Reproductive System Male Part 1 Honors Anatomy Physiology






















- Slides: 76
Reproductive System Male Part 1 Honors Anatomy & Physiology
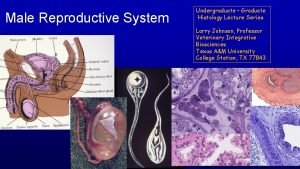
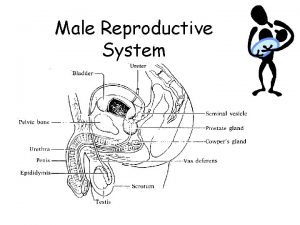
Organs of the Male Reproductive System Scrotum Testes 1. 2. • 3. • System of Ducts epididymis, ductus deferens, ejaculatory ducts, and urethra Accessory Sex Glands 4. • 5. paired gonads seminal vesicles, prostate, bulbourethral glands Penis
Functions of the Male Reproductive System 1. 2. 3. 4. Testes produce sperm & male reproductive hormones Ducts transport, store, & assist in maturation of sperrm Accessory Sex Glands secret most of the liquid portion of semen Penis contains the urethra, a passageway for ejaculation of semen
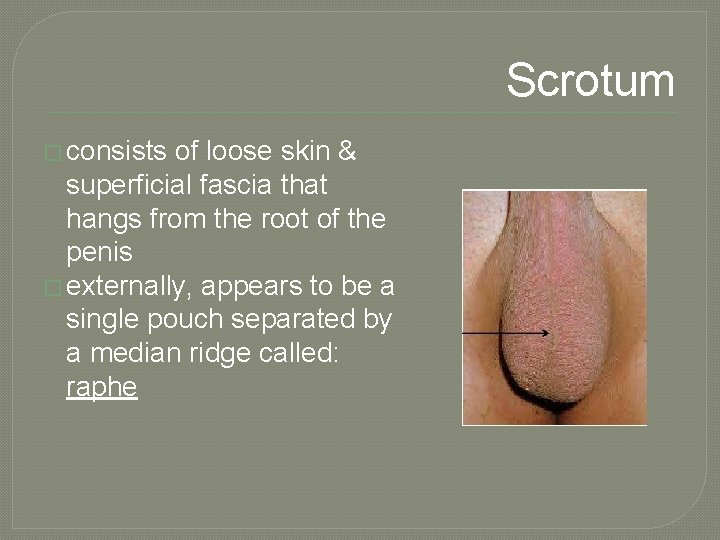
Scrotum � consists of loose skin & superficial fascia that hangs from the root of the penis � externally, appears to be a single pouch separated by a median ridge called: raphe
Scrotal Septum � internally to raphe is a scrotal septum separating it into 2 sacs, each containing a testis � septum made up of dartos muscle • smooth muscle • contraction (gives wrinkled appearance) reduces heat loss � cremaster muscle: extension of internal oblique muscle (skeletal) • contraction of these muscles helps regulate temperature of testes • in response to cold temperatures contraction brings testes closer to body where they will absorb heat

The Male Perineum �Diamond-shaped region between pubic symphysis, coccyx, and ischial tuberosities �Suspends scrotum; contains root of penis and anus © 2013 Pearson Education, Inc.

Figure 27. 4 The male perineum, inferior view. Penis Scrotum Pubic symphysis Ischial tuberosity Anus Coccyx © 2013 Pearson Education, Inc.
Testes �aka testicles �paired oval glands �~5 cm long x 2. 5 cm in diameter �~10 – 15 g �develop in abd cavity near kidneys & descend to scrotum thru inguinal canals during latter half of 7 th month of pregnancy

