TraumaInformed Approaches in HIV HepatitisC and Opioid Use















- Slides: 58
Trauma-Informed Approaches in HIV, Hepatitis-C, and Opioid Use Disorder Care Triple Threat II: HIV, HCV & Opioids June 25 th, 2019 ©ncdvtmh

Gabriela Zapata-Alma, LCSW, CADC Director of Policy and Practice for Domestic Violence and Substance Use ©ncdvtmh
US DHHS ACF FVPSA-Funded Special Issue Resource Center Dedicated to Addressing the Intersection of Domestic Violence, Trauma, Substance Use and Mental Health ▪ Comprehensive Array of Training & Technical Assistance Services and Resources ▪ Research and Evaluation ▪ Policy Development & Analysis ▪ Public Awareness ©ncdvtmh
This training is supported by Grant #90 EV 0437 -01 -00 from the Administration on Children, Youth and Families, Family and Youth Services Bureau, U. S. Department of Health and Human Services. Points of view in this document are those of the presenters and do not necessarily reflect the official positions or policies of the U. S. Department of Health and Human Services. 4
Objectives ▪ Understanding trauma, and the connections between victimization, trauma, HIV, Hepatitis-C, and opioid use disorders. ▪ Operationalize a trauma-informed framework that includes practical strategies for providers to better serve survivors of ©ncdvtmh trauma.
Understanding Trauma ©ncdvtmh
Defining Trauma Individual trauma: “. . . results from an event, series of events, or set of circumstances that is experienced by an individual as physically or emotionally harmful or life threatening and that has lasting adverse effects on the individual’s functioning and mental, physical, social, emotional or spiritual well-being. ” (SAMHSA, 2014) Collective Trauma: “Cultural, historical, insidious and political/economic trauma that impacts individuals and communities across generations” (National Indigenous Women’s Resource Center, 2014, NCDVTMH 2014) ©ncdvtmh
Types of Trauma ■ Acute: a single event that lasts for a specific period of time. ■ Chronic: many traumatic events over a prolonged period of time. ○ Trauma can be of the same kind or mixed. ○ Often begins in childhood. ■ Complex: chronic trauma beginning in early childhood, experienced at the hands of caregivers. ©ncdvtmh National Child Traumatic Stress Network
Types of Trauma: Neglect ■ Not merely the absence of something that was needed. ■ Can produce life-threatening and terrifying situations which are traumatic. ■ Can reduce resiliency and increase risk of developing trauma-related disorders. ©ncdvtmh National Child Traumatic Stress Network

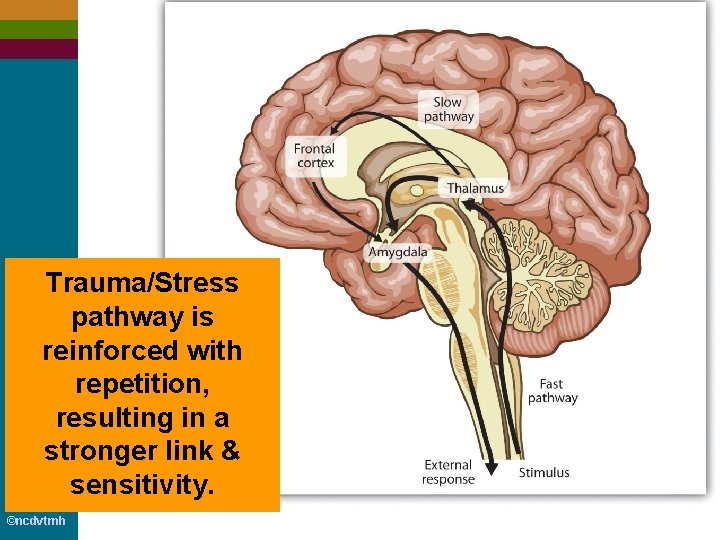
Basic Neurological Activity ■ Thalamus: processes sensory input and alerts different areas of the brain ■ Amygdala: the brain’s alarm system. Very quickly responds to danger. Shuts down all nonessential brain/body functions and sends power to physical functions needed for “flight” or “fight” ■ Hippocampus: memory center ©ncdvtmh
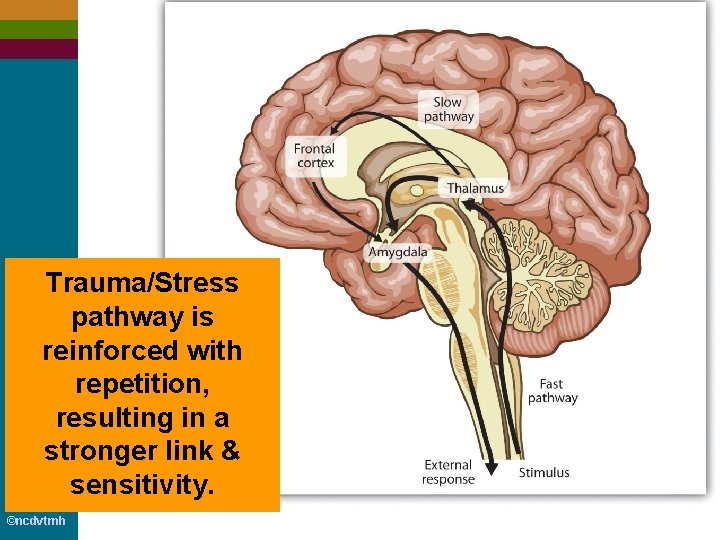
Trauma/Stress pathway is reinforced with repetition, resulting in a stronger link & sensitivity. ©ncdvtmh
Basic Physiological Activity ©ncdvtmh
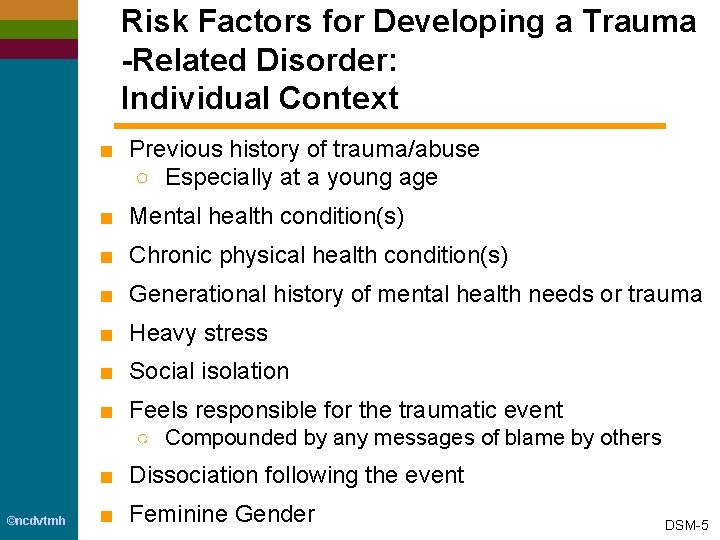
Risk Factors for Developing a Trauma -Related Disorder: Individual Context ■ Previous history of trauma/abuse ○ Especially at a young age ■ Mental health condition(s) ■ Chronic physical health condition(s) ■ Generational history of mental health needs or trauma ■ Heavy stress ■ Social isolation ■ Feels responsible for the traumatic event ○ Compounded by any messages of blame by others ■ Dissociation following the event ©ncdvtmh ■ Feminine Gender DSM-5

Risk Factors for Developing a Trauma -Related Disorder: Stressor ■ Interpersonal nature of trauma ○ especially when involving caregivers ■ Anticipated vs. Unexpected ■ Ability to act during event ■ Outcome of event ■ Severity of event ■ Proximity to event ■ Frequency of trauma ■ Complexity of trauma ■ Being in the position of perpetrator of violence ©ncdvtmh DSM-5

