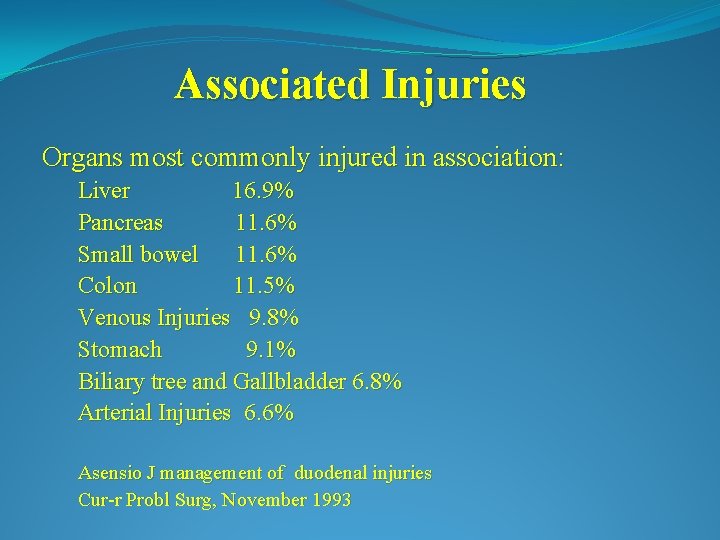
Associated Injuries Organs most commonly injured in association: Liver 16. 9% Pancreas 11. 6% Small bowel 11. 6% Colon 11. 5% Venous Injuries 9. 8% Stomach 9. 1% Biliary tree and Gallbladder 6. 8% Arterial Injuries 6. 6% Asensio J management of duodenal injuries Cur-r Probl Surg, November 1993
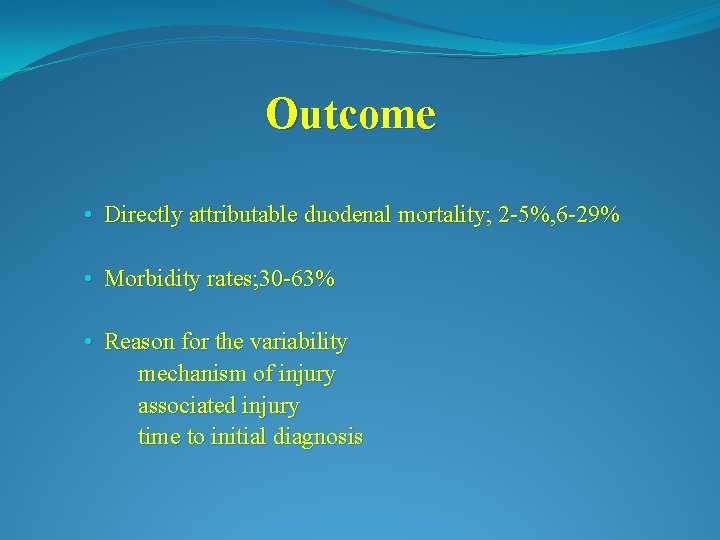
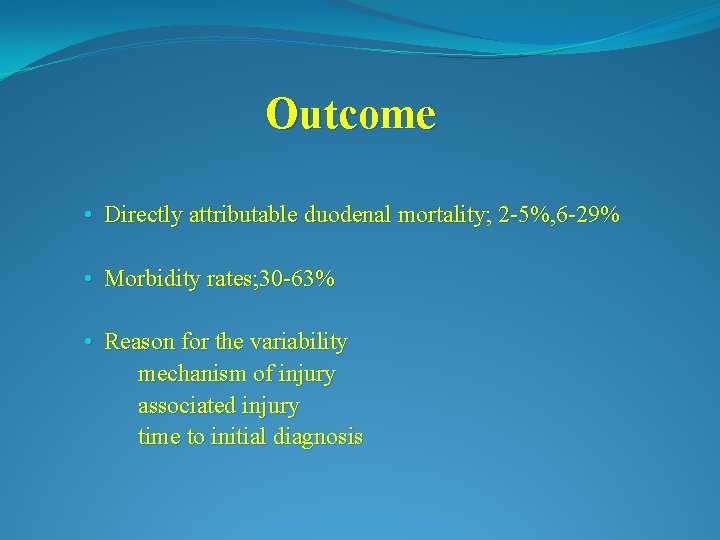
Outcome • Directly attributable duodenal mortality; 2 -5%, 6 -29% • Morbidity rates; 30 -63% • Reason for the variability mechanism of injury associated injury time to initial diagnosis
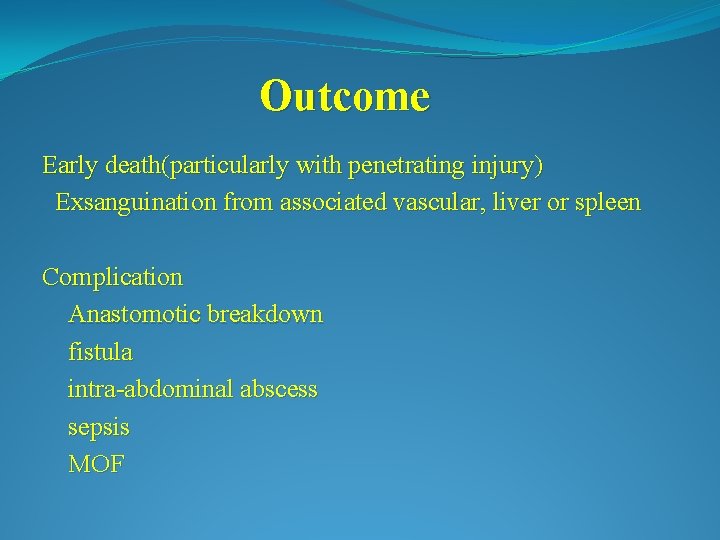
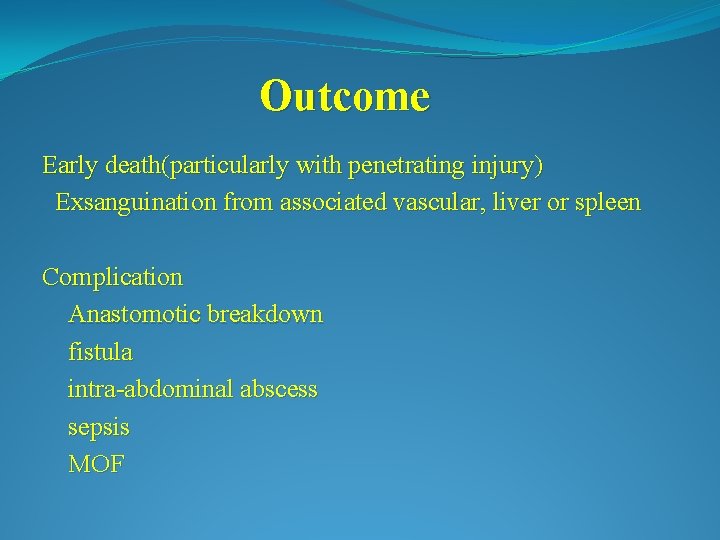
Outcome Early death(particularly with penetrating injury) Exsanguination from associated vascular, liver or spleen Complication Anastomotic breakdown fistula intra-abdominal abscess sepsis MOF
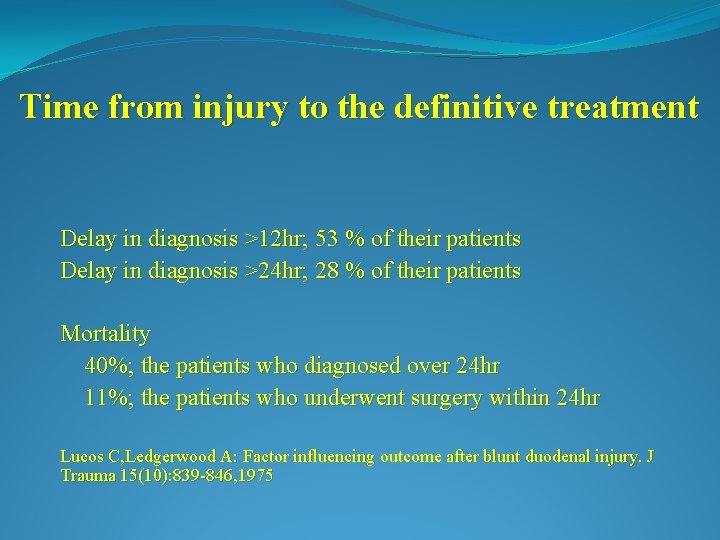
Time from injury to the definitive treatment Delay in diagnosis >12 hr; 53 % of their patients Delay in diagnosis >24 hr; 28 % of their patients Mortality 40%; the patients who diagnosed over 24 hr 11%; the patients who underwent surgery within 24 hr Lucos C, Ledgerwood A: Factor influencing outcome after blunt duodenal injury. J Trauma 15(10): 839 -846, 1975
