VULVOVAGINITIS Rukset Attar MD Ph D Department of








- Slides: 37
VULVOVAGINITIS Rukset Attar, MD, Ph. D Department of Obstetrics and Gynecology
Causes of Vulvovaginitis n Infectious n Vulvovaginal candidiasis n Bacterial vaginosis n Bacterial infections n Trichomoniasis n Viral infections n Desquamative inflammatory vaginitis (clindamycin responsive) n Secondary bacterial infection associated with foreign body n Parasitic
Causes of Vulvovaginitis n Noninfectious n Atrophic vaginitis n Allergic vaginitis n Foreign body n Desquamative inflammatory vaginitis (steroid responsive) n Collagen vascular disease n Behçet's syndrome n Pemphigus syndromes
Candidiasis n n 75% of women will experience an episode of vulvovaginal candidiasis. Candida albicans is the most common Candida species causing symptomatic candidiasis in approximately 90% of cases C albicans frequently inhabits the mouth, throat, large intestine, and vagina normally. Clinical infection may be associated with a systemic disorder (diabetes mellitus, human immunodeficiency virus [HIV], obesity), pregnancy, medication (antibiotics, corticosteroids, oral contraceptives), and chronic debilitation.
Candidiasis n n presents with intense vulvar pruritus; a white curdlike, cheesy vaginal discharge; and vulvar erythema. Diagnosis is based on demonstration of candidal mycelia and a normal vaginal p. H 4. 5. Identification of C albicans requires finding filamentous forms (pseudohyphae) of the organism when vaginal secretions are mixed with 10% KOH solution. The gold standard for its diagnosis is a vaginal culture.
Candidiasis n n Chemicals and dyes n 1% Gentian violet (once per week) n Boric acid Polyenes n Nystatin-have been largely replaced by imidazoles. Imidazole n clotrimazole and oral agents such as ketoconazole (mostly used as topical agents and are effective against C albicans. n A single 150 -mg oral dose of fluconazole Inclusion of a topical steroid
Bacterial infections n n n Gardnerella vaginalis Neisseria gonorrhoeae Chlamydia Mycoplasma hominis Ureaplasma urealyticum.

Bacterial Vaginosis n n The most common cause of symptomatic bacterial infection in reproductive-age women. In bacterial vaginosis the normal vaginal flora is altered. The concentration of the hydrogen peroxide–producing lactobacilli is decreased There is overgrowth of Gardnerella vaginalis, Mobiluncus spp. , anaerobic gram-negative rods (Prevotella spp. , Porphyromonas spp. , Bacteroides spp. ), and Peptostreptococcus spp
Bacterial Vaginosis n n Presents as a "fishy" vaginal discharge, which is more noticeable following unprotected intercourse. The patient complains of a malodorous, nonirritating discharge, and examination reveals homogeneous, graywhite secretions with a p. H of 5. 0– 5. 5. A transient "fishy" odor can be released on application of 10% KOH to the vaginal secretions on a glass slide. A wet mount of the vaginal secretions using normal saline under microscopy demonstrates the characteristic clue cells, decreased lactobacilli, and few white blood cells.
Bacterial Vaginosis n n n Gram stain reveals a large number of small gramnegative bacilli and a relative absence of lactobacilli. Gram stain provides a more sensitive (93%) and specific (70%) diagnosis than does wet mount. Treatment in nonpregnant women include n metronidazole 500 mg orally twice daily for 7 days, metronidazole gel 0. 75% (1 full applicator, 5 g) intravaginally once or twice daily for 5 days, or n clindamycin cream 2% (1 full applicator, 5 g) intravaginally at bedtime for 7 days. n Alternative regimens include metronidazole 2 g orally in a single dose, clindamycin 300 mg orally twice daily for 7 days, or clindamycin ovules 100 g intravaginally once at bedtime for 3 days.

Bacterial Vaginosis n n Pregnant women, the recommended treatment n metronidazole 250 mg orally 3 times daily for 7 days. n Alternatively, clindamycin 300 mg orally twice daily for 7 days can be given. Possible management strategies for recurrent vaginosis includes use of condoms, longer treatment periods, prophylactic maintenance therapy, oral or vaginal application of yogurt containing lactobacillus acidophilus, intravaginal planting of other exogenous lactobacilli, and hydrogen peroxide douches.

