Management of Traumatic Solid Organ Injury Liver Spleen






- Slides: 27
Management of Traumatic Solid Organ Injury: Liver, Spleen, and Pancreas Catherine Martin Frederick, ACNP, CCRN September 14, 2015
Trauma Care – Initial Assessment and Resuscitation • • • Airway with cervical spine precautions Breathing Circulation Disability Exposure
Abdominal Assessment • Vital Signs and Physical Exam • Investigational Studies – FAST – DPL – CT Abdomen/Pelvis

Diagnostic Peritoneal Lavage • First described in 1965 • Rapid • Accurate, predictive value greater than 90% • Able to detect minimal blood • High sensitivity, low specificity • Useful in unstable patient, gross blood predictive in intra-abdominal hemorrhage

CT Scan • Gold standard • Not for use in hemodynamically unstable patient • Must be done with IV contrast to be sensitive for solid organ injury • Determines source and amount of bleeding • Reveals associated injuries: pancreas, genitourinary, orthopedic • Poor for hollow viscous injury
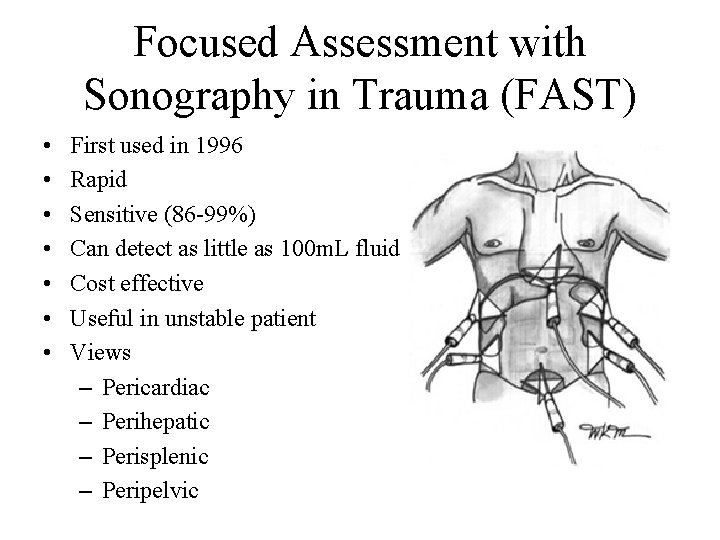
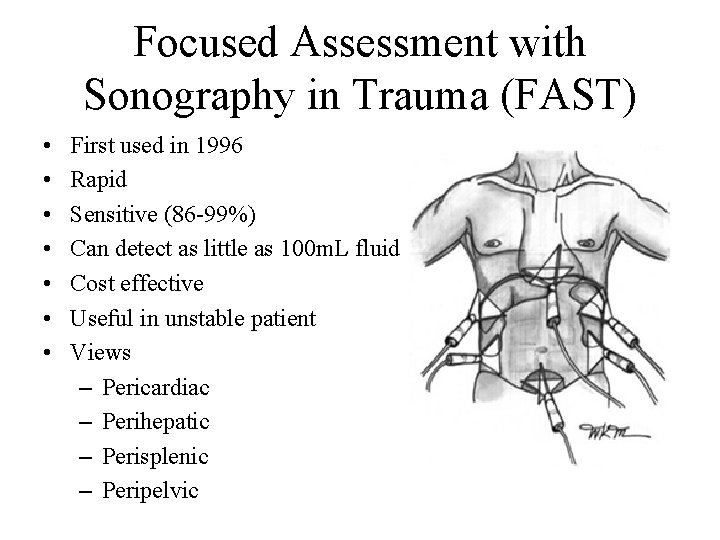