Cryptochidism �“undescended” testes �~3% full-term males �~30% preterm males �some will descend on own during 1 st 6 mo of life �must surgically place them (by 18 mos age) in scrotum or: • initial stage of spermatogenesis destroyed • 30 -50 xs more likely to have testicular cancer
Homeostatic Imbalance �Testicular • • cancer Rare; most common cancer in men 15 -35 Cryptorchidism is risk factor Sign – painless, solid mass in testis 90% cured by surgical removal of testis and often radiation or chemotherapy © 2013 Pearson Education, Inc.
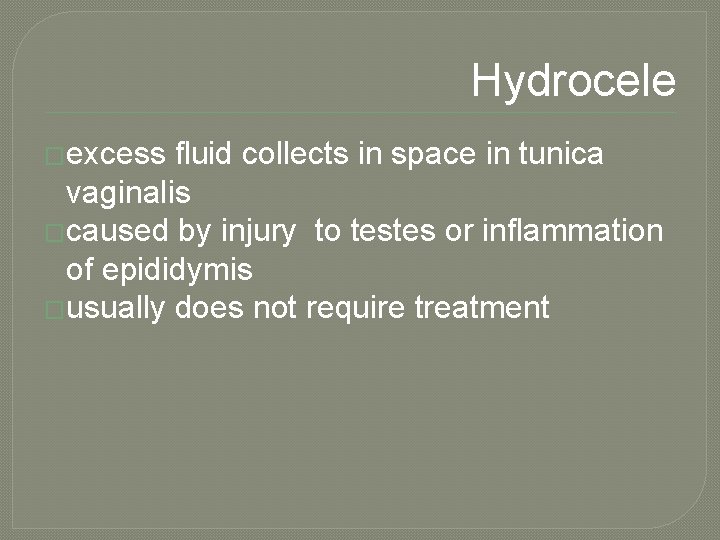
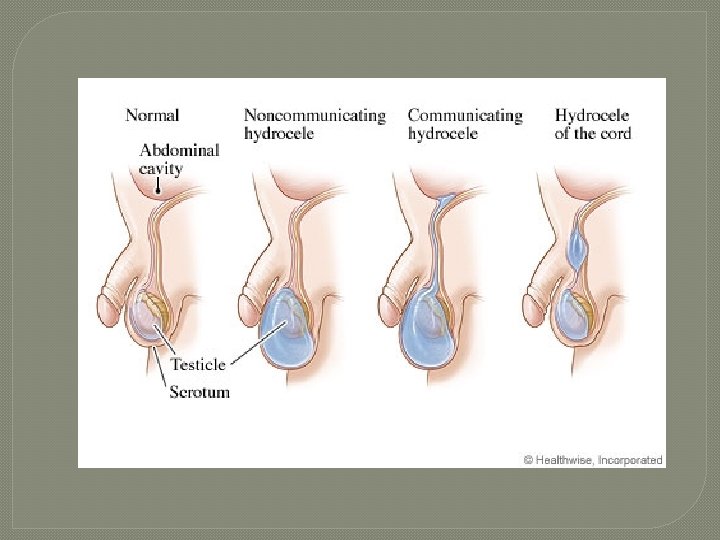
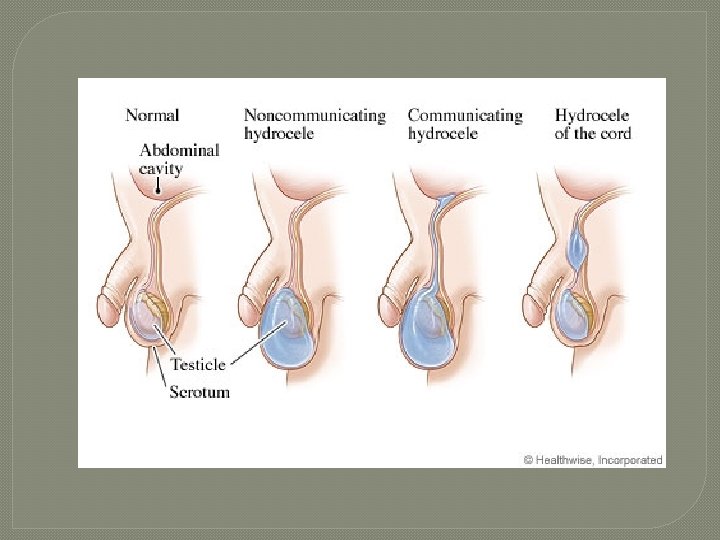
Hydrocele �excess fluid collects in space in tunica vaginalis �caused by injury to testes or inflammation of epididymis �usually does not require treatment
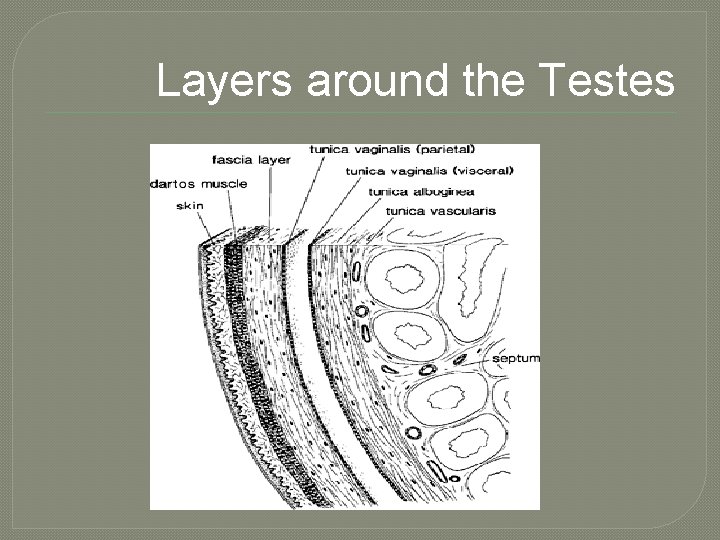
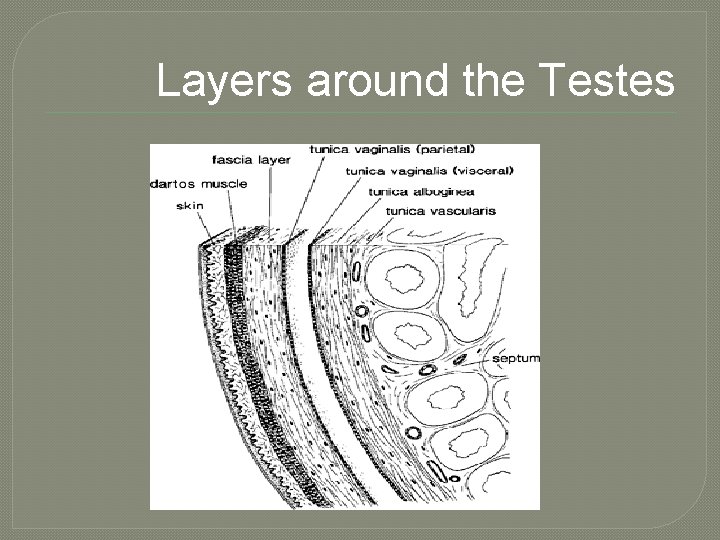
Layers around the Testes
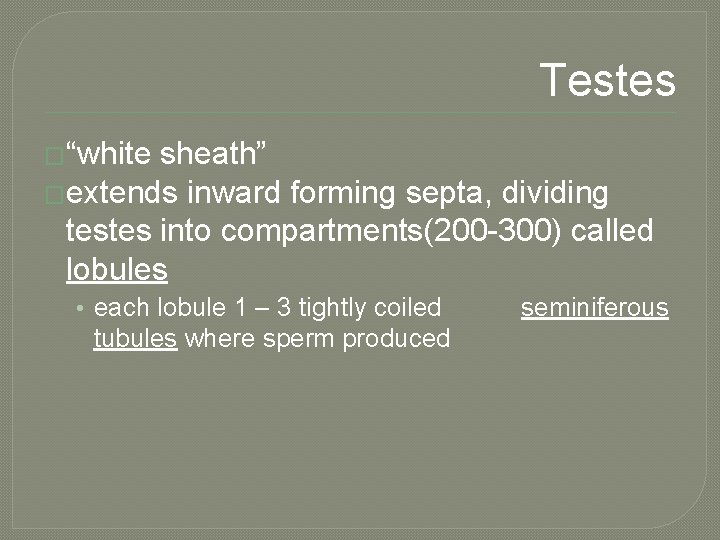
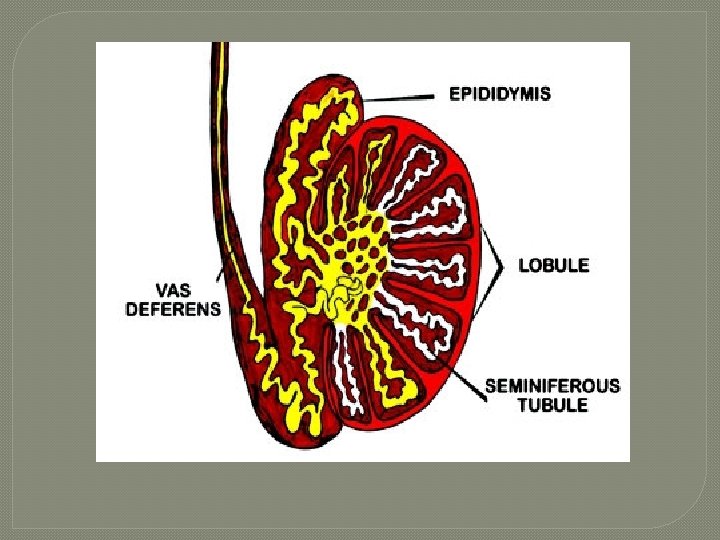
Testes �“white sheath” �extends inward forming septa, dividing testes into compartments(200 -300) called lobules • each lobule 1 – 3 tightly coiled tubules where sperm produced seminiferous
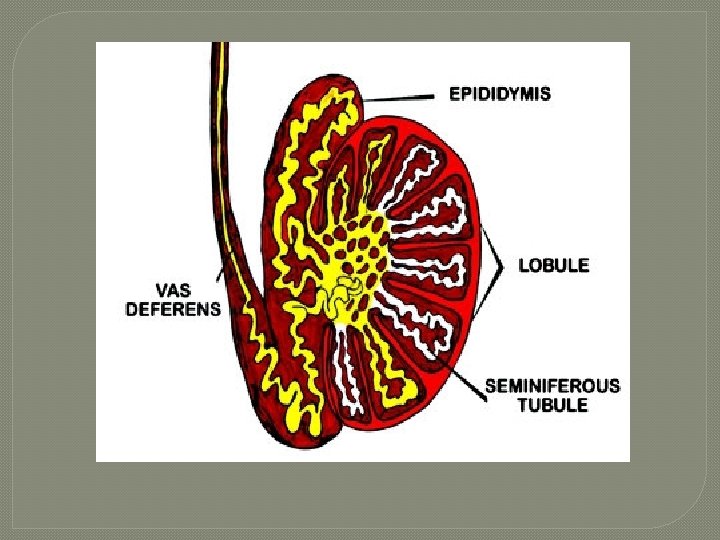

