Acute coronary syndromes DR G SWARNA LATHA DEVI


- Slides: 66
Acute coronary syndromes DR. G. SWARNA LATHA DEVI. M. D. PROF. MEDICINE
ACS - introduction an umbrella term for any condition where the blood supplied to the heart muscle is reduced the most feared complications of coronary artery disease (CAD) are associated with high mortality and morbidity Cardiovascular diseases (CVD) - presently the leading causes of death in industrialized countries
Definition The clinical presentations of CAD include: silent ischaemia stable angina pectoris heart failure unstable angina myocardial infarction (MI) sudden death
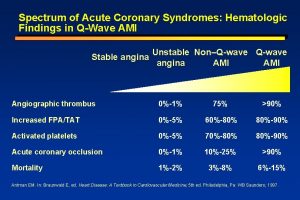
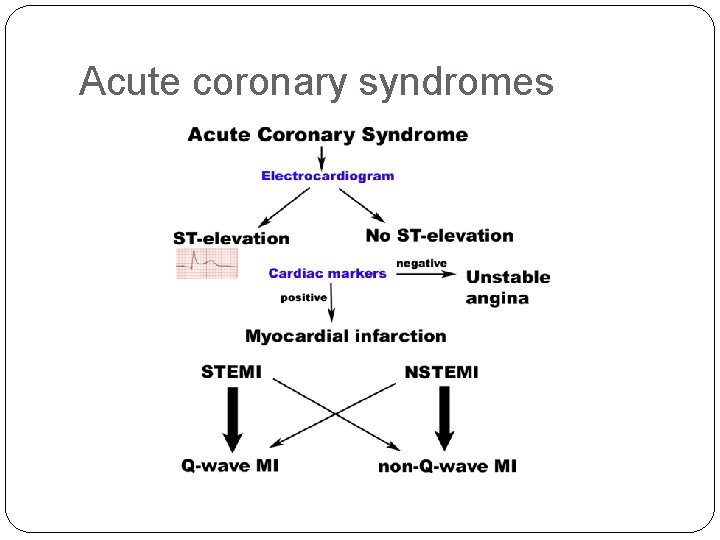
Acute coronary syndromes ACS are usually divided into: Unstable angina - only ischemia, lack of necrosis STEMI - ST - elevation MI NSTEMI - non-ST elevation MI Sudden death - due to cardiac arrhythmias
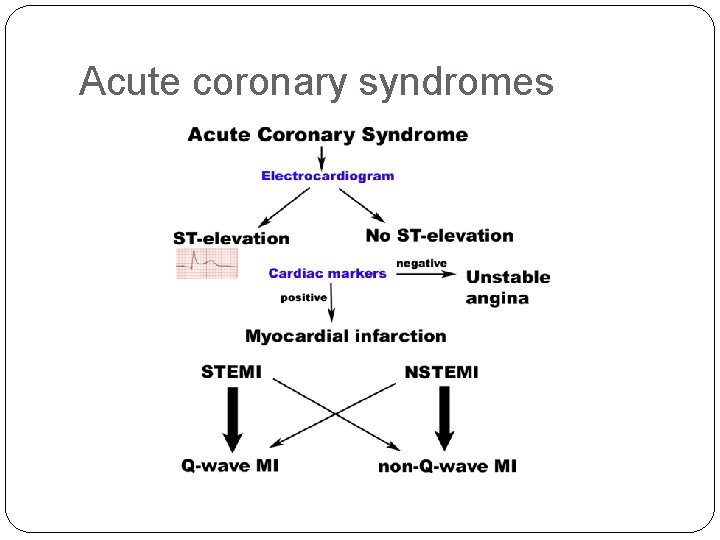
Acute coronary syndromes
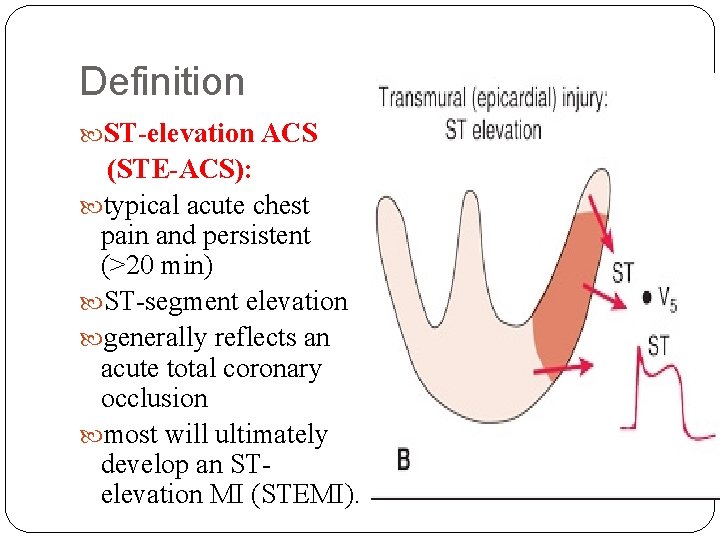
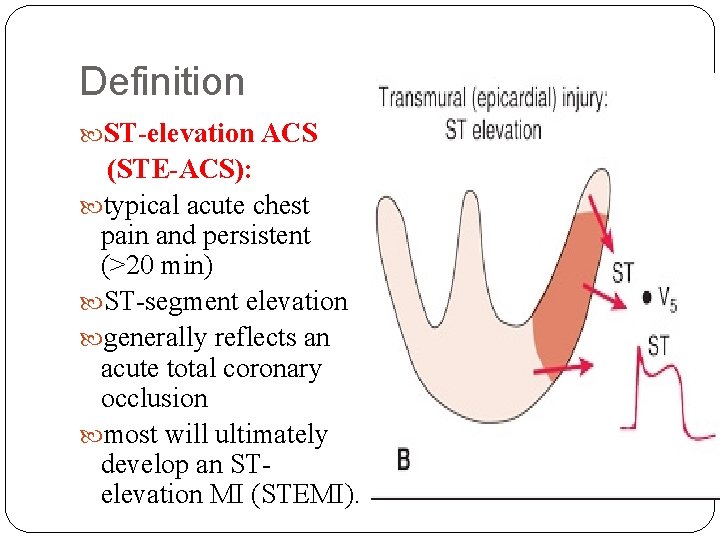
Definition ST-elevation ACS (STE-ACS): typical acute chest pain and persistent (>20 min) ST-segment elevation generally reflects an acute total coronary occlusion most will ultimately develop an STelevation MI (STEMI).
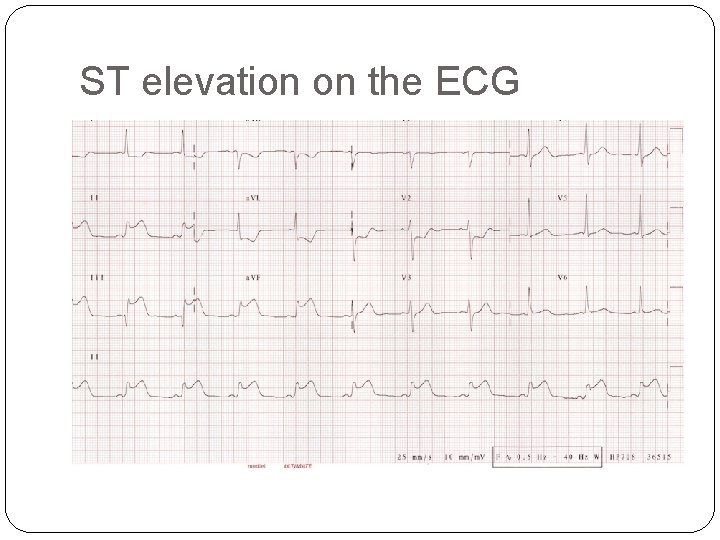
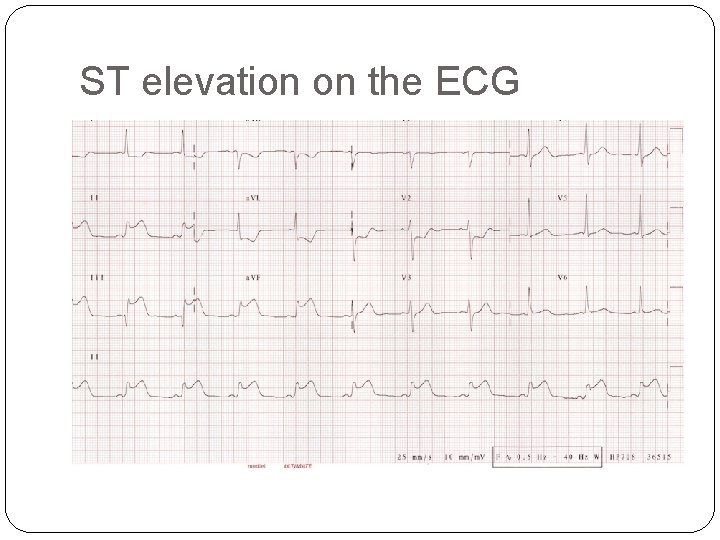
ST elevation on the ECG
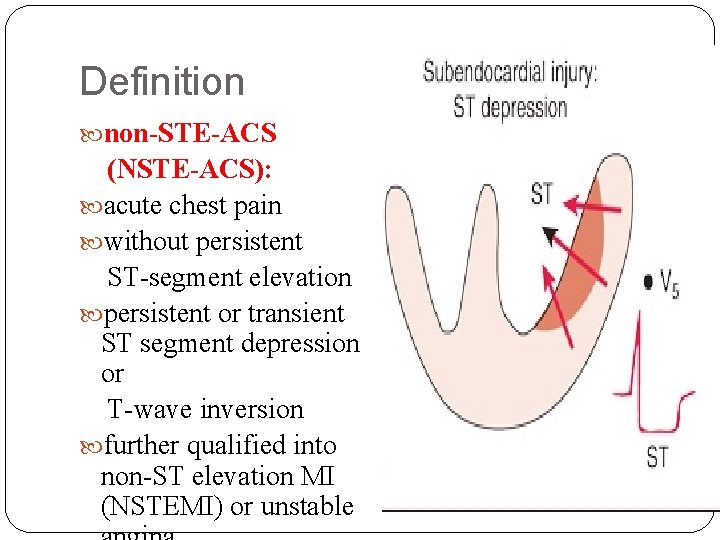
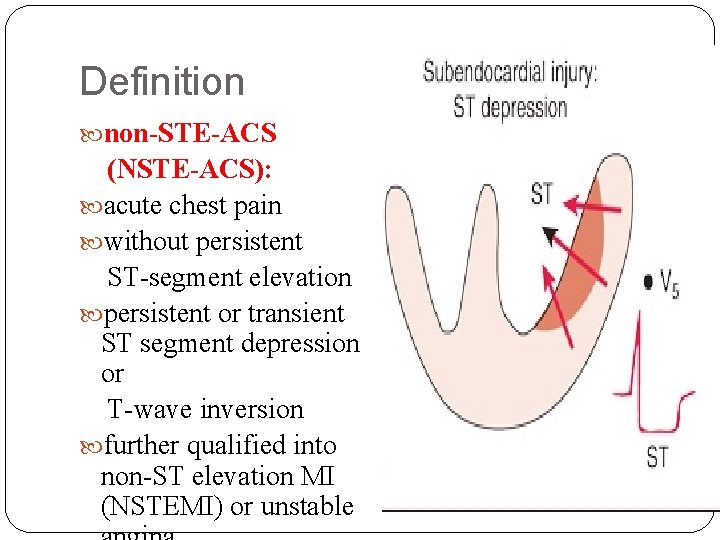
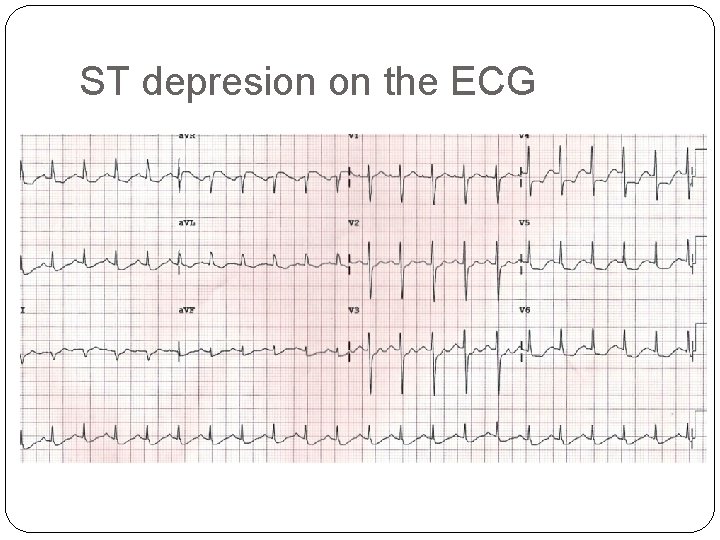
Definition non-STE-ACS (NSTE-ACS): acute chest pain without persistent ST-segment elevation persistent or transient ST segment depression or T-wave inversion further qualified into non-ST elevation MI (NSTEMI) or unstable
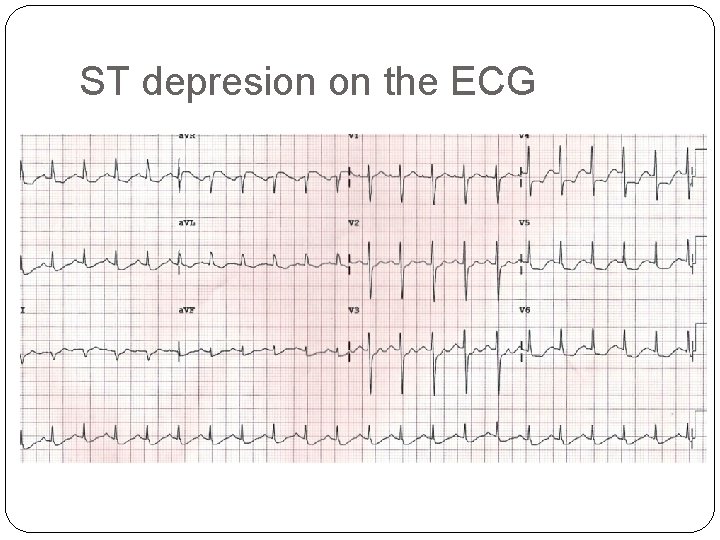
ST depresion on the ECG

Pathophysiology of ACS Atherothrombosis Atherosclerosis - a fixed and barely reversible process of gradual luminal narrowing (slowly over decades) Thrombosis - a dynamic and potentially reversible process causing rapid complete or partial occlusion of the coronary artery
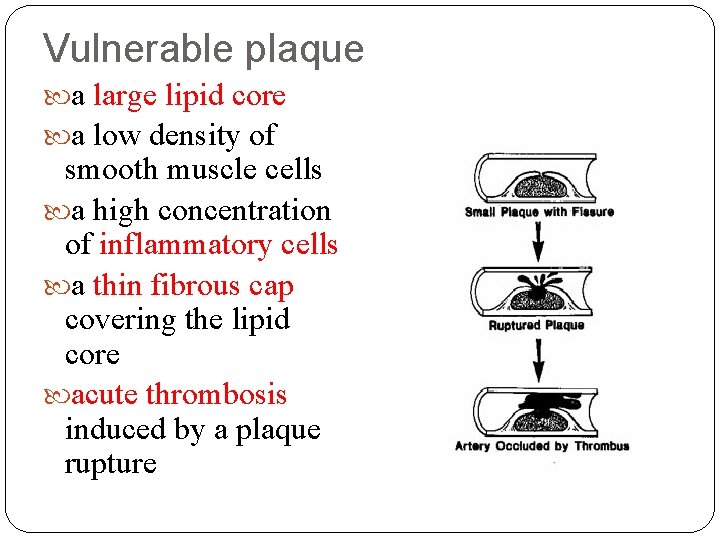
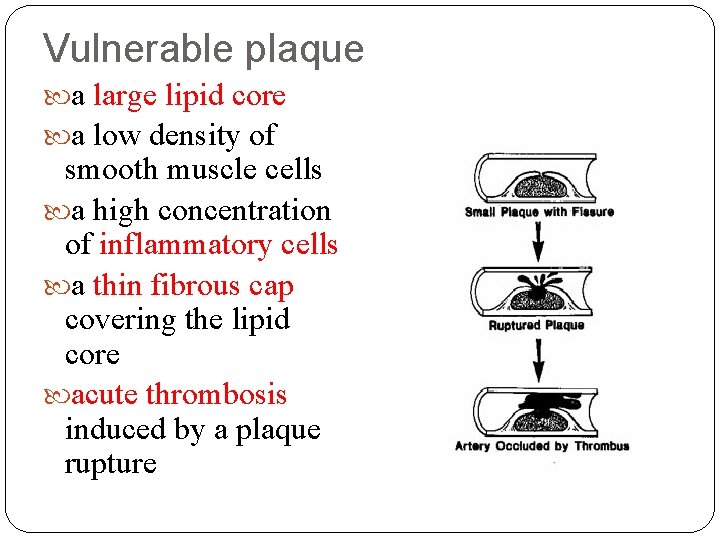
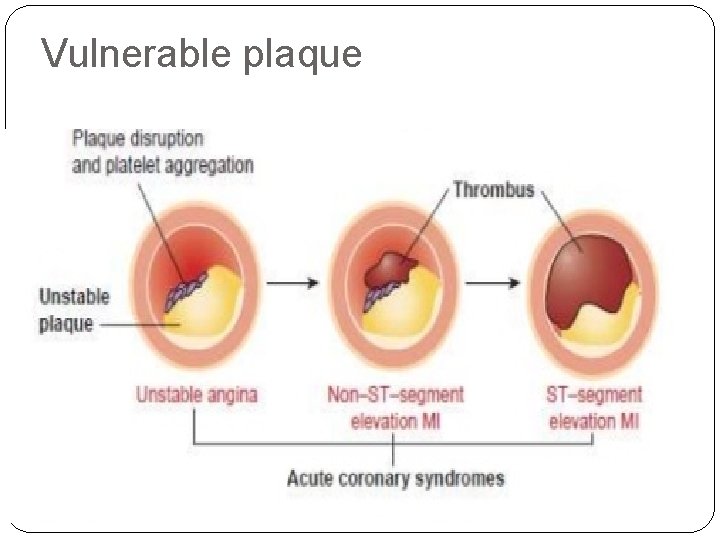
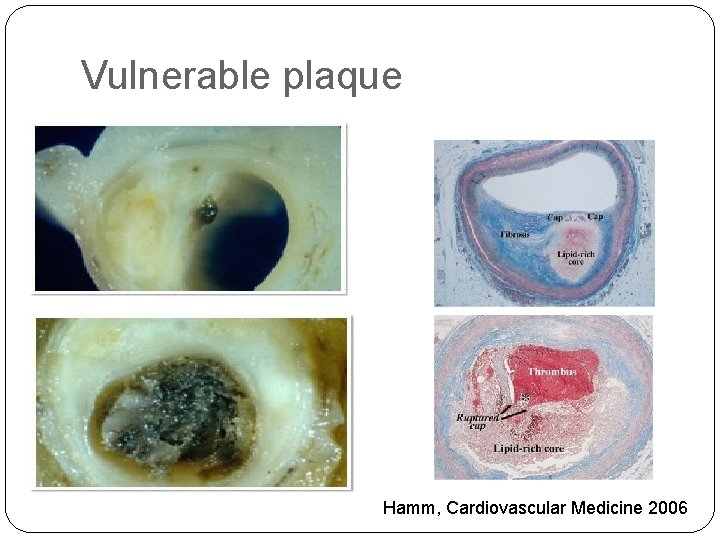
Vulnerable plaque a large lipid core a low density of smooth muscle cells a high concentration of inflammatory cells a thin fibrous cap covering the lipid core acute thrombosis induced by a plaque rupture
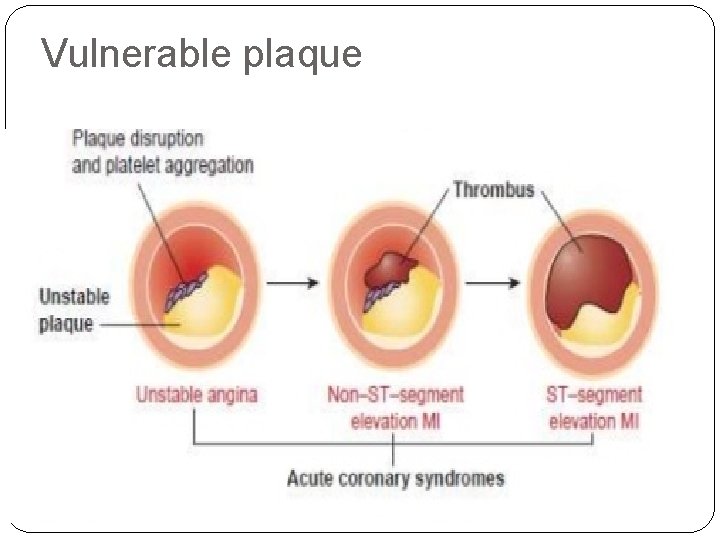
Vulnerable plaque
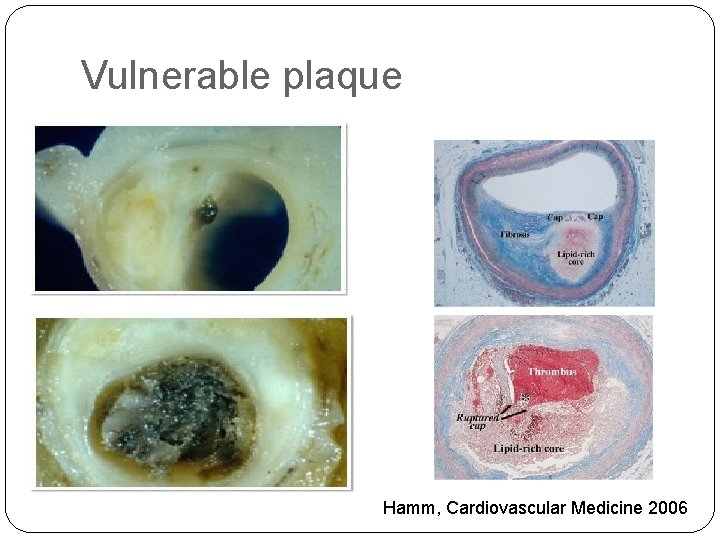
Vulnerable plaque Hamm, Cardiovascular Medicine 2006
Vulnerable patient Multiple sites of plaque rupture with or without intracoronary thrombosis Elevated levels of various systemic markers of inflammation, thrombosis and coagulation system activation Hypercholesterolaemia Tobacco smoking