Important steps for duodenal injury 1. Early diagnosis 2. Control of hemorrhage 3. Control of bacterial contamination

Diagnosis • Requires a high index of suspicion Accurate H&P • More difficult to diagnose in blunt trauma than penetrating As penetrating injuries tend to necessitate an operative exploration • No specific diagnostic test found to be accurate all of the time Abdominal X-rays UGI Endoscopy CT Scan
Abdominal X-Ray Often quite subtle Air collections outlining right kidney Presence of gas around the right psoas muscle
Diagnosis Upper GI Series Usually with Gastrograffin or thin barium May see a leak with fluoroscopy Consider changing position for oblique or lateral views to get a 3 D picture Endoscopy May visualize a intra-luminal blood, a perforation or a hematoma directly May be considered in conjunction with UGI or CT Not usually used acutely due to the possibility of worsening injury with either the scope or the insufflation
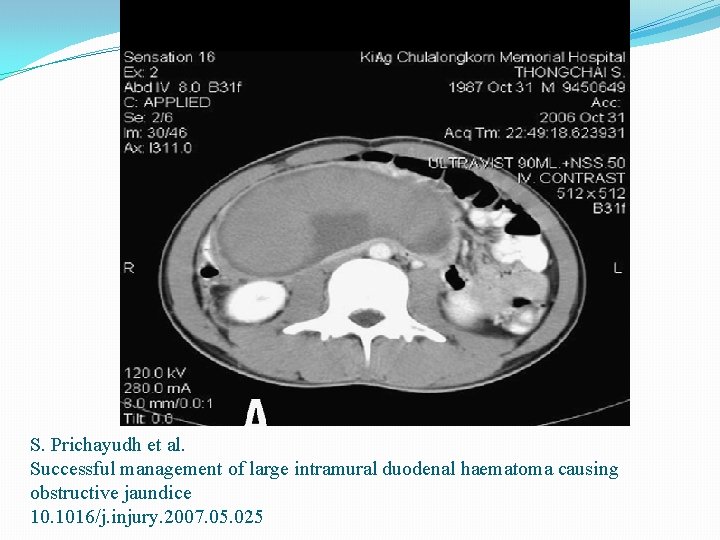
CT Scan • Must be performed with both oral and intravenous contrast • Best method for visualizing retroperitoneal structures without an operation • Helpful in evaluating the remaining intra-abdominal cavity in stable patients • Not always very sensitive Extravasation of oral contrast from the duodenum with a retroperitoneal hematoma Extraluminal gas/fluid around the duodenum Focal bowel wall thickening Interruption of progress of the bowel contrast medium

