Trauma Zhanfei Li MD Ph D Associate professor

- Slides: 90
Trauma Zhanfei Li. MD &Ph. D Associate professor and attending surgeon Division of Traumatic Surgery, TJH
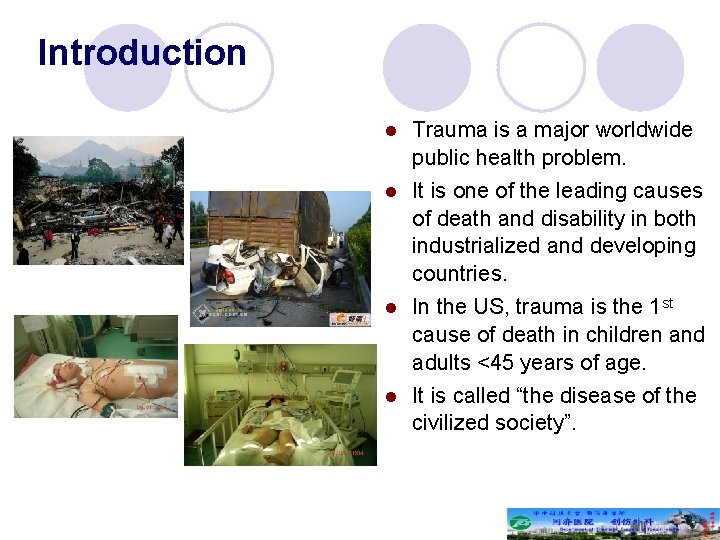
Introduction l l Trauma is a major worldwide public health problem. It is one of the leading causes of death and disability in both industrialized and developing countries. In the US, trauma is the 1 st cause of death in children and adults <45 years of age. It is called “the disease of the civilized society”.
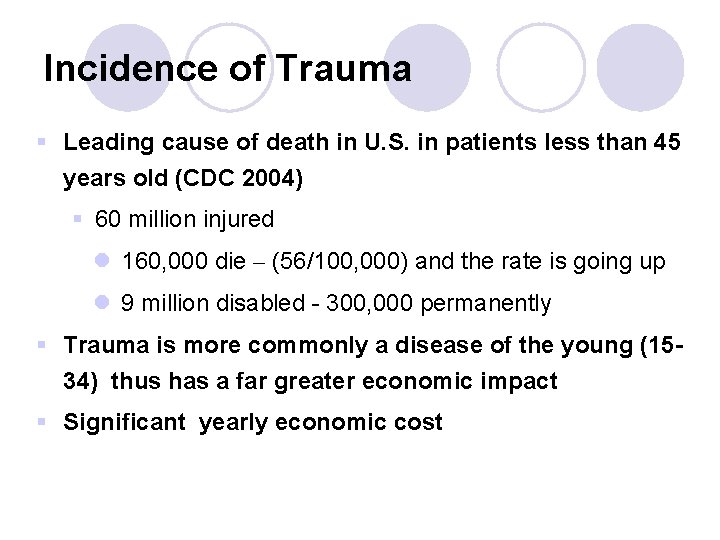
Incidence of Trauma § Leading cause of death in U. S. in patients less than 45 years old (CDC 2004) § 60 million injured l 160, 000 die – (56/100, 000) and the rate is going up l 9 million disabled - 300, 000 permanently § Trauma is more commonly a disease of the young (1534) thus has a far greater economic impact § Significant yearly economic cost
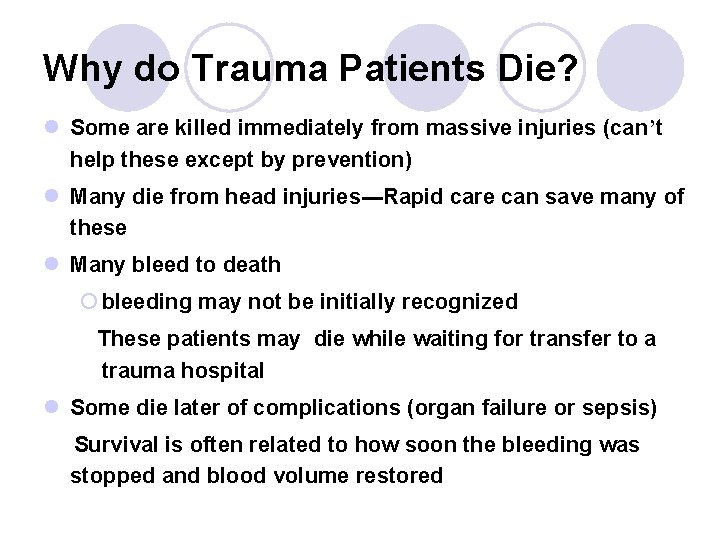
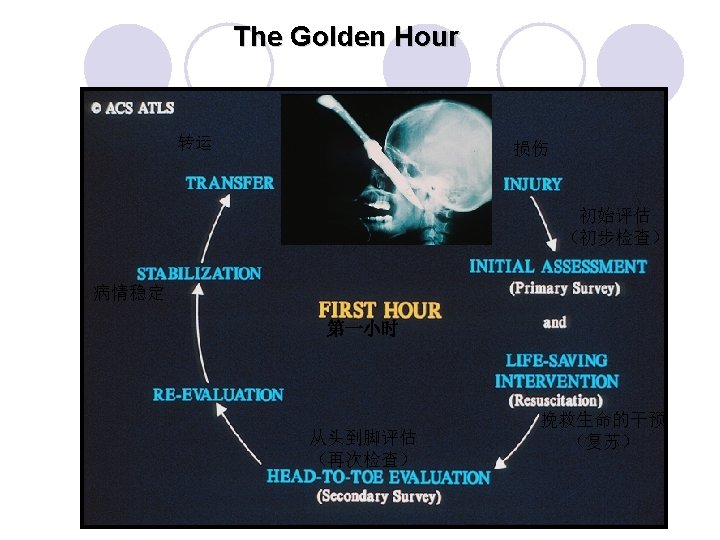
Why do Trauma Patients Die? l Some are killed immediately from massive injuries (can’t help these except by prevention) l Many die from head injuries---Rapid care can save many of these l Many bleed to death ¡ bleeding may not be initially recognized These patients may die while waiting for transfer to a trauma hospital l Some die later of complications (organ failure or sepsis) Survival is often related to how soon the bleeding was stopped and blood volume restored
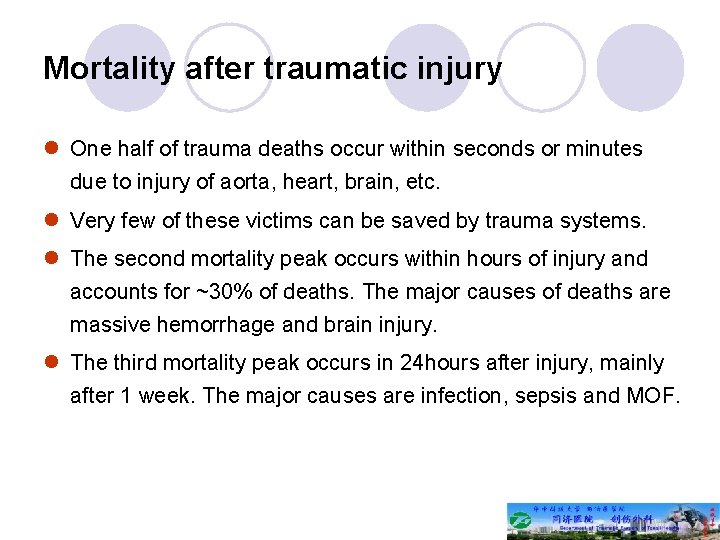
Mortality after traumatic injury l One half of trauma deaths occur within seconds or minutes due to injury of aorta, heart, brain, etc. l Very few of these victims can be saved by trauma systems. l The second mortality peak occurs within hours of injury and accounts for ~30% of deaths. The major causes of deaths are massive hemorrhage and brain injury. l The third mortality peak occurs in 24 hours after injury, mainly after 1 week. The major causes are infection, sepsis and MOF.
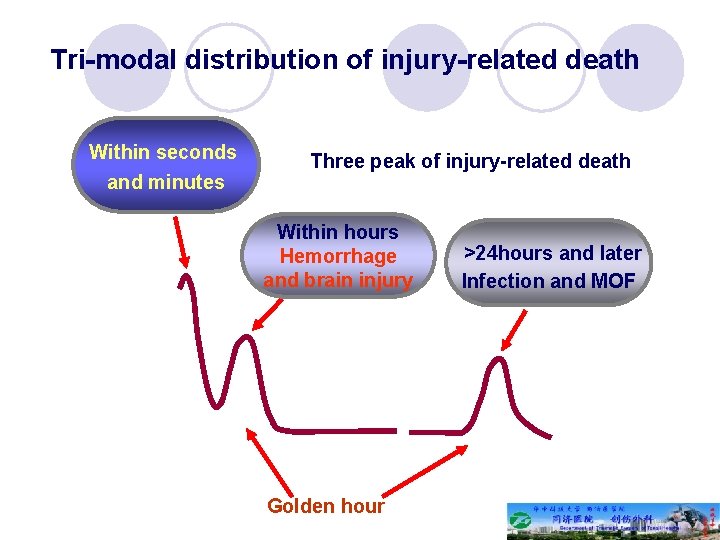
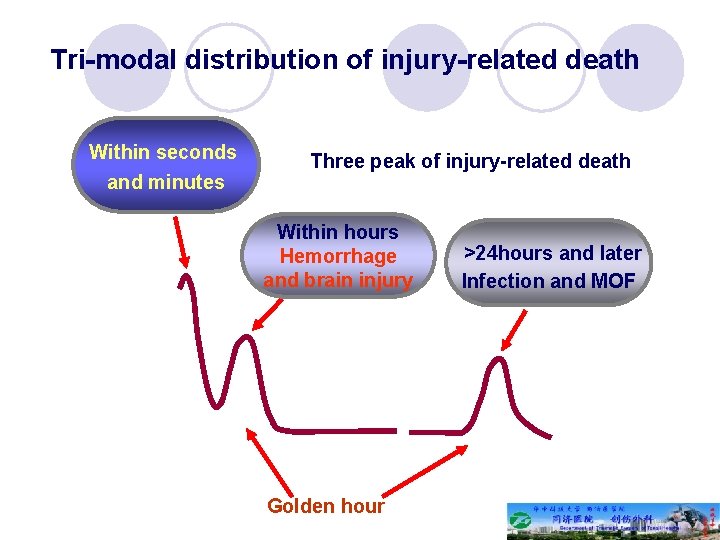
Tri-modal distribution of injury-related death Within seconds and minutes Three peak of injury-related death Within hours Hemorrhage and brain injury Golden hour >24 hours and later Infection and MOF
Development of trauma care l Modern trauma care has evolved from the close relation of surgery and casualty management in war. l Many important concepts, including prehospital transport, volume resuscitation, life support and critical care have been advanced based on the observations during war. l The first organized trauma unit opened in 1961 at the University of Maryland. l Trauma care requires collaboration of pre-hospital care, ER, multiple disciplines (general surgery, neurosurgery, orthopaedic surgery, thoracic surgery, vascular surgery, as well as rehabilitation.
A System Saving Lives SURVIVOR OR STATISTIC?
