Rickettsiaceae Do not confuse with Rickets Vitamin D






























- Slides: 78

Rickettsiaceae
Do not confuse with Rickets Vitamin D or calcium deficiency that leads to soft bones
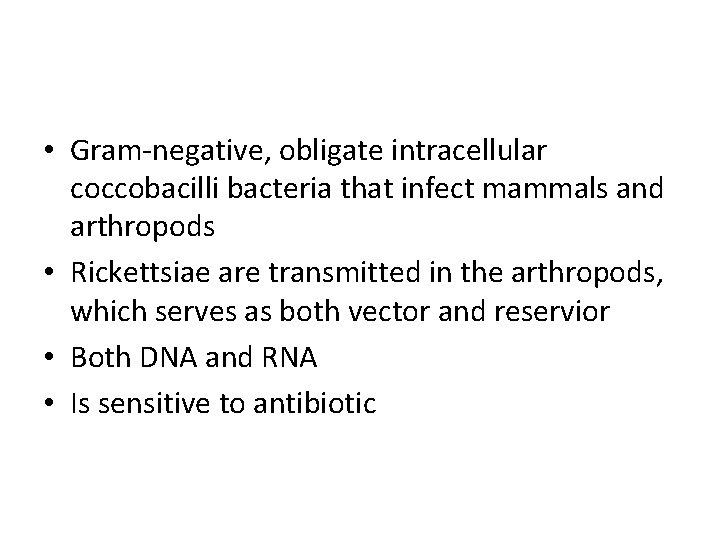
• Gram-negative, obligate intracellular coccobacilli bacteria that infect mammals and arthropods • Rickettsiae are transmitted in the arthropods, which serves as both vector and reservior • Both DNA and RNA • Is sensitive to antibiotic
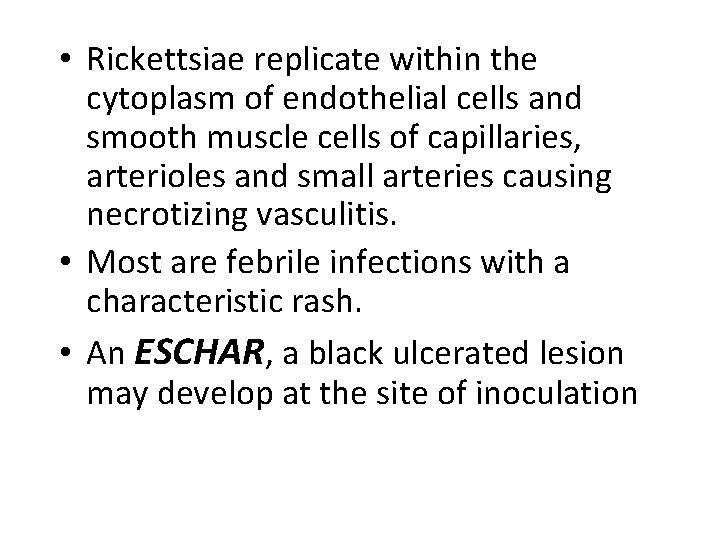
• Rickettsiae replicate within the cytoplasm of endothelial cells and smooth muscle cells of capillaries, arterioles and small arteries causing necrotizing vasculitis. • Most are febrile infections with a characteristic rash. • An ESCHAR, a black ulcerated lesion may develop at the site of inoculation
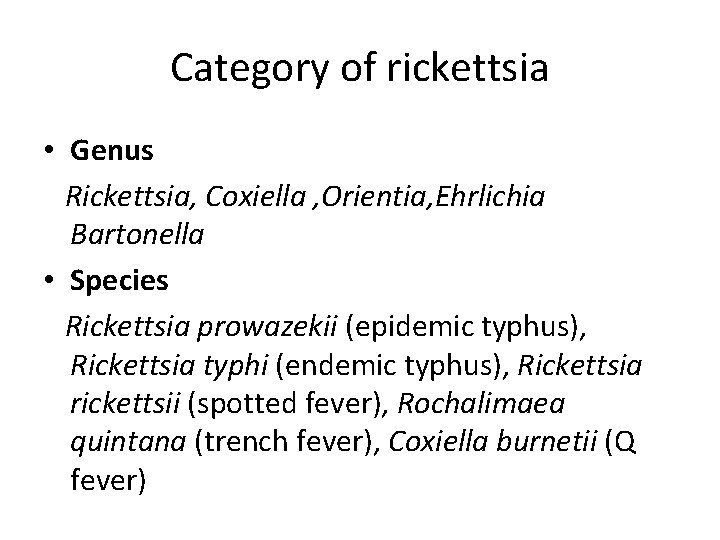
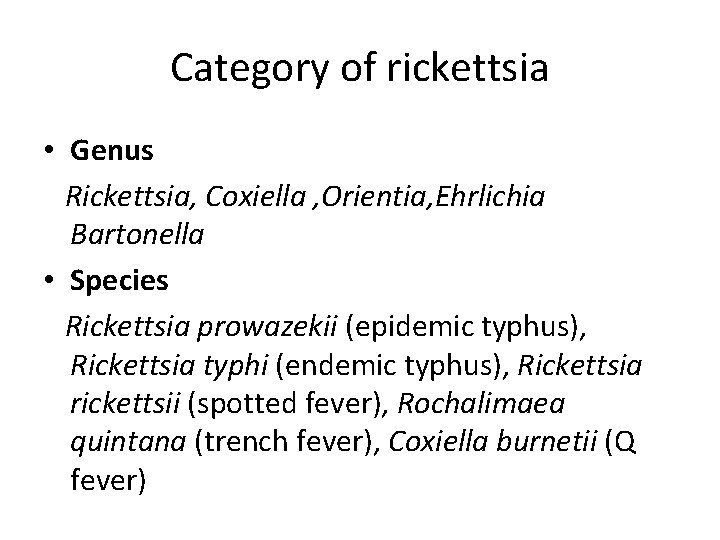
Category of rickettsia • Genus Rickettsia, Coxiella , Orientia, Ehrlichia Bartonella • Species Rickettsia prowazekii (epidemic typhus), Rickettsia typhi (endemic typhus), Rickettsia rickettsii (spotted fever), Rochalimaea quintana (trench fever), Coxiella burnetii (Q fever)
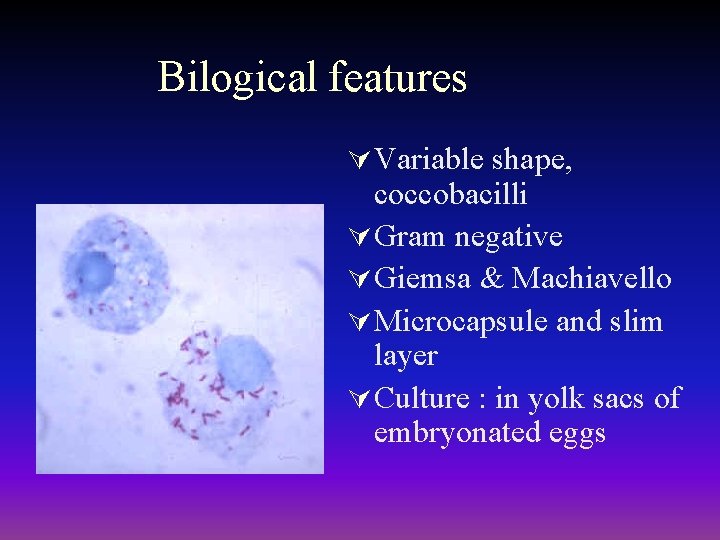
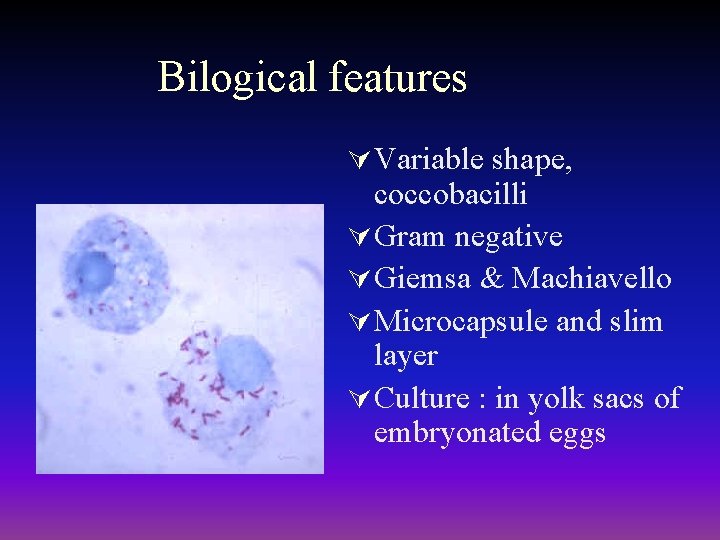
Bilogical features Ú Variable shape, coccobacilli Ú Gram negative Ú Giemsa & Machiavello Ú Microcapsule and slim layer Ú Culture : in yolk sacs of embryonated eggs

