The Four Heart Sounds S 1 S 2


- Slides: 43
The Four Heart Sounds (S 1, S 2, S 3, S 4) William K. Freeman, MD
Learning Objectives • Understand the mechanisms and timing of the four heart sounds: S 1, S 2, S 3, and S 4 • Integrate auscultation, carotid upstroke, and jugular venous pulsation in the identification of the four heart sounds • Discuss common abnormalities of S 1 and S 2 • Understand the pathophysiology associated with S 3 and S 4 and the differential diagnosis of these findings
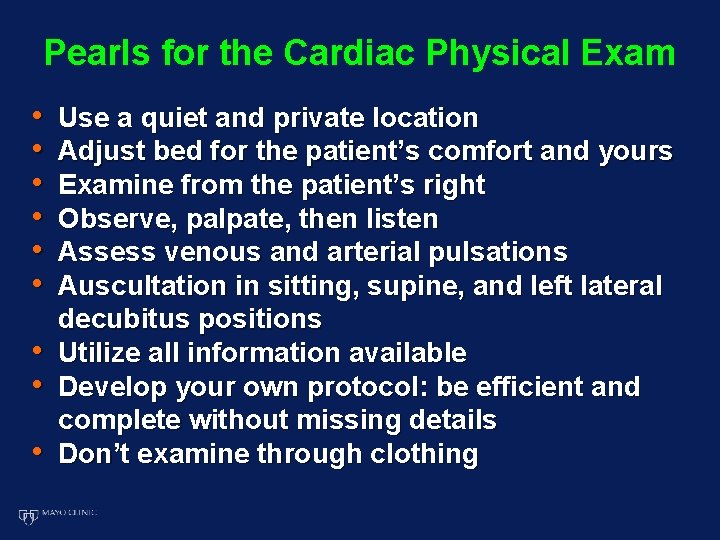
Pearls for the Cardiac Physical Exam • • • Use a quiet and private location Adjust bed for the patient’s comfort and yours Examine from the patient’s right Observe, palpate, then listen Assess venous and arterial pulsations Auscultation in sitting, supine, and left lateral decubitus positions Utilize all information available Develop your own protocol: be efficient and complete without missing details Don’t examine through clothing
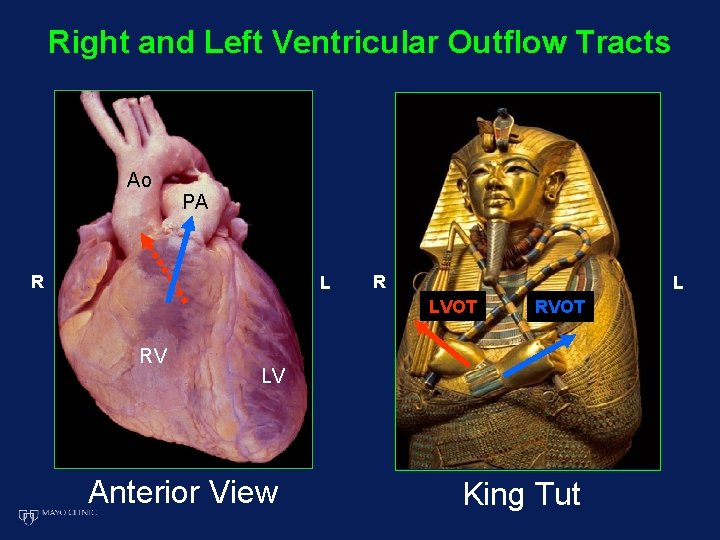
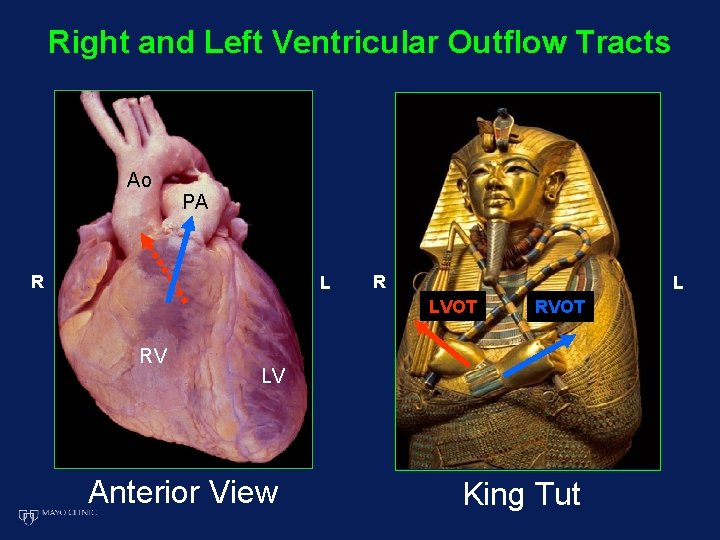
Right and Left Ventricular Outflow Tracts Ao PA R L LVOT RV RVOT LV Anterior View King Tut
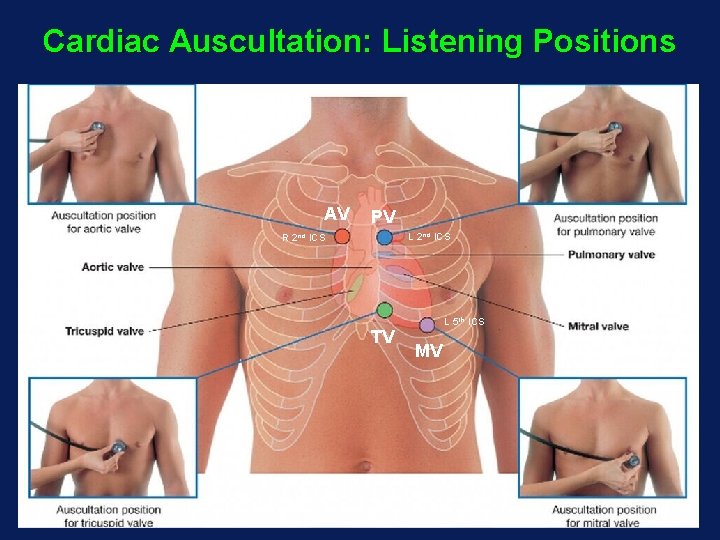
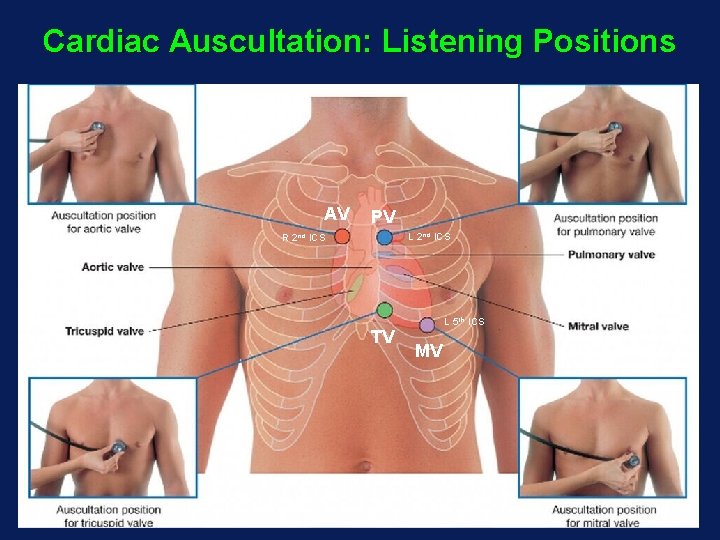
Cardiac Auscultation: Listening Positions AV PV L 2 nd ICS R 2 nd ICS TV L 5 th ICS MV