Protective Factors Mitigating the Risk of Developing a Trauma-Related Disorders ■ Social support ■ Positive connection with caregiver ■ Socioeconomic stability ■ Access to medical and mental health care ©ncdvtmh DSM-5
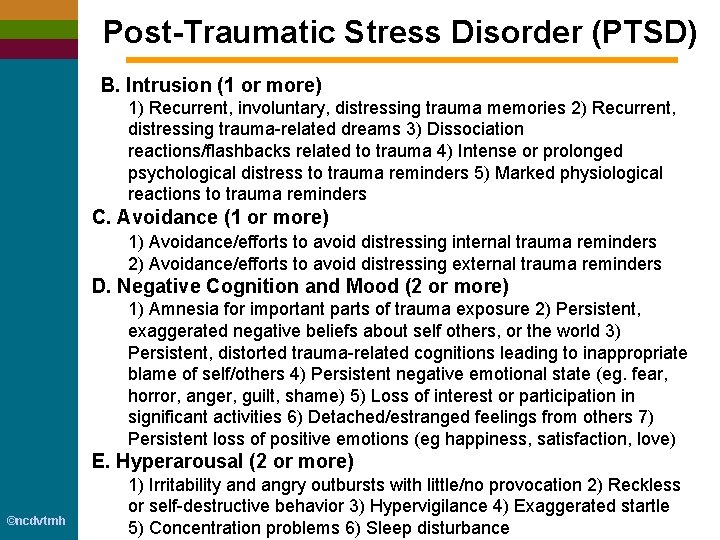
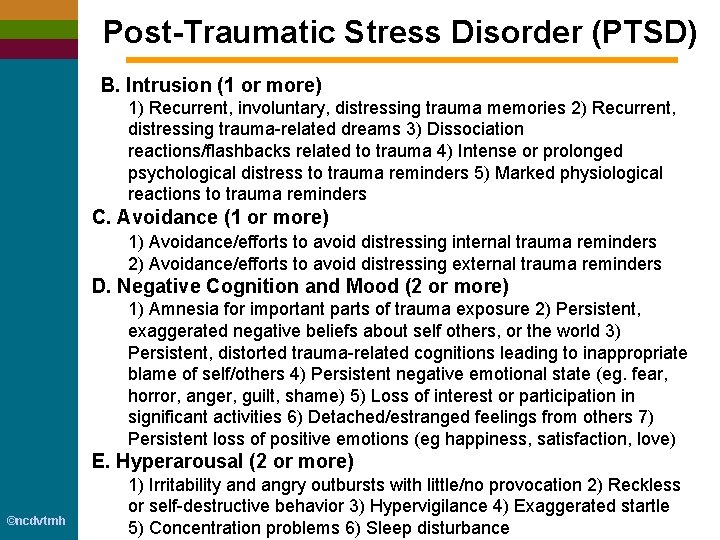
Post-Traumatic Stress Disorder (PTSD) B. Intrusion (1 or more) 1) Recurrent, involuntary, distressing trauma memories 2) Recurrent, distressing trauma-related dreams 3) Dissociation reactions/flashbacks related to trauma 4) Intense or prolonged psychological distress to trauma reminders 5) Marked physiological reactions to trauma reminders C. Avoidance (1 or more) 1) Avoidance/efforts to avoid distressing internal trauma reminders 2) Avoidance/efforts to avoid distressing external trauma reminders D. Negative Cognition and Mood (2 or more) 1) Amnesia for important parts of trauma exposure 2) Persistent, exaggerated negative beliefs about self others, or the world 3) Persistent, distorted trauma-related cognitions leading to inappropriate blame of self/others 4) Persistent negative emotional state (eg. fear, horror, anger, guilt, shame) 5) Loss of interest or participation in significant activities 6) Detached/estranged feelings from others 7) Persistent loss of positive emotions (eg happiness, satisfaction, love) E. Hyperarousal (2 or more) ©ncdvtmh 1) Irritability and angry outbursts with little/no provocation 2) Reckless or self-destructive behavior 3) Hypervigilance 4) Exaggerated startle 5) Concentration problems 6) Sleep disturbance
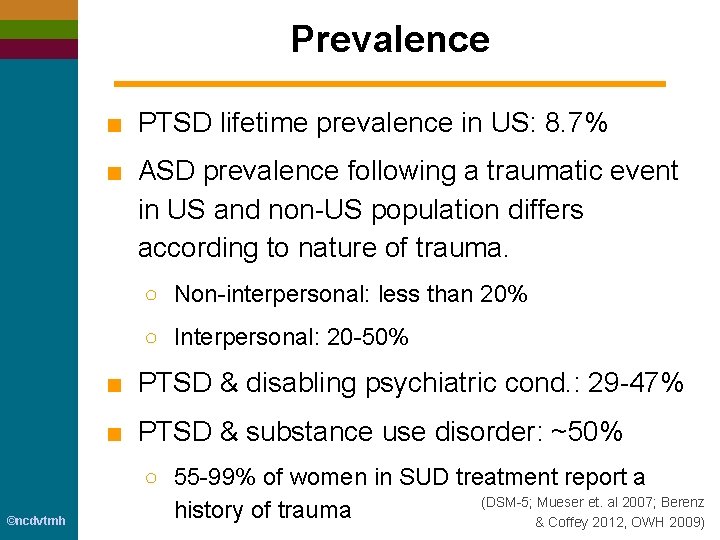
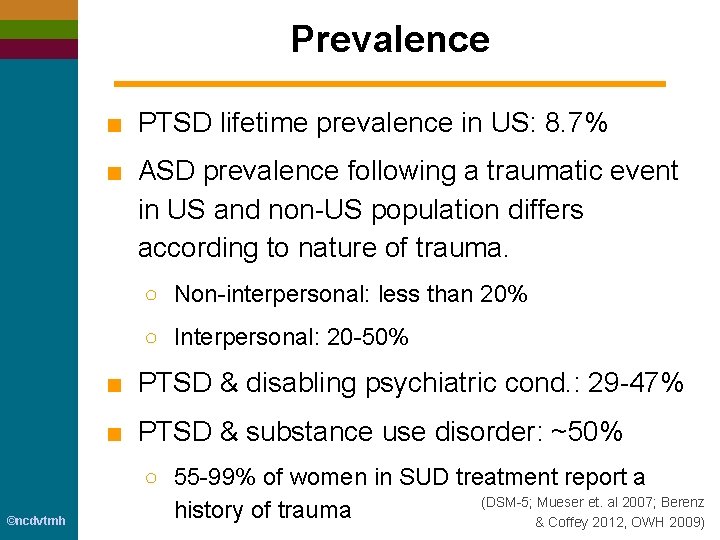
Prevalence ■ PTSD lifetime prevalence in US: 8. 7% ■ ASD prevalence following a traumatic event in US and non-US population differs according to nature of trauma. ○ Non-interpersonal: less than 20% ○ Interpersonal: 20 -50% ■ PTSD & disabling psychiatric cond. : 29 -47% ■ PTSD & substance use disorder: ~50% ©ncdvtmh ○ 55 -99% of women in SUD treatment report a (DSM-5; Mueser et. al 2007; Berenz history of trauma & Coffey 2012, OWH 2009)
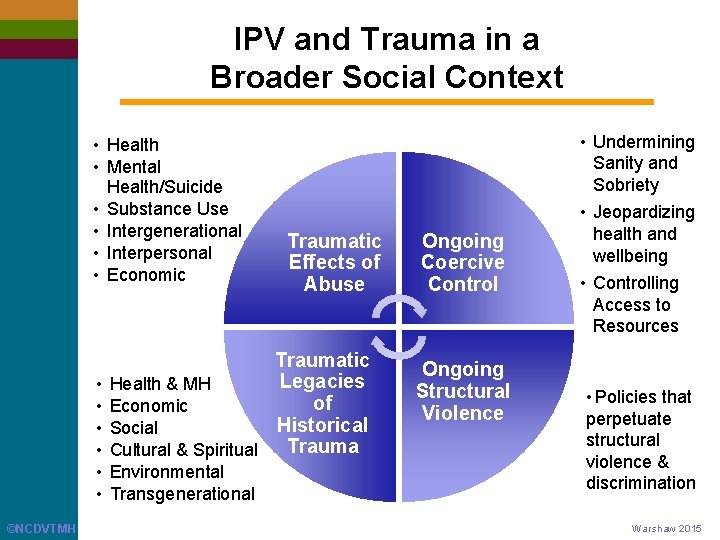
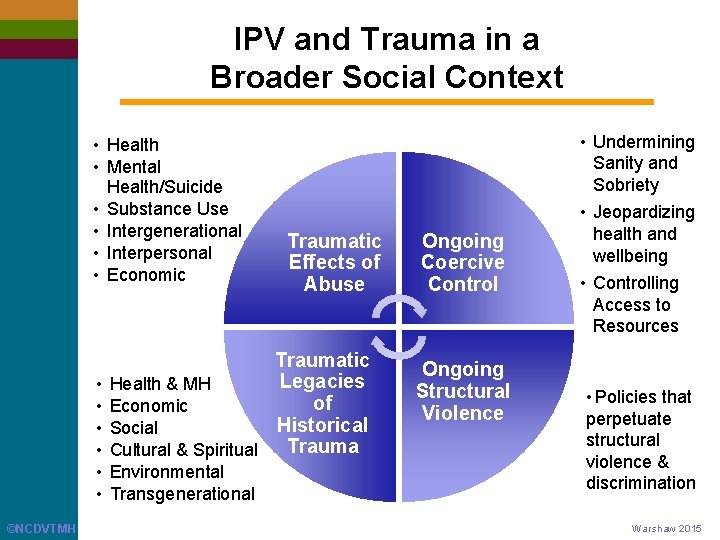
IPV and Trauma in a Broader Social Context • Health • Mental Health/Suicide • Substance Use • Intergenerational • Interpersonal • Economic • Undermining Sanity and Sobriety Traumatic Effects of Abuse Traumatic Legacies Health & MH of Economic Historical Social Trauma Cultural & Spiritual • • • Environmental • Transgenerational ©NCDVTMH Ongoing Coercive Control Ongoing Structural Violence • Jeopardizing health and wellbeing • Controlling Access to Resources • Policies that perpetuate structural violence & discrimination Warshaw 2015
Recognizing the Connections Between Trauma, Victimization, HIV, HCV & Opioid Use Disorders ©ncdvtmh