Antigenic structure Ú LPS Rickettsia tsutsugamushi Coxiella burnetii (Q fever) LPSⅠ smooth LPSⅡ rough Ú Surface protein(SPA)

Replication cycle of Rickettsia and Orientia
Ú Rickettsial diseases may be grouped on the basis of Clinical features and Epidemiological aspects as follows:
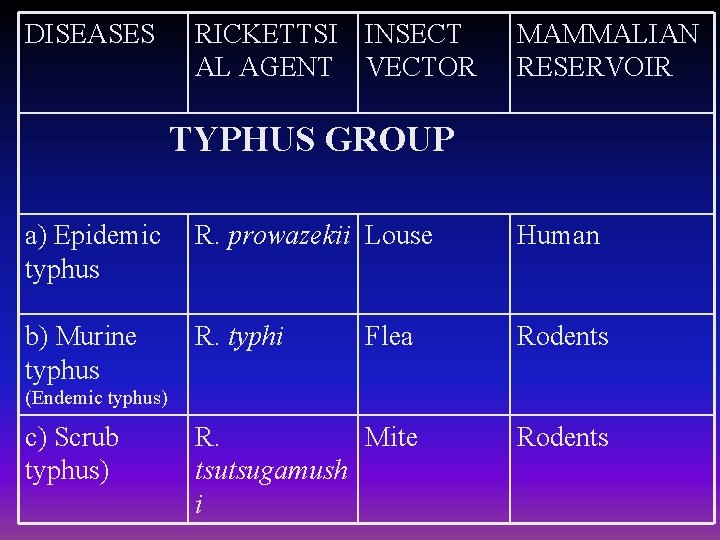
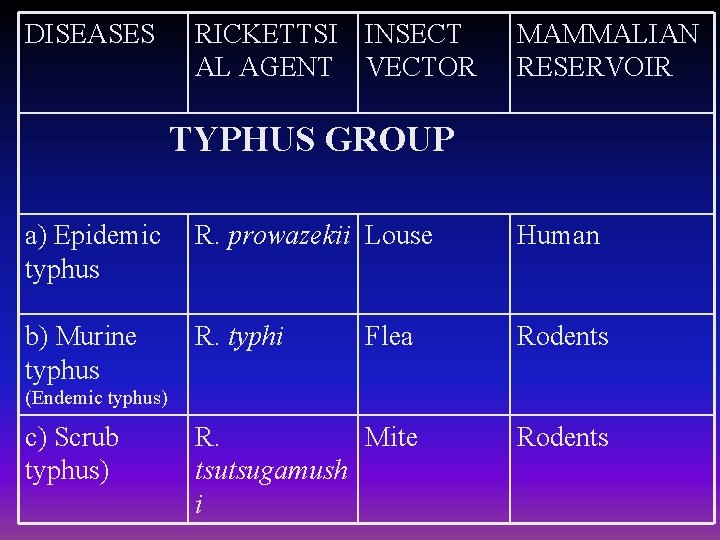
DISEASES RICKETTSI INSECT AL AGENT VECTOR MAMMALIAN RESERVOIR TYPHUS GROUP a) Epidemic typhus R. prowazekii Louse Human b) Murine typhus R. typhi Flea Rodents R. Mite tsutsugamush i Rodents (Endemic typhus) c) Scrub typhus)
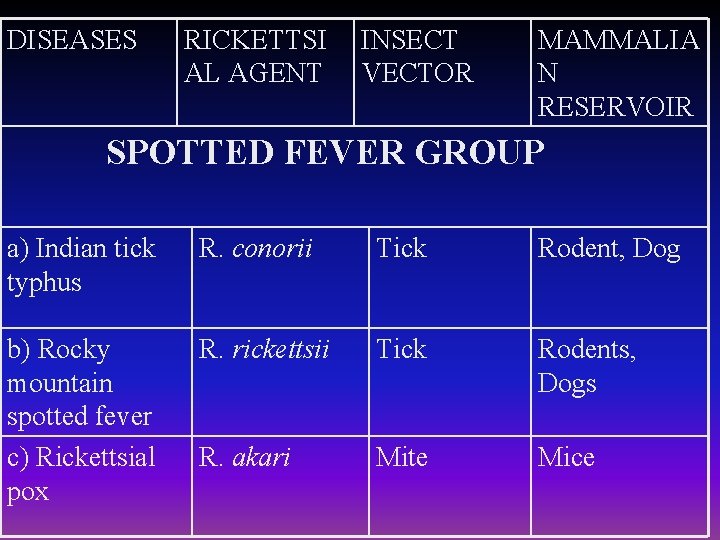
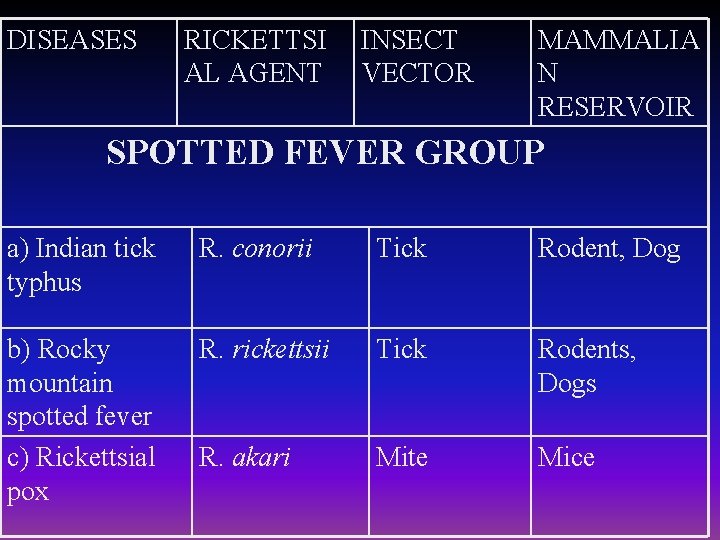
DISEASES RICKETTSI AL AGENT INSECT VECTOR MAMMALIA N RESERVOIR SPOTTED FEVER GROUP a) Indian tick typhus R. conorii Tick Rodent, Dog b) Rocky mountain spotted fever c) Rickettsial pox R. rickettsii Tick Rodents, Dogs R. akari Mite Mice
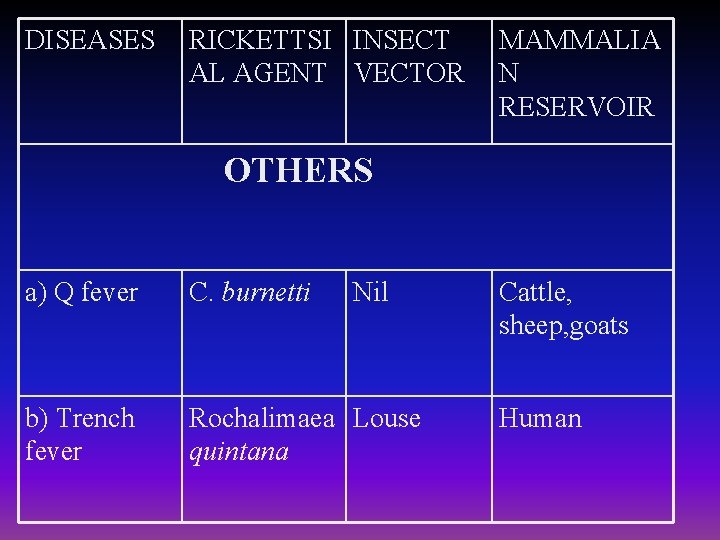
