Scleroderma and Inflammatory Myositis Kathryn Dao MD Arthritis

![DDX of Tight Skin n n Pseudosclerodactyly ] IDDM, Hypothyroidism Drugs: Tryptophan, bleomycin, pentazocine, DDX of Tight Skin n n Pseudosclerodactyly ] IDDM, Hypothyroidism Drugs: Tryptophan, bleomycin, pentazocine,](https://slidetodoc.com/presentation_image/0aff954a635d8b9be45431ecb1571192/image-6.jpg)
![ACR Systemic Sclerosis Preliminary Classification Criteria* n Major Criterion ] Proximal n Scleroderma Minor ACR Systemic Sclerosis Preliminary Classification Criteria* n Major Criterion ] Proximal n Scleroderma Minor](https://slidetodoc.com/presentation_image/0aff954a635d8b9be45431ecb1571192/image-8.jpg)
![Scleroderma A disorder of Collagen, Vessels ] ] n Small to medium-sized blood vessels, Scleroderma A disorder of Collagen, Vessels ] ] n Small to medium-sized blood vessels,](https://slidetodoc.com/presentation_image/0aff954a635d8b9be45431ecb1571192/image-11.jpg)


![Scleroderma Renal Crisis n Risk Factors ] diffuse skin involvement ] rapid progression of Scleroderma Renal Crisis n Risk Factors ] diffuse skin involvement ] rapid progression of](https://slidetodoc.com/presentation_image/0aff954a635d8b9be45431ecb1571192/image-23.jpg)
![DDX MYOPATHIIES n Toxic/Drugs ] n Infectious ] n n n Etoh, Cocaine, Steroids, DDX MYOPATHIIES n Toxic/Drugs ] n Infectious ] n n n Etoh, Cocaine, Steroids,](https://slidetodoc.com/presentation_image/0aff954a635d8b9be45431ecb1571192/image-39.jpg)
![NONMYOPATHIC CONSIDERATIONS n Fibromyalgia/Fibrositis/Myofascial n n Pain disorder Polymyalgia Rheumatica ] Caucasians, > 55 NONMYOPATHIC CONSIDERATIONS n Fibromyalgia/Fibrositis/Myofascial n n Pain disorder Polymyalgia Rheumatica ] Caucasians, > 55](https://slidetodoc.com/presentation_image/0aff954a635d8b9be45431ecb1571192/image-40.jpg)






- Slides: 64
Scleroderma and Inflammatory Myositis Kathryn Dao, MD Arthritis Center February 16, 2006
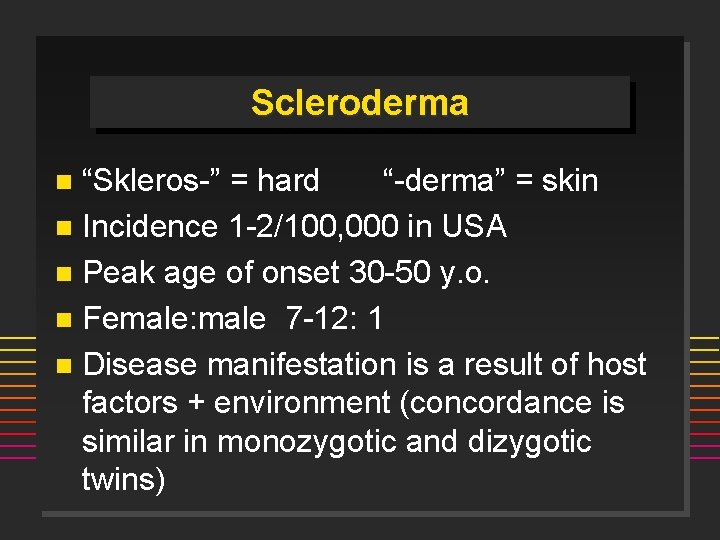
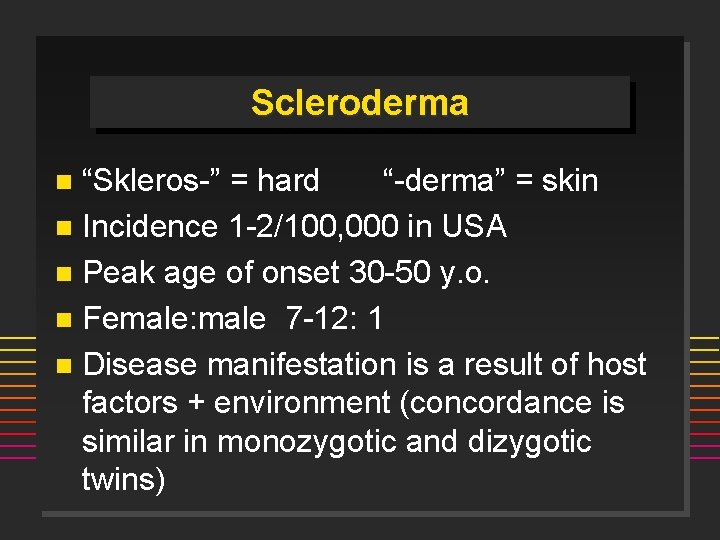
Scleroderma “Skleros-” = hard “-derma” = skin n Incidence 1 -2/100, 000 in USA n Peak age of onset 30 -50 y. o. n Female: male 7 -12: 1 n Disease manifestation is a result of host factors + environment (concordance is similar in monozygotic and dizygotic twins) n
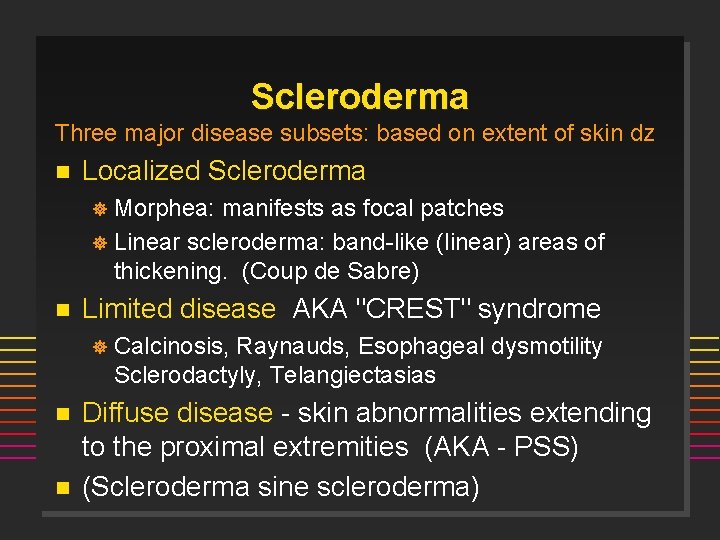
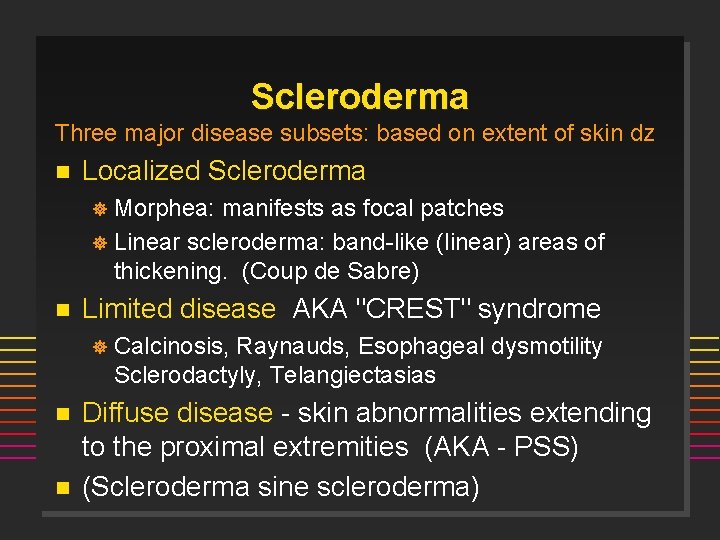
Scleroderma Three major disease subsets: based on extent of skin dz n Localized Scleroderma Morphea: manifests as focal patches ] Linear scleroderma: band-like (linear) areas of thickening. (Coup de Sabre) ] n Limited disease AKA "CREST" syndrome ] n n Calcinosis, Raynauds, Esophageal dysmotility Sclerodactyly, Telangiectasias Diffuse disease - skin abnormalities extending to the proximal extremities (AKA - PSS) (Scleroderma sine scleroderma)

![DDX of Tight Skin n n Pseudosclerodactyly IDDM Hypothyroidism Drugs Tryptophan bleomycin pentazocine DDX of Tight Skin n n Pseudosclerodactyly ] IDDM, Hypothyroidism Drugs: Tryptophan, bleomycin, pentazocine,](https://slidetodoc.com/presentation_image/0aff954a635d8b9be45431ecb1571192/image-6.jpg)
DDX of Tight Skin n n Pseudosclerodactyly ] IDDM, Hypothyroidism Drugs: Tryptophan, bleomycin, pentazocine, vinyl chloride, solvents Eosinophilic fasciitis Overlap syndromes Scleredema
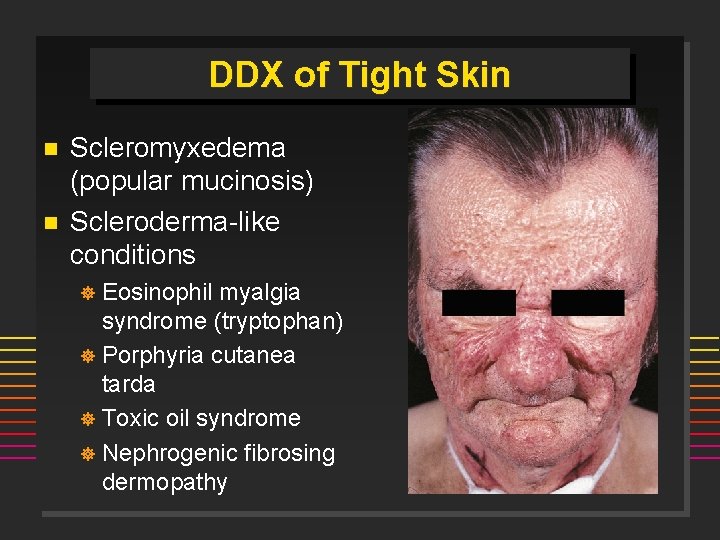
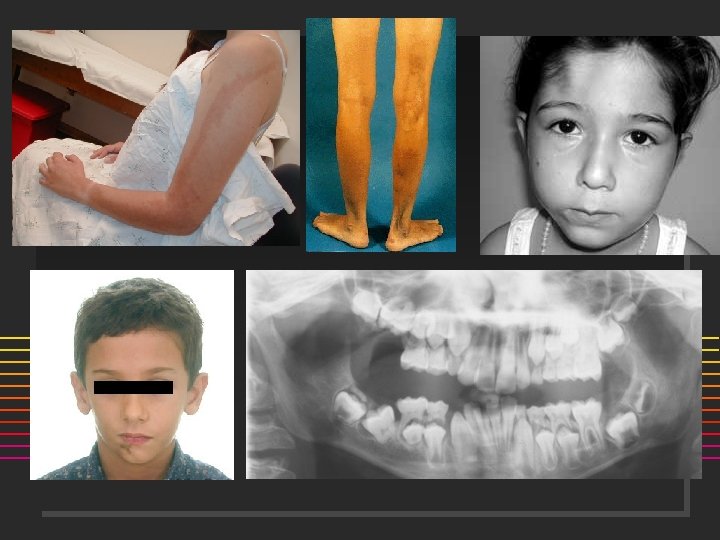
DDX of Tight Skin n n Scleromyxedema (popular mucinosis) Scleroderma-like conditions Eosinophil myalgia syndrome (tryptophan) ] Porphyria cutanea tarda ] Toxic oil syndrome ] Nephrogenic fibrosing dermopathy ]
![ACR Systemic Sclerosis Preliminary Classification Criteria n Major Criterion Proximal n Scleroderma Minor ACR Systemic Sclerosis Preliminary Classification Criteria* n Major Criterion ] Proximal n Scleroderma Minor](https://slidetodoc.com/presentation_image/0aff954a635d8b9be45431ecb1571192/image-8.jpg)
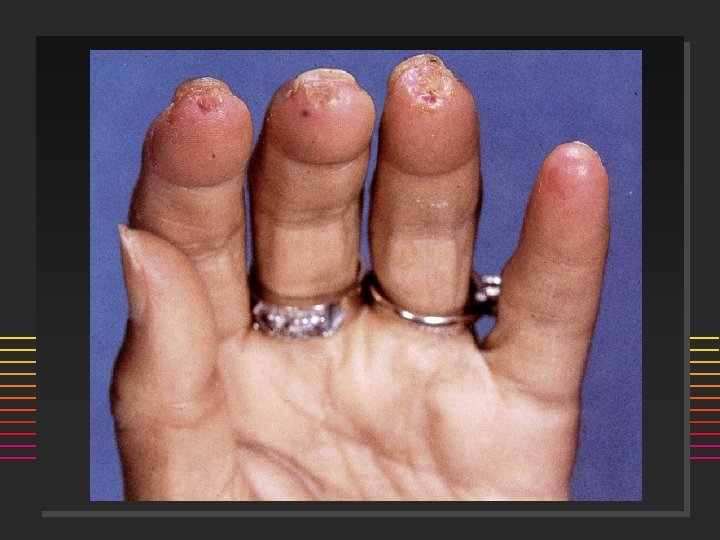
ACR Systemic Sclerosis Preliminary Classification Criteria* n Major Criterion ] Proximal n Scleroderma Minor Criteria ] Sclerodactyly ] Digital pitting or scars or loss of finger pad ] Bibasilar pulmonary fibrosis * One major and two minor required for diagnosis
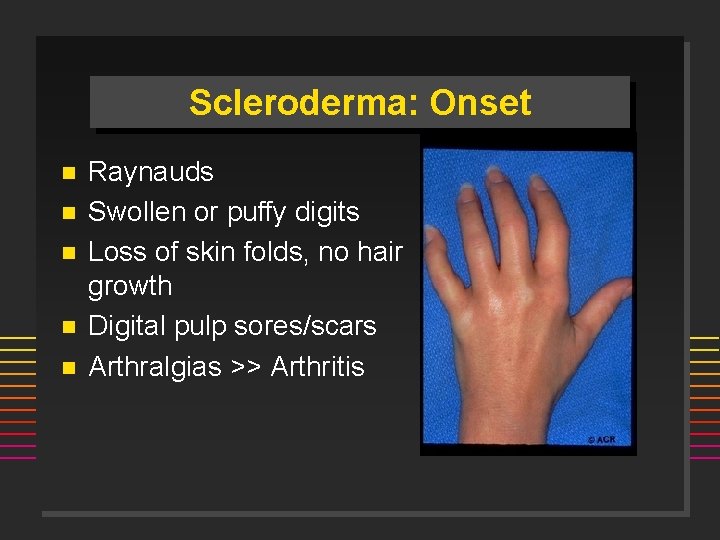
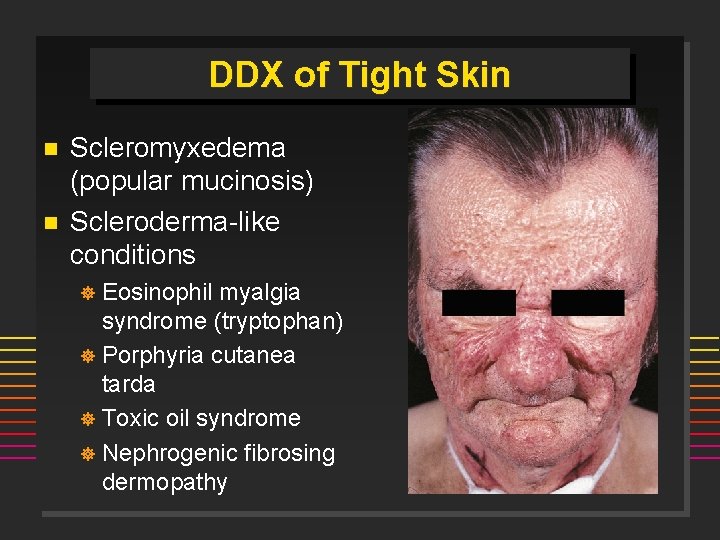
Scleroderma: Onset n n n Raynauds Swollen or puffy digits Loss of skin folds, no hair growth Digital pulp sores/scars Arthralgias >> Arthritis
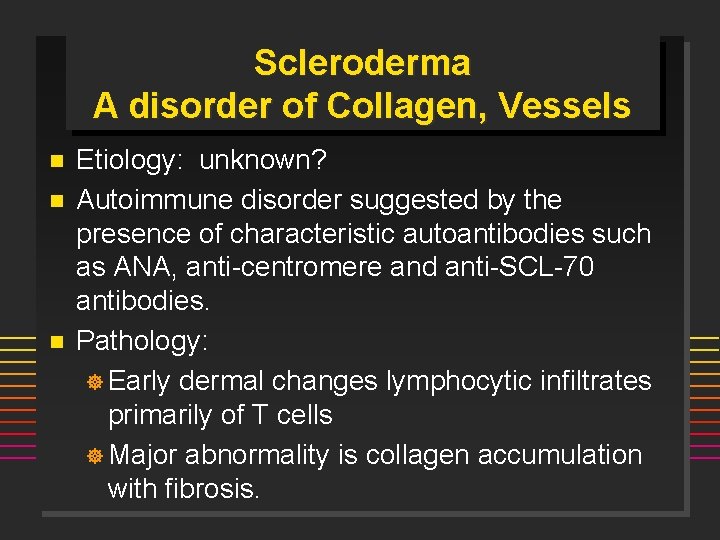
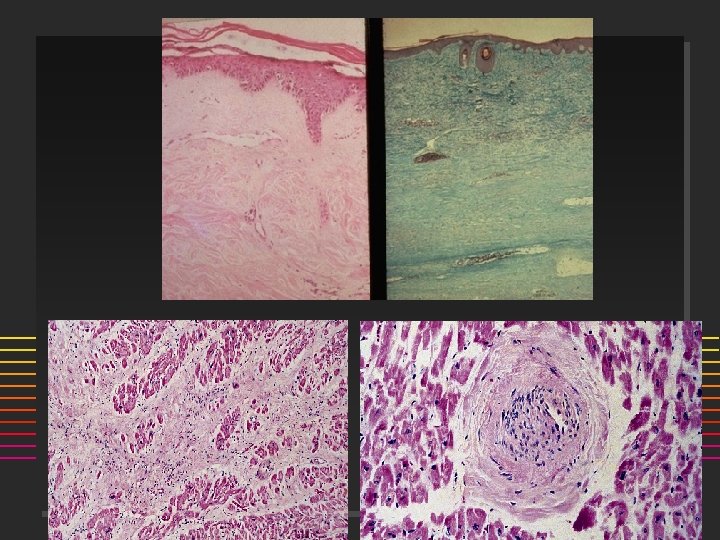
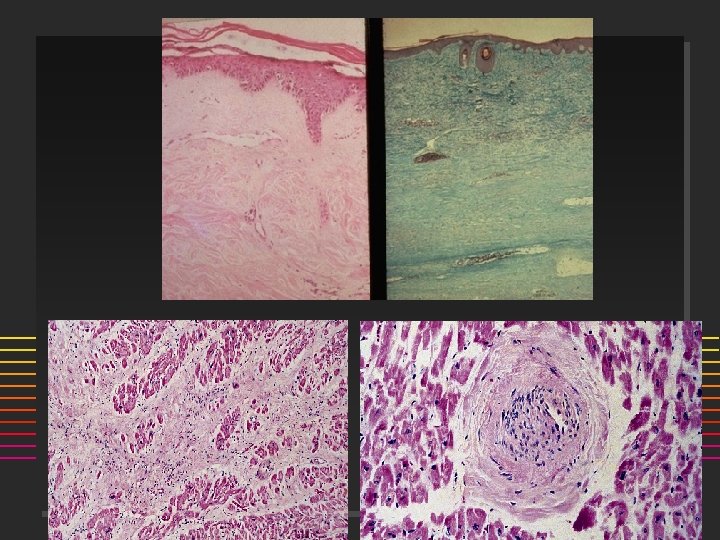
Scleroderma A disorder of Collagen, Vessels n n n Etiology: unknown? Autoimmune disorder suggested by the presence of characteristic autoantibodies such as ANA, anti-centromere and anti-SCL-70 antibodies. Pathology: ] Early dermal changes lymphocytic infiltrates primarily of T cells ] Major abnormality is collagen accumulation with fibrosis.
