The Adrenal Glands Part The Adrenal Cortex Ziying











- Slides: 80
The Adrenal Glands PartⅡ: The Adrenal Cortex Ziying WANG Institute of Pharmacology School of Medicine, Shandong University wangziying@sdu. edu. cn
Part 1 Introduction More important than adrenal medulla
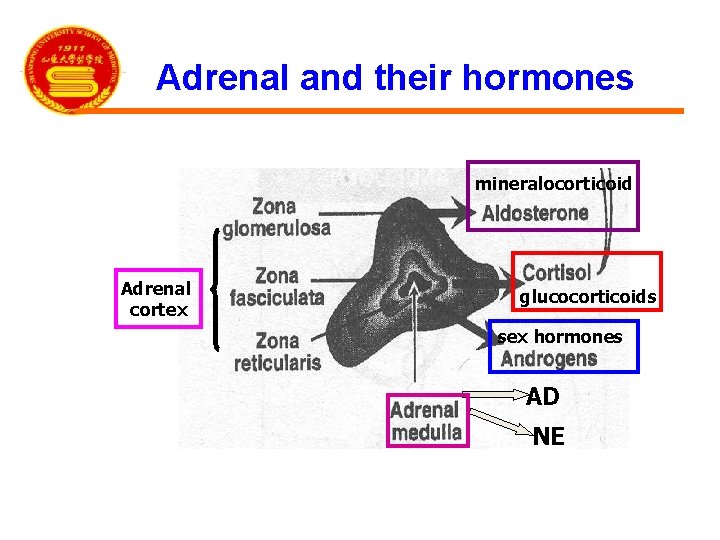
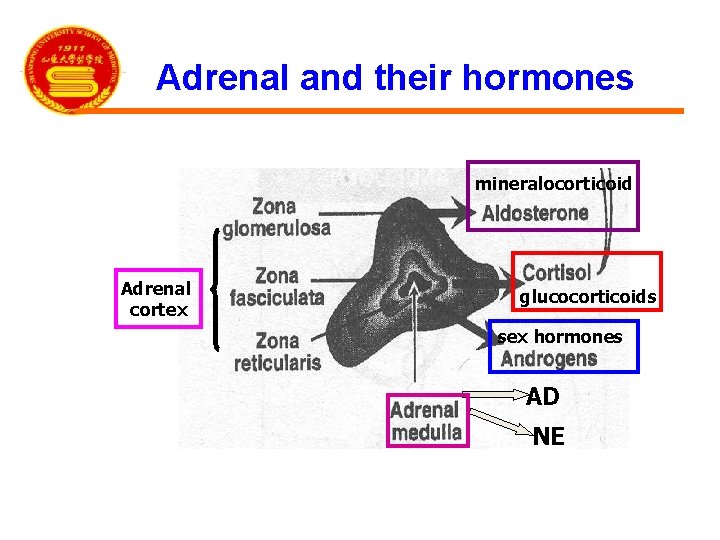
Adrenal and their hormones mineralocorticoid Adrenal cortex glucocorticoids sex hormones AD NE
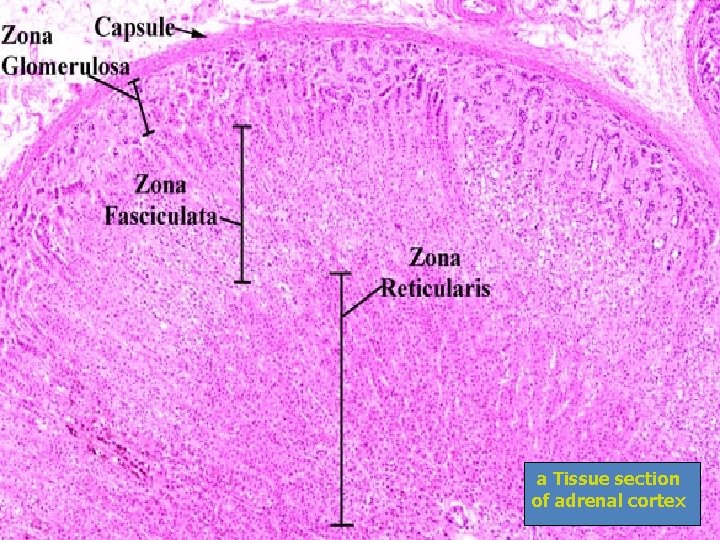
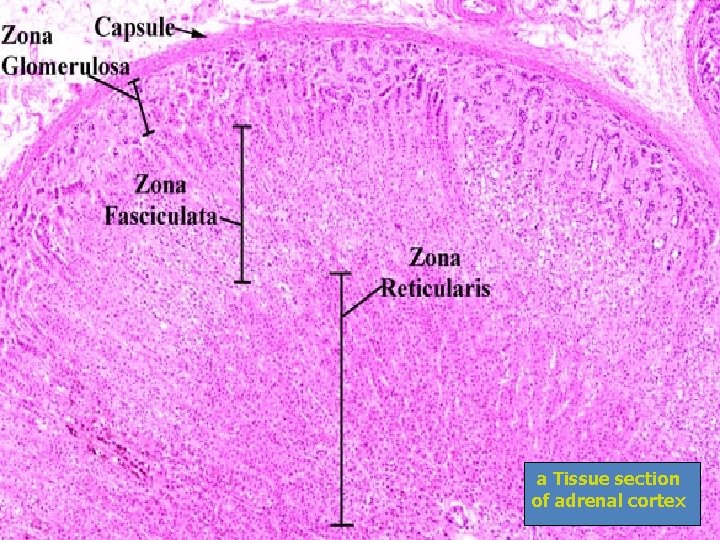
a Tissue section of adrenal cortex
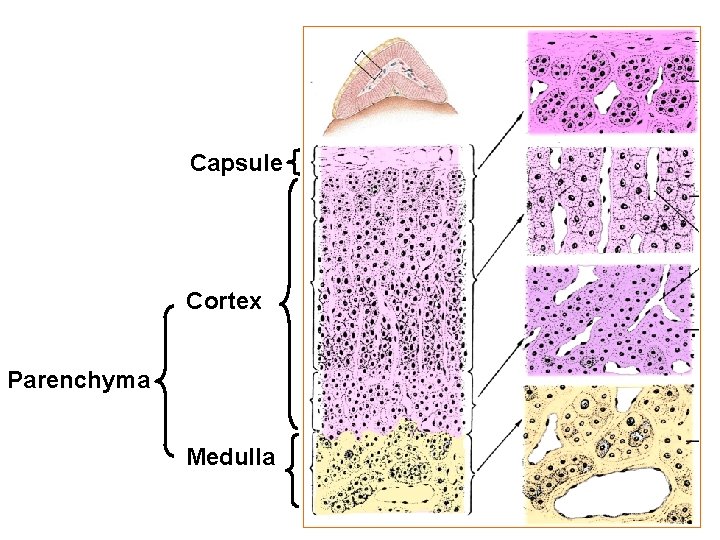
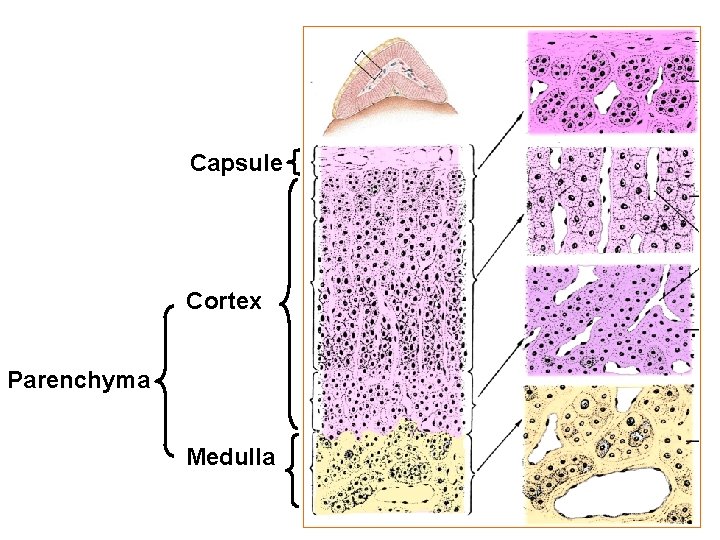
Capsule Cortex Parenchyma Medulla

Electron micrograph Zona glomerulosa Zona fasciculata
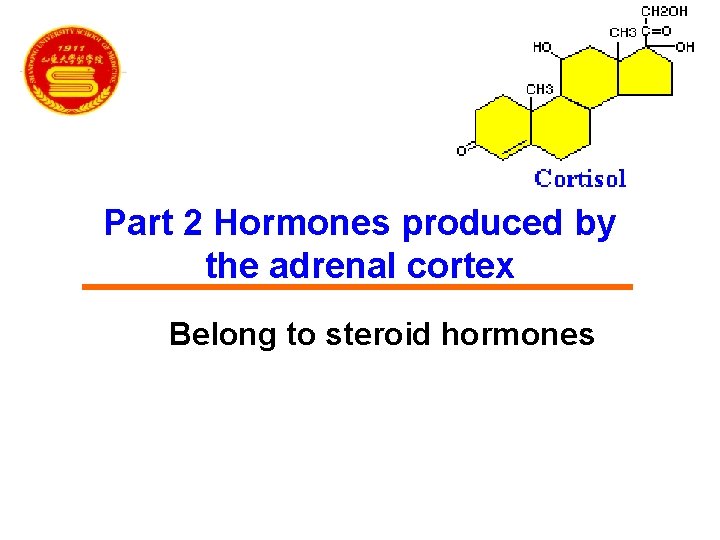
Part 2 Hormones produced by the adrenal cortex Belong to steroid hormones

Basic Structure of Adrenocortical Hormones 11 C O A 4 B 5 CH 2 OH 20 c 18 R 3 21 17 D o OH Basic structure: Steroid nucleus C 3 = 0 (酮基) C 4 -5 (双键) C 20 =0 (羰基) are necessary for adrenocortical hormones
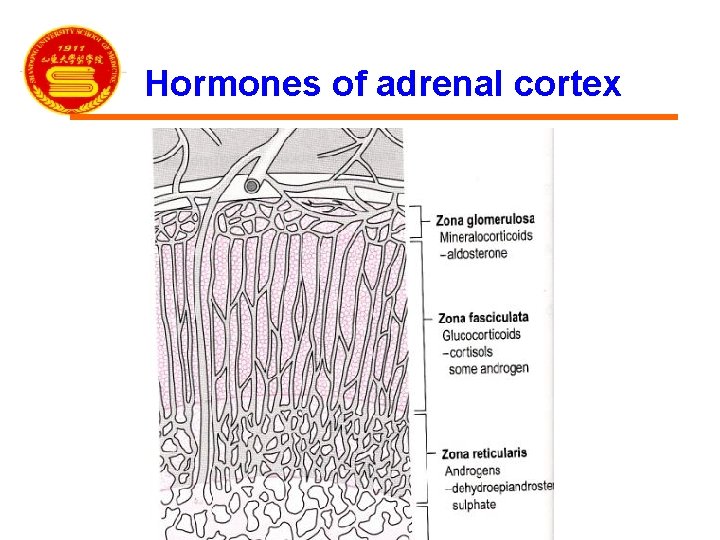
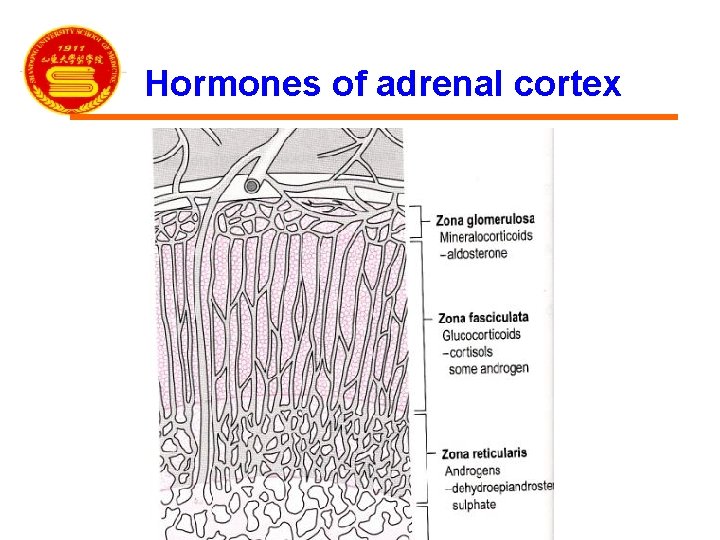
Hormones of adrenal cortex

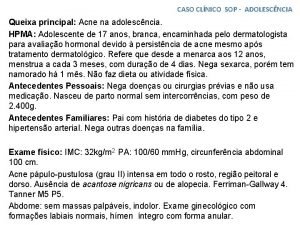
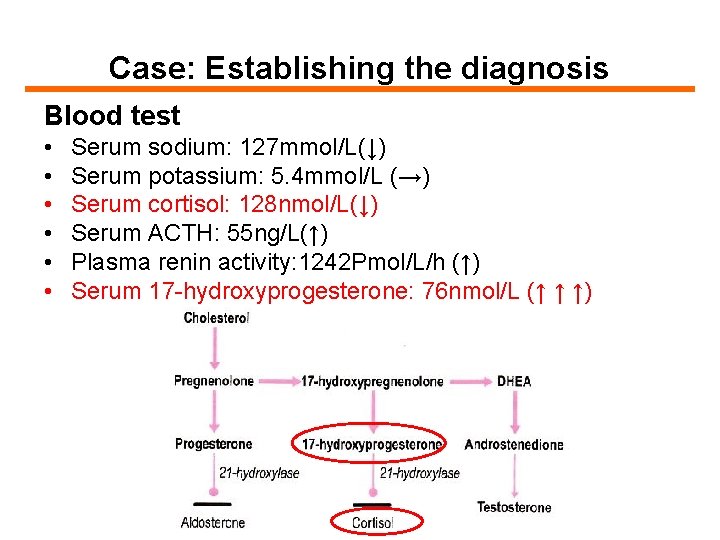
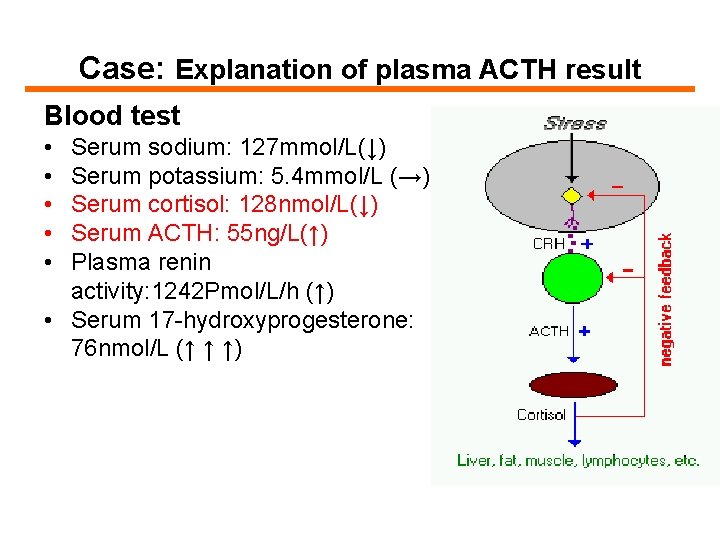
Case: 4 -year-old girl Report from her mother • • Height and weight lower than expected Ambiguous genitalia Public hair developed from 3 BP: 70/30 mm. Hg(↓) Blood test • • • Serum sodium: 127 mmol/L(↓) Serum potassium: 5. 4 mmol/L (→) Serum cortisol: 128 nmol/L(↓) Serum ACTH: 55 ng/L(↑) Plasma renin activity: 1242 Pmol/L/h (↑) Serum 17 -hydroxyprogesterone: 76 nmol/L (↑ ↑ ↑)
