Inflammation and Cancer Puangrat Yongvanit Inflammation and cancer


- Slides: 39
Inflammation and Cancer Puangrat Yongvanit
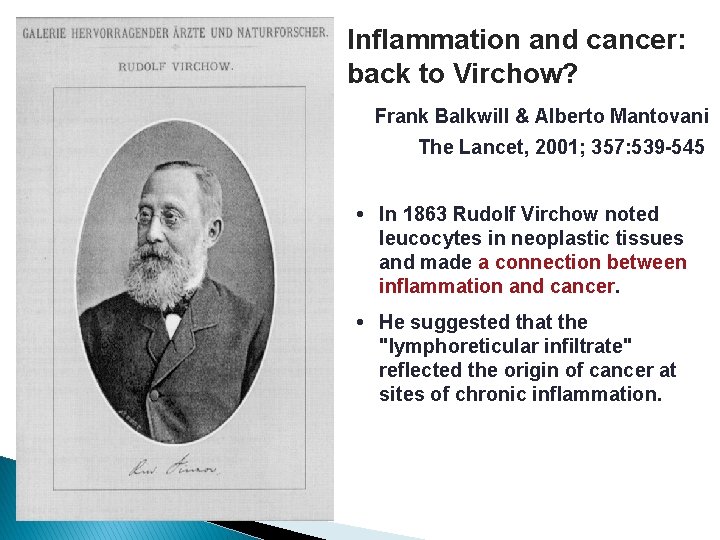
Inflammation and cancer: back to Virchow? Frank Balkwill & Alberto Mantovani The Lancet, 2001; 357: 539 -545 • In 1863 Rudolf Virchow noted leucocytes in neoplastic tissues and made a connection between inflammation and cancer. • He suggested that the "lymphoreticular infiltrate" reflected the origin of cancer at sites of chronic inflammation.
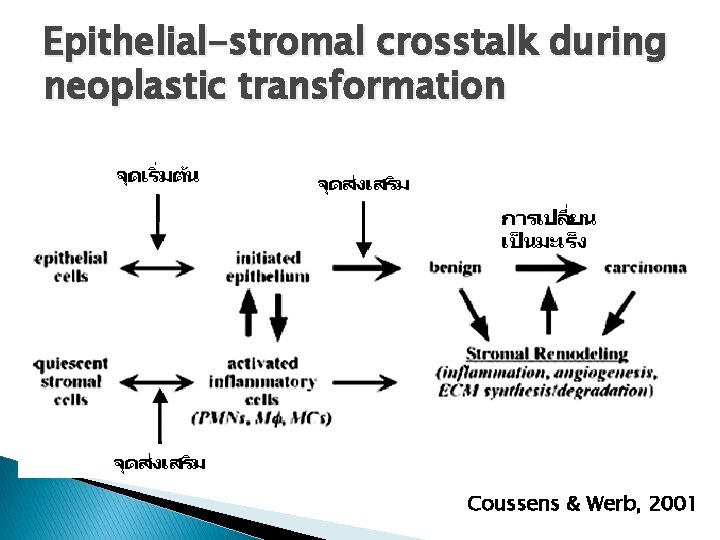
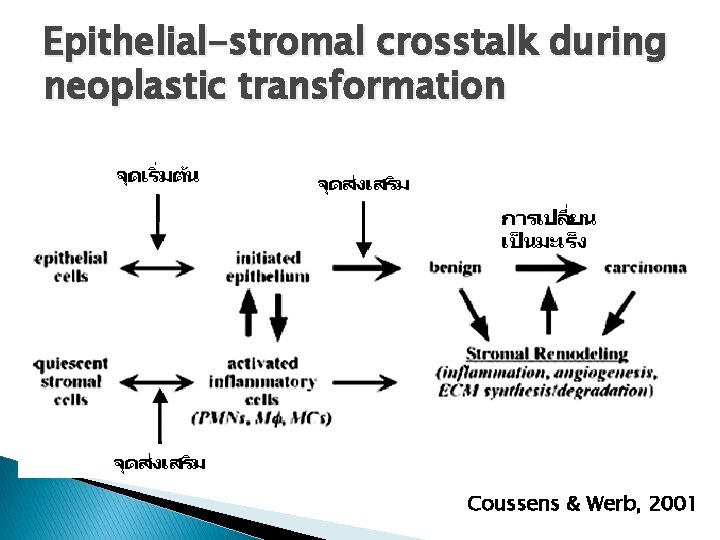
Epithelial-stromal crosstalk during neoplastic transformation Coussens & Werb, 2001
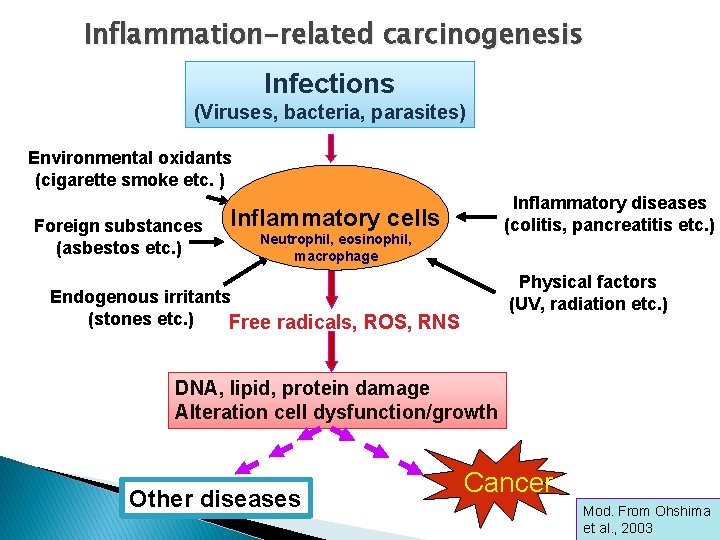
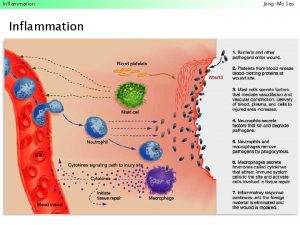
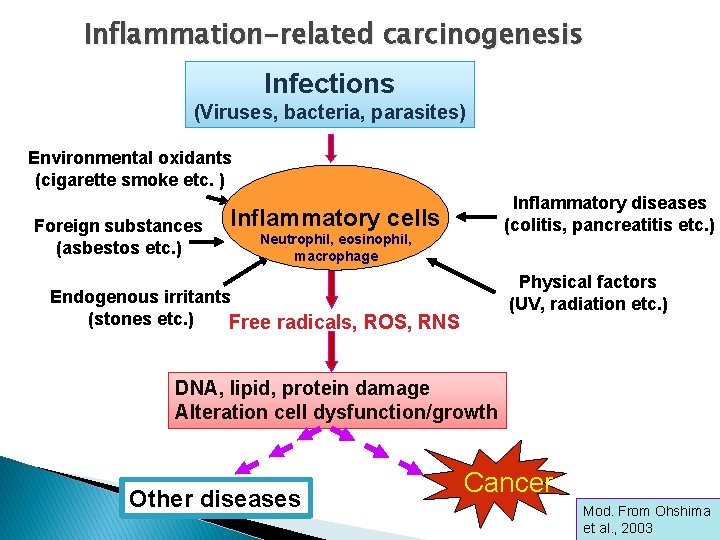
Inflammation-related carcinogenesis Infections (Viruses, bacteria, parasites) Environmental oxidants (cigarette smoke etc. ) Foreign substances (asbestos etc. ) Inflammatory diseases (colitis, pancreatitis etc. ) Inflammatory cells Neutrophil, eosinophil, macrophage Physical factors (UV, radiation etc. ) Endogenous irritants (stones etc. ) Free radicals, ROS, RNS DNA, lipid, protein damage Alteration cell dysfunction/growth Other diseases Cancer Mod. From Ohshima et al. , 2003
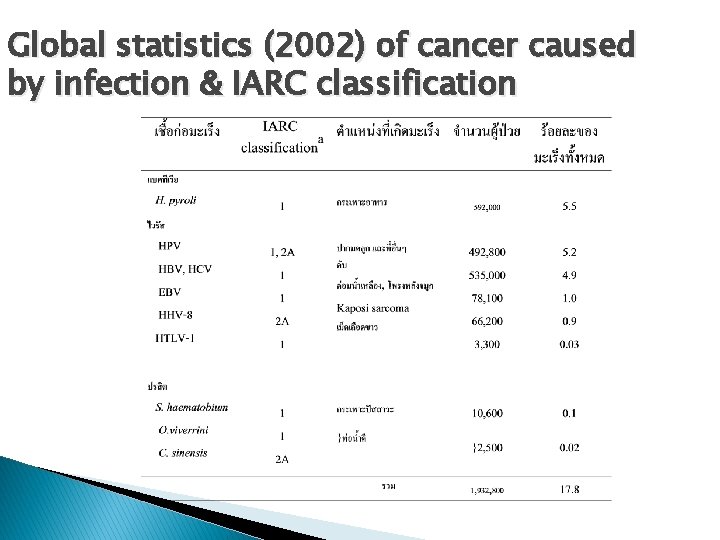
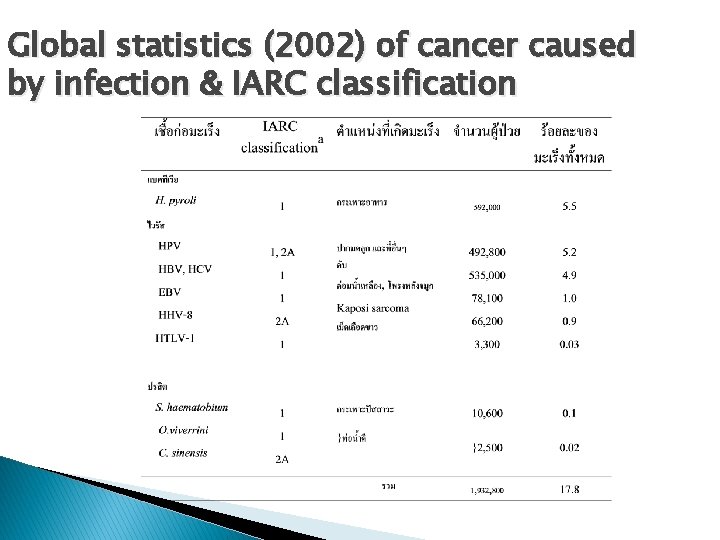
Global statistics (2002) of cancer caused by infection & IARC classification

