OPTIC NERVE DISEASES VISUAL FIELD Dr Canan Asl


- Slides: 67
OPTIC NERVE DISEASES & VISUAL FIELD Dr. Canan Aslı Yıldırım Ophthalmology
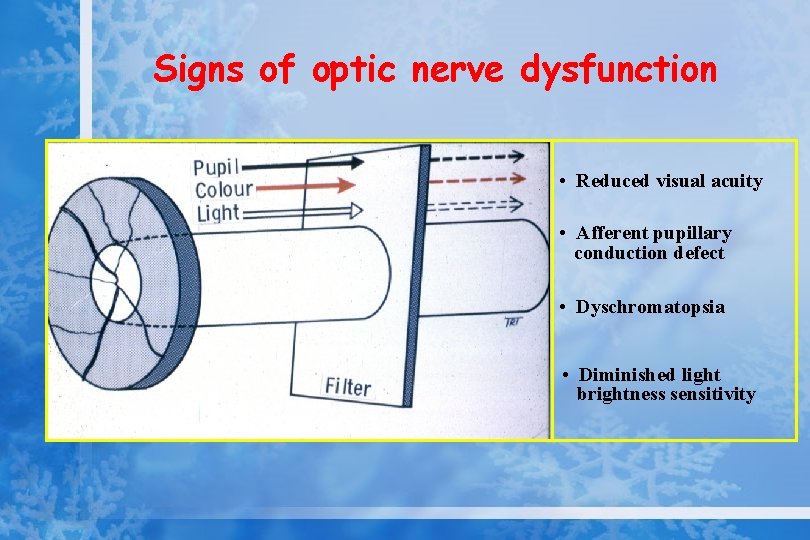
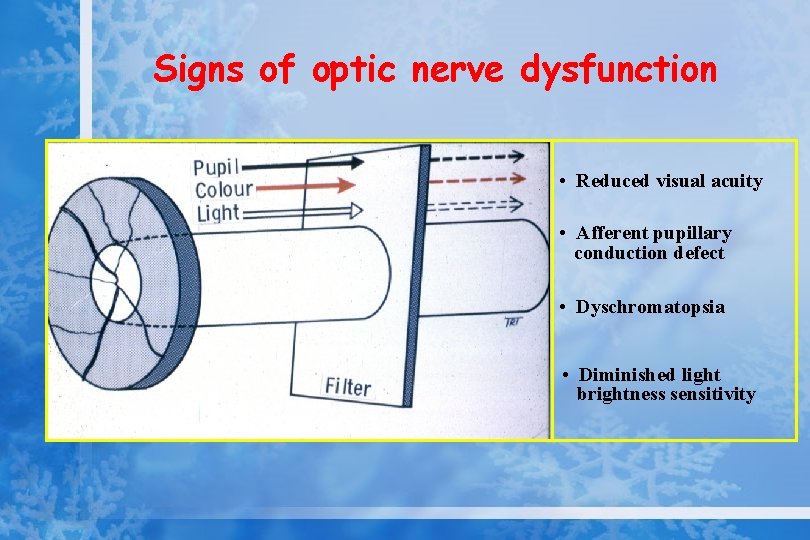
Signs of optic nerve dysfunction • Reduced visual acuity • Afferent pupillary conduction defect • Dyschromatopsia • Diminished light brightness sensitivity
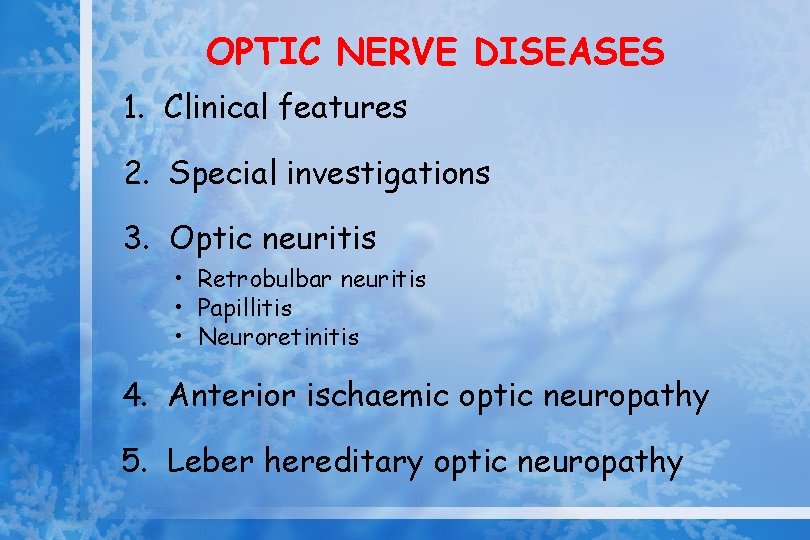
OPTIC NERVE DISEASES 1. Clinical features 2. Special investigations 3. Optic neuritis • Retrobulbar neuritis • Papillitis • Neuroretinitis 4. Anterior ischaemic optic neuropathy 5. Leber hereditary optic neuropathy
Clinical features • Reduced visual acuity • Visual field defects • Diminished pupillary light reactions • Impairment of colour vision • Diminished light brightness sensitivity
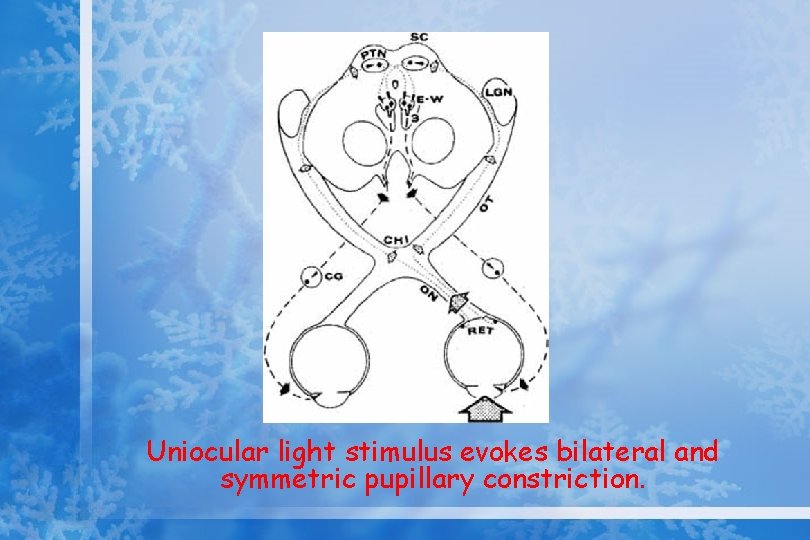
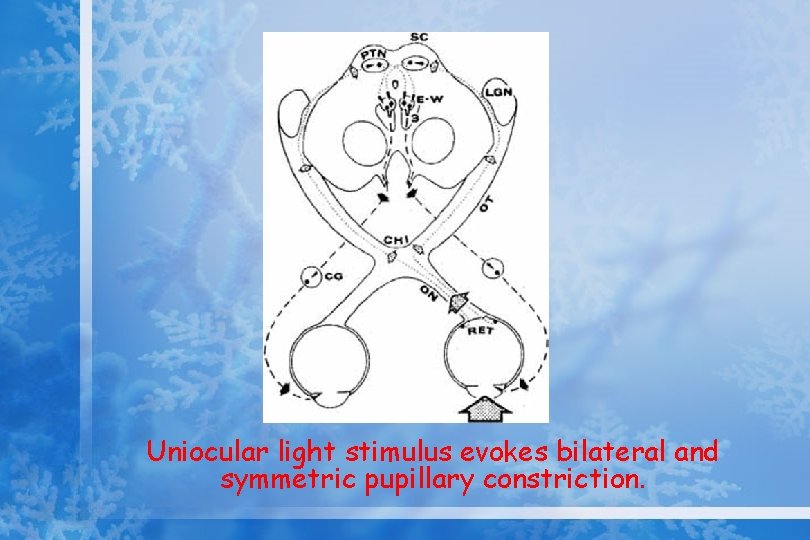
Uniocular light stimulus evokes bilateral and symmetric pupillary constriction.
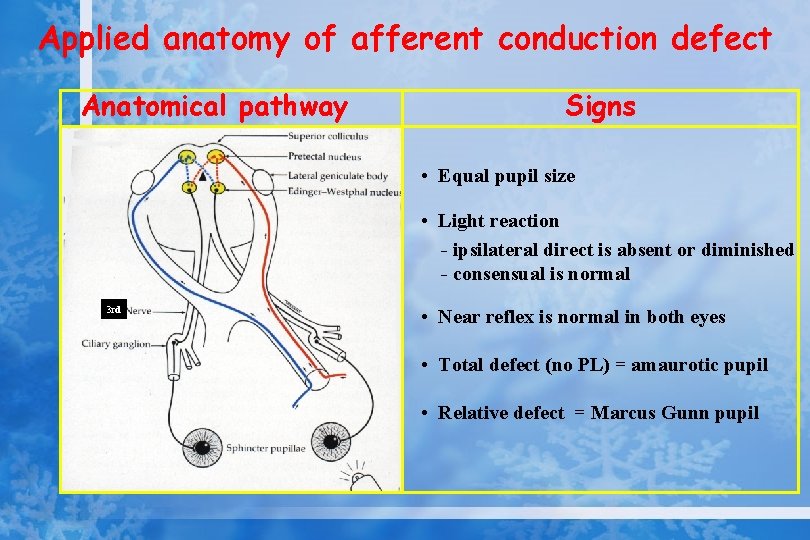
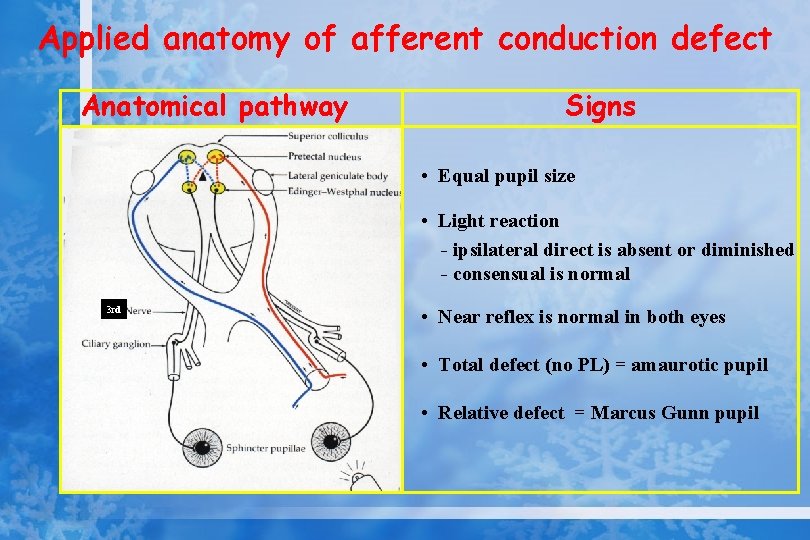
Applied anatomy of afferent conduction defect Anatomical pathway Signs • Equal pupil size • Light reaction - ipsilateral direct is absent or diminished - consensual is normal 3 rd • Near reflex is normal in both eyes • Total defect (no PL) = amaurotic pupil • Relative defect = Marcus Gunn pupil
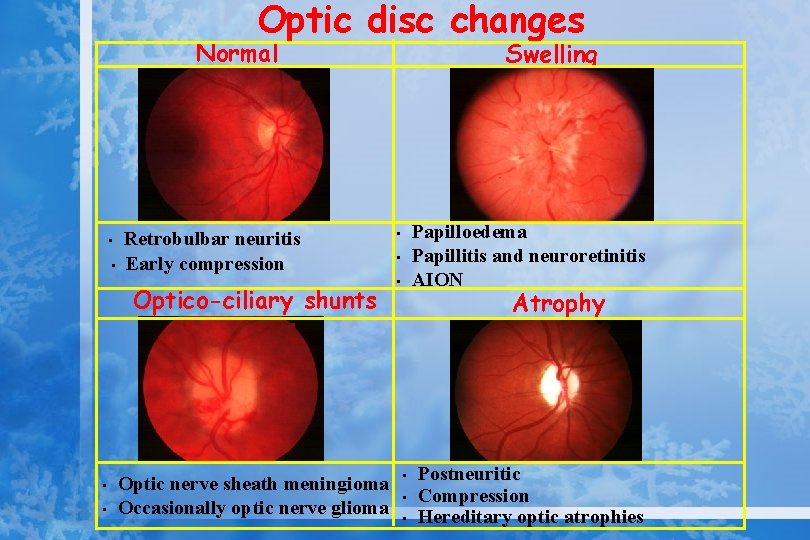
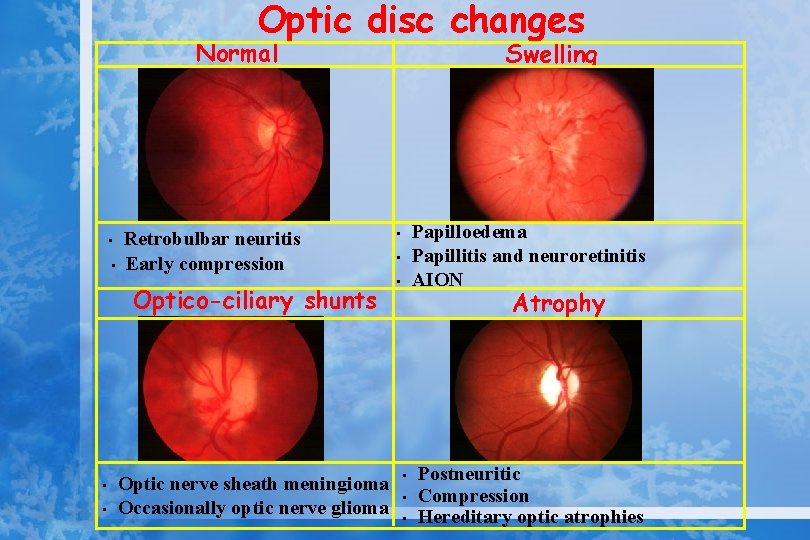
Optic disc changes Normal • • Retrobulbar neuritis Early compression Optico-ciliary shunts • • Optic nerve sheath meningioma Occasionally optic nerve glioma Swelling Papilloedema Papillitis and neuroretinitis AION • • • Atrophy • • • Postneuritic Compression Hereditary optic atrophies
