Granulomatous inflammation Granulomatous inflammation A granuloma is a


![TB q. Primary tuberculosis [initial infection] qsecondary tuberculosis [ re-activation or re -infection ] TB q. Primary tuberculosis [initial infection] qsecondary tuberculosis [ re-activation or re -infection ]](https://slidetodoc.com/presentation_image/9050a328c089a8f9f9ef2b73af4ad449/image-26.jpg)
![Primary tuberculosis • Non immunized individual [initial infection] – children • Subpleural zone of Primary tuberculosis • Non immunized individual [initial infection] – children • Subpleural zone of](https://slidetodoc.com/presentation_image/9050a328c089a8f9f9ef2b73af4ad449/image-27.jpg)







- Slides: 75
Granulomatous inflammation
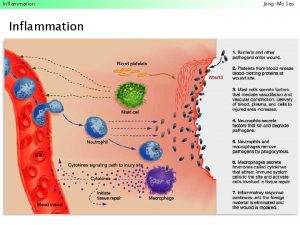
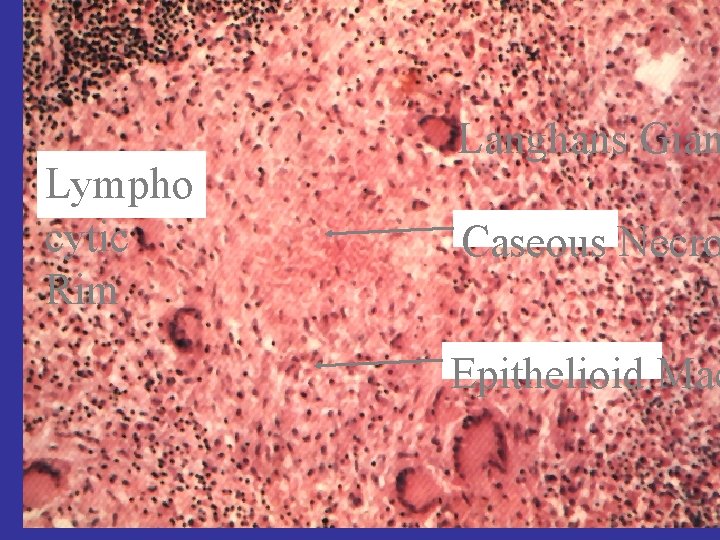
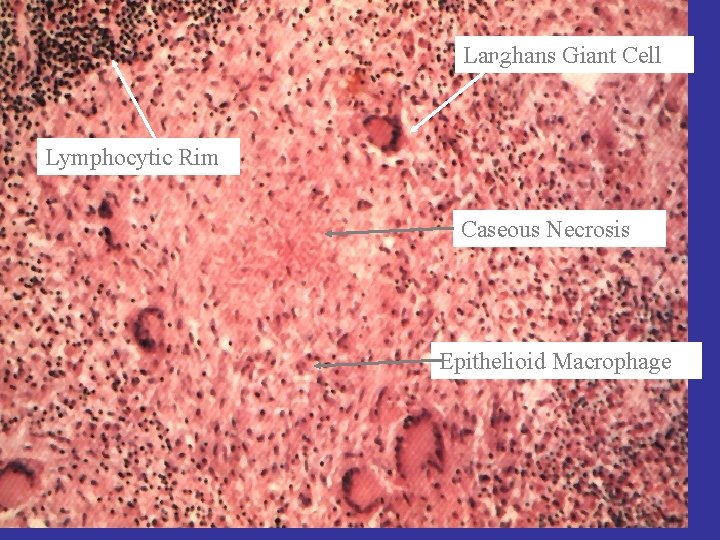
Granulomatous inflammation • A granuloma is a microscopic aggregation of macrophages that are transformed into epithelium-like cells surrounded by a collar of mononuclear leukocytes, principally lymphocytes and occasionally plasma cells.
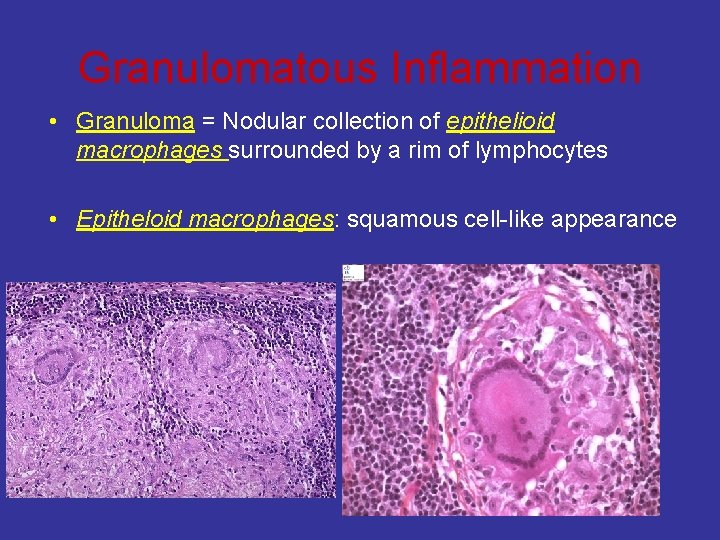
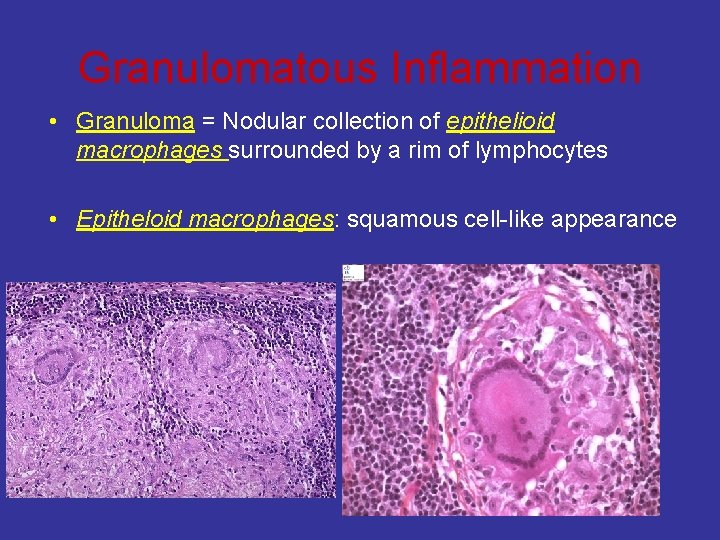
Granulomatous Inflammation • Granuloma = Nodular collection of epithelioid macrophages surrounded by a rim of lymphocytes • Epitheloid macrophages: squamous cell-like appearance
Why is it important? • Granulomas are encountered in certain specific pathologic states; consequently, recognition of the granulomatous pattern is important because of the limited number of conditions (some life-threatening) that cause it
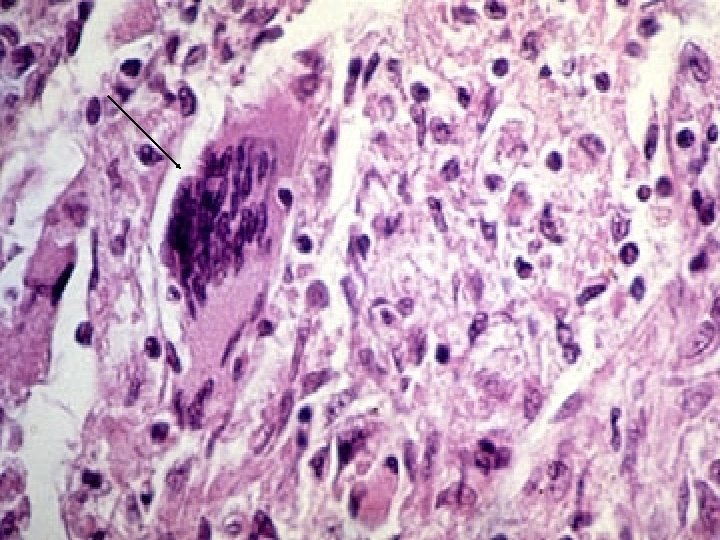
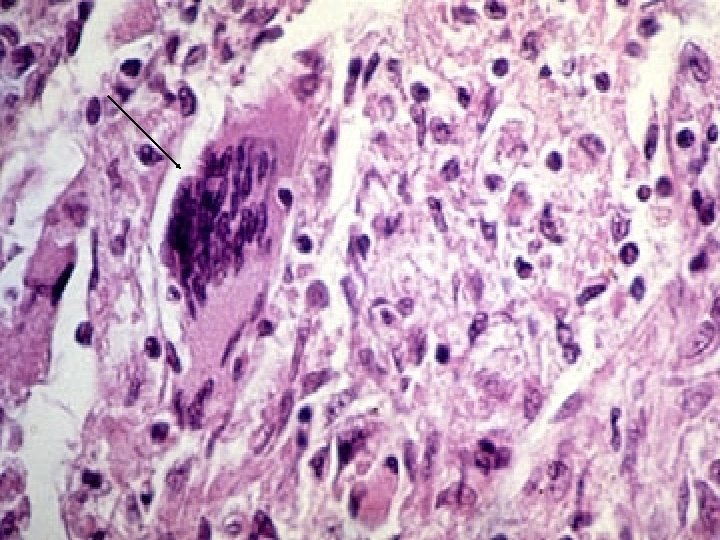
Granulomatous inflammation • Epithelioid cells fuse to form giant cells containing 20 or more nuclei. • The nuclei arranged either peripherally (Langhans-type giant cell) or • haphazardly (foreign body-type giant cell). • These giant cells can be found either at the periphery or the center of the granuloma.
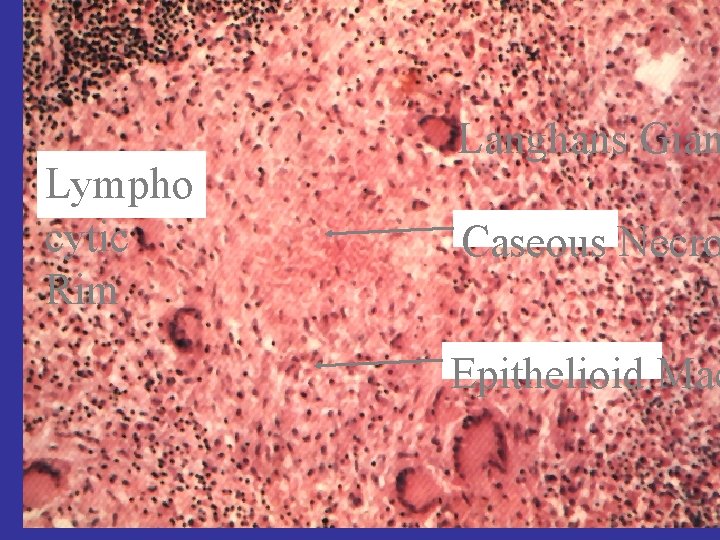