![Scleroderma A disorder of Collagen Vessels n Small to mediumsized blood vessels Scleroderma A disorder of Collagen, Vessels ] ] n Small to medium-sized blood vessels,](https://slidetodoc.com/presentation_image/0aff954a635d8b9be45431ecb1571192/image-11.jpg)
Scleroderma A disorder of Collagen, Vessels ] ] n Small to medium-sized blood vessels, which show bland fibrotic change Vasculopathy, NOT vasculitis! Small thrombi may form on the altered intimal surfaces. Microvascular disease Cold Normal PSS
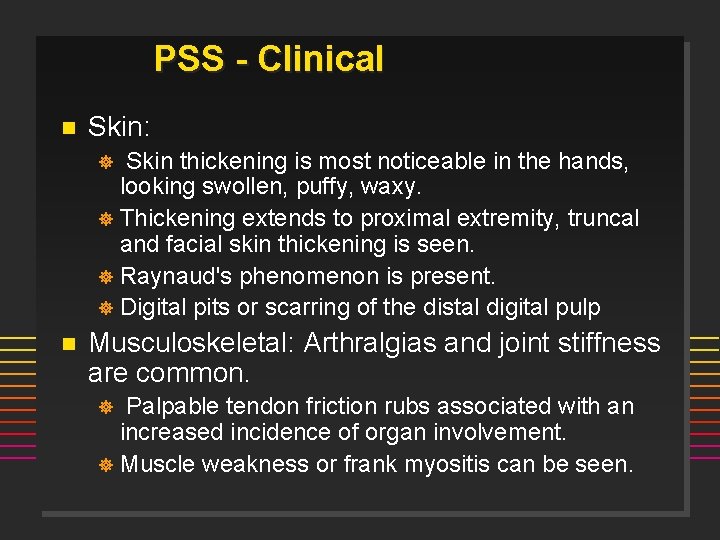
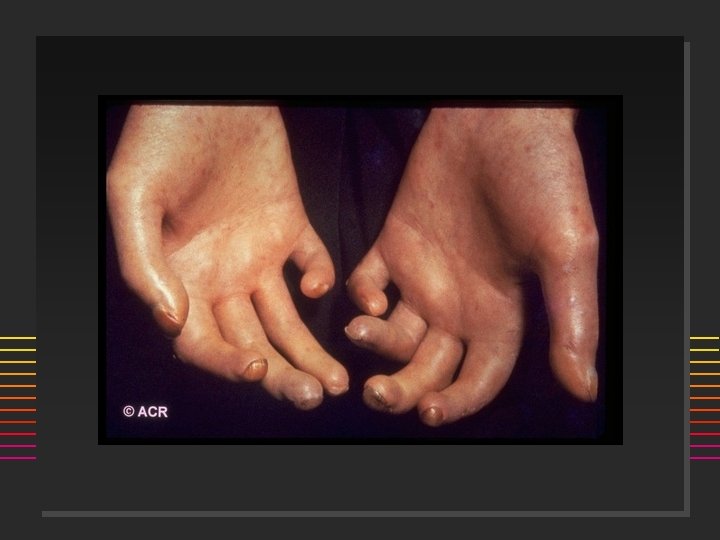
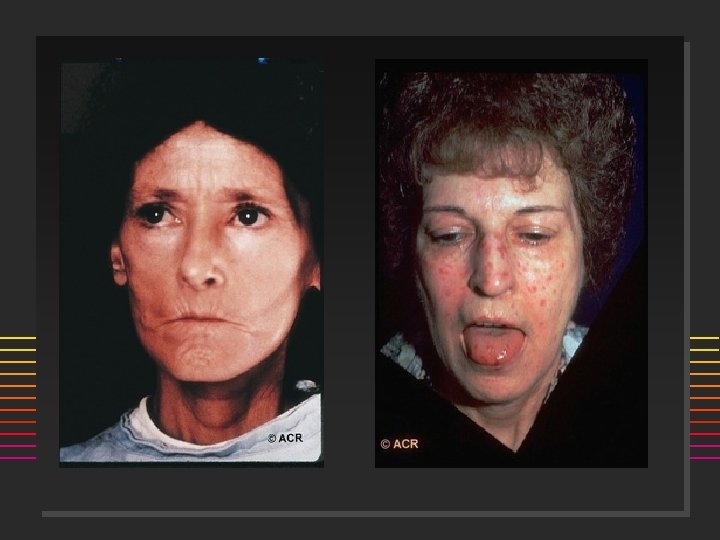
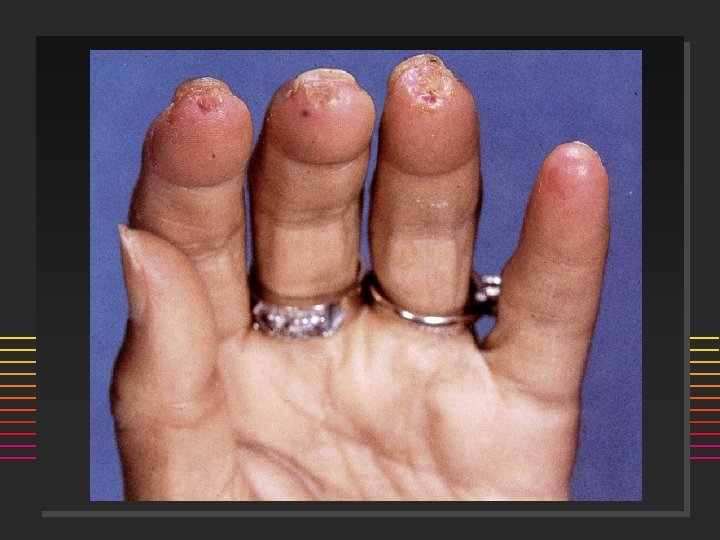
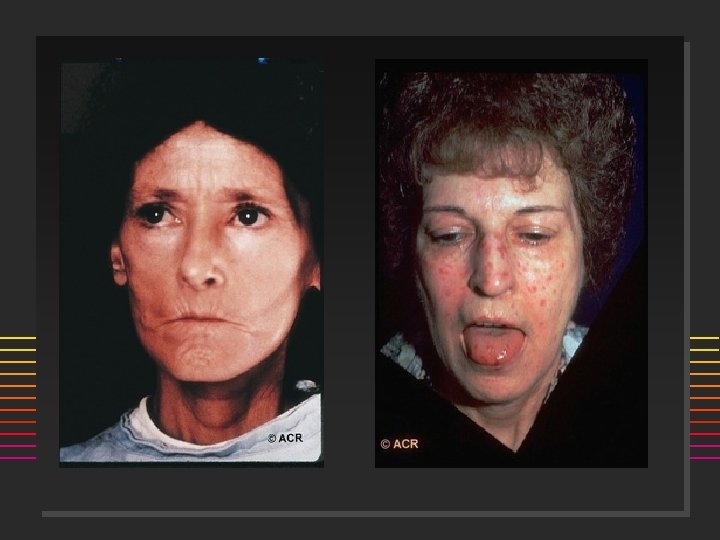
PSS - Clinical n Skin: Skin thickening is most noticeable in the hands, looking swollen, puffy, waxy. ] Thickening extends to proximal extremity, truncal and facial skin thickening is seen. ] Raynaud's phenomenon is present. ] Digital pits or scarring of the distal digital pulp ] n Musculoskeletal: Arthralgias and joint stiffness are common. Palpable tendon friction rubs associated with an increased incidence of organ involvement. ] Muscle weakness or frank myositis can be seen. ]

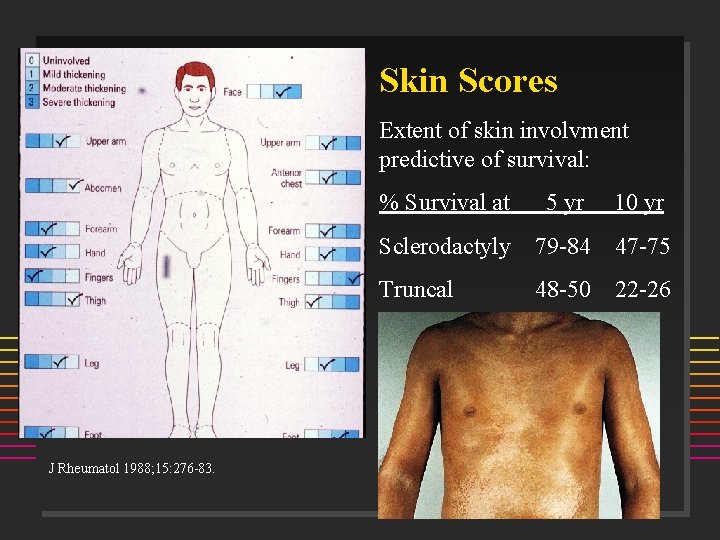
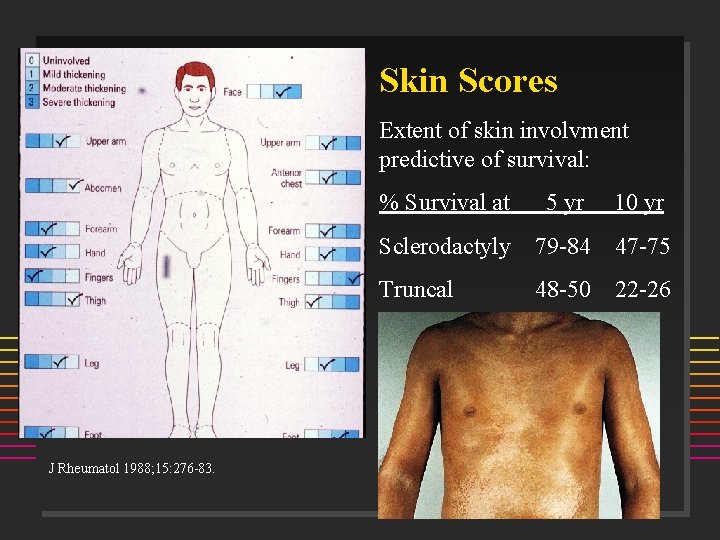
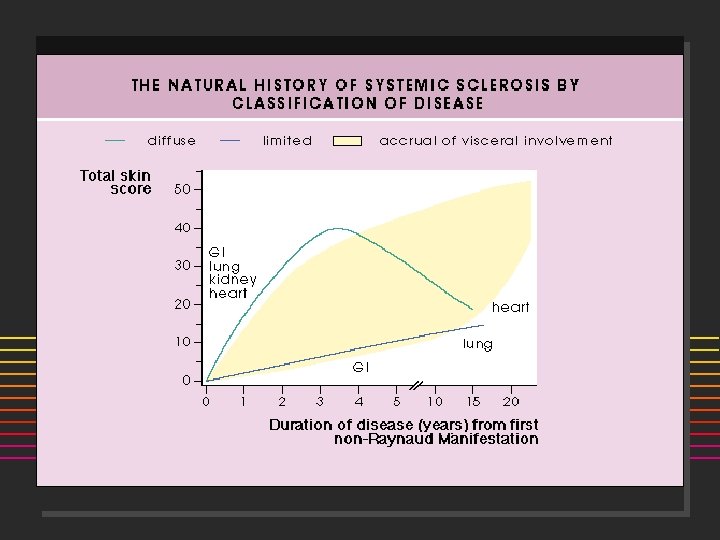
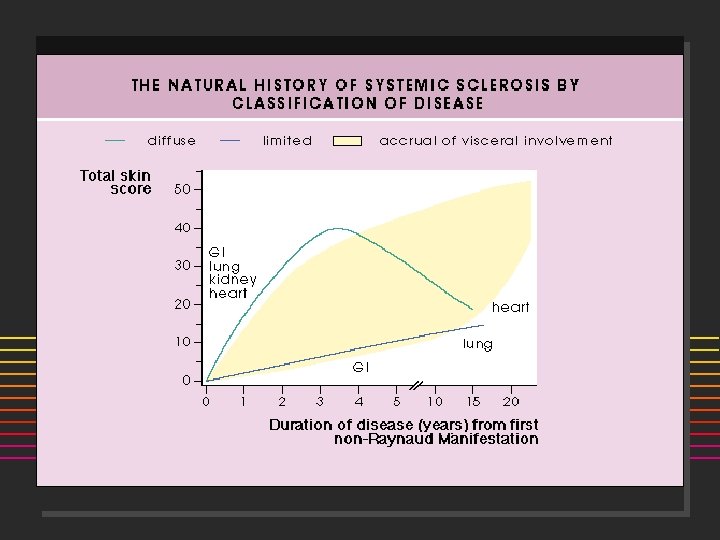
Skin Scores Extent of skin involvment predictive of survival: J Rheumatol 1988; 15: 276 -83. % Survival at 5 yr 10 yr Sclerodactyly 79 -84 47 -75 Truncal 48 -50 22 -26

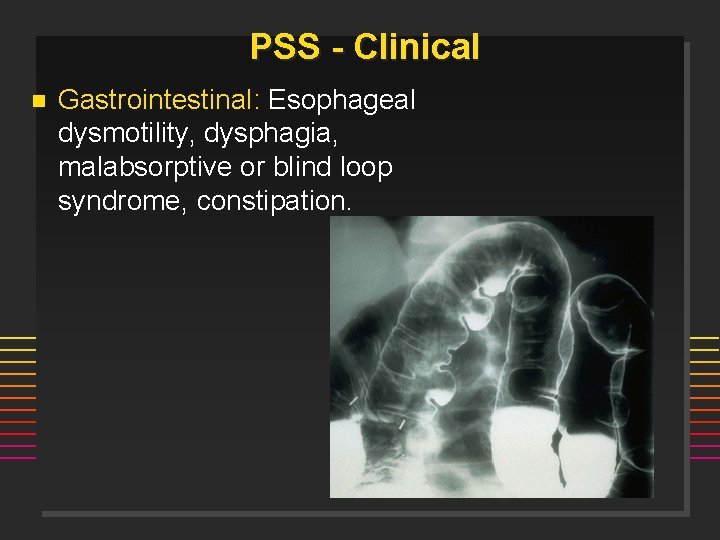
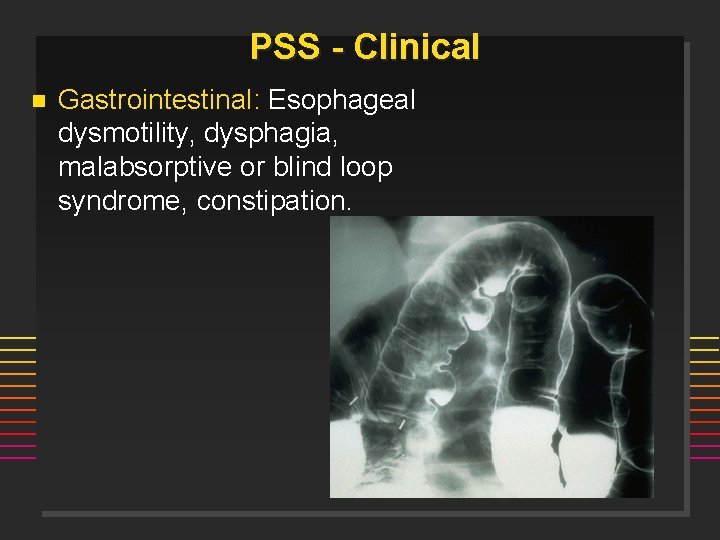
PSS - Clinical n Gastrointestinal: Esophageal dysmotility, dysphagia, malabsorptive or blind loop syndrome, constipation.