Classification of optic neuropathies • Optic neuritis • • – Retrobulbar neuritis – Papillitis – Neuroretinitis Ischemic optic neuropathy Hereditary optic neuropathy Toxic optic neuropathy Post-infectious optic neuropathy
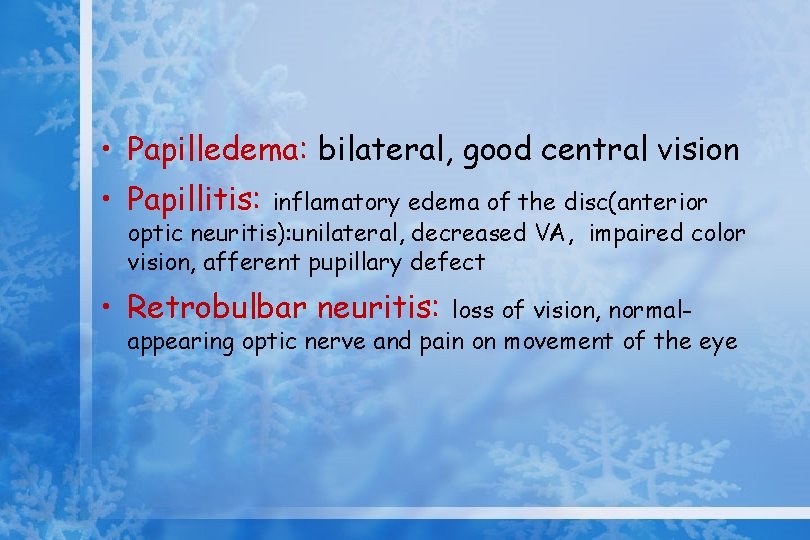
• Papilledema: bilateral, good central vision • Papillitis: inflamatory edema of the disc(anterior optic neuritis): unilateral, decreased VA, impaired color vision, afferent pupillary defect • Retrobulbar neuritis: loss of vision, normalappearing optic nerve and pain on movement of the eye
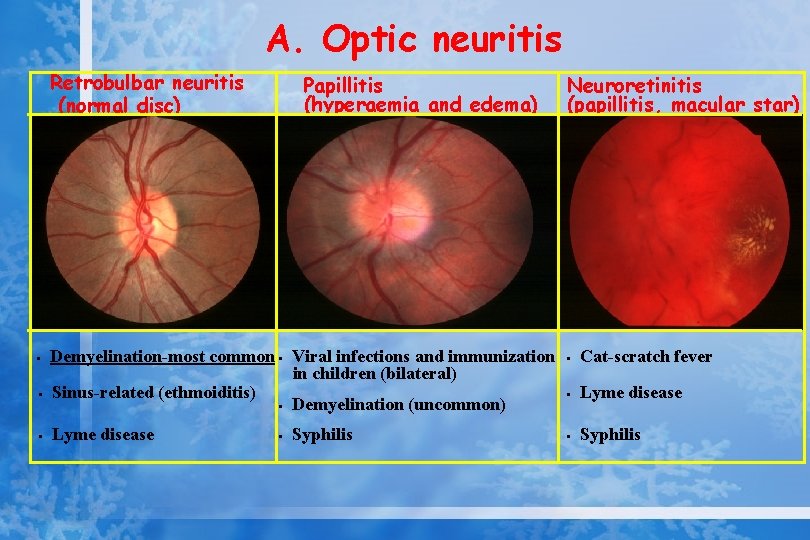
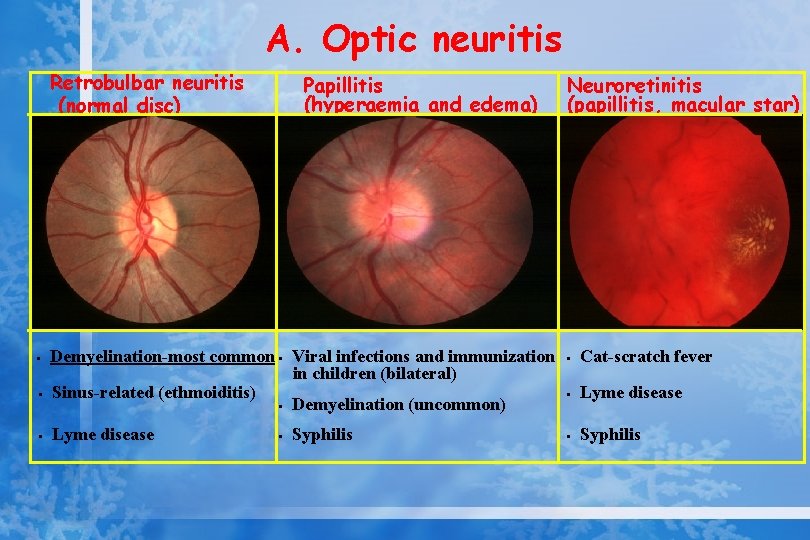
A. Optic neuritis Retrobulbar neuritis (normal disc) • • • Papillitis (hyperaemia and edema) Demyelination-most common • Viral infections and immunization in children (bilateral) Sinus-related (ethmoiditis) • Demyelination (uncommon) Lyme disease • Syphilis Neuroretinitis (papillitis, macular star) • Cat-scratch fever • Lyme disease • Syphilis
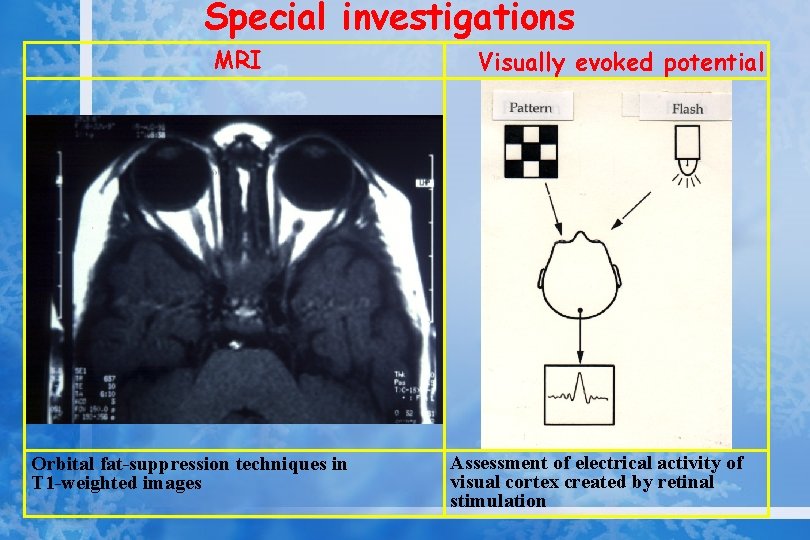
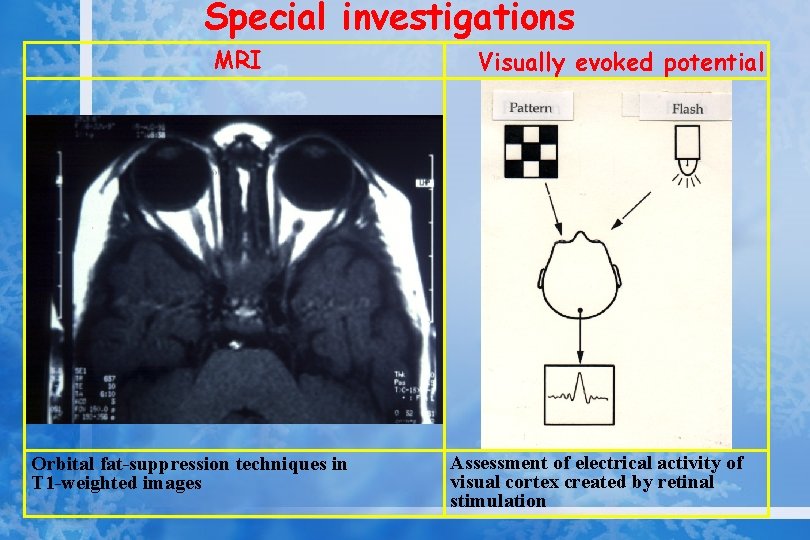
Special investigations MRI Orbital fat-suppression techniques in T 1 -weighted images Visually evoked potential Assessment of electrical activity of visual cortex created by retinal stimulation
Optic neuritis • • Women %74, men %34 %70 with multiple sclerosis Uhthoff’s phenomenon + Clinical features; -acute onset of monocular visual loss -periocular discomfort -frontal headache -impairment of colour vision
