OVARY AND MAMMARY GLAND Dr Iram Tassaduq OVARIES


























- Slides: 46


OVARY AND MAMMARY GLAND Dr Iram Tassaduq

OVARIES • Ovarian ligament • Suspensory ligament • Mesovarium

FUNCTIONS OF OVARIES 1. Ova production 2. Hormone production
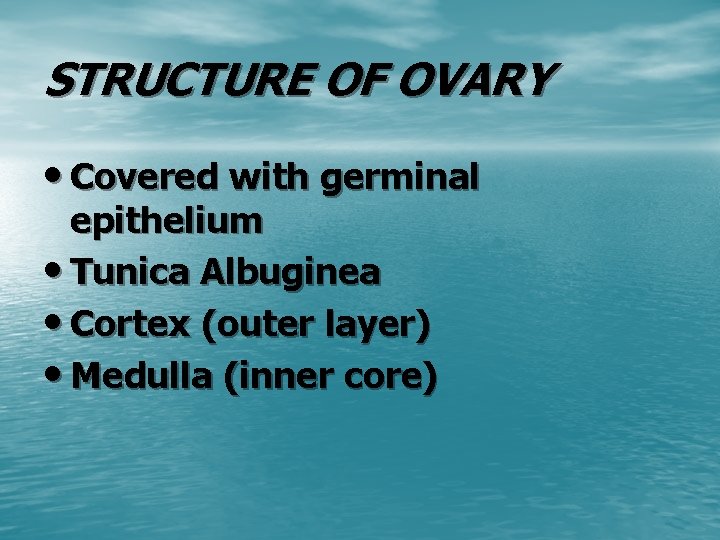
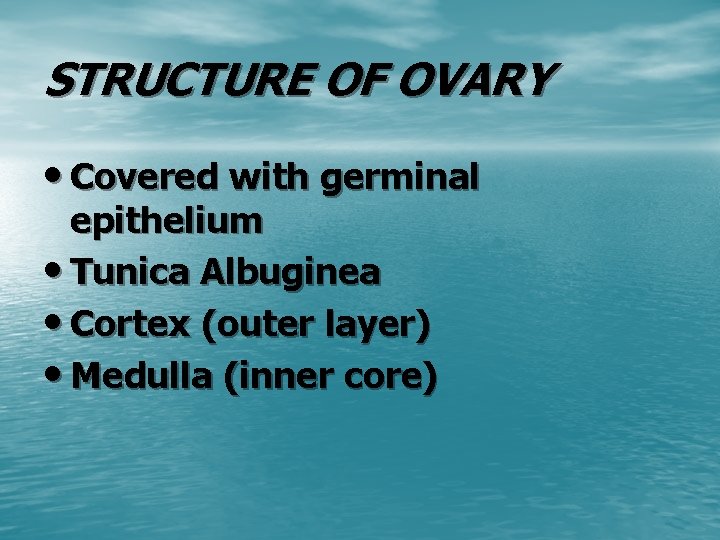
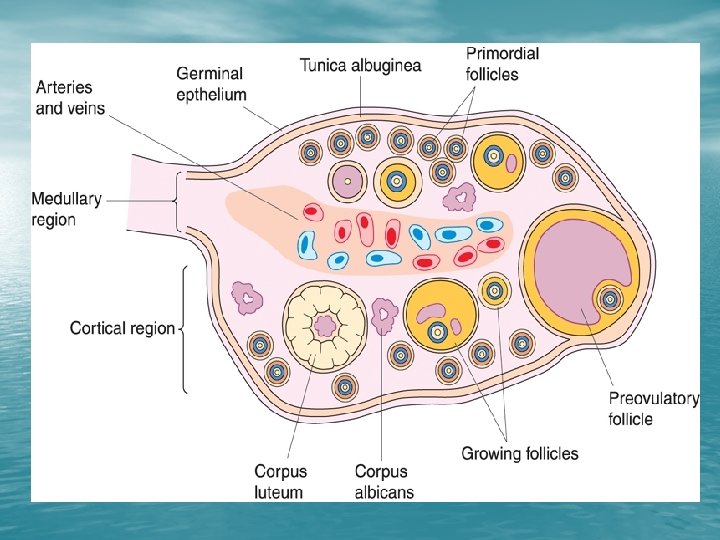
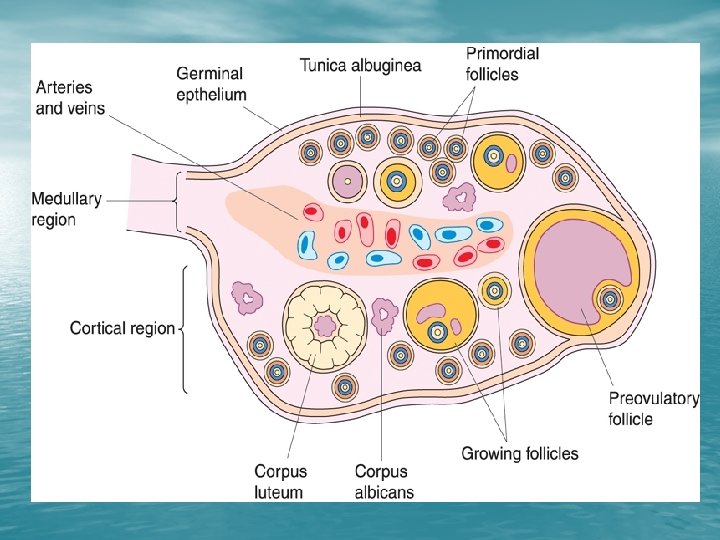
STRUCTURE OF OVARY • Covered with germinal epithelium • Tunica Albuginea • Cortex (outer layer) • Medulla (inner core)