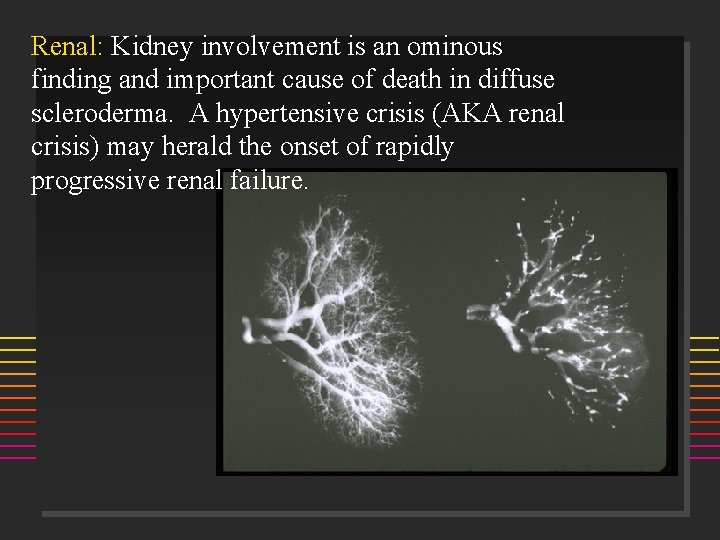
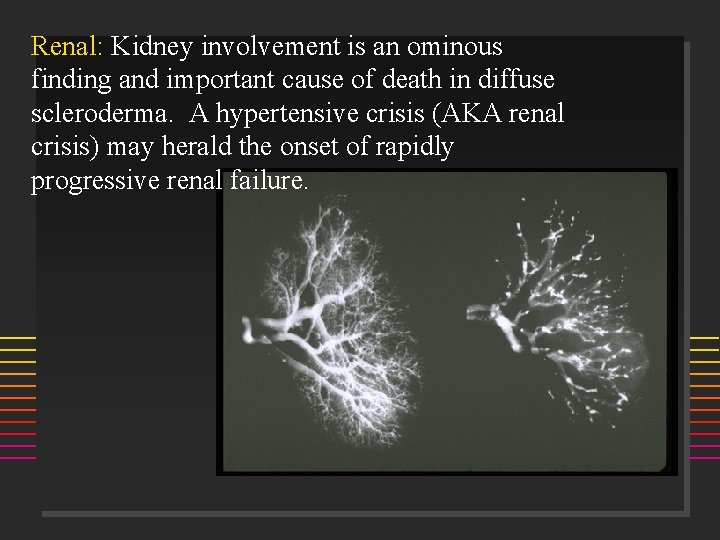
Renal: Kidney involvement is an ominous finding and important cause of death in diffuse scleroderma. A hypertensive crisis (AKA renal crisis) may herald the onset of rapidly progressive renal failure.
![Scleroderma Renal Crisis n Risk Factors diffuse skin involvement rapid progression of Scleroderma Renal Crisis n Risk Factors ] diffuse skin involvement ] rapid progression of](https://slidetodoc.com/presentation_image/0aff954a635d8b9be45431ecb1571192/image-23.jpg)
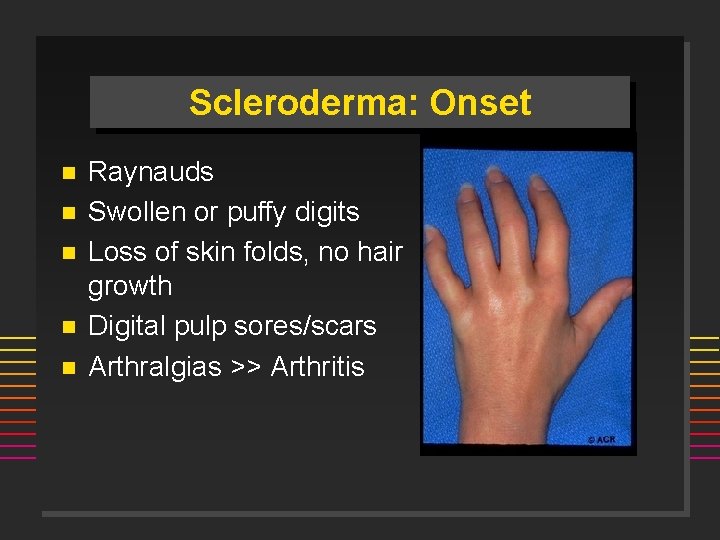
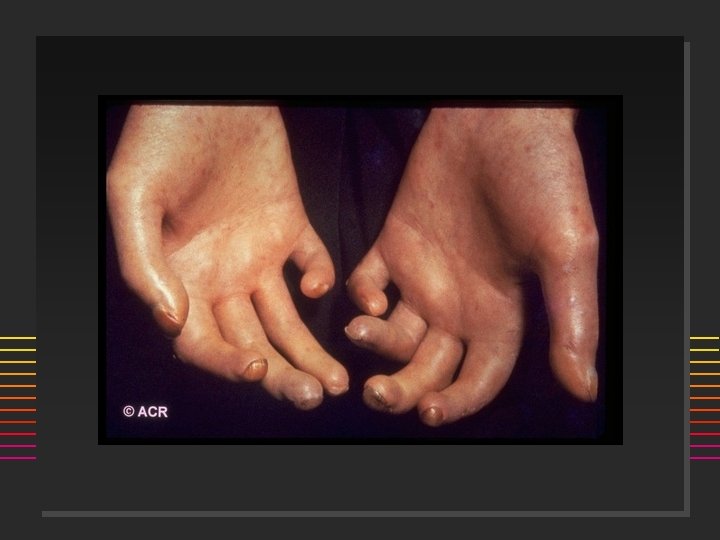
Scleroderma Renal Crisis n Risk Factors ] diffuse skin involvement ] rapid progression of skin thickening ] disease course < 4 years ] anti-RNA-polymerase III-antibodies ] newly manifested anemia ] newly manifested cardiac involvement äpericardial effusion äheart insufficiency preceded high-dose corticoid therapy ] pregnancy ] Am J Med 1984; 76: 779 -786.
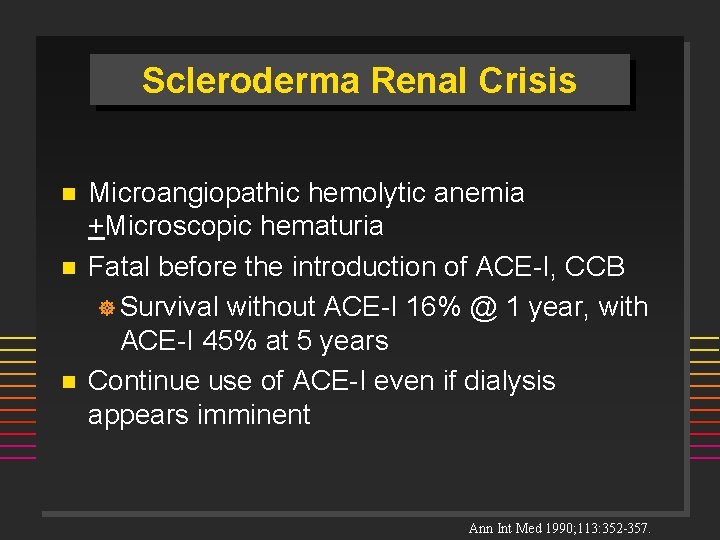
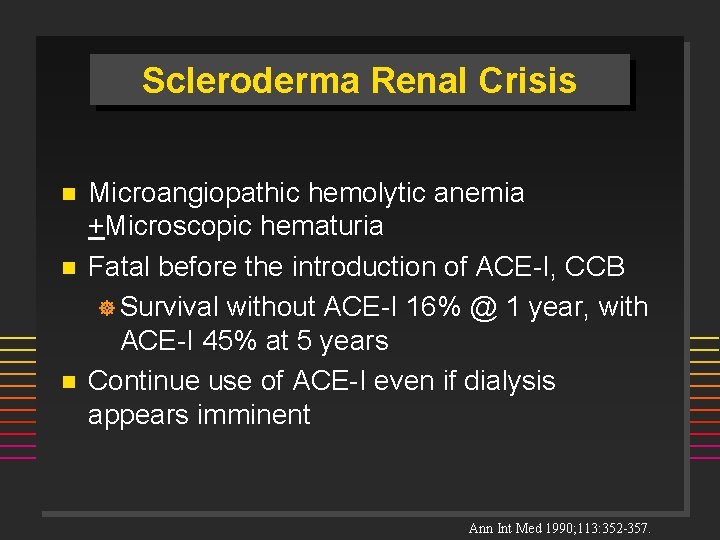
Scleroderma Renal Crisis n n n Microangiopathic hemolytic anemia +Microscopic hematuria Fatal before the introduction of ACE-I, CCB ] Survival without ACE-I 16% @ 1 year, with ACE-I 45% at 5 years Continue use of ACE-I even if dialysis appears imminent Ann Int Med 1990; 113: 352 -357.
