LowGrade Inflammation and Exercise Wren L Mc Laughlin

- Slides: 37
Low-Grade Inflammation and Exercise Wren L. Mc. Laughlin Department of Physical Education, Health, and Recreation Western Washington University
Overview • • Definitions Potential Causes Detection Exercise Effects – – Overall Effects Aging Population Insulin-Resistant Population Type of Exercise • Exercise Recommendations
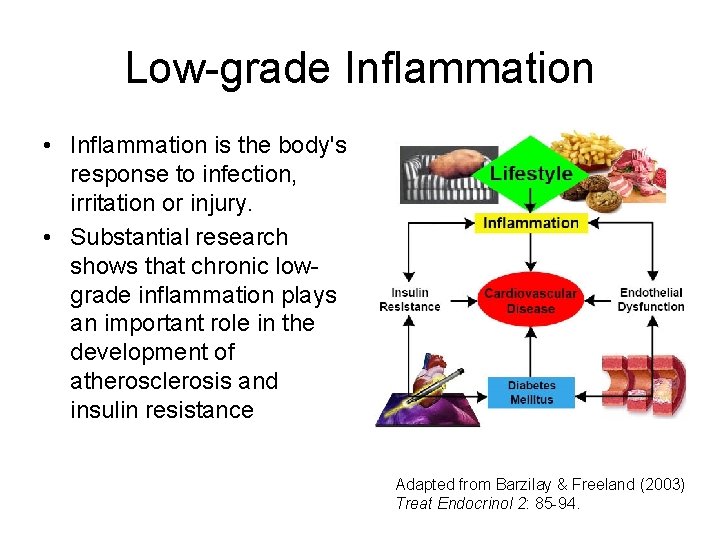
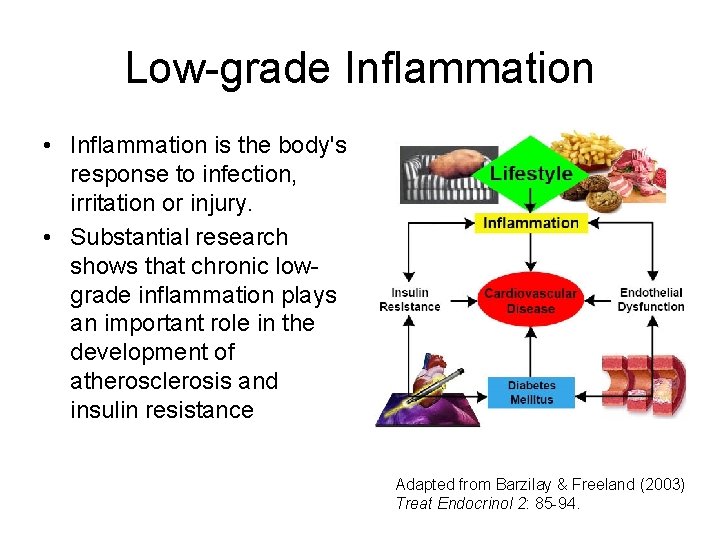
Low-grade Inflammation • Inflammation is the body's response to infection, irritation or injury. • Substantial research shows that chronic lowgrade inflammation plays an important role in the development of atherosclerosis and insulin resistance Adapted from Barzilay & Freeland (2003) Treat Endocrinol 2: 85 -94.
Associated Diseases • Low-grade inflammation is an independent risk factor for: – – Heart disease 1 Stroke 2 Diabetes 3, 4 All-cause mortality 5 1 Hansson (2005) N Engl J Med 352: 1685 -95. 2 Corrado et al. (2006) Stroke 37: 482 -6. 3 Pradhan et al. (2001) JAMA 286: 327 -34. 4 Spranger et al. (2003) Diabetes 52: 812 -7 5 Ford (2005) Diabetes Care 28: 1769 -78.
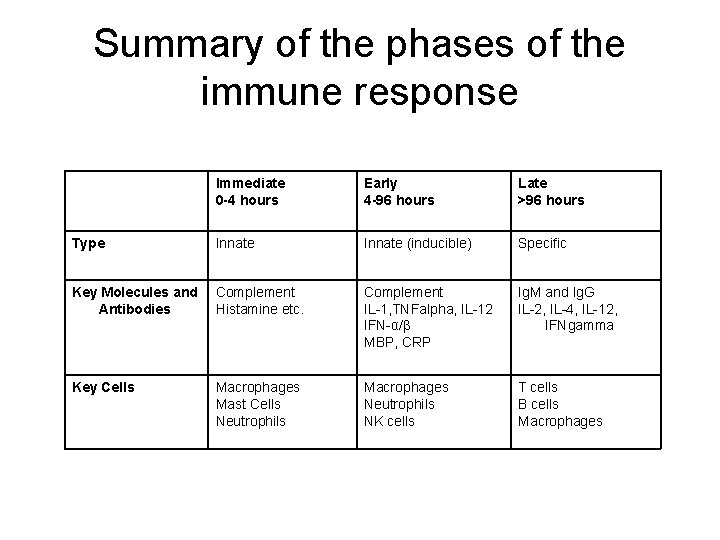
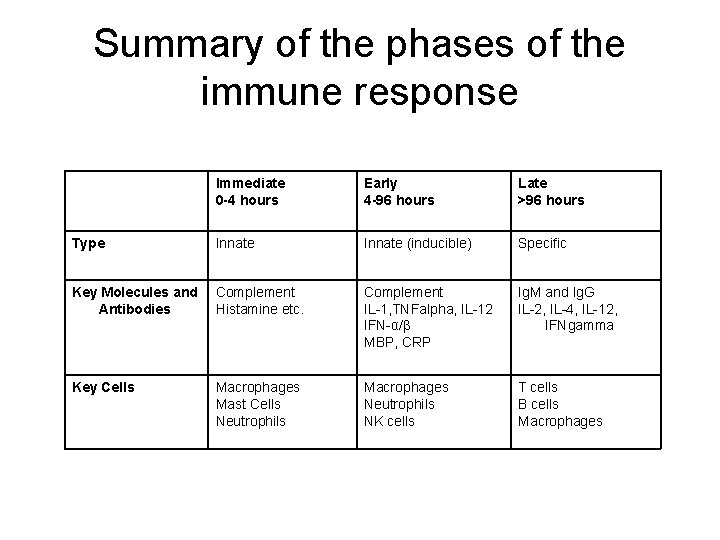
Summary of the phases of the immune response Immediate 0 -4 hours Early 4 -96 hours Late >96 hours Type Innate (inducible) Specific Key Molecules and Antibodies Complement Histamine etc. Complement IL-1, TNFalpha, IL-12 IFN-α/β MBP, CRP Ig. M and Ig. G IL-2, IL-4, IL-12, IFNgamma Key Cells Macrophages Mast Cells Neutrophils Macrophages Neutrophils NK cells T cells B cells Macrophages
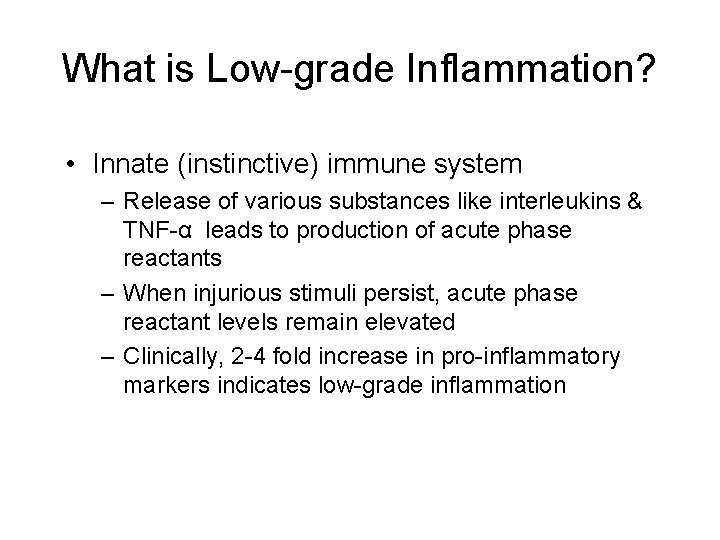
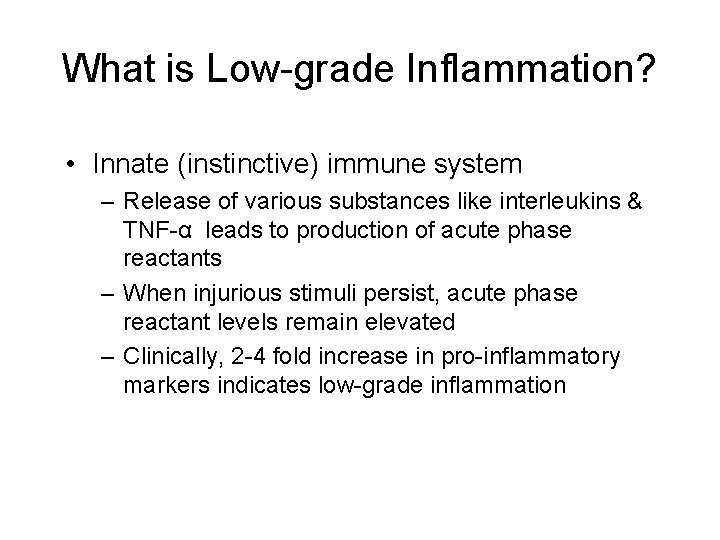
What is Low-grade Inflammation? • Innate (instinctive) immune system – Release of various substances like interleukins & TNF-α leads to production of acute phase reactants – When injurious stimuli persist, acute phase reactant levels remain elevated – Clinically, 2 -4 fold increase in pro-inflammatory markers indicates low-grade inflammation
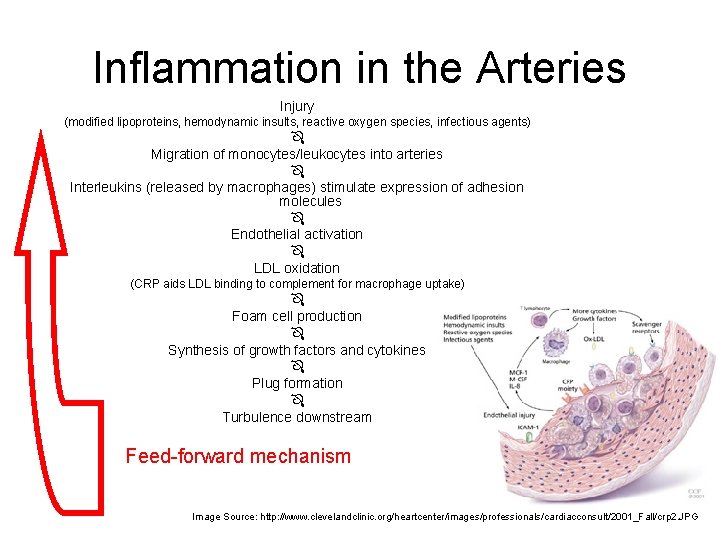
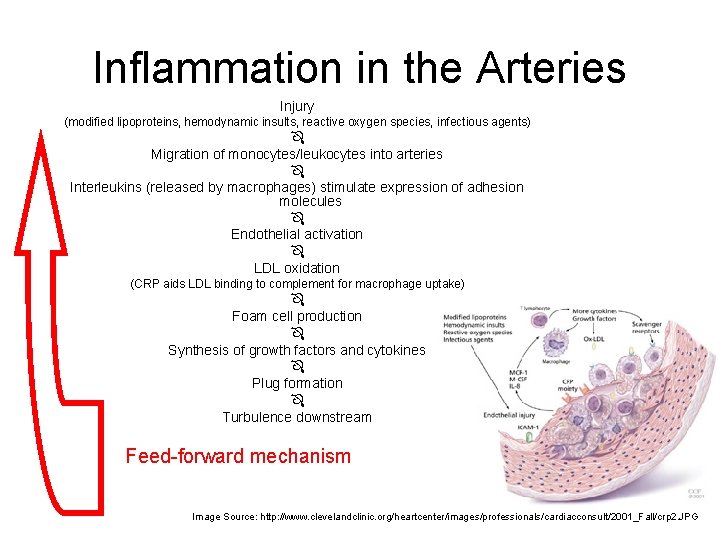
Inflammation in the Arteries Injury (modified lipoproteins, hemodynamic insults, reactive oxygen species, infectious agents) Migration of monocytes/leukocytes into arteries Interleukins (released by macrophages) stimulate expression of adhesion molecules Endothelial activation LDL oxidation (CRP aids LDL binding to complement for macrophage uptake) Foam cell production Synthesis of growth factors and cytokines Plug formation Turbulence downstream Feed-forward mechanism Image Source: http: //www. clevelandclinic. org/heartcenter/images/professionals/cardiacconsult/2001_Fall/crp 2. JPG
Potential Causes • • Activity Level Diet Obesity Infection