Neisseria Gonorrhoeae n n n Up to 85% of women are asymptomatic In acute disease, patients present with a copious mucopurulent discharge, and Gram's stain reveals gramnegative diplococci within leukocytes. However, diagnosis should be confirmed with a culture or with nucleic acid amplification. The specimen is collected from the endocervix. Cultures may also be taken from the urethra, rectum, and mouth.
Neisseria Gonorrhoeae n n n An estimated 15– 20% of women with lower tract disease will develop upper tract disease presenting with salpingitis, tubo-ovarian abscess, and peritonitis. Ectopic pregnancy and infertility may result. If active infection is present during delivery, the newborn may develop conjunctivitis by contamination during vaginal delivery
Neisseria Gonorrhoeae n n n Treatment of uncomplicated gonococcal infections of the cervix consists of ceftriaxone 125 mg IM in a single dose. Cefixime 400 mg orally in a single dose, ciprofloxacin 500 mg orally in a single dose, ofloxacin 400 mg orally in a single dose, or levofloxacin 250 mg orally in a single dose are other recommended regimens. Spectinomycin 2 g IM in a single dose can be given to patients sensitive to cephalosporins and quinolones. Treatment of Chlamydia trachomatis infection should be considered

Chlamydia Trachomatis n n present with a mucopurulent cervicitis, dysuria, and/or postcoital bleeding can also cause an ascending infection, salpingitis, in 20– 40% of untreated patients. More than 50% of upper tract infections may be caused by C trachomatis, leading to tubal occlusion, ectopic pregnancy, or infertility. C trachomatis also can cause neonatal conjunctivitis if untreated and atypical cytologic findings on Papanicolaou smear. C trachomatis may present as lymphogranuloma venereum (LGV), which most commonly affects the vulvar tissues. Retroperitoneal lymphadenopathy may be present
Chlamydia Trachomatis n n n Can be identified by culture (50– 90% sensitivity), a direct fluorescent antibody (50– 80% sensitivity) and enzyme immunoassay (40– 60% sensitivity), or most recently using nucleic acid amplification tests (polymerase chain reaction or ligase chain reaction, 60– 100% sensitivity) Azithromycin 1 g orally in a single dose or doxycycline 100 mg orally twice daily for 7 days. Erythromycin base 500 mg orally 4 times daily for 7 days, Ofloxacin 300 mg orally twice daily, or Levofloxacin 50 mg once daily for 7 days are alternative regimens. Doxycycline, levofloxacin, and ofloxacin should be avoided in pregnancy and during lactation.
M Hominis and U Urealyticum n n May cause infertility, spontaneous abortion, postpartum fever, nongonococcal urethritis in men, and possibly salpingitis and pelvic abscess. The most effective treatment is doxycycline 100 mg orally twice daily for 10 days.
Trichomonas Vaginitis n n n Trichomonas vaginalis is a unicellular flagellate protozoan T vaginalis organisms are larger than polymorphonuclear leukocytes but smaller than mature epithelial cells. T vaginalis infects the lower urinary tract in both women and men A persistent vaginal discharge is the principal symptom with or without secondary vulvar pruritus. The discharge is profuse, extremely frothy, greenish, and at times foul-smelling.
Trichomonas Vaginitis n n The p. H of the vagina usually exceeds 5. 0. The labia minora may become edematous and tender. Urinary symptoms may occur; however, burning with urination is most often associated with severe vulvitis. Examination of the vaginal epithelium and cervix shows generalized vaginal erythema with multiple small petechiae, the so-called strawberry spots, which may be confused with epithelial punctation.
Trichomonas Vaginitis n n Wet mount with normal saline reveals an increase in polymorphonuclear cells and characteristic motile flagellates in 50– 70% of culture-confirmed cases (Fig 37 – 3). Papanicolaou smears have a sensitivity of approximately 60% and may yield false-positive results. Culture is the gold standard, providing 95% sensitivity and 100% specificity. DNA probes and monoclonal antibodies may assist with accurate diagnosis.

Trichomonas Vaginitis n n n Metronidazole is the only Food and Drug Administration (FDA)-approved treatment in the United States, with cure rates of approximately 90– 95%. A single-dose regimen of 2 g may assure compliance. Other regimens include a 500 -mg tablet orally twice daily for 7 days. In resistant cases, which most likely are related to reinfection, oral metronidazole can be repeated after 4– 6 weeks if the presence of trichomonads has been confirmed and the white blood cell count and differential are normal.

