Adrenal Glands Part 2 Control of Adrenal Cortical
- Slides: 16
Adrenal Glands Part 2
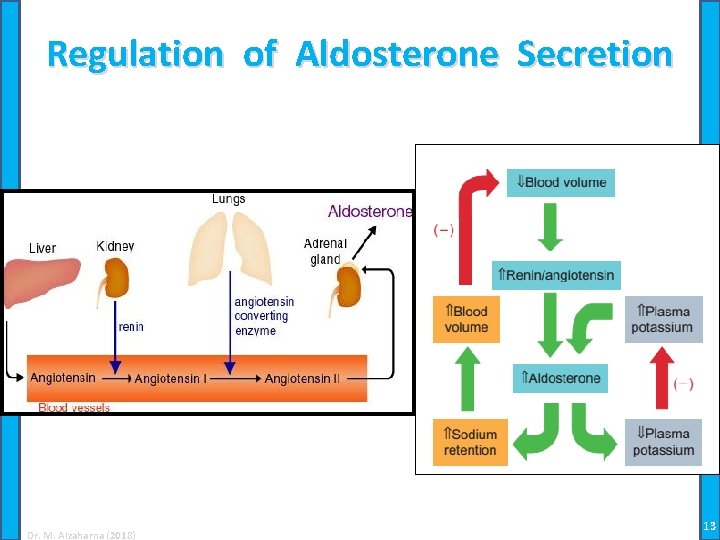
Control of Adrenal Cortical Hormone Synthesis Control of aldosterone synthesis: • The control of aldosterone synthesis is more complex than that of the glucocorticoids • Although cells of the zona glomerulosa express ACTH receptors and ACTH is required for optimal secretion, ACTH is not an important regulator of aldosterone production in most species • Angiotensin II production is the hormonal signal for increase production of aldosterone • Angiotensin II reacts with specific G-protein-coupled membrane receptors, but does not use cyclic AMP as its second messenger Dr. M. Alzaharna (2018) 2
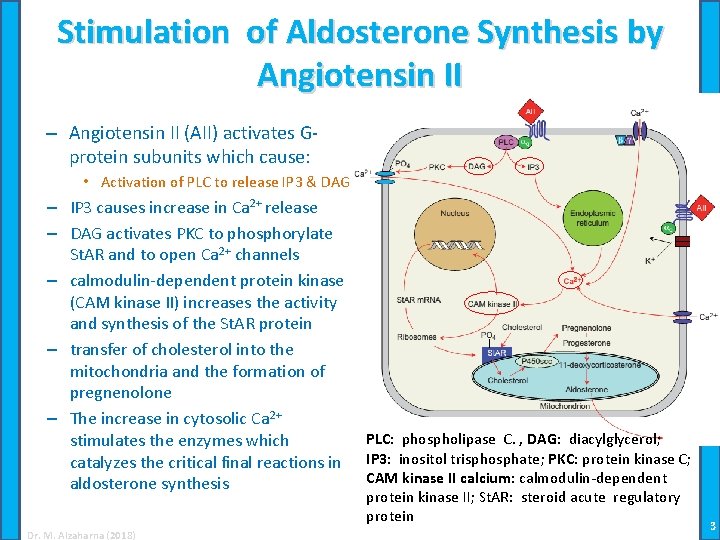
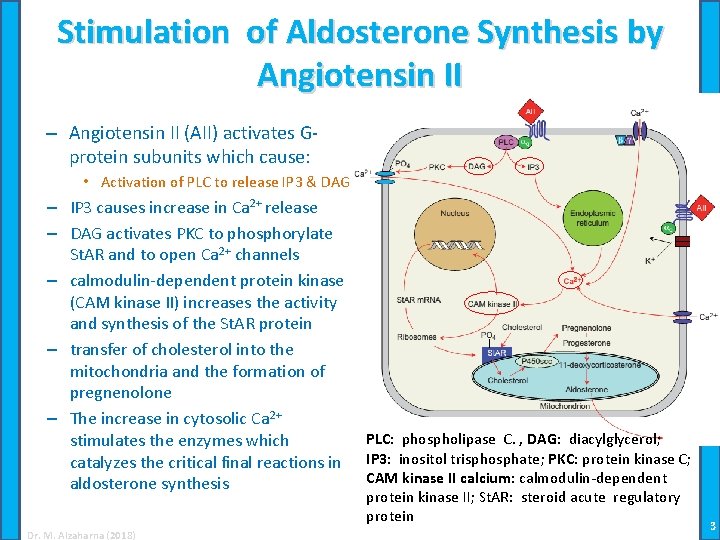
Stimulation of Aldosterone Synthesis by Angiotensin II – Angiotensin II (AII) activates Gprotein subunits which cause: • Activation of PLC to release IP 3 & DAG – IP 3 causes increase in Ca 2+ release – DAG activates PKC to phosphorylate St. AR and to open Ca 2+ channels – calmodulin-dependent