Recurrent Pregnancy Loss An Overview Dr Uma T


- Slides: 64
Recurrent Pregnancy Loss An Overview Dr Uma. T Department of Obstetrics and Gynecology SAT Hospital, Government Medical College Trivandrum
Recurrent miscarriages ≥ 3 consecutive losses before 20 weeks of gestation or less than 500 gms.
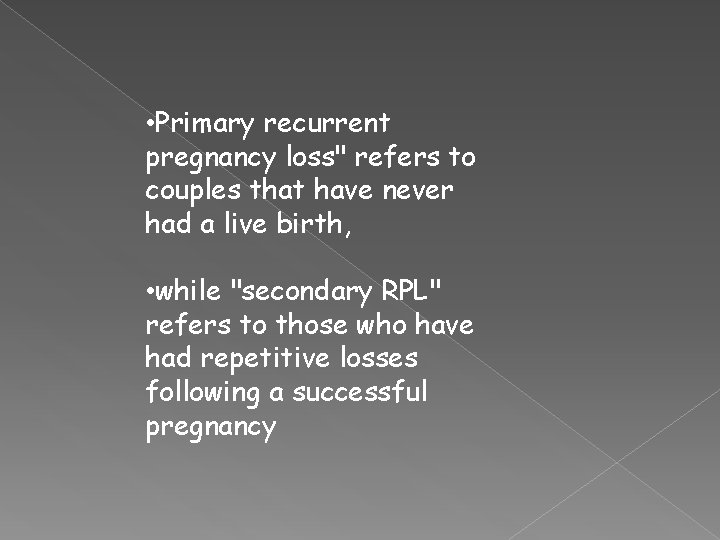
• Primary recurrent pregnancy loss" refers to couples that have never had a live birth, • while "secondary RPL" refers to those who have had repetitive losses following a successful pregnancy
Incidence • 1% of all pregnancies. • 10 -15 % clinically recognized pregnancy end in miscarriage ( RCOG )
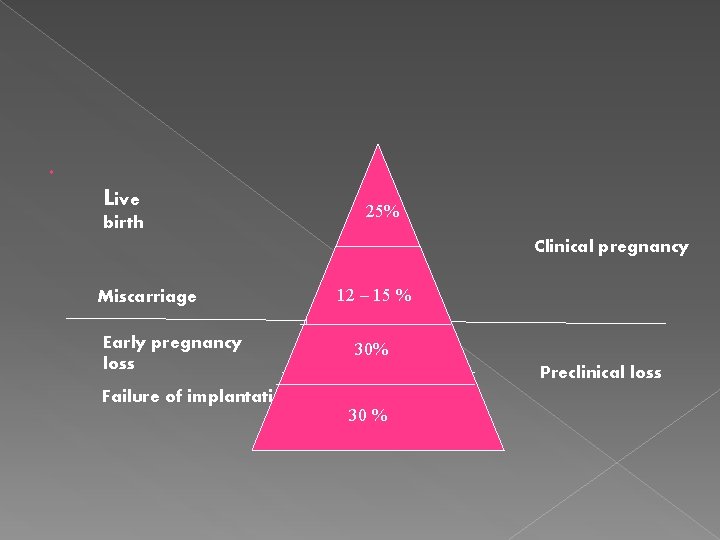
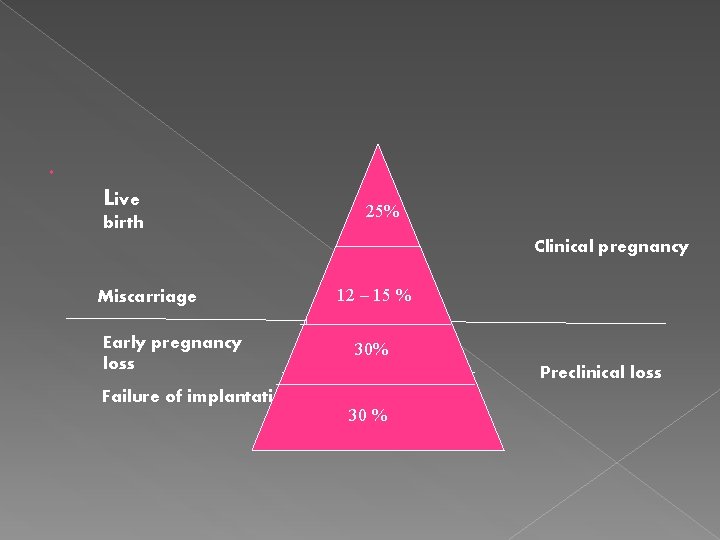
Live birth 25% 2% Miscarriage Early pregnancy loss Failure of implantation Clinical pregnancy 12 -15% 12 – 15 % 30% 30 % Preclinical loss
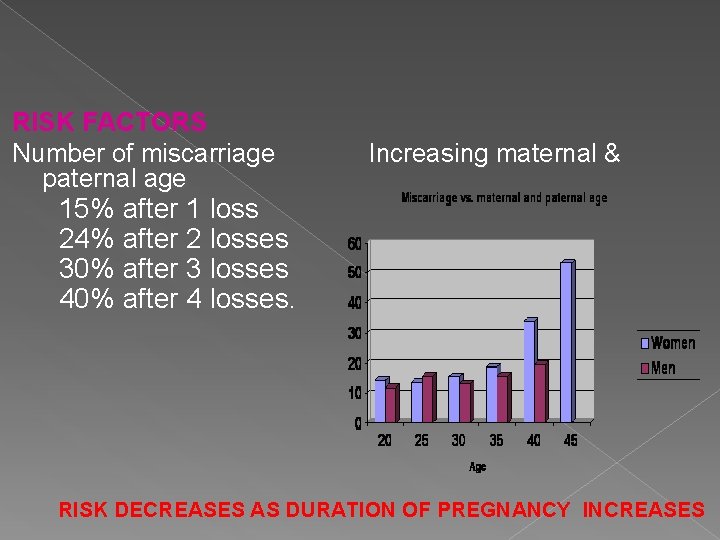
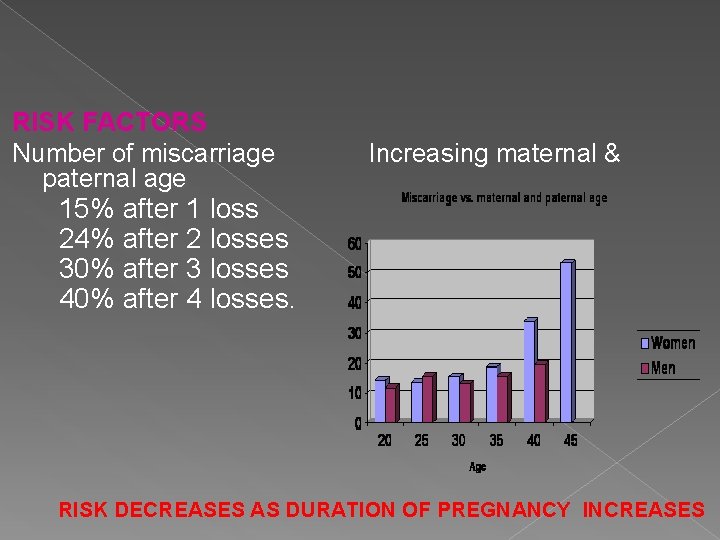
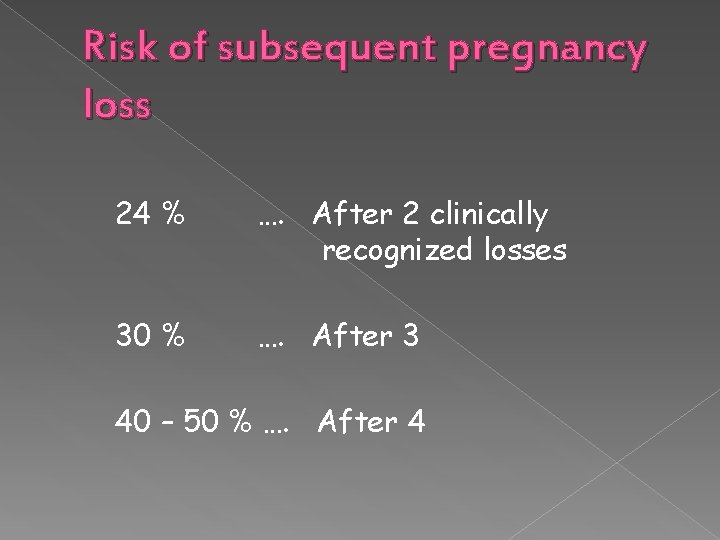
RISK FACTORS Number of miscarriage paternal age Increasing maternal & 15% after 1 loss 24% after 2 losses 30% after 3 losses 40% after 4 losses. RISK DECREASES AS DURATION OF PREGNANCY INCREASES
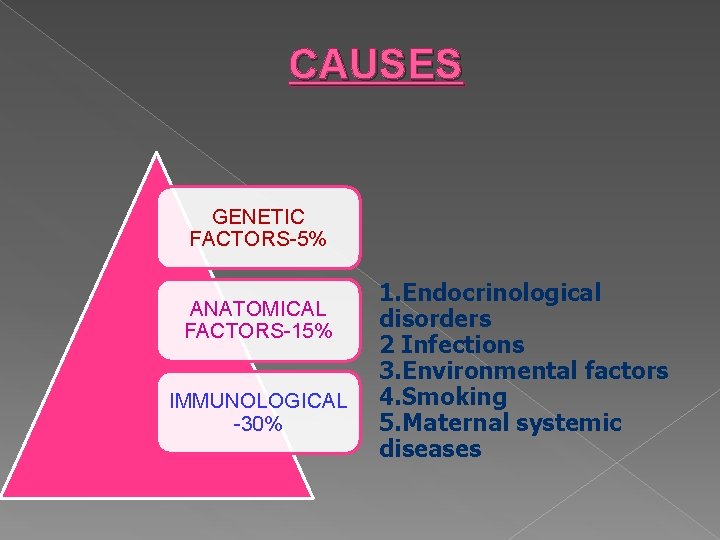
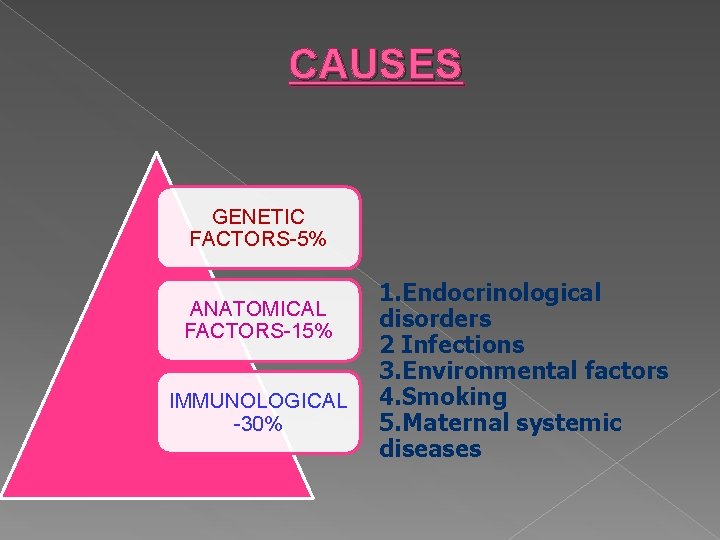