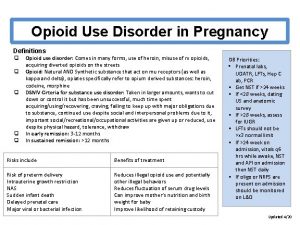
Adverse Childhood Experiences (ACEs) 1. Physical abuse 2. Sexual abuse 3. Emotional abuse 4. Physical neglect 5. Emotional neglect 6. Mother treated violently 7. Substance misuse within household 8. Household mental illness 9. Parental separation or divorce 10. Incarcerated household member ©ncdvtmh (Felitti et al. 1998)
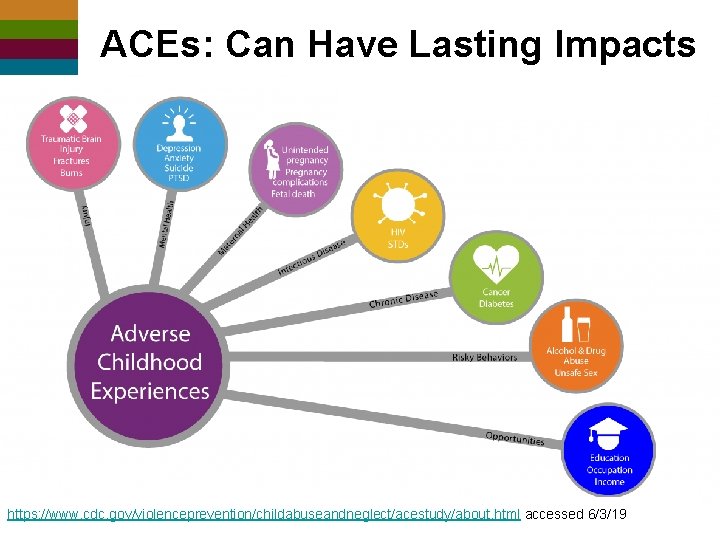
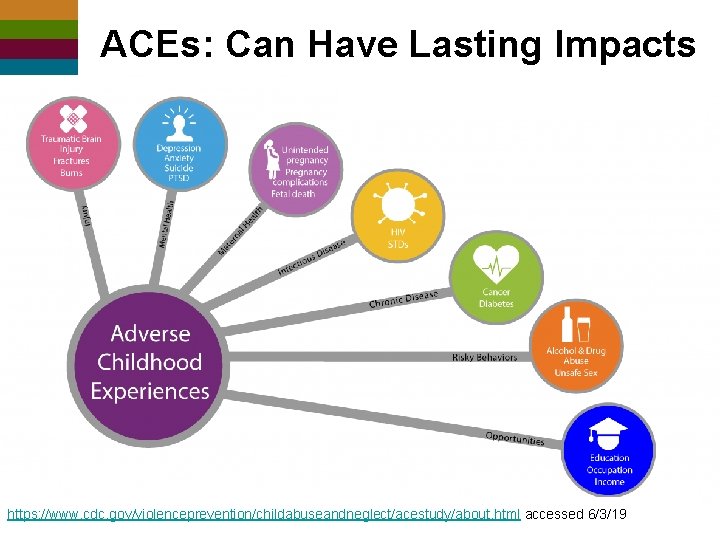
ACEs: Can Have Lasting Impacts https: //www. cdc. gov/violenceprevention/childabuseandneglect/acestudy/about. html accessed 6/3/19 ©ncdvtmh
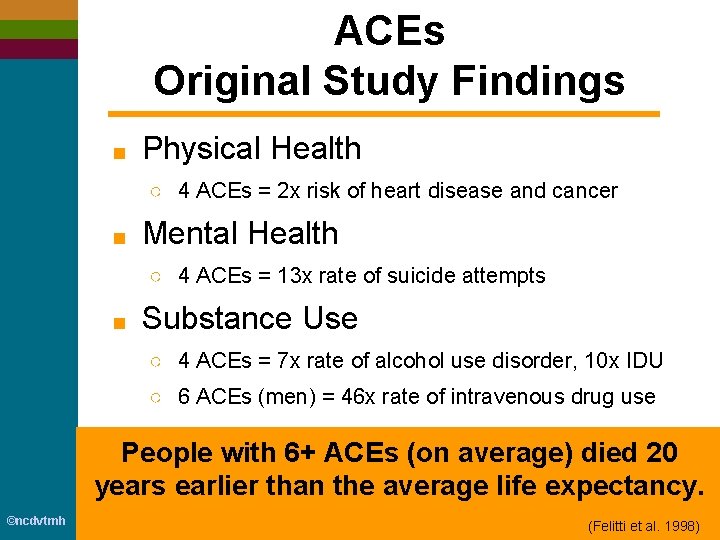
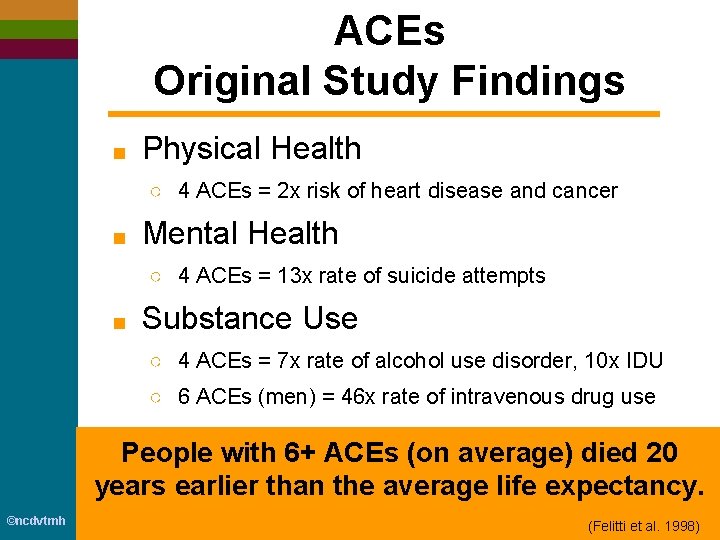
ACEs Original Study Findings ■ Physical Health ○ 4 ACEs = 2 x risk of heart disease and cancer ■ Mental Health ○ 4 ACEs = 13 x rate of suicide attempts ■ Substance Use ○ 4 ACEs = 7 x rate of alcohol use disorder, 10 x IDU ○ 6 ACEs (men) = 46 x rate of intravenous drug use People with 6+ ACEs (on average) died 20 years earlier than the average life expectancy. ©ncdvtmh (Felitti et al. 1998)