Seminiferous Tubules � thick, stratified epithelium surrounding central fluid-containing lumen � epithelium • Spheroid spermatogenic cells embedded in sustentocytes � myoid cells surround each tubule • may squeeze sperm, testicular fluids out of testes � tubules of each lobule form straight tubule © 2013 Pearson Education, Inc.
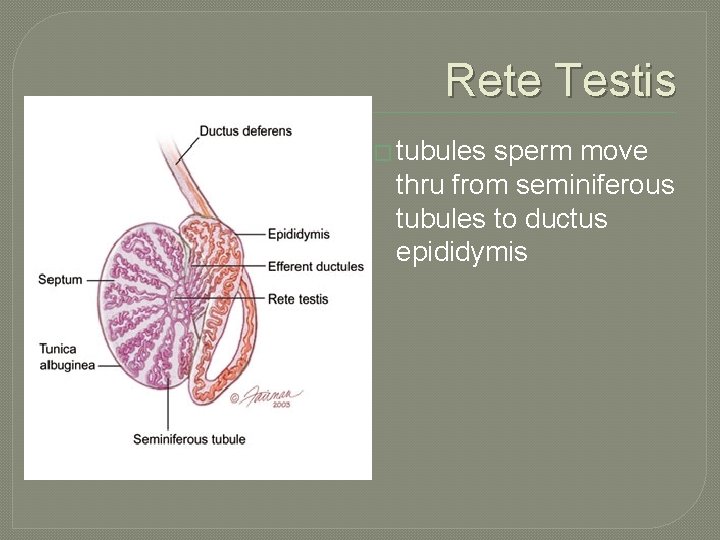
The Testes �Sperm • • • travel route: Seminiferous tubules Straight tubule Rete testis Efferent ductules Epididymis © 2013 Pearson Education, Inc.
Seminiferous Tubules �Interstitial endocrine cells in soft tissue surrounding seminiferous tubules �produce androgens, e. g. , testosterone • secrete it into interstitial fluid © 2013 Pearson Education, Inc.
The Testes �Blood supply • Testicular arteries arise from abdominal aorta • Testicular veins arise from pampiniform venous plexus surrounding each testicular artery �cooler; absorb heat from testicular arteries �keeps testes cool �Spermatic cord • nerve fibers, blood vessels, & lymphatics that supply testes © 2013 Pearson Education, Inc.
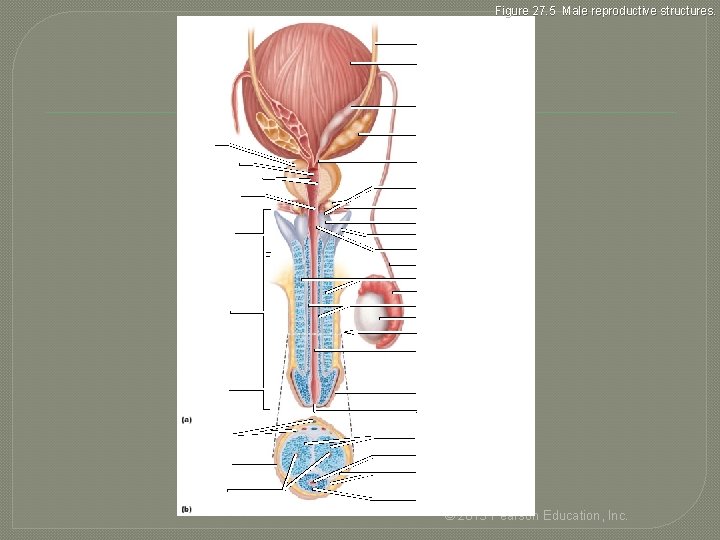
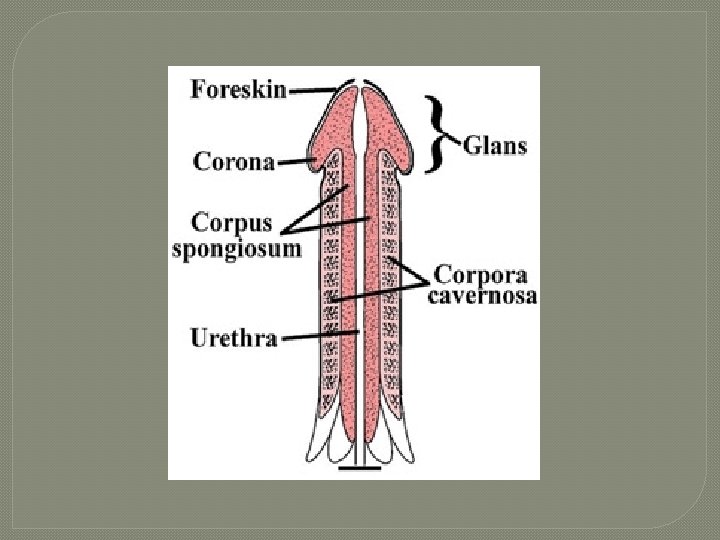
The Penis �consists of • Root and shaft that ends in glans penis • Prepuce, or foreskin—cuff of loose skin covering glans • Crura �proximal ends of corpora cavernosa surrounded by ischiocavernosus muscle; �anchors penis to pubic arch © 2013 Pearson Education, Inc.
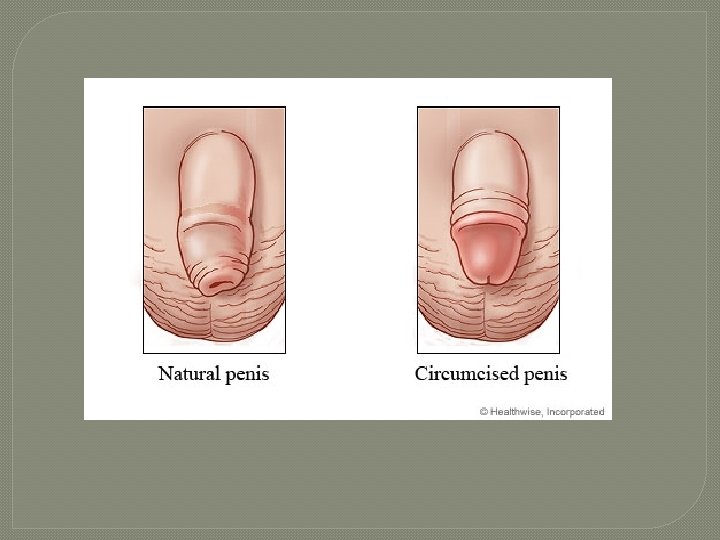
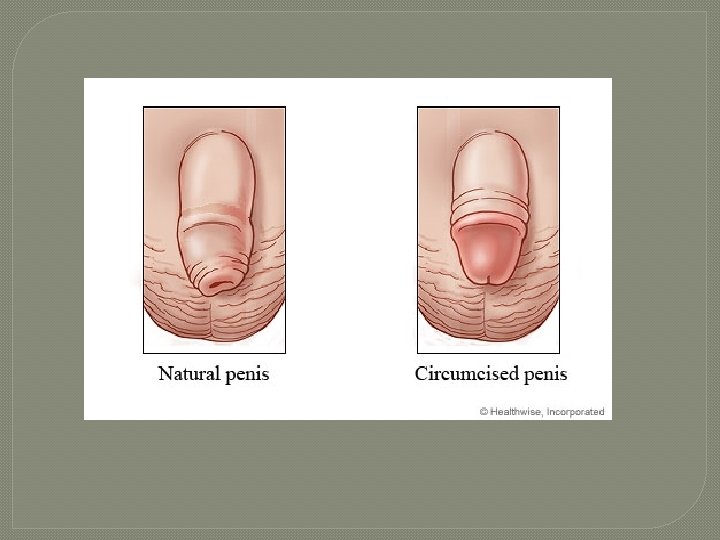
Circumcision �Surgical removal of foreskin � 60% newborn boys in US circumcised • 15% in other parts of world • some claim medically unnecessary • studies show � 60% reduction in HIV risk �Reduced risk for other reproductive system infections © 2013 Pearson Education, Inc.
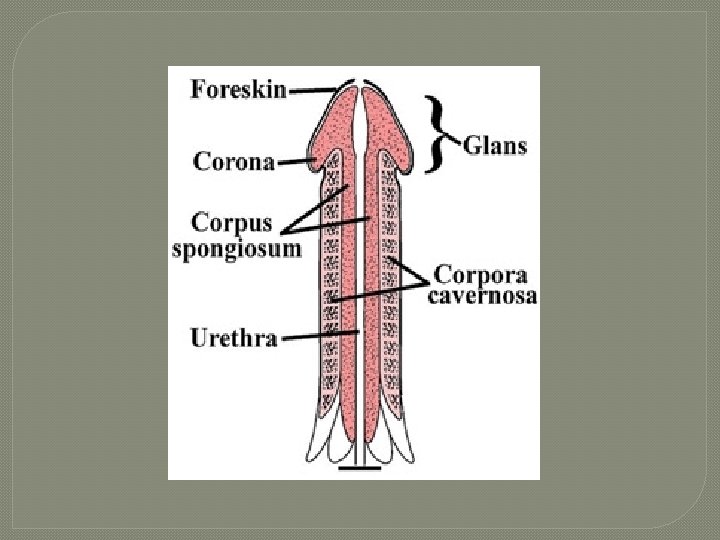
The Penis: Internally � Spongy urethra and three cylindrical bodies of erectile tissue (spongy network of connective tissue and smooth muscle with vascular spaces) • Corpus spongiosum - surrounds urethra and expands to form glans and bulb • Corpora cavernosa - paired dorsal erectile bodies � Erection - erectile tissue fills with blood, causing penis to enlarge and become rigid © 2013 Pearson Education, Inc.
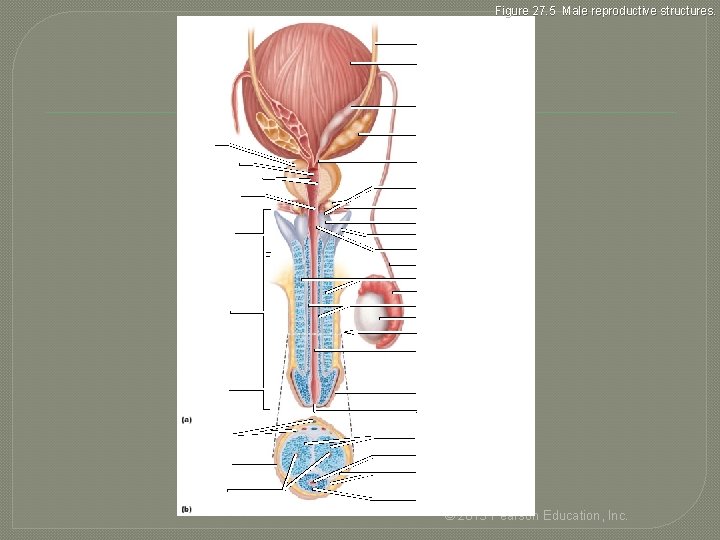
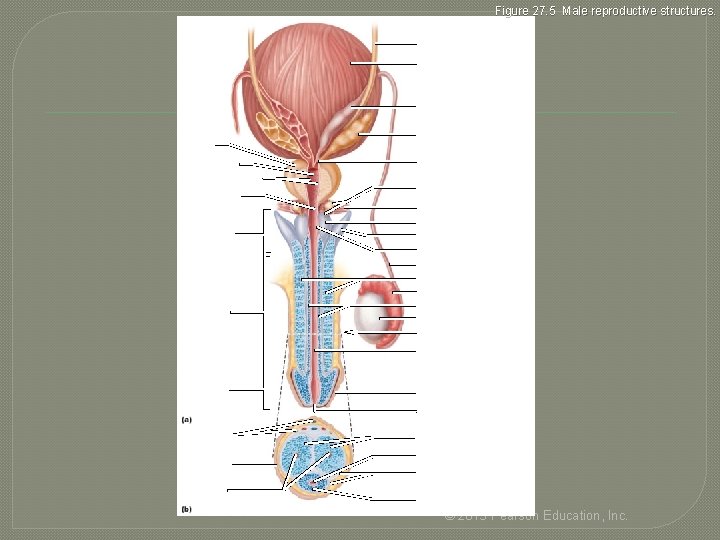
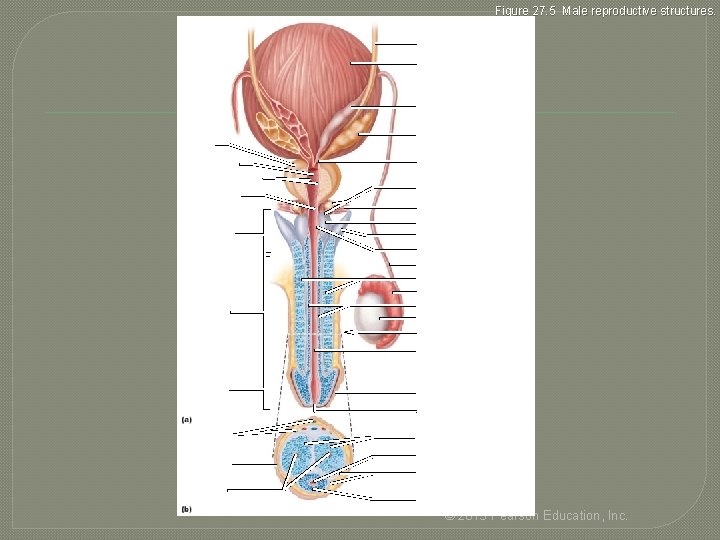