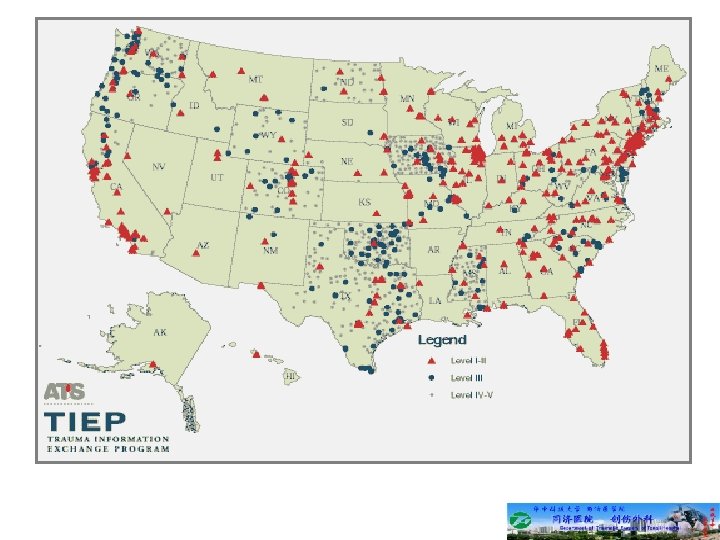
Trauma System l Organized system within a given region including prehospital care, acute hospital care, and rehabilitation
Trauma System A trauma system involves trauma centers working together with 9 -1 -1, EMTs, ambulances, helicopters, and other health care resources in a coordinated and preplanned way. This network of care is designed to get seriously injured people to the place with the right resources as quickly as possible
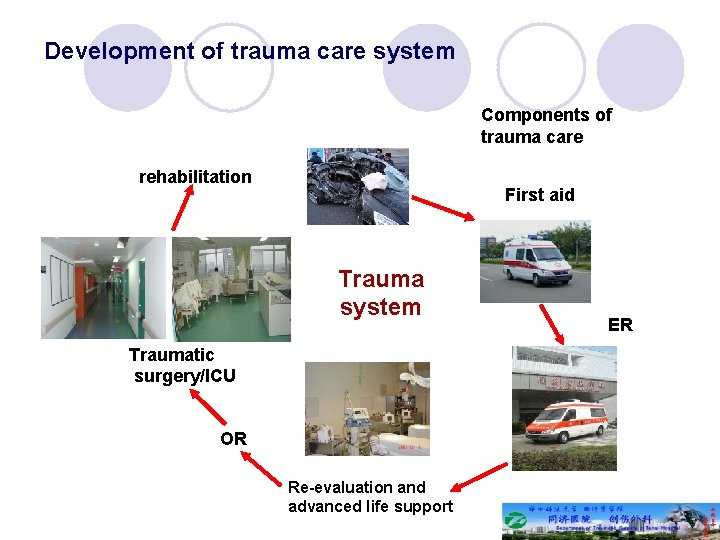
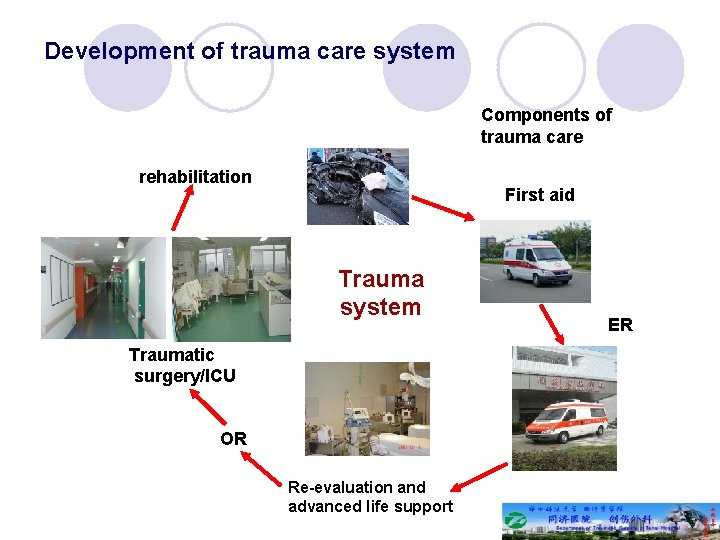
Development of trauma care system Components of trauma care rehabilitation First aid Trauma system Traumatic surgery/ICU OR Re-evaluation and advanced life support ER
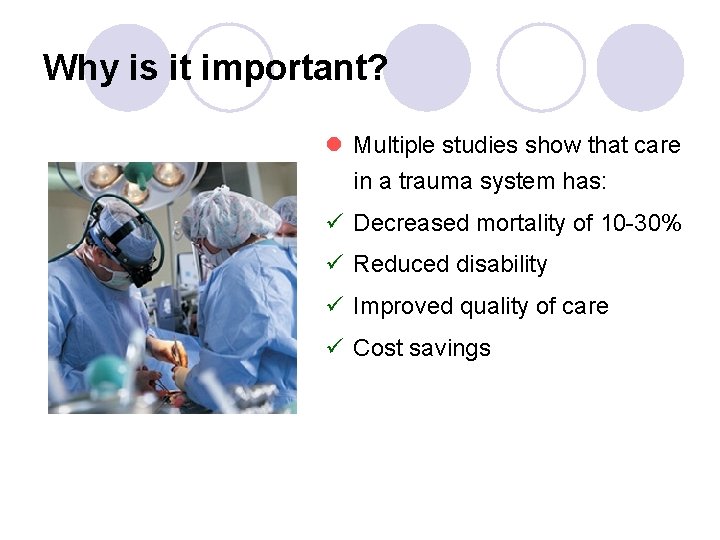
Why is it important? l Multiple studies show that care in a trauma system has: ü Decreased mortality of 10 -30% ü Reduced disability ü Improved quality of care ü Cost savings
Trauma Center Trauma centers are selected hospitals that provide a full range of care for severely injured patients 24 hours a day, seven days a week. The trauma care includes ready-to-go teams that perform immediate surgery and other necessary procedures for people with lifethreatening injuries, for example, due to car accident, burn, bad fall, or gunshot.
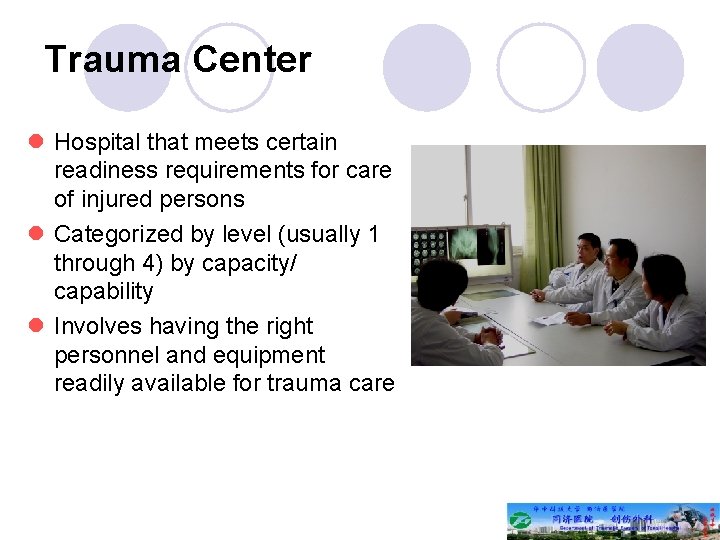
Trauma Center l Hospital that meets certain readiness requirements for care of injured persons l Categorized by level (usually 1 through 4) by capacity/ capability l Involves having the right personnel and equipment readily available for trauma care
Trauma Center Designation T T
How does the System Save Lives? l It correctly identifies the patients who need trauma care l Anticipates the resources needed to treat the patients l Locates the available needed resources l Routes the patient “right” the first time to reduce time to appropriate care l Arranges interfacility transfers if needed to reduce time to appropriate care l Improves care by the QI process and Research activity
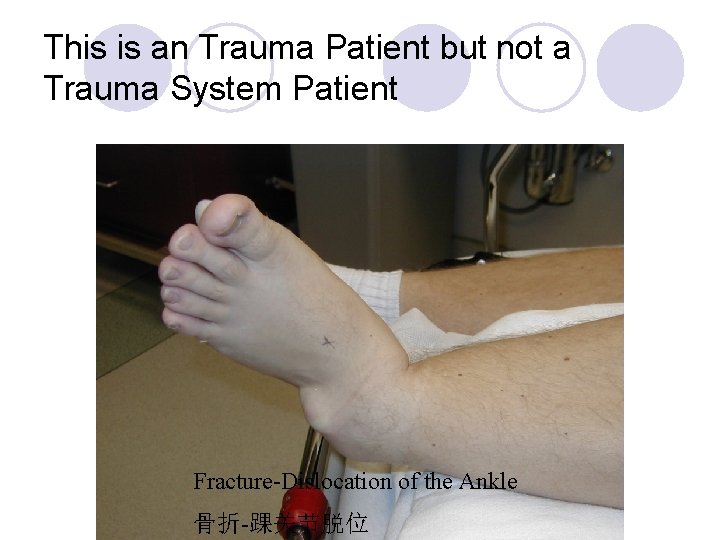
Who is a “Trauma System” Patient? l A “trauma” patient is any patient who is injured l Most injuries are minor and should be treated at a local community hospital l Less than 10% of patients with injuries need to go to a trauma center. These are Trauma System patients. l A “Trauma System” patient has life-threatening injuries that require rapid, specialized care. Examples are: l Injured patients with signs of shock l Injured patients with airway problems l Head or spinal injuries l Multiple long bone fractures l Ejection from vehicle l Major burns or smaller burns with other injuries
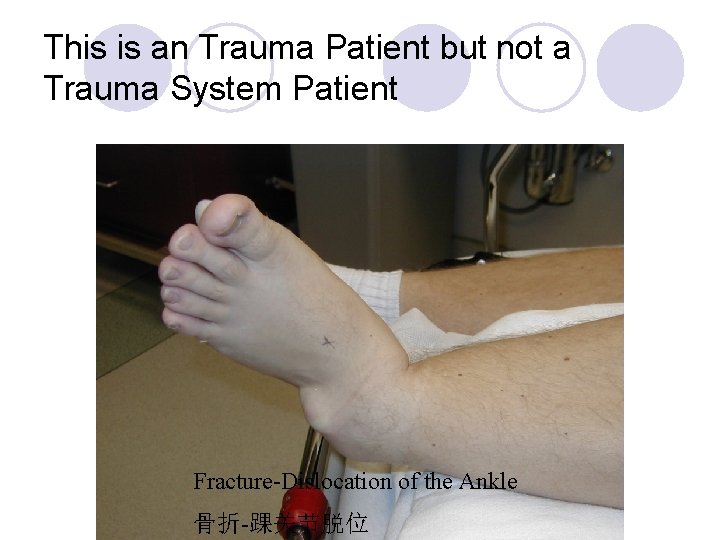
This is an Trauma Patient but not a Trauma System Patient Fracture-Dislocation of the Ankle 骨折-踝关节脱位
This is a Trauma System Patient
What are the Qualities of a Good Trauma System? l Network of hospitals with the commitment and the resources to care for trauma system patients l Organized plan to route critical patients to the right hospital that is ready to care for them l Constant monitoring of the system to correct problems, improve the system, and validate the quality of care provided