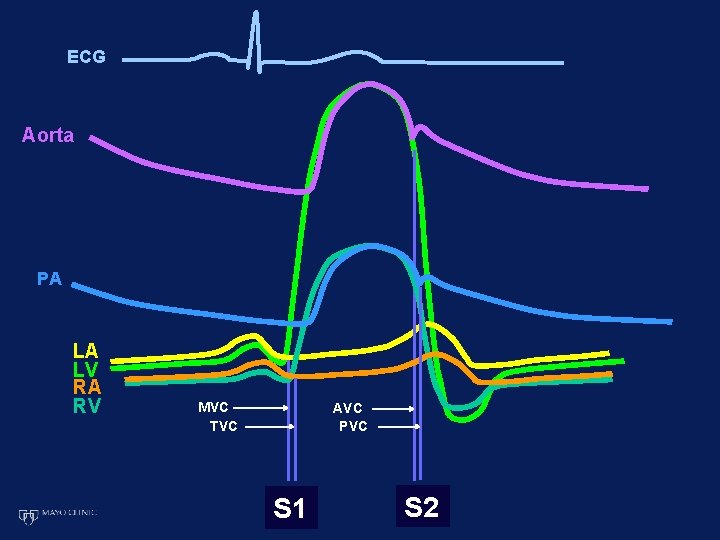
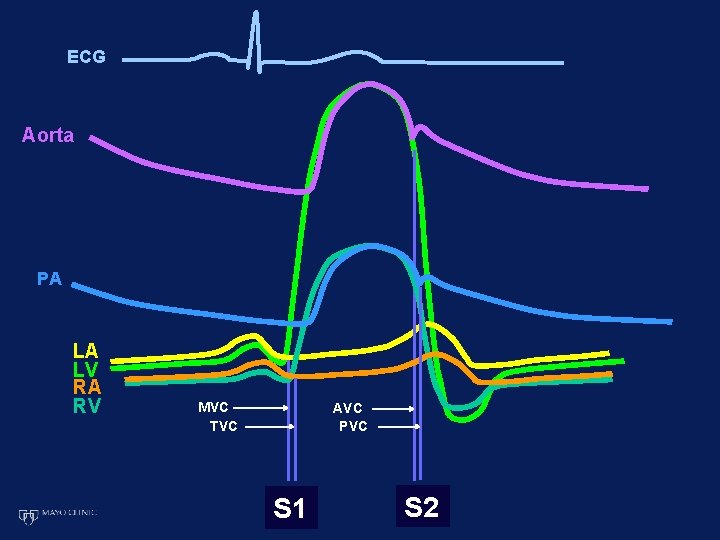
ECG Aorta PA LA LV RA RV MVC TVC AVC PVC S 1 S 2
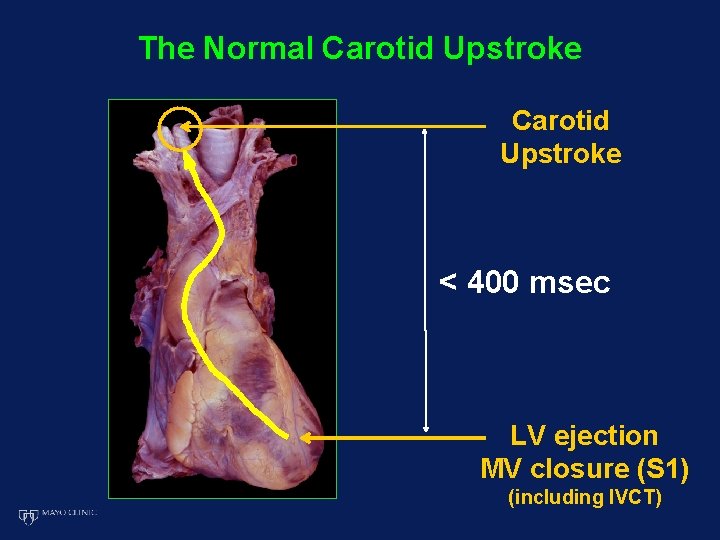
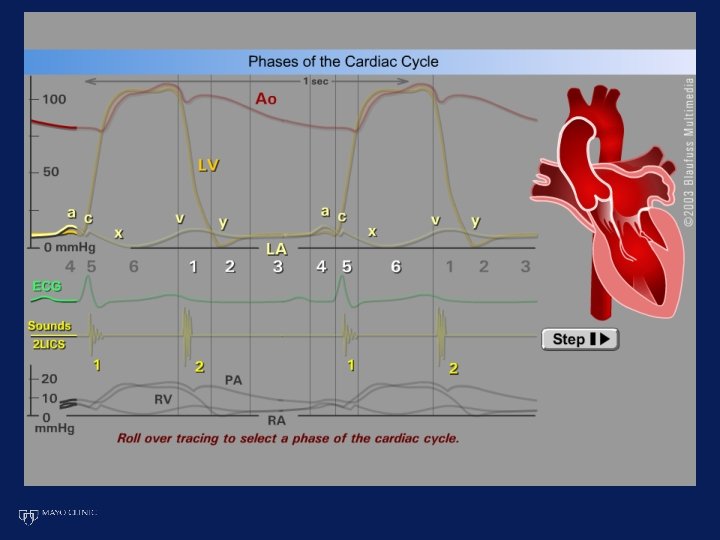
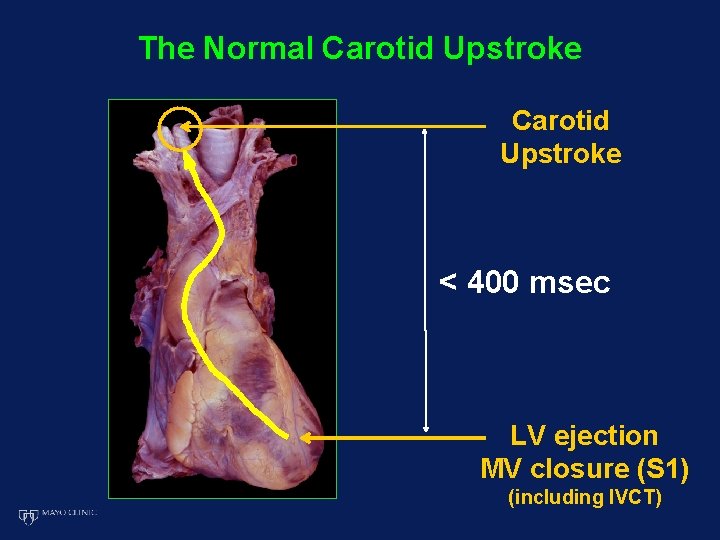
The Normal Carotid Upstroke < 400 msec LV ejection MV closure (S 1) (including IVCT)
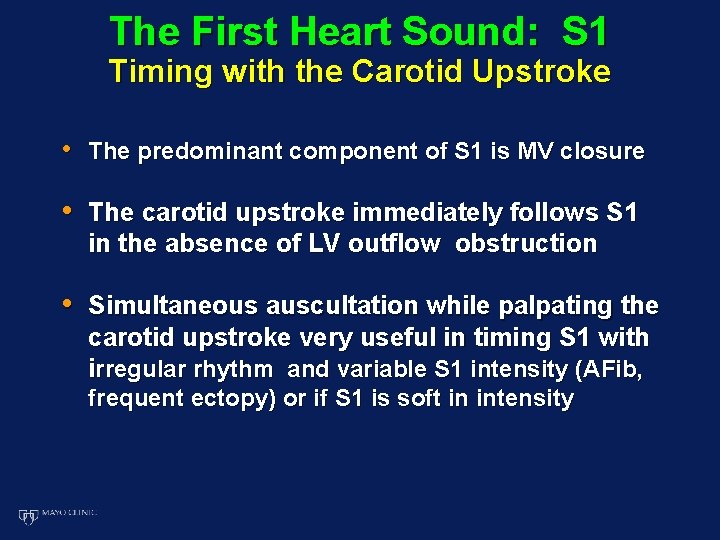
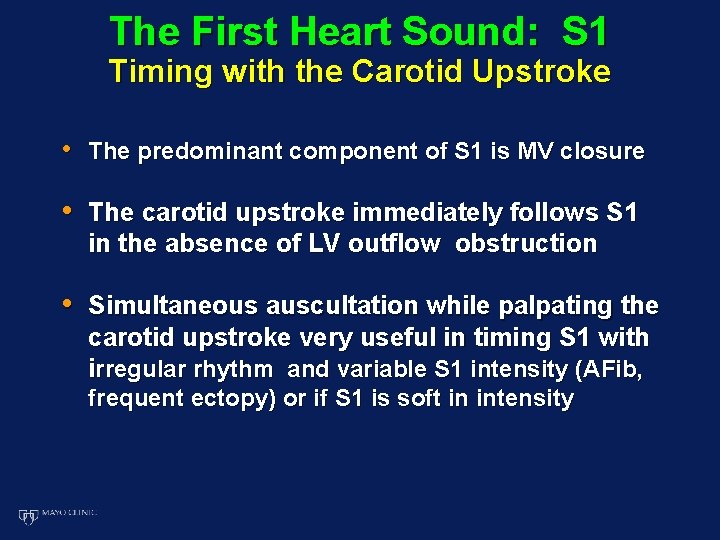
The First Heart Sound: S 1 Timing with the Carotid Upstroke • The predominant component of S 1 is MV closure • The carotid upstroke immediately follows S 1 in the absence of LV outflow obstruction • Simultaneous auscultation while palpating the carotid upstroke very useful in timing S 1 with irregular rhythm and variable S 1 intensity (AFib, frequent ectopy) or if S 1 is soft in intensity
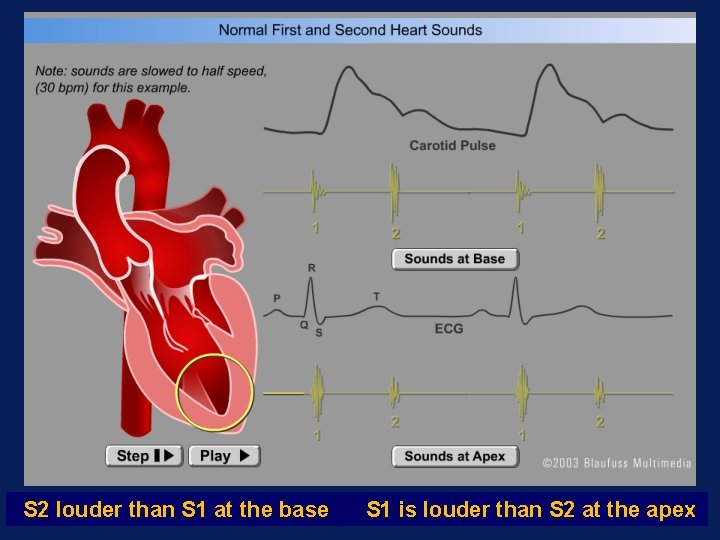
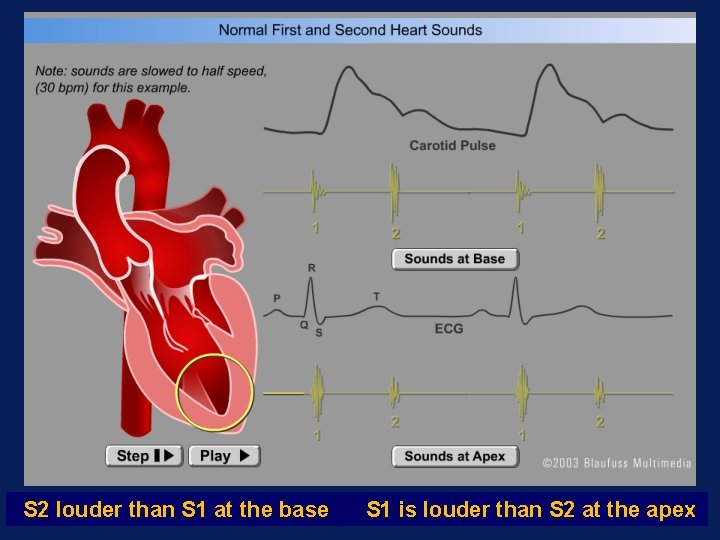
S 2 louder than S 1 at the base S 1 is louder than S 2 at the apex
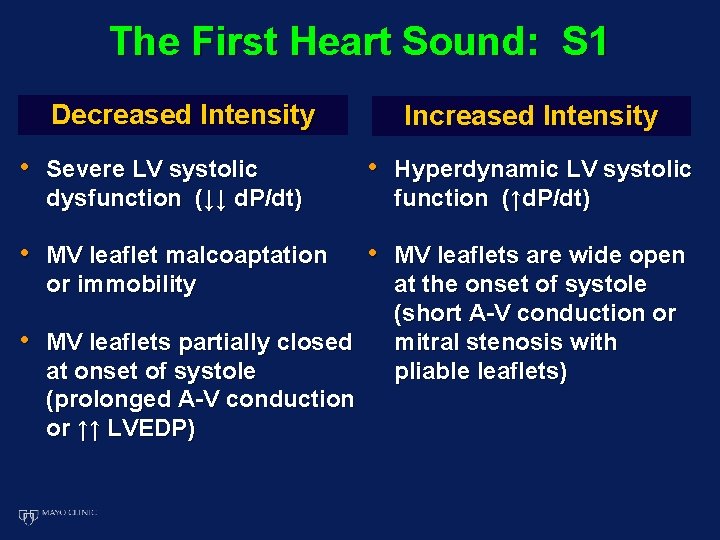
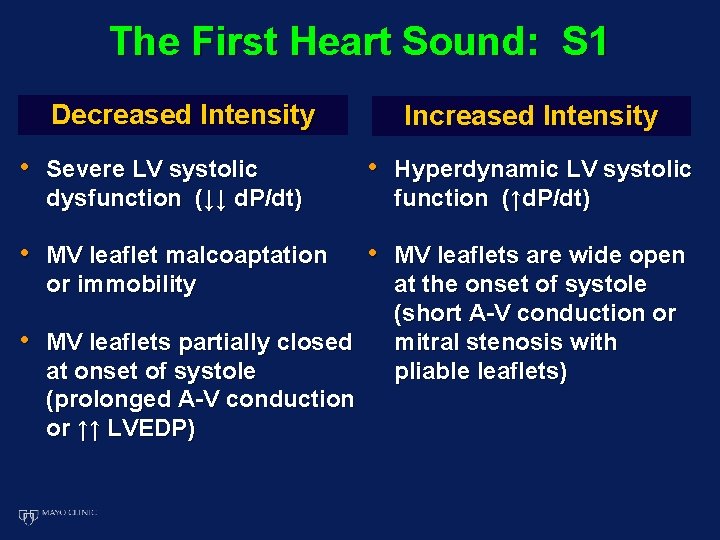
The First Heart Sound: S 1 Decreased Intensity Increased Intensity • Severe LV systolic • Hyperdynamic LV systolic • MV leaflet malcoaptation • MV leaflets are wide open dysfunction (↓↓ d. P/dt) or immobility • MV leaflets partially closed at onset of systole (prolonged A-V conduction or ↑↑ LVEDP) function (↑d. P/dt) at the onset of systole (short A-V conduction or mitral stenosis with pliable leaflets)