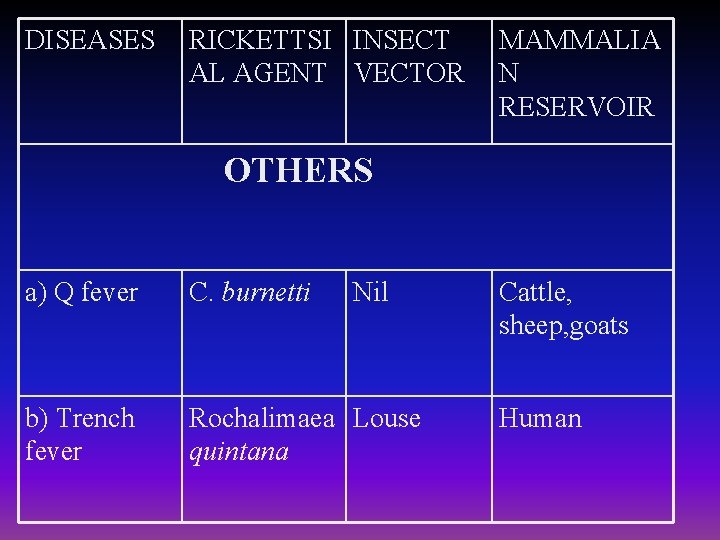
DISEASES RICKETTSI INSECT AL AGENT VECTOR MAMMALIA N RESERVOIR OTHERS a) Q fever C. burnetti Nil b) Trench fever Rochalimaea Louse quintana Cattle, sheep, goats Human
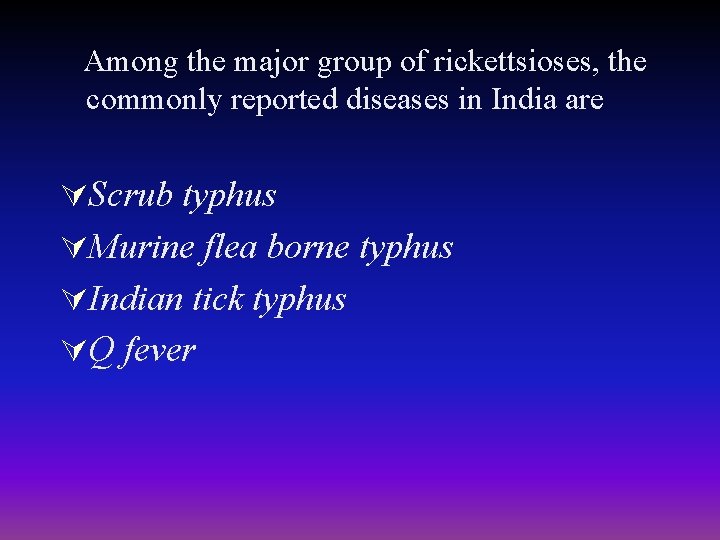
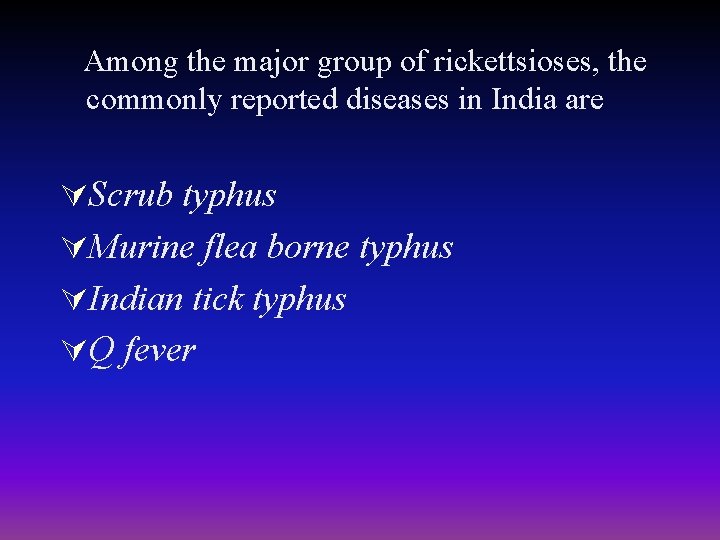
Among the major group of rickettsioses, the commonly reported diseases in India are ÚScrub typhus ÚMurine flea borne typhus ÚIndian tick typhus ÚQ fever
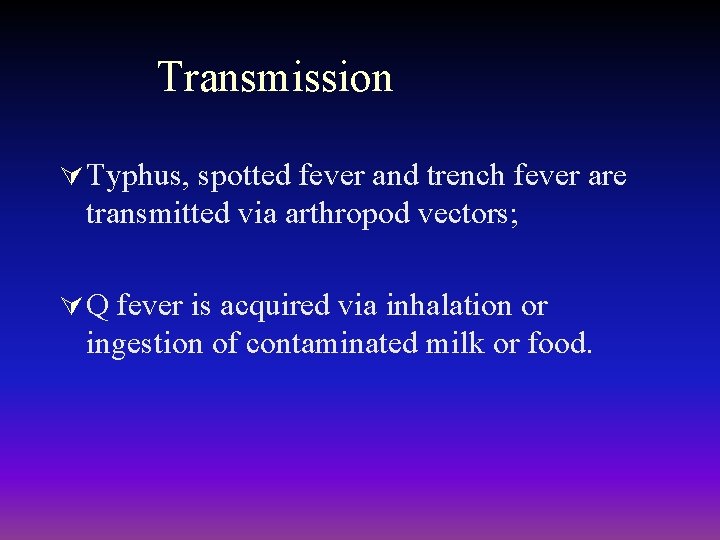
Transmission Ú Typhus, spotted fever and trench fever are transmitted via arthropod vectors; Ú Q fever is acquired via inhalation or ingestion of contaminated milk or food.
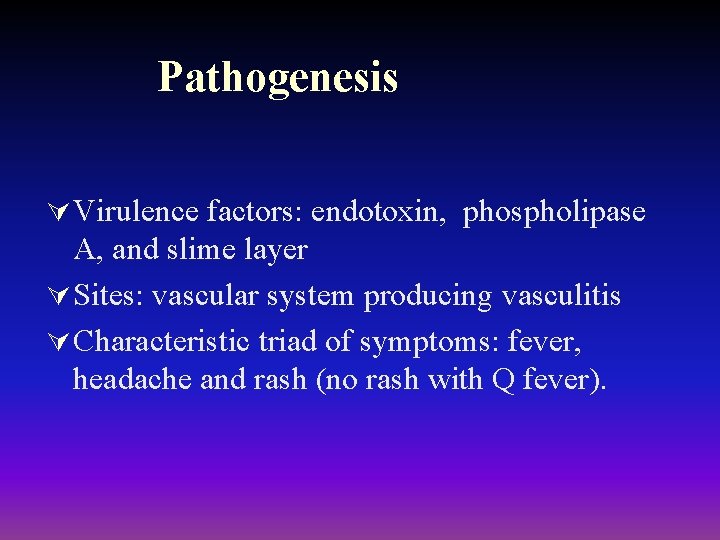
Pathogenesis Ú Virulence factors: endotoxin, phospholipase A, and slime layer Ú Sites: vascular system producing vasculitis Ú Characteristic triad of symptoms: fever, headache and rash (no rash with Q fever).

