CHRONIC INFLAMMATION CHRONIC INFLAMMATION Prolonged inflammatory response to























- Slides: 57
CHRONIC INFLAMMATION

CHRONIC INFLAMMATION • Prolonged inflammatory response to persistent or recurrent stimulous. • Destruction and inflammation are proceeding at the same time along with an attempt at healing.
Causes of chronic inflammation • Persistent infections – Organisms usually of low toxicity that invoke delayed hypersensitivity reaction – M. tuberculosis and T. pallidum causes granulomatous reaction • Prolonged exposure to potentially toxic agents – Exogenous agents include silica which causes silicosis – Endogenous causes include atherosclerosis caused by toxic plasma lipid components
• Autoimmunity – Auto-antigens provoke self-perpetuating immune responses that cause chronic inflammatory diseases like RA, MS – Responses against common environmental substances cause chronic allergic diseases, such as bronchial asthma
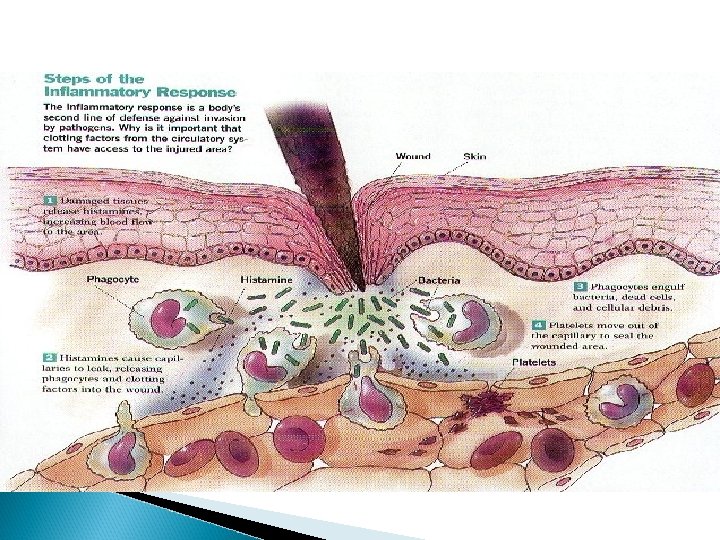
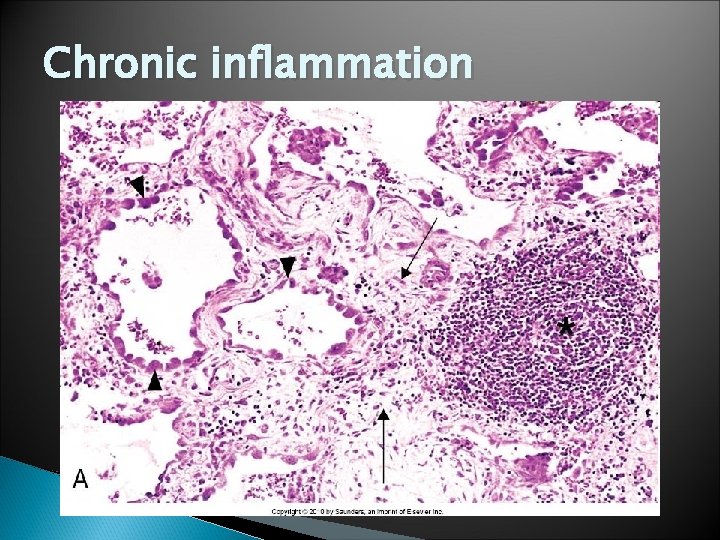
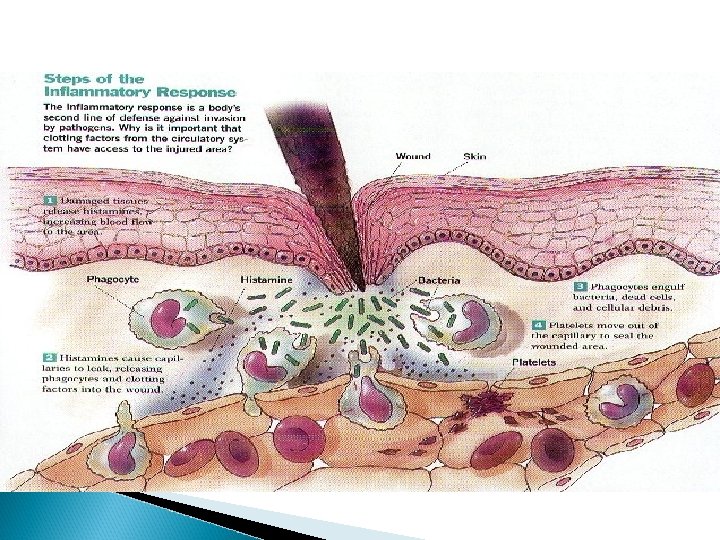
HISTOLOGICAL CHARACTERISTICS � Infiltration with mononuclear cells (eg. macrophages, lymphocytes and plasma cells) due to persistent reaction to injury � Tissue destruction induced by persistent agent or inflammatory cells � Attempts at healing by connective tissue replacement of damaged tissue with angiogenesis and fibrosis
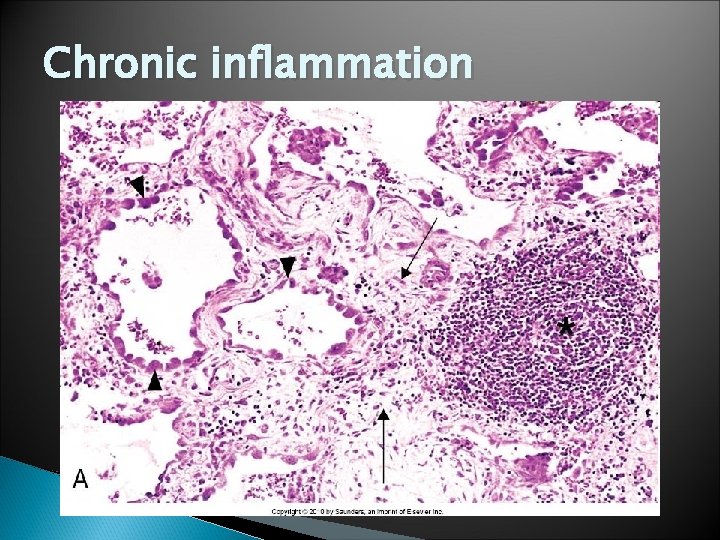
Chronic inflammation
MORPHOLOGY • INFILTRATION • TISSUE DESTRUCTION • HEALING
CELLS IN CHRONIC INFLAMMATION
Cellular Players • MACROPHAGES (aka, HISTIOCYTES) • LYMPHOCYTES • PLASMA CELLS • EOSINOPHILS • MAST CELLS
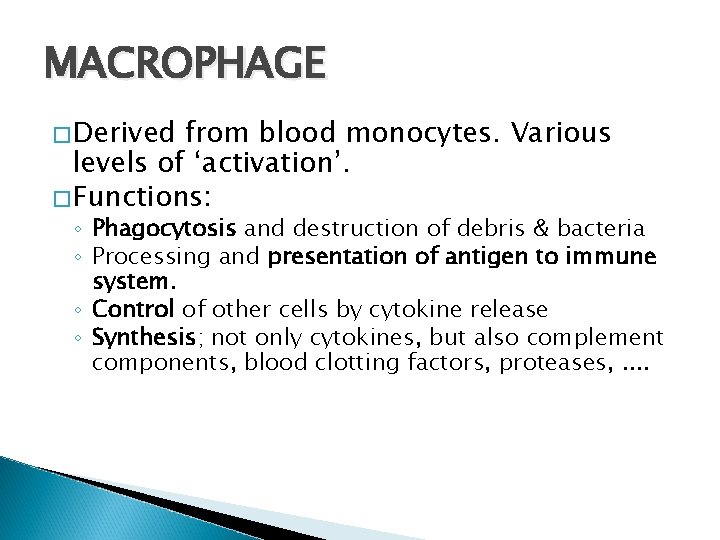
MACROPHAGE �Derived from blood monocytes. Various levels of ‘activation’. �Functions: ◦ Phagocytosis and destruction of debris & bacteria ◦ Processing and presentation of antigen to immune system. ◦ Control of other cells by cytokine release ◦ Synthesis; not only cytokines, but also complement components, blood clotting factors, proteases, . .