protein kinase (CAM kinase II) increases the activity and synthesis of the St. AR protein – transfer of cholesterol into the mitochondria and the formation of pregnenolone – The increase in cytosolic Ca 2+ stimulates the enzymes which catalyzes the critical final reactions in aldosterone synthesis Dr. M. Alzaharna (2018) PLC: phospholipase C. , DAG: diacylglycerol; IP 3: inositol trisphosphate; PKC: protein kinase C; CAM kinase II calcium: calmodulin-dependent protein kinase II; St. AR: steroid acute regulatory protein 3
Regulation of Aldosterone by Potassium and Atrial Natriuretic Factor • Cells of the zona glomerulosa are exquisitely sensitive to changes in concentration of potassium in the extracellular fluid • As extracellular potassium increases – voltage-sensitive calcium channels are activated – This increases intracellular calcium and activates calmodulin kinase II which increases aldosterone as already described • Synthesis and secretion of aldosterone are negatively regulated by atrial natriuretic factor (ANF): – which activates potassium channels and thereby opposes opening of voltage sensitive calcium channels – Additionally, ANF reduces synthesis and phosphorylation of the St. AR protein and inhibits transcription of its gene Dr. M. Alzaharna (2018) 4
Adrenal Steroid Hormones in Blood • Adrenal cortical hormones are transported in blood bound to a specific plasma protein: – Transcortin or corticosteroid binding globulin (CBG), – and to a lesser extent to albumin • CBG has a single steroid hormone binding site whose affinity for cortisol is nearly 20 times higher than for aldosterone • The androgens bind mainly to albumin • Other endogenous steroids usually do not significantly affect cortisol binding to CBG; – an exception is in late pregnancy, when progesterone may occupy about 25% of the binding sites on CBG Dr. M. Alzaharna (2018) 5
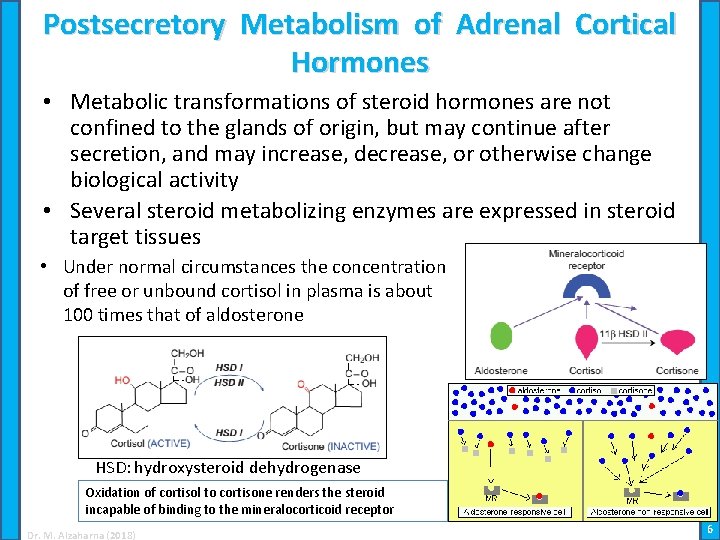
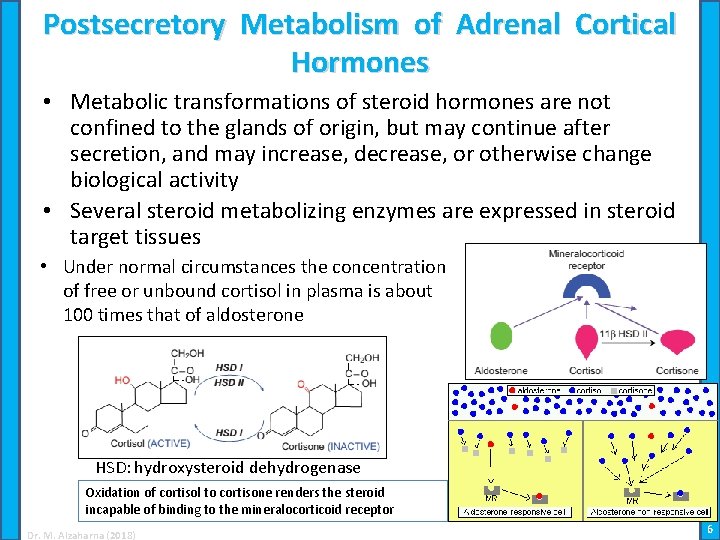
Postsecretory Metabolism of Adrenal Cortical Hormones • Metabolic transformations of steroid hormones are not confined to the glands of origin, but may continue after secretion, and may increase, decrease, or otherwise change