Typhus Group

Rickettsia prowazekii Ú Epidemic typhus Ú Brill-Zinsser disease Fluorescent-Ab staining Vector - Louse

Epidemiology - R. prowazekii Epidemic typhus Ú Associated with unsanitary conditions – War, famine, etc. (also called camp fever) Ú Vector - human body louse – Bacteria found in feces and when bite scratched the bacteria infect Ú Reservoir – Primarily humans (epidemic form) – No transovarian transmission in the louse (bacteria kills louse) Ú Sporadic disease in Southeastern USA – Reservoir - flying squirrels – Vector - squirrel fleas
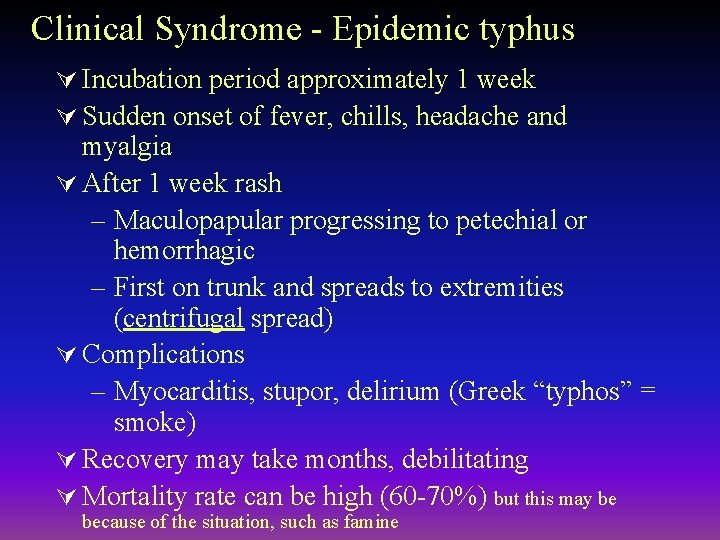
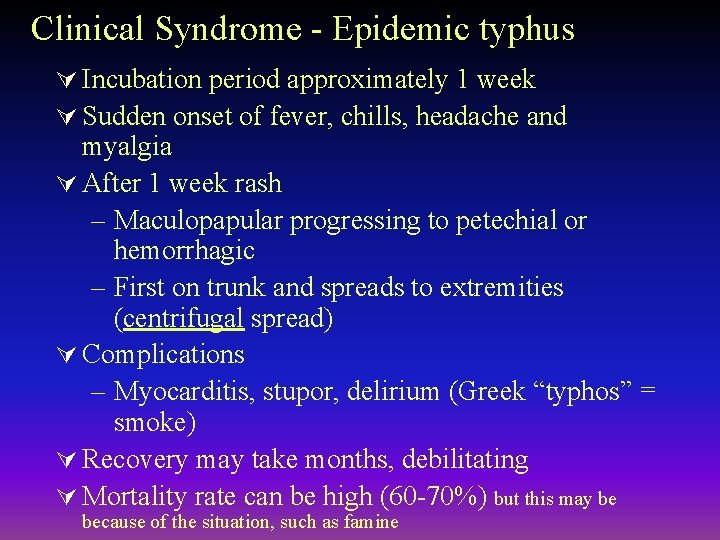
Clinical Syndrome - Epidemic typhus Ú Incubation period approximately 1 week Ú Sudden onset of fever, chills, headache and myalgia Ú After 1 week rash – Maculopapular progressing to petechial or hemorrhagic – First on trunk and spreads to extremities (centrifugal spread) Ú Complications – Myocarditis, stupor, delirium (Greek “typhos” = smoke) Ú Recovery may take months, debilitating Ú Mortality rate can be high (60 -70%) but this may be because of the situation, such as famine
Clinical Syndrome - Brill-Zinsser Disease Ú Recrudescent epidemic typhus – Commonly seen in those exposed during WWII (maybe decades later) – Rickettsiae remain latent in lymphatic tissues Ú Disease is similar to epidemic typhus but milder Ú Rash is rare
Laboratory Diagnosis - R. prowazekii Ú Weil-Felix antibodies - not recommended Ú Isolation possible but dangerous Ú Serology – Indirect fluorescent Ab and latex agglutination tests – Epidemic typhus - Ig. M followed by Ig. G Abs – Brill-Zinsser - Ig. G anamnestic response