Multiple sclerosis A common idiopathic demyelination disorder of the CNS characterized by intermittent disturbances of neurological function Clinical features; • spinal cord lesions (weakness, stiffness, muscle spasms) • brain stem lesions (diplopia, nistagmus, ataxia, dysarthria) • hemisphere lesions (depression, dementia, hemianopia, hemiparesis) • transient phenomena (epilepsy, uhthoff’s phenomenon)
Uhthoff’s phenomenon • Sudden, temporary worsening of visual or other symptoms brought on by physical exercise or increase in body temperature
Diagnosis of Multiple sclerosis • Lumbar puncture • Evoked potential recordings • Magnetic resonance imaging (MRI)
B. Ischemic optic neuropathy 1. Non-arteritic 2. Arteritic
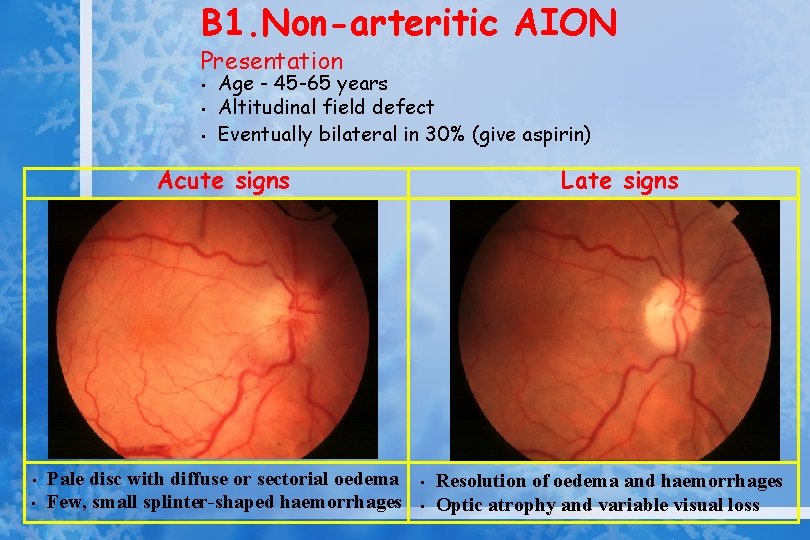
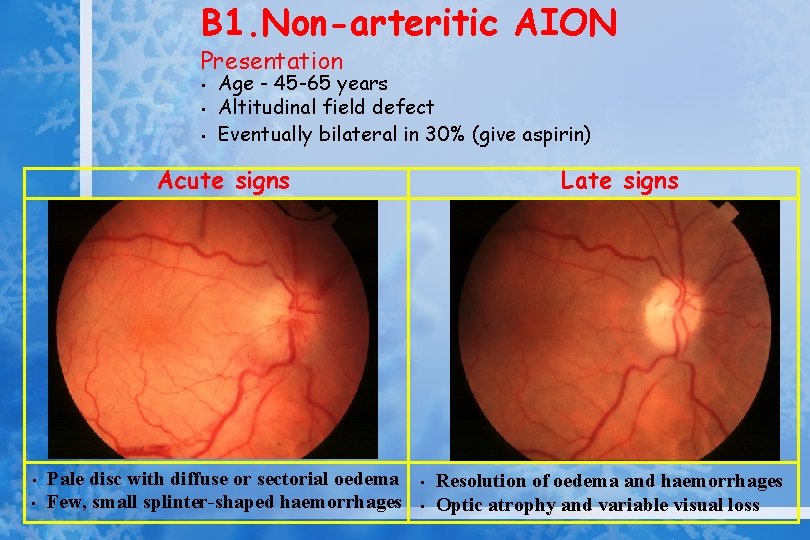
B 1. Non-arteritic AION Presentation • • • Age - 45 -65 years Altitudinal field defect Eventually bilateral in 30% (give aspirin) Acute signs • • Pale disc with diffuse or sectorial oedema Few, small splinter-shaped haemorrhages Late signs • • Resolution of oedema and haemorrhages Optic atrophy and variable visual loss
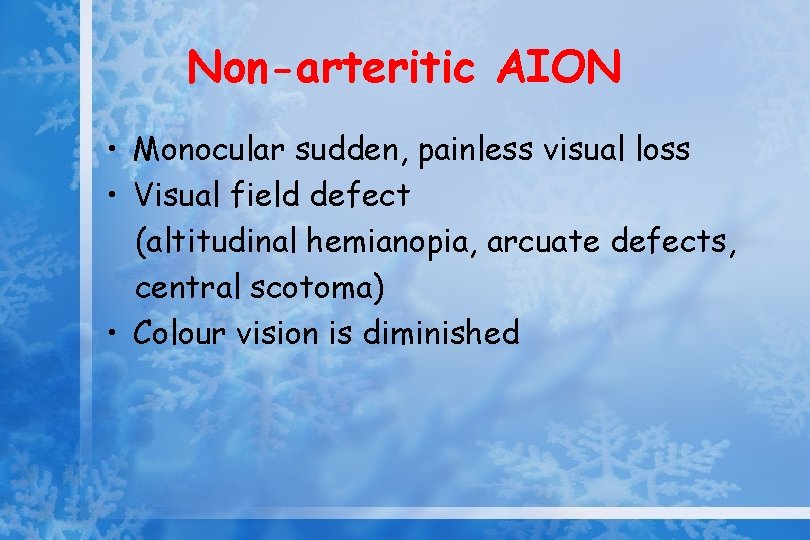
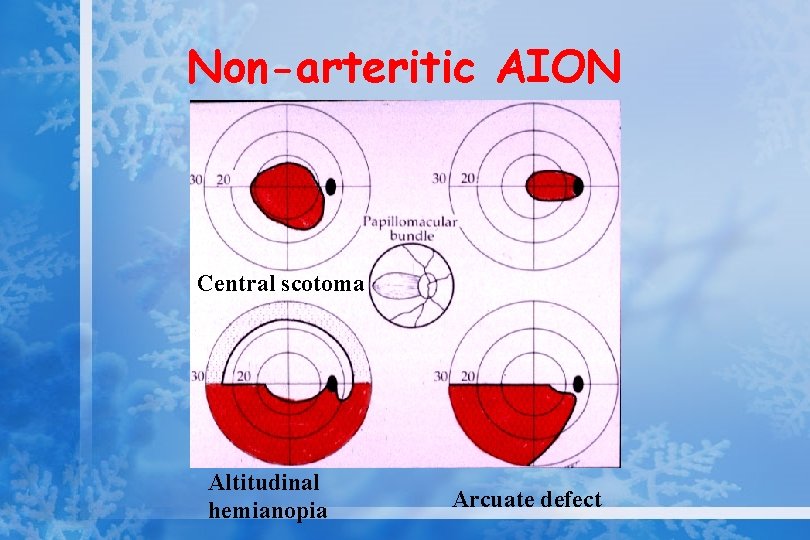
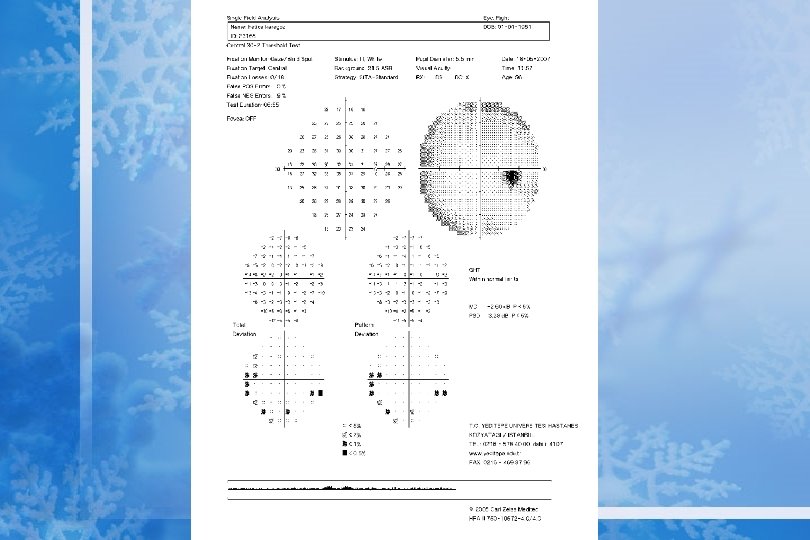
Non-arteritic AION • Monocular sudden, painless visual loss • Visual field defect (altitudinal hemianopia, arcuate defects, central scotoma) • Colour vision is diminished
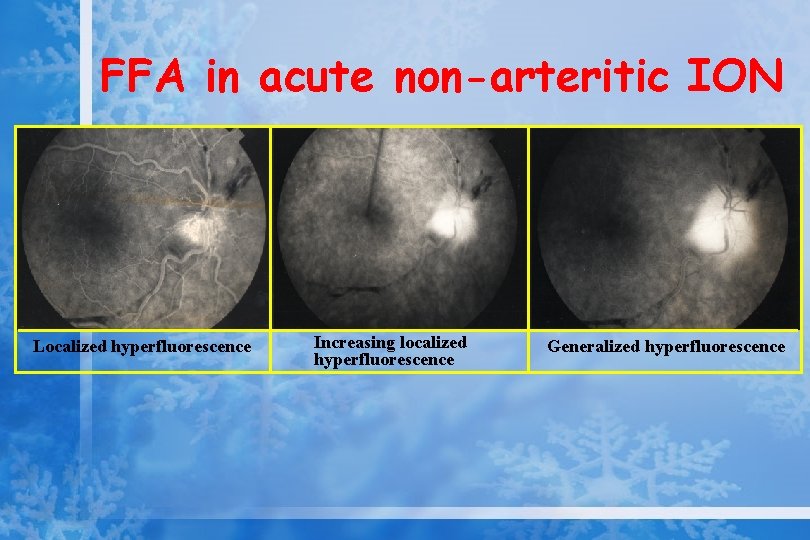
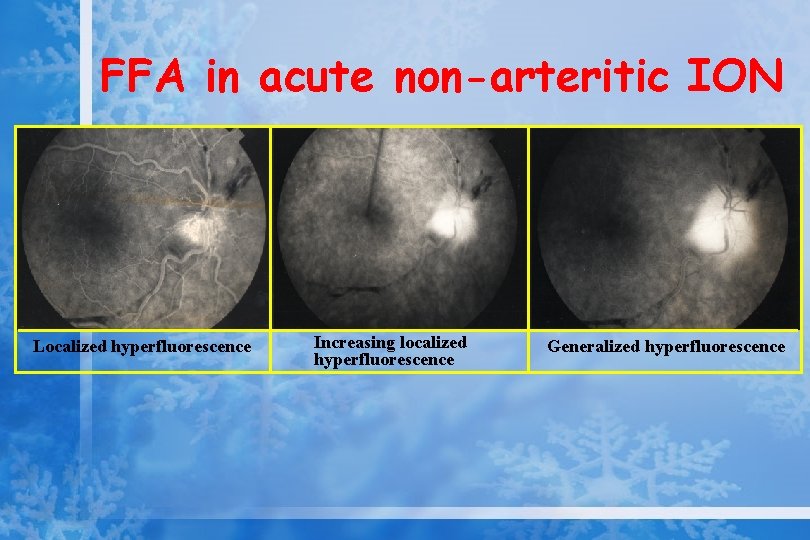