A Sedentary Lifestyle • Skeletal muscle may act as an endocrine organ – Influencing metabolism (“IL-6 as energy sensor”) – Modify immune system message production in other tissues including endothelial and adipose tissues 1 – Production and release anti-inflammatory substances into the blood 2 – Exercise training reduces skeletal muscle TNF-α, IL-1 b, IL-6 expression in patients with heart failure 3 • Exercise may improve endothelial function – Exercise may limit leukocyte adhesion molecules and thus modify monocyte-endothelial cell interaction – Preserved NO availability – Up-regulation of antioxidant enzymes therefore increasing antioxidant effect in vessels (less LDL oxidization) 1 Bruungsgaard (2005) J Leukoc Biol 78: 819 -35. 2 Febbraio & Pederson (2006) Exerc Sport Sci Rev 33: 114 -9. 3 Gielen et al. (2003) J Am Coll Cardiol 42: 861 -8.
Western Diet • Refined foods may boost inflammation • Necessary nutrients for optimal immune function and prevention of cardiovascular disease and diabetes is lacking 1 • Glycemic load – Predictor of type 2 diabetes independent of total calories consumed – Increase the risk of diabetes by 2. 5 times in both men and women 2, 3 – High glycemic load is related to high levels of C-reactive protein independent of weight and total caloric intake in healthy middle-aged women 4 1 Calder & Kew (2002) Br J Nutr 88: S 165 -77. 2 Salmeron et al. (1997) Diabetes Care 20: 545 -50. 3 Salmeron et al. (1997) JAMA 277: 472 -7. 4 Liu et al. (2002) Am J Clin Nutr 75: 492 -8.
Western Diet • Polyunsaturated fatty acids – Cell membrane functioning – Ratio Omega-6: Omega 3 1: 1 to 15: 1 1 – Associated with lower levels of proinflammatory markers (IL-6, TNF-α, CRP) and higher levels of anti-inflammatory markers 2 – Mediterranean-inspired diet (one month) showed no significant change in IL-6 or CRP 3 1 Simpoulo (2002) Biomed Pharmacother 56: 365 -79. 2 Ferrucci et al. (2006) J Clin Endocrinol Metab 91: 439 -46. 3 Ambring et al. (2006) Am J Clin Nutr 83: 575 -81. Image Source: http: //www. ec. gc. ca/Enviro. Zine/images/Issue 43/omega 3 source_l. jpg
Western Diet • Vitamins and Minerals – Insufficient consumption of B vitamins and folic acid can harm the lining of blood vessels by increasing clotting, oxidative stress, and interactions with white blood cells 1 – Potential role of magnesium deficiency in chronic inflammation 2, 3 – High meat diet + low antioxidant vitamin (E &C) consumption may increase free radical production in the blood vessels 4, 5 1 Jonasson et al. (2005) Clin Chem Lab Med 43: 628 -34. 2 King et al. (2005) J Am Coll Nutr 24: 166 -71. 3 Song et al. (2005) Diabetes Care 28: 1438 -44. 4 Ford et al. (2005) Am J Kidney Dis 45: 248 -55. 5 Accinni et al. (2006) Nutr Metab Cardiovasc Dis 16: 121 -7.