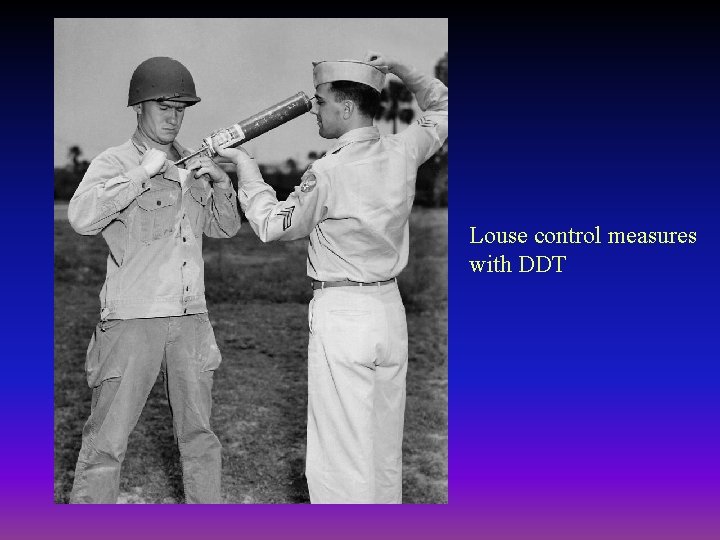
Treatment, prevention and Control R. prowazekii Ú Tetracycline (doxycycline) and chloramphenicol Ú Louse control measures Ú Vaccine available for high risk populations
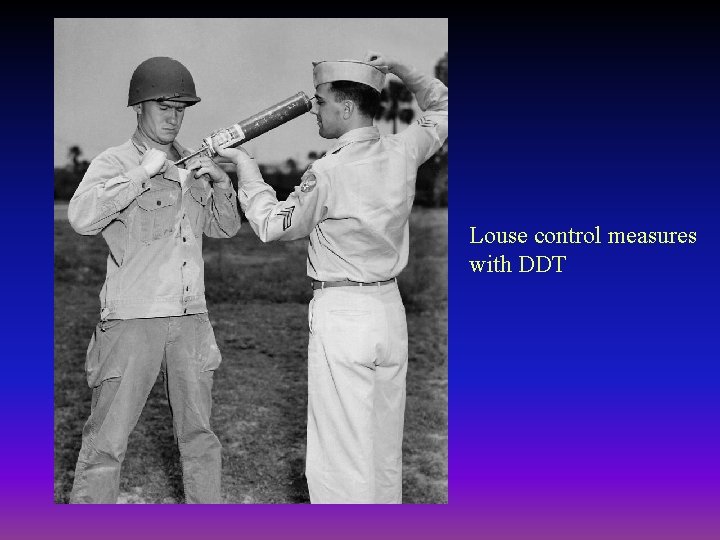
Louse control measures with DDT

Rickettsia typhi (R. mooseri) - Murine or endemic typhus Epidemiology • Occurs worldwide • Vector - rat flea – Bacteria in feces • Reservoir - rats – No transovarian transmission – Normal cycle - rat to flea to rat • Humans accidentally infected
Clinical Syndrome- Murine Typhus Ú Incubation period 1 - 2 weeks Ú Sudden onset of fever, chills, headache and myalgia Ú Rash in most cases – Begins on trunk and spreads to extremities (centrifugal spread) Ú Mild disease - resolves even if untreated
Laboratory Diagnosis - R. typhi Ú Neil-Mooser reaction – Blood from patient is injected intraperitoneally to male Guinea pigs – Develop fever and scrotal inflammation – Enlarged testes cannot be pushed back into abdomen – Neil-Mooser reaction – Negative in epidemic typhus Ú Serology – Indirect fluorescent antibody test (not done in a routine laboratory
Treatment, Prevention, and Control R. typhi Ú Tetracycline (doxycycline) Ú Control rodent reservoir Ú No effective vaccine

