ERYTHROPOIESI S In adults if liver and spleen





- Slides: 36
ERYTHROPOIESI S
In adults, if liver and spleen produce RBCs if bone marrow is destroyed or fibrosed. Bone marrow is equal to liver in size and weight. Involved in the production of cells. 75% leukocytes are produced and 25% erythrocytes. WBC-RBC ratio: 1: 500 Difference in life span.

Erythropoiesis: Process of origin, development and maturation of red blood cells. Hemopoiesis or hematopoiesis: � Process of origin, development and maturation of all blood cells.
PROCESS OF ERYTHROPOIESIS: STEM CELLS: Blood cells are formed in the bone marrow from stem cells called pluripotential haematopoietic stem cells. Also called uncommitted pluripotential haematopoietic stem cells (PHSC). All the cells of circulation are derived from these cells. During reproduction, few PHSC remain like the cells of origin to maintain the supply. When cells are differentiated to form particular types of blood cells, uncommitted PHSC are converted to committed PHSC. These are the cells restricted to give rise to specific type of blood cells.
Two types of PHSCs: 1. lymphoid stem cells: � Lymphocytic cells. 2. colony forming blastocytes: � Myeloid cells. � When grown in culture these cells form colonies.
Units of colony forming cells: A committed stem cell that forms erythrocytes is called colony forming unit erythrocytes. CFU -E Colony forming units that form granulocytes and monocytes have designation CFU-GM. These cells give rise to neutrophils, eosinophils and basophils. Colony forming unit-megakaryocytes CFU-M. Platelets are developed from these cells.

Changes during erythropoiesis: CFU-E in the process of maturation pass through 4 stages: Reduction in size of cells: � 25 to 7. 2 micrometer. Disappearance of nuclei and nucleus. Appearance of haemoglobin. Changes in the staining properties of cytoplasm.
STAGES OF ERYTHROPOIESIS: 1. Proerythroblast. 2. Early normoblast. 3. Intermediate normoblast. 4. Late normoblast. 5. Reticulocyte. 6. Matured erythrocyte.
1. PROERYTHROBLAST: Megaloblast First cell derived from CFU-E Large with 20 micrometer diameter. Cytoplasm is basophilic in nature. Large nucleus occupying the cell completely. Nucleus has 2 or more nucleoli and reticular network. No haemoglobin. Multiplies several times to form early normoblasts.
2. EARLY NORMOBLAST: Synthesis of haemoglobin starts in this stage. Smaller than proerythroblasts. 15 micrometer diameter. Cytoplasm is basophillic in nature. Cell is also called basophilic erythroblast. Nucleoli disappear. Chromatin network becomes dense. These cells develops into next stage called intermediate normoblast.