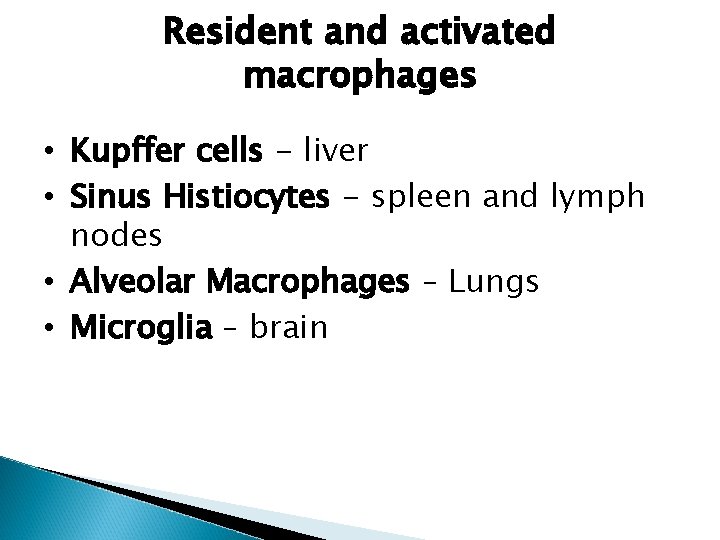
Resident and activated macrophages • Kupffer cells - liver • Sinus Histiocytes - spleen and lymph nodes • Alveolar Macrophages – Lungs • Microglia – brain


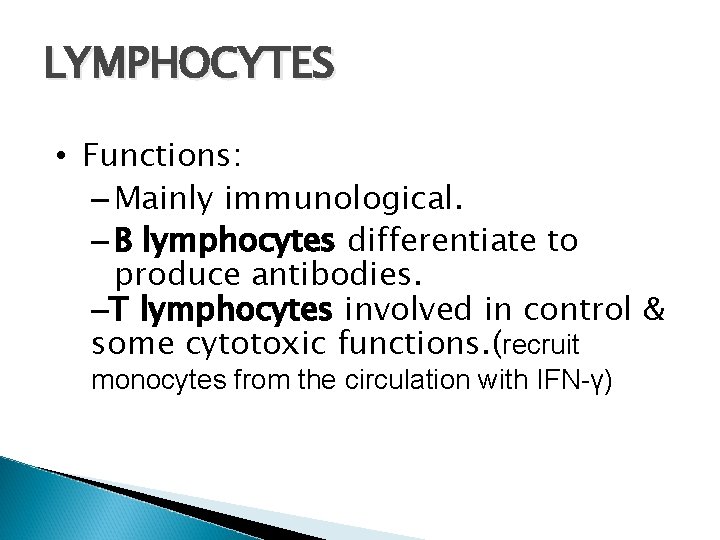
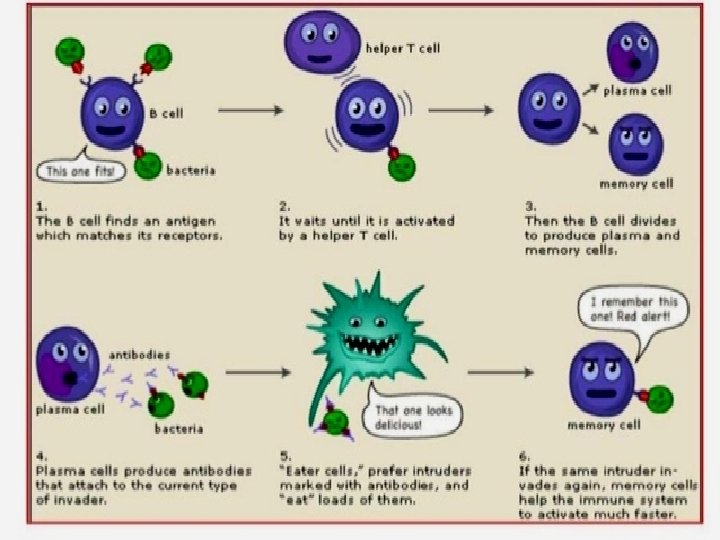
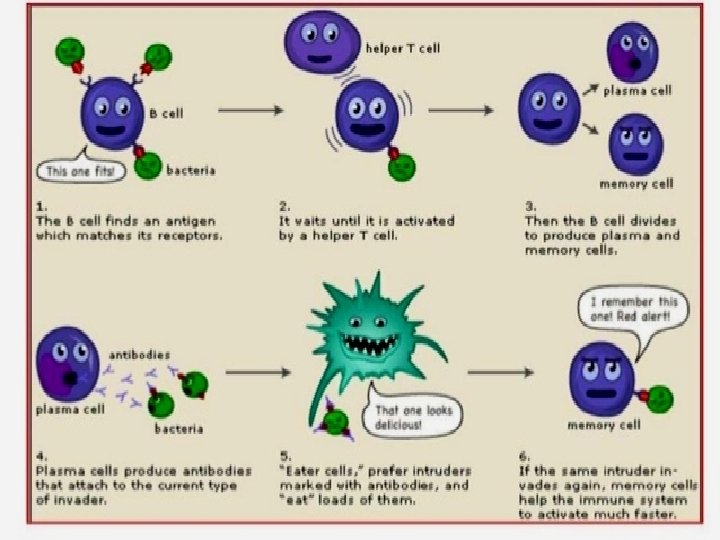
LYMPHOCYTES • Functions: – Mainly immunological. – B lymphocytes differentiate to produce antibodies. –T lymphocytes involved in control & some cytotoxic functions. (recruit monocytes from the circulation with IFN-γ)