biological activity • Several steroid metabolizing enzymes are expressed in steroid target tissues • Under normal circumstances the concentration of free or unbound cortisol in plasma is about 100 times that of aldosterone HSD: hydroxysteroid dehydrogenase Oxidation of cortisol to cortisone renders the steroid incapable of binding to the mineralocorticoid receptor Dr. M. Alzaharna (2018) 6
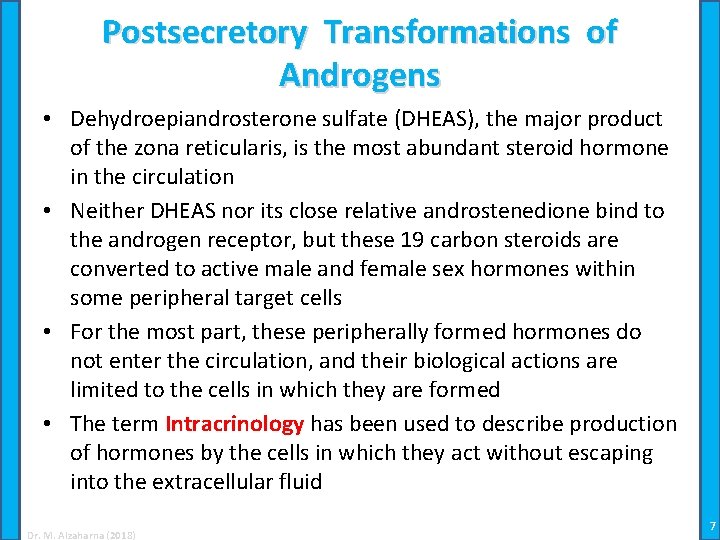
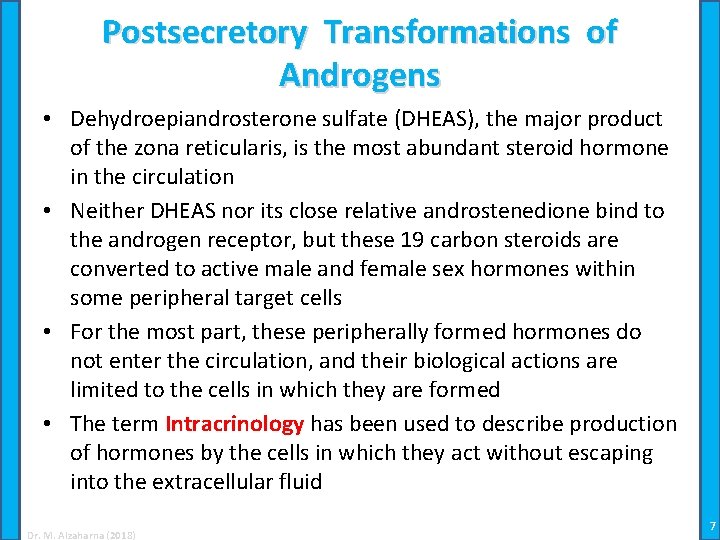
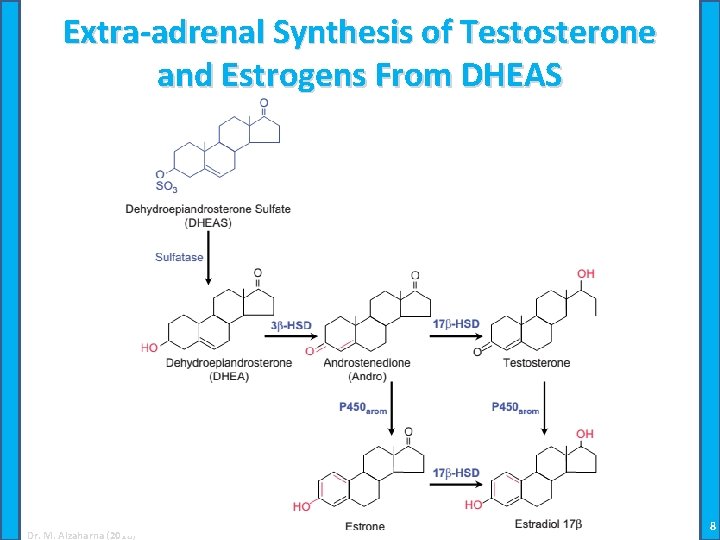
Postsecretory Transformations of Androgens • Dehydroepiandrosterone sulfate (DHEAS), the major product of the zona reticularis, is the most abundant steroid hormone in the circulation • Neither DHEAS nor its close relative androstenedione bind to the androgen receptor, but these 19 carbon steroids are converted to active male and female sex hormones within some peripheral target cells • For the most part, these peripherally formed hormones do not enter the circulation, and their biological actions are limited to the cells in which they are formed • The term Intracrinology has been used to describe production of hormones by the cells in which they act without escaping into the extracellular fluid Dr. M. Alzaharna (2018) 7