Spotted Fever Group
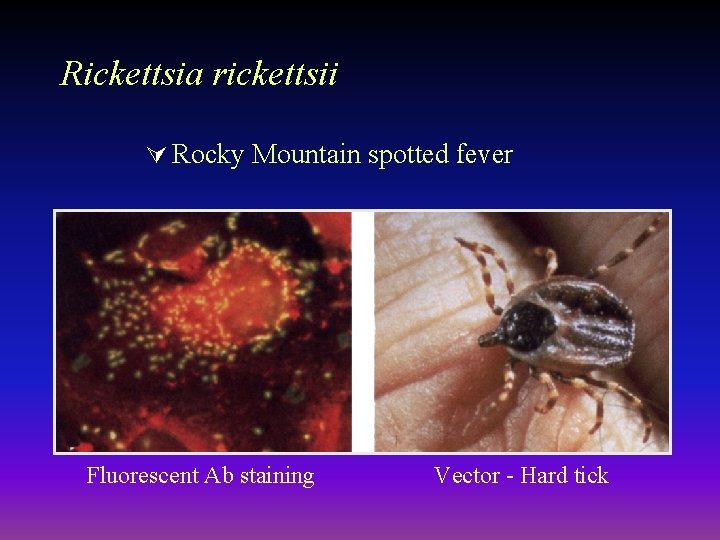
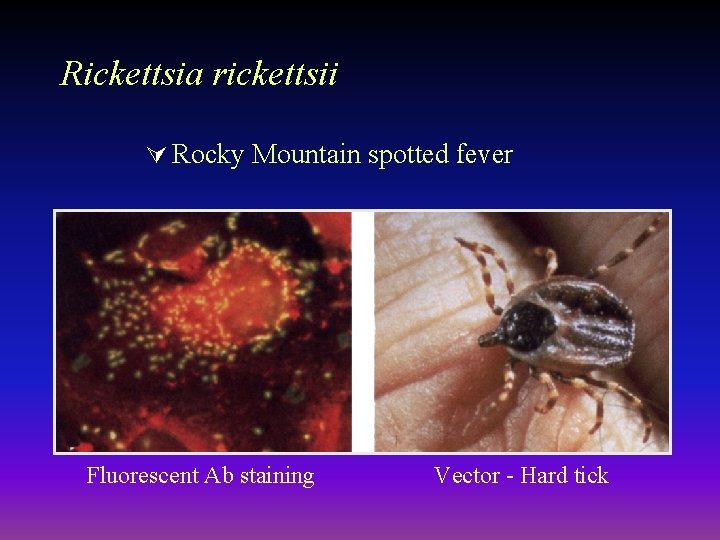
Rickettsia rickettsii Ú Rocky Mountain spotted fever Fluorescent Ab staining Vector - Hard tick
Epidemiology - R. rickettsii Rocky Mountain Spotted Fever Ú Most common from April - September Ú Vector - Ixodid (hard) tick via saliva – Prolonged exposure to tick is necessary (bacteria in gut and blood meal stimulates bacteria to divide, goes to salivary glands, then to human) Ú Reservoirs - ticks (transovarian passage to eggs) and rodents – Humans are accidentally infected
Clinical Syndrome - Rocky Mountain Spotted Fever Ú Incubation period - 2 to 12 days Ú Abrupt onset fever, chills, headache and myalgia (present in many conditions) Ú Rash appears 2 -3 days later in most (90%) patients – Begins on hands and feet and spreads to trunk, regardless of bite location (centripetal spread) – Palms and soles commonly have rash – Maculopapular but can become petechial or hemorrhagic

Rash of Rocky Mountain Spotted Fever rash

Clinical Syndrome - Rocky Mountain Spotted Fever ÚComplications from widespread vasculitis – Gastrointestinal, respiratory, seizures, coma, renal failure – Most common when rash does not appear (10% of cases) ÚMortality in untreated cases - 20%
Laboratory Diagnosis - R. rickettsii Ú Initial diagnosis - clinical grounds (important to begin treatment) Ú Fluorescent Ab test for Ag in punch biopsy reference labs Ú PCR based tests - reference labs Ú Weil-Felix test Ú Serology – Indirect fluorescent Ab test for Ab – Latex agglutination test for Ab
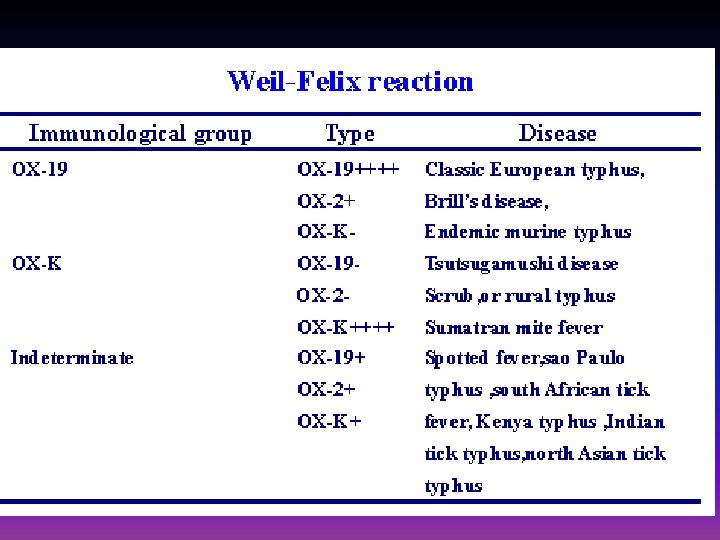
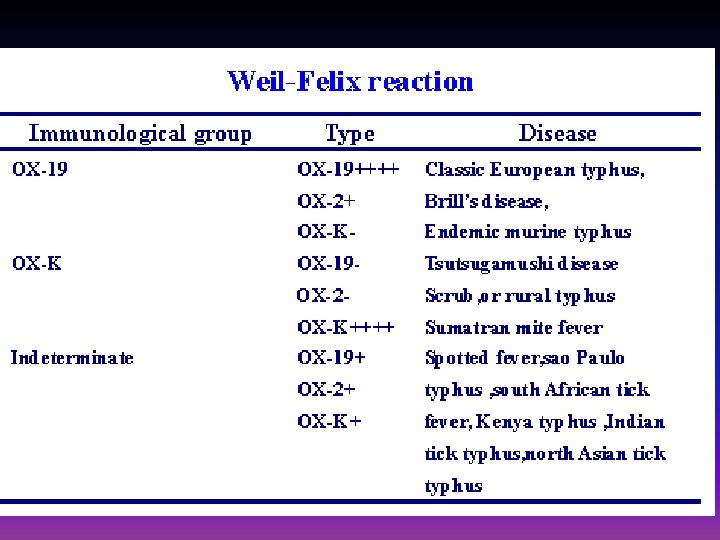
WEIL-FELIX TEST Ú Sera from Epidemic and Endemic typhus agglutinate OX 19 and sometimes OX 2. Ú In tick borne spotted fever, both OX 19 and Ox 2 are agglutinated. Ú OXK agglutinins are found only in scrub typhus. The test is negative in Rickettsial pox, Trench fever, and Q fever.
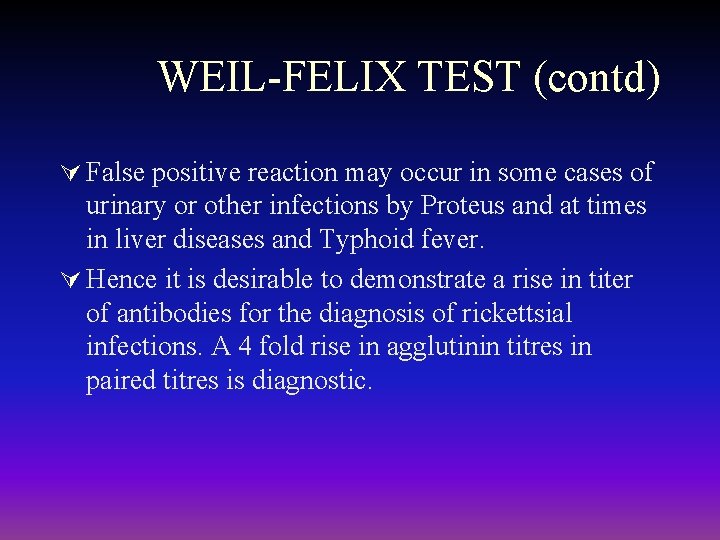
WEIL-FELIX TEST (contd) Ú False positive reaction may occur in some cases of urinary or other infections by Proteus and at times in liver diseases and Typhoid fever. Ú Hence it is desirable to demonstrate a rise in titer of antibodies for the diagnosis of rickettsial infections. A 4 fold rise in agglutinin titres in paired titres is diagnostic.