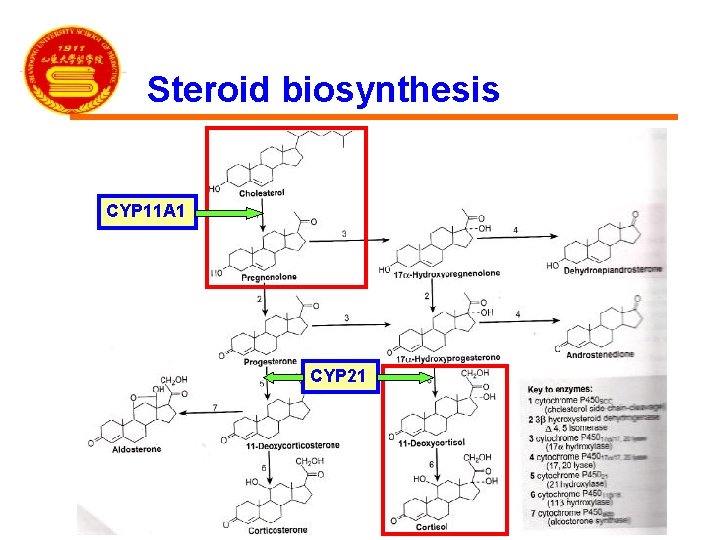
Steroid biosynthesis • From cholesterol • Hydroxylation reactions: CYP 450 family • Rate-limiting enzyme: CYP 11 A 1
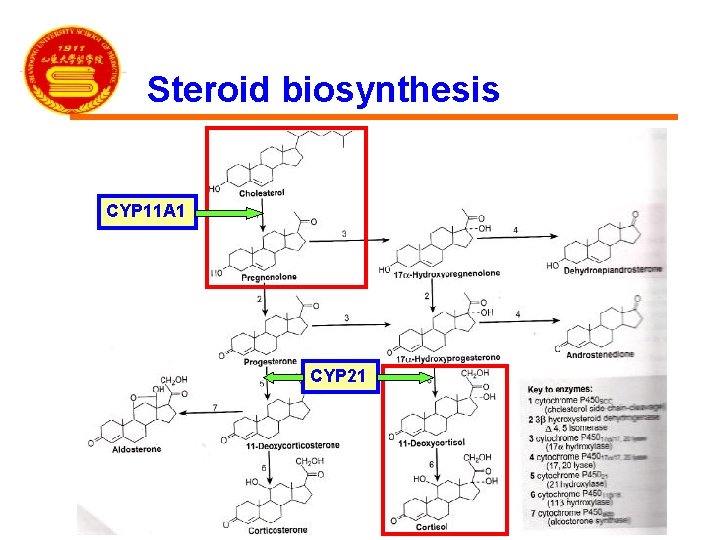
Steroid biosynthesis CYP 11 A 1 CYP 21
Steroid biosynthesis • St. AR: (steroidogenic acute regulatory) protein • St. AR deficiency: lipid adrenal hyperplasia
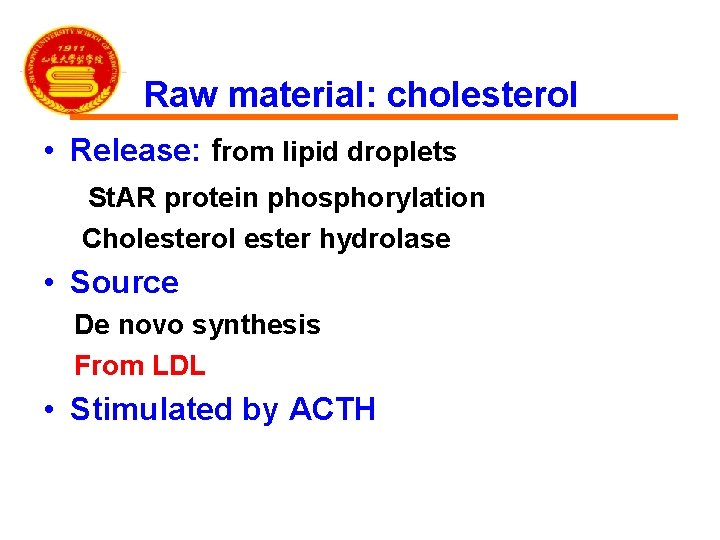
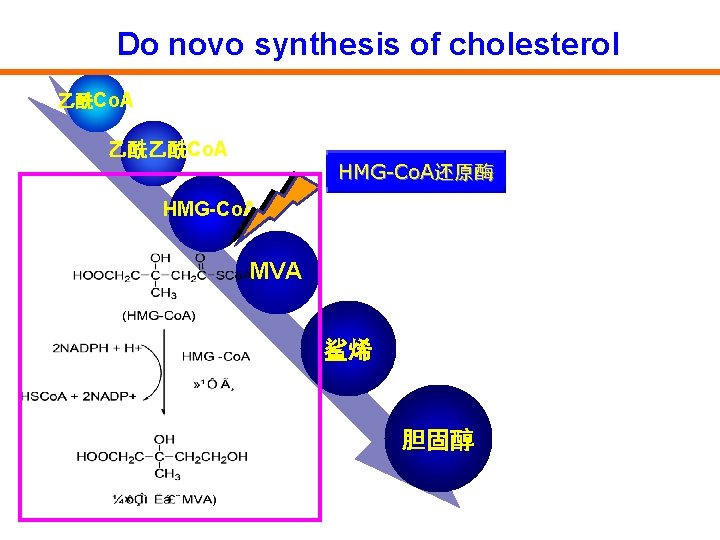
Raw material: cholesterol • Release: from lipid droplets St. AR protein phosphorylation Cholesterol ester hydrolase • Source De novo synthesis From LDL • Stimulated by ACTH
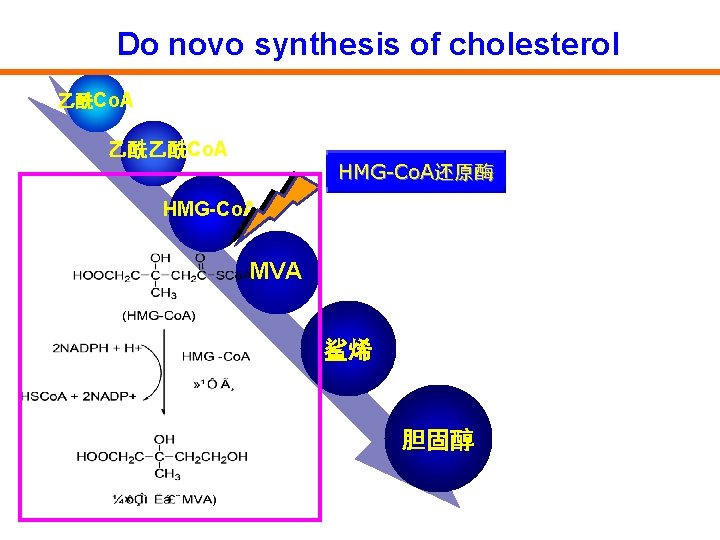
Do novo synthesis of cholesterol 乙酰Co. A 乙酰乙酰Co. A HMG-Co. A还原酶 HMG-Co. A MVA 鲨烯 胆固醇
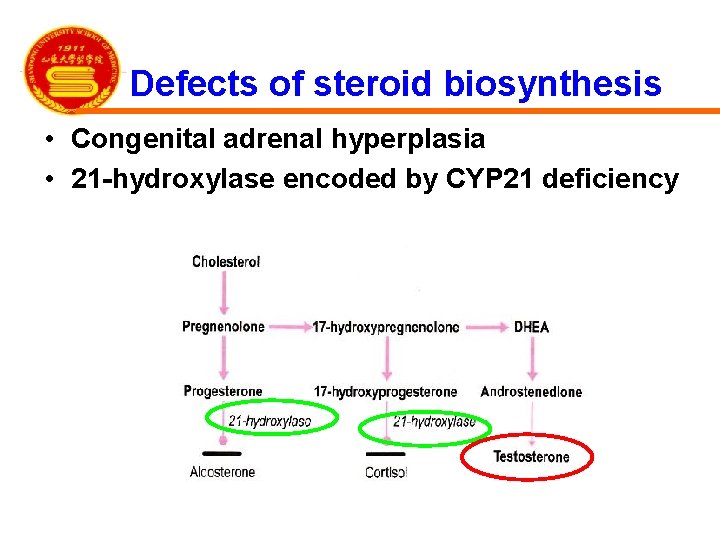
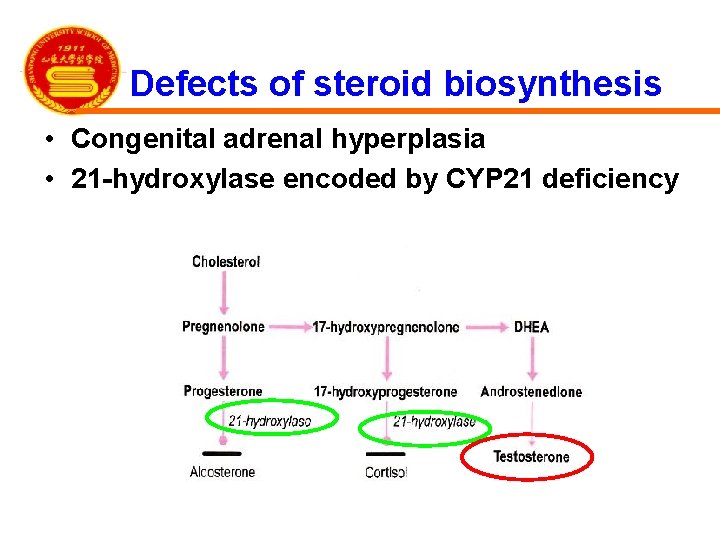
Defects of steroid biosynthesis • Congenital adrenal hyperplasia • 21 -hydroxylase encoded by CYP 21 deficiency
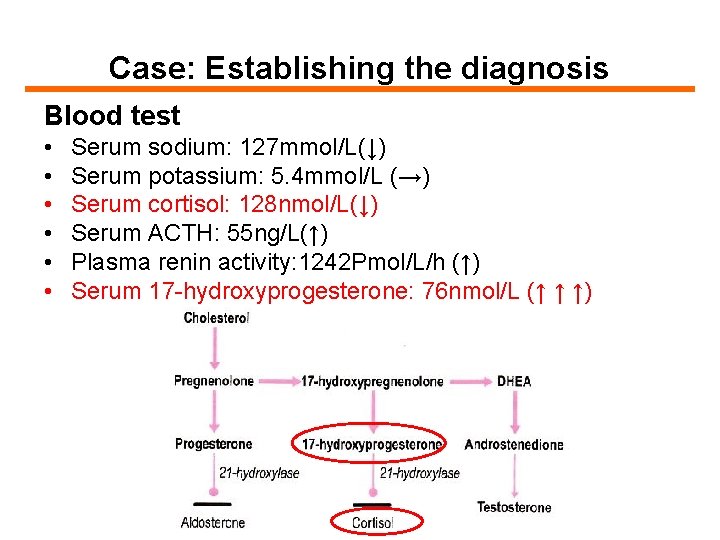
Case: Establishing the diagnosis Blood test • • • Serum sodium: 127 mmol/L(↓) Serum potassium: 5. 4 mmol/L (→) Serum cortisol: 128 nmol/L(↓) Serum ACTH: 55 ng/L(↑) Plasma renin activity: 1242 Pmol/L/h (↑) Serum 17 -hydroxyprogesterone: 76 nmol/L (↑ ↑ ↑)
Part 3 Regulation of steroid production
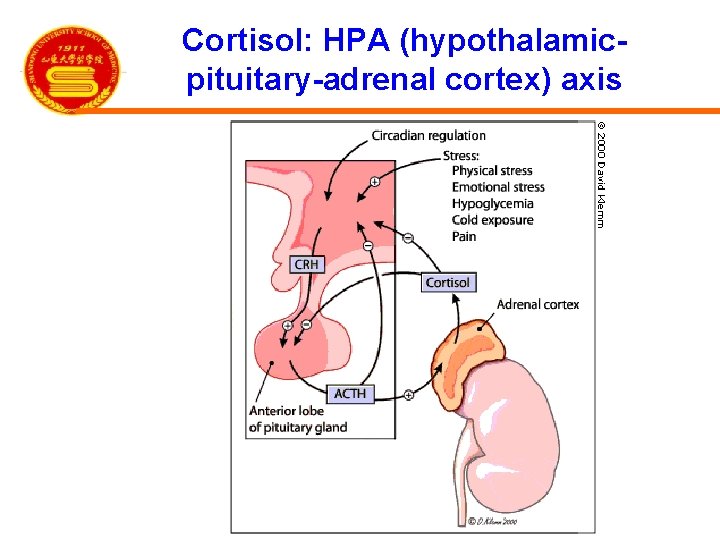
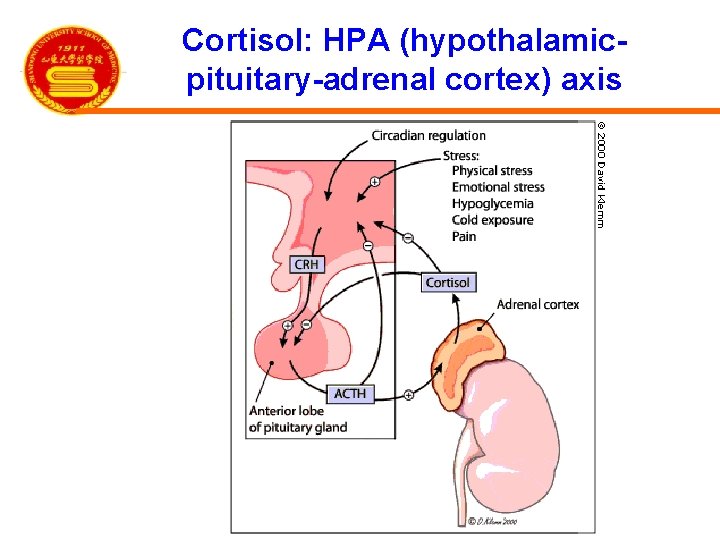
Cortisol: HPA (hypothalamicpituitary-adrenal cortex) axis
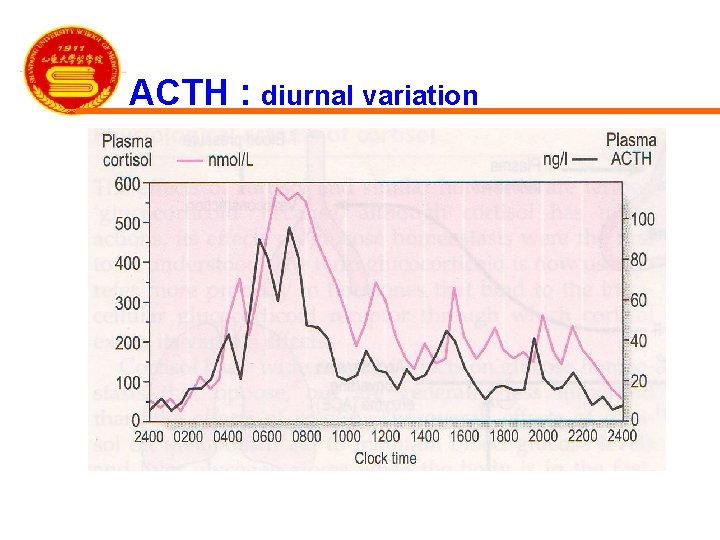
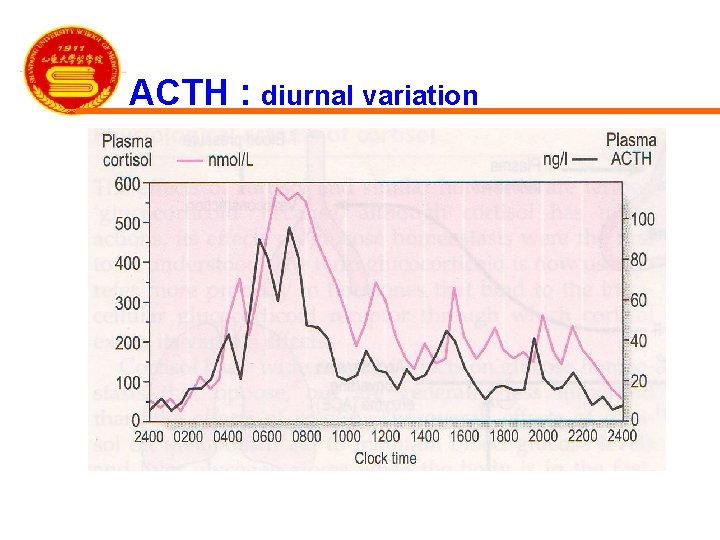
ACTH : diurnal variation