CAUSES GENETIC FACTORS-5% ANATOMICAL FACTORS-15% IMMUNOLOGICAL -30% 1. Endocrinological disorders 2 Infections 3. Environmental factors 4. Smoking 5. Maternal systemic diseases
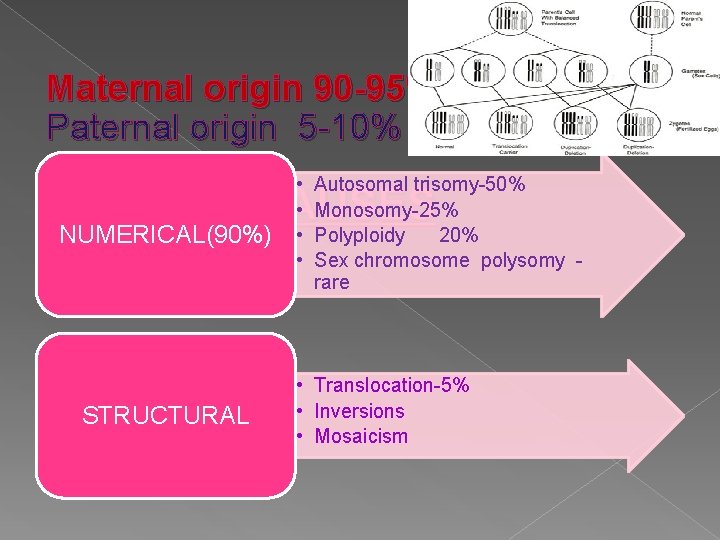
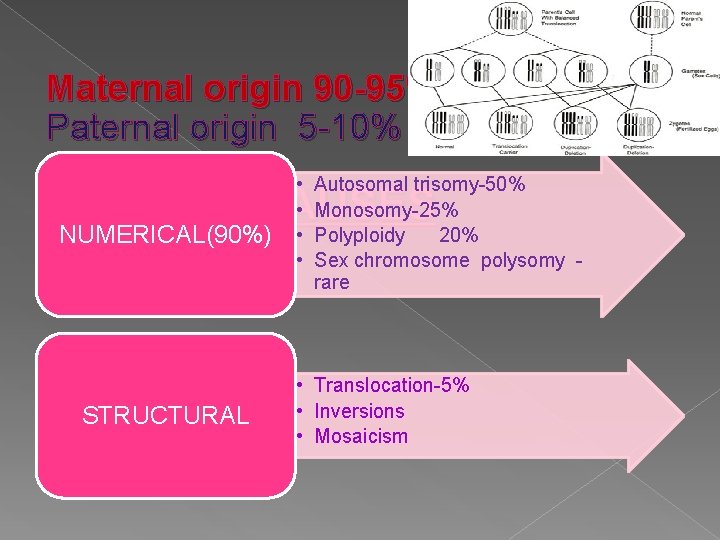
Maternal origin 90 -95% Paternal origin 5 -10% • • Autosomal trisomy-50% Monosomy-25% Polyploidy 20% Sex chromosome polysomy rare GENETIC CAUSES NUMERICAL(90%) STRUCTURAL • Translocation-5% • Inversions • Mosaicism
When to start investigating? no specific number or criteria that justifies evaluation for RPL or defines the scope of investigation Usually ……. ≥ 3 pregnancy losses
Investigate after 2 losses if ●Female partner > 35 yrs ●Infertility ●Foetal heart activity observed in any of the pregnancy losses ●Normal karyotype of conceptus
Risk of subsequent pregnancy loss 24 % …. After 2 clinically recognized losses 30 % …. After 3 40 – 50 % …. After 4
ETIOLOGY ? Only 2 undisputed causes ●Parental chromosomal abnormality ●APLA < 10 – 15 % of RPL
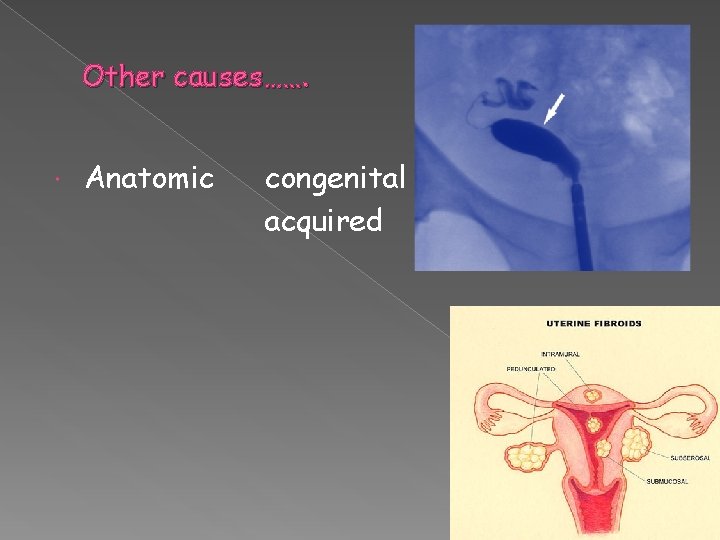
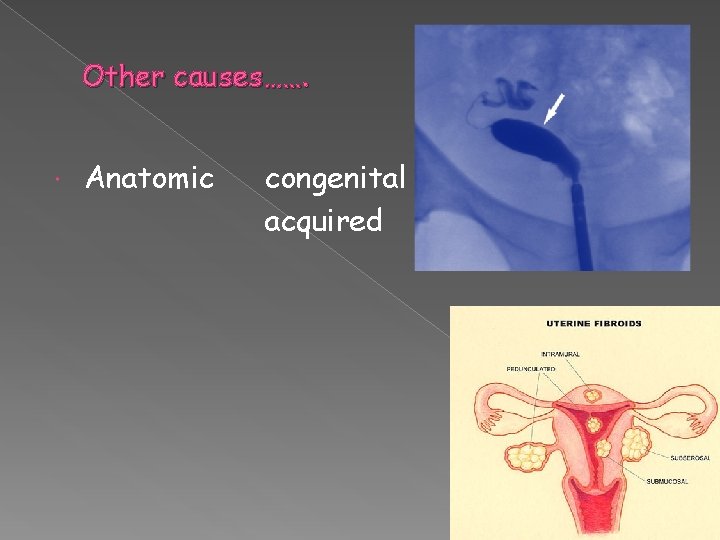
Other causes……. Anatomic congenital acquired
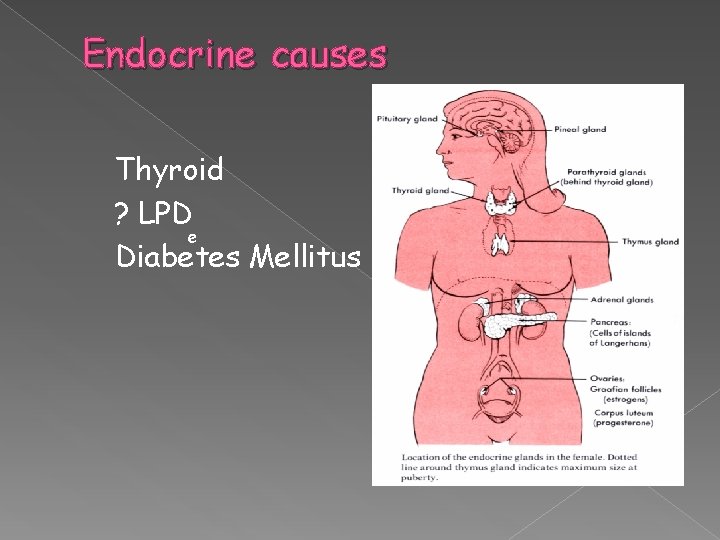
Endocrine causes Thyroid ? LPD e Diabetes Mellitus