Figure 27. 5 Male reproductive structures. Ureter Urinary bladder Ampulla of ductus deferens Seminal gland Prostate Prostatic urethra Ejaculatory duct Orifices of prostatic ducts Intermediate part of the urethra (membranous urethra) Urogenital diaphragm Root of penis Crus of penis Bulbo-urethral gland duct Bulb of penis Bulbo-urethral duct opening Ductus deferens Corpora cavernosa Epididymis Body (shaft) of penis Corpus spongiosum Testis Section of (b) Spongy urethra Glans penis Prepuce (foreskin) External urethral orifice Dorsal vessels and nerves Corpora cavernosa Urethra Skin Tunica albuginea of erectile bodies Deep arteries Corpus spongiosum © 2013 Pearson Education, Inc.
The Male Duct System �Ducts carry sperm from testes to body exterior • • Epididymis Ductus deferens Ejaculatory duct Urethra © 2013 Pearson Education, Inc.
Epididymis � Head - contains efferent ductules; superior aspect of testis; body and tail on posterolateral area of testis � Duct of the epididymis ~ 6 m in length • Microvilli (stereocilia) absorb testicular fluid and pass nutrients to stored sperm � nonmotile sperm enter, pass slowly through (~ 20 days), become motile; can be stored several months � during ejaculation epididymis contracts, expelling sperm into ductus deferens © 2013 Pearson Education, Inc.
Ductus Deferens and Ejaculatory Duct �Ductus deferens (vas deferens) ~ 45 cm • passes through inguinal canal to pelvic cavity • expands to form ampulla; joins duct of seminal vesicle to form ejaculatory duct �smooth muscle in walls propels sperm from epididymis to urethra �Vasectomy - cutting and ligating ductus deferens; nearly 100% effective form of birth control © 2013 Pearson Education, Inc.
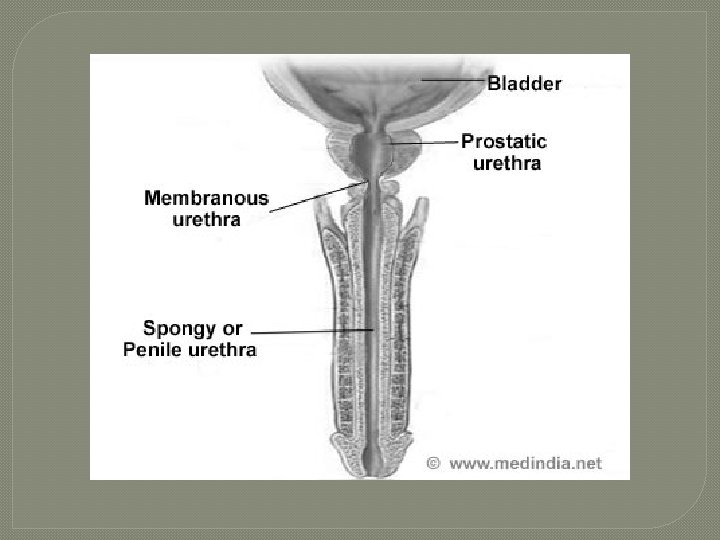
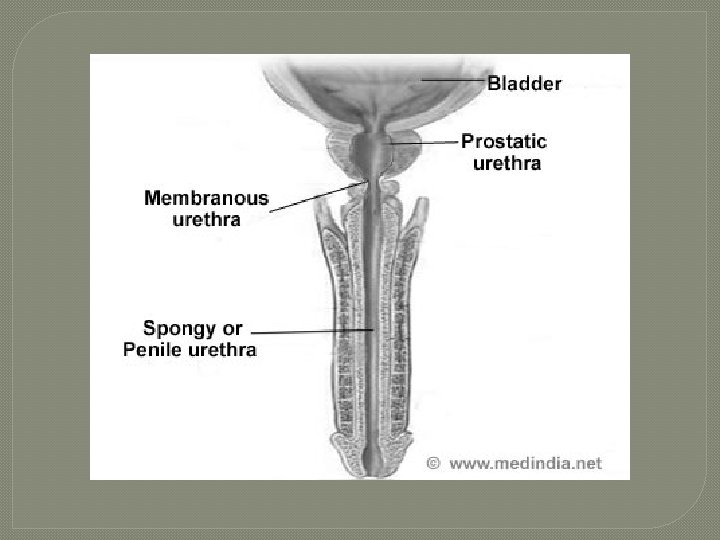
Urethra �conveys both urine and semen (at different times) � 3 regions 1. Prostatic urethra – surrounded by prostate 2. Intermediate part of the urethra (membranous urethra) – in urogenital diaphragm 3. Spongy urethra – runs through penis; opens at external urethral orifice © 2013 Pearson Education, Inc.
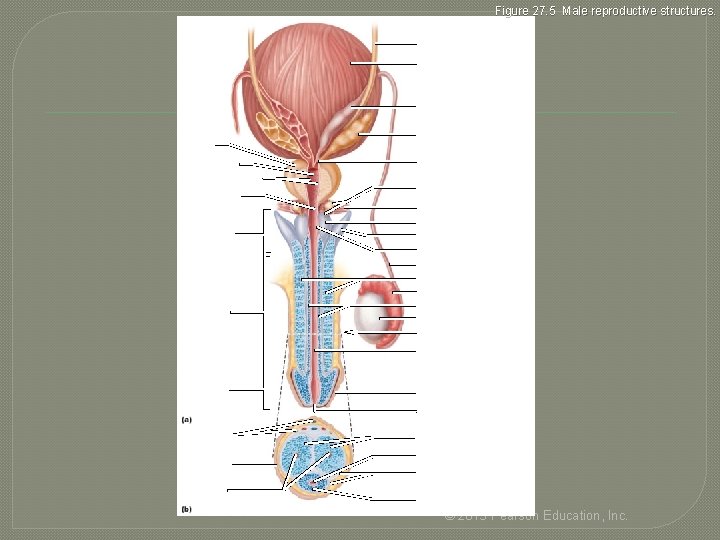
Figure 27. 5 Male reproductive structures. Ureter Urinary bladder Ampulla of ductus deferens Seminal gland Prostate Prostatic urethra Ejaculatory duct Orifices of prostatic ducts Intermediate part of the urethra (membranous urethra) Urogenital diaphragm Root of penis Crus of penis Bulbo-urethral gland duct Bulb of penis Bulbo-urethral duct opening Ductus deferens Corpora cavernosa Epididymis Body (shaft) of penis Corpus spongiosum Testis Section of (b) Spongy urethra Glans penis Prepuce (foreskin) External urethral orifice Dorsal vessels and nerves Corpora cavernosa Urethra Skin Tunica albuginea of erectile bodies Deep arteries Corpus spongiosum © 2013 Pearson Education, Inc.
The Male Accessory Glands �Paired seminal glands (seminal vesicles) �Paired bulbo-urethral glands �Prostate � together produce bulk of semen • remainder - sperm from testes © 2013 Pearson Education, Inc.