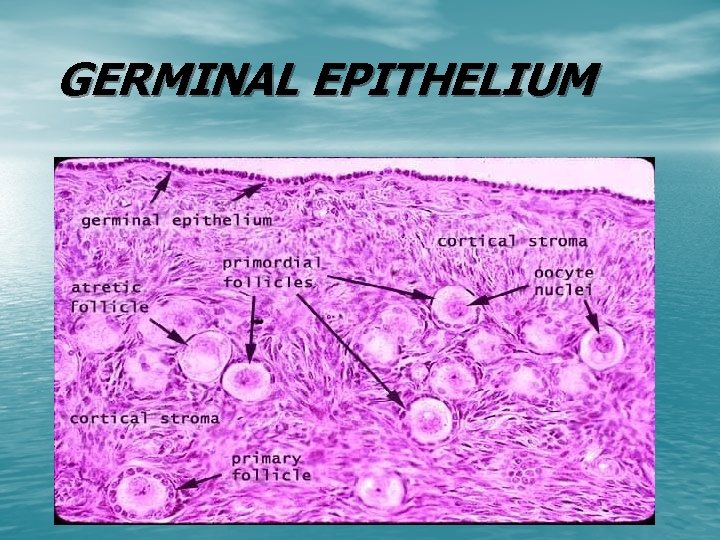
GERMINAL EPITHELIUM • Surface epithelium having a single layer of columnar or cuboidal cells
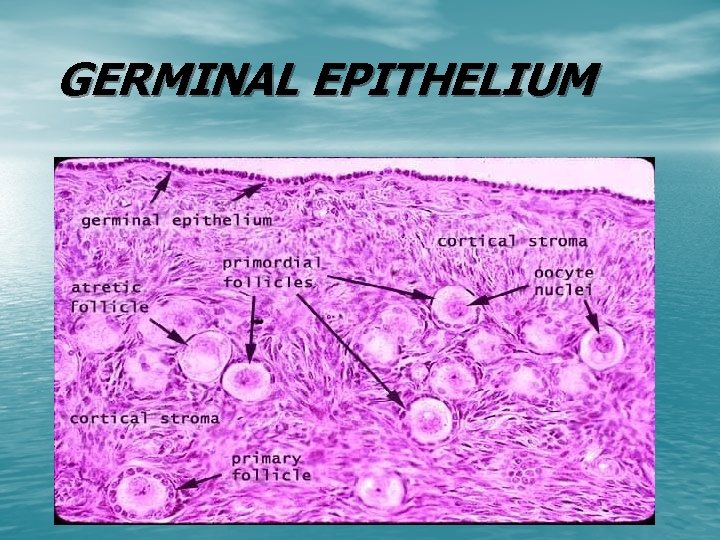
GERMINAL EPITHELIUM
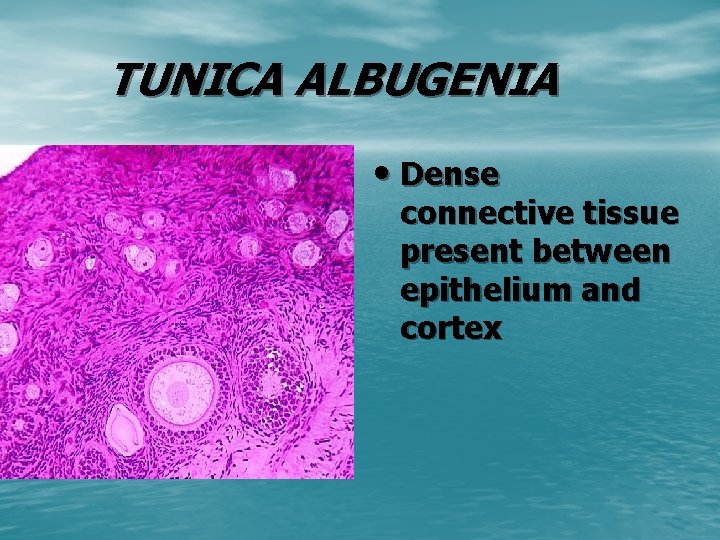
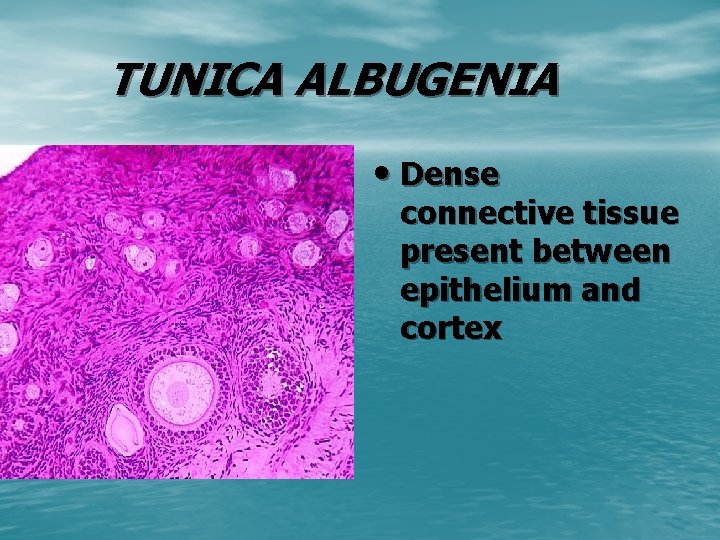
TUNICA ALBUGENIA • Dense connective tissue present between epithelium and cortex

CORTEX

CORTEX • Outer zone • Contains follicles and smooth muscle fibres • Only primordial and primary follicles before puberty
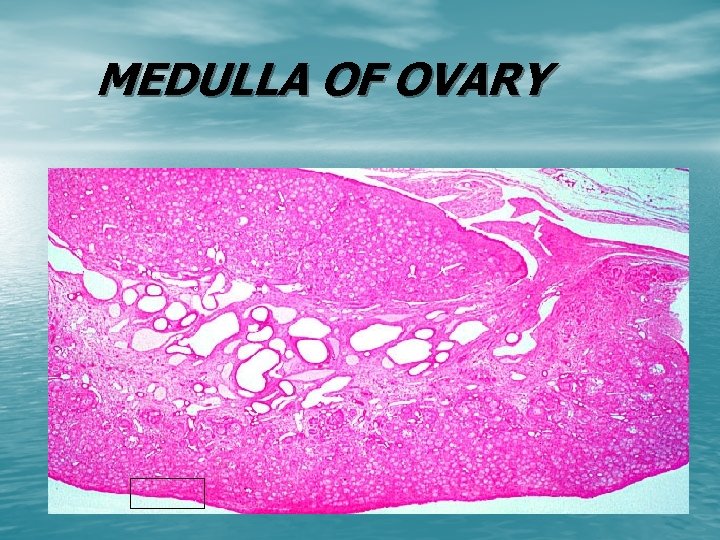
MEDULLA • Inner zone • Contains loose , connective tissue, blood vessels , lymphatics and nerves
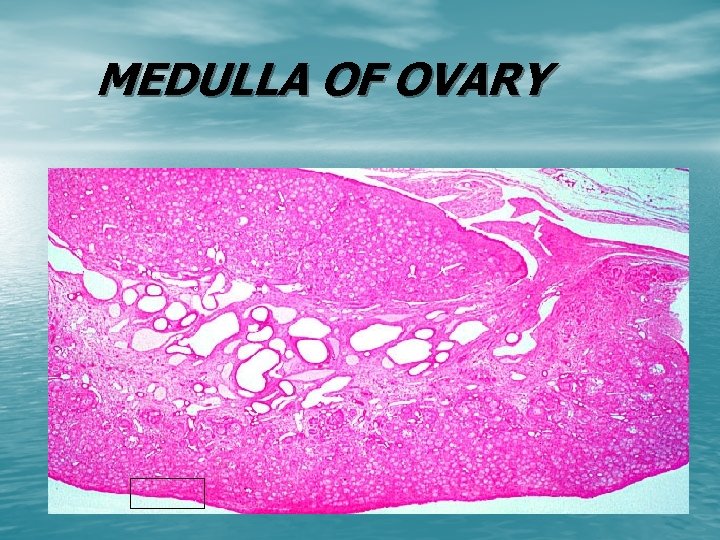
MEDULLA OF OVARY