Other causes……. Inherited thrombophilias Infections ? Bacterial vaginosis Environmental exposure Smoking / Alcohol / Caffeine
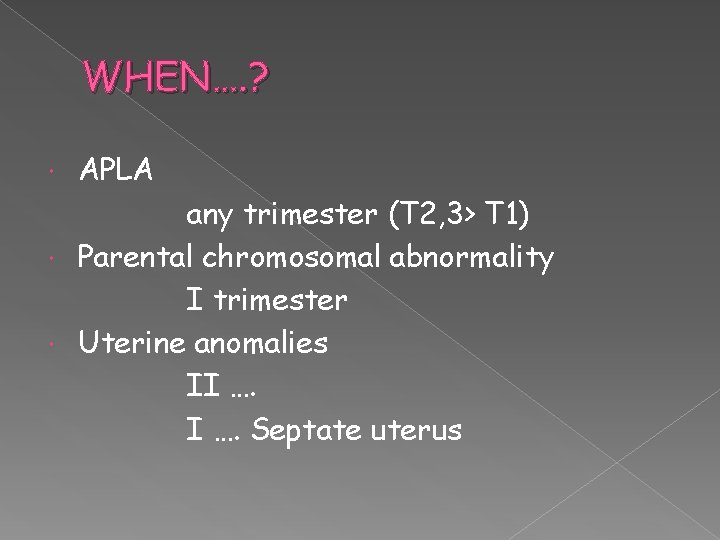
WHEN…. ? APLA any trimester (T 2, 3> T 1) Parental chromosomal abnormality I trimester Uterine anomalies II …. Septate uterus
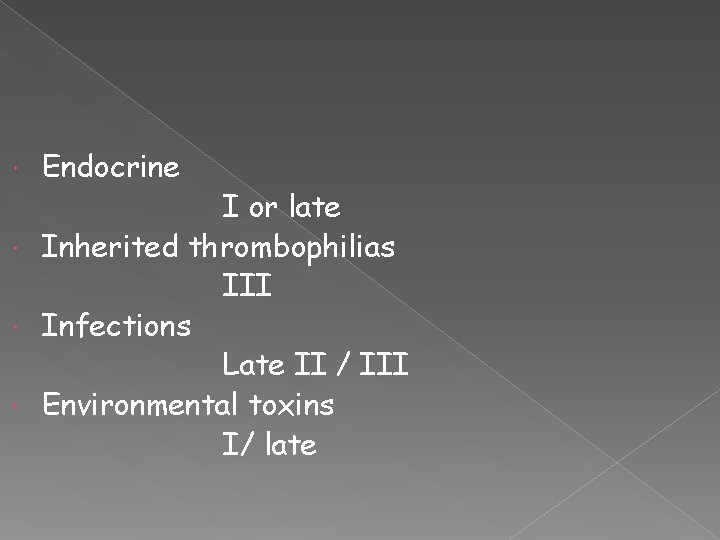
Endocrine I or late Inherited thrombophilias III Infections Late II / III Environmental toxins I/ late
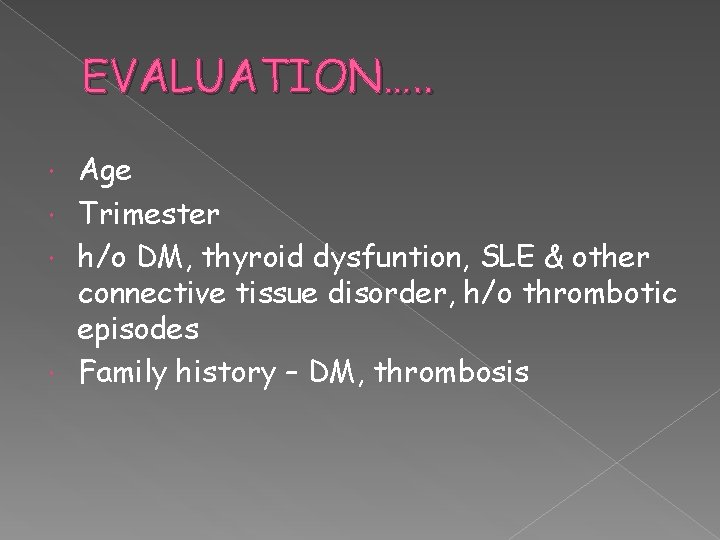
EVALUATION…. . Age Trimester h/o DM, thyroid dysfuntion, SLE & other connective tissue disorder, h/o thrombotic episodes Family history – DM, thrombosis
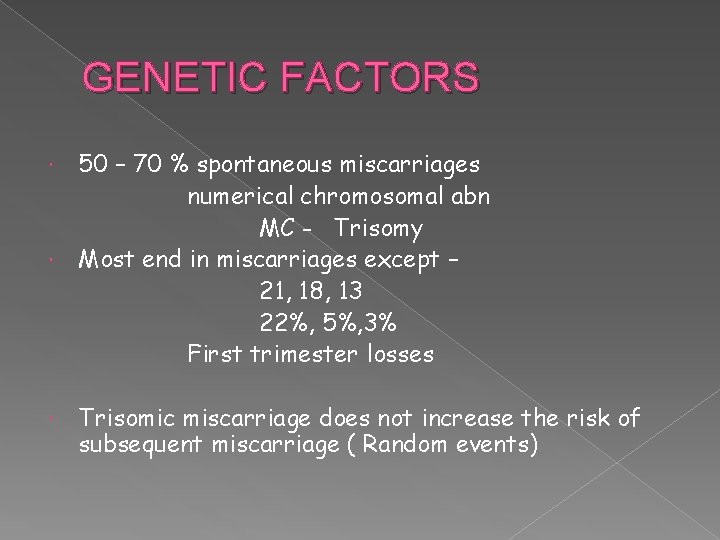
GENETIC FACTORS 50 – 70 % spontaneous miscarriages numerical chromosomal abn MC - Trisomy Most end in miscarriages except – 21, 18, 13 22%, 5%, 3% First trimester losses Trisomic miscarriage does not increase the risk of subsequent miscarriage ( Random events)
Structural genetic defects 3 – 5 % couples with RPL Most common. Balanced reciprocal or Robertsonian more frequent in female partner > 50% live birth rate Homologous – all pregnancies affected
peripheral blood karyotyping performed. Abnormal - Geneticist PGD – translocation carriers Disadvantage – IVF pregnancy success lower * without treatment > 50% live birth