Lympho cytic Rim Langhans Gian Caseous Necro Epithelioid Mac
CAUSES OF GRANULOMATOUS DISEASES
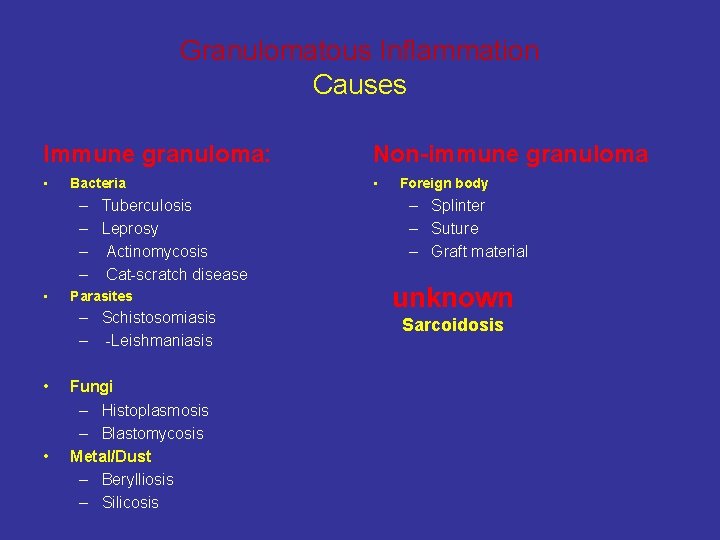
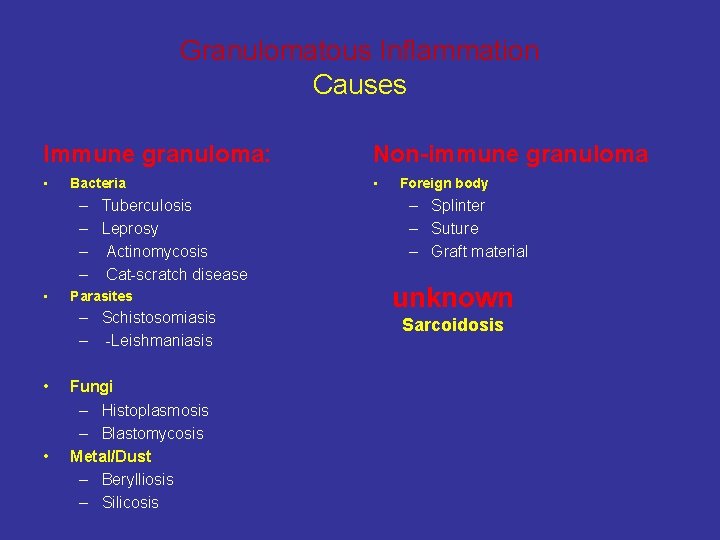
Granulomatous Inflammation Causes Immune granuloma: Non-immune granuloma • • Bacteria – Tuberculosis – Leprosy – Actinomycosis – Cat-scratch disease • Parasites – Schistosomiasis – -Leishmaniasis • • Fungi – Histoplasmosis – Blastomycosis Metal/Dust – Berylliosis – Silicosis Foreign body – Splinter – Suture – Graft material unknown Sarcoidosis
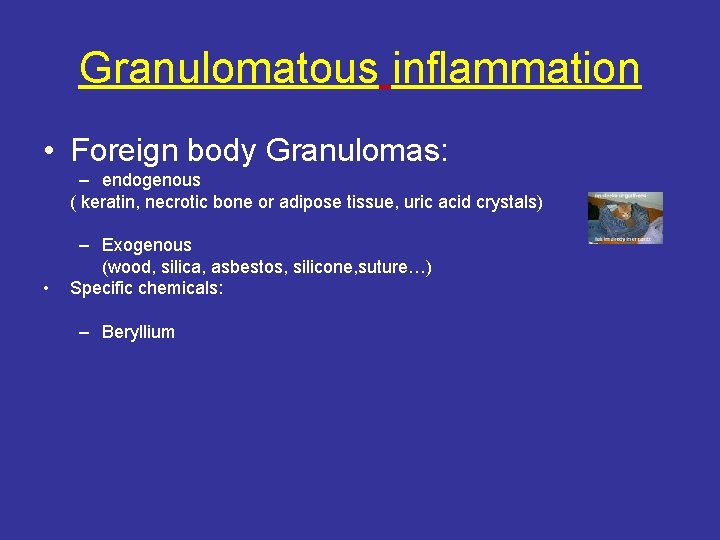
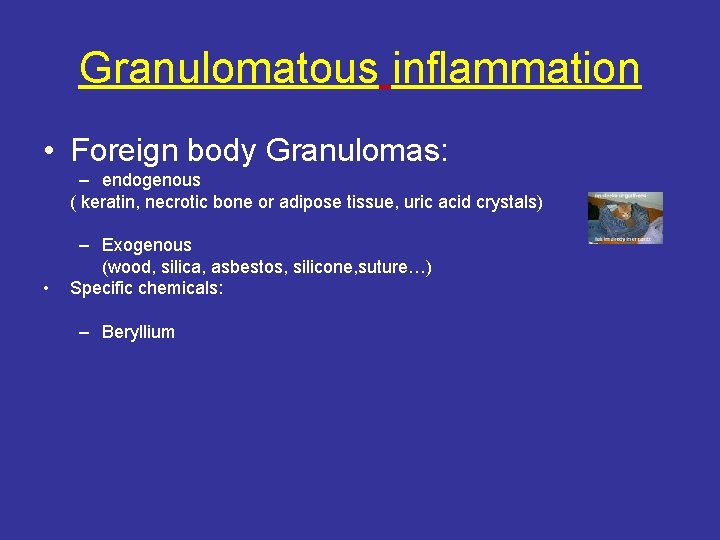
Granulomatous inflammation • Foreign body Granulomas: – endogenous ( keratin, necrotic bone or adipose tissue, uric acid crystals) • – Exogenous (wood, silica, asbestos, silicone, suture…) Specific chemicals: – Beryllium

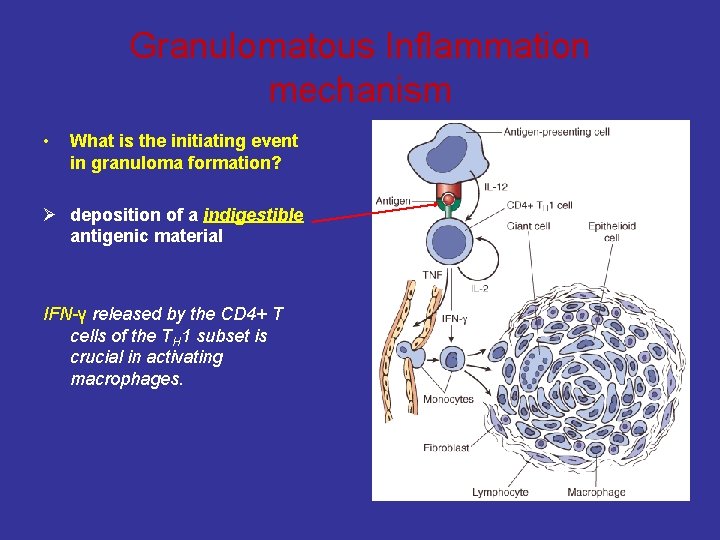
Mechanism Of granuloma formation
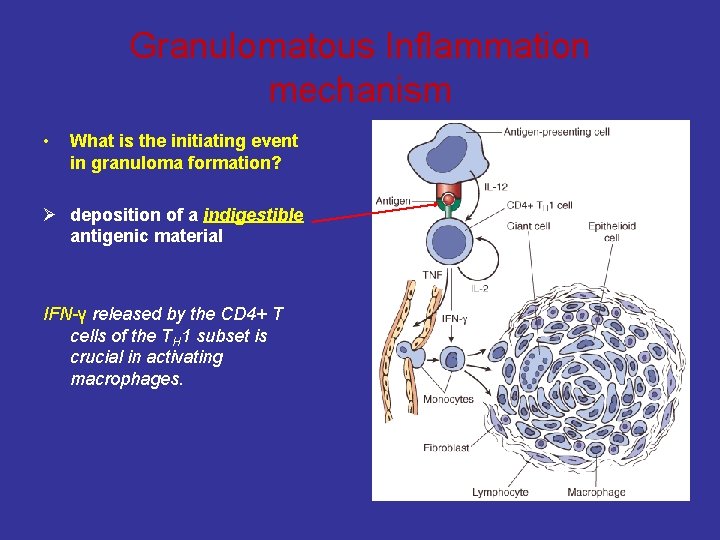
Granulomatous Inflammation mechanism • What is the initiating event in granuloma formation? Ø deposition of a indigestible antigenic material IFN-γ released by the CD 4+ T cells of the TH 1 subset is crucial in activating macrophages.
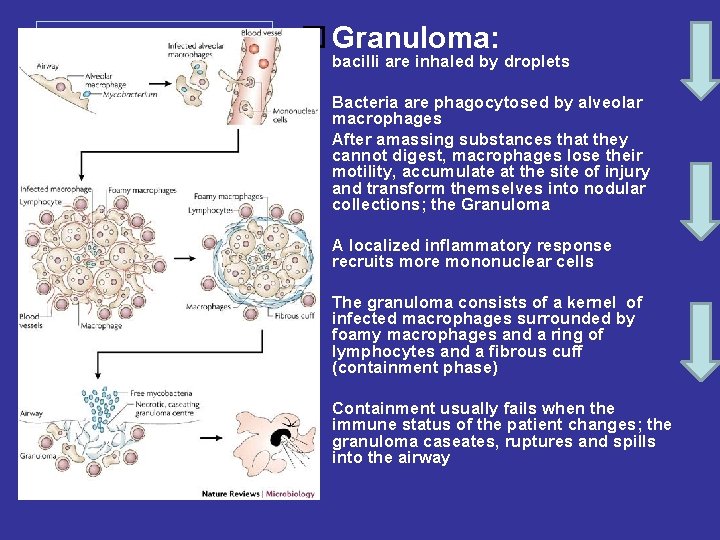
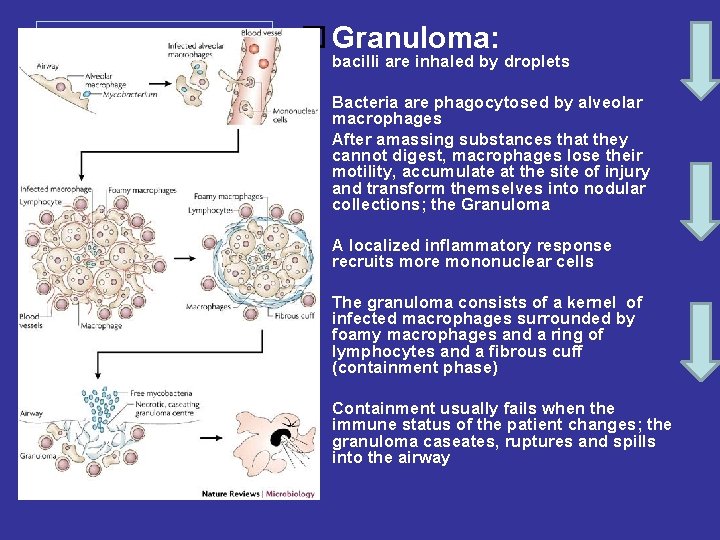
Granuloma: bacilli are inhaled by droplets Bacteria are phagocytosed by alveolar macrophages After amassing substances that they cannot digest, macrophages lose their motility, accumulate at the site of injury and transform themselves into nodular collections; the Granuloma A localized inflammatory response recruits more mononuclear cells The granuloma consists of a kernel of infected macrophages surrounded by foamy macrophages and a ring of lymphocytes and a fibrous cuff (containment phase) Containment usually fails when the immune status of the patient changes; the granuloma caseates, ruptures and spills into the airway
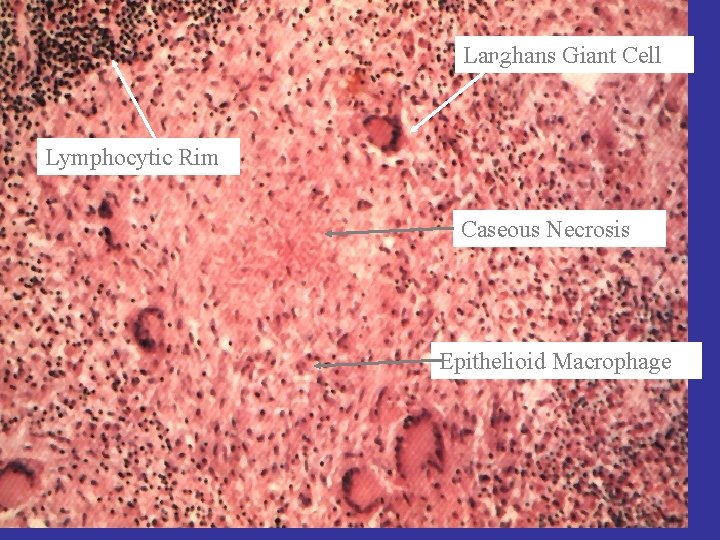
Langhans Giant Cell Granuloma Lymphocytic Rim Caseous Necrosis Epithelioid Macrophage