The actions of ACTH • • • 1. Increase adrenal blood flow 2. Increase steroidogenic enzyme expression 3. Activate St. AR protein 4. Activate cholesterol ester hydrolase 4. Increase the size of adrenal gland
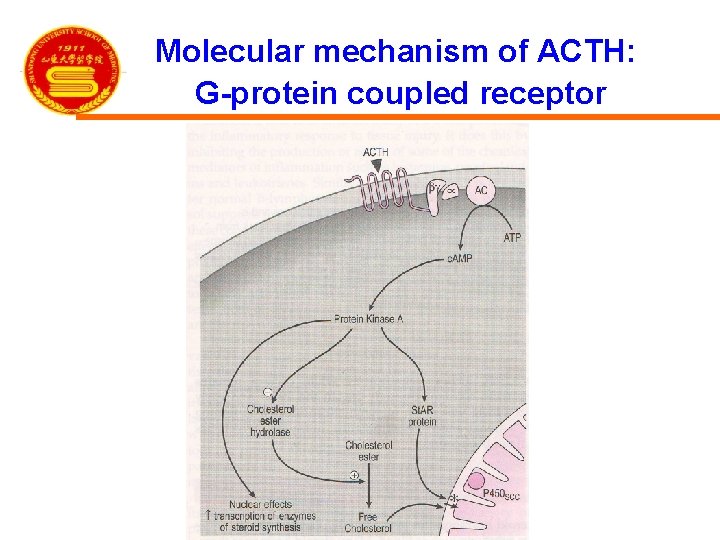
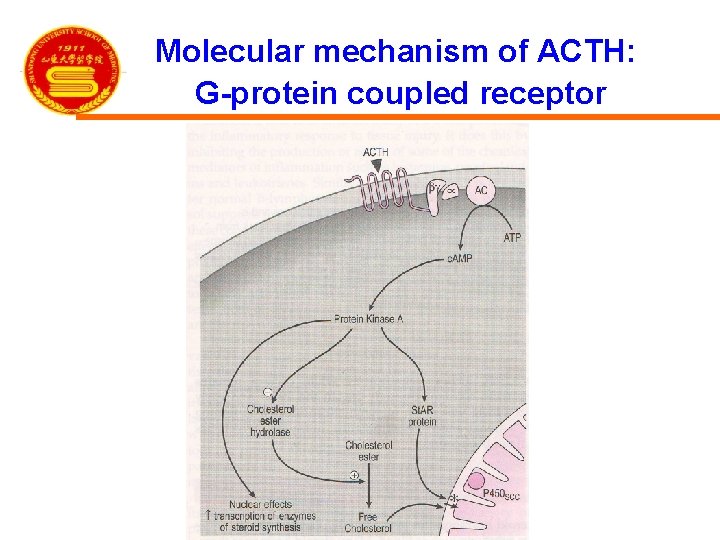
Molecular mechanism of ACTH: G-protein coupled receptor
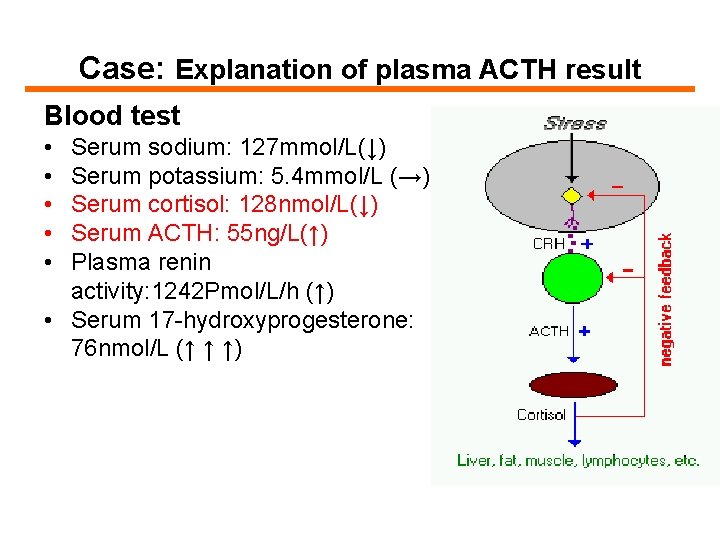
Case: Explanation of plasma ACTH result Blood test • • • Serum sodium: 127 mmol/L(↓) Serum potassium: 5. 4 mmol/L (→) Serum cortisol: 128 nmol/L(↓) Serum ACTH: 55 ng/L(↑) Plasma renin activity: 1242 Pmol/L/h (↑) • Serum 17 -hydroxyprogesterone: 76 nmol/L (↑ ↑ ↑)
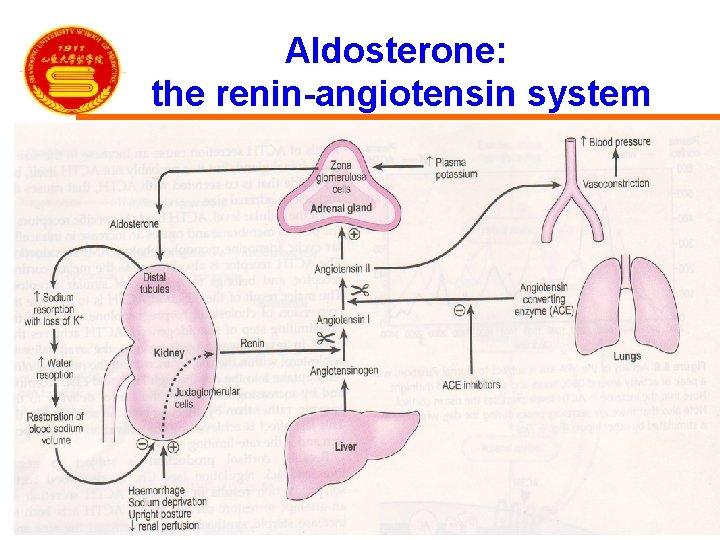
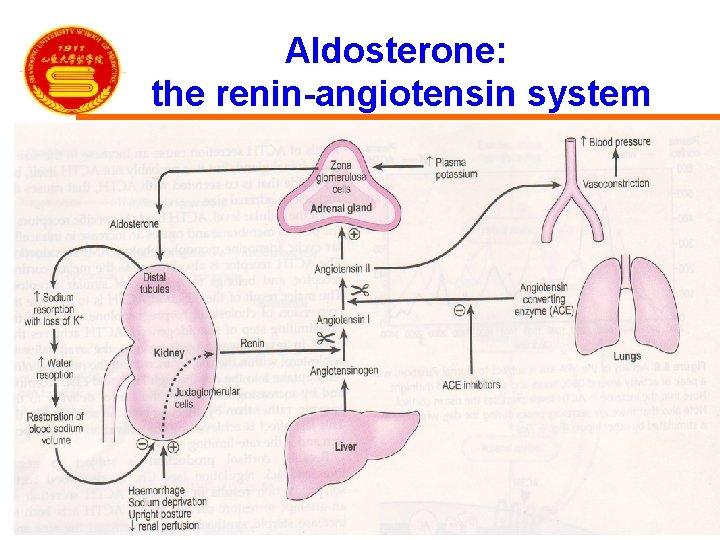
Aldosterone: the renin-angiotensin system
Part 4 Actions of adrenal steroids Glucocorticoids Mineralocorticoids Adrenal androgens
Actions of glucocorticoids (GCS) (glucose + cortex + steroid)
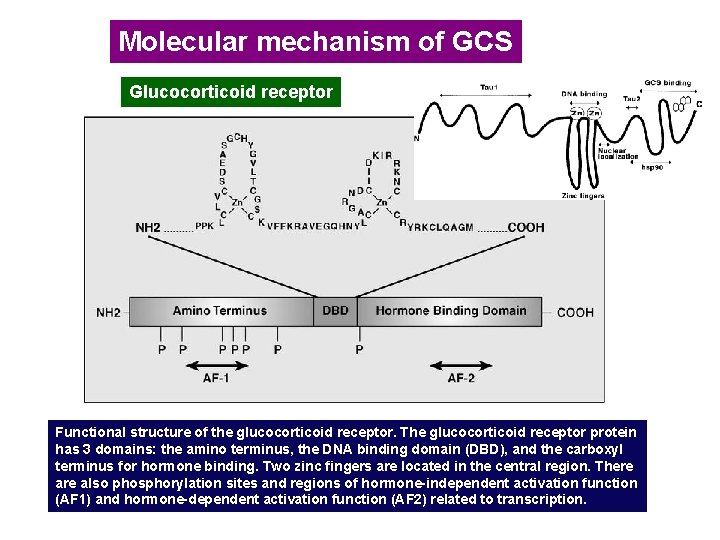
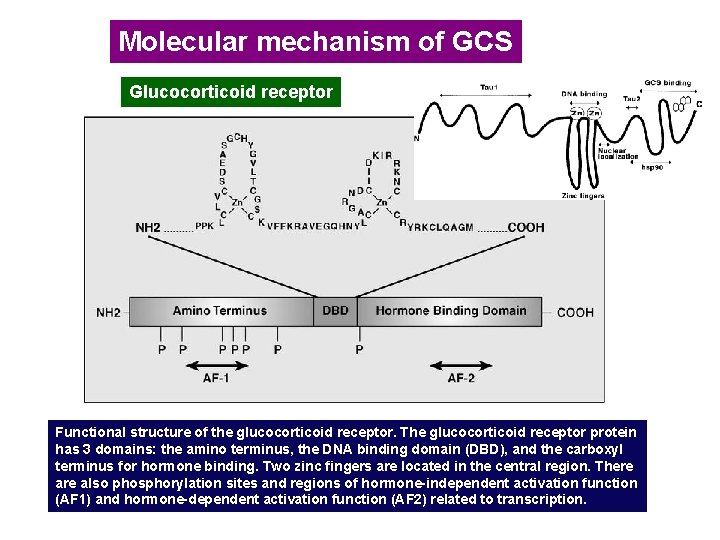
Molecular mechanism of GCS Glucocorticoid receptor Functional structure of the glucocorticoid receptor. The glucocorticoid receptor protein has 3 domains: the amino terminus, the DNA binding domain (DBD), and the carboxyl terminus for hormone binding. Two zinc fingers are located in the central region. There also phosphorylation sites and regions of hormone-independent activation function (AF 1) and hormone-dependent activation function (AF 2) related to transcription.
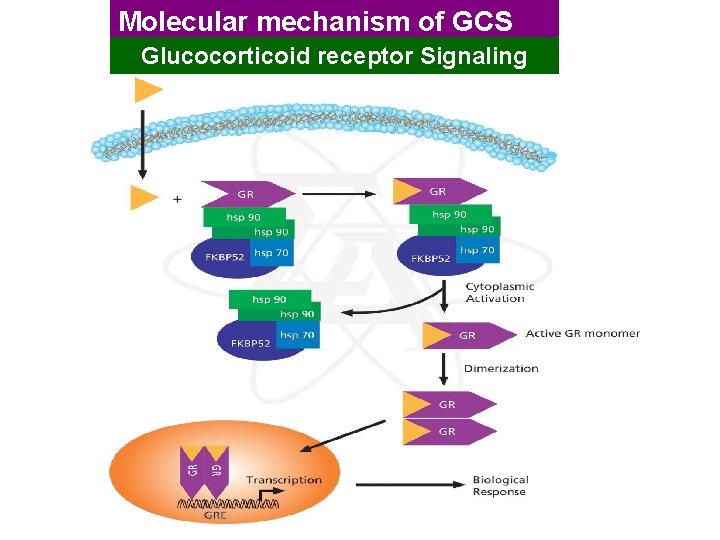
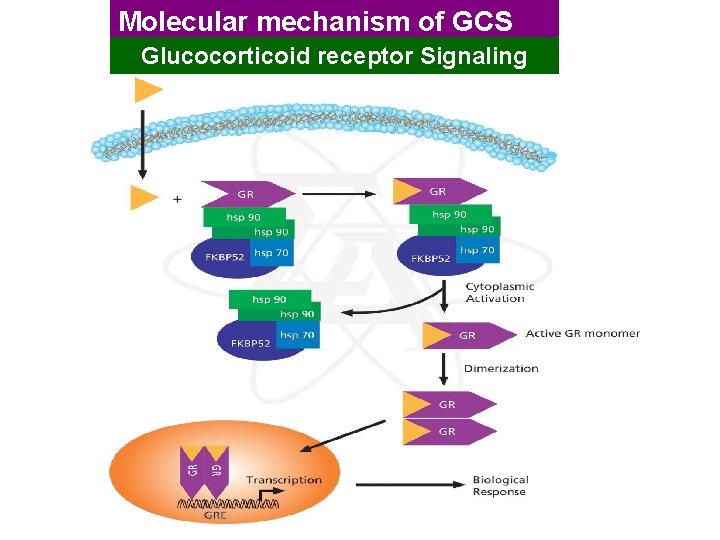
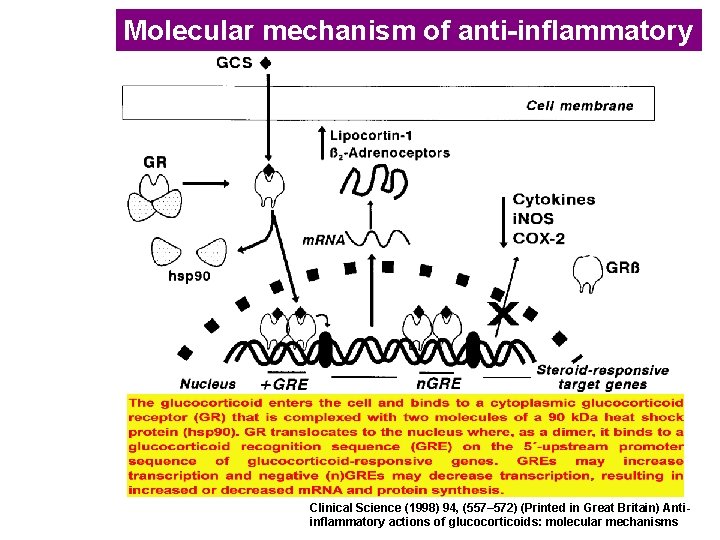
Molecular mechanism of GCS Glucocorticoid receptor Signaling