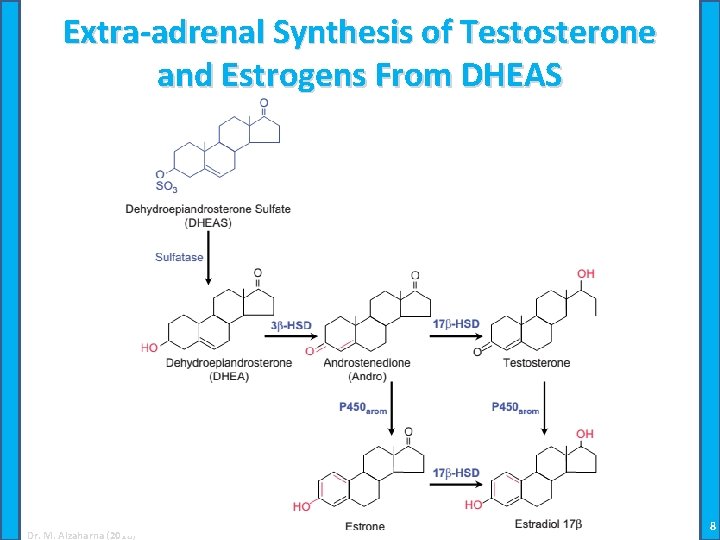
Extra-adrenal Synthesis of Testosterone and Estrogens From DHEAS Dr. M. Alzaharna (2018) 8
Inactivation of Adrenal Cortical Steroids • Mammals cannot degrade the ring structure of the steroid nucleus • Steroid hormones are inactivated, mainly in the liver, by metabolic changes that make them unrecognizable to their receptors • This also makes them more soluble to pass through renal glomerular capillaries and to be excreted in the urine • Because recognizable hormonal derivatives are excreted in urine, it is possible to estimate daily secretory rates of steroid hormones by the noninvasive technique of measuring their abundance in urine Dr. M. Alzaharna (2018) 9
Physiology of the Mineralocorticoids • Aldosterone is by far the most important mineralocorticoid which can produce mineralocorticoid effects • Reabsorption of sodium is diminished in the absence of aldosterone, and with loss of sodium, there