Juvenile Idiopathic arthritis and infectious arthritis Division of

























- Slides: 50
Juvenile Idiopathic arthritis and infectious arthritis 郭三元 Division of R-I-A TSGH
Juvenile rheumatoid arthritis Juvenile Idiopathic arthritis Juvenile chronic arthritis
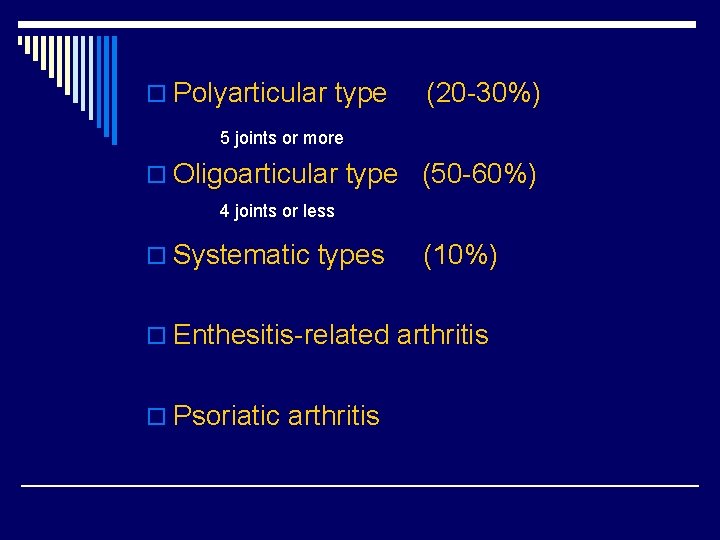
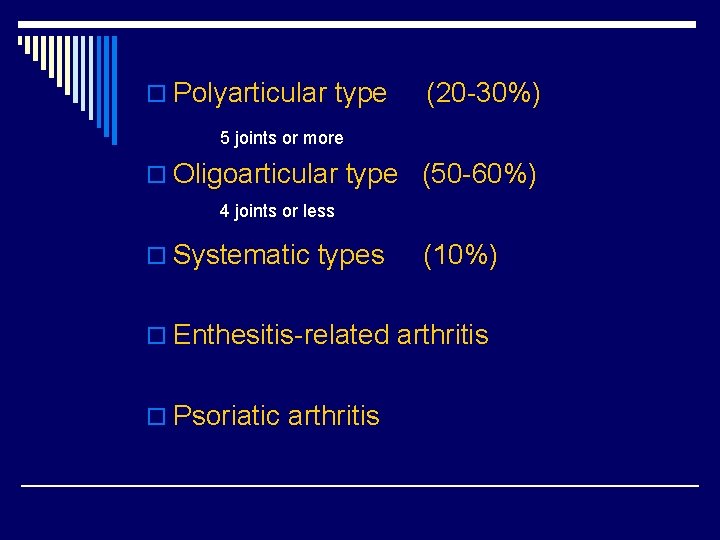
o Polyarticular type (20 -30%) 5 joints or more o Oligoarticular type (50 -60%) 4 joints or less o Systematic types (10%) o Enthesitis-related arthritis o Psoriatic arthritis
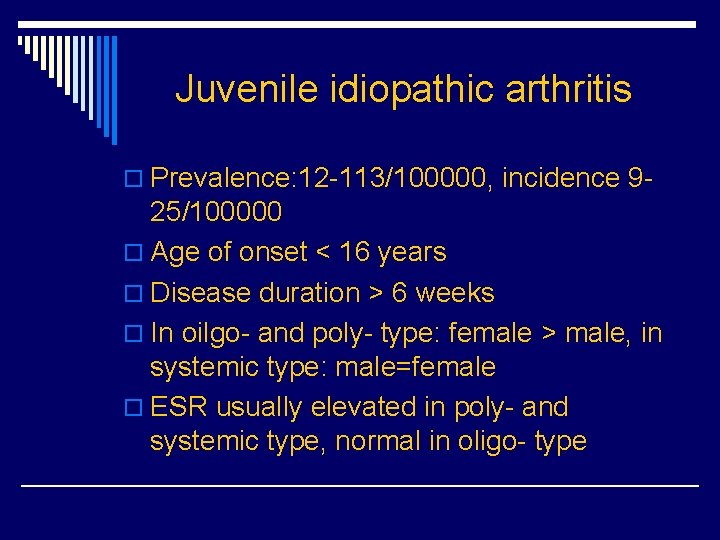
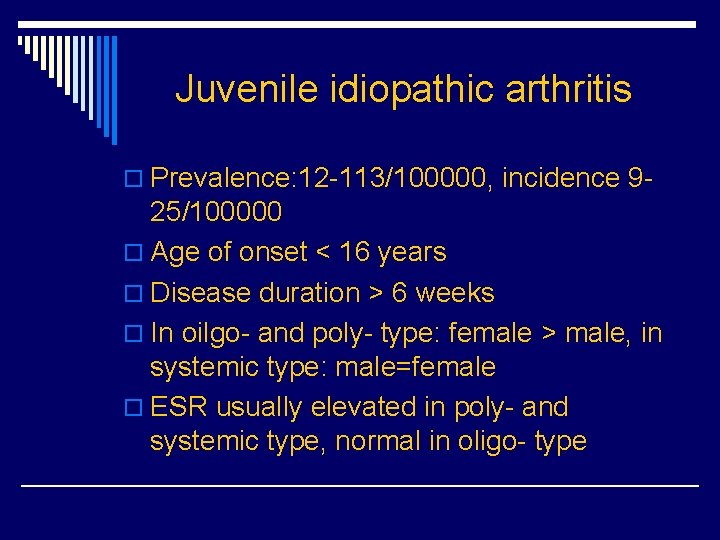
Juvenile idiopathic arthritis o Prevalence: 12 -113/100000, incidence 9 - 25/100000 o Age of onset < 16 years o Disease duration > 6 weeks o In oilgo- and poly- type: female > male, in systemic type: male=female o ESR usually elevated in poly- and systemic type, normal in oligo- type
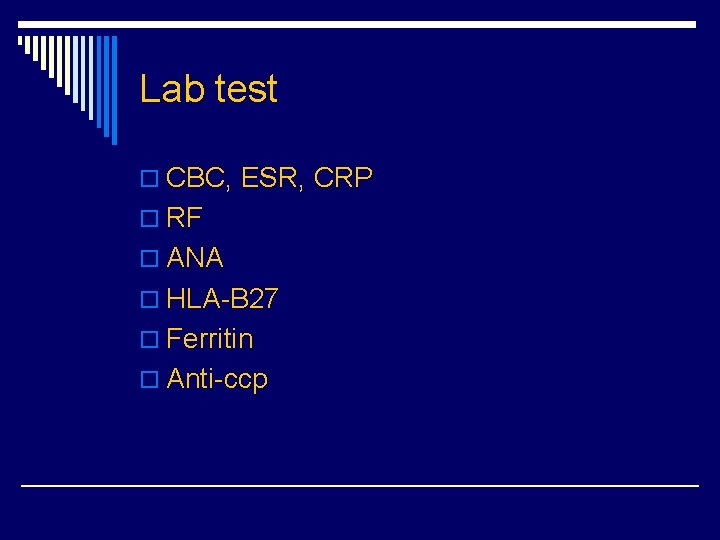
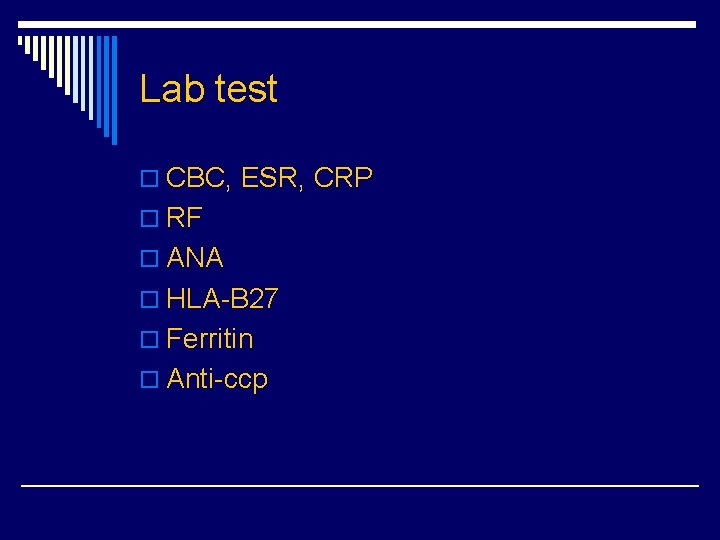
Lab test o CBC, ESR, CRP o RF o ANA o HLA-B 27 o Ferritin o Anti-ccp