Epidemiology The annual incidence of NSTE-ACS is higher than STEMI The annual incidence of hospital admissions for NSTE-ACS is in the range of 3 per 1000 inhabitants sex differences - men account for more than 90% of patients with AMI at the age under 40 y. (a hormonal profile of woman has a protective effect) age differences - in patients aged under 40 y. only one heart artery is affected
Prognosis of STE vs. NSTE-ACS Hospital mortality - higher in patients with STEMI than among those with NSTE-ACS (7 vs. 5%) 6 months mortality - the mortality rates are very similar in both conditions (12 vs. 13%) Long-term follow-up - death rates higher among those with NSTE-ACS than with STE-ACS
Prognosis of STE vs. NSTE-ACS The causes of the higher death rates of NSTE-ACS than of STE-ACS pts. during long-term follow-up are: older pts. more co-morbidities (diabetes and renal failure). a greater extent of coronary artery and vascular diseases persistent triggering factors such as inflammation
Classification of MI Type 1 – spontaneous MI related to ischemia due to a primary coronary event such as plaque erosion and/or rupture, fissuring, or dissection Type 2 – MI secondary to ischemia due to either increased oxygen demand or decreased supply, e. g. coronary artery spasm Coronary embolism, Anemia, arrhythmias , Hypertension, or hypotension
Classification of MI Type 3 – sudden unexpected cardiac death, including cardiac arrest but death occurring before blood samples could be obtained Type 4 – associated with PCI: Type 4 a – MI associated with the procedure of PCI Type 4 b – MI associated with stent thrombosis Type 5 – MI associated with CABG
Myocardial infarction 1. Atherosclerotic aetiology (type 1) 2. Non-atherosclerotic aetiology: (type 2 -5) arteritis trauma dissection congenital anomalies cocaine abuse complications of cardiac catheterization, CABG

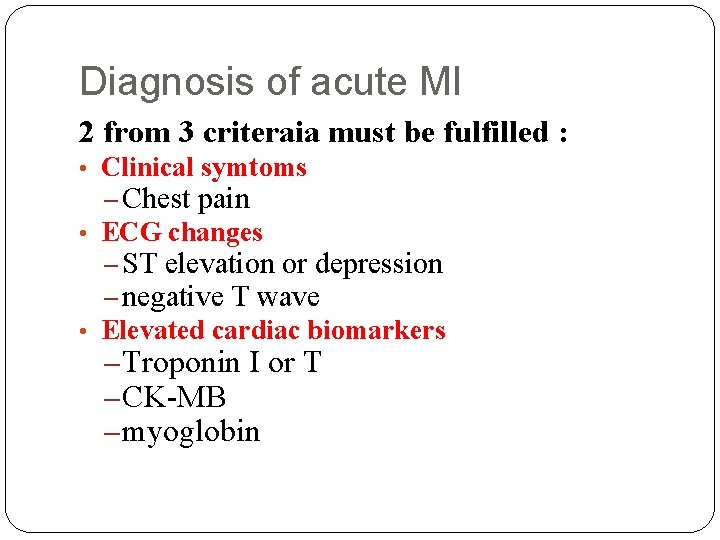
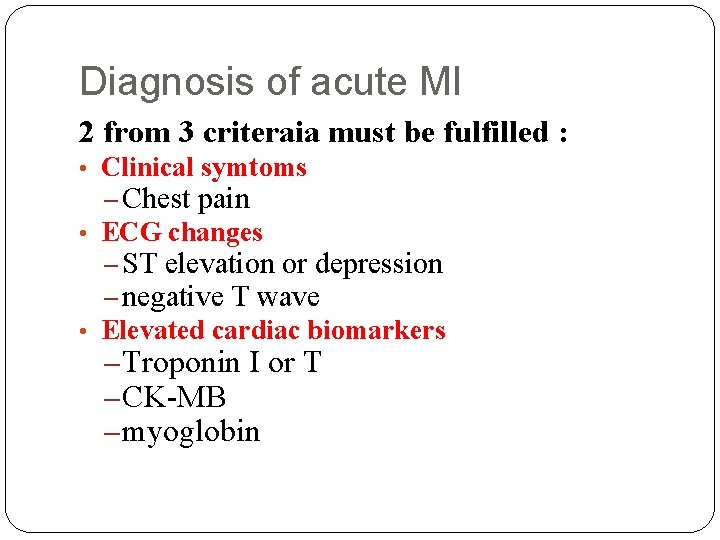
Diagnosis of acute MI 2 from 3 criteraia must be fulfilled : • Clinical symtoms – Chest pain • ECG changes – ST elevation or depression – negative T wave • Elevated cardiac biomarkers – Troponin I or T – CK-MB – myoglobin
Diagnosis of ACS Clinical presentation History of patient Physical examination Electrocardiogram Biochemical markers - troponin Non-invasive imaging - Echo Imaging of coronary arteries - coronary angiography
Clinical presentation STE/NSTE-ACS: Intense prolonged (20 min) pain at rest - retrosternal pressure or heaviness (‘angina’) radiating up to the neck, shoulder and jaw and down to the ulnar aspekt of the left arm May be accompanied by other symptoms such as diaphoresis, nausea, abdominal pain, dyspnoea, … Unstable angina: New onset severe angina (class III of CCS) Post-MI angina.