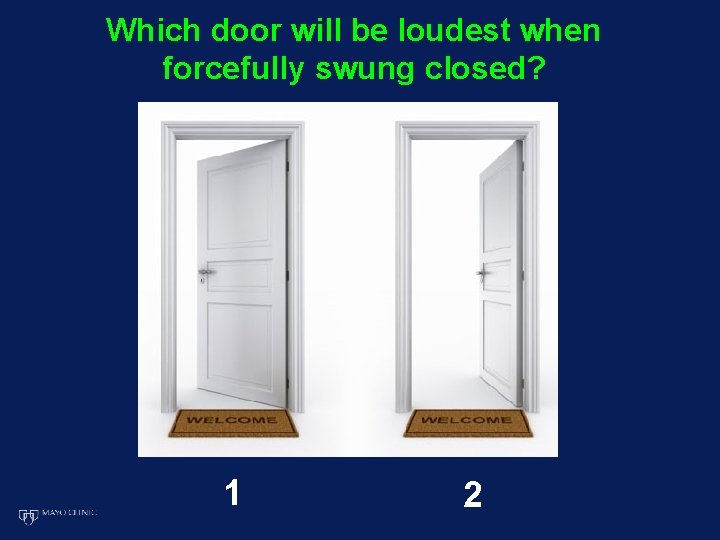
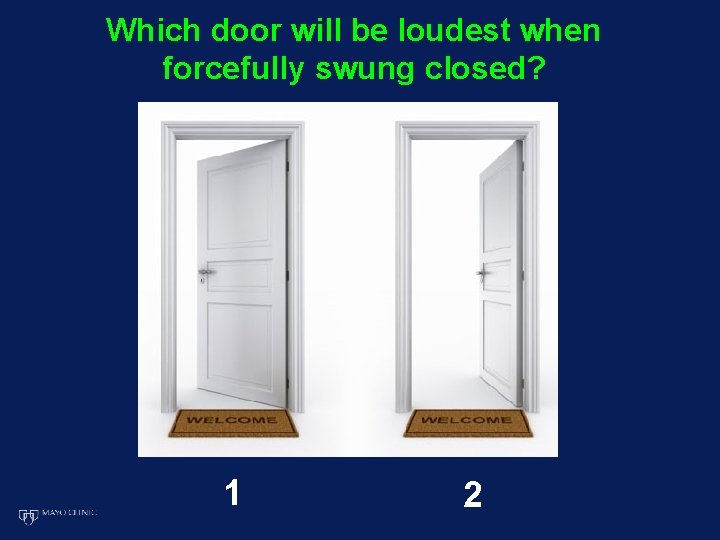
Which door will be loudest when forcefully swung closed? 1 2
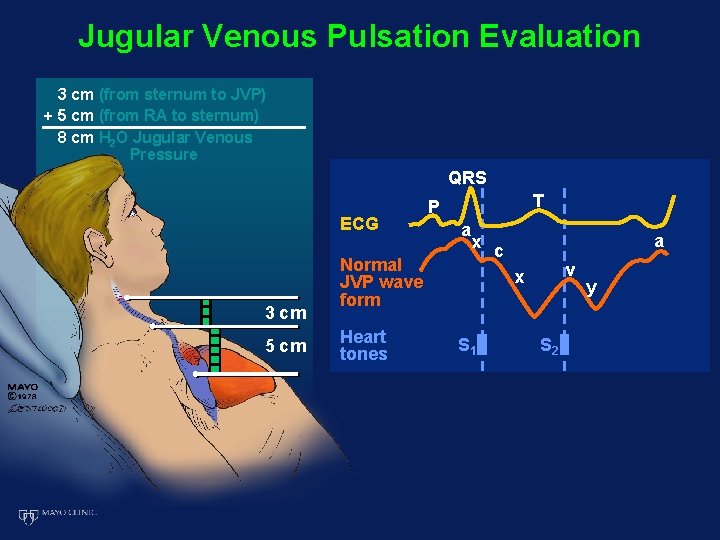
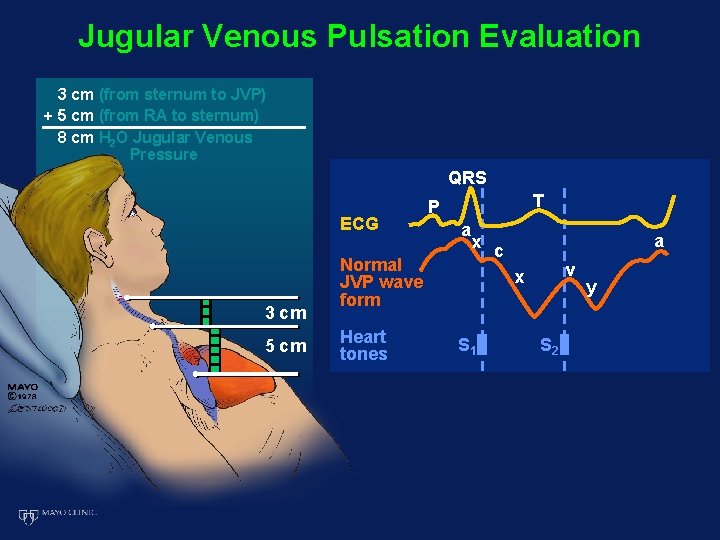
Jugular Venous Pulsation Evaluation 3 cm (from sternum to JVP) + 5 cm (from RA to sternum) 8 cm H 2 O Jugular Venous Pressure QRS ECG 3 cm 5 cm T P a x Normal JVP wave form Heart tones a c v x S 1 S 2 y
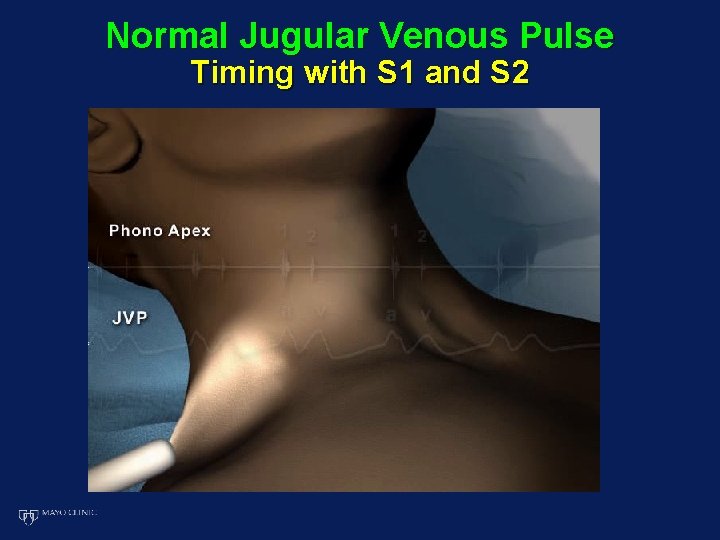
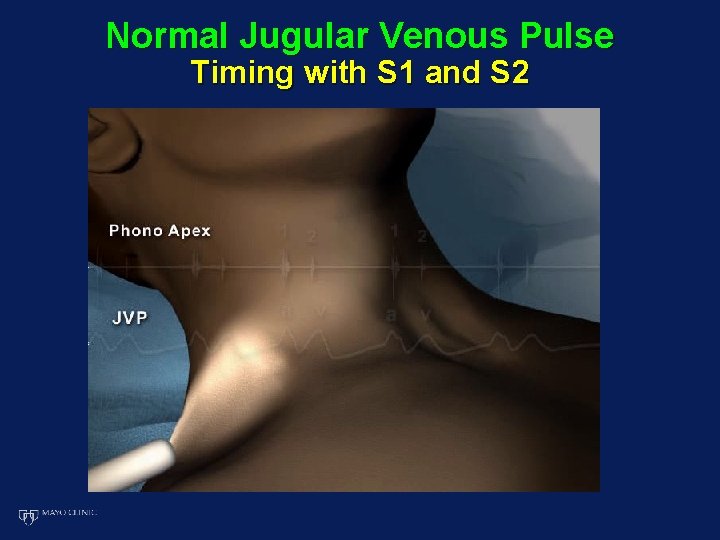
Normal Jugular Venous Pulse Timing with S 1 and S 2
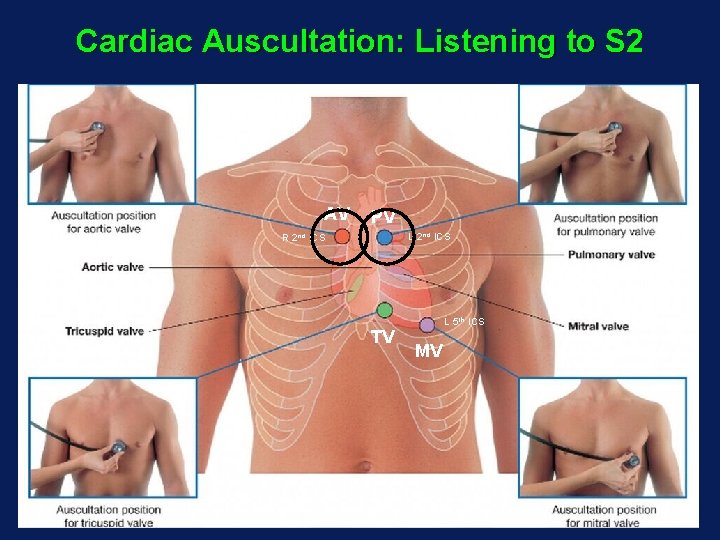
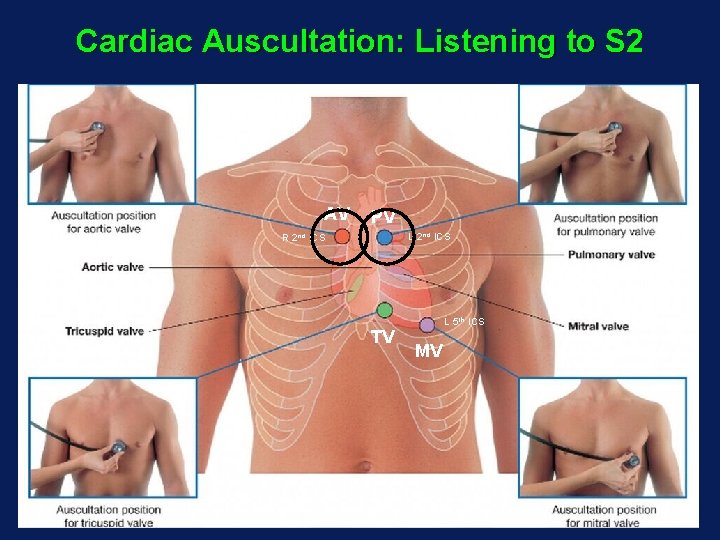
Cardiac Auscultation: Listening to S 2 AV PV L 2 nd ICS R 2 nd ICS TV L 5 th ICS MV
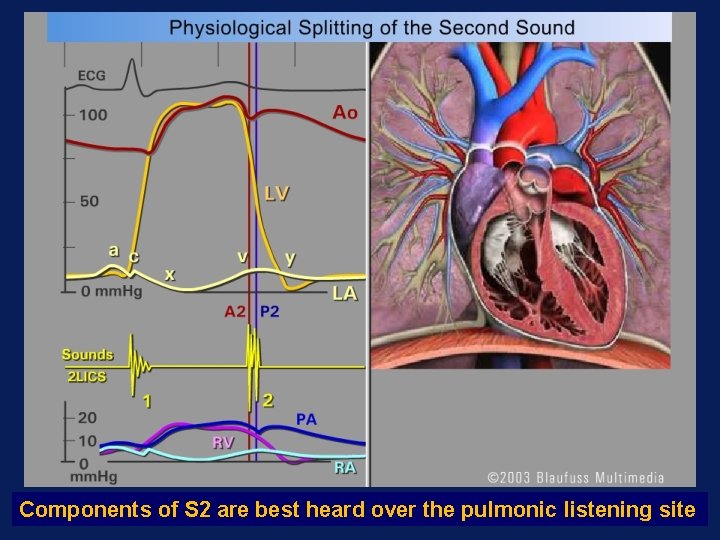
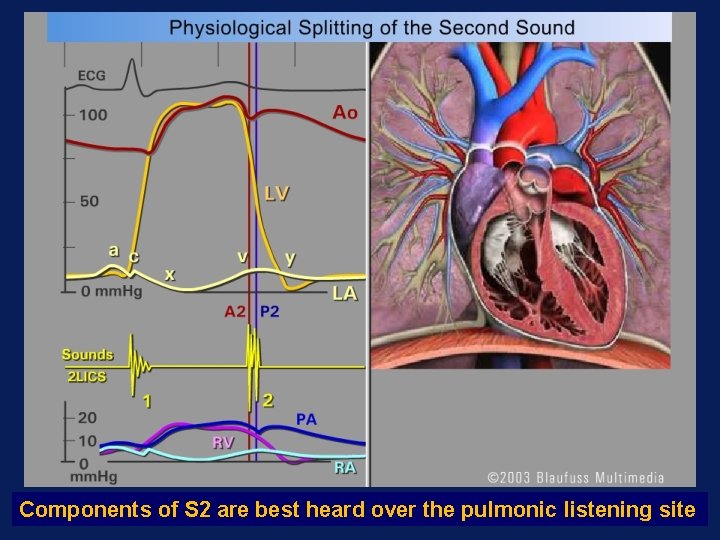
Components of S 2 are best heard over the pulmonic listening site
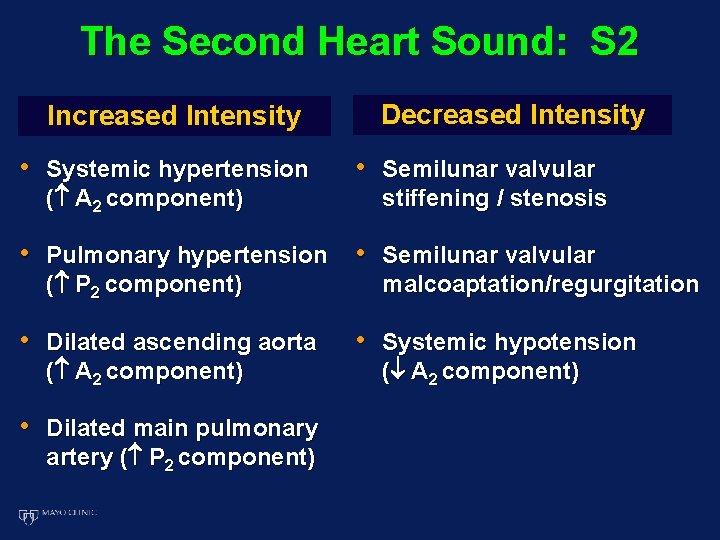
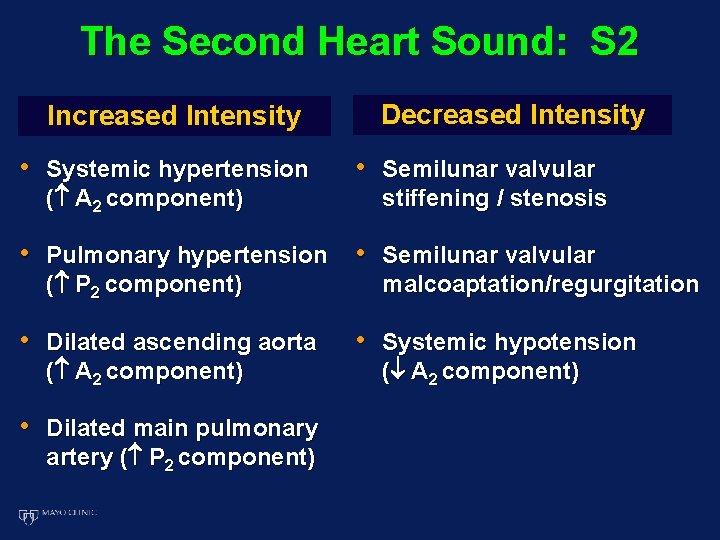
The Second Heart Sound: S 2 Increased Intensity • Systemic hypertension ( A 2 component) Decreased Intensity • Semilunar valvular stiffening / stenosis • Pulmonary hypertension • Semilunar valvular ( P 2 component) • Dilated ascending aorta ( A 2 component) • Dilated main pulmonary artery ( P 2 component) malcoaptation/regurgitation • Systemic hypotension ( A 2 component)