TYPES OF OVARIAN FOLLICLES • Primordial Follicle • Growing Follicle/Antral Follicles 1. Primary Follicle 2. Secondary Follicle • Mature /Graffian Follicle


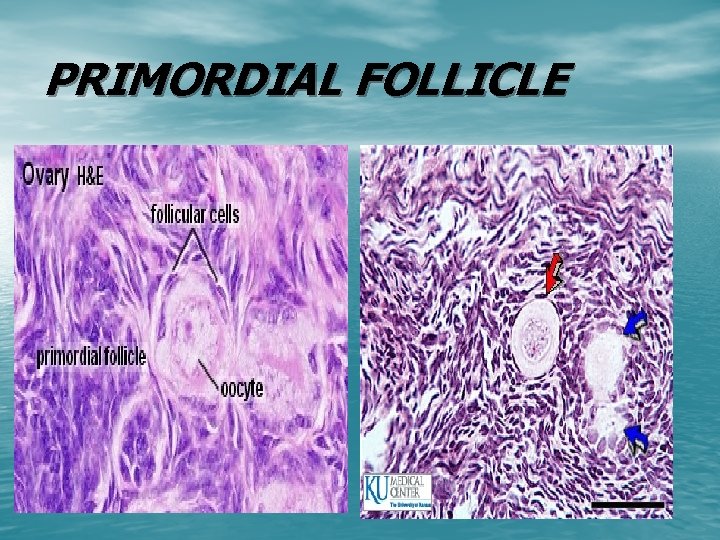
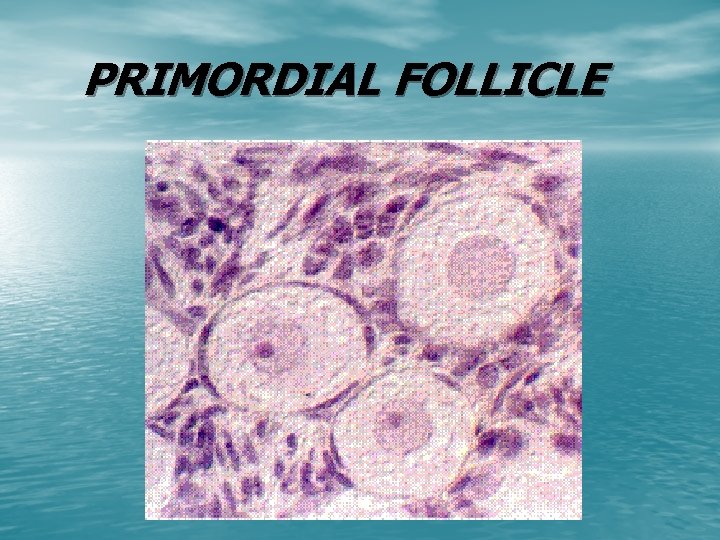
PRIMORDIAL FOLLICLE • Earliest stage of development • Independent of gonadotrophin stimulation • Oocyte is 30 micrometer
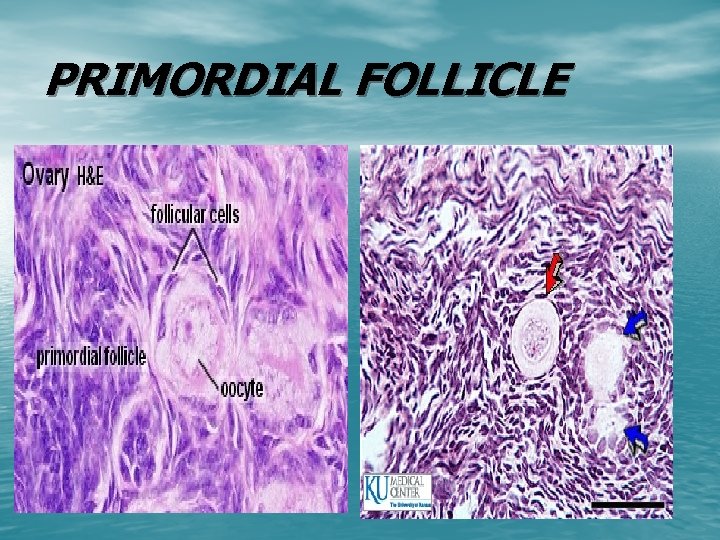
PRIMORDIAL FOLLICLE
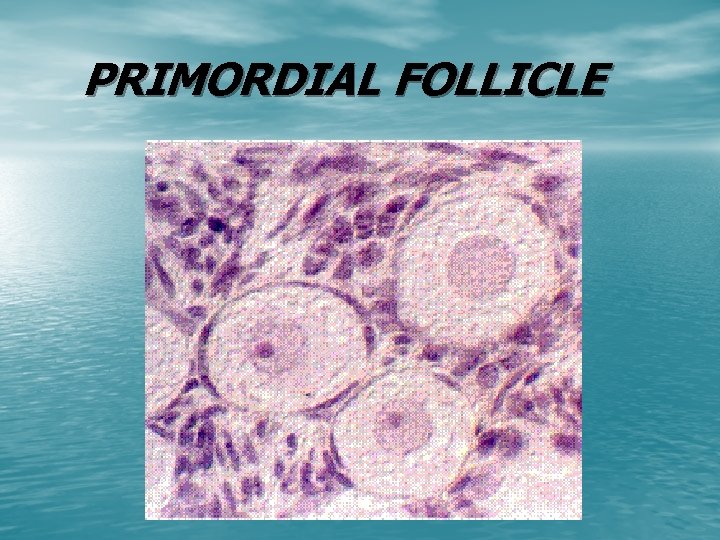
PRIMORDIAL FOLLICLE