is an: – accompanying loss of water – and a resulting decrease in blood volume • Simultaneous with the loss of sodium, the ability to excrete potassium is impaired, and with continued dietary intake, plasma concentrations of potassium may increase – Causes cardiac arrhythmia and weakness of muscles including the heart Dr. M. Alzaharna (2018) 10
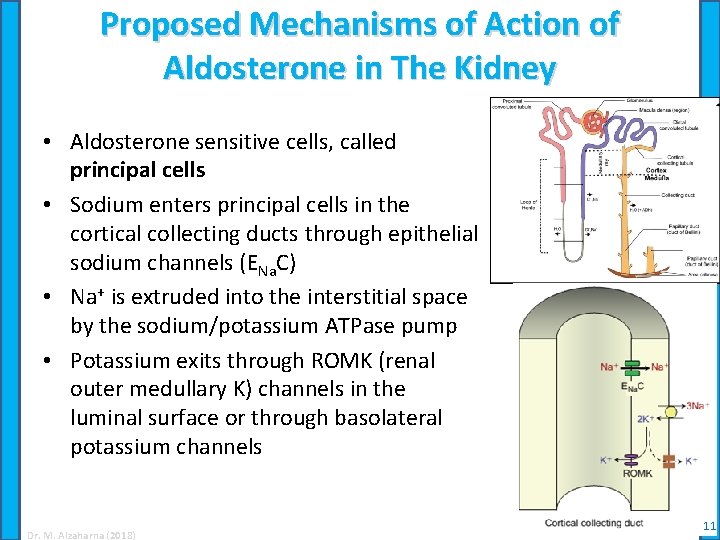
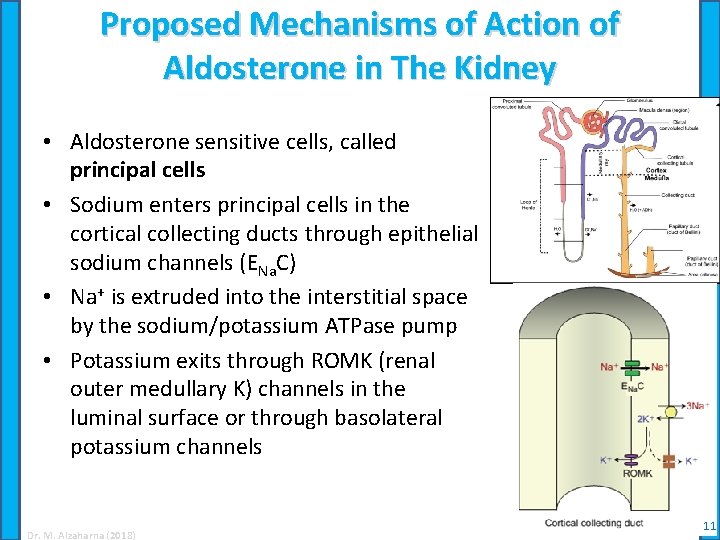
Proposed Mechanisms of Action of Aldosterone in The Kidney • Aldosterone sensitive cells, called principal cells • Sodium enters principal cells in the cortical collecting ducts through epithelial sodium channels (ENa. C) • Na+ is extruded into the interstitial space by the sodium/potassium ATPase pump • Potassium exits through ROMK (renal outer medullary K) channels in the luminal surface or through basolateral potassium channels Dr. M. Alzaharna (2018) 11
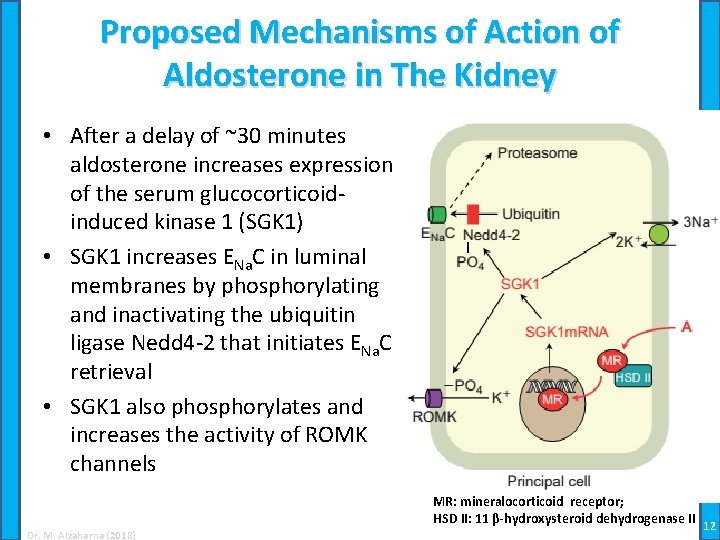
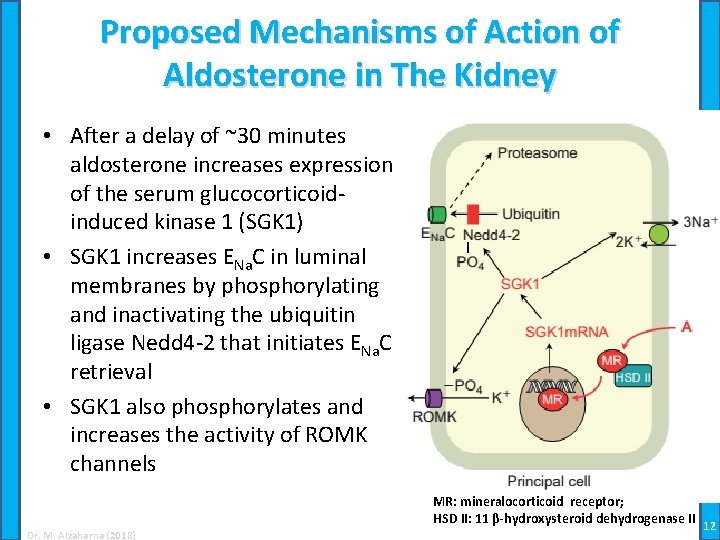
