TWIN LAKES Lymph nodes in conjunction with the



- Slides: 55
TWIN LAKES,

Lymph nodes, in conjunction with the spleen, tonsils, adenoids, and Peyer patches, are highly organized centers of immune cells that filter antigen from the extracellular fluid Lymph node size depends on the person's age, the location of the lymph node in the body, and antecedent immunological events
Lymphadenopathy reflects disease involving the RES nodal accumulation of inflammatory cells in response to an infection in the node (lymphadenitis) Localized lymphadenitis is most often caused by staphylococci and beta-hemolytic streptococci.
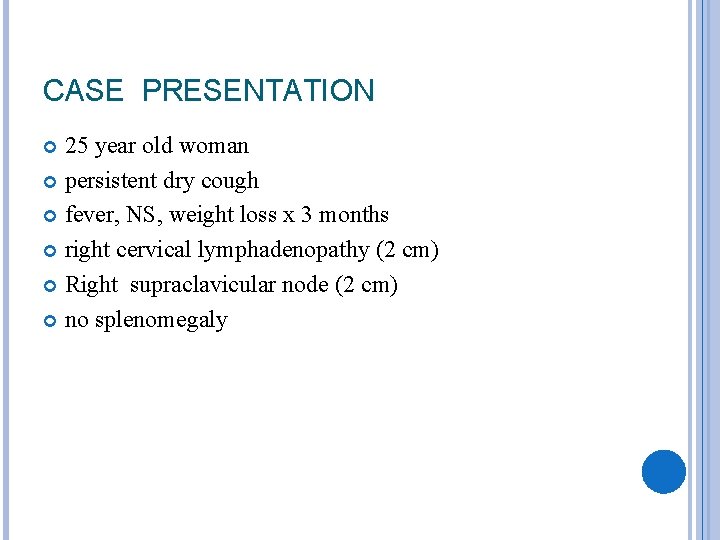
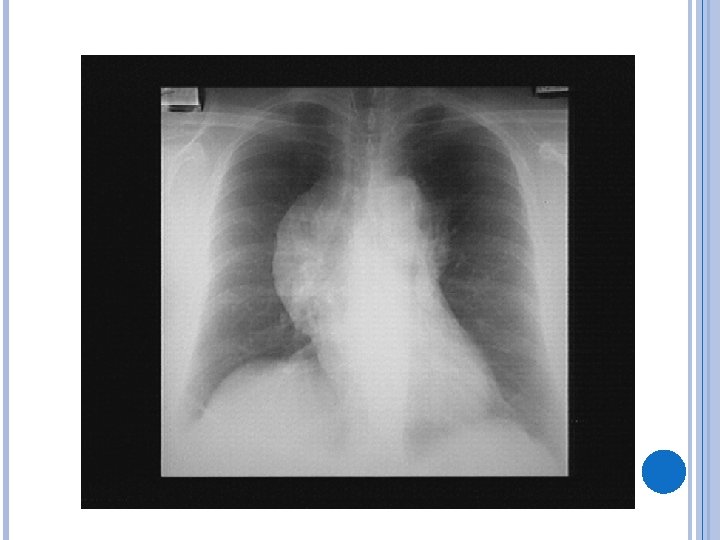
CASE PRESENTATION 25 year old woman persistent dry cough fever, NS, weight loss x 3 months right cervical lymphadenopathy (2 cm) Right supraclavicular node (2 cm) no splenomegaly
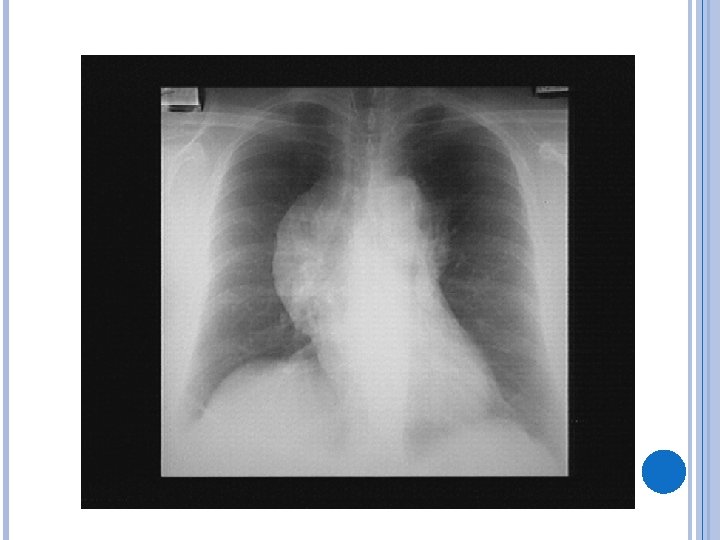
DIFFERENTIAL DIAGNOSIS lymphoma Hodgkin non-Hodgkin lung cancer(bronchogenic carcinoma, metastase) other neoplasms: thyroid, mediastinal non-neoplastic causes less likely sarcoid, TB, fungal( histoplasmosis), . . Inorganic dust disease(Silicosis)
WHAT NEXT? Needle aspirate of LN: a few necrotic cells Needle biopsy of LN: admixture of B- and Tlymphocytes. A few atypical cells.