Proposed main mehanism for infection-associated carcinogenesis � Direct action of infectious agents: insertion, delesion, translocation, amplification of viral DNA into host cells : E 6, E 7 of HPV � Immunosuppression � Production : Kaposi’s sarcoma of reactive O 2 & N 2 species (ROS & RNS) : Prolonged activation of inflammed cells generates ROS & RNS that can damage host DNA
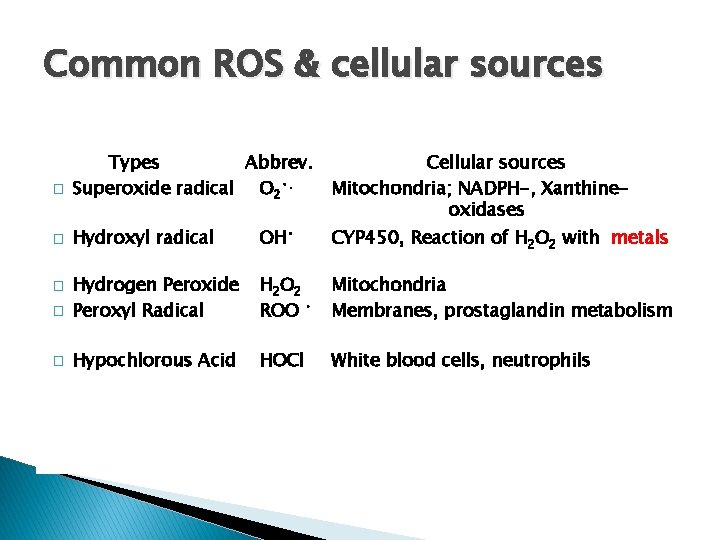
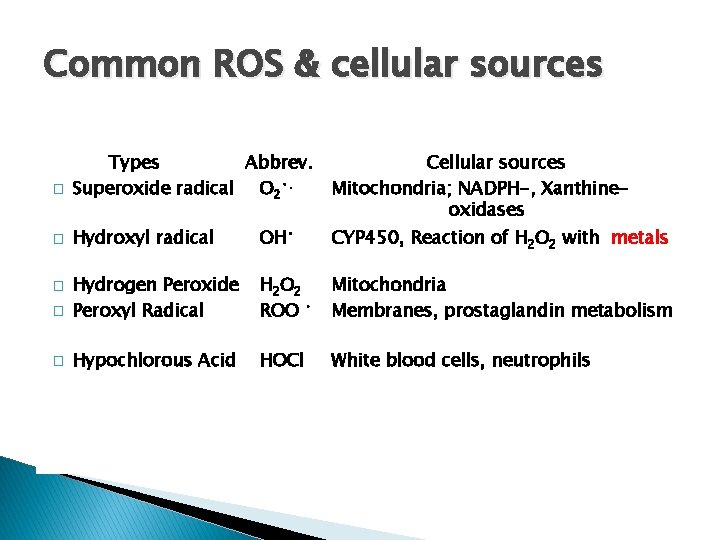
Common ROS & cellular sources � Types Abbrev. Superoxide radical O 2 • . Cellular sources Mitochondria; NADPH-, Xanthineoxidases Hydroxyl radical OH • � Hydrogen Peroxide Peroxyl Radical H 2 O 2 ROO • Mitochondria Membranes, prostaglandin metabolism � Hypochlorous Acid HOCl White blood cells, neutrophils � � CYP 450, Reaction of H 2 O 2 with metals
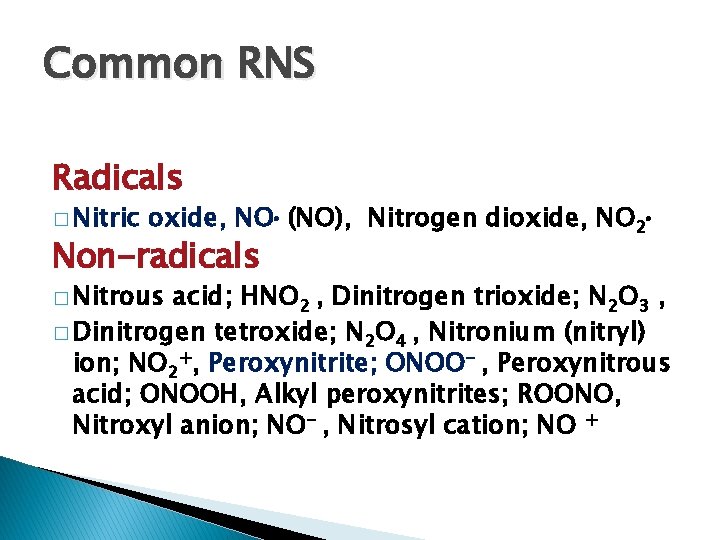
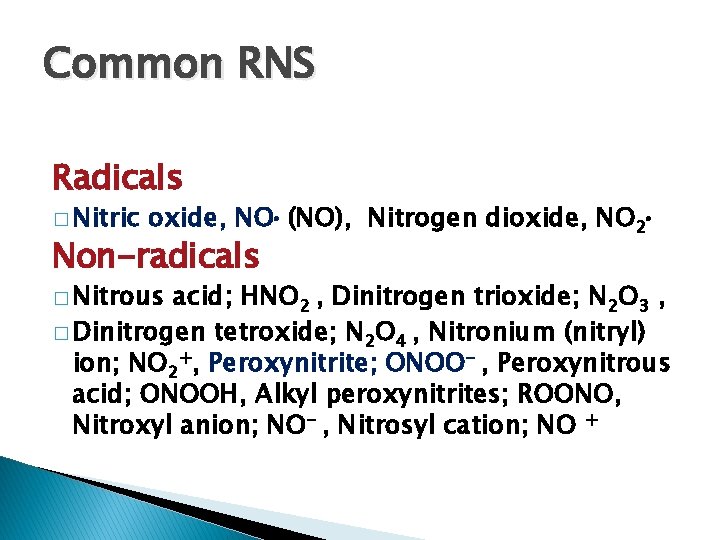
Common RNS Radicals � Nitric oxide, NO (NO), Nitrogen dioxide, NO 2 Non-radicals � Nitrous acid; HNO 2 , Dinitrogen trioxide; N 2 O 3 , � Dinitrogen tetroxide; N 2 O 4 , Nitronium (nitryl) ion; NO 2+, Peroxynitrite; ONOO- , Peroxynitrous acid; ONOOH, Alkyl peroxynitrites; ROONO, Nitroxyl anion; NO- , Nitrosyl cation; NO +
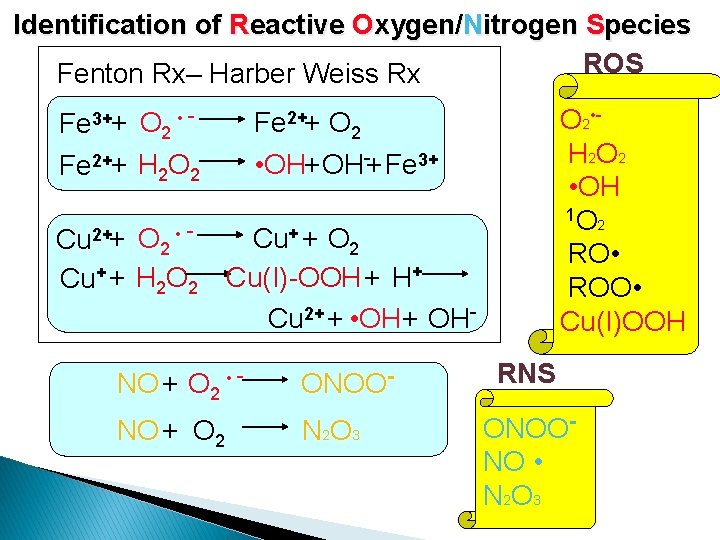
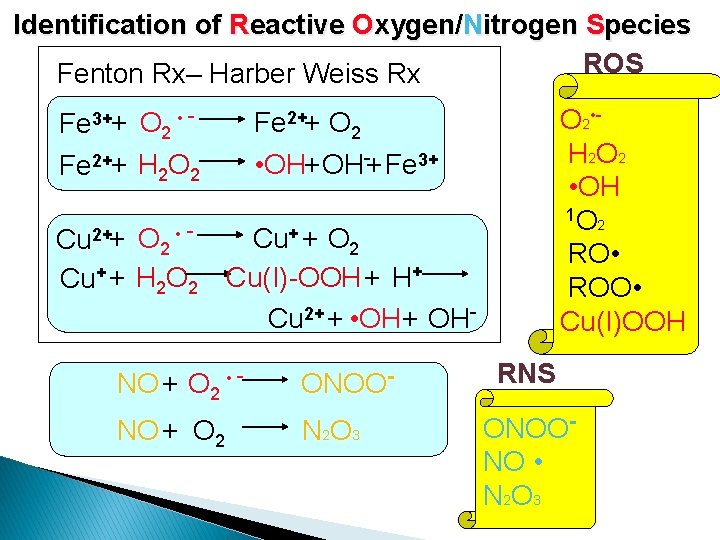