Obesity • Adipocytes may promote inflammation 1 • Concentrations of IL-6, TNF-α, MMP-9 and CRP from mononuclear cells were significantly higher in obese subjects 2 • In severely obese individuals treatment of caloric reduction and exercise changed levels of inflammatory markers in adipose tissue but not in skeletal muscle 3 • Association established between inflammatory cytokines and adipose tissue function 4 • In centrally obese individuals, adipocytes produce more IL-6 than subcutaneous adipocytes 5 1 Bastard et al. (2006) Eur Cytokine Netw 17: 4 -12. . et al. (2004) Circulation 110: 1564 -71. 3 Bruun et al. (2006) Am J Physiol Endocrinol Metab. 2006 May; 290(5): E 961 -7 4 Trayhurn & Wood (2004) Br J Nutr. 2004 Sep; 92(3): 347 -55. 5 Barzilay & Freedland (2003) Treat Endocrinol 2: 85 -94. 2 Ghanim
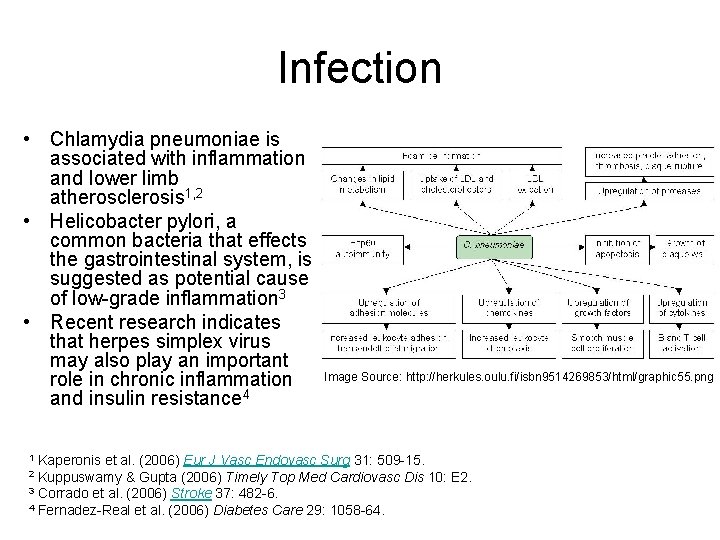
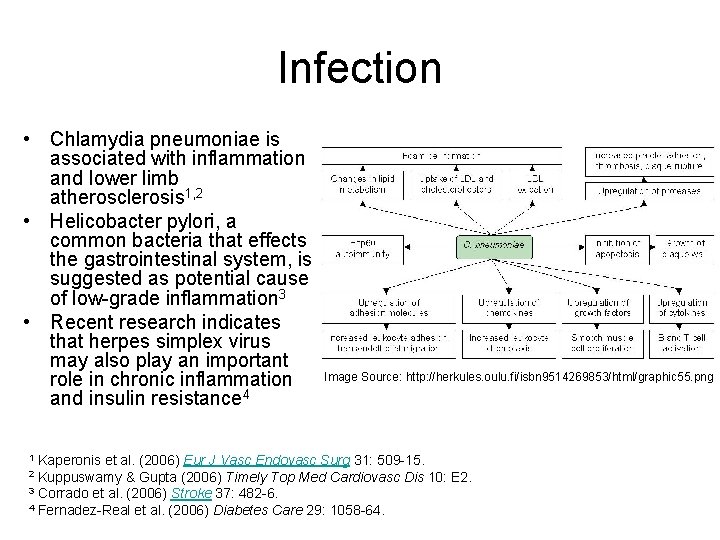
Infection • Chlamydia pneumoniae is associated with inflammation and lower limb atherosclerosis 1, 2 • Helicobacter pylori, a common bacteria that effects the gastrointestinal system, is suggested as potential cause of low-grade inflammation 3 • Recent research indicates that herpes simplex virus may also play an important role in chronic inflammation and insulin resistance 4 Image Source: http: //herkules. oulu. fi/isbn 9514269853/html/graphic 55. png Kaperonis et al. (2006) Eur J Vasc Endovasc Surg 31: 509 -15. Kuppuswamy & Gupta (2006) Timely Top Med Cardiovasc Dis 10: E 2. 3 Corrado et al. (2006) Stroke 37: 482 -6. 4 Fernadez-Real et al. (2006) Diabetes Care 29: 1058 -64. 1 2
Detection Methods • Clinical Blood Test for C-Reactive Protein Global Risk Assessment http: //www. americanheart. org/presenter. jhtml? identifier=3003500 – provided by American Heart Association – Low Risk = no test – Moderate or High Risk = CRP testing warranted Ridker (2001) Circulation 103: 1813 -8.
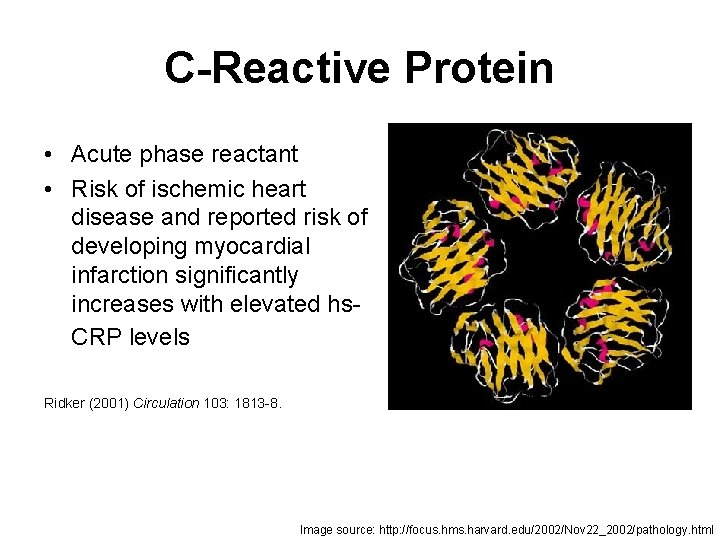
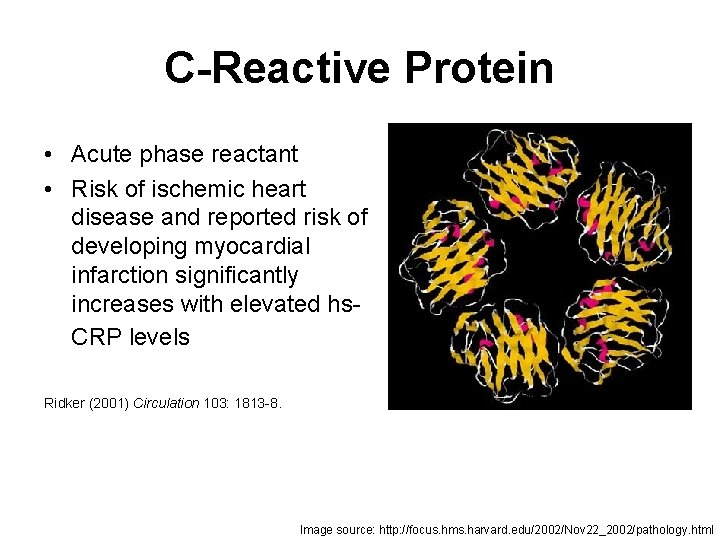
C-Reactive Protein • Acute phase reactant • Risk of ischemic heart disease and reported risk of developing myocardial infarction significantly increases with elevated hs. CRP levels Ridker (2001) Circulation 103: 1813 -8. Image source: http: //focus. hms. harvard. edu/2002/Nov 22_2002/pathology. html
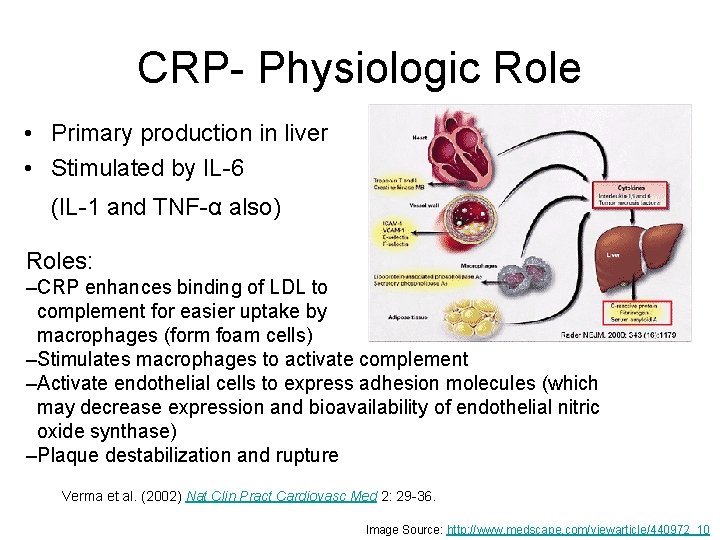
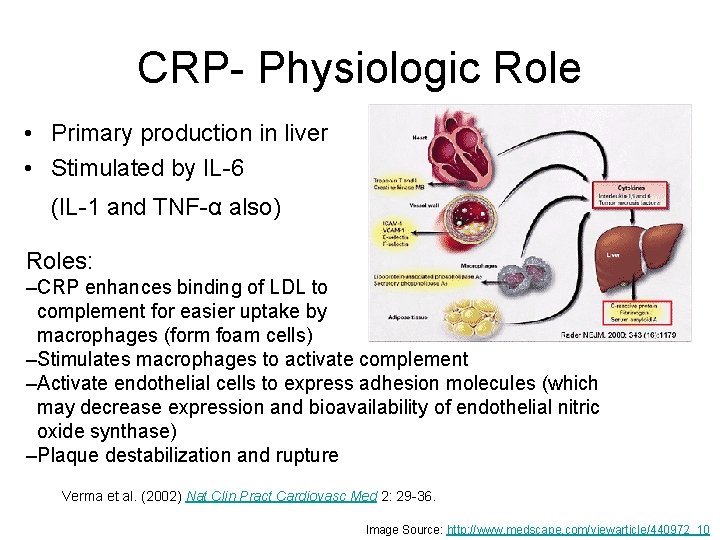