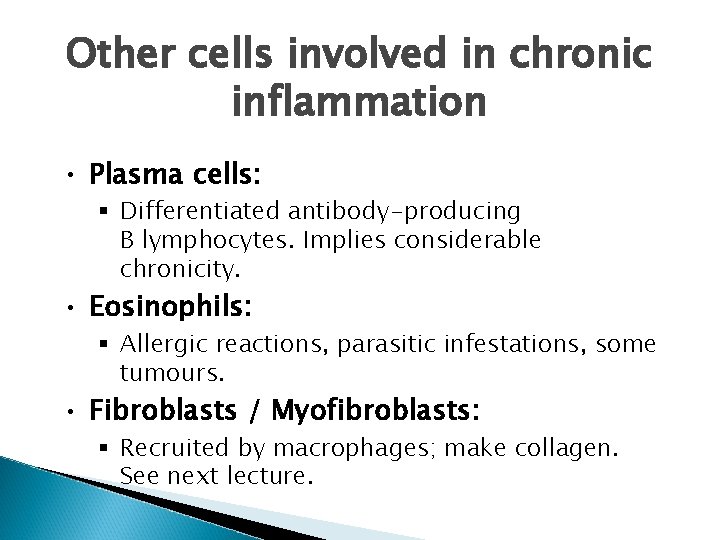
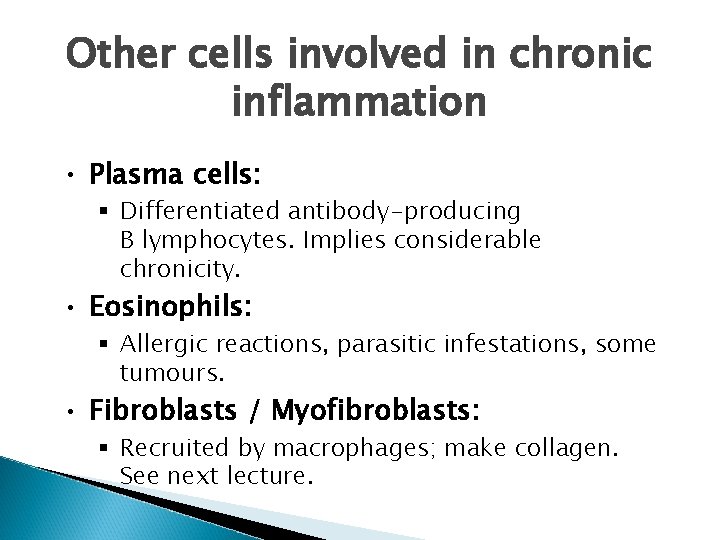
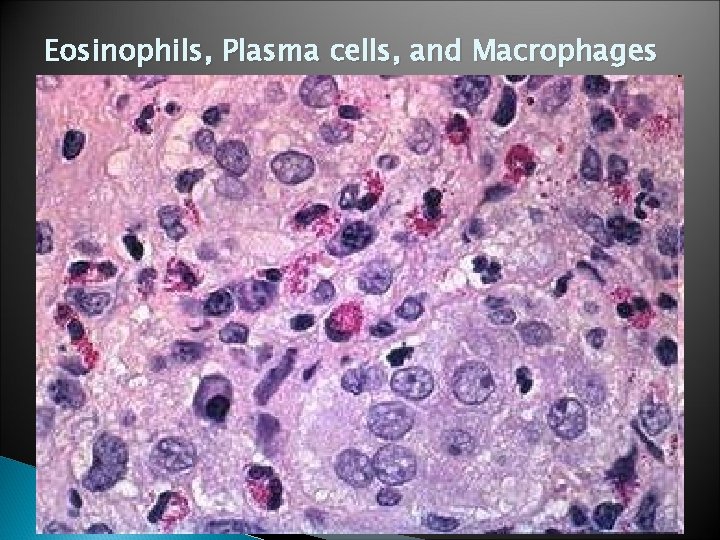
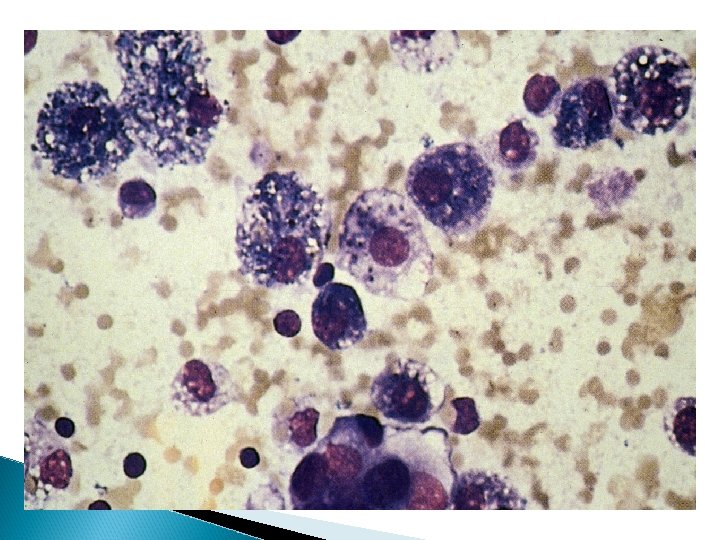
Other cells involved in chronic inflammation • Plasma cells: § Differentiated antibody-producing B lymphocytes. Implies considerable chronicity. • Eosinophils: § Allergic reactions, parasitic infestations, some tumours. • Fibroblasts / Myofibroblasts: § Recruited by macrophages; make collagen. See next lecture.