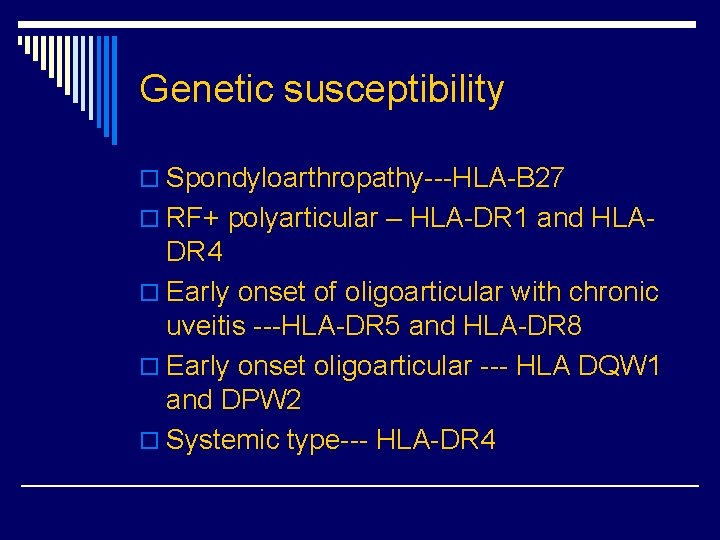
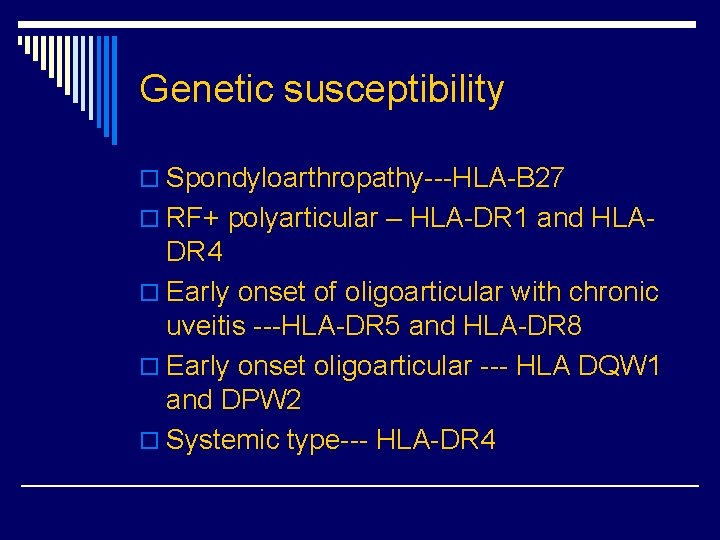
Genetic susceptibility o Spondyloarthropathy---HLA-B 27 o RF+ polyarticular – HLA-DR 1 and HLA- DR 4 o Early onset of oligoarticular with chronic uveitis ---HLA-DR 5 and HLA-DR 8 o Early onset oligoarticular --- HLA DQW 1 and DPW 2 o Systemic type--- HLA-DR 4
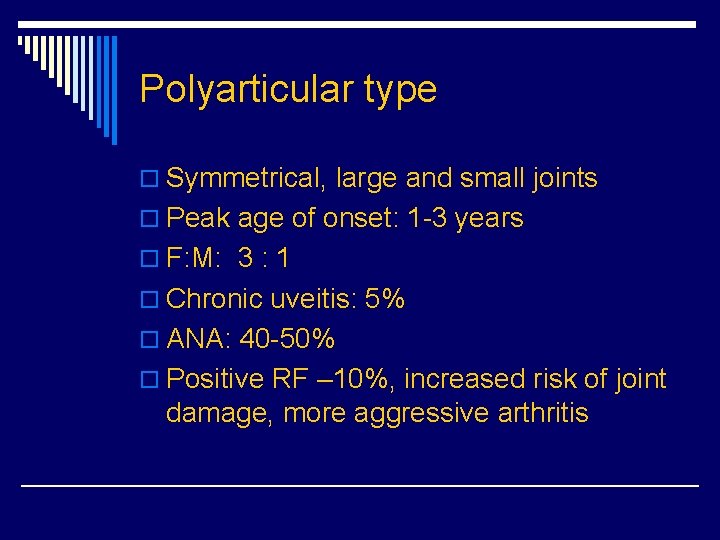
Polyarticular type o Symmetrical, large and small joints o Peak age of onset: 1 -3 years o F: M: 3 : 1 o Chronic uveitis: 5% o ANA: 40 -50% o Positive RF – 10%, increased risk of joint damage, more aggressive arthritis




Oligoarticular type o Peak age of onset: 2 -5 years o F: M 5 : 1 o High frequency of positive ANA (70 -80%) o Chronic uveitis- related to positive ANA o RF: rare o Old age of onset (> 6 year), more often in males, with often HLA-B 27 positive

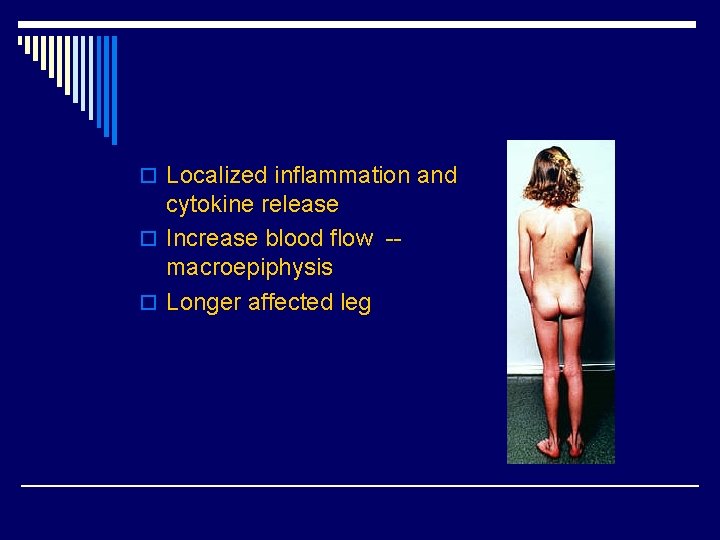
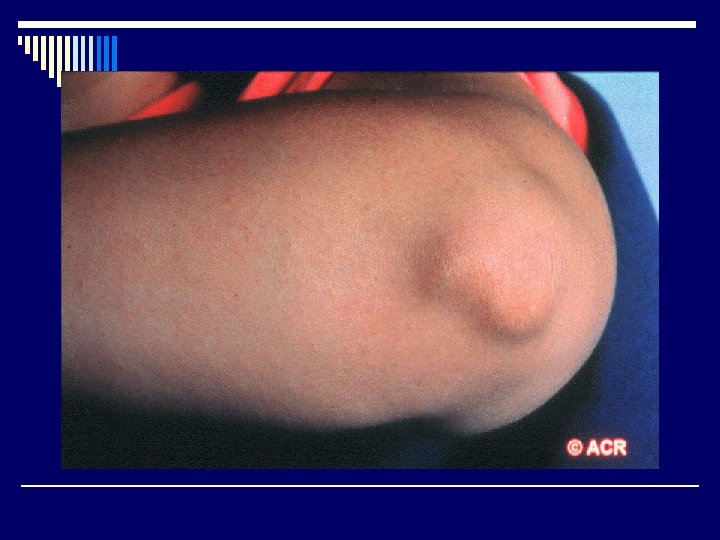
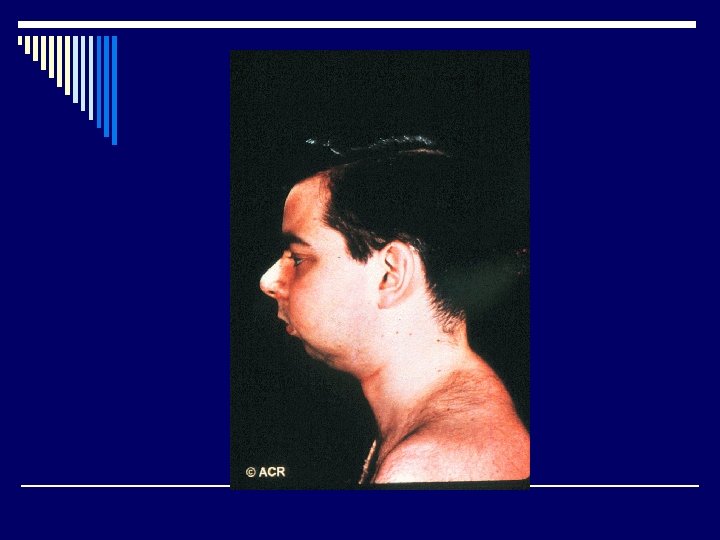
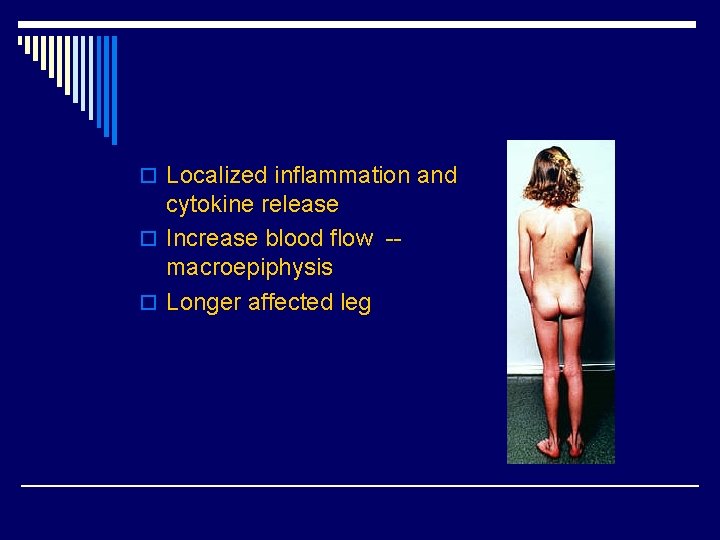