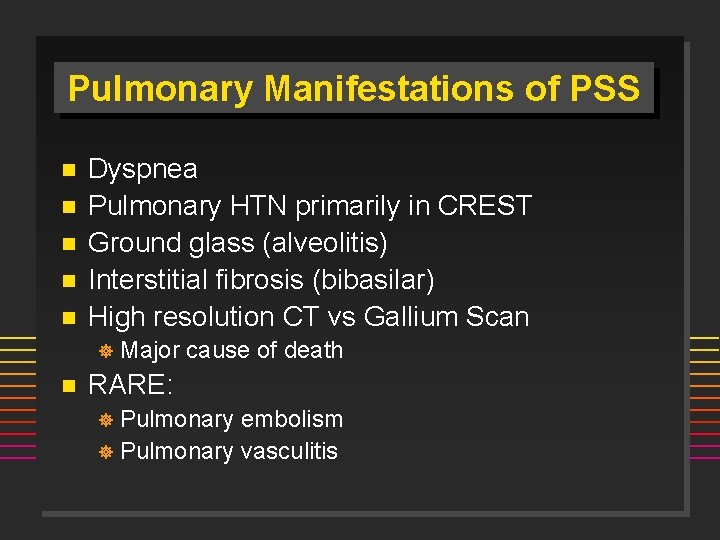
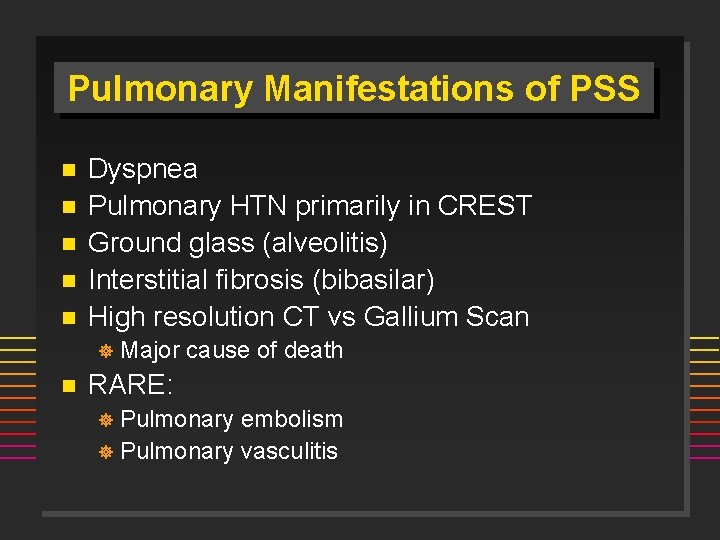
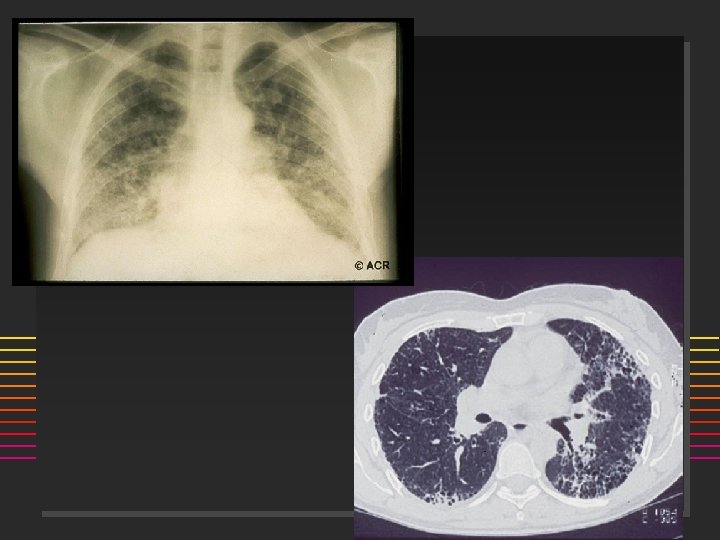
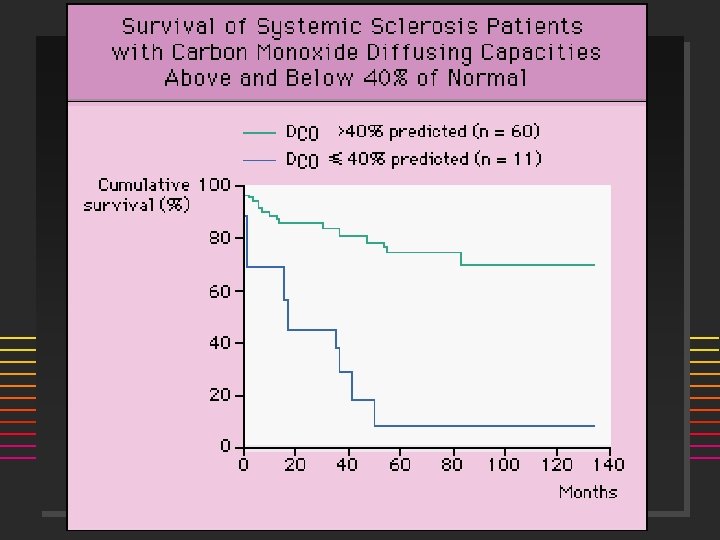
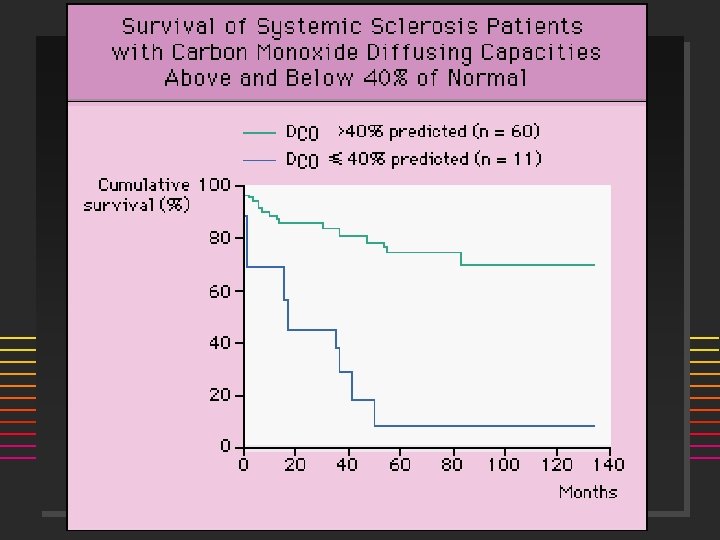
Pulmonary Manifestations of PSS n n n Dyspnea Pulmonary HTN primarily in CREST Ground glass (alveolitis) Interstitial fibrosis (bibasilar) High resolution CT vs Gallium Scan ] n Major cause of death RARE: Pulmonary embolism ] Pulmonary vasculitis ]
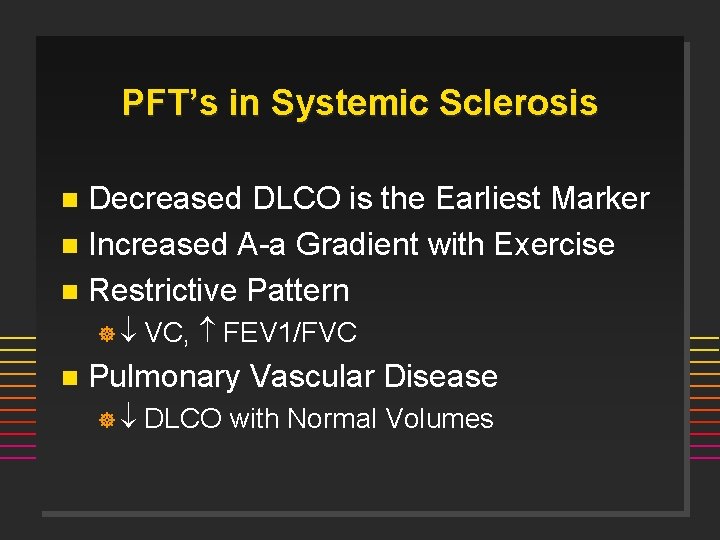
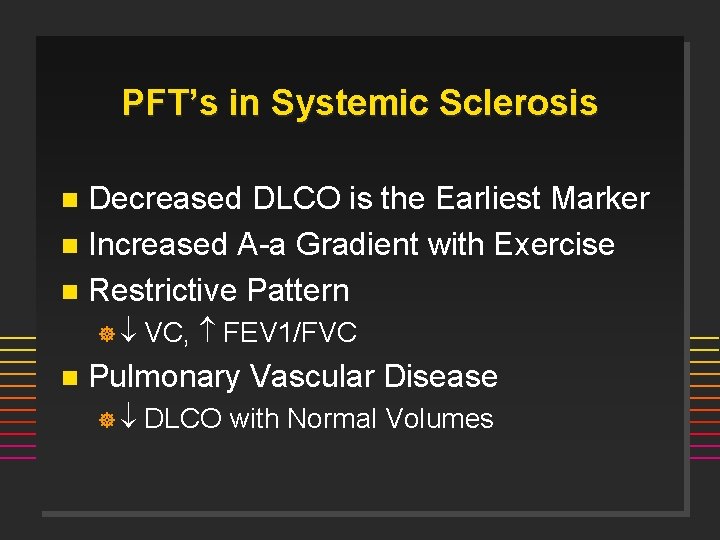
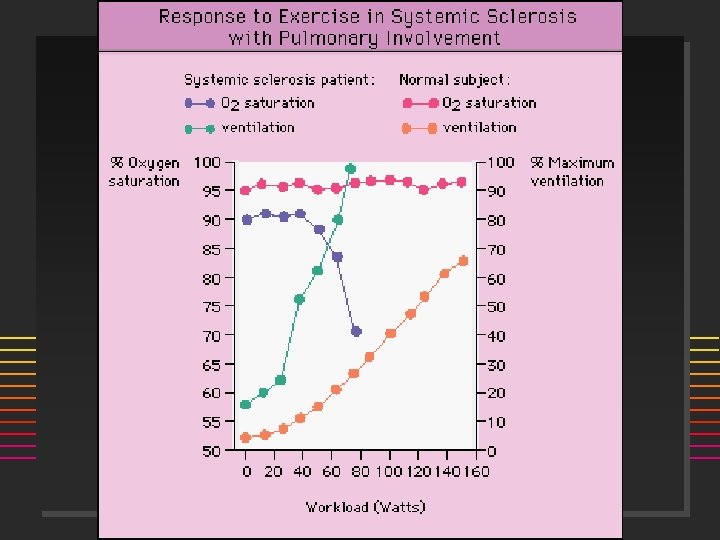
PFT’s in Systemic Sclerosis Decreased DLCO is the Earliest Marker n Increased A-a Gradient with Exercise n Restrictive Pattern n ] n VC, FEV 1/FVC Pulmonary Vascular Disease ] DLCO with Normal Volumes
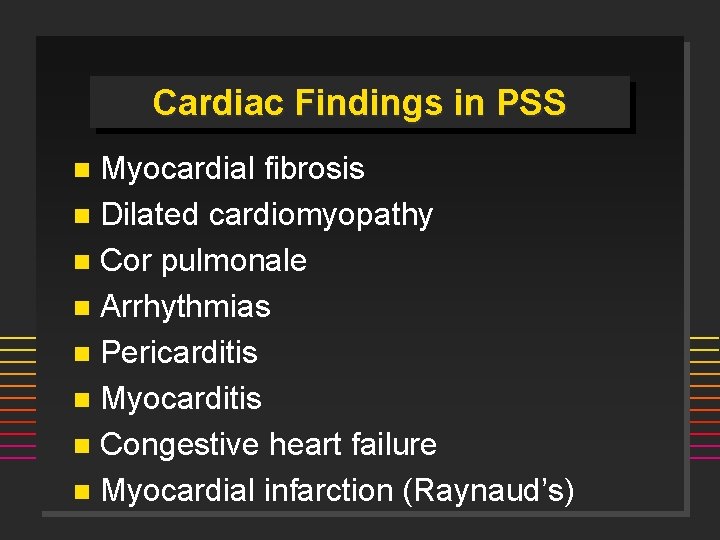
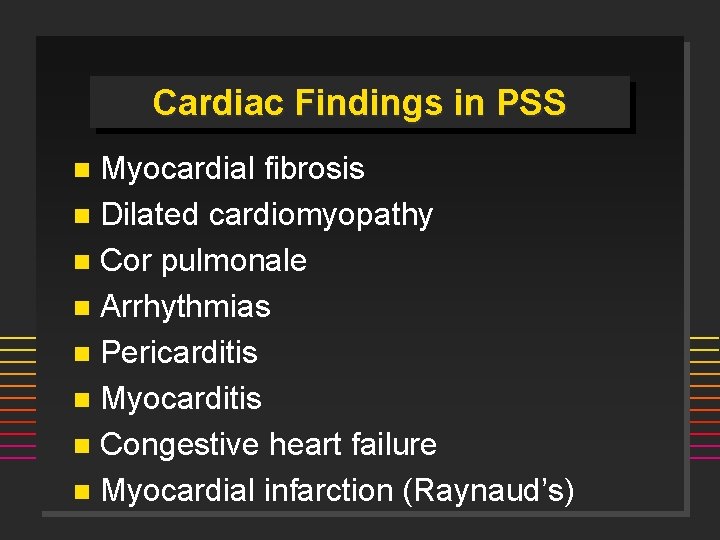
Cardiac Findings in PSS Myocardial fibrosis n Dilated cardiomyopathy n Cor pulmonale n Arrhythmias n Pericarditis n Myocarditis n Congestive heart failure n Myocardial infarction (Raynaud’s) n
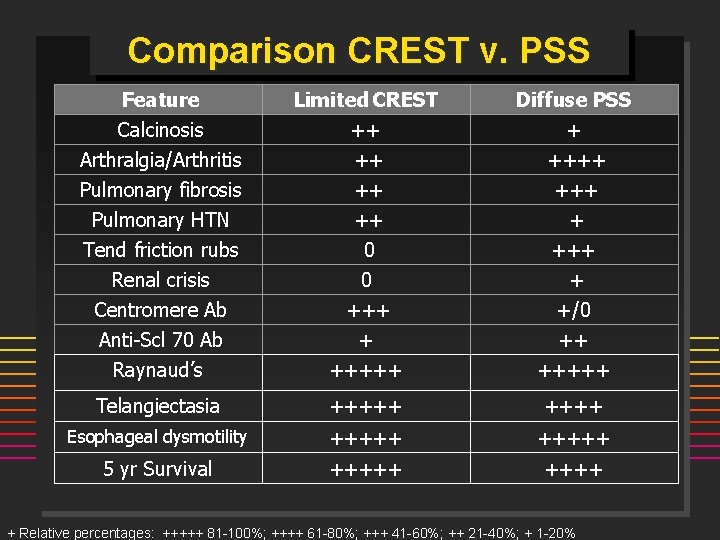
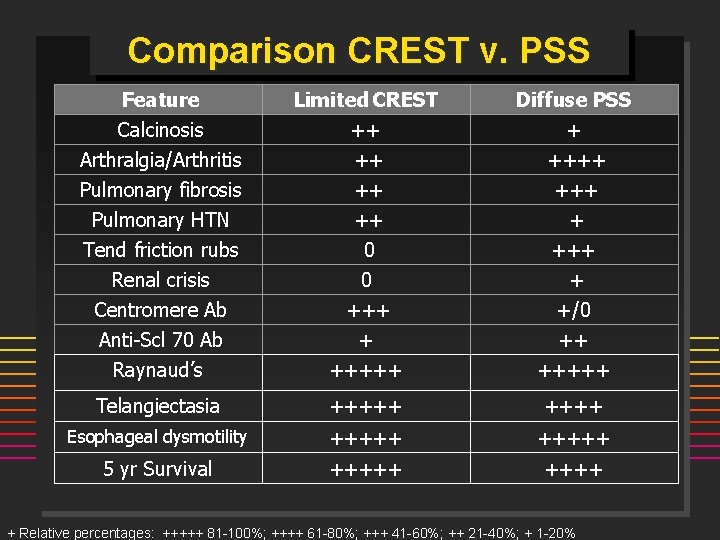
Comparison CREST v. PSS Feature Calcinosis Limited CREST ++ Diffuse PSS + Arthralgia/Arthritis Pulmonary fibrosis Pulmonary HTN ++ ++ ++ ++++ + Tend friction rubs Renal crisis Centromere Ab Anti-Scl 70 Ab Raynaud’s 0 0 +++ + +++++ + +/0 ++ +++++ Telangiectasia +++++ Esophageal dysmotility +++++ 5 yr Survival +++++ + Relative percentages: +++++ 81 -100%; ++++ 61 -80%; +++ 41 -60%; ++ 21 -40%; + 1 -20%
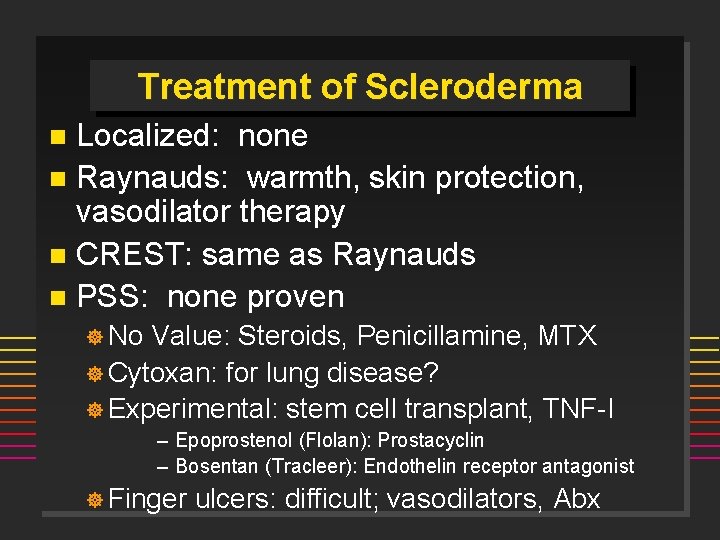
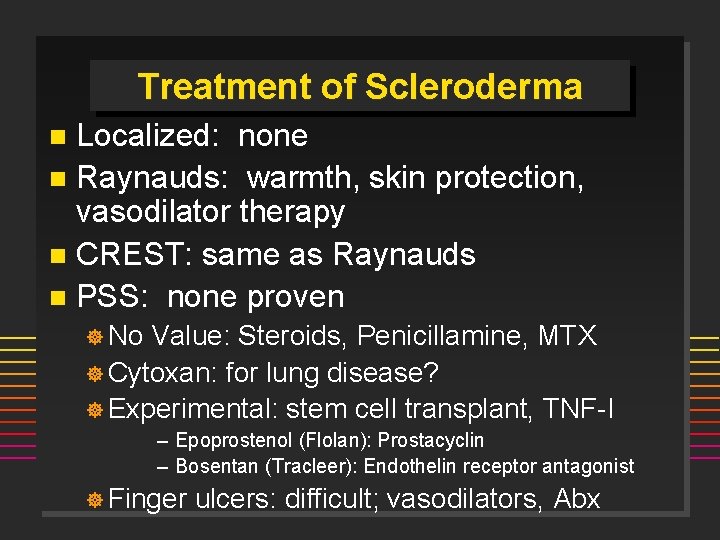
Treatment of Scleroderma Localized: none n Raynauds: warmth, skin protection, vasodilator therapy n CREST: same as Raynauds n PSS: none proven n ] No Value: Steroids, Penicillamine, MTX ] Cytoxan: for lung disease? ] Experimental: stem cell transplant, TNF-I – Epoprostenol (Flolan): Prostacyclin – Bosentan (Tracleer): Endothelin receptor antagonist ] Finger ulcers: difficult; vasodilators, Abx
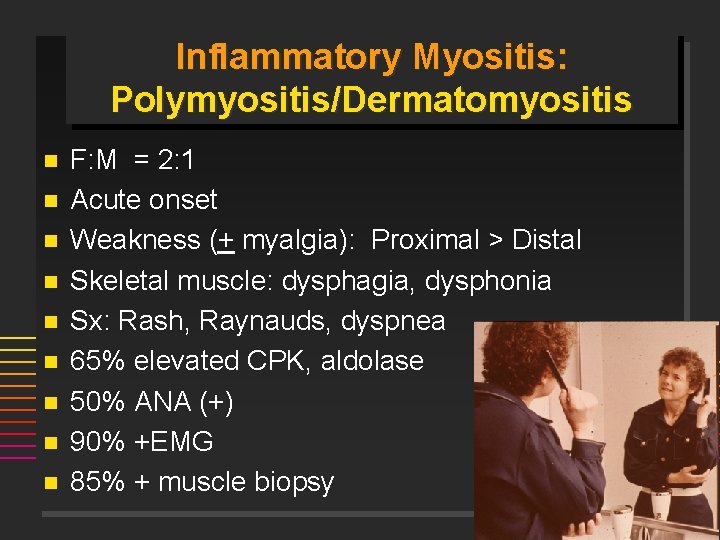
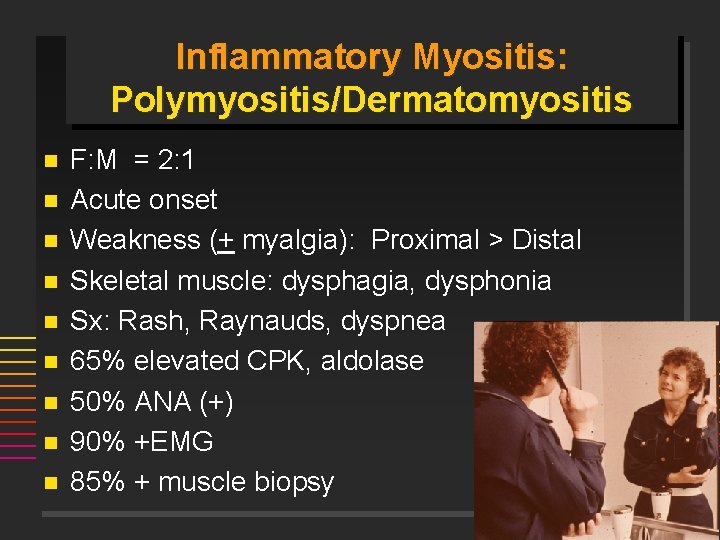
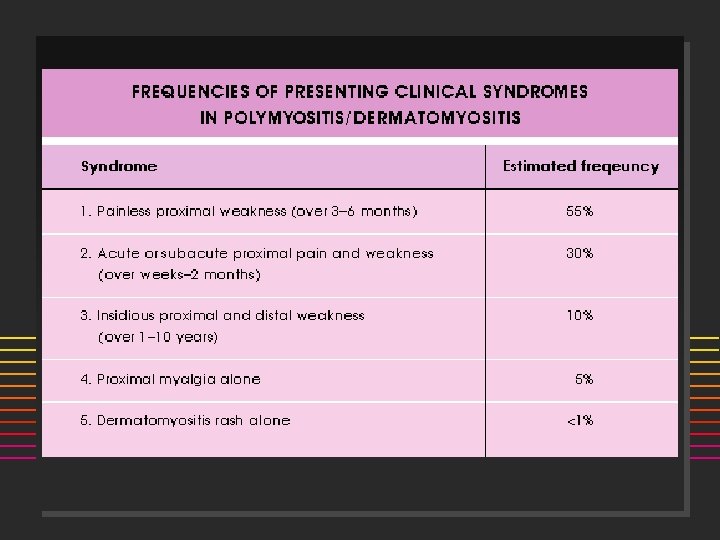
Inflammatory Myositis: Polymyositis/Dermatomyositis n n n n n F: M = 2: 1 Acute onset Weakness (+ myalgia): Proximal > Distal Skeletal muscle: dysphagia, dysphonia Sx: Rash, Raynauds, dyspnea 65% elevated CPK, aldolase 50% ANA (+) 90% +EMG 85% + muscle biopsy
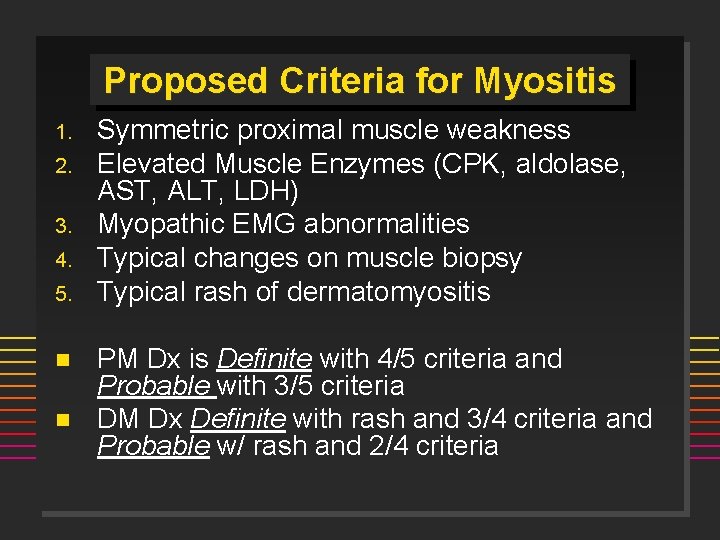
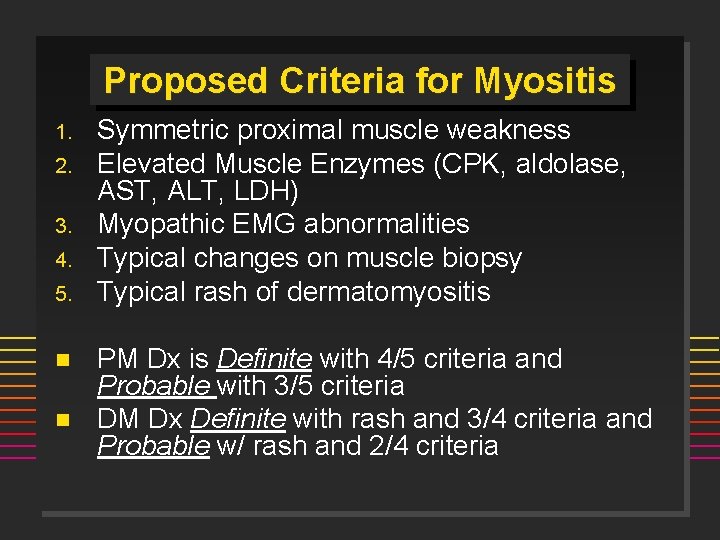
Proposed Criteria for Myositis 1. 2. 3. 4. 5. n n Symmetric proximal muscle weakness Elevated Muscle Enzymes (CPK, aldolase, AST, ALT, LDH) Myopathic EMG abnormalities Typical changes on muscle biopsy Typical rash of dermatomyositis PM Dx is Definite with 4/5 criteria and Probable with 3/5 criteria DM Dx Definite with rash and 3/4 criteria and Probable w/ rash and 2/4 criteria