Proposed Mechanisms of Action of Aldosterone in The Kidney • After a delay of ~30 minutes aldosterone increases expression of the serum glucocorticoidinduced kinase 1 (SGK 1) • SGK 1 increases ENa. C in luminal membranes by phosphorylating and inactivating the ubiquitin ligase Nedd 4 -2 that initiates ENa. C retrieval • SGK 1 also phosphorylates and increases the activity of ROMK channels MR: mineralocorticoid receptor; HSD II: 11 β-hydroxysteroid dehydrogenase II Dr. M. Alzaharna (2018) 12
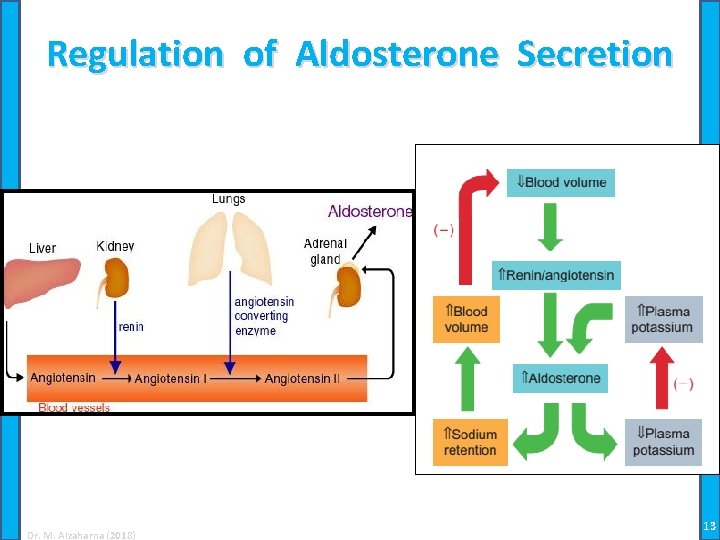
Regulation of Aldosterone Secretion Dr. M. Alzaharna (2018) 13
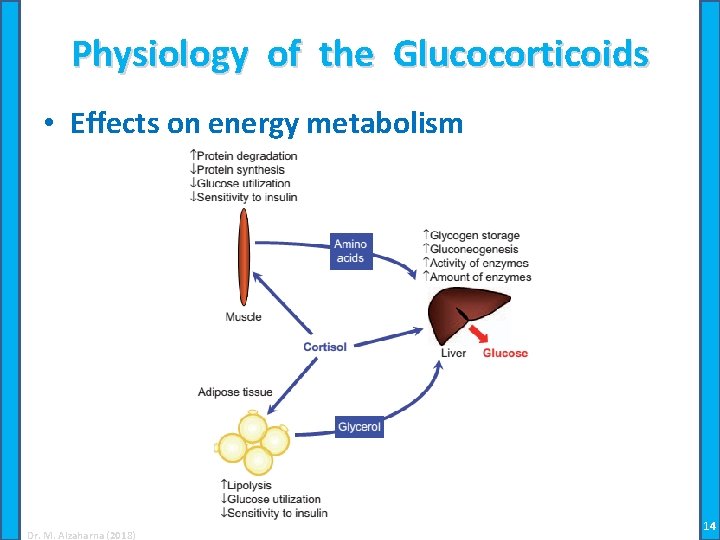
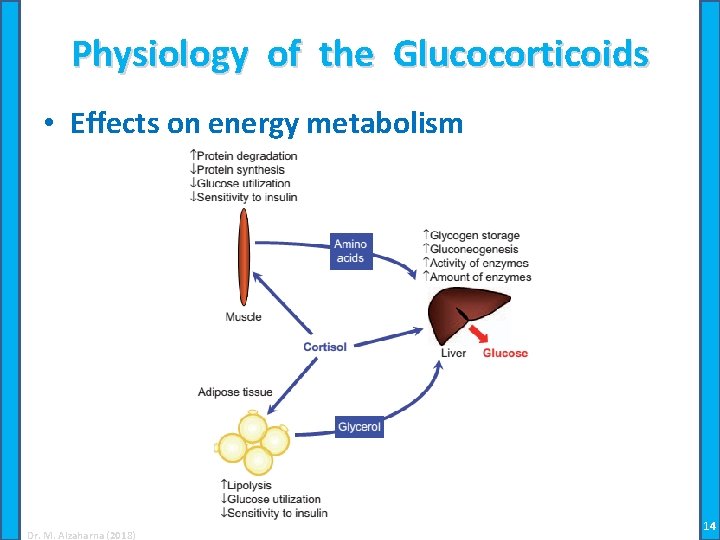
Physiology of the Glucocorticoids • Effects on energy metabolism Dr. M. Alzaharna (2018) 14
Physiology of the Glucocorticoids • Effects on lung development – Increase maturation and surfactant production during fetal development • Glucocorticoids and responses to injury – Exert anti-inflammatory effects, modulate synthesis, secretion, and actions of inflammatory mediators Dr. M. Alzaharna (2018) 15
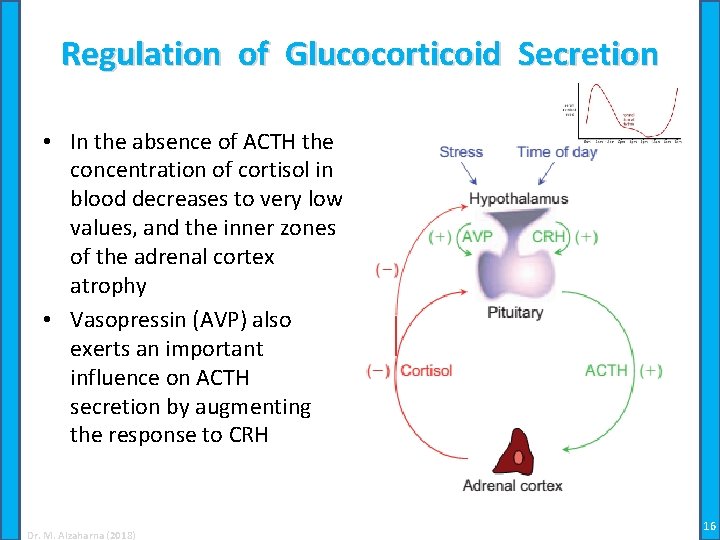
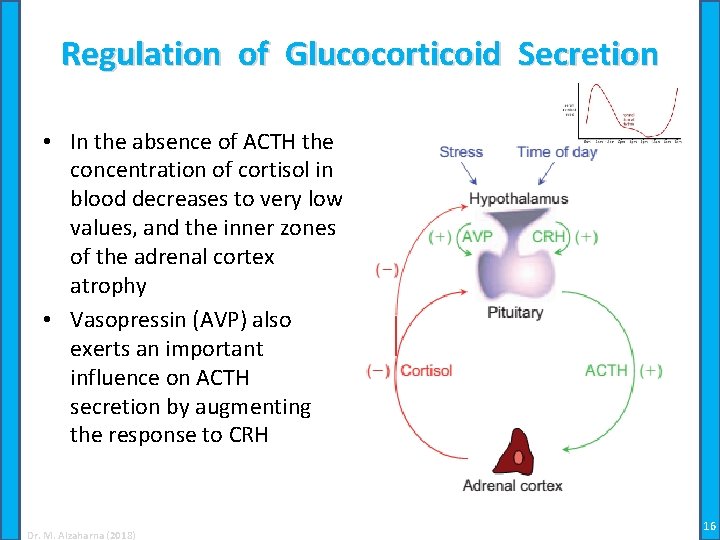