Identification of Reactive Oxygen/Nitrogen Species ROS Fenton Rx– Harber Weiss Rx Fe 3++ O 2 • Fe 2++ H 2 O 2 Cu 2++ O 2 • Cu+ + H 2 O 2 • OH 1 O 2 RO • ROO • Cu(I)OOH Fe 2++ O 2 • OH+ OH-+ Fe 3+ Cu+ + O 2 Cu(I)-OOH+ H+ Cu 2+ + • OH+ OH- NO + O 2 • - ONOO- NO + O 2 N 2 O 3 RNS ONOONO • N 2 O 3
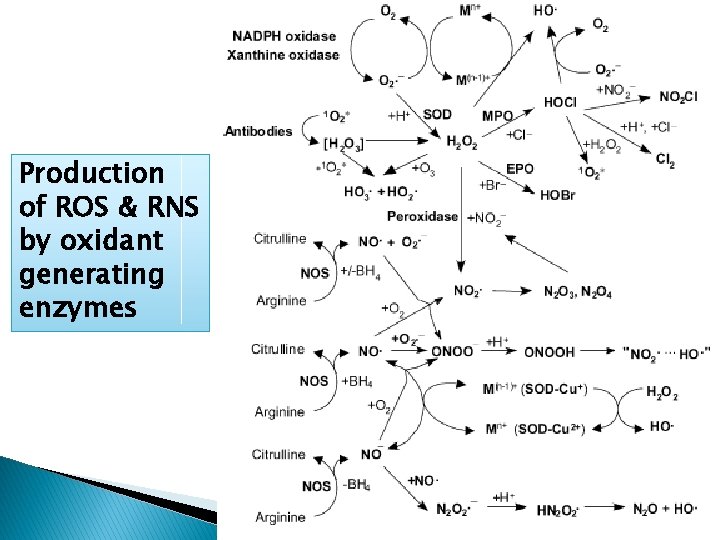
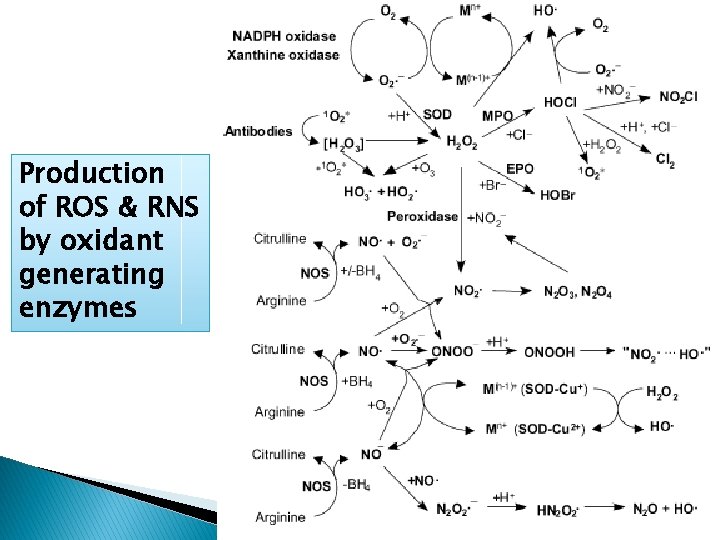
Production of ROS & RNS by oxidant generating enzymes
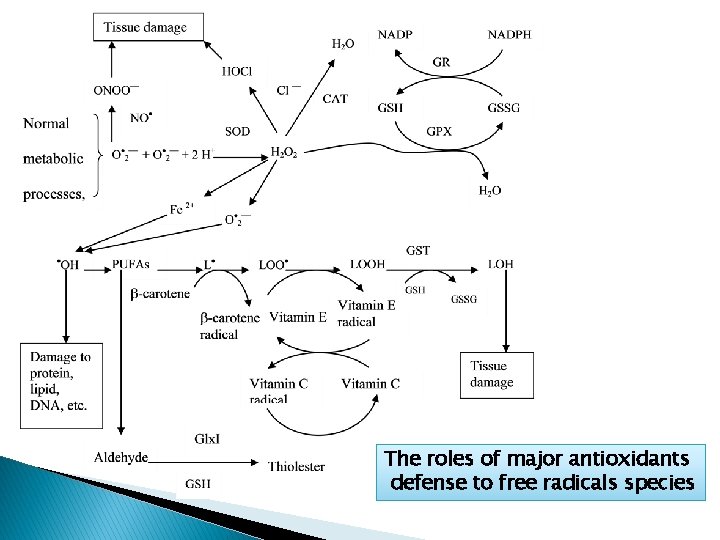
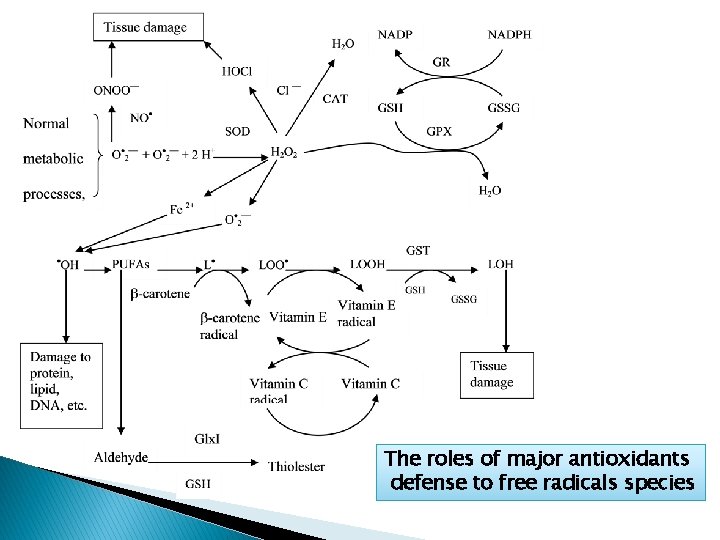
The roles of major antioxidants defense to free radicals species
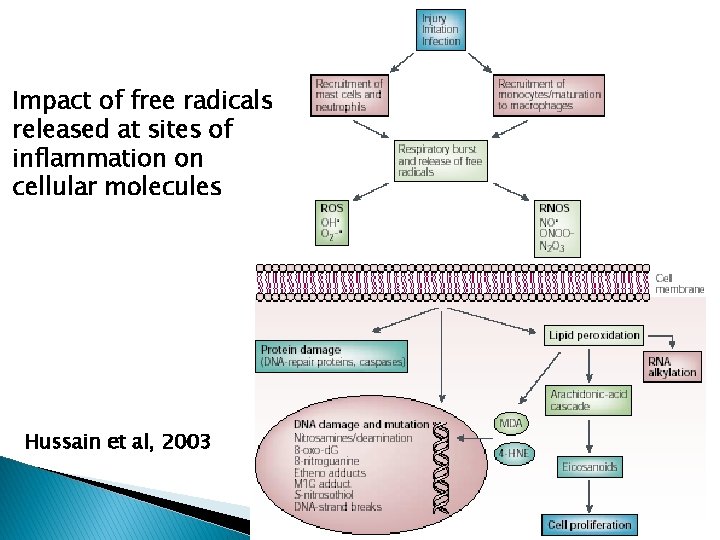
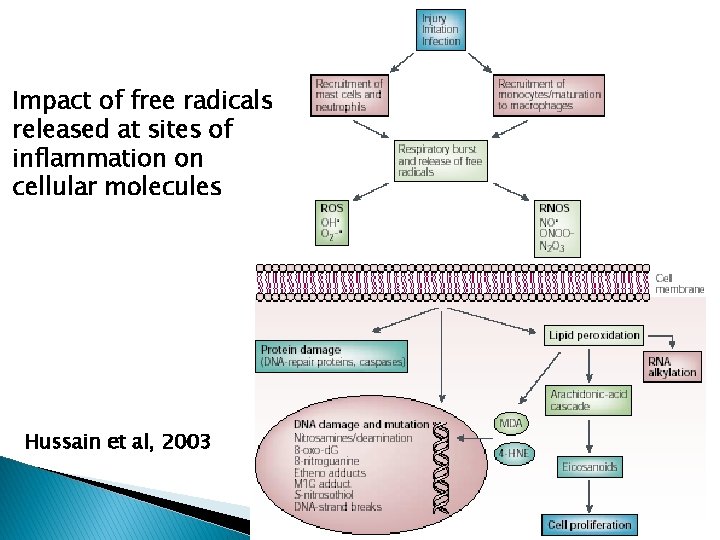
Impact of free radicals released at sites of inflammation on cellular molecules Hussain et al, 2003
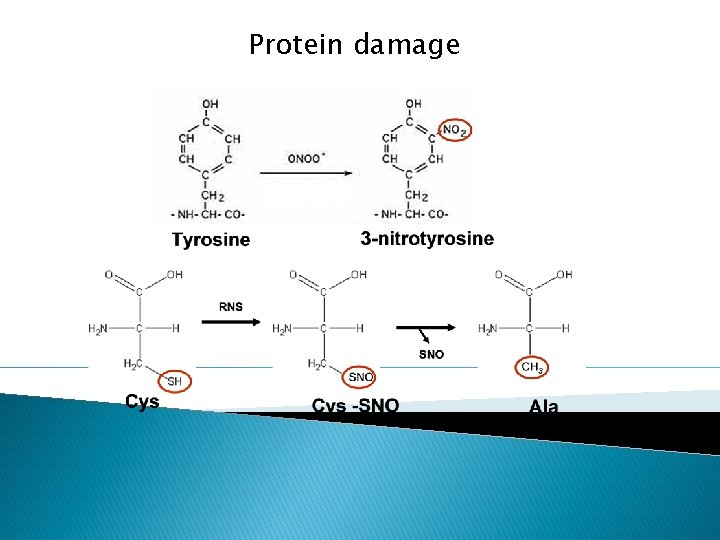
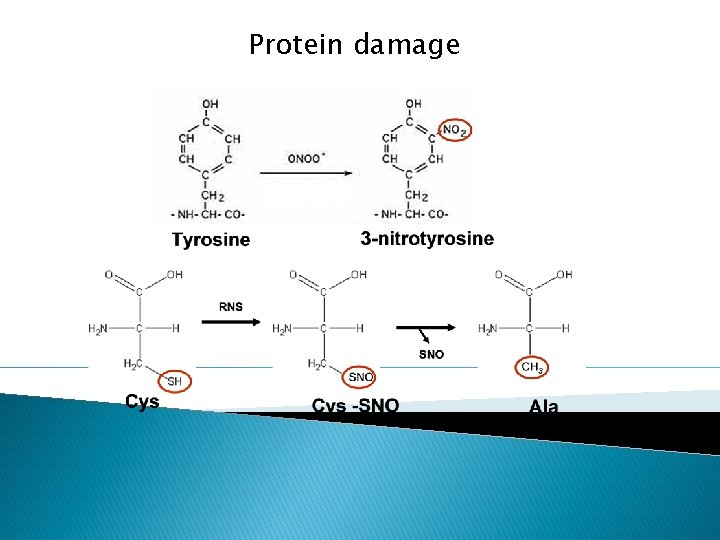
Protein damage
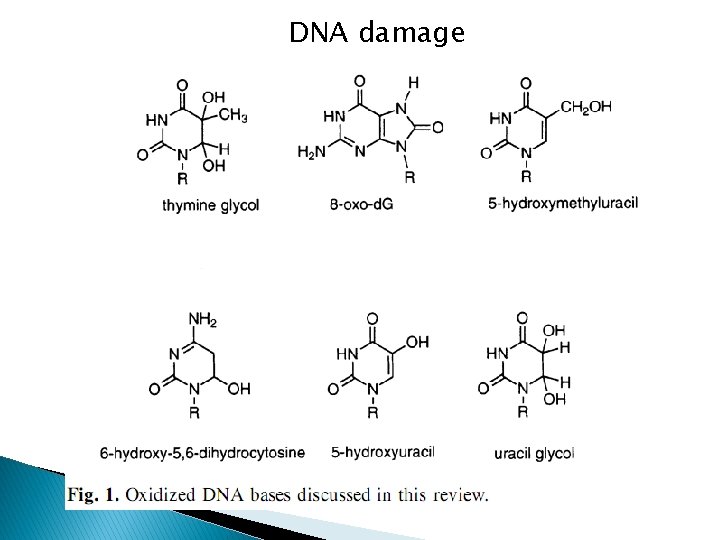
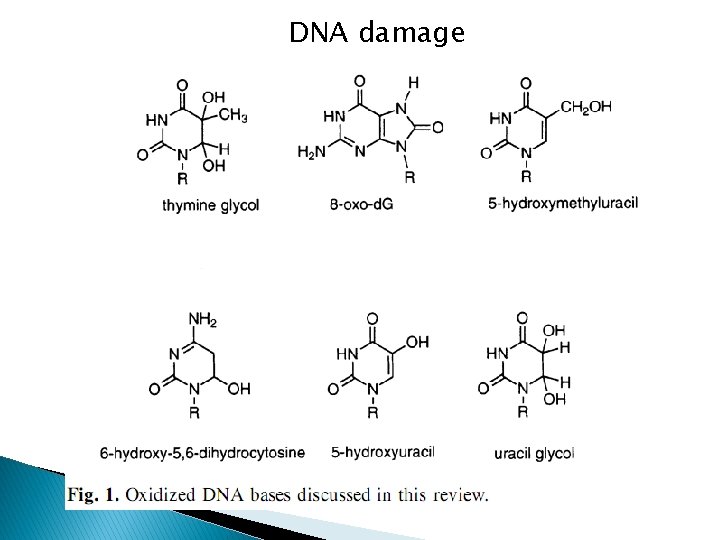
DNA damage
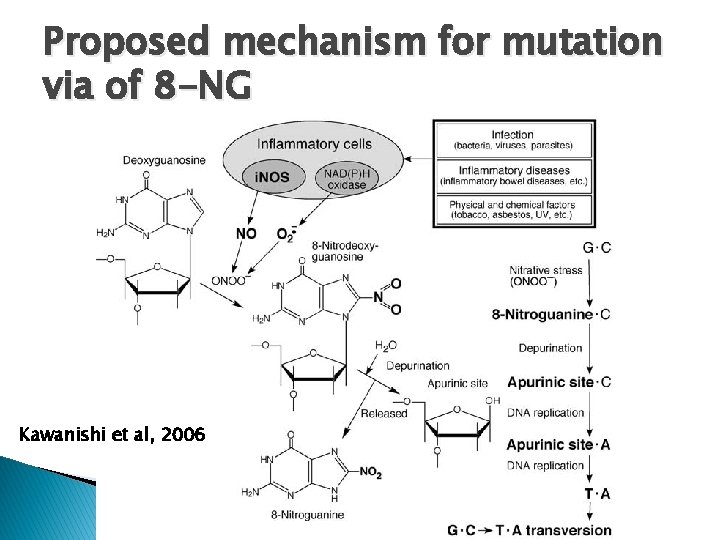
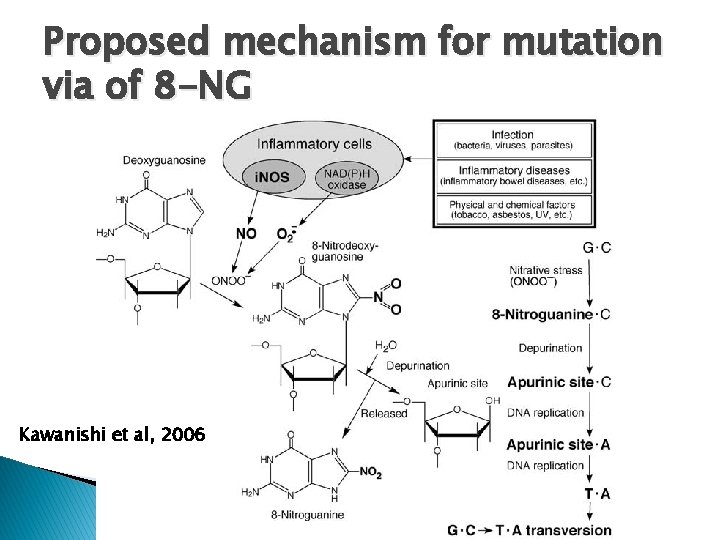
Proposed mechanism for mutation via of 8 -NG Kawanishi et al, 2006
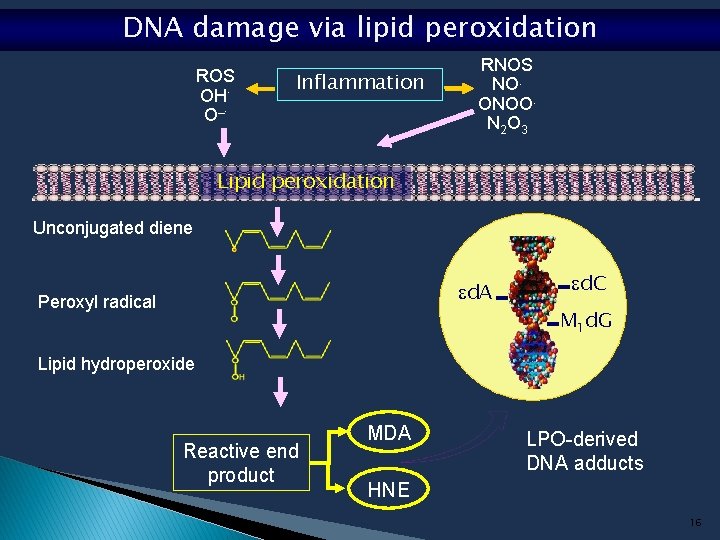
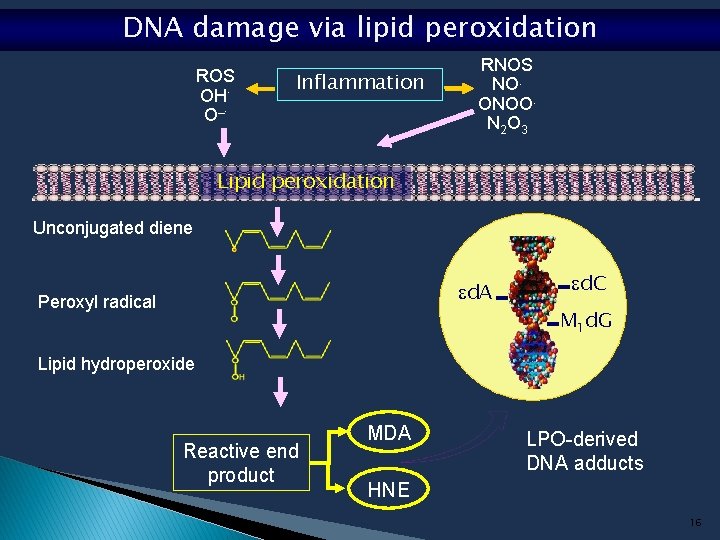
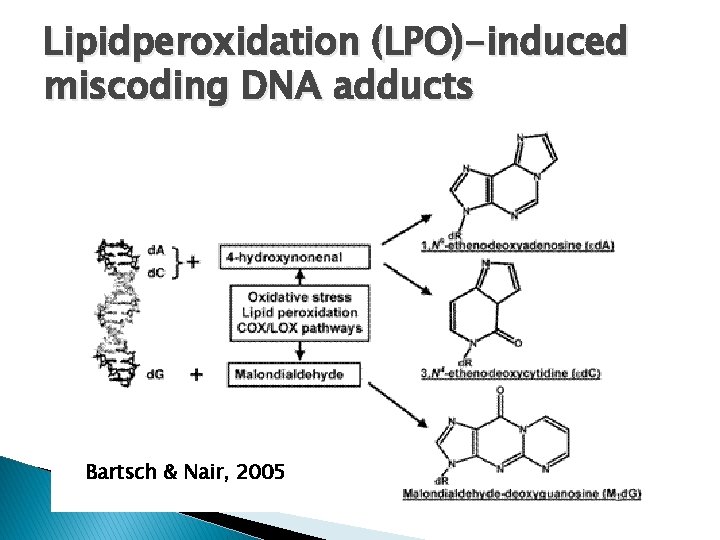
DNA damage via lipid peroxidation ROS OH. O_. Inflammation RNOS NO. ONOO. N 2 O 3 Lipid peroxidation Unconjugated diene d. A Peroxyl radical d. C M 1 d. G Lipid hydroperoxide Reactive end product MDA LPO-derived DNA adducts HNE 16
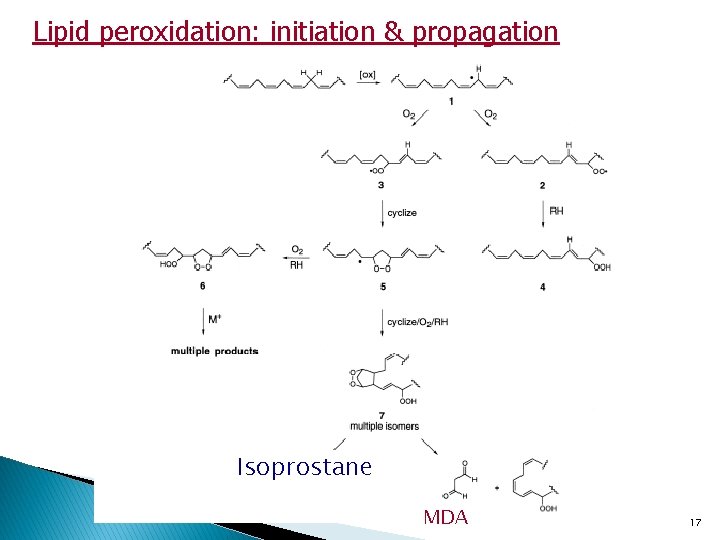