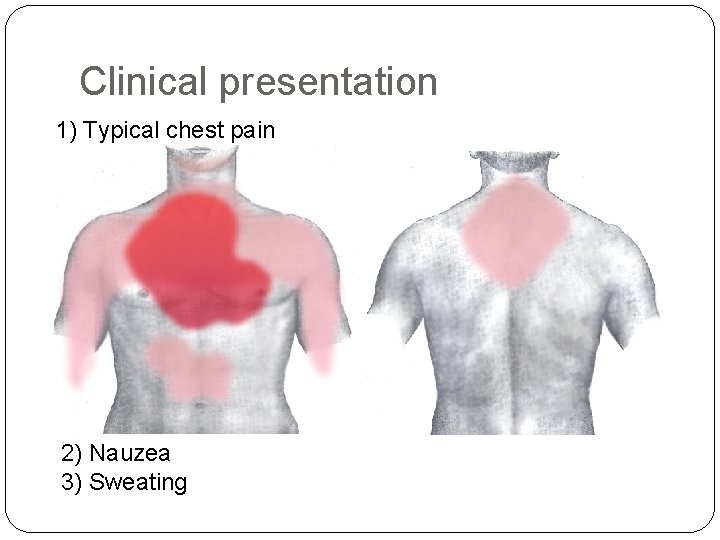
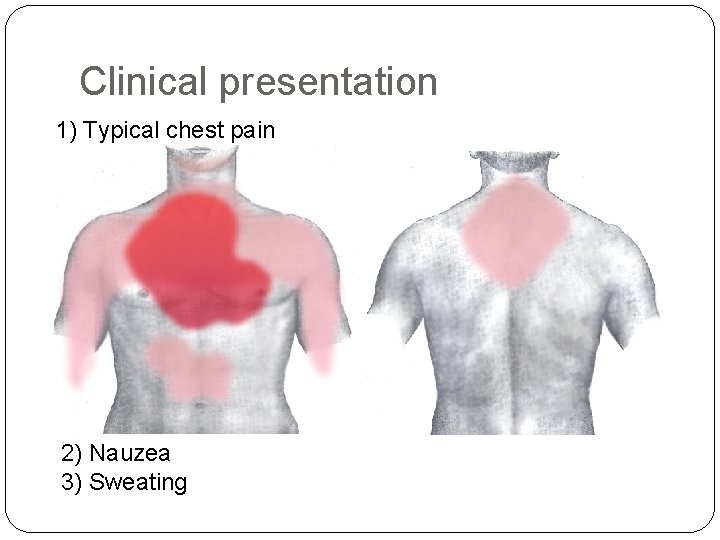
Clinical presentation 1) Typical chest pain 2) Nauzea 3) Sweating
Clinical presentation Atypical presentations are not uncommon epigastric pain recent-onset indigestion stabbing chest pain with some pleuritic features increasing dyspnoea - often can be observed in younger (25 -40 y. ), older (75 y. ), in women, in pts. with diabetes, chronic renal failure, or dementia.
Clinical presentation The presence of tachycardia, hypotension, or heart failure needs rapid diagnosis and management, often indicating a poor prognosis of this patient with ACS It is important to identify the clinical circumstances such as anaemia, infection, inflammation, fever, and metabolic or endocrine (in particular thyroid) disorders (may exacerbate or precipitate ACS)
Physical examination Frequently normal Signs of heart failure or haemodynamic instability Dif. dg. : - nonischaemic cardiac disorders: pulmonary embolism, aortic dissection, pericarditis, valvular heart disease) - extra-cardiac causes: pulmonary diseases - pneumothorax, pneumonia, pleural effusion)
Physical examination Heart failure Tachycardia, tachypnoe Pulmonary rales (pulmonary congestion) RV failure - ↑ jugular congestion, hepatomegaly Hypotension ↓ 100/60 mmhg cardiac shock (tachycardia) ↑ vagal nerve activity (bradycardia - inferior IM) Bradycardia AV block Inferior IM - non-serious, frequent Anterior IM - serious, rare