Actions of GCS 1. Effects on metabolism 2. Permissive action 3. Anti-inflammatory effects 4. Immunosuppressive and anti-allergic effects 5. Anti-toxic effects 6. Anti-shock effects 7. Effects on blood and hematopoietic system 8. Other effects
1. Effects on metabolism (1) Effects on carbohydrate metabolism: BS↑ a. increase glyconeogenesis b. increase glycogenolysis c. decrease the oxidation and utilization of glucose • Net result: hyperglycemia
1. Effects on metabolism (2) Effects on protein metabolism a. stimulates protein catabolism b. inhibit protein synthesis Net result: negative nitrogen balance
1. Effects on metabolism (3) Effects on lipid metabolism: a. stimulate lipolysis b. cause dramatic redistribution of body fat. Result: concentric obesity
1. Effects on metabolism (4) Effects on salt and water metabolism • • a. mineralocorticoids-like activity: weak b. antagonizing Vitamin D
2. Permissive action Definition: GCS facilitates other hormonal effects other than direct effects. eg. Increase the vasoconstriction of CA, increase the hyperglycemic effect of glycagon
3. Anti-inflammatory effects Characteristics: rapid, strong , nonspecific , both the early phase and late phase
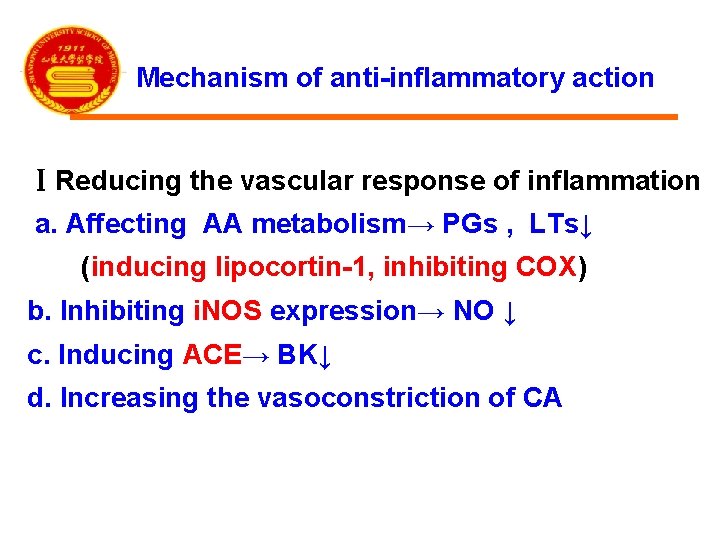
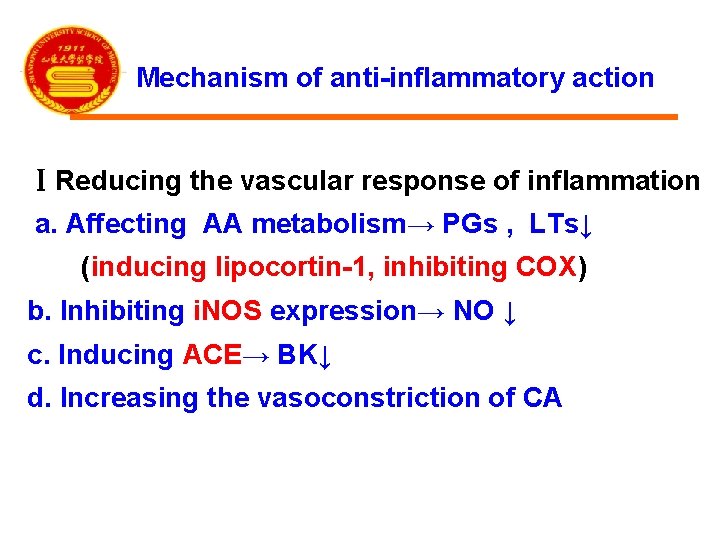
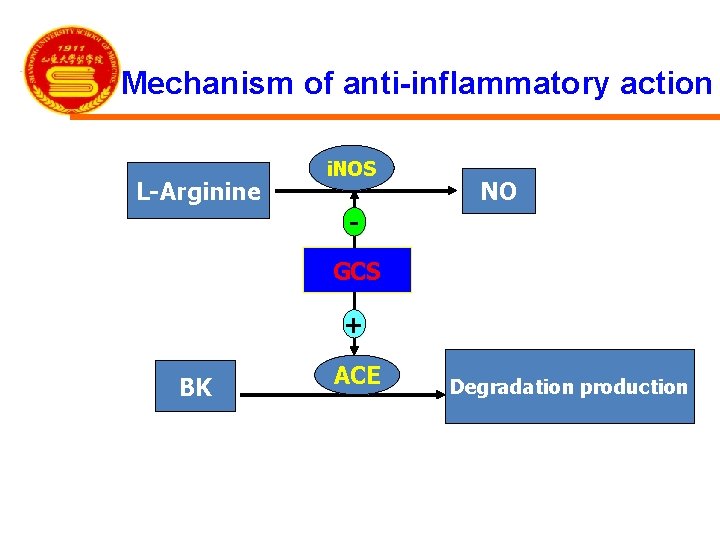
Mechanism of anti-inflammatory action ⅠReducing the vascular response of inflammation a. Affecting AA metabolism→ PGs , LTs↓ (inducing lipocortin-1, inhibiting COX) b. Inhibiting i. NOS expression→ NO ↓ c. Inducing ACE→ BK↓ d. Increasing the vasoconstriction of CA