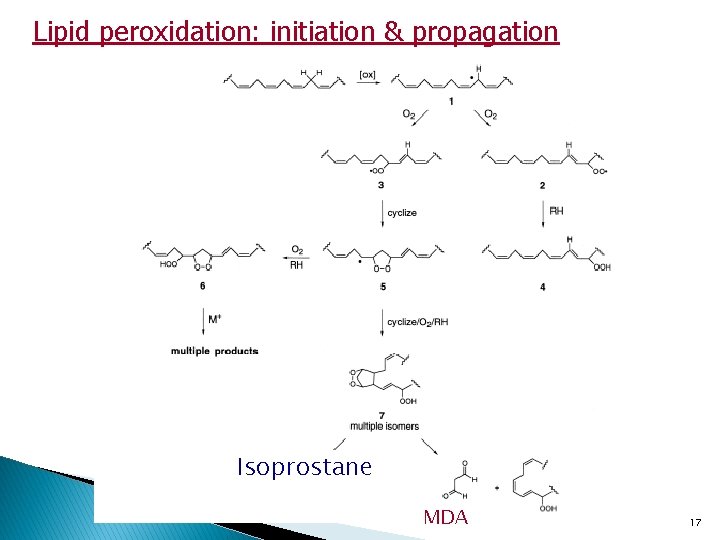
Lipid peroxidation: initiation & propagation Isoprostane MDA 17
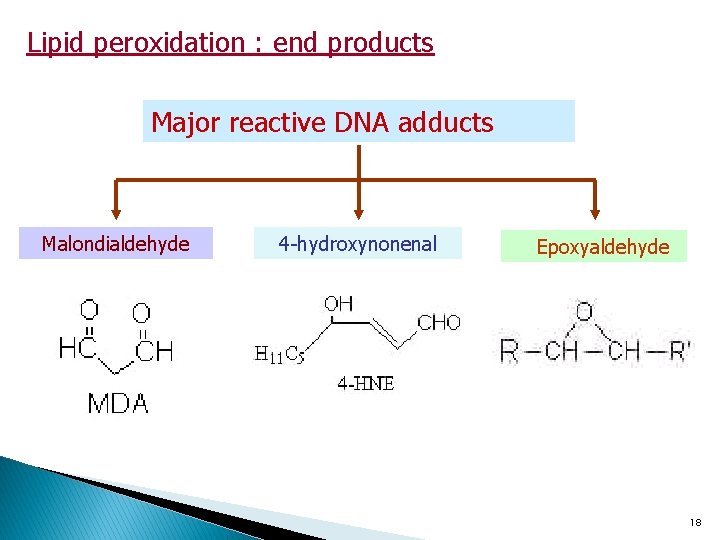
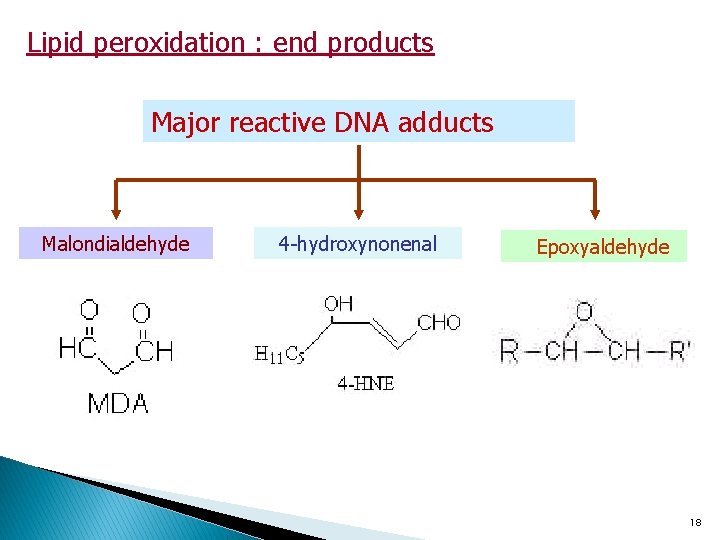
Lipid peroxidation : end products Major reactive DNA adducts Malondialdehyde 4 -hydroxynonenal Epoxyaldehyde 18
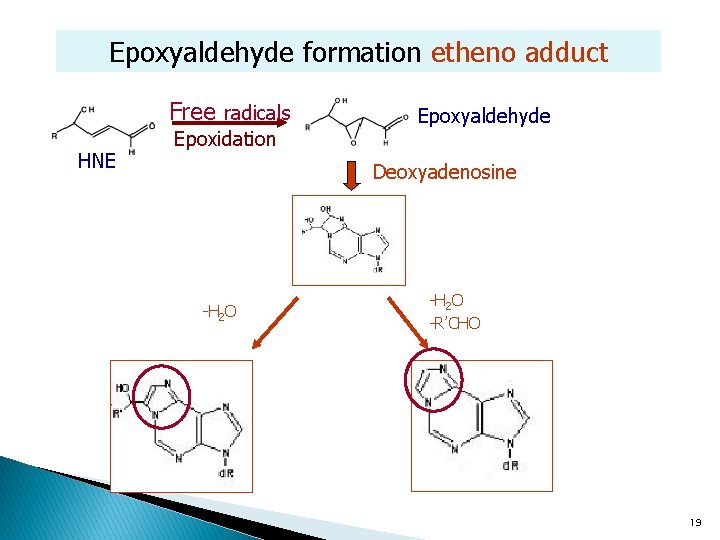
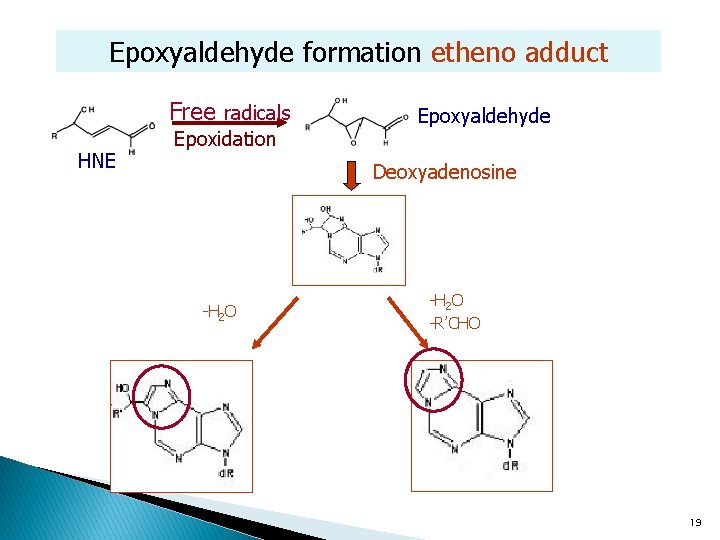
Epoxyaldehyde formation etheno adduct Free radicals HNE Epoxidation Epoxyaldehyde Deoxyadenosine -H 2 O -R’CHO d. A 19
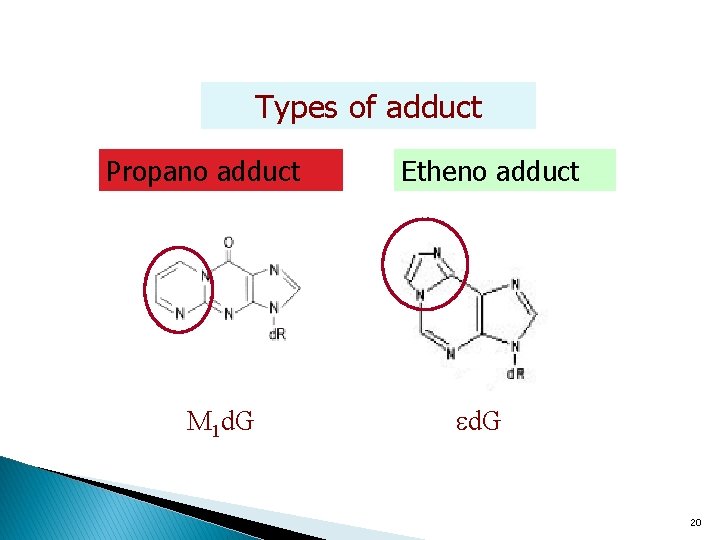
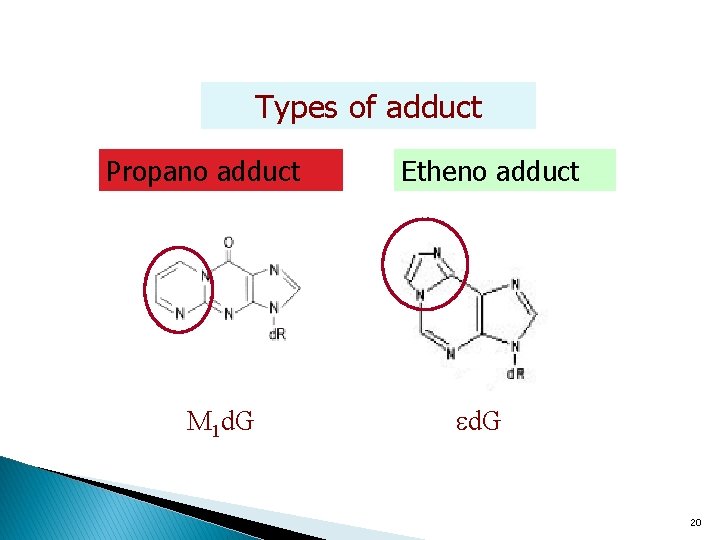
Types of adduct Propano adduct M 1 d. G Etheno adduct d. G 20
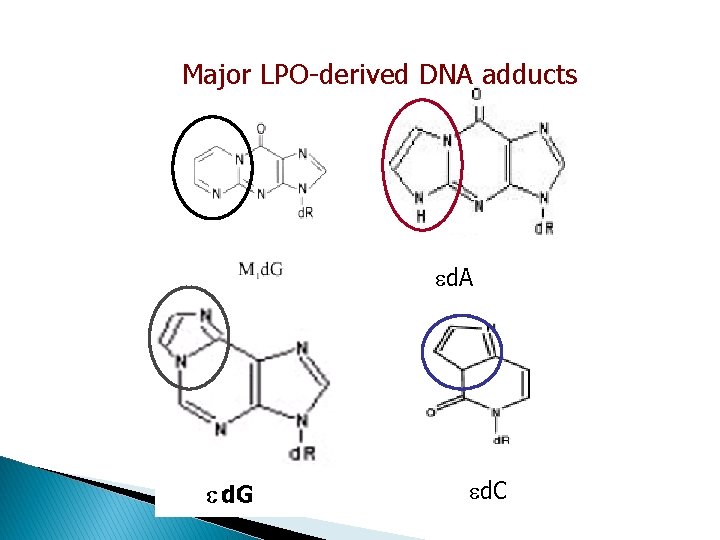
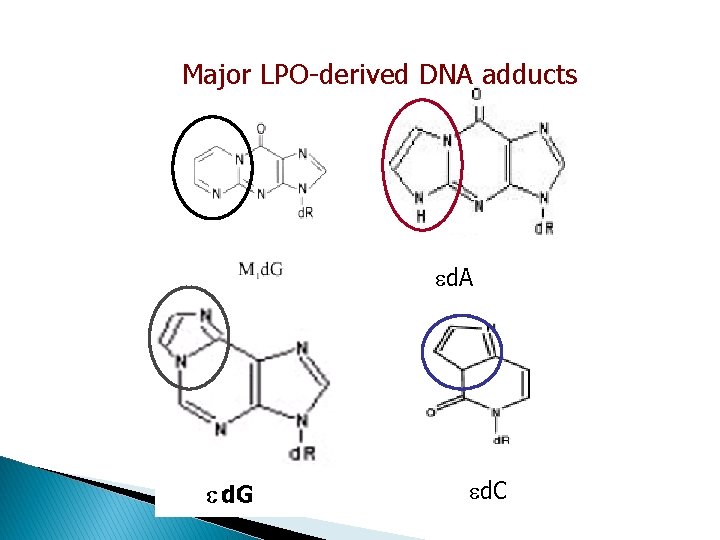
Major LPO-derived DNA adducts d. A d. C
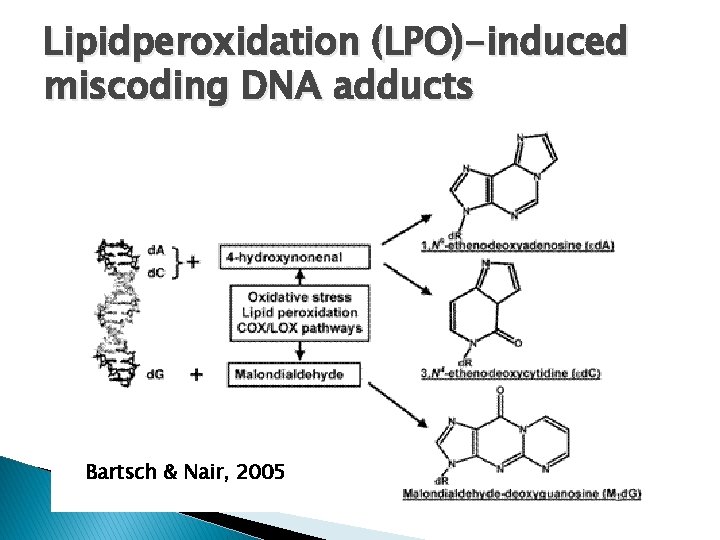
Lipidperoxidation (LPO)-induced miscoding DNA adducts Bartsch & Nair, 2005
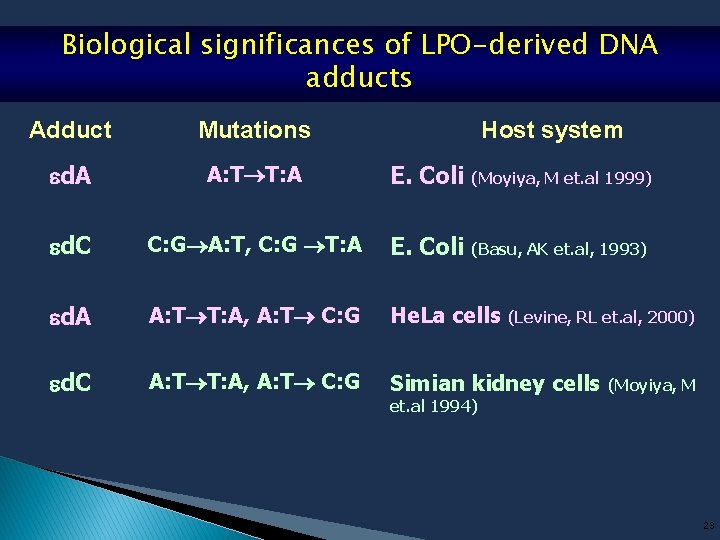
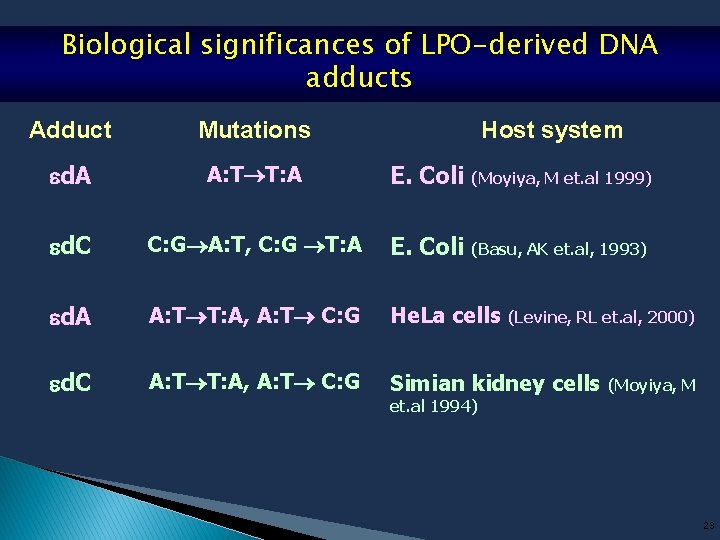
Biological significances of LPO-derived DNA adducts Adduct Mutations Host system d. A A: T T: A E. Coli (Moyiya, M et. al 1999) d. C C: G A: T, C: G T: A E. Coli (Basu, AK et. al, 1993) d. A A: T T: A, A: T C: G He. La cells (Levine, RL et. al, 2000) d. C A: T T: A, A: T C: G Simian kidney cells (Moyiya, M et. al 1994) 23
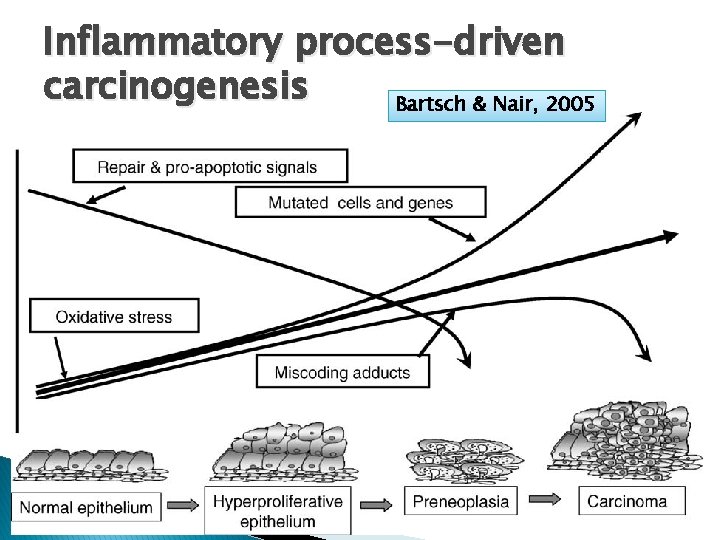
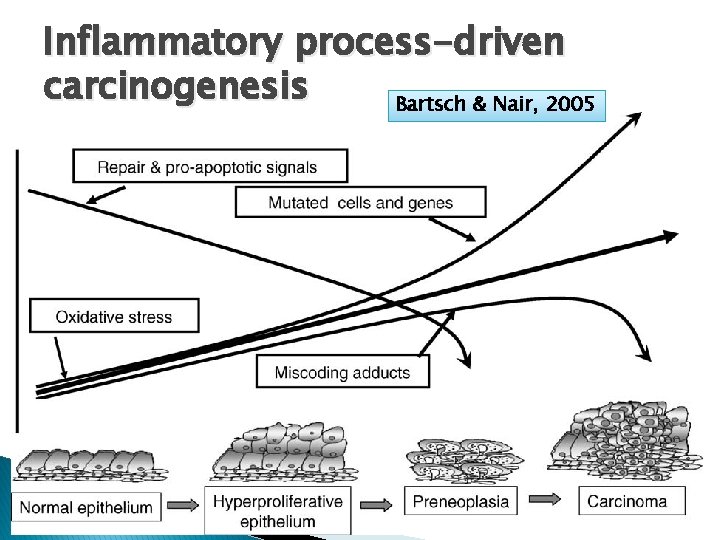