FFA in acute non-arteritic ION Localized hyperfluorescence Increasing localized hyperfluorescence Generalized hyperfluorescence
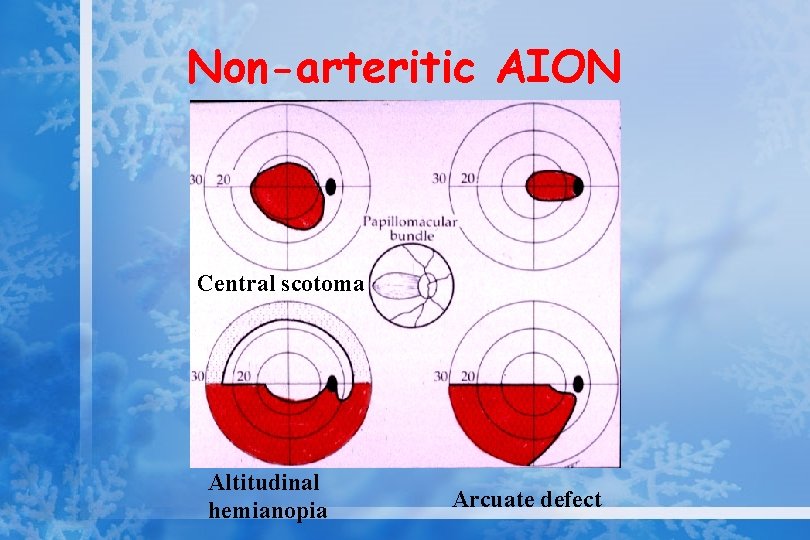
Non-arteritic AION Central scotoma Altitudinal hemianopia Arcuate defect
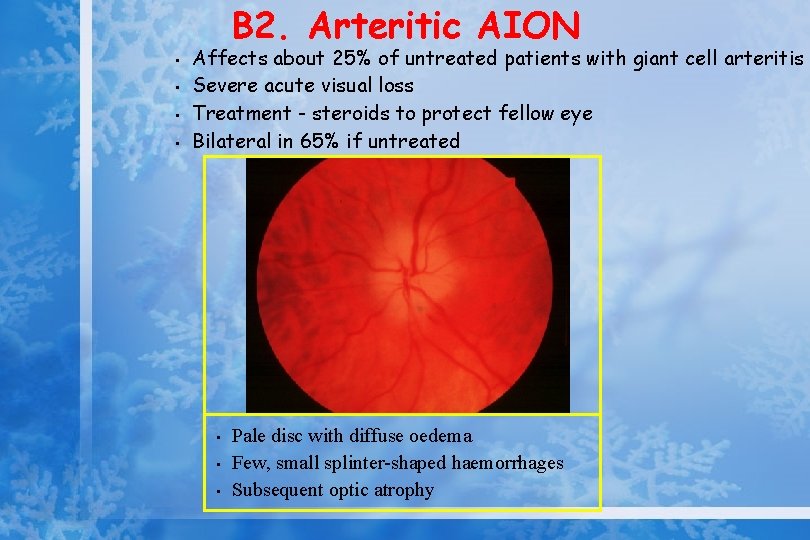
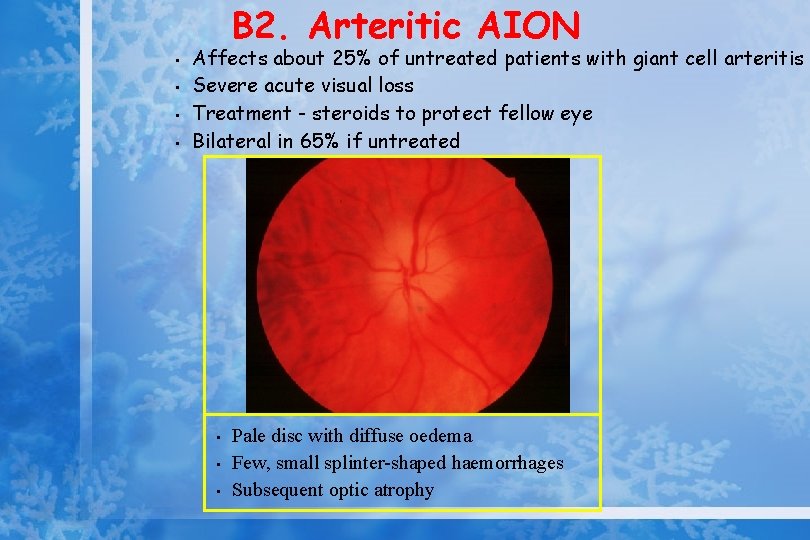
B 2. Arteritic AION • • Affects about 25% of untreated patients with giant cell arteritis Severe acute visual loss Treatment - steroids to protect fellow eye Bilateral in 65% if untreated • • • Pale disc with diffuse oedema Few, small splinter-shaped haemorrhages Subsequent optic atrophy
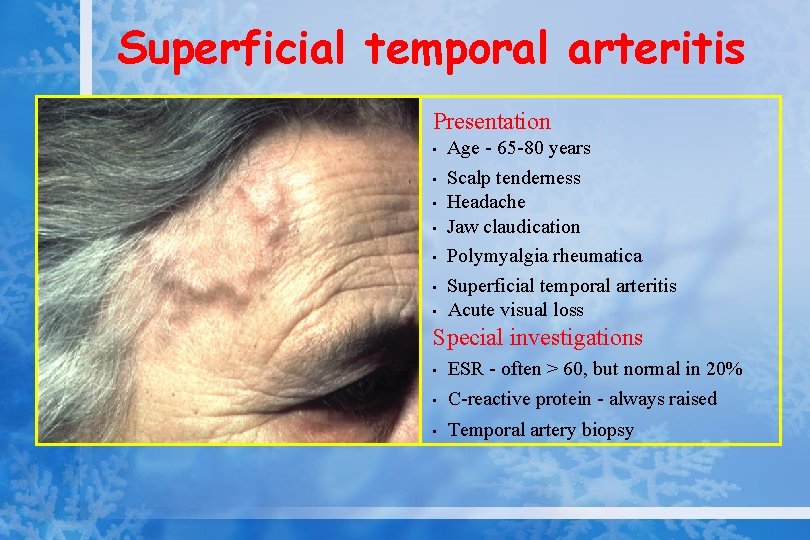
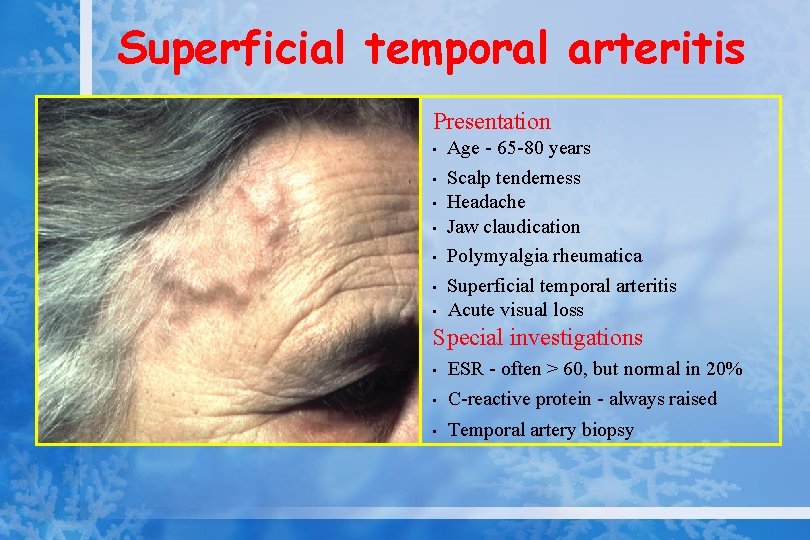
Superficial temporal arteritis Presentation • • Age - 65 -80 years Scalp tenderness Headache Jaw claudication Polymyalgia rheumatica Superficial temporal arteritis Acute visual loss Special investigations • ESR - often > 60, but normal in 20% C-reactive protein - always raised • Temporal artery biopsy •
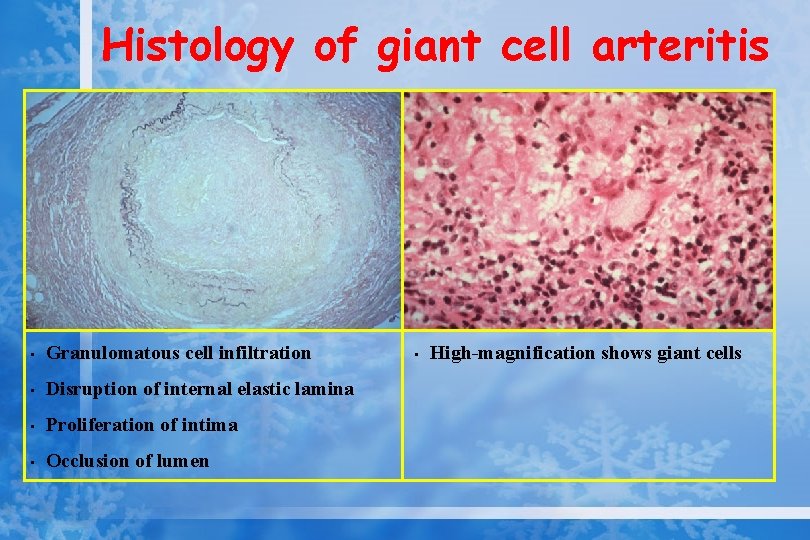
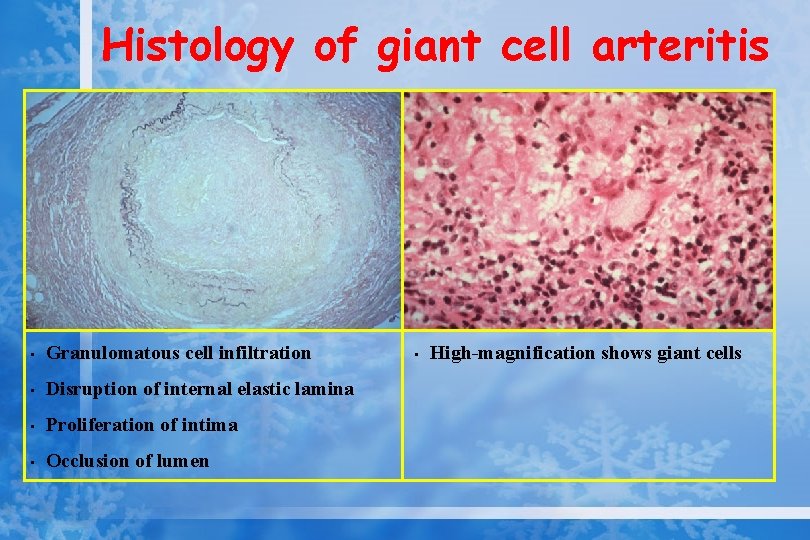
Histology of giant cell arteritis • Granulomatous cell infiltration • Disruption of internal elastic lamina • Proliferation of intima • Occlusion of lumen • High-magnification shows giant cells
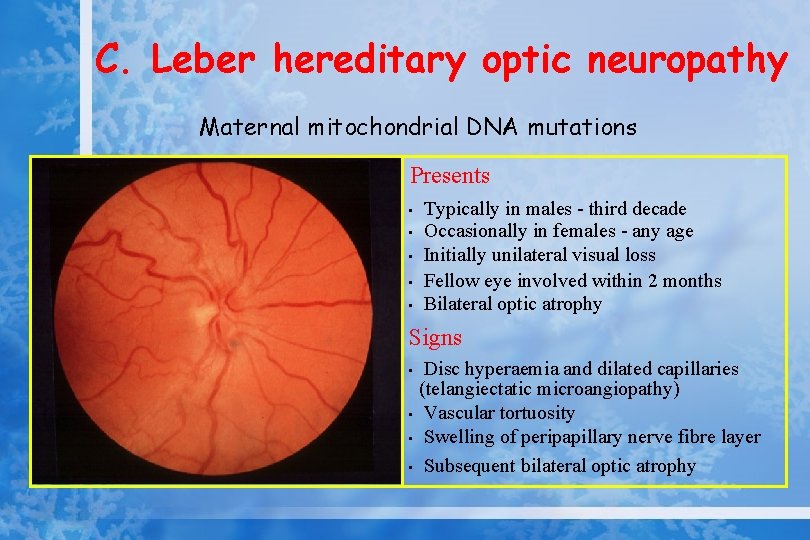
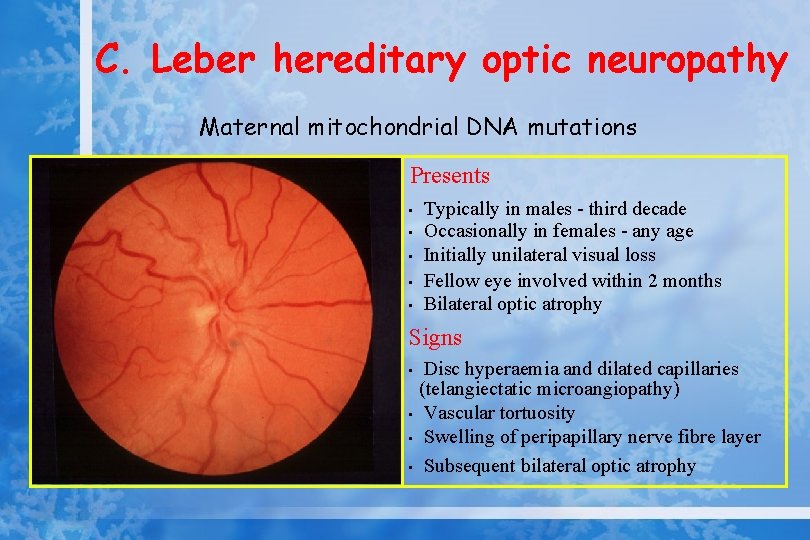
C. Leber hereditary optic neuropathy Maternal mitochondrial DNA mutations Presents • • • Typically in males - third decade Occasionally in females - any age Initially unilateral visual loss Fellow eye involved within 2 months Bilateral optic atrophy Signs Disc hyperaemia and dilated capillaries (telangiectatic microangiopathy) • Vascular tortuosity • Swelling of peripapillary nerve fibre layer • Subsequent bilateral optic atrophy •