Tuberculosis
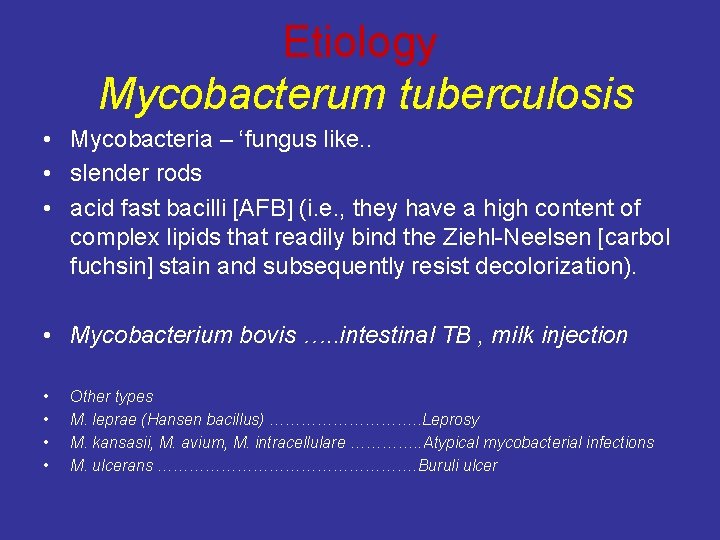
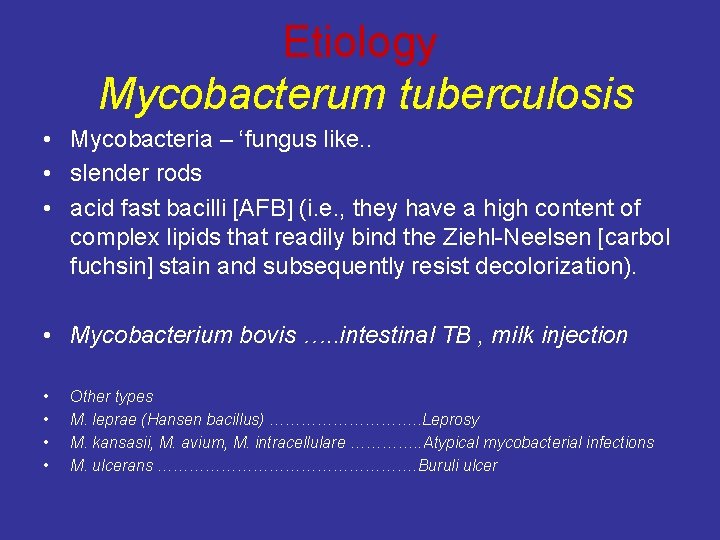
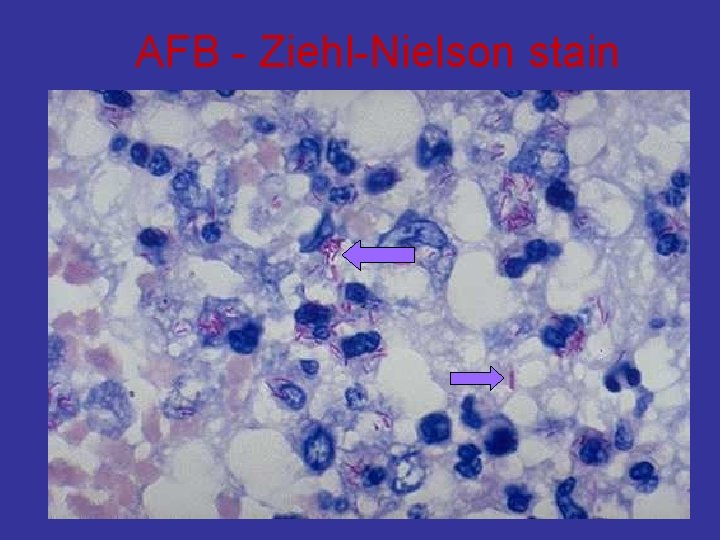
Etiology Mycobacterum tuberculosis • Mycobacteria – ‘fungus like. . • slender rods • acid fast bacilli [AFB] (i. e. , they have a high content of complex lipids that readily bind the Ziehl-Neelsen [carbol fuchsin] stain and subsequently resist decolorization). • Mycobacterium bovis …. . intestinal TB , milk injection • • Other types M. leprae (Hansen bacillus) ……………. . Leprosy M. kansasii, M. avium, M. intracellulare …………. . Atypical mycobacterial infections M. ulcerans ……………………. Buruli ulcer
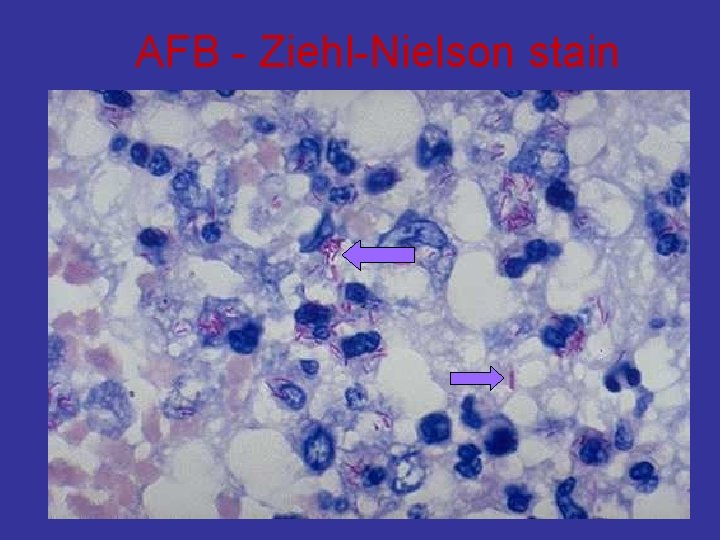
AFB - Ziehl-Nielson stain
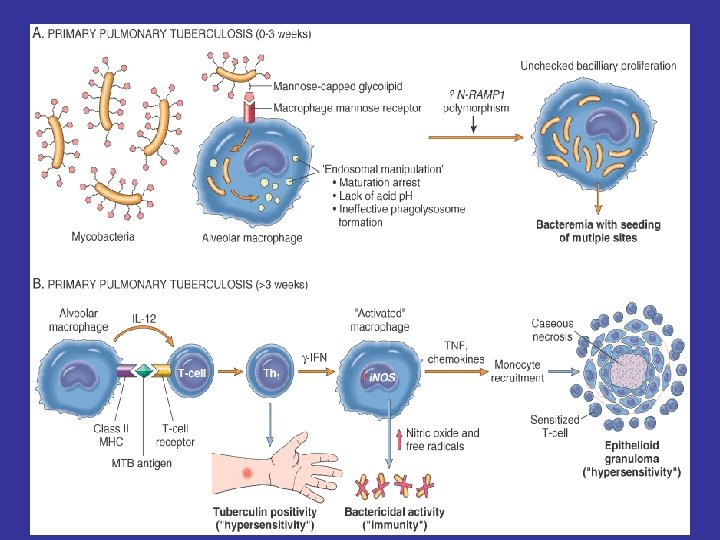
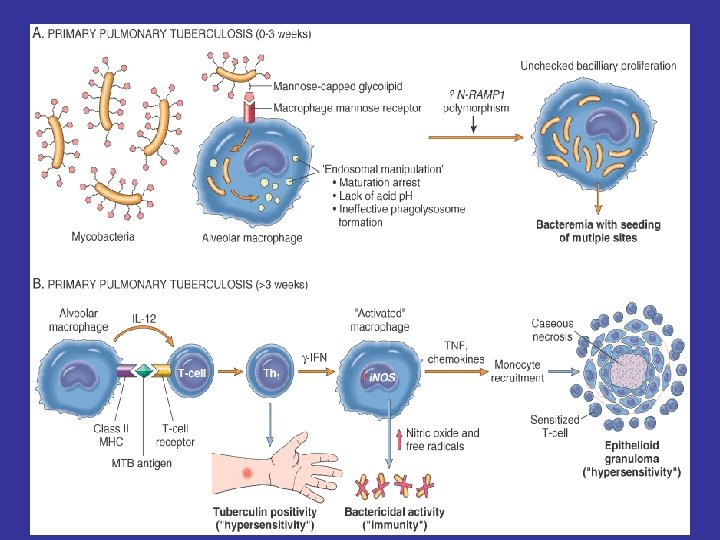
Pathogenesis of TB: Infection - Immunity
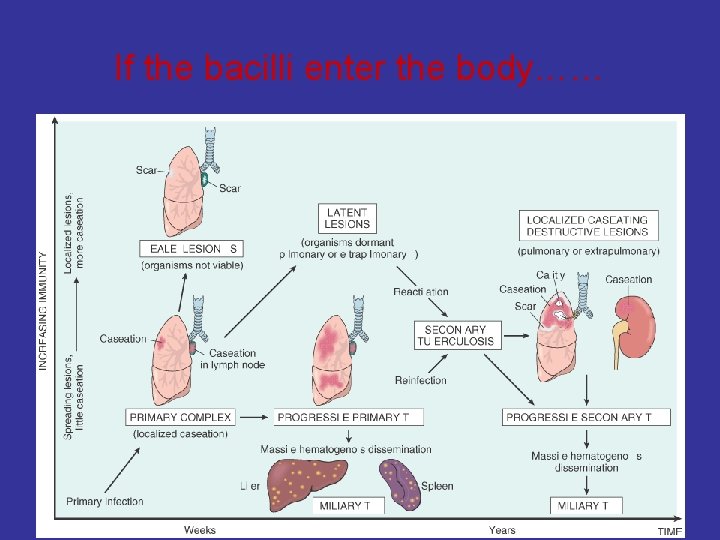
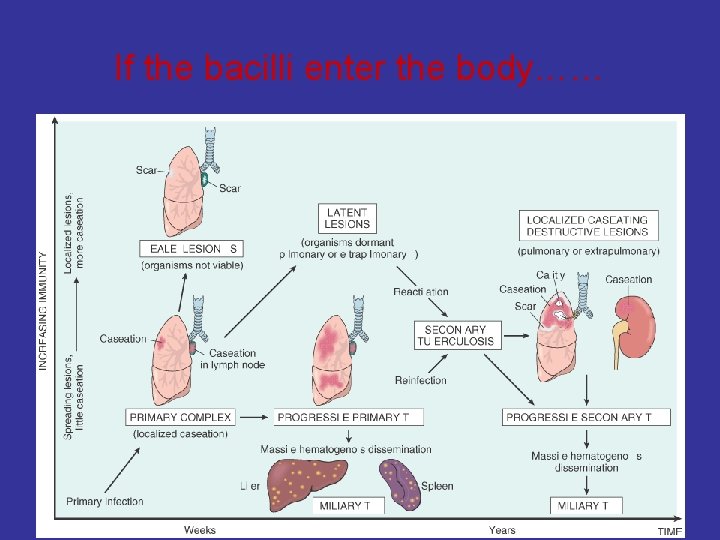
If the bacilli enter the body……
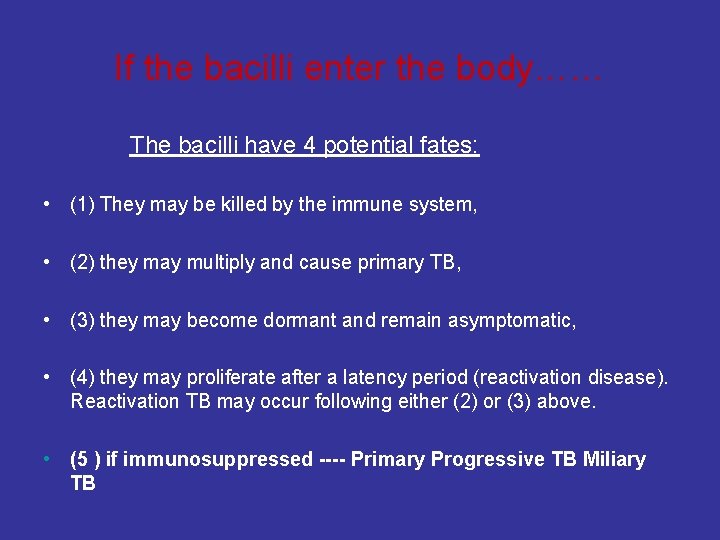
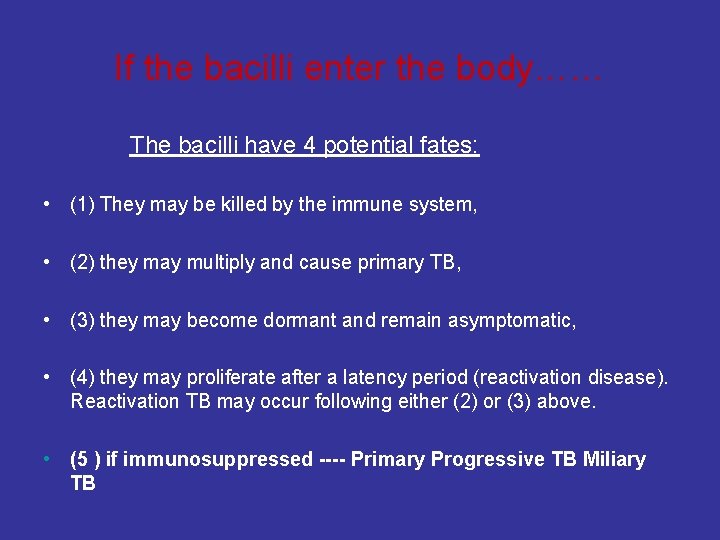
If the bacilli enter the body…… The bacilli have 4 potential fates: • (1) They may be killed by the immune system, • (2) they may multiply and cause primary TB, • (3) they may become dormant and remain asymptomatic, • (4) they may proliferate after a latency period (reactivation disease). Reactivation TB may occur following either (2) or (3) above. • (5 ) if immunosuppressed ---- Primary Progressive TB Miliary TB

![TB q Primary tuberculosis initial infection qsecondary tuberculosis reactivation or re infection TB q. Primary tuberculosis [initial infection] qsecondary tuberculosis [ re-activation or re -infection ]](https://slidetodoc.com/presentation_image/9050a328c089a8f9f9ef2b73af4ad449/image-26.jpg)
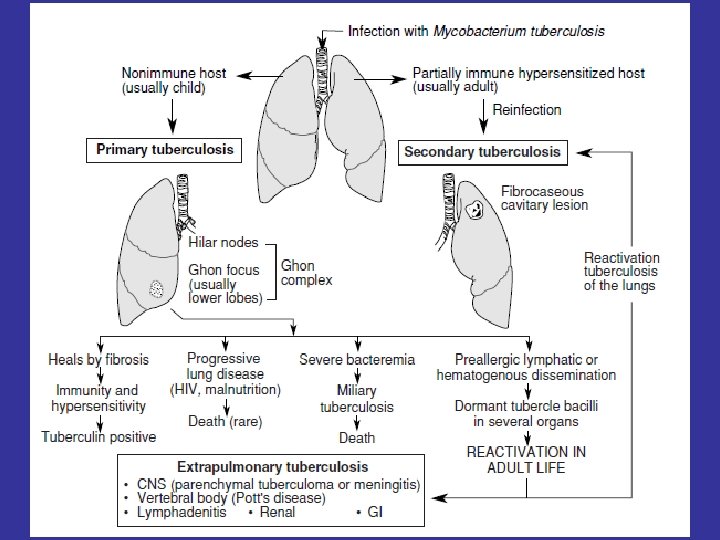
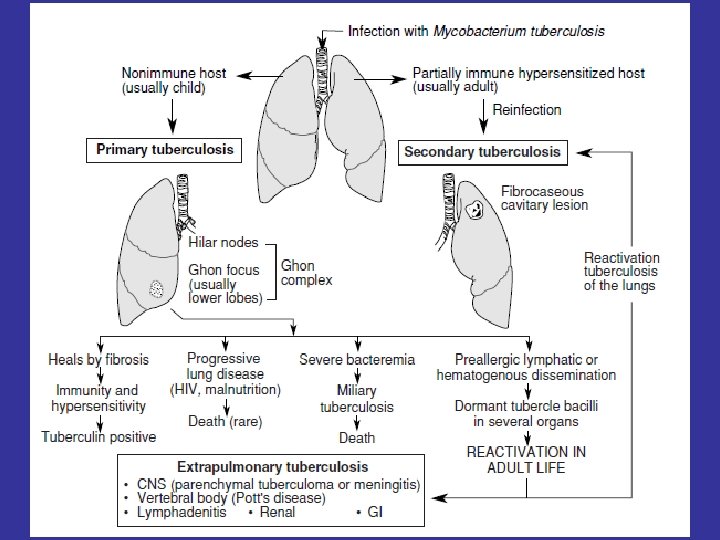
TB q. Primary tuberculosis [initial infection] qsecondary tuberculosis [ re-activation or re -infection ]