Inflammatory process-driven carcinogenesis Bartsch & Nair, 2005
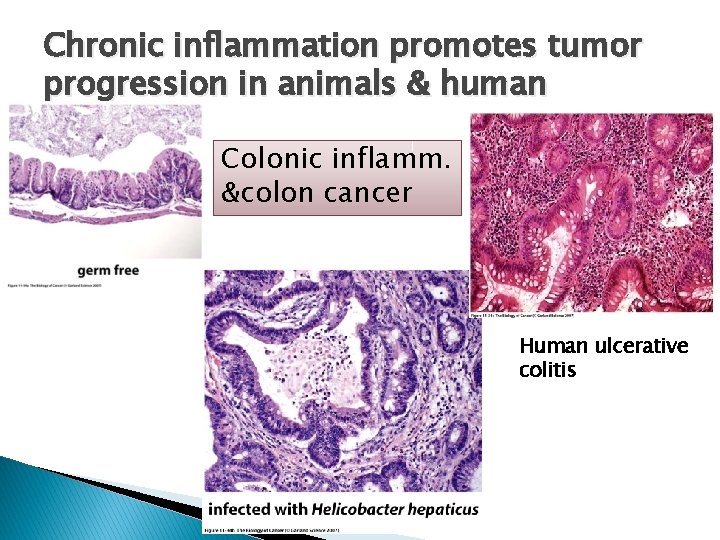
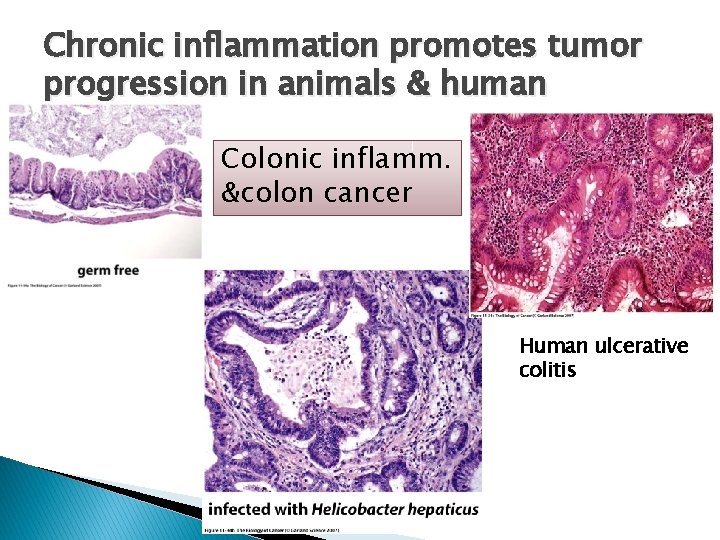
Chronic inflammation promotes tumor progression in animals & human Colonic inflamm. &colon cancer Human ulcerative colitis
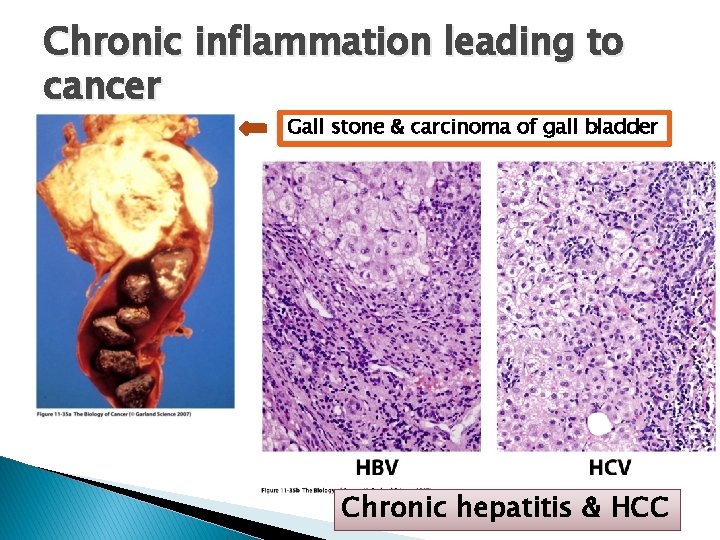
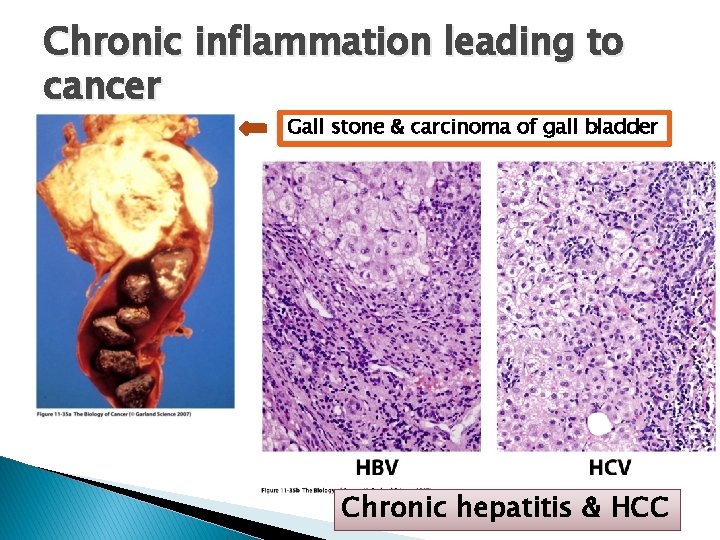
Chronic inflammation leading to cancer Gall stone & carcinoma of gall bladder Chronic hepatitis & HCC
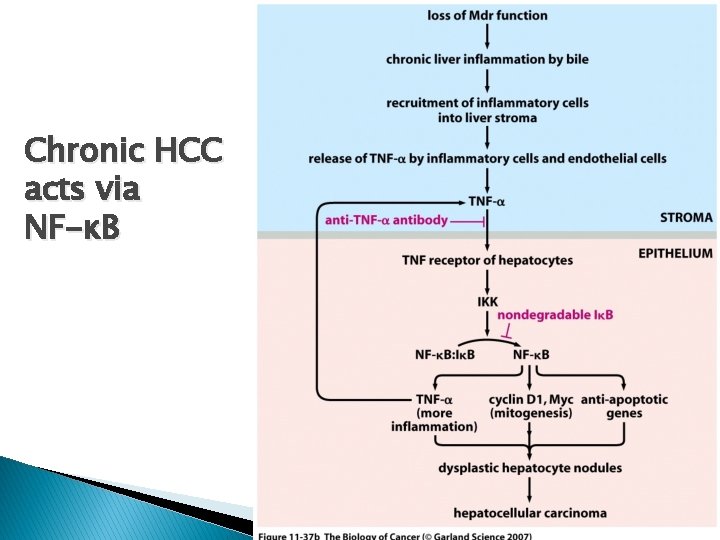
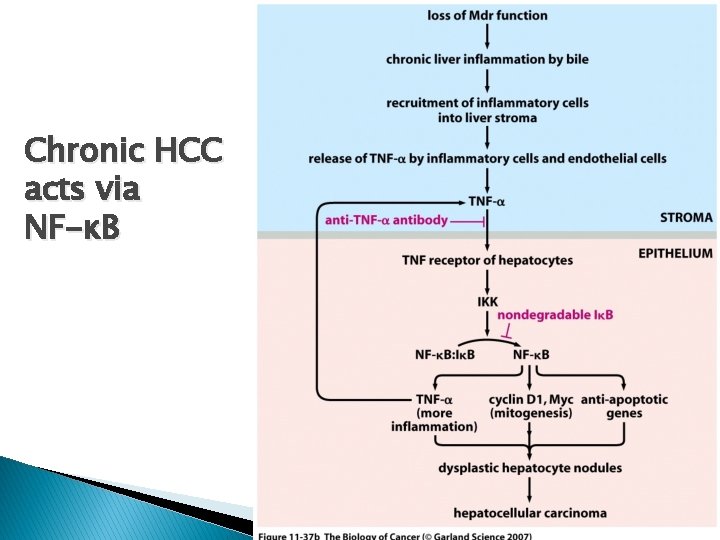
Chronic HCC acts via NF-κB
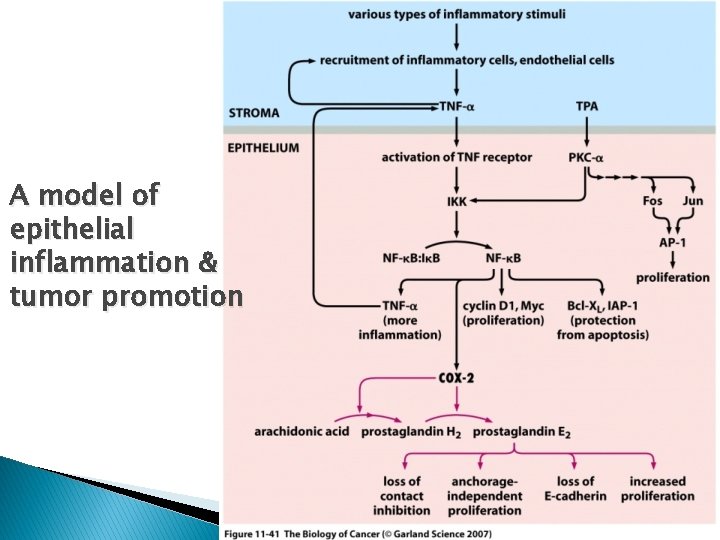
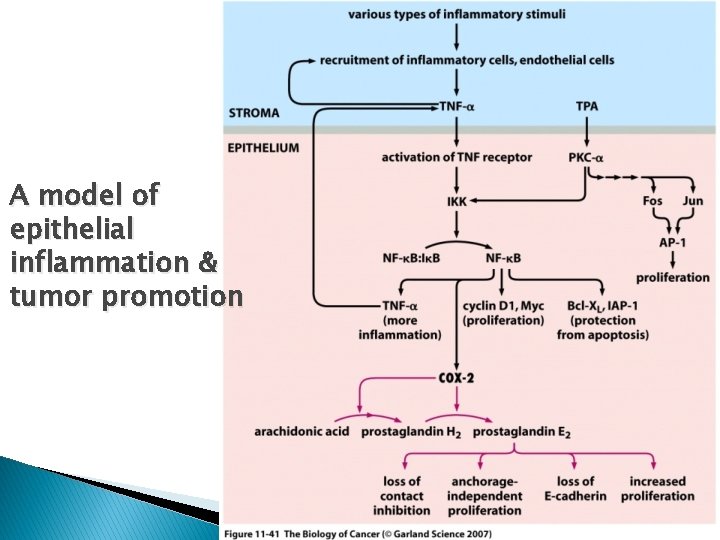
A model of epithelial inflammation & tumor promotion
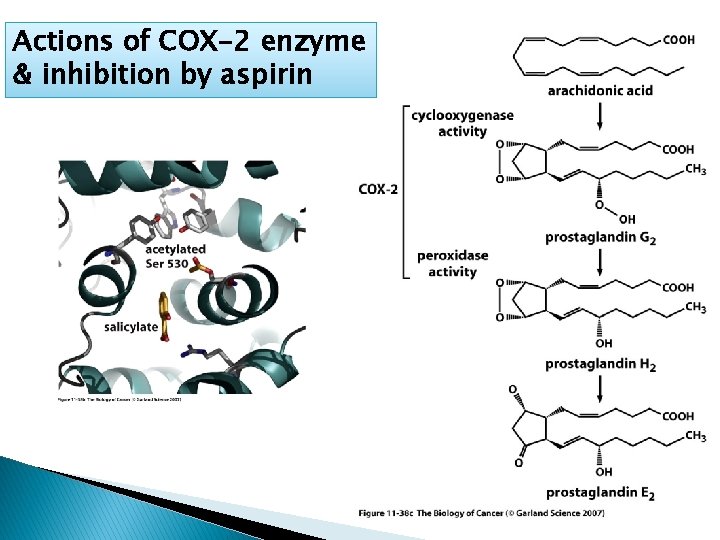
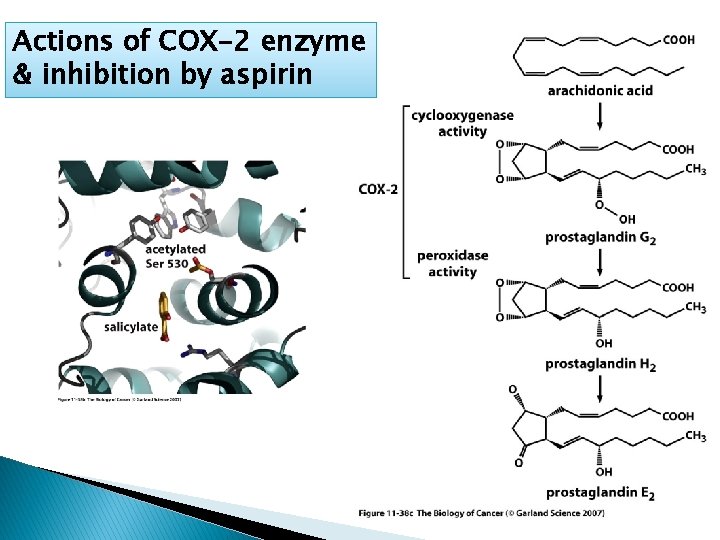
Actions of COX-2 enzyme & inhibition by aspirin
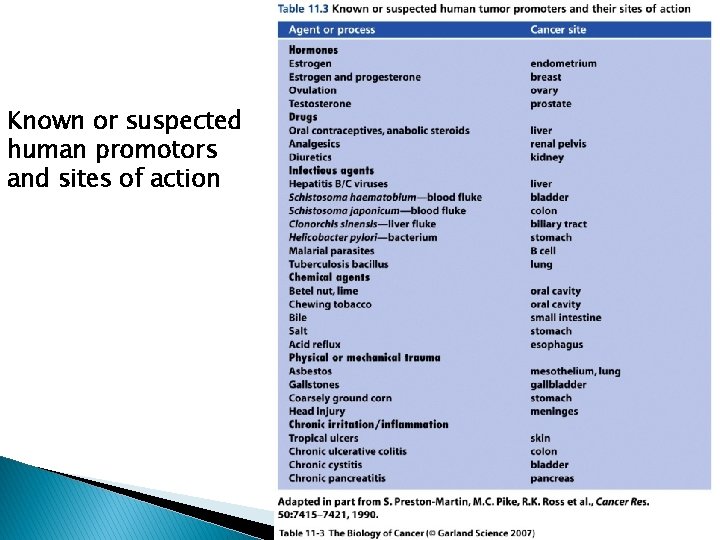
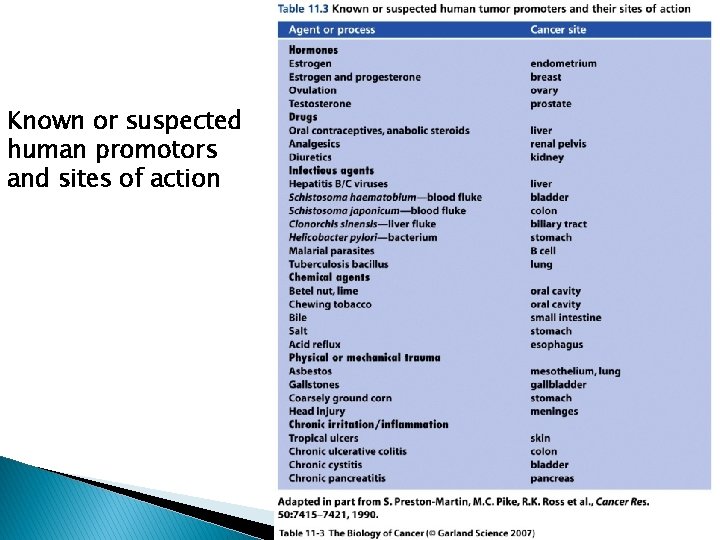
Known or suspected human promotors and sites of action
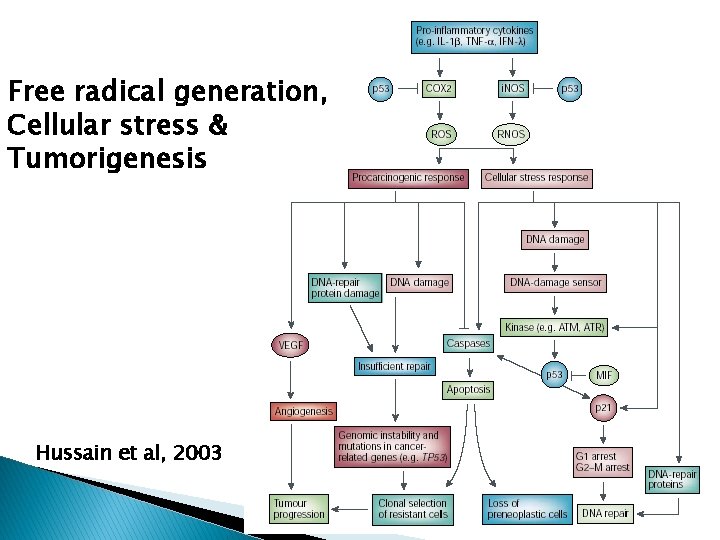
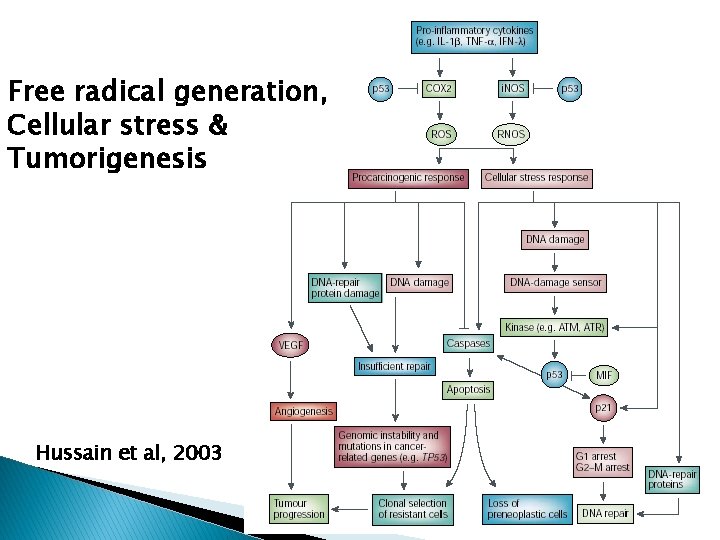
Free radical generation, Cellular stress & Tumorigenesis Hussain et al, 2003
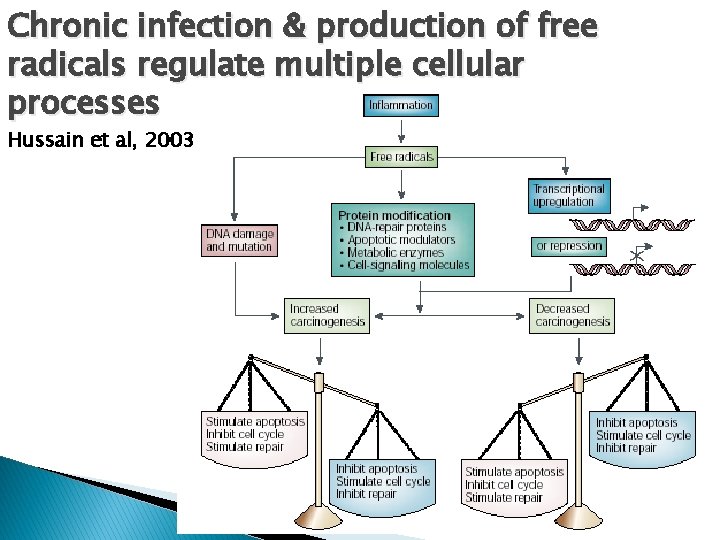
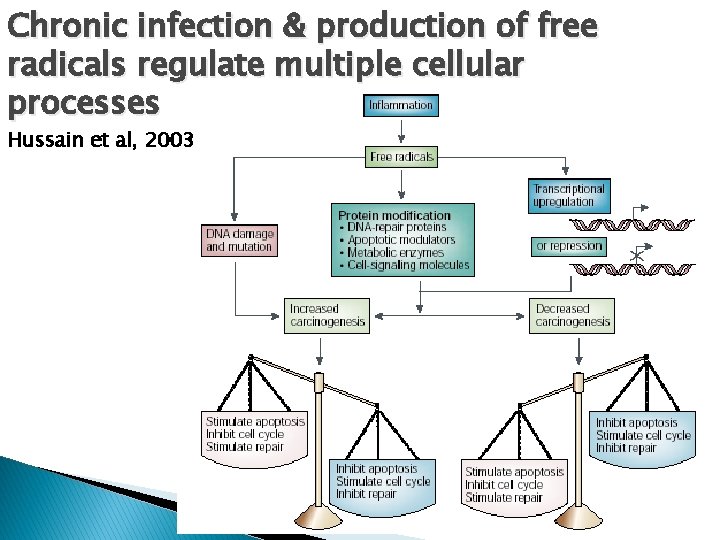
Chronic infection & production of free radicals regulate multiple cellular processes Hussain et al, 2003
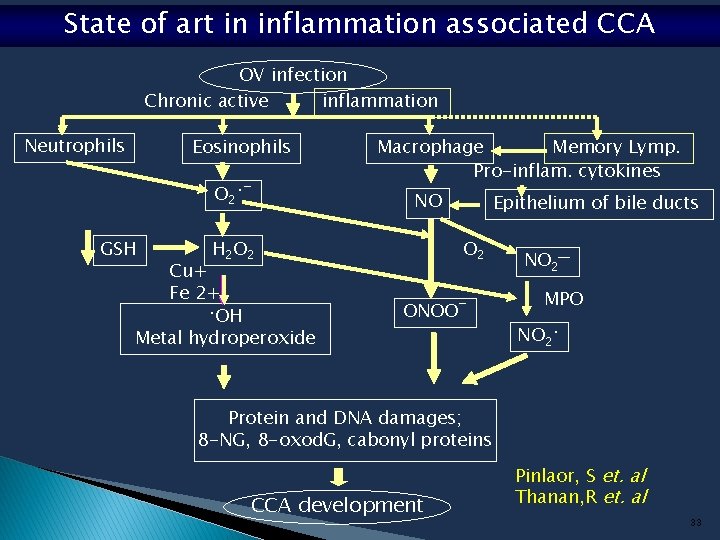
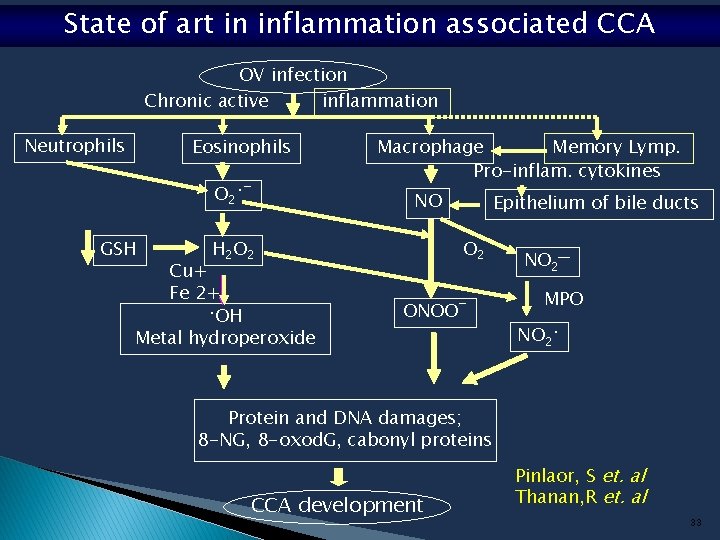