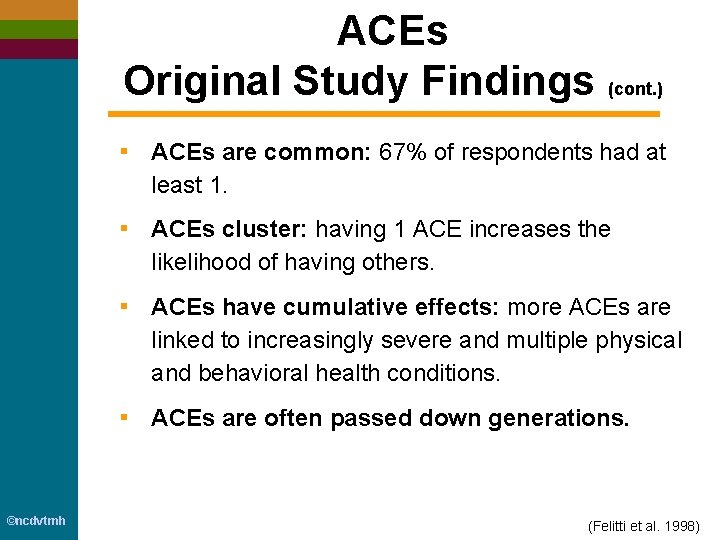
ACEs Original Study Findings (cont. ) ▪ ACEs are common: 67% of respondents had at least 1. ▪ ACEs cluster: having 1 ACE increases the likelihood of having others. ▪ ACEs have cumulative effects: more ACEs are linked to increasingly severe and multiple physical and behavioral health conditions. ▪ ACEs are often passed down generations. ©ncdvtmh (Felitti et al. 1998)
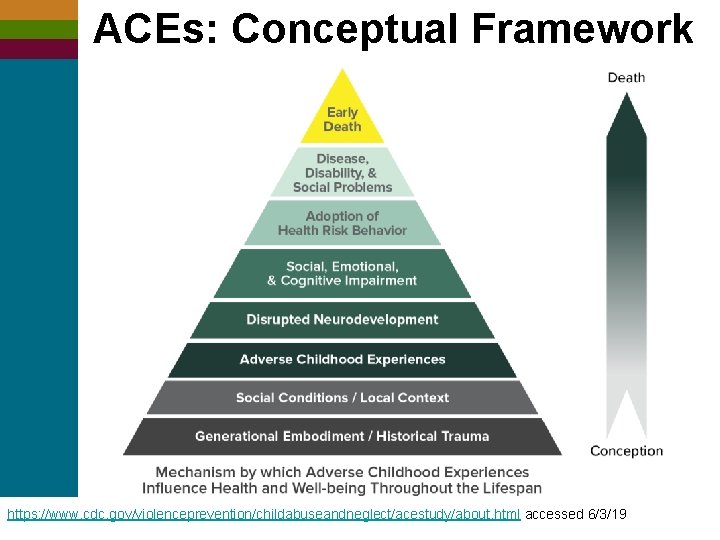
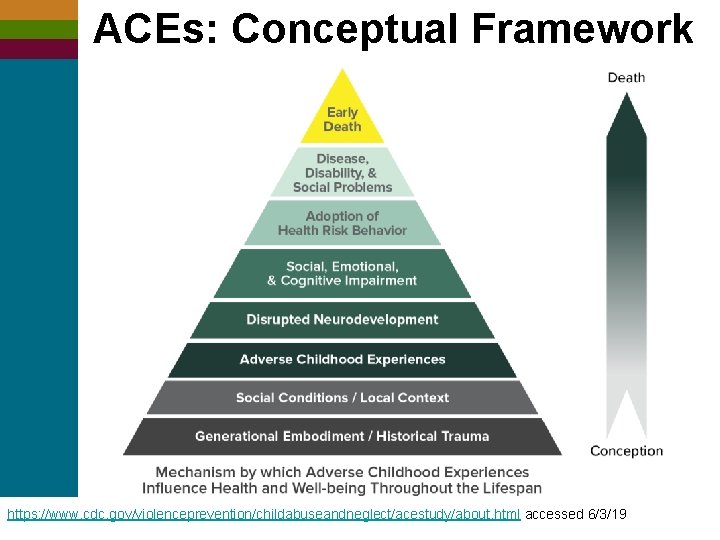
ACEs: Conceptual Framework https: //www. cdc. gov/violenceprevention/childabuseandneglect/acestudy/about. html accessed 6/3/19 ©ncdvtmh
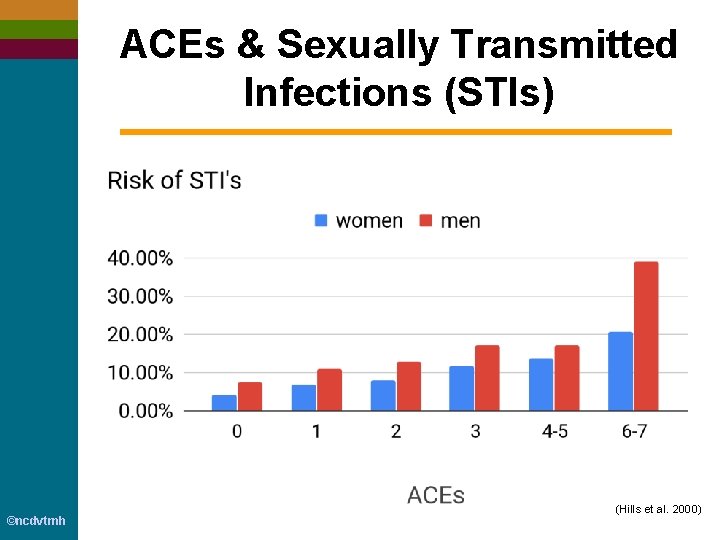
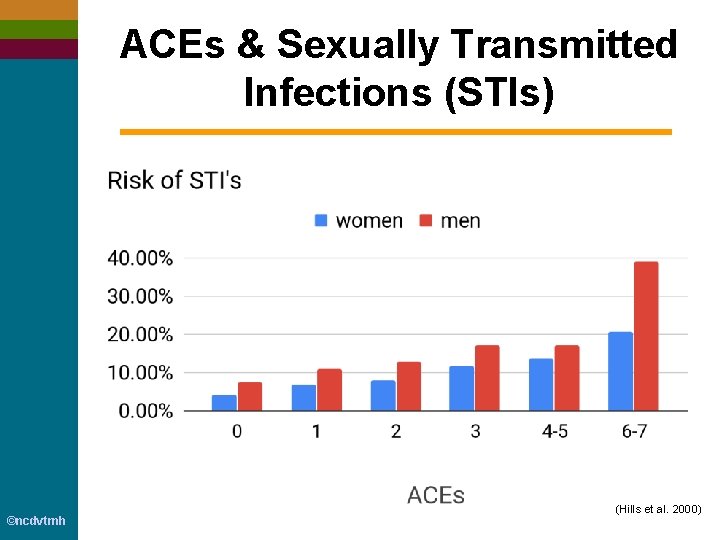
ACEs & Sexually Transmitted Infections (STIs) ©ncdvtmh (Hills et al. 2000)
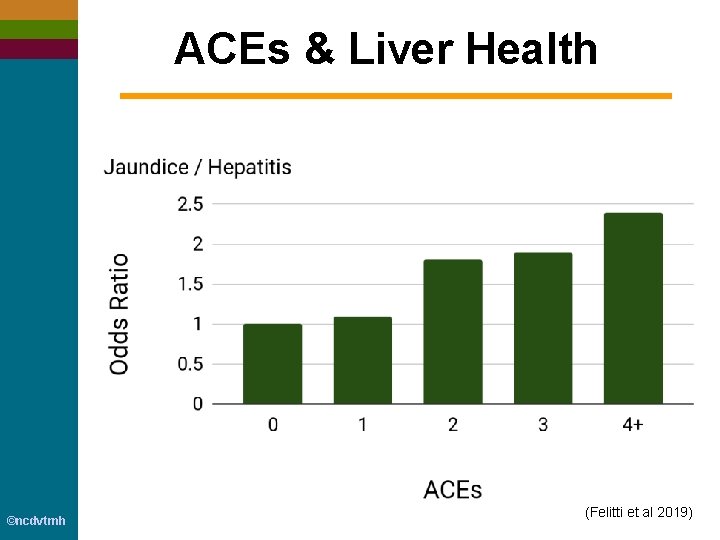
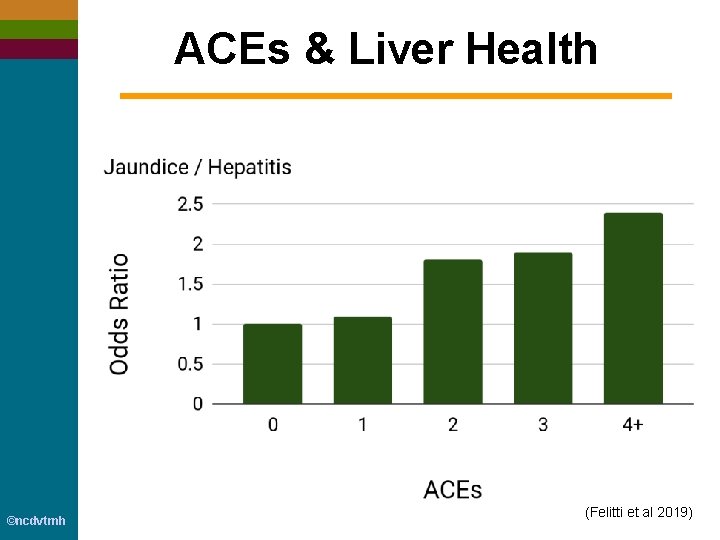
ACEs & Liver Health ©ncdvtmh (Felitti et al 2019)