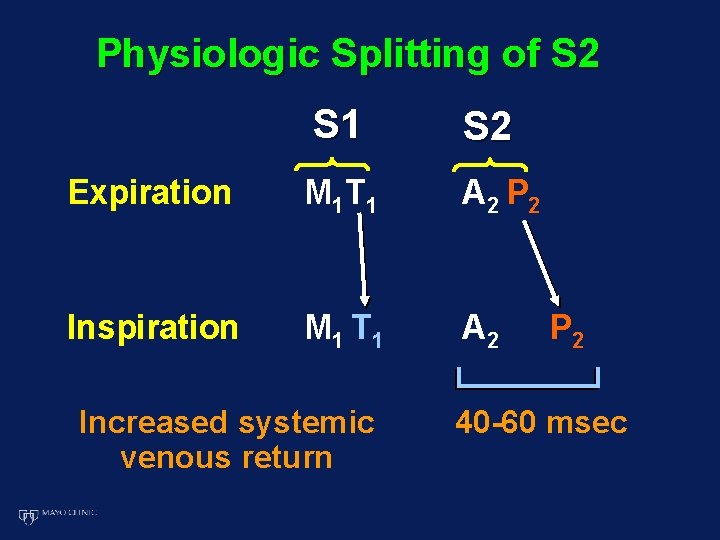
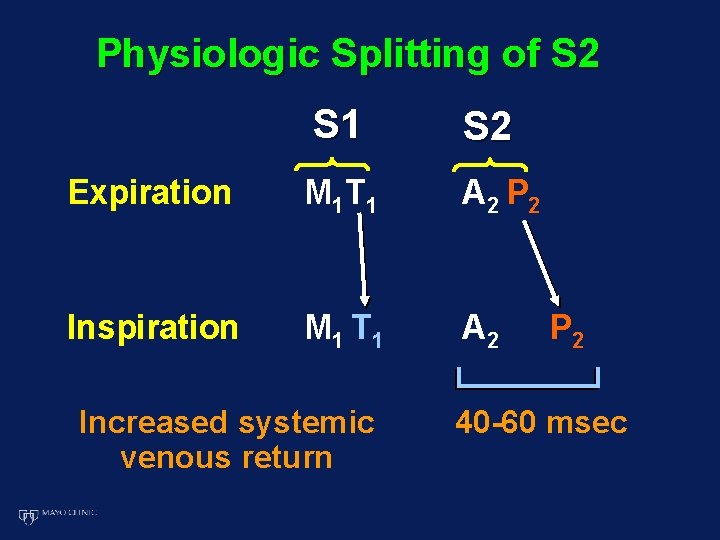
Physiologic Splitting of S 2 S 1 S 2 Expiration M 1 T 1 A 2 P 2 Inspiration M 1 T 1 A 2 Increased systemic venous return P 2 40 -60 msec
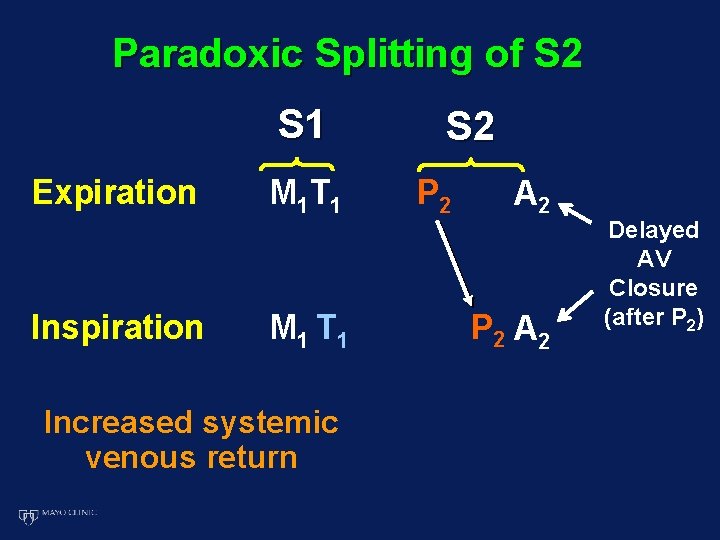
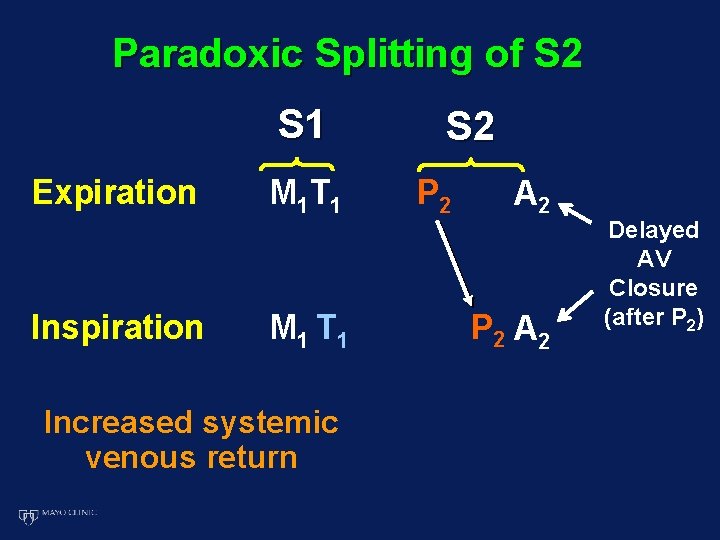
Paradoxic Splitting of S 2 S 1 Expiration Inspiration M 1 T 1 Increased systemic venous return S 2 P 2 A 2 Delayed AV Closure (after P 2)
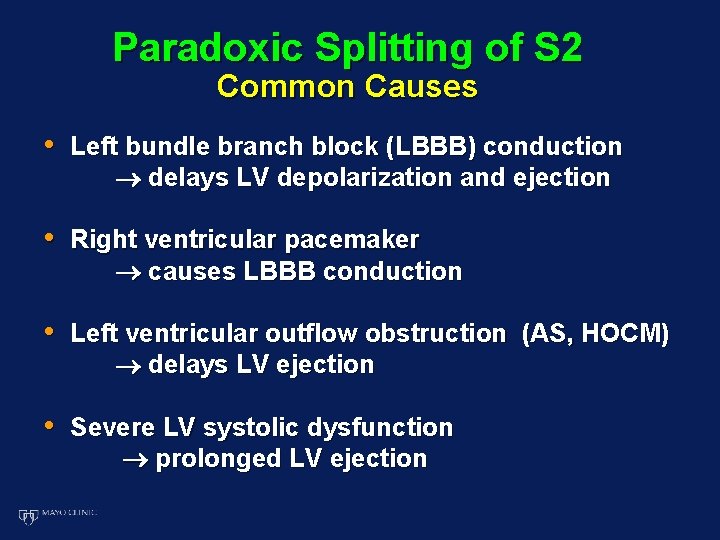
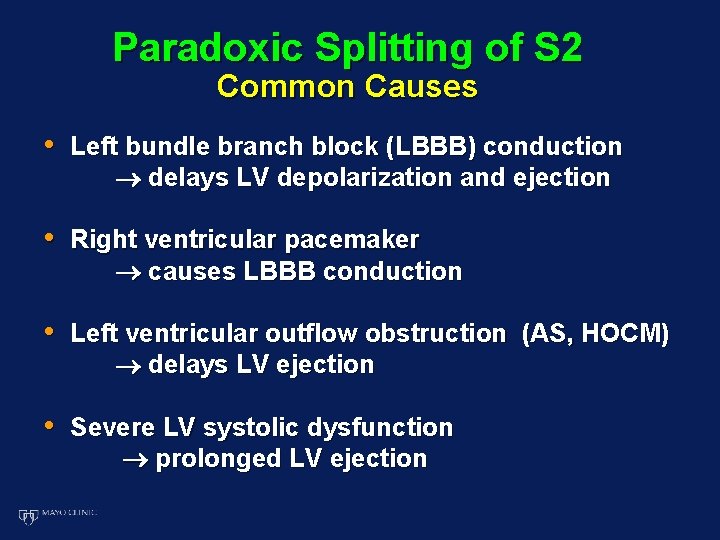
Paradoxic Splitting of S 2 Common Causes • Left bundle branch block (LBBB) conduction delays LV depolarization and ejection • Right ventricular pacemaker causes LBBB conduction • Left ventricular outflow obstruction (AS, HOCM) delays LV ejection • Severe LV systolic dysfunction prolonged LV ejection
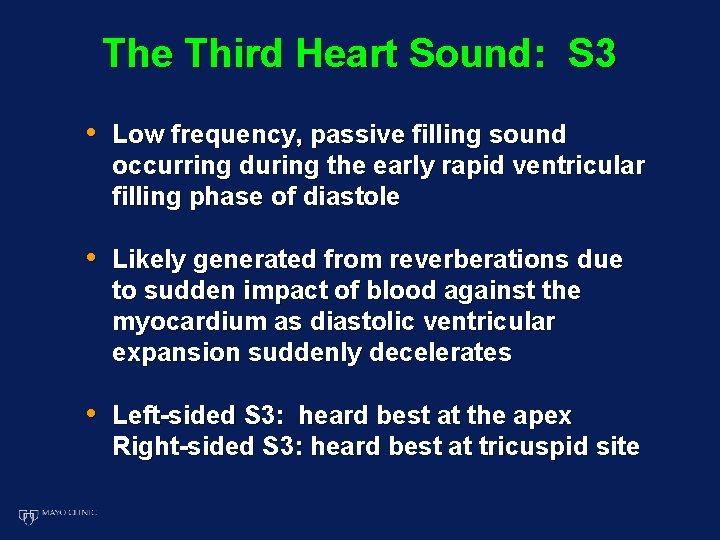
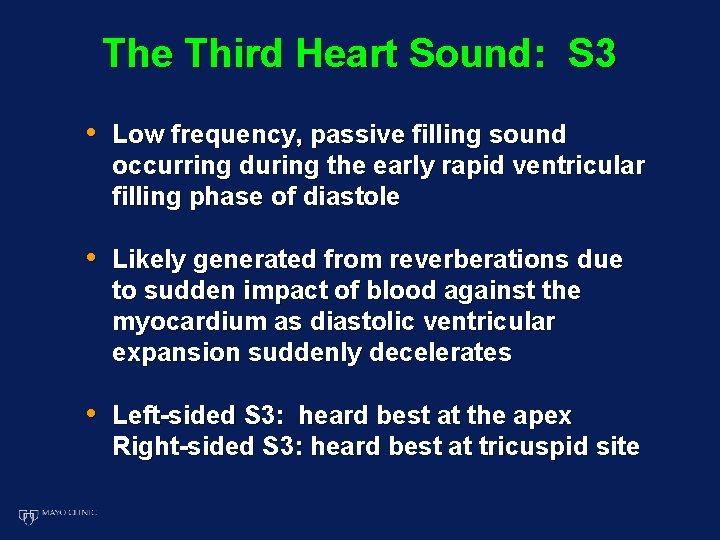
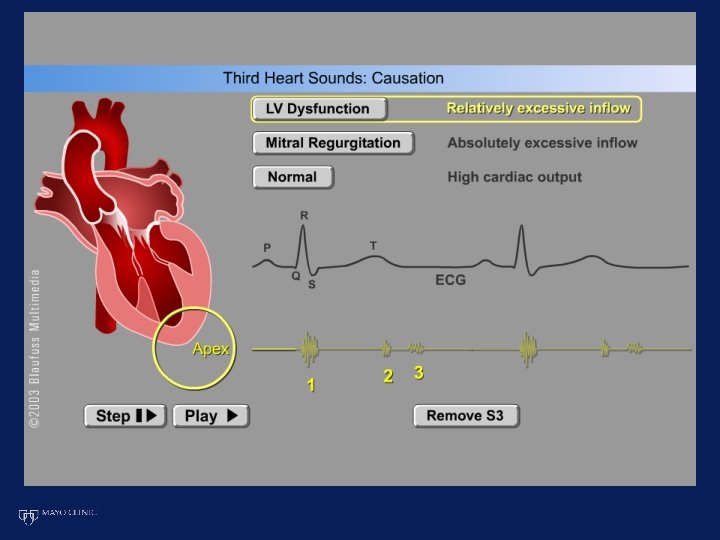
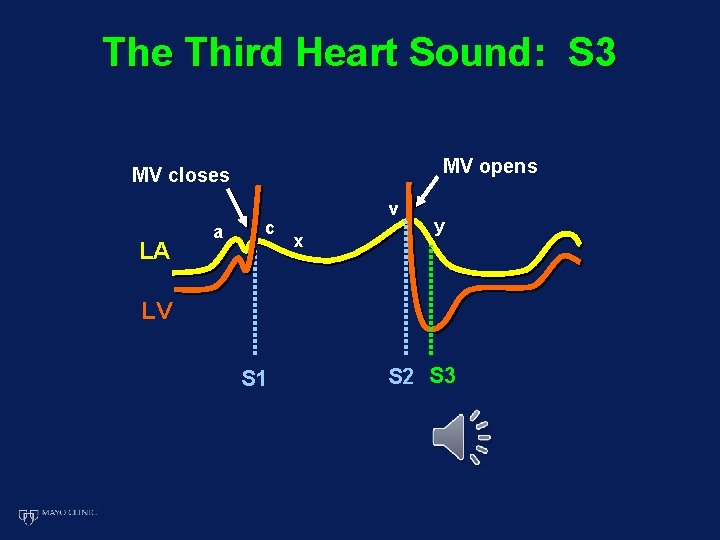
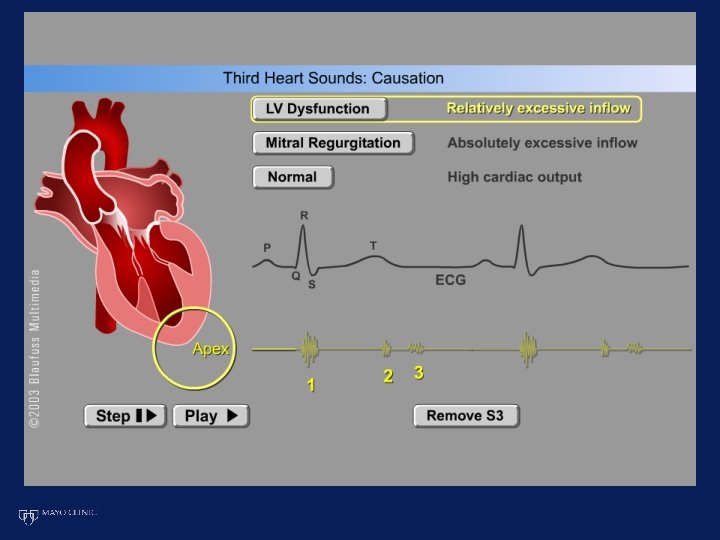