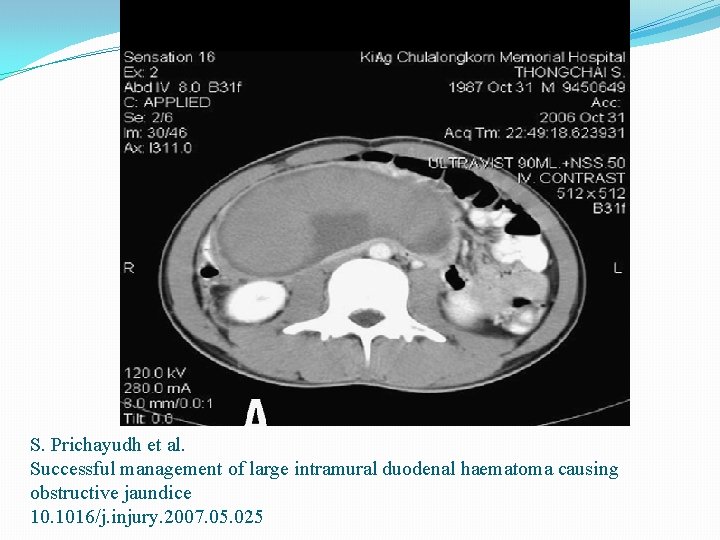
S. Prichayudh et al. Successful management of large intramural duodenal haematoma causing obstructive jaundice 10. 1016/j. injury. 2007. 05. 025
DPL • Unreliable in detecting isolated duodenal and other retroperitoneal injuries • But DPL is often helpful because of 40% of patients have associated intra-abdominal injuries that will result in a positive DPL • The finding of amylase or bile are more specific indicators of possible duodenal injury
Exploratory Laparotomy • Midline incision • Immediate control of life-threatening hemorrhage • Control of GI contamination • Thorough exploration of the abdominal cavity and retroperitoneum
Operative Exposure of Duodenal Injuries Intra-op findings that require exploration Crepitus along the duodenal sweep Bile staining of paraduodenal or adjacent tissues Documented bile leak Right-sided retroperitoneal or periduodenal hematoma
Operative Exposure of Duodenal Injuries Thorough exploration requires evaluation of all 4 portions Kocher Maneuver Transection of the ligament of Treitz Cattell and Braasch maneuver
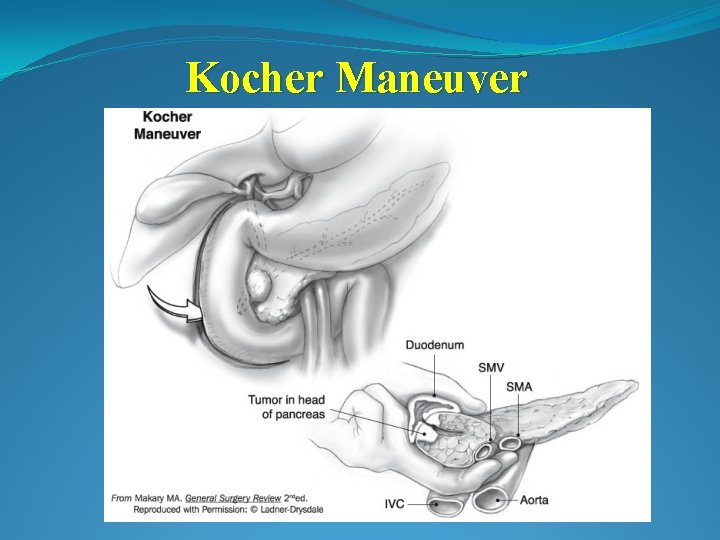