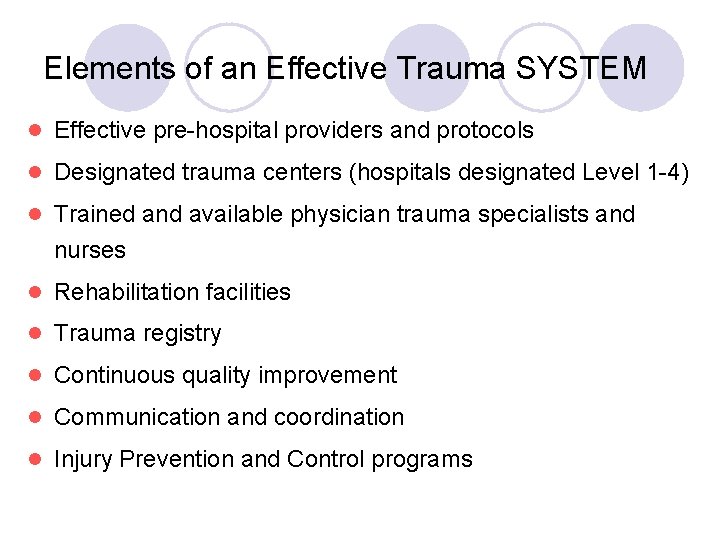
Elements of an Effective Trauma SYSTEM l Effective pre-hospital providers and protocols l Designated trauma centers (hospitals designated Level 1 -4) l Trained and available physician trauma specialists and nurses l Rehabilitation facilities l Trauma registry l Continuous quality improvement l Communication and coordination l Injury Prevention and Control programs
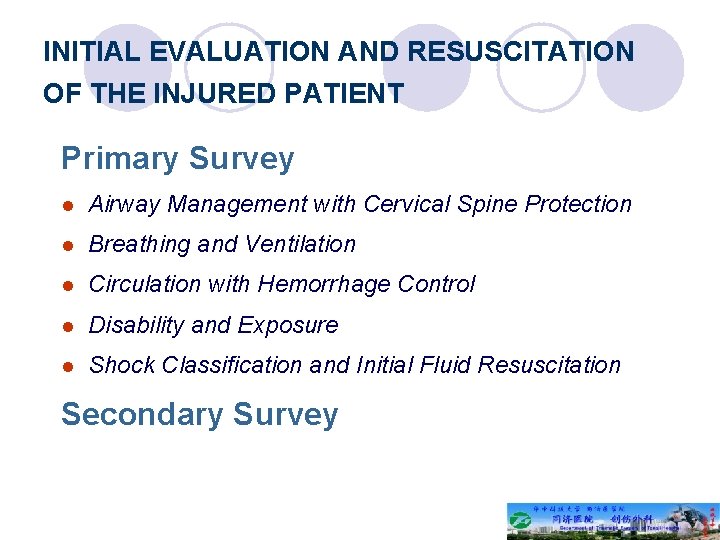
INITIAL EVALUATION AND RESUSCITATION OF THE INJURED PATIENT Primary Survey l Airway Management with Cervical Spine Protection l Breathing and Ventilation l Circulation with Hemorrhage Control l Disability and Exposure l Shock Classification and Initial Fluid Resuscitation Secondary Survey
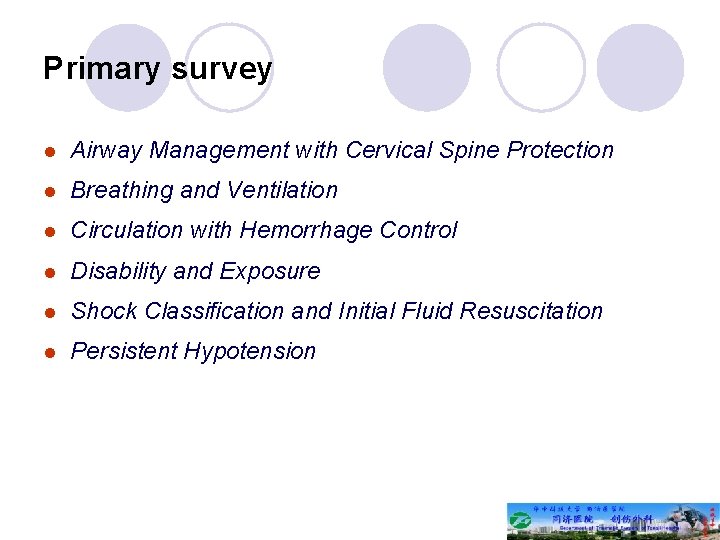
Primary survey l Airway Management with Cervical Spine Protection l Breathing and Ventilation l Circulation with Hemorrhage Control l Disability and Exposure l Shock Classification and Initial Fluid Resuscitation l Persistent Hypotension
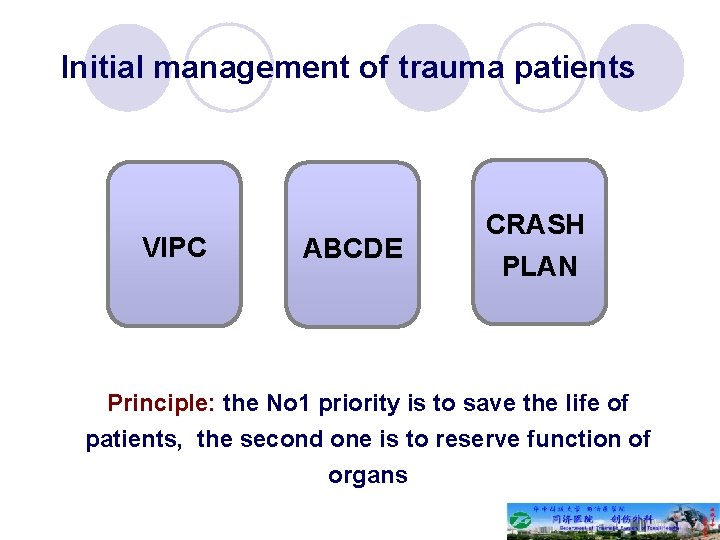
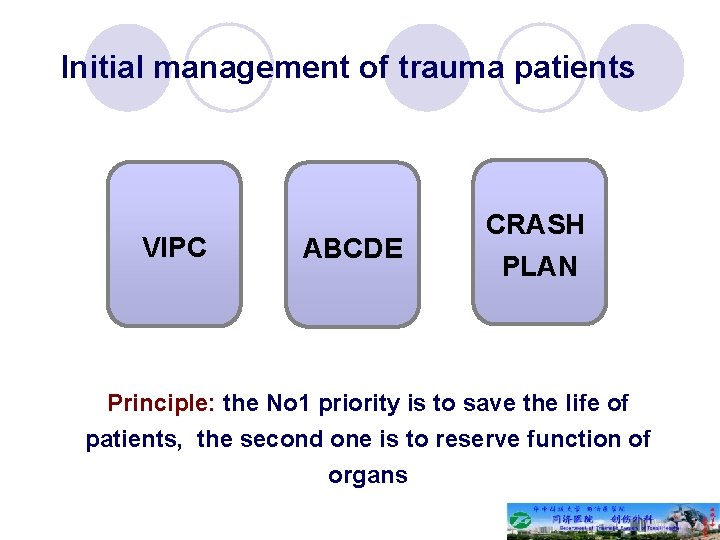
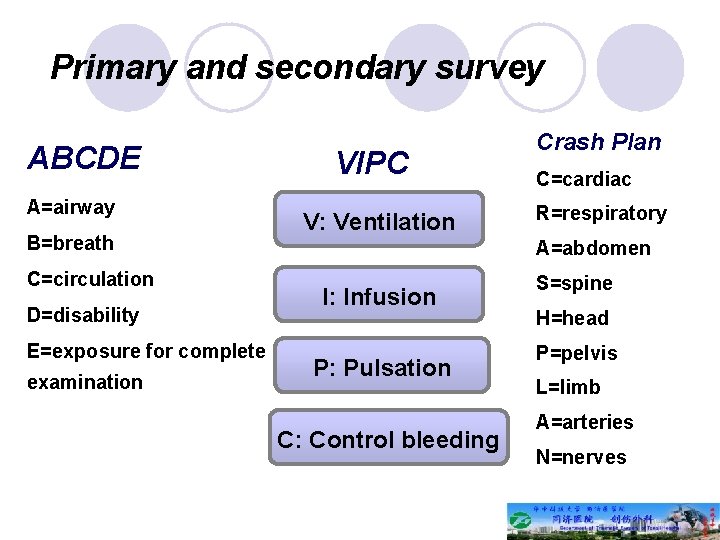
Initial management of trauma patients VIPC ABCDE CRASH PLAN Principle: the No 1 priority is to save the life of patients, the second one is to reserve function of organs
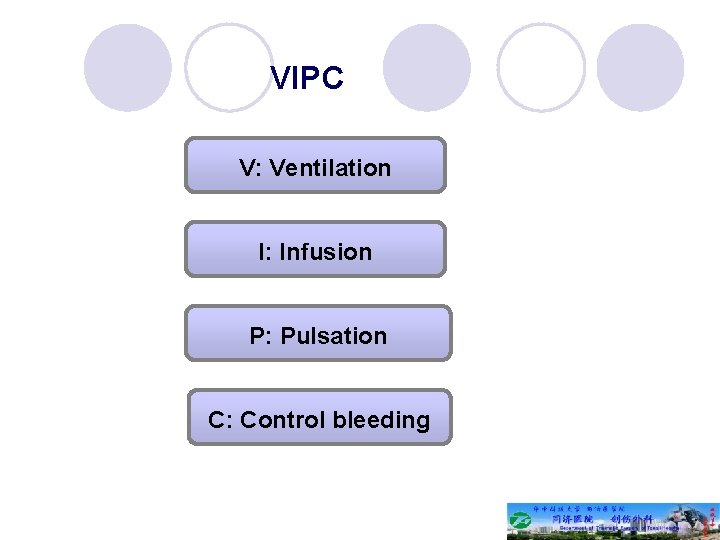
VIPC V: Ventilation I: Infusion P: Pulsation C: Control bleeding
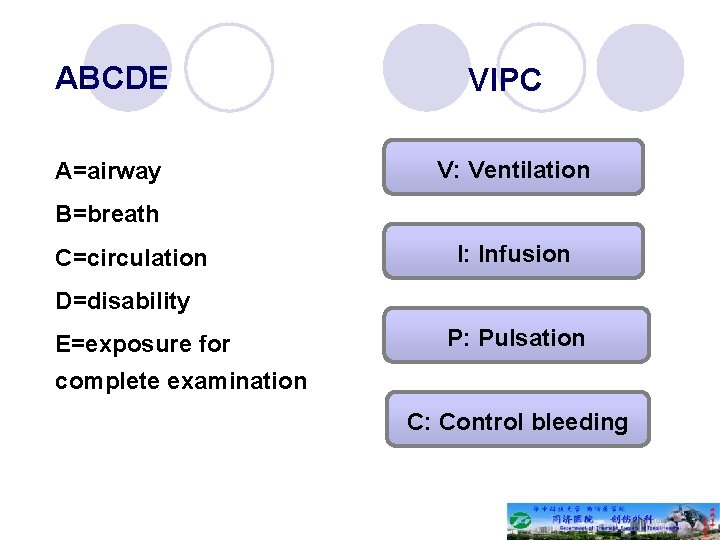
ABCDE A=airway VIPC V: Ventilation B=breath C=circulation I: Infusion D=disability E=exposure for P: Pulsation complete examination C: Control bleeding
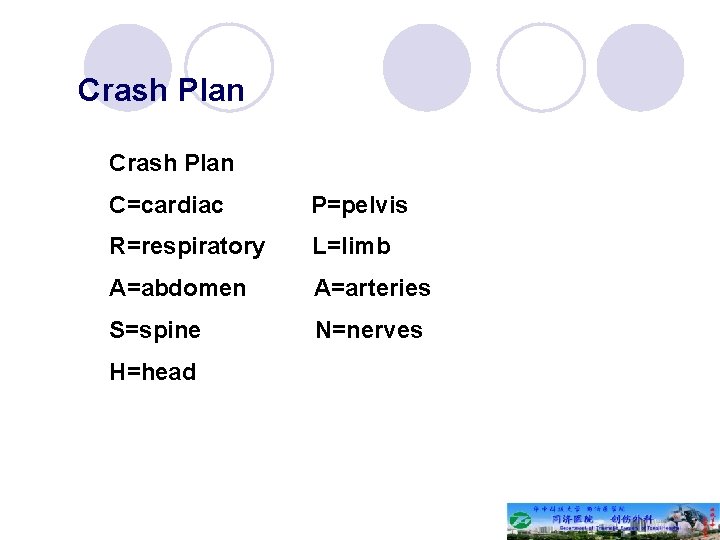
Crash Plan C=cardiac P=pelvis R=respiratory L=limb A=abdomen A=arteries S=spine N=nerves H=head
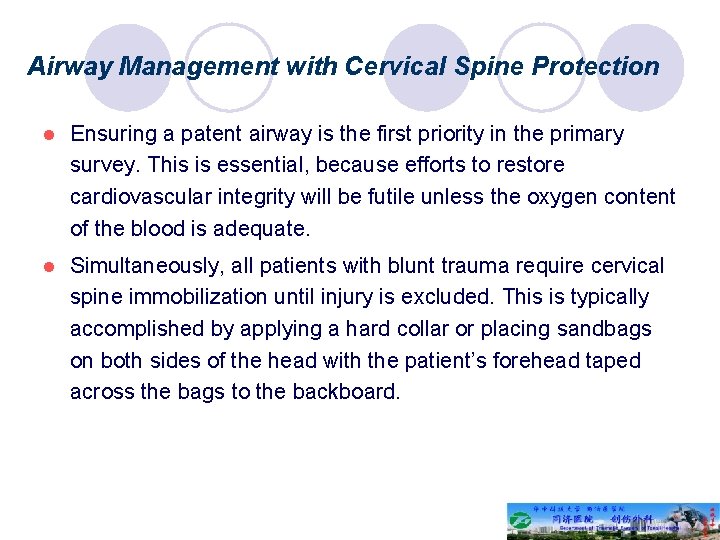
Airway Management with Cervical Spine Protection l Ensuring a patent airway is the first priority in the primary survey. This is essential, because efforts to restore cardiovascular integrity will be futile unless the oxygen content of the blood is adequate. l Simultaneously, all patients with blunt trauma require cervical spine immobilization until injury is excluded. This is typically accomplished by applying a hard collar or placing sandbags on both sides of the head with the patient’s forehead taped across the bags to the backboard.
Airway Management with Cervical Spine Protection l Patients who have an abnormal voice, abnormal breathing sounds, tachypnea, or altered mental status require further airway evaluation. l Cricothyroidotomy is performed through a generous vertical incision, with sharp division of the subcutaneous tissues and strap muscles. Visualization may be improved by having an assistant retract laterally on the neck incision using army-navy retractors.
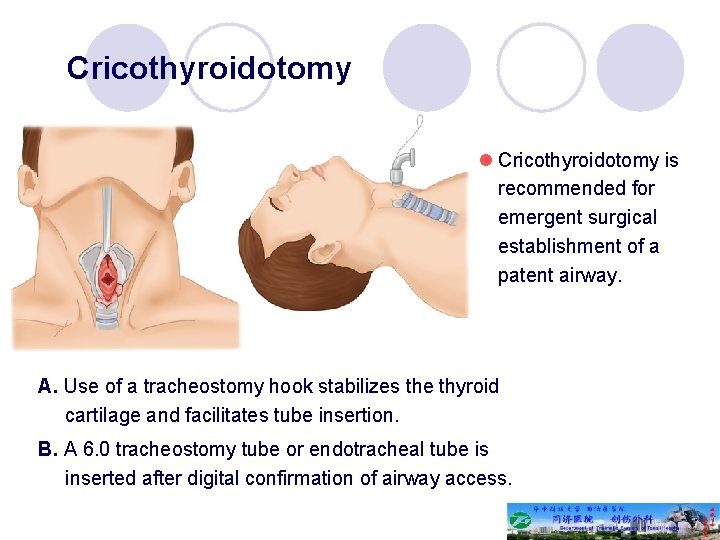
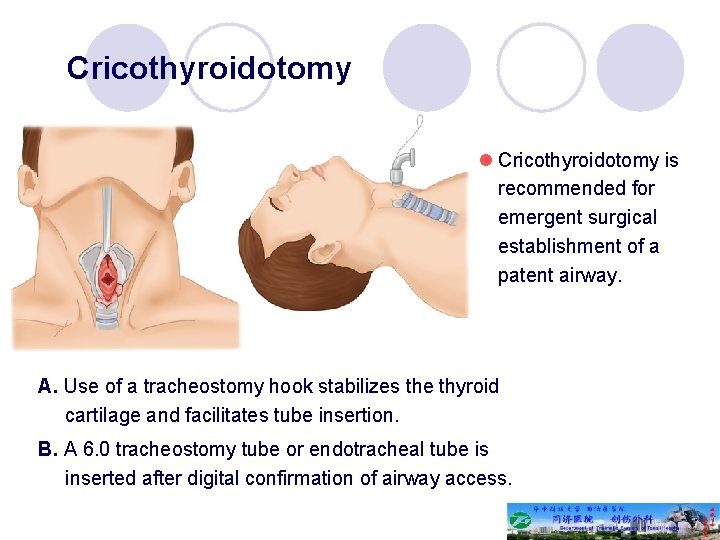
Cricothyroidotomy l Cricothyroidotomy is recommended for emergent surgical establishment of a patent airway. A. Use of a tracheostomy hook stabilizes the thyroid cartilage and facilitates tube insertion. B. A 6. 0 tracheostomy tube or endotracheal tube is inserted after digital confirmation of airway access.