The Third Heart Sound: S 3 • Low frequency, passive filling sound occurring during the early rapid ventricular filling phase of diastole • Likely generated from reverberations due to sudden impact of blood against the myocardium as diastolic ventricular expansion suddenly decelerates • Left-sided S 3: heard best at the apex Right-sided S 3: heard best at tricuspid site
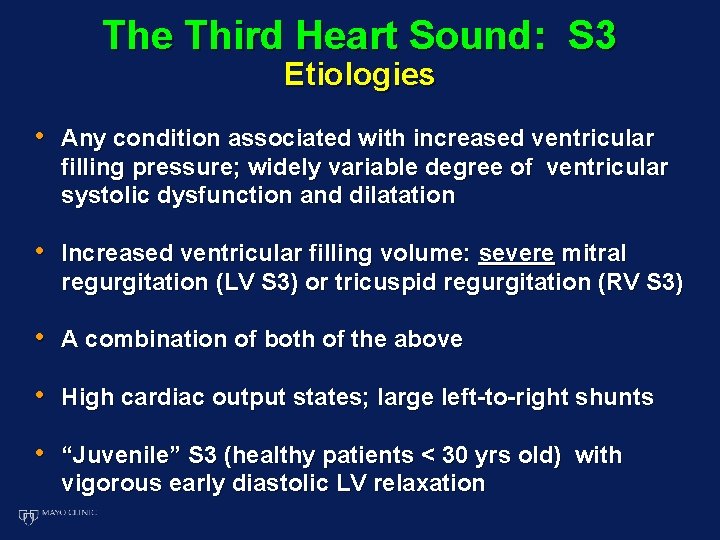
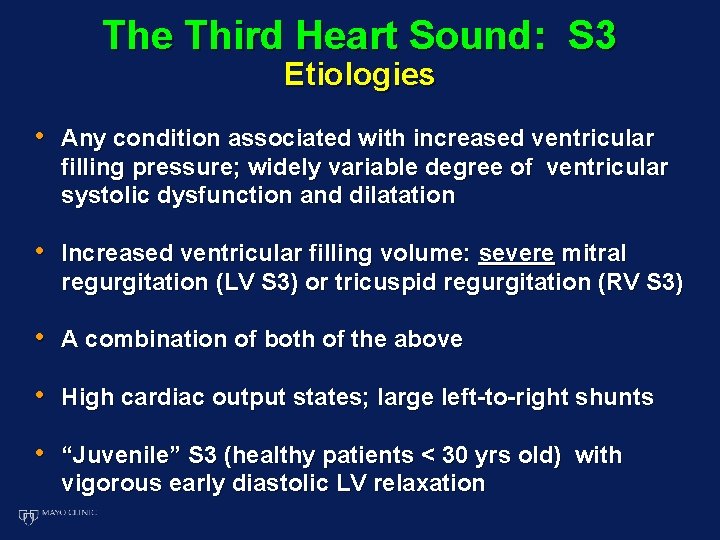
The Third Heart Sound: S 3 Etiologies • Any condition associated with increased ventricular filling pressure; widely variable degree of ventricular systolic dysfunction and dilatation • Increased ventricular filling volume: severe mitral regurgitation (LV S 3) or tricuspid regurgitation (RV S 3) • A combination of both of the above • High cardiac output states; large left-to-right shunts • “Juvenile” S 3 (healthy patients < 30 yrs old) with vigorous early diastolic LV relaxation
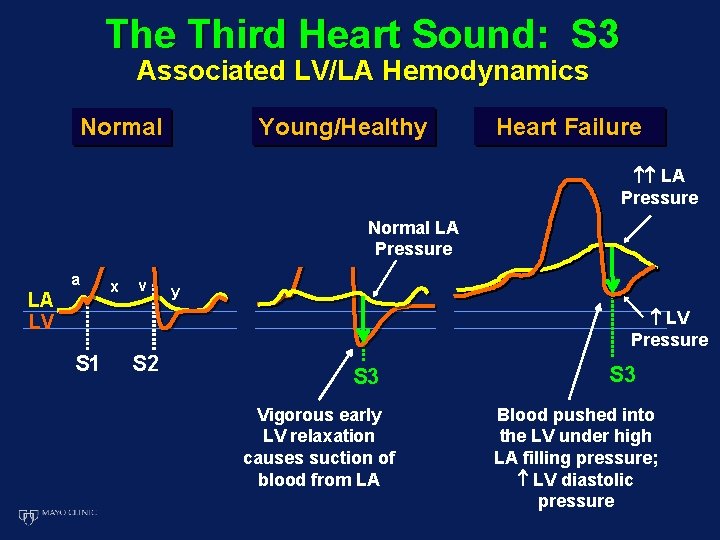
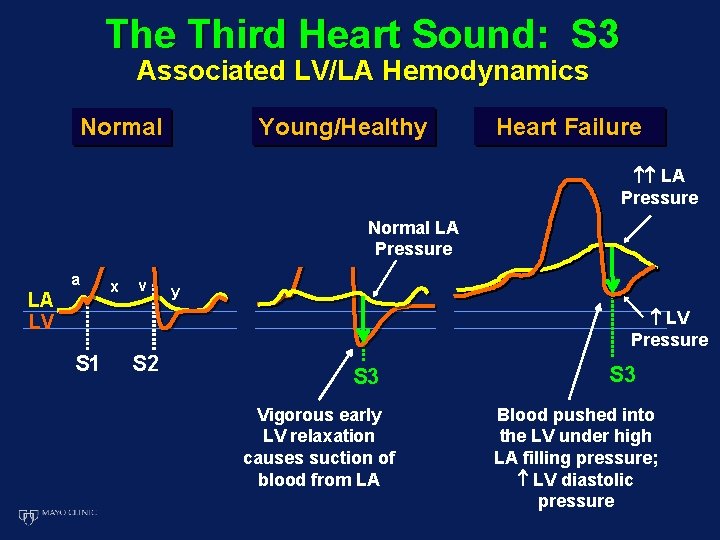
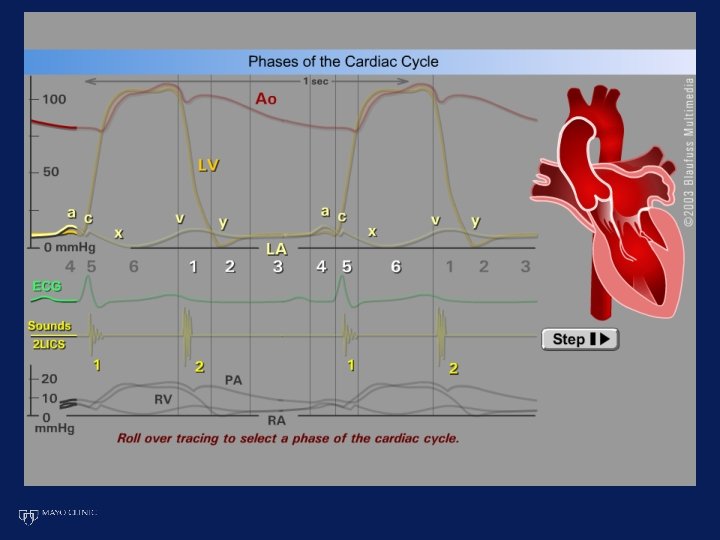
The Third Heart Sound: S 3 Associated LV/LA Hemodynamics Young/Healthy Normal Heart Failure LA Pressure Normal LA Pressure a LA LV x v y LV Pressure S 1 S 2 S 3 Vigorous early LV relaxation causes suction of blood from LA S 3 Blood pushed into the LV under high LA filling pressure; LV diastolic pressure
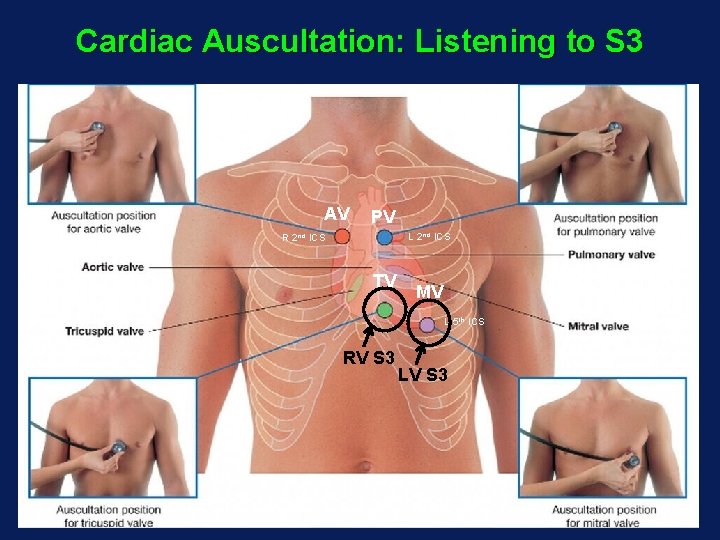