Balanced Translocation carrier 14; 21
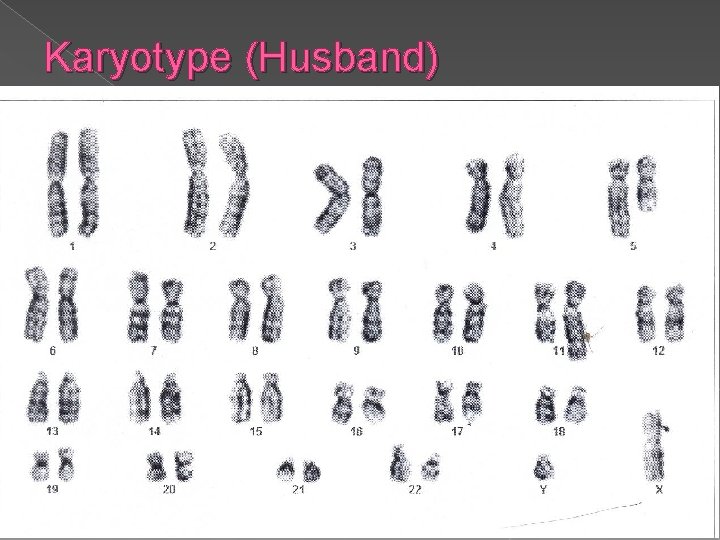
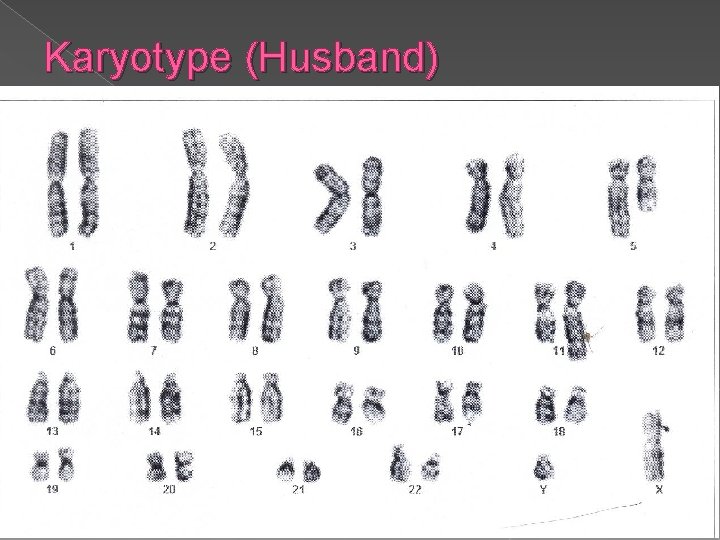
Karyotype (Husband)
Karyotyping of abortus? 2 schools of thought 1. Unnecessary & expensive luxury 2. Important to differentiate b/w those who need further evaluation from those who do not
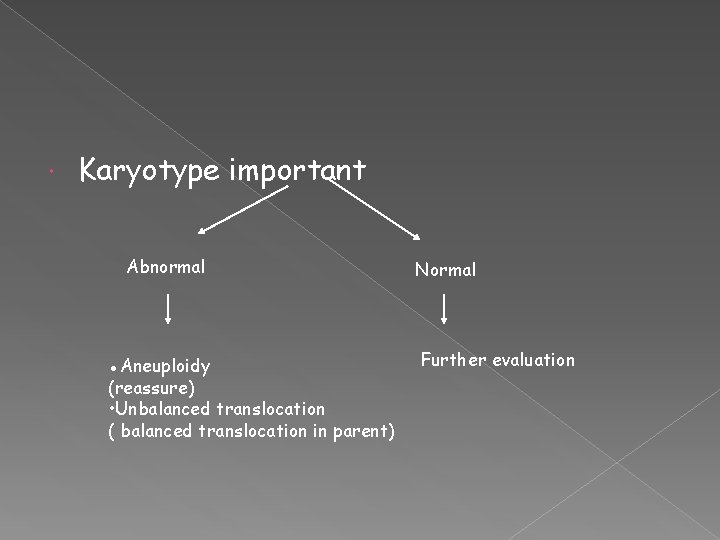
Karyotype important Abnormal ●Aneuploidy (reassure) • Unbalanced translocation ( balanced translocation in parent) Normal Further evaluation
APLA 15 % of women with RPL
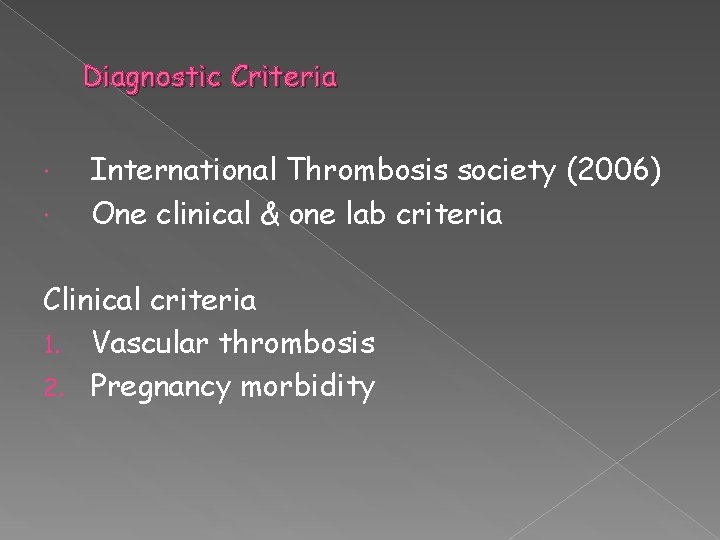
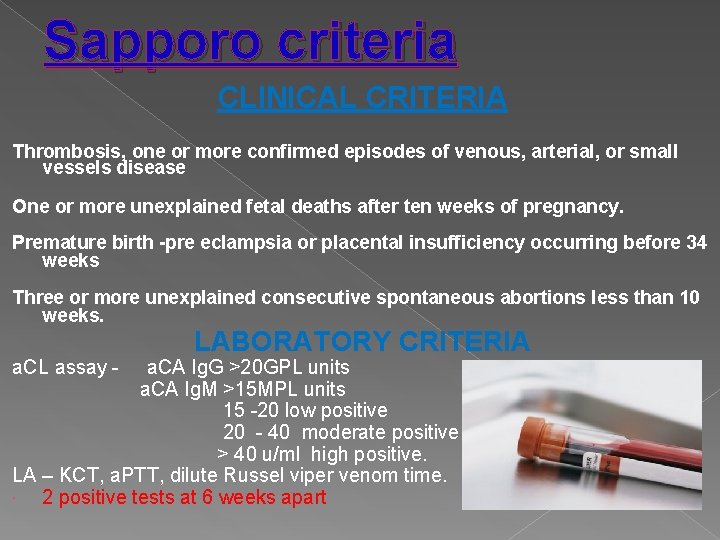
Diagnostic Criteria International Thrombosis society (2006) One clinical & one lab criteria Clinical criteria 1. Vascular thrombosis 2. Pregnancy morbidity
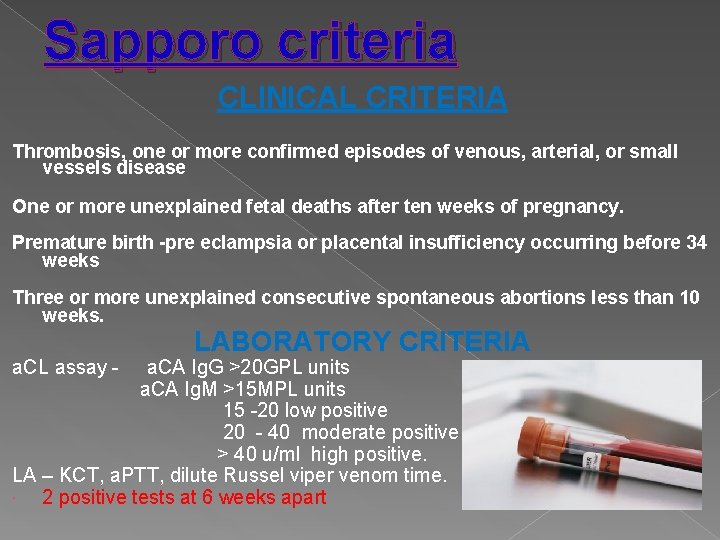
Sapporo criteria CLINICAL CRITERIA Thrombosis, one or more confirmed episodes of venous, arterial, or small vessels disease One or more unexplained fetal deaths after ten weeks of pregnancy. Premature birth -pre eclampsia or placental insufficiency occurring before 34 weeks Three or more unexplained consecutive spontaneous abortions less than 10 weeks. a. CL assay - LABORATORY CRITERIA