o Localized inflammation and cytokine release o Increase blood flow -macroepiphysis o Longer affected leg




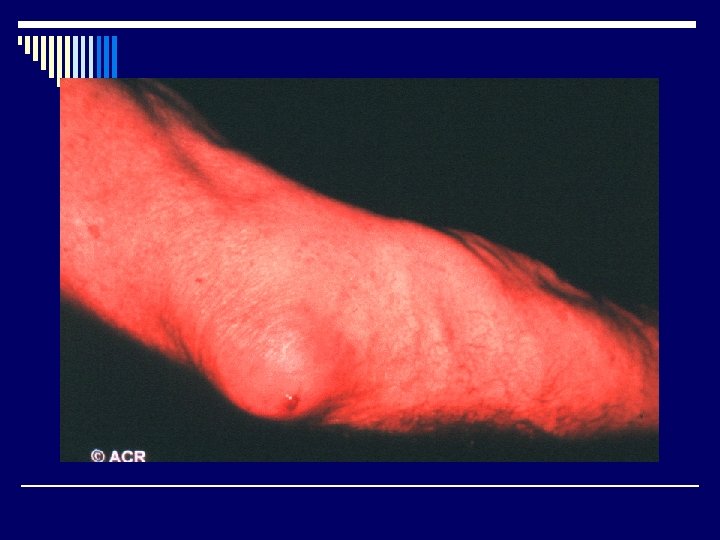
Systemic type (Still’s disease) o Evanescent skin rash (salmon-pink) o High fever o Polyarthragia/arthritis o F: M: 1: 1 o RF: rare o ANA: <10% o Uveitis: rare o hepatosplenomegaly, lymphadenopathy, pericarditis o high ferritin

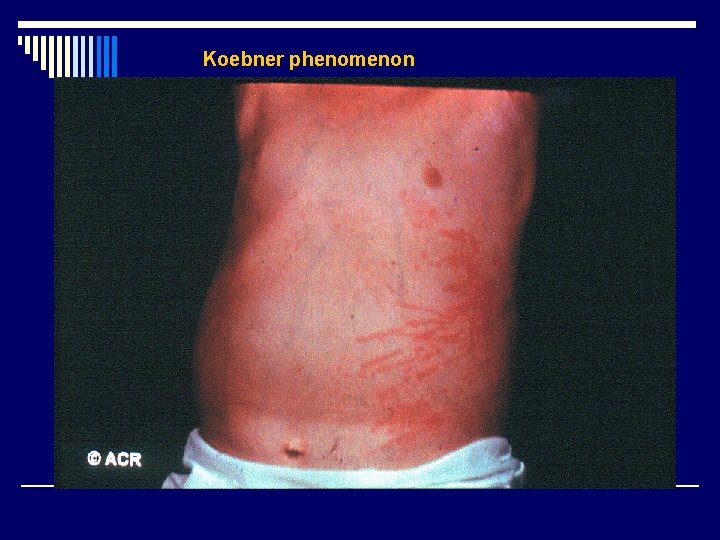
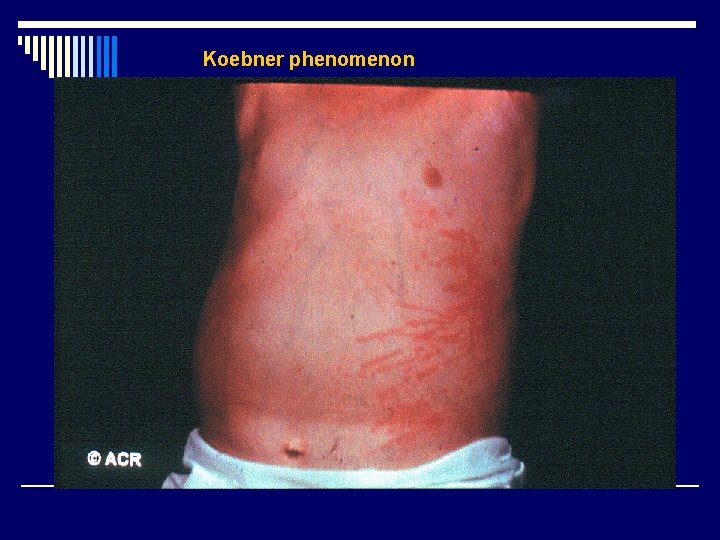
Koebner phenomenon

Management o Minimize the joint damage, early diagnosis and early treatment o Keep muscle strong and limb in good position, keep joint moving o Physical therapy and exercise o Routine eye examination from 3 -4 months interval to one year

Management o NSAIDs o Steroid o DMARDs o Biological agents ( anti-TNFα, anti-IL 6)


Prognosis o Oligoarticular type: 80% resolved after 15 years, 15% develop polyarticular type with severe joints problems, 50% decreased visual acuity after 10 years ( uveitis ) and 25% developed cataract or glaucoma o Polyarticular type: RF(+) showed more severe