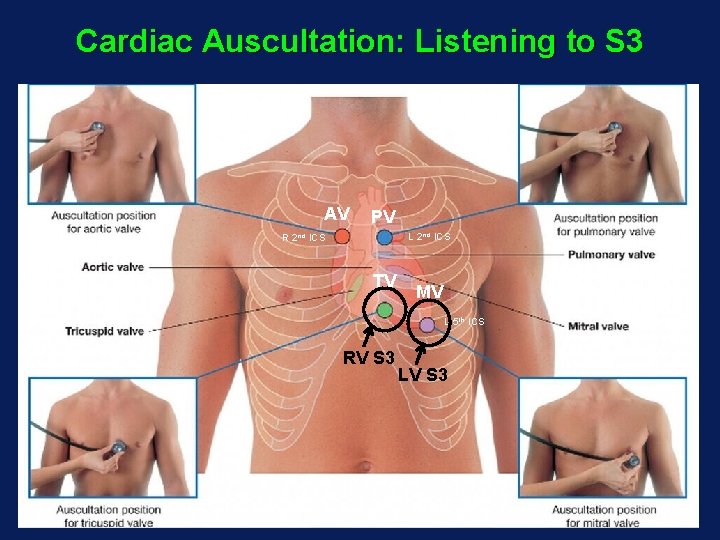
Cardiac Auscultation: Listening to S 3 AV PV L 2 nd ICS R 2 nd ICS TV MV L 5 th ICS RV S 3 LV S 3
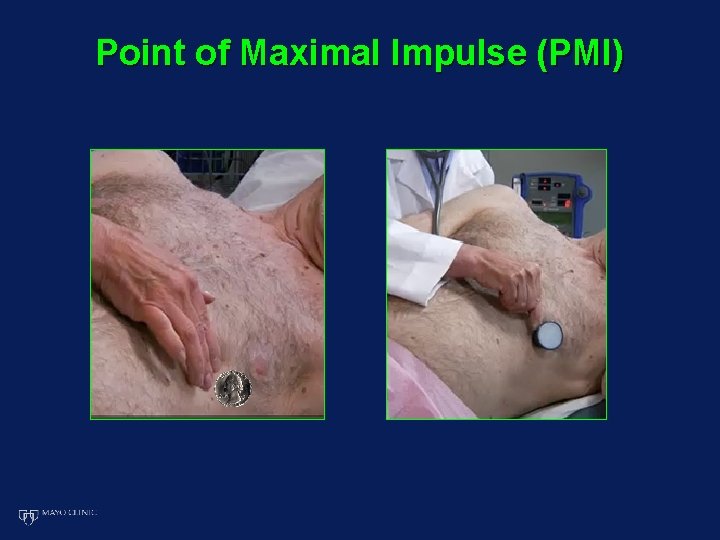
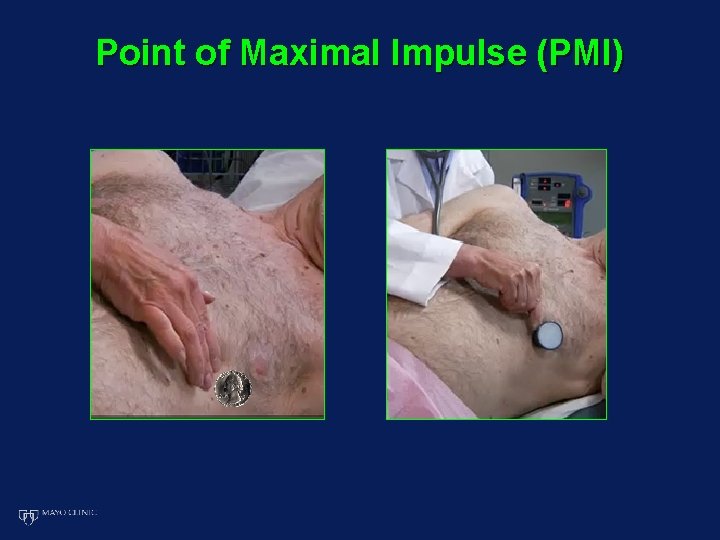
Point of Maximal Impulse (PMI)
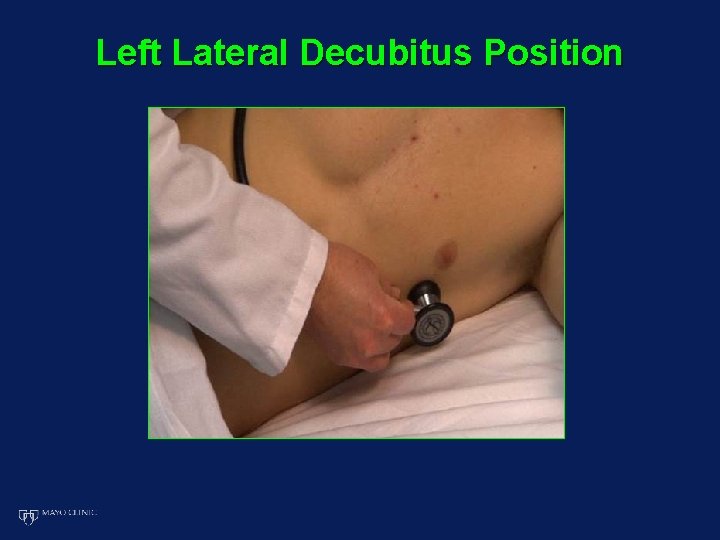
Left Lateral Decubitus Position
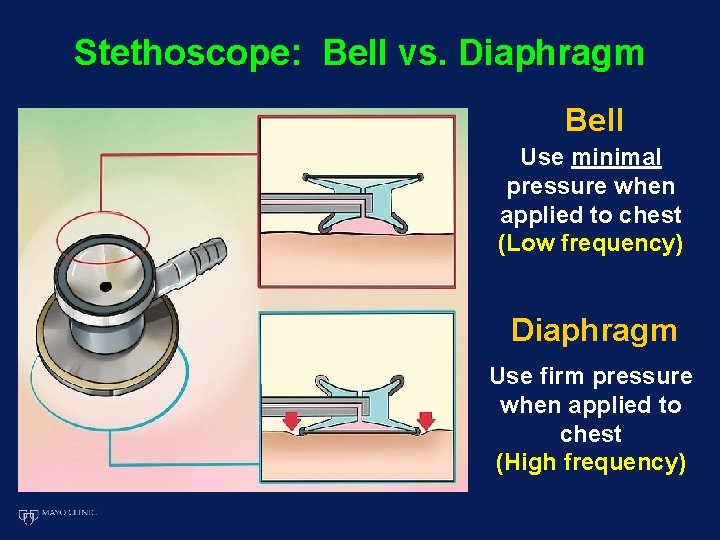
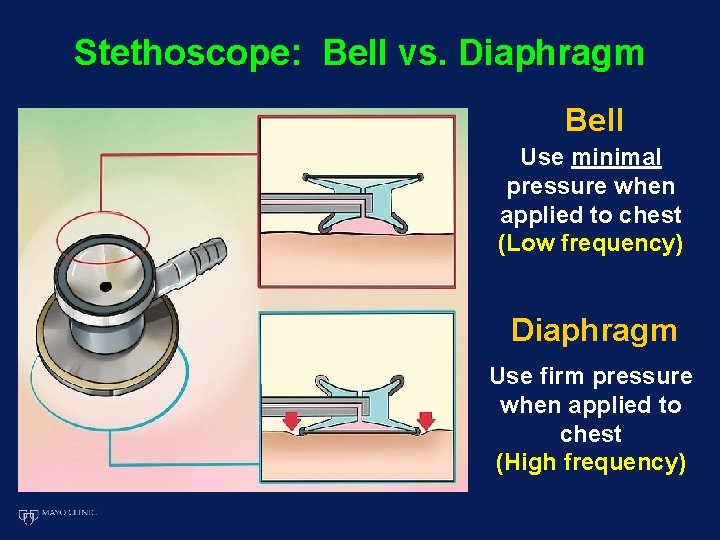
Stethoscope: Bell vs. Diaphragm Bell Use minimal pressure when applied to chest (Low frequency) Diaphragm Use firm pressure when applied to chest (High frequency)

Low and High Frequency Sounds Explained Listening with the Stethoscope Low frequency = Bell High frequency = Diaphragm
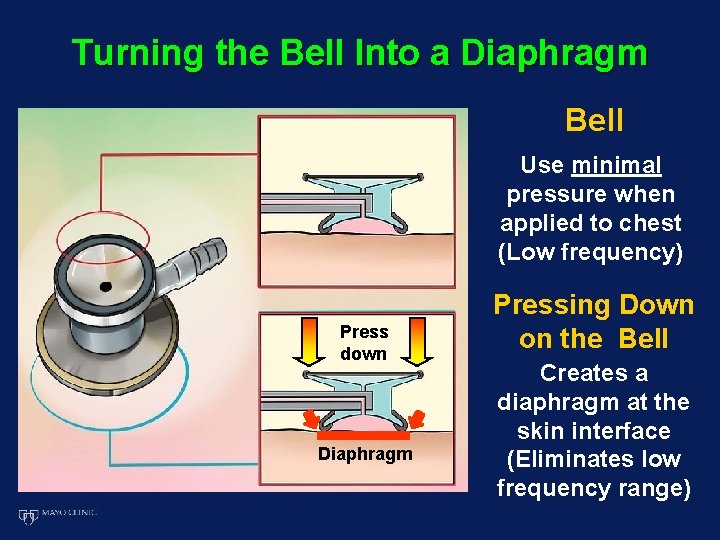
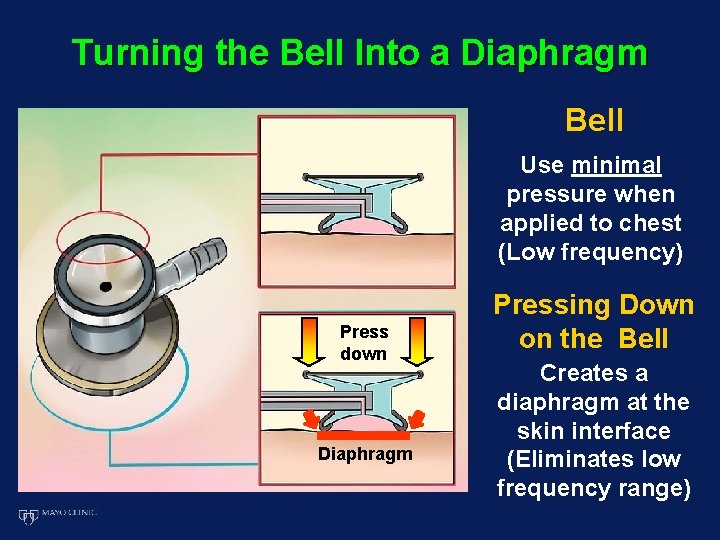
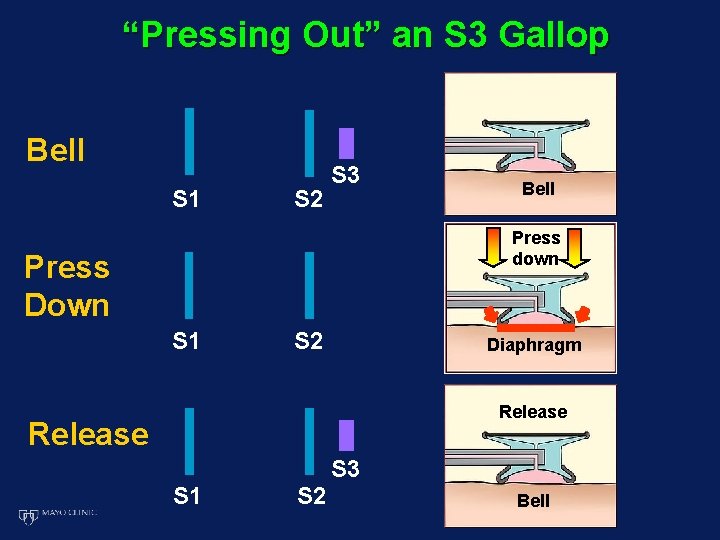
Turning the Bell Into a Diaphragm Bell Use minimal pressure when applied to chest (Low frequency) Press down Diaphragm Pressing Down on the Bell Creates a diaphragm at the skin interface (Eliminates low frequency range)
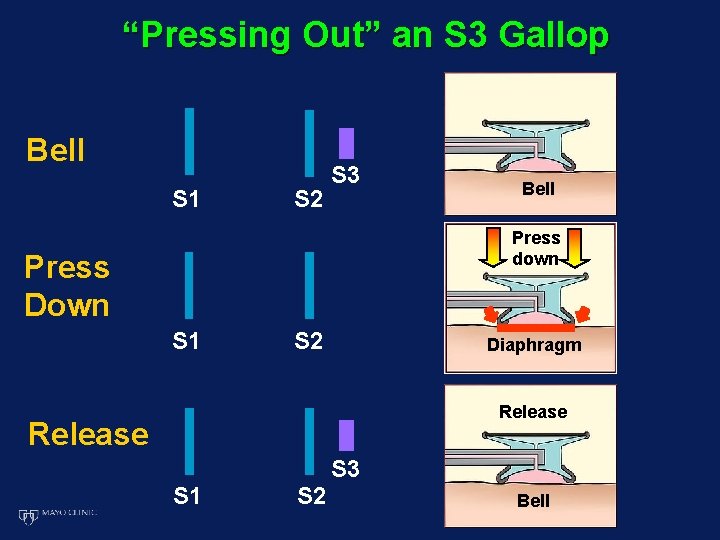
“Pressing Out” an S 3 Gallop Bell S 1 S 2 S 3 Bell Press down Press Down S 1 S 2 Diaphragm Release S 3 S 1 S 2 Bell
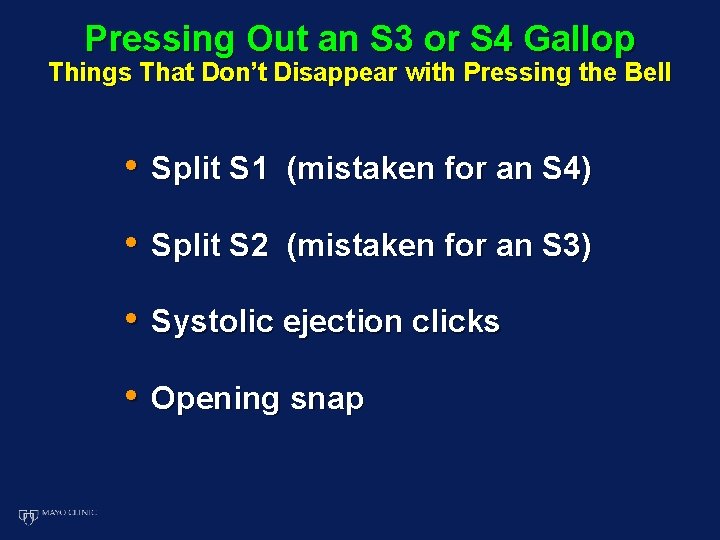
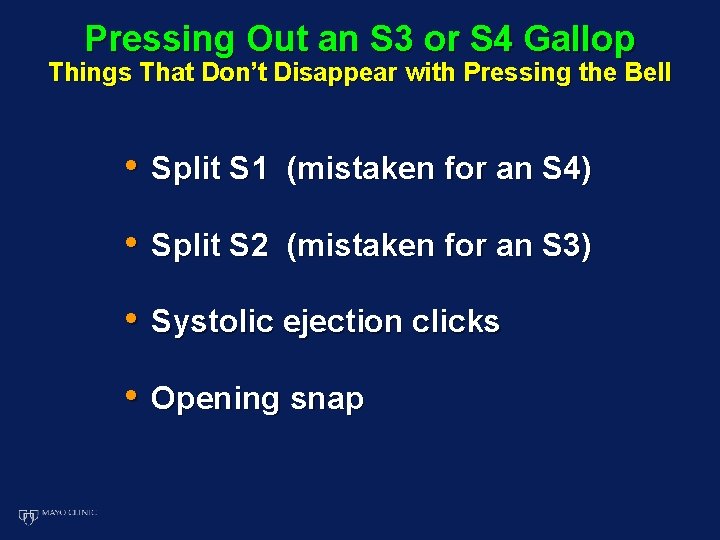