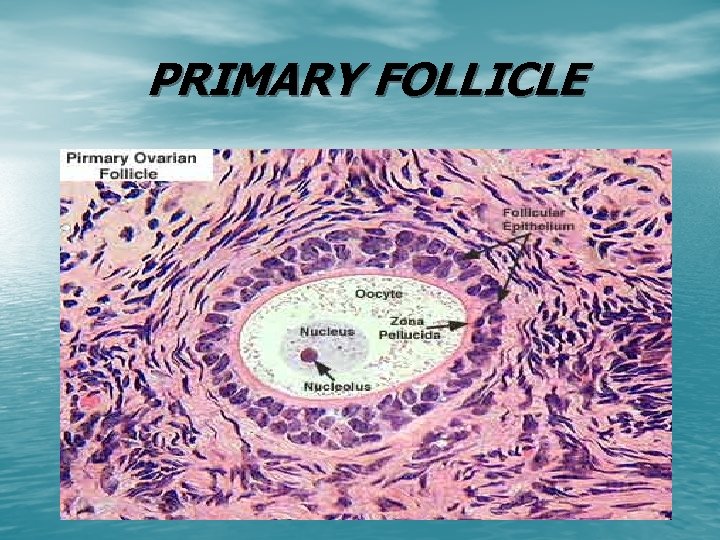
PRIMARY FOLLICLE • Changes in oocyte , follicular cells and stroma • Follicular cells become cuboidal • Zona pellucida appears between oocyte and follicles • Oocyte size 50 to 80 micrometer • Basal lamina separates the follicle from stroma
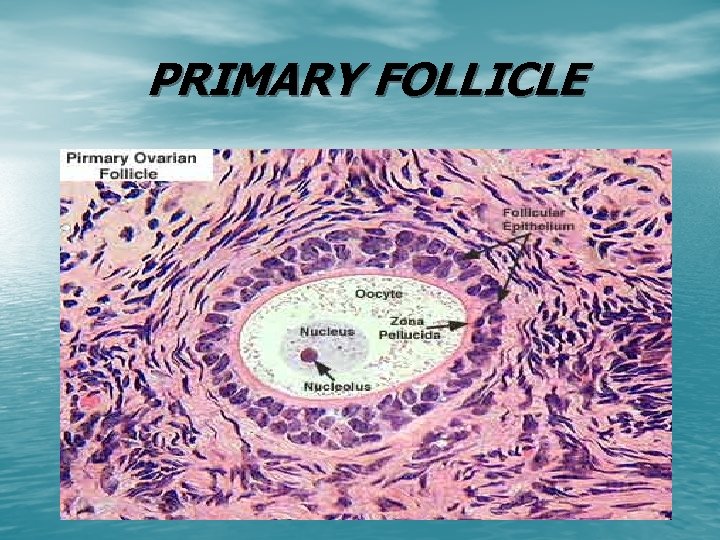
PRIMARY FOLLICLE
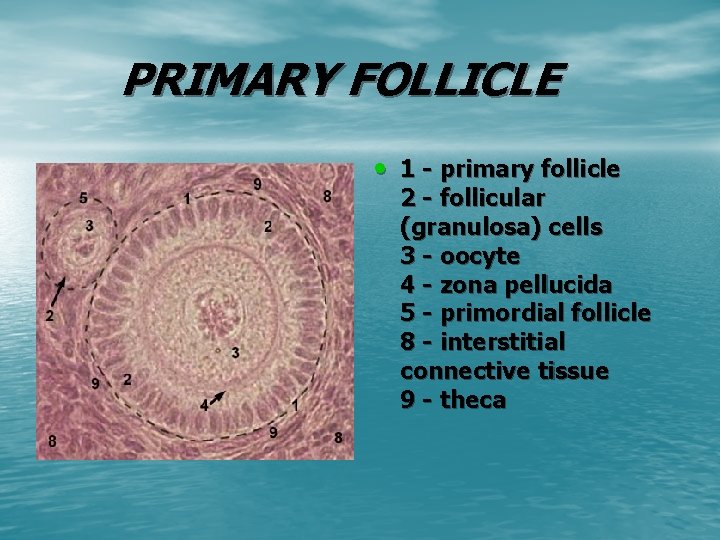
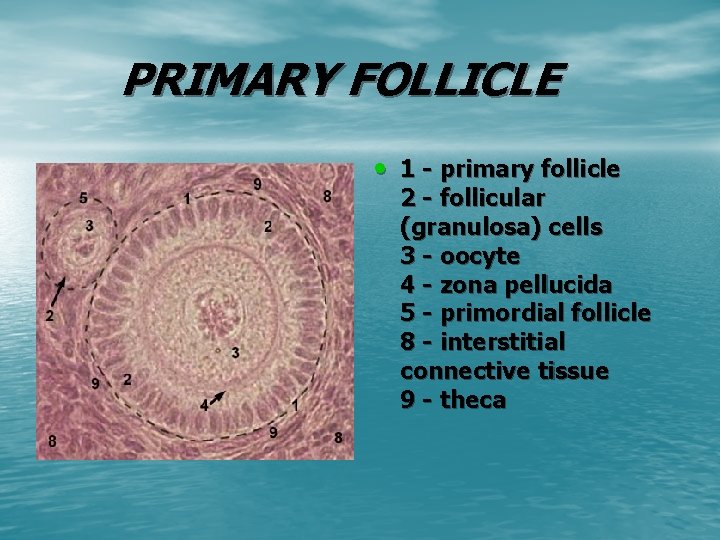
PRIMARY FOLLICLE • 1 - primary follicle 2 - follicular (granulosa) cells 3 - oocyte 4 - zona pellucida 5 - primordial follicle 8 - interstitial connective tissue 9 - theca
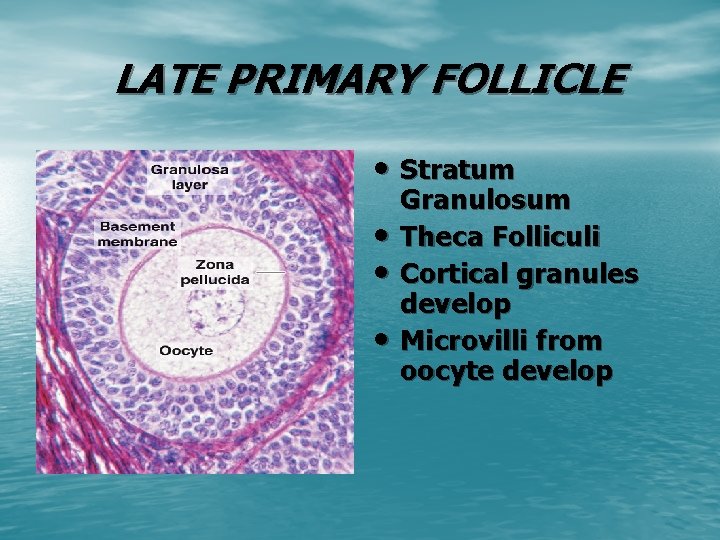
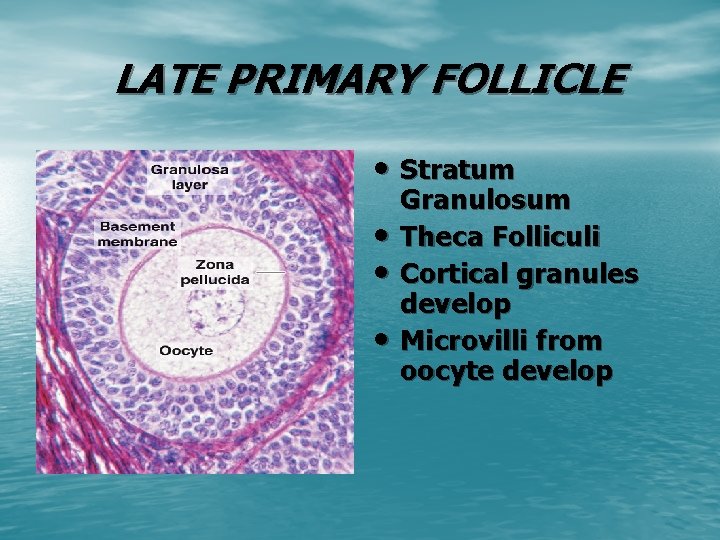
LATE PRIMARY FOLLICLE • Stratum • • • Granulosum Theca Folliculi Cortical granules develop Microvilli from oocyte develop