course and only 33% became independent after 15 years o Systemic type : 50% remission, others developed severe arthritis and especially in cases of disease onset < 5 years-old
Growing pain o Age attacked: 4 -12 years o F: M: 1: 1 o Deep aching, cramping pain in thigh or calf o Usually in evening or during the night, never in the morning o Normal physical examination and laboratory
Infection related arthritis
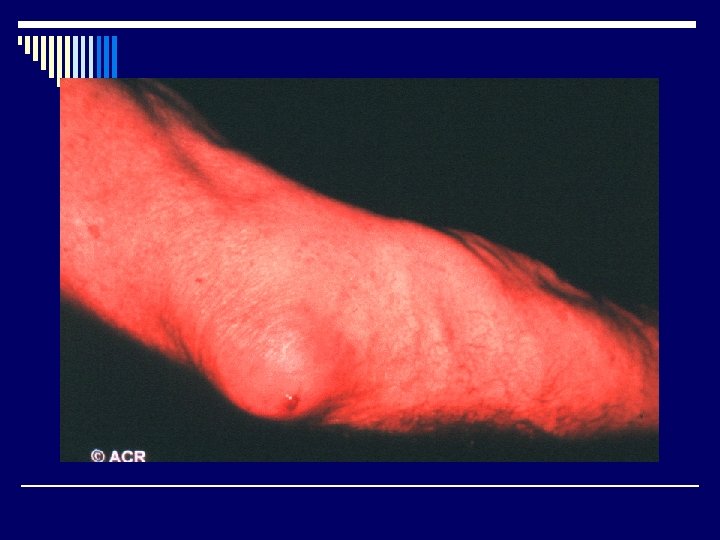
Septic arthritis o Acute onset of monoarthritis o Fever o Elevated ESR or CRP o Synovial fluid: WBC> 50000
Incidence of septic arthritis o 2 -5 /100, 000/year in general population o 5. 5 -12/100, 000/year in children o 28 -38/100, 000/year in RA patients o 40 -68/100, 000/year in prosthetic joint



Pathogenesis o Hematogenous route from a kind of remote o o infectious disease (70% ) – abundant vascular supply of synovium and lack of limiting basement membrane dissemination from near osteomyelitis Lymphatic spread from infection near the joint Iatrogenic infections from arthrocentesis or arthroscope (20% ) Penetrating trauma from plant thorns or other contaminated objects