CRP- Physiologic Role • Primary production in liver • Stimulated by IL-6 (IL-1 and TNF-α also) Roles: –CRP enhances binding of LDL to complement for easier uptake by macrophages (form foam cells) –Stimulates macrophages to activate complement –Activate endothelial cells to express adhesion molecules (which may decrease expression and bioavailability of endothelial nitric oxide synthase) –Plaque destabilization and rupture Verma et al. (2002) Nat Clin Pract Cardiovasc Med 2: 29 -36. Image Source: http: //www. medscape. com/viewarticle/440972_10
Interleukins • Messengers • Pro/anti-inflammatory • Secreted by leukocytes to stimulate immune response to trauma • IL-1, IL-4, 1 L-6, 1 L-10 etc. Image source: http: //www. rndsystems. com/DAM_public/5645. jpg
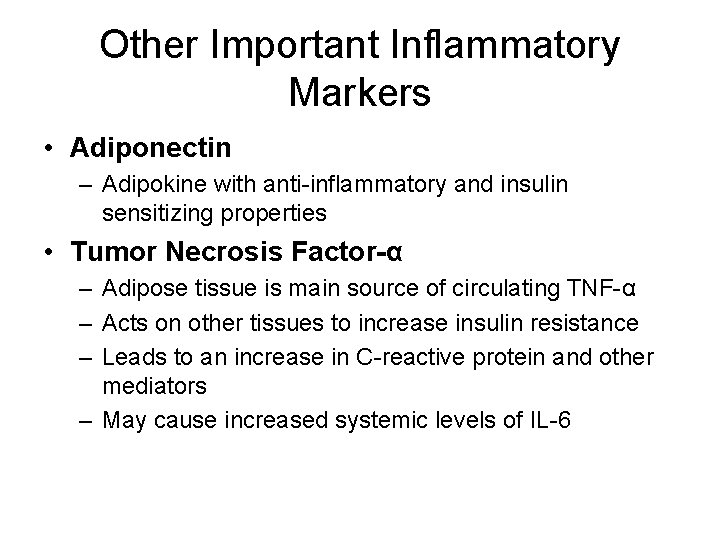
Other Important Inflammatory Markers • Adiponectin – Adipokine with anti-inflammatory and insulin sensitizing properties • Tumor Necrosis Factor-α – Adipose tissue is main source of circulating TNF-α – Acts on other tissues to increase insulin resistance – Leads to an increase in C-reactive protein and other mediators – May cause increased systemic levels of IL-6
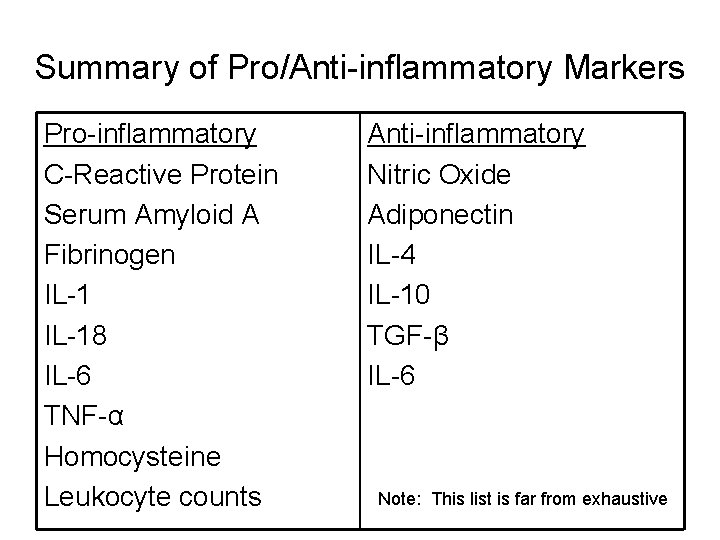
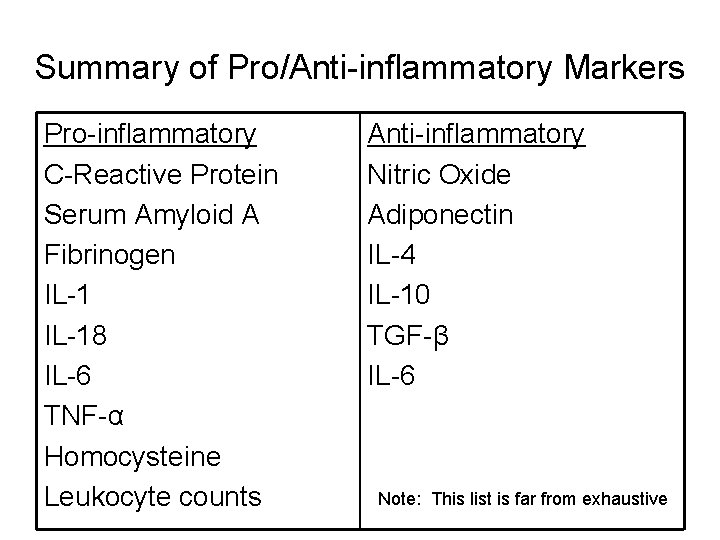
Summary of Pro/Anti-inflammatory Markers Pro-inflammatory C-Reactive Protein Serum Amyloid A Fibrinogen IL-18 IL-6 TNF-α Homocysteine Leukocyte counts Anti-inflammatory Nitric Oxide Adiponectin IL-4 IL-10 TGF-β IL-6 Note: This list is far from exhaustive
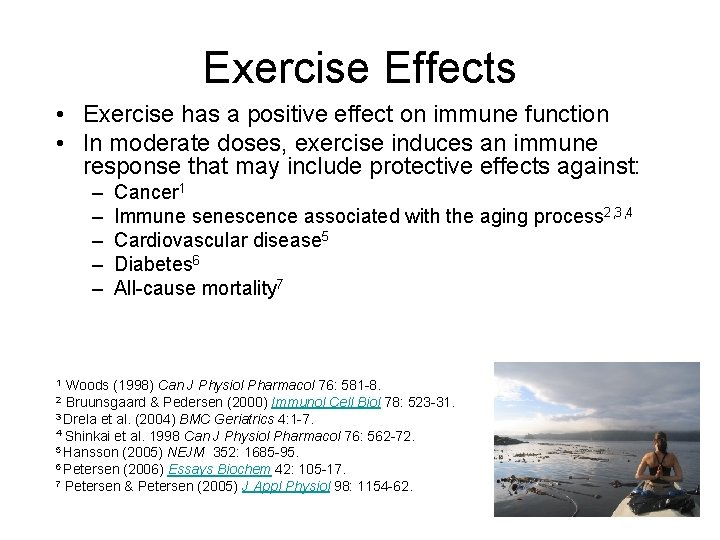
Exercise Effects • Exercise has a positive effect on immune function • In moderate doses, exercise induces an immune response that may include protective effects against: – – – Cancer 1 Immune senescence associated with the aging process 2, 3, 4 Cardiovascular disease 5 Diabetes 6 All-cause mortality 7 Woods (1998) Can J Physiol Pharmacol 76: 581 -8. Bruunsgaard & Pedersen (2000) Immunol Cell Biol 78: 523 -31. 3 Drela et al. (2004) BMC Geriatrics 4: 1 -7. 4 Shinkai et al. 1998 Can J Physiol Pharmacol 76: 562 -72. 5 Hansson (2005) NEJM 352: 1685 -95. 6 Petersen (2006) Essays Biochem 42: 105 -17. 7 Petersen & Petersen (2005) J Appl Physiol 98: 1154 -62. 1 2
Over-training • Overtraining can induce oxidative stress and compromise resistance to minor illnesses such as upper respiratory track infections 1, 2 • “Open-window” time period in athletes following physical exertion during which they are more susceptible to invasion by viruses and bacteria 3 1 Mac. Kinnon 2 3 (2000) Med Sci Sports Exerc 32: S 369 -76. Nieman (2000) Immunol Cell Biol 78: 496 -501. Nieman (2000) Med Sci Sports Exerc 32: S 406 -11. Image Source: http: //athleticssuperstars. tripod. com/paula_marathon. jpg