Focused Assessment with Sonography in Trauma (FAST) • • First used in 1996 Rapid Sensitive (86 -99%) Can detect as little as 100 m. L fluid Cost effective Useful in unstable patient Views – Pericardiac – Perihepatic – Perisplenic – Peripelvic

Liver
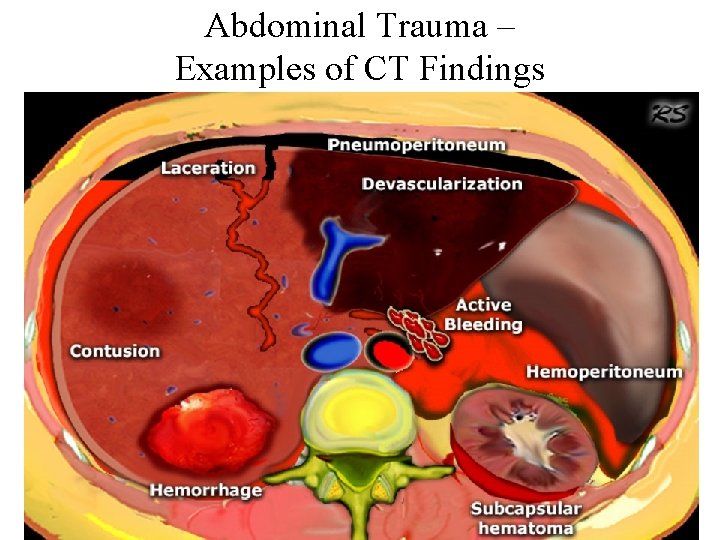
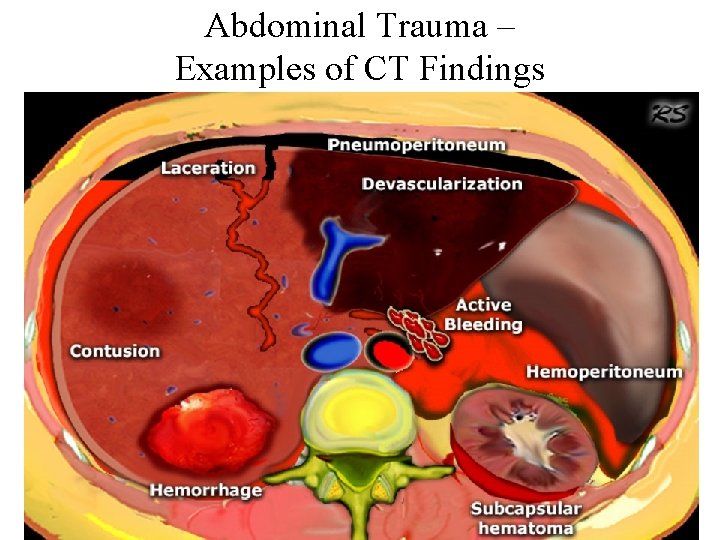
Abdominal Trauma – Examples of CT Findings
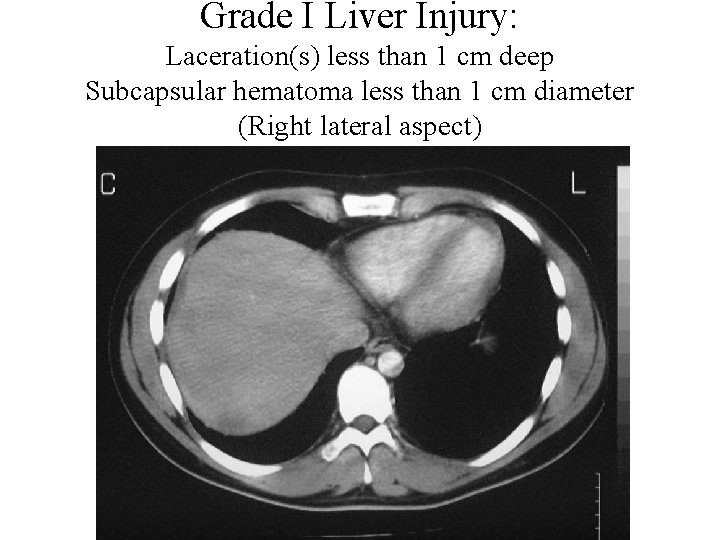
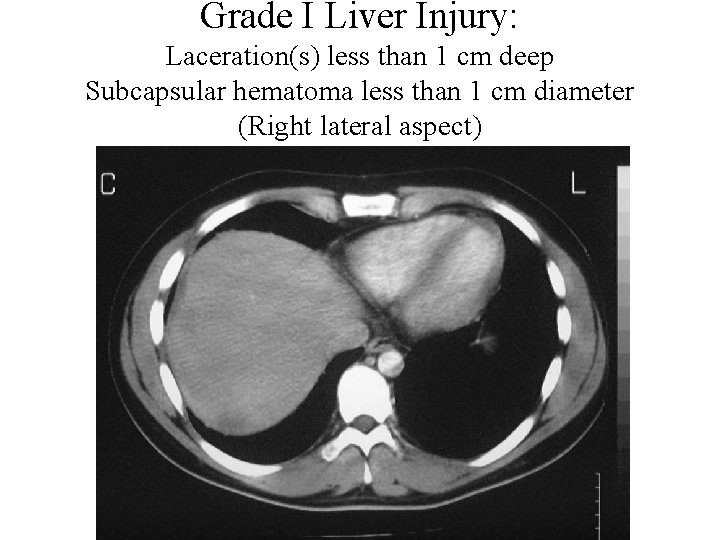
Grade I Liver Injury: Laceration(s) less than 1 cm deep Subcapsular hematoma less than 1 cm diameter (Right lateral aspect)
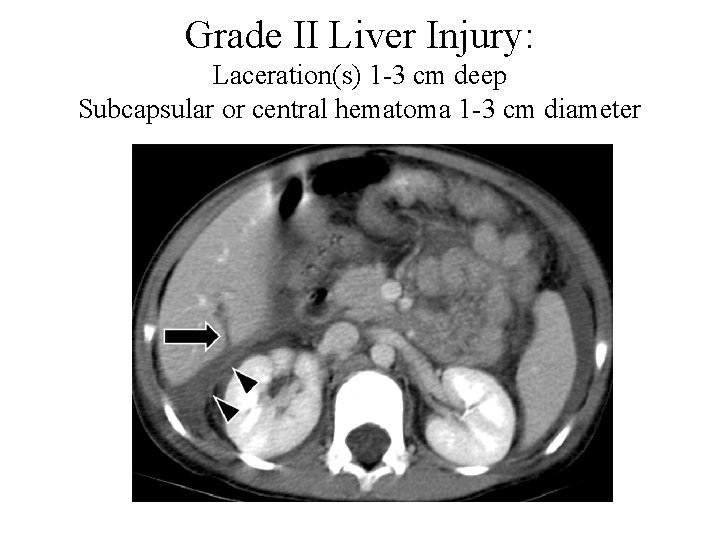
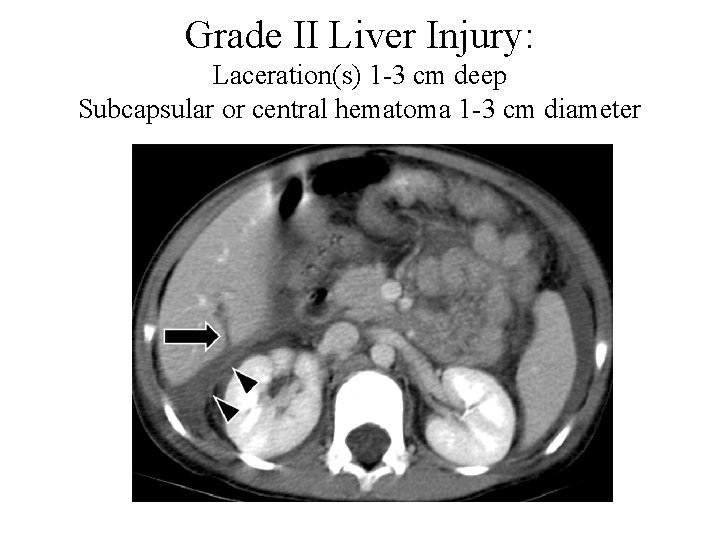
Grade II Liver Injury: Laceration(s) 1 -3 cm deep Subcapsular or central hematoma 1 -3 cm diameter
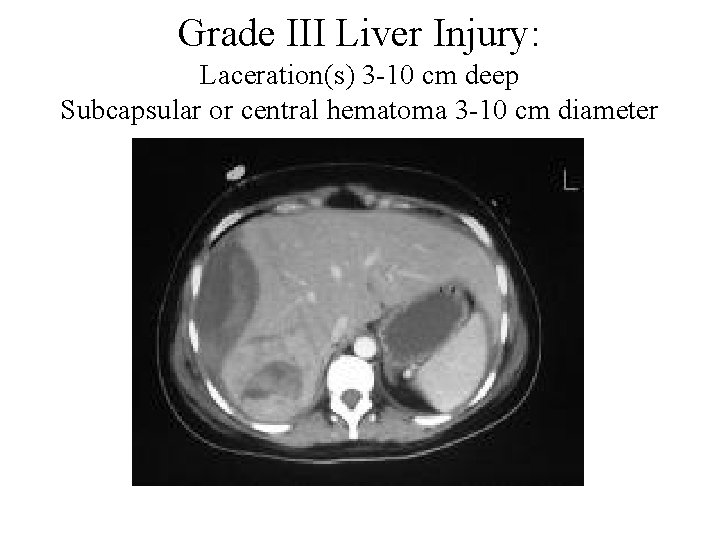
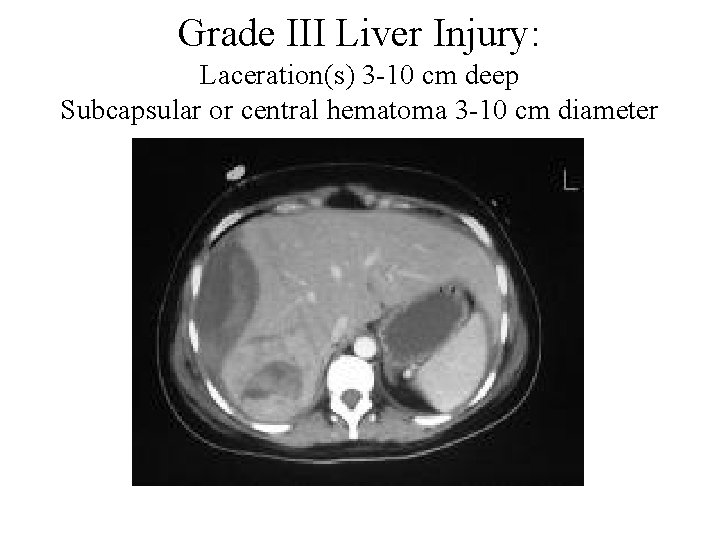
Grade III Liver Injury: Laceration(s) 3 -10 cm deep Subcapsular or central hematoma 3 -10 cm diameter

Grade IV Liver Injury: Laceration(s) greater than 10 cm deep Subcapsular or central hematoma greater than 10 cm diameter Lobar maceration or devascularization