Stratum Granulosum • Stratified • • epithelium appear due to proliferation of follicle cells Outermost layer is columnar Gap junctions between granulosa cells
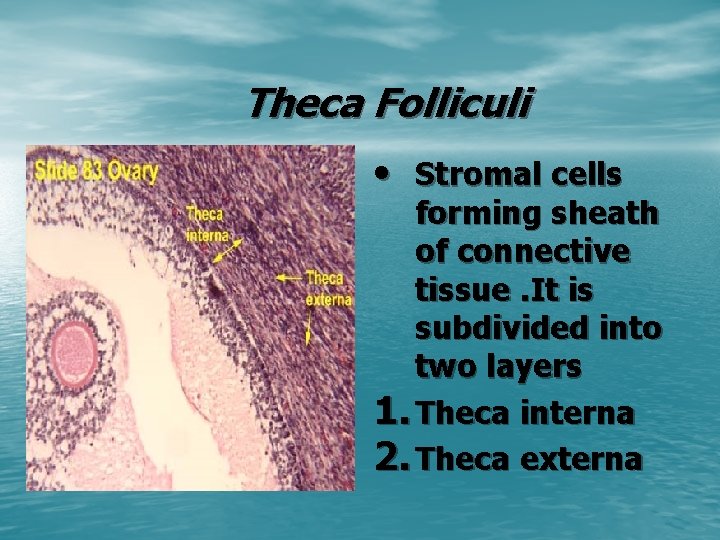
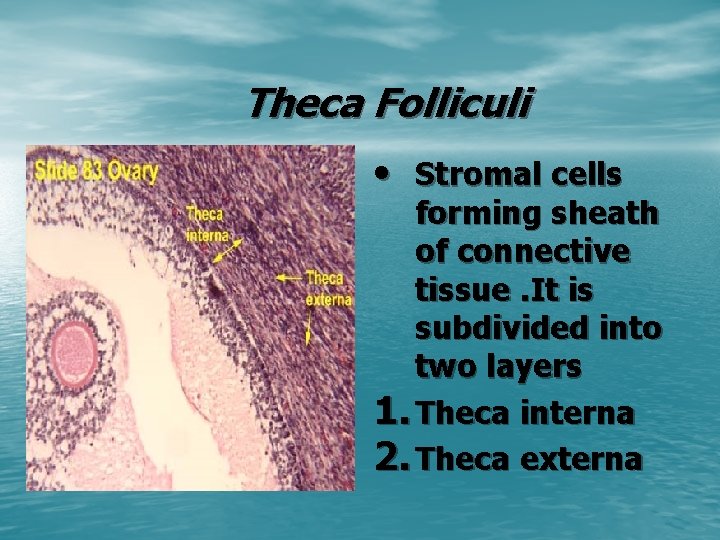
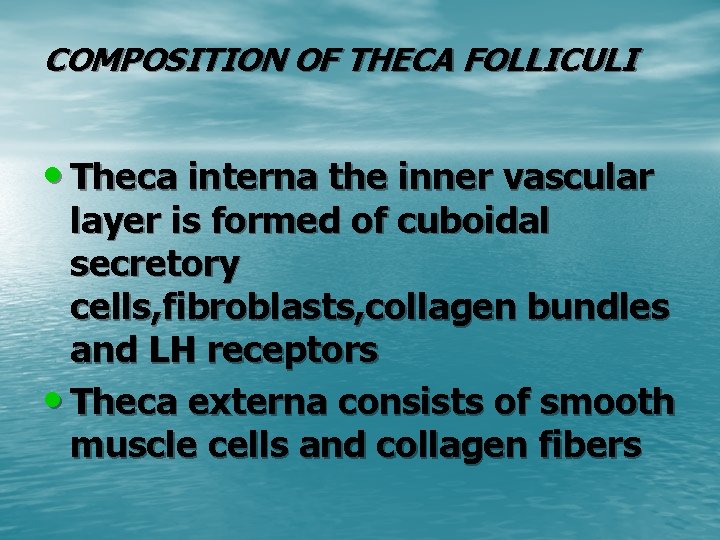
Theca Folliculi • Stromal cells forming sheath of connective tissue. It is subdivided into two layers 1. Theca interna 2. Theca externa
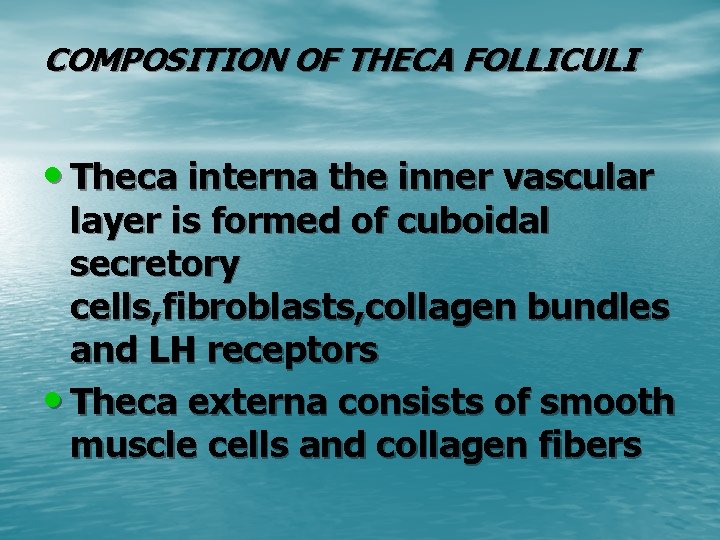
COMPOSITION OF THECA FOLLICULI • Theca interna the inner vascular layer is formed of cuboidal secretory cells, fibroblasts, collagen bundles and LH receptors • Theca externa consists of smooth muscle cells and collagen fibers
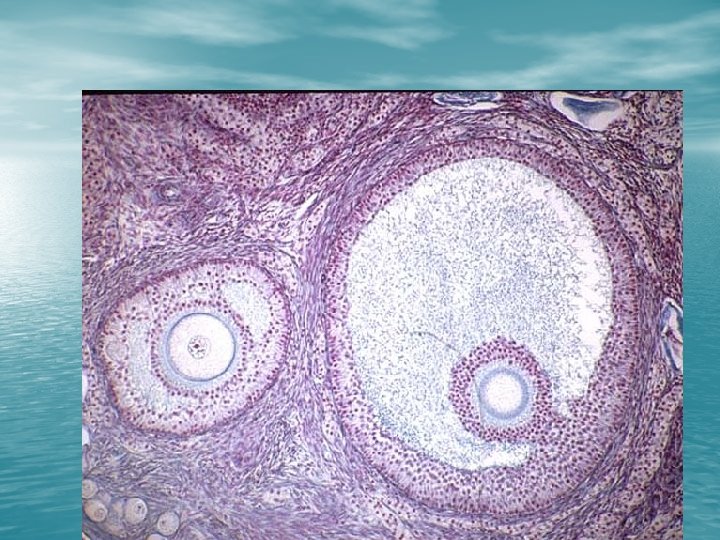
SECONDARY FOLLICLE • Few relative to number of primary follicles • Produce follicular fluid • Rapid enlargement • Cumulus Oophorus