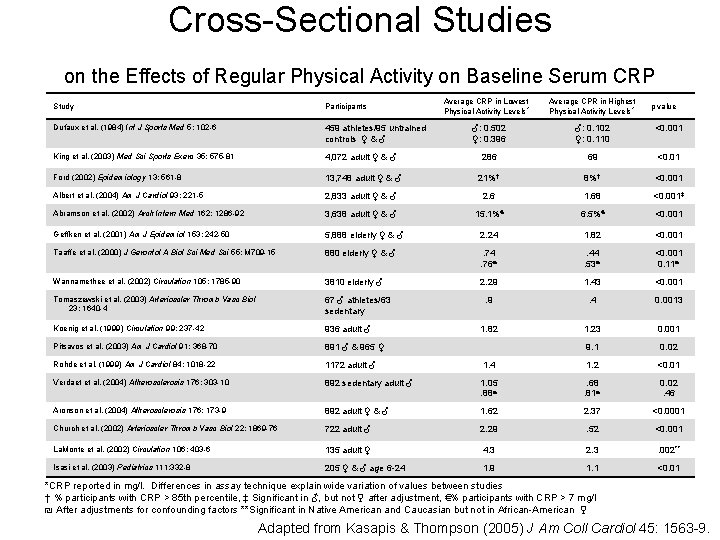
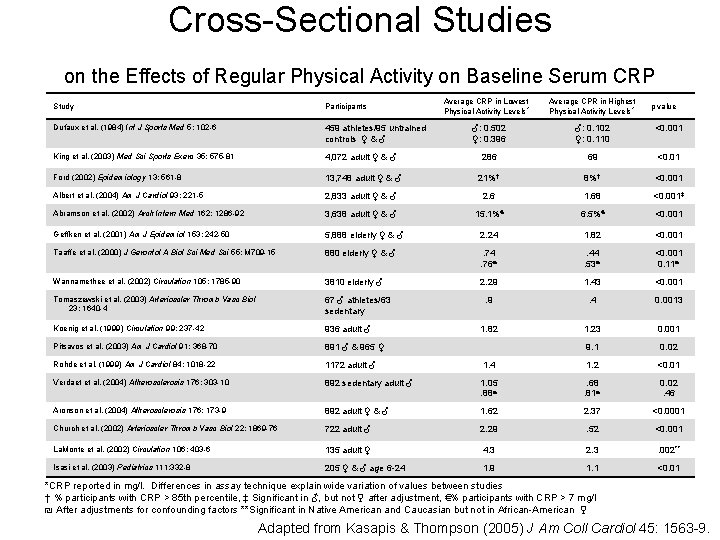
Cross-Sectional Studies on the Effects of Regular Physical Activity on Baseline Serum CRP Study Participants Dufaux et al. (1984) Int J Sports Med 5: 102 -6 459 athletes/95 untrained controls ♀ & ♂ King et al. (2003) Med Sci Sports Exerc 35: 575 -81 Average CRP in Lowest Physical Activity Levels * Average CPR in Highest Physical Activity Levels * p value ♂: 0. 502 ♀: 0. 396 ♂: 0. 102 ♀: 0. 110 <0. 001 4, 072 adult ♀ & ♂ 286 69 <0. 01 Ford (2002) Epidemiology 13: 561 -8 13, 748 adult ♀ & ♂ 21%† 8%† <0. 001 Albert et al. (2004) Am J Cardiol 93: 221 -5 2, 833 adult ♀ & ♂ 2. 6 1. 68 <0. 001‡ Abramson et al. (2002) Arch Intern Med 162: 1286 -92 3, 638 adult ♀ & ♂ 15. 1%€ 6. 5%€ <0. 001 Geffken et al. (2001) Am J Epidemiol 153: 242 -50 5, 888 elderly ♀ & ♂ 2. 24 1. 82 <0. 001 Taaffe et al. (2000) J Gerontol A Biol Sci Med Sci 55: M 709 -15 880 elderly ♀ & ♂ . 74. 76₪ . 44. 53₪ <0. 001 0. 11₪ Wannamethee et al. (2002) Circulation 105: 1785 -90 3810 elderly ♂ 2. 29 1. 43 <0. 001 Tomaszewski et al. (2003) Arterioscler Thromb Vasc Biol 23: 1640 -4 67 ♂ athletes/63 sedentary . 9 . 4 0. 0013 Koenig et al. (1999) Circulation 99: 237 -42 936 adult ♂ 1. 82 1. 23 0. 001 Pitsavos et al. (2003) Am J Cardiol 91: 368 -70 891 ♂ & 965 ♀ 9. 1 0. 02 Rohde et al. (1999) Am J Cardiol 84: 1018 -22 1172 adult ♂ 1. 4 1. 2 <0. 01 Verdaet et al. (2004) Atherosclerosis 176: 303 -10 892 sedentary adult ♂ 1. 05. 88₪ . 68. 81₪ 0. 02. 46 Aronson et al. (2004) Atherosclerosis 176: 173 -9 892 adult ♀ & ♂ 1. 62 2. 37 <0. 0001 Church et al. (2002) Arterioscler Thromb Vasc Biol 22: 1869 -76 722 adult ♂ 2. 29 . 52 <0. 001 La. Monte et al. (2002) Circulation 106: 403 -6 135 adult ♀ 4. 3 2. 3 . 002** Isasi et al. (2003) Pediatrics 111: 332 -8 205 ♀ & ♂ age 6 -24 1. 9 1. 1 <0. 01 *CRP reported in mg/l. Differences in assay technique explain wide variation of values between studies † % participants with CRP > 85 th percentile, ‡ Significant in ♂, but not ♀ after adjustment, €% participants with CRP > 7 mg/l ₪ After adjustments for confounding factors **Significant in Native American and Caucasian but not in African-American ♀ Adapted from Kasapis & Thompson (2005) J Am Coll Cardiol 45: 1563 -9.