Viral Infections n The viruses that affect the vulva and vagina are n Herpesvirus (herpes simplex, varicella-zoster, and cytomegalovirus) n Poxvirus (molluscum contagiosum) and n Papovavirus types
Herpesvirus n n n Infection occurs through direct contact with secretions or mucosal surfaces contaminated with the virus. The virus enters the skin through cracks or other lesions but can enter through an intact mucosa. The virus initially replicates in the dermis and epidermis. Incubation time is 2– 7 days. Prodromal symptoms of tingling, burning, or itching may occur shortly before vesicular eruptions appear. The vesicles erode rapidly, resulting in painful ulcers distributed in small patches, or they may involve most of the vulvar surfaces
Herpesvirus n n n Bilateral inguinal adenopathy may be present. Dysuria or other urinary symptoms may develop, including urinary retention. Approximately one-third of patients demonstrate systemic manifestations such as fever, malaise, headaches, and myalgia. In other cases the primary infection is asymptomatic. Lesions may persist for 2– 6 weeks with no subsequent scarring
Herpesvirus n n n Approximately 85% of patients develop immunoglobulin (Ig)M antibodies to type II virus within 21 days of exposure. Serologic tests are best used to determine whether the patient has been infected in the past. A 4 -fold or higher increase in neutralizing complement fixation antibody titers between acute and convalescent sera may be useful to document a primary infection. Only 5% of patients with recurrent infection demonstrate a 4 -fold or higher rise in antibody titer. New type-specific serologic tests for herpes simplex virus are available.
Herpesvirus n n The incidence of neonatal simplex virus infection ranges from 1 in 5000 to 1 in 20, 000 live births. Infection in the newborn is associated with a 60% mortality rate, and at least half of the survivors have significant neurologic and/or ocular sequelae. The risk of infection to an infant born vaginally in a mother with active primary genital infection is 40– 50%; for recurrent infection the risk is 5%. Suppressive antiviral therapy may be initiated at 36 weeks to decrease the need for cesarean section
Human Papillomavirus n n n is responsible for condyloma acuminata of the vagina, cervix, vulva, perineum, and perianal areas as well as for dysplasia and cancer. Condylomatous vaginitis causes a rough vaginal surface, demonstrating white projections from the pink vaginal mucosa. Vaginal discharge and pruritus are the most common symptom with florid condylomas. Postcoital bleeding may occur. No specific symptoms are related to the other types of condylomas.
Human Papillomavirus n Treatment n Bichloroacetic acid (BCA) or trichloroacetic acid (TCA), 50– 80% solution, Xylocaine 1% gel can be applied around the wart to prevent damage to adjacent skin. Repeat weekly as necessary. n Podophyllin 10– 25% in tincture of benzoin n Cryosurgery, n electrosurgery, n simple surgical excision, n laser vaporization n Podofilox 0. 5% solution or gel n Imiquimod 5% cream (topically active immune enhancer that stimulates production of interferon and other cytokines)
Atrophic Vaginitis n n Prepubertal, lactating, and postmenopausal women lack the vaginal effects of estrogen production. The p. H of the vagina is abnormally high, and the normally acidogenic flora of the vagina may be replaced by mixed flora. The vaginal epithelium is thinned and more susceptible to infection and trauma. Although most patients are asymptomatic, many postmenopausal women report vaginal dryness, spotting, presence of a serosanguineous or watery discharge, and/or dyspareunia.
Atrophic Vaginitis n n Treatment includes intravaginal application of estrogen cream. Approximately one-third of the vaginal estrogen is systemically absorbed; therefore, this treatment may be contraindicated in women with a history of breast or endometrial cancer. The estradiol vaginal ring, which is changed every 90 days, may provide a more preferable route of administration for some women, or Estradiol hemihydrate (Vagifem) 1 tablet intravaginally daily for 2 weeks and then 2 times per week for at least 3 – 6 months may be less messy. Systemic estrogen therapy should be considered if there are no contraindications.
Foreign Bodies n n n Treatment involves removal of the foreign body. Rarely, antibiotics are required for ulcerations or cellulitis of the vulva or vagina. Dryness or ulceration of the vagina secondary to use of menstrual tampons is transient and heals spontaneously.