![Primary tuberculosis Non immunized individual initial infection children Subpleural zone of Primary tuberculosis • Non immunized individual [initial infection] – children • Subpleural zone of](https://slidetodoc.com/presentation_image/9050a328c089a8f9f9ef2b73af4ad449/image-27.jpg)
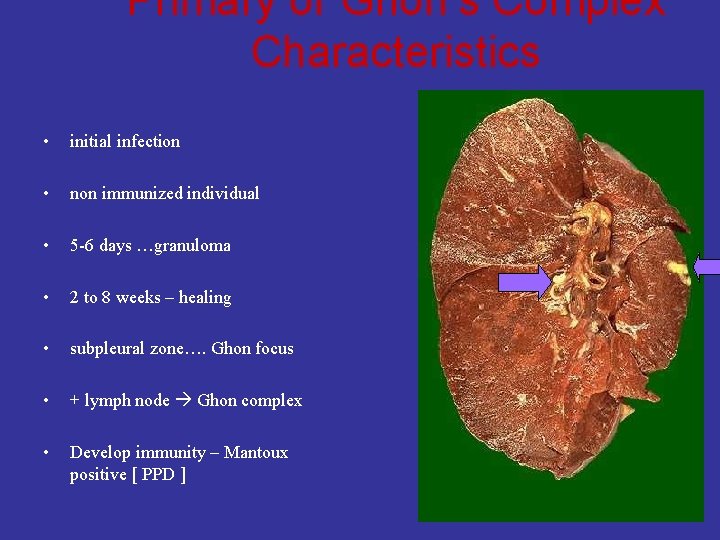
Primary tuberculosis • Non immunized individual [initial infection] – children • Subpleural zone of lung – can be at other sites • Brief acute inflammation – neutrophils. • 5 -6 days invoke granuloma formation. • 2 to 8 weeks – healing – Ghon focus (+ lymph node Ghon complex) • Develop immunity – Mantoux positive ( tuberculin test , PPD )
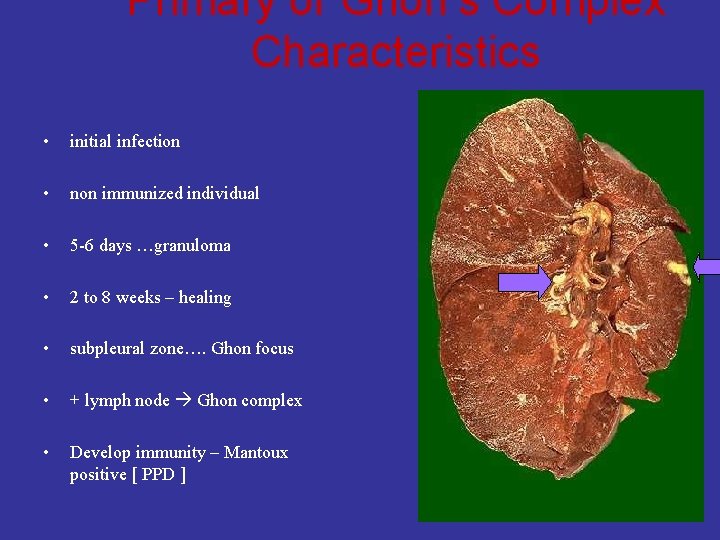
Primary or Ghon’s Complex Characteristics • initial infection • non immunized individual • 5 -6 days …granuloma • 2 to 8 weeks – healing • subpleural zone…. Ghon focus • + lymph node Ghon complex • Develop immunity – Mantoux positive [ PPD ]
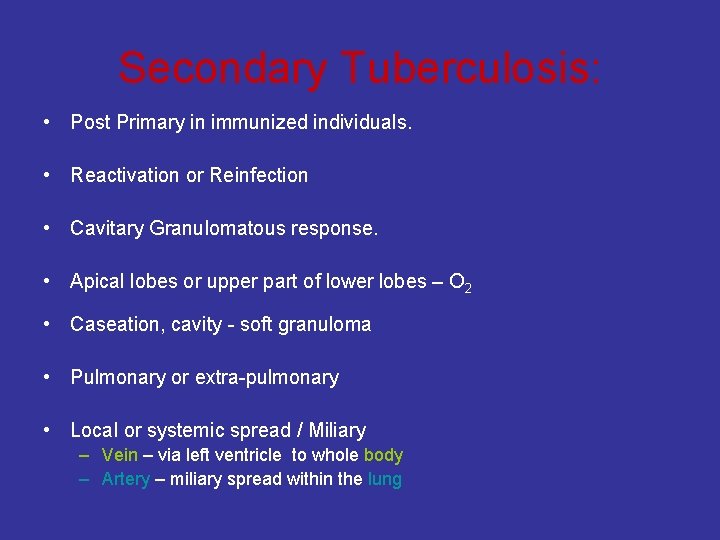
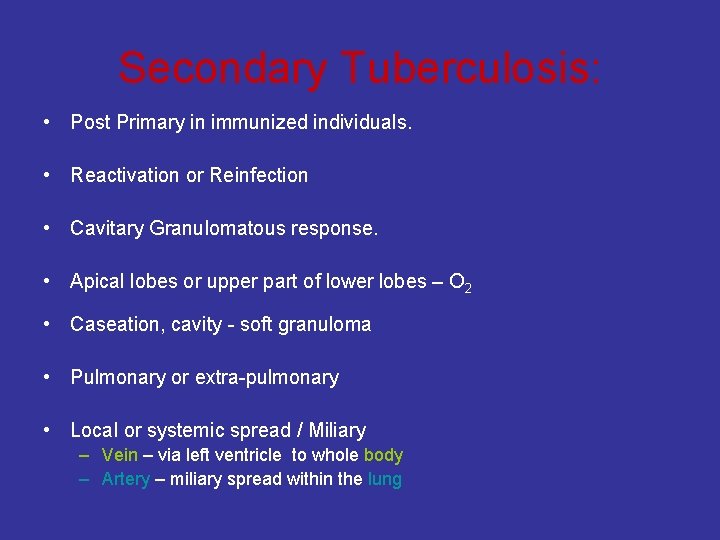
Secondary Tuberculosis: • Post Primary in immunized individuals. • Reactivation or Reinfection • Cavitary Granulomatous response. • Apical lobes or upper part of lower lobes – O 2 • Caseation, cavity - soft granuloma • Pulmonary or extra-pulmonary • Local or systemic spread / Miliary – Vein – via left ventricle to whole body – Artery – miliary spread within the lung
Secondary Tuberculosis: • Cough, sputum, Low grade fever, night sweats, fatigue and weight loss. • Hemoptysis or pleuritic pain = severe disease
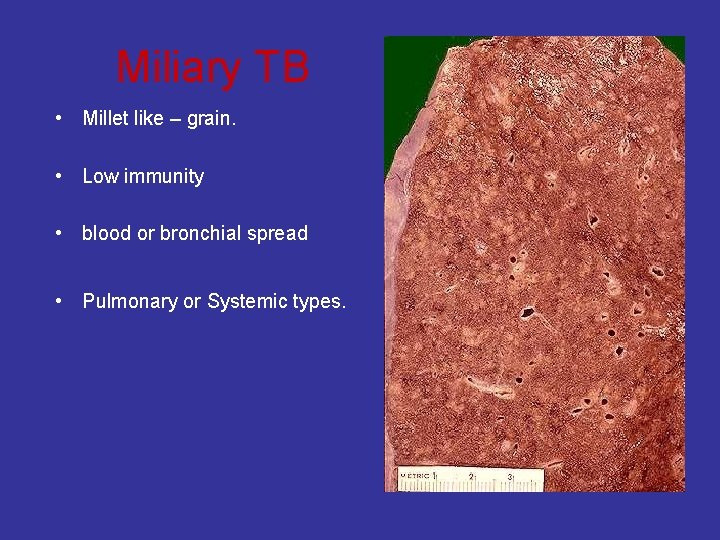
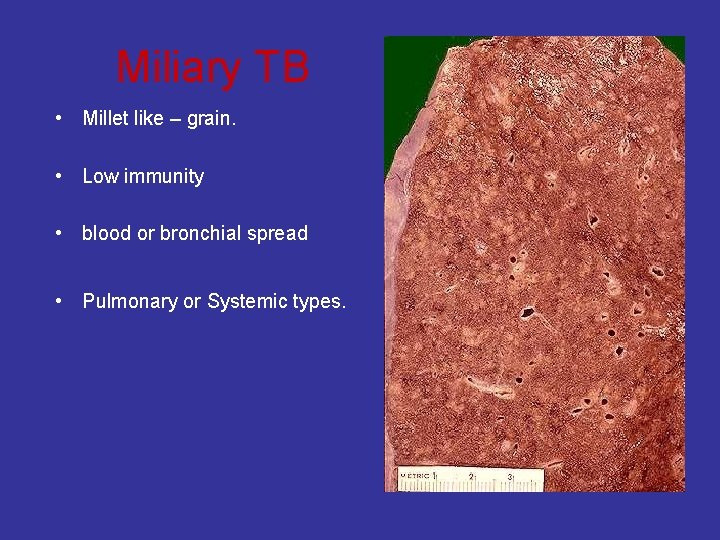
Miliary TB • Millet like – grain. • Low immunity • blood or bronchial spread • Pulmonary or Systemic types.
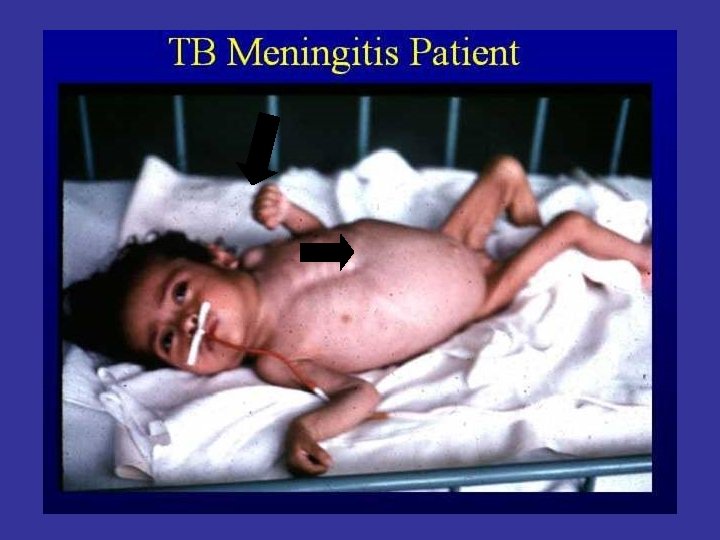
TB OF DIFFERENT ORGANS

Adrenal TB - Addison Disease
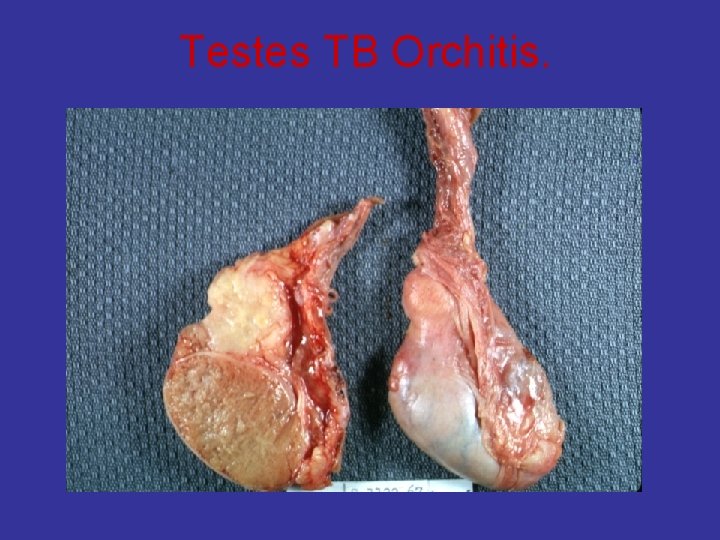
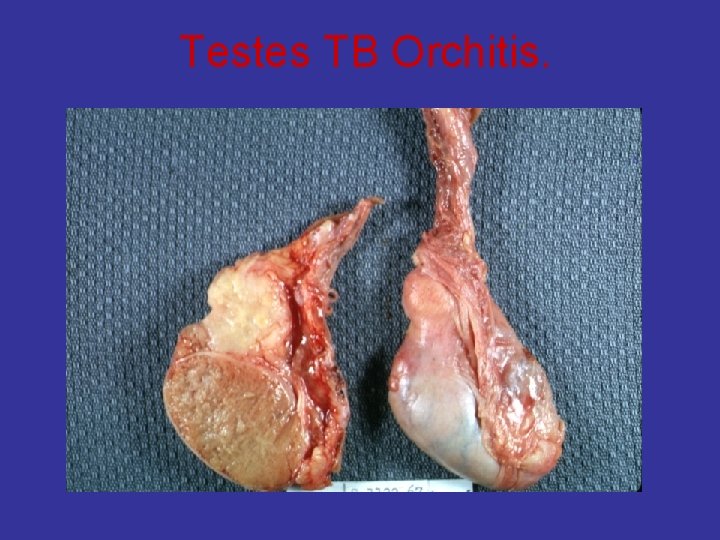
Testes TB Orchitis.

TB Peritonitis + liver Miliary TB

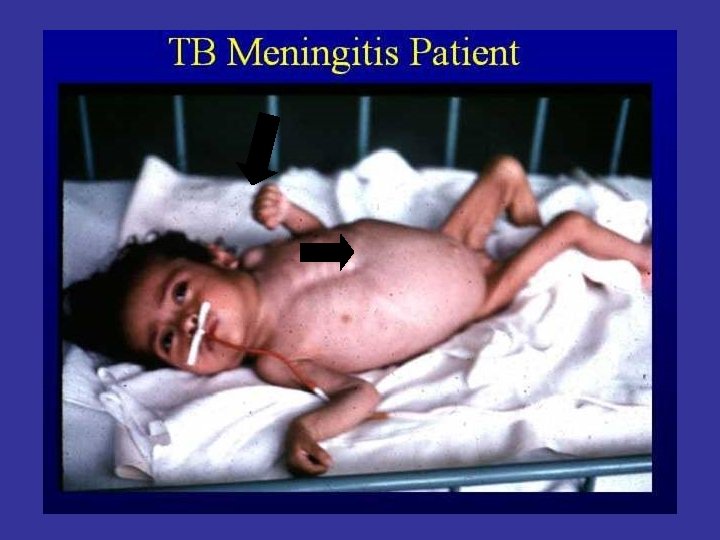
TB Brain – Caudate n.