Predisposing factors o Impaired host defense o Direct penetration o Joint damage o Host phagocytic defect

Impaired host defense o Neoplastic disease o Elderly (>65 years) o Children (<5 years) o Chronic illness ( DM, cirrhosis, chronic renal disease, HIV) o Immunosuppressive agents

Direct penetration o Intravenous drug abuse o Puncture wounds o Invasive procedures
Joint damage o Prosthetic joints o RA o Hemarthrosis o OA
Host phagocytic defects o Complement deficiency o Impaired chemotaxis
Relate to joint o Knee o Hip o Ankle o Shoulder o Wrist o Elbow o Bursa






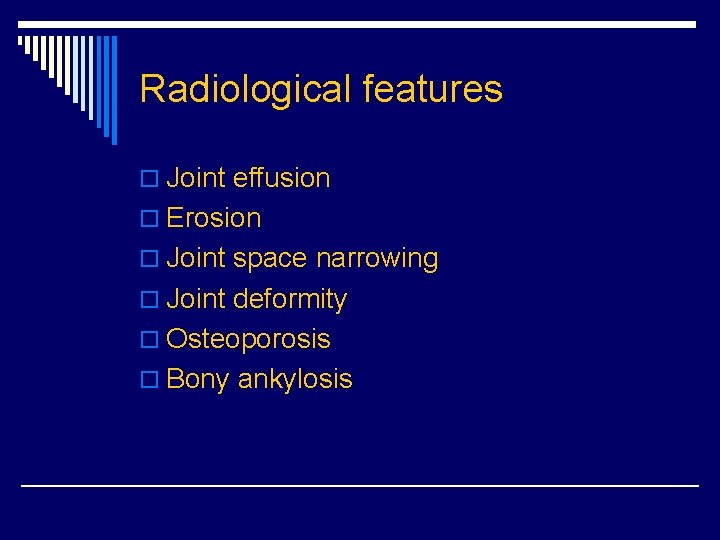
Radiological features o Joint effusion o Erosion o Joint space narrowing o Joint deformity o Osteoporosis o Bony ankylosis
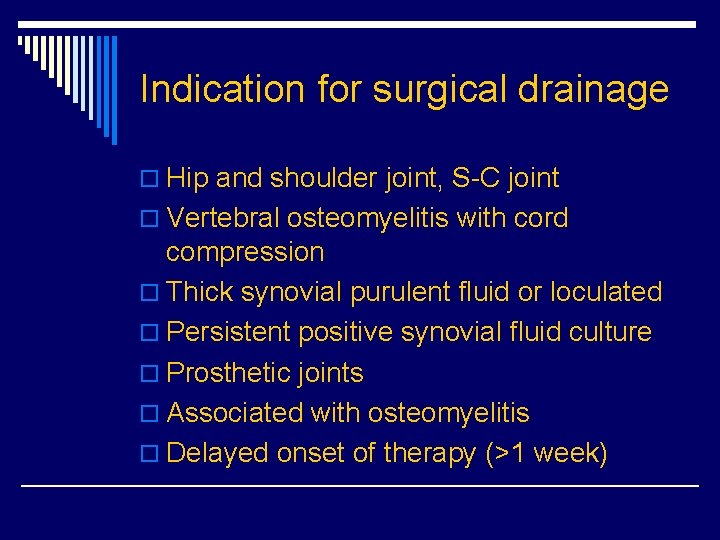
Indication for surgical drainage o Hip and shoulder joint, S-C joint o Vertebral osteomyelitis with cord compression o Thick synovial purulent fluid or loculated o Persistent positive synovial fluid culture o Prosthetic joints o Associated with osteomyelitis o Delayed onset of therapy (>1 week)