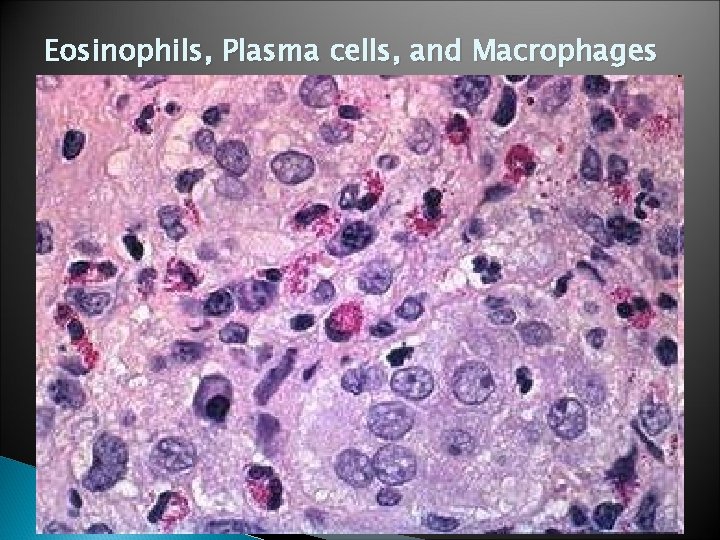
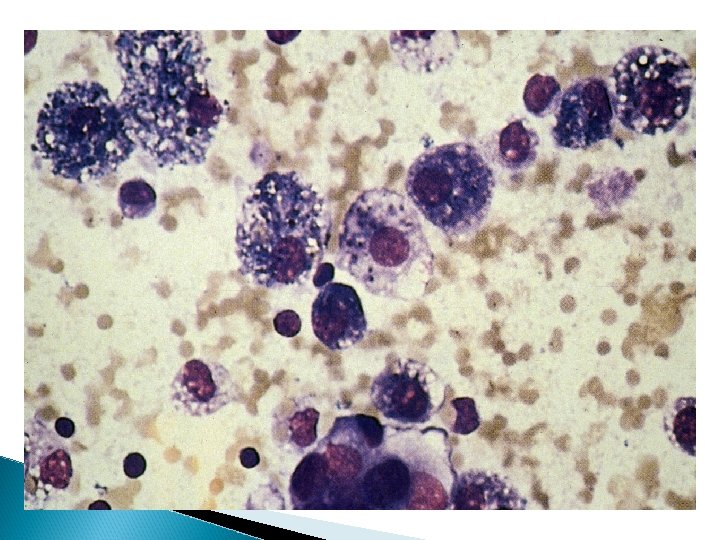
Eosinophils, Plasma cells, and Macrophages


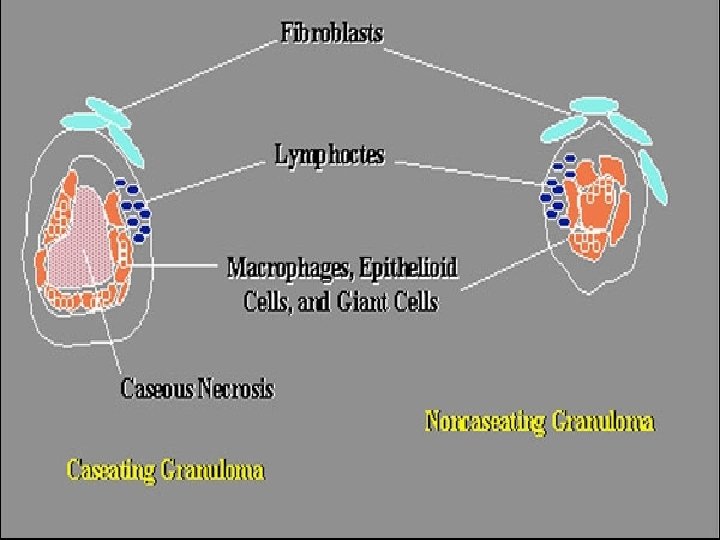
CHRONIC INFLAMMATION GRANULOMATOUS CASEATING NON SPECIFIC NON CASEATING
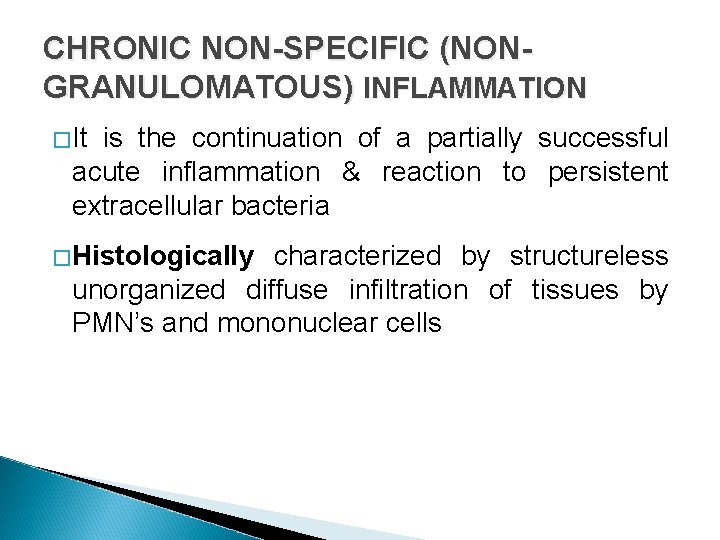
CHRONIC NON-SPECIFIC (NONGRANULOMATOUS) INFLAMMATION �It is the continuation of a partially successful acute inflammation & reaction to persistent extracellular bacteria �Histologically characterized by structureless unorganized diffuse infiltration of tissues by PMN’s and mononuclear cells

Granulomatous inflammation Distinctive pattern of chronic inflammation. Cellular attempt to contain an offending agent that is difficult to eradicate (i. e. Tb) Protective response to chronic infection or foreign material, preventing dissemination and restricting inflammation. �Persistent, low-grade antigenic stimulation �Hypersensitivity
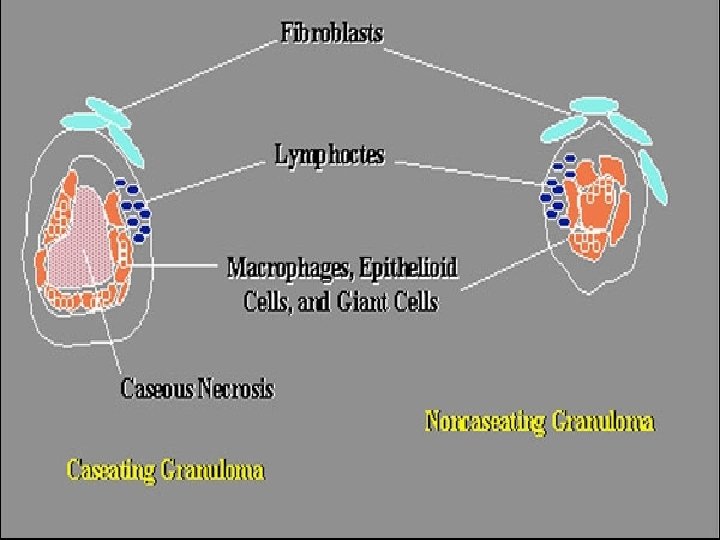