D. Toxic optic neuropathies • Toxic amblyopia -heavy drinkers and pipe smokers -slowly progressive, bilateral, visual impairment -loss of colour vision -centrocaecal scotoma -treatment: 1000 units hydroxycobalamin 10 wks, abstain from drinking-smoking
Toxic optic neuropathies • Ethambutol-ınduced optic neuropathy -sudden, dramatic visual loss -impairment colour perception -visual field temporal defect - drug is stopped (recovery time-12 mo)
E. Post-infectious optic neuritis • • • Acute papillitis Measles, mumps, chickenpox, immunization Acute severe visual loss in both eyes Headache, ataxia Treatment; unnecessary (spontaneous recovery) IV steroids for dramatic improvement
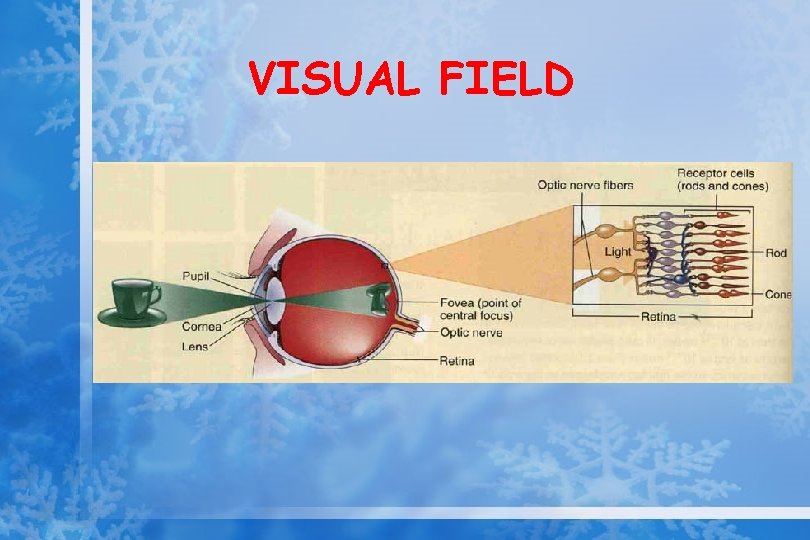
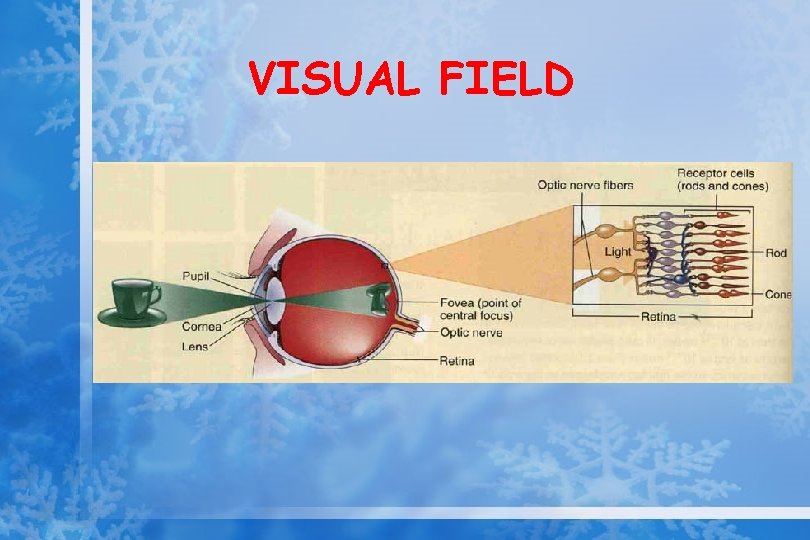
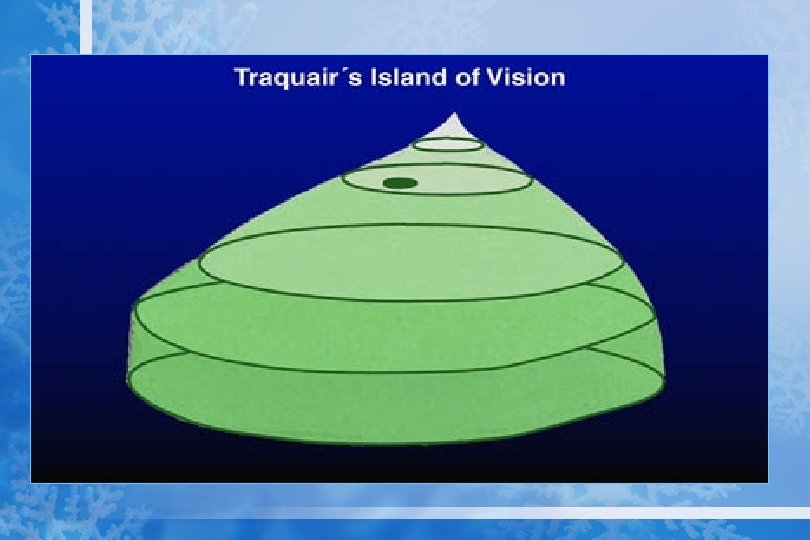
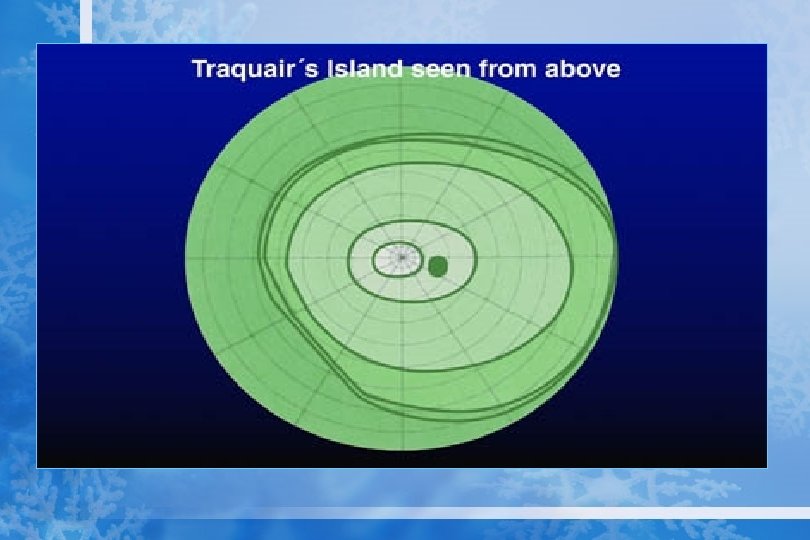
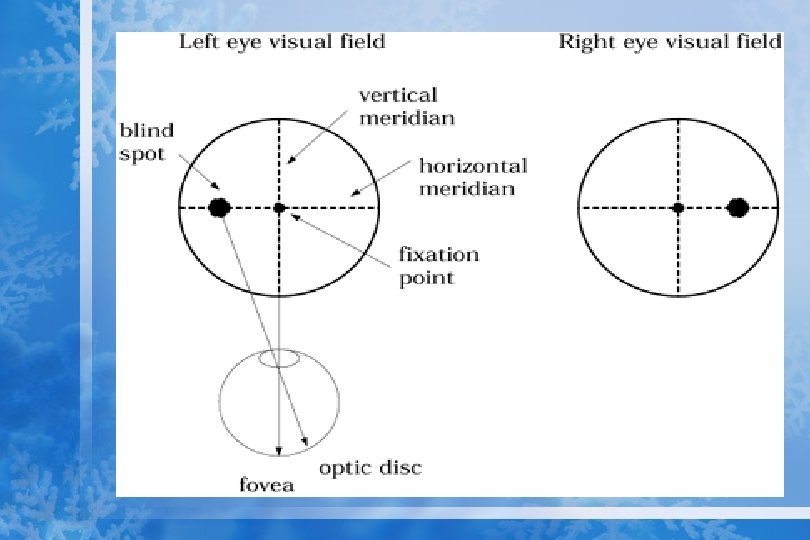
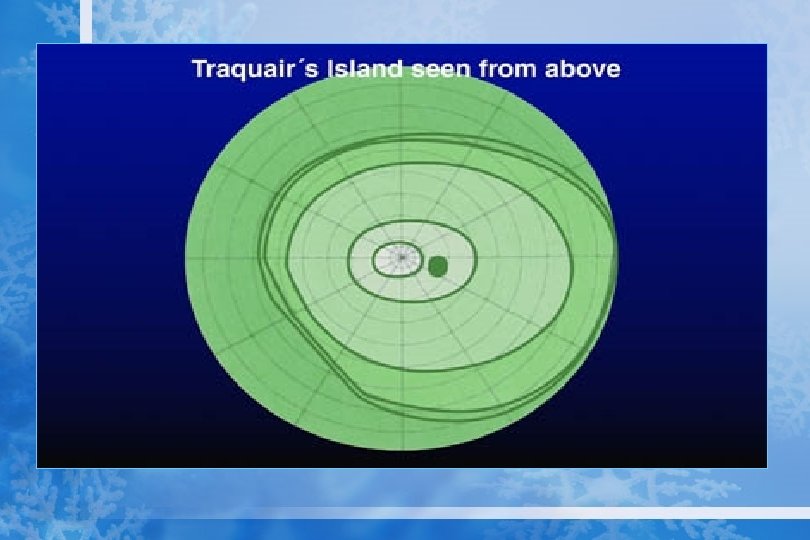
VISUAL FIELD
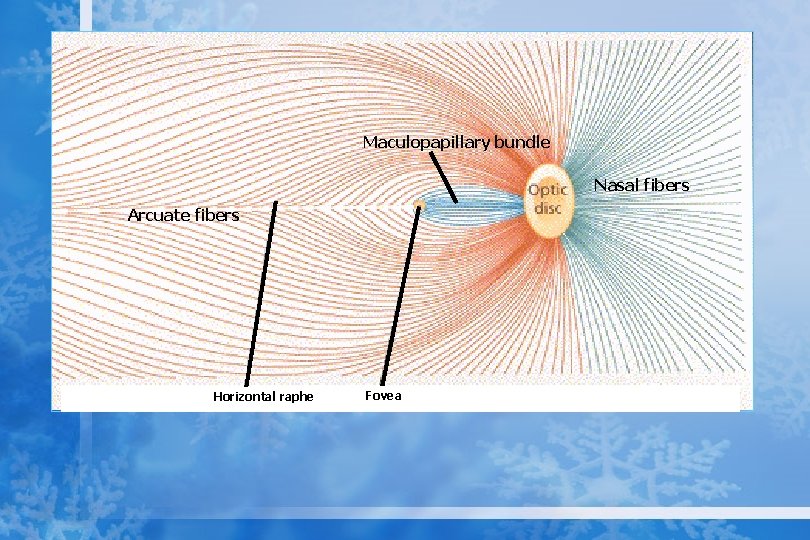
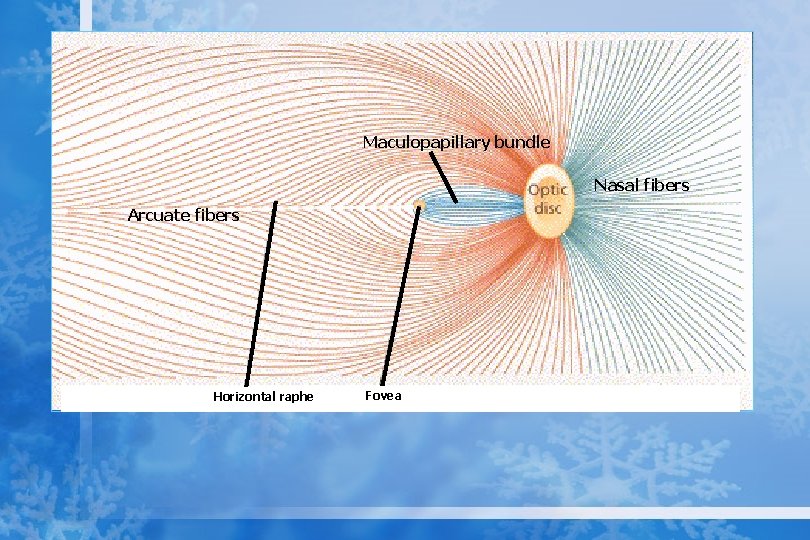
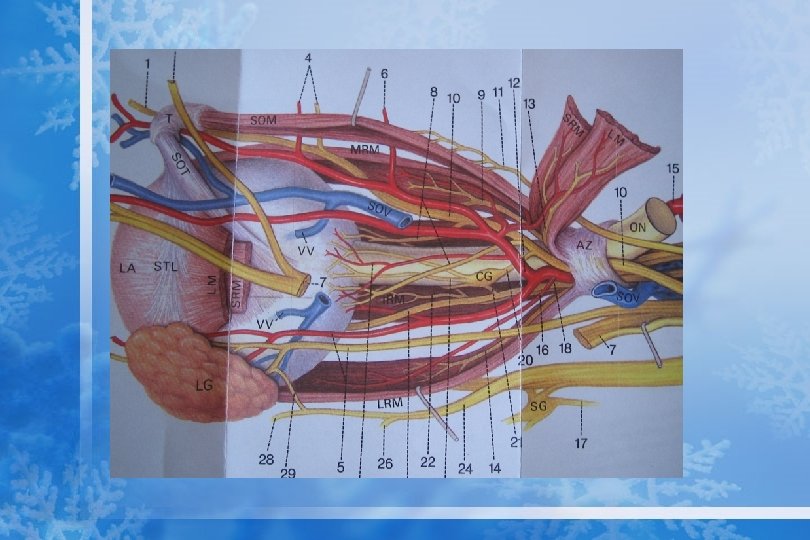
Maculopapillary bundle Nasal fibers Arcuate fibers Horizontal raphe Fovea
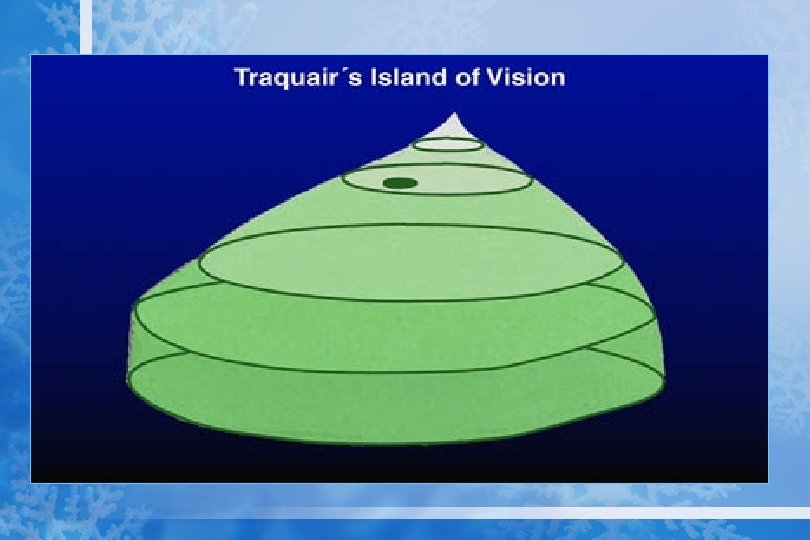
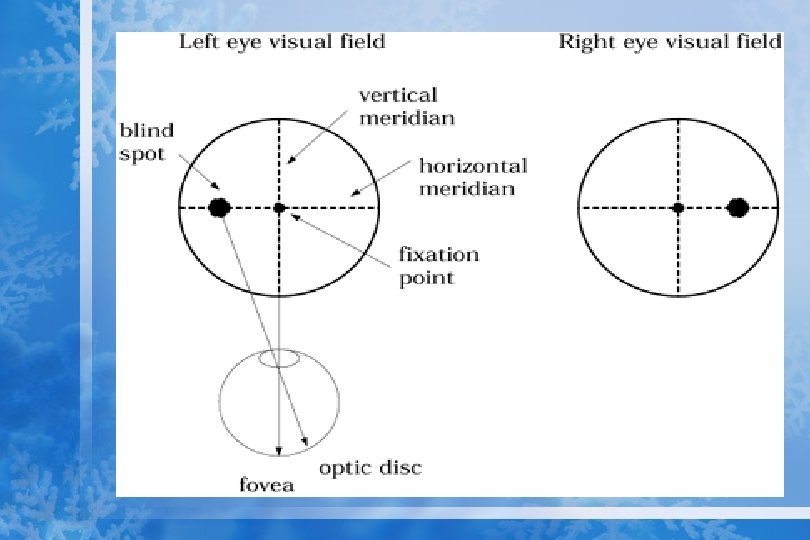
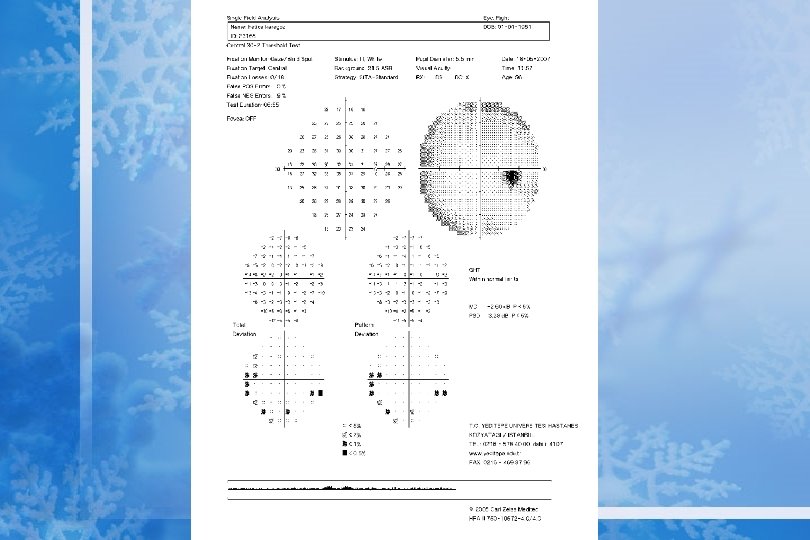
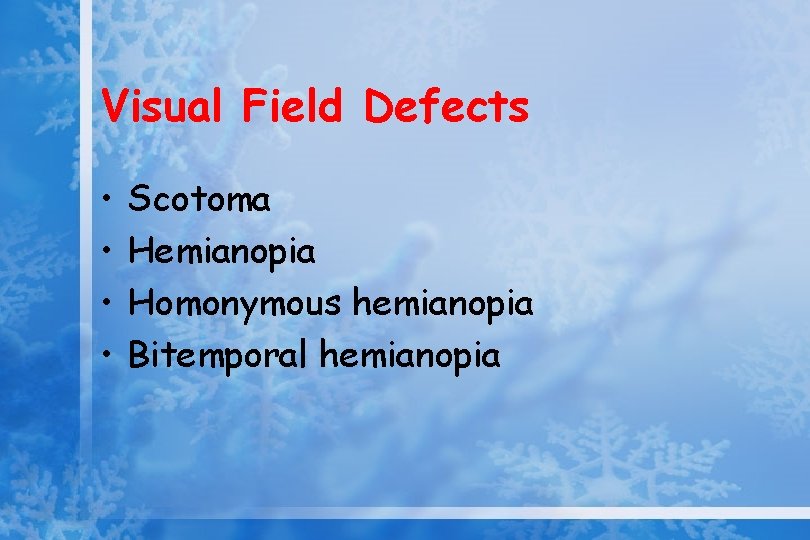
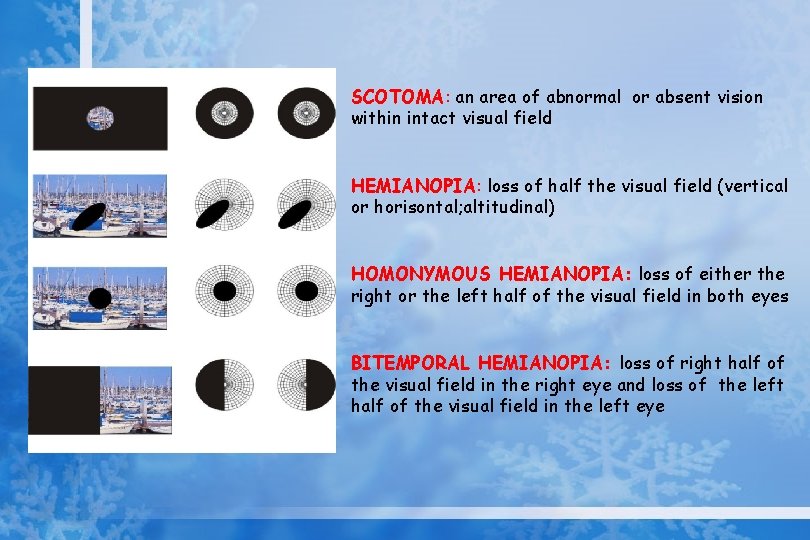
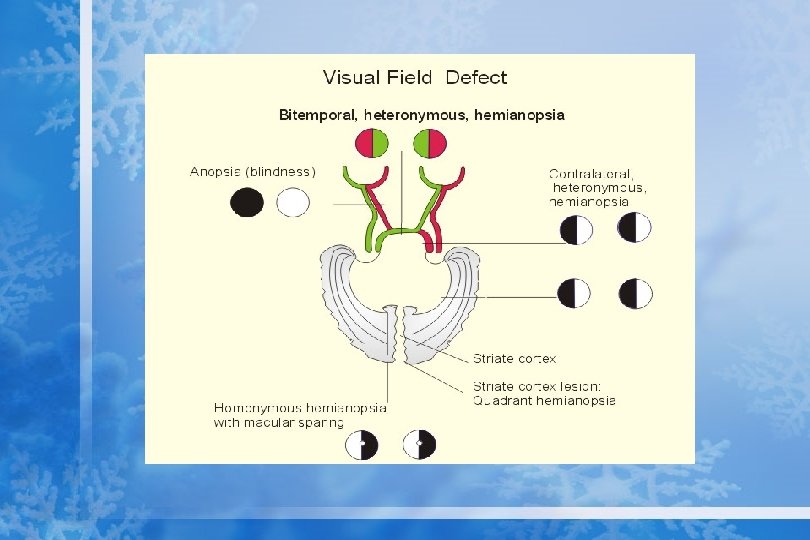
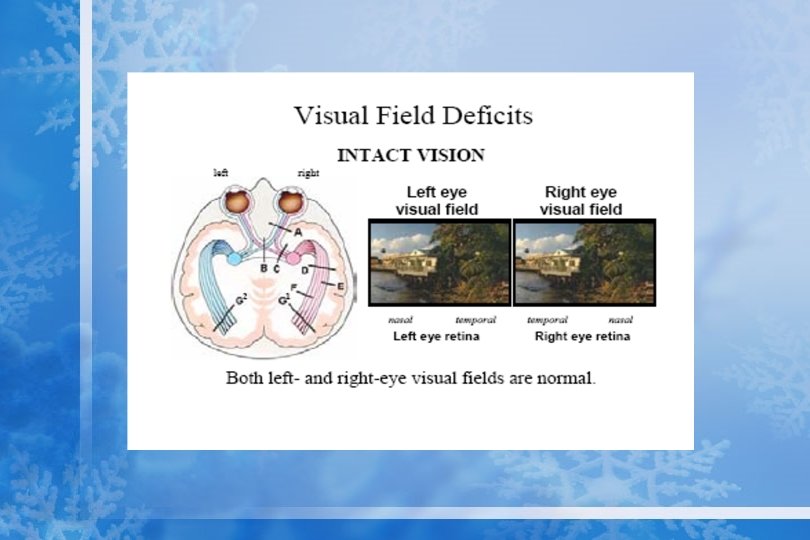