Tracheostomy l Emergent tracheostomy is indicated in patients with laryngotracheal separation or laryngeal fractures, in whom cricothyroidotomy may cause further damage or result in complete loss of the airway
Breathing and ventilation l Once a secure airway is obtained, adequate oxygenation and ventilation must be assured. All injured patients should receive supplemental oxygen and be monitored by pulse oximetry.
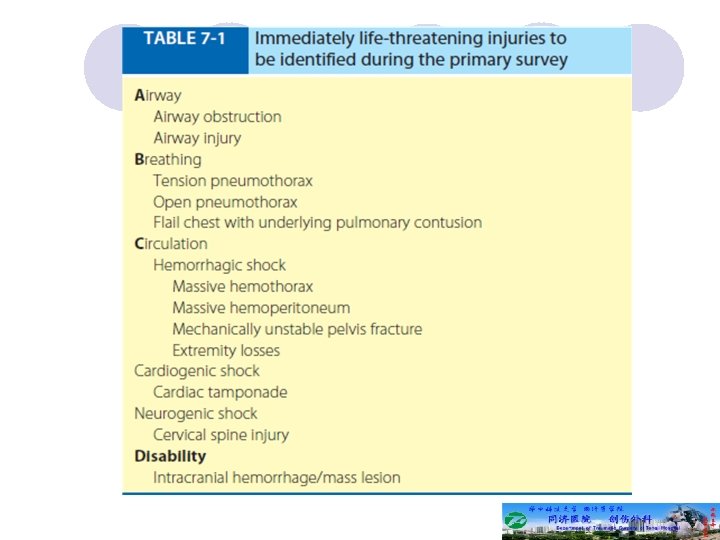
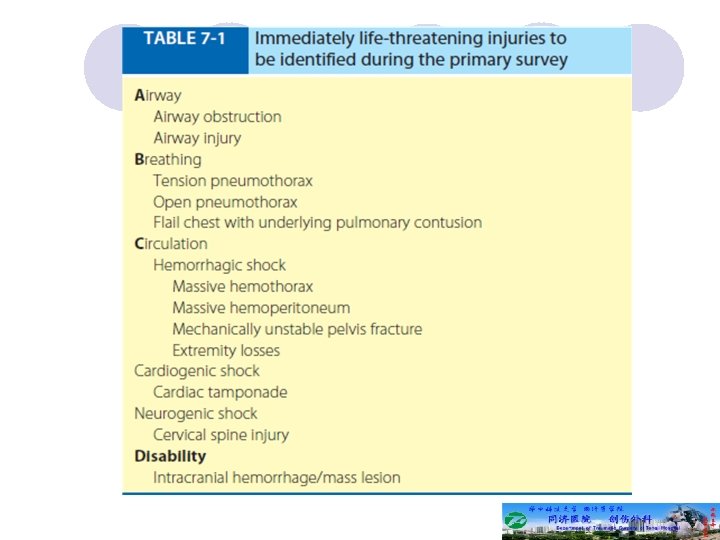
Breathing and ventilation l The following conditions constitute an immediate threat to life due to inadequate ventilation and should be recognized during the primary survey: tension pneumothorax open pneumothorax flail chest with underlying pulmonary contusion l All of these diagnoses should be made during the initial physical examination.
Tension pneumothorax l The diagnosis of tension pneumothorax is implied by respiratory distress and hypotension in combination with any of the following physical signs in patients with chest trauma: tracheal deviation away from the affected side lack of or decreased breath sounds on the affected side subcutaneous emphysema on the affected side
Tension pneumothorax l In cases of tension pneumothorax, the paren-chymal tear in the lung acts as a one-way valve, with each inhalation allowing additional air to accumulate in the pleural space. l The normally negative intrapleural pressure becomes positive, which depresses the ipsilateral hemidiaphragm and shifts the mediastinal structures into the contralateral chest.
Tension pneumothorax l Subsequently, the contralat-eral lung is compressed and the heart rotates about the superior and inferior vena cava; l This decreases venous return and ultimately cardiac output, which results in cardiovascular collapse.
Tension pneumothorax l Vital signs differentiate a tension pneumothorax from a simple pneumothorax; each can have similar signs, symptoms, and examination findings, but hypotension qualifies the pneumothorax as a tension pneumothorax.
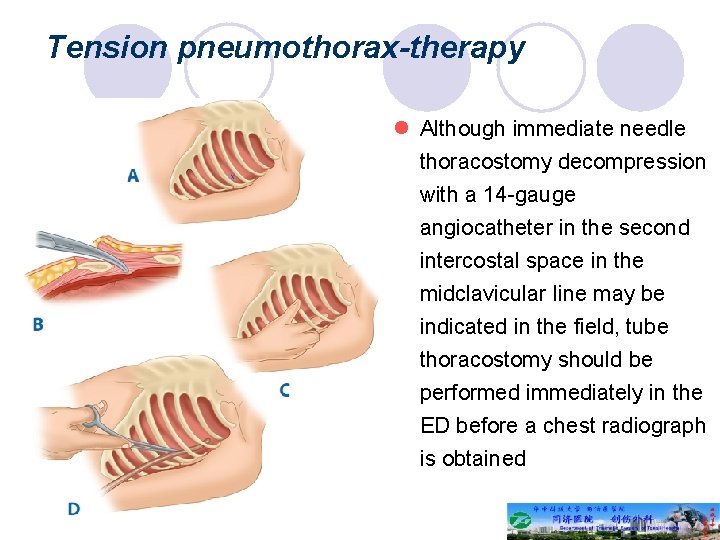
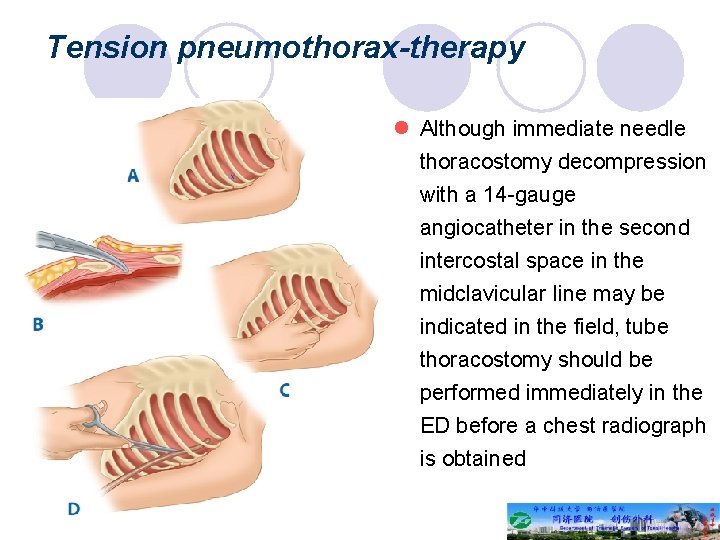
Tension pneumothorax-therapy l Although immediate needle thoracostomy decompression with a 14 -gauge angiocatheter in the second intercostal space in the midclavicular line may be indicated in the field, tube thoracostomy should be performed immediately in the ED before a chest radiograph is obtained
Open pneumothorax l An open pneumothorax or “sucking chest wound” occurs with full-thickness loss of the chest wall, permitting free communication between the pleural space and the atmosphere. l This compromises ventilation due to equilibration of atmospheric and pleural pressures, which prevents lung inflation and alveolar ventilation, and results in hypoxia and hypercarbia.
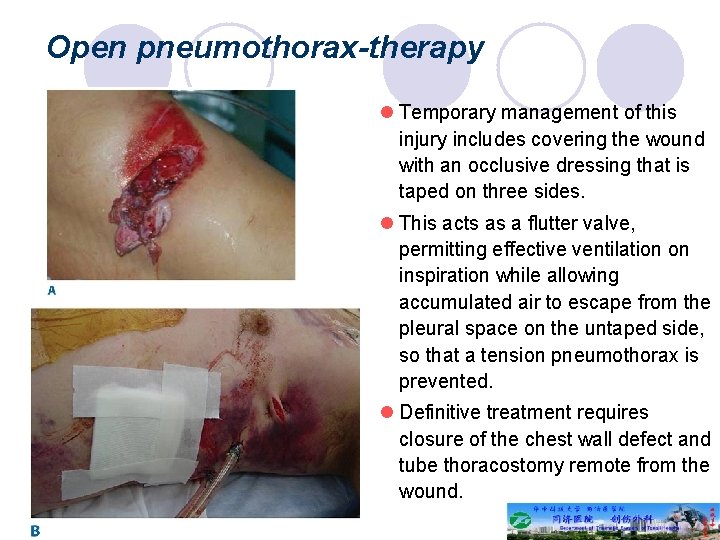
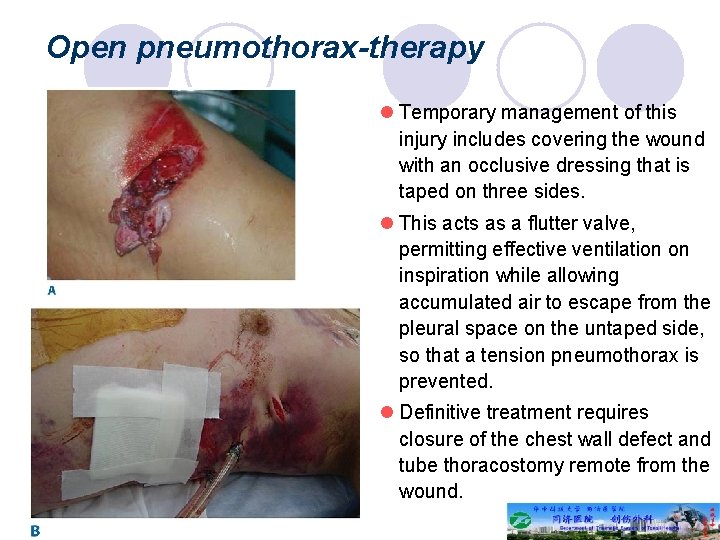
Open pneumothorax-therapy l Temporary management of this injury includes covering the wound with an occlusive dressing that is taped on three sides. l This acts as a flutter valve, permitting effective ventilation on inspiration while allowing accumulated air to escape from the pleural space on the untaped side, so that a tension pneumothorax is prevented. l Definitive treatment requires closure of the chest wall defect and tube thoracostomy remote from the wound.
Flail chest l Flail chest occurs when three or more contiguous ribs are fractured in at least two locations. Paradoxical movement of this free-floating segment of chest wall may be evident in patients with spontaneous ventilation, due to the negative intrapleural pressure of inspiration.
Flail chest l Rarely the additional work of breathing and chest wall pain caused by the flail segment is sufficient to compromise ventilation. l However, it is the decreased compliance and increased shunt fraction caused by the associated pulmonary contusion that is typically the source of postinjury pulmonary dysfunction.
Flail chest l Pulmonary contusion often progresses during the first 12 hours. Resultant hypoventilation and hypoxemia may require presumptive intubation and mechanical ventilation.
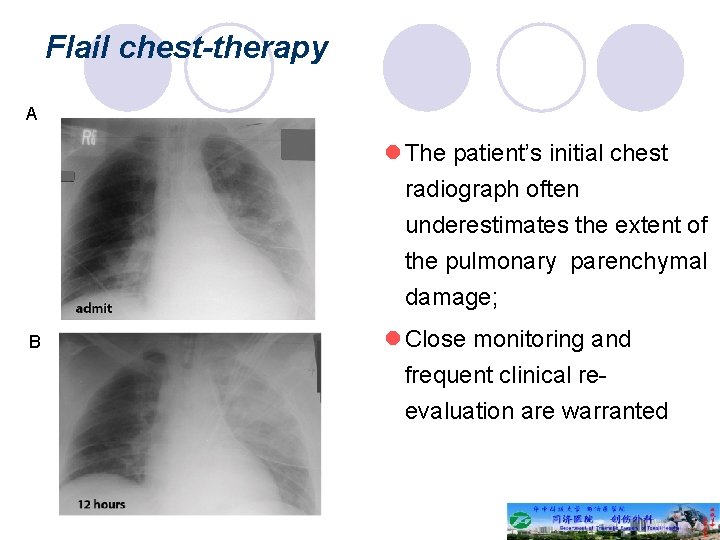
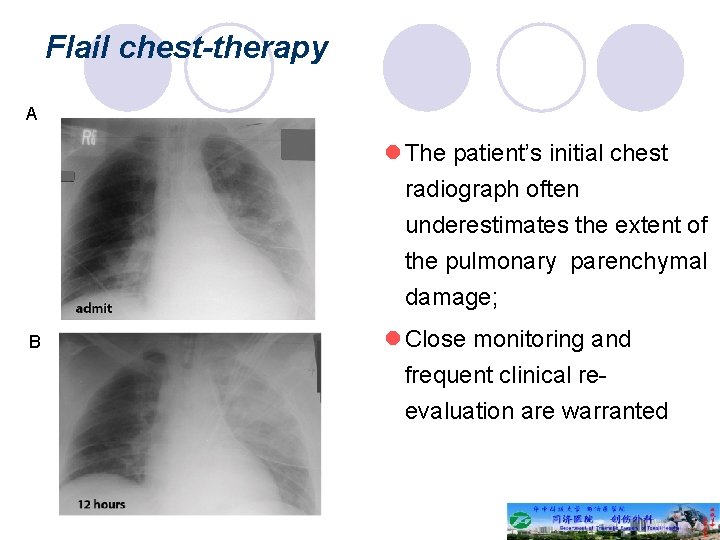
Flail chest-therapy A l The patient’s initial chest radiograph often underestimates the extent of the pulmonary parenchymal damage; B l Close monitoring and frequent clinical reevaluation are warranted
Circulation with hemorrhage control l With a secure airway and adequate ventilation established, circulatory status is the next priority. l An initial approximation of the patient’s cardiovascular status can be obtained by palpating peripheral pulses. l In general, systolic blood pressure (SBP) must be 60 mm. Hg for the carotid pulse to be palpable, 70 mm. Hg for the femoral pulse, and 80 mm. Hg for the radial pulse.