Accessory Glands: Prostate �Encircles urethra inferior to bladder; size of peach pit; smooth muscle contracts during ejaculation �Secretes milky, slightly acid fluid • Contains citrate, enzymes, and prostate-specific antigen (PSA) • Role in sperm activation • Enters prostatic urethra during ejaculation � 1/3 semen volume © 2013 Pearson Education, Inc.
Prostate Disorders �Prostatitis – inflammatory disorders • Bacterial infection; acute and chronic; treated with antibiotics �Benign prostatic hyperplasia • May be age-related; distorts urethra; treated with surgery, microwaves, drugs, balloon compression, radio-frequency radiation © 2013 Pearson Education, Inc.
Prostate Disorders �Prostate cancer • 2 nd most common cause of cancer death in males • digital exam screening, PSA levels �biopsy if abnormal • treated with surgery and sometimes radiation; castration; drugs • in clinical trials - cryosurgery, chemotherapy, ultrasound, proton beam therapy © 2013 Pearson Education, Inc.
Accessory Glands: Bulbo-Urethral Glands (Cowper's Glands) �pea-sized glands inferior to prostate �produce thick, clear mucus during sexual arousal • lubricate glans penis • neutralize traces of acidic urine in urethra © 2013 Pearson Education, Inc.
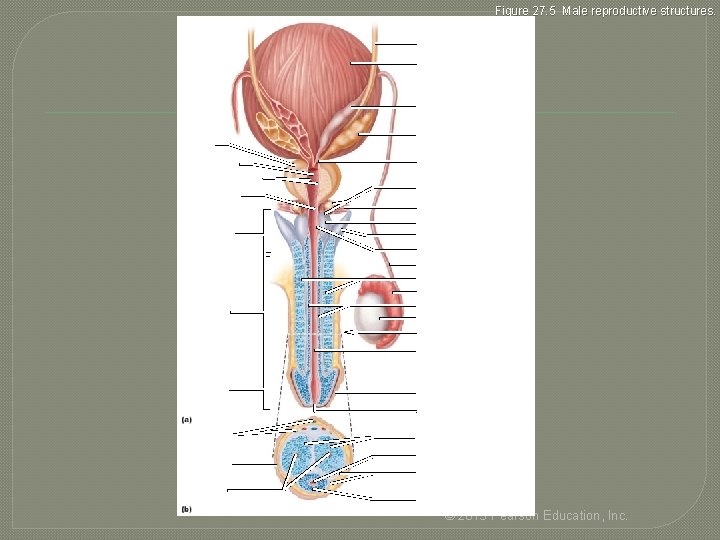
Figure 27. 5 Male reproductive structures. Ureter Urinary bladder Ampulla of ductus deferens Seminal gland Prostate Prostatic urethra Ejaculatory duct Orifices of prostatic ducts Intermediate part of the urethra (membranous urethra) Urogenital diaphragm Root of penis Crus of penis Bulbo-urethral gland duct Bulb of penis Bulbo-urethral duct opening Ductus deferens Corpora cavernosa Epididymis Body (shaft) of penis Corpus spongiosum Testis Section of (b) Spongy urethra Glans penis Prepuce (foreskin) External urethral orifice Dorsal vessels and nerves Corpora cavernosa Urethra Skin Tunica albuginea of erectile bodies Deep arteries Corpus spongiosum © 2013 Pearson Education, Inc.
Semen �milky-white mixture of sperm and accessory gland secretions • 2– 5 ml semen ejaculated, contains 20– 150 million sperm/ml �contains fructose for ATP production; protects and activates sperm; facilitates sperm movement �alkaline neutralizes acidity of male urethra and female vagina enhanced motility © 2013 Pearson Education, Inc.

