Renal Epithelial Cell cells exposed to interstitium and

- Slides: 54
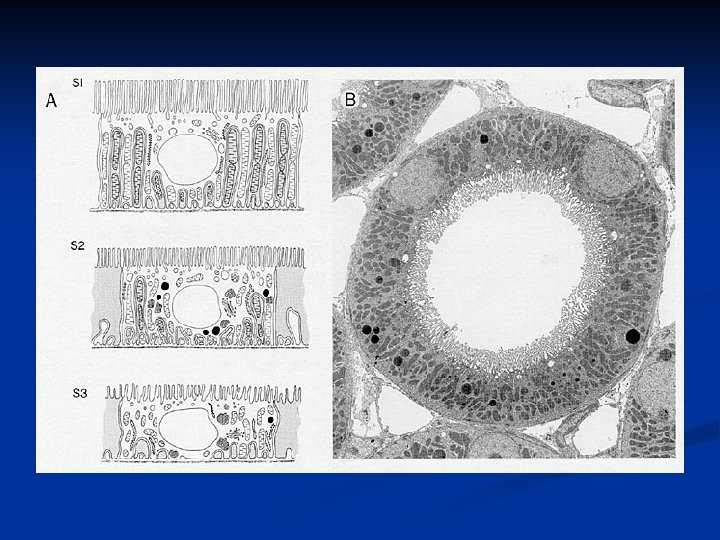
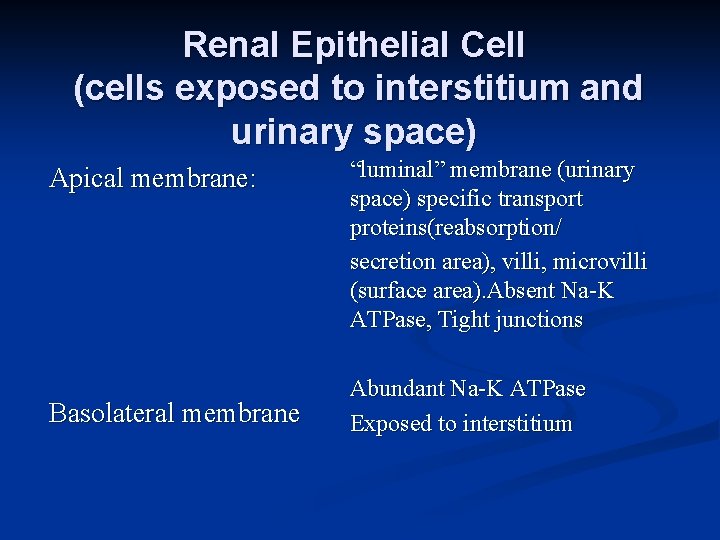
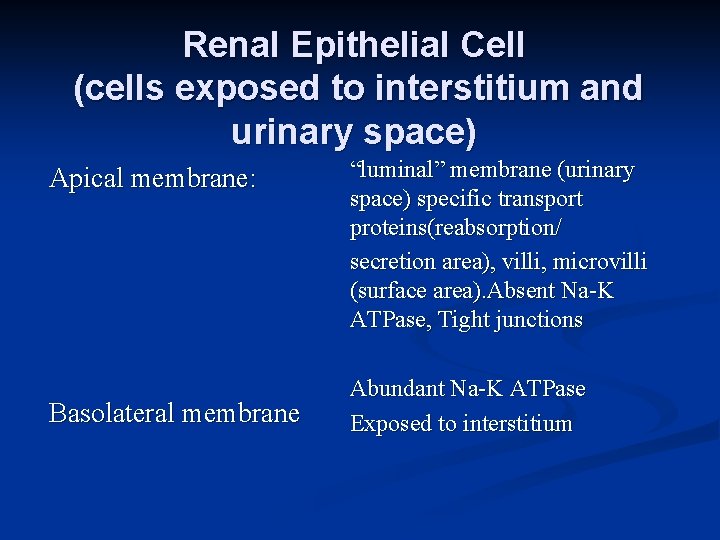
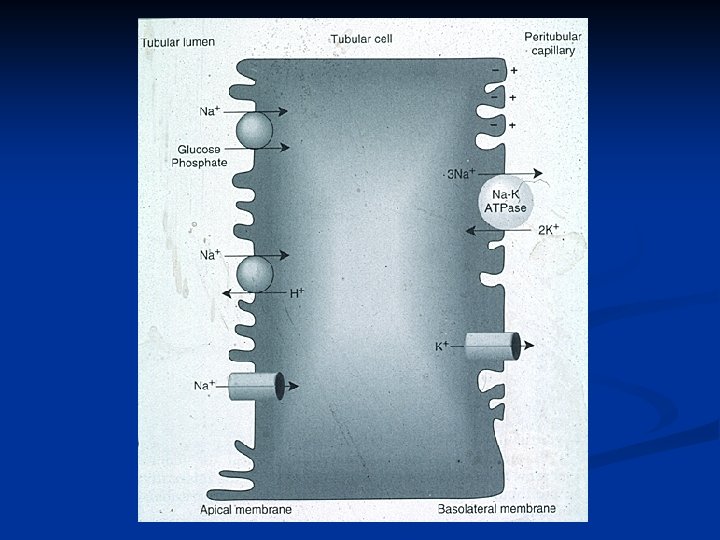
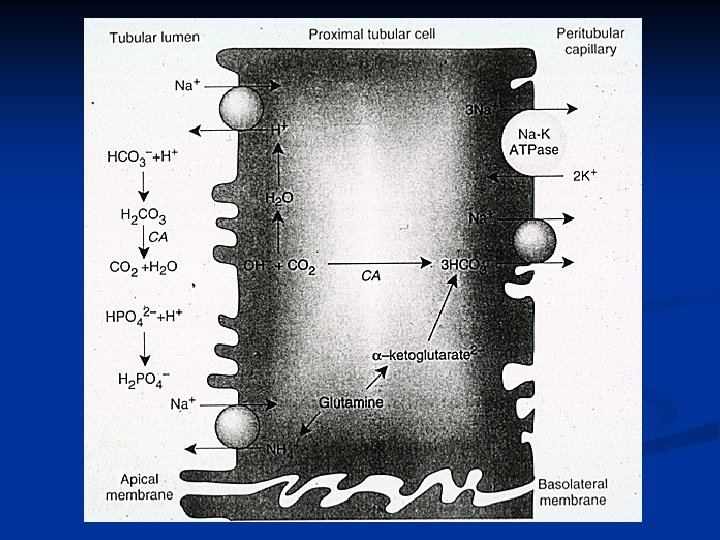
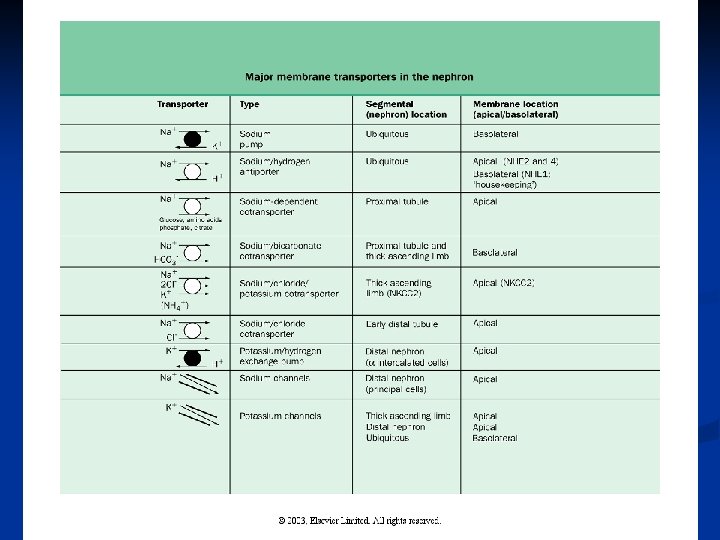
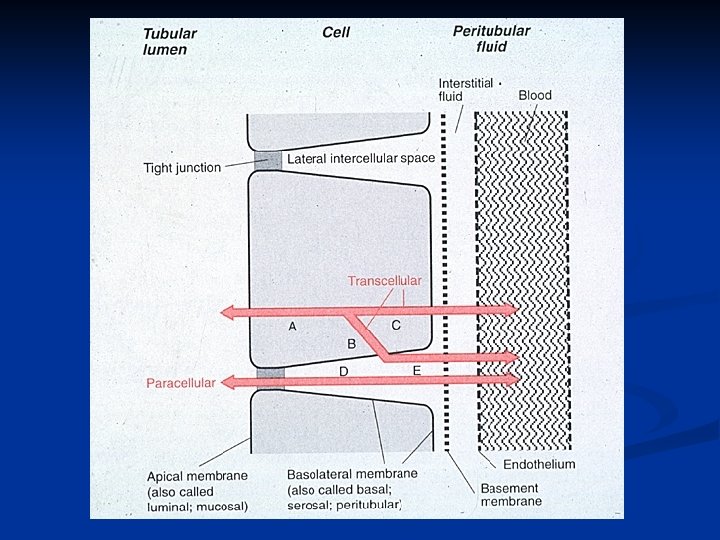
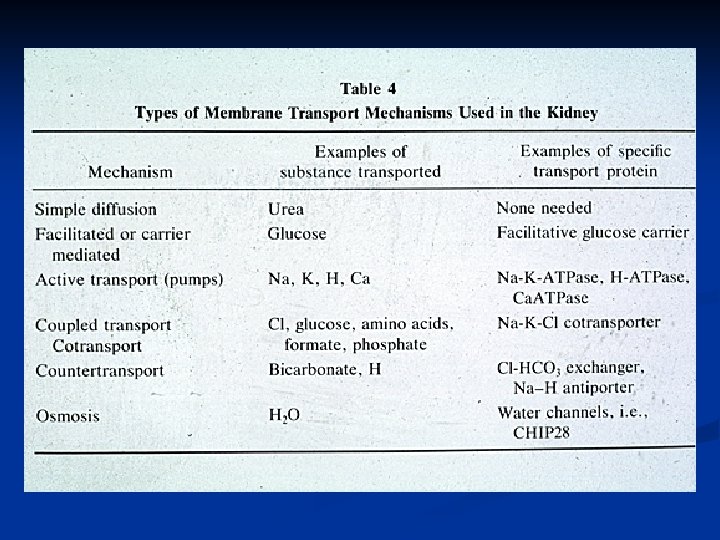
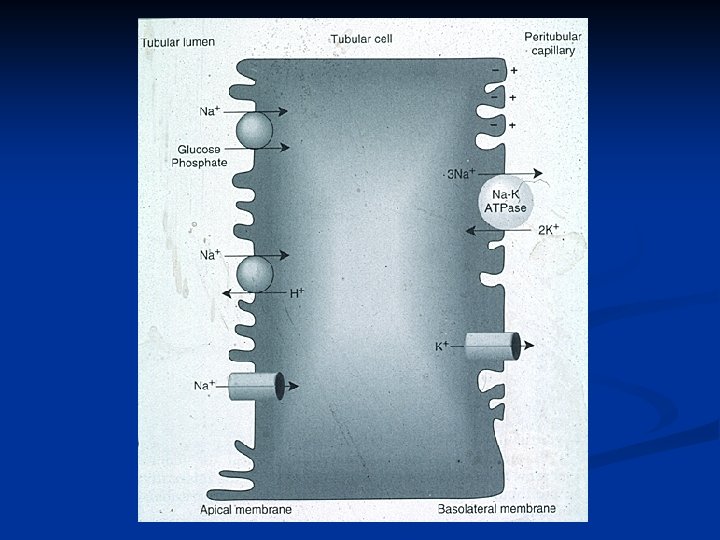
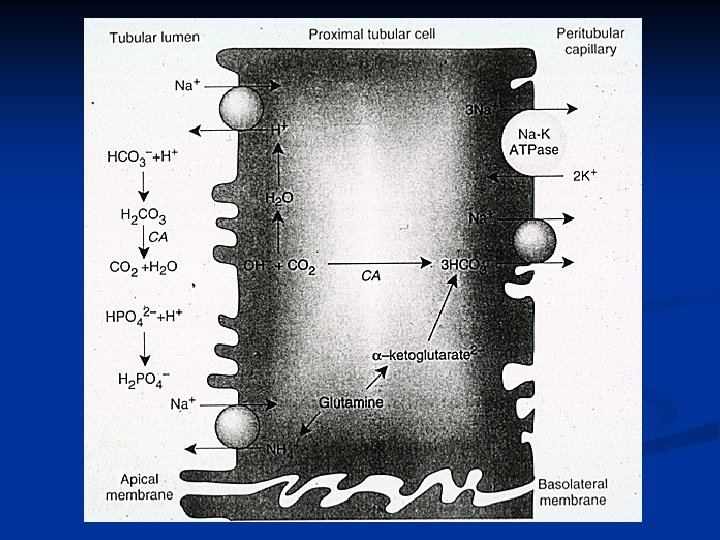
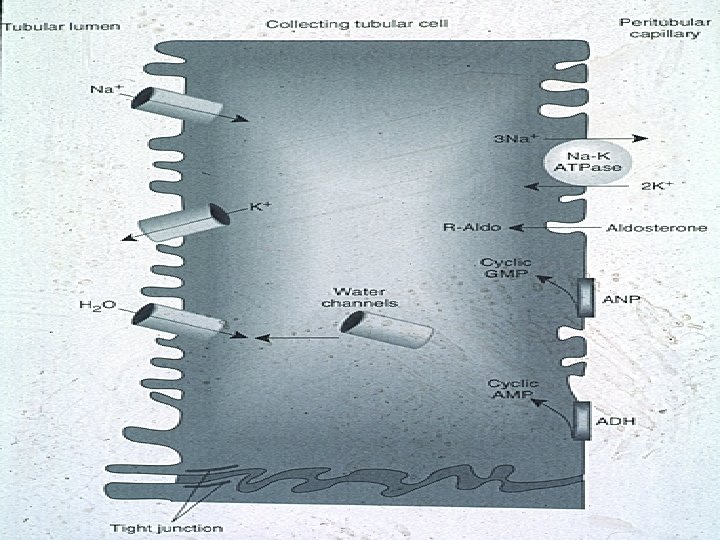
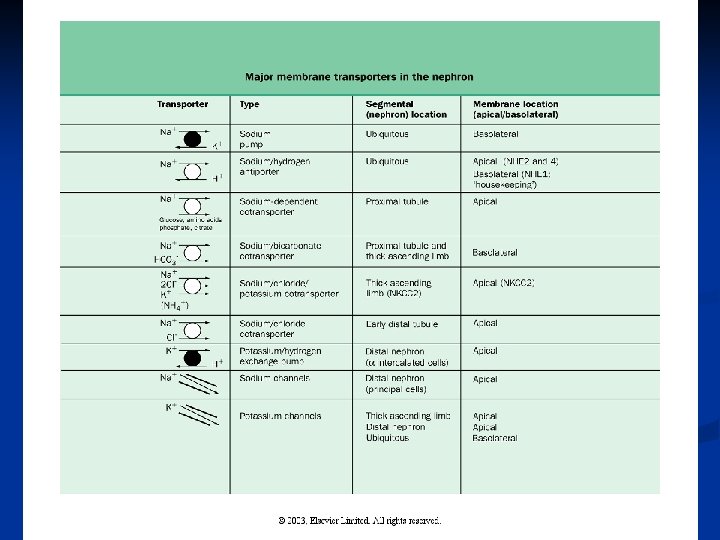
Renal Epithelial Cell (cells exposed to interstitium and urinary space) Apical membrane: Basolateral membrane “luminal” membrane (urinary space) specific transport proteins(reabsorption/ secretion area), villi, microvilli (surface area). Absent Na-K ATPase, Tight junctions Abundant Na-K ATPase Exposed to interstitium
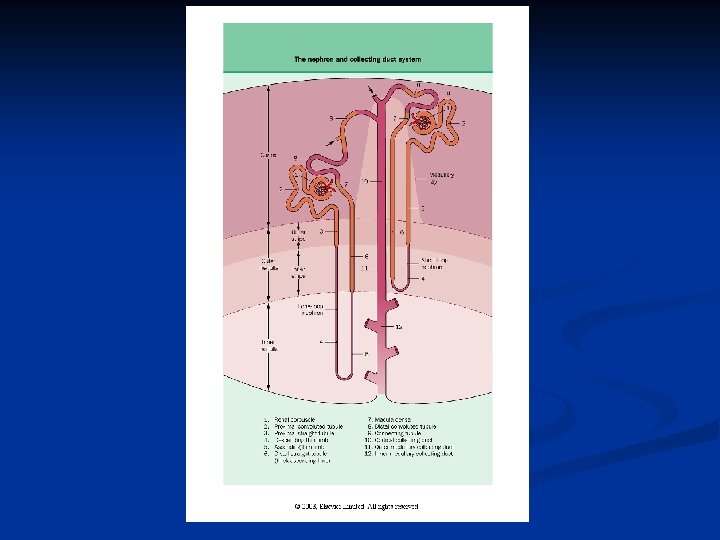
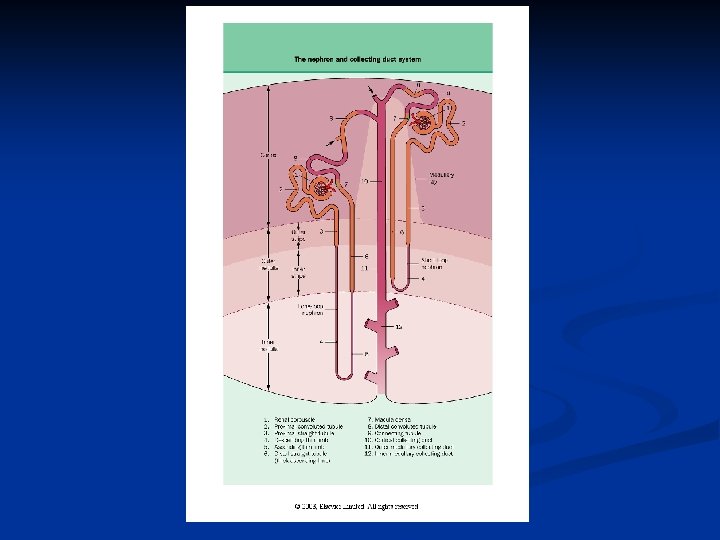
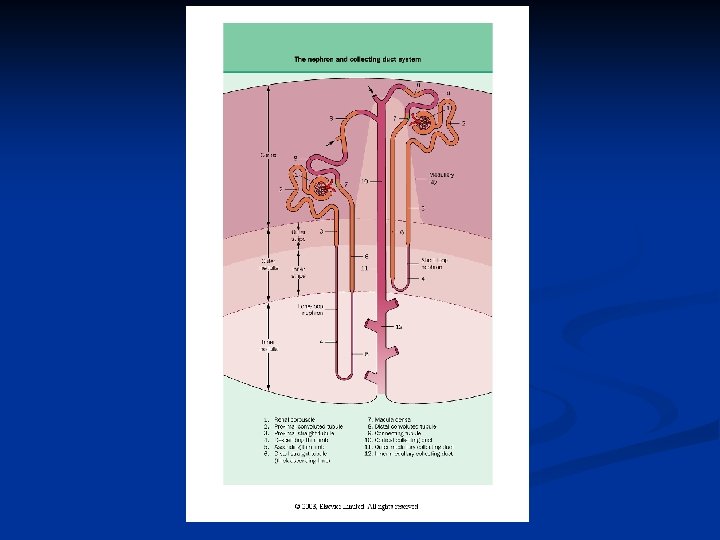
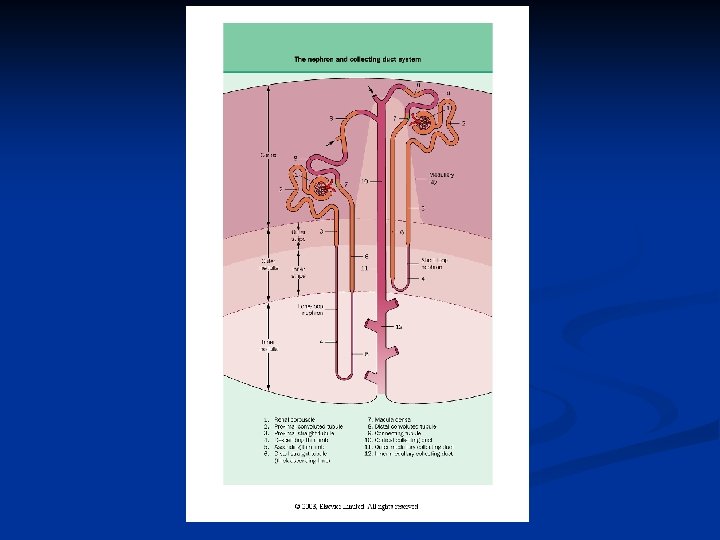
Proximal Nephron n Proximal convoluted tubule and Proximal straight tubule The Loop of Henle: thin descending limb, thin ascending limb, medullary thick ascending limb, cortical thick ascending limb The proximal nephron is considered to end at the macula densa segment which occurs at the end of the cortical thick ascending limb