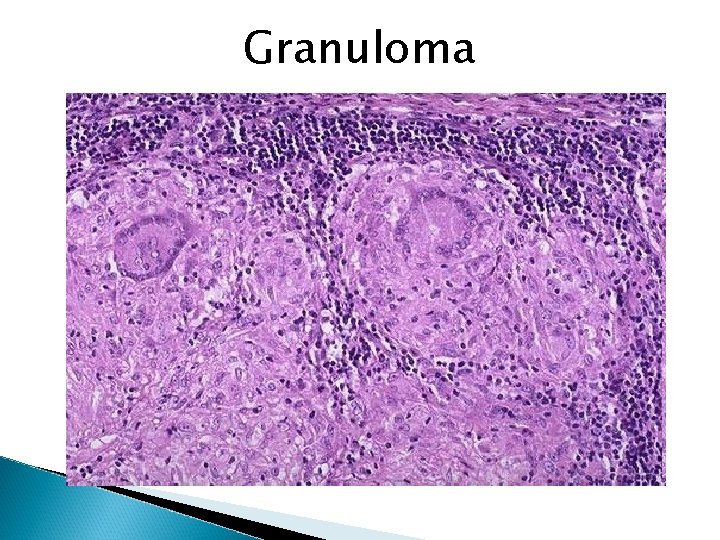
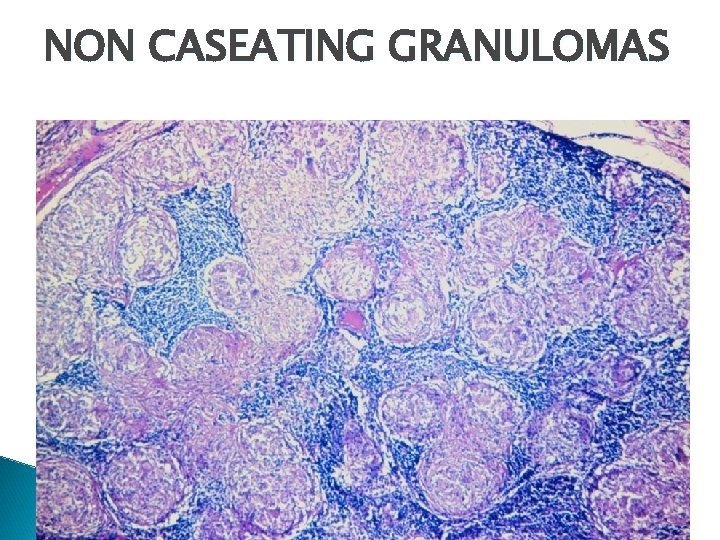
�A granuloma is a microscopic aggregation of macrophages that are transformed into epithelioid cells and giant cells surrounded by a collar of mononuclear leukocytes, principally lymphocytes and occasionally plasma cells


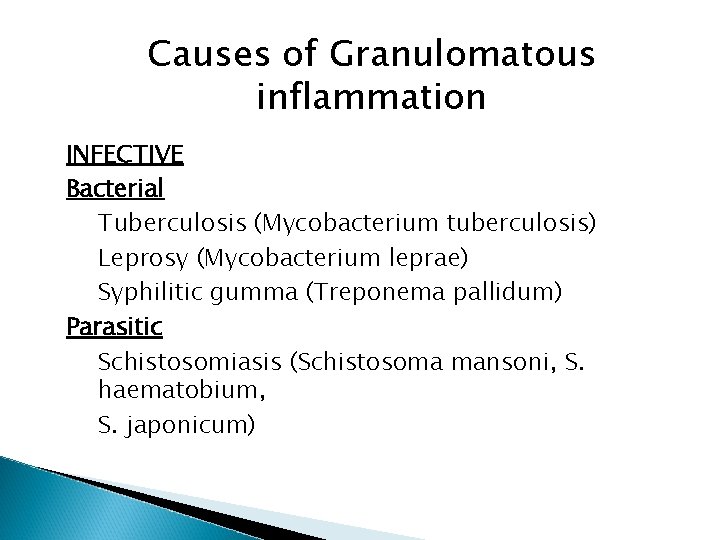
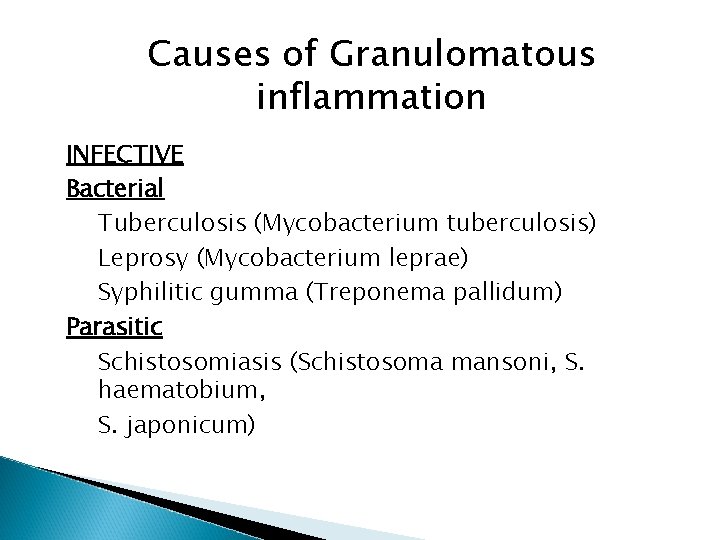
Causes of Granulomatous inflammation INFECTIVE Bacterial Tuberculosis (Mycobacterium tuberculosis) Leprosy (Mycobacterium leprae) Syphilitic gumma (Treponema pallidum) Parasitic Schistosomiasis (Schistosoma mansoni, S. haematobium, S. japonicum)
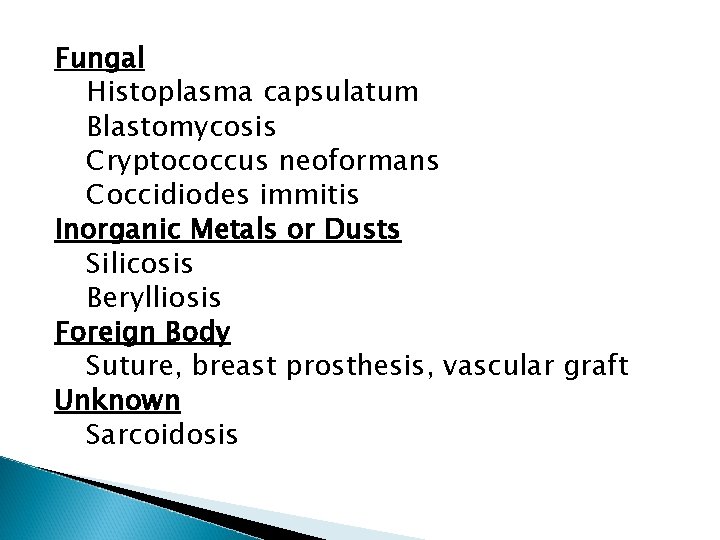
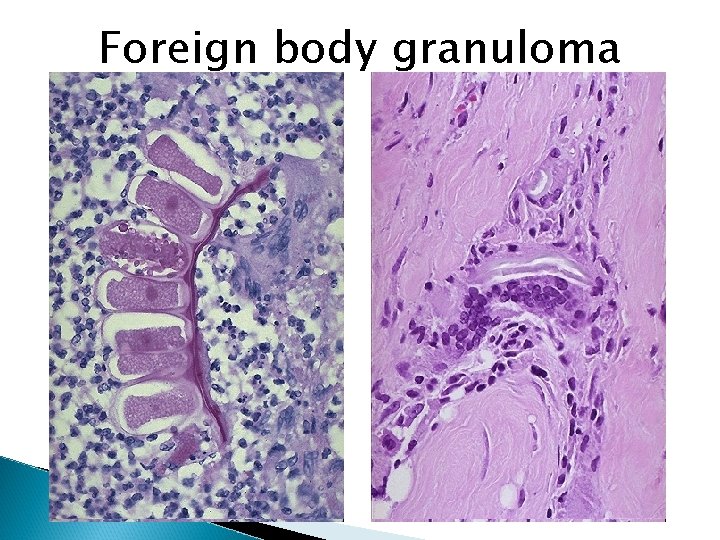
Fungal Histoplasma capsulatum Blastomycosis Cryptococcus neoformans Coccidiodes immitis Inorganic Metals or Dusts Silicosis Berylliosis Foreign Body Suture, breast prosthesis, vascular graft Unknown Sarcoidosis
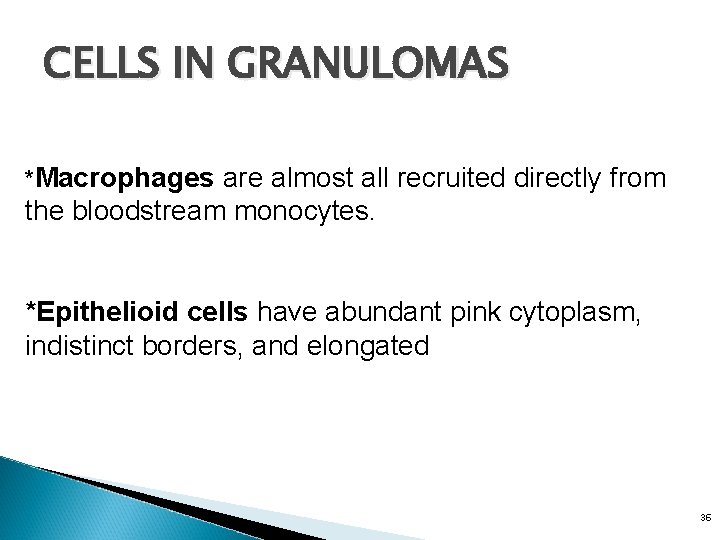