Kocher Maneuver • Should be able to palpate the head of the pancreas to the level of the mesenteric vessels • Be able to visualize the anterior and posterior aspects of the 2 nd and 3 rd portions of the duodenum, the head of the pancreas and the infrarenal IVC
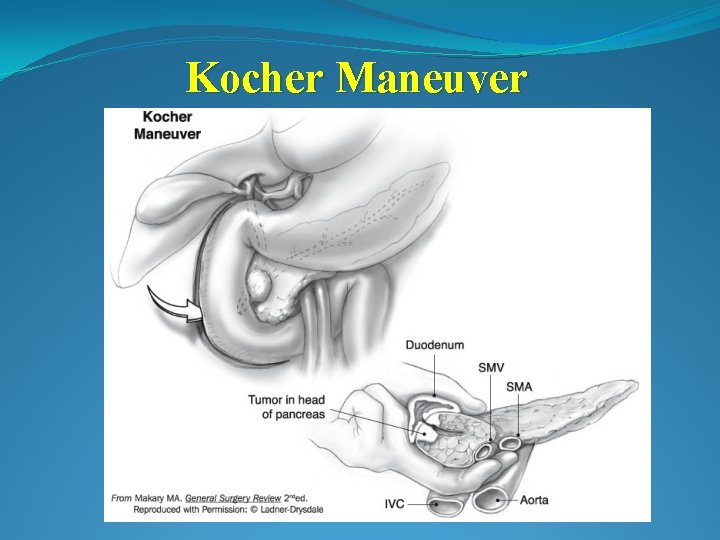
Kocher Maneuver

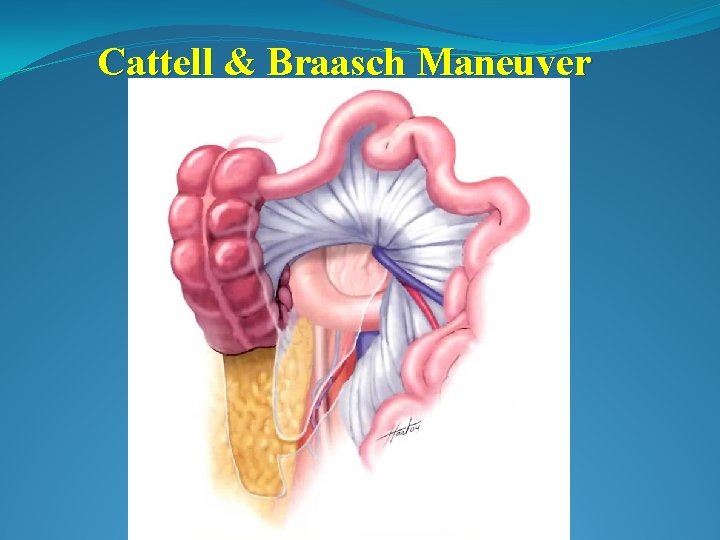
Cattell & Braasch Maneuver Technique for exposure of 3 rd and 4 th portion of the duodenum 1. Incise the avascular line of Toldt 2. Mobilize the asending colon and the hepatic flexure 3. Sharply incise the retroperitoneal attachments of the Small bowel from the RLQ to the duodenojejunal junction 4. Reflect the Small bowel out of the abdominal cavity Gives excellent exposure, however it is a somewhat complex maneuver that may not be required
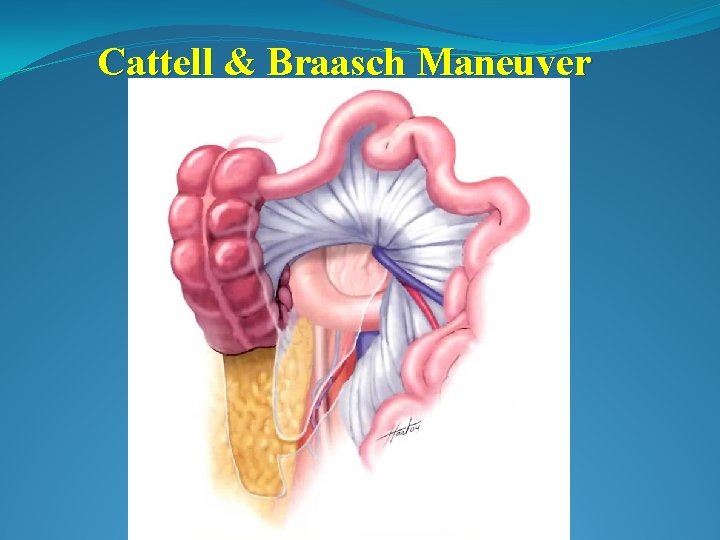
Cattell & Braasch Maneuver
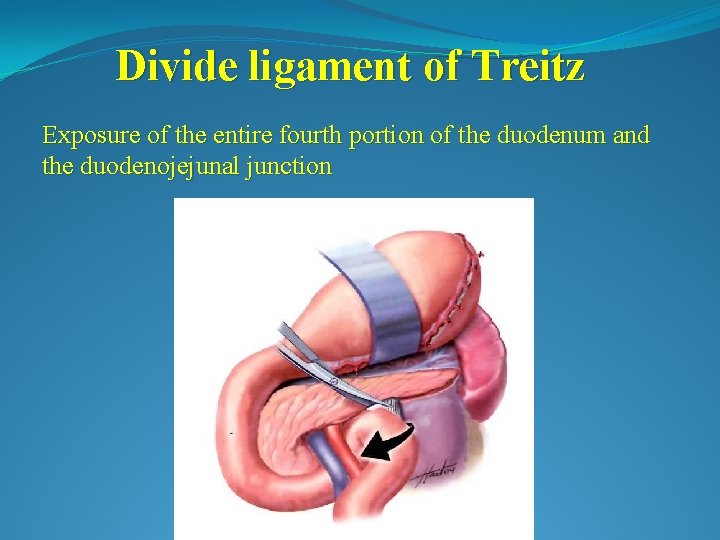
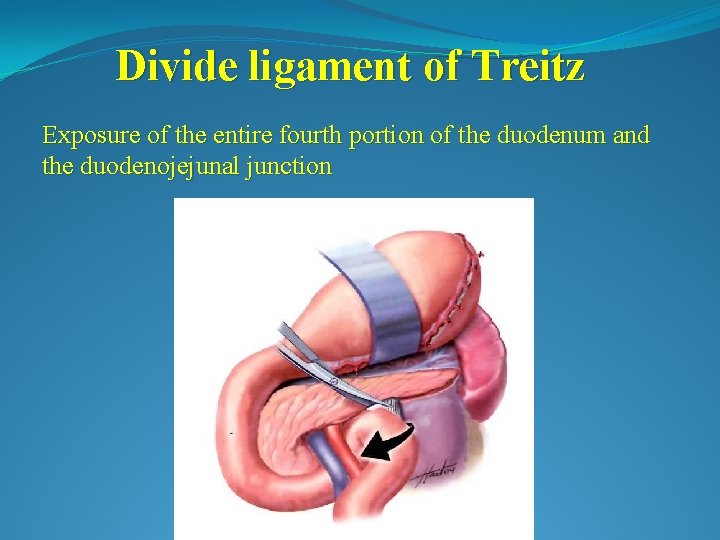
Divide ligament of Treitz Exposure of the entire fourth portion of the duodenum and the duodenojejunal junction
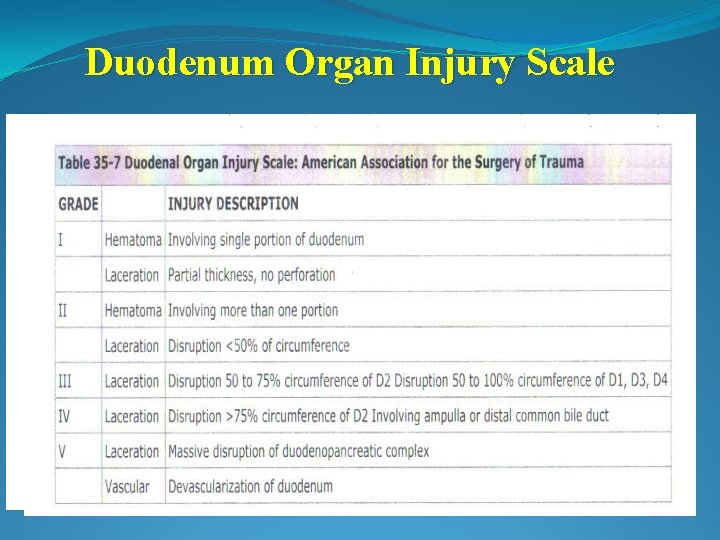
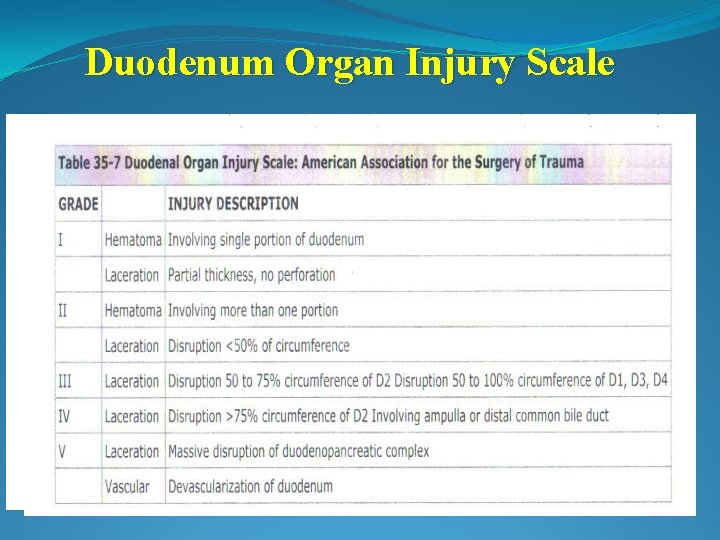
Duodenum Organ Injury Scale
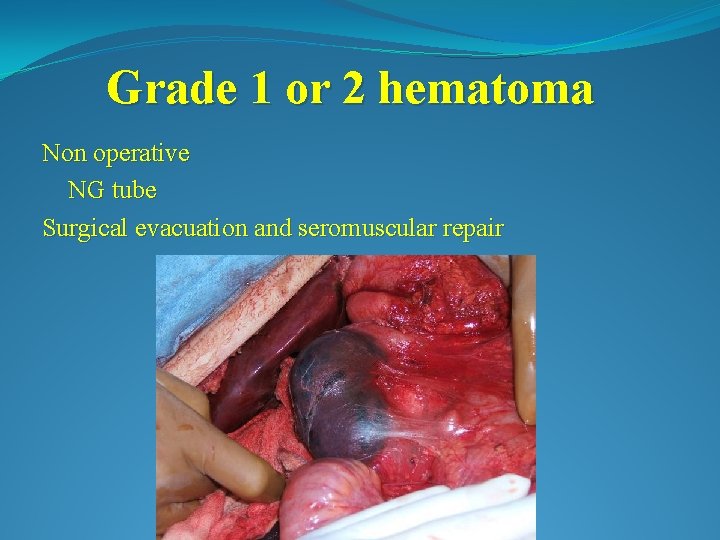
Grade 1 or 2 hematoma Non operative NG tube Surgical evacuation and seromuscular repair
Grade 1 or 2 laceration Duodenorrhaphy
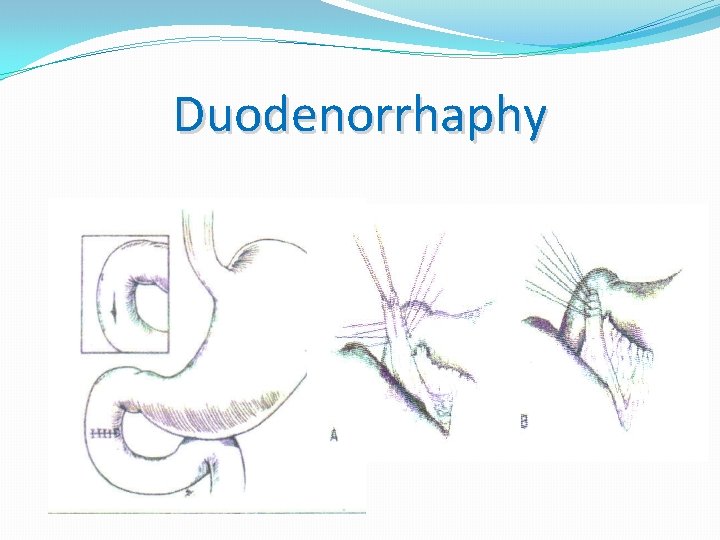