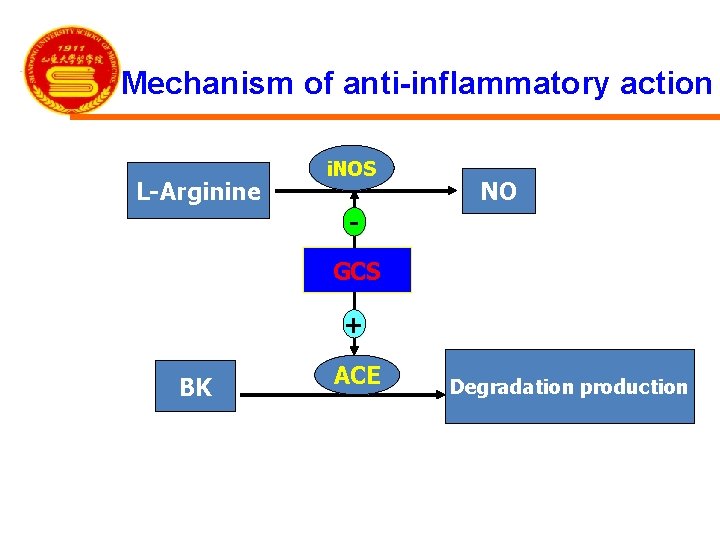
Mechanism of anti-inflammatory action L-Arginine i. NOS NO GCS + BK ACE Degradation production
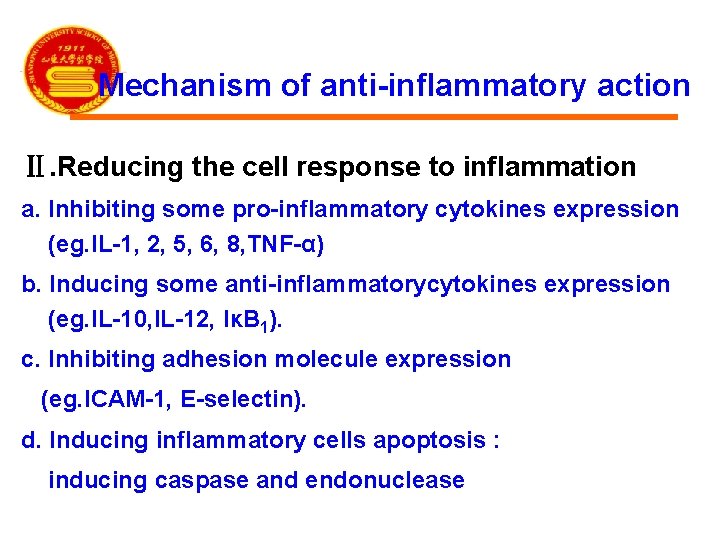
Mechanism of anti-inflammatory action Ⅱ. Reducing the cell response to inflammation a. Inhibiting some pro-inflammatory cytokines expression (eg. IL-1, 2, 5, 6, 8, TNF-α) b. Inducing some anti-inflammatorycytokines expression (eg. IL-10, IL-12, IκB 1). c. Inhibiting adhesion molecule expression (eg. ICAM-1, E-selectin). d. Inducing inflammatory cells apoptosis : inducing caspase and endonuclease

Mechanism of anti-inflammatory action Ⅲ. Postponing the inflammatory sequela Mechanism: inhibiting hyperplasy of blood capillary and fibroblast, preventing adhesion and scar formation
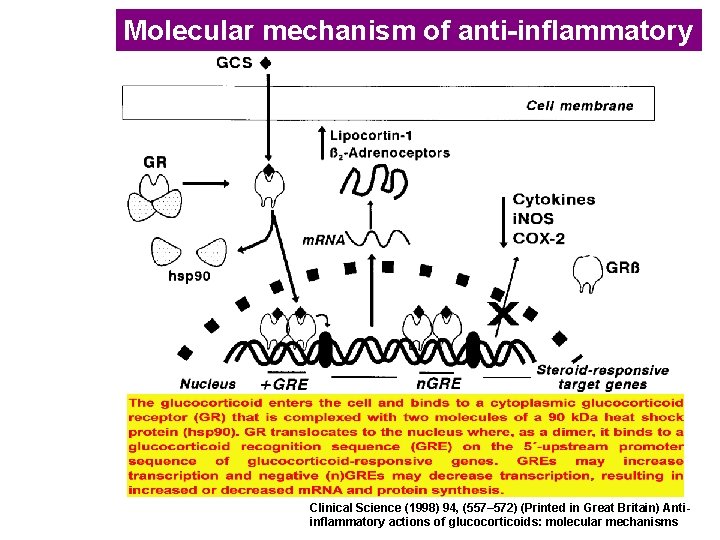
Molecular mechanism of anti-inflammatory Clinical Science (1998) 94, (557– 572) (Printed in Great Britain) Antiinflammatory actions of glucocorticoids: molecular mechanisms
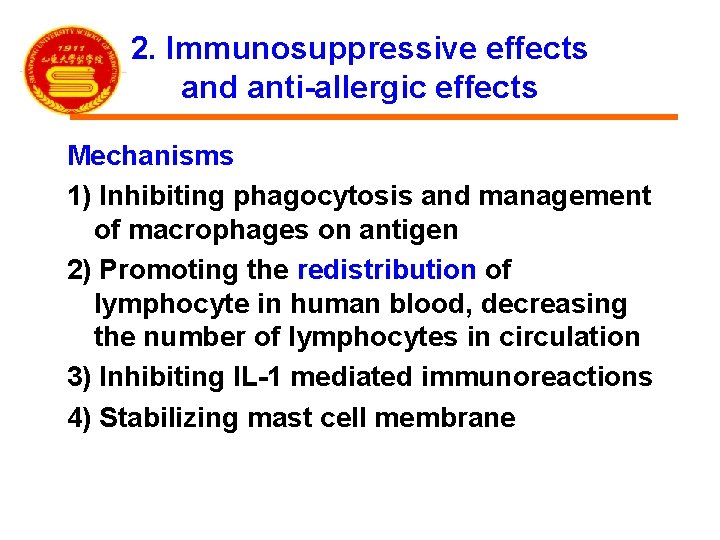
2. Immunosuppressive effects and anti-allergic effects Mechanisms 1) Inhibiting phagocytosis and management of macrophages on antigen 2) Promoting the redistribution of lymphocyte in human blood, decreasing the number of lymphocytes in circulation 3) Inhibiting IL-1 mediated immunoreactions 4) Stabilizing mast cell membrane
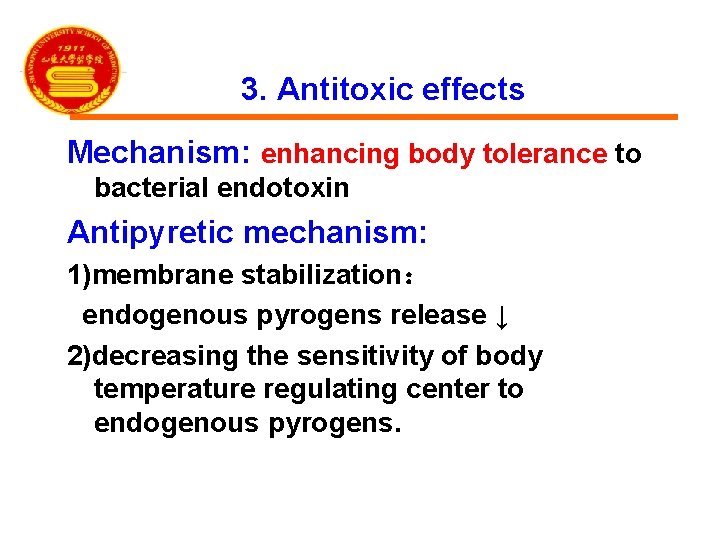
3. Antitoxic effects Mechanism: enhancing body tolerance to bacterial endotoxin Antipyretic mechanism: 1)membrane stabilization: endogenous pyrogens release ↓ 2)decreasing the sensitivity of body temperature regulating center to endogenous pyrogens.