Circulation with hemorrhage control l At this point of patient evaluation, any episode of hypotension (defined as a SBP <90 mm. Hg) is assumed to be caused by hemorrhage until proven otherwise. l Patients should be closely monitored until normal vital sign values are restored.
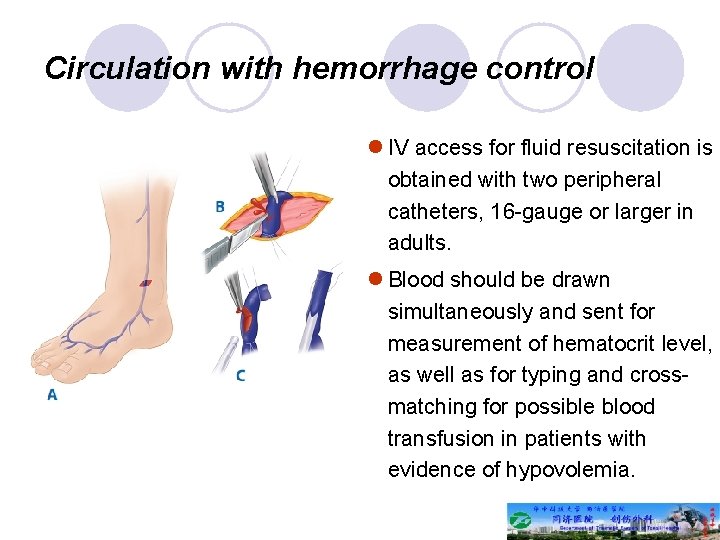
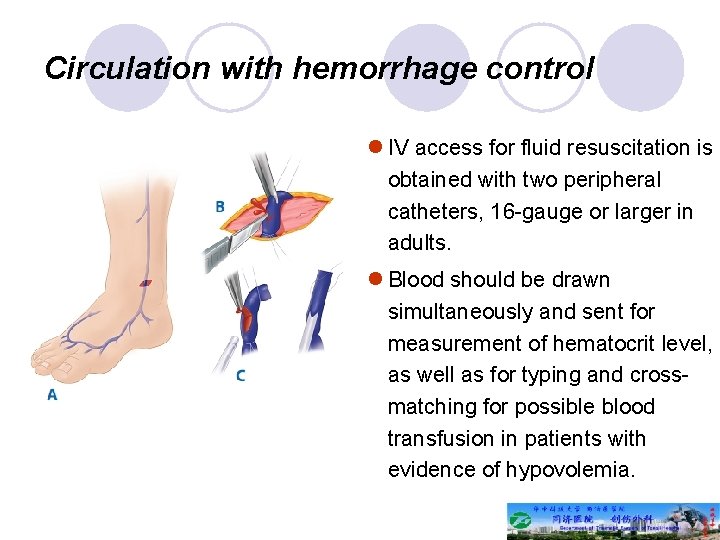
Circulation with hemorrhage control l IV access for fluid resuscitation is obtained with two peripheral catheters, 16 -gauge or larger in adults. l Blood should be drawn simultaneously and sent for measurement of hematocrit level, as well as for typing and crossmatching for possible blood transfusion in patients with evidence of hypovolemia.
Circulation with hemorrhage control l External control of hemorrhage should be achieved promptly while circulating volume is restored. Manual compression of open wounds with ongoing bleeding should be done with a single 4 4 gauze and a gloved hand. l Blind clamping of bleeding vessels should be avoided because of the risk to adjacent structures, including nerves.
Circulation with hemorrhage control l During the circulation section of the primary survey, four life-threatening injuries that must be identified are: ü (a) massive hemothorax ü (b) cardiac tamponade ü (c) massive hemoperitoneum ü (d) mechanically unstable pelvic fractures.
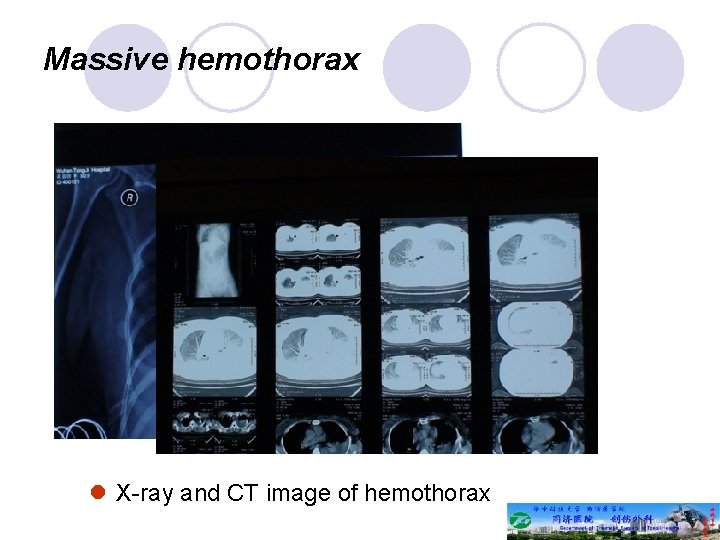
Massive hemothorax l A massive hemothorax (life-threatening injury number one) is defined as >1500 m. L of blood or, in the pediatric population, one third of the patient’s blood volume in the pleural space
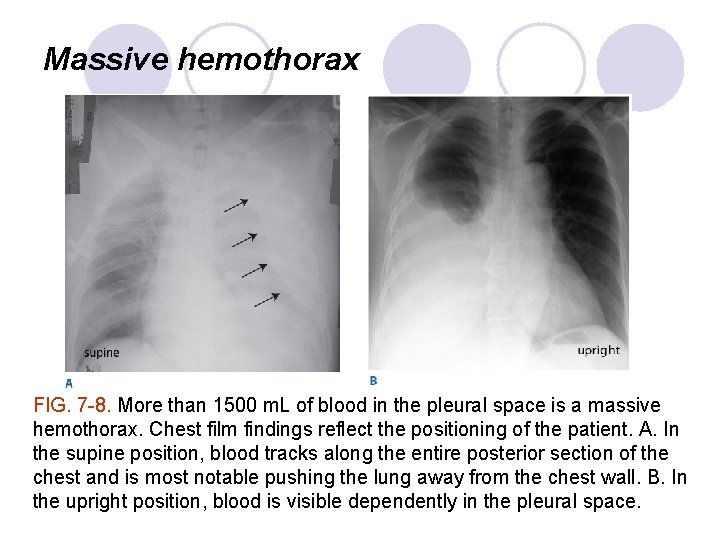
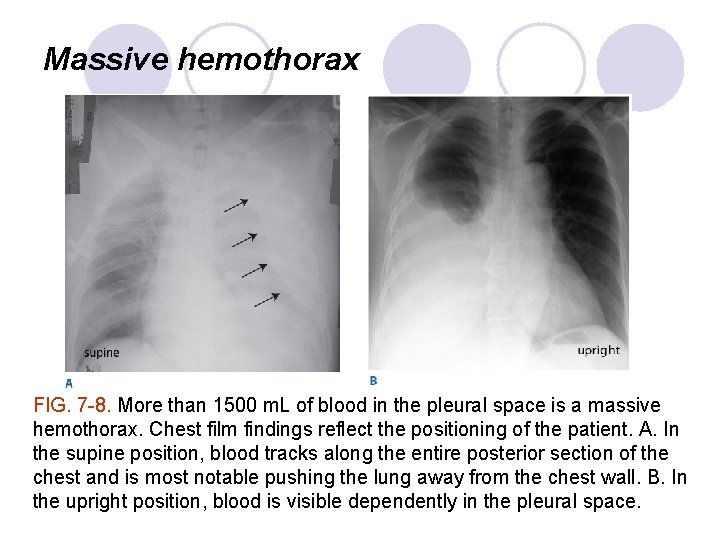
Massive hemothorax FIG. 7 -8. More than 1500 m. L of blood in the pleural space is a massive hemothorax. Chest film findings reflect the positioning of the patient. A. In the supine position, blood tracks along the entire posterior section of the chest and is most notable pushing the lung away from the chest wall. B. In the upright position, blood is visible dependently in the pleural space.
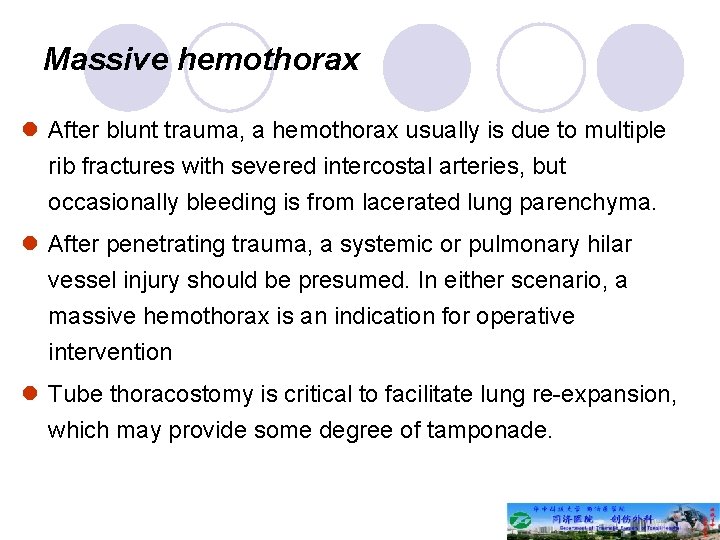
Massive hemothorax l After blunt trauma, a hemothorax usually is due to multiple rib fractures with severed intercostal arteries, but occasionally bleeding is from lacerated lung parenchyma. l After penetrating trauma, a systemic or pulmonary hilar vessel injury should be presumed. In either scenario, a massive hemothorax is an indication for operative intervention l Tube thoracostomy is critical to facilitate lung re-expansion, which may provide some degree of tamponade.
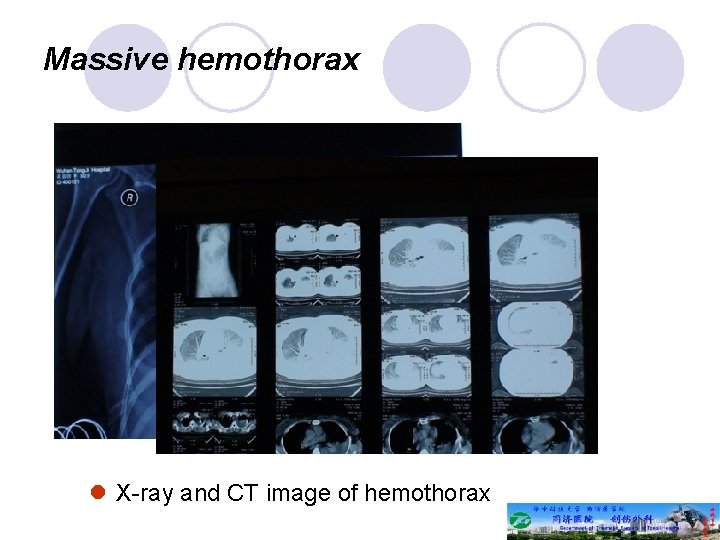
Massive hemothorax l X-ray and CT image of hemothorax
Cardiac tamponade l Cardiac tamponade (life-threatening injury number two) occurs most commonly after penetrating thoracic injuries, although occasionally blunt rupture of the heart, particularly the atrial appendage, is seen. l Acutely, <100 m. L of pericardial blood may cause pericardial tamponade.