TB Intestine any part can be affected ileum
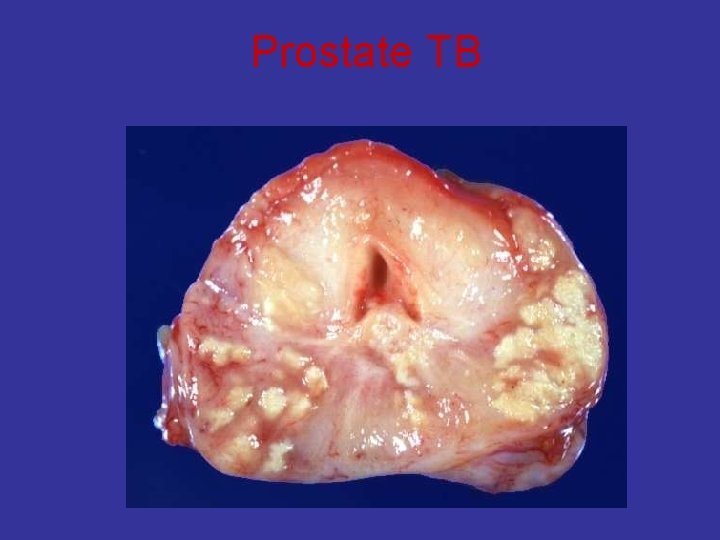
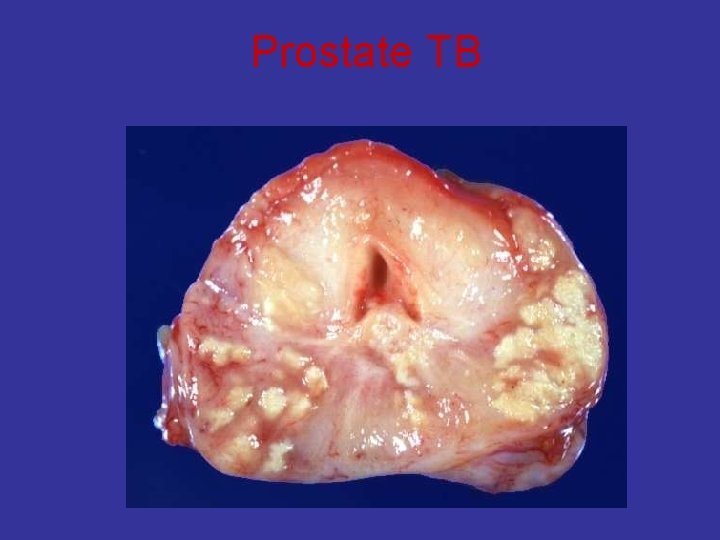
Prostate TB
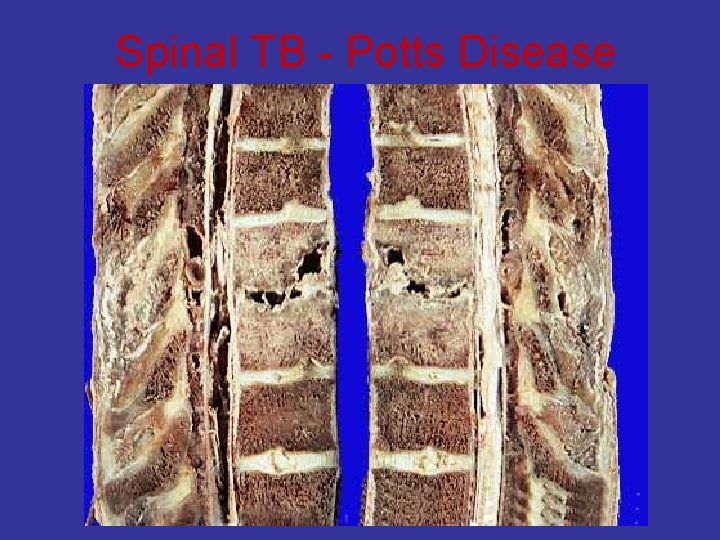
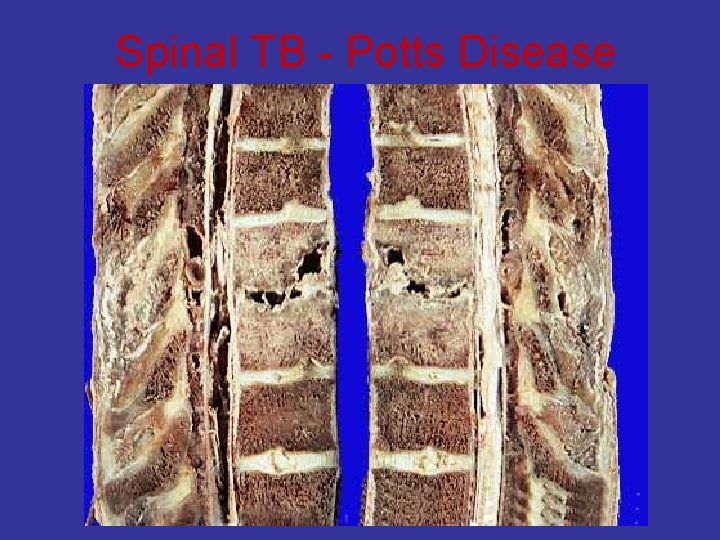
Spinal TB - Potts Disease
Diagnosis of TB • Clinical features • Depend on organ involved. • Pulmonary tuberculosis (TB): Ø productive cough, fever, and weight loss, night sweats.
Investigations • Patients suspected of having tuberculosis (TB) q Ø Ø Tuberculin skin testing (Mantoux test, PPD) Intradermal injection of purified protein derivative ( PPD). The response is measured as the amount of induration at 48 -72 hours. The size of induration, rather than erythema, is diagnostic. BCG gives + result q Ø Ø Ø Sputum, bronchial wash or biopsy Acid fast smear ( ZN stain ) cultures require weeks for growth and identification Newer technologies, including ribosomal RNA probes or DNA polymerase chain reaction, allow identification within 24 hours. q Chest radiographs Ø patchy or nodular infiltrate. Ø may be found in any part of the lung, but upper-lobe involvement is most common

PPD result after – 72 hours

What will be your action after diagnosis? • Patients with TB should remain in isolation until sputum becomes negative;
• 1° TB usually involves the middle or lower lung zones and is associated with hilar adenopathy (Gohn complex). • 2 ° TB represents reactivation and typically involves the upper lungs and cavitation. • regimen RIPE—Rifampin, Isoniazid (INH), Pyrazinamide, and Ethambutol daily for eight weeks, followed by INH and rifampin for an additional 16 weeks. Give vitamin B 6 to prevent INHassociated neuropathy.
Leprosy
Leprosy • Leprosy is a chronic infection caused by the acid-fast, rod-shaped bacillus Mycobacterium leprae. qskin qperipheral nerves
Leprosy Symptoms qskin – Painless skin patch qperipheral nerves – Loss of sensation – Wasting and muscle weakness – Foot drop or clawed hands – Ulcerations on hands or feet
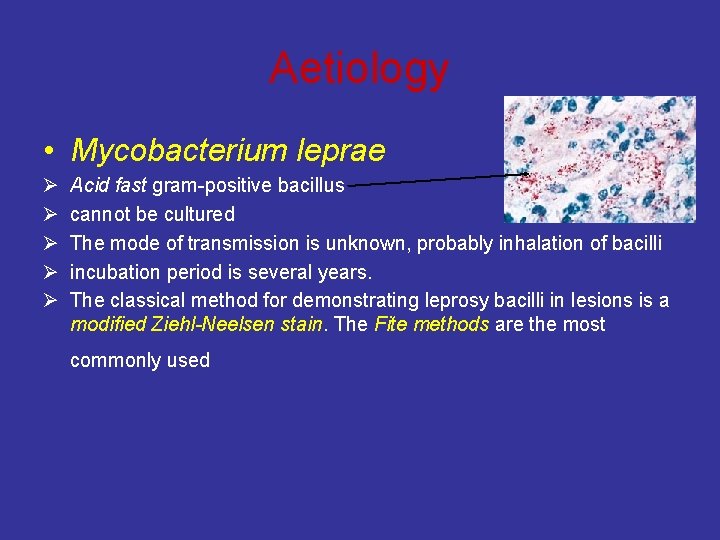
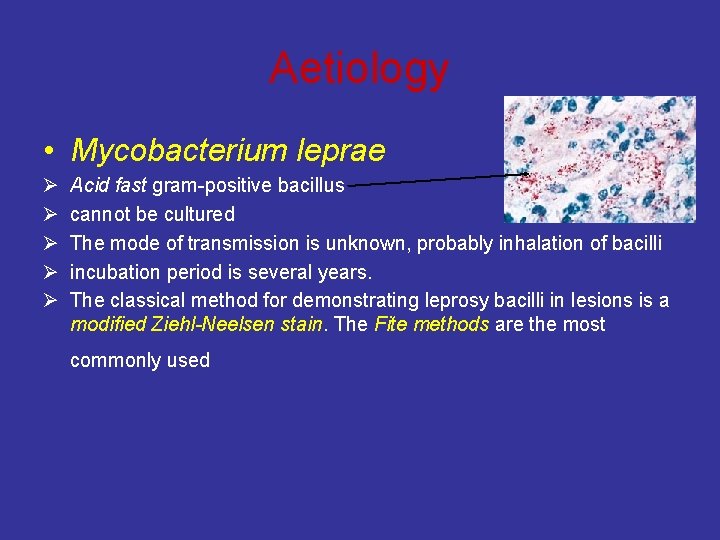
Aetiology • Mycobacterium leprae Ø Ø Ø Acid fast gram-positive bacillus cannot be cultured The mode of transmission is unknown, probably inhalation of bacilli incubation period is several years. The classical method for demonstrating leprosy bacilli in lesions is a modified Ziehl-Neelsen stain. The Fite methods are the most commonly used
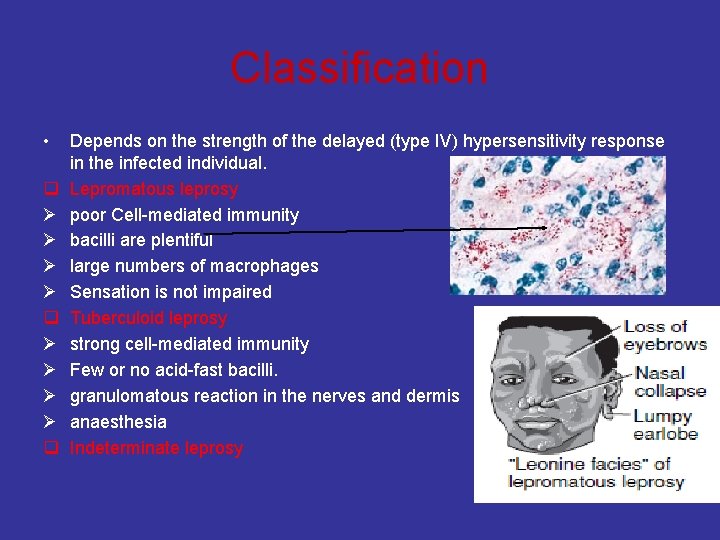
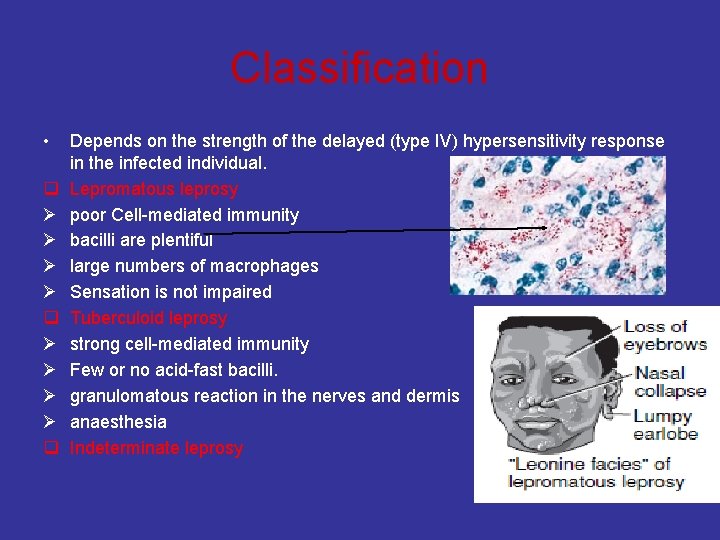
Classification • q Ø Ø Ø Ø q Depends on the strength of the delayed (type IV) hypersensitivity response in the infected individual. Lepromatous leprosy poor Cell-mediated immunity bacilli are plentiful large numbers of macrophages Sensation is not impaired Tuberculoid leprosy strong cell-mediated immunity Few or no acid-fast bacilli. granulomatous reaction in the nerves and dermis anaesthesia Indeterminate leprosy
The lepromin skin test • Intradermal injection of a preparation of M. leprae • A positive reaction consists of the formation of a nodule measuring 5 mm or more in diameter after 2 to 4 weeks. On histologic examination, the nodule shows an epithelioid cell granuloma. • Tuberculoid …. . • lepromatous …. .
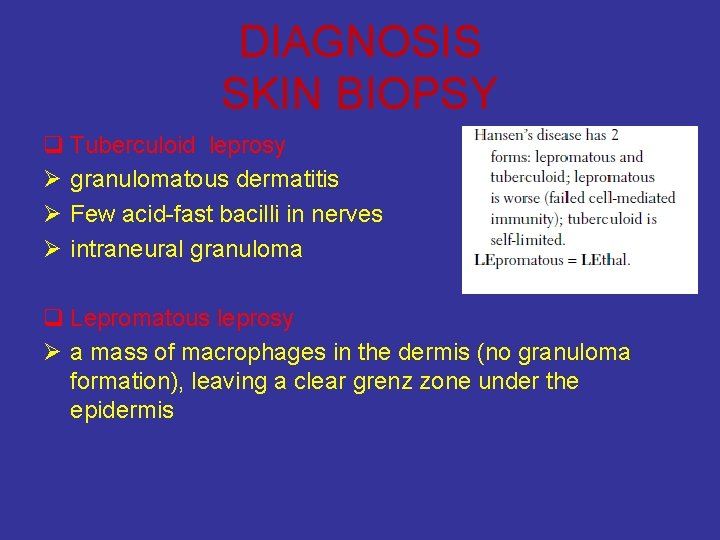
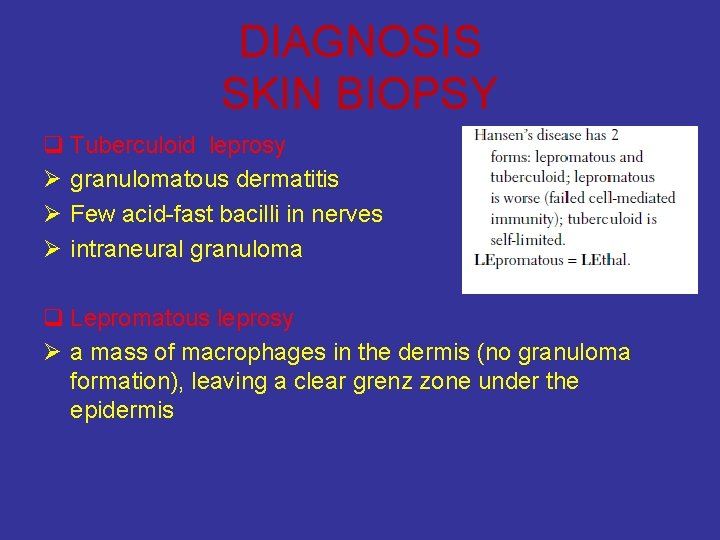
DIAGNOSIS SKIN BIOPSY q Tuberculoid leprosy Ø granulomatous dermatitis Ø Few acid-fast bacilli in nerves Ø intraneural granuloma q Lepromatous leprosy Ø a mass of macrophages in the dermis (no granuloma formation), leaving a clear grenz zone under the epidermis
Schistosomiasis
Schistosomiasis • Also known as bilharziasis • Parasite • • • The main forms of human schistosomiasis : Schistosoma hematobium, Schistosoma mansoni, Schistosoma japonicum, Schistosoma intercalatum, Schistosoma mekongi.