Semen Functions � prostaglandins decrease viscosity of mucus in cervix; stimulate reverse peristalsis in uterus � hormone relaxin, enzymes sperm motility � contains ATP for energy � suppresses female immune response � antibacterial action � clotting factors coagulate semen initially to prevent draining out; then liquefied by fibrinolysin sperm begin journey © 2013 Pearson Education, Inc.
End of Male Reproductive System Part 1

Spermatogenesis �process by which sperm are produced

Seminiferous Tubules � 2 types of cells Spermatogenic cells 1. • sperm-forming cells: include stem cells, spermatogonia ( 1◦ spermatocytes 2◦ spermatocytes spermatids spermatozoon which is released into lumen of seminiferous tubules) Sertoli cells 2. • • functions in supporting spermatogenesis aka sustentacular cells


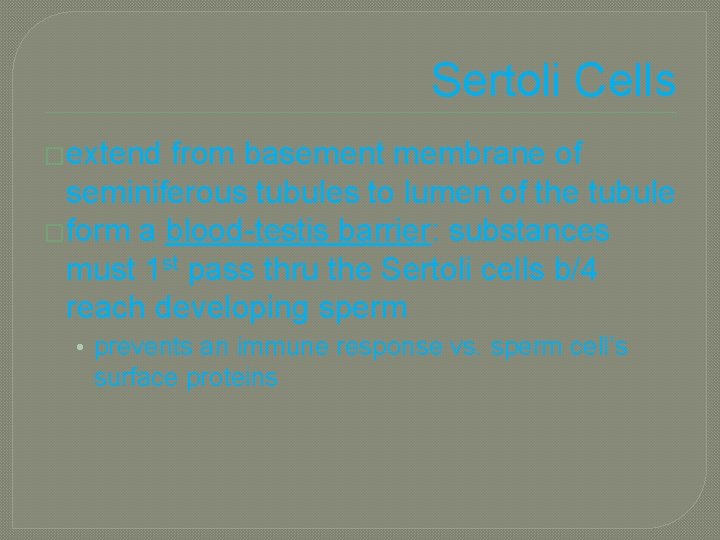
Sertoli Cells �extend from basement membrane of seminiferous tubules to lumen of the tubule �form a blood-testis barrier: substances must 1 st pass thru the Sertoli cells b/4 reach developing sperm • prevents an immune response vs. sperm cell’s surface proteins
Sertoli Cells �support & protect devoloping spermatogenic cells in a few ways: • • nourishment phagocytize excess spermatid cytoplasm produce fluid for sperm transport into lumen secrete hormone inhibin: mediates effects of T & FSH

Leydig Cells � endocrine � secrete T function

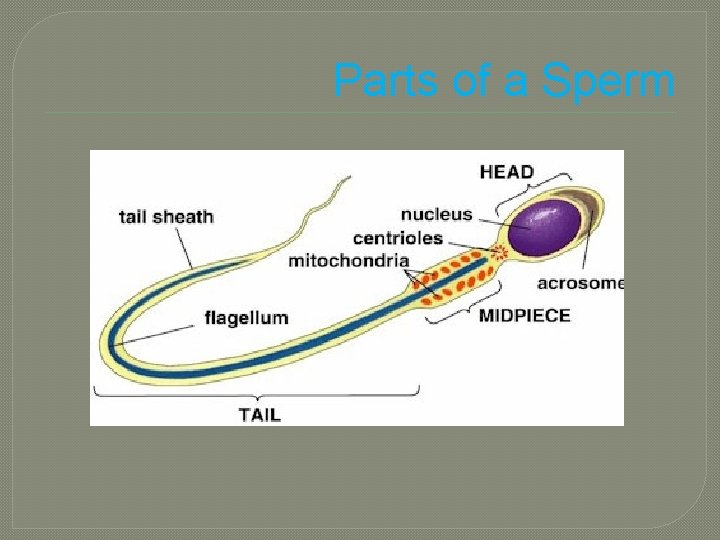
Sperm �~300 million sperm complete spermatogenesis every day (after puberty) �~60 µm long �major parts: 1. Head 2. Nucleus 3. Acrosome 4. Tail
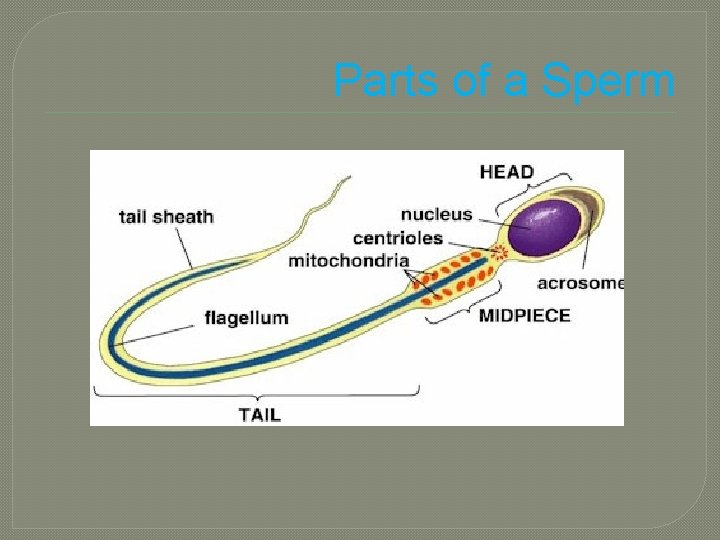
Parts of a Sperm
Parts of a Sperm � Acrosome: • covers anterior 2/3 of nucleus • contains enzymes used in fertilization � Head: • contains nucleus � Neck • constricted part behind head � Middle Piece • contains mitochondria arranged in a spiral � Principal Piece • longest portion of tail � End Piece • terminus of tail