Duodenorrhaphy • Used to repair approximately 75 -85% of all injuries • Debride nonviable tissue • Double layer closure • Close longitudinal injuries transversely if less than 50% of the duodenal circumference to avoid duodenal narrowing • Consider placing omentum over your repair
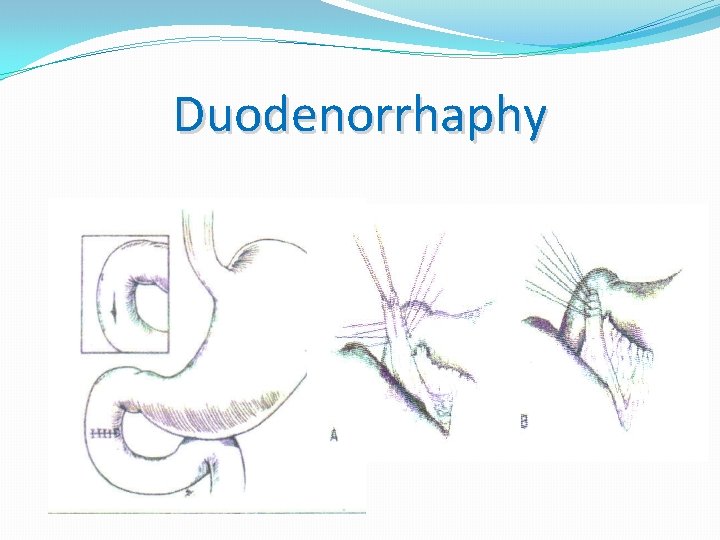
Duodenorrhaphy
Grade 3 or 4 laceration Primary repair(with Tube Duodenostomy) Resection anastomosis Roux-en-Y duodenojejunostomy Pyloric Exclusion

Synder Duodenal severity scale Mild Severe Agent Stab Blunt or missile Size <75%wall ≥ 75%wall Duodenal site 3, 4 1, 2 Injury repair interval <24 ≥ 24 Adjacent injury No CBD No pancreatic injury Protection of the duodenalrepair is not necessary in the mild group
Duodenorrhaphy with Tube Duodenostomy “protecting the repair” with decompression maneuvers 1. Primary Tube is placed through a separate stab incision in the duodenum 2. Antegrade Duodenum is decompressed by passage of a tube through the pylorus 3. Retrograde Tube is passed retrograde from insertion in the jejunum

Duodenorrhaphy with Tube Duodenostomy
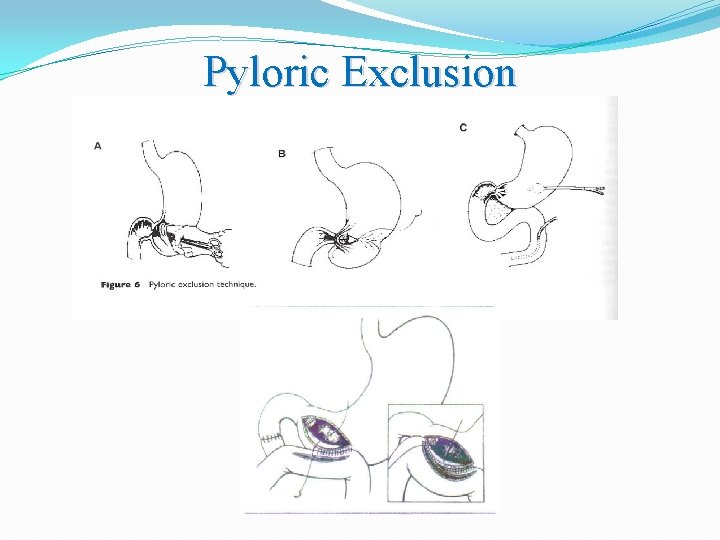
Pyloric Exclusion • An alternative to duodenal diverticulization • Secures exclusion of the duodenal suture line and diversion of the gastric contents • Through the gastrotomy, the pylorus is closed using absorbable suture • Alternative method includes using a stapler across the pylorus (TA-50)