State of art in inflammation associated CCA OV infection Chronic active inflammation Neutrophils Eosinophils O 2 • ¯ GSH Macrophage Memory Lymp. Pro-inflam. cytokines NO H 2 O 2 Cu+ Fe 2+ • OH Metal hydroperoxide Epithelium of bile ducts O 2 ONOO¯ NO 2─ MPO NO 2 • Protein and DNA damages; 8 -NG, 8 -oxod. G, cabonyl proteins CCA development Pinlaor, S et. al Thanan, R et. al 33
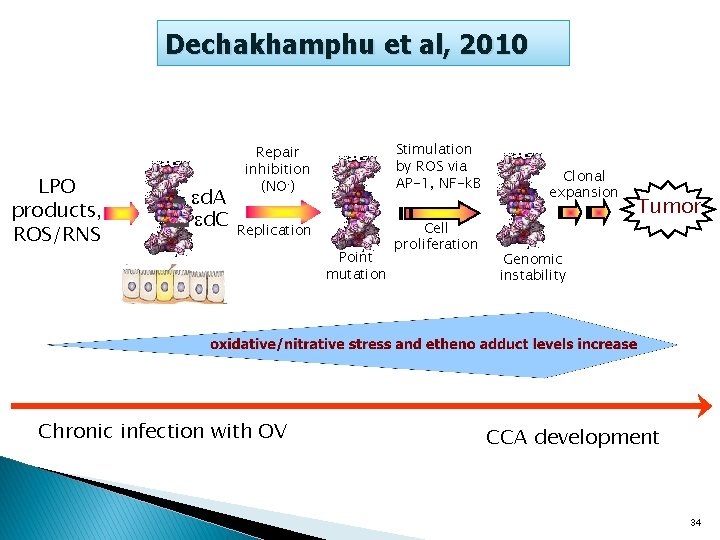
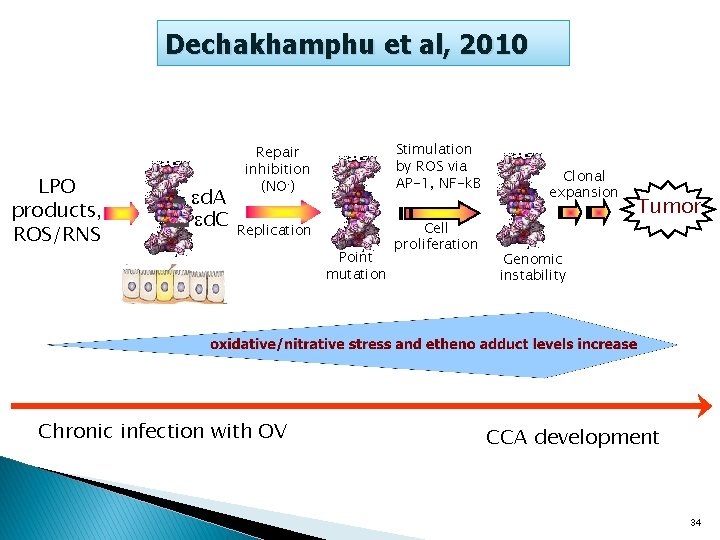
Dechakhamphu et al, 2010 LPO products, ROS/RNS d. A d. C Repair inhibition (NO. ) Stimulation by ROS via AP-1, NF-k. B Replication Cell proliferation Chronic infection with OV Point mutation Clonal expansion Tumor Genomic instability CCA development 34

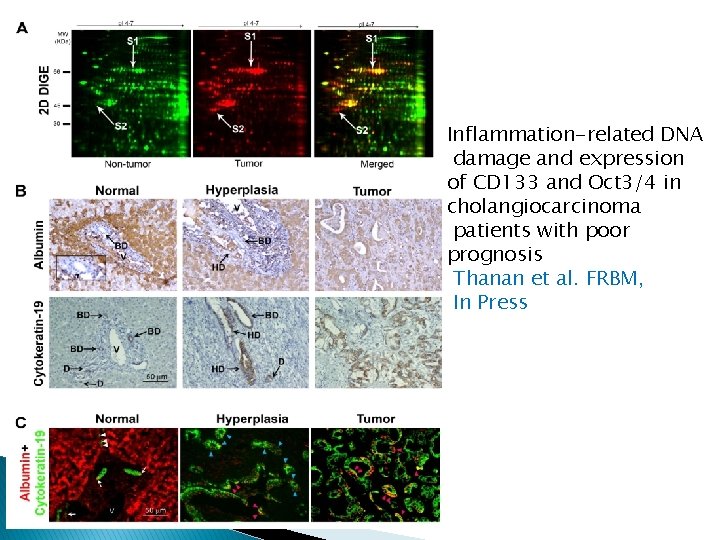
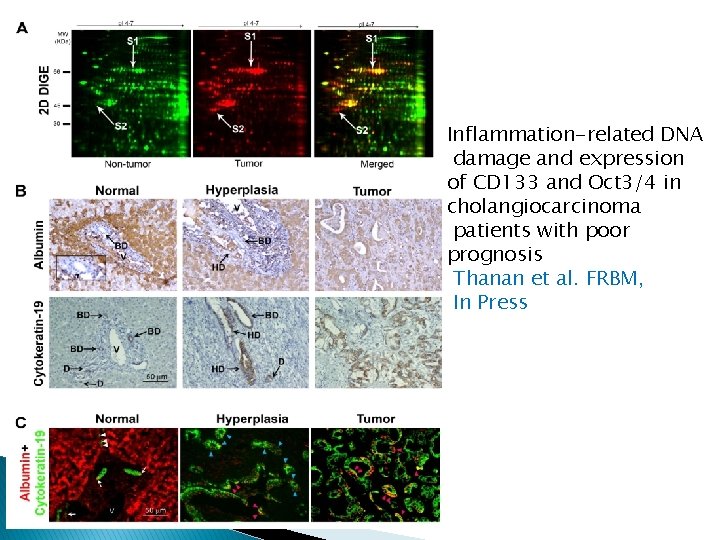
Inflammation-related DNA damage and expression of CD 133 and Oct 3/4 in cholangiocarcinoma patients with poor prognosis Thanan et al. FRBM, In Press
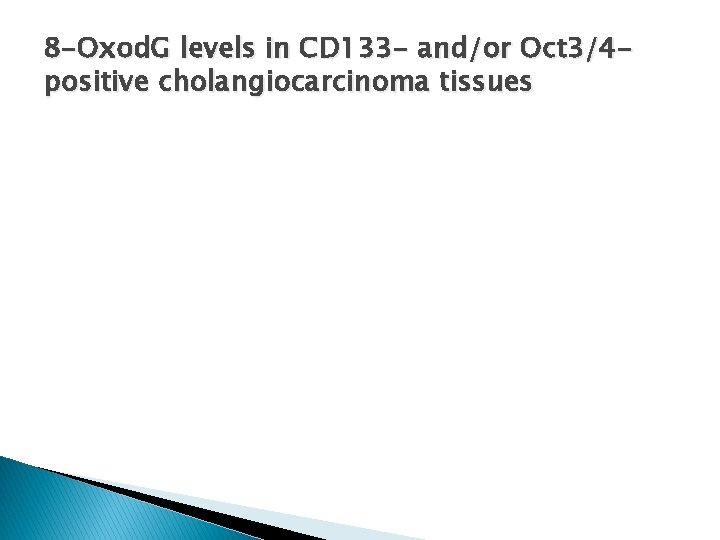
8 -Oxod. G levels in CD 133 - and/or Oct 3/4 positive cholangiocarcinoma tissues
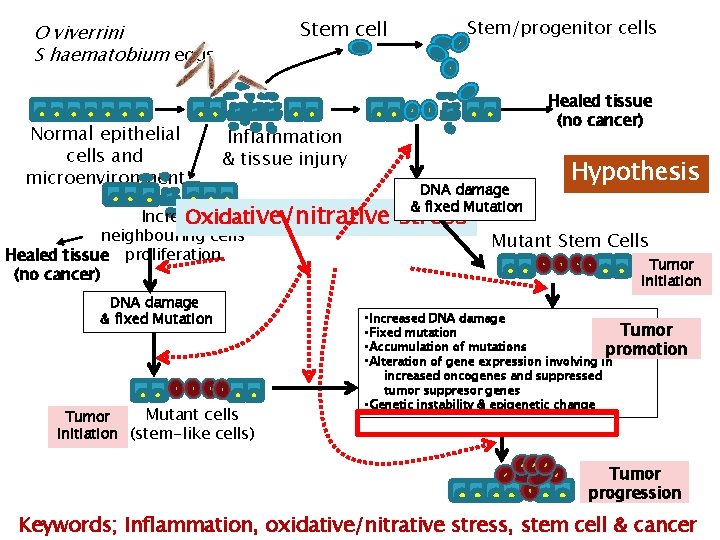
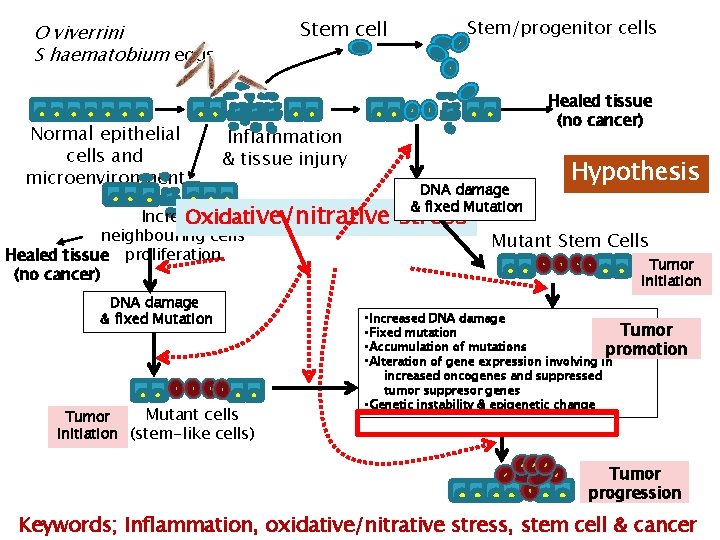
Stem cell O viverrini S haematobium eggs Normal epithelial cells and microenvironment Stem/progenitor cells Healed tissue (no cancer) Inflammation & tissue injury Increase Oxidative/nitrative neighbouring cells Healed tissue proliferation (no cancer) DNA damage & fixed Mutation Mutant