WHAT IS HER DIAGNOSIS ? nodular sclerosis HD with bulky mediastinal mass
LYMPHADENOPATHY Medical hx should reveal the setting in which lymphadenopathy is occuring Sorethroat , cough, fever, night sweat, wt loss, pain in nodes Patient`s age , sex, occupation, exposure to pet, sexual behaviour, and use of drugs such as diphenylhydantoin
Physical exam: 1 - extent of LAP( localized or generalized) 2 -size of nodes , texture, tenderness, inflammation on it, skin lesion and splenomegaly ENT exam in cervical LAP and hx of tobacco use
Site of adenopathy: Occipital( infection of scalp) Preauricular ( conjunctival infection and cat scratch disease) Neck( usually benign such as URTI , oral and dental lesion , IM, or other viral) supraclavicular nodes due to lymphomas, other cancers and infectious processes arising in lung and retroperitoneal space( and from testis, ovaries) Virchow`s node in left supraclavicular infiltrated with metastatic cancer from GI Nonspecific causes of supraclavicular nodes : TB, sarcoidosis and toxoplasmosis
Axillary adenopathy due to injuries or infections of upper extremity but malignant causes are lymphoma or melanoma and breast cancer Inguinal adenopathy usually due to trauma or infection of the lower extremities and may due to STDs ( also may be due to lymphoma and metastatic cancers)
Size: < 1 cm by 1 cm almost always benign and reactive Retrospective analysis results: *> 2 cm predict for need to Bx * > 1. 5 by 1. 5 cm was the best size limit for distinguish malignant or granulomatous LAP from other causes