a. CA Ig. G >20 GPL units a. CA Ig. M >15 MPL units 15 -20 low positive 20 - 40 moderate positive > 40 u/ml high positive. LA – KCT, a. PTT, dilute Russel viper venom time. 2 positive tests at 6 weeks apart
1. Vascular thrombosis arterial venous small vessel
2. Pregnancy morbidity ●≥ 1 unexplained deaths of a morpholgically normal fetus at or beyond 10 weeks of gest with normal fetal morphology- USS/direct exam ≥ 1 premature births of a morphologically normal neonate before 34 weeks of gestation - eclampsia or preeclampsia/ features of placental insufficiency ≥ 3 unexplained consecutive spontaneous abortions before 10 weeks of gestation with maternal anatomic or hormonal abnormalities & paternal & maternal chromosomal causes to be excluded.
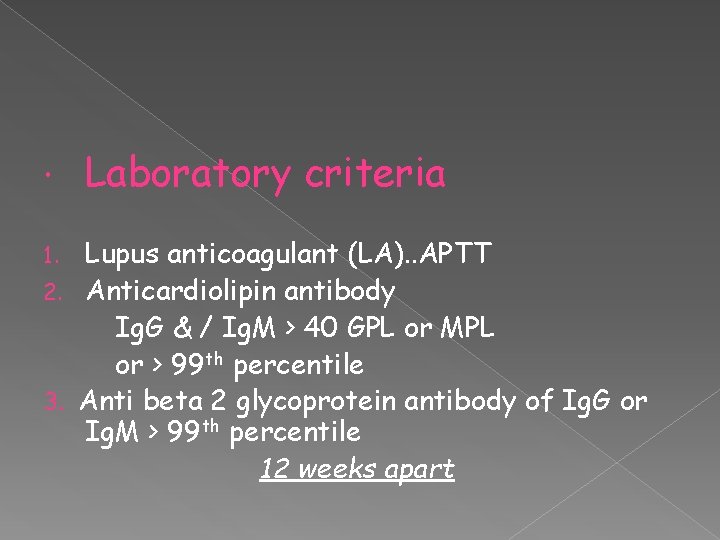
Laboratory criteria Lupus anticoagulant (LA). . APTT 2. Anticardiolipin antibody Ig. G & / Ig. M > 40 GPL or MPL or > 99 th percentile 3. Anti beta 2 glycoprotein antibody of Ig. G or Ig. M > 99 th percentile 12 weeks apart 1.
Without treatment…. chance of a live pregnancy only 10% Treatment…. Aspirin & Heparin
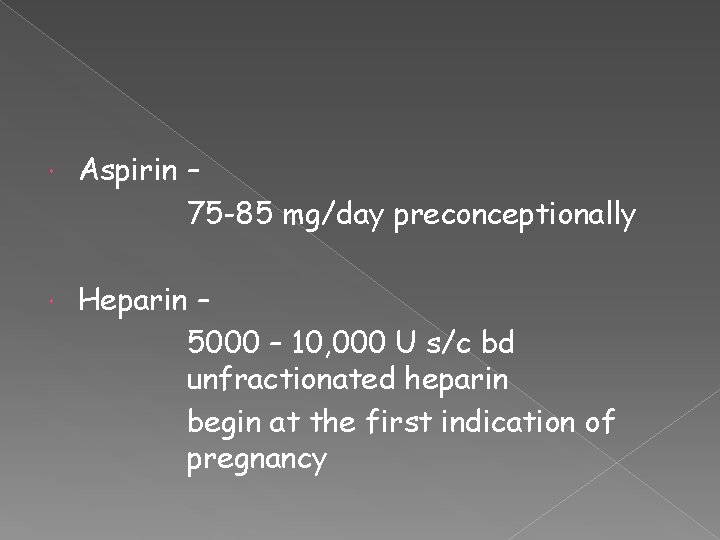
Aspirin – 75 -85 mg/day preconceptionally Heparin – 5000 – 10, 000 U s/c bd unfractionated heparin begin at the first indication of pregnancy