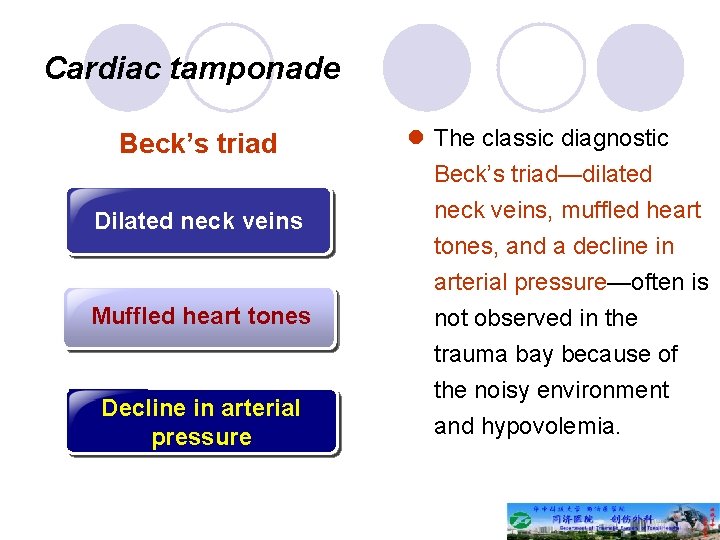
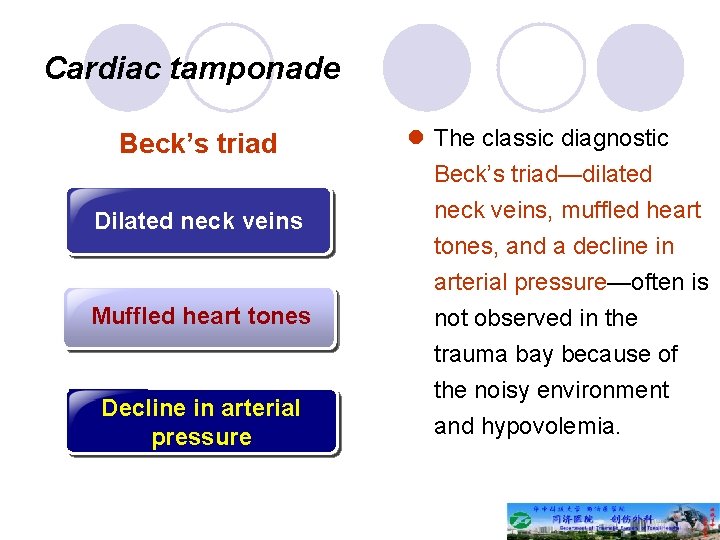
Cardiac tamponade Beck’s triad 临床 作 Dilated neck veins Muffled heart tones Decline in arterial pressure l The classic diagnostic Beck’s triad—dilated neck veins, muffled heart tones, and a decline in arterial pressure—often is not observed in the trauma bay because of the noisy environment and hypovolemia.
Cardiac tamponade l Because the pericardium is not acutely distensible, the pressure in the pericardial sac will rise to match that of the injured chamber.
Cardiac tamponade l Because the pericardium is not acutely distensible, the pressure in the pericardial sac will rise to match that of the injured chamber. l When this pressure exceeds that of the right atrium, right atrial filling is impaired and right ventricular preload is reduced. This leads to decreased right ventricular output and increased CVP. l Increased intrapericardial pressure also impedes myocardial blood flow, which leads to subendocardial ischemia and a further reduction in cardiac output.
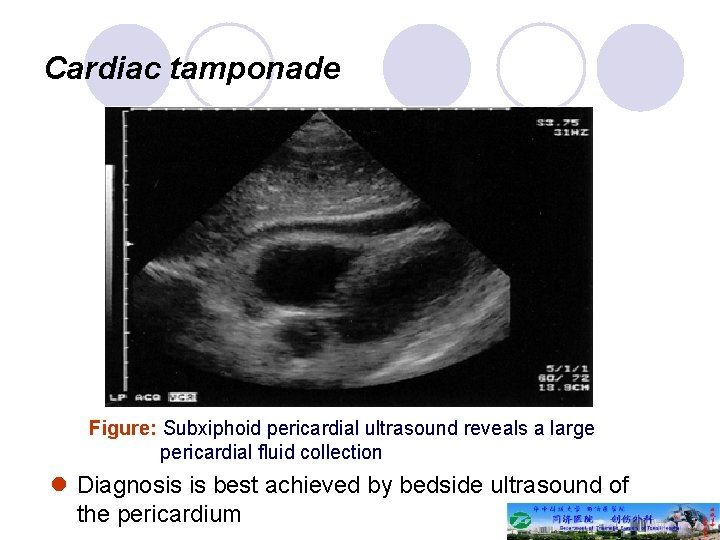
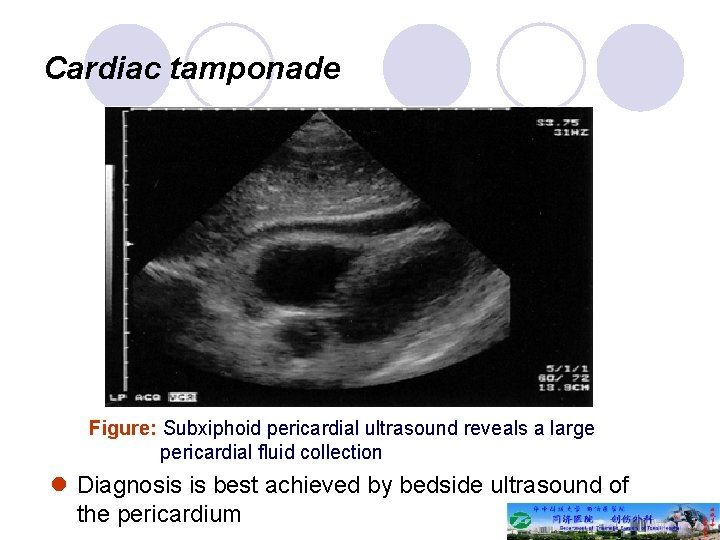
Cardiac tamponade Figure: Subxiphoid pericardial ultrasound reveals a large pericardial fluid collection l Diagnosis is best achieved by bedside ultrasound of the pericardium
Cardiac tamponade l Removing as little as 15 to 20 m. L of blood will often temporarily stabilize the patient’s hemodynamic status, prevent subendocardial ischemia and associated lethal arrhythmias, and allow transport to the OR for sternotomy. l Pericardiocentesis is successful in decompressing tamponade in approximately 80% of cases; the majority of failures are due to the presence of clotted blood within the pericardium.
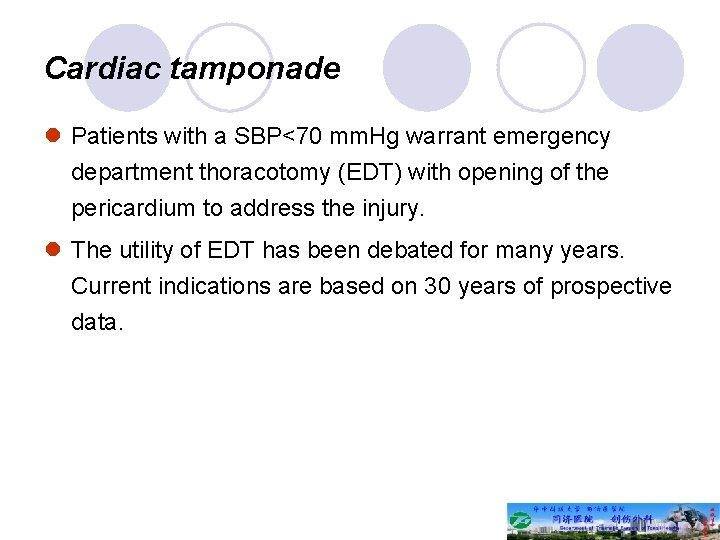
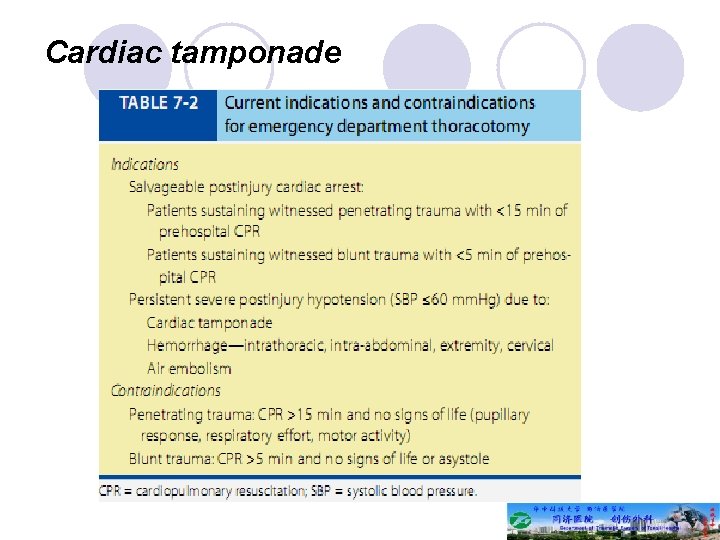
Cardiac tamponade l Patients with a SBP<70 mm. Hg warrant emergency department thoracotomy (EDT) with opening of the pericardium to address the injury. l The utility of EDT has been debated for many years. Current indications are based on 30 years of prospective data.
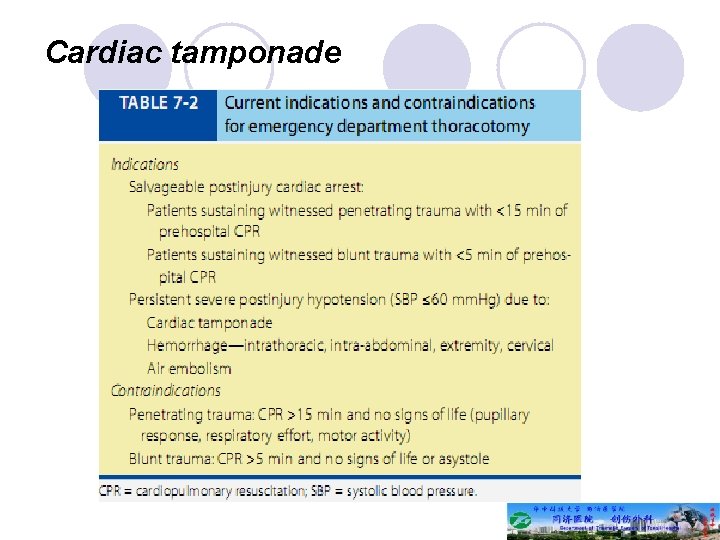
Cardiac tamponade
Massive hemoperitonium and unstable pelvic fracture l Three critical tools used to differentiate these in the multisystem trauma patient are chest radiograph, pelvis radiograph, and focused abdominal sonography for trauma (FAST)
Disability and exposure l Glascow coma score (GCS) should be determined for all injured patients. l An abnormal mental status should prompt an immediate re-evaluation of the ABCs and consideration of central nervous system injury. l Deterioration in mental status may be subtle and may not progress in a predictable fashion.
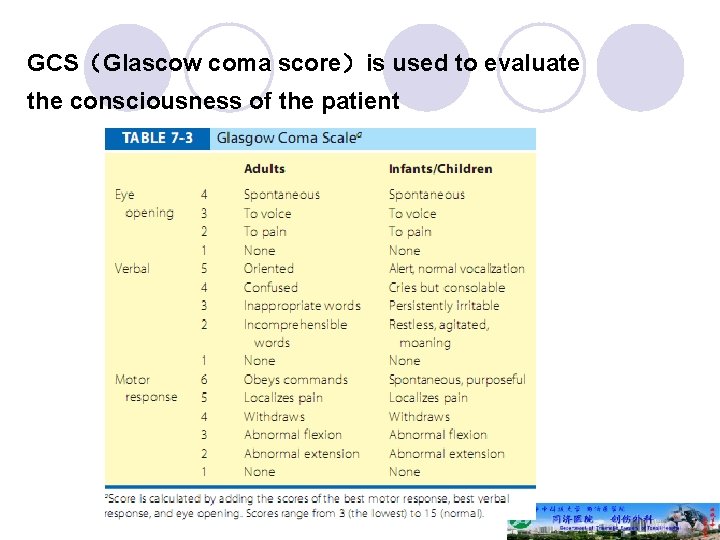
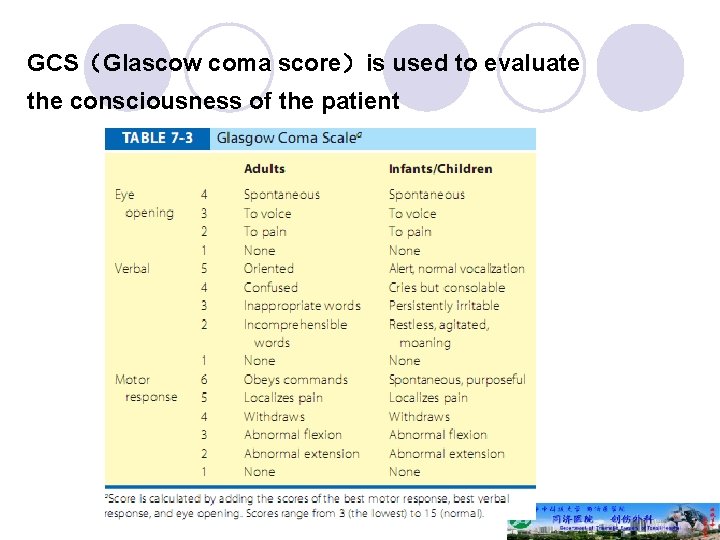
GCS(Glascow coma score)is used to evaluate the consciousness of the patient
Disability and exposure l Seriously injured patients must have all of their clothing removed to avoid overlooking limb- or life-threatening injuries.