Proximal Tubule n Proximal convoluted tubule (cortex) n Proximal straight tubule (descends to the corticomedullary junction)
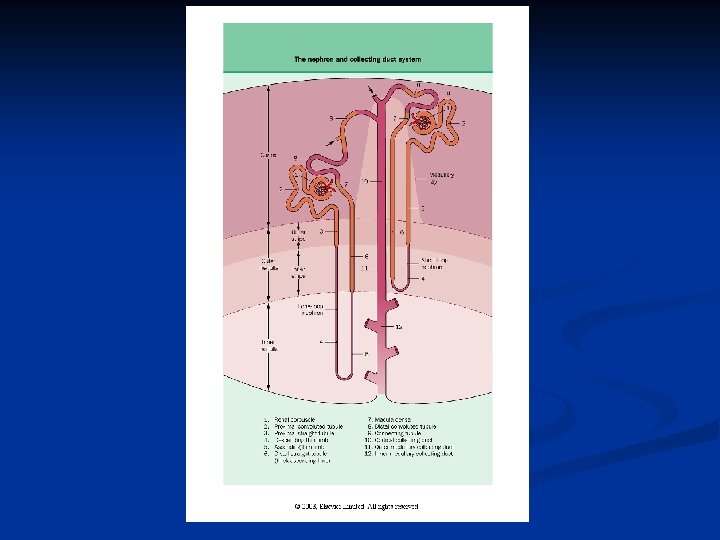
Loop of Henle n n n v Thin descending limb Thin ascending limb Thick ascending limb (medullary and cortical portions) Note: cortical nephrons are “short loop” juxtomedullary nephrons are “long loop” nephrons
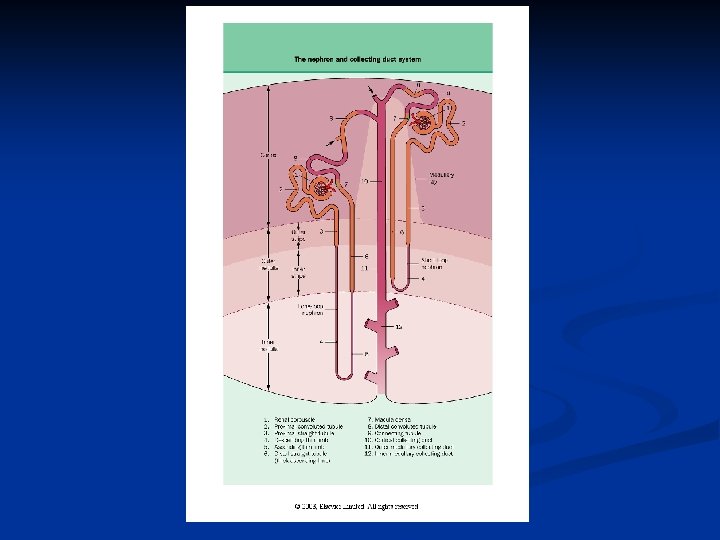

Distal Nephron Distal convoluted tubule n Connecting segment n Cortical collecting duct n Medullary collecting duct (outer and inner portions) n
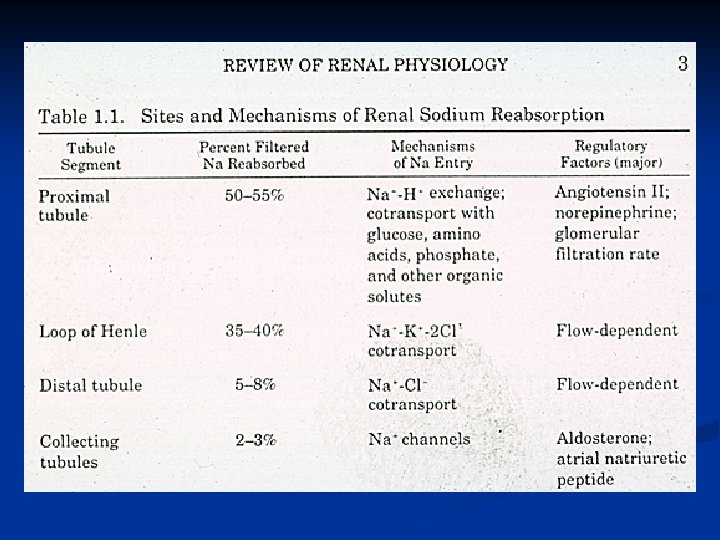
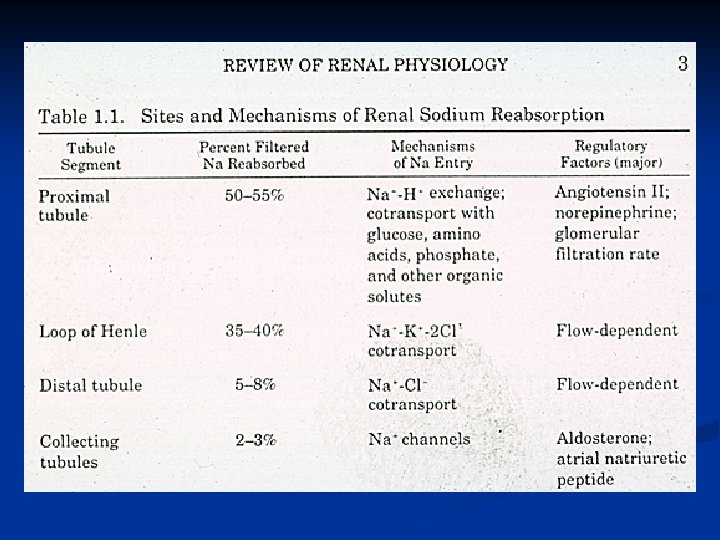
Proximal Tubule Functions Reabsorption occurs in an isotonic manner (isotonic fluid enters and isotonic fluid exits, but the composition is altered) Bulk reabsorption: ~50 -55%Na. Cl and H 20 ~90% Na. HCO 3 Organic nutrients: 100% glucose, amino acids Organic anion and cation secretory pathways PO 4 and urate reabsorption Major site of NH 3 production (via glutamine metabolism) Major site of glomerulotubular balance
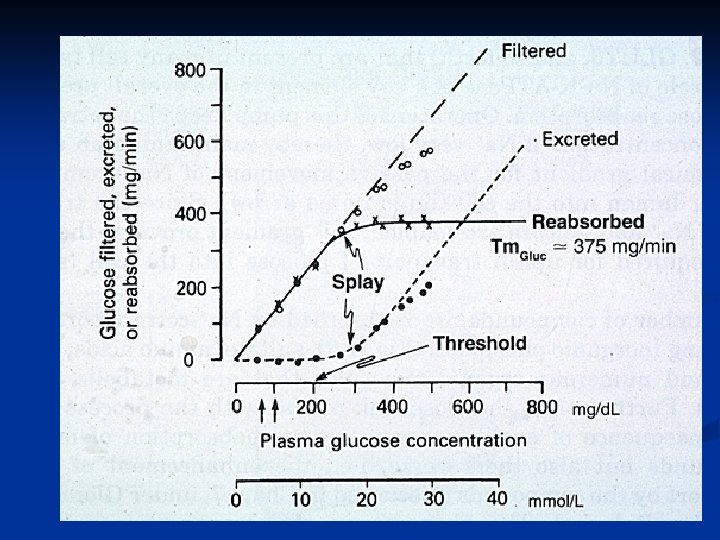
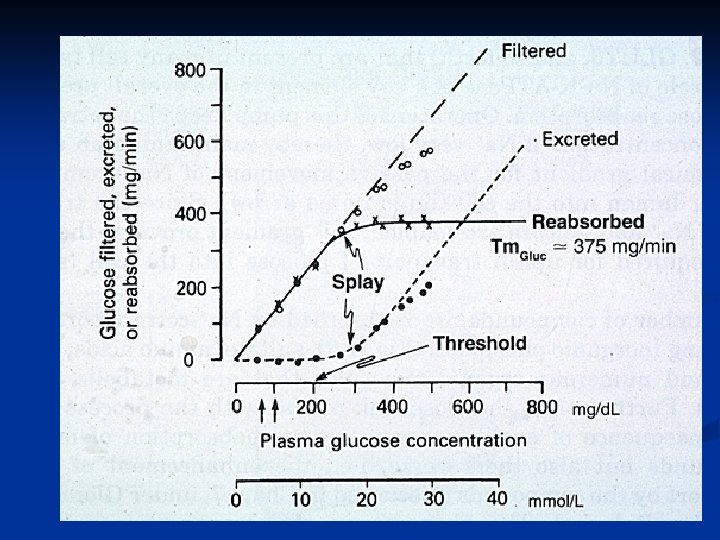