WEIL-FELIX TEST (contd) ÚHowever, with a single serum sample available, the test is suggestive of infection only at a high cut off titer (≥ 1: 320) at which the positive predictive value and the specificity is reliable.
ÚThe serological tests for Rickettsial diseases including the specific Ig. M antibody tests become positive only in the second week and a second sample is often required. ÚSerological tests cannot provide early diagnosis and a specific diagnosis may not be available until after the patient has died or recovered.
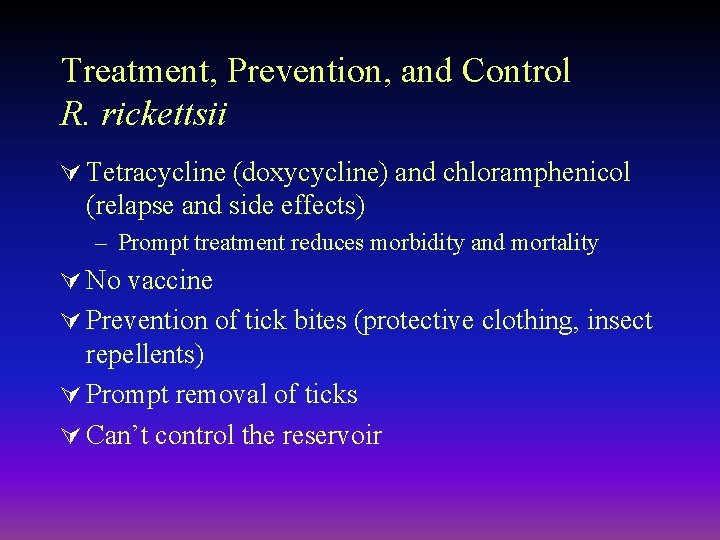
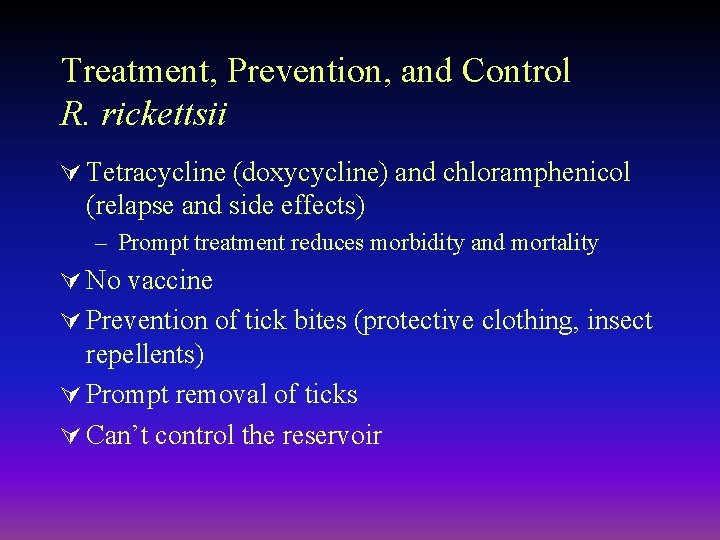
Treatment, Prevention, and Control R. rickettsii Ú Tetracycline (doxycycline) and chloramphenicol (relapse and side effects) – Prompt treatment reduces morbidity and mortality Ú No vaccine Ú Prevention of tick bites (protective clothing, insect repellents) Ú Prompt removal of ticks Ú Can’t control the reservoir
Rickettsia akari - Rickettsialpox Epidemiology • Sporadic infection in USA (urban areas) • Vector - house mite • Reservoir - mites (transovarian transmission) and mice • Humans accidentally infected
Clinical Syndrome -Rickettsialpox Ú Phase I (1 week incubation period) – papule at bite site – Eschar formation Ú Phase II (1 -3 week later) – Sudden onset of fever, chills headache and myaglia – Generalized rash - papulovesicular, crusts (rash resembles chicken pox) Ú Mild disease; fatalities are rare
Laboratory Diagnosis - R. akari Ú Not available except in reference laboratories
Treatment, Prevention, and Control R. akari ÚTetracycline (doxycycline) ÚControl of mouse population

Scrub Typhus Group

Orientsia (Rickettsia) tsutsugamushi ÚScrub typhus ÚJapanese “tsutsuga” = small and dangerous and “mushi” = creature Ú“Scrub” - associated with terrain with scrub vegetation
Epidemiology - O. tsutstugamushi Scrub Typhus ÚVector - Trombicula deliensis (mite larva) ÚReservoir - chiggers and rats – Transovarian transmission – Normal cycle - rat to mite to rat ÚHumans are accidentally infected
Clinical Syndrome - Scrub Typhus ÚIncubation period - 1 to 3 weeks ÚSudden onset of fever, chills, headache and myalgia ÚMaculopapular rash (spots and bumps) – Begins on trunk and spreads to extremities (centrifugal spread) ÚMortality rates variable (1 -15%)
CLINICAL FEATURES: § Fever, Chills, Generalised Lymphadenopathy § ESCHAR – A punched out ulcer covered with a blackened scab which indicates the location of the mite bite.
ÚEschar is found only in around 50% of patients. ÚEschar is painless and patient wont complain of it. ÚOften the patient wont notice it because of its presence in concealed sites.