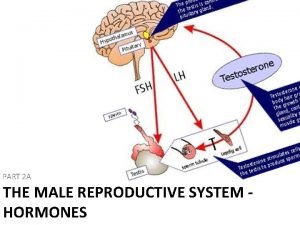
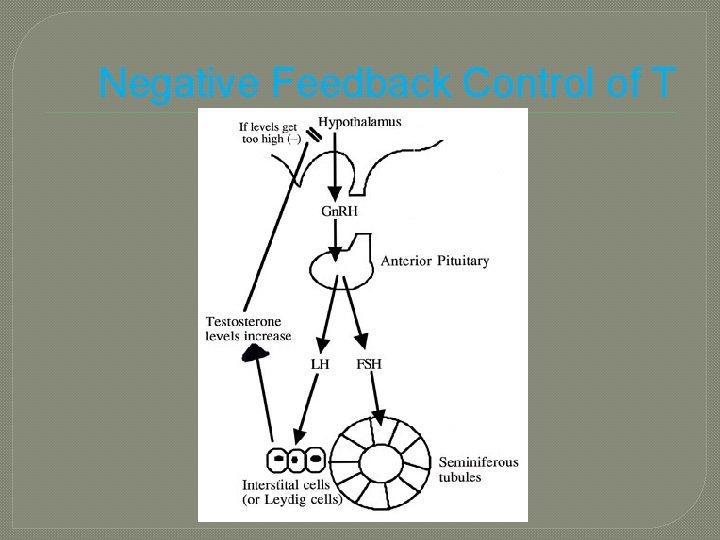
Hormonal Control of the Testes �@ puberty hypothalamus increases secretion of Gn. RH stimulates anterior pituitary to release 2 gonadotropins: 1. LH • stimulates Leydig cells T FSH 2. • with T stimulates spermatogenesis
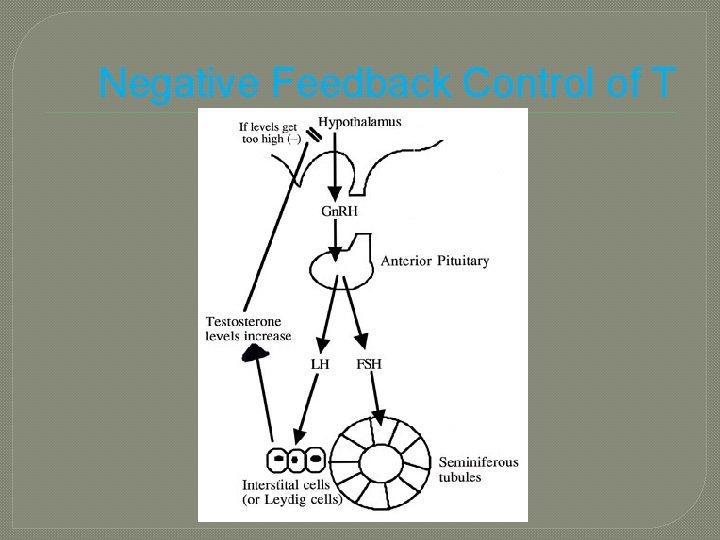
Negative Feedback Control of T
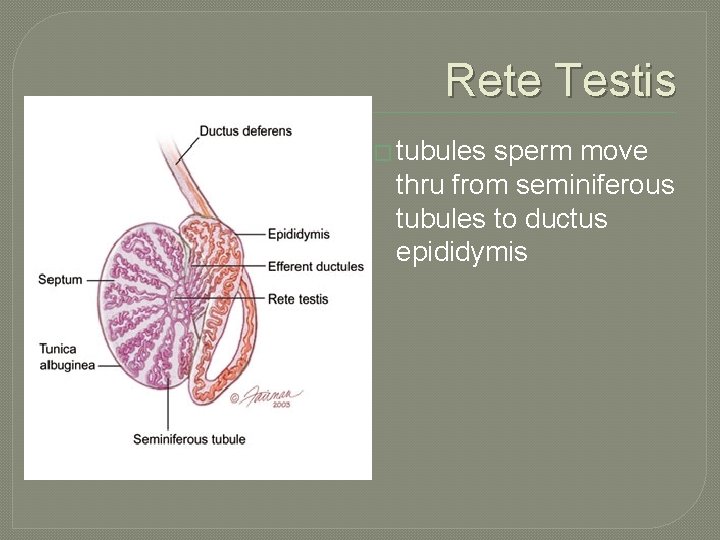
Rete Testis � tubules sperm move thru from seminiferous tubules to ductus epididymis
Epididymis �comma-shaped �lies along posterior border of each testis �made up of tightly coiled ductus epididymis �Function: site of sperm maturation �Head • superior portion �Body • Narrow midportion �Tail • smaller inferior portion

Ductus Deferens �aka vas deferens �terminal portion dilated = ampulla �duct ascends along posterior border of epididymis thru inguinal canal into pelvic cavity loops over ureter down posterior surface of bladder prostatic urethra �function: release sperm during ejacuolation
Vasectomy �principle method of sterilization for males �portion of each vas deferens removed �sperm production continues in testes but do not go far �sperm degenerate over time phagocytozed �T levels remain normal

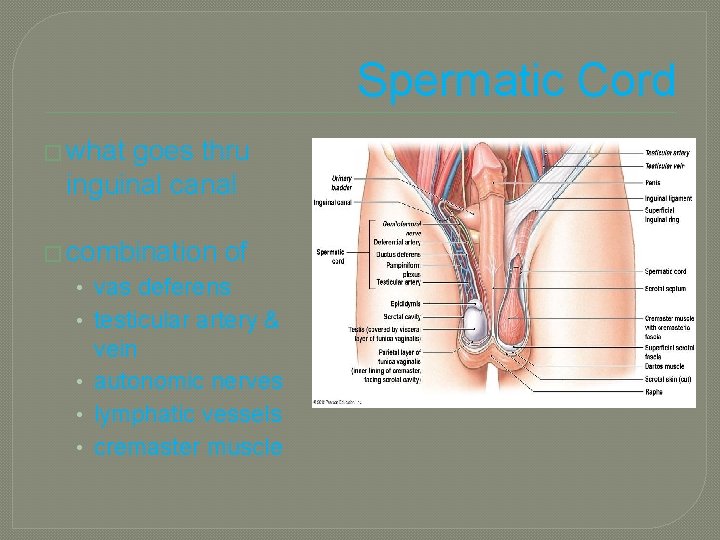
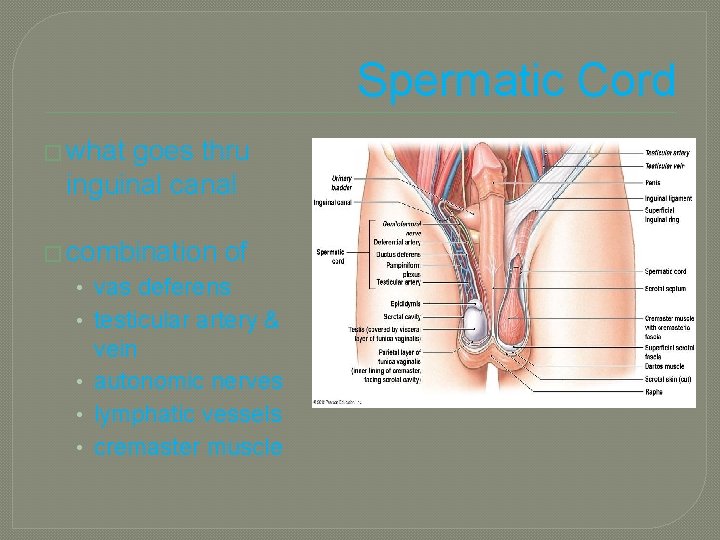
Spermatic Cord � what goes thru inguinal canal � combination of • vas deferens • testicular artery & vein • autonomic nerves • lymphatic vessels • cremaster muscle
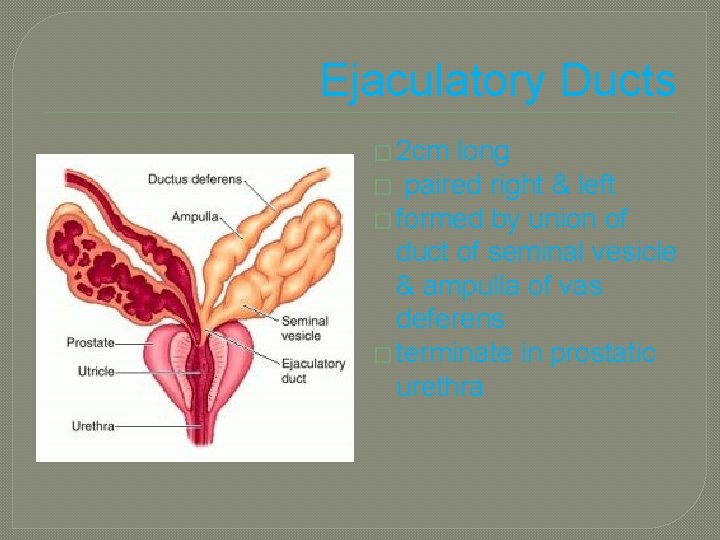
Ejaculatory Ducts � 2 cm long � paired right & left � formed by union of duct of seminal vesicle & ampulla of vas deferens � terminate in prostatic urethra
Urethra �shared duct for urinary & reproductive system �passes from bladder prostatic urethra membranous urethra(thru deep muscles of perineum spongy or penile urethra external urethral orifice
Accessory Sex Glands �secrete most of the liquid portion of semen �Include: 1. 2. 3. Seminal Vesicles Prostate Bulbourethral Glands