Pressing Out an S 3 or S 4 Gallop Things That Don’t Disappear with Pressing the Bell • Split S 1 (mistaken for an S 4) • Split S 2 (mistaken for an S 3) • Systolic ejection clicks • Opening snap
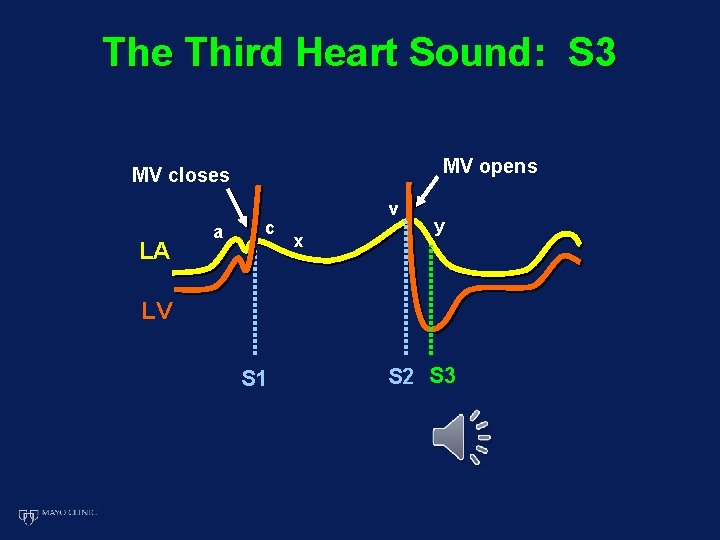
The Third Heart Sound: S 3 MV opens MV closes LA a c v x y LV S 1 S 2 S 3
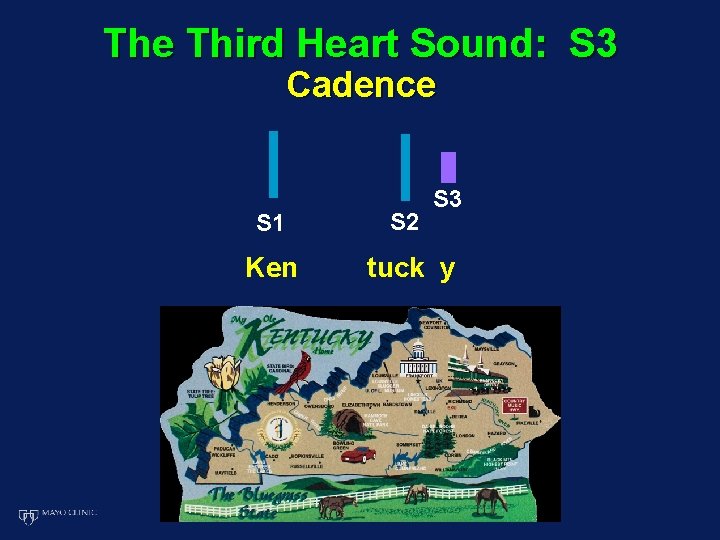
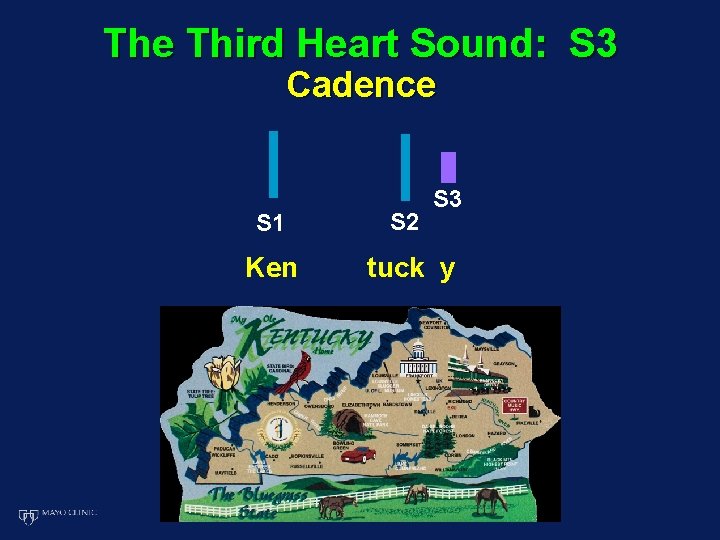
The Third Heart Sound: S 3 Cadence S 3 S 1 S 2 Ken tuck y
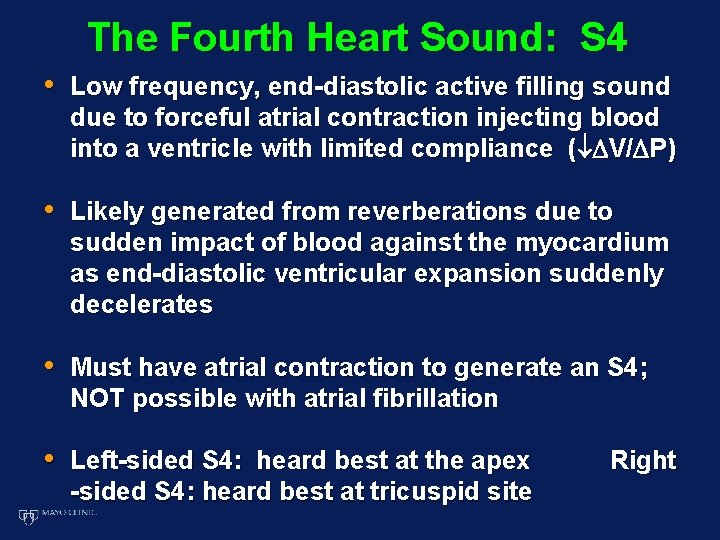
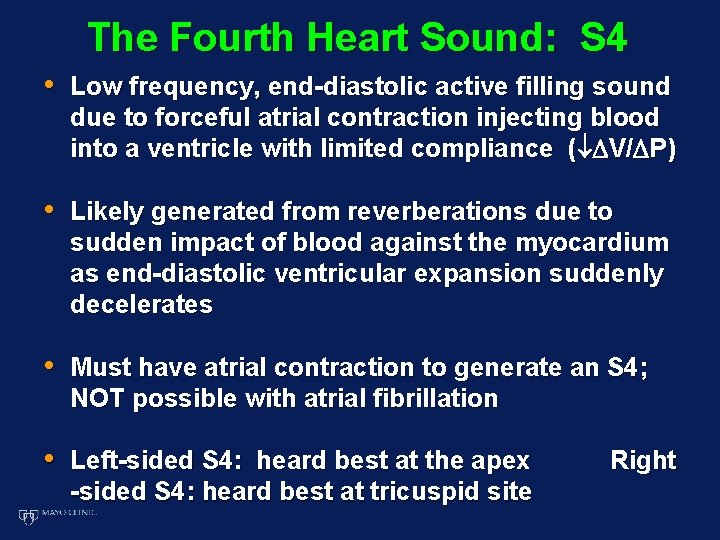
The Fourth Heart Sound: S 4 • Low frequency, end-diastolic active filling sound due to forceful atrial contraction injecting blood into a ventricle with limited compliance ( V/ P) • Likely generated from reverberations due to sudden impact of blood against the myocardium as end-diastolic ventricular expansion suddenly decelerates • Must have atrial contraction to generate an S 4; NOT possible with atrial fibrillation • Left-sided S 4: heard best at the apex -sided S 4: heard best at tricuspid site Right
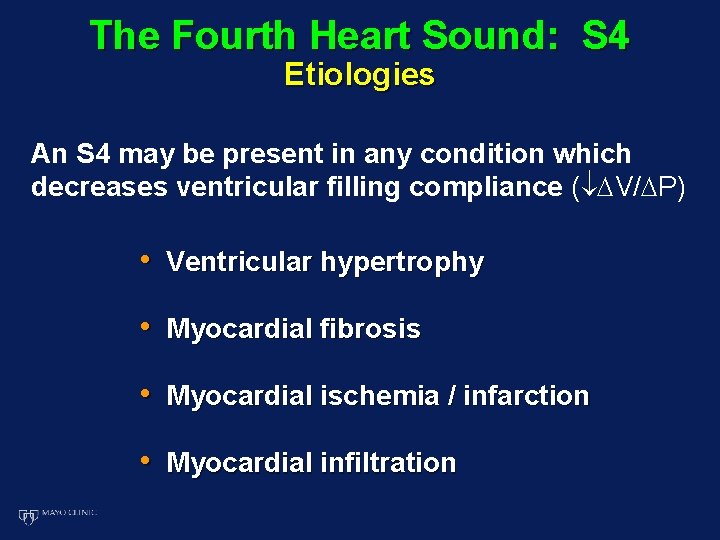
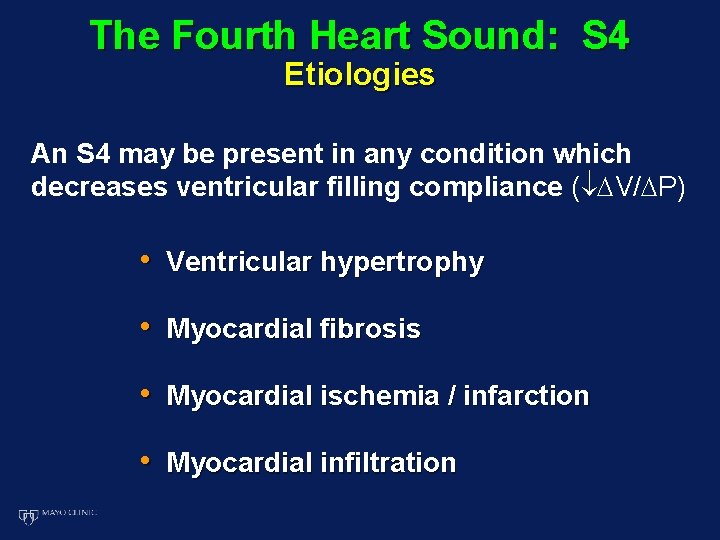
The Fourth Heart Sound: S 4 Etiologies An S 4 may be present in any condition which decreases ventricular filling compliance ( V/ P) • Ventricular hypertrophy • Myocardial fibrosis • Myocardial ischemia / infarction • Myocardial infiltration