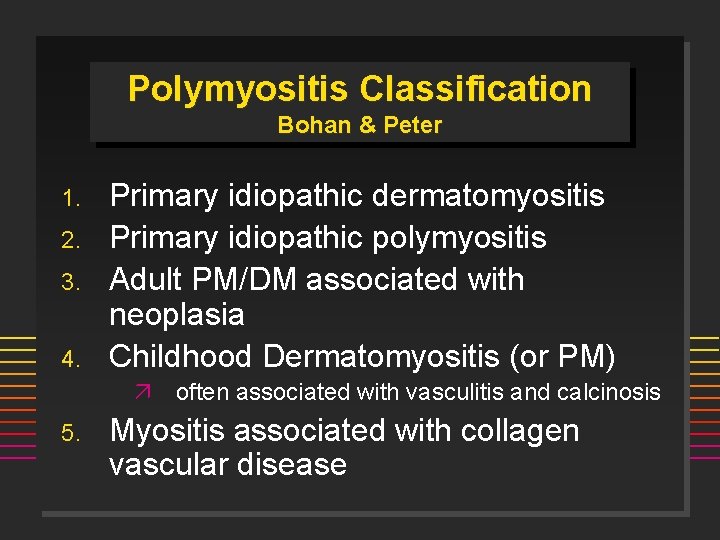
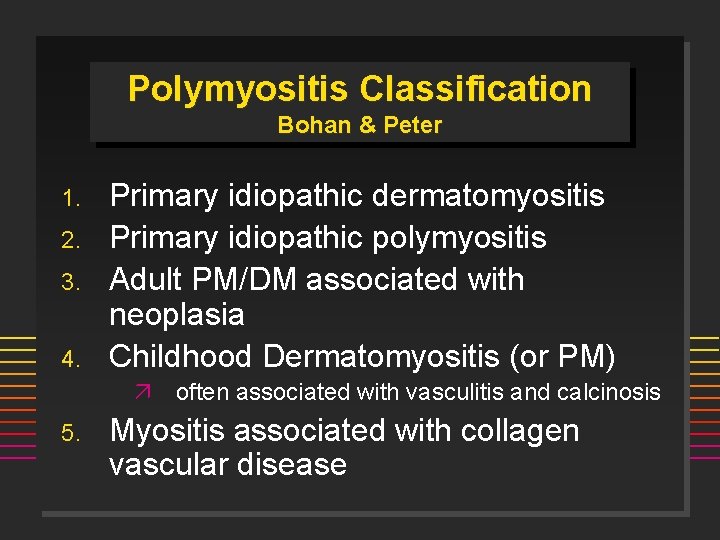
Polymyositis Classification Bohan & Peter 1. 2. 3. 4. Primary idiopathic dermatomyositis Primary idiopathic polymyositis Adult PM/DM associated with neoplasia Childhood Dermatomyositis (or PM) ä often associated with vasculitis and calcinosis 5. Myositis associated with collagen vascular disease
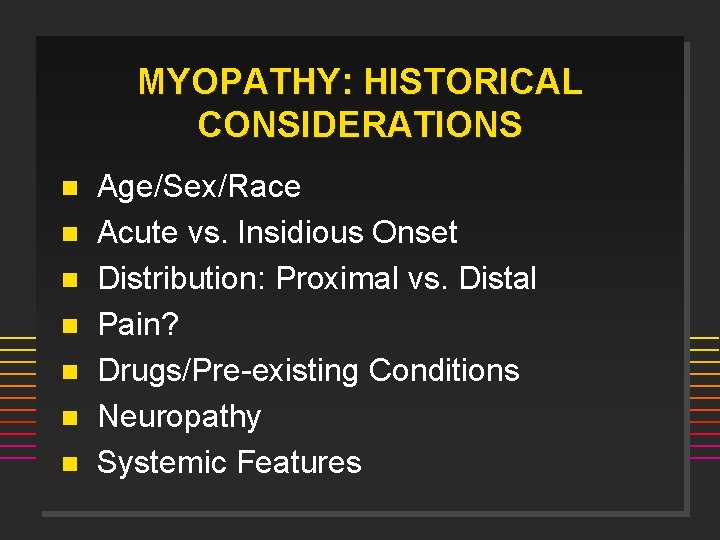
MYOPATHY: HISTORICAL CONSIDERATIONS n n n n Age/Sex/Race Acute vs. Insidious Onset Distribution: Proximal vs. Distal Pain? Drugs/Pre-existing Conditions Neuropathy Systemic Features
![DDX MYOPATHIIES n ToxicDrugs n Infectious n n n Etoh Cocaine Steroids DDX MYOPATHIIES n Toxic/Drugs ] n Infectious ] n n n Etoh, Cocaine, Steroids,](https://slidetodoc.com/presentation_image/0aff954a635d8b9be45431ecb1571192/image-39.jpg)
DDX MYOPATHIIES n Toxic/Drugs ] n Infectious ] n n n Etoh, Cocaine, Steroids, Plaquenil, Penicillamine, Colchicine, AZT, Statins, Clofibrate, Tryptophan, Taxol, Emetine Coxsackie, HBV, HIV, Stept, Staph, Clostridium, Toxoplasma, Trichinella Inflammatory Myopathies Congenital/metabolic myopathies Neuropathic/Motor Neuron Disorders-MG, MD Endocrine/Metabolic-hypothyroidism Inclusion body myositis
![NONMYOPATHIC CONSIDERATIONS n FibromyalgiaFibrositisMyofascial n n Pain disorder Polymyalgia Rheumatica Caucasians 55 NONMYOPATHIC CONSIDERATIONS n Fibromyalgia/Fibrositis/Myofascial n n Pain disorder Polymyalgia Rheumatica ] Caucasians, > 55](https://slidetodoc.com/presentation_image/0aff954a635d8b9be45431ecb1571192/image-40.jpg)
NONMYOPATHIC CONSIDERATIONS n Fibromyalgia/Fibrositis/Myofascial n n Pain disorder Polymyalgia Rheumatica ] Caucasians, > 55 yrs, M=F ] ESR > 100, normal strength, no synovitis CTD (SLE, RA, SSc) Vasculitis Adult Still's Disease
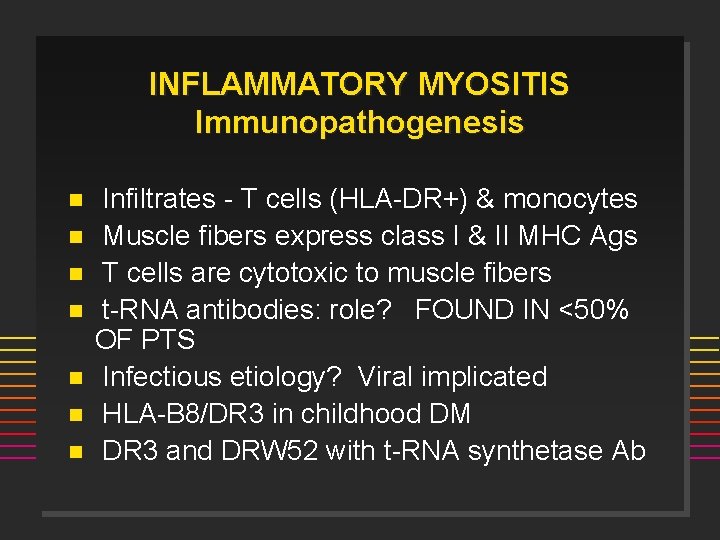
INFLAMMATORY MYOSITIS Immunopathogenesis n n n n Infiltrates - T cells (HLA-DR+) & monocytes Muscle fibers express class I & II MHC Ags T cells are cytotoxic to muscle fibers t-RNA antibodies: role? FOUND IN <50% OF PTS Infectious etiology? Viral implicated HLA-B 8/DR 3 in childhood DM DR 3 and DRW 52 with t-RNA synthetase Ab
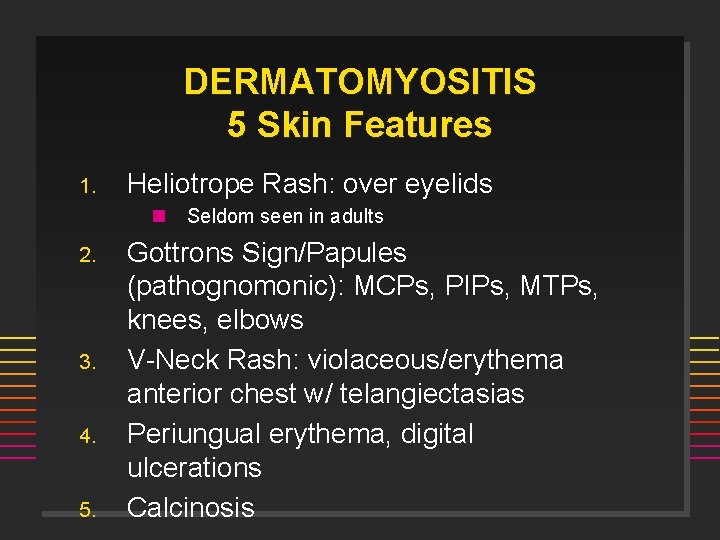
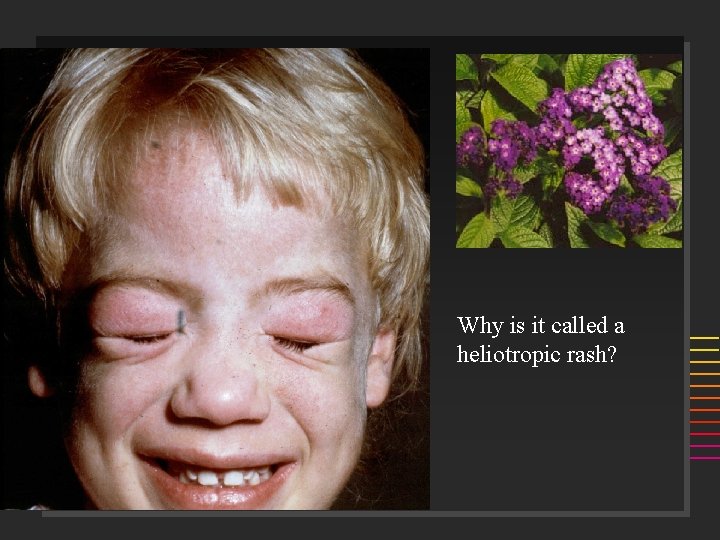
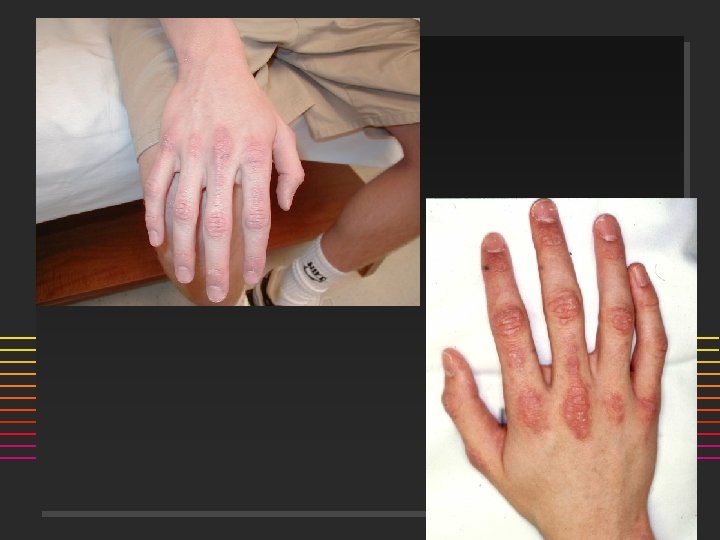
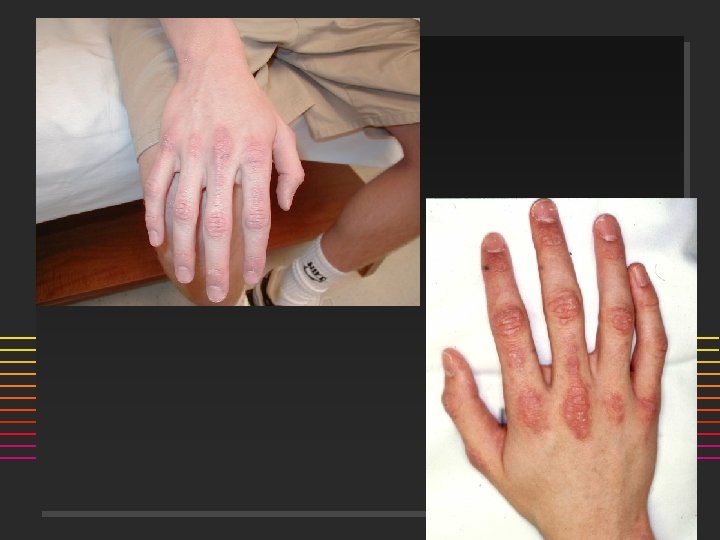
DERMATOMYOSITIS 5 Skin Features 1. Heliotrope Rash: over eyelids n 2. 3. 4. 5. Seldom seen in adults Gottrons Sign/Papules (pathognomonic): MCPs, PIPs, MTPs, knees, elbows V-Neck Rash: violaceous/erythema anterior chest w/ telangiectasias Periungual erythema, digital ulcerations Calcinosis
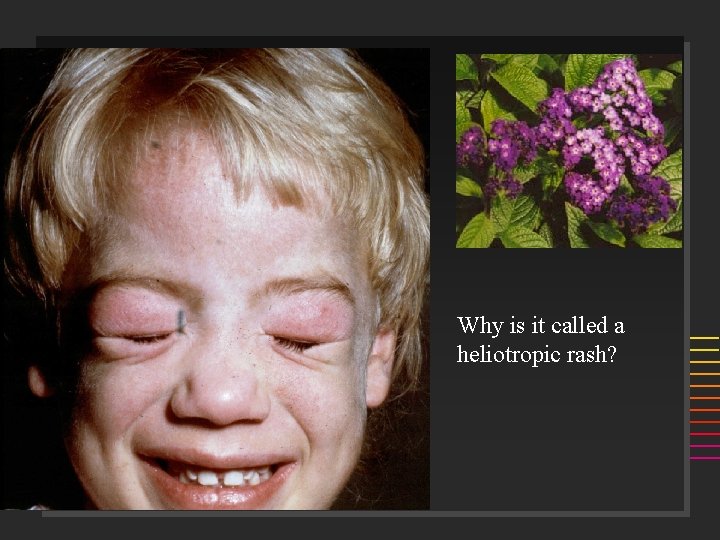
Why is it called a heliotropic rash?