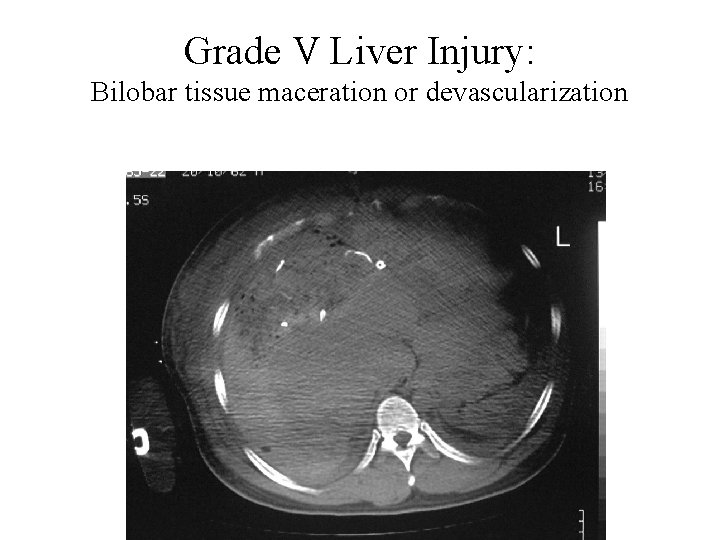
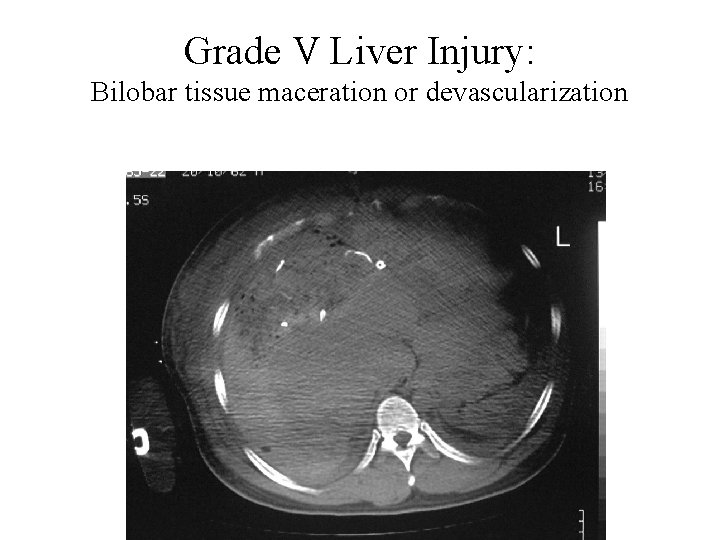
Grade V Liver Injury: Bilobar tissue maceration or devascularization
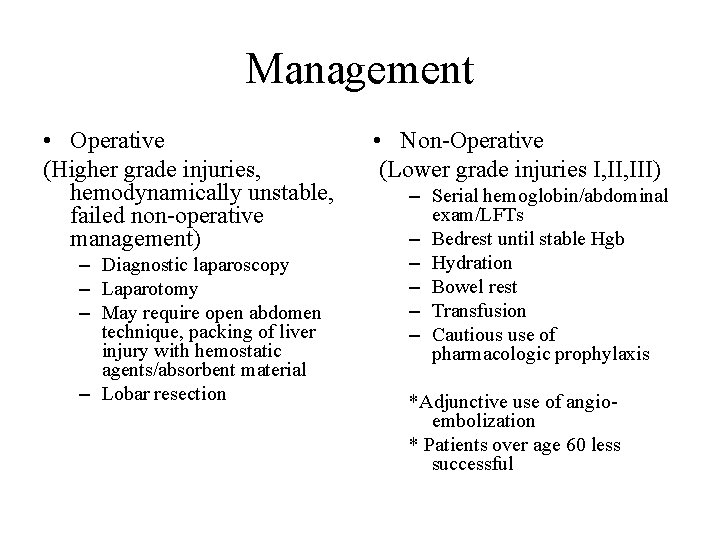
Management • Operative (Higher grade injuries, hemodynamically unstable, failed non-operative management) – Diagnostic laparoscopy – Laparotomy – May require open abdomen technique, packing of liver injury with hemostatic agents/absorbent material – Lobar resection • Non-Operative (Lower grade injuries I, III) – Serial hemoglobin/abdominal exam/LFTs – Bedrest until stable Hgb – Hydration – Bowel rest – Transfusion – Cautious use of pharmacologic prophylaxis *Adjunctive use of angioembolization * Patients over age 60 less successful
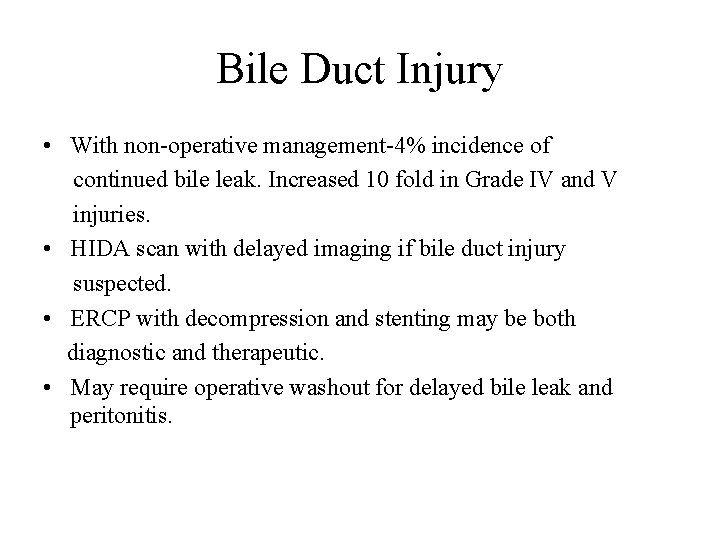
Bile Duct Injury • With non-operative management-4% incidence of continued bile leak. Increased 10 fold in Grade IV and V injuries. • HIDA scan with delayed imaging if bile duct injury suspected. • ERCP with decompression and stenting may be both diagnostic and therapeutic. • May require operative washout for delayed bile leak and peritonitis.