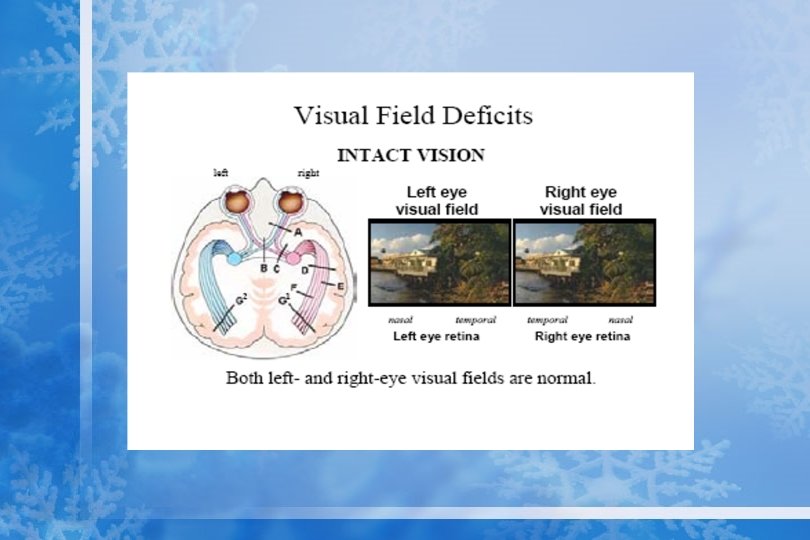
Visual Field Defects • • Scotoma Hemianopia Homonymous hemianopia Bitemporal hemianopia
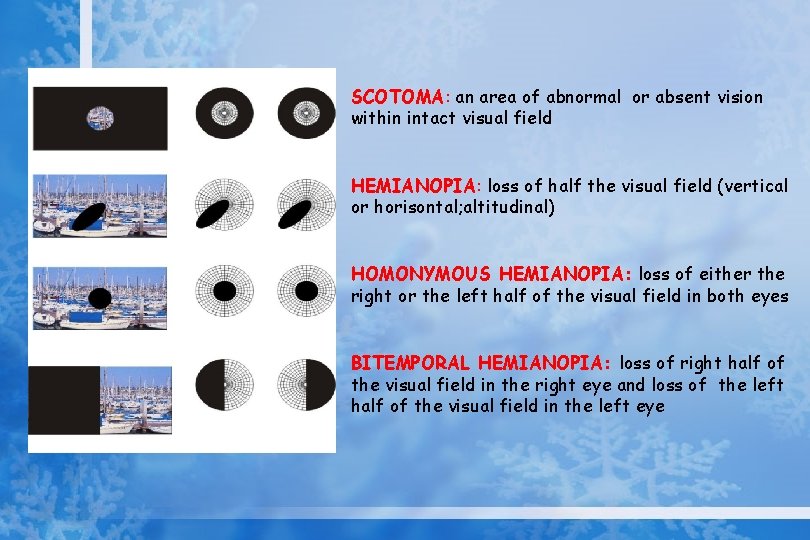
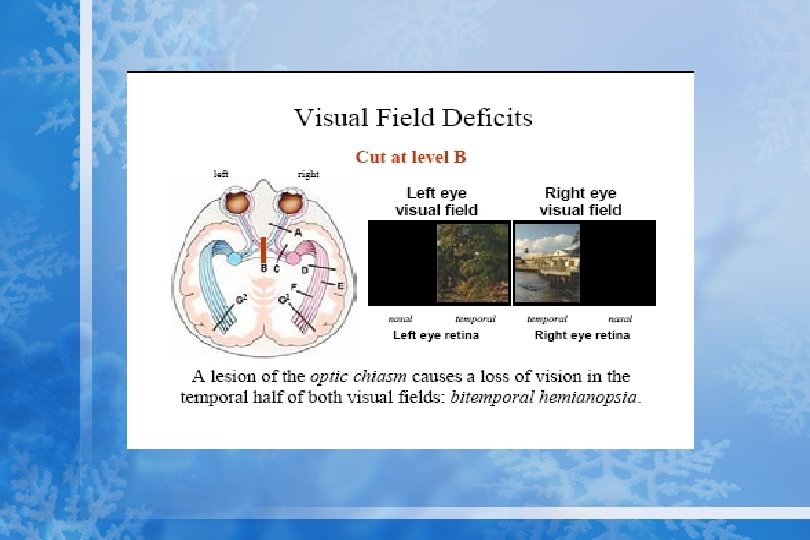
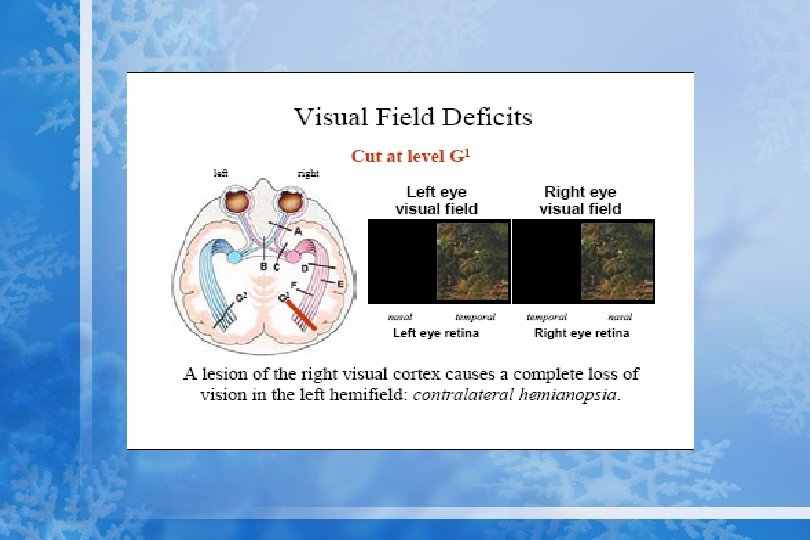
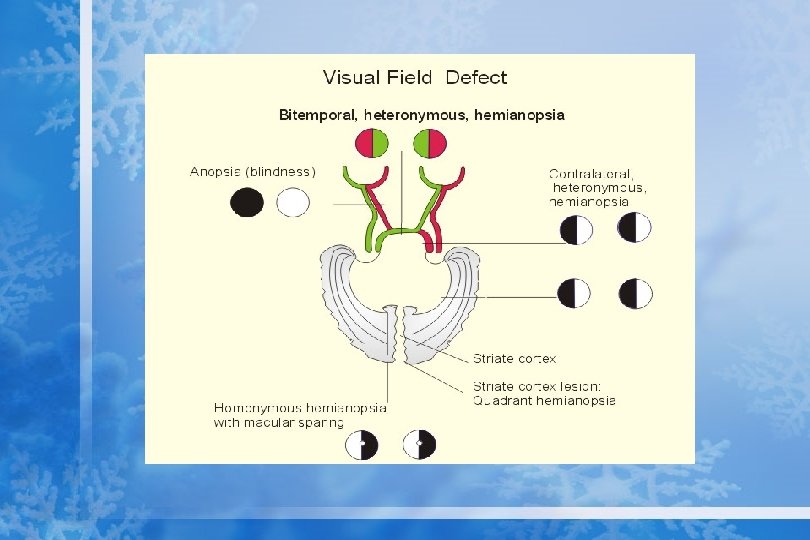
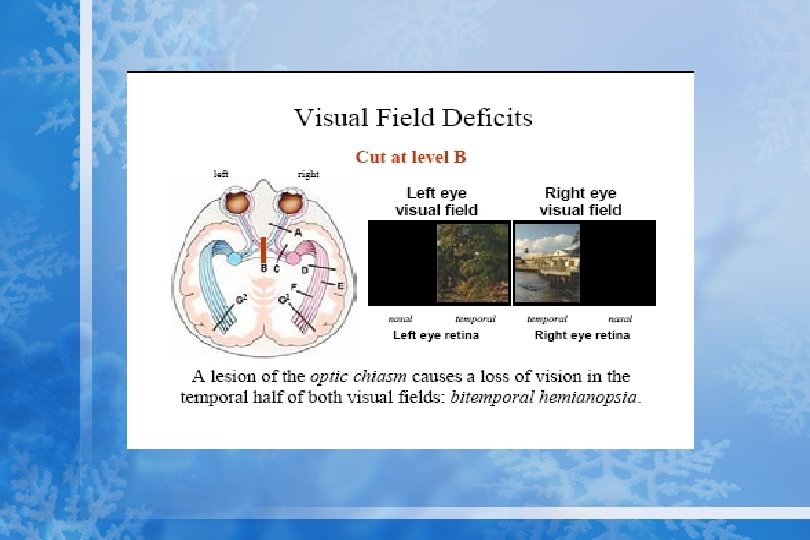
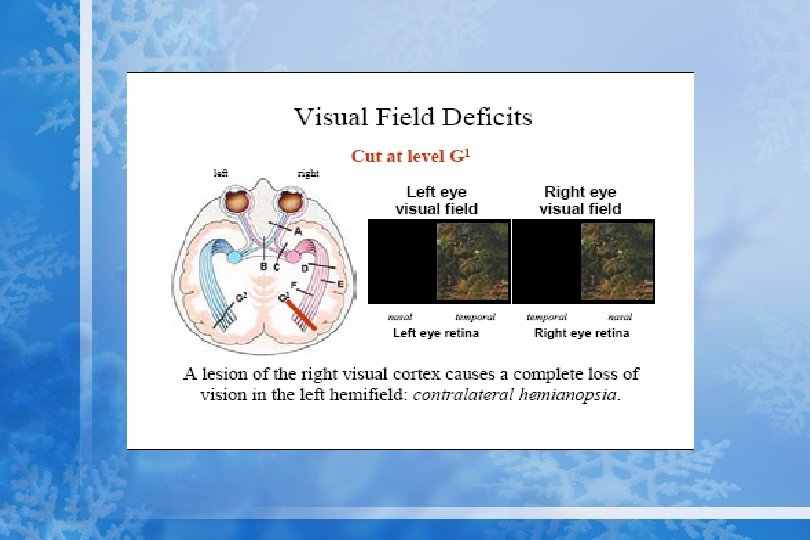
SCOTOMA: an area of abnormal or absent vision within intact visual field HEMIANOPIA: loss of half the visual field (vertical or horisontal; altitudinal) HOMONYMOUS HEMIANOPIA: loss of either the right or the left half of the visual field in both eyes BITEMPORAL HEMIANOPIA: loss of right half of the visual field in the right eye and loss of the left half of the visual field in the left eye
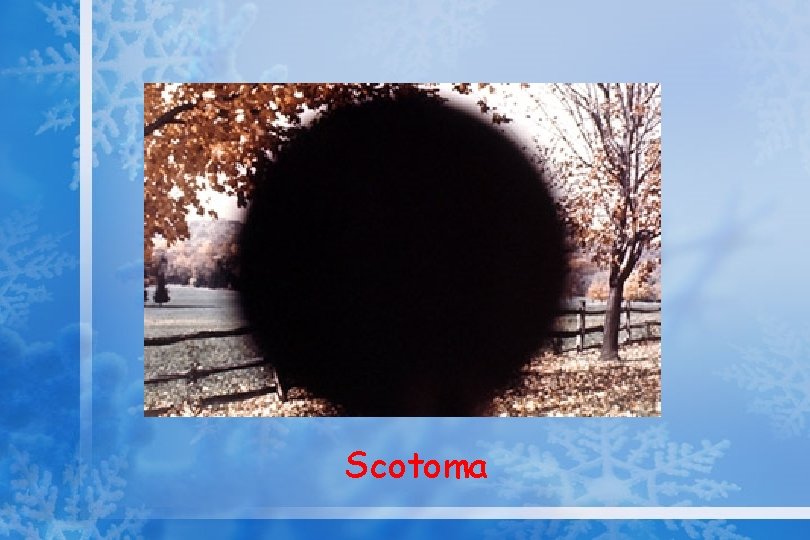
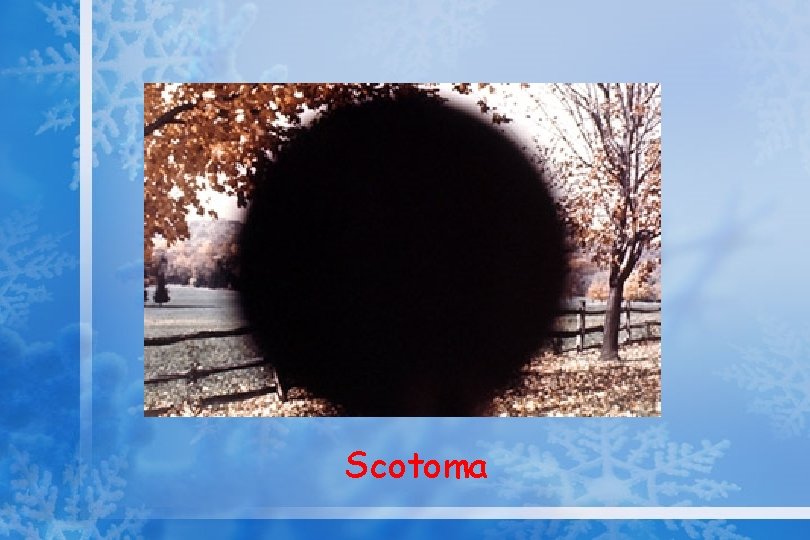
Scotoma
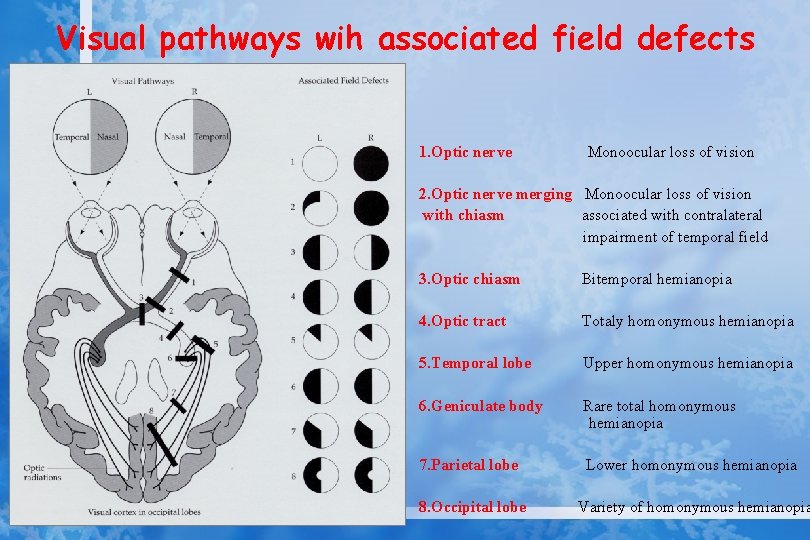
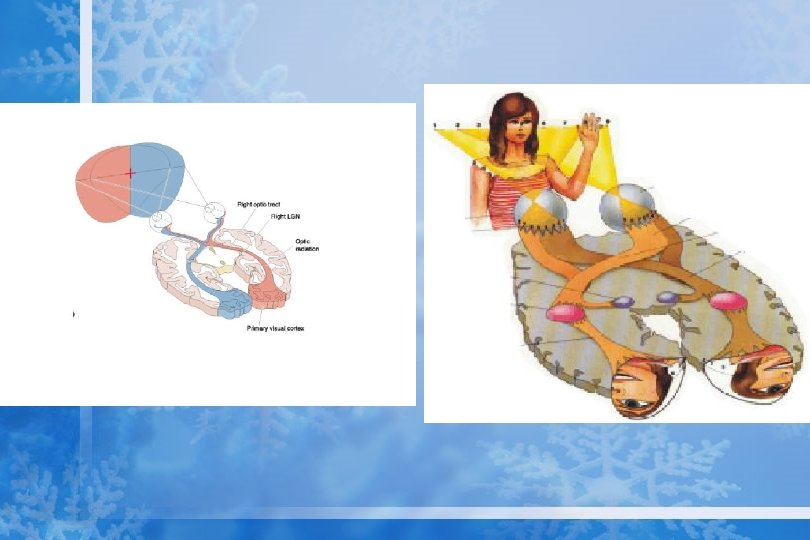
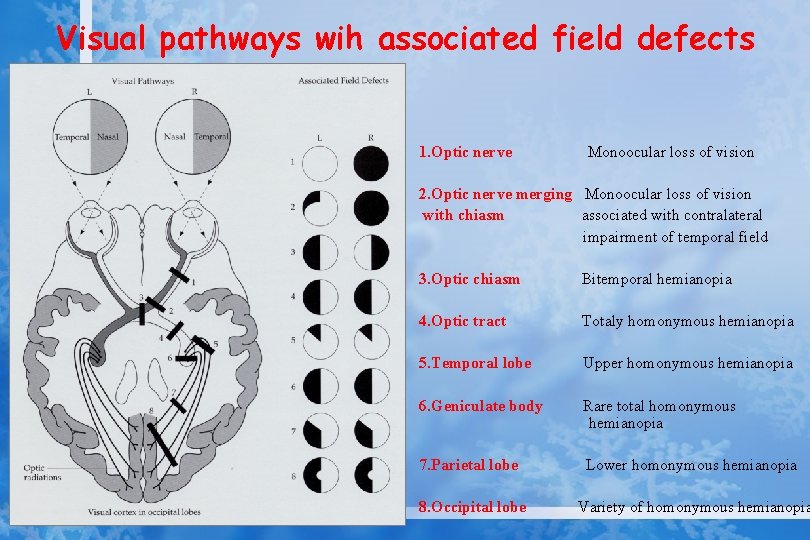
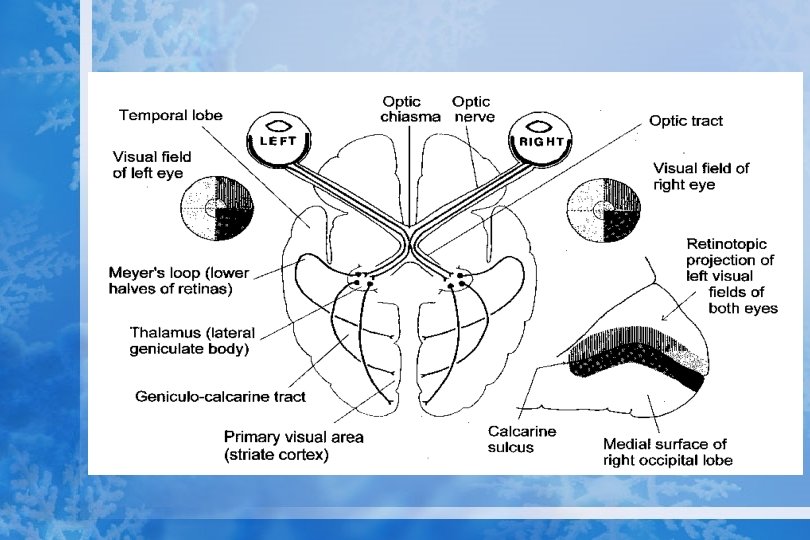
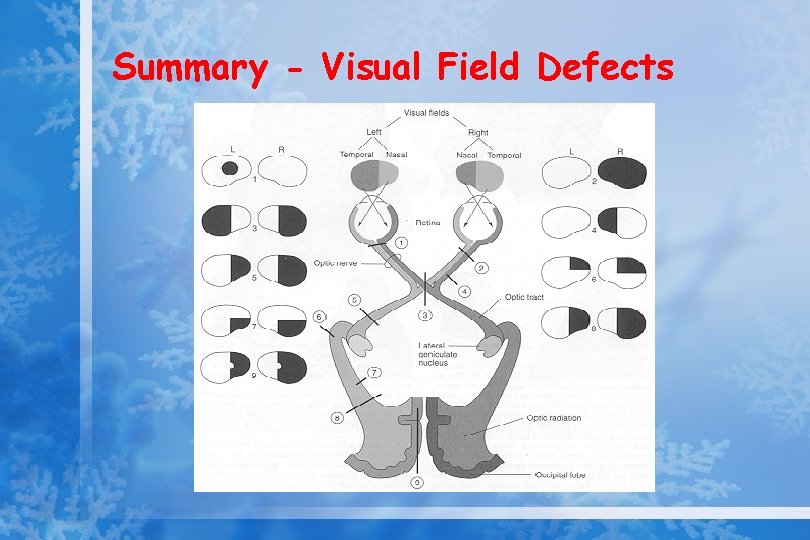
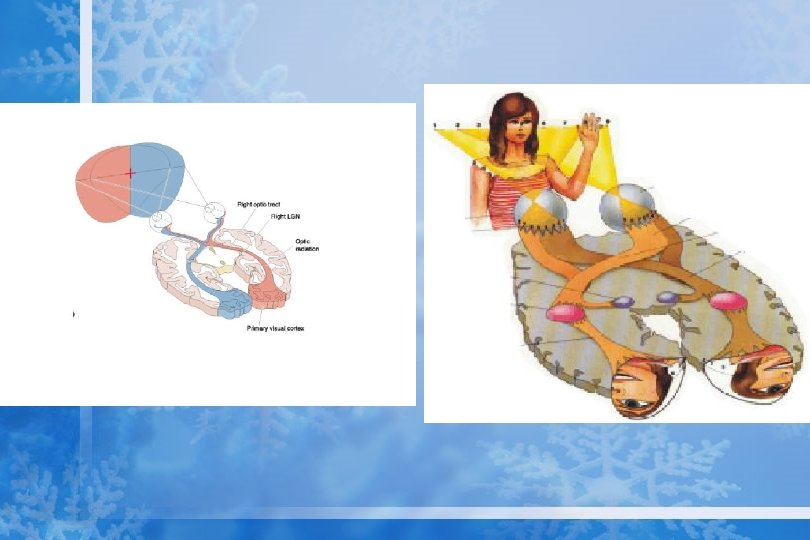
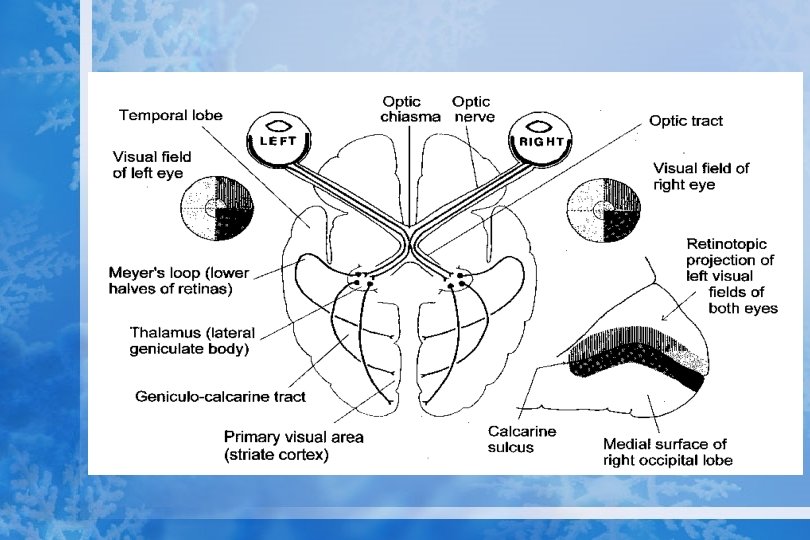
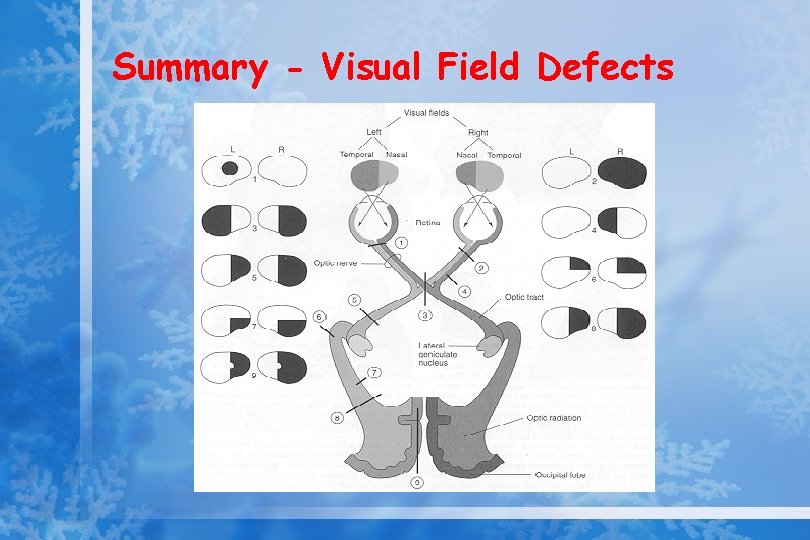
Visual pathways wih associated field defects 1. Optic nerve Monoocular loss of vision 2. Optic nerve merging Monoocular loss of vision with chiasm associated with contralateral impairment of temporal field 3. Optic chiasm Bitemporal hemianopia 4. Optic tract Totaly homonymous hemianopia 5. Temporal lobe Upper homonymous hemianopia 6. Geniculate body Rare total homonymous hemianopia 7. Parietal lobe Lower homonymous hemianopia 8. Occipital lobe Variety of homonymous hemianopia