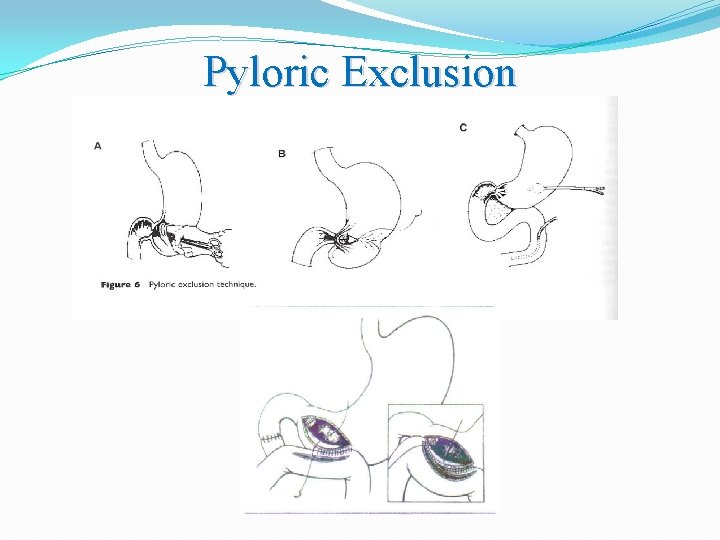
Pyloric Exclusion
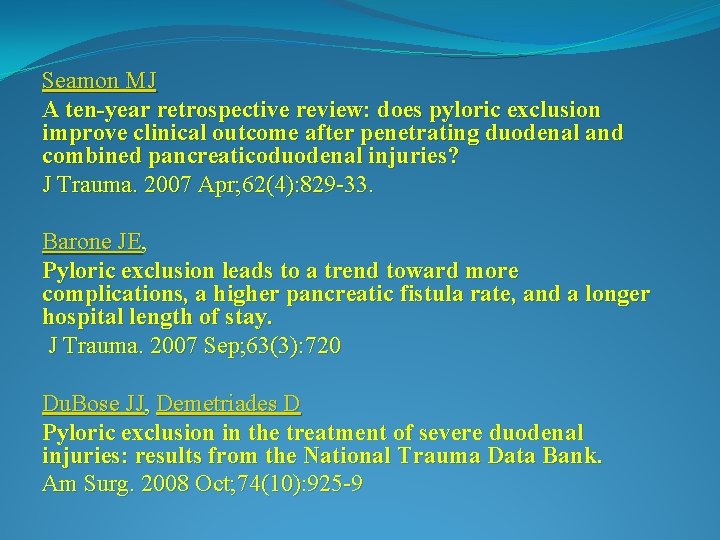
Seamon MJ A ten-year retrospective review: does pyloric exclusion improve clinical outcome after penetrating duodenal and combined pancreaticoduodenal injuries? J Trauma. 2007 Apr; 62(4): 829 -33. Barone JE, Pyloric exclusion leads to a trend toward more complications, a higher pancreatic fistula rate, and a longer hospital length of stay. J Trauma. 2007 Sep; 63(3): 720 Du. Bose JJ, Demetriades D Pyloric exclusion in the treatment of severe duodenal injuries: results from the National Trauma Data Bank. Am Surg. 2008 Oct; 74(10): 925 -9
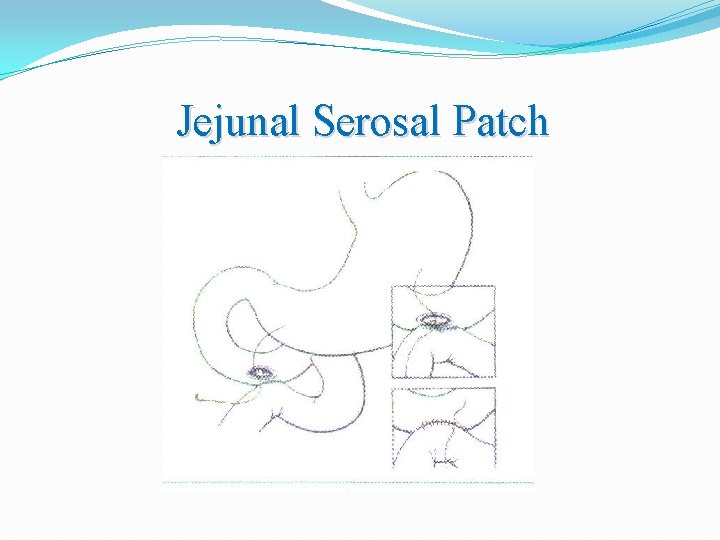
Jejunal Serosal Patch • The serosa of a loop of jejunum is sutured to the edge of the duodenal defect • The serosa exposed to the duodenal lumen rapidly undergoes complete mucosal resurfacing.
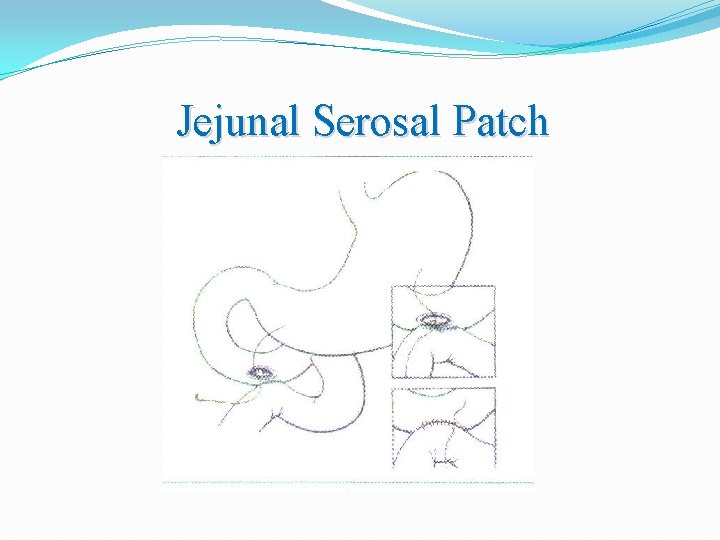
Jejunal Serosal Patch

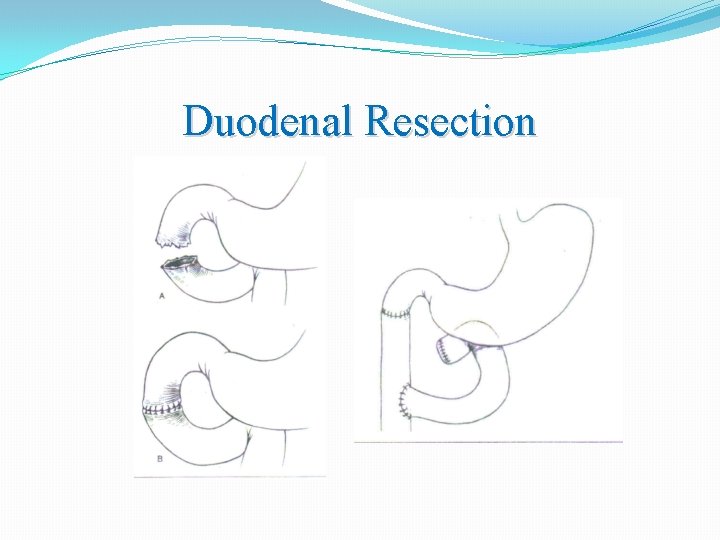
Duodenal Resection • If nearly the entire circumference of the duodenum is devitalized, a segmental resection with an end-to-end duodenostomy may be performed • If it is not possible to mobilize the duodenum without tension, a Roux-en-Y duodenojejunostomy can be performed with the distal duodenum oversewn.