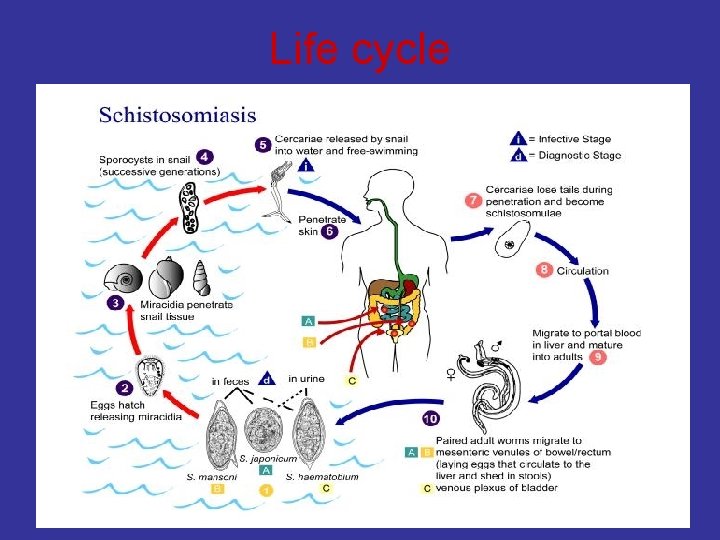
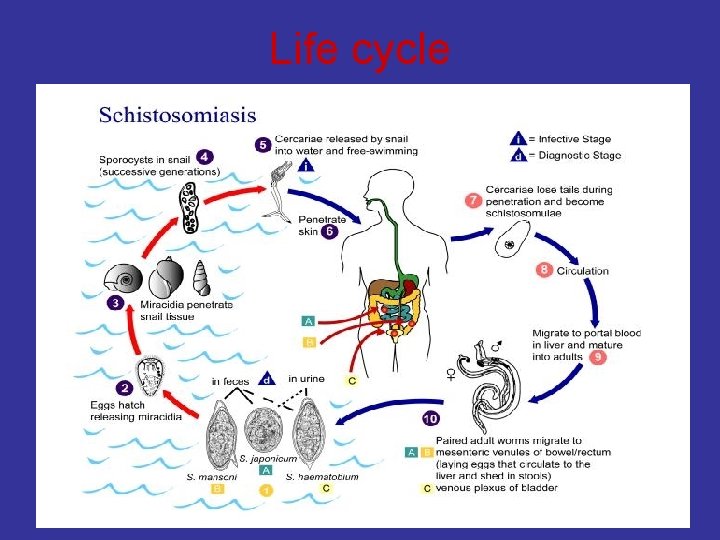
Life cycle
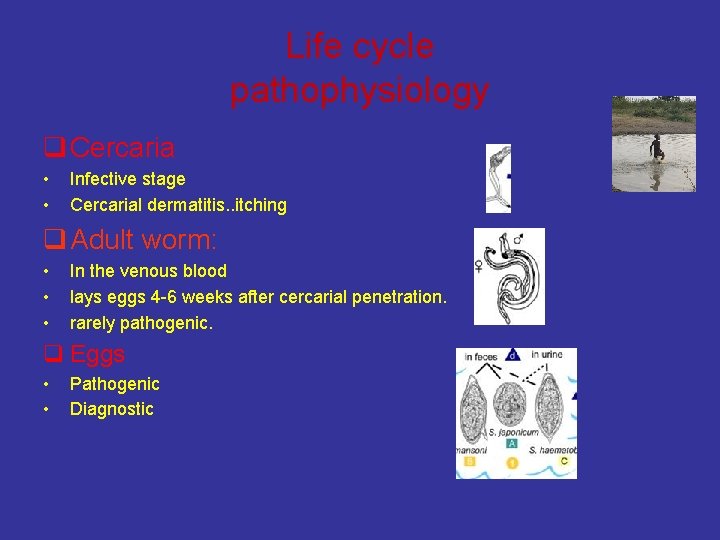
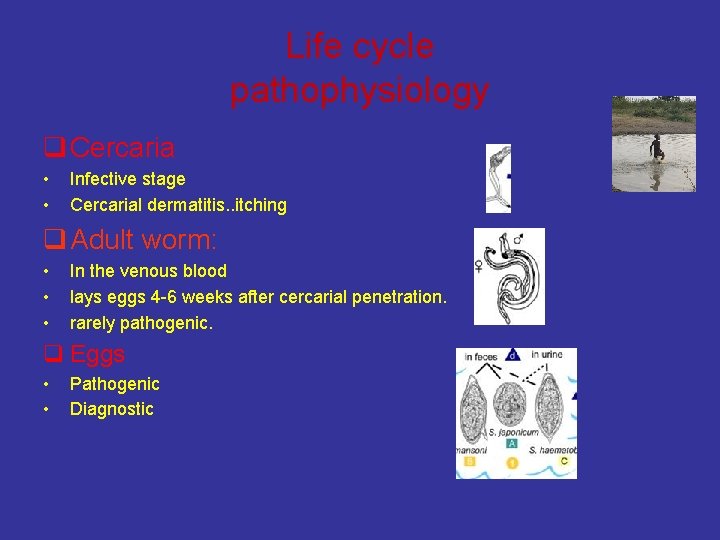
Life cycle pathophysiology q Cercaria • • Infective stage Cercarial dermatitis. . itching q Adult worm: • • • In the venous blood lays eggs 4 -6 weeks after cercarial penetration. rarely pathogenic. q Eggs • • Pathogenic Diagnostic
Acute schistosomiasis • most clinical manifestations are benign • Cercarial dermatitis: Individuals who have been exposed to fresh or salt water may develop a pruritic rash due to cercarial dermatitis (also called swimmer's itch). • some are severe and may require hospitalization.
Chronic schistosomiasis • Most patients are asymptomatic or mildly symptomatic and do not require medical attention. • Only a small proportion of the endemic population harbors a heavy worm burden that later leads to clinical complications.
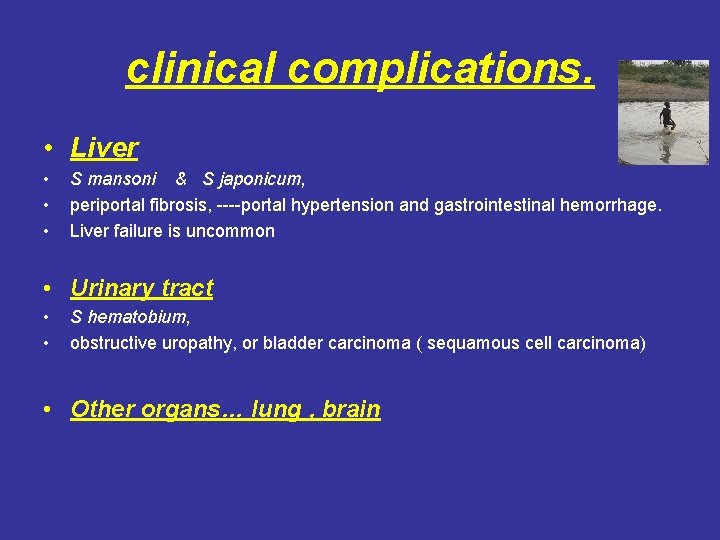
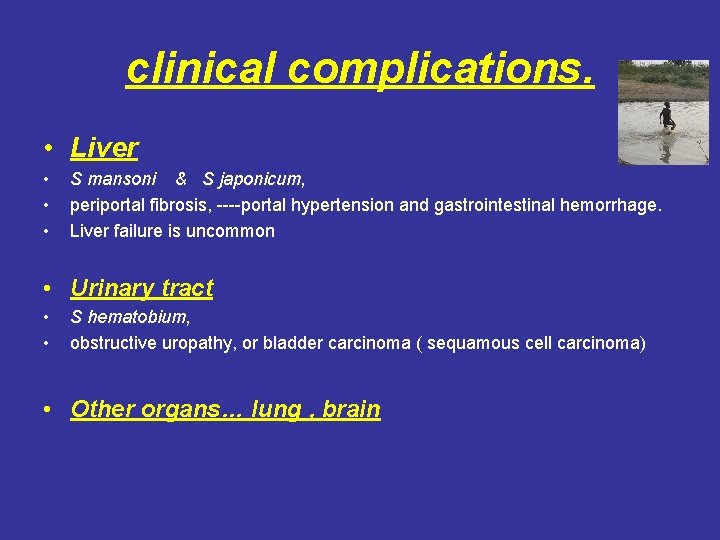
clinical complications. • Liver • • • S mansoni & S japonicum, periportal fibrosis, ----portal hypertension and gastrointestinal hemorrhage. Liver failure is uncommon • Urinary tract • • S hematobium, obstructive uropathy, or bladder carcinoma ( sequamous cell carcinoma) • Other organs… lung , brain
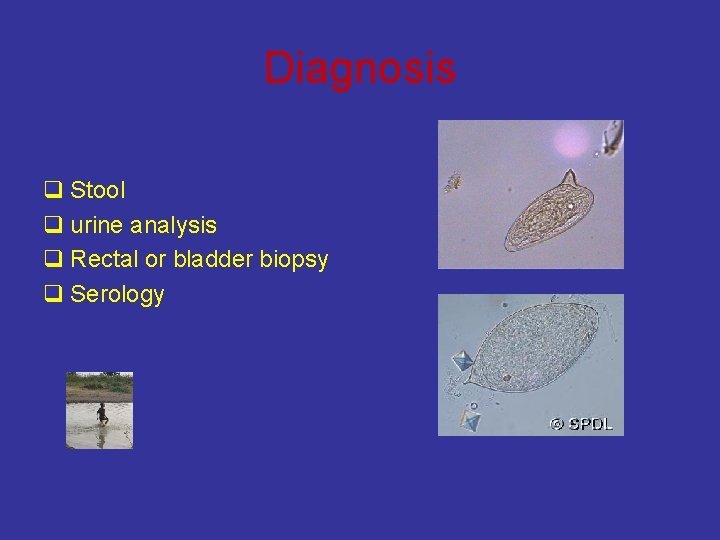
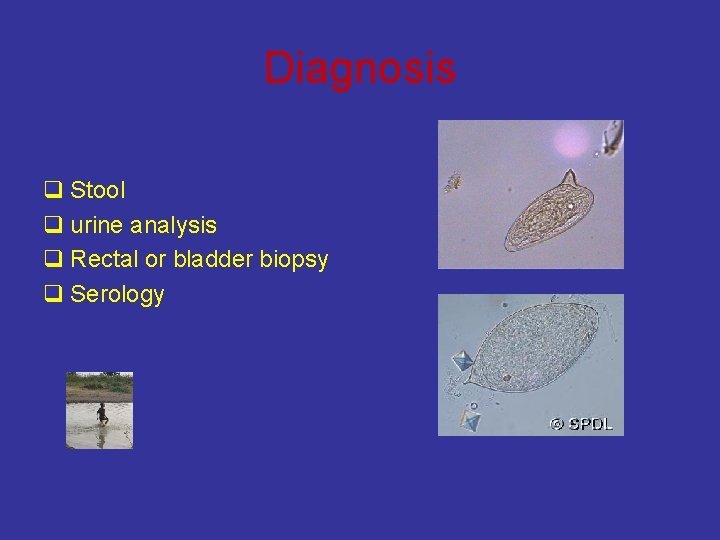
Diagnosis q Stool q urine analysis q Rectal or bladder biopsy q Serology
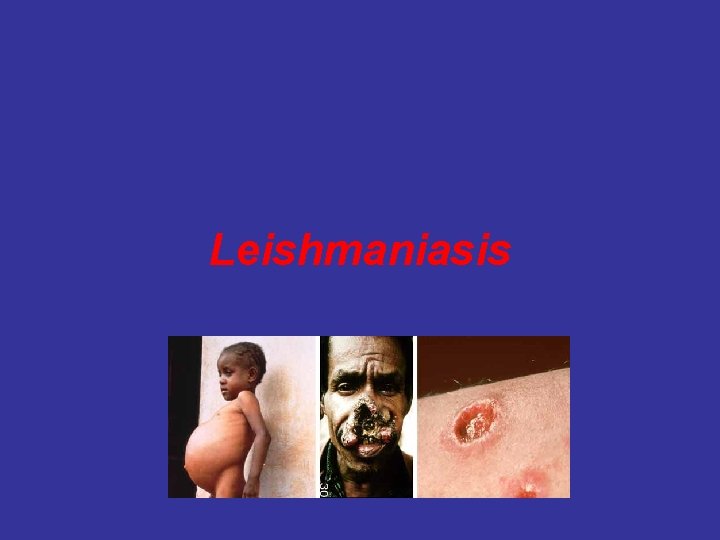
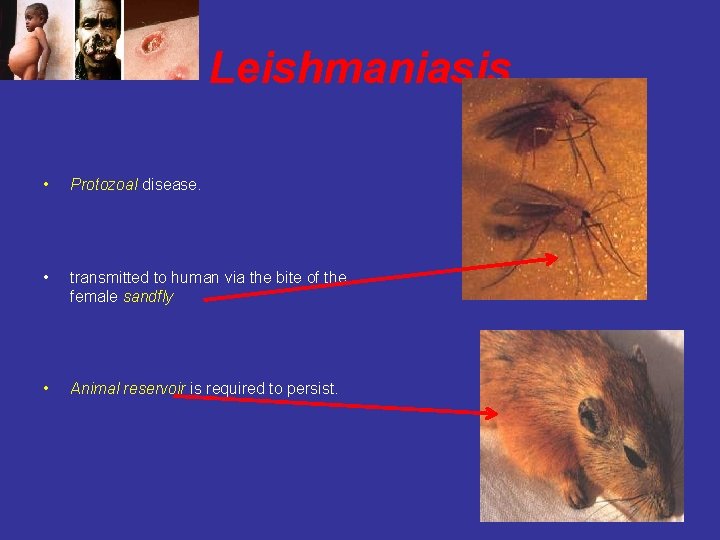
Leishmaniasis
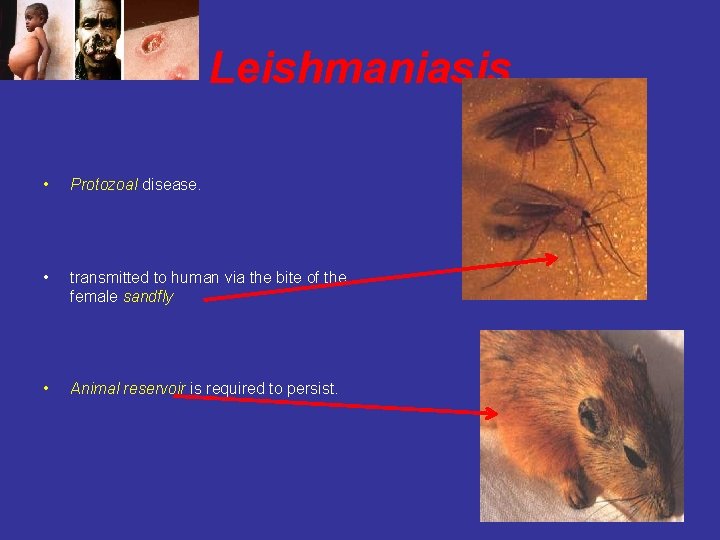
Leishmaniasis • Protozoal disease. • transmitted to human via the bite of the female sandfly • Animal reservoir is required to persist.