Secondary Follicle
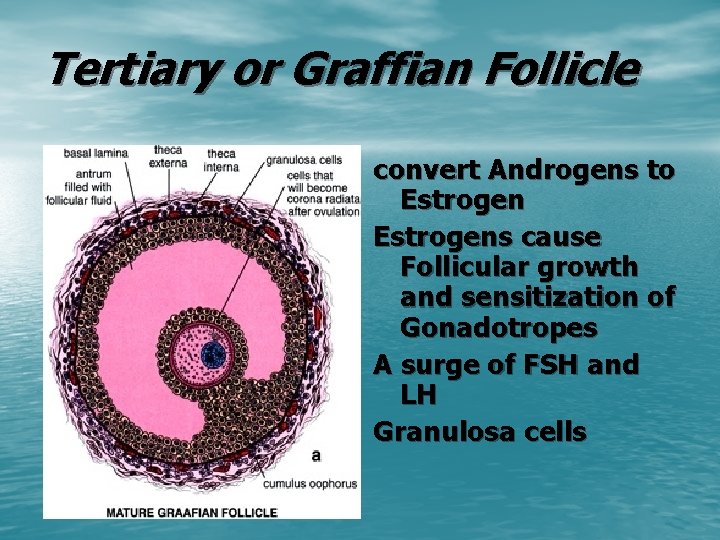
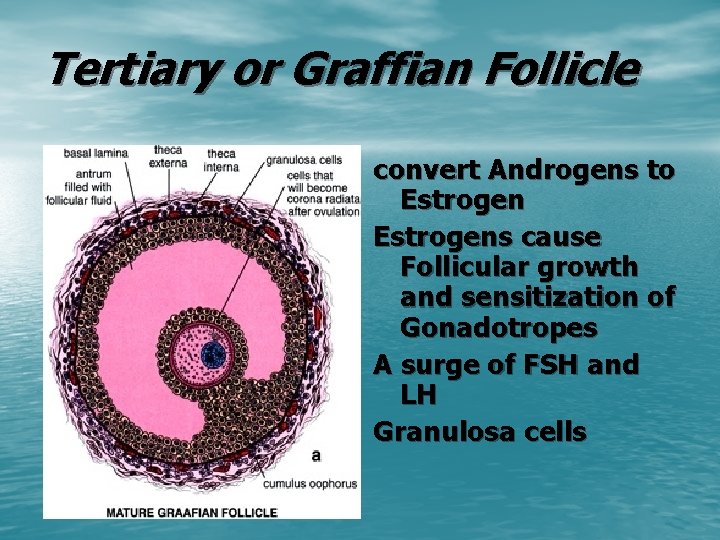
Tertiary or Graffian Follicle convert Androgens to Estrogens cause Follicular growth and sensitization of Gonadotropes A surge of FSH and LH Granulosa cells

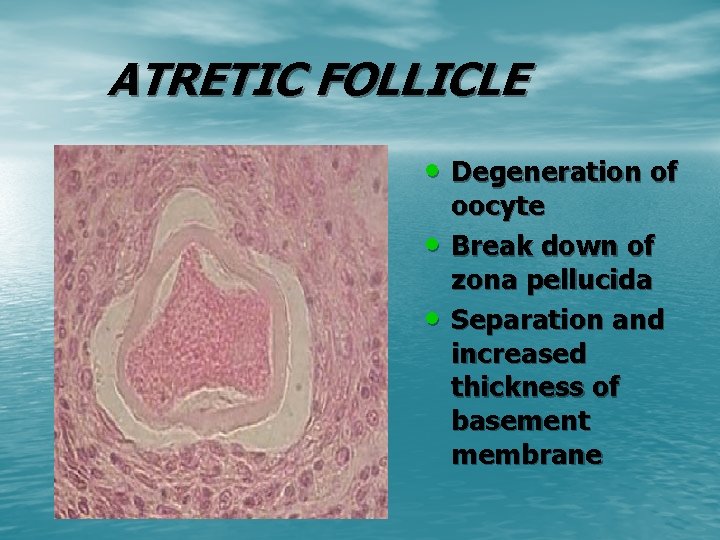
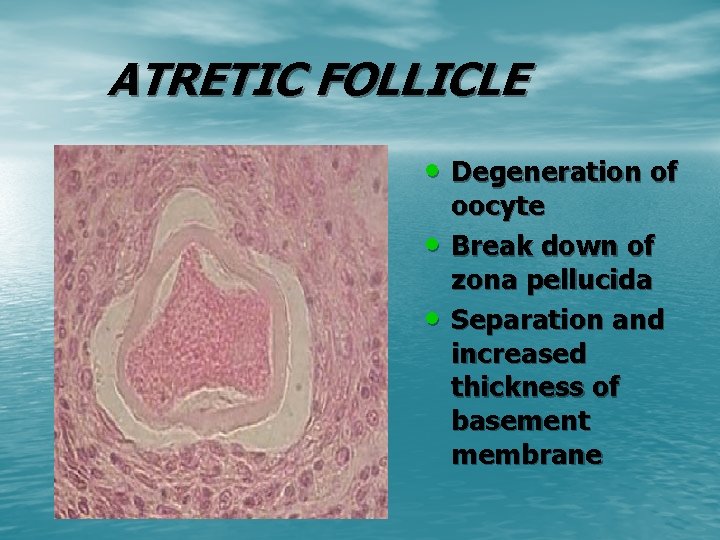
ATRETIC FOLLICLE • Degeneration of • • oocyte Break down of zona pellucida Separation and increased thickness of basement membrane