 Juvenile rheumatoid arthritis symptoms
Juvenile rheumatoid arthritis symptoms What is subluxation
What is subluxation Mononeuritis multiplex
Mononeuritis multiplex Idiopathic hirsutism
Idiopathic hirsutism Idiopathic oat
Idiopathic oat Pediatric surgery
Pediatric surgery Chapter 26 infectious disease prevention and control
Chapter 26 infectious disease prevention and control Icd 10 morbus hansen
Icd 10 morbus hansen Whmis symbols skeleton hand
Whmis symbols skeleton hand Long division and short division
Long division and short division Short division vs long division
Short division vs long division Synthetic division pattern
Synthetic division pattern Stnthetic division
Stnthetic division Infectious waste meaning
Infectious waste meaning Infectious disease quality controls
Infectious disease quality controls Periods of infectious disease
Periods of infectious disease Stages of infectious disease
Stages of infectious disease Infectious canine hepatitis in dogs
Infectious canine hepatitis in dogs Stridor
Stridor Smallest infectious agents
Smallest infectious agents Papillomitosis
Papillomitosis Infectious nucleic acid
Infectious nucleic acid Blood smear
Blood smear Infectious disease
Infectious disease Infectious mononucleosis
Infectious mononucleosis Hennepin county infectious disease manual
Hennepin county infectious disease manual Emerging infectious diseases
Emerging infectious diseases Noncellular infectious protein particles are called
Noncellular infectious protein particles are called Infectious stunting syndrome
Infectious stunting syndrome Flitting and fleeting arthritis
Flitting and fleeting arthritis Food allergies and arthritis
Food allergies and arthritis Difference between osteoarthritis and rheumatoid arthritis
Difference between osteoarthritis and rheumatoid arthritis Arthritis and food allergies
Arthritis and food allergies Department of juvenile observation and protection
Department of juvenile observation and protection What is the nature and extent of juvenile delinquency
What is the nature and extent of juvenile delinquency Chapter 11 basic concepts street law
Chapter 11 basic concepts street law Poverty and delinquency
Poverty and delinquency Diversion program under ra 9344
Diversion program under ra 9344 Poststreptococcal reactive arthritis
Poststreptococcal reactive arthritis Steinbrocker stage rheumatoid arthritis
Steinbrocker stage rheumatoid arthritis Arthritis care plan ppt
Arthritis care plan ppt Eular recommendations psoriatic arthritis
Eular recommendations psoriatic arthritis Gonorrhea
Gonorrhea Anatomi fisiologi gout arthritis
Anatomi fisiologi gout arthritis Septic arthritis complications
Septic arthritis complications Septic arthritis antibiotics
Septic arthritis antibiotics Abatacept
Abatacept Septic arthritis antibiotics
Septic arthritis antibiotics Arthritis foundation indiana
Arthritis foundation indiana Septic arthritis complications
Septic arthritis complications Caprine arthritis encefalitis
Caprine arthritis encefalitis