Definitions Filtered Load: The amount of a substance, X, that is deposited in Bowman’s space by filtration: (GFR) x (Px) Transport Maximum The maximal amount of substance X that can be reabsorbed or secreted: Tmx
Glomerulotubular balance Glomerulotubular Balance Normal matching of proximal tubule reabsorptive capacity to the filtering capacity of its glomerulus (euvolemic conditions) Alternative meaning: The phenomenon that the fraction of filtered Na+ that is reabsorbed by the proximal tubule is constant n Incr GFR, incr FL, but 50 -55% reabsorbed n Decr GFR, decr FL, but 50 -55%
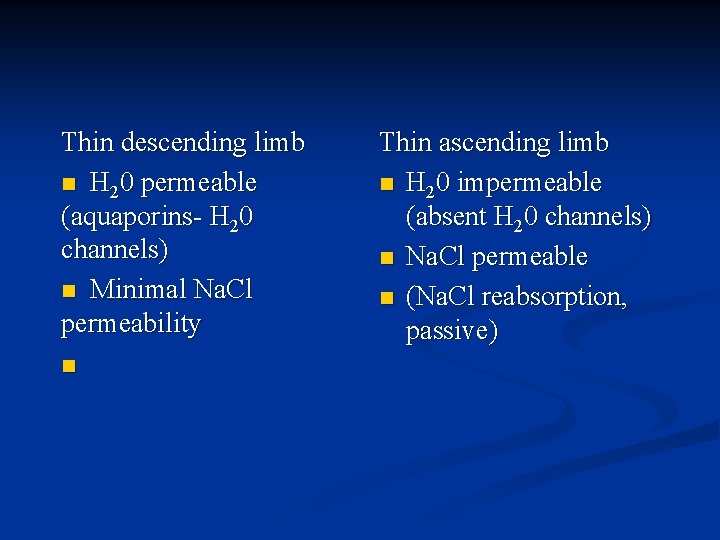
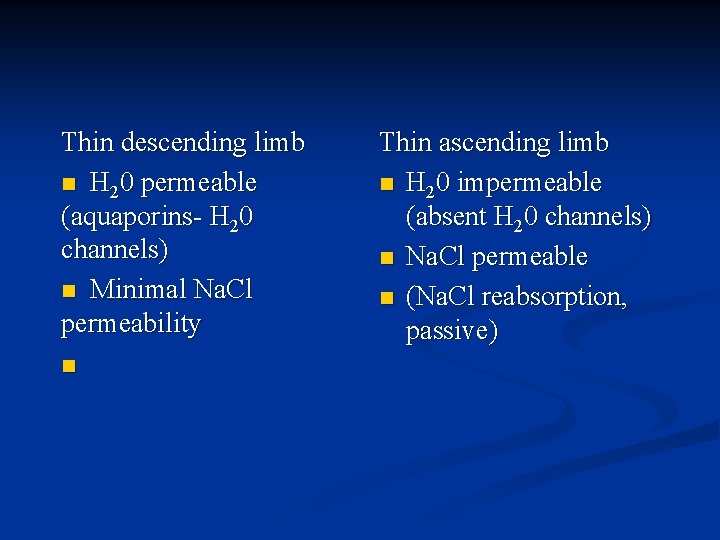
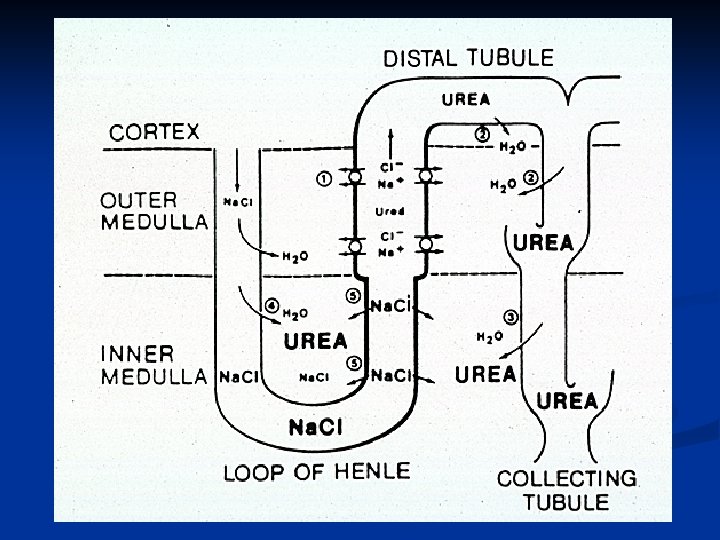
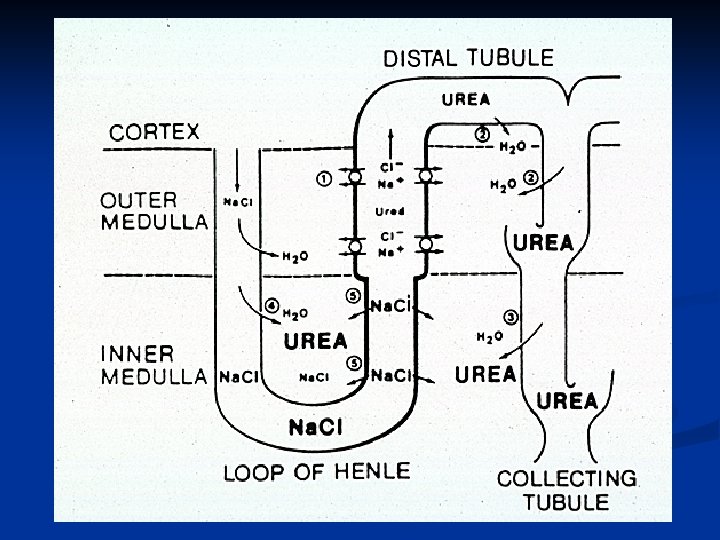
Thin descending limb n H 20 permeable (aquaporins- H 20 channels) n Minimal Na. Cl permeability n Thin ascending limb n H 20 impermeable (absent H 20 channels) n Na. Cl permeable n (Na. Cl reabsorption, passive)
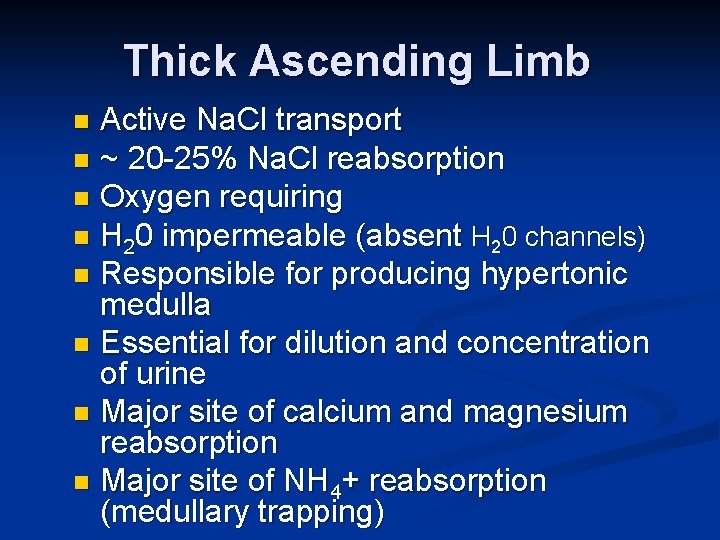
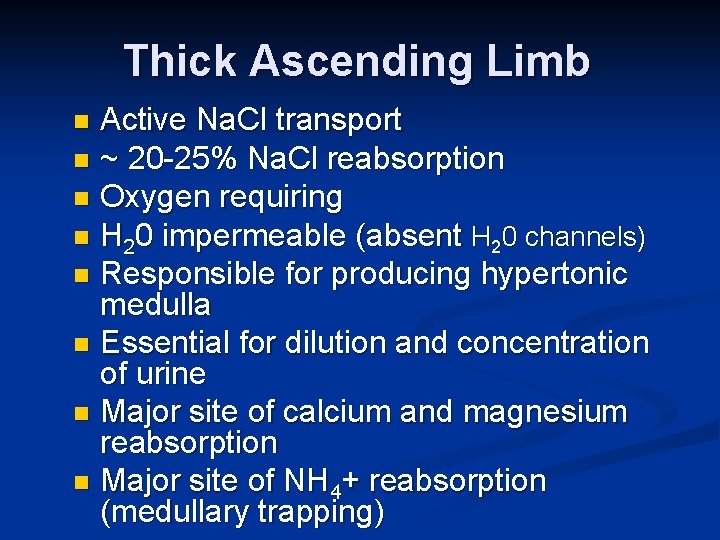
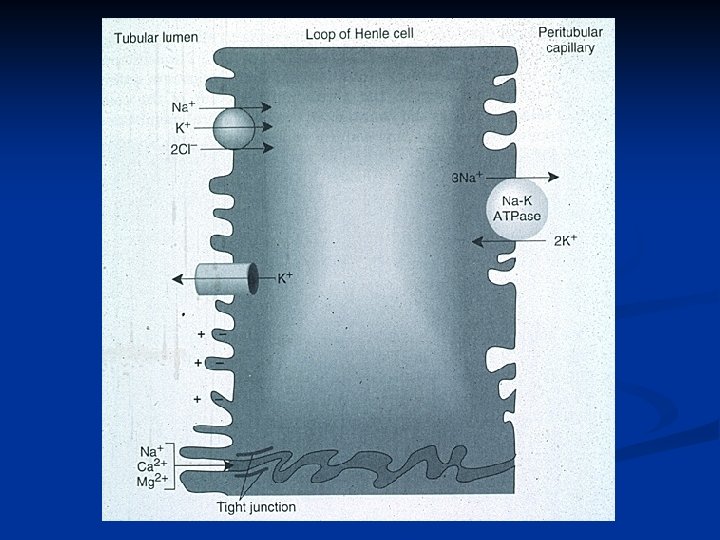
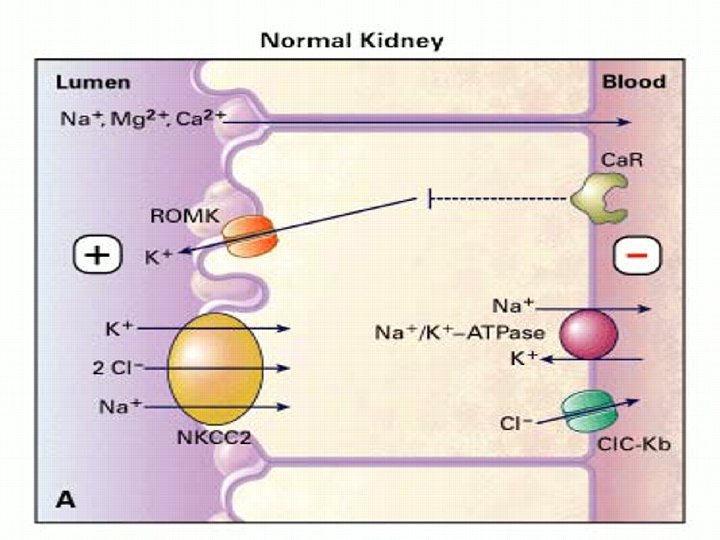
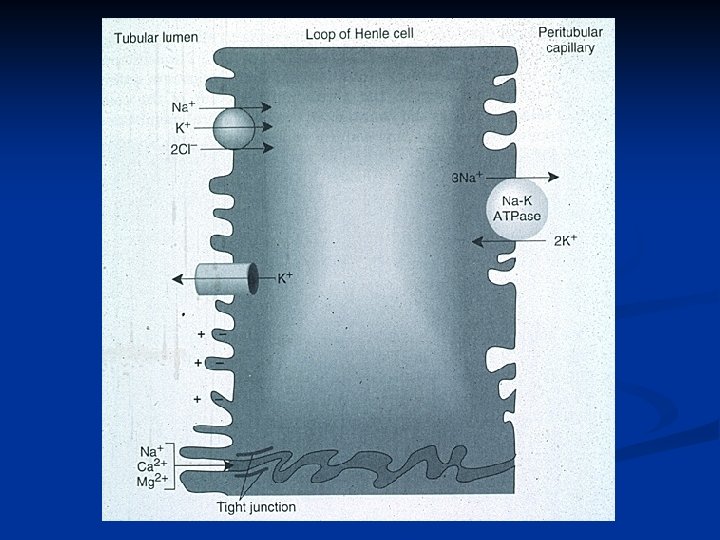
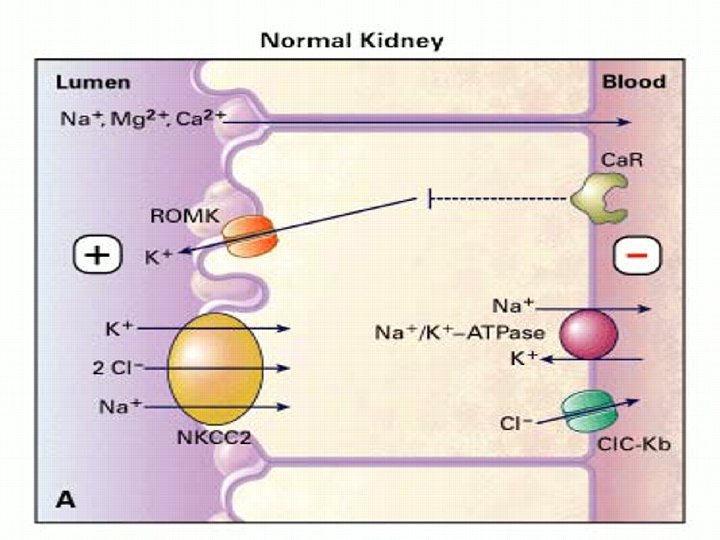
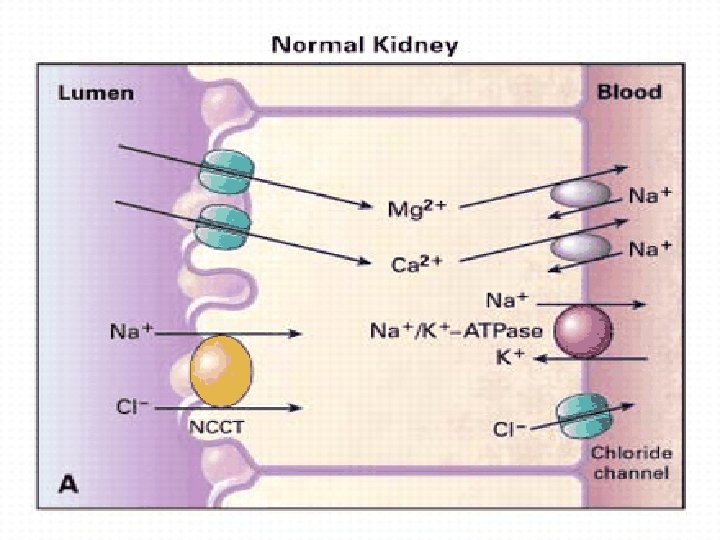