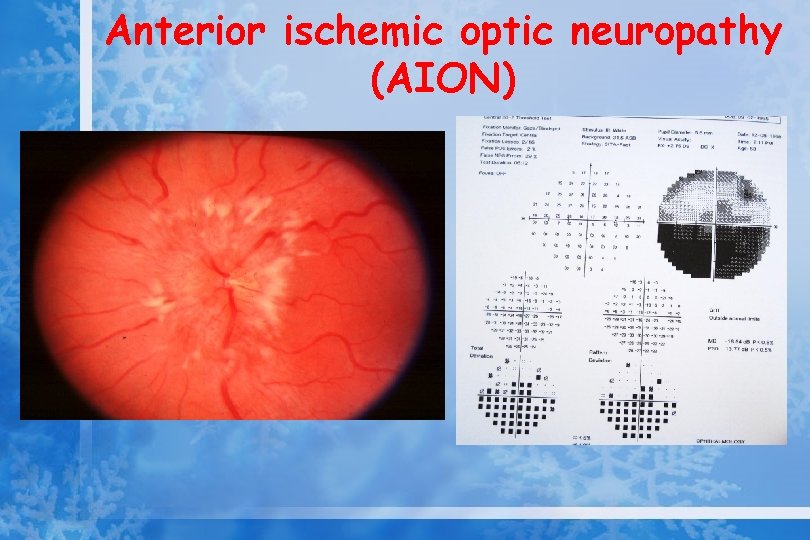
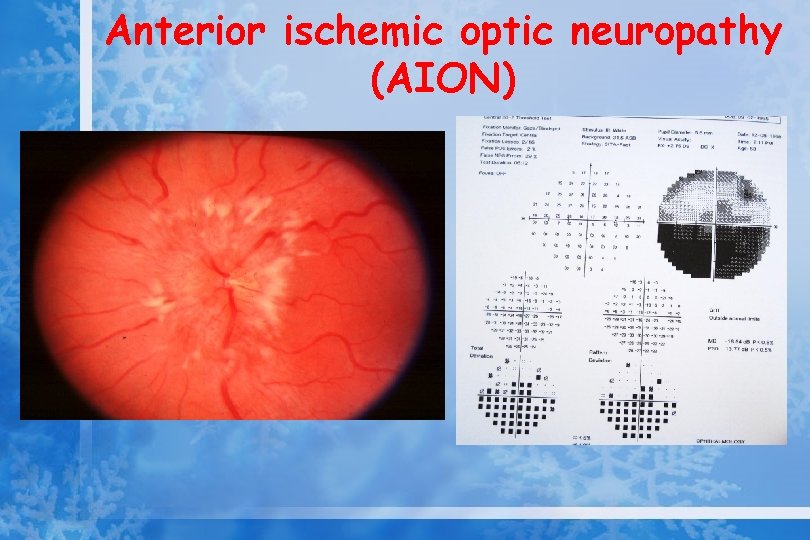
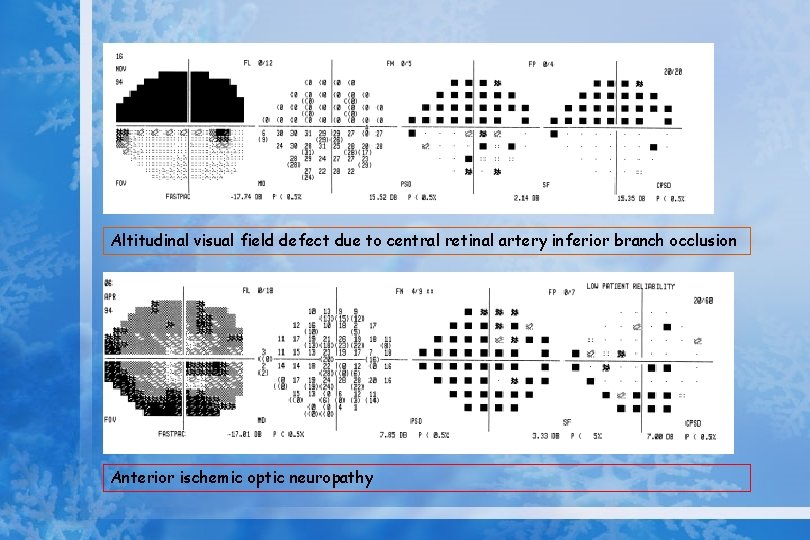
Anterior ischemic optic neuropathy (AION)
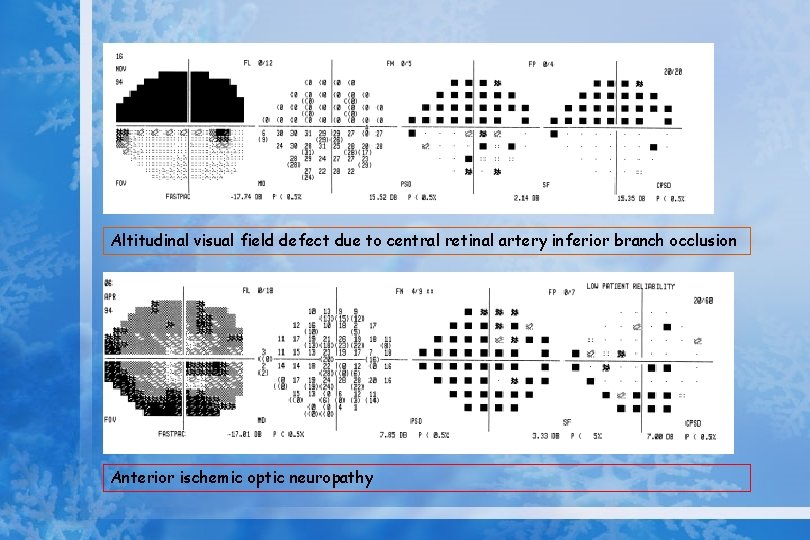
Altitudinal visual field defect due to central retinal artery inferior branch occlusion Anterior ischemic optic neuropathy
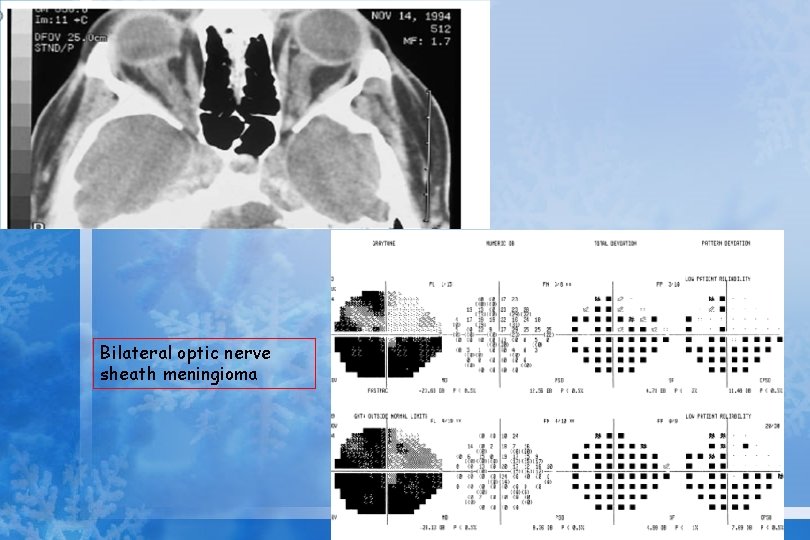
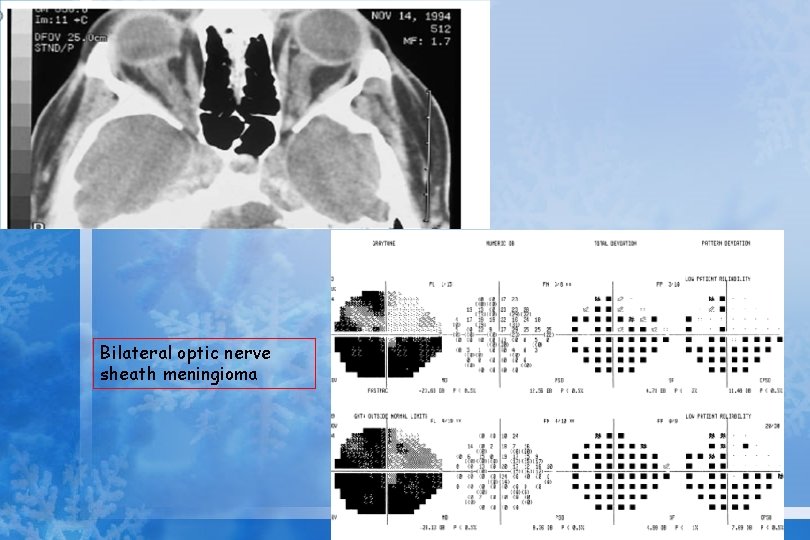
Bilateral optic nerve sheath meningioma
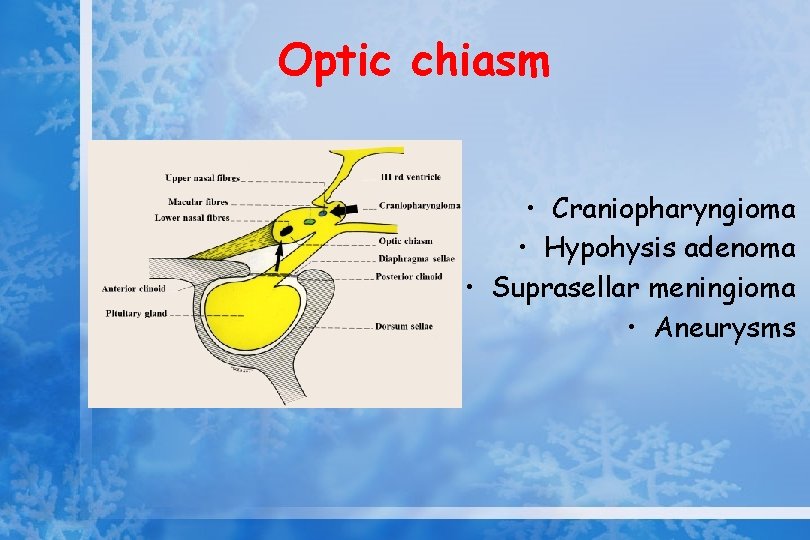
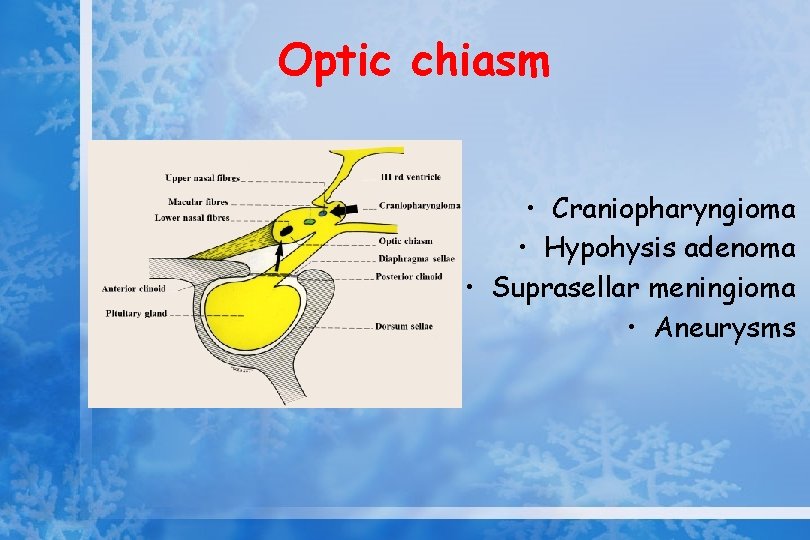
Optic chiasm • Craniopharyngioma • Hypohysis adenoma • Suprasellar meningioma • Aneurysms
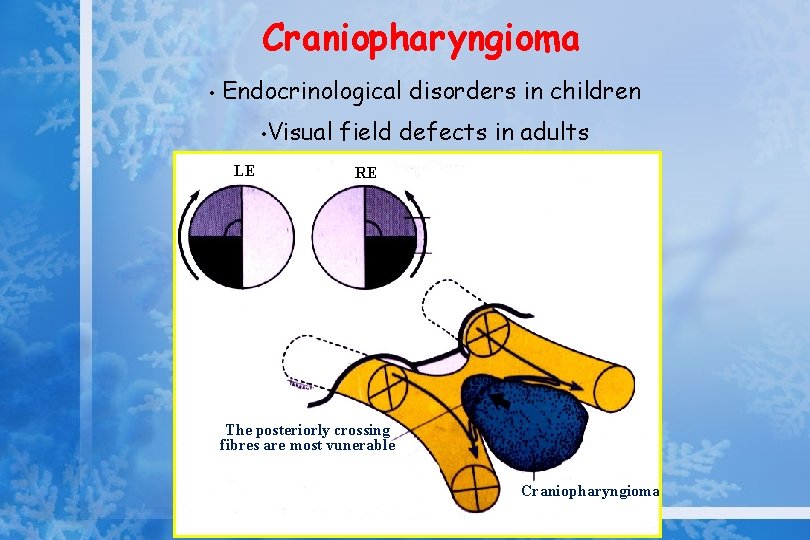
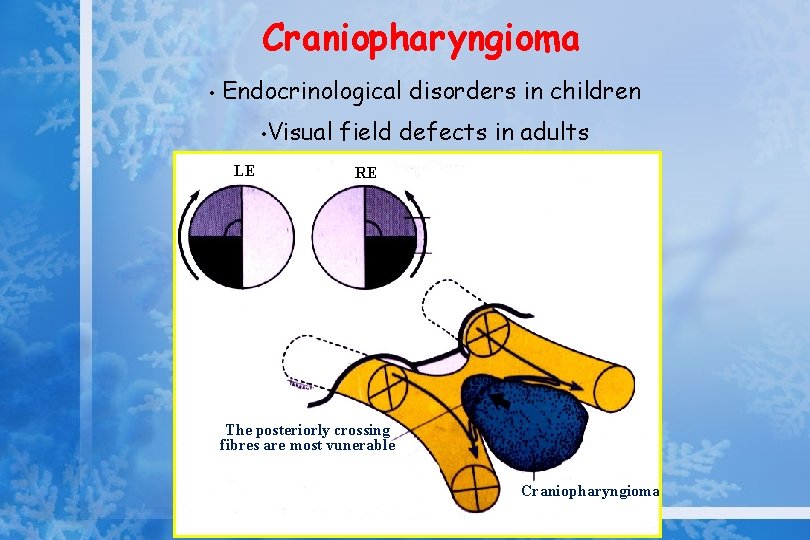
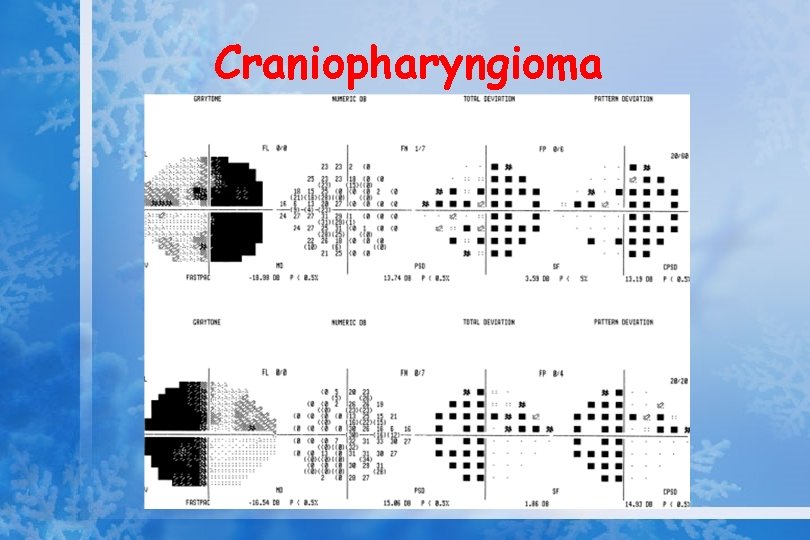
Craniopharyngioma • Endocrinological disorders in children • LE Visual field defects in adults RE CF HM The posteriorly crossing fibres are most vunerable Craniopharyngioma
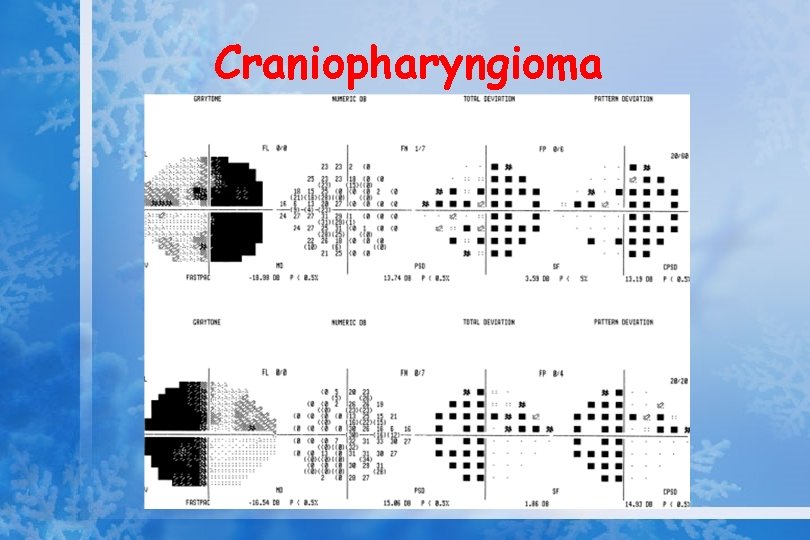
Craniopharyngioma
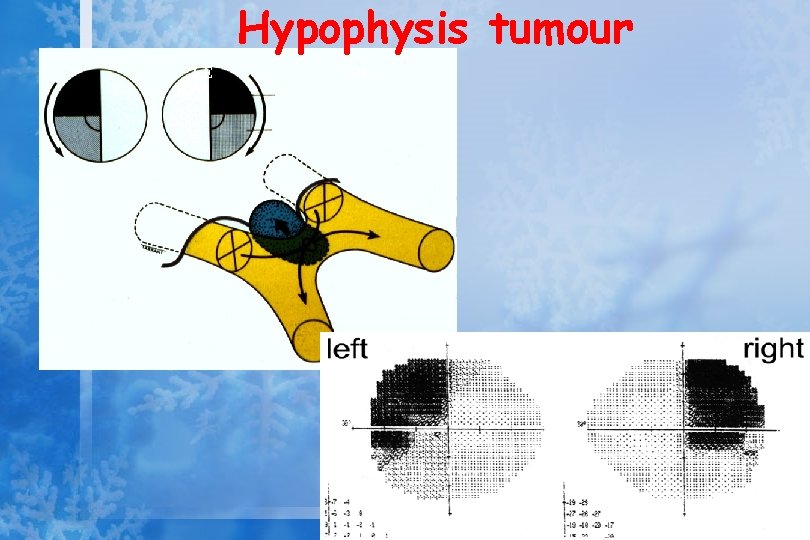
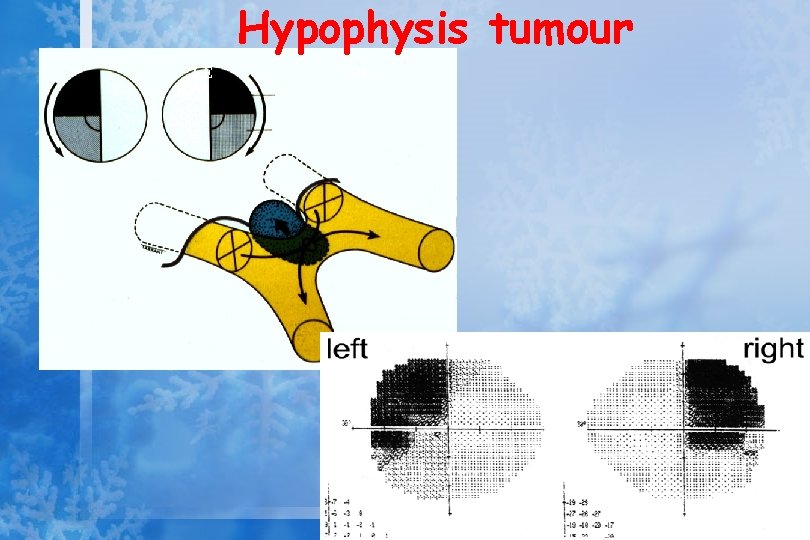
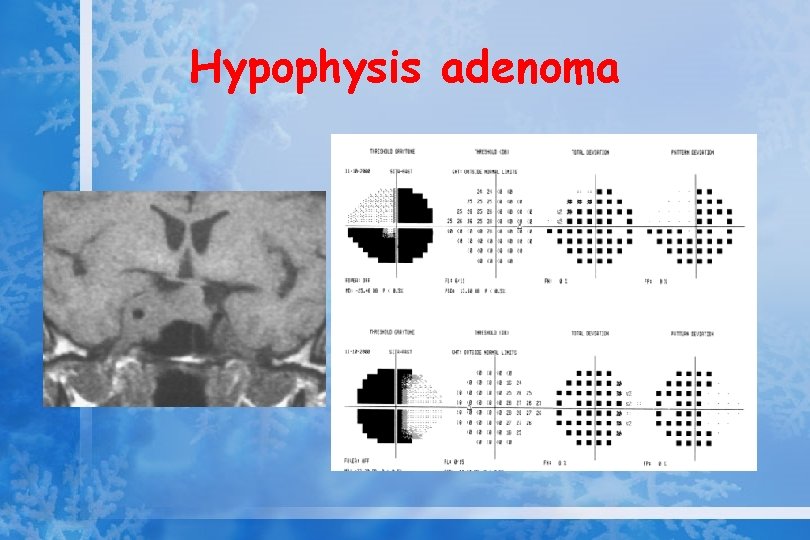
Hypophysis tumour LE RE Decussating fibres are most vunerable
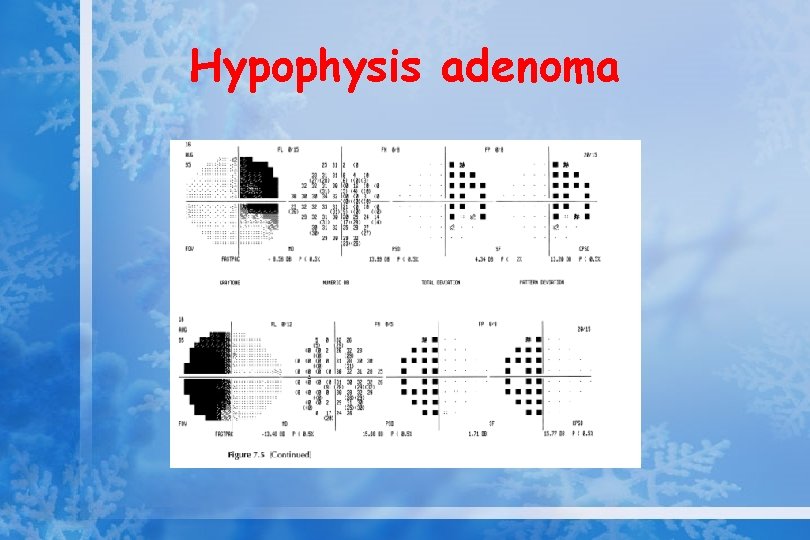
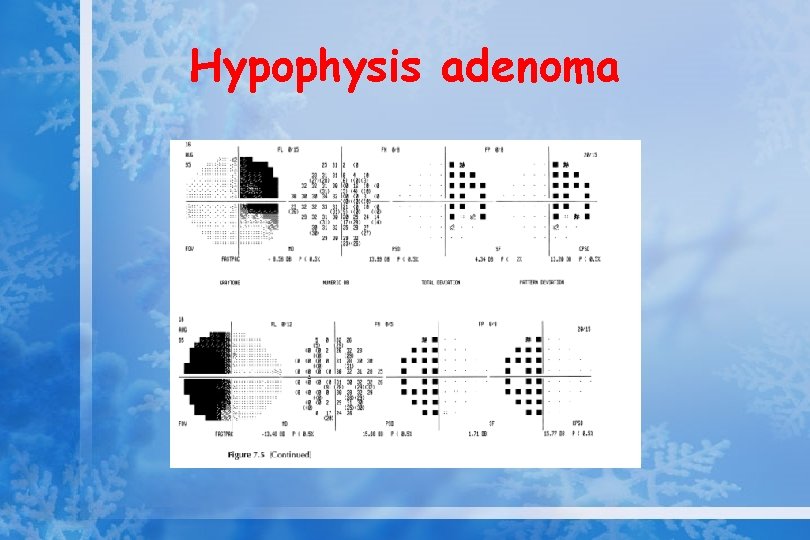
Hypophysis adenoma
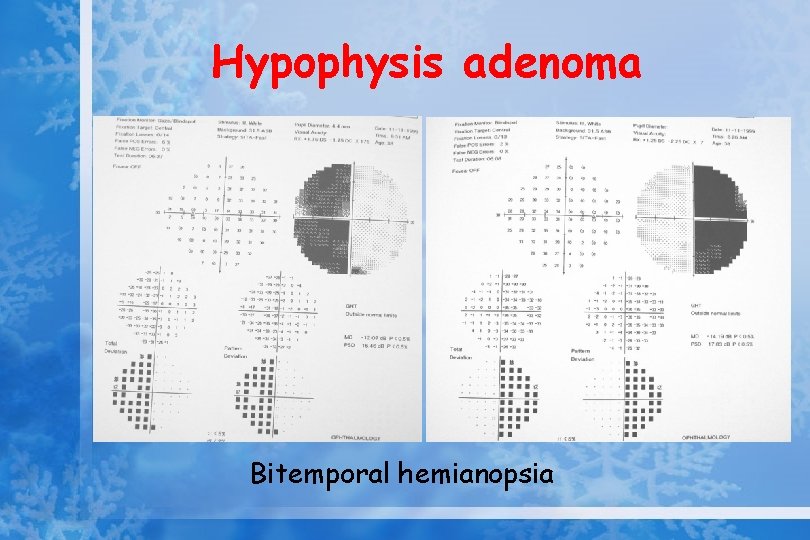
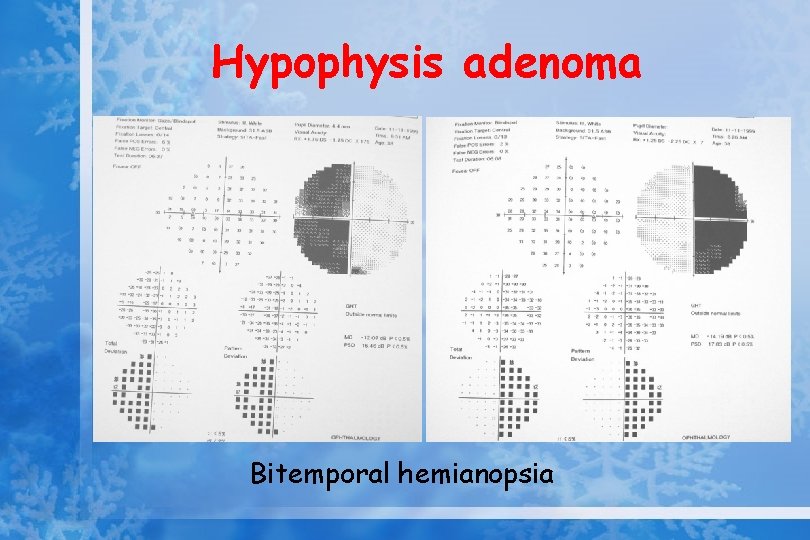
Hypophysis adenoma Bitemporal hemianopsia
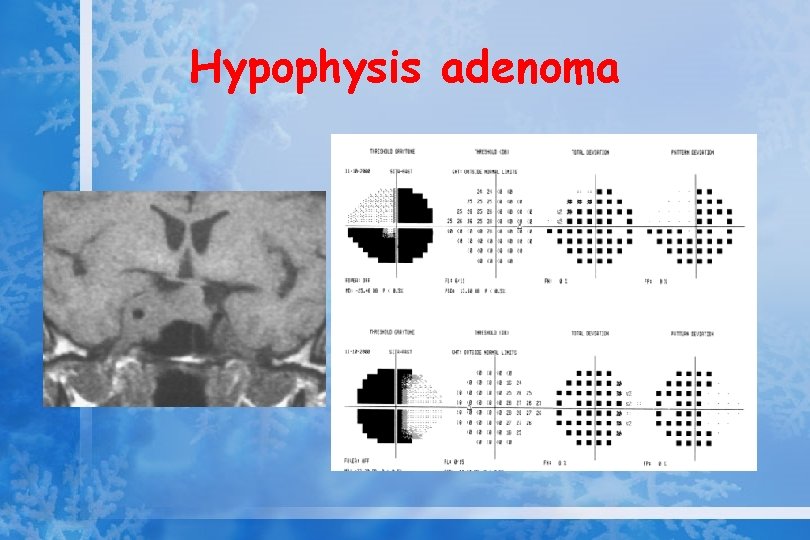
Hypophysis adenoma
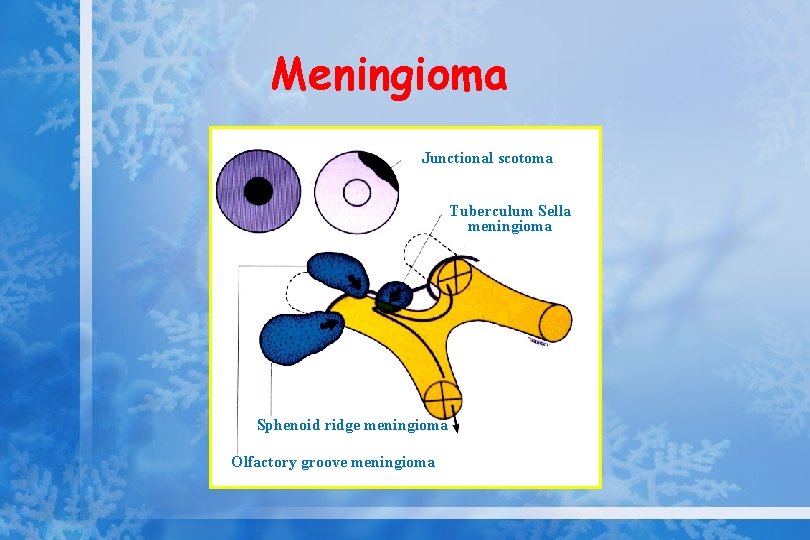