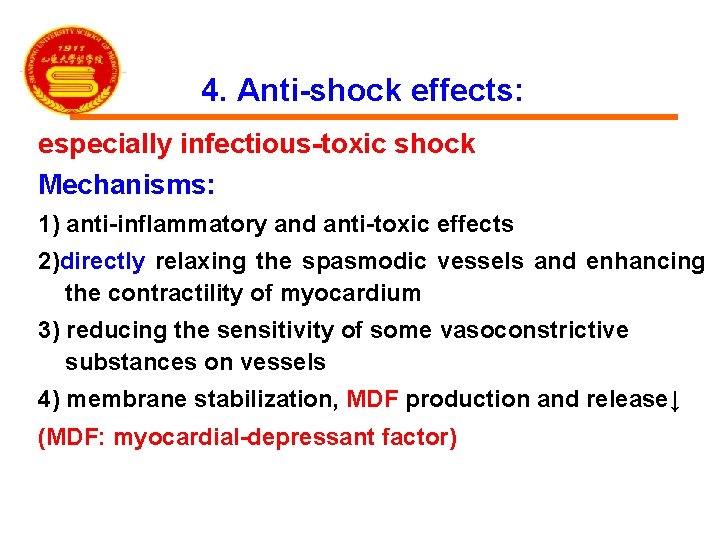
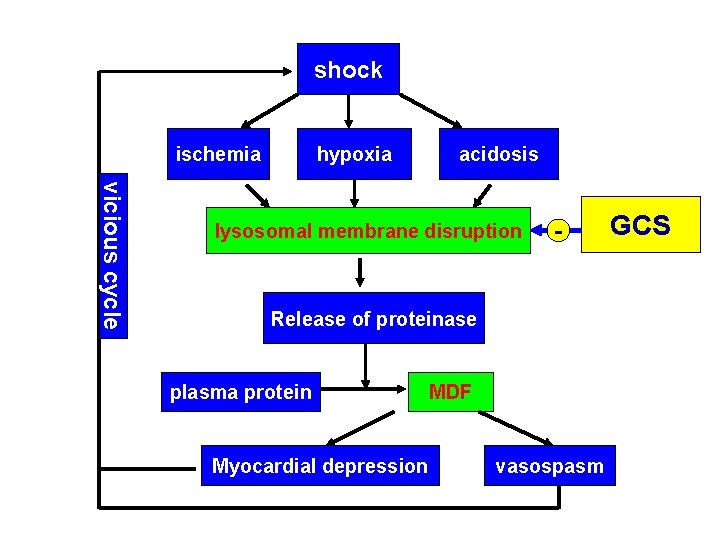
4. Anti-shock effects: especially infectious-toxic shock Mechanisms: 1) anti-inflammatory and anti-toxic effects 2)directly relaxing the spasmodic vessels and enhancing the contractility of myocardium 3) reducing the sensitivity of some vasoconstrictive substances on vessels 4) membrane stabilization, MDF production and release↓ (MDF: myocardial-depressant factor)
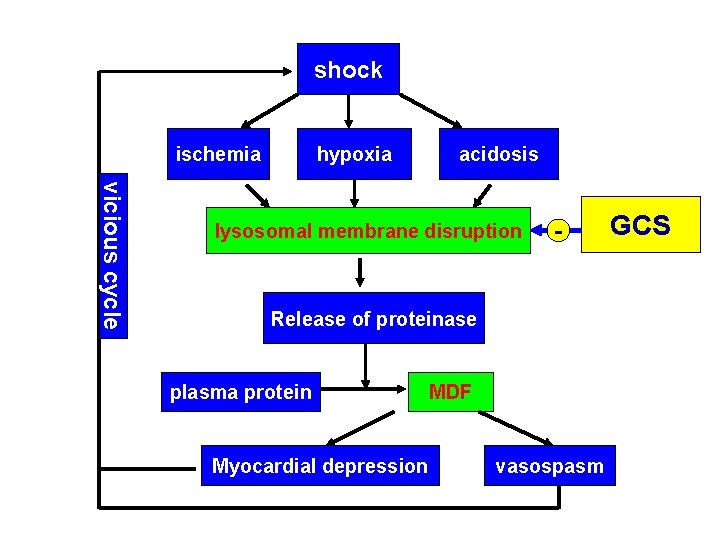
shock ischemia hypoxia acidosis vicious cycle lysosomal membrane disruption - Release of proteinase plasma protein Myocardial depression MDF vasospasm GCS
5. Effects on blood system (1) Stimulating hemopoiesis: RBC, PLT , Hb↑ (2) Neutrophils : number ↑, function↓ (3) Other blood cells: ↓ ( lymphocytes, basophilic , eosinophile granulocytes )
6. Other effects (1) Central nervous system: excitation (2) Digestive system: excitation (3) Skin and bone ① relieving itching ② anti-hyperplasy ③ osteoporosis
The effects of GCS in stress 1. Stress 2. Stress hormone is increased 3. Cortisol is an essential part of the body’s response to stress.
Actions of mineralocorticoids (mineral+ cortex + steroid)
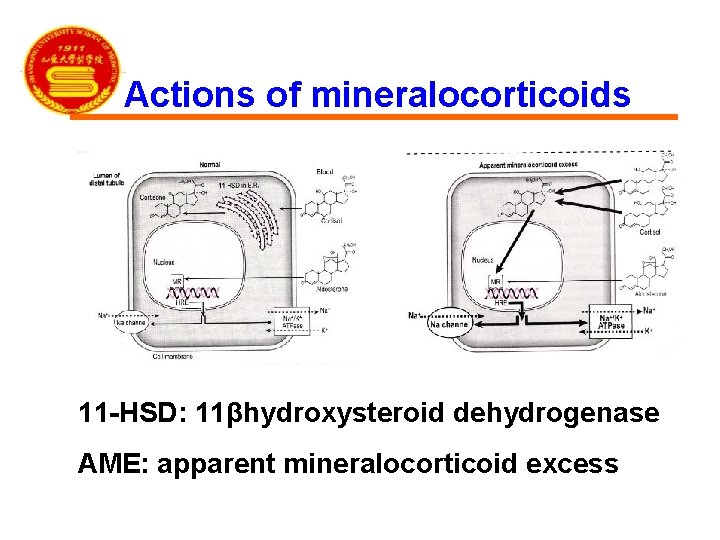
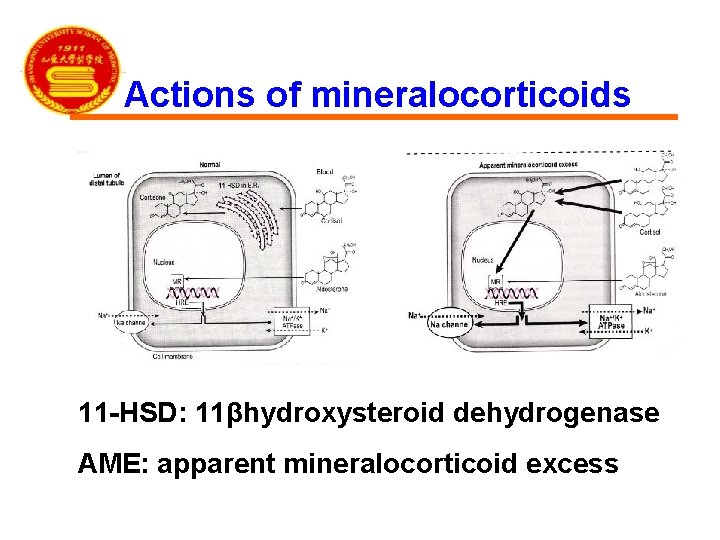
Actions of mineralocorticoids 11 -HSD: 11βhydroxysteroid dehydrogenase AME: apparent mineralocorticoid excess
Actions of adrenal androgens In disease states Virilizing effects Can be converted to estrogens
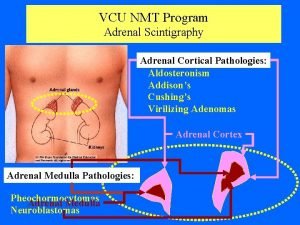
Part 5 Disorders of adrenal steroids Congenital adrenal hyperplasia Glucocorticoid excess Mineralocorticoid excess Adenal insufficiency

Congenital adrenal hyperplasia (CAH) • Deficiency of biosynthesis enzyme
Glucocorticoid excess: Cushing’s syndrome Causes • • 1. Exogenous corticosteroid administration 2. Cushing’s disease 3. Adrenal adenoma 4. Ectopic ACTH production
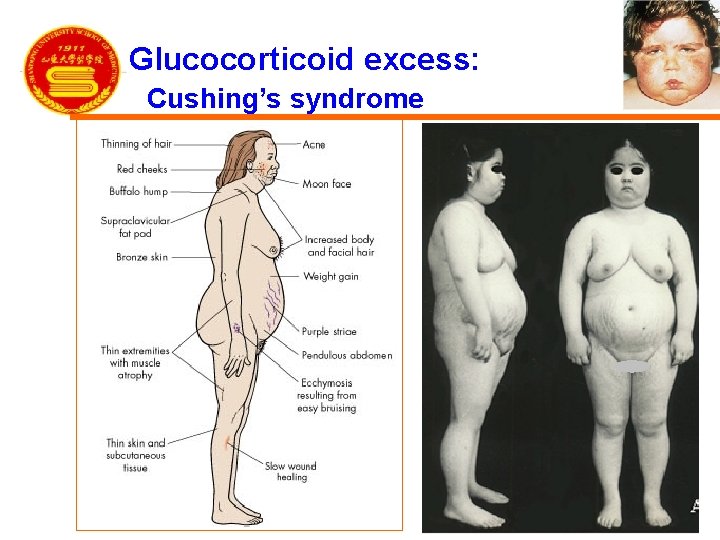
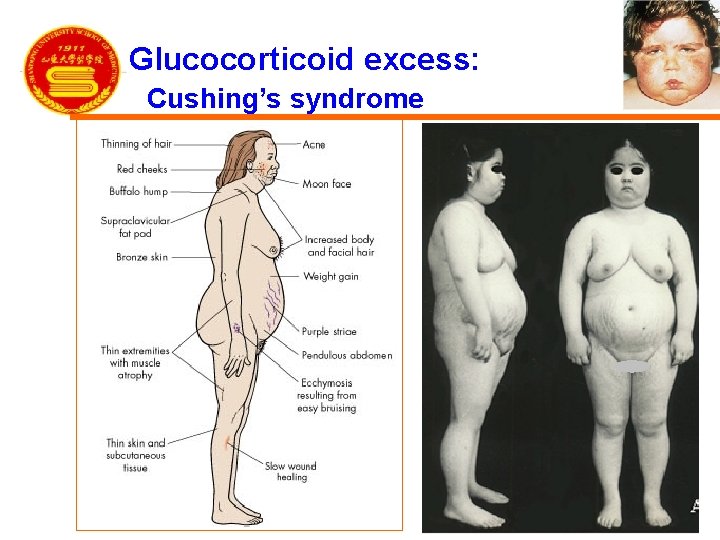
Glucocorticoid excess: Cushing’s syndrome
Investigations of GCS excess 1. Blood test (1) Basic test: Serum levels of cortisol and ACTH (2) Dynamic test: Dex suppression test 2. Image examination: CT and MRI
Mineralocorticoid excess: Conn’s syndrome Causes • 1. Aldosterone-secreting adrenal adenoma • 2. Idiopathic hyperaldosteronism Sympotoms: • hepertension and hypokalaemia Treatment: ADS receptor blockers
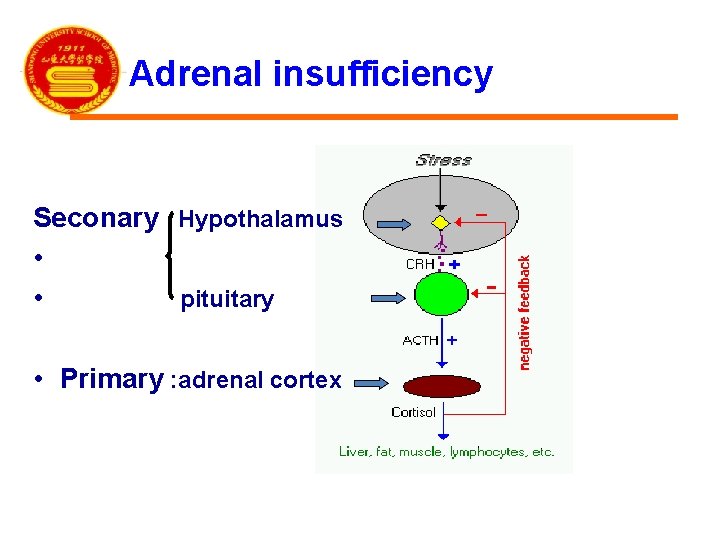
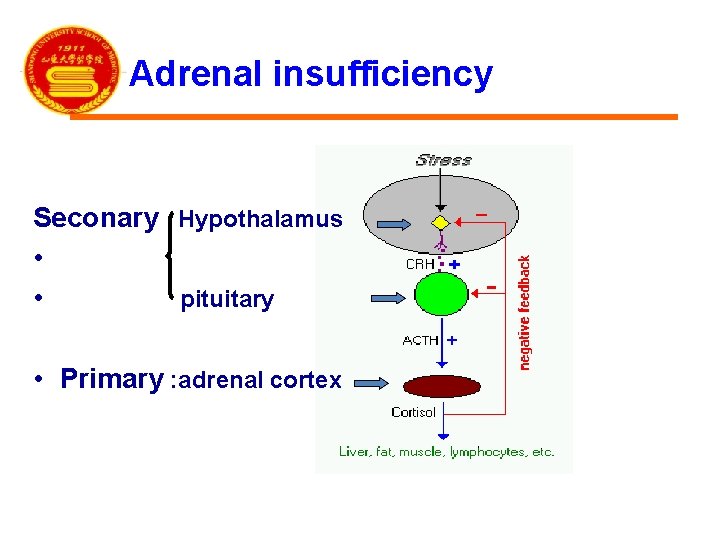
Adrenal insufficiency Seconary Hypothalamus • • pituitary • Primary : adrenal cortex
Adrenal insufficiency Acute: Water-house Friderichsen syndrome adrenal crisis ablation of bilateral adrenal glands Chronic: Addison’ s disease (primary) hypofunction of hypothalamus or pituitary (secondary)

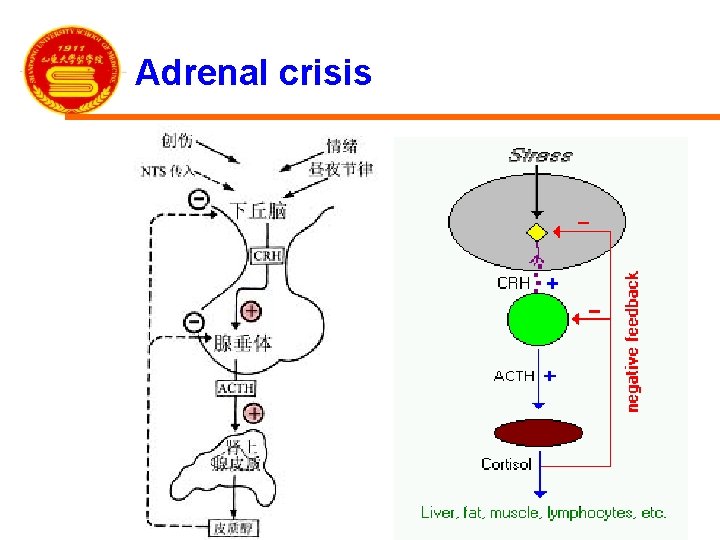
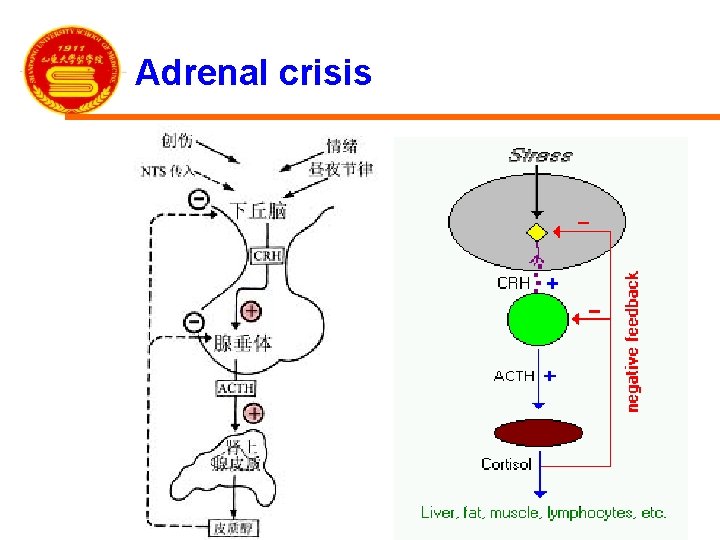
Adrenal crisis
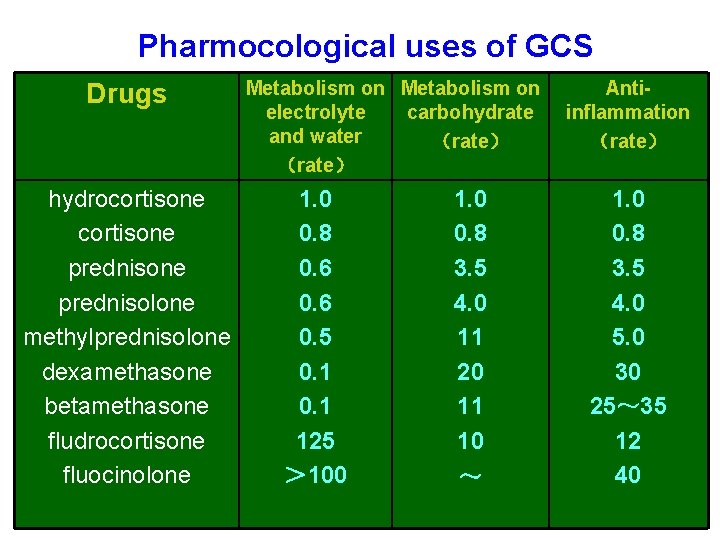