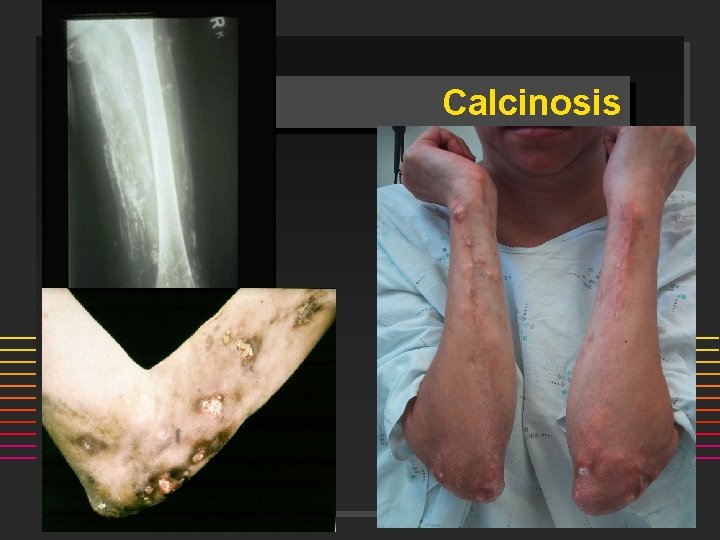
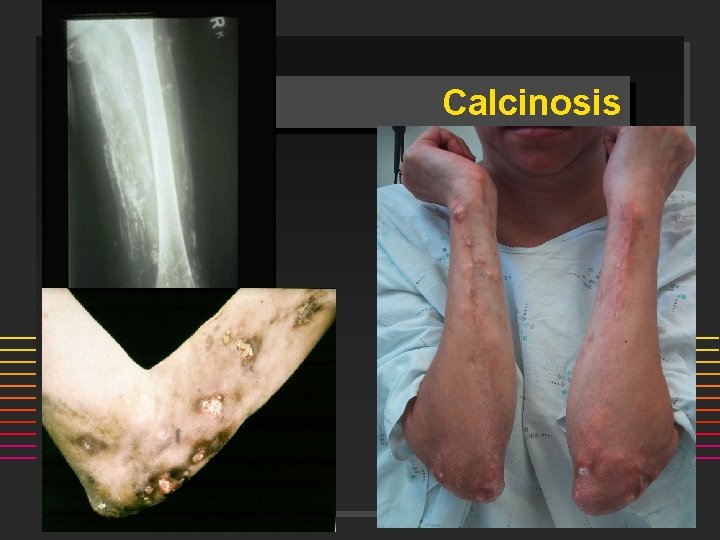
Calcinosis

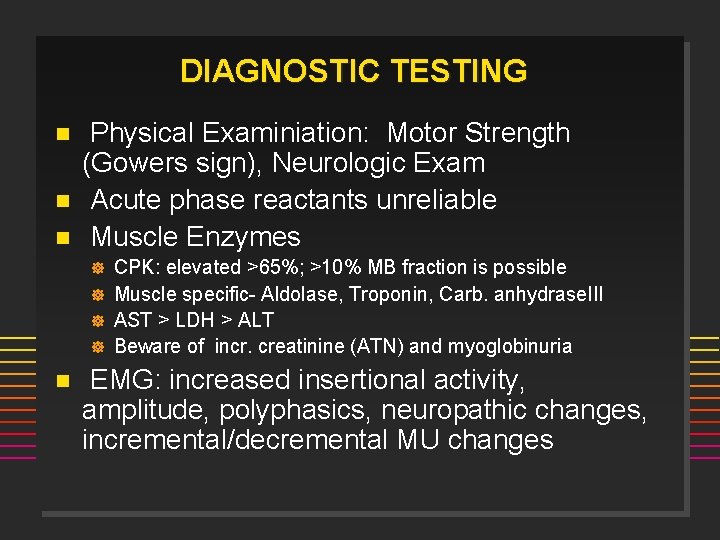
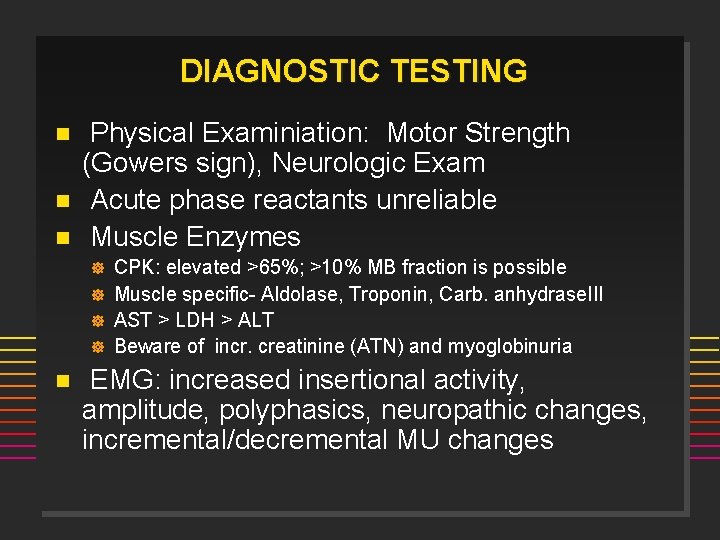
DIAGNOSTIC TESTING n n n Physical Examiniation: Motor Strength (Gowers sign), Neurologic Exam Acute phase reactants unreliable Muscle Enzymes ] ] n CPK: elevated >65%; >10% MB fraction is possible Muscle specific- Aldolase, Troponin, Carb. anhydrase. III AST > LDH > ALT Beware of incr. creatinine (ATN) and myoglobinuria EMG: increased insertional activity, amplitude, polyphasics, neuropathic changes, incremental/decremental MU changes
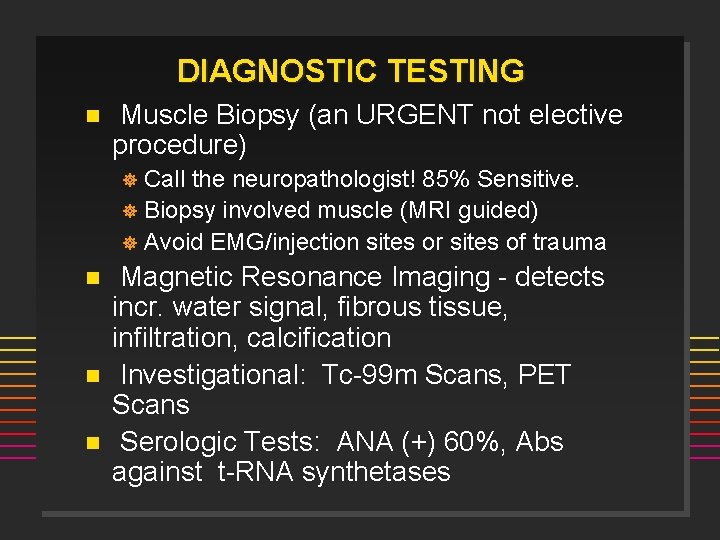
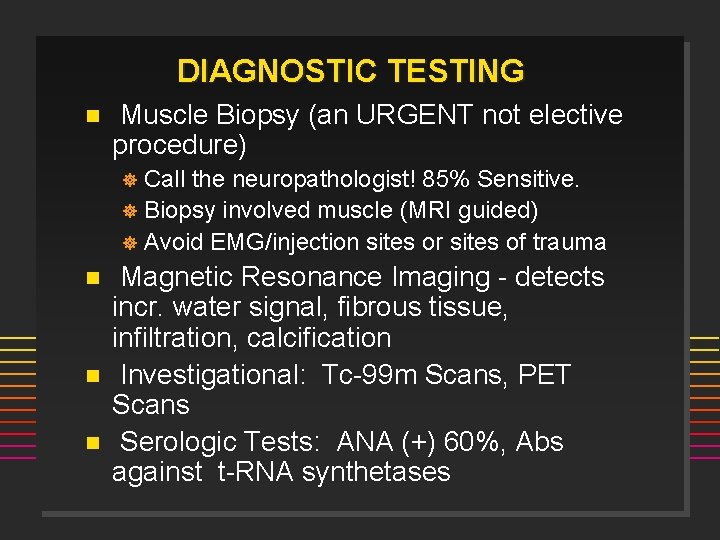
DIAGNOSTIC TESTING n Muscle Biopsy (an URGENT not elective procedure) Call the neuropathologist! 85% Sensitive. ] Biopsy involved muscle (MRI guided) ] Avoid EMG/injection sites or sites of trauma ] n n n Magnetic Resonance Imaging - detects incr. water signal, fibrous tissue, infiltration, calcification Investigational: Tc-99 m Scans, PET Scans Serologic Tests: ANA (+) 60%, Abs against t-RNA synthetases
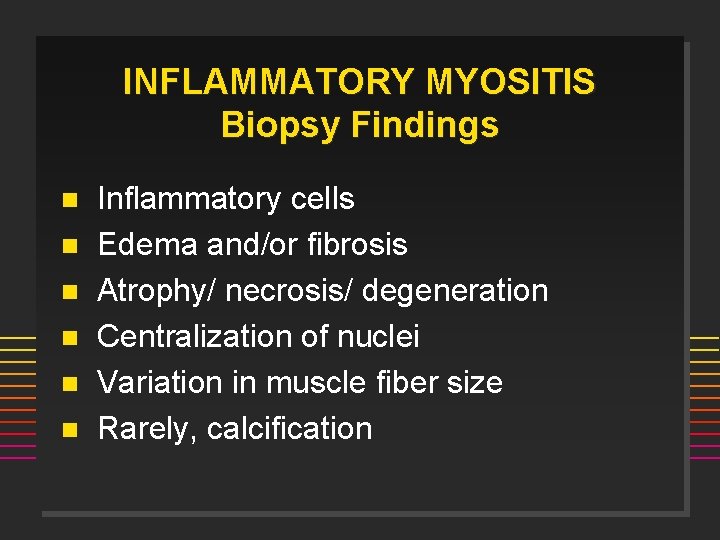
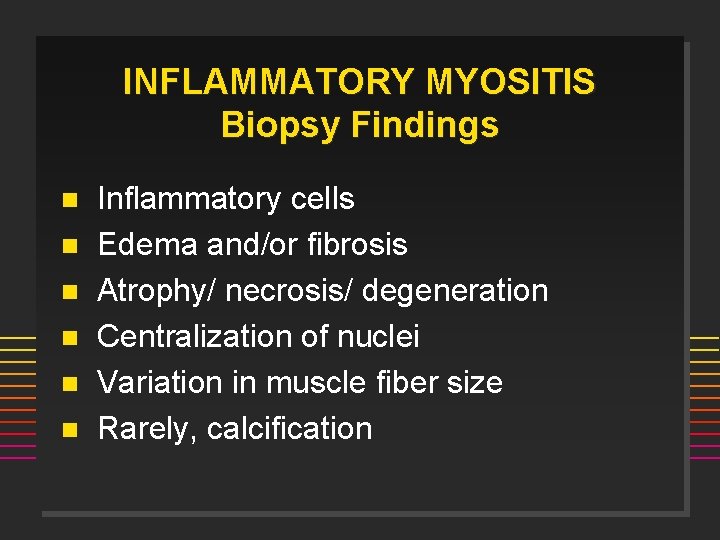
INFLAMMATORY MYOSITIS Biopsy Findings n n n Inflammatory cells Edema and/or fibrosis Atrophy/ necrosis/ degeneration Centralization of nuclei Variation in muscle fiber size Rarely, calcification
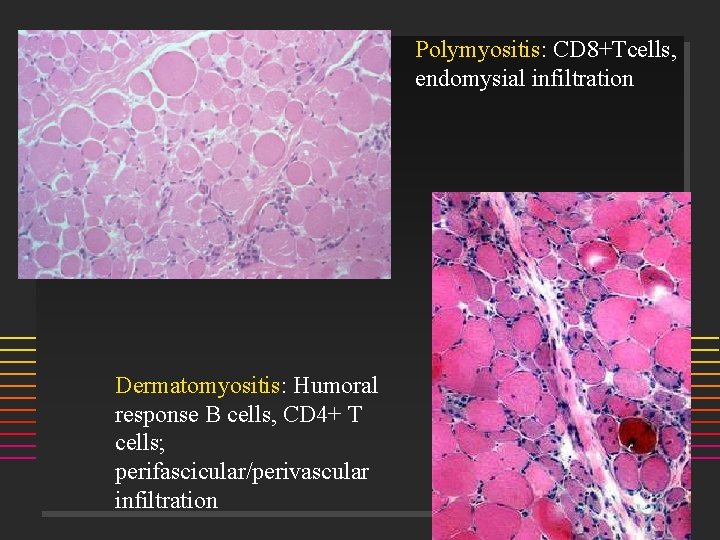
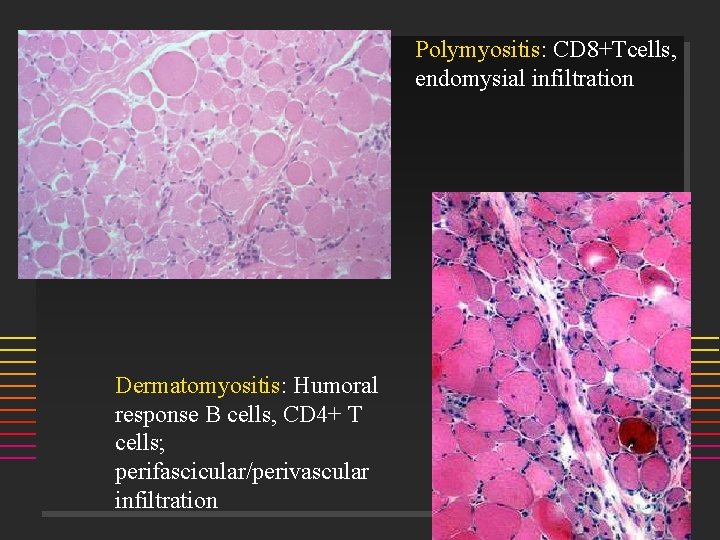
Polymyositis: CD 8+Tcells, endomysial infiltration Dermatomyositis: Humoral response B cells, CD 4+ T cells; perifascicular/perivascular infiltration
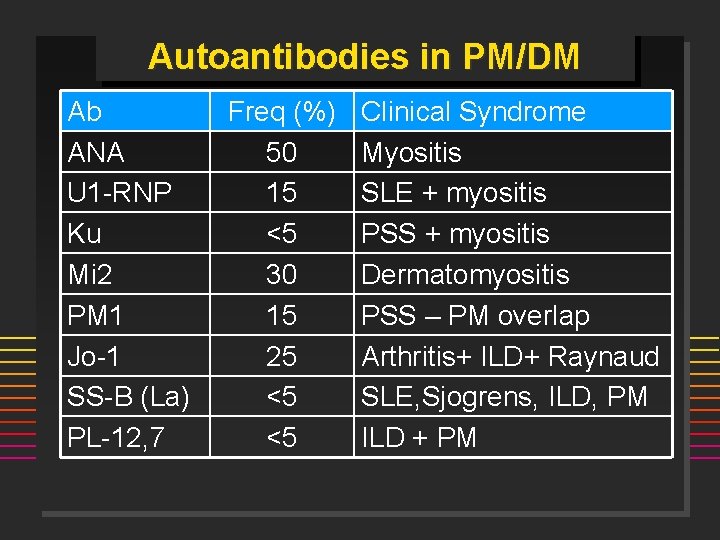
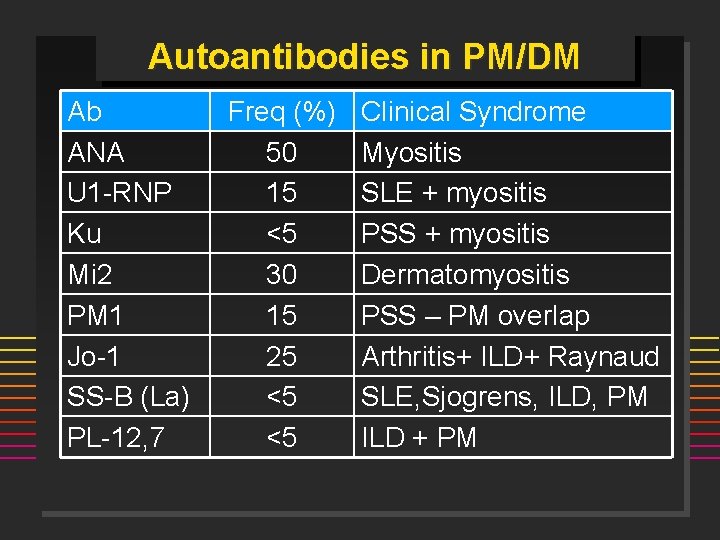
Autoantibodies in PM/DM Ab ANA U 1 -RNP Ku Mi 2 PM 1 Jo-1 SS-B (La) PL-12, 7 Freq (%) 50 15 <5 30 15 25 <5 <5 Clinical Syndrome Myositis SLE + myositis PSS + myositis Dermatomyositis PSS – PM overlap Arthritis+ ILD+ Raynaud SLE, Sjogrens, ILD, PM ILD + PM
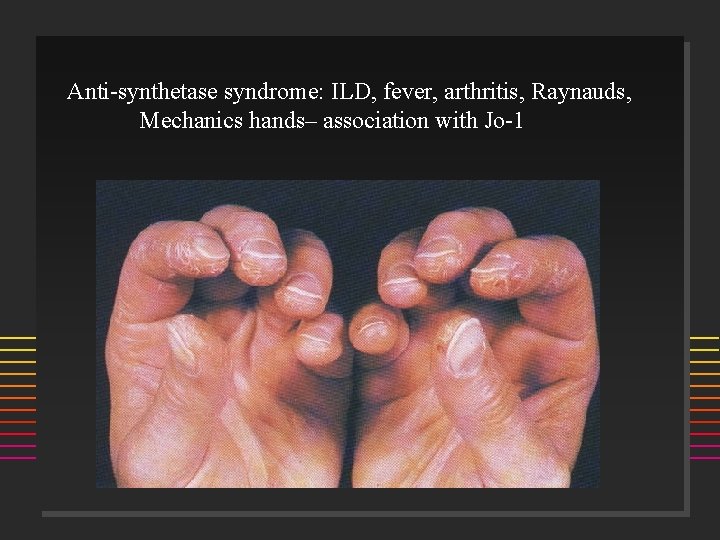
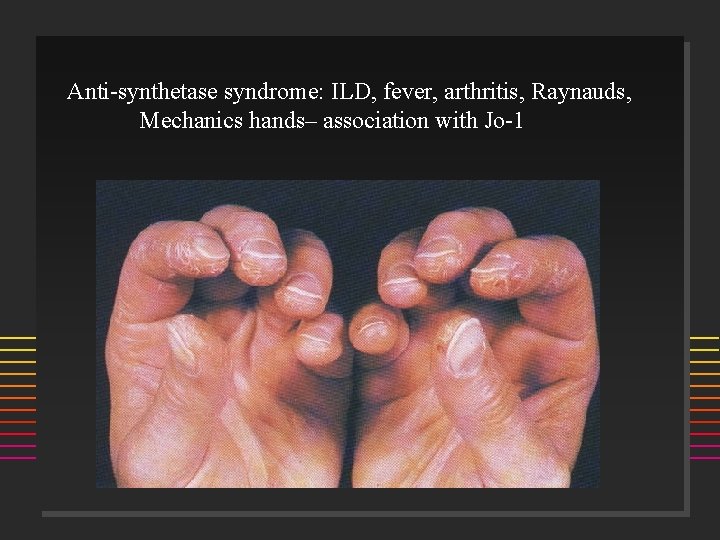
Anti-synthetase syndrome: ILD, fever, arthritis, Raynauds, Mechanics hands– association with Jo-1
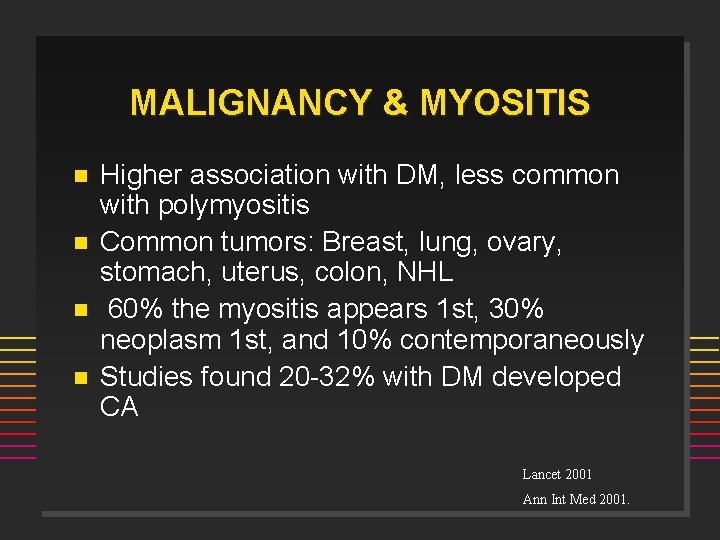
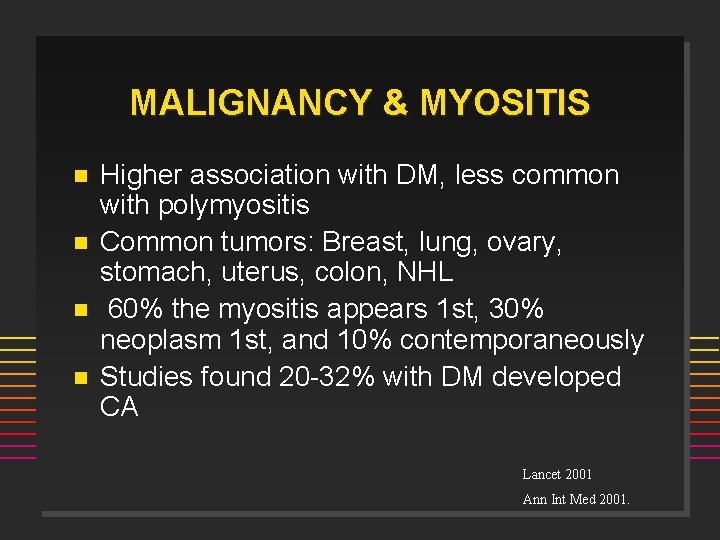
MALIGNANCY & MYOSITIS n n Higher association with DM, less common with polymyositis Common tumors: Breast, lung, ovary, stomach, uterus, colon, NHL 60% the myositis appears 1 st, 30% neoplasm 1 st, and 10% contemporaneously Studies found 20 -32% with DM developed CA Lancet 2001 Ann Int Med 2001.
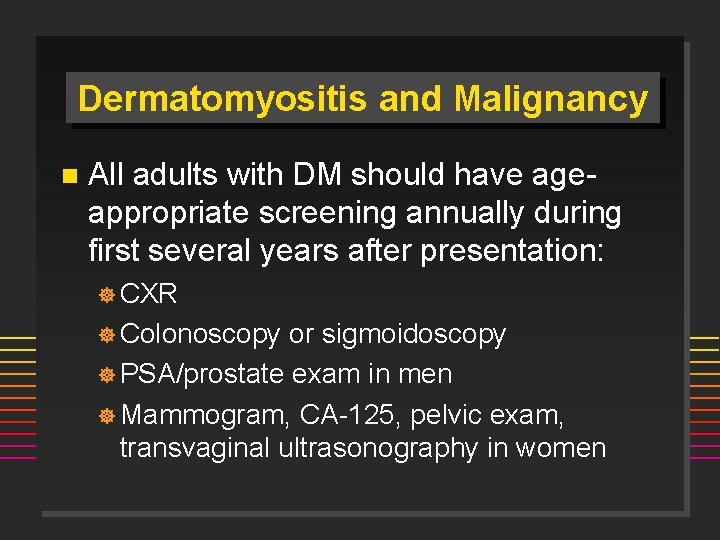
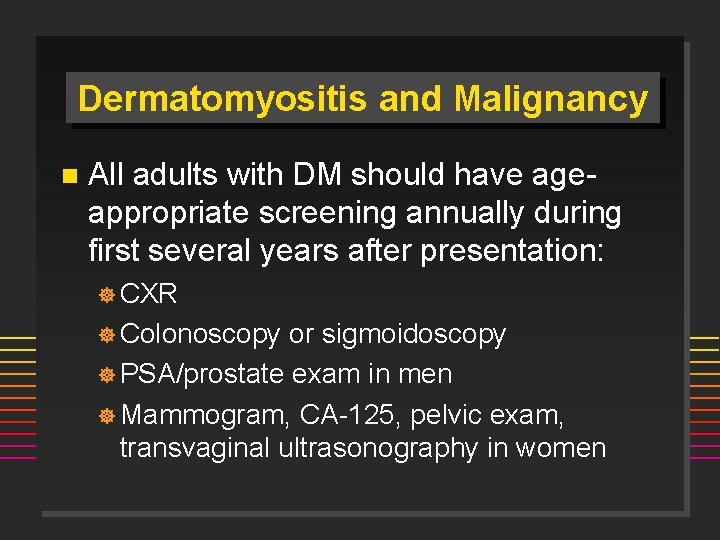
Dermatomyositis and Malignancy n All adults with DM should have ageappropriate screening annually during first several years after presentation: ] CXR ] Colonoscopy or sigmoidoscopy ] PSA/prostate exam in men ] Mammogram, CA-125, pelvic exam, transvaginal ultrasonography in women