Texture: Soft, firm, rubbery, hard, discrete, matted, tender, movable or fixed. Tenderness in inflammatory diseases due to rapid stretch of capsule Also some malignancies ( acute leukemia) may produce rapid enlargement and pain in node In lymphoma : large, discrete, symmetric, rubbery, firm, mobile and nontender In metastatic cancers: hard, nontender, nonmovable
Coexistence with splenomegaly in the patient with LAP implies a systemic illness IM, lymphoma , ALL and CLL, SLE, sarcoidosis, toxoplasmosis, cat-scratch dis.
Nonsuperficial presentation(thoracic or abdominal) : Thoracic may be detected by routine CXR or during the w/o for superficial adenopathy Also may be found because of symptoms such as cough, wheeze , hoarseness , dysphagia and swelling of face, neck and arms DDX for mediastinal and hilar adenopathy: *in youngers : IM , sarcoidosis *in endemic : histoplasmosis , TB *in olders: primary lung cancers, lymphoma, metastatic cancers, TB, fungal, sarcoidosis
Intraabdominal or retroperitoneal nodes are usually malignant
LABORATORY INVESTIGATION CBC ( for leukemia, EBV or CMV mononucleosis, lymphoma with a leukemic component, immune cytopenia in dis. such as lupus and pyogenic infections) Serology ( for EBV, CMV, HIV, and other viruses, Toxoplasmosis, Brucella) ANA and ds-DNA ( for lupus) CXR Other imagings for differentiate benign from malignancy