3. INTERMEDIATE NORMOBLAST: Haemoglobin appears in this stage. Cells have diameter of 1 -0 -12 micrometer. Nucleus is still present. Chromatin network is further condensed. Cytoplasm is basophilic. Due to haemoglobin it stains both acidic and basic. Cells are also called polychromophilic or polychromatic erythroblast. Develop into late normoblast.
4. LATE NORMOBLAST: 8 -10 micrometer diameter. Very small nucleus with condensed chromatin. Ink spot nucleus. Increased haemoglobin. Acidophilic cytoplasm. Orthochromatic erythroblast. Before passing to next stage, nucleus disappears. Pyknosis. Final remnants of nucleus are extruded from the cell.
5. RETICULOCYTE: Immature RBC. Slightly larger than mature RBC. Reticulum. Remnants of disintegrated organelles. Named because of reticular network. In newborns, reticulocyte count is 2% to 6% of RBCs. Number decreases in first week of birth. In mature life, its below 1%. Count increases when production and release of RBCs increases. Basophilic because of remnants of golgi apparatus. , mitochondria and other organelles Enter the blood through capillary membrane by diapedesis.
6. MATURED ERYTHROCYTES: Reticular network disappears. Cell becomes mature RBC. 7. 2 micrometer. Biconcave shape. Haemoglobin but no nucleus. 7 days to convert to mature erythrocyte from proerythroblasts. 5 days to convert to reticulocytes from proerythroblasts. 2 days to convert to mature erythrocytes.
FACTORS NECESSARY FOR ERYTHROPOIESIS: Factors are generally classified into three categories: General factors. Erythropoietin � Thyroxine. � Hemopoietic growth factors. � Vitamins. � Maturation factors Vitamin B 12. � Intrinsic factor of castle. � Folic acid � Factors necessary for haemoglobin formation.
ERYTHROPOIETIN: Hormone for erythropoiesis. Hematopoietin/ erythrocyte stimulating factor. Secreted by peritubular capillaries of kidney. Small quantity also secreted from brain and liver. Hypoxia is the stimulant of erythropoietin. Actions: Proerythroblasts from CFU-E. Proerythropoietin into mature RBCs. Release of matured erythrocytes and some reticulocytes into blood. Level of erythropoietin increases with anemia.
THYROXINE: General metabolic hormone. Accelerates the process of erythropoiesis at many levels. Hyperthyroidism and polycythemia are common.
Hemopoietic growth factor: Growth factors or growth inducers. E. g interleukins and stem cell factors Induce the proliferation of PHSCs. Interleukins involved in erythropoiesis: Interleukin 3 secreted by T cells. Interleukin 6 secreted by T cells, endothelial cells and macrophages. Interleukin 11 secreted by ostoblasts.
VITAMINS: Some vitamins necessary for erythropoiesis. Deficiency will result in anemia along with other disorders. Vitamin B deficiency causes anemia and pellagra. Vitamin C deficiency causes anemia and scurvy. Vitamin D deficiency causes anemia and rickets. Vitamin E deficiency causes anemia and malnutrition.
MATURATION FACTORS: 1: VITAMIN B 12: Maturaion factor necessary for erythropoiesis. Obtained from diet. Its absorption requires intrinsic factor of castle. Also by large intestine flora. Stored in liver and some in muscle. Transported to bone marrow when required for maturation of RBCs. Required for synthesis of DNA in RBCs. Deficiency results in failure of maturation and reduction in cell division. Large cells with weak cell membrane. Pernicious anemia.
2. INTRINSIC FACTOR OF CASTLE: Produced in gastric mucosa from parietal cells. Essential for absorption of vitamin B 12 from intestine. Deficiency of intrinsic factor occurs in � Severe gatritis � Ulcer � Gastrectomy.
3. FOLIC ACID: Required for synthesis of DNA. Maturation factor. Absence causes decrease in DNA synthesis leading to failure of maturation. This makes cells appear larger and in Megaloblastic/ proerythroblastic stage. This anemia is called megaloblastic anemia.
FACTORS NECESSARY FOR HEMOGLOBIN FORMATION: First class proteins and amino acids. Iron. Copper. Cobalt and nickel. Vitamins.
HEMOGLOBI N AND IRON METABOLISM
INTRODUCTION: Iron containing matter of RBCs. Chromoprotein. 95% of dry weight of RBC 30% to 34% net weight. Carries respiratory gases. Acts as buffer. Molecular weight is 68, 000. Average Hb is 14 -16 g/d. L.
FUNCTIONS OF HEMOGLOBIN: 1. TRANSPORT OF GASES: � Oxygen: O 2 binds with hemoglobin. Oxyhemoglobin. Process is called oxygenation. Iron is in ferrous state. Its an unstable compound. Reversible. Release of oxygen from oxyhemoglobin results in ferrohemoglobin or reduced hemoglobin.

� Carbon Dioxide: Binds with hemoglobin to form carbhemoglobin. Unstable and reversible. Affinity of Hb to combine with CO 2 is 20 times more than that for O 2 2. BUFFER ACTION: Important to maintain acid base balance.
STRUCTURE OF HEMOGLOBIN: Conjugated protein. Protein combined with iron containing pigment. Also forms a part of structure of myoglobin and neuroglobin. Iron is present in ferrous form. Fe+2 Abnormally can convert to ferric form which is stable. Fe+3.
Globin: � Contains four polypeptide chains. � 2 alpha chains and 2 beta chains.
TYPES OF NORMAL HEMOGLOBIN: Two types: Adult Hb. A Fetal Hb. F is replaced by Hb. A immediately after birth. Completes at 10 th to 12 th week after birth. Hb. F and Hb. A are different on basis of structure and function.
Structural difference: � Hb. A contains 2 alpha chains and 2 beta chains. � Hb. F contains 2 alpha chains and 2 gama chains. Functional difference: � Hb. F has more affinity to O 2 than adult Hb.
ABNORMAL HEMOGLOBIN: Pathologic mutant forms of Hb. Variations are due to structural changes in the polypeptide chains. Due to mutation is the gene of globin chains. Categories: � Hemoglobinopathies. � Hemoglobin in thalassemia and related disorders