CELLS IN GRANULOMAS *Macrophages are almost all recruited directly from the bloodstream monocytes. *Epithelioid cells have abundant pink cytoplasm, indistinct borders, and elongated 36
The giant cells 40 to 50 µ in dia -abundant cytoplasm, multiple nuclei. *Plasma cells produce antibodies against the persistent antigen or the altered tissue components. *Lymphocytes are likely to be present even where there is no involvement of the immune system.

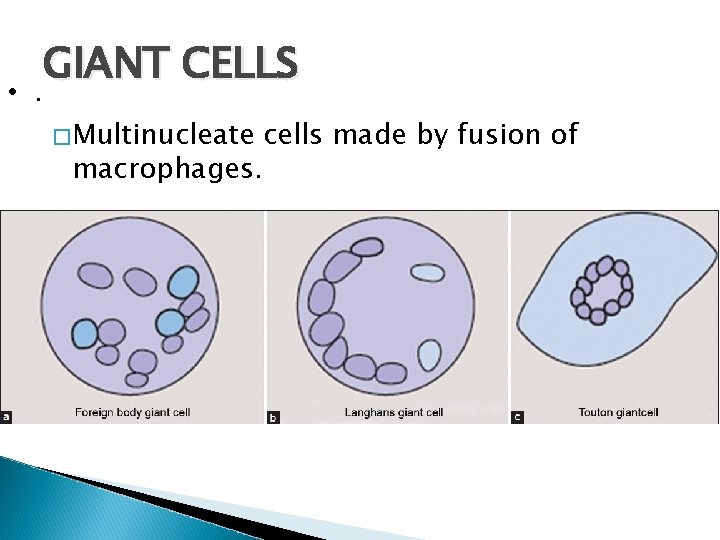
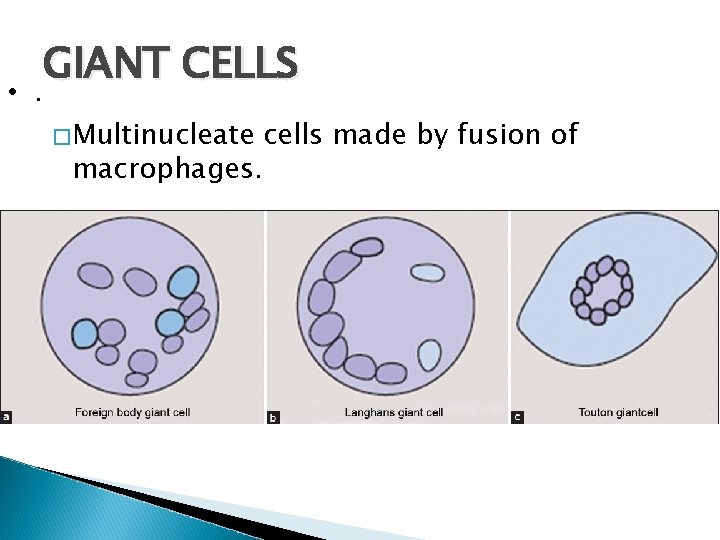
• . GIANT CELLS �Multinucleate macrophages. cells made by fusion of
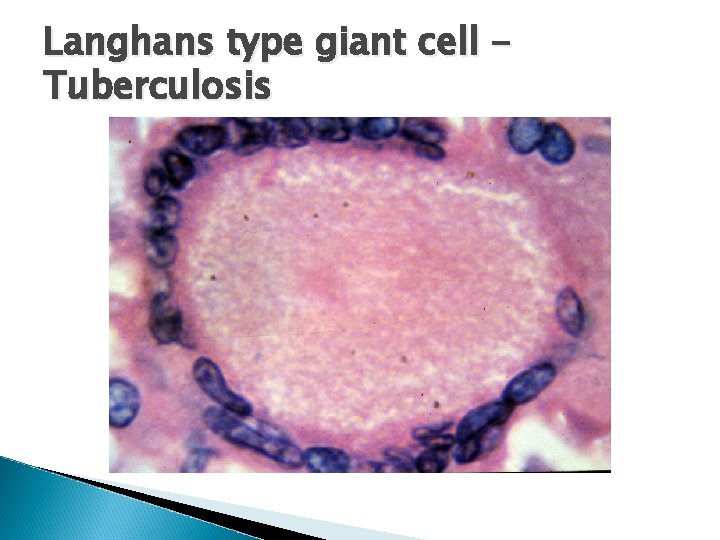
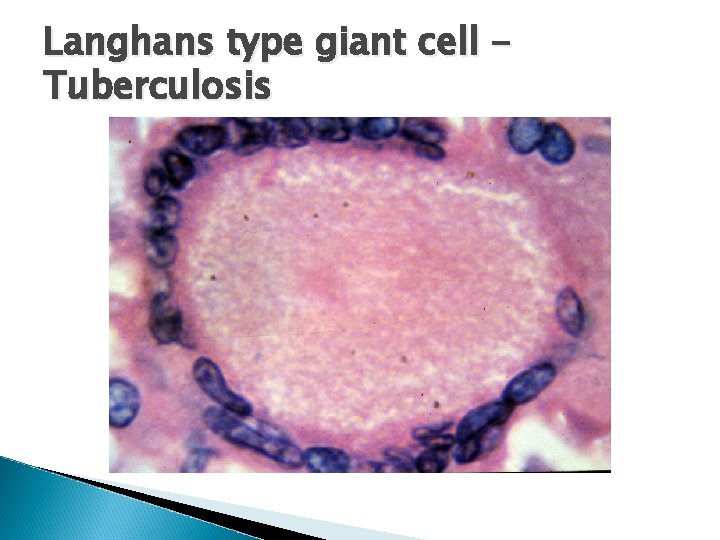
Langhans type giant cell Tuberculosis

Foreign body type giant cells

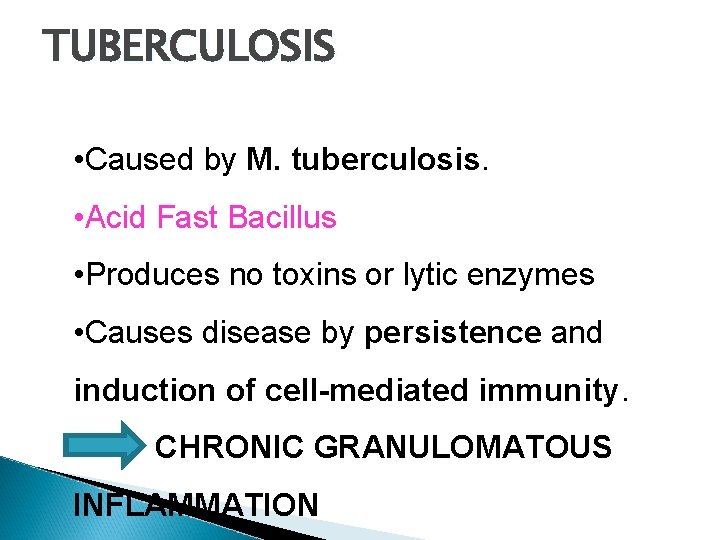
TUBERCULOSIS • Caused by M. tuberculosis. • Acid Fast Bacillus • Produces no toxins or lytic enzymes • Causes disease by persistence and induction of cell-mediated immunity. • CHRONIC GRANULOMATOUS INFLAMMATION