Limitations of Cross-sectional Studies • Self-reported – Recall bias, reporting bias – Ability to classify fitness level • Cardiorespiratory fitness correlates to CRP levels – Must adjust for all potential confounders
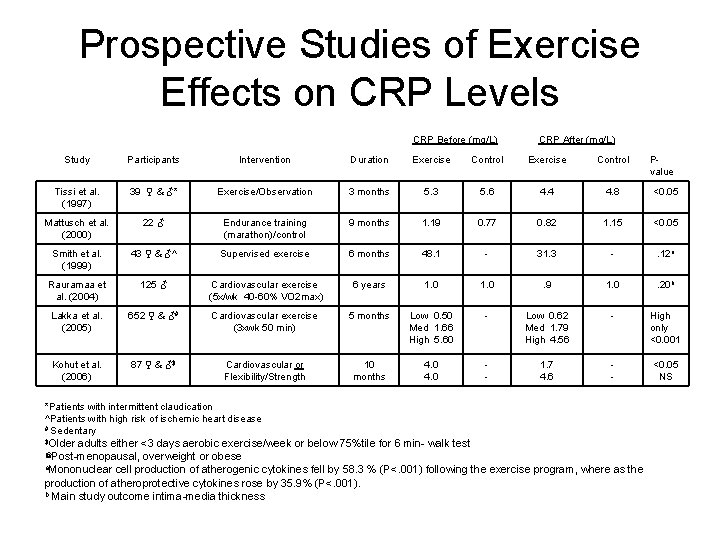
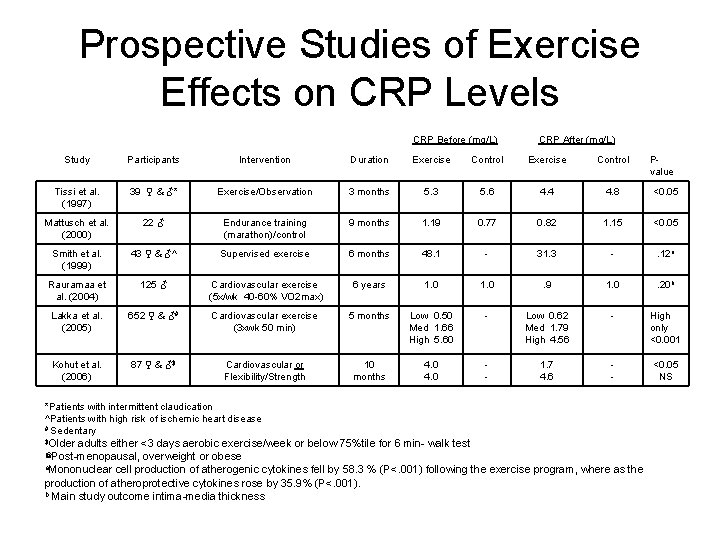
Prospective Studies of Exercise Effects on CRP Levels CRP Before (mg/L) CRP After (mg/L) Study Participants Intervention Duration Exercise Control Tissi et al. (1997) 39 ♀ & ♂* Exercise/Observation 3 months 5. 3 5. 6 4. 4 4. 8 <0. 05 Mattusch et al. (2000) 22 ♂ Endurance training (marathon)/control 9 months 1. 19 0. 77 0. 82 1. 15 <0. 05 Smith et al. (1999) 43 ♀ & ♂^ Supervised exercise 6 months 48. 1 - 31. 3 - . 12 a Rauramaa et al. (2004) 125 ♂ Cardiovascular exercise (5 x/wk 40 -60% VO 2 max) 6 years 1. 0 . 9 1. 0 . 20 b Lakka et al. (2005) 652 ♀ & ♂# Cardiovascular exercise (3 xwk 50 min) 5 months Low 0. 50 Med 1. 66 High 5. 60 - Low 0. 62 Med 1. 79 High 4. 56 - High only <0. 001 Kohut et al. (2006) 87 ♀ & ♂$ Cardiovascular or Flexibility/Strength 10 months 4. 0 - 1. 7 4. 6 - <0. 05 NS *Patients with intermittent claudication ^Patients with high risk of ischemic heart disease # Sedentary Older adults either <3 days aerobic exercise/week or below 75%tile for 6 min- walk test Post-menopausal, overweight or obese a. Mononuclear cell production of atherogenic cytokines fell by 58. 3 % (P<. 001) following the exercise program, where as the production of atheroprotective cytokines rose by 35. 9% (P<. 001). b Main study outcome intima-media thickness $ @ Pvalue
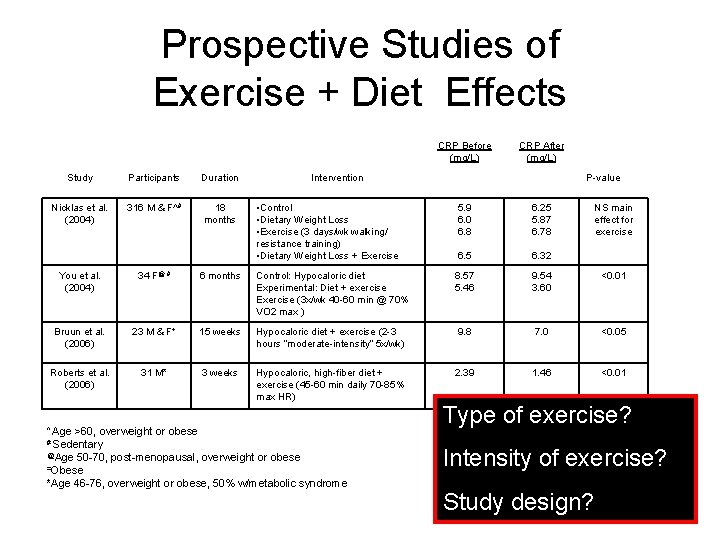
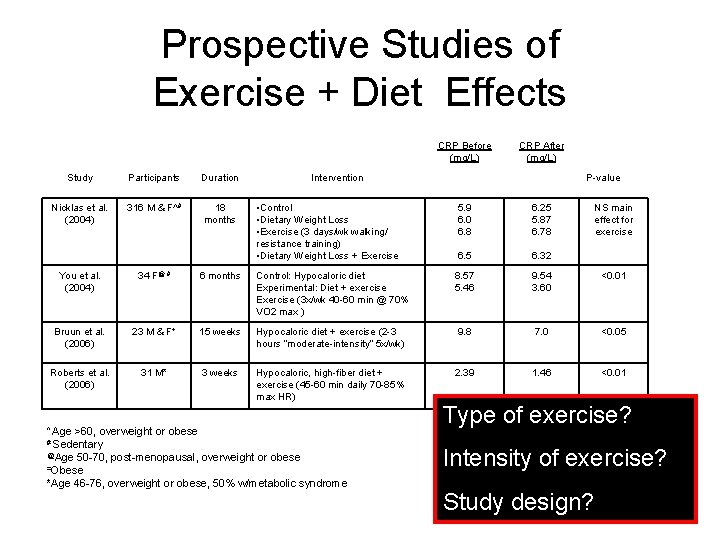
Prospective Studies of Exercise + Diet Effects CRP Before (mg/L) Study Participants Duration Nicklas et al. (2004) 316 M & F^# 18 months CRP After (mg/L) Intervention P-value • Control • Dietary Weight Loss • Exercise (3 days/wk walking/ resistance training) • Dietary Weight Loss + Exercise 5. 9 6. 0 6. 8 6. 25 5. 87 6. 78 6. 5 6. 32 NS main effect for exercise You et al. (2004) 34 F@ # 6 months Control: Hypocaloric diet Experimental: Diet + exercise Exercise (3 x/wk 40 -60 min @ 70% VO 2 max ) 8. 57 5. 46 9. 54 3. 60 <0. 01 Bruun et al. (2006) 23 M & F+ 15 weeks Hypocaloric diet + exercise (2 -3 hours “moderate-intensity” 5 x/wk) 9. 8 7. 0 <0. 05 Roberts et al. (2006) 31 M* 3 weeks Hypocaloric, high-fiber diet + exercise (45 -60 min daily 70 -85% max HR) 2. 39 1. 46 <0. 01 Age >60, overweight or obese # Sedentary @Age 50 -70, post-menopausal, overweight or obese =Obese *Age 46 -76, overweight or obese, 50% w/metabolic syndrome ^ Type of exercise? Intensity of exercise? Study design?