ACEs & HIV Focusing only on childhood experiences of physical and/or sexual abuse, differences found according to gender: For masculine-identified: ▪ physical abuse: 3 x HIV-risk behaviors ▪ sexual abuse: 8 x HIV-risk behaviors For feminine-identified: ▪ sexual & physical abuse: 5 x HIV-risk behaviors ▪ early & chronic sexual abuse: 7. 4 x HIV-risk behaviors ©ncdvtmh (Bensley et al 2000)
HIV & Interpersonal Violence Across the Lifespan Masculine-identified individuals living w/ HIV ▪ 62% reported at least one traumatic experience. ▪ 50% of those who experienced physical harm indicated it was due to their HIV status. Feminine-identified individuals living w/ HIV ▪ 61. 1% sexual assault (5 x the gen. pop. rate) ▪ 55. 3% IPV (almost 2 x the rate in a national sample) ▪ 39. 3% childhood sexual abuse (>2 x the gen. pop. rate) ▪ 71. 6% abuse (almost 2 x the rate in a national sample) LGBTQ IPV survivors face multiple types of trauma ▪ Family violence, sexual violence, hate crimes, and police brutality. May be subject to abuse by multiple perpetrators and at multiple points in time. ©NCDVTMH Brief et al. , 2004; Zierler 2000; Boarts 2006; Matchinger et al. , 2012, Neti 2005, Pence et al. , 2002, Cohen et al. , 2004, Miller et al. , 2017