Thick Ascending Limb Active Na. Cl transport n ~ 20 -25% Na. Cl reabsorption n Oxygen requiring n H 20 impermeable (absent H 20 channels) n Responsible for producing hypertonic medulla n Essential for dilution and concentration of urine n Major site of calcium and magnesium reabsorption n Major site of NH 4+ reabsorption (medullary trapping) n
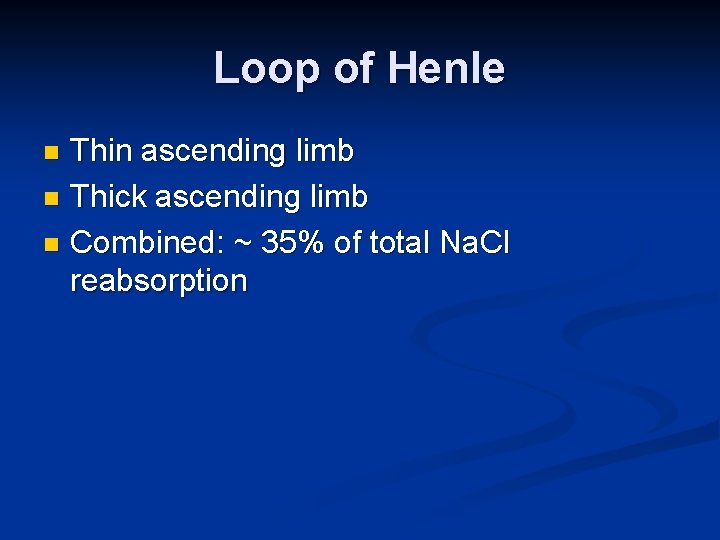
Loop of Henle Thin ascending limb n Thick ascending limb n Combined: ~ 35% of total Na. Cl reabsorption n
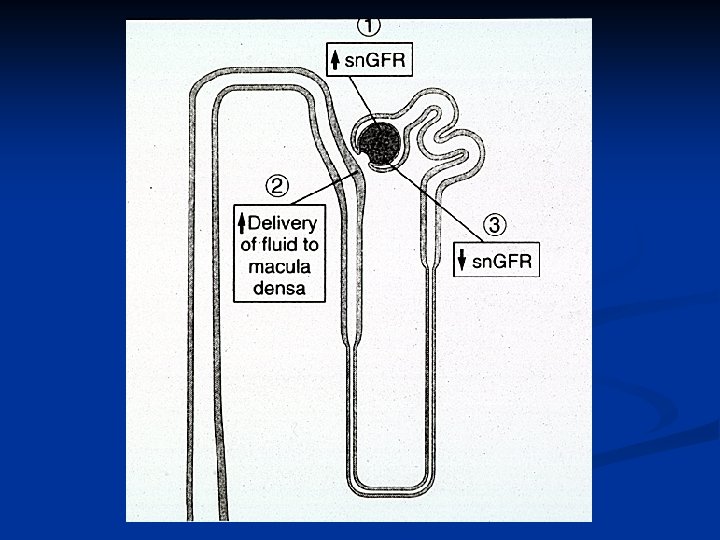
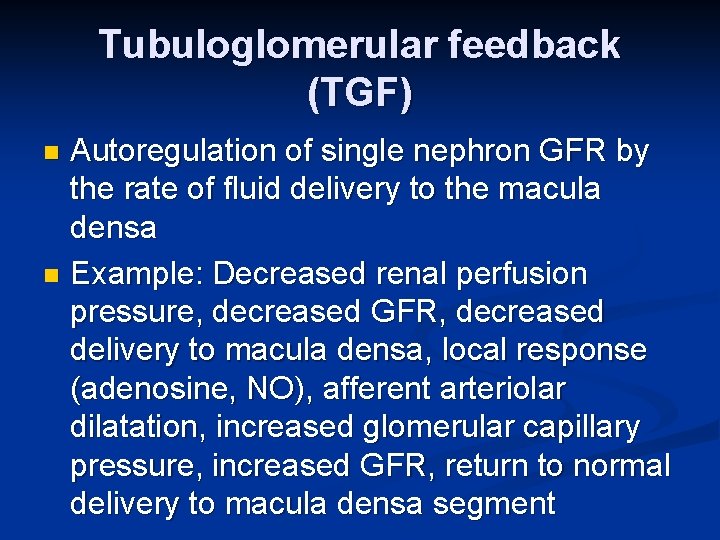
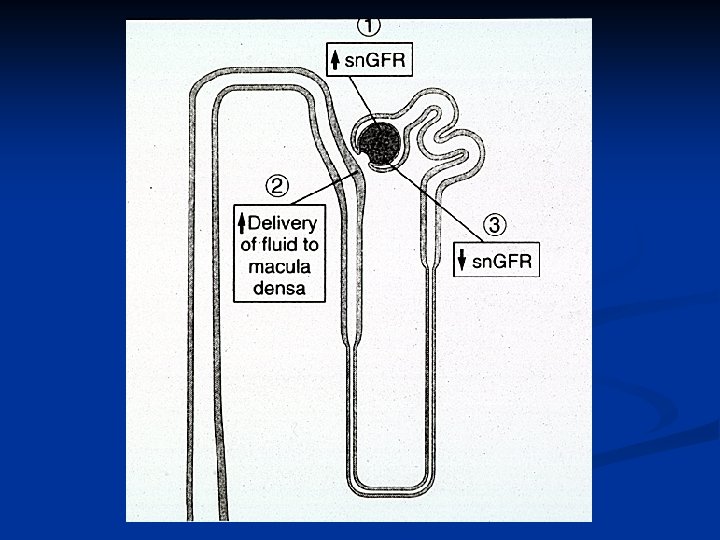
Tubuloglomerular feedback (TGF) Autoregulation of single nephron GFR by the rate of fluid delivery to the macula densa n Example: Decreased renal perfusion pressure, decreased GFR, decreased delivery to macula densa, local response (adenosine, NO), afferent arteriolar dilatation, increased glomerular capillary pressure, increased GFR, return to normal delivery to macula densa segment n
Tubuloglomerular feedback Example: increased renal perfusion pressure (which increases GFR) n Afferent arteriole constricts and GFR falls in the presence of increased renal perfusion pressure n TGF contributes to maintaining distal delivery of tubular fluid at a relatively constant rate. n