Monitor platelet count No increased risk of osteoporosis
Low molecular weight heparin equally beneficial Once daily administration Enoxaparine (clexane) – 1 mg/kg Dalteparine (fragmin )- 100 U/kg
Stop aspirin by 34 weeks Planned delivery stop unfractionated heparin 6 hrs before delivery LMW Heparin – 12 hrs
Post natal thromboprophylaxis Reintroduce following delivery Unfractionated – 6 hrs LMW Heparin - 12 hrs
Aspirin + Heparin …. 70 % live birth rate Aspirin alone …. 40 % only
INHERITED THROMBOPHILIAS Activated protein C Resist( Factor V Leiden gene mutation ) Deficiency of protein C/S Deficiency of antithrombin III Hyperhomocysteinemia PT gene mutation
established causes of systemic thrombosis Pregnancy – data scarce due to low prevelance Thrombophilia screen
Treatment of women with Inherited/acquired thrombophilias Unfractionated / LMW Heparin Therapeutic / Prophylactic dose Monitor a. PTT
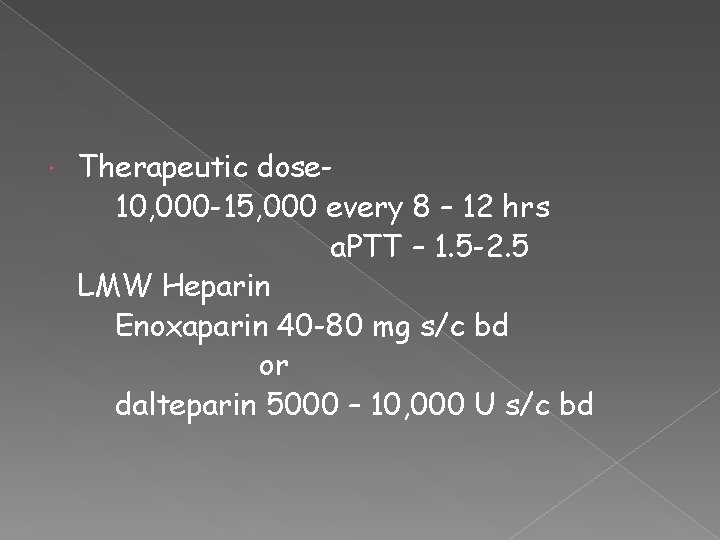
Therapeutic dose 10, 000 -15, 000 every 8 – 12 hrs a. PTT – 1. 5 -2. 5 LMW Heparin Enoxaparin 40 -80 mg s/c bd or dalteparin 5000 – 10, 000 U s/c bd
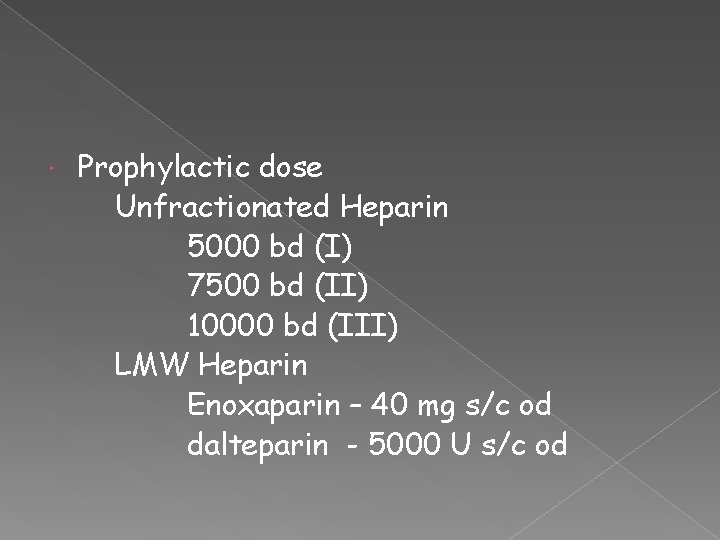
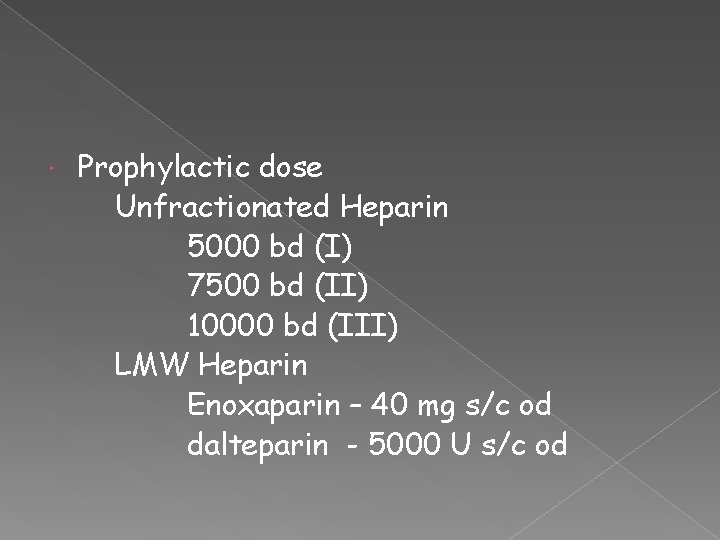