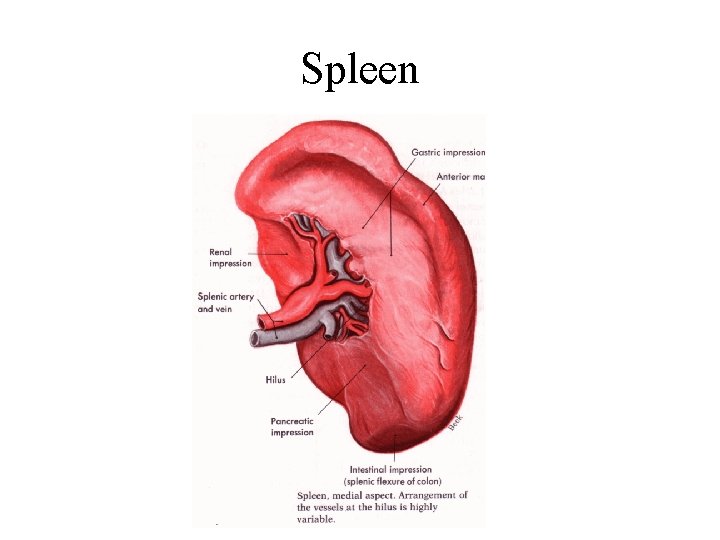
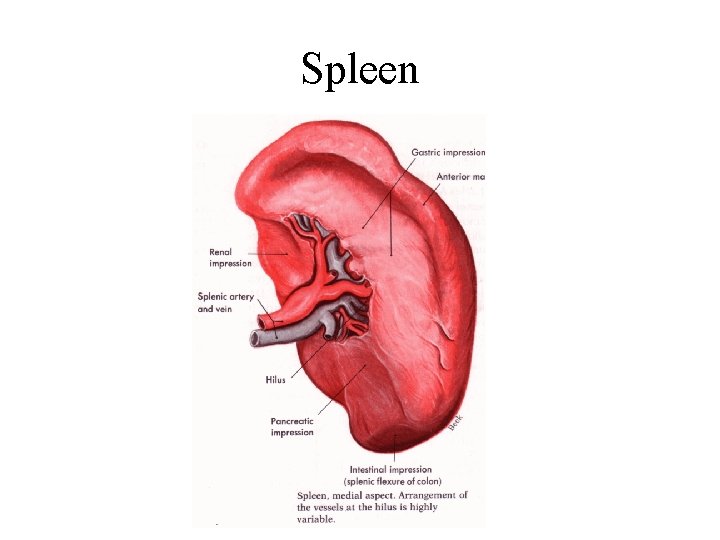
Spleen
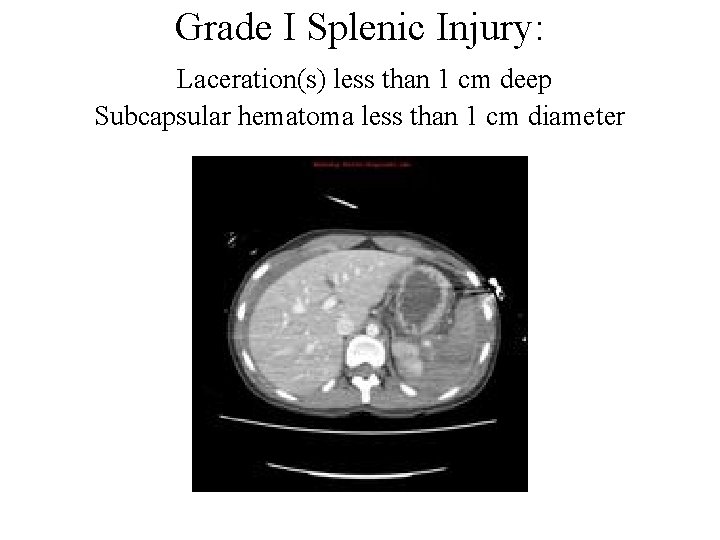
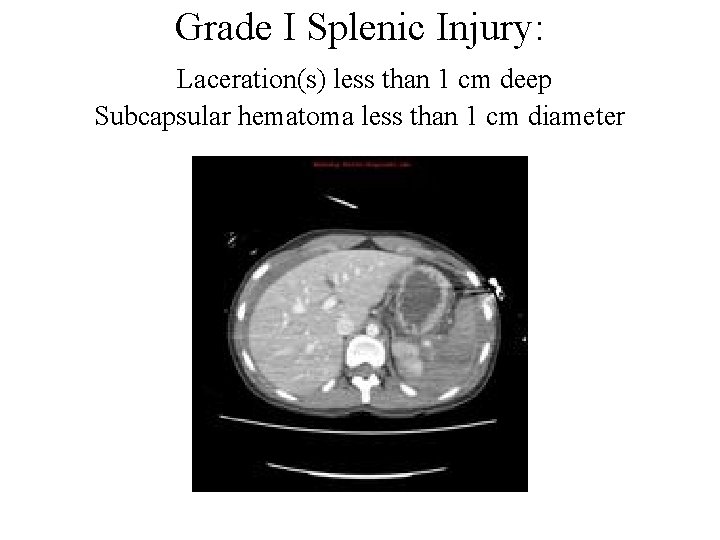
Grade I Splenic Injury: Laceration(s) less than 1 cm deep Subcapsular hematoma less than 1 cm diameter
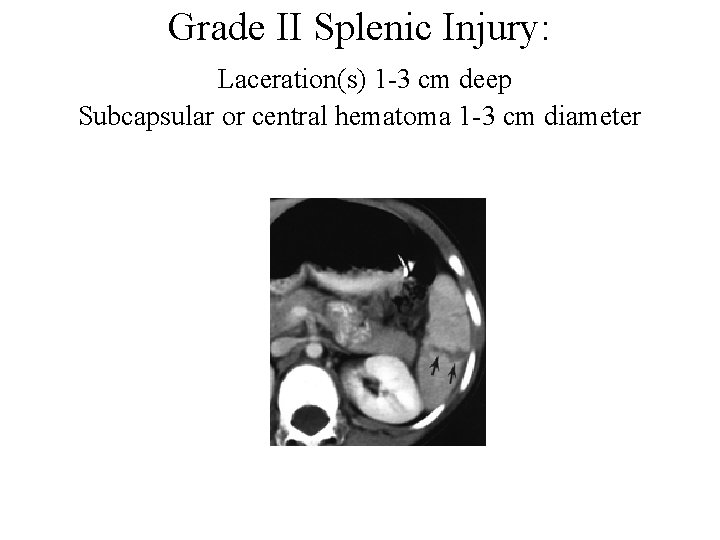
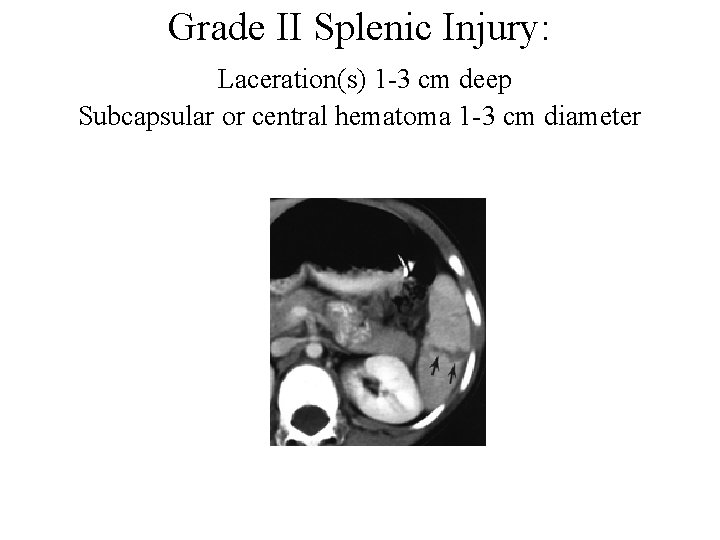
Grade II Splenic Injury: Laceration(s) 1 -3 cm deep Subcapsular or central hematoma 1 -3 cm diameter
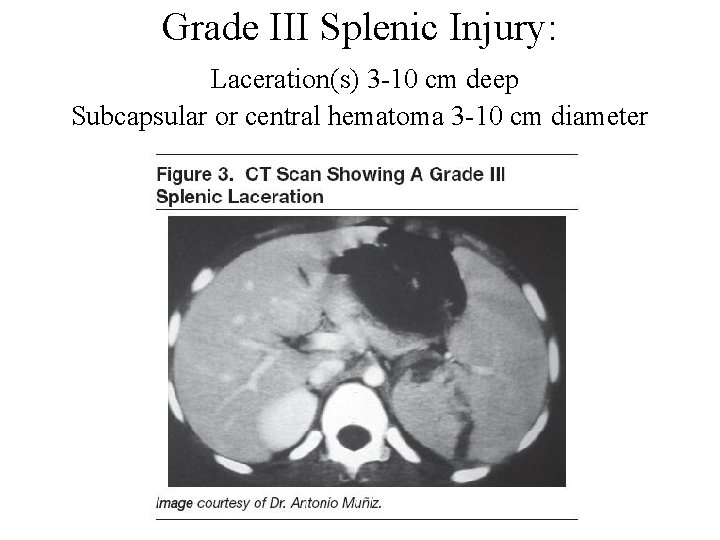
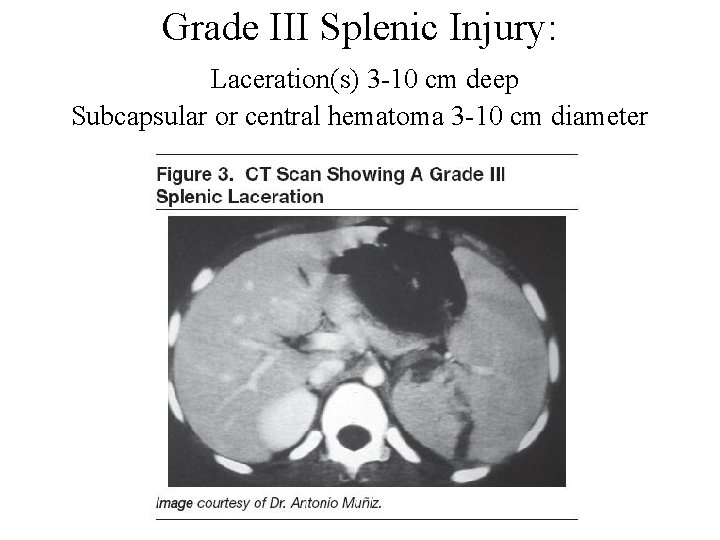
Grade III Splenic Injury: Laceration(s) 3 -10 cm deep Subcapsular or central hematoma 3 -10 cm diameter
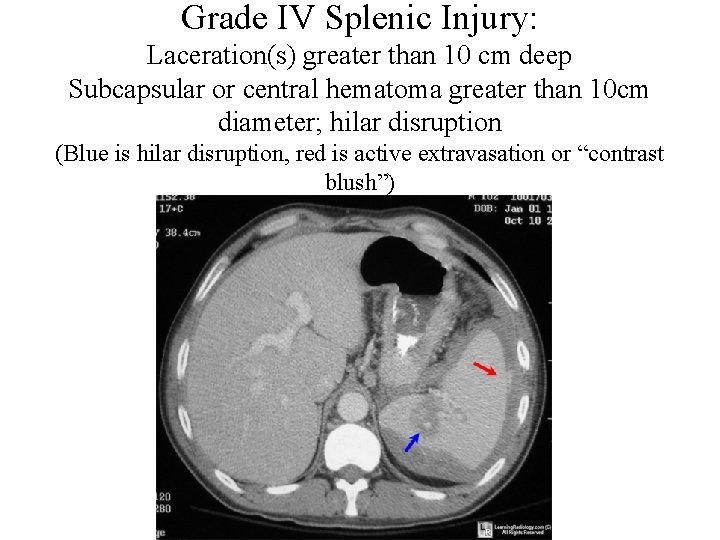
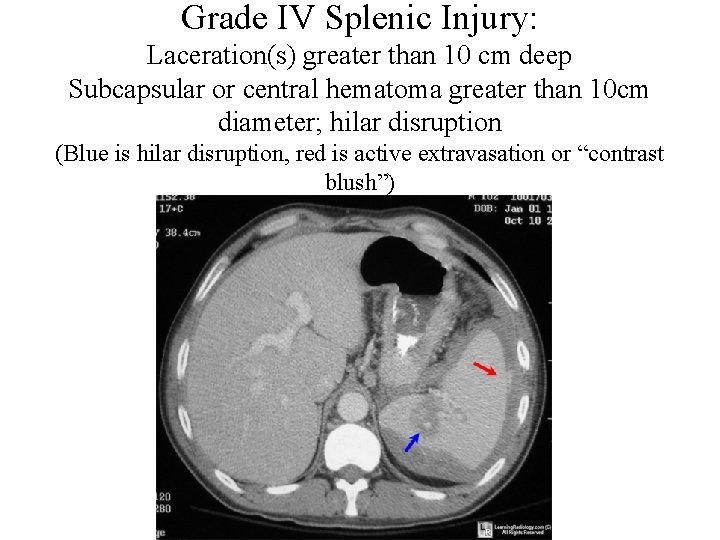
Grade IV Splenic Injury: Laceration(s) greater than 10 cm deep Subcapsular or central hematoma greater than 10 cm diameter; hilar disruption (Blue is hilar disruption, red is active extravasation or “contrast blush”)

Grade V Splenic Injury: “Shattered Spleen” – Splenic tissue maceration or devascularization