Juxtaglomerular apparatus n n n TGF (macula densa) Renal renin secretion (afferent arteriole) (decreased renal perfusion pressure results in enhanced renin secretion and activation of TGF) Both contribute to maintaining GFR and to maintaining a normal distal tubular flow rate. Proximal nephrons segments: Bulk reabsorption. Distal nephron segments: Fine tuning of final urine composition
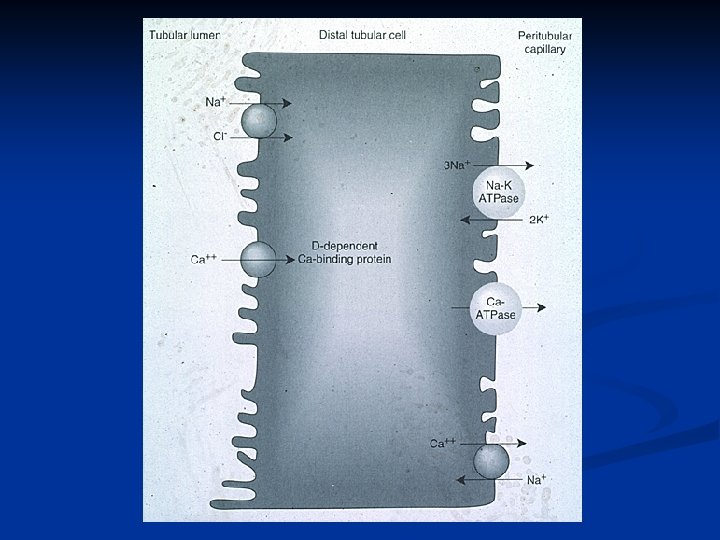
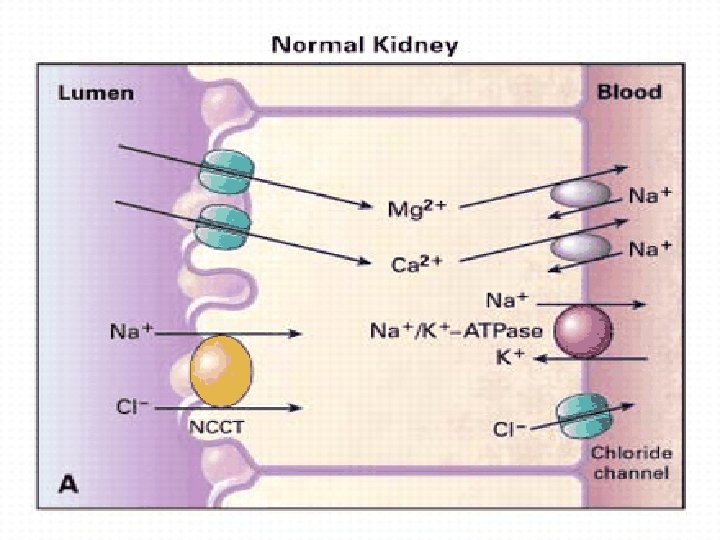
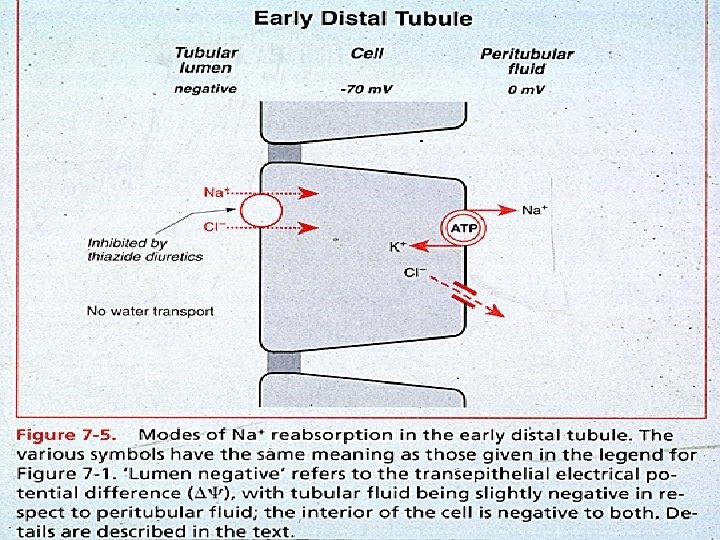
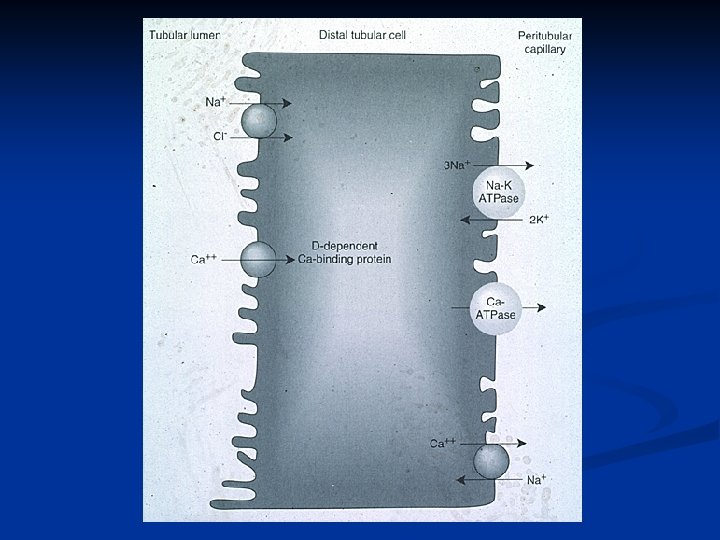
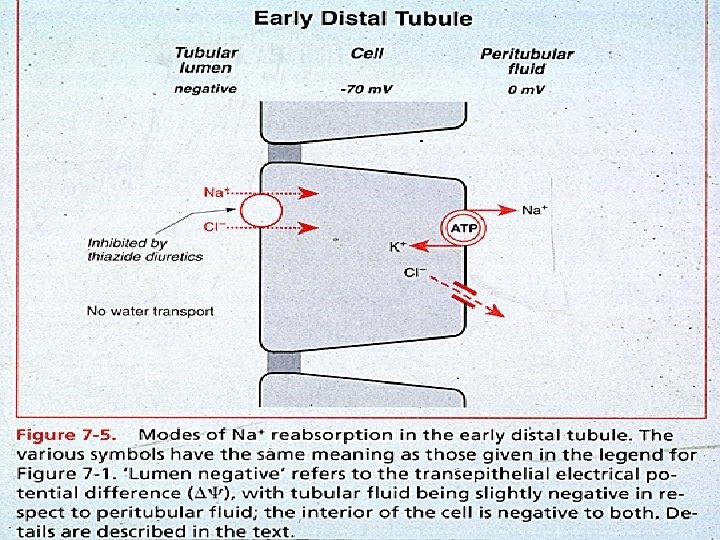
Distal Convoluted Tubule 5 -8% of Na. Cl reabsorption n H 20 and urea impermeable n Major site of calcium reabsorption (stimulated by PTH) n Important for maximal urinary diluting ability (i. e. , for maximal free H 20 excretion) n
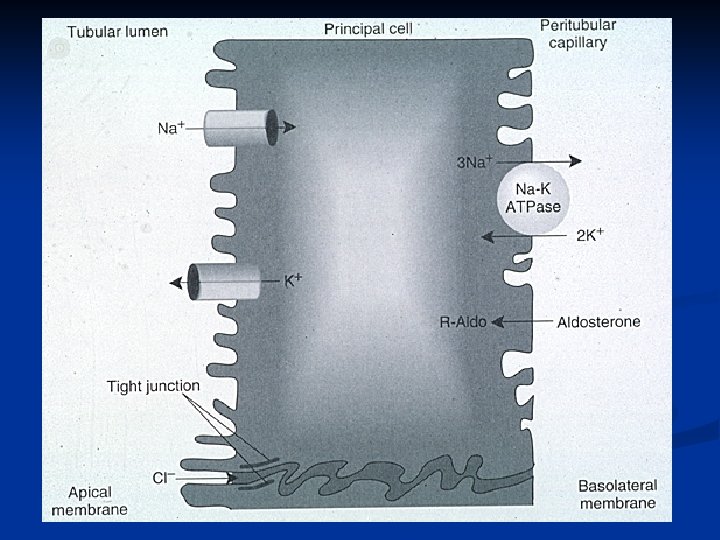
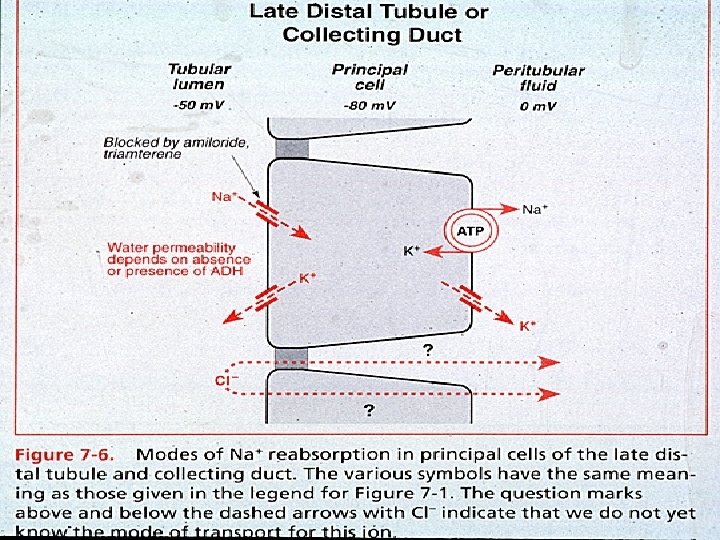
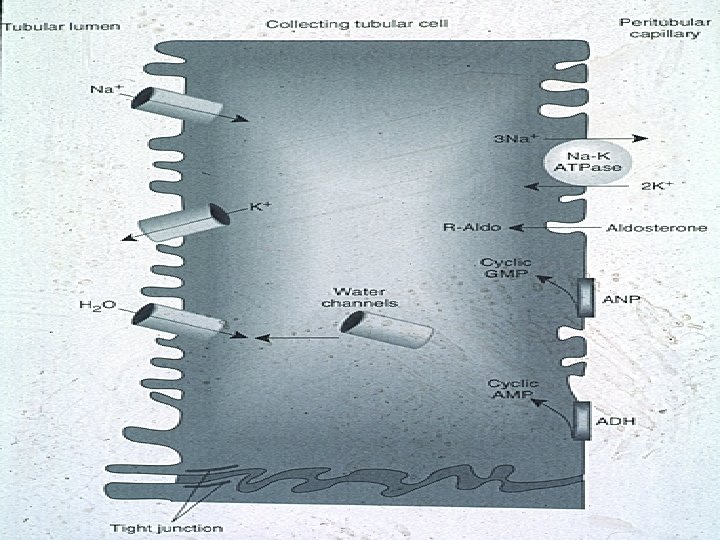
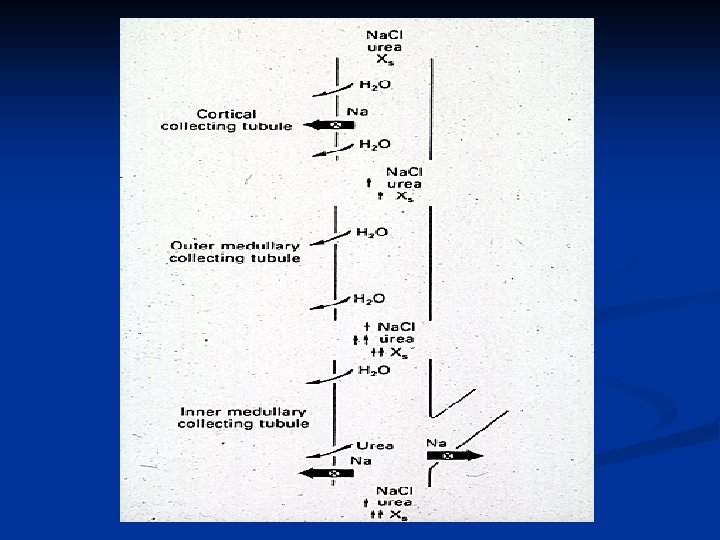
Collecting Duct Cortical and medullary segments n 2 -3 % Na. Cl reabsorption n Built for fine tuning of solute and H 20 handling n Not built for bulk reabsorption n
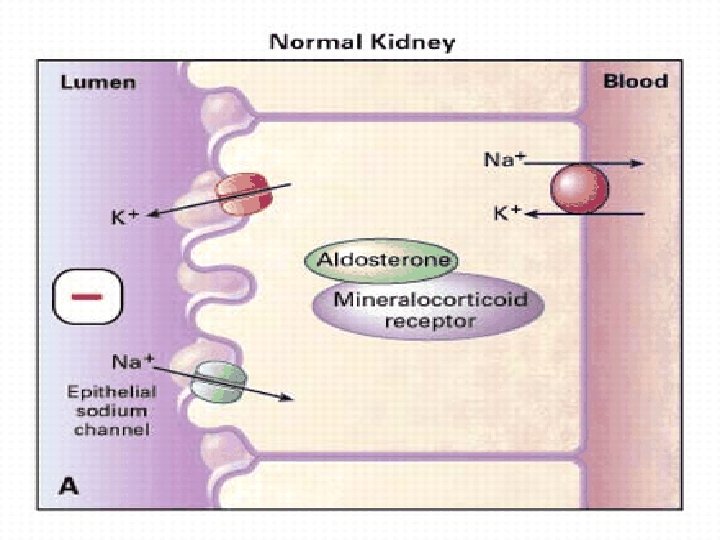