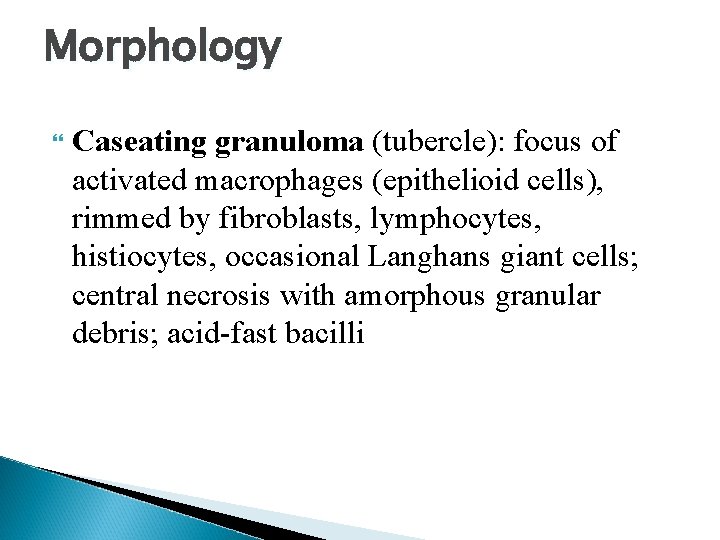
Morphology Caseating granuloma (tubercle): focus of activated macrophages (epithelioid cells), rimmed by fibroblasts, lymphocytes, histiocytes, occasional Langhans giant cells; central necrosis with amorphous granular debris; acid-fast bacilli






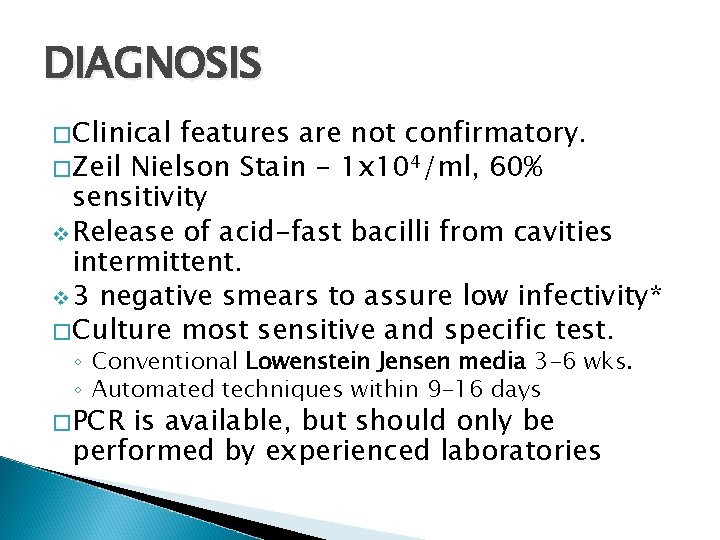
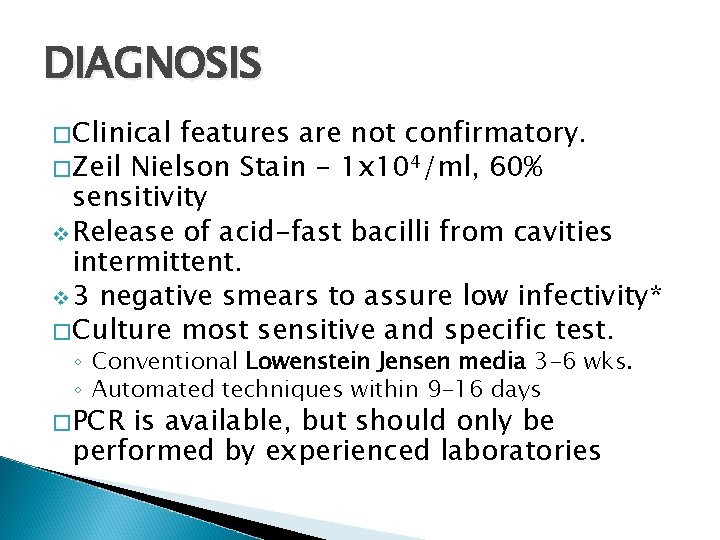
DIAGNOSIS � Clinical features are not confirmatory. � Zeil Nielson Stain - 1 x 104/ml, 60% sensitivity v Release of acid-fast bacilli from cavities intermittent. v 3 negative smears to assure low infectivity* � Culture most sensitive and specific test. ◦ Conventional Lowenstein Jensen media 3 -6 wks. ◦ Automated techniques within 9 -16 days � PCR is available, but should only be performed by experienced laboratories


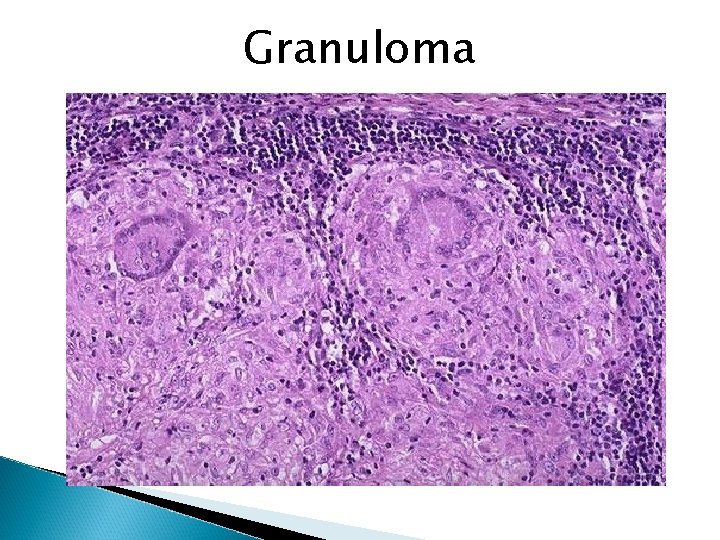
Granuloma
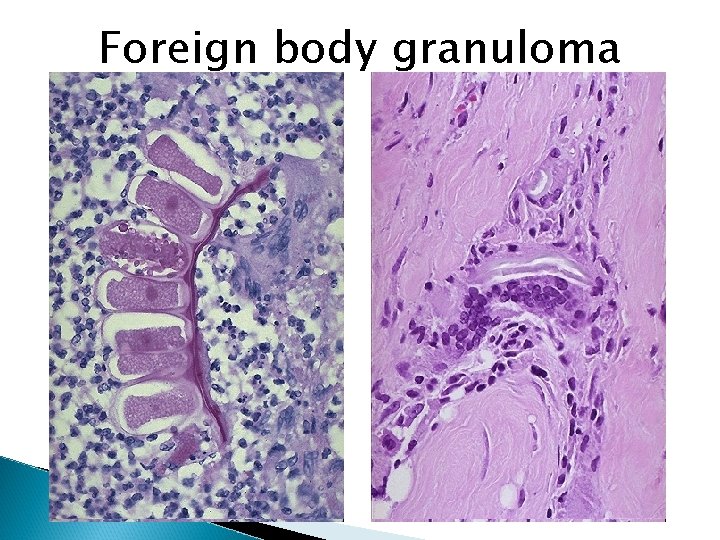