Desquamative Inflammatory Vaginitis n n n The cause is unknown. Patients complain of a profuse purulent vaginal discharge, vaginal burning or irritation, dyspareunia, and occasional spotting. The process is patchy and usually localized to the upper half of the vagina. The purulent discharge contains many immature epithelial and pus cells without any identifiable cause. Vaginal erythema is present and synechiae may develop in the upper vagina, causing partial occlusion
Desquamative Inflammatory Vaginitis n Treatment often is unsatisfactory but has included local application of estrogen, antibiotics (particularly clindamycin cream 2% 5 g intravaginally daily for 7 days), and corticosteroids.

Noninfectious Vaginitis n n Chemical vaginitis secondary to multiple irritating offenders, including topical irritants (sanitary supplies, spermicides, feminine hygiene supplies, soaps, perfumes), allergens (latex, antimycotic creams), and possibly excessive sexual activity can cause pruritus, irritation, burning, and vaginal discharge. The etiology may be confused with vulvovaginal candidiasis. The offending agent should be removed for treatment. A short course of corticosteroid treatment may be used along with sodium bicarbonate sitz baths and topical vegetable oils.
Cervical Mucorrhea or Vaginal Epithelial Discharge n n Cervicitis due to cervical polyps or cervical or vaginal cancer can cause a mucopurulent discharge and bleeding. Excessive cervical ectropion may cause excessive discharge of cervical mucus from normal endocervical cells. Vaginal adenosis (the presence of the metaplastic cervical or endometrial epithelium within the vaginal wall) may cause the same type of clear, mucoid-type discharge with no associated symptoms. Excessive desquamation of the vaginal epithelium may produce a diffuse gray-white pasty vaginal discharge, which may be confused with candidiasis
Cervical Mucorrhea or Vaginal Epithelial Discharge n n Vaginal p. H is normal. Microscopic evaluation shows normal bacterial flora, mature vaginal squamae, and no increase in the number of leukocytes. Excessive but normal vaginal discharge should be treated with reassurance and, if required at times, with cryosurgery or carbon dioxide treatment of the cervix. Continuous use of a tampon should be avoided.
Parasitic Infection n n Pinworms (Enterobius vermicularis) and Entamoeba histolytica Trophozoites of E histolytica may be demonstrated on wet-mount preparations or occasionally on a Papanicolaou smear. The parasite is generally detected by pressing a strip of adhesive cellulose tape to the perineum. The tape is then adhered to a slide, allowing the doublewalled ova to be identified under the microscope.
 Rukset attar
Rukset attar Vagenectomy
Vagenectomy L
L Sara el attar
Sara el attar Diana attar
Diana attar Diana attar
Diana attar Haidar al attar
Haidar al attar Haidar al attar
Haidar al attar Columbia county road department
Columbia county road department Nevada department of business and industry
Nevada department of business and industry Kentucky department of revenue
Kentucky department of revenue Nys department of labor
Nys department of labor Blondel
Blondel Name department
Name department Nevada department of business and industry
Nevada department of business and industry Human resource management lecture chapter 1
Human resource management lecture chapter 1 Uta math clinic
Uta math clinic Ga department of audits and accounts
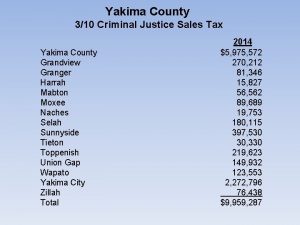
Ga department of audits and accounts Yakima assigned counsel
Yakima assigned counsel San luis obispo planning department
San luis obispo planning department Banquet function prospectus
Banquet function prospectus Department overview template
Department overview template Cowlitz county health department
Cowlitz county health department Nj department of labor
Nj department of labor Federal department of home affairs fdha
Federal department of home affairs fdha Ridgefield department of health
Ridgefield department of health Department of us
Department of us Catering organization
Catering organization Bloomington indiana police department
Bloomington indiana police department City of joliet water and garbage
City of joliet water and garbage Room service department
Room service department University of toronto anthropology masters
University of toronto anthropology masters Baltimore county zoning department
Baltimore county zoning department Tuscarawas county health department
Tuscarawas county health department Ksu math department
Ksu math department Buffalo wild wings payroll department
Buffalo wild wings payroll department Human resorces department
Human resorces department Arkansas child nutrition unit
Arkansas child nutrition unit