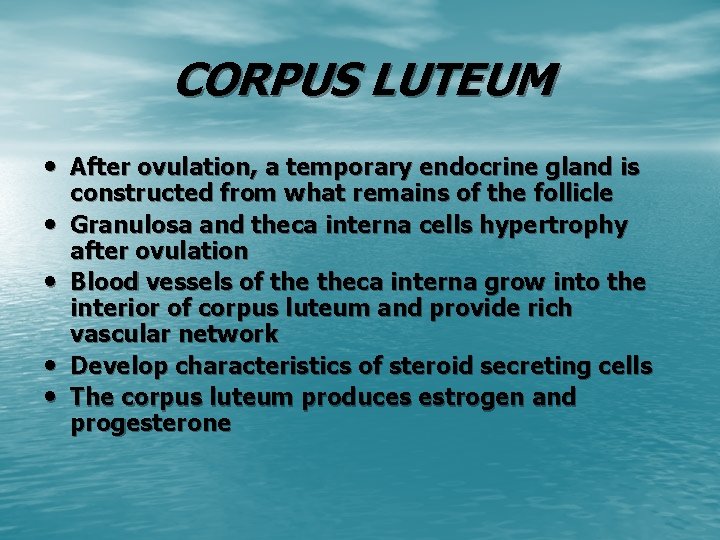
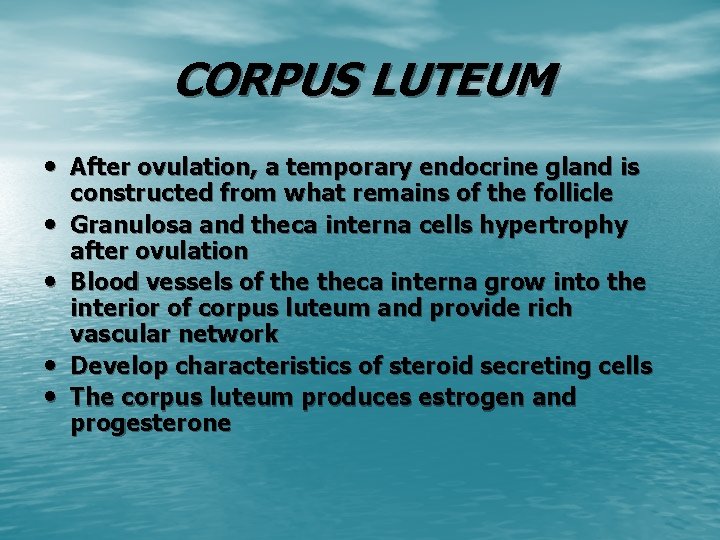
CORPUS LUTEUM • After ovulation, a temporary endocrine gland is • • constructed from what remains of the follicle Granulosa and theca interna cells hypertrophy after ovulation Blood vessels of theca interna grow into the interior of corpus luteum and provide rich vascular network Develop characteristics of steroid secreting cells The corpus luteum produces estrogen and progesterone



CORPUS LUTEUM v Theca lutein cells • Smaller in size , contain dark staining nuclei v Granulosa lutein cells • Large pale staining cells with large vesicular nuclei • Form a thick folded layer

CORPUS ALBICANS • Degenerated Corpus Luteum • large masses of amorphous eosinophilic staining material • Low cellularity. • Collagenous scar tissue that has filled the space occupied by the corpus luteum.