Seminal Vesicles �secrete alkaline, viscous fluid �helps neutralize acid in female reproductive tract �provides fructose for ATP production in sperm �contributes to sperm motility & viability �helps semen coagulate after ejaculation
Prostate Gland �single, donut-shaped gland (golf ball size) �inferior to urinary bladder �surrounds prostatic urethra �increases in size slowly from birth to puberty then rapidly grows until ~age 30 �further enlargement can occur after age 45

Prostate Gland �secretes milky, slightly acidic fluid that helps semen coagulate after ejaculation and then breaks down the clot

Bulbourethral Glands �aka Cowper’s Gland �Secretes 1. alkaline fluid that neutralizes the acidic environment of the urethra 2. mucus that lubricates lining of urethra & tip of penis during sexual intercourse

Semen �“seed” �sperm + secretions of accessory sex glands • p. H 7. 2 – 7. 7 • coagulates w/in 5 min (functional role unknown) �volume ~ 2. 5 – 5 m. L with: • 50 – 150 million sperm • <20 million/m. L likely to cause infertility
Penis � cylindrical 1. 2. 3. body � Body of the penis: body 1 & 2: corpora cavernosa • 3 cylindricalmasses of 3: smaller, midventral tissue corpus spongiosum glans penis • corona erectile tissue composed • prepuce (foreskin) of many vascular root spaces called sinuses • attaches penis to surrounded by smooth body muscle & elastic CT

Circumcision �surgical removal of part of foreskin (prepuce) �performed 3 to 8 days after delivery �may have benefits of fewer UTI and transmission of STDs
Erection �with stimulation(visual, tactile, auditory, olfactory, or imagined) parasympathetic fibers from sacral spine

Ejaculation �powerful release of semen from urethra controlled by a sympathetic spinal reflex (lumbar spine)

 Art-labeling activity: the male reproductive system, part 1
Art-labeling activity: the male reproductive system, part 1 Chapter 2 human reproductive anatomy and physiology
Chapter 2 human reproductive anatomy and physiology Male prostate anatomy
Male prostate anatomy Male reproductive system from front
Male reproductive system from front Fungsi bagian yang ditunjuk oleh huruf p adalah
Fungsi bagian yang ditunjuk oleh huruf p adalah Seminal tubules
Seminal tubules Exercise 42 anatomy of the reproductive system
Exercise 42 anatomy of the reproductive system Oogenesis process
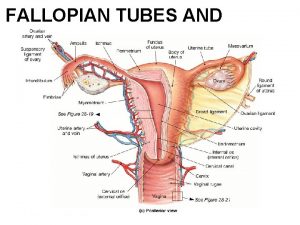
Oogenesis process Broad ligament
Broad ligament Female and male reproductive system
Female and male reproductive system Male reproductive system
Male reproductive system Luteinizing hormone in male reproductive system
Luteinizing hormone in male reproductive system Male plant reproductive system
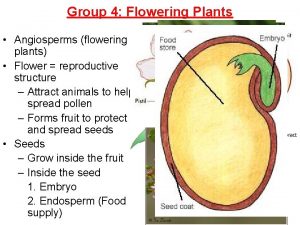
Male plant reproductive system Male reproductive system information
Male reproductive system information Where sperm is stored
Where sperm is stored Functions of testes
Functions of testes Male reproductive system plants
Male reproductive system plants Function of male reproductive system
Function of male reproductive system Fish reproductive system
Fish reproductive system Reproductive system of pila
Reproductive system of pila Pig male reproductive system
Pig male reproductive system Male plant reproductive system
Male plant reproductive system Figure 28-1 the male reproductive system
Figure 28-1 the male reproductive system Base of prostate gland
Base of prostate gland Lesson 20.2 the male reproductive system
Lesson 20.2 the male reproductive system Ram reproductive system
Ram reproductive system Pearson
Pearson Colon function in male reproductive system
Colon function in male reproductive system Figure 16-1 male reproductive system
Figure 16-1 male reproductive system Differences between male and female reproductive organ
Differences between male and female reproductive organ Male reproductive system labeled
Male reproductive system labeled Pathway of sperm in male reproductive system
Pathway of sperm in male reproductive system 90/2
90/2 Plants reproductive system
Plants reproductive system Reproductive system summary
Reproductive system summary Fornix of vagina
Fornix of vagina Layers of scrotum anatomy
Layers of scrotum anatomy Note on male reproductive system
Note on male reproductive system Where does meiosis occur? *
Where does meiosis occur? * Male reproductive system
Male reproductive system Similarities between male and female reproductive system
Similarities between male and female reproductive system Basic animal reproduction crossword
Basic animal reproduction crossword Unit 6 human development lesson 1 pregnancy
Unit 6 human development lesson 1 pregnancy Figure 16-5 is a sagittal view of the female
Figure 16-5 is a sagittal view of the female Male reproductive system side view
Male reproductive system side view Reproductive system
Reproductive system Figure 28-1 the male reproductive system
Figure 28-1 the male reproductive system Figure 16-2 is a longitudinal section of a testis
Figure 16-2 is a longitudinal section of a testis Masoderm
Masoderm Male reproductive system table
Male reproductive system table Primary spermatocyte
Primary spermatocyte Lesson 2 the male reproductive system
Lesson 2 the male reproductive system Male reproductive system
Male reproductive system What is reproductive system
What is reproductive system Prostatic utricle
Prostatic utricle Cylindrical pendant organ located anterior to the scrotum
Cylindrical pendant organ located anterior to the scrotum Male reproductive system
Male reproductive system Anatomy and physiology unit 7 cardiovascular system
Anatomy and physiology unit 7 cardiovascular system Respiration
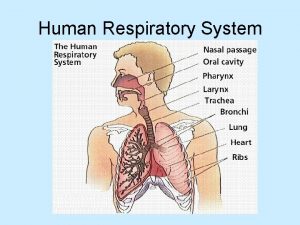
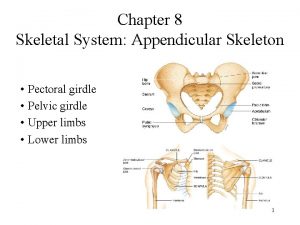
Respiration Appendicular skeleton pectoral girdle
Appendicular skeleton pectoral girdle Oviduct
Oviduct Gandotropin
Gandotropin Organ reproduksi laki-laki
Organ reproduksi laki-laki Male part of flower
Male part of flower Upper respiratory tract
Upper respiratory tract Tattoo anatomy and physiology
Tattoo anatomy and physiology International anatomy olympiad
International anatomy olympiad External parts of a leaf
External parts of a leaf Bone metabolism
Bone metabolism Pud
Pud Liver anatomy
Liver anatomy Epigastric region
Epigastric region Epigastric region
Epigastric region Anatomy and physiology blood
Anatomy and physiology blood Chapter 14 anatomy and physiology
Chapter 14 anatomy and physiology 3 layers of muscle
3 layers of muscle Http://anatomy and physiology
Http://anatomy and physiology