Collecting duct n n Principal cells (cortical collecting duct and inner medullary collecting duct) Sodium chloride and water reabsorption, potassium secretion Intercalated cells (cortical collecting duct and outer medullary collecting duct) acid-base maintenance Alpha intercalated cells -H+ secretion (H+ATPase) Beta intercalated cells- HCO 3 secretion (Cl. HCO 3 exchanger
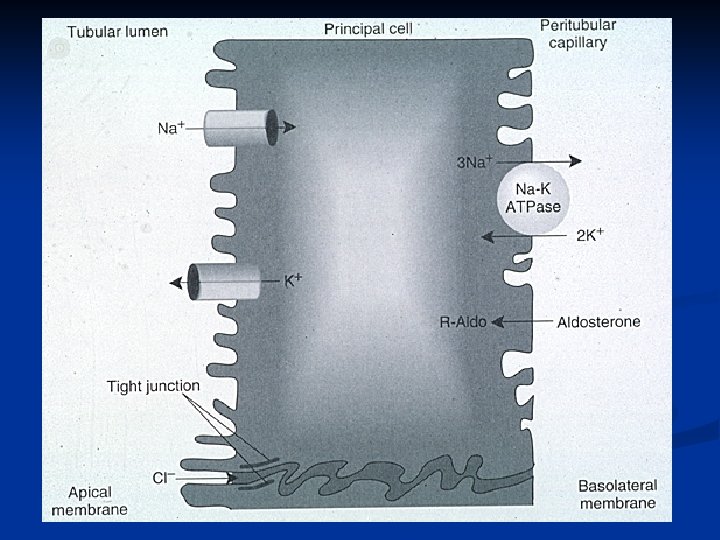
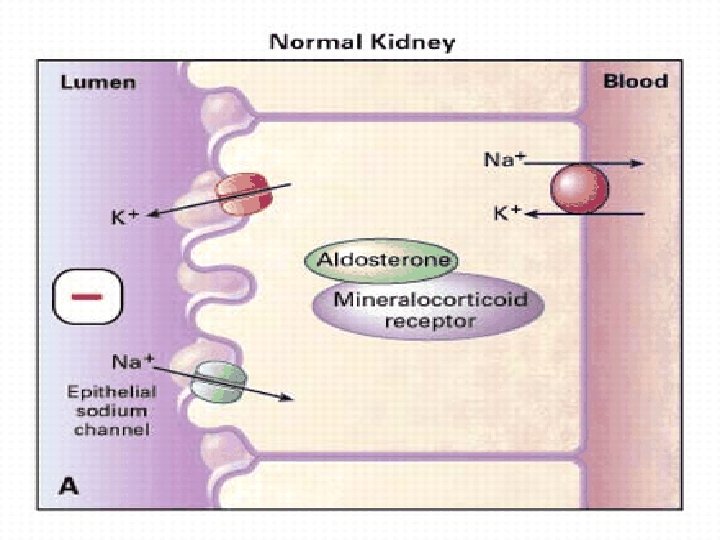
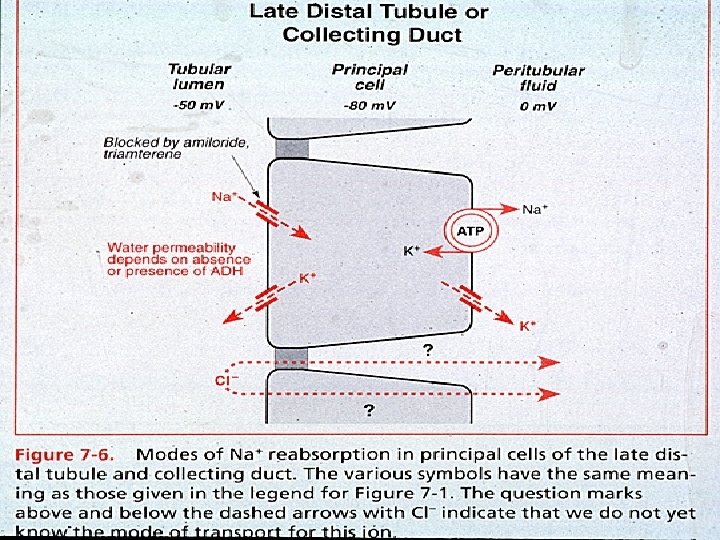
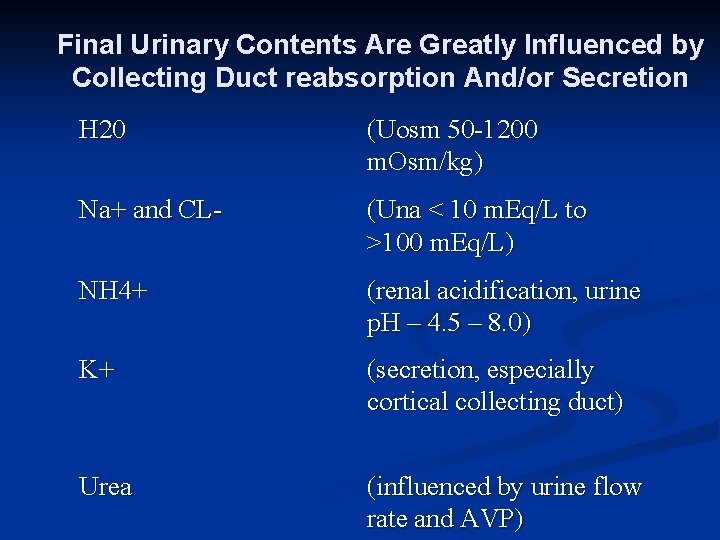
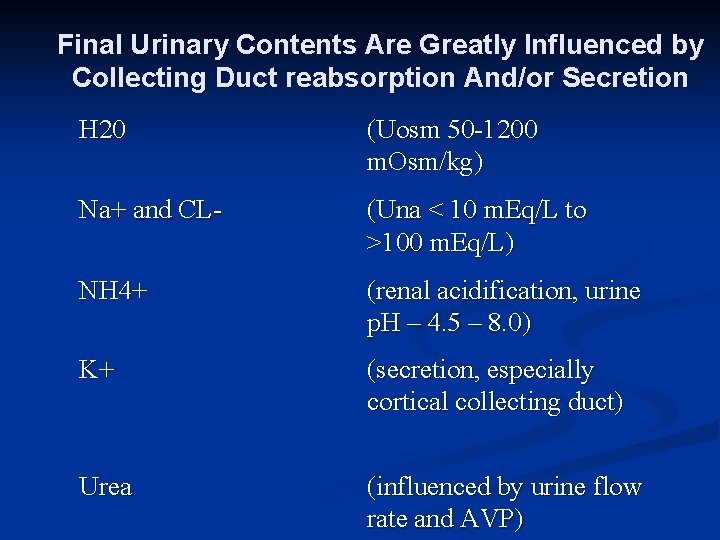
Final Urinary Contents Are Greatly Influenced by Collecting Duct reabsorption And/or Secretion H 20 (Uosm 50 -1200 m. Osm/kg) Na+ and CL- (Una < 10 m. Eq/L to >100 m. Eq/L) NH 4+ (renal acidification, urine p. H – 4. 5 – 8. 0) K+ (secretion, especially cortical collecting duct) Urea (influenced by urine flow rate and AVP)
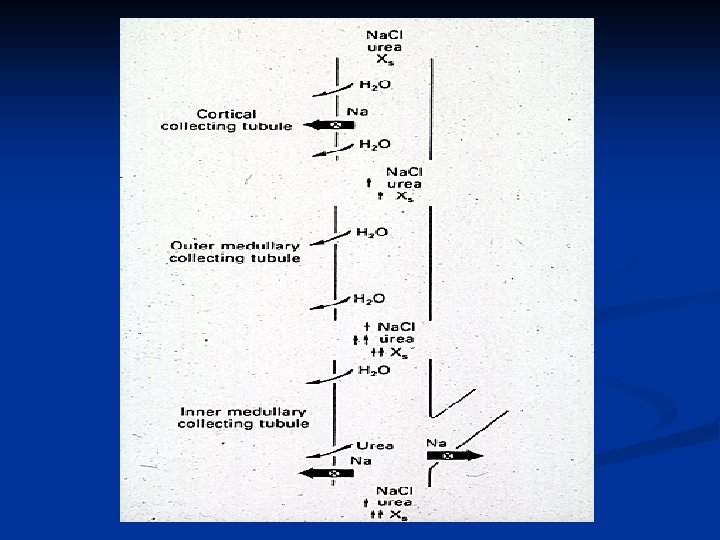
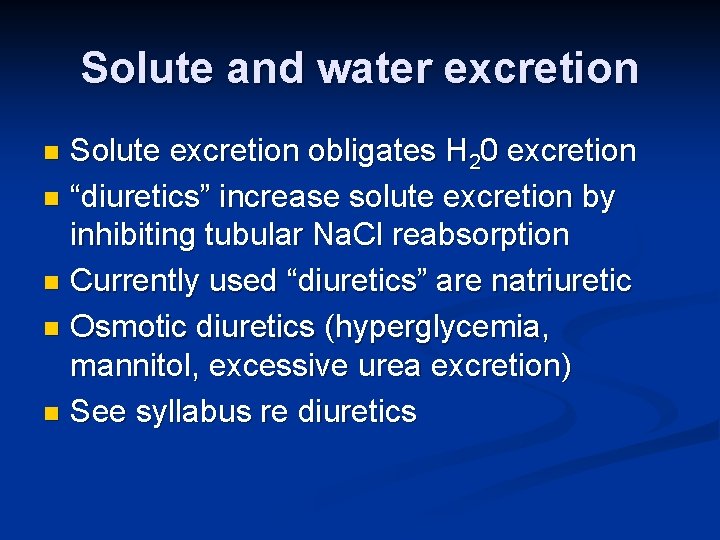
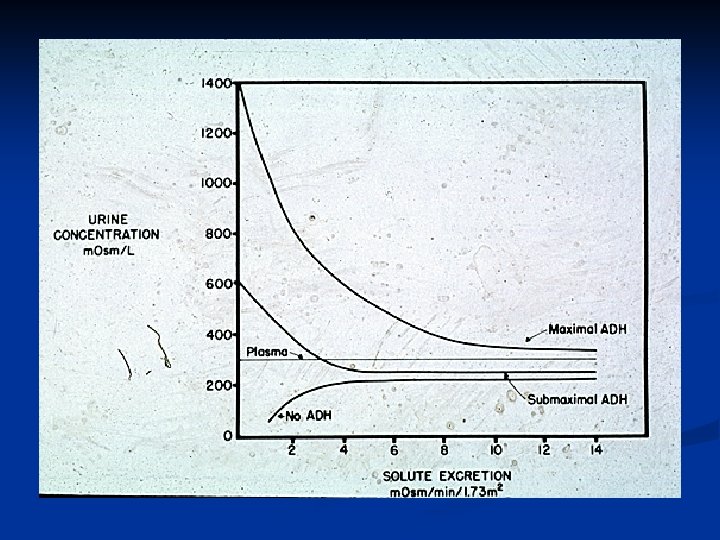
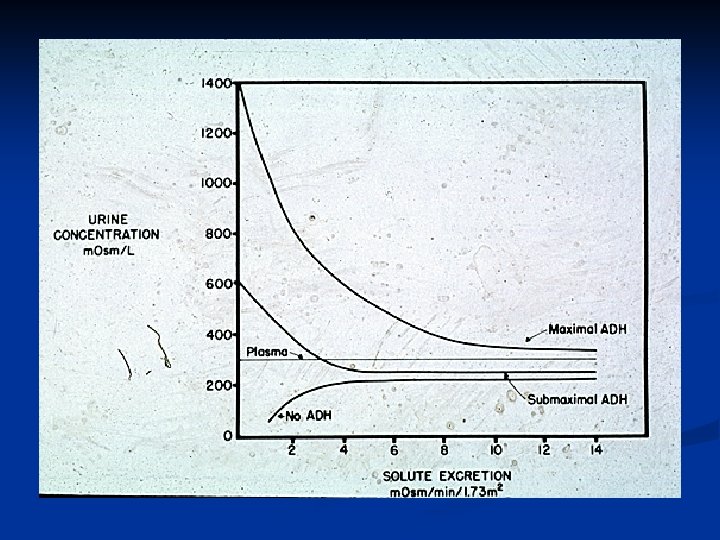
Solute and water excretion Solute excretion obligates H 20 excretion n “diuretics” increase solute excretion by inhibiting tubular Na. Cl reabsorption n Currently used “diuretics” are natriuretic n Osmotic diuretics (hyperglycemia, mannitol, excessive urea excretion) n See syllabus re diuretics n