Prophylactic dose Unfractionated Heparin 5000 bd (I) 7500 bd (II) 10000 bd (III) LMW Heparin Enoxaparin – 40 mg s/c od dalteparin - 5000 U s/c od
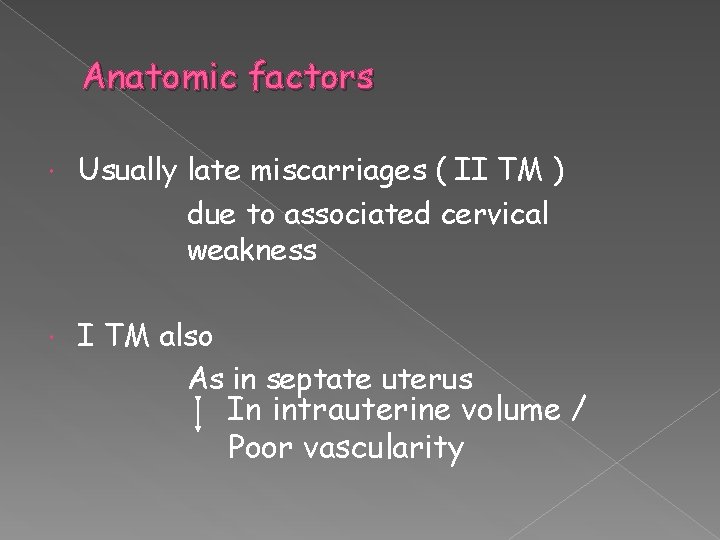
Anatomic factors Usually late miscarriages ( II TM ) due to associated cervical weakness I TM also As in septate uterus In intrauterine volume / Poor vascularity
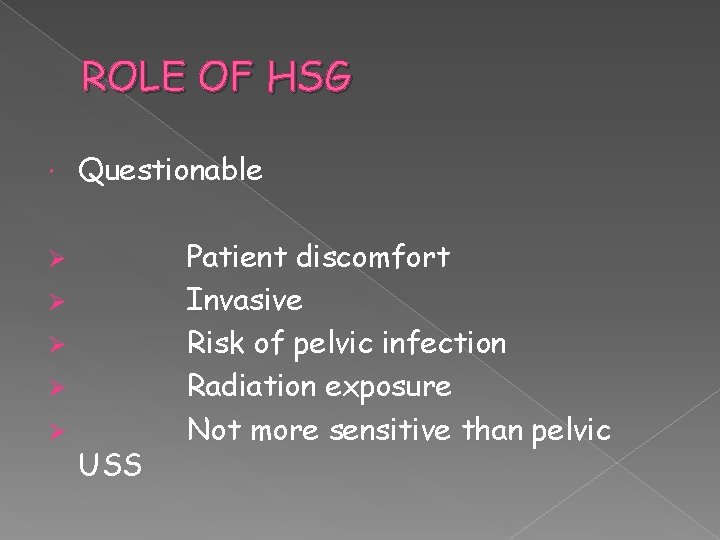
ROLE OF HSG Questionable Ø Ø Ø USS Patient discomfort Invasive Risk of pelvic infection Radiation exposure Not more sensitive than pelvic
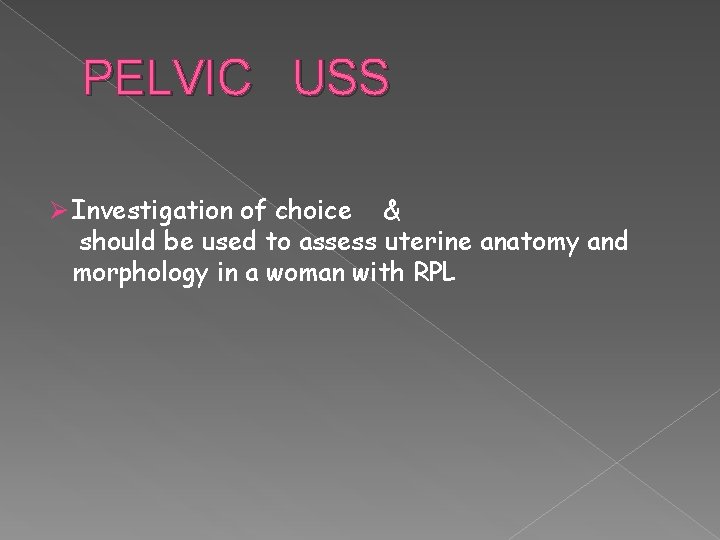
PELVIC USS Ø Investigation of choice & should be used to assess uterine anatomy and morphology in a woman with RPL
Role of encerclage? QUESTIONABLE ! Definite history – should be done suspicion – monitor with serial USS
Hysteroscopic septal resection Septate uterus with RPL Didelphis / Bicornuate no correction Asherman Syndrome hysteroscopic lysis
Uterine leiomyomas * submucous * large intramural - remove only if compressing cavity
ENDOCRINE CAUSES Well controlled DM and thyroid is not a risk factor for RPL Routine screening for occult thyroid and DM ? Uninformative (RCOG)
Progesterone supplementation Insufficient evidence in RPL Preterm labour IVF pregnancies