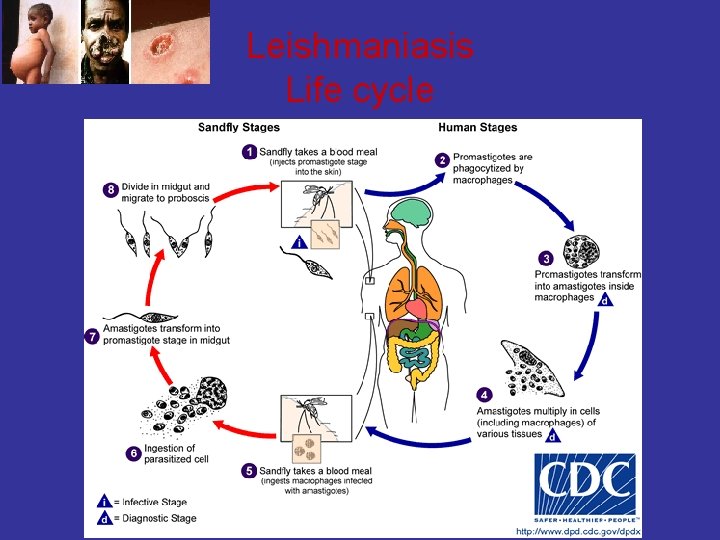
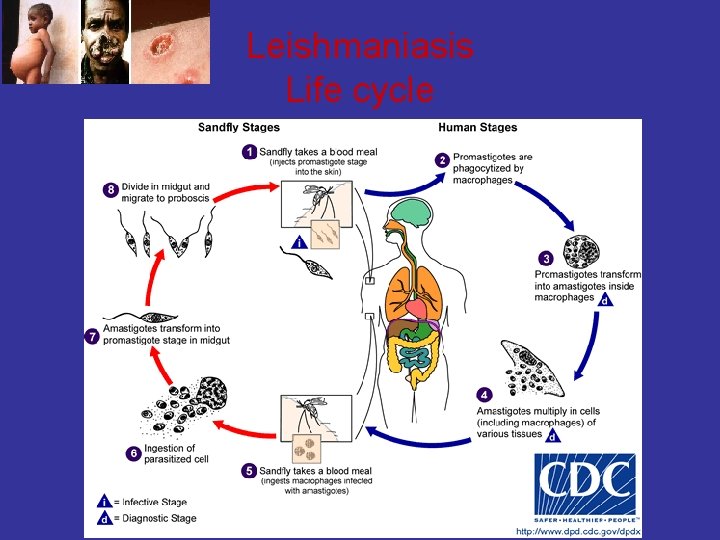
Leishmaniasis Life cycle

Leishmaniasis • Cutaneous • • L. tropica …. middle east L. major exposed parts of the body, such as face, scalp, and arms Ulceration is common • Mucocutaneous • • • L. b. braziliensis lips , oral cavity, pharynx, nose Disfiguring tissue distruction • • Visceral (kala-azar] L. donovani • • • L. tropica fever, lymphadenopathy, hepatosplenomegaly, ascites, pancytopenia, may die if untreated Indian name kala-azar [black fever] ……. . diffuse darkening of the skin,
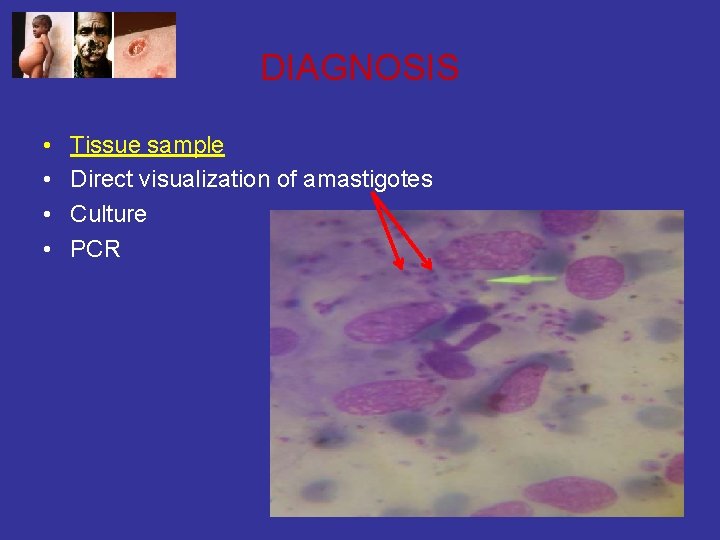
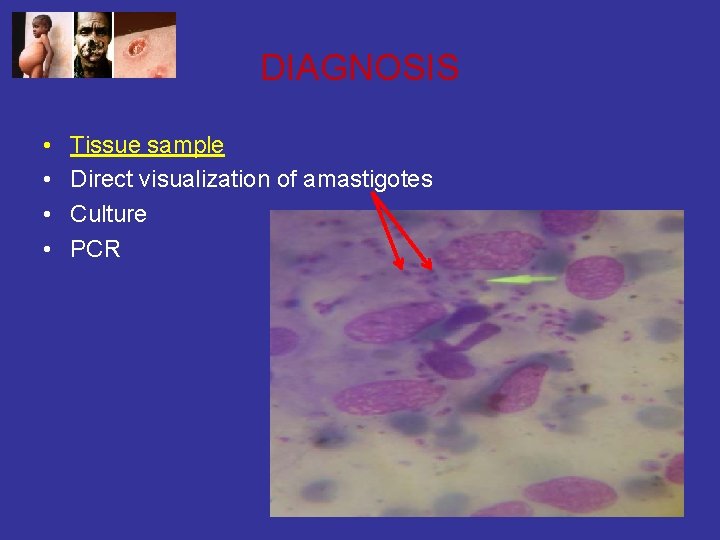
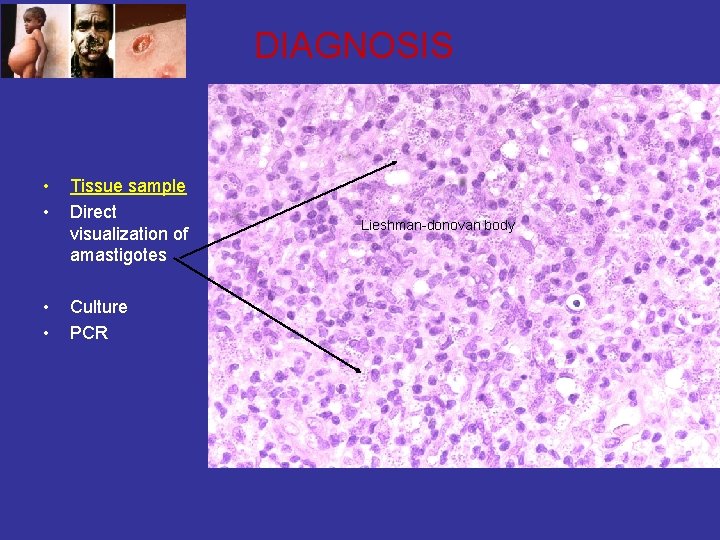
DIAGNOSIS • • Tissue sample Direct visualization of amastigotes Culture PCR
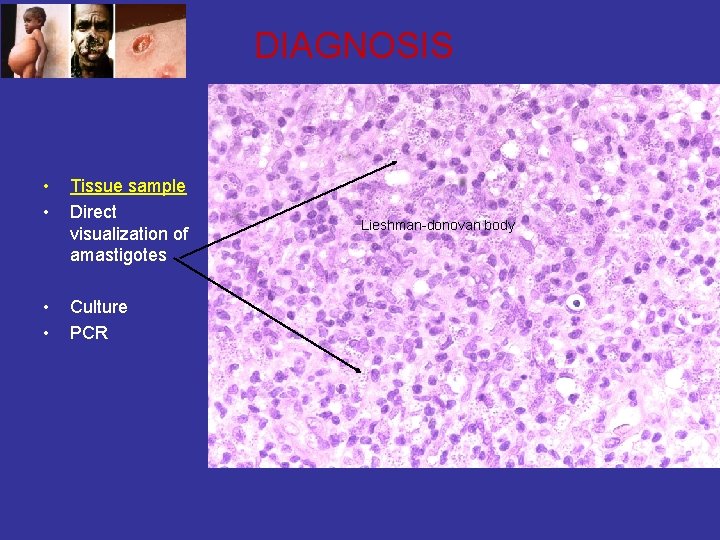
DIAGNOSIS • • Tissue sample Direct visualization of amastigotes • • Culture PCR Lieshman-donovan body
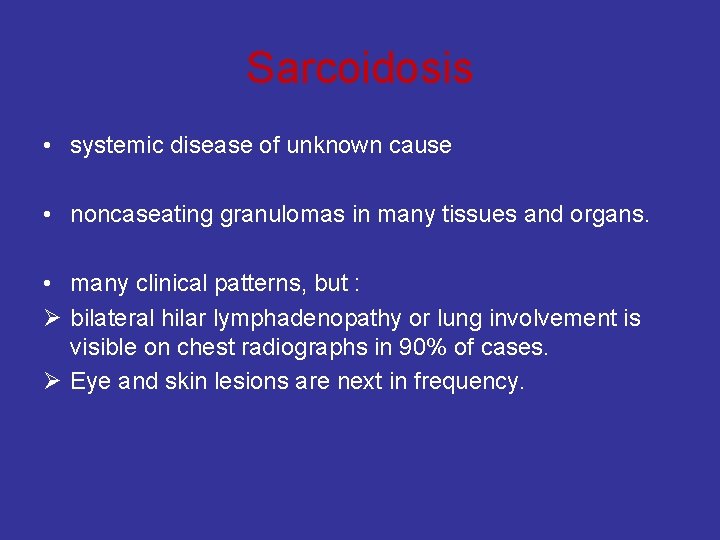
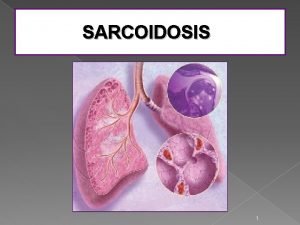
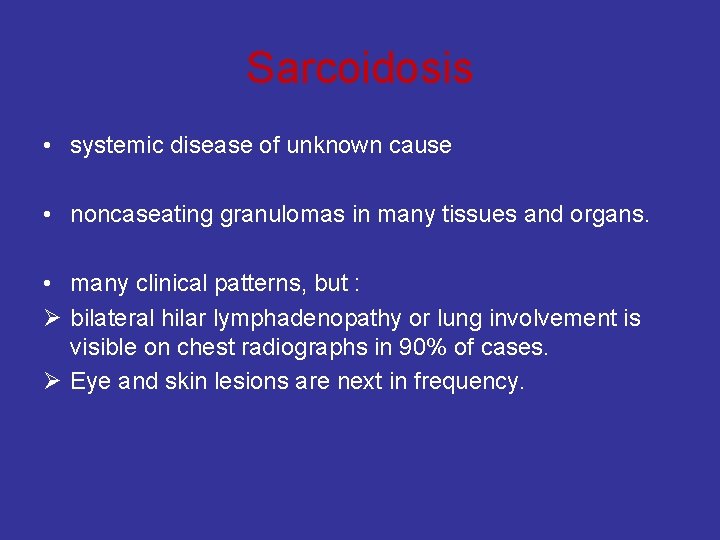
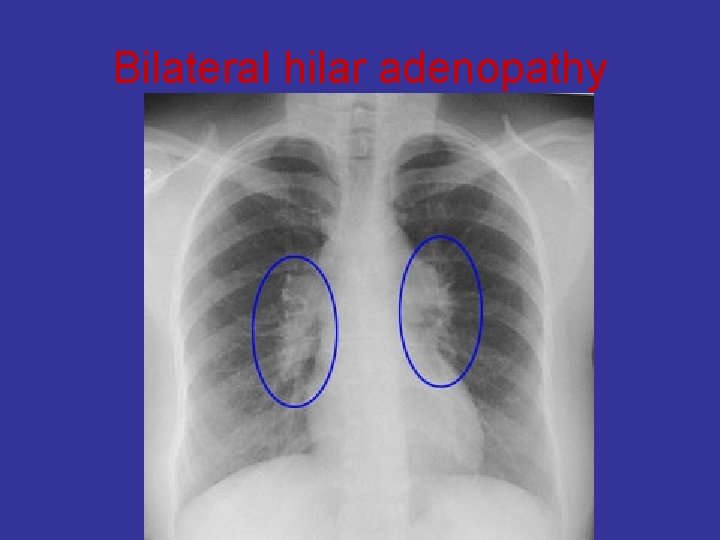
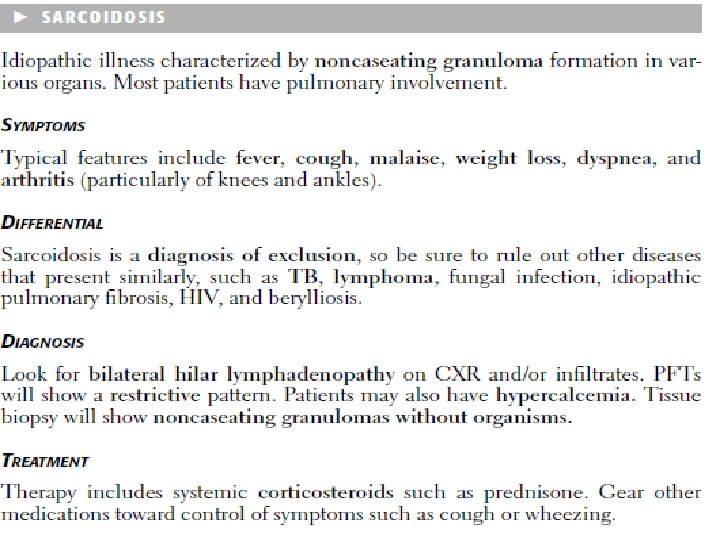
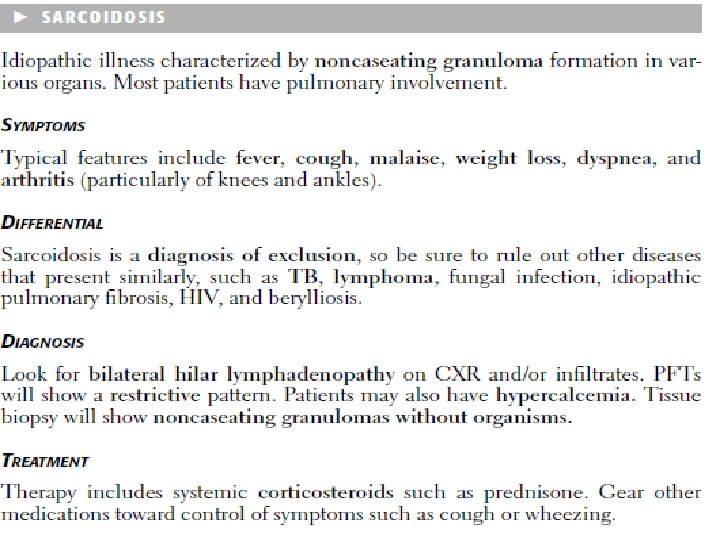
Sarcoidosis • systemic disease of unknown cause • noncaseating granulomas in many tissues and organs. • many clinical patterns, but : Ø bilateral hilar lymphadenopathy or lung involvement is visible on chest radiographs in 90% of cases. Ø Eye and skin lesions are next in frequency.