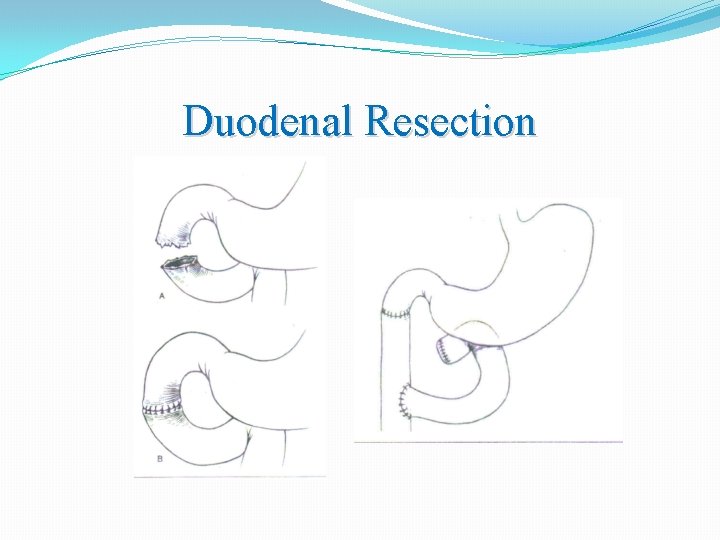
Duodenal Resection
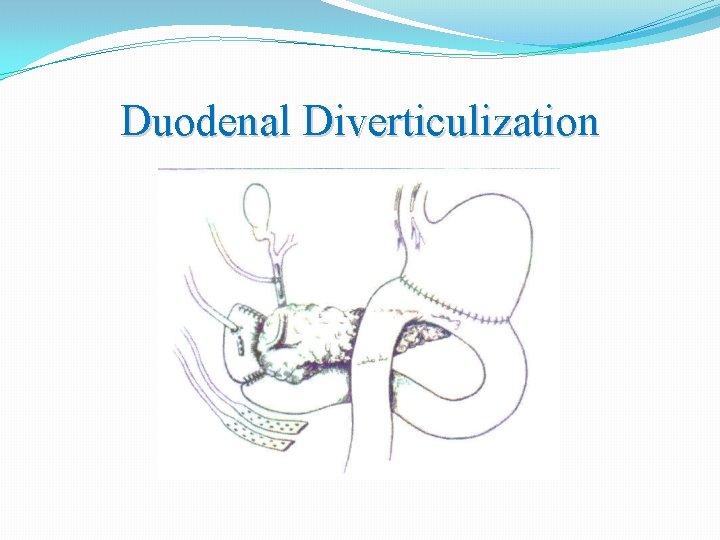
Duodenal Diverticulization • Originally described by Berne in 1968 • The concept is to completely divert both gastric and biliary contents • antrectomy, debridement and repair of the duodenum tube duodenostomy vagotomy biliary tract drainage(T-tube) feeding jejunostomy tube • Procedure is very time-consuming and may or may not require all of the steps
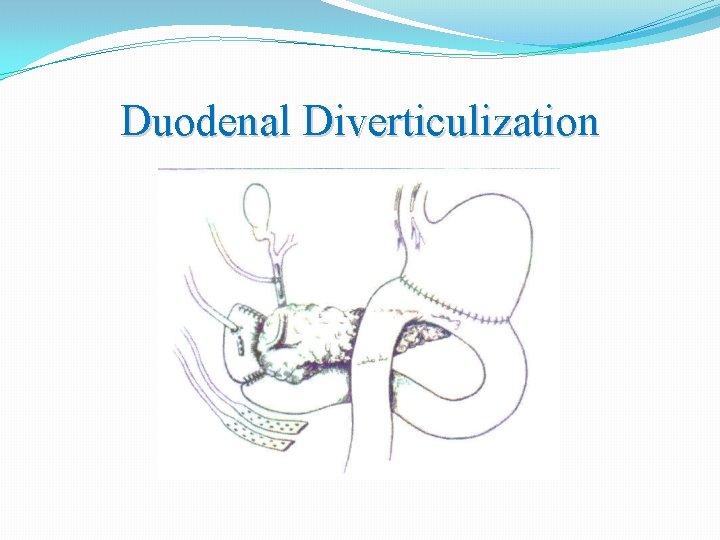
Duodenal Diverticulization
Grade 5 duodenal injury • Massive disruption of duodeopancreatic complex • Duodenal devascularization • Whipple for Trauma
Whipple for Trauma • Performed as a staged procedure • Control of hemorrhage, resection debridement in the initial laparotomy stapler resection of the duodenal sweep and pancreatic head, ligation of the common bile duct at pancreatic head • Resuscitation in the ICU • Gastrointestinal reconstruction with pancreatic remnant anastomosis and choledochojejunal anastomosis
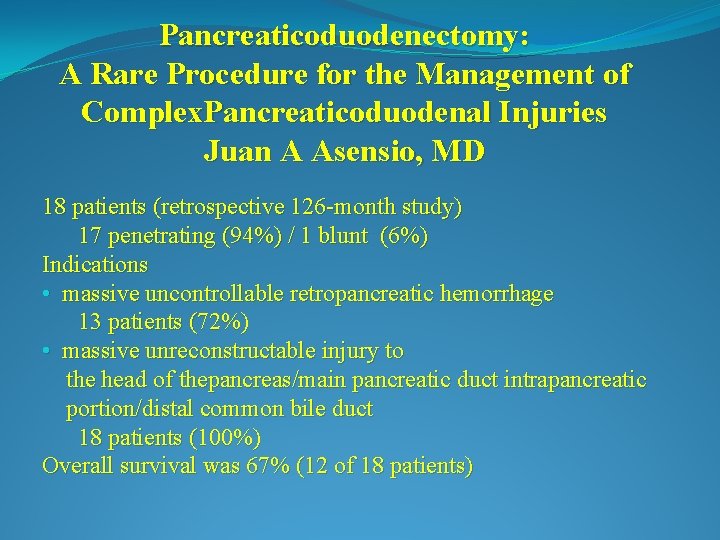
Pancreaticoduodenectomy: A Rare Procedure for the Management of Complex. Pancreaticoduodenal Injuries Juan A Asensio, MD 18 patients (retrospective 126 -month study) 17 penetrating (94%) / 1 blunt (6%) Indications • massive uncontrollable retropancreatic hemorrhage 13 patients (72%) • massive unreconstructable injury to the head of thepancreas/main pancreatic duct intrapancreatic portion/distal common bile duct 18 patients (100%) Overall survival was 67% (12 of 18 patients)
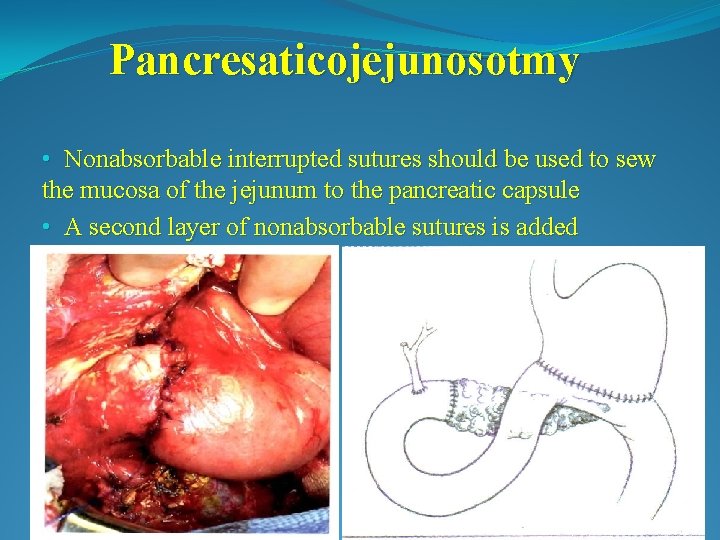
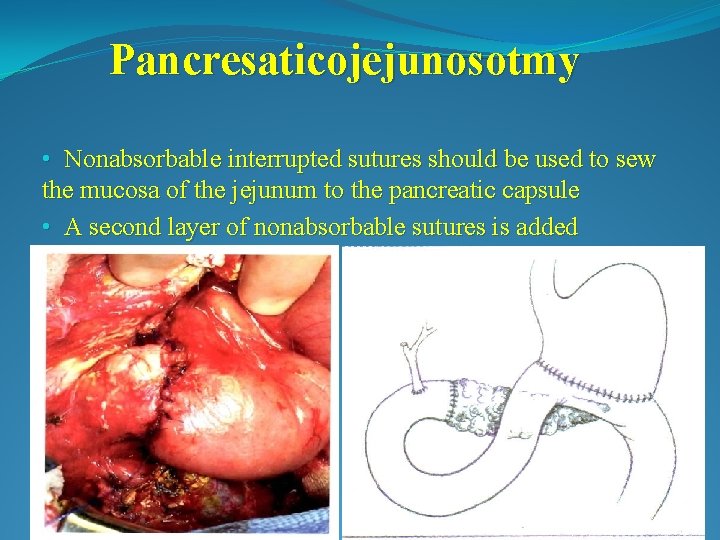
Pancresaticojejunosotmy • Nonabsorbable interrupted sutures should be used to sew the mucosa of the jejunum to the pancreatic capsule • A second layer of nonabsorbable sutures is added
 Antigentest åre
Antigentest åre Sleeve gastrectomy complications
Sleeve gastrectomy complications Gastric ucler
Gastric ucler Kelling madlener procedure
Kelling madlener procedure Anatomy and physiology of peptic ulcer ppt
Anatomy and physiology of peptic ulcer ppt Duodenoduodenostomy
Duodenoduodenostomy Duodenal atresia jaundice
Duodenal atresia jaundice Vagotomia
Vagotomia Dynamic vs adynamic intestinal obstruction
Dynamic vs adynamic intestinal obstruction Derivación biliopancreática con cruce duodenal
Derivación biliopancreática con cruce duodenal Duodenorrhaphy anastomosis
Duodenorrhaphy anastomosis Duodenorrhaphy
Duodenorrhaphy Tercera porción del duodeno
Tercera porción del duodeno Ot pufagi toshi
Ot pufagi toshi Gastro duodenal junction
