Should we undertake surveillance for HCC in patients






- Slides: 25
Should we undertake surveillance for HCC in patients with NAFLD ? ? DR. Ahmed Zeid (MD) Ass. Prof. Internal Medicine HPB UNIT-Alexandria
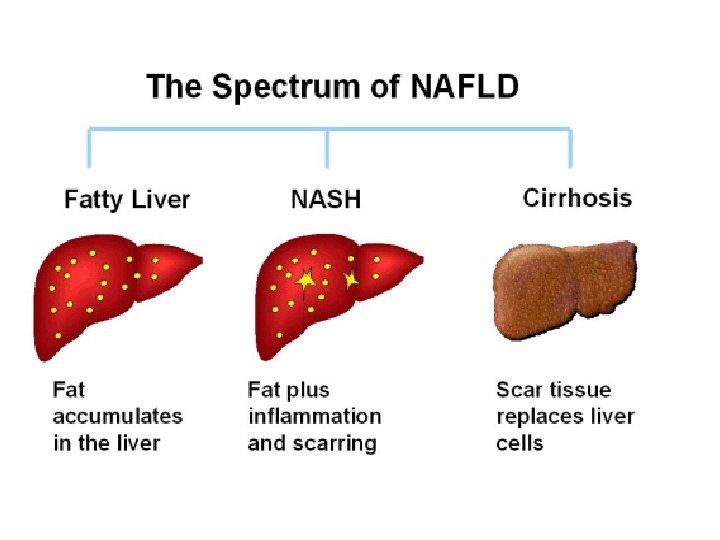
The term NASH was first introduced by Ludwig and co-workers in 1980, when they described the histological findings that occurred in obese, diabetic patients (mainly women) who denied alcohol intake.
• Up to 30% of adults in North America and Western Europe are known to have excess fat accumulation in the liver. Of these, nearly 10% have NASH, which represents 2%-3% of all adults. • NAFLD may soon become one of the main causes of ESLD requiring liver transplantation in North America. Roberto HA et al. World J Gastroenterol. 2012

NAFLD HCC ? ? ?
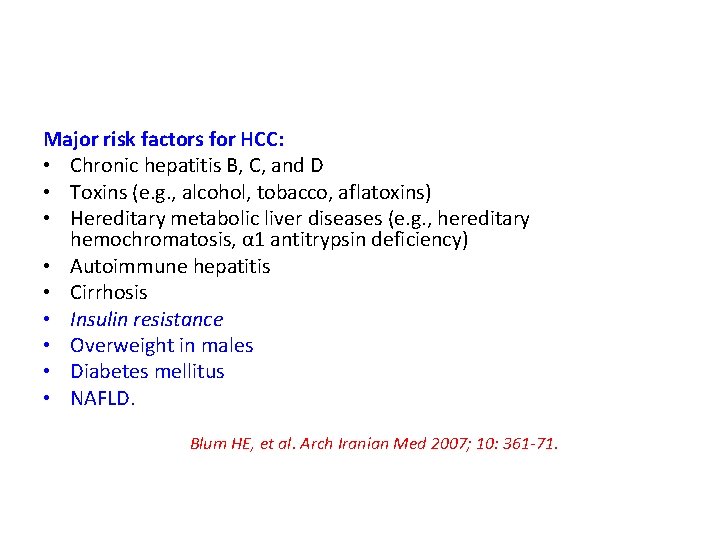
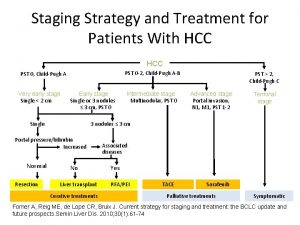
Major risk factors for HCC: • Chronic hepatitis B, C, and D • Toxins (e. g. , alcohol, tobacco, aflatoxins) • Hereditary metabolic liver diseases (e. g. , hereditary hemochromatosis, α 1 antitrypsin deficiency) • Autoimmune hepatitis • Cirrhosis • Insulin resistance • Overweight in males • Diabetes mellitus • NAFLD. Blum HE, et al. Arch Iranian Med 2007; 10: 361 -71.
• NAFLD is the most rapidly increasing cause of HCC, in parallel with the spread of obesity and diabetes in the general population.
• The annual incidence of HCC in patients with HCV is 4% and NAFLD-cirrhosis 2. 5%, while the 5 - year incidence rises to 30% in HCV in comparison to 11% in NAFLD patients.