cells Tumor initiation (stem-like cells) DNA damage & fixed Mutation stress Hypothesis Mutant Stem Cells Tumor initiation • Increased DNA damage Tumor • Fixed mutation • Accumulation of mutations promotion • Alteration of gene expression involving in increased oncogenes and suppressed tumor suppresor genes • Genetic instability & epigenetic change Tumor progression Keywords; Inflammation, oxidative/nitrative stress, stem cell & cancer
Key references �Weinberg, RA. The Biology of Cancer (2007), Garland Science, Taylor & Francis Group, NY. Chapters 11 �Bartsch & Nair, 2005; 2006 �Kawanishi et al, 2006 �Coussens & Werb, 2002 �Balkwill & Mantovani, 2001
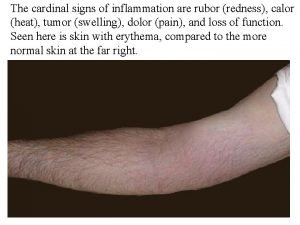
 Cardinal sign of inflammation
Cardinal sign of inflammation Cellular events of acute inflammation
Cellular events of acute inflammation Morphologic patterns of acute and chronic inflammation
Morphologic patterns of acute and chronic inflammation Cell injury and inflammation
Cell injury and inflammation Dry gangrene vs wet gangrene
Dry gangrene vs wet gangrene Trigeminal neuralgia
Trigeminal neuralgia Cardinals signs of inflammation
Cardinals signs of inflammation Cardinal signs of inflammation
Cardinal signs of inflammation Morphological pattern of acute inflammation
Morphological pattern of acute inflammation Acute inflammation
Acute inflammation Non odontogenic infection
Non odontogenic infection Stages of inflammation