Electrocardiogram The resting 12 -lead ECG is the first-line diagnostic tool in the assessment of patients with suspected ACS. STE-ACS… ST-elevation NSTE-ACS…ST-segment shifts and Twave changes A completely normal ECG does not exclude the possibility of ACS.
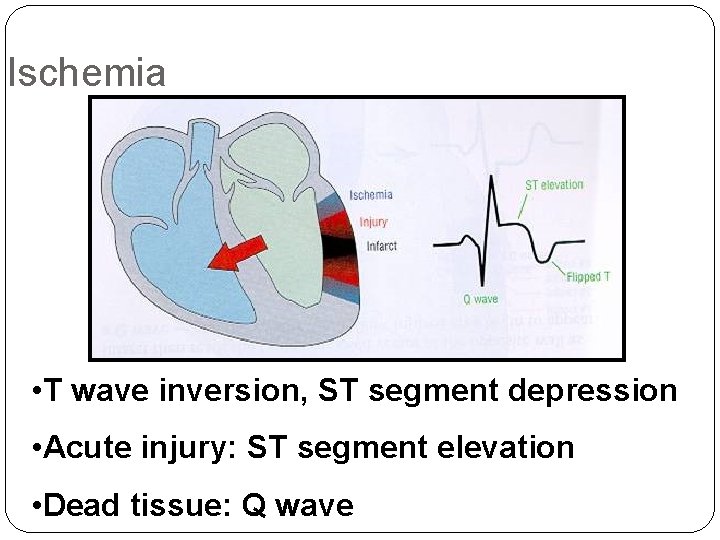
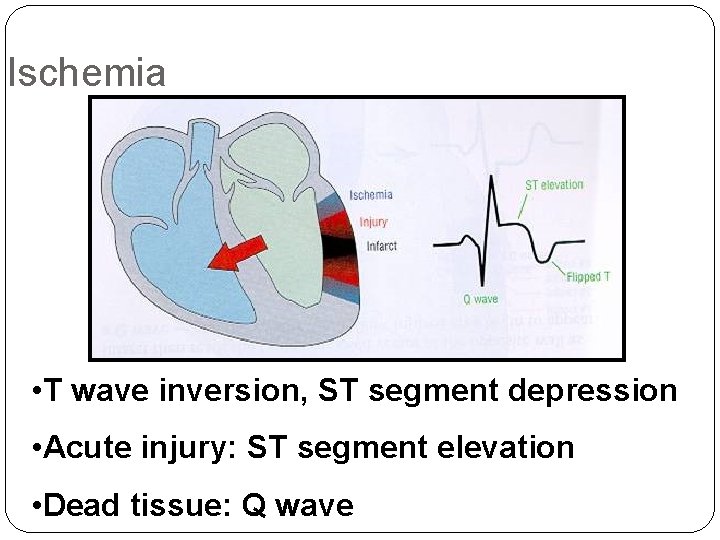
Ischemia • T wave inversion, ST segment depression • Acute injury: ST segment elevation • Dead tissue: Q wave
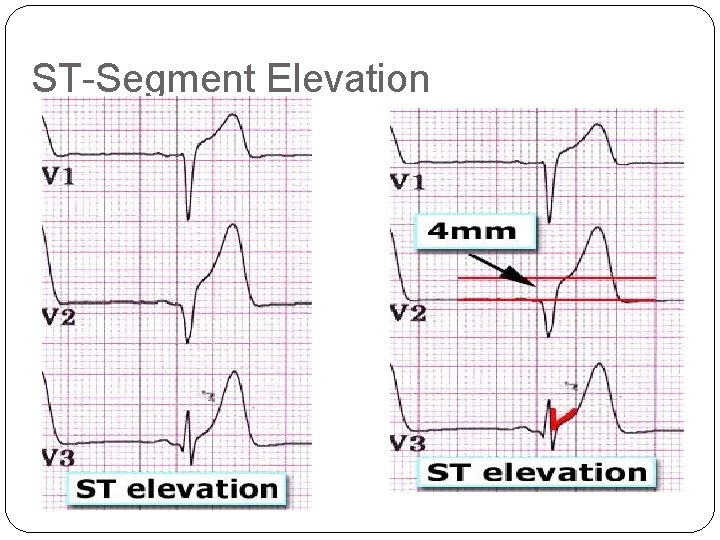
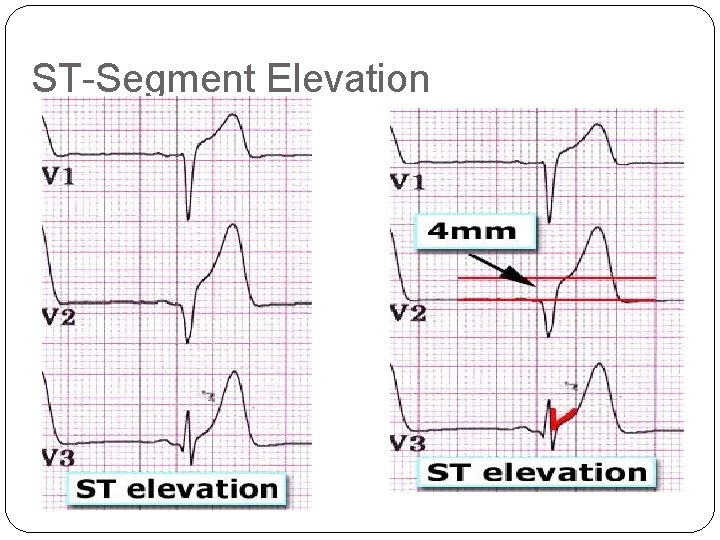
ST-Segment Elevation
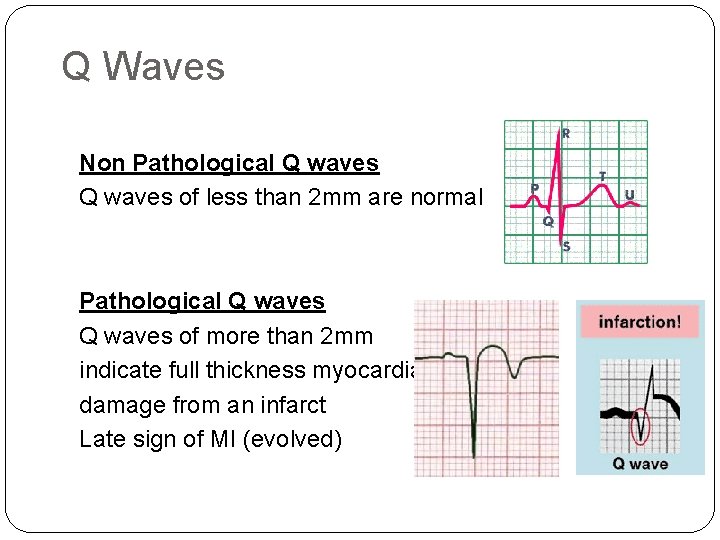
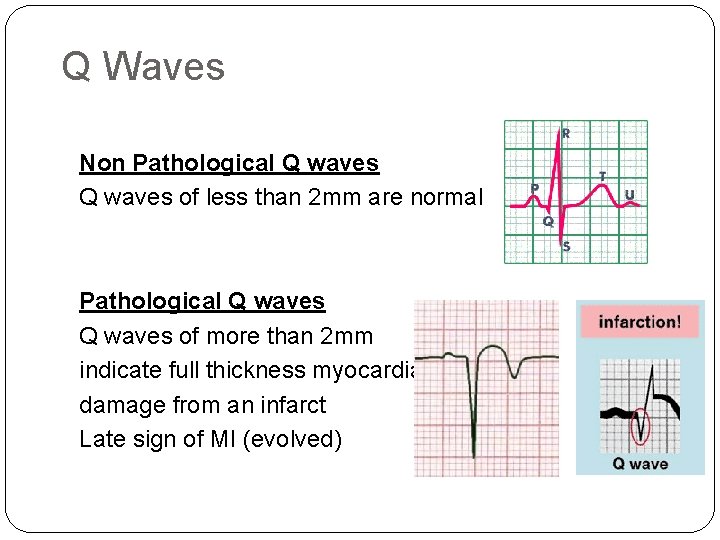
Q Waves Non Pathological Q waves of less than 2 mm are normal Pathological Q waves of more than 2 mm indicate full thickness myocardial damage from an infarct Late sign of MI (evolved)
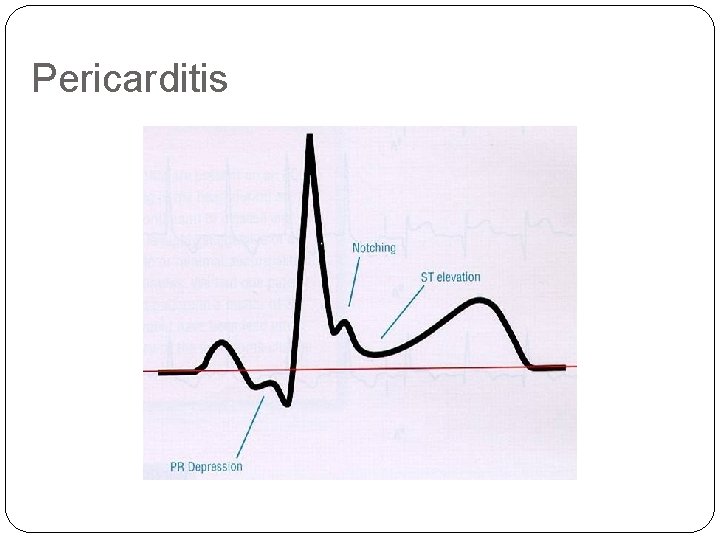
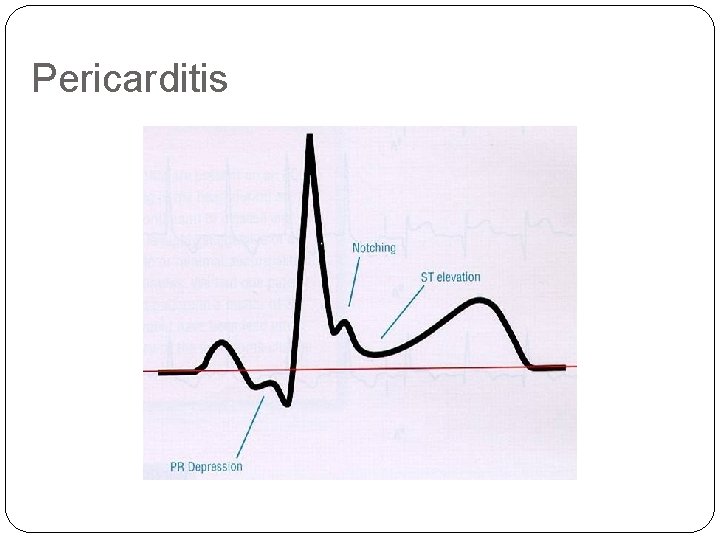
Pericarditis
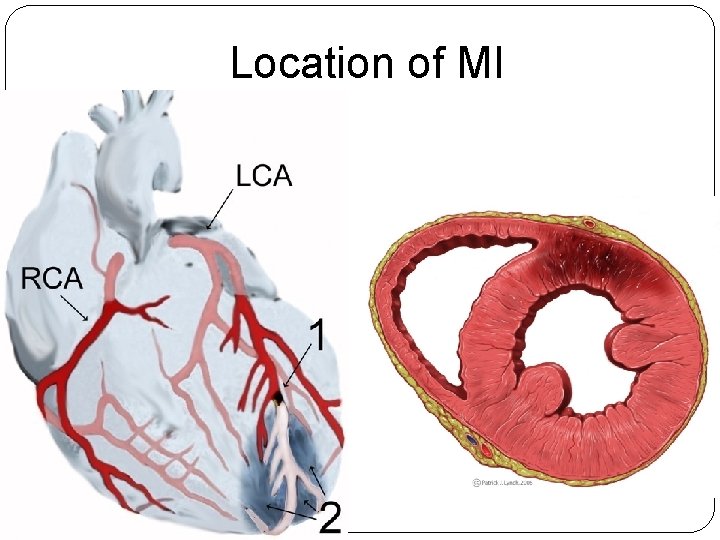
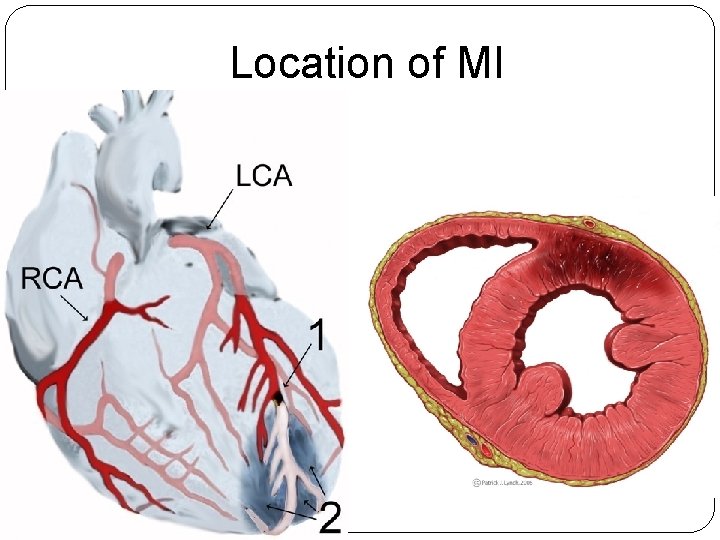
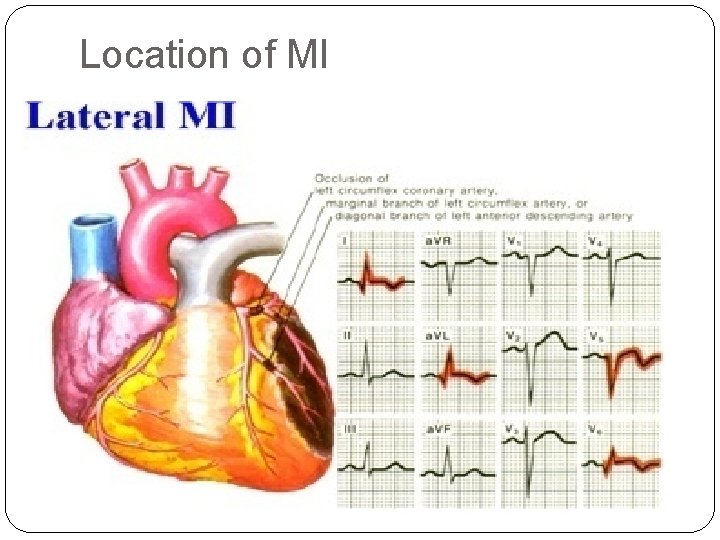
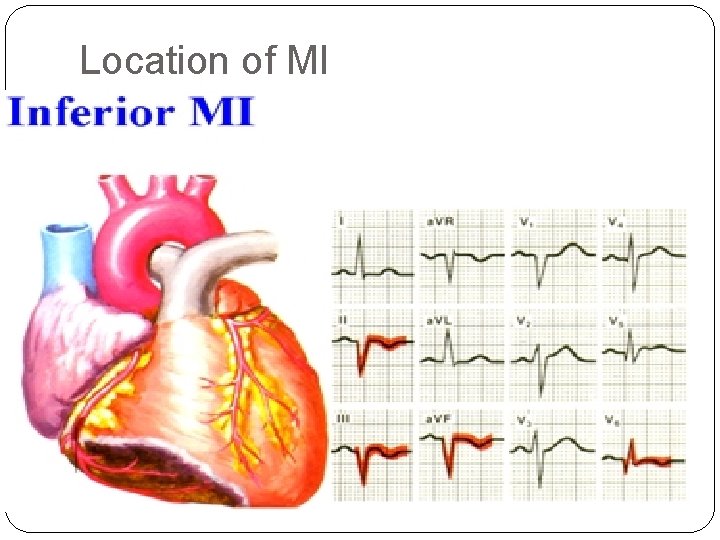
Location of MI
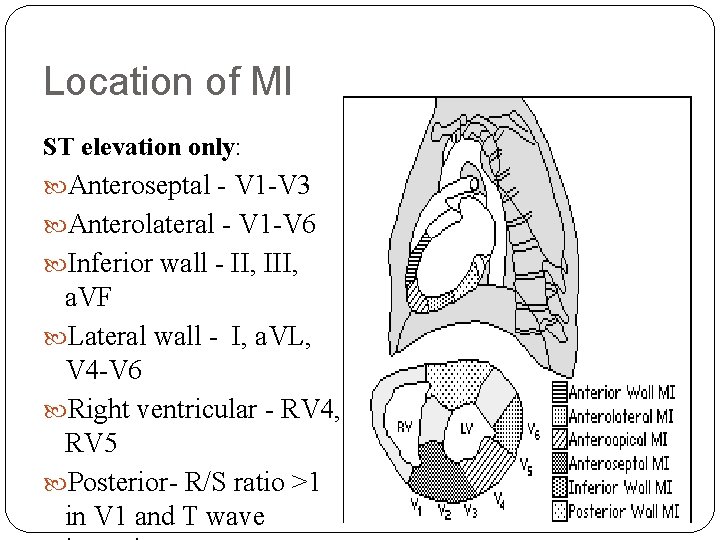
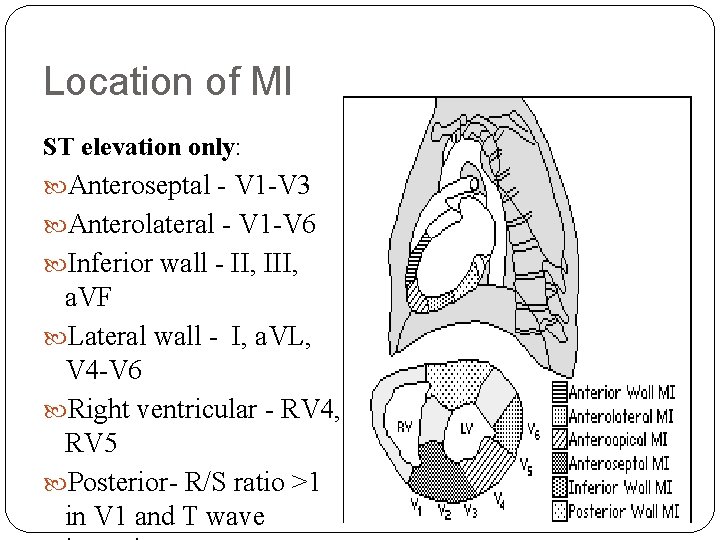
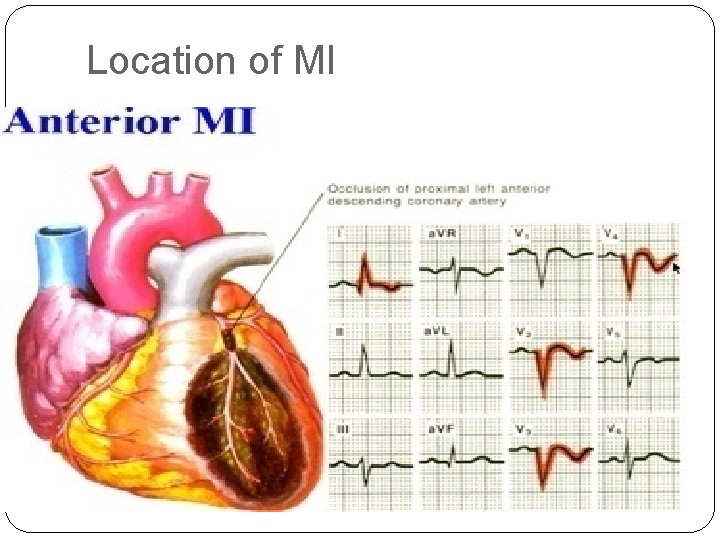
Location of MI ST elevation only: Anteroseptal - V 1 -V 3 Anterolateral - V 1 -V 6 Inferior wall - II, III, a. VF Lateral wall - I, a. VL, V 4 -V 6 Right ventricular - RV 4, RV 5 Posterior- R/S ratio >1 in V 1 and T wave