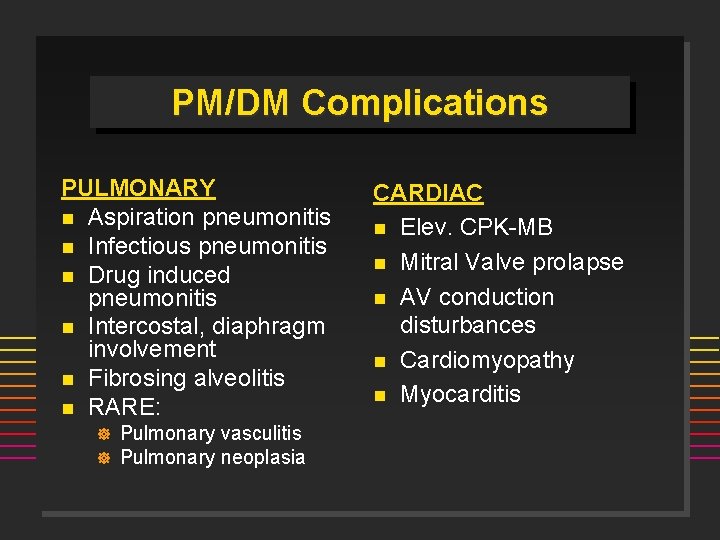
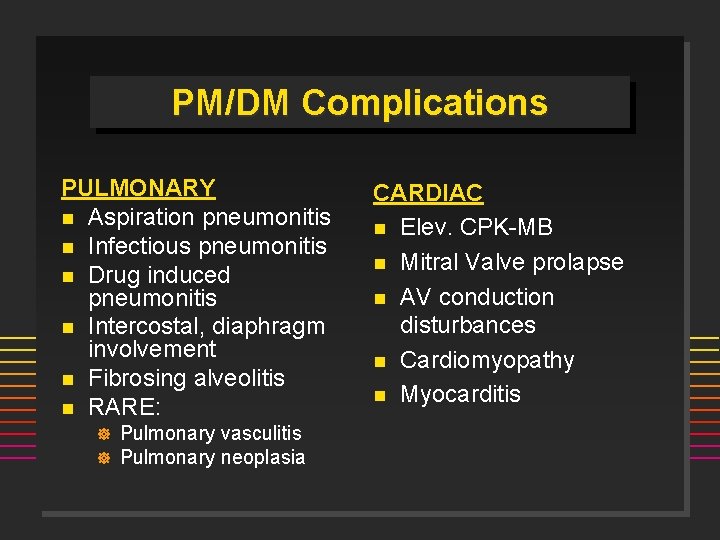
PM/DM Complications PULMONARY n Aspiration pneumonitis n Infectious pneumonitis n Drug induced pneumonitis n Intercostal, diaphragm involvement n Fibrosing alveolitis n RARE: ] ] Pulmonary vasculitis Pulmonary neoplasia CARDIAC n Elev. CPK-MB n Mitral Valve prolapse n AV conduction disturbances n Cardiomyopathy n Myocarditis
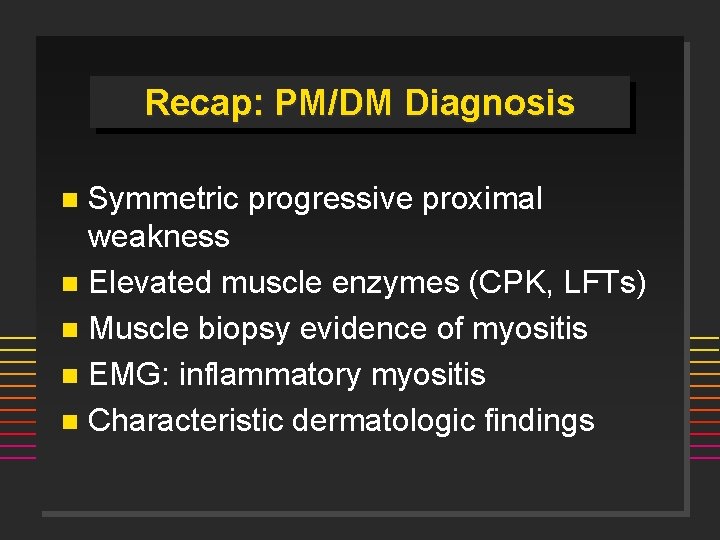
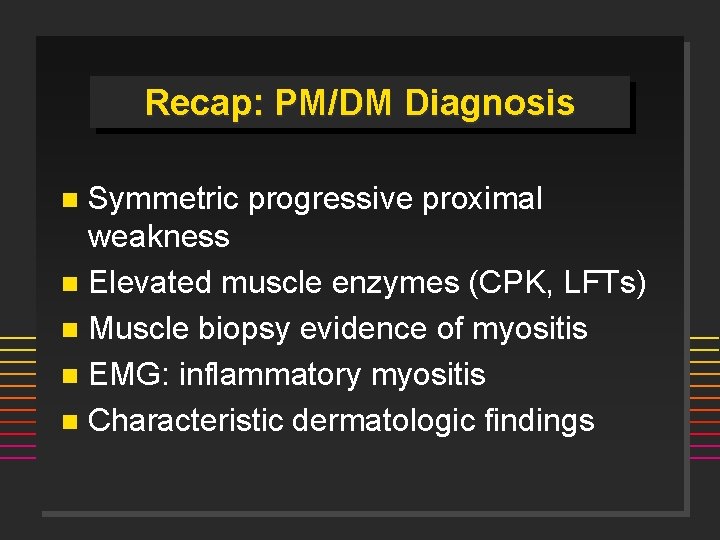
Recap: PM/DM Diagnosis Symmetric progressive proximal weakness n Elevated muscle enzymes (CPK, LFTs) n Muscle biopsy evidence of myositis n EMG: inflammatory myositis n Characteristic dermatologic findings n
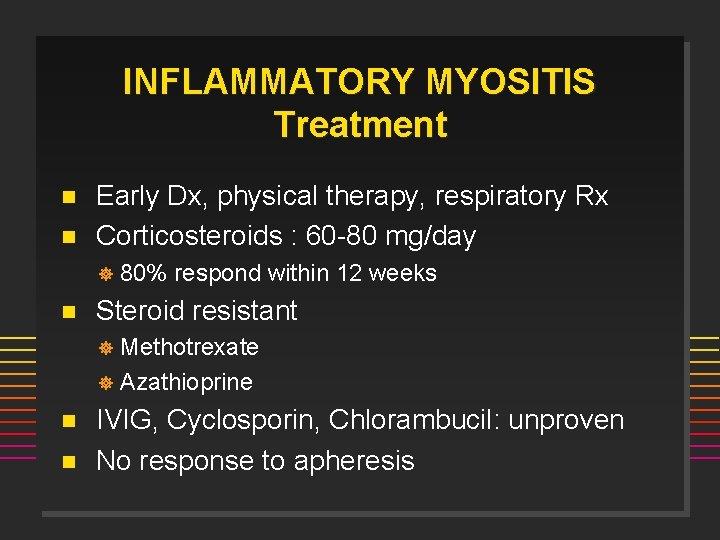
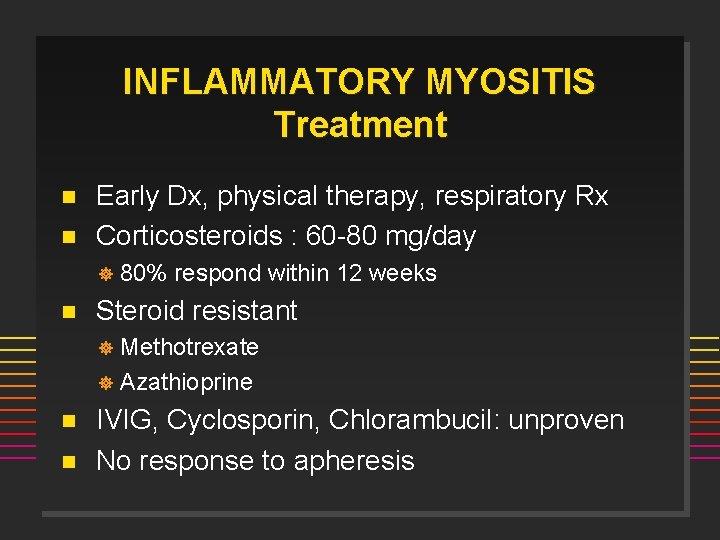
INFLAMMATORY MYOSITIS Treatment n n Early Dx, physical therapy, respiratory Rx Corticosteroids : 60 -80 mg/day ] n 80% respond within 12 weeks Steroid resistant Methotrexate ] Azathioprine ] n n IVIG, Cyclosporin, Chlorambucil: unproven No response to apheresis
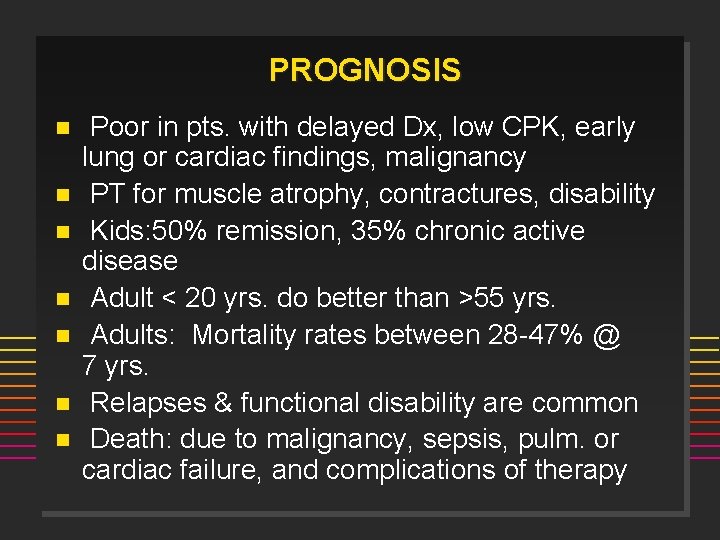
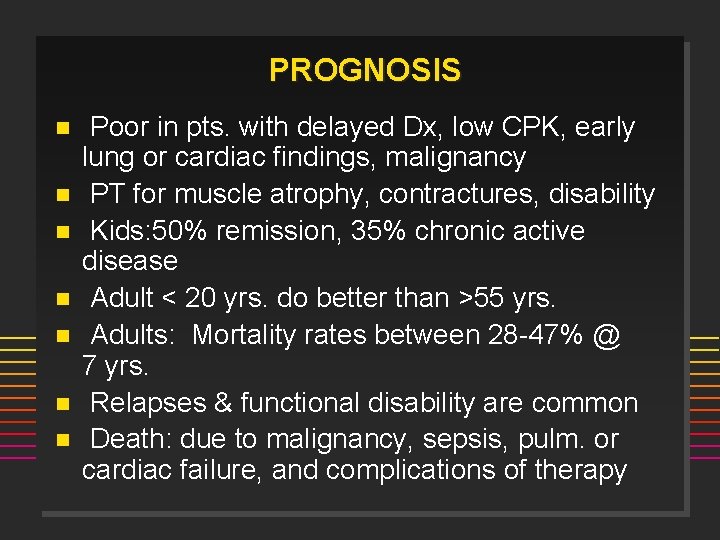
PROGNOSIS n n n n Poor in pts. with delayed Dx, low CPK, early lung or cardiac findings, malignancy PT for muscle atrophy, contractures, disability Kids: 50% remission, 35% chronic active disease Adult < 20 yrs. do better than >55 yrs. Adults: Mortality rates between 28 -47% @ 7 yrs. Relapses & functional disability are common Death: due to malignancy, sepsis, pulm. or cardiac failure, and complications of therapy

RHABDOMYOLYSIS n n n Injury to the sarcolemma of skeletal muscle with systemic release of muscle macromolecules such as CPK, aldolase, actin, myoglobin, etc Maybe LIFE-THREATENING: from hyperkalemia, met. acidosis, ATN from myoglobinuria Common causes: Et. OH, Cocaine, K+ deficiency, infection, PM/DM, infection (clostridial, staph, strept), medications, exertion/exercise, cytokines
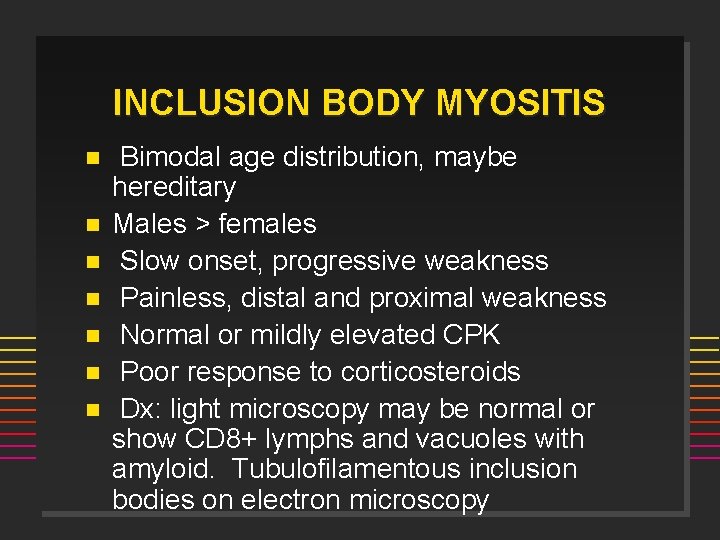
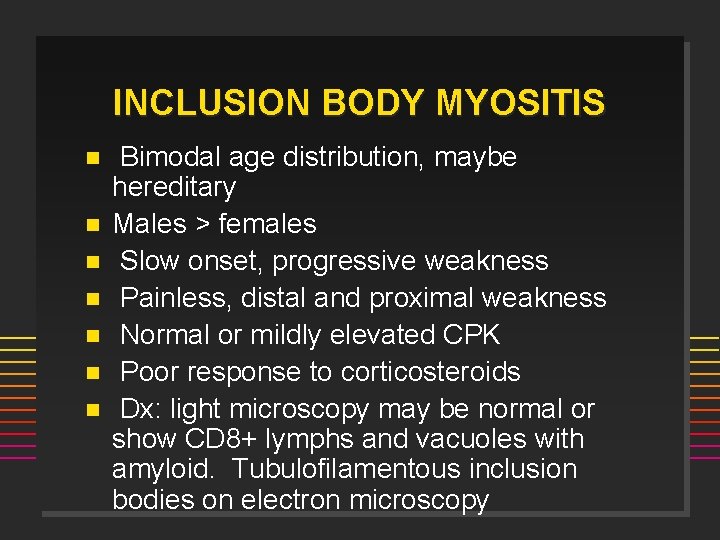
INCLUSION BODY MYOSITIS n n n n Bimodal age distribution, maybe hereditary Males > females Slow onset, progressive weakness Painless, distal and proximal weakness Normal or mildly elevated CPK Poor response to corticosteroids Dx: light microscopy may be normal or show CD 8+ lymphs and vacuoles with amyloid. Tubulofilamentous inclusion bodies on electron microscopy
 Kathryn dao
Kathryn dao Imacs tis
Imacs tis Muscles of the mastication
Muscles of the mastication Proximal scleroderma
Proximal scleroderma And gi
And gi Scleroderma occupational therapy
Scleroderma occupational therapy Acrolysis finger
Acrolysis finger Scleroderma symptoms
Scleroderma symptoms Scleroderma face changes