Interconnections of Trauma, IPV, HIV & MH/SU Experiencing gender-based violence places women at greater risk for acquiring HIV, and for more rapid disease progression, reduced medication adherence, and more frequent hospitalization as well as for depression, PTSD, and substance use disorders. ©NCDVTMH Experiencing childhood sexual abuse and IPV are associated with increased use of substances, higher rates of depression, and increased HIV risk among men who have sex with men. Illangasekare et al. , 2013; Leserman, 2008
What you need to know about addiction ©ncdvtmh Gabor Mate, MD
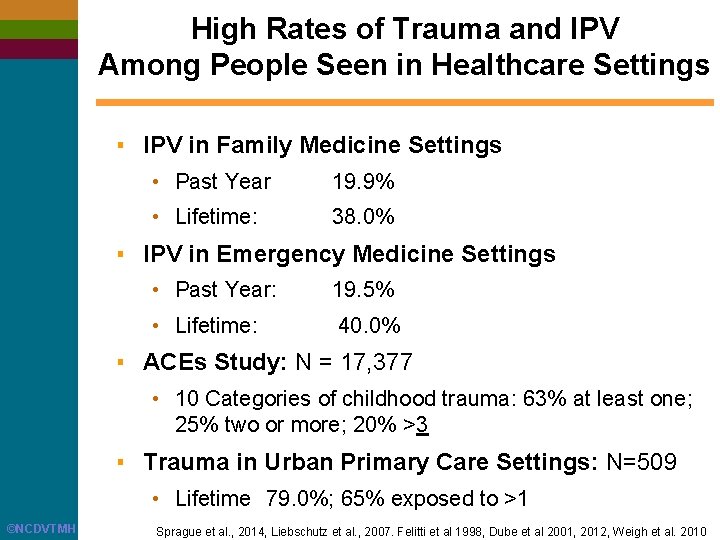
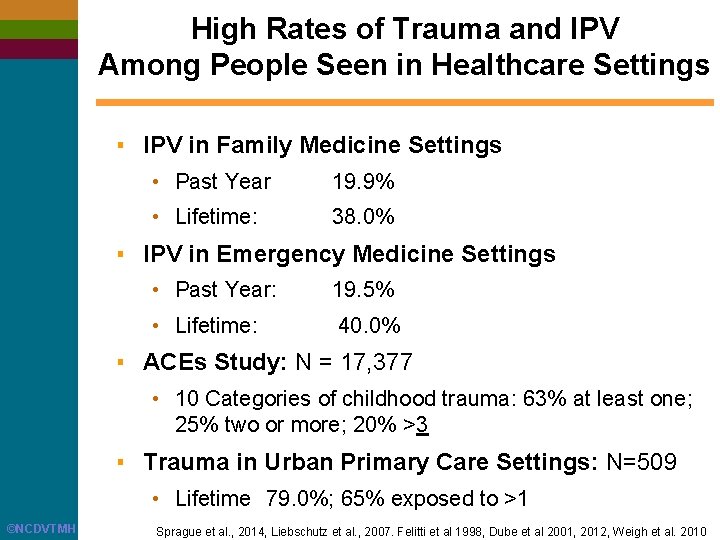
High Rates of Trauma and IPV Among People Seen in Healthcare Settings ▪ IPV in Family Medicine Settings • Past Year 19. 9% • Lifetime: 38. 0% ▪ IPV in Emergency Medicine Settings • Past Year: 19. 5% • Lifetime: 40. 0% ▪ ACEs Study: N = 17, 377 • 10 Categories of childhood trauma: 63% at least one; 25% two or more; 20% >3 ▪ Trauma in Urban Primary Care Settings: N=509 • Lifetime 79. 0%; 65% exposed to >1 ©NCDVTMH Sprague et al. , 2014, Liebschutz et al. , 2007. Felitti et al 1998, Dube et al 2001, 2012, Weigh et al. 2010
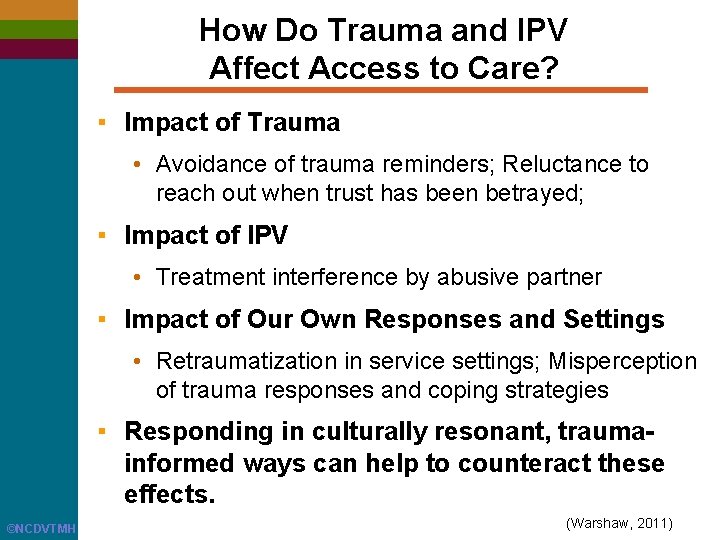
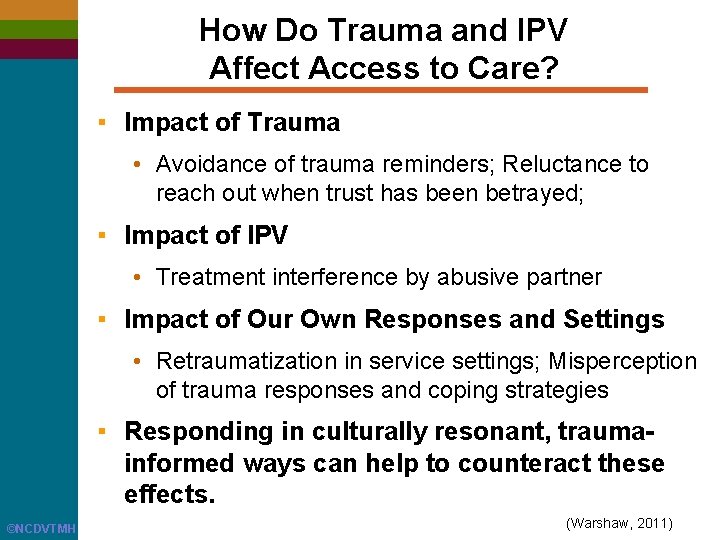
How Do Trauma and IPV Affect Access to Care? ▪ Impact of Trauma • Avoidance of trauma reminders; Reluctance to reach out when trust has been betrayed; ▪ Impact of IPV • Treatment interference by abusive partner ▪ Impact of Our Own Responses and Settings • Retraumatization in service settings; Misperception of trauma responses and coping strategies ▪ Responding in culturally resonant, traumainformed ways can help to counteract these effects. ©NCDVTMH (Warshaw, 2011)
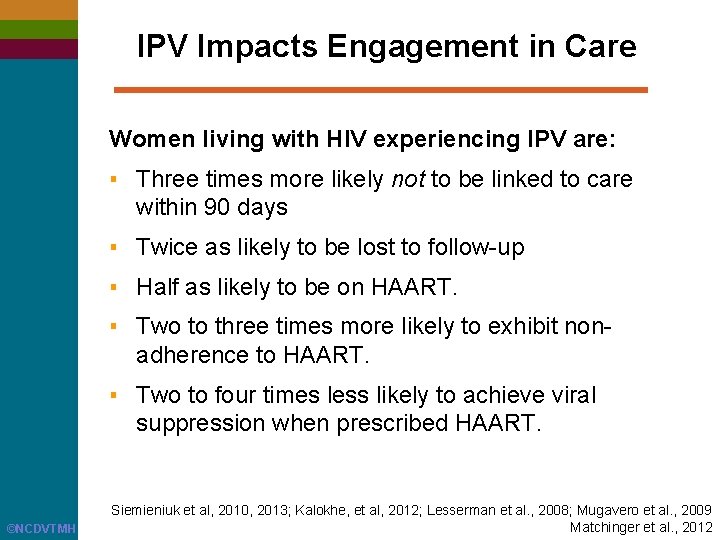
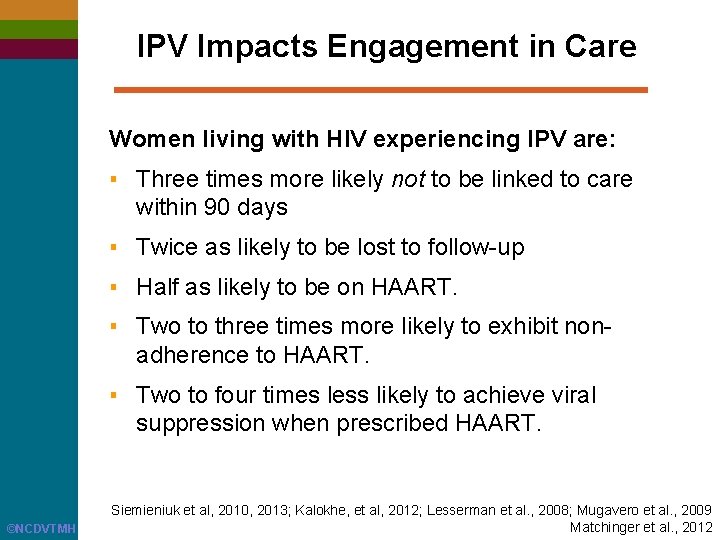
IPV Impacts Engagement in Care Women living with HIV experiencing IPV are: ▪ Three times more likely not to be linked to care within 90 days ▪ Twice as likely to be lost to follow-up ▪ Half as likely to be on HAART. ▪ Two to three times more likely to exhibit nonadherence to HAART. ▪ Two to four times less likely to achieve viral suppression when prescribed HAART. ©NCDVTMH Siemieniuk et al, 2010, 2013; Kalokhe, et al, 2012; Lesserman et al. , 2008; Mugavero et al. , 2009 Matchinger et al. , 2012
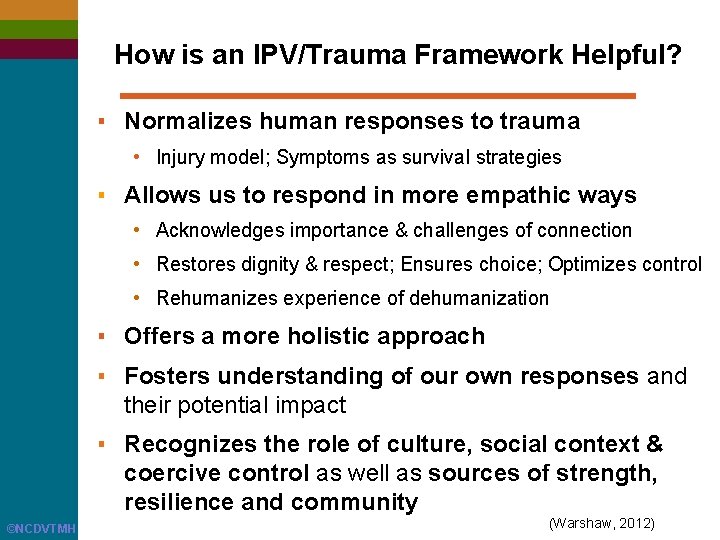
How is an IPV/Trauma Framework Helpful? ▪ Normalizes human responses to trauma • Injury model; Symptoms as survival strategies ▪ Allows us to respond in more empathic ways • Acknowledges importance & challenges of connection • Restores dignity & respect; Ensures choice; Optimizes control • Rehumanizes experience of dehumanization ▪ Offers a more holistic approach ▪ Fosters understanding of our own responses and their potential impact ▪ Recognizes the role of culture, social context & coercive control as well as sources of strength, resilience and community ©NCDVTMH (Warshaw, 2012)
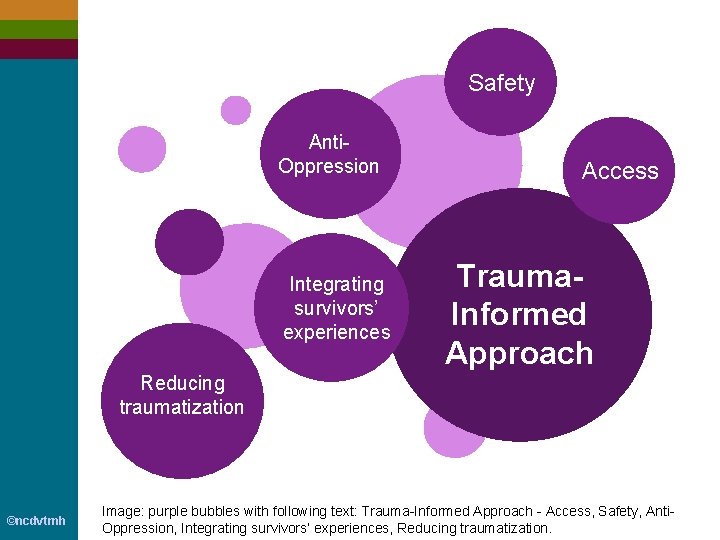
Safety Anti. Oppression Integrating survivors’ experiences Access Trauma. Informed Approach Reducing traumatization ©ncdvtmh Image: purple bubbles with following text: Trauma-Informed Approach - Access, Safety, Anti. Oppression, Integrating survivors’ experiences, Reducing traumatization.
Defining a Trauma-Informed Approach ■ Recognizes the pervasiveness and impact of trauma ○ on survivors, staff, organizations, and communities ■ Ensures that this understanding is incorporated ○ into every aspect of administration, culture, environment, and service delivery ■ Provides guidance on and actively works to decrease retraumatization and support resilience, healing, and well-being ©ncdvtmh ○ at every level of the organization through the work we do and the way we work
Defining a Trauma-Informed Approach (cont. ) ■ Fosters an awareness of what we, as service providers, bring to our interactions ○ including our own experiences of trauma as well as the ways we are affected when we are truly open to the experiences of other people ©ncdvtmh ■ Recognizes ongoing and historical experiences of discrimination and oppression, and works to address social conditions that perpetuate abuse, trauma, discrimination and disparities
Trauma-Informed Approaches Generally recognize: ■ The individual’s need to be respected, informed, connected, and hopeful regarding their own recovery. ■ The interrelation between trauma and symptoms of trauma such as substance use, risk behaviors, eating disorders, depression, and anxiety. ■ The need to work collaboratively with an individual (and their social supports) while actively supporting their empowerment. ©ncdvtmh