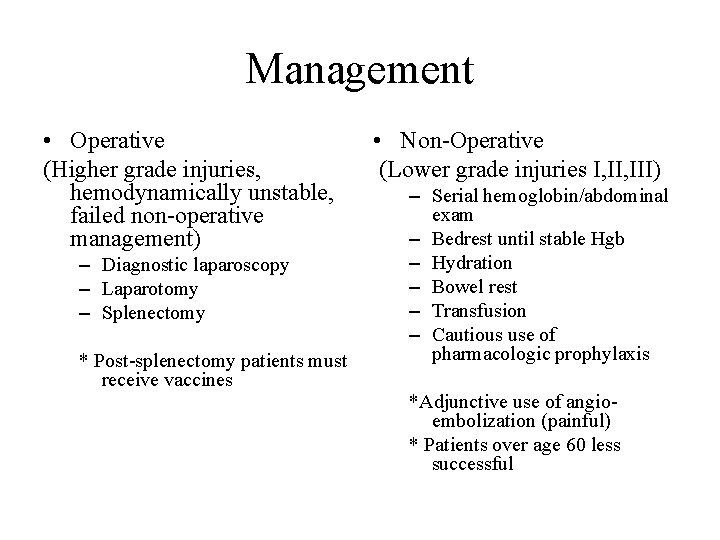
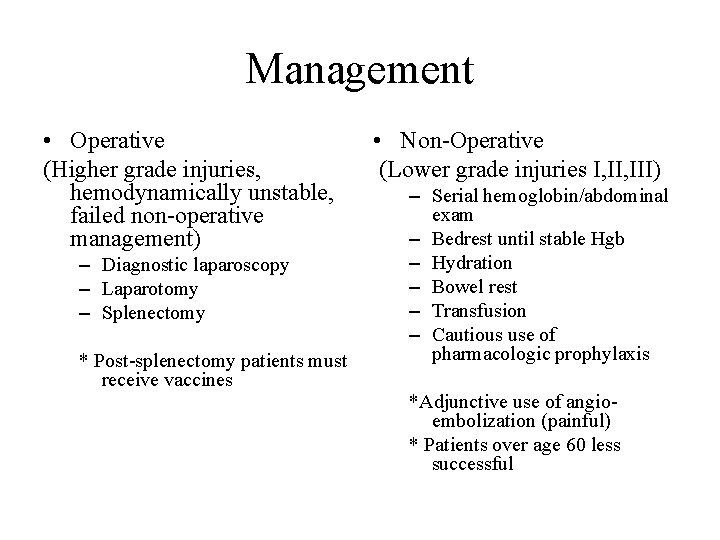
Management • Operative (Higher grade injuries, hemodynamically unstable, failed non-operative management) – Diagnostic laparoscopy – Laparotomy – Splenectomy * Post-splenectomy patients must receive vaccines • Non-Operative (Lower grade injuries I, III) – Serial hemoglobin/abdominal exam – Bedrest until stable Hgb – Hydration – Bowel rest – Transfusion – Cautious use of pharmacologic prophylaxis *Adjunctive use of angioembolization (painful) * Patients over age 60 less successful
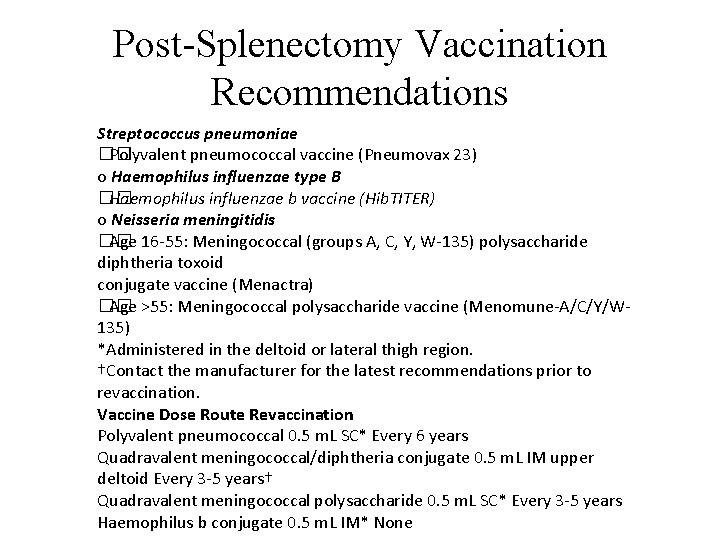
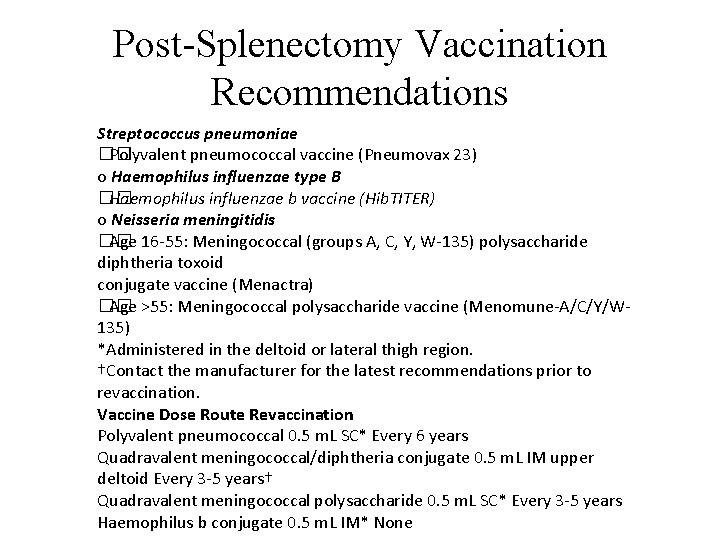
Post-Splenectomy Vaccination Recommendations Streptococcus pneumoniae �� Polyvalent pneumococcal vaccine (Pneumovax 23) o Haemophilus influenzae type B �� Haemophilus influenzae b vaccine (Hib. TITER) o Neisseria meningitidis �� Age 16 -55: Meningococcal (groups A, C, Y, W-135) polysaccharide diphtheria toxoid conjugate vaccine (Menactra) �� Age >55: Meningococcal polysaccharide vaccine (Menomune-A/C/Y/W 135) *Administered in the deltoid or lateral thigh region. †Contact the manufacturer for the latest recommendations prior to revaccination. Vaccine Dose Route Revaccination Polyvalent pneumococcal 0. 5 m. L SC* Every 6 years Quadravalent meningococcal/diphtheria conjugate 0. 5 m. L IM upper deltoid Every 3 -5 years† Quadravalent meningococcal polysaccharide 0. 5 m. L SC* Every 3 -5 years Haemophilus b conjugate 0. 5 m. L IM* None
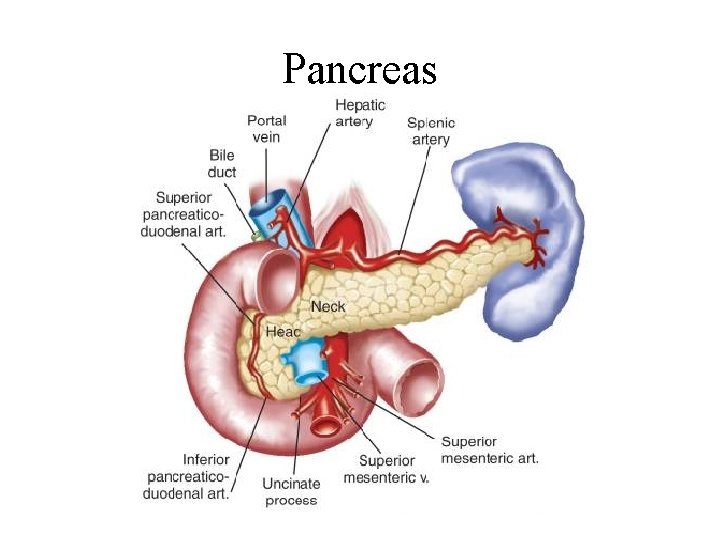
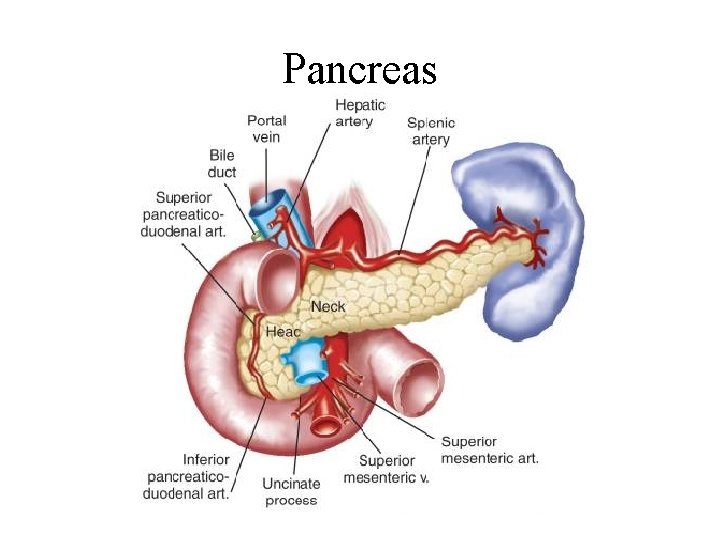
Pancreas

AAST Classification of Pancreatic Trauma • Grade I: Minor contusion without ductal injury • Grade II: Major contusion without ductal injury or tissue loss • Grade III: Distal transection or pancreatic parenchymal injury with ductal injury • Grade IV: Proximal transection or pancreatic parenchymal injury involving the ampulla • Grade V: Massive disruption of the pancreatic head
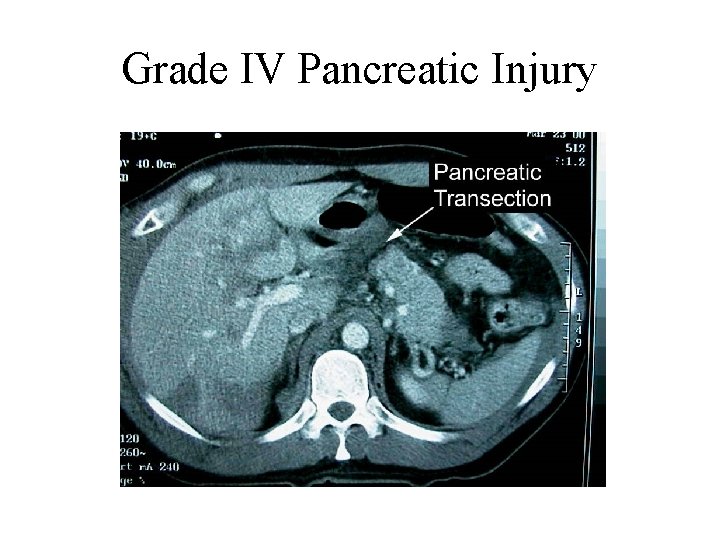