Biopsy: In a hx and physical exam compatible with malignancy In primary care centers < 5% of LAPs will require Bx If the patient`s hx and ph. exam point to a benign cause , careful follow up at 2 -4 week interval can be used The patient should be instructed to return for reevluate if increase in size Antibiotic not indicated unless strong evidence for bacterial infection
Glucocorticoid should not be used because their lympholytic effect obscures some diagnoses( lymphoma, leukemia) and they contribute to delayed healing or activation of underlying infection –( an exception is the life-threatening pharyngeal obstruction by enlarged lymphoid tissue in weldeyer`s ring thas is occasionally seen in IM)

SPLENOMEGALY By : Minoosh Sha`bani MD
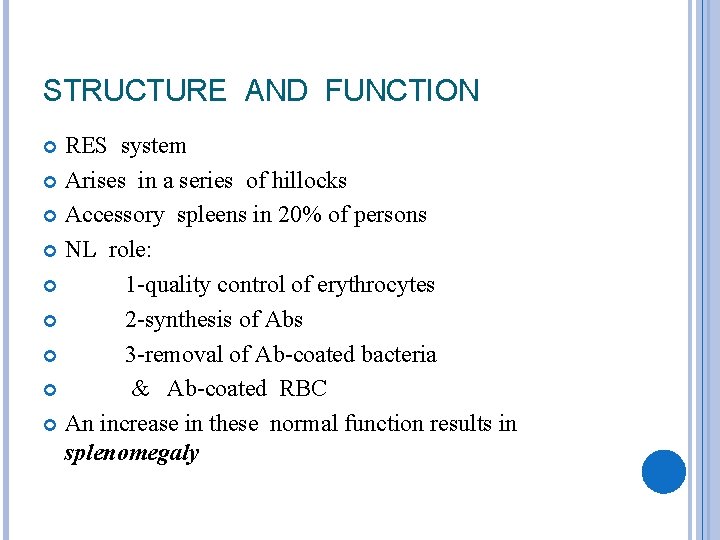
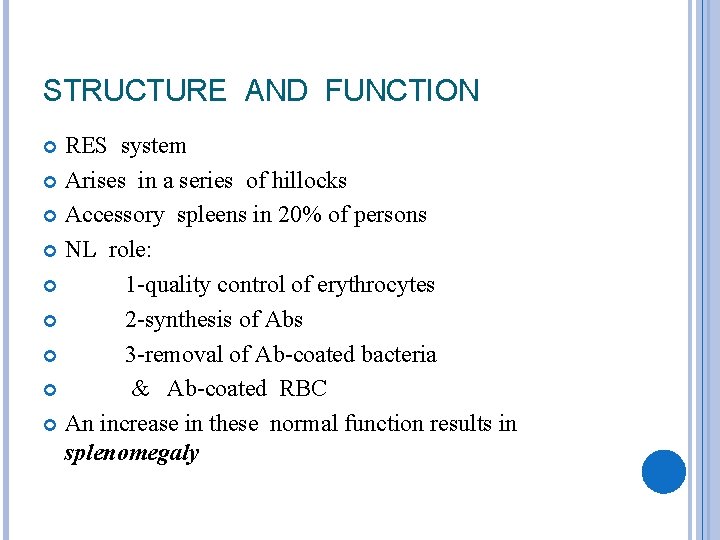
STRUCTURE AND FUNCTION RES system Arises in a series of hillocks Accessory spleens in 20% of persons NL role: 1 -quality control of erythrocytes 2 -synthesis of Abs 3 -removal of Ab-coated bacteria & Ab-coated RBC An increase in these normal function results in splenomegaly
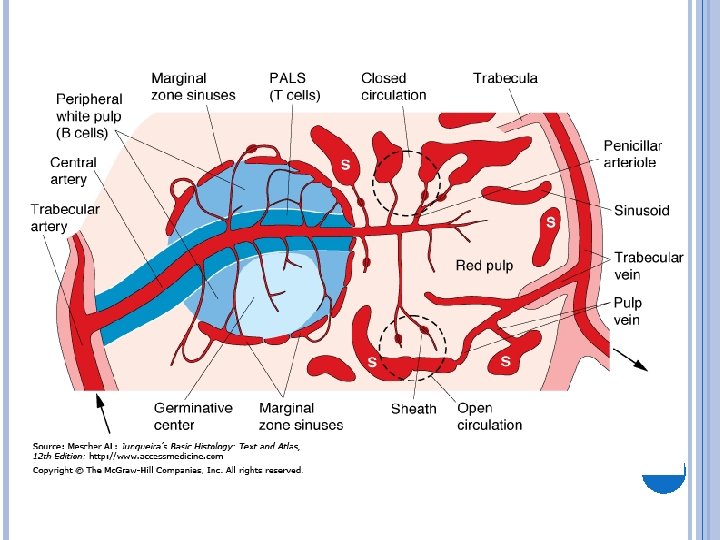
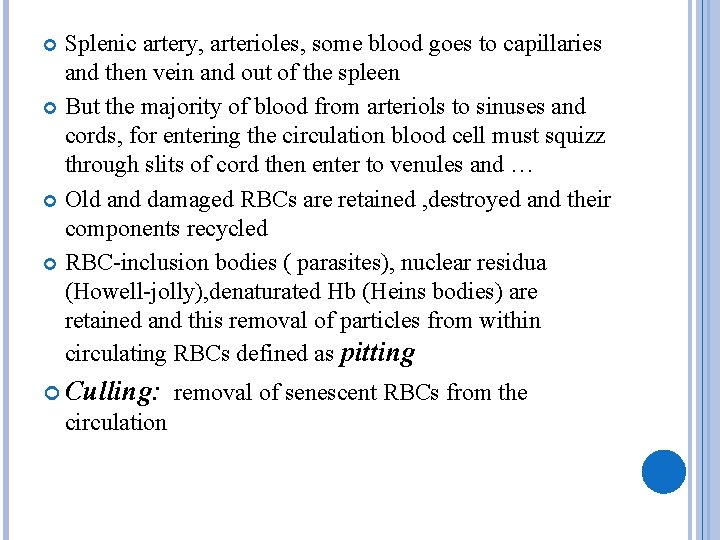
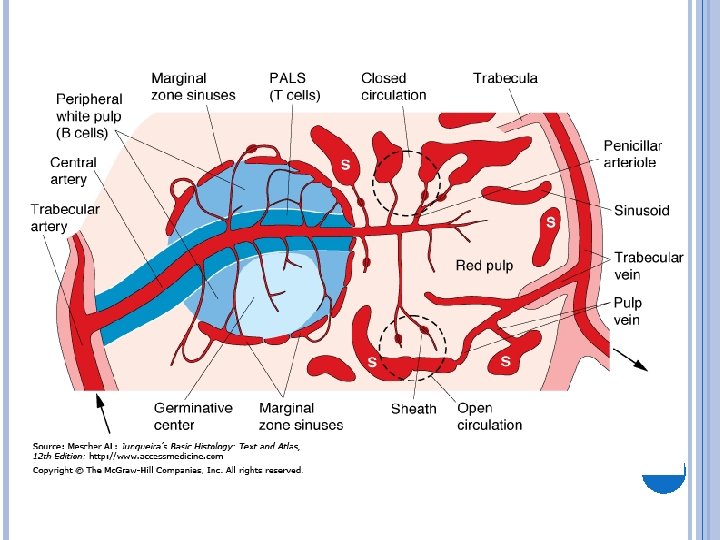
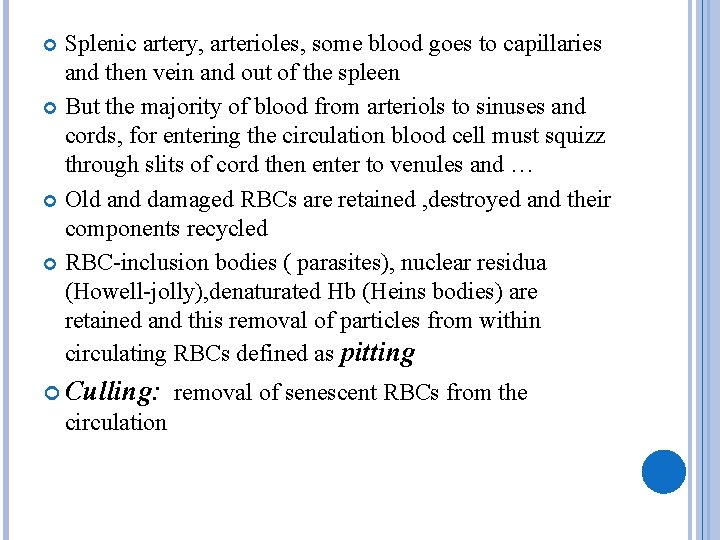
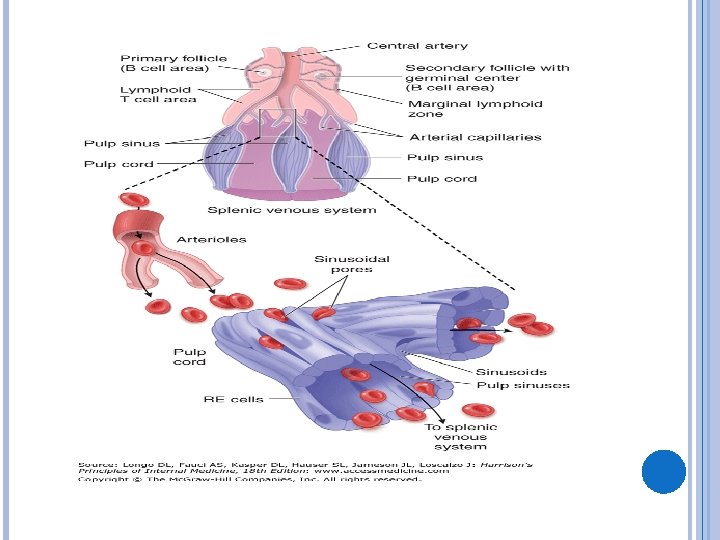
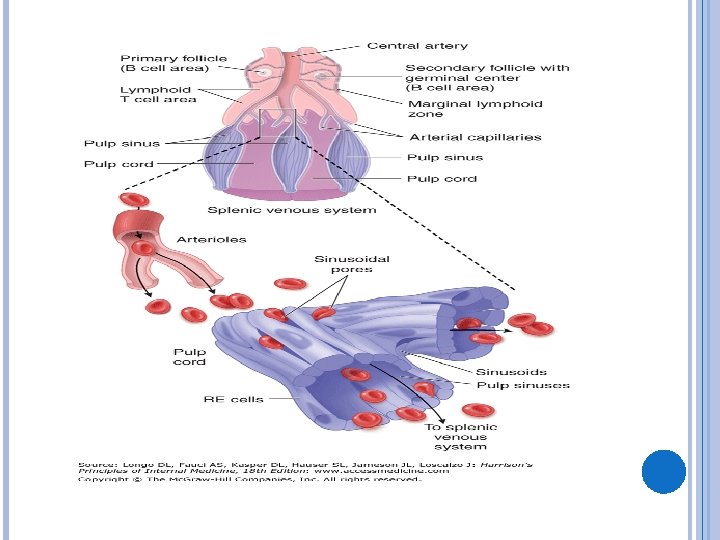