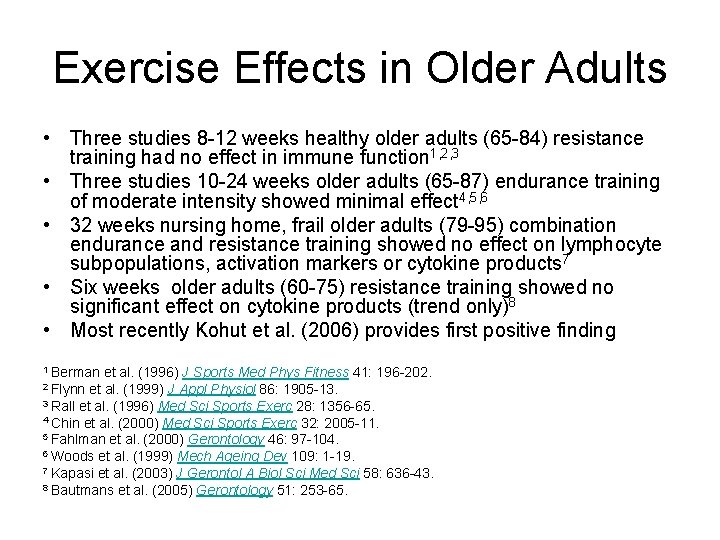
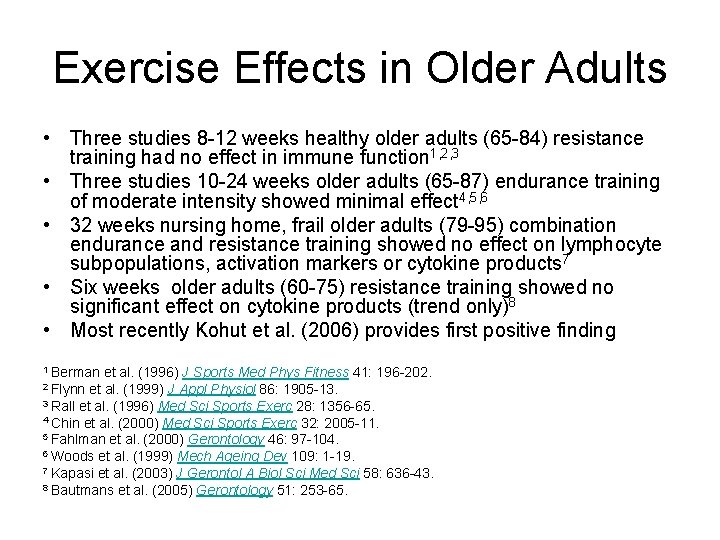
Exercise Effects in Older Adults • Three studies 8 -12 weeks healthy older adults (65 -84) resistance training had no effect in immune function 1, 2, 3 • Three studies 10 -24 weeks older adults (65 -87) endurance training of moderate intensity showed minimal effect 4, 5, 6 • 32 weeks nursing home, frail older adults (79 -95) combination endurance and resistance training showed no effect on lymphocyte subpopulations, activation markers or cytokine products 7 • Six weeks older adults (60 -75) resistance training showed no significant effect on cytokine products (trend only)8 • Most recently Kohut et al. (2006) provides first positive finding 1 Berman et al. (1996) J Sports Med Phys Fitness 41: 196 -202. et al. (1999) J Appl Physiol 86: 1905 -13. 3 Rall et al. (1996) Med Sci Sports Exerc 28: 1356 -65. 4 Chin et al. (2000) Med Sci Sports Exerc 32: 2005 -11. 5 Fahlman et al. (2000) Gerontology 46: 97 -104. 6 Woods et al. (1999) Mech Ageing Dev 109: 1 -19. 7 Kapasi et al. (2003) J Gerontol A Biol Sci Med Sci 58: 636 -43. 8 Bautmans et al. (2005) Gerontology 51: 253 -65. 2 Flynn
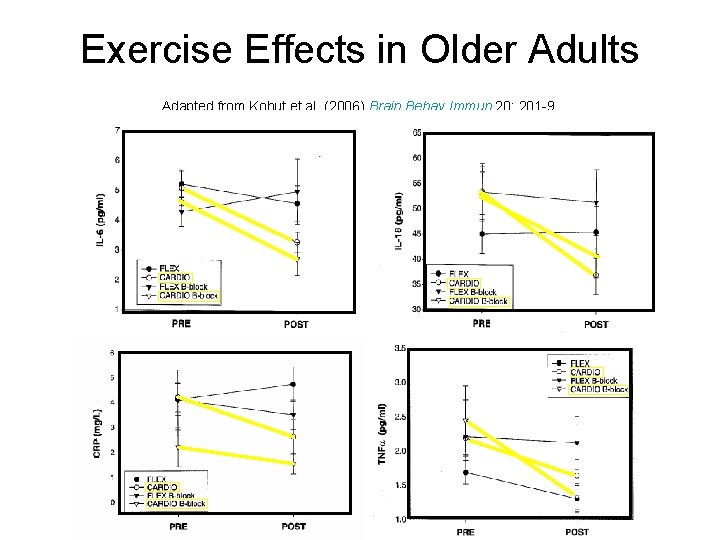
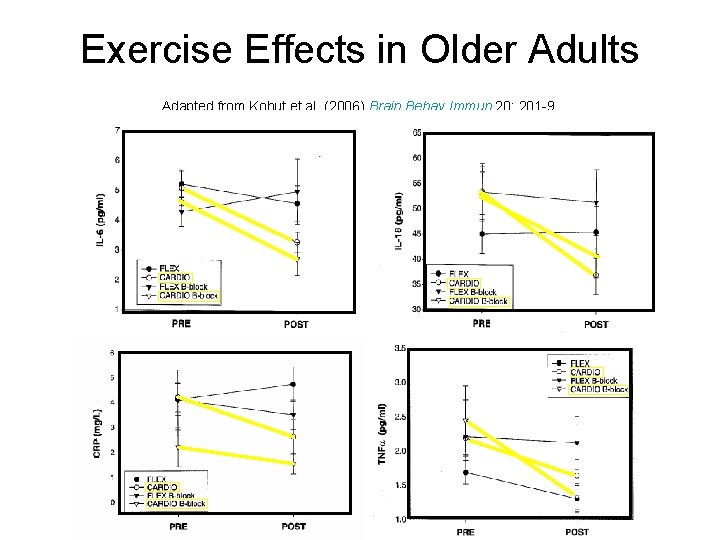
Exercise Effects in Older Adults Adapted from Kohut et al. (2006) Brain Behav Immun 20: 201 -9.
Insulin Resistance • CRP and IL-6 predict the development of type-2 diabetes in women 1 and older adults 2 • Possible relationship between inflammation and glucose utilization and insulin sensitivity in overweight and obese postmenopausal women – Improvements in glucose metabolism associated w/ decreased cytokine concentrations during weight loss program 3 • Possible association between low cardio respiratory fitness and C-reactive protein levels in women with type 2 diabetes 4 1 Prahhan et al. (2001) JAMA 286: 327 -34. et al. (2001) Diabetes 50: 2384 -9. 3 Ryan & Nicklas (2004) Diabetes Care 27: 1699 -705 4 Mc. Gavock et al. (2004) Diabetes Care 27: 320 -5. 2 Barzilay
Insulin Resistance and Inflammatory Markers • Middle-aged white M & F • 4 week training – 3 x/week 60 minutes (20 min warm-up/cool down, 20 min run/bike, 20 min power training) + 1 x/week 60 minutes swimming – Significant reduction in adiponectin in impaired glucose tolerant and type-2 diabetes participants – Significant reduction in CRP levels in normal, impaired, and type 2 diabetes groups, however reduction in normal glucose tolerant participants did not change as much. – NO significant change in IL-6 or IL-10 Oberbach et al. (2006) Eur J Endocrinol 154: 577 -85.