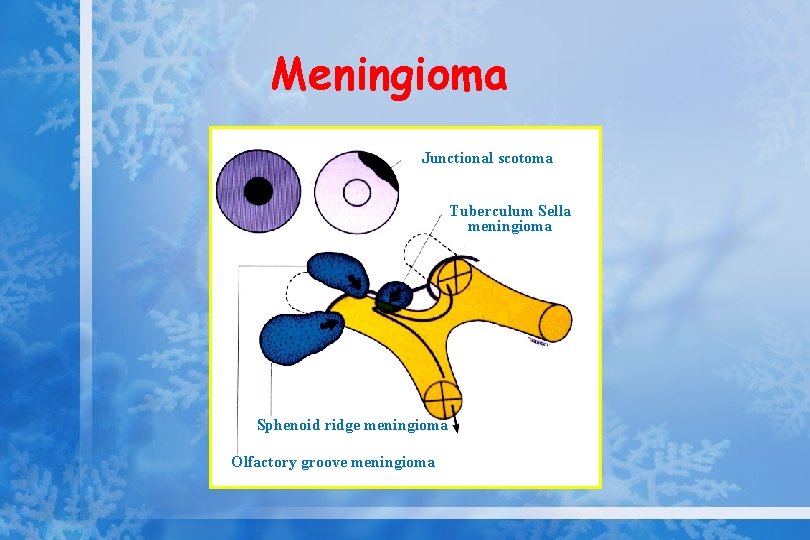
Meningioma LE RE Junctional scotoma Tuberculum Sella meningioma Sphenoid ridge meningioma Olfactory groove meningioma
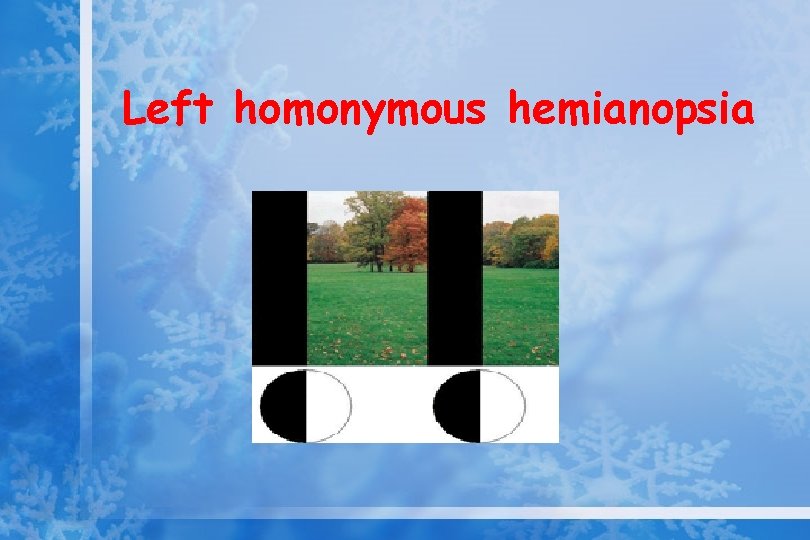
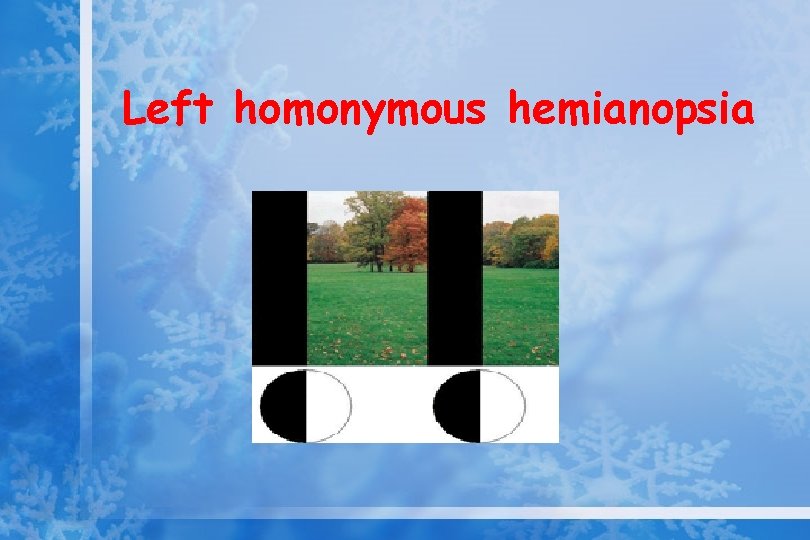
Left homonymous hemianopsia
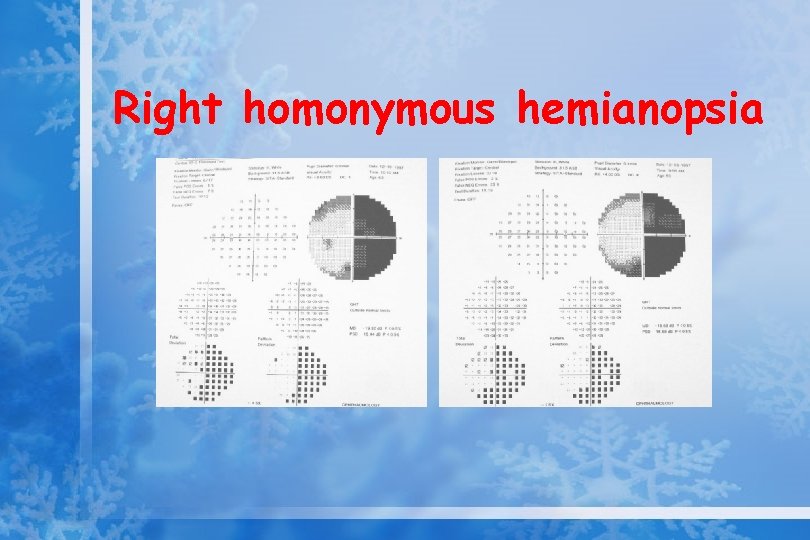
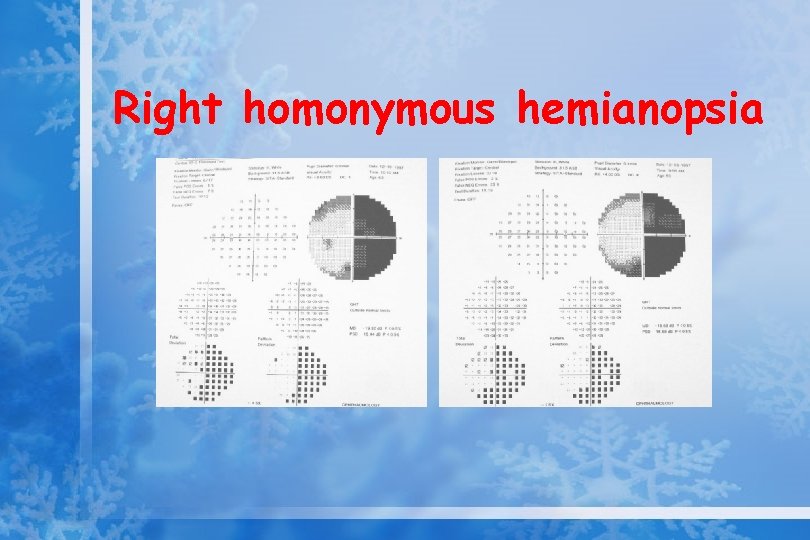
Right homonymous hemianopsia
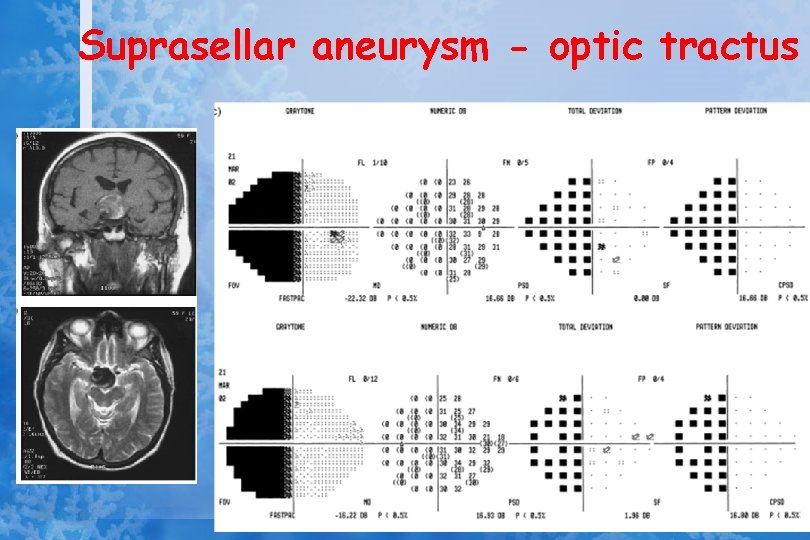
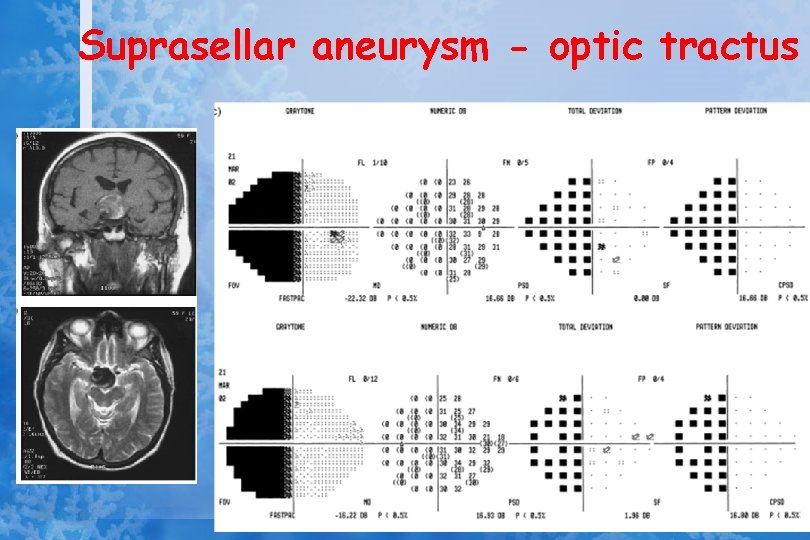
Suprasellar aneurysm - optic tractus
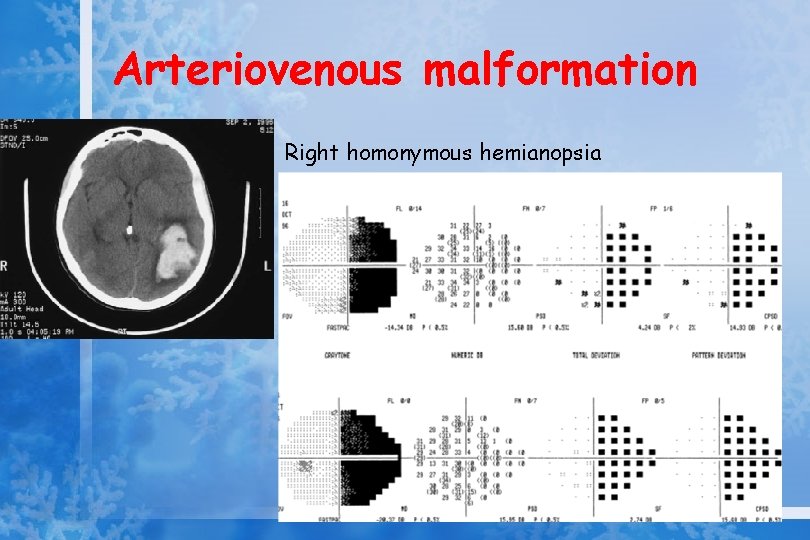
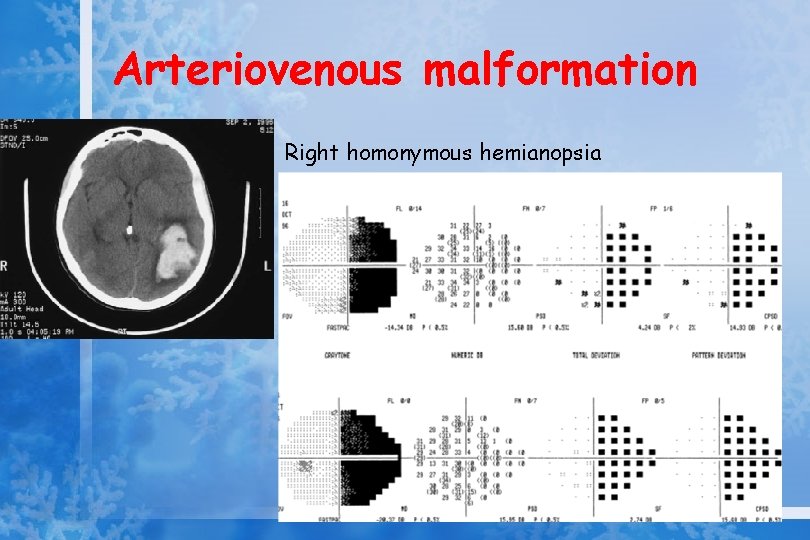
Arteriovenous malformation Right homonymous hemianopsia
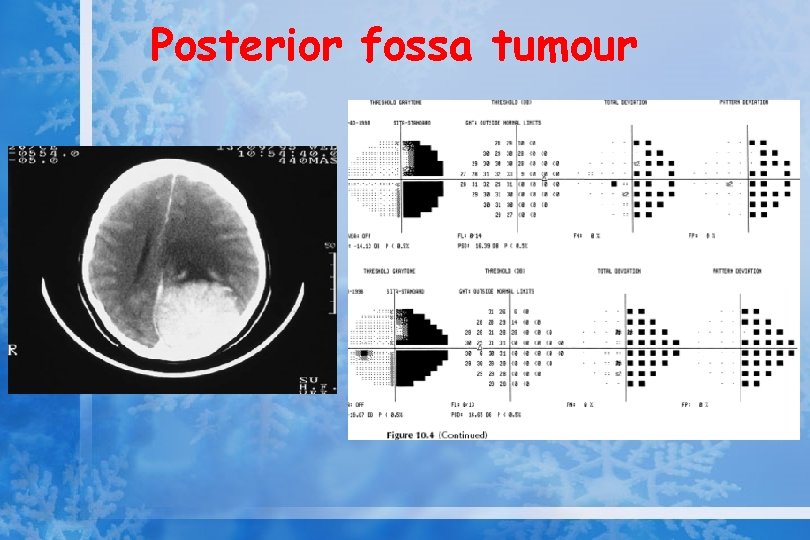
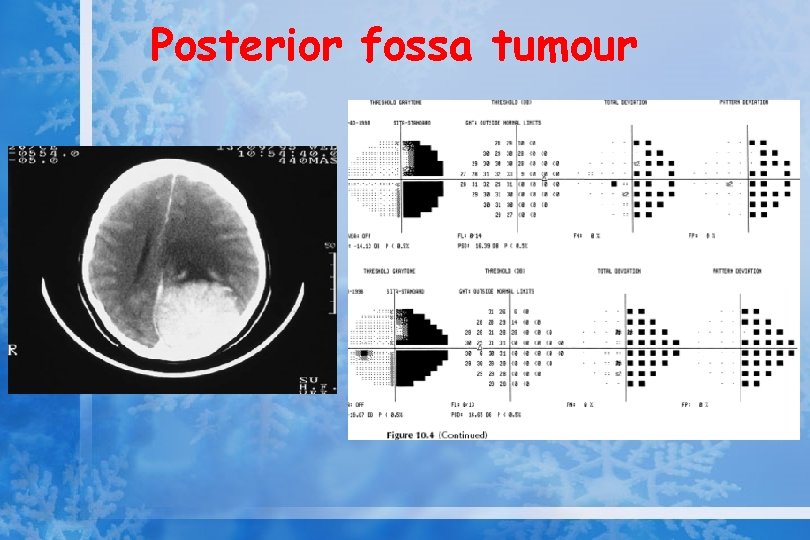
Posterior fossa tumour
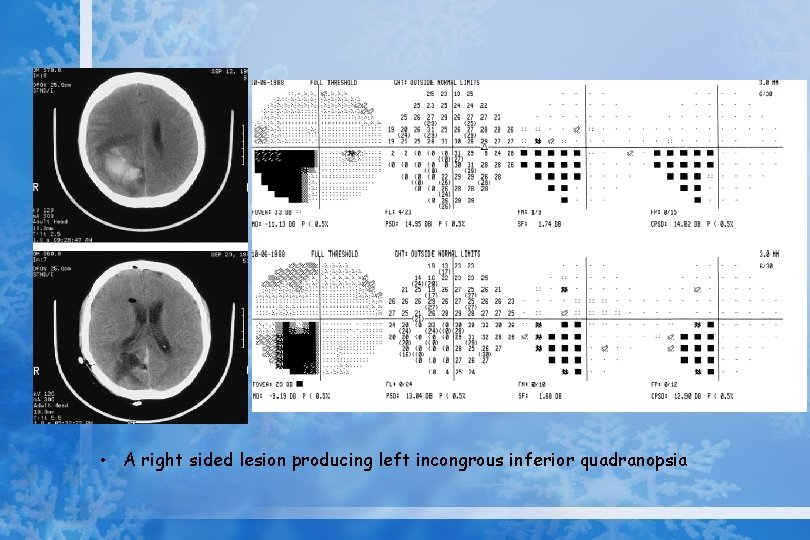
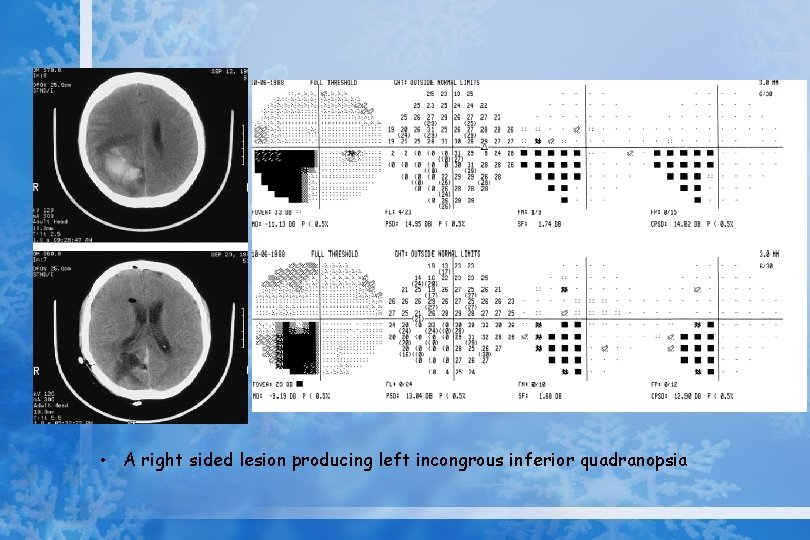
• A right sided lesion producing left incongrous inferior quadranopsia
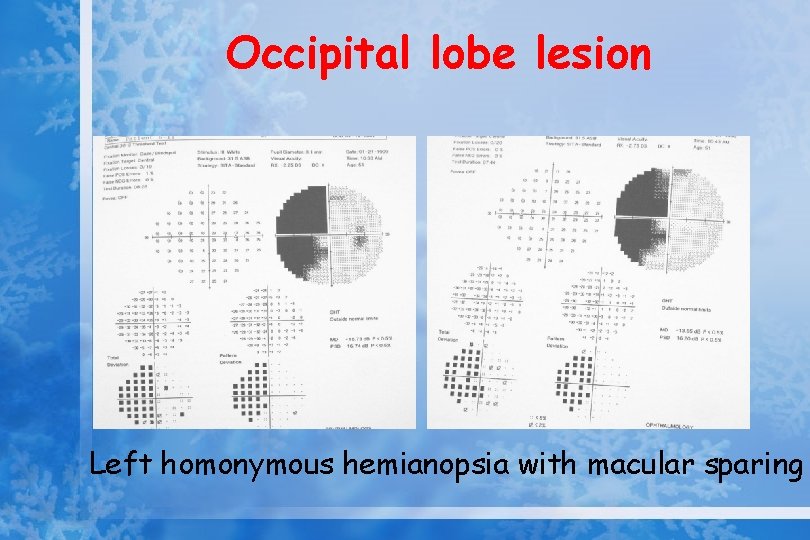
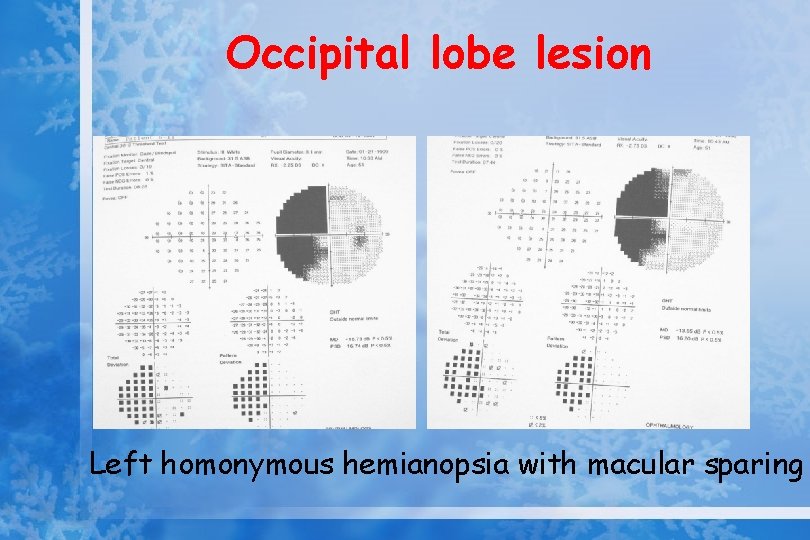
Occipital lobe lesion Left homonymous hemianopsia with macular sparing
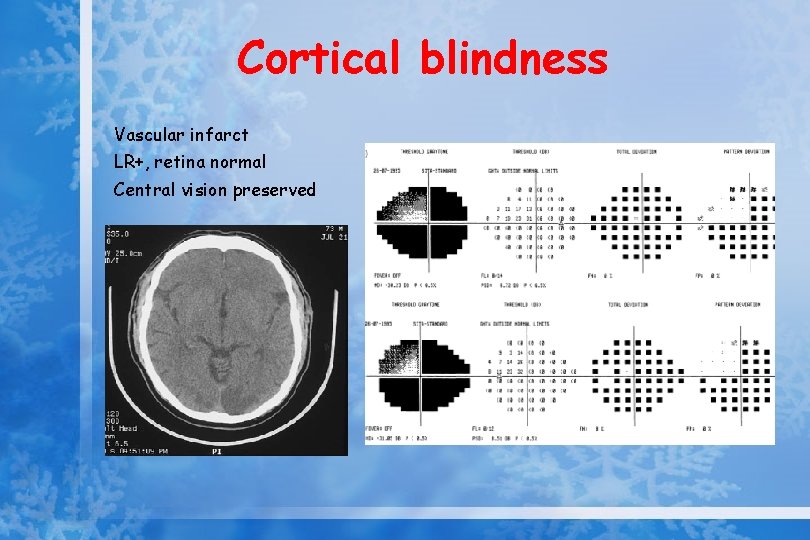
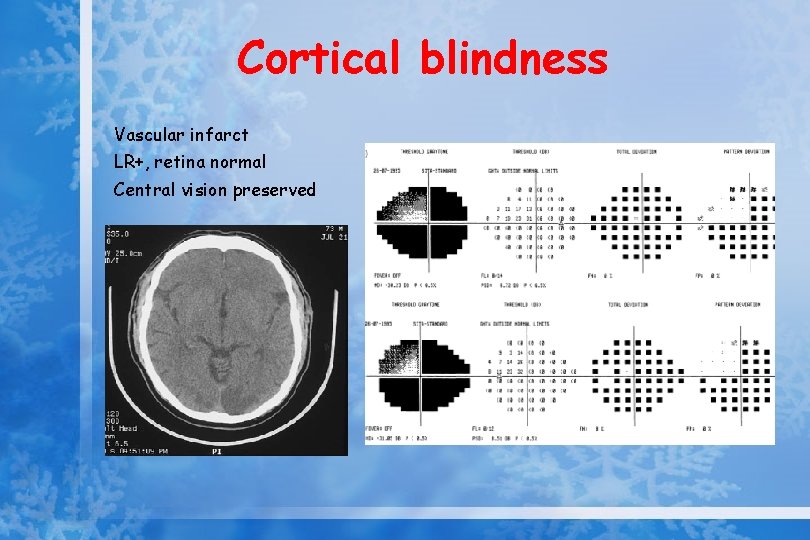
Cortical blindness Vascular infarct LR+, retina normal Central vision preserved
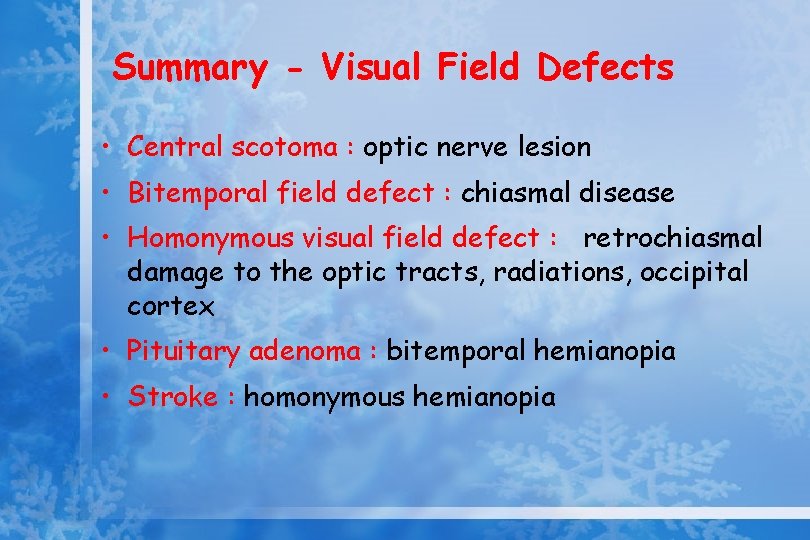
Summary - Visual Field Defects • Central scotoma : optic nerve lesion • Bitemporal field defect : chiasmal disease • Homonymous visual field defect : retrochiasmal damage to the optic tracts, radiations, occipital cortex • Pituitary adenoma : bitemporal hemianopia • Stroke : homonymous hemianopia
Summary - Visual Field Defects

• Any questions ?