Location of MI
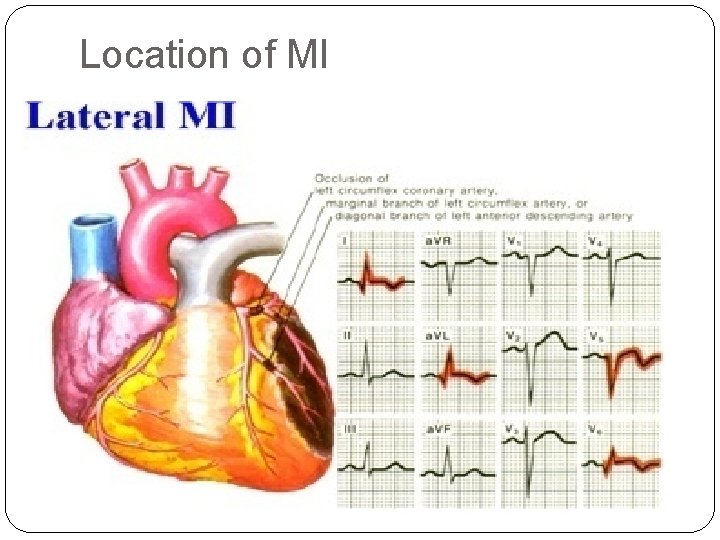
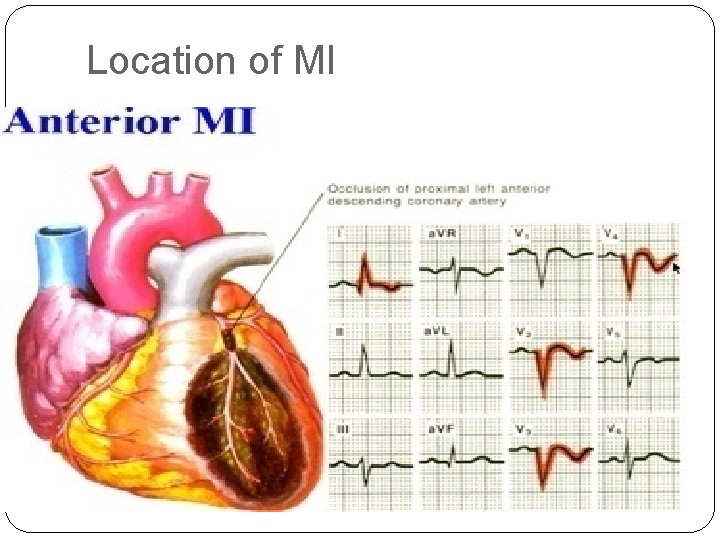
Location of MI
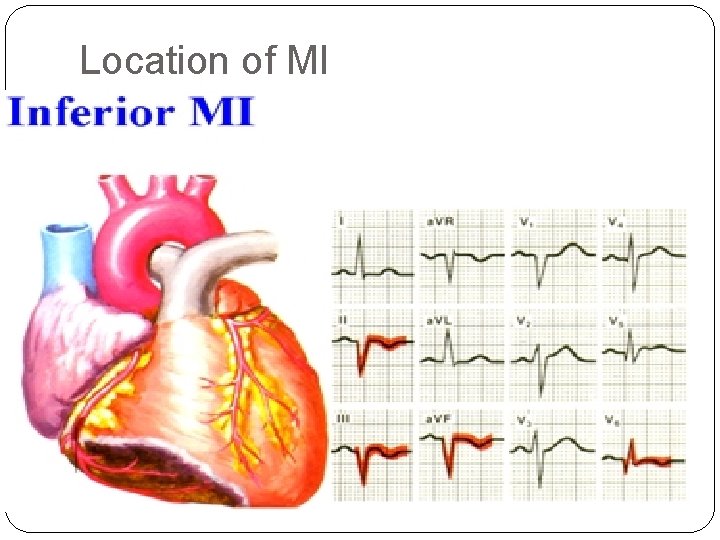
Location of MI
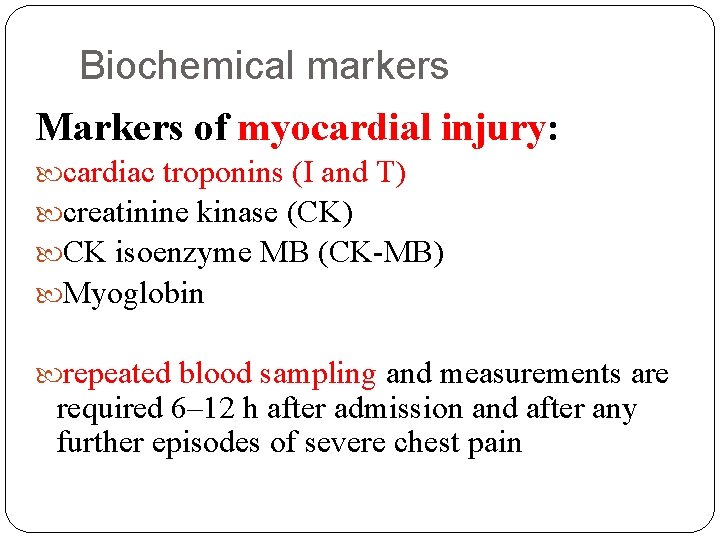
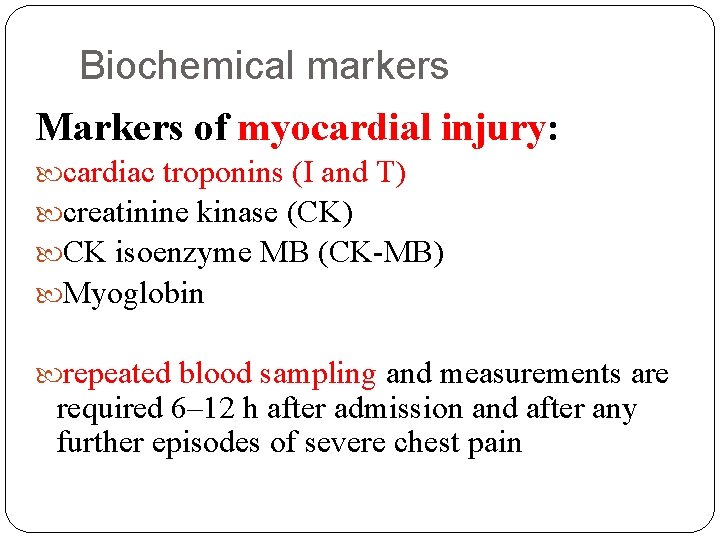
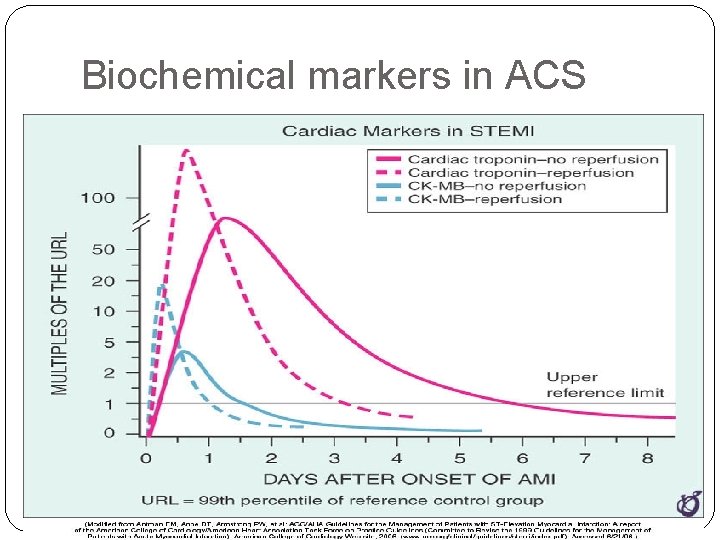
Biochemical markers Markers of myocardial injury: cardiac troponins (I and T) creatinine kinase (CK) CK isoenzyme MB (CK-MB) Myoglobin repeated blood sampling and measurements are required 6– 12 h after admission and after any further episodes of severe chest pain
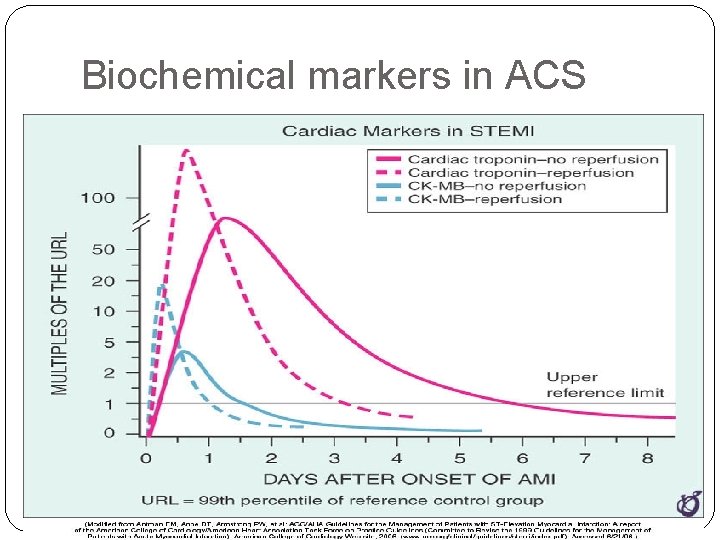
Biochemical markers in ACS
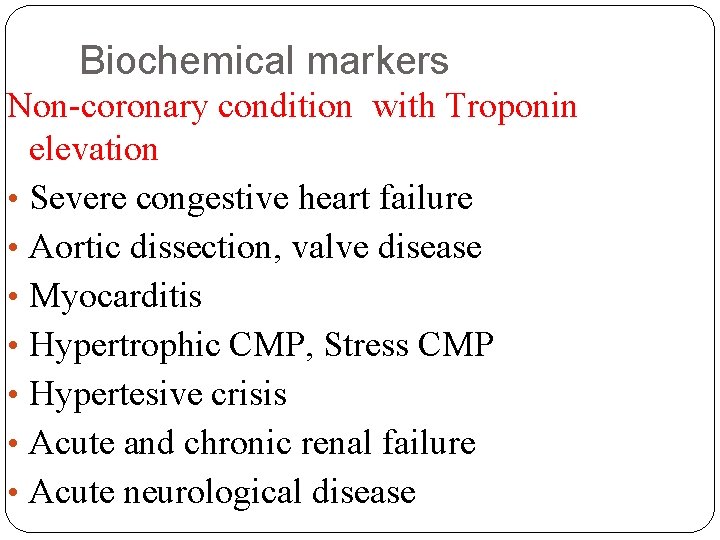
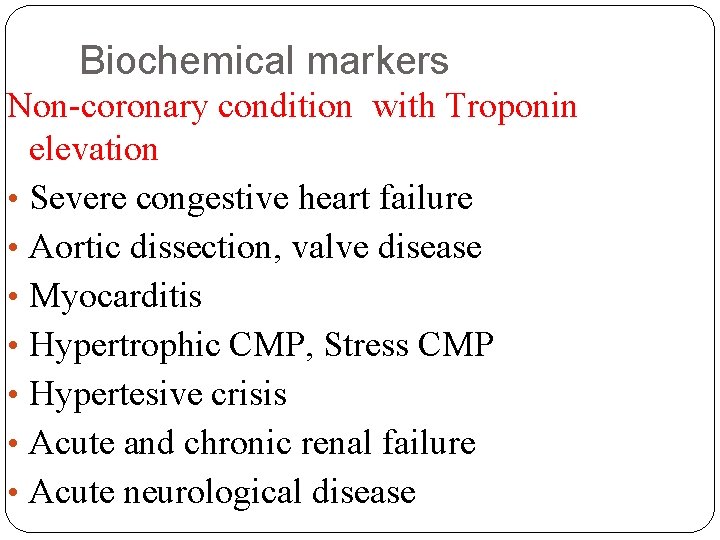
Biochemical markers Non-coronary condition with Troponin elevation • Severe congestive heart failure • Aortic dissection, valve disease • Myocarditis • Hypertrophic CMP, Stress CMP • Hypertesive crisis • Acute and chronic renal failure • Acute neurological disease
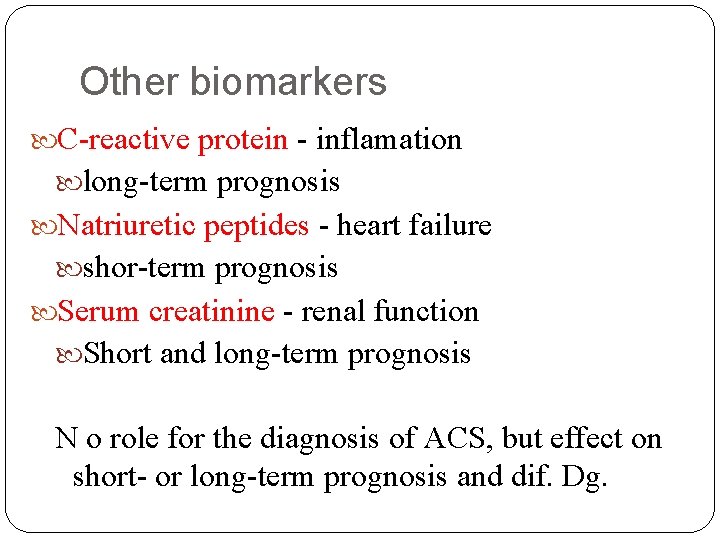
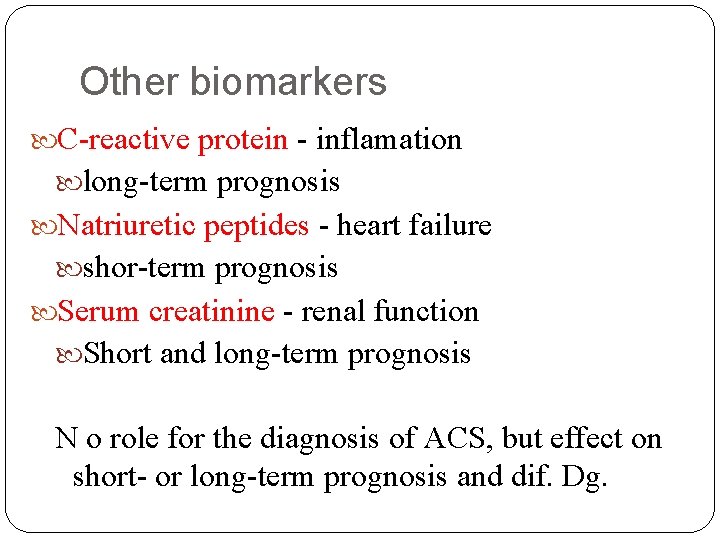
Other biomarkers C-reactive protein - inflamation long-term prognosis Natriuretic peptides - heart failure shor-term prognosis Serum creatinine - renal function Short and long-term prognosis N o role for the diagnosis of ACS, but effect on short- or long-term prognosis and dif. Dg.