Foreign body granuloma
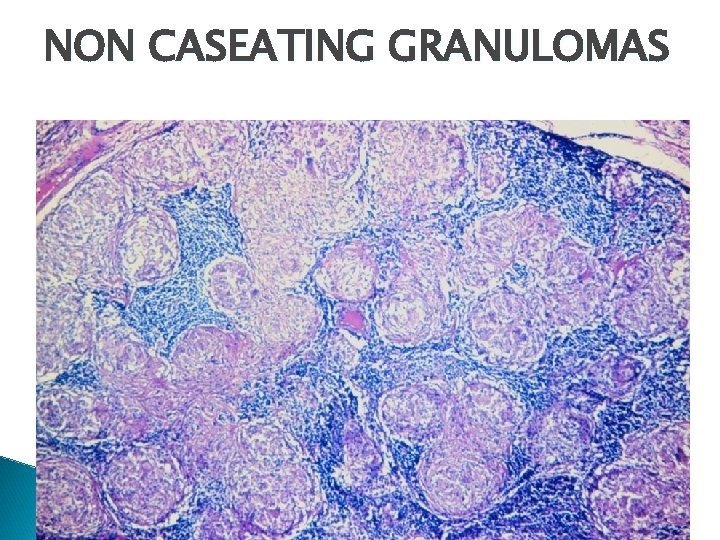
NON CASEATING GRANULOMAS
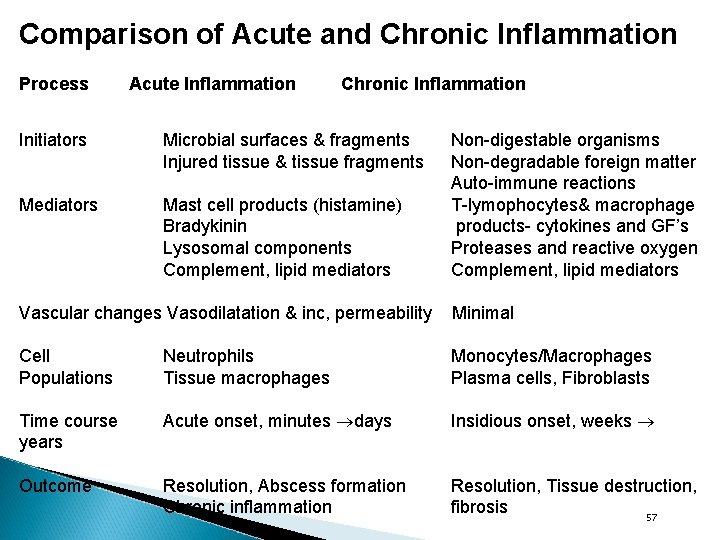
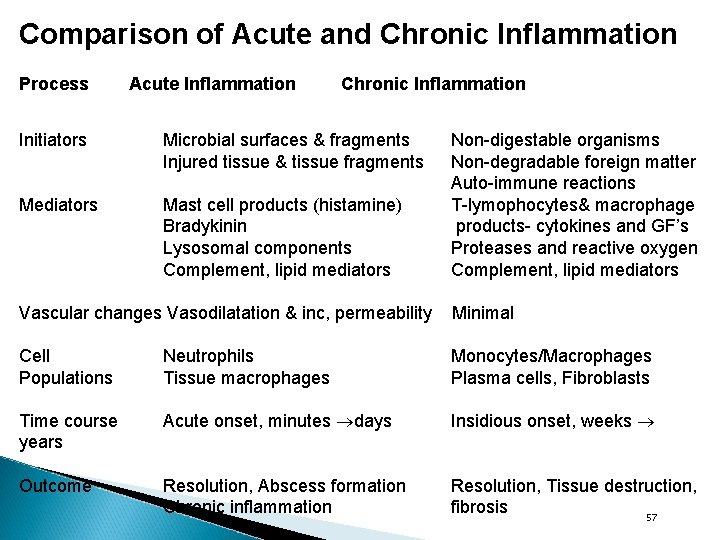
Comparison of Acute and Chronic Inflammation Process Acute Inflammation Chronic Inflammation Initiators Microbial surfaces & fragments Injured tissue & tissue fragments Mediators Mast cell products (histamine) Bradykinin Lysosomal components Complement, lipid mediators Non-digestable organisms Non-degradable foreign matter Auto-immune reactions T-lymophocytes& macrophage products- cytokines and GF’s Proteases and reactive oxygen Complement, lipid mediators Vascular changes Vasodilatation & inc, permeability Minimal Cell Populations Neutrophils Tissue macrophages Monocytes/Macrophages Plasma cells, Fibroblasts Time course years Acute onset, minutes days Insidious onset, weeks Outcome Resolution, Abscess formation Chronic inflammation Resolution, Tissue destruction, fibrosis 57