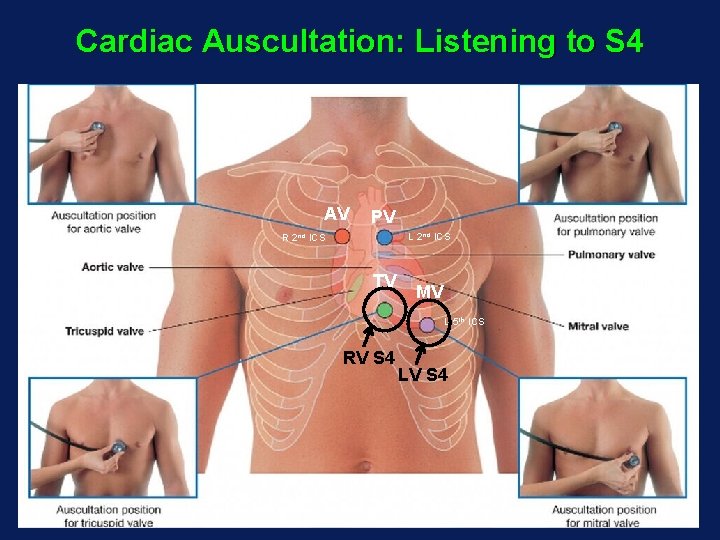
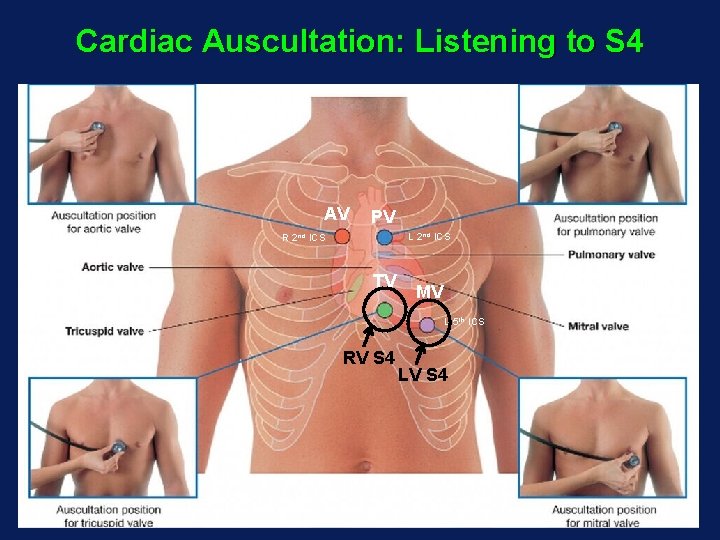
Cardiac Auscultation: Listening to S 4 AV PV L 2 nd ICS R 2 nd ICS TV MV L 5 th ICS RV S 4 LV S 4
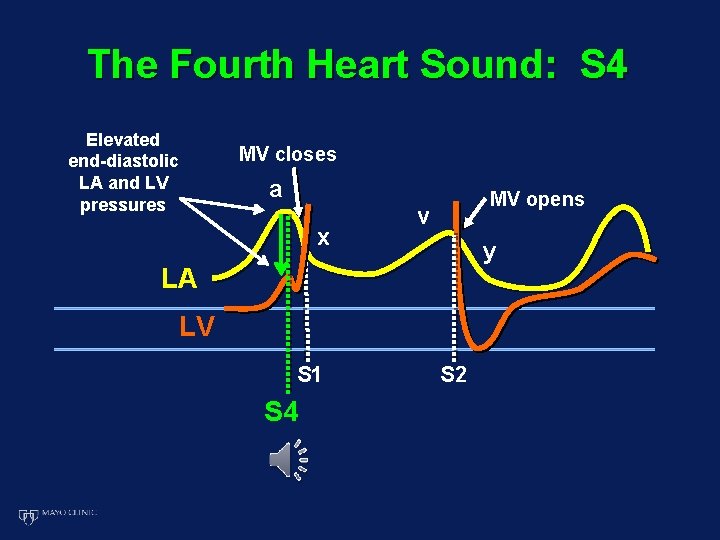
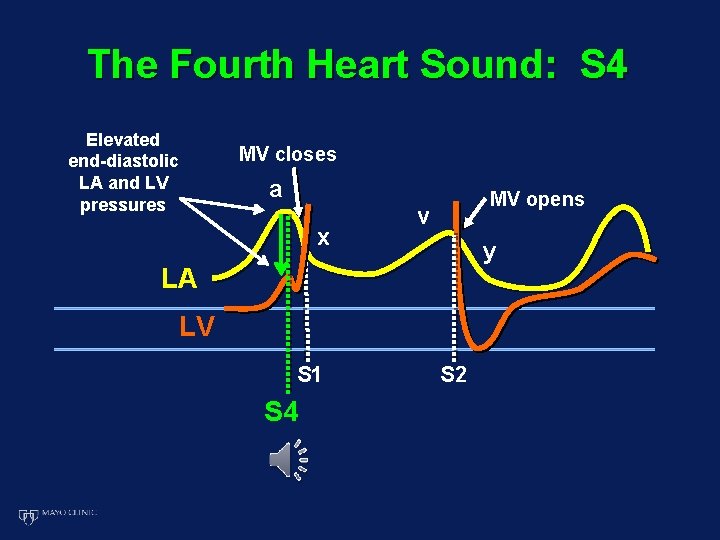
The Fourth Heart Sound: S 4 Elevated end-diastolic LA and LV pressures MV closes a x MV opens v y LA LV S 1 S 4 S 2
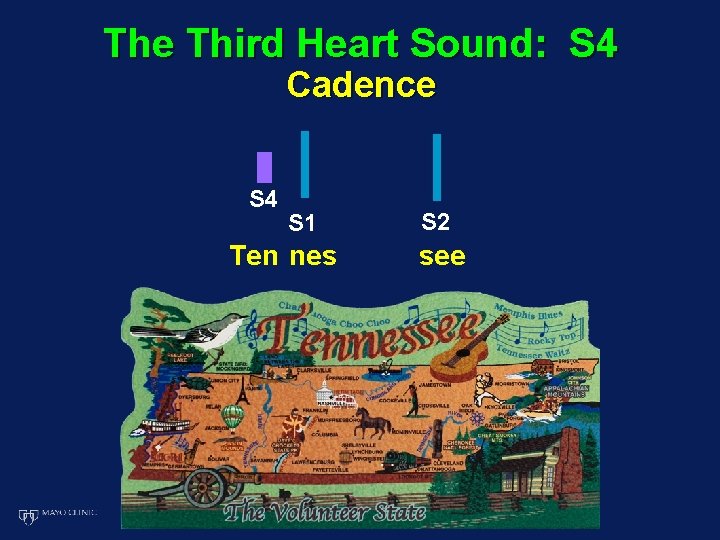
The Third Heart Sound: S 4 Cadence S 4 S 1 Ten nes S 2 see
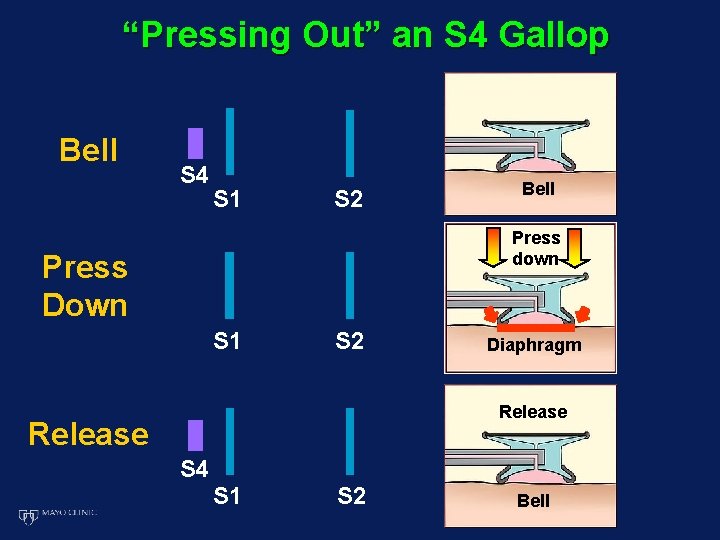
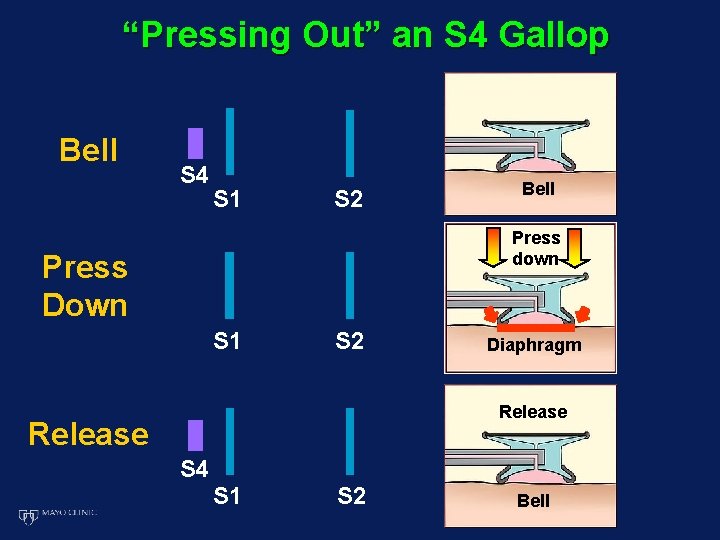
“Pressing Out” an S 4 Gallop Bell S 4 S 1 S 2 Bell Press down Press Down S 1 S 2 Diaphragm Release S 4 S 1 S 2 Bell

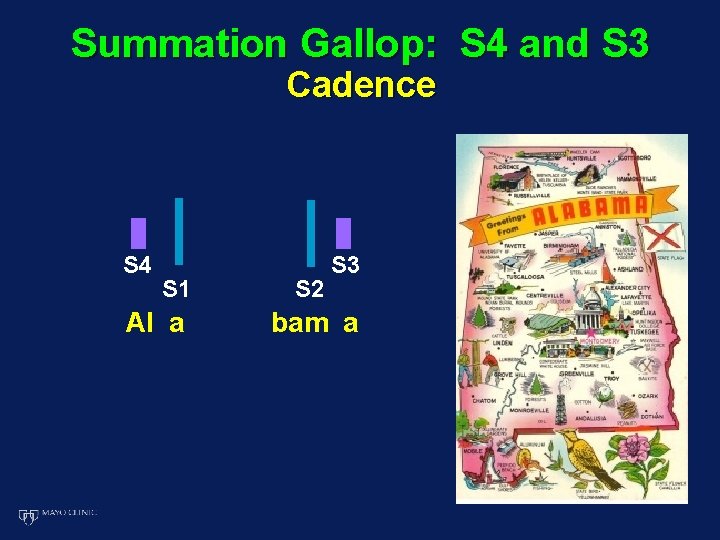
Summation Gallop: S 4 and S 3 Cadence S 4 S 1 Al a S 2 S 3 bam a
The Four Heart Sounds (S 1, S 2, S 3, S 4) Conclusions • The first (S 1) and second (S 2) heart sounds are the foundation of the cardiac physical exam and must be timed and characterized correctly • Corroborate S 1 and S 2 timing with the carotid and jugular venous exams • Careful listening with the bell, including the press-out maneuver, allows accurate detection of the S 3 and S 4 gallop • Detection of S 3 and S 4 heart sounds provide important clues to underlying cardiac pathophysiology