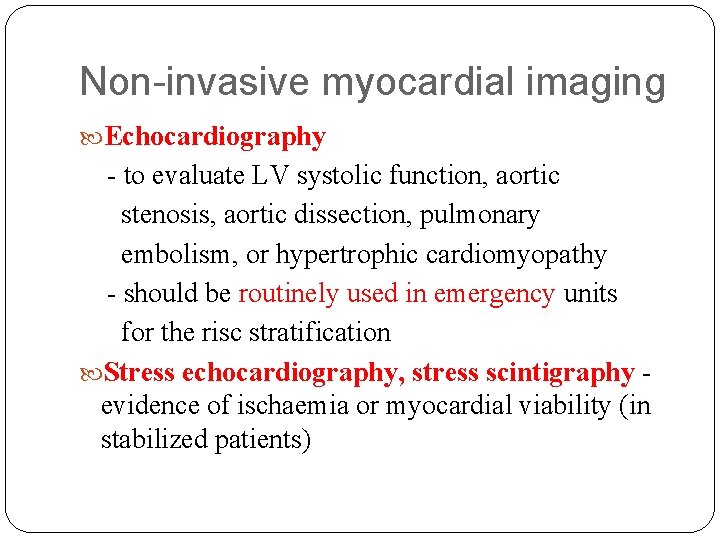
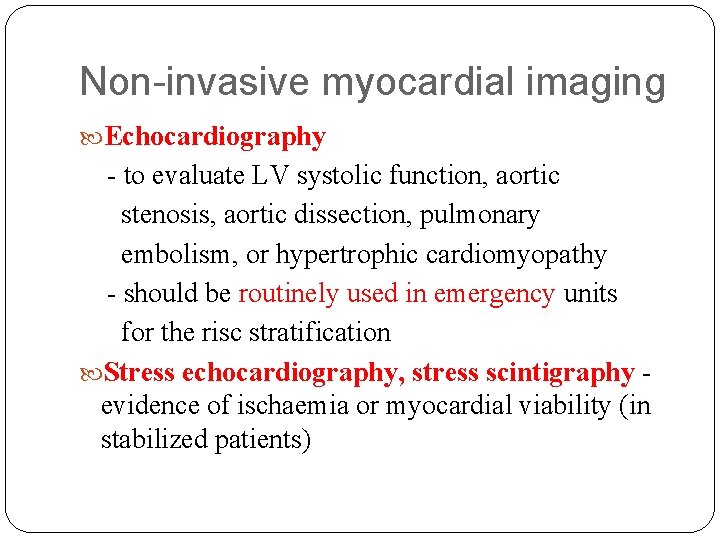
Non-invasive myocardial imaging Echocardiography - to evaluate LV systolic function, aortic stenosis, aortic dissection, pulmonary embolism, or hypertrophic cardiomyopathy - should be routinely used in emergency units for the risc stratification Stress echocardiography, stress scintigraphy evidence of ischaemia or myocardial viability (in stabilized patients)
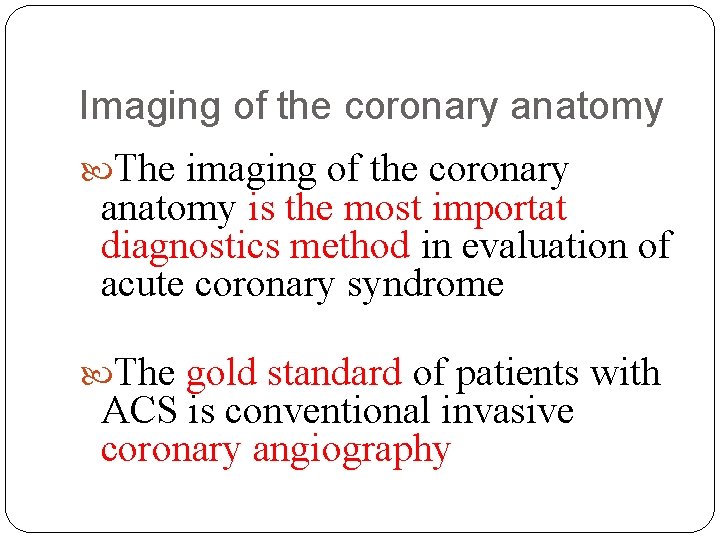
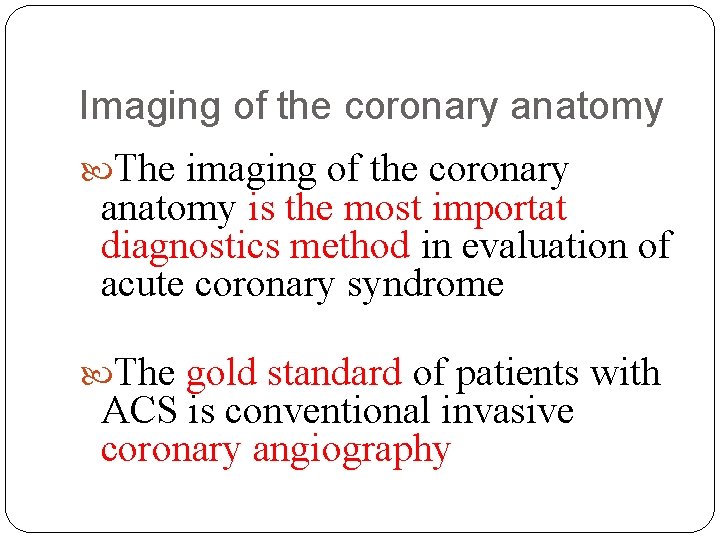
Imaging of the coronary anatomy The imaging of the coronary anatomy is the most importat diagnostics method in evaluation of acute coronary syndrome The gold standard of patients with ACS is conventional invasive coronary angiography
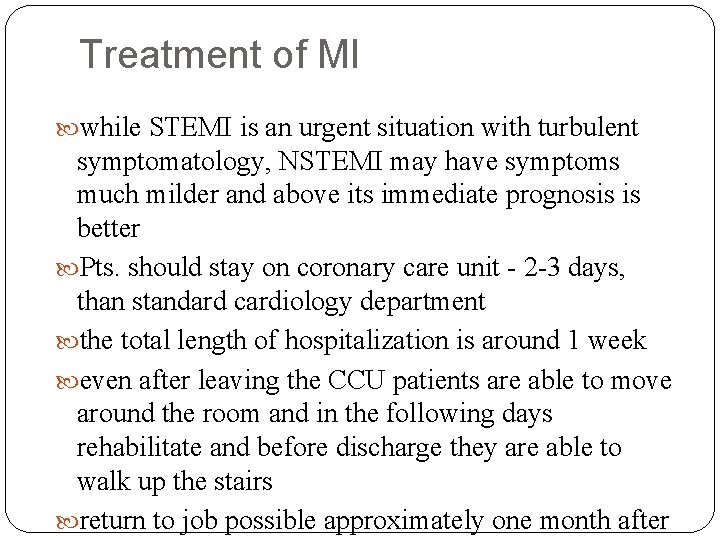
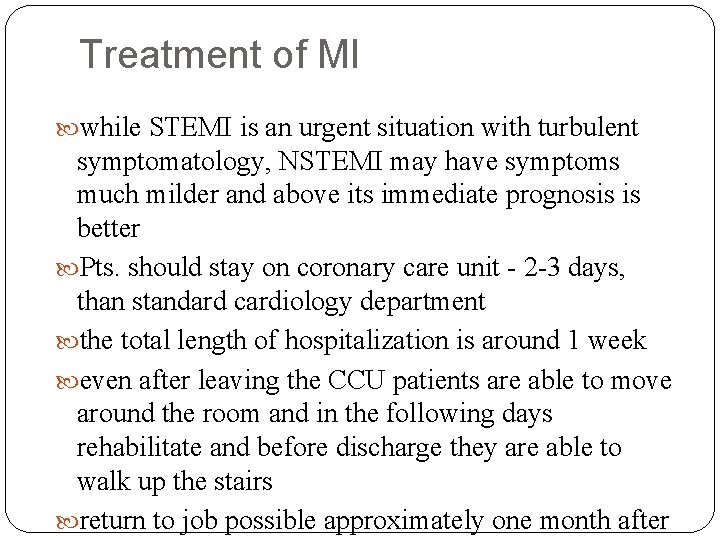
Treatment of MI while STEMI is an urgent situation with turbulent symptomatology, NSTEMI may have symptoms much milder and above its immediate prognosis is better Pts. should stay on coronary care unit - 2 -3 days, than standard cardiology department the total length of hospitalization is around 1 week even after leaving the CCU patients are able to move around the room and in the following days rehabilitate and before discharge they are able to walk up the stairs return to job possible approximately one month after
Treatment of STEMI Open the occluded artery as soon as possible to restore blood flow for the heart ‘‘Time is muscle“ Check for complication of myocardial infarction and treat them: arrhythmia heart failure bleeding
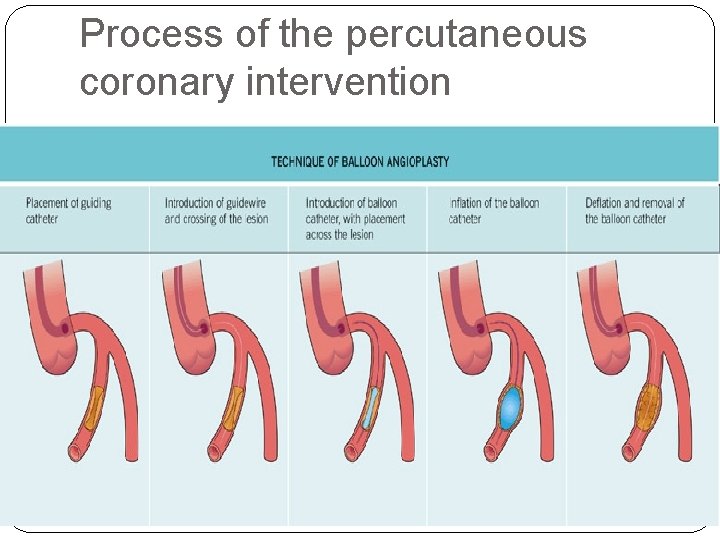
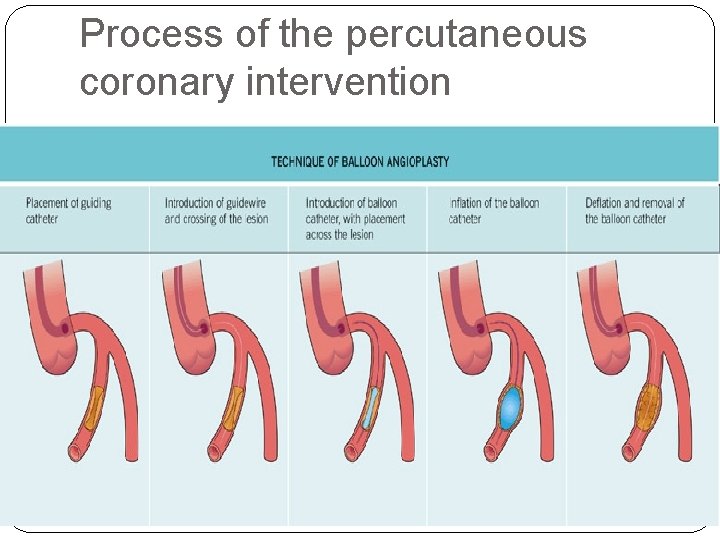
Process of the percutaneous coronary intervention
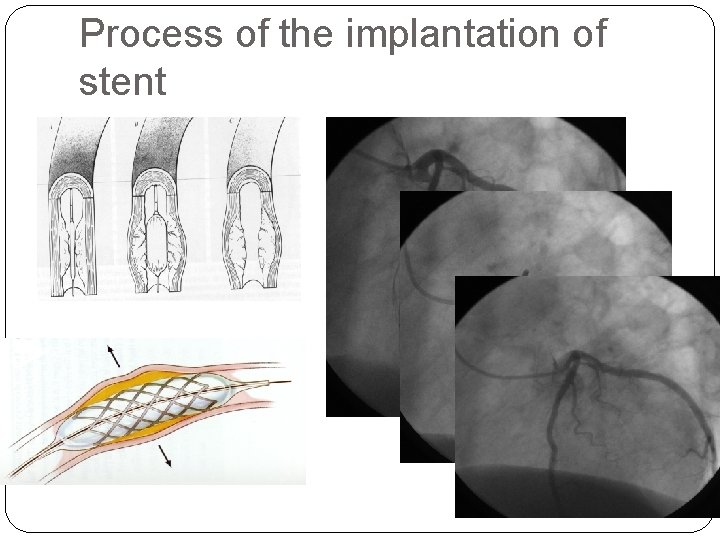
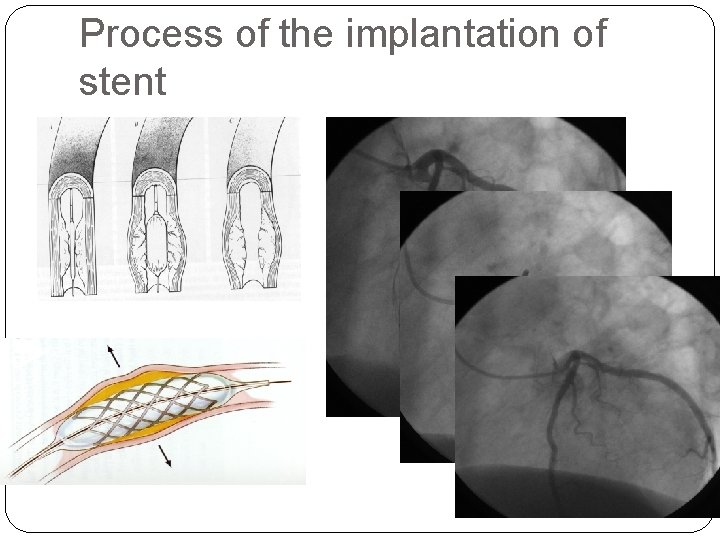
Process of the implantation of stent
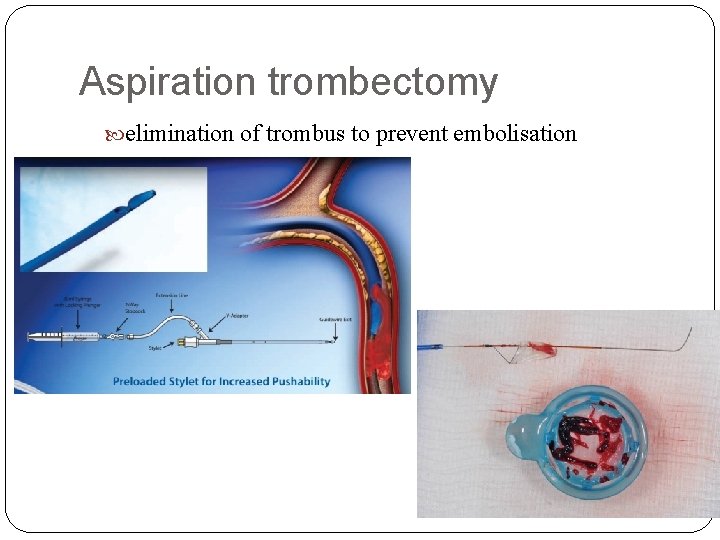
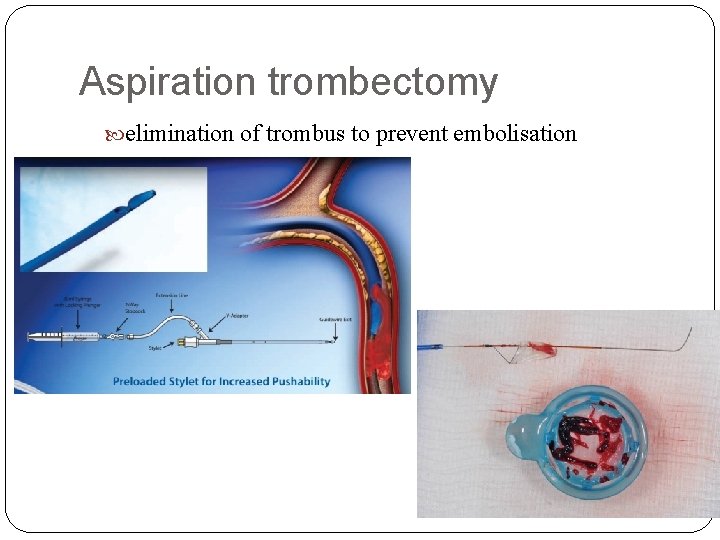
Aspiration trombectomy elimination of trombus to prevent embolisation
Pre-hospital management Antiplatelet therapy Acetylosalicid acid 400 -500 mg (i. v. or p. o. ), Clopidogrel 600 mg or ticagrelor 180 mg or prasugrel 60 mg Antithrombin therapy Heparin 5 000 - 10 000 IU i. v. or enoxaparine Resolve pain and fear analgesic drugs benzodiazepine
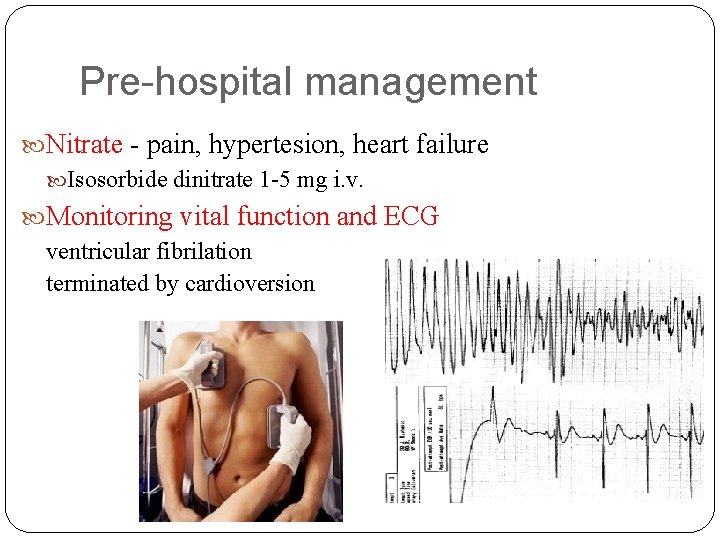
Pre-hospital management Nitrate - pain, hypertesion, heart failure Isosorbide dinitrate 1 -5 mg i. v. Monitoring vital function and ECG ventricular fibrilation terminated by cardioversion
Pre-hospital management Betablockers - tachycardia, hypertension Metoprolol - dose 25 -50 mg oral or 2 mg i. v. ACE inhibitors - hypertension Perindopril - dose 5 mg oral Diuretic - heart failure Furosemide 20 - 40 mg i. v. Anti-arrhythmic drugs -no prophylaxis Mesocain 1% 10 m. L i. v. Amiodarone 150 mg i. v. bolus
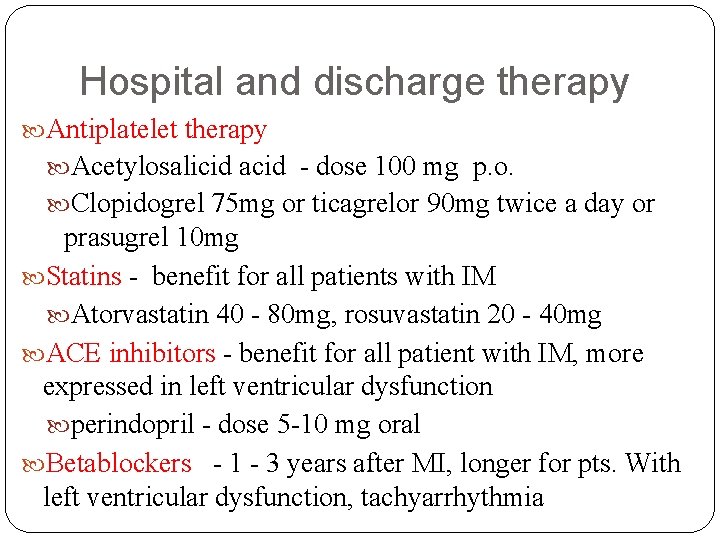