Splenic artery, arterioles, some blood goes to capillaries and then vein and out of the spleen But the majority of blood from arteriols to sinuses and cords, for entering the circulation blood cell must squizz through slits of cord then enter to venules and … Old and damaged RBCs are retained , destroyed and their components recycled RBC-inclusion bodies ( parasites), nuclear residua (Howell-jolly), denaturated Hb (Heins bodies) are retained and this removal of particles from within circulating RBCs defined as pitting Culling: removal of senescent RBCs from the circulation
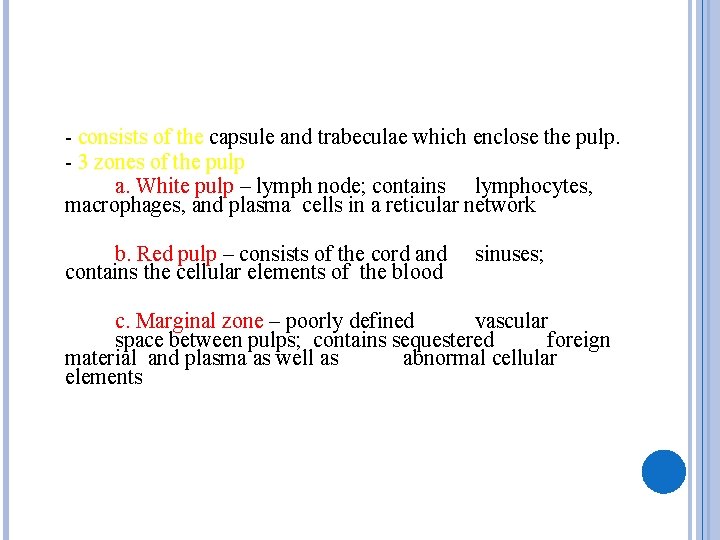
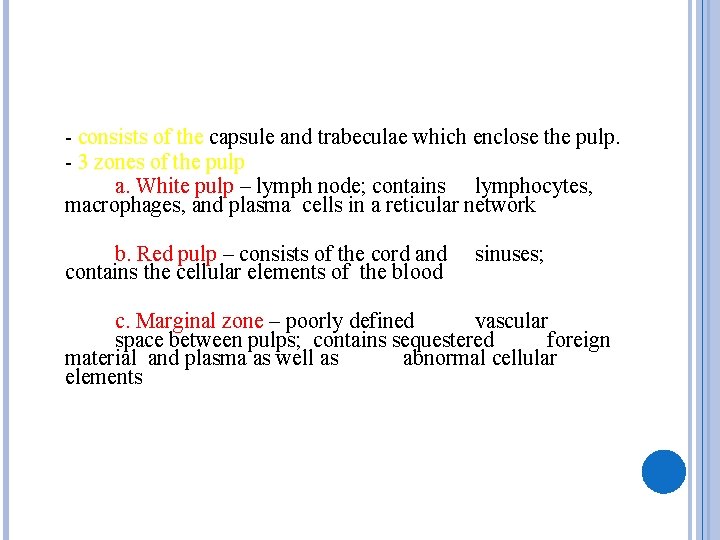
- consists of the capsule and trabeculae which enclose the pulp. - 3 zones of the pulp a. White pulp – lymph node; contains lymphocytes, macrophages, and plasma cells in a reticular network b. Red pulp – consists of the cord and contains the cellular elements of the blood sinuses; c. Marginal zone – poorly defined vascular space between pulps; contains sequestered foreign material and plasma as well as abnormal cellular elements
Exrtacellular hematopoesis in myelofibrosis, marrow damage by toxin or radiation and marrow infiltration by tumors The normal spleen contains 1/3 of total plts and a significant number of merginated neutrophils
The spleen is the major organ of RES. Blood cells leave the splenic arterial bed through afferent arterioles , which pass through lymphoid nodules(white pulp) and then terminates in the cords of Billroth(red pulp) into which the blood cells are discharged The normal slow flow permits selective action on the blood cells by macrophages