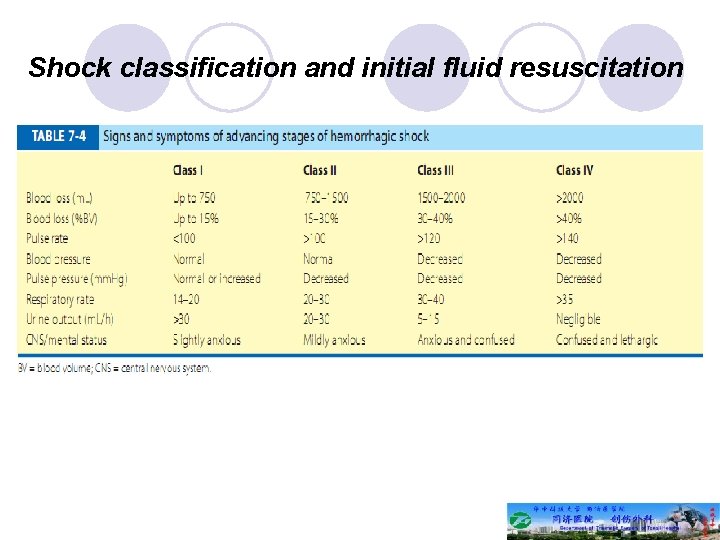
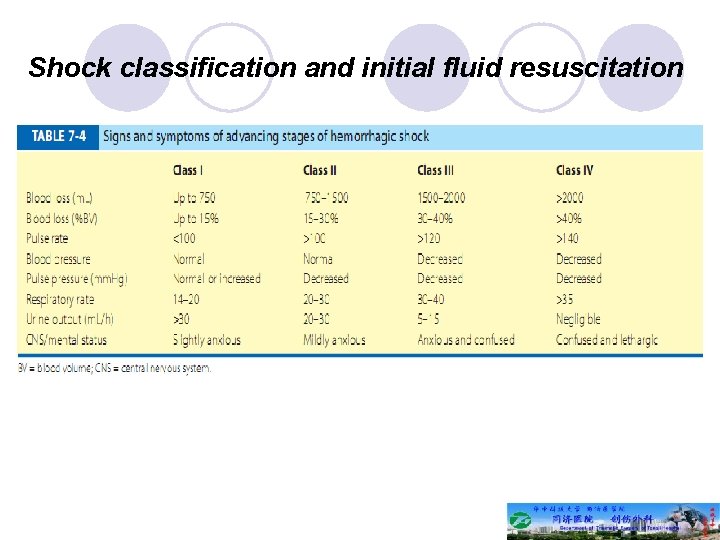
Shock classification and initial fluid resuscitation
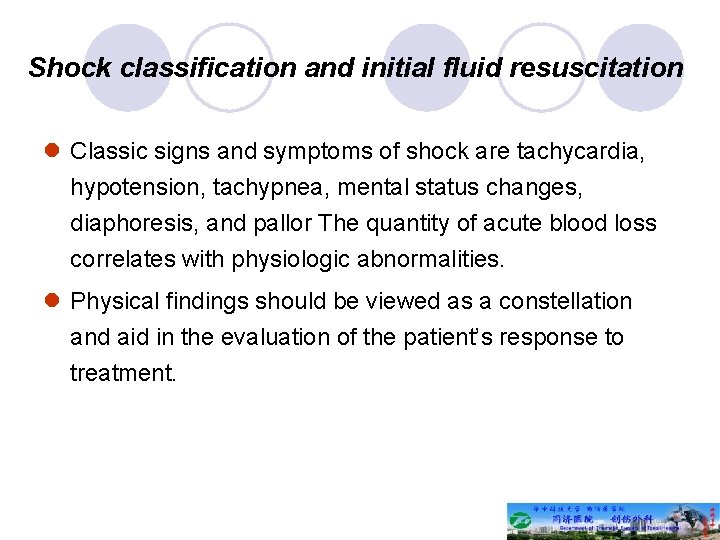
Shock classification and initial fluid resuscitation l Classic signs and symptoms of shock are tachycardia, hypotension, tachypnea, mental status changes, diaphoresis, and pallor The quantity of acute blood loss correlates with physiologic abnormalities. l Physical findings should be viewed as a constellation and aid in the evaluation of the patient’s response to treatment.
Shock classification and initial fluid resuscitation l The goal of fluid resuscitation is to re-establish tissue perfusion. Fluid resuscitation begins with a 2 L (adult) or 20 m. L/kg (child) IV bolus of isotonic crystalloid, typically Ringer’s lactate. l For persistent hypotension, this is repeated once in an adult and twice in a child before red blood cells (RBCs) are administered.
Shock classification and initial fluid resuscitation l Urine output is a quantitative, reliable indicator of organ perfusion. l Adequate urine output is 0. 5 m. L/kg per hour in an adult, 1 m. L/kg per hour in a child, and 2 m. L/kg per hour in an infant <1 year of age. l Measurement of urine output is time-dependent.
Pitfalls in evaluation for patients with shock l Relative tachycardia or tachycardia caused by other conditions l Hypotension is not a reliable sign for hypovolemia, because blood volume must decrease by >30% before hypotension occurs.
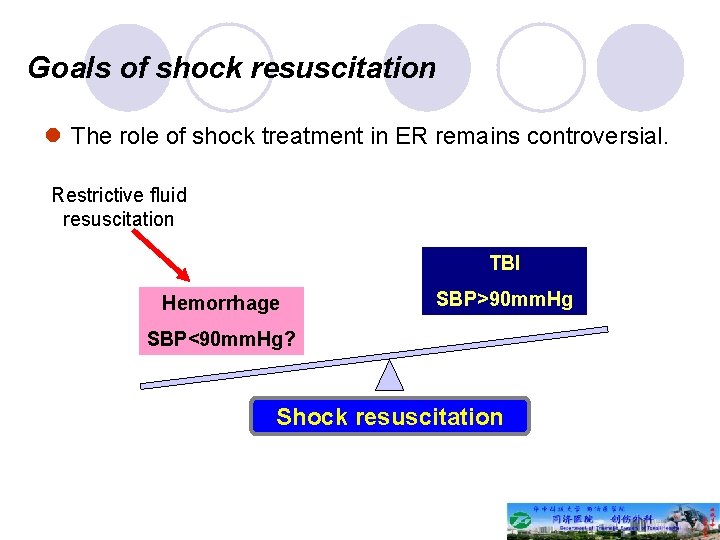
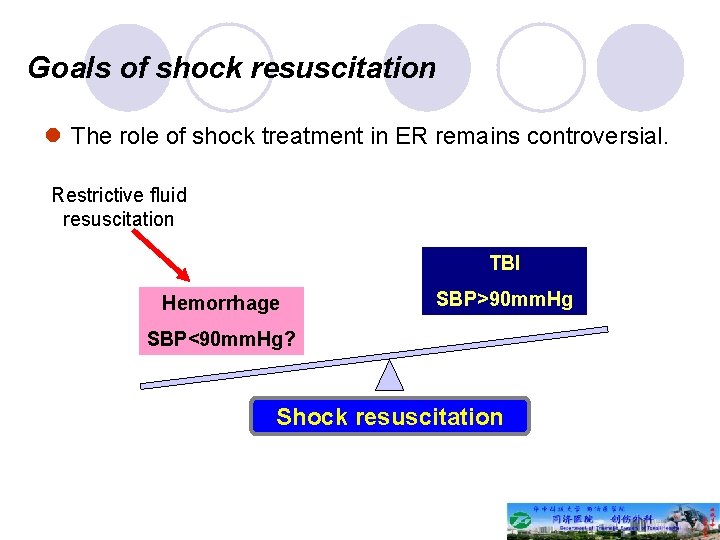
Goals of shock resuscitation l The role of shock treatment in ER remains controversial. Restrictive fluid resuscitation TBI Hemorrhage SBP>90 mm. Hg SBP<90 mm. Hg? Shock resuscitation
Secondary survey l Once the immediate threats to life have been addressed, a thorough history is obtained and the patient is examined in a systematic fashion. l The patient and surrogates should be queried to obtain an AMPLE history (Allergies, Medications, Past illnesses or Pregnancy, Last meal, and Events related to the injury). l The physical examination should be head to toe, with special attention to the patient’s back, axillae, and perineum, because injuries here are easily overlooked.
Secondary survey l All potentially seriously injured patients should undergo digital rectal examination to evaluate for sphincter tone, presence of blood, rectal perforation, or a high-riding prostate; this is particularly critical in patients with suspected spinal cord injury, pelvic fracture, or transpelvic gunshot wounds. l Vaginal examination with a speculum also should be performed in women with pelvic fractures to exclude an open fracture.
Secondary survey l Adjuncts to the physical examination include: ü vital sign and CVP monitoring ü ECG monitoring ü nasogastric tube placement ü Foley catheter placement ü repeat FAST ü laboratory measurements ü and radiographs.
Secondary survey l A nasogastric tube should be inserted in all intubated patients to decrease the risk of gastric aspiration but may not be indicated in the awake patient. l Placement of a nasogastric tube is also contraindicated in patients with complex facial fractures. l A Foley catheter should be inserted in patients unable to void to decompress the bladder, obtain a urinespecimen, and monitor urine output.
Secondary survey l Selective radiography: lateral cervical, chest and pelvic (big three) l Laboratory test: blood routine, Hg quantitation, WBC and differential, Plt, urine routine, etc.
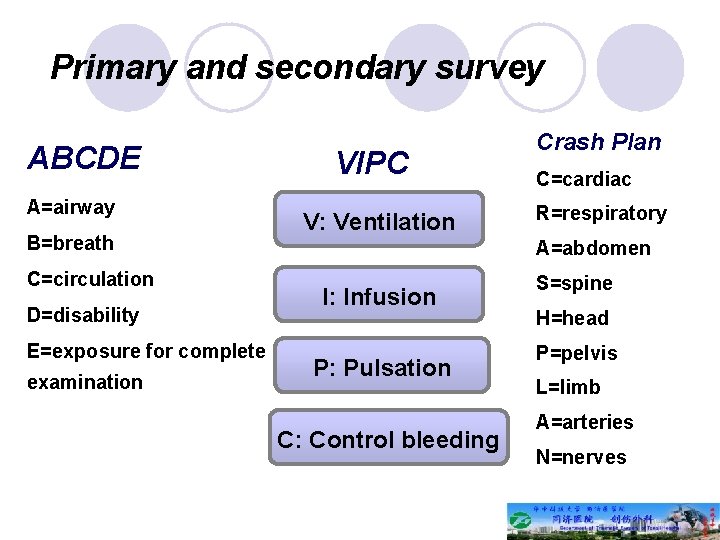
Primary and secondary survey ABCDE A=airway B=breath C=circulation D=disability E=exposure for complete examination VIPC V: Ventilation Crash Plan C=cardiac R=respiratory A=abdomen I: Infusion P: Pulsation C: Control bleeding S=spine H=head P=pelvis L=limb A=arteries N=nerves
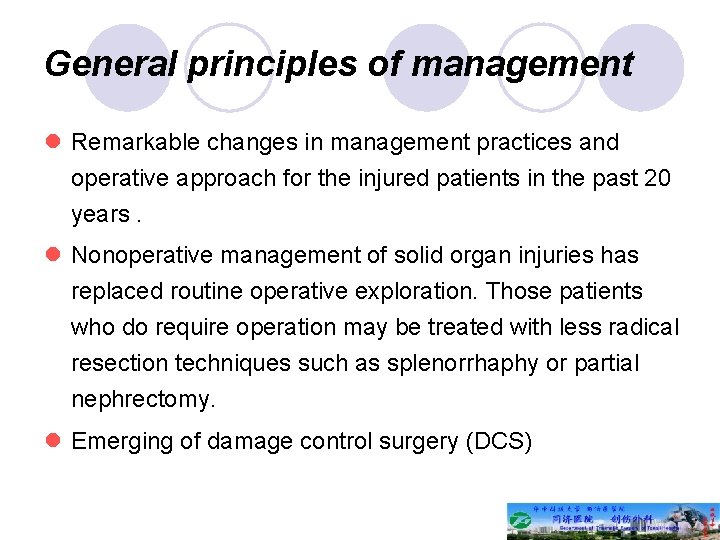
General principles of management l Remarkable changes in management practices and operative approach for the injured patients in the past 20 years. l Nonoperative management of solid organ injuries has replaced routine operative exploration. Those patients who do require operation may be treated with less radical resection techniques such as splenorrhaphy or partial nephrectomy. l Emerging of damage control surgery (DCS)
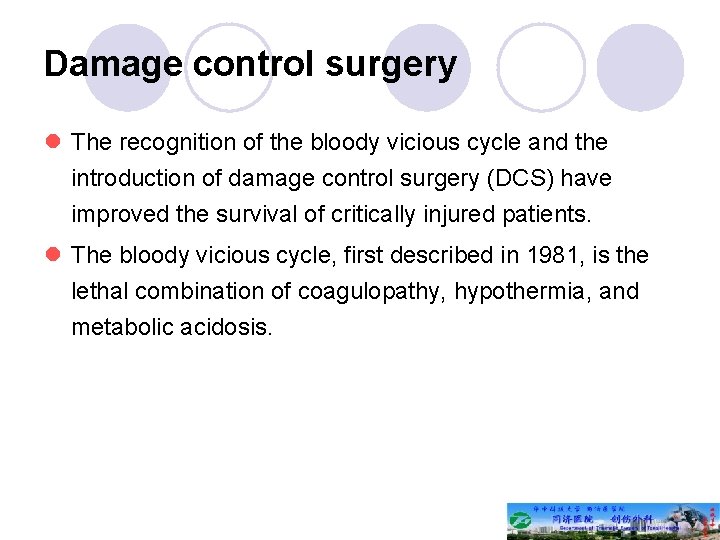
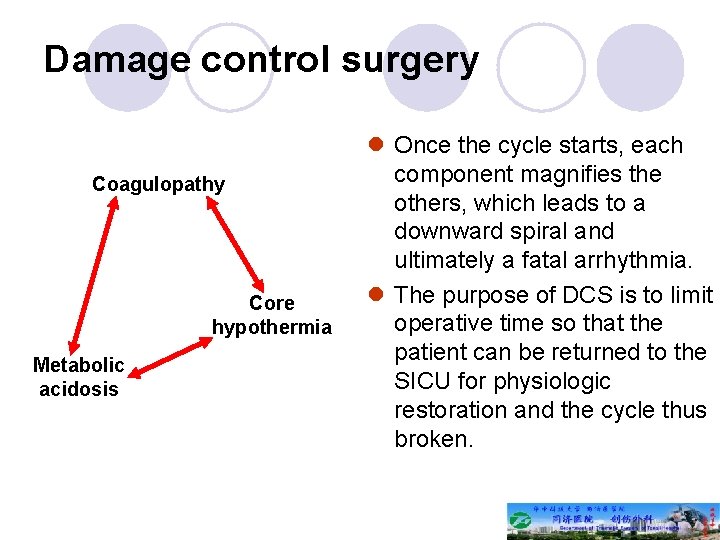
Damage control surgery l The recognition of the bloody vicious cycle and the introduction of damage control surgery (DCS) have improved the survival of critically injured patients. l The bloody vicious cycle, first described in 1981, is the lethal combination of coagulopathy, hypothermia, and metabolic acidosis.