Multiple mechanisms exist within the proximal nephron which function to avoid excessive delivery of filtrate to the distal nephron. These mechanism include: n glomerulotubular feedback n tubuloglomerular feedback n autoregulation of arteriolar resistance at the afferent and efferent arterioles n ability to shift cortical blood flow from superficial cortical nephrons to juxtamedullary nephrons which have a greater capacity for salt and water reabsorption
Effect of Angiotensin II Vasoconstriction (especially efferent arteriole) n Stimulates aldosterone secretion n Enhances proximal tubule Na+ reabsorption n Augments sympathetic stimulation n May augment vasopressin secretion n Contraction of mesangial cells which decreases glomerular capillary surface area and reduces permeability; thus, decreasingle nephron GFR n
Slides to augment small groupsessions n The following slides are to supplement the small group sessions, Problems 1 and 2 and the sodium chloride and water problems (3 -8)
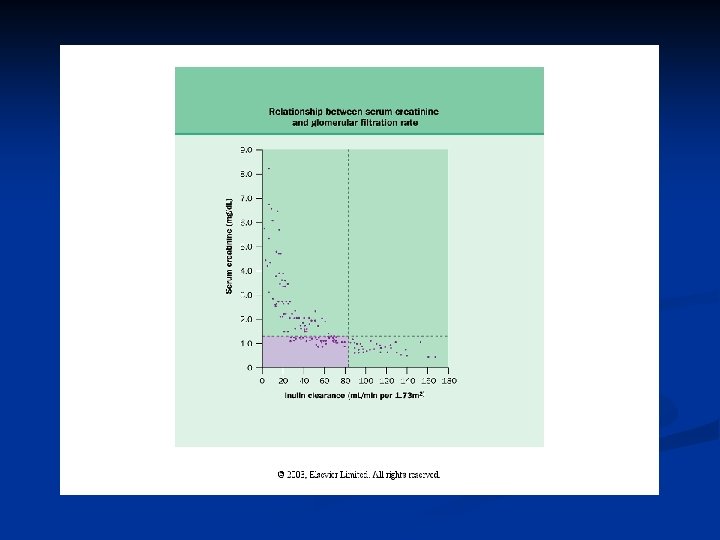
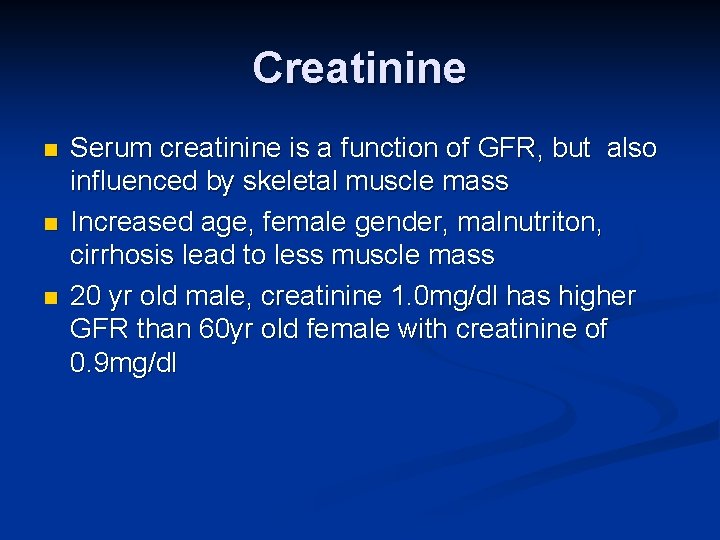
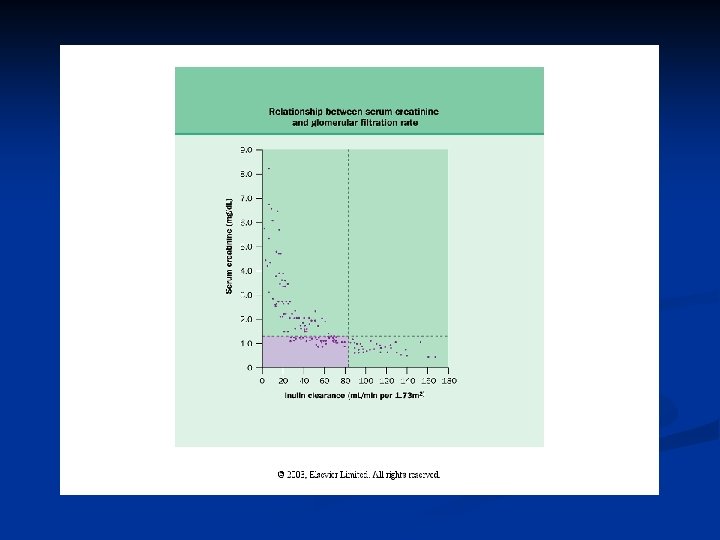
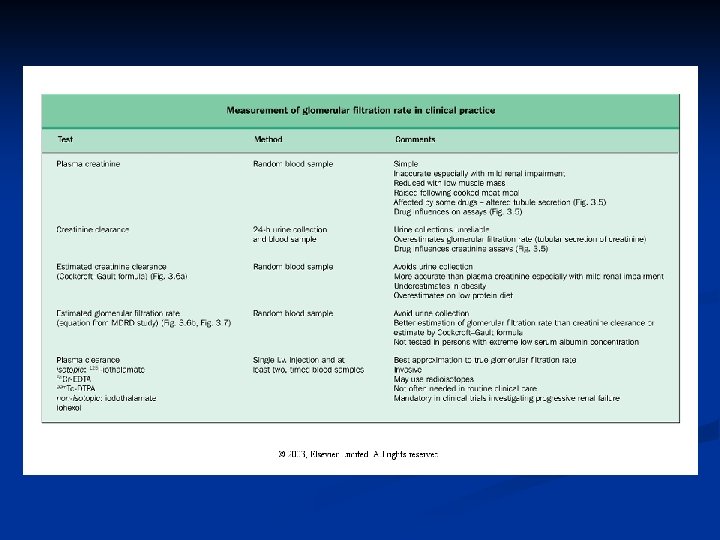
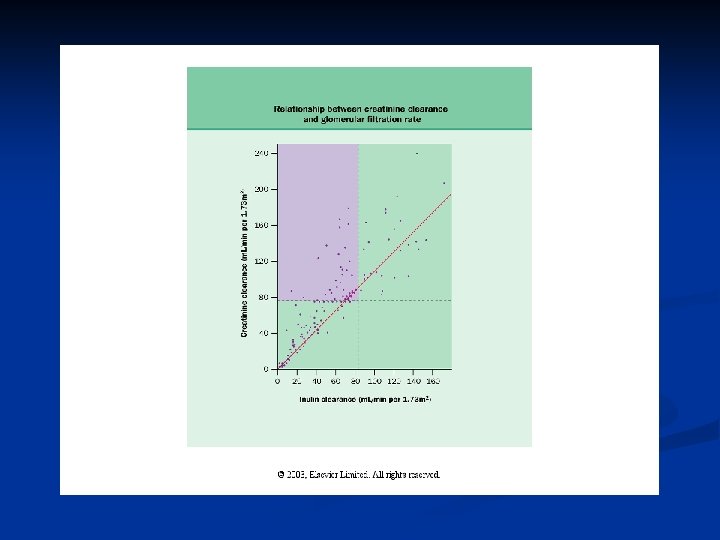
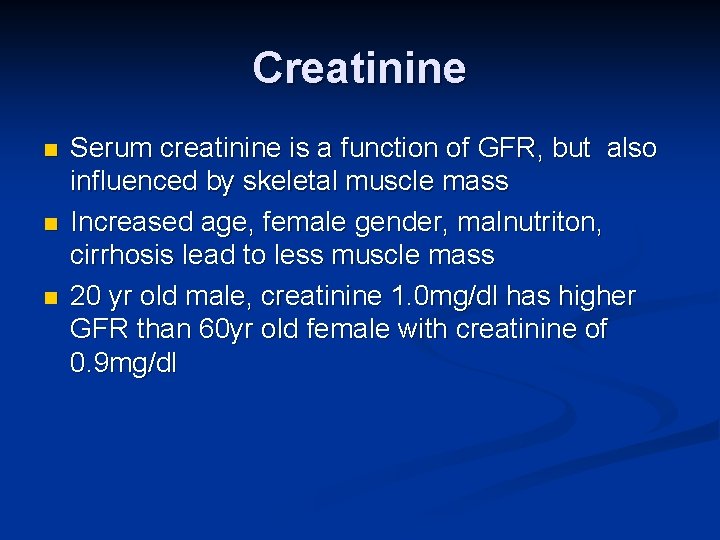