APPROACH TO SPLENOMEGALY Clinical: (pain- heavy sense) Rupture of spleen ( trauma , infiltrative ) Intraperitoneal bleeding, shock and death -Weight < 250 gr- with age- cephalocaudal diameter : 13 cm- -Usually not palpable -A palapble spleen does not always equate with the presence of disease
PHYSICAL EXAM Palapation : Middleton maneuver: (start from LLQ) Percussion : Castel : ant. axillary line Traube: mid. axillary line( 6 th rib and A tympanitic area overlying gastric stomach bubble in semilunar space that will be displaced downward following splenomegaly and . . Nixon : post. axillary line( on a line vertical to. . . ) We recommend percuss at first if positive. . . Reproducibillity with palpation is better Spleen lies adjacent to the 9 th to the 11 th ribs, stomach, colon and left kidney
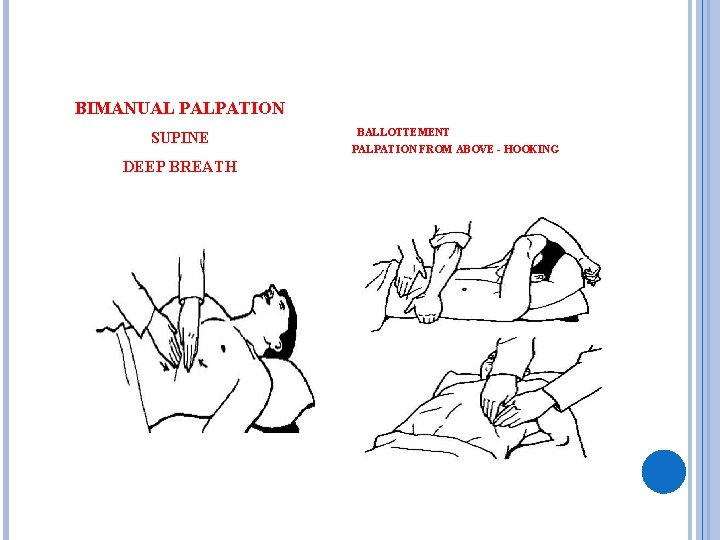
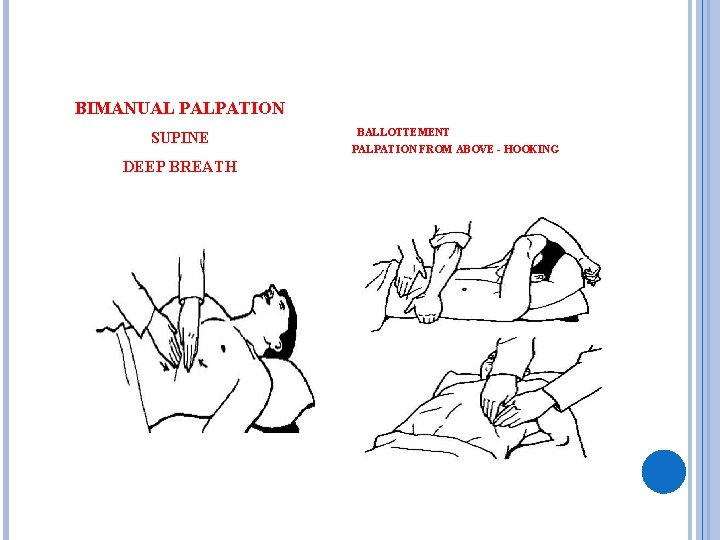
BIMANUAL PALPATION SUPINE DEEP BREATH BALLOTTEMENT PALPATION FROM ABOVE - HOOKING
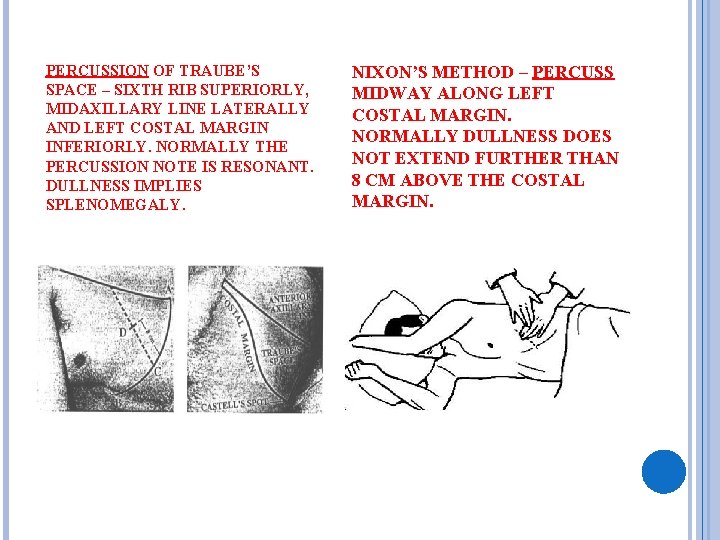
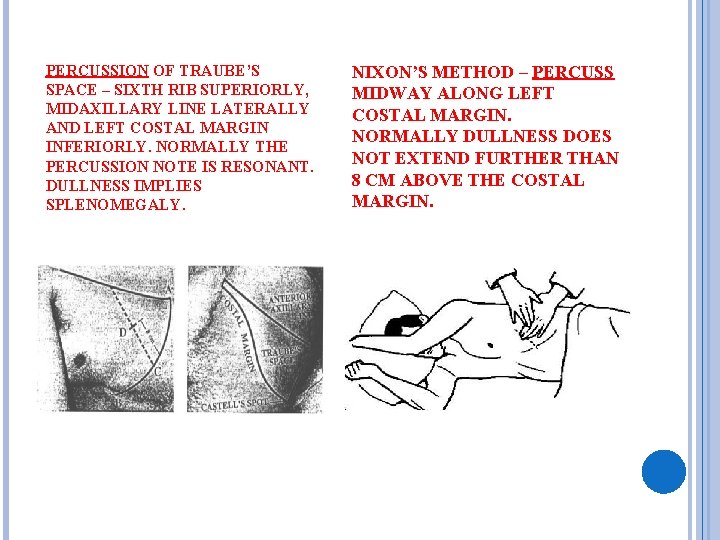
PERCUSSION OF TRAUBE’S SPACE – SIXTH RIB SUPERIORLY, MIDAXILLARY LINE LATERALLY AND LEFT COSTAL MARGIN INFERIORLY. NORMALLY THE PERCUSSION NOTE IS RESONANT. DULLNESS IMPLIES SPLENOMEGALY. NIXON’S METHOD – PERCUSS MIDWAY ALONG LEFT COSTAL MARGIN. NORMALLY DULLNESS DOES NOT EXTEND FURTHER THAN 8 CM ABOVE THE COSTAL MARGIN.