Gastro duodenal junction Types of vagotomy
Types of vagotomy Epiploic foramen
Epiploic foramen Duodenal switch
Duodenal switch Modified johnson classification for gastric ulcer
Modified johnson classification for gastric ulcer Left mesenteric sinus
Left mesenteric sinus El sistema digestivo de las aves es completo o incompleto
El sistema digestivo de las aves es completo o incompleto Que tipo de glandula es el pancreas
Que tipo de glandula es el pancreas Duodenal exclusion
Duodenal exclusion Méthode de taylor ulcère
Méthode de taylor ulcère Supracristal plane
Supracristal plane Regio lumbalis sinistra
Regio lumbalis sinistra Pancreas embryology
Pancreas embryology Nursing management of duodenal ulcer
Nursing management of duodenal ulcer Tim madsen everest
Tim madsen everest Unit 15:6 providing first aid for burns
Unit 15:6 providing first aid for burns Hunger games chapter 22 questions and answers
Hunger games chapter 22 questions and answers Sentinel injuries in infants are
Sentinel injuries in infants are Westfield sports injuries
Westfield sports injuries Stobhill miu
Stobhill miu Human crutch method first aid
Human crutch method first aid A short backboard or vest-style immobilization
A short backboard or vest-style immobilization Chapter 21 caring for head and spine injuries
Chapter 21 caring for head and spine injuries Test chapter 17 first aid
Test chapter 17 first aid Chapter 15 injuries to muscles and bones
Chapter 15 injuries to muscles and bones Chapter 14 promotion of safety
Chapter 14 promotion of safety Jones and bartlett learning
Jones and bartlett learning Chapter 13:2 preventing accidents and injuries
Chapter 13:2 preventing accidents and injuries Chapter 11 injuries to the shoulder region
Chapter 11 injuries to the shoulder region Chapter 11 assessment and evaluation of sports injuries
Chapter 11 assessment and evaluation of sports injuries Tnt swimming
Tnt swimming Pallet jack injuries
Pallet jack injuries The cause-specific mortality rate from roller-skating was:
The cause-specific mortality rate from roller-skating was: Jsp 539
Jsp 539 Climatic injury
Climatic injury Chapter 12 lesson 3 planning a personal activity program
Chapter 12 lesson 3 planning a personal activity program Chapter 4 preventing injuries through fitness
Chapter 4 preventing injuries through fitness Chapter 13 worksheet recognizing different sports injuries
Chapter 13 worksheet recognizing different sports injuries Chapter 4 basics of tissue injuries
Chapter 4 basics of tissue injuries Bo taoshi injuries
Bo taoshi injuries Miniscus replacement
Miniscus replacement