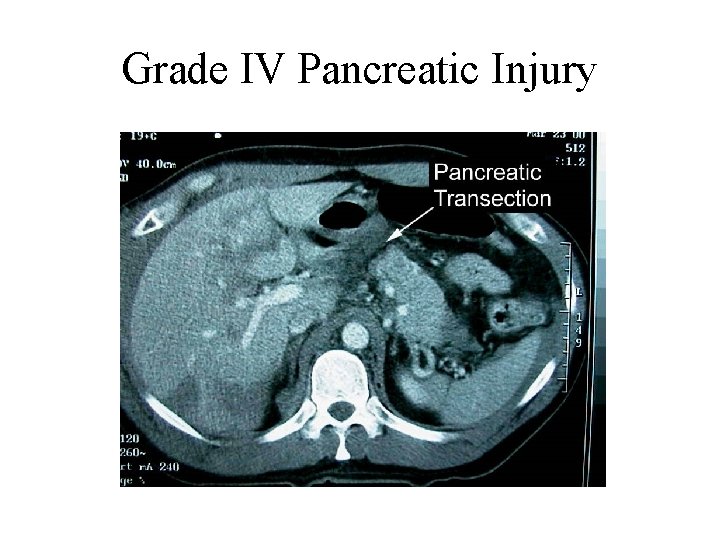
Grade IV Pancreatic Injury
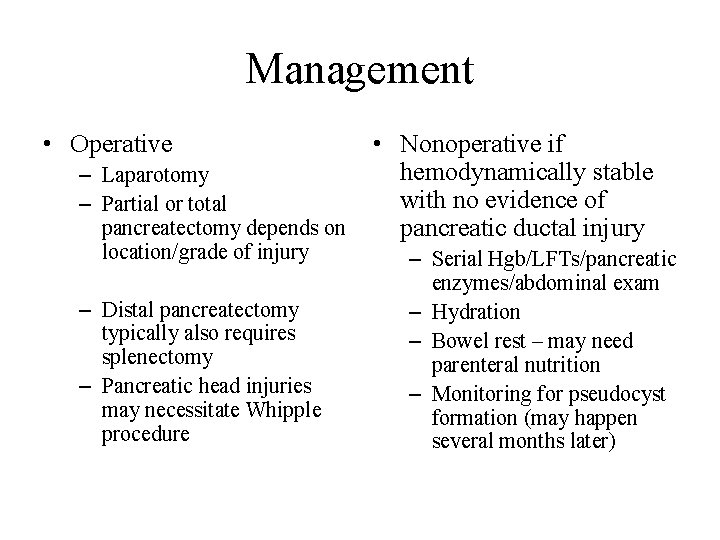
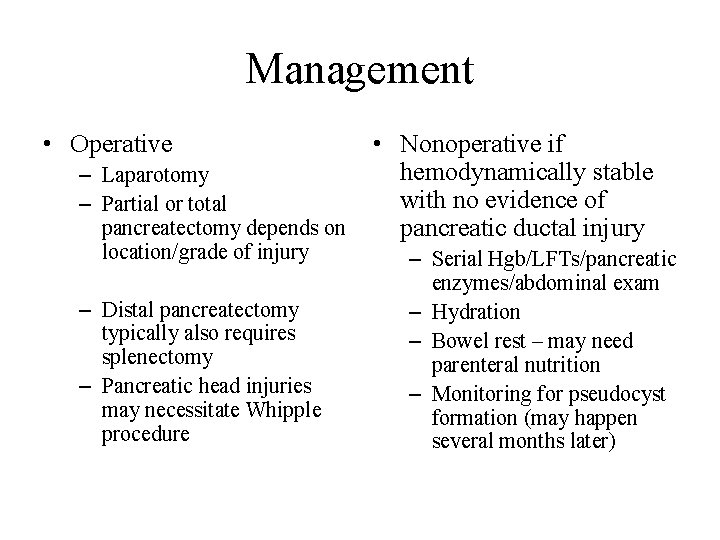
Management • Operative – Laparotomy – Partial or total pancreatectomy depends on location/grade of injury – Distal pancreatectomy typically also requires splenectomy – Pancreatic head injuries may necessitate Whipple procedure • Nonoperative if hemodynamically stable with no evidence of pancreatic ductal injury – Serial Hgb/LFTs/pancreatic enzymes/abdominal exam – Hydration – Bowel rest – may need parenteral nutrition – Monitoring for pseudocyst formation (may happen several months later)
 Spleen solid organ
Spleen solid organ Subdural hematoma concept map
Subdural hematoma concept map Tbi concept map
Tbi concept map Spleen injury grade
Spleen injury grade Gallbladder and spleen
Gallbladder and spleen Intentional injury examples
Intentional injury examples Liver injury grading
Liver injury grading Portal triad
Portal triad Cell tissue organ organ system organism
Cell tissue organ organ system organism Tissues group together to form
Tissues group together to form Organ penyusun gerak manusia
Organ penyusun gerak manusia Organ and organ system
Organ and organ system Organ organ pernafasan
Organ organ pernafasan Penyusun sistem saraf pusat adalah
Penyusun sistem saraf pusat adalah C ptsd
C ptsd Acute stress disorder diagnosis
Acute stress disorder diagnosis Subfalcine herniation
Subfalcine herniation Traumatic subdural hematoma
Traumatic subdural hematoma Damselfly
Damselfly Post traumatic cervical dystonia
Post traumatic cervical dystonia Traumatic overbite definition
Traumatic overbite definition Csf traumatic tap
Csf traumatic tap Post traumatic stress disorder
Post traumatic stress disorder Hyponuria
Hyponuria Tbi long term servival after traumatic
Tbi long term servival after traumatic Honors its atomic
Honors its atomic Solid solution example
Solid solution example Covalent molecular and covalent network
Covalent molecular and covalent network