Scleroderma face changes Pro and anti inflammatory
Pro and anti inflammatory Mucorrhea causes
Mucorrhea causes Mechanical vs inflammatory back pain
Mechanical vs inflammatory back pain Odontogenic inflammation
Odontogenic inflammation Inflammatory breast cancer
Inflammatory breast cancer Treatment of inflammatory breast cancer
Treatment of inflammatory breast cancer Paul charlson
Paul charlson Immune reconstitution inflammatory syndrome
Immune reconstitution inflammatory syndrome Immune reconstitution inflammatory syndrome
Immune reconstitution inflammatory syndrome Pelvic inflammatory disease men
Pelvic inflammatory disease men Pelvic girdle pain
Pelvic girdle pain Inflammatory cells
Inflammatory cells Ulcerative colitis vs crohn's
Ulcerative colitis vs crohn's Pus formation
Pus formation Dao and dto
Dao and dto Flitting and fleeting arthritis
Flitting and fleeting arthritis Diabetes and allergies
Diabetes and allergies Subchondrial
Subchondrial Arthritis and food allergies
Arthritis and food allergies Ti dao si nam čvrstu riječ
Ti dao si nam čvrstu riječ Dao deficiency
Dao deficiency Do nebesa nek se ori tekst
Do nebesa nek se ori tekst Data access object pattern java
Data access object pattern java Các kiểu liệt kê
Các kiểu liệt kê Verse dao
Verse dao Irene zhao dao
Irene zhao dao The dao of pooh
The dao of pooh What do you mean by duty cycle
What do you mean by duty cycle Irene zhao
Irene zhao Pashalna noć
Pashalna noć As ondas do mar se revolta
As ondas do mar se revolta Hosana u visini tekst
Hosana u visini tekst Nebo gori zemlja blista tekst
Nebo gori zemlja blista tekst Data access object
Data access object Decentralized autonomous organization (dao)
Decentralized autonomous organization (dao) Lateranska bazilika
Lateranska bazilika Jmt cern
Jmt cern Tko je isusu dao rubac
Tko je isusu dao rubac Dao moral
Dao moral Ca dao tục ngữ về tự lập
Ca dao tục ngữ về tự lập Dao cofactors
Dao cofactors Dao as a service
Dao as a service Dao dang
Dao dang Poststreptococcal reactive arthritis
Poststreptococcal reactive arthritis Steinbrocker stage rheumatoid arthritis
Steinbrocker stage rheumatoid arthritis Arthritis care plan ppt
Arthritis care plan ppt Juvenile rheumatoid arthritis symptoms
Juvenile rheumatoid arthritis symptoms Eular psoriatic arthritis guidelines
Eular psoriatic arthritis guidelines Gonorrhea symptoms female
Gonorrhea symptoms female Anatomi fisiologi asam urat
Anatomi fisiologi asam urat Septic arthritis complications
Septic arthritis complications Septic arthritis antibiotics
Septic arthritis antibiotics Soft tissue rheumatoid arthritis
Soft tissue rheumatoid arthritis Septic arthritis antibiotics
Septic arthritis antibiotics Arthritis foundation indiana
Arthritis foundation indiana Septic arthritis complications
Septic arthritis complications