• HCC can also develop in non- cirrhotic NAFLD, with hundreds of cases reported. The initial observation was made in a single-centre study in USA on 128 patients undergoing liver resection for HCC; 16 HCC occurence in livers without significant fibrosis was more frequent in patients with metabolic syndrome and NAFLD than in patients with liver disease of other etiologies
• The life expectancy of NAFLD patients with HCC is generally thought to be poor because of their associated co-morbidity of MS that often limits therapeutic choices including orthotopic liver transplantation. Heuer M, et al. Digestion 2012; 86: 107 -13
• Patients with NAFLD cirrhosis had a significantly greater prevalence of advanced HCC stage, lower amenability to any treatment, and shorter survival times compared with HCV patients, because HCC in these patients is often diagnosed at an advanced stage owing to lack of surveillance Giannini et al Clin Gastroenterol Hepatol 2009; 7: 580 -5
NAFLD-HCC multiple hits Risk factors for the development of HCC in NAFLD: 1. Old age. 2. Cirrhosis. 3. Obesity especially visceral fat. 4. Type 2 DM. 5. Cardiovascular comorbidities. 6. Genetic background: • PNPLA 3 rs 738409 [G] risk allele, is repeatedly reported to increase risk of HCC by 12 fold. • TERT, MBOAT other genes have been reported
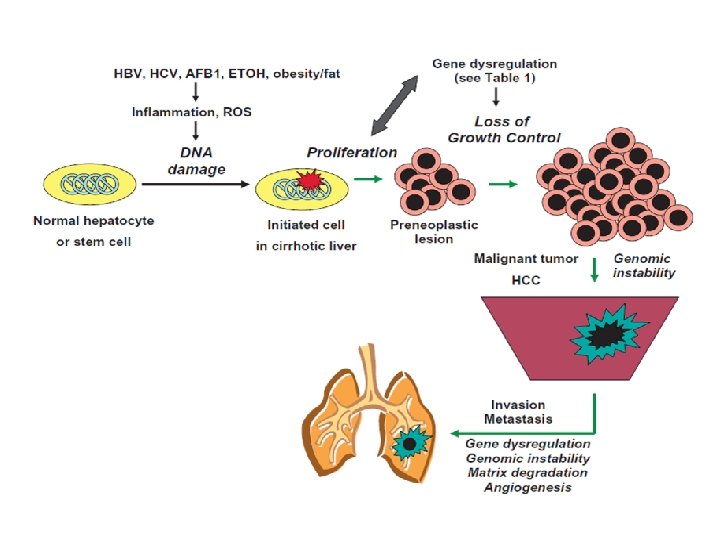
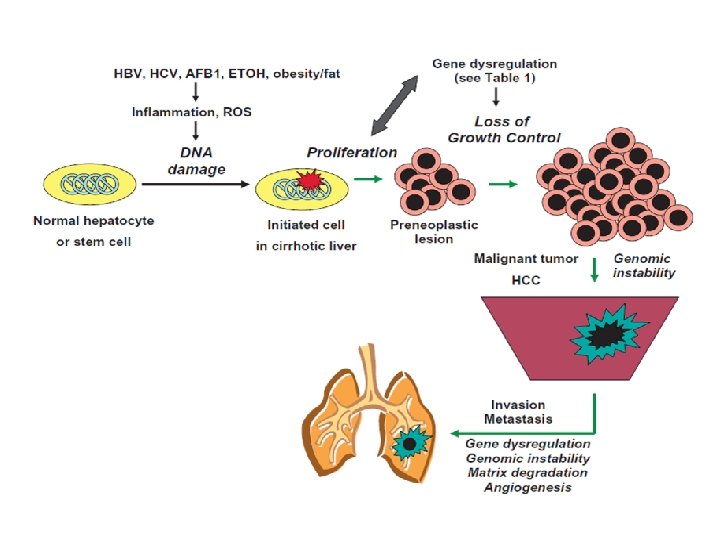
HEPATOCARCINOGENESIS • Ongoing chronic liver cell injury, inflammation, regeneration, fibrosis and subsequently cirrhosis can lead to uncontrolled focal liver cell growth and eventually HCC. • Mostly, HCC slowly unfolds on a background of chronic inflammation triggered by exposure to HBV, HCV, toxic compounds (ethanol), or metabolic impairment.
NAFLD CARCINOGENESIS ? ? insulin resistance + oxidative stress • NASH-associated insulin resistance causes inhibition of hepatic mitochondrial fatty acid oxidation and increased intracellular fatty acids may lead to oxidative DNA damage. • Insulin resistance with hyperinsulinaemia, Insulin -like growth factor 1 significantly activated MAPK and increased overexpression of protooncogenes in cultured hepatoma cells.
HCC Survillence NAFLD with cirrhosis: Poor surveillance is a constant problem. In a multicentre prospective study in Italy, which included 756 patients with HCC related either to NAFLD or HCV, 52% of patients with NAFLDrelated HCC were not diagnosed on regular surveillance compared to 37% of patients with HCV-related HCC , resulting in more advanced HCC burden at diagnosis.
HCC Survillence NAFLD with cirrhosis: • In a national USA cohort study from Veterans Administration hospitals, including 1, 500 patients who developed HCC from 2005 -2010, diagnosis was made by surveillance in 40% of patients with NAFLD compared to 80% of patients with HCV • Surveillance for HCC occurrence in NAFLD-cirrhosis is included in ‘‘other conditions” in the AASLD guidelines for management of HCC with no specific recommendations.
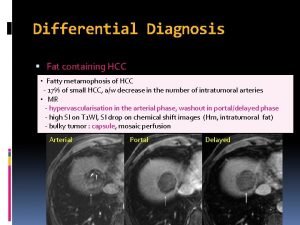
HCC Survillence NAFLD with cirrhosis: • Surveillance by abdominal ultrasound has a suboptimal performance in these patients, because of attenuation of ultrasound beam in bright liver, echostructural heterogeneity and focal fatty infiltration, leading to a high rate of underrecognition or misinterpretation of small nodules.