Trauma-Informed Environment Physical and Sensory Environment ▪ ▪ ▪ ©ncdvtmh Accessible Welcoming Inclusive Healing Attends to potential trauma reminders
Trauma-Informed Environment 2 Cultural and Linguistic Environment that is responsive to the people and communities being served ©ncdvtmh
Trauma-Informed Environment 3 Relational Environment ▪ ▪ ▪ Caring Respectful Empowering Transparent Demonstrates Trustworthiness ▪ Strives to create emotional safety ©ncdvtmh
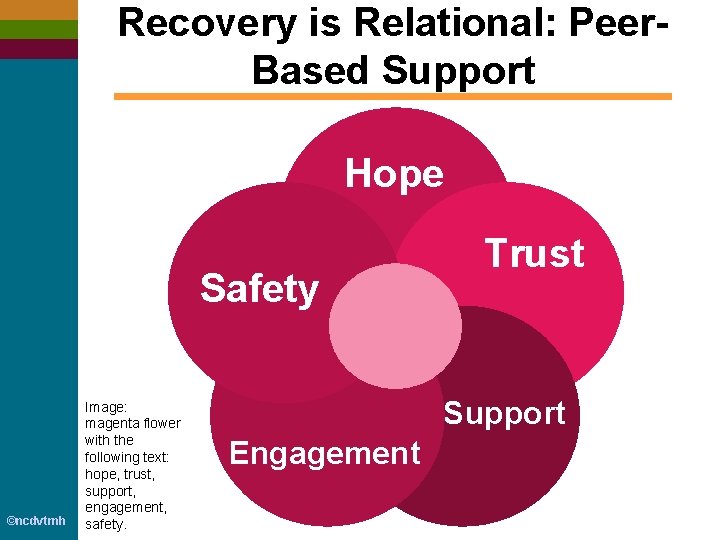
Recovery is Relational: Peer. Based Support Hope Safety ©ncdvtmh Image: magenta flower with the following text: hope, trust, support, engagement, safety. Trust Support Engagement
Trauma-Informed Environment 4 Programmatic Environment Predictable and consistent, while also maximizing flexibility and responsiveness to individual and family needs. Image source: Mark Strobl https: //flic. kr/p/9 xcu. Cw ©ncdvtmh
Increasing Access for People Who Experience Trauma & IPV ▪ Recognize that experiences of lifetime trauma and IPV are common among the people we are serving. ▪ Build safety into services and interactions for people to be able to discuss trauma, IPV, safety, and MH/SU coercion. ▪ Offer services and/or referrals that help address self-defined concerns about trauma, IPV and MH/SU coercion, as part of treatment and continuing recovery. ▪ Treatment-on-demand, array of options. ▪ Services based on need, not ‘compliance’. ▪ Partner with DV/SA programs to ensure a continuum of services for survivors and their children. ©ncdvtmh
Building Safety for Survivors to Talk about their Experiences ■ Integrating awareness and sensitivity to IPV/traumarelated needs starts with the very first contact. ■ Neither pry into, nor silence, trauma stories. ■ Build trusting relationships characterized by mutuality, allow time for relationship to develop. ■ Engender and express nonjudgmental approach and unconditional positive regard. ■ Informed consent, confidentiality, transparency. ■ Minimally invasive, focus on building safety and trust rather than focusing on collecting information. ■ Culturally-responsive, trans-affirming care. ©ncdvtmh
Universal Precautions: Anticipate and Prepare for Potential Trauma Triggers ▪ Medical Procedures • Pap smear or pelvic exam, L&D, Mammograms, Breastfeeding, Ultrasound gel • Catheterization, Intubation, IV insertion • Laryngoscopy/endoscopy/colonoscopy/MRI/CT, Oral exam • Surgery, Anesthesia, Recovery room ▪ Chaotic sensory environment; Gender-related concerns ▪ Relational triggers • Closed room, Having to disrobe, Masked and gowned providers, Being touched, False reassurances, Lying down, Lying still Wagner 2009; www. csacliniciansguide. net ©NCDVTMH