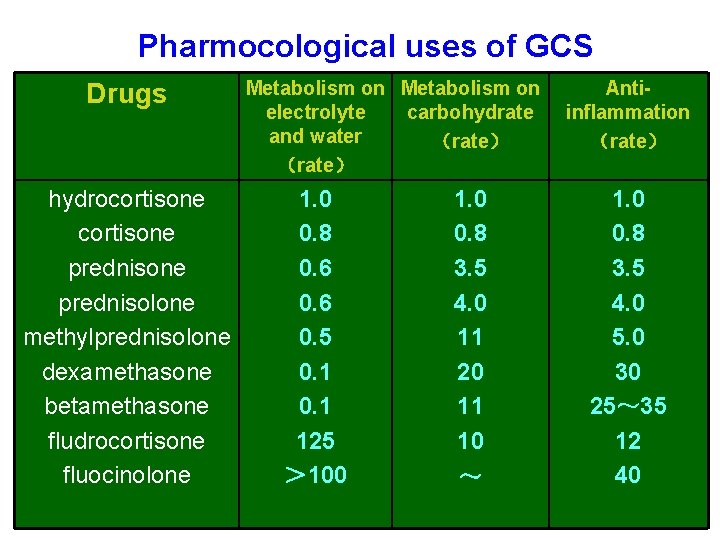
Pharmocological uses of GCS Drugs hydrocortisone prednisone prednisolone methylprednisolone dexamethasone betamethasone fludrocortisone fluocinolone Metabolism on electrolyte carbohydrate and water (rate) 1. 0 0. 8 0. 6 0. 5 0. 1 125 > 100 1. 0 0. 8 3. 5 4. 0 11 20 11 10 ~ Antiinflammation (rate) 1. 0 0. 8 3. 5 4. 0 5. 0 30 25~ 35 12 40
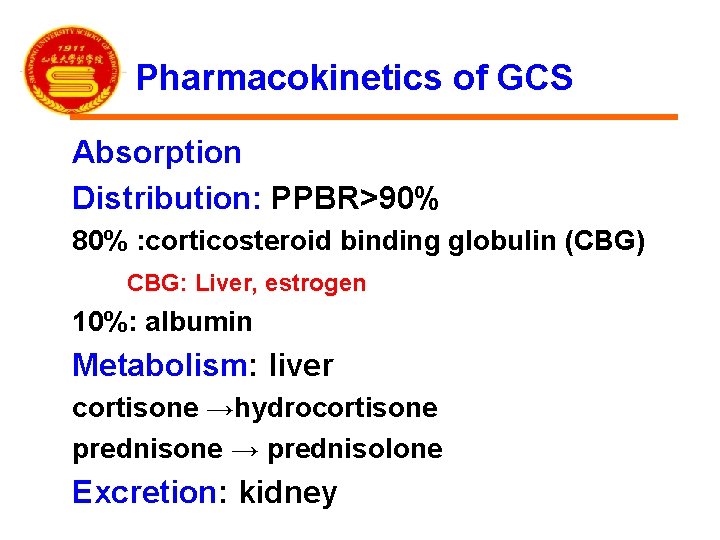
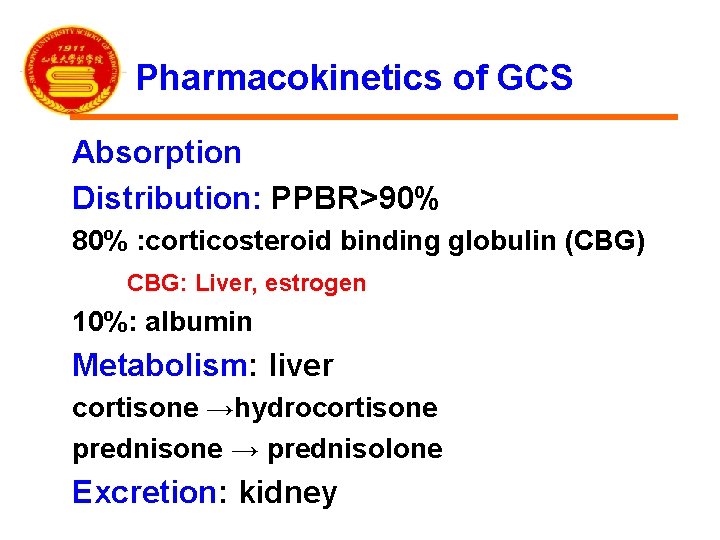
Pharmacokinetics of GCS Absorption Distribution: PPBR>90% 80% : corticosteroid binding globulin (CBG) CBG: Liver, estrogen 10%: albumin Metabolism: liver cortisone →hydrocortisone prednisone → prednisolone Excretion: kidney
Pharmocological uses of GCS • • 1. Replacement therapy 2. Severe infection and inflammation 3. Autoimmune and allergic diseases 4. Shock 5. Others (1) blood disorder (2) topical use (3) cancer
1. Replacement therapy: in small dose Primary/secondary, acute/chronic adrenal cortex hypofunction Acute: Water-house Friderichsen syndrome adrenal crisis ablation of bilateral adrenal glands Chronic: Addison’ s disease (primary) hypofunction of hypothalamus or pituitary (secondary)
2. Severe infection and inflammation 1)Severe acute bacterial infections Eg: fulminant epidemic meningitis(暴发性流脑), toxic bacillary dysentery(中毒性菌痢), toxic pneumonia, scarlet fever, acute miliary tuberculosis of lung, septicemia(败血症) large-dose , short-term treatment of GCS may help patients go through dangerous stage. Attention: must be used plus enough effective antibacterial agents. (why? )
2. Severe infection and inflammation 2) Some virus infection Eg. severe infective hepatitis epidemic parotitis (流行性腮腺炎) measles (麻疹) Japanese B encephalitis (乙脑) SARS

2. Severe infection and inflammation 3) Prevention for inflammatory sequela (1) tuberculous diseases: Eg. meningitis, pleuritis(胸膜炎), pericarditis(心包炎) (2) ocular diseases: iritis(虹膜炎), keratitis(角膜炎), retinitis(视网膜炎)
3. Autoimmune and allergic diseases 1) Autoimmune diseases: used widely rheumatic fever, rheumatic or rheumatoid arthritis rheumatic myocarditis systemic lupus erythematosus (SLE), autoimmune hemolytic anemia nephrotic syndrome

3. Autoimmune and allergic diseases 2) Organ transplantation: Combined with immunosupressive agents 3)Allergic diseases: bronchial asthma, urticaria(荨麻疹), hay fever, anaphylactic rhinitis(过敏性鼻炎) be given as supplements to the primary therapy
4. Shock effective to all kinds of shock 1)infectious-toxic shock : first choice 2)other shocks: supplements
5. Other clinical uses (1)Blood disorders acute lymphatic leukemia, aplastic anemia (AA), thrombocytopenia, granulocytopenia (2) Topical uses : local therapy some skin diseases some ocular diseases (3) Some cancers
Adverse reactions caused by continuous and longtime use of large doses of GCS Withdrawl reactions: adverse reactions caused by sudden withdrawl after a continuous and longtime use.