Stages of inflammation Mediators of inflammation
Mediators of inflammation Sequelae of acute inflammation
Sequelae of acute inflammation Cellular events of acute inflammation
Cellular events of acute inflammation 5 cardinal signs of inflammation
5 cardinal signs of inflammation Cardinal signs inflammation
Cardinal signs inflammation Inflammation fever
Inflammation fever Vascular response in acute inflammation
Vascular response in acute inflammation Ganzimmun
Ganzimmun Dr el sabbagh
Dr el sabbagh Subfebris febris
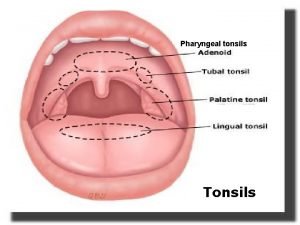
Subfebris febris Where are the tonsils located
Where are the tonsils located Cortisol tagesprofil ganzimmun
Cortisol tagesprofil ganzimmun Morphologic patterns of acute inflammation
Morphologic patterns of acute inflammation Bradykinin nitric oxide
Bradykinin nitric oxide Sistema complemento funções
Sistema complemento funções Lochkerne
Lochkerne Acute inflammation
Acute inflammation Sublingual dermoid
Sublingual dermoid Morphologic patterns of acute inflammation
Morphologic patterns of acute inflammation Chemical mediators of inflammation
Chemical mediators of inflammation Serous inflammation examples
Serous inflammation examples Chronic inflammation
Chronic inflammation Inflammation
Inflammation Jointitis
Jointitis Acute inflammation
Acute inflammation Bệnh gì
Bệnh gì Inflammation
Inflammation Dlc smear
Dlc smear