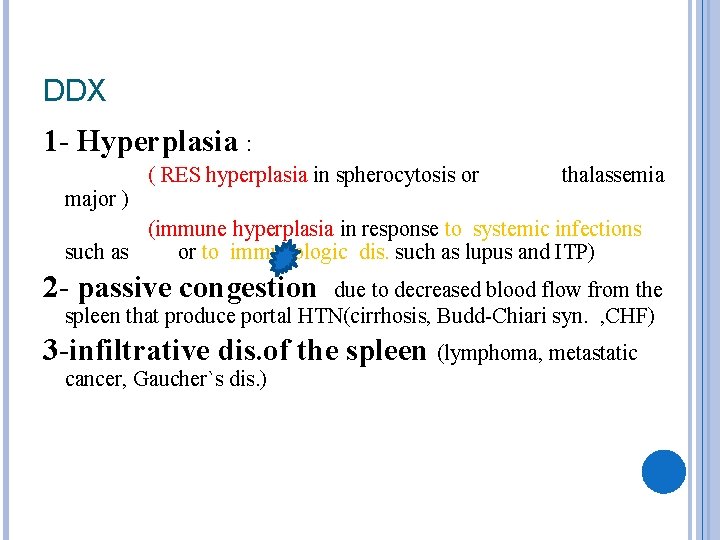
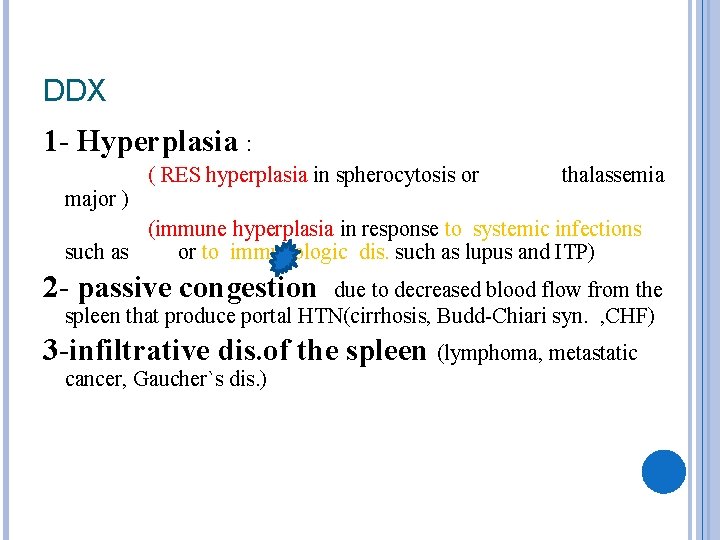
DDX 1 - Hyperplasia : ( RES hyperplasia in spherocytosis or thalassemia major ) (immune hyperplasia in response to systemic infections such as or to immunologic dis. such as lupus and ITP) 2 - passive congestion due to decreased blood flow from the spleen that produce portal HTN(cirrhosis, Budd-Chiari syn. , CHF) 3 -infiltrative dis. of the spleen (lymphoma, metastatic cancer, Gaucher`s dis. )
-IM -AIDS -viral hepatitis -CMV -SBE -Bacterial septicemia -TB -Histoplasmosis -Malaria -Leishmaniasis -Congenital syphilis -Splenic abscess
The presence of splenomegaly, posterior cervical adenopathy, axillary adenopathy, and inguinal adenopathy is most useful in considering the possibility of infectious mononucleosis, while the absence of cervical adenopathy and fatigue is most helpful in dismissing the diagnosis. . Because the physical examination is quite insensitive for detecting splenomegaly (between 27 and 58 percent, depending on the examiner’s index of suspicion), the absence of splenomegaly should not be used as evidence against the diagnosis of infectious mononucleosis.
The original serologic test for infectious mononucleosis, the Paul-Bunnell test, detected heterophile antibodies by agglutination of sheep or horse red blood cells. Although they are relatively specific, heterophile antibody tests are somewhat insensitive, particularly in the first weeks of illness VCA-Ig. G and VCA-Ig. M tests are useful in diagnosing patients who have highly suggestive clinical features but negative heterophile antibody test results
Because an enlarged spleen is at risk for rupture, athletes should not compete in contact sports for a minimum of four weeks after the onset of symptoms. The risk of splenic rupture is estimated at 0. 1 percent
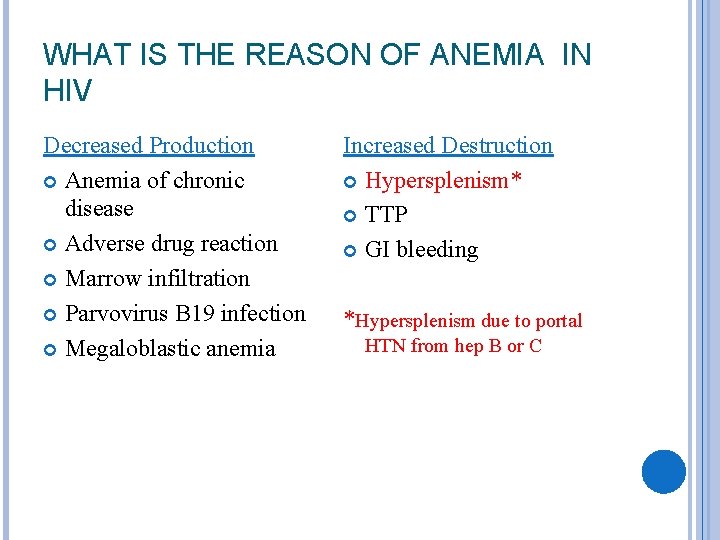
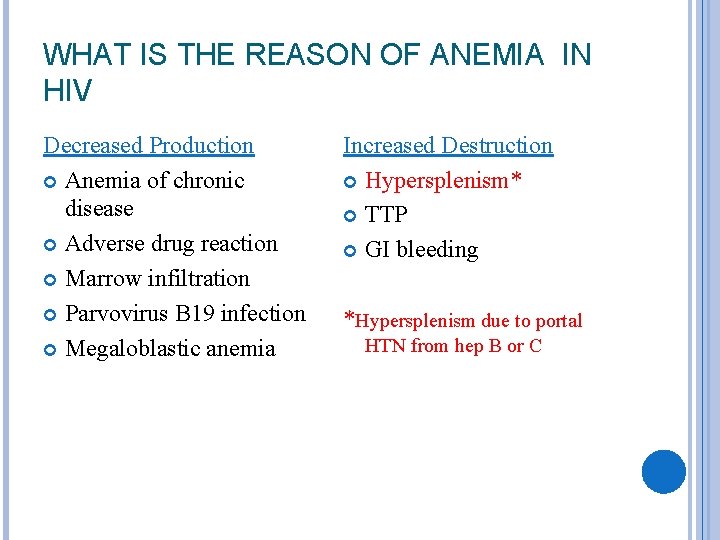
WHAT IS THE REASON OF ANEMIA IN HIV Decreased Production Anemia of chronic disease Adverse drug reaction Marrow infiltration Parvovirus B 19 infection Megaloblastic anemia Increased Destruction Hypersplenism* TTP GI bleeding *Hypersplenism due to portal HTN from hep B or C

CMV In most cases, primary CMV infection is asymptomatic or produces mild flulike symptoms. The lymph nodes and spleen may be enlarged Some studies have shown that, as a group, patients infected with CMV have less hepatomegaly, splenomegaly, and pharyngitis than those infected with EBV. Patients with CMV mononucleosis may be older, have a longer duration of fever, and have less cervical lymphadenopathy
SBE Splenic infarction may occur as a result of emboli. In this case, splenic palpation may be painful and tender, and a rub may be heard.