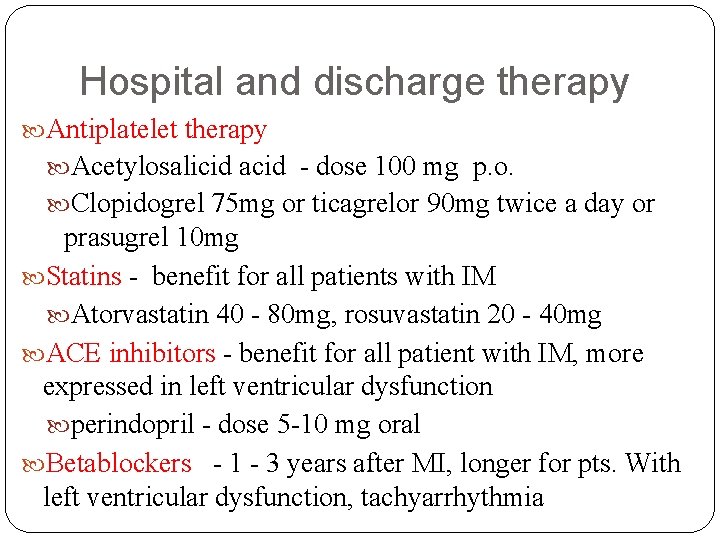
Hospital and discharge therapy Antiplatelet therapy Acetylosalicid acid - dose 100 mg p. o. Clopidogrel 75 mg or ticagrelor 90 mg twice a day or prasugrel 10 mg Statins - benefit for all patients with IM Atorvastatin 40 - 80 mg, rosuvastatin 20 - 40 mg ACE inhibitors - benefit for all patient with IM, more expressed in left ventricular dysfunction perindopril - dose 5 -10 mg oral Betablockers - 1 - 3 years after MI, longer for pts. With left ventricular dysfunction, tachyarrhythmia
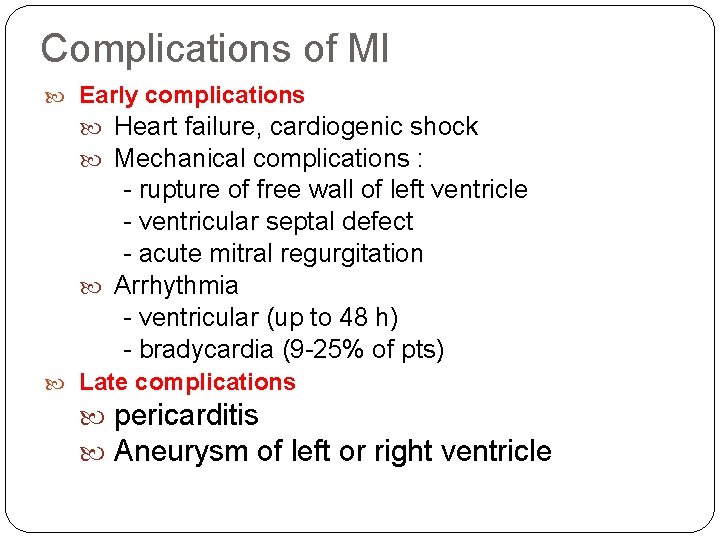
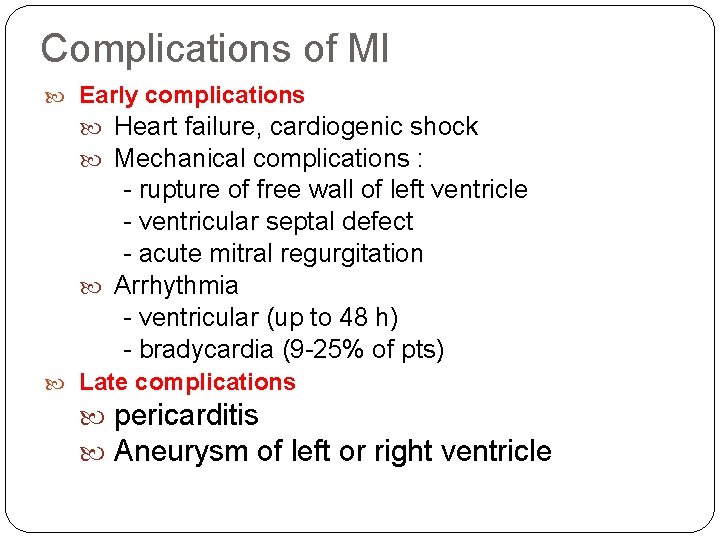
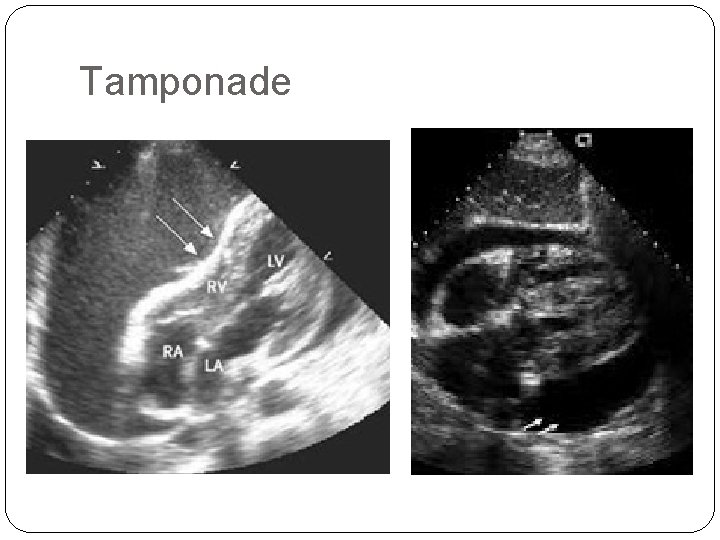
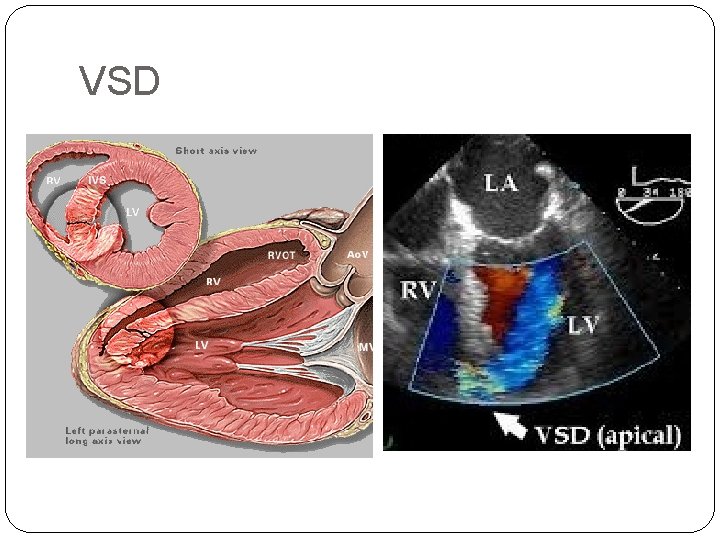
Complications of MI Early complications Heart failure, cardiogenic shock Mechanical complications : - rupture of free wall of left ventricle - ventricular septal defect - acute mitral regurgitation Arrhythmia - ventricular (up to 48 h) - bradycardia (9 -25% of pts) Late complications pericarditis Aneurysm of left or right ventricle
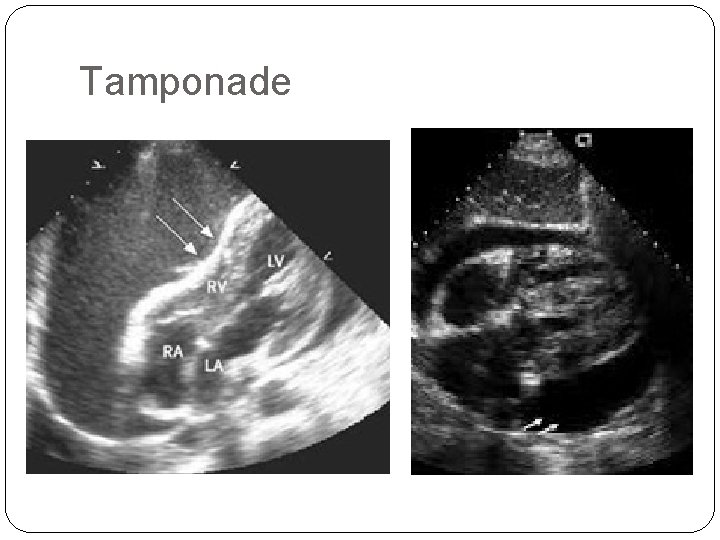
Tamponade
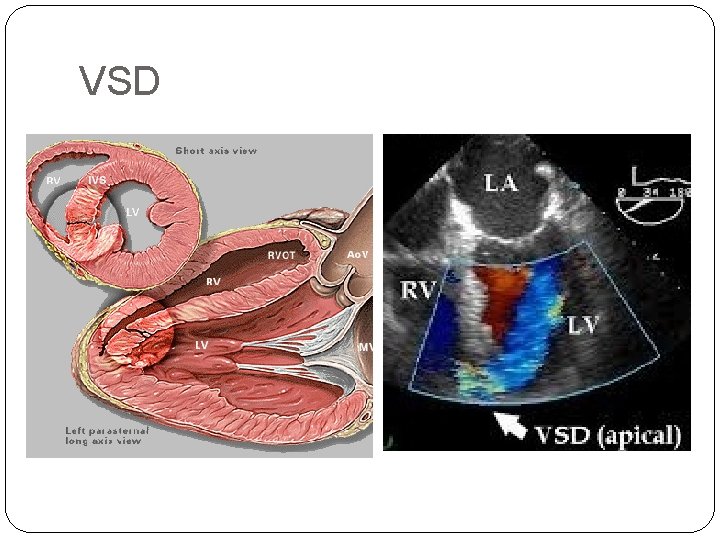
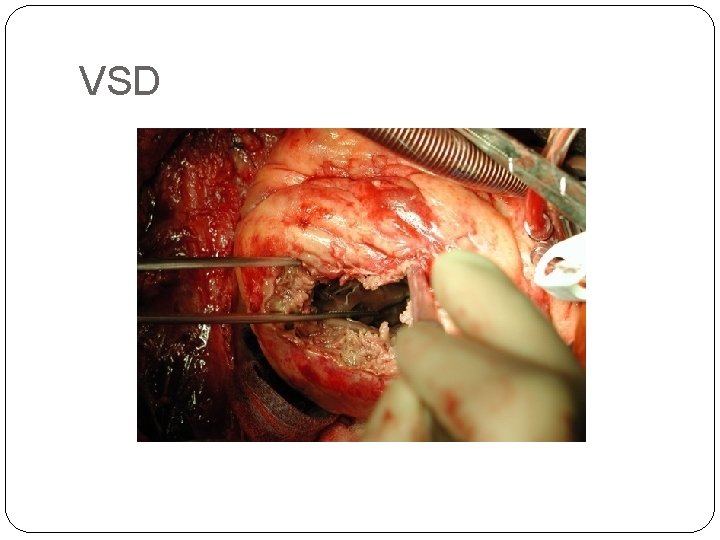
VSD
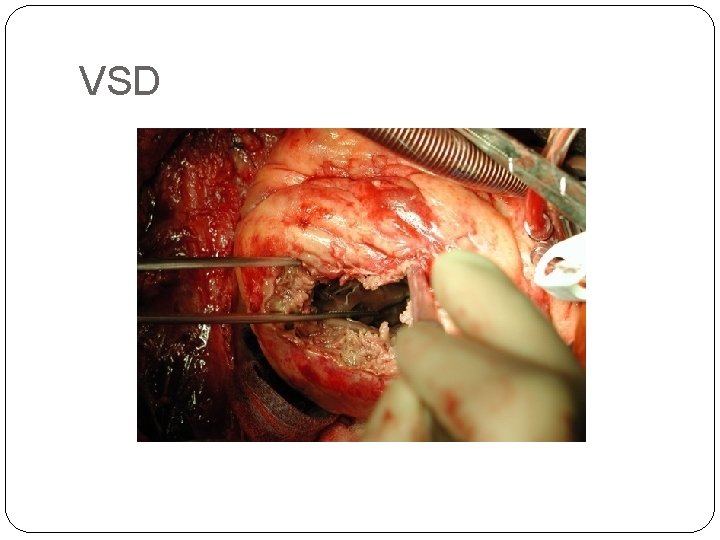
VSD
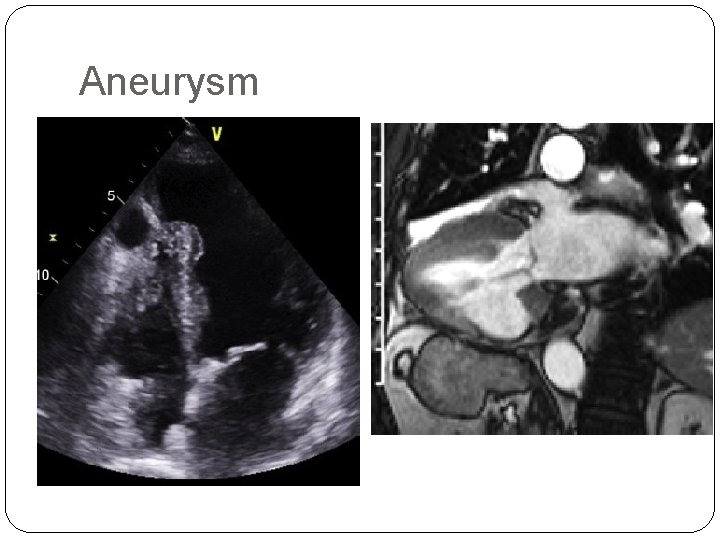
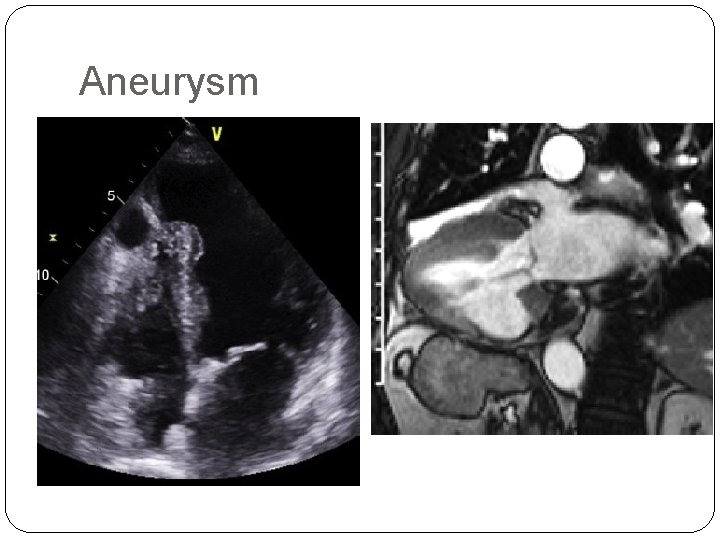
Aneurysm
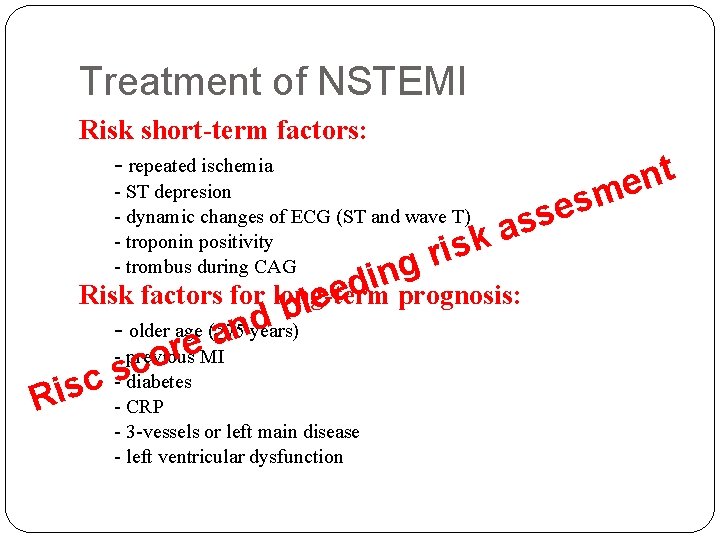
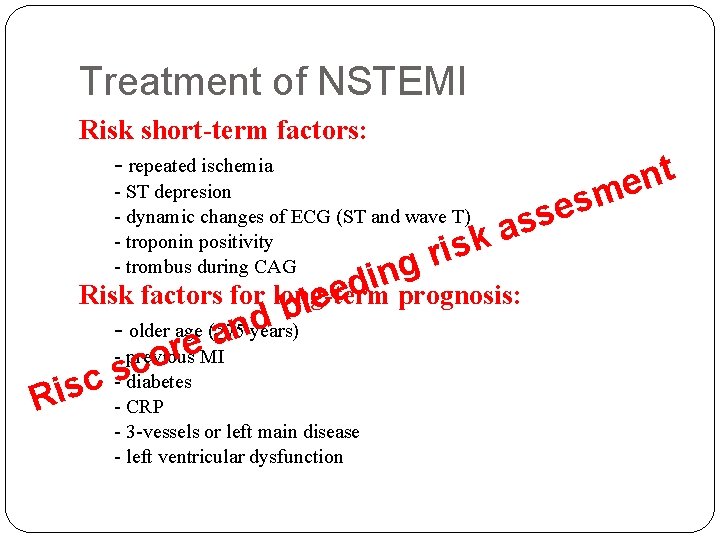
Treatment of NSTEMI Risk short-term factors: - repeated ischemia - ST depresion - dynamic changes of ECG (ST and wave T) - troponin positivity - trombus during CAG sk i r g s e ass n i d e Risk factors for long-term prognosis: e l b d - older age (≥ 75 years) n a e. MI r - previous o c s sc - diabetes Ri - CRP - 3 -vessels or left main disease - left ventricular dysfunction t n me
Treatment of NSTE-ACS To immediate examination are indicated patients with: history of CAD or previous revascularization severe recurrent angina left ventricular dysfunction, heart failure or ventricular arrhythmias
Treatment of NSTE-ACSvs. STE thrombolysis is not at NSTEMI used the base of treatment is again antithrombotic therapy and revascularization - mostly via PCI in patients with multiple coronary disease more frequently to surgery revascularization
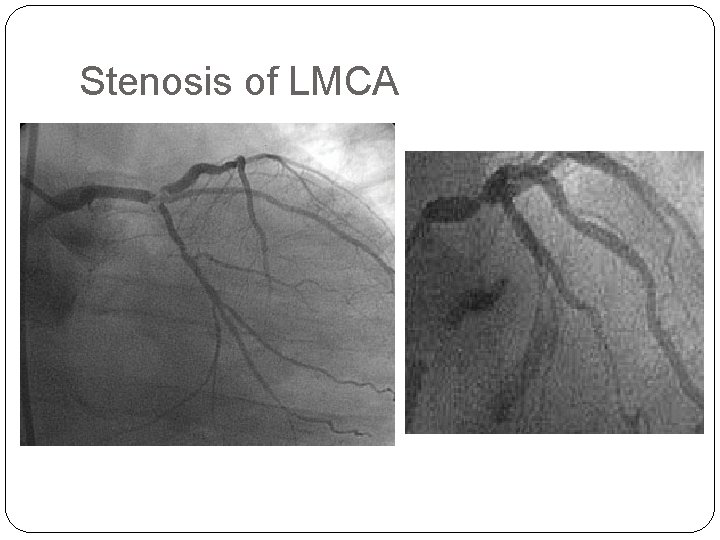
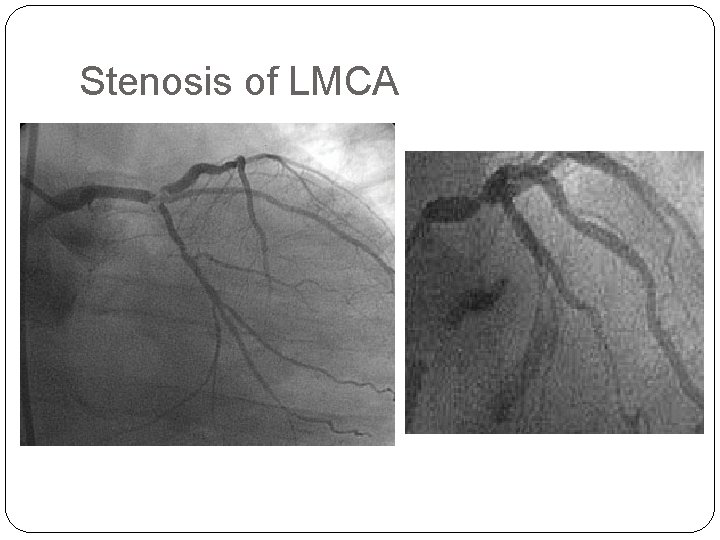
Stenosis of LMCA
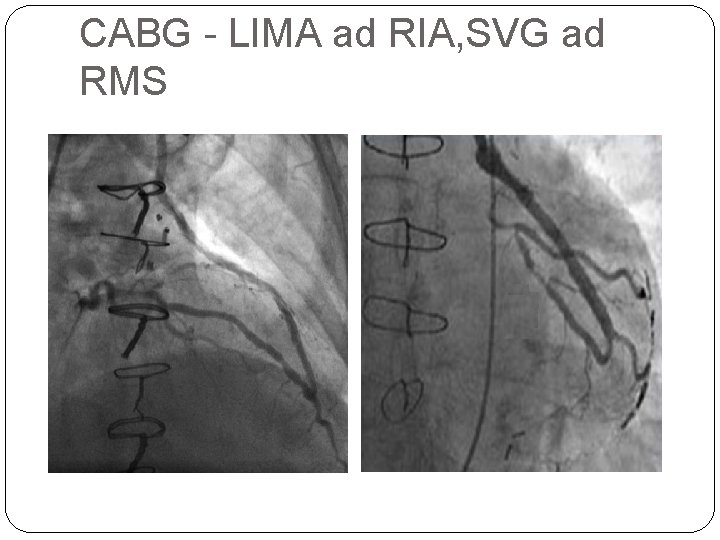
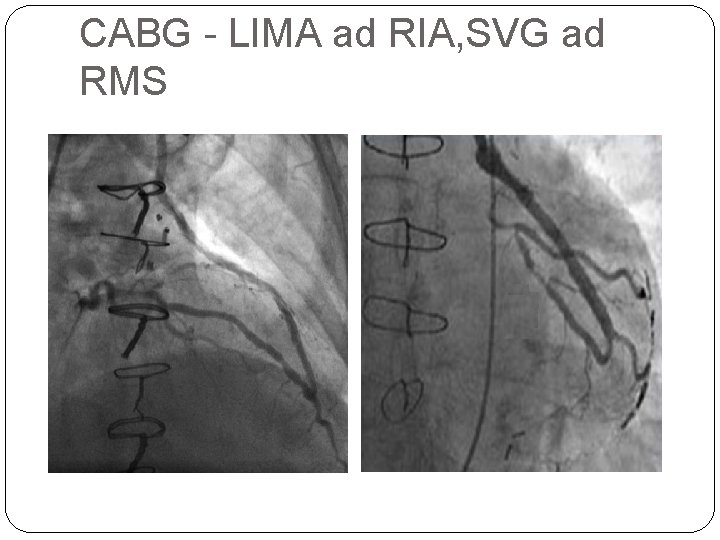
CABG - LIMA ad RIA, SVG ad RMS
Thank you for your attention
 R latha devi
R latha devi Global registry of acute coronary events
Global registry of acute coronary events Acute coronary syndrome
Acute coronary syndrome Cerebellar syndromes
Cerebellar syndromes Neuroendocrine syndrome in gynecology
Neuroendocrine syndrome in gynecology Differential diagnosis of stroke
Differential diagnosis of stroke N
N Cerebellar syndromes