Creatinine n n n Serum creatinine is a function of GFR, but also influenced by skeletal muscle mass Increased age, female gender, malnutriton, cirrhosis lead to less muscle mass 20 yr old male, creatinine 1. 0 mg/dl has higher GFR than 60 yr old female with creatinine of 0. 9 mg/dl
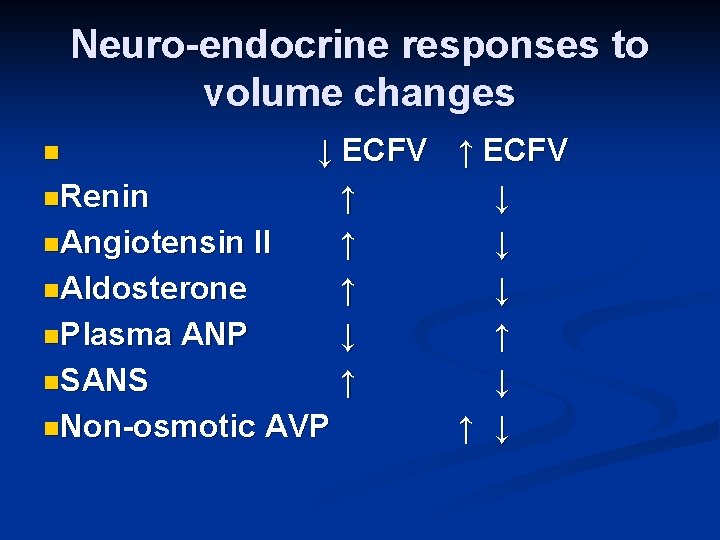
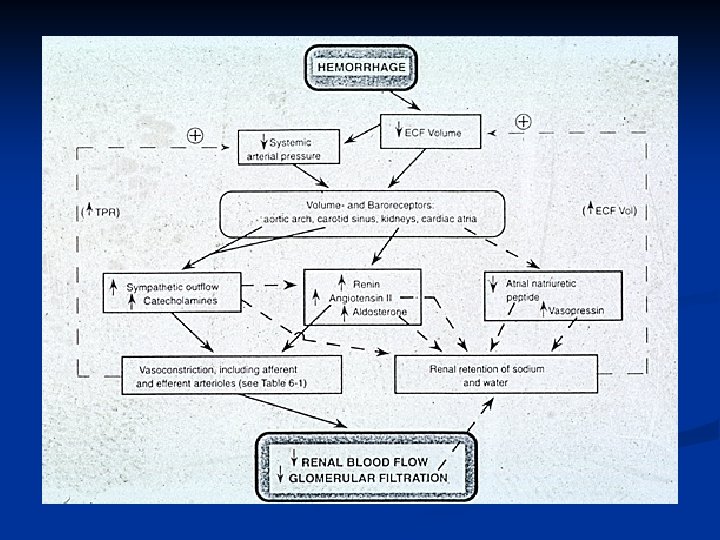
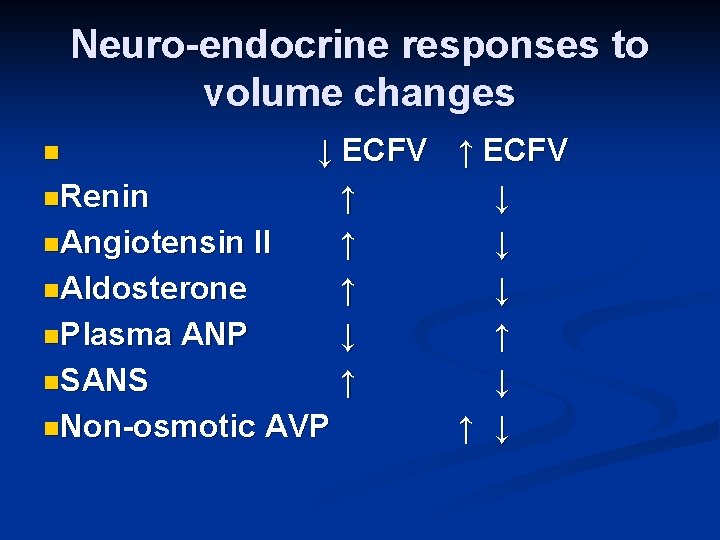
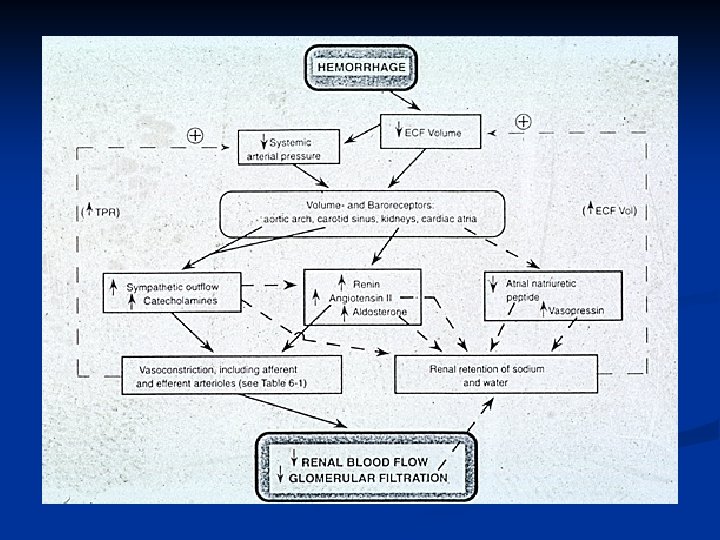
Neuro-endocrine responses to volume changes ↓ ECFV ↑ ECFV n. Renin ↑ ↓ n. Angiotensin II ↑ ↓ n. Aldosterone ↑ ↓ n. Plasma ANP ↓ ↑ n. SANS ↑ ↓ n. Non-osmotic AVP ↑ ↓ n
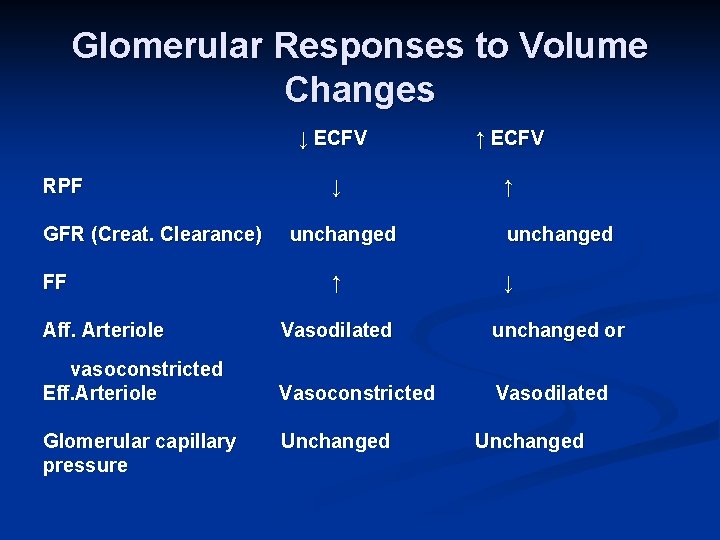
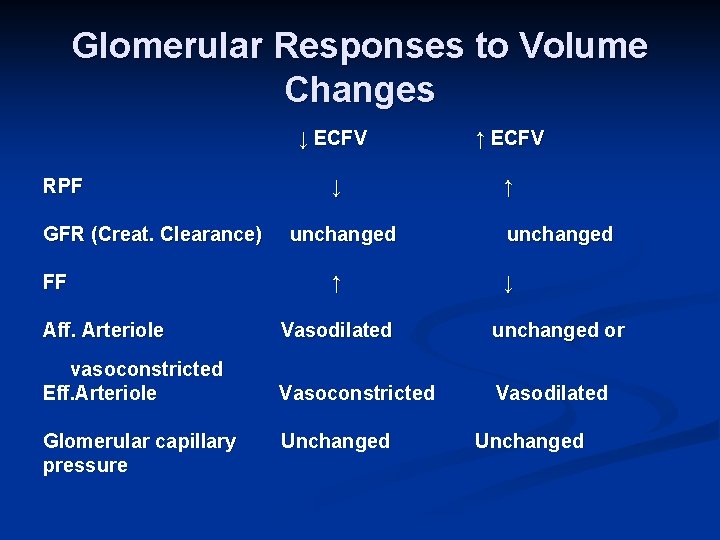
Glomerular Responses to Volume Changes RPF GFR (Creat. Clearance) FF ↓ ECFV ↑ ECFV ↓ ↑ unchanged ↓ Aff. Arteriole Vasodilated unchanged or vasoconstricted Eff. Arteriole Vasoconstricted Vasodilated Glomerular capillary pressure Unchanged
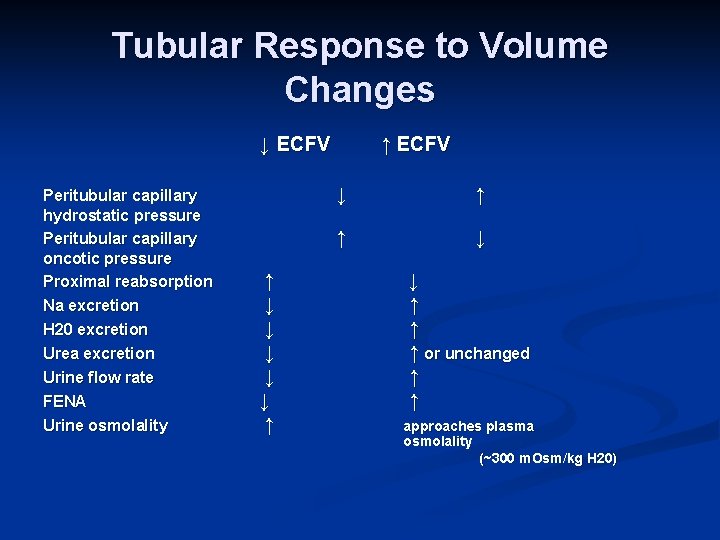
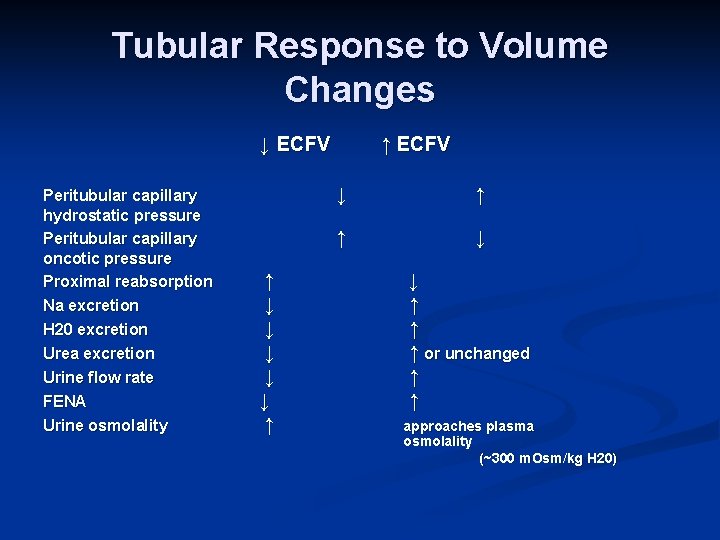
Tubular Response to Volume Changes ↓ ECFV Peritubular capillary hydrostatic pressure Peritubular capillary oncotic pressure Proximal reabsorption Na excretion H 20 excretion Urea excretion Urine flow rate FENA Urine osmolality ↑ ↓ ↓ ↓ ↑ ↑ ECFV ↓ ↑ ↑ ↓ ↓ ↑ ↑ ↑ or unchanged ↑ ↑ approaches plasma osmolality (~300 m. Osm/kg H 20)