Trauma-Informed Medical Examinations ▪ Always ask for consent. Ensure continued consent at each step. Offer choice-points. ▪ Explain what will be done, how it will be done, and intended purpose. ▪ Ask whether the person would like someone with them. ▪ Do not assume that any procedure or examination is routine. ▪ Observe body language. Ask ‘‘Are you comfortable with this? ’’ or ‘‘Is it OK if I continue with the exam? ’’. ©NCDVTMH https: //healthasahumanright. wordpress. com; Aaron et al. 2013; Cole et al. 2009
Trauma-Informed Medical Examinations (cont). ▪ Avoid false reassurance. Offer specific strategies for self-soothing with permission. Discuss in advance. Have written materials. ▪ If the person’s trauma response is activated, speak in calm voice & let them know where they are and that they are in a safe place. Encourage them to look at you and focus on immediate sensory surroundings and to take breaths. ▪ Use similar precautions if examining a person’s children ©NCDVTMH https: //healthasahumanright. wordpress. com; Aaron et al. 2013; Cole et al. 2009
Additional Resources ©ncdvtmh www. National. Center. DVTrauma. MH. org

Tools for Transformation: Becoming Accessible, Culturally Responsive, and Trauma-Informed Organizations ©ncdvtmh
Coercion Related to Mental Health and Substance Use in the Context of Intimate Partner Violence: A Toolkit for Screening, Assessment, Brief Counseling in Primary Care and Behavioral Health Settings ©ncdvtmh

A Health Care Guide for Survivors of Domestic & Sexual Violence (brochure) www. futureswithoutviolence. org/ new-resource-survivor-brochure/ ©NCDVTMH
Current Evidence: Intimate Partner Violence, Trauma-Related Mental Health & Chronic Illness (fact sheet) http: //www. nationalcenterdvtraumamh. org/wpcontent/uploads/2014/10/Fact. Sheet_IPVTrauma. MHChro nic. Illness_2014_Final. pdf The Relationship Between Intimate Partner Violence & Substance Use (applied research paper) http: //www. nationalcenterdvtraumamh. org/wpcontent/uploads/2014/09/IPV-SABFinal 202. 29. 1620 NO 20 LOGO-1. pdf ©ncdvtmh

Trauma-Focused Interventions for Survivors of Intimate Partner Violence: http: //www. nationalcenterdvtraumamh. org/publicationsproducts/ncdvtmh-online-repository-of-trauma-focusedinterventions-for-survivors-of-intimate-partner-violence/ Trauma-Informed Approaches for LGBT* Survivors of Intimate Partner Violence: http: //www. nationalcenterdvtraumamh. org/publicationsproducts/trauma-informed-approaches-for-lgbqtsurvivors-of-intimate-partner-violence-a-review-ofliterature-and-a-set-of-practice-observations/ ©ncdvtmh

Question & Answer ©ncdvtmh

Thank You! ©ncdvtmh

Future Offerings Stay connected and find out about future offerings www. National. Center. DVTrauma. MH. org/newsletter-sign-up/ ©ncdvtmh
Gabriela Zapata-Alma LCSW, CADC 55 E. Jackson Blvd. , Suite 301 Chicago, IL 60604 P: 312 -726 -7020 TTY: 312 -726 -4110 www. nationalcenterdvtraumamh. org gzapata. alma@ncdvtmh. org Twitter: @ncdvtmh ©ncdvtmh Funded by Administration on Children Youth and Families Administration for Children and Families, US Department of Health and Human Services
 Traumainformed care
Traumainformed care Rass vs poss
Rass vs poss Opioid reseptörleri
Opioid reseptörleri äquivalenzdosis opioide
äquivalenzdosis opioide Opioid overdose
Opioid overdose Opioid overdose
Opioid overdose Opioid overdose
Opioid overdose Types of pain
Types of pain Mechanism of action of opioid analgesics
Mechanism of action of opioid analgesics Nips pain score
Nips pain score Opioid receptors location
Opioid receptors location Non-opioid
Non-opioid Suzanne nesbit
Suzanne nesbit Non-opioid
Non-opioid Kentucky opioid response effort
Kentucky opioid response effort A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Chapter 24 sexually transmitted diseases and hiv/aids
Chapter 24 sexually transmitted diseases and hiv/aids Triệu chứng nhiễm hiv
Triệu chứng nhiễm hiv Hiv reverse transcription
Hiv reverse transcription Aidsfobia
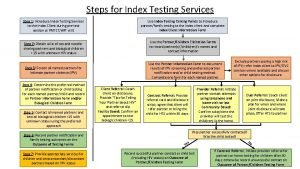
Aidsfobia Steps of index testing
Steps of index testing Elemen penilaian prognas snars edisi 1.1
Elemen penilaian prognas snars edisi 1.1 Phdp in hiv
Phdp in hiv Chii chinonzi hiv
Chii chinonzi hiv Window period hiv
Window period hiv Dot
Dot Iris hiv
Iris hiv Where did hiv come from
Where did hiv come from Hiv risk factors
Hiv risk factors Asante hiv-1 rapid recency assay
Asante hiv-1 rapid recency assay Fiebig hiv
Fiebig hiv Hiv case-based surveillance in ethiopia
Hiv case-based surveillance in ethiopia Triệu chứng nhiễm hiv
Triệu chứng nhiễm hiv Basic hiv course
Basic hiv course Stakeholders in hiv prevention
Stakeholders in hiv prevention Hiv treatments
Hiv treatments Causative organism of hiv/aids
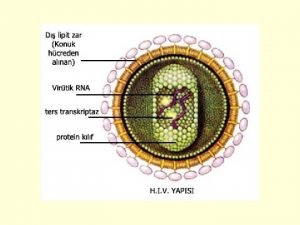
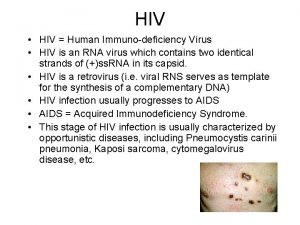
Causative organism of hiv/aids What does hiv stand
What does hiv stand What does hiv stand
What does hiv stand Hiv test window period
Hiv test window period Hiv stool color
Hiv stool color Seks oralny a hiv
Seks oralny a hiv Leukopenia
Leukopenia Hiv lifecycle
Hiv lifecycle 4.jenerasyon vidas hıv duo ultra testi güvenilir mi
4.jenerasyon vidas hıv duo ultra testi güvenilir mi Hiv lifecycle
Hiv lifecycle Hiv
Hiv Name the five lesions associated with hiv/aids chapter 17
Name the five lesions associated with hiv/aids chapter 17 Incubation period of hiv
Incubation period of hiv Icb usp
Icb usp Vidas hiv duo ultra package insert
Vidas hiv duo ultra package insert Profilaksis pasca pajanan
Profilaksis pasca pajanan Bízom benned uram jézus
Bízom benned uram jézus Hiv patologia
Hiv patologia Cytomegalavirus
Cytomegalavirus Most complex characters evolve
Most complex characters evolve Indurerat
Indurerat Burkitt lymphoma
Burkitt lymphoma Negative hiv test result
Negative hiv test result