HEMOGLOBINOPATHIES: Caused by abnormal polypeptide chains. Hb-S: Sickel cell anemia. Alpha chains are normal. Beta chains abnormal. Hb-C: Abnormal beta chains. mild hemolytic anemia and splenomegaly.
Hb-E: � Abnormal beta chains. Mild hemolytic anemia and splenomegaly. Hb-M: � Abnormal Hb in form of methemoglobin. � Mutation of genes in both alpha and beta chains. � Present in babies in Hb M disease or blue baby syndrome. � Inherited disease characterised by methemoglobinemia.
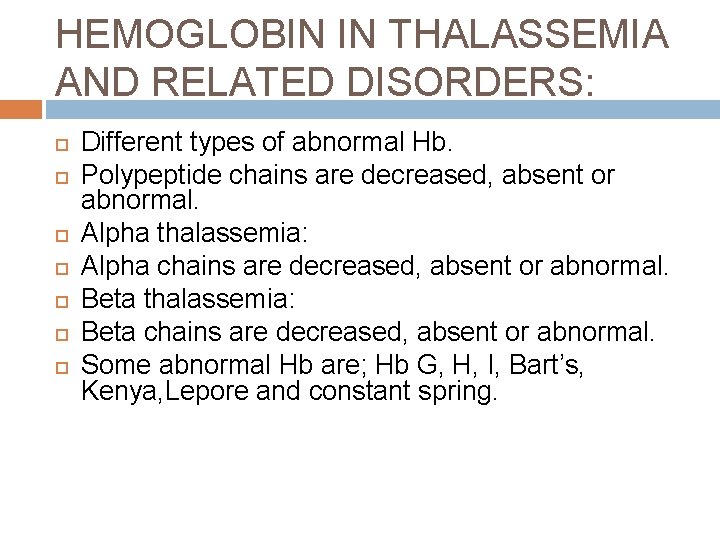
HEMOGLOBIN IN THALASSEMIA AND RELATED DISORDERS: Different types of abnormal Hb. Polypeptide chains are decreased, absent or abnormal. Alpha thalassemia: Alpha chains are decreased, absent or abnormal. Beta thalassemia: Beta chains are decreased, absent or abnormal. Some abnormal Hb are; Hb G, H, I, Bart’s, Kenya, Lepore and constant spring.
 Factors necessary for erythropoiesis
Factors necessary for erythropoiesis Spleen liver gallbladder
Spleen liver gallbladder Organs in the four quadrants
Organs in the four quadrants Wide leaky capillaries found in bone marrow and spleen.
Wide leaky capillaries found in bone marrow and spleen. Vegetative system
Vegetative system Rat diaphragm
Rat diaphragm Nixon method spleen percussion
Nixon method spleen percussion Spleen solid organ
Spleen solid organ Splenic injury grade
Splenic injury grade Porta hepatis
Porta hepatis What is bile for
What is bile for Images of spleen
Images of spleen What is the latin meaning of the phylum and class
What is the latin meaning of the phylum and class Frog
Frog Frog spleen
Frog spleen Dogfish classification
Dogfish classification Just palpable spleen
Just palpable spleen White pulp
White pulp Spleen congestion
Spleen congestion Ascites examination
Ascites examination Applied anatomy of spleen
Applied anatomy of spleen Paul verlaine spleen
Paul verlaine spleen Apikomplex
Apikomplex Spleen not palpable
Spleen not palpable Spleen histology slide labeled
Spleen histology slide labeled Dr dahla
Dr dahla Liver span
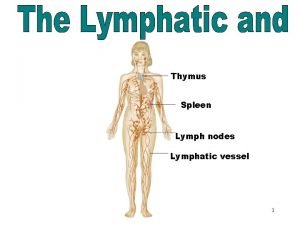
Liver span Lymphatic system
Lymphatic system Lig phrenicocolic
Lig phrenicocolic Spleen
Spleen Spleen cat dissection
Spleen cat dissection Pen test for abductor pollicis brevis
Pen test for abductor pollicis brevis Traube space
Traube space Picture of stomach organs
Picture of stomach organs Spleen
Spleen Septic spleen
Septic spleen Spleen histology
Spleen histology