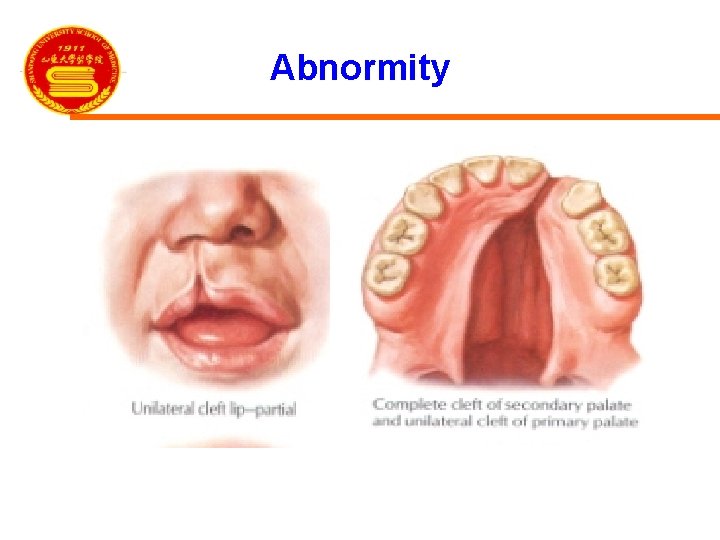
1. Adverse reactions caused by continuous and longtime use of large doses of GCS 1) Latrogenic(医源性) Cushing’s syndrome 2) Induction and aggravation of infection 3) Possible risk of peptic ulcers 4) Cardiovascular complications:HBP, AS 5) Other complications a. osteoporosis b. psychosis, euphoria c. growth retardation d. glaucoma:GIG e. abnormity
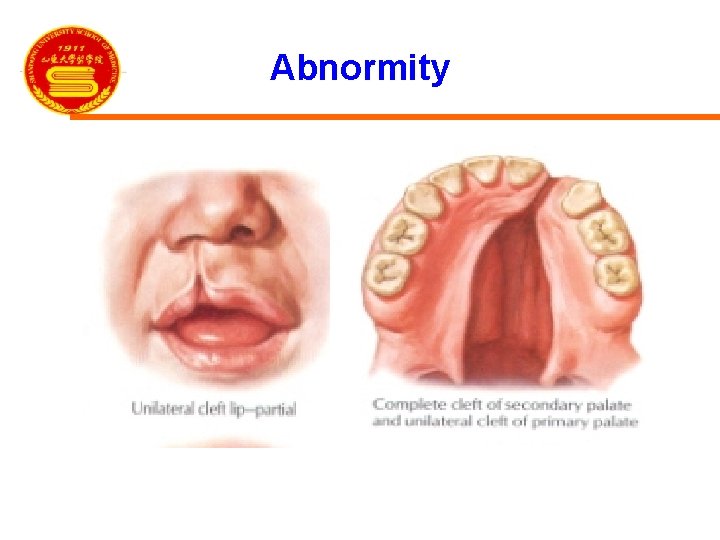
Abnormity

2. Withdrawal reactions 1) Latrogenic adrenocortical insufficiency : adrenocortical atrophy adrenal crisis 2) Rebound phenomenon
Contraindications Severe psychosis and epilepsy active peptic ulcer restore period of fracture and wound corneal ulcer severe hypertension diabetes pregnancy uncontrolled infection
Methods of application 1) Substitution therapy with small dose 2) Impact therapy with large dose 3) Long-term therapy with moderate dose (1) Therapy on every morning (2) Therapy on every other morning

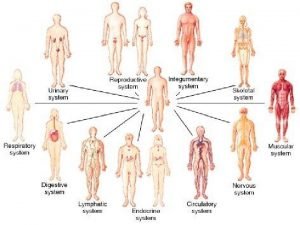
 Organ systems
Organ systems Adrenal glands
Adrenal glands Holocrine gland
Holocrine gland Adrenal medulla cortex
Adrenal medulla cortex Zona fasciculata
Zona fasciculata Zona reticularis gonadocorticoids
Zona reticularis gonadocorticoids Adrenal cortex develops from
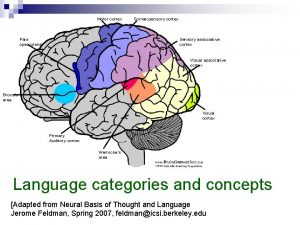
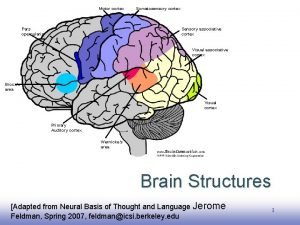
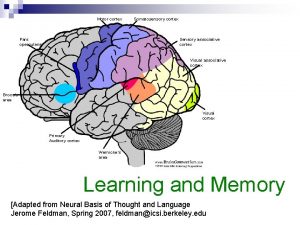
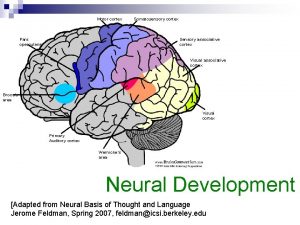
Adrenal cortex develops from Motor cortex sensory cortex
Motor cortex sensory cortex Summary of adrenal gland
Summary of adrenal gland Visceral autonomic nervous system
Visceral autonomic nervous system Neural groove
Neural groove The suprarenal (adrenal) medullae secrete
The suprarenal (adrenal) medullae secrete Adrenal sympathetic pathway
Adrenal sympathetic pathway Site:slidetodoc.com
Site:slidetodoc.com Hiperplasia adrenal congênita não clássica
Hiperplasia adrenal congênita não clássica Oktay eray
Oktay eray Pankreas öz suyunda bulunan enzimler
Pankreas öz suyunda bulunan enzimler Adrenal gland
Adrenal gland Conns and addison's
Conns and addison's Congenital adrenal hyperplasia genitalia
Congenital adrenal hyperplasia genitalia Congenital adrenal hyperplasia
Congenital adrenal hyperplasia Sella turcica
Sella turcica Adrenal bez histolojisi
Adrenal bez histolojisi Adrenal drugs pharmacology
Adrenal drugs pharmacology Adrenal hormone pathway
Adrenal hormone pathway Frontal sinus
Frontal sinus Acth
Acth Non klasik kah
Non klasik kah Congenital adrenal hyperplasia characteristics
Congenital adrenal hyperplasia characteristics Adrenal bezin hipofonksiyonu sonucu gelişen tablo
Adrenal bezin hipofonksiyonu sonucu gelişen tablo Adrenal gland hormones
Adrenal gland hormones Adrenal gland regions
Adrenal gland regions Adrenal sympathetic pathway
Adrenal sympathetic pathway Ectocrine
Ectocrine Arritimias
Arritimias Adrenal gland epithelium
Adrenal gland epithelium Objectives of stress management
Objectives of stress management Betoderm
Betoderm Psödocushing
Psödocushing Suprarenal gland relations
Suprarenal gland relations Menopause and mania
Menopause and mania Nursing management of adrenal tumor
Nursing management of adrenal tumor Insuficiencia adrenal
Insuficiencia adrenal Psammoma bodies
Psammoma bodies Adrenal tumour
Adrenal tumour Non classical adrenal hyperplasia
Non classical adrenal hyperplasia 21 hydroxylase deficiency
21 hydroxylase deficiency Medulla
Medulla Kolekalsiferol
Kolekalsiferol Hipotiroidismo congénito primario
Hipotiroidismo congénito primario Adrenal gland regions
Adrenal gland regions Adrenal cushing
Adrenal cushing Difference between serous and mucous acini
Difference between serous and mucous acini Gross anatomy of the gallbladder pancreas and bile passages
Gross anatomy of the gallbladder pancreas and bile passages Plicae digestive system
Plicae digestive system Colon
Colon Endocrine glands
Endocrine glands Thymic carcinoma
Thymic carcinoma Papillary layer
Papillary layer Anteromedial surface of parotid gland
Anteromedial surface of parotid gland Exocrine glands
Exocrine glands Cretinism
Cretinism Vesper rat
Vesper rat Oxyntic glands
Oxyntic glands Coiled gland
Coiled gland Type 2 pneumocytes surfactant
Type 2 pneumocytes surfactant Female reproductive system definition
Female reproductive system definition Flask shaped gland
Flask shaped gland Endocrine system of rat
Endocrine system of rat Basal cell adenoma
Basal cell adenoma Histological structure of parathyroid gland
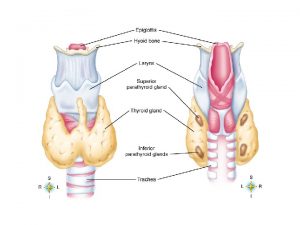
Histological structure of parathyroid gland Male accessory glands
Male accessory glands Female hymen
Female hymen Parathyroid gland supplied by
Parathyroid gland supplied by Types of salivary glands
Types of salivary glands Mammary gland merocrine
Mammary gland merocrine Where are the gastric glands located
Where are the gastric glands located Difference between serous and mucous acini slideshare
Difference between serous and mucous acini slideshare Dysphagia terminology
Dysphagia terminology Glands secrete what in reflex actions
Glands secrete what in reflex actions General structure of exocrine glands
General structure of exocrine glands