SPLENIC ABSCESS A rare entity( 0. 05 -0. 7%) Etiology: - The most common is hematogenous spread *Infective endocarditis, a condition associated with systemic embolization in 22 -50% of cases, has a 10 -20% incidence of associated splenic abscess. -Other infective sources include typhoid, paratyphoid, malaria, urinary tract infection, pneumonias, osteomyelitis, otitis, mastoiditis, and pelvic infections Contiguous spread - This includes direct involvement from a pancreatic abscess, gastric or colonic perforations, or subphrenic abscesses. -Splenic trauma -Splenic infarction resulting from systemic disorders (see the image below), such as hemoglobinopathies (especially sickle cell disease), leukemia, polycythemia, or vasculitis, can become infected and evolve into splenic abscesses
Microbiology Aerobes (in most published cases)Gram-positive cocci Streptococcus, Staphylococcus, Enterococcus(predominant in most reports) Gram-negative bacilli -Escherichia coli, Klebsiella pneumoniae, Proteus, Pseudomonas species, Salmonella species (occasionally predominant) Anaerobes -Peptostreptococcus, Bacteroides, Fusobacterium, Clostridium, Propionibacterium acnes Polymicrobial (up to 50% of cases) Fungal -Candida
History Fever (>90%) can be moderate, continuous, intermittent, or even absent. Abdominal pain (>60%) typically occurs suddenly Involvement of the diaphragmatic pleura can cause shoulder pain Physical examination Abdominal tenderness (>50%) Splenomegaly (< 50%) is less frequently observed, probably because of early diagnosis resulting from the widespread use of imaging methods.
Medical Therapy : -Early supportive care and parenteral broad-spectrum antibiotics Surgical Therapy : -Splenectomy has long been considered the standard treatment of splenic abscess
SPLENECTOMY Absolute Indications for Splenectomy 1. splenic tumors – echinoccocal cyst 2. metastatic disease 3. splenic abscess 4. hereditary spherocytosis – most common hemolytic anemia for which splenectomy is indicated 5. bleeding esophageal varices
6. chronic lymphocytic leukemia 7. hairy cell leukemia 8. Chronic myeloid leukemia – more to the pain 9. Sarcomas 10. trauma ease
Splenectomy Outcomes - post-operative appearance of: a. siderocytes b. Howell-Jolly bodies c. leukocytosis d. increased platelete count
Complications 1. left lower lobe atelectasis – most common 2. subphrenic hematoma 3. subphrenic abscess – can occur with placement of a drain 4. pancreatitis – trauma to the tail of the pancreas 5. deep vein thrombosis – low dose
Massive splenomegaly in : -CML( chronic myeloid leukemia) -Lymphomas (esp. NHL) -HCL -PCV -Gaucher`s dis. -CLL( chronic lymphocytic leukemia) -Sarcoidosis -Autoimmune hemolytic anemia
Hematologic outcomes: -leukocytosis and thrombocytosis But After 2 -3 wks this profile will be normal
Overwhelming Post-Splenectomy Infection (OPSI) 1. lifetime risk of severe infection( the lowest risk is for trauma and ITP) and overall 6% of total OPSI 2. incidence of 3. 2% post-splenectomy 3. loss of the spleen’s ability to filter and phagocytose bacteria and infected RBC
most common sources of infection a. Streptococcus pneumoniae – most common b. Heamophilus influenzae B c. meninggococcus prevention a. vaccine against i. pneumoccocus ii. H. influenzae iii. meninggococcus - to be given 14 days before elective splenectomy
THANK YOU ANY QUESTION?