HCC Survillence • Recently a scoring system based on age, sex, smoking, physical activity, medical history of DM, aminotransferases and AFP identified almost all HCC cases detected by U/S in highrisk Taiwanese patients. The PNPLA 3 rs 738409 C>G gene polymorphism might provide patient-risk stratification, but it is not considered cost-effective yet.

HCC Survillence NAFLD without cirrhosis: • surveillance for HCC is deemed cost-effective if the expected risk of incident HCC exceeds a threshold of 1. 5% per year, but epidemiological studies remain inadequate. • In this specific subgroup, diagnosis of HCC should be established by liver biopsy
CONCLUSIONS • The growing burden of NAFLD related HCC is becoming a serious challenge for public health, in terms of surveillance and treatment.
CONCLUSIONS • We need more epidemiological and clinical data and a better understanding of the molecular events leading from obesity to NAFLD and HCC, particularly in patients without cirrhosis. This will enable the development of scoring algorithms and serological tests to stratify the risk of HCC in NAFLD patients.

THANK YOU
Prevention of HCC in NAFLD: what is possible? • The earlier the exposure to risk factors, the earlier the onset of malignancy, particularly on a genetically predisposed background. The casual association with other ‘‘superimposed hits”, such as viral infection, alcohol abuse or adenoma formation.
 Entrepreneur means “to undertake.” *
Entrepreneur means “to undertake.” * How do you undertake community scoping
How do you undertake community scoping Purpose of project proposal
Purpose of project proposal Bsbpmg522 assessment answers
Bsbpmg522 assessment answers What magnificent work does hrothgar undertake
What magnificent work does hrothgar undertake The ability to undertake strength performances quickly
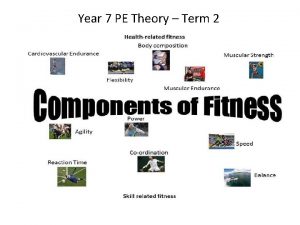
The ability to undertake strength performances quickly Fitt stands for
Fitt stands for Hcc hbv
Hcc hbv Hcc bclc
Hcc bclc Hcc genealogie
Hcc genealogie Oregon homecare registry
Oregon homecare registry Tace hcc
Tace hcc Hcc ybor bookstore
Hcc ybor bookstore Hcc coding cheat sheet
Hcc coding cheat sheet Hcc differential equations
Hcc differential equations Ibc portal hants
Ibc portal hants Interessante obligaties
Interessante obligaties Hcc recapture rate
Hcc recapture rate Gebouwinspectie met drone
Gebouwinspectie met drone Hcc middle college
Hcc middle college Saigon institute for techniques & technology
Saigon institute for techniques & technology Shumihito
Shumihito Oberfinanzdirektion frankfurt am main
Oberfinanzdirektion frankfurt am main Hcc differential equations
Hcc differential equations Hawkmail hcc
Hawkmail hcc Standardavvikelse formel
Standardavvikelse formel