COMPLICATIONS Occurs mainly in untreated cases ÚMyocarditis ÚAnicteric Hepatitis ÚEncephalitis ÚInterstitial pneumonitis
INVESTIGATIONS Ú PCR – Amplification of O tsutsugamushi DNA from the blood of febrile patients. SEROLOGICAL TESTS such as Ú Indirect Flourescent antibody test (IFA) test ( Titer ≥ 1: 200 ), Ú the Complement Fixation Test. Ú The Weil Felix Test Ú Scrub Ig. M ELISA Test: Highly specific test
TREATMENT Ú Tetracycline is the DOC. Ú Doxycycline 100 mg Bid PO × 7 -15 days. Ú Chloramphenicol 500 mg qid PO× 7 -15 days. Ú IV Chloramphenicol 150 mg/ kg per day for 5 days.
CONTROL: ÚVector control. Clearing the vegetation where rats and mice live. ÚRodent control

Coxiella burnetti ÚQ fever ÚCow and sheep Útick ÚHigh resistance abrupt onset , fever, headache, chills, myalgia, granulomatous hepatitis chronic diaease with subacute onset , endocarditis, hepatic dysfunction

ÚReservoir - Wild animals like bandicoot ÚTicks transmit disease to cattle ÚOrganisms shed in milk. Urine, feces, placenta ÚMan – man transmission is rare

Replication of C. burnetii

Lab diagnosis Ú Serology – CFT – IIFT – Weil-Felix is neagtive Ú Treatment – Doxycycline Ú Vaccine – Killed and attenuated vaccines

Bartonella
Microbiology - Bartonella ÚSmall Gram-negative aerobic bacilli ÚDifficult to culture ÚInfect animals but do not cause disease in animals ÚInsects are thought to be the vectors in human disease ÚSome species infect erythrocytes others attach to cells


Bartonella quintana Ú Trench fever (in WWI trenches) – Shin-bone fever – 5 day fever (reoccurs every 5 days)
Epidemiology - B. quintana Trench Fever Ú Associated with war and famine Ú Vector - human body louse – Organism found in feces (like typhus) Ú Reservoir - humans – No transovarian transmission – Cycle - human to louse to human
Clinical Syndrome - Trench Fever Ú Infection may be asymptomatic or severe Ú Sudden onset of fever, chills, headache and myalgia Ú Severe pain in the tibia (shin-bone fever) Ú Symptoms may appear at 5 day intervals (5 day fever) Ú Maculopapular rash may or may not develop on the trunk Ú Mortality rates very low.
Laboratory Diagnosis - B. quintana Ú Blood cultured on sheep blood agar Ú Serology – Weil-Felix test is negative Ú PCR -

Treatment, Prevention, and Control B. quintana Ú Various antibiotics (erythromycin or doxycycline) Ú Control of body louse
Bartonella henselae Ú Cat-scratch disease Ú Acquired from cat bite or scratch and possibly from cat fleas

Clinical Syndrome Cat-scratch Disease ÚBenign disease ÚChronic regional lymphadenopathy
Laboratory Diagnosis - B. henselae ÚLymph node biopsies stained with Warthin-Starry silver stains ÚCulture – blood agar ÚSerology

Treatment - B. henselae ÚTreatment is controversial since it is benign ÚIf treated with antibiotic, then azithromycin is drug of choice

B. bacilliformis Ú Pleomorphic GNB Ú Within RBC’s Ú Causes Oroya fever Ú Transmitted by sandflies Ú Fever, headache, severe anemia, nodular lesions Ú Blood smear – giemsa stain Ú Pencillin, streptomycin

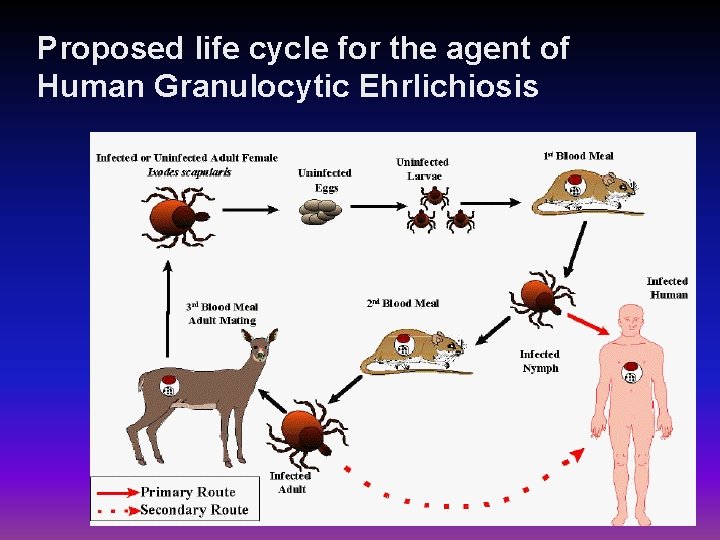
Ehrlichia Ú Ehrlichia chaffeensis: human monocytotropic ehrlichiosis Ú Transmitted by ticks Ú Fever, lecucopenia, thrombocytopenia Ú Ehrlichia phagocytophila; human granulocytic ehrlichiosis – Fever, lecucopenia, thrombocytopenia – Ticks

Ú Ehrlichia sennetsu : human granulocyto- tropic ehrlichiosis Ú Ingestion of raw fish Ú No insect vector Ú Reembles gandular fever
Lab diagnosis Ú Giemsa stain of peripheral blood smear Ú Serology - IIFT

Replication of Ehrlichia
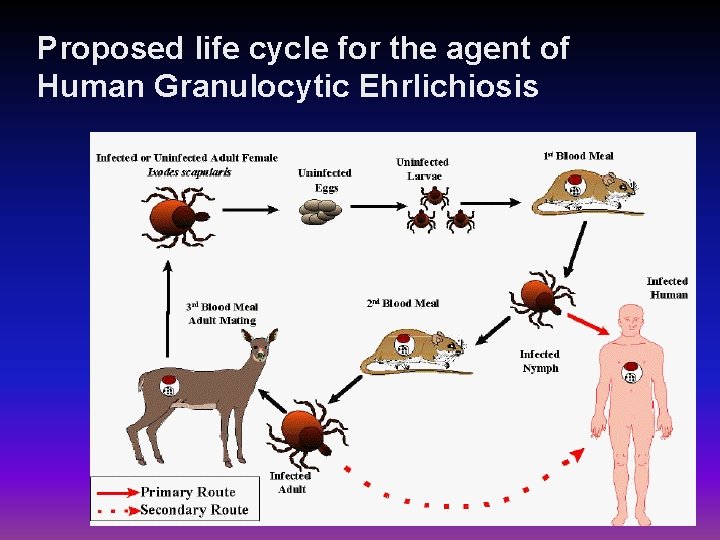
Proposed life cycle for the agent of Human Granulocytic Ehrlichiosis