Regulation of Glucocorticoid Secretion • In the absence of ACTH the concentration of cortisol in blood decreases to very low values, and the inner zones of the adrenal cortex atrophy • Vasopressin (AVP) also exerts an important influence on ACTH secretion by augmenting the response to CRH Dr. M. Alzaharna (2018) 16
 Adrenal glands
Adrenal glands Reproductive organ system
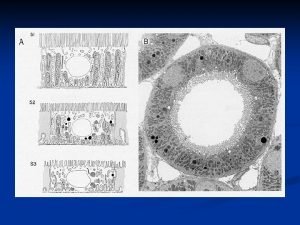
Reproductive organ system Epithelia
Epithelia Cortical region of kidney
Cortical region of kidney Afferent arteriole
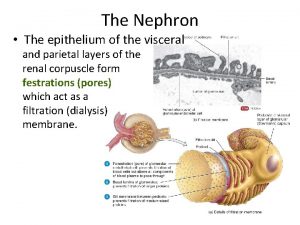
Afferent arteriole Nephron structure
Nephron structure Difference between cortical and juxtamedullary nephrons
Difference between cortical and juxtamedullary nephrons Juxtamedullary nephrons
Juxtamedullary nephrons Juxtamedullary vs cortical nephrons
Juxtamedullary vs cortical nephrons Interstitium
Interstitium Hyperfluorescence
Hyperfluorescence Lib tech crack'n
Lib tech crack'n Cortical columns
Cortical columns Charulata sankhla
Charulata sankhla Cortical drift and displacement
Cortical drift and displacement Medulla hair
Medulla hair Cortical defect
Cortical defect