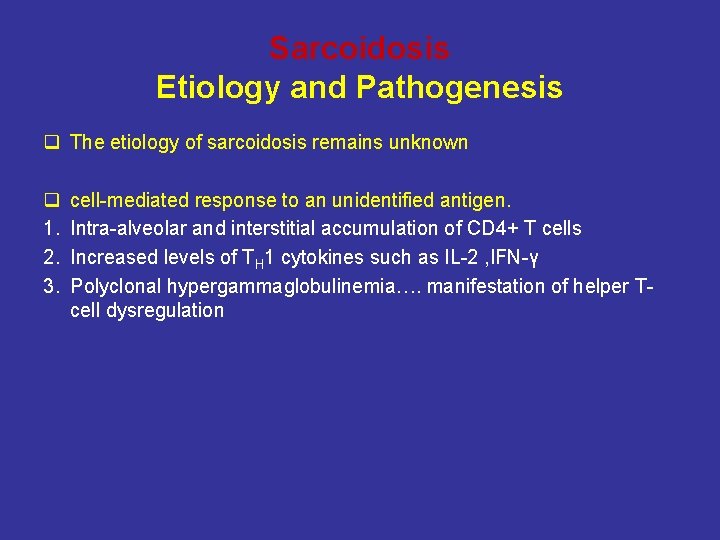
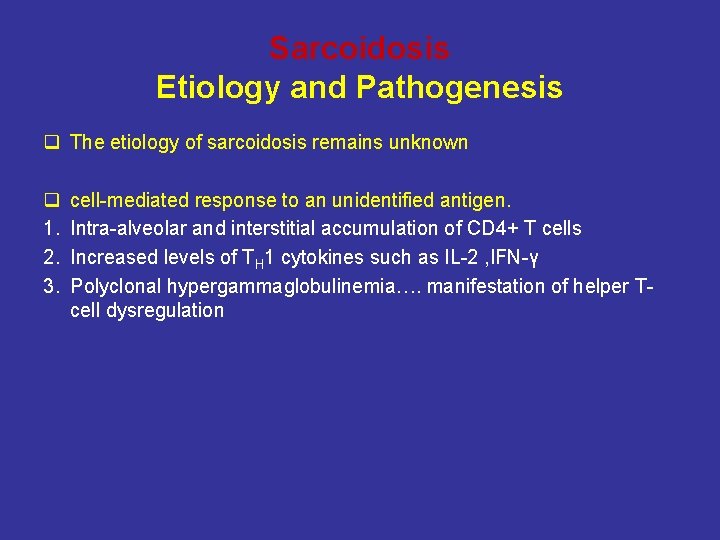
Sarcoidosis Etiology and Pathogenesis q The etiology of sarcoidosis remains unknown q 1. 2. 3. cell-mediated response to an unidentified antigen. Intra-alveolar and interstitial accumulation of CD 4+ T cells Increased levels of TH 1 cytokines such as IL-2 , IFN-γ Polyclonal hypergammaglobulinemia…. manifestation of helper Tcell dysregulation
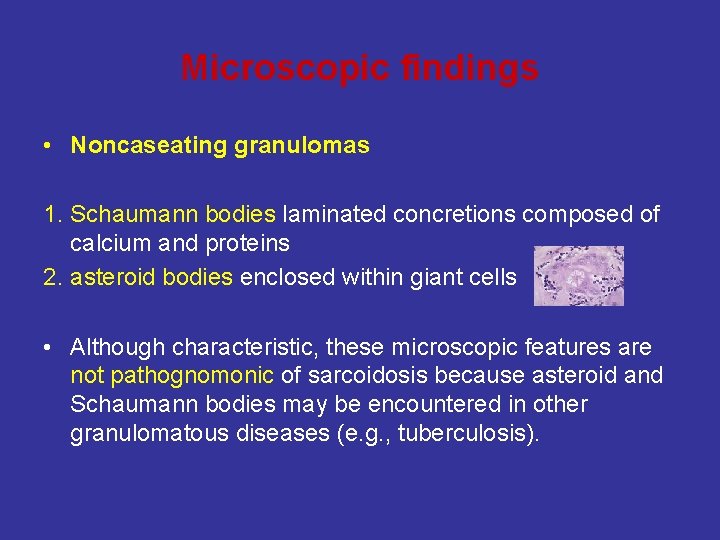
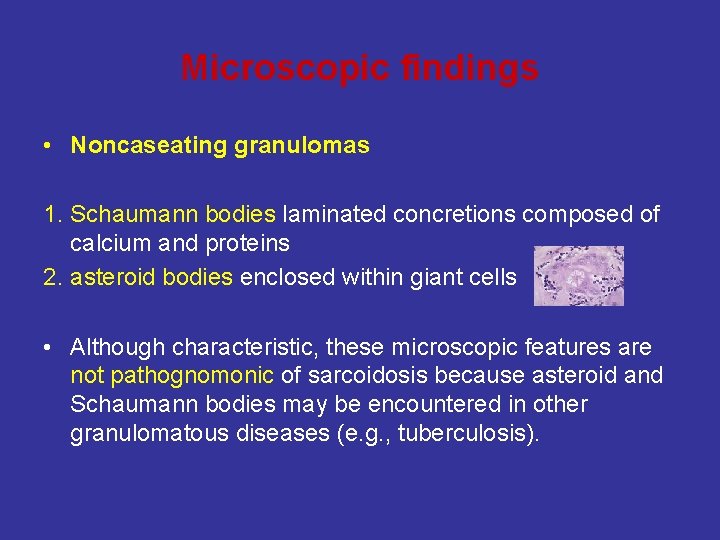
Microscopic findings • Noncaseating granulomas 1. Schaumann bodies laminated concretions composed of calcium and proteins 2. asteroid bodies enclosed within giant cells • Although characteristic, these microscopic features are not pathognomonic of sarcoidosis because asteroid and Schaumann bodies may be encountered in other granulomatous diseases (e. g. , tuberculosis).
Any Organs involved • Lungs common sites of involvement • Lymph nodes are involved in almost all cases, specifically the hilar and mediastinal nodes • Spleen • bone marrow • Skin lesions • eye, • salivary glands
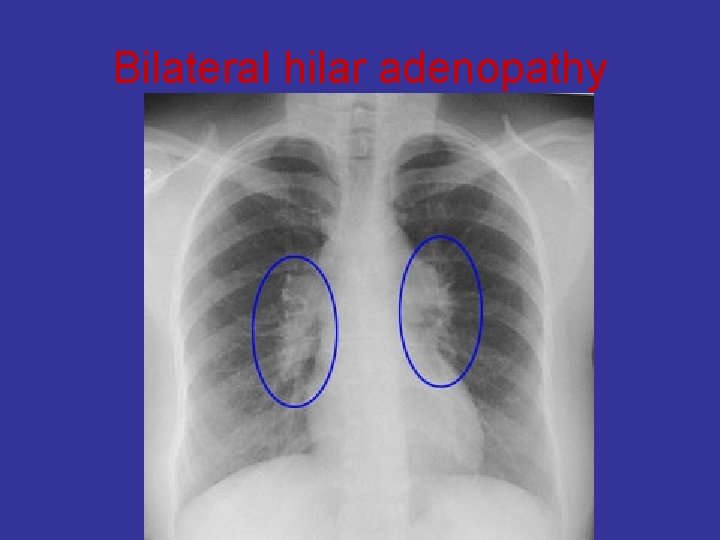
Bilateral hilar adenopathy
Clinical Course • In the great majority of cases, patients seek medical attention because of the : 1. respiratory abnormalities (shortness of breath, cough, chest pain, hemoptysis) or 2. constitutional signs and symptoms (fever, fatigue, weight loss, anorexia, night sweats).
Prognosis Ø 65% to 70% recover with minimal or no residual manifestations. Ø 20 % permanent loss of some lung function or some permanent visual impairment. Ø 10% to 15%, some die of cardiac or central nervous system damage,
 Planatis
Planatis Seclusio vs occlusio pupillae
Seclusio vs occlusio pupillae Causes of granulomatous inflammation
Causes of granulomatous inflammation Respiratory failure types
Respiratory failure types Granulomatous disease
Granulomatous disease Eyeritis disease
Eyeritis disease Granulomatous lesion
Granulomatous lesion Chronic granulomatous disease
Chronic granulomatous disease Granuloma anulare diabete
Granuloma anulare diabete Tbc
Tbc Testicular atrophy
Testicular atrophy Periapical granuloma
Periapical granuloma Pulpitis classification
Pulpitis classification Cactus granuloma
Cactus granuloma Pigmento antracotico
Pigmento antracotico Granuloma periférico de células gigantes
Granuloma periférico de células gigantes Lumnitzer fogó
Lumnitzer fogó Periapical granuloma
Periapical granuloma Dr kiran bidari
Dr kiran bidari Caseating granuloma causes
Caseating granuloma causes Nevo melanocitico adquirido
Nevo melanocitico adquirido Primary biliary cholangitis skin
Primary biliary cholangitis skin Central giant-cell granuloma
Central giant-cell granuloma Tuberculous granuloma
Tuberculous granuloma Noncaseating granuloma vs caseating
Noncaseating granuloma vs caseating Granuloma
Granuloma Periradicular disease definition
Periradicular disease definition Trichomoniasis incubation
Trichomoniasis incubation Sinonim diagnosis
Sinonim diagnosis Schistosomiasis granuloma
Schistosomiasis granuloma Non corticated
Non corticated Sifilide
Sifilide Granuloma piogenik
Granuloma piogenik Granuloma formation
Granuloma formation Vascular response in acute inflammation
Vascular response in acute inflammation Necrosis
Necrosis Acute inflammation
Acute inflammation Morphological types of inflammation
Morphological types of inflammation Inflammation
Inflammation Systemic effect of inflammation
Systemic effect of inflammation Inflammatio latin
Inflammatio latin Chemical mediators of inflammation
Chemical mediators of inflammation Acute inflammation definition
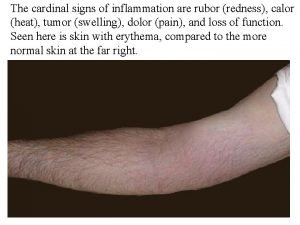
Acute inflammation definition 5 cardinal signs of inflammation
5 cardinal signs of inflammation Cardinal sign of inflammation
Cardinal sign of inflammation Articular circumference of ulna
Articular circumference of ulna Bradykinin nitric oxide
Bradykinin nitric oxide Cellular events of acute inflammation
Cellular events of acute inflammation Jointitis
Jointitis Inflammation of angle of mouth
Inflammation of angle of mouth Odontogenic inflammatory diseases of maxillofacial area
Odontogenic inflammatory diseases of maxillofacial area Dlc in physiology
Dlc in physiology Infection du colon
Infection du colon Lingual tonsil
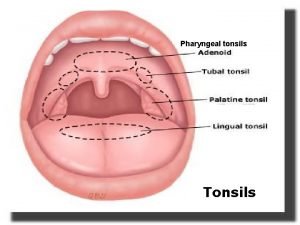
Lingual tonsil Serous inflammation examples
Serous inflammation examples Cellular events of acute inflammation
Cellular events of acute inflammation Acute inflammation
Acute inflammation Morphological pattern of inflammation
Morphological pattern of inflammation Mediators of inflammation
Mediators of inflammation übergewicht vla
übergewicht vla Otitis media with effusion otoscopy
Otitis media with effusion otoscopy Stages of inflammation
Stages of inflammation Intracellular accumulation
Intracellular accumulation Karbamasepin
Karbamasepin Silent inflammation - chronisch krank
Silent inflammation - chronisch krank Carbuncle
Carbuncle Middle meatus
Middle meatus Types of inflammation
Types of inflammation Chronic inflammation
Chronic inflammation Cell injury and inflammation
Cell injury and inflammation Acute inflammation
Acute inflammation Lochkerne
Lochkerne Sick
Sick Dr el sabbagh
Dr el sabbagh Morphological patterns of acute inflammation
Morphological patterns of acute inflammation Inflammation
Inflammation