Cerebellar syndromes What is geriatric syndromes
What is geriatric syndromes Devi personality type
Devi personality type Chandi prasad bhatt quotes
Chandi prasad bhatt quotes Language planning
Language planning Devi parikh
Devi parikh Io devo tu devi
Io devo tu devi Citate despre erotism
Citate despre erotism Aditi devi bhava
Aditi devi bhava Devi parikh
Devi parikh The hunt by mahasweta devi question answer
The hunt by mahasweta devi question answer Ic ambrogio lorenzetti
Ic ambrogio lorenzetti Om prano devi saraswati mantra
Om prano devi saraswati mantra Devi pratami
Devi pratami Devi parikh
Devi parikh Srimati devi indira
Srimati devi indira Matematta
Matematta Digilogous
Digilogous Cardiac output animation
Cardiac output animation Mesa coronary calcium score
Mesa coronary calcium score Ischemic heart disease classification
Ischemic heart disease classification Coronary personality
Coronary personality Cardiac plexus
Cardiac plexus Dr eter
Dr eter Coronary heart disease
Coronary heart disease Coronary blood flow
Coronary blood flow Coronary steal
Coronary steal Pulmonary trunk
Pulmonary trunk Coronary circulation of heart
Coronary circulation of heart Pk papyrus covered coronary stent system
Pk papyrus covered coronary stent system The pulmonary semilunar valve
The pulmonary semilunar valve Coronary artery disease
Coronary artery disease Spider view cag
Spider view cag Coronary circulatory routes
Coronary circulatory routes Ischemic heart disease
Ischemic heart disease Good morning blood
Good morning blood 3 main functions heart
3 main functions heart Pk papyrus stent
Pk papyrus stent Where is the pulmonary semilunar valve located
Where is the pulmonary semilunar valve located Flow of coronary circulation
Flow of coronary circulation Ali sepahdari
Ali sepahdari Cpr routine
Cpr routine Coronary calcium score guidelines
Coronary calcium score guidelines Coronary artery disease pathophysiology
Coronary artery disease pathophysiology Circulatory system crash course
Circulatory system crash course Annulus of vieussens
Annulus of vieussens Coronary sulcus
Coronary sulcus Bursa omentum
Bursa omentum Mesa coronary calcium score
Mesa coronary calcium score Intracapsular but extrasynovial
Intracapsular but extrasynovial Right and left aortic sinus
Right and left aortic sinus Qfr coronary
Qfr coronary Is gout like arthritis
Is gout like arthritis Acute gingival infections
Acute gingival infections Patho
Patho Acute interstitial nephritis urine findings
Acute interstitial nephritis urine findings @nezupoi: title : she is working out chp.14
@nezupoi: title : she is working out chp.14 Pernicious anemia vs megaloblastic anemia
Pernicious anemia vs megaloblastic anemia Whats an acute angle
Whats an acute angle What is a negative acute phase protein
What is a negative acute phase protein