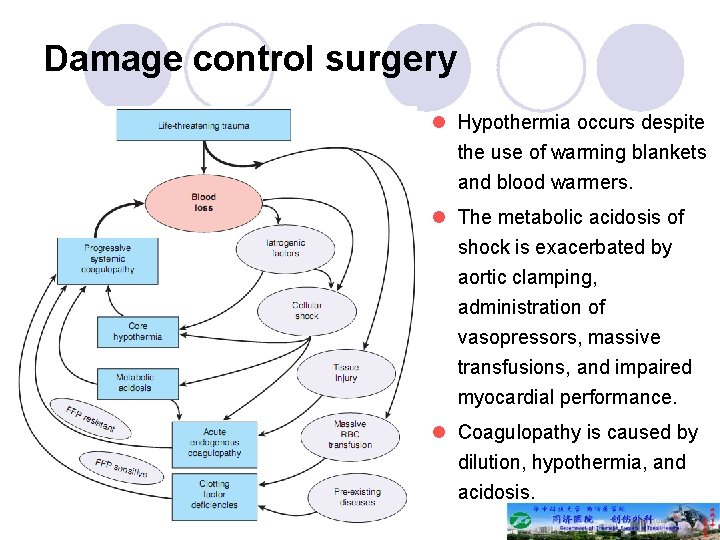
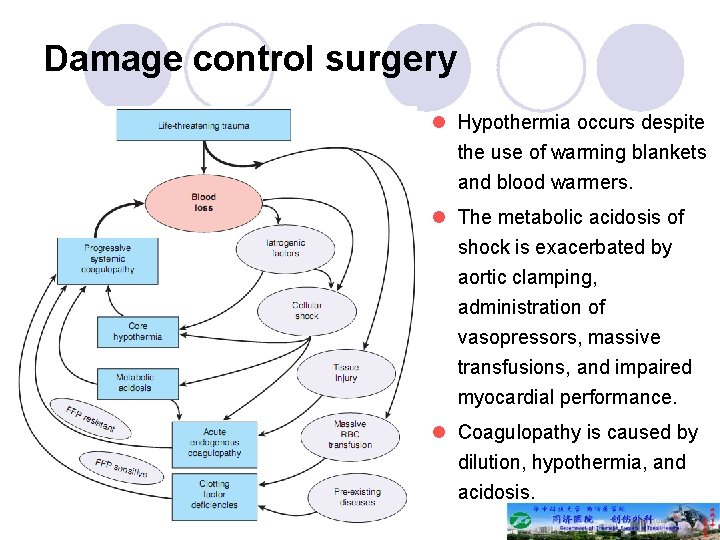
Damage control surgery l Hypothermia occurs despite the use of warming blankets and blood warmers. l The metabolic acidosis of shock is exacerbated by aortic clamping, administration of vasopressors, massive transfusions, and impaired myocardial performance. l Coagulopathy is caused by dilution, hypothermia, and acidosis.
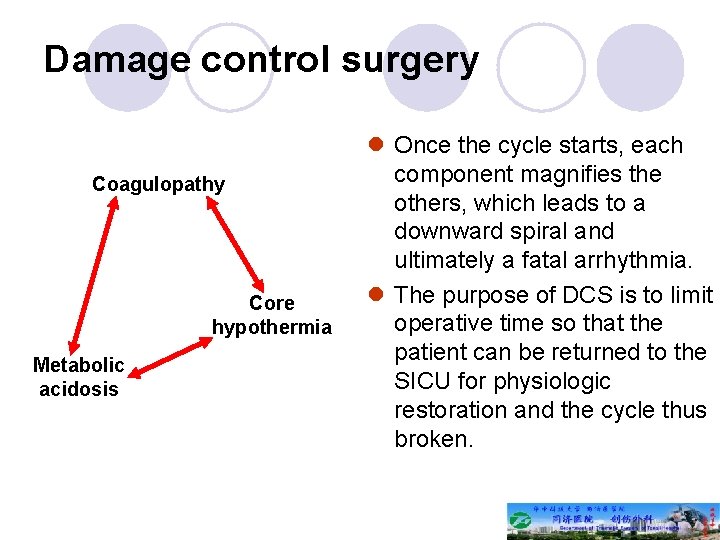
Damage control surgery Coagulopathy Core hypothermia Metabolic acidosis l Once the cycle starts, each component magnifies the others, which leads to a downward spiral and ultimately a fatal arrhythmia. l The purpose of DCS is to limit operative time so that the patient can be returned to the SICU for physiologic restoration and the cycle thus broken.
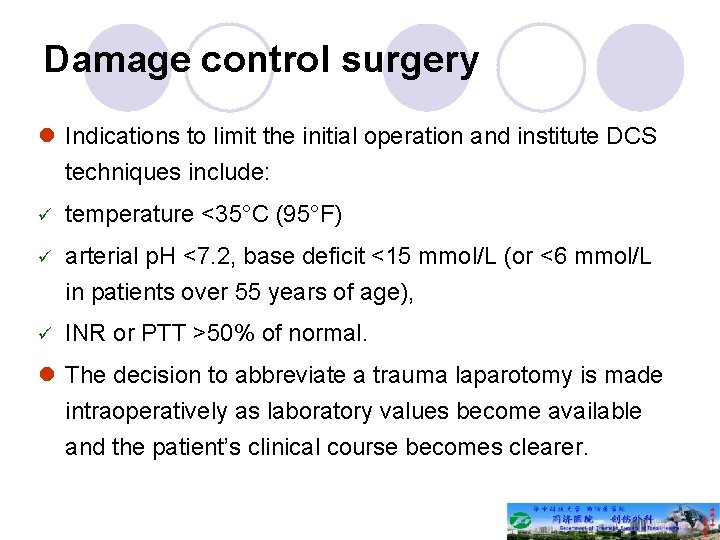
Damage control surgery l Indications to limit the initial operation and institute DCS techniques include: ü temperature <35°C (95°F) ü arterial p. H <7. 2, base deficit <15 mmol/L (or <6 mmol/L in patients over 55 years of age), ü INR or PTT >50% of normal. l The decision to abbreviate a trauma laparotomy is made intraoperatively as laboratory values become available and the patient’s clinical course becomes clearer.
Evaluation of the severity of injured patients AIS-ISS system Abbreviated injury score (AIS): assess the severity of injury and give a score from 1 to 6. Injury severity score (ISS): this system divides the whole body into 6 parts, head and neck, facial, thorax (including the thoracic spine), abdomen and pelvic viscera, limbs and pelvis, skin. ISS is the of square of three most severe AIS
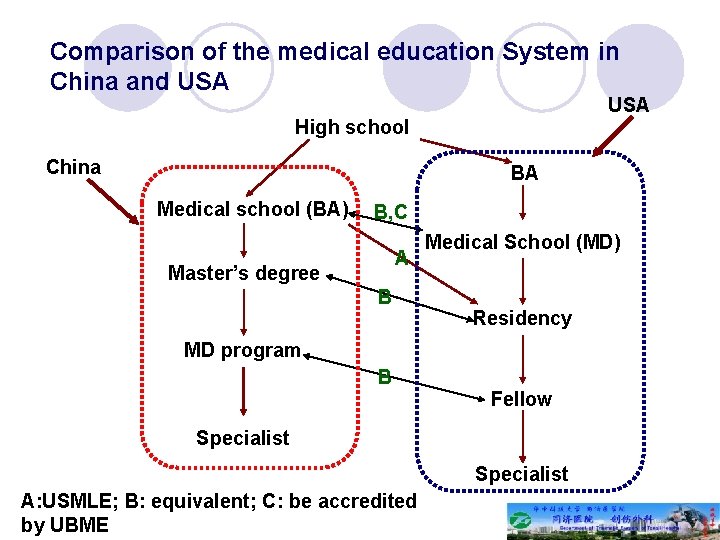
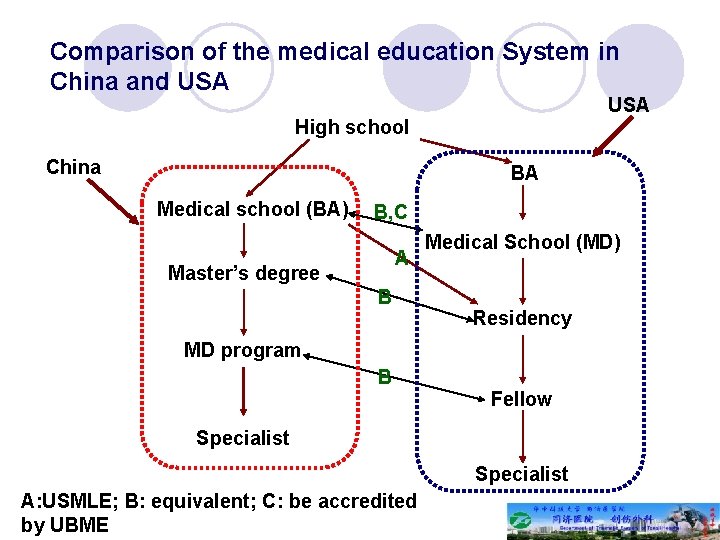
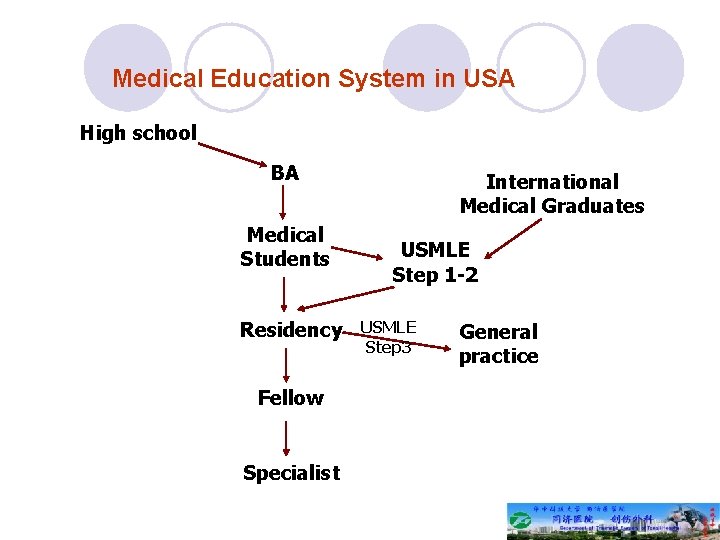
Comparison of the medical education System in China and USA High school China BA Medical school (BA) B, C A Master’s degree B Medical School (MD) Residency MD program B Fellow Specialist A: USMLE; B: equivalent; C: be accredited by UBME
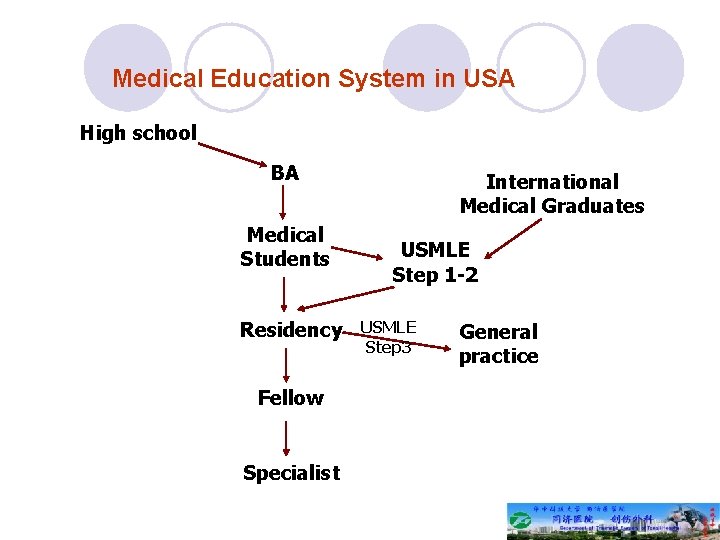
Medical Education System in USA High school BA Medical Students Residency Fellow Specialist International Medical Graduates USMLE Step 1 -2 USMLE Step 3 General practice

Zhanfei Li. MD&Ph. D Division of Traumatology, TJH of HUST www. chinatrauma. cn