CORPUS ALBICANS



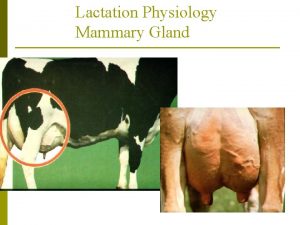
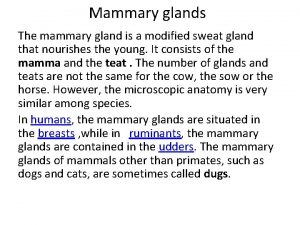
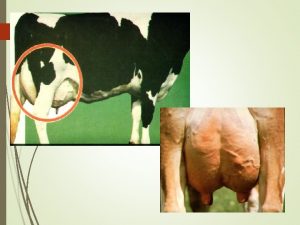
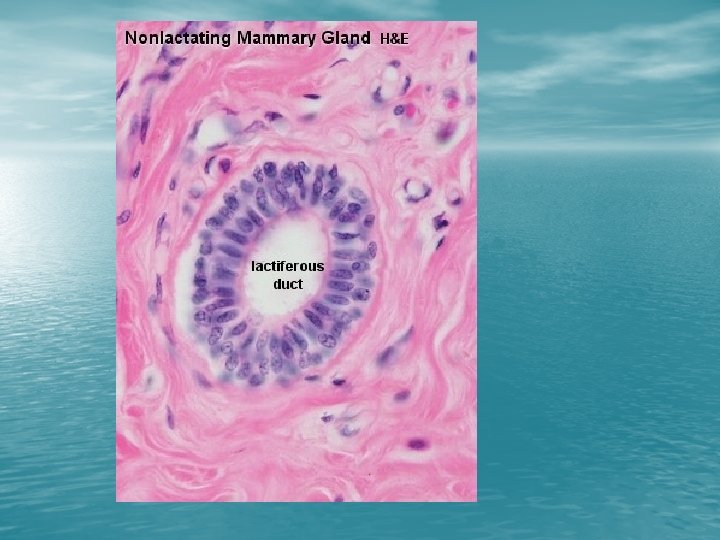
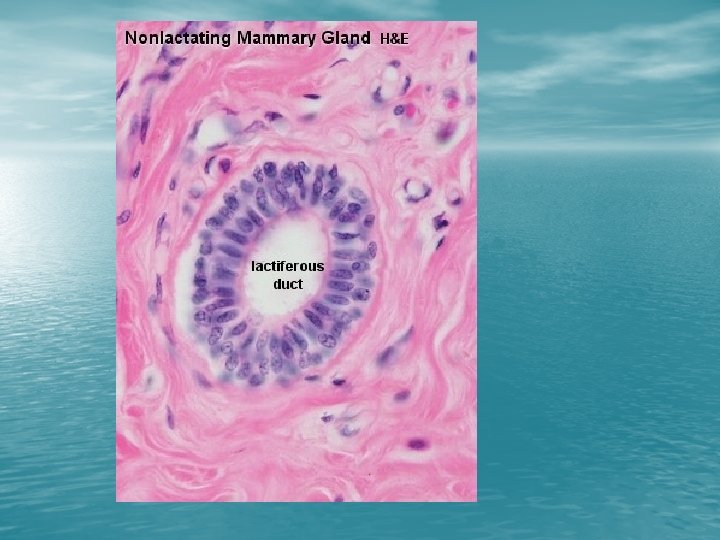
INACTIVE MAMMARY GLAND • Sparse glandular • tissue Consist of tubules having the appearance of ducts
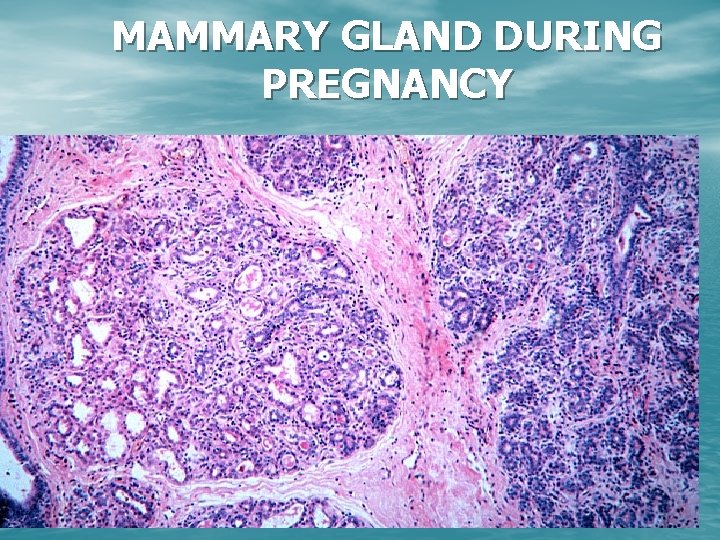
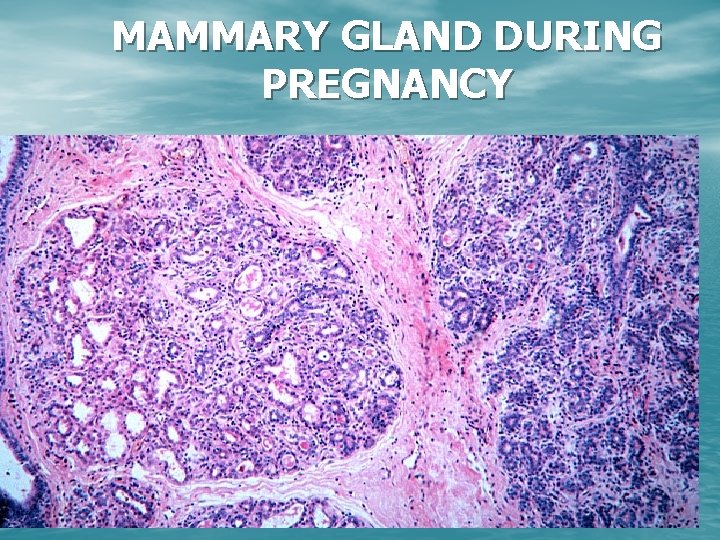
MAMMARY GLAND DURING PREGNANCY


 Supraglenoid gland
Supraglenoid gland Kow kant kick
Kow kant kick Mons pubis model
Mons pubis model Alveoli
Alveoli Mamma non lactans
Mamma non lactans Pituitary gland and pineal gland spiritual
Pituitary gland and pineal gland spiritual Pineal gland pituitary gland
Pineal gland pituitary gland Distinguish between ova, ovaries, and ovulation
Distinguish between ova, ovaries, and ovulation It has fur and mammary glands
It has fur and mammary glands Functions of the ovaries
Functions of the ovaries Gonads in squid
Gonads in squid Tunica albuginea of ovary
Tunica albuginea of ovary Conical breast shape
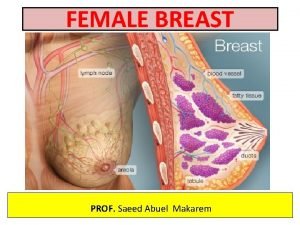
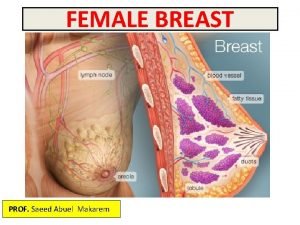
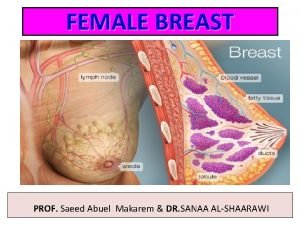
Conical breast shape Blood supply of the breast
Blood supply of the breast Blood supply of the breast
Blood supply of the breast Mammary ridge
Mammary ridge How to determine gender of fetal pig
How to determine gender of fetal pig Pig male reproductive system
Pig male reproductive system Milk is continually secreted into the mammary acini
Milk is continually secreted into the mammary acini Upper outer quadrant of the breast pictures
Upper outer quadrant of the breast pictures Cynocephalus variegatus
Cynocephalus variegatus Convert the venn diagram into a cladogram
Convert the venn diagram into a cladogram Mammary crest
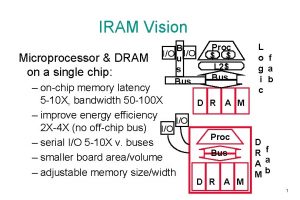
Mammary crest Iram 3801
Iram 3801 Istoreos
Istoreos Iram aron
Iram aron Norma iram 3610:2015
Norma iram 3610:2015 Iram 2325
Iram 2325 Iram 3620 casco de seguridad para uso industrial
Iram 3620 casco de seguridad para uso industrial Ikev
Ikev Iram 3626-2004
Iram 3626-2004 Iram 3625
Iram 3625 Iram
Iram Normas iram cursogramas
Normas iram cursogramas Iram software
Iram software Iram grenoble
Iram grenoble Difference between ovary and ovule
Difference between ovary and ovule Difference between ovule and ovary
Difference between ovule and ovary Part of flower comprising stigma style and ovary
Part of flower comprising stigma style and ovary Rotterdam criteria for pcos
Rotterdam criteria for pcos Ovarian ligament
Ovarian ligament Female external reproductive system
Female external reproductive system Pollination in hibiscus flower
Pollination in hibiscus flower Icd 10 metroragia
Icd 10 metroragia Flower parts and functions
Flower parts and functions Chicken ovary function
Chicken ovary function Primary follicle function
Primary follicle function