Insulin Resistance, Endothelial Dysfunction and Low-grade Inflammation • Proposed mechanisms – Liberation of fatty acids from adipose tissue leads to increased production of free radicals which inhibits nitric oxide (important for healthy arterial walls) – IL-6 from skeletal muscle may be involved in mediation of glucose uptake during exercise – TNF-α involvement in increased insulin resistance • Precise role of inflammation in insulin resistance and the relationship to endothelial dysfunction remains unclear Barzilay & Freeland (2003) Treat Endocrinol 2: 85 -94.
Post-menopausal Women • Special risk factors with Hormone Replacement Therapy (HRT) • HRT has a vascular inflammation effect and may lead to increased risk of adverse cardiovascular events • Women's Health Initiative 1 – Elevated levels of CRP and IL-6 were associated with HRT use – Use or nonuse of HRT is less important as a predictor of cardiovascular risk than baseline levels of either CRP or IL-6 • Stauffer Study 2 – CRP levels unchanged from normal values in women who exercised while taking hormone replacement therapy (HRT) – CRP levels were significantly higher in sedentary HRT users – Exercise may be beneficial to counteract the negative impacts of HRT 1 Pradhan 2 et al. (2002) JAMA 288: 980 -7. Stauffer et al. (2004) J Appl Physiol 96: 143 -8.
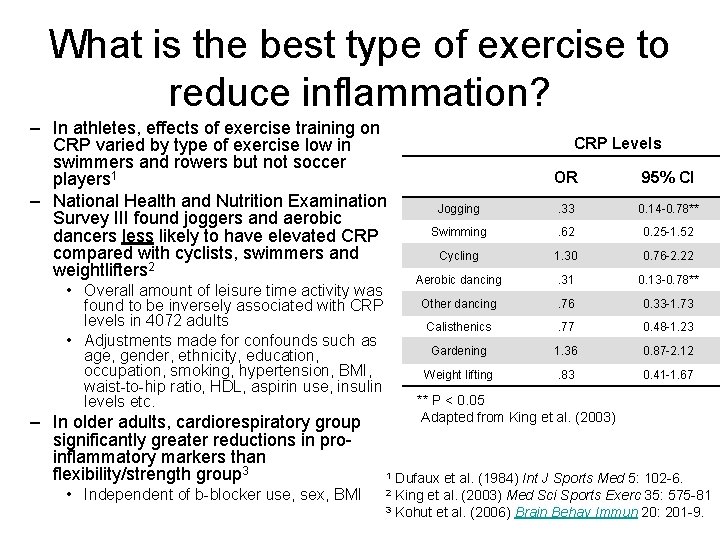
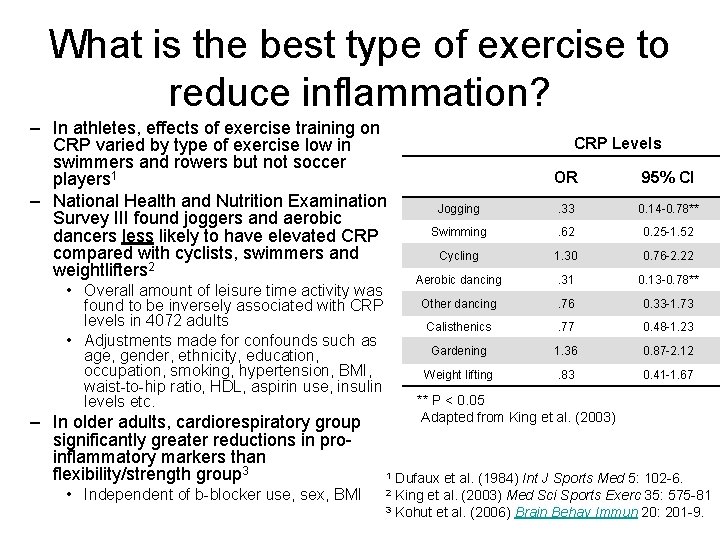
What is the best type of exercise to reduce inflammation? – In athletes, effects of exercise training on CRP varied by type of exercise low in swimmers and rowers but not soccer players 1 – National Health and Nutrition Examination Survey III found joggers and aerobic dancers less likely to have elevated CRP compared with cyclists, swimmers and weightlifters 2 • Overall amount of leisure time activity was found to be inversely associated with CRP levels in 4072 adults • Adjustments made for confounds such as age, gender, ethnicity, education, occupation, smoking, hypertension, BMI, waist-to-hip ratio, HDL, aspirin use, insulin levels etc. – In older adults, cardiorespiratory group significantly greater reductions in proinflammatory markers than flexibility/strength group 3 • Independent of b-blocker use, sex, BMI CRP Levels OR 95% CI Jogging . 33 0. 14 -0. 78** Swimming . 62 0. 25 -1. 52 Cycling 1. 30 0. 76 -2. 22 Aerobic dancing . 31 0. 13 -0. 78** Other dancing . 76 0. 33 -1. 73 Calisthenics . 77 0. 48 -1. 23 Gardening 1. 36 0. 87 -2. 12 Weight lifting . 83 0. 41 -1. 67 ** P < 0. 05 Adapted from King et al. (2003) Dufaux et al. (1984) Int J Sports Med 5: 102 -6. King et al. (2003) Med Sci Sports Exerc 35: 575 -81 3 Kohut et al. (2006) Brain Behav Immun 20: 201 -9. 1 2
American College of Sports Medicine Exercise Prescription Guidelines • No specific section devoted to low-grade inflammation • Section on metabolic syndrome (pg 219 -220) – Standard exercise prescription – Hypertension, diabetes, obesity may be present and require special exercise prescription – Referral to Obesity section • Exercise progression should include increased training intensity (50 -75% max VO 2 or HR) ACSM's Quidelines for Exercise Testing and Prescription (2006) 7 ed. , Philadephia: Lippincott Williams & Wilkins
Exercise Prescription Recommendations – Low-grade inflammation may be present in asymptomatic individuals… – Pre-exercise Testing • Assess global risk factors; recommendation for follow-up with physician • History of work-related MSD – Pathophysiology of disorder, wide-spread symptoms may be present – Cardiorespiratory 3 -5 days/wk • Progressive up to 75% Maximum Oxygen consumption (VO 2 max) or 16 Rating of Perceived Exertion (RPE) • Progress up to 30 minute minimum – Strength training 2 days/wk • Progressive up to 19 -20 RPE • 8 -10 reps on all major muscle groups Note: strength training important for sarcopenia prevention but likely not as important in the reduction of chronic low-grade inflammation

Consumer Education Materials: Exercise doesn’t make money, drugs and supplements DO! Stop Inflammation NOW! A Step-by-Step Plan to Prevent, Treat, and Reverse Inflammationthe Leading Cause of Heart Disease and Related Conditions Richard M. Fleming, M. D. 0 Approximately 25. 7% of women, representing approximately 26. 8 million women, did not report using hormone replacement therapy and had a CRP concentration >3. 0 to 10 mg/L, a category considered to indicate high risk for cardiovascular disease 1 1 Ford et al. (2004) Clin Chem 50: 574 -81. C-Reactive Protein: Everything You Need to Know About CRP and Why It’s More Important than Cholesterol to You Health What CRP is and why you need to be concerned about it What do to do if your CRP level is high Lifestyle information on nutrition, supplements, exercise and medication Scott J. Deron, D. O. , FACC
Resources on the Web • American Heart Association: Inflammation, Heart Disease and Stroke: The Role of C-Reactive Protein http: //www. americanheart. org/presenter. jhtml? identifier=4648 • Diabetes Drug Reduces Development of Heart Stent Blockage http: //www. diabetes. org/for-media/scientific-sessions/06 -14 -03 -1. jsp • Vitamins C And E: Protection For Your Blood Vessels? http: //www. diabetes. org/diabetes-forecast/jun 2005/research. jsp • Low-grade inflammation ready to move to the mainstream http: //www. theheart. org/view. Article. do? simple. Name=336538 • Inflammation and the Metabolic Syndrome- A powerpoint presentation by Dr. Jorge Plutzky http: //www. medscape. com/viewarticle/440972_8 • Latest News and Resources on Metabolic Syndrome X from Medline http: //www. nlm. nih. gov/medlineplus/metabolicsyndromex. html