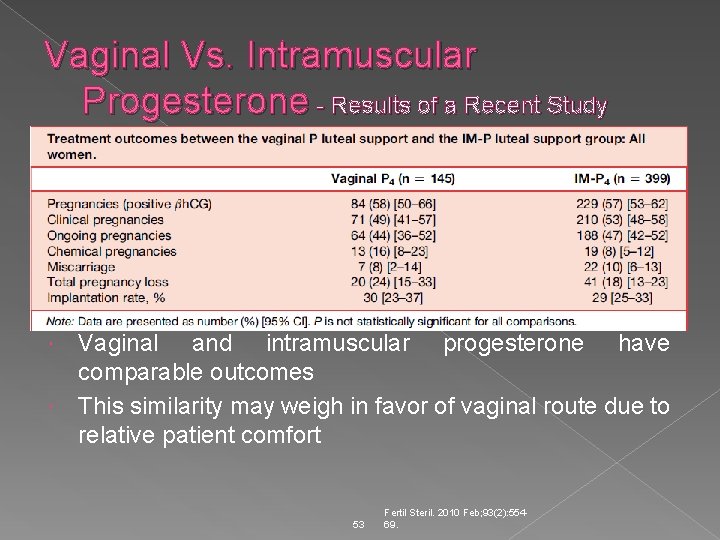
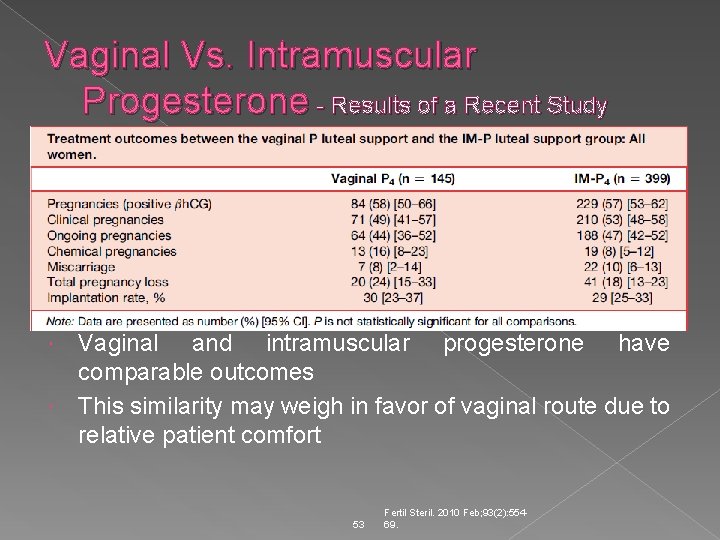
Vaginal Vs. Intramuscular Progesterone - Results of a Recent Study Vaginal and intramuscular progesterone have comparable outcomes This similarity may weigh in favor of vaginal route due to relative patient comfort 53 Fertil Steril. 2010 Feb; 93(2): 55469.
? h. CG failed to show any benefit not given
… PCOS … role for prepregnancy LH suppression? NO role as it does not improve the live birth rate
Prolactin levels? Insufficient evidence
? Role of immunotherapy Paternal cell immunisation 3 rd party donor leucocyte Trophoblast membranes IVIg Not recommended Does not improve the live birth rate
TORCH screening To be abandoned
Bacterial vaginosis I TM loss- evidence inconsistent For women with a previous history of preterm birth- detection & treatment of bacterial vaginosis………. Prevents further preterm birth
ENVIRONMENTAL FACTORS Smoking Alcohol Caffeine
UNEXPLAINED RPL ? Role for empirical Heparin , Aspirin Resisted (RCOG)
In unexplained pregnancy loss , the woman should be reassured that with supportive care alone, the chance for a successful pregnancy outcome is 75%
What these women need ? ? ? Psychological support & reassurance Tender loving care

Thank you……. .