Neurological complications of acute ischemic stroke Neurology R

- Slides: 35
Neurological complications of acute ischemic stroke Neurology R 5 林念穎 2012/03/22
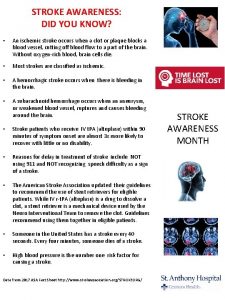
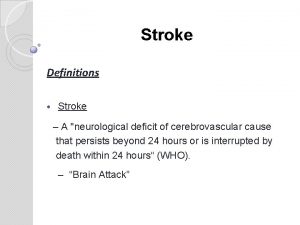
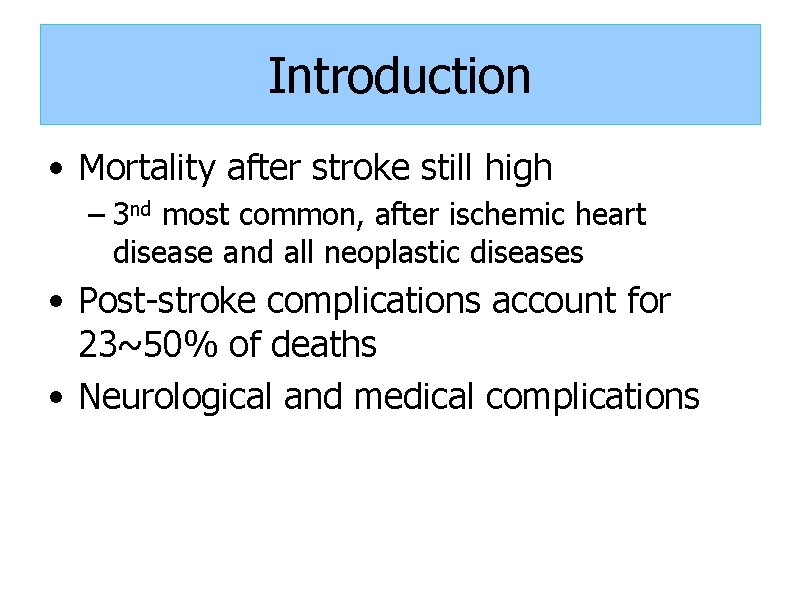
Introduction • Mortality after stroke still high – 3 nd most common, after ischemic heart disease and all neoplastic diseases • Post-stroke complications account for 23~50% of deaths • Neurological and medical complications
Introduction • Neurological complications (1) brain edema (2) haemorrhagic transformation (3) seizures and epilepsy (4) recurrent stroke (5) sleep disorders & sleep-disordered breathing…etc. • Less frequent than medical complications, but occur earlier – Within 48~72 hours of stroke onset
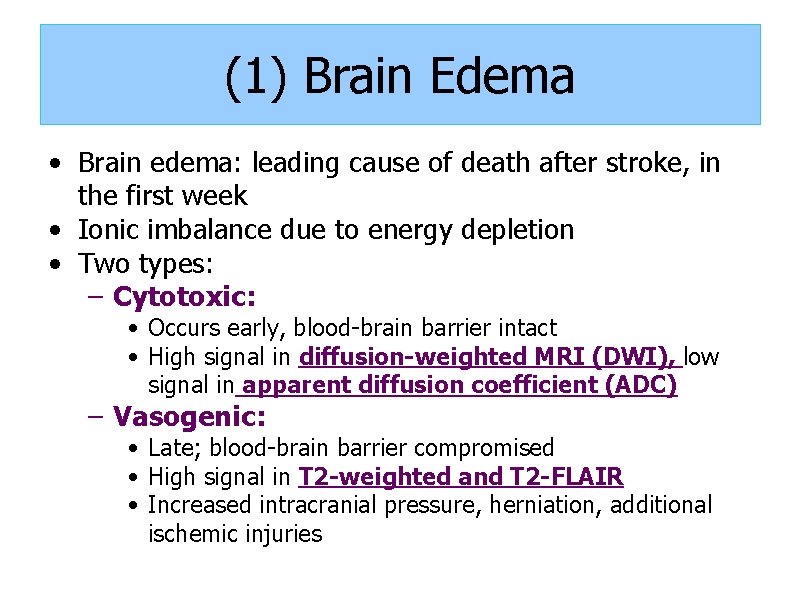
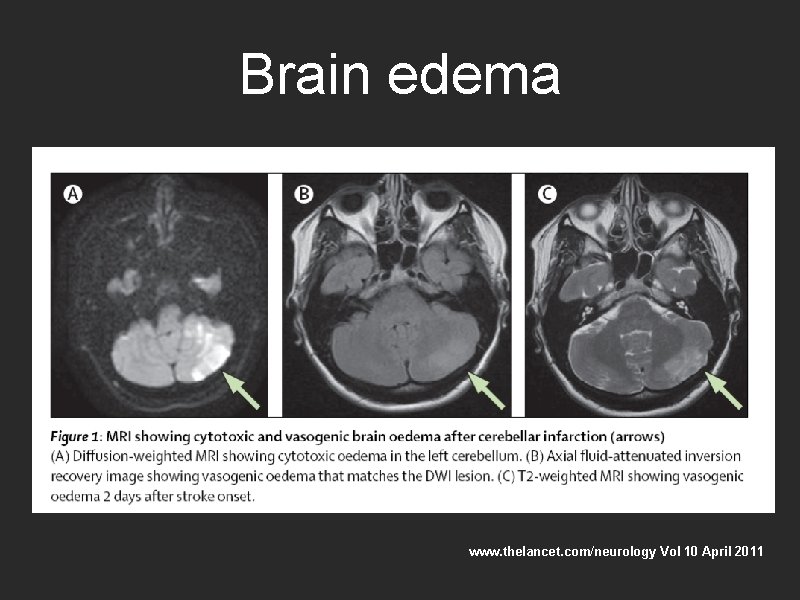
(1) Brain Edema • Brain edema: leading cause of death after stroke, in the first week • Ionic imbalance due to energy depletion • Two types: – Cytotoxic: • Occurs early, blood-brain barrier intact • High signal in diffusion-weighted MRI (DWI), low signal in apparent diffusion coefficient (ADC) – Vasogenic: • Late; blood-brain barrier compromised • High signal in T 2 -weighted and T 2 -FLAIR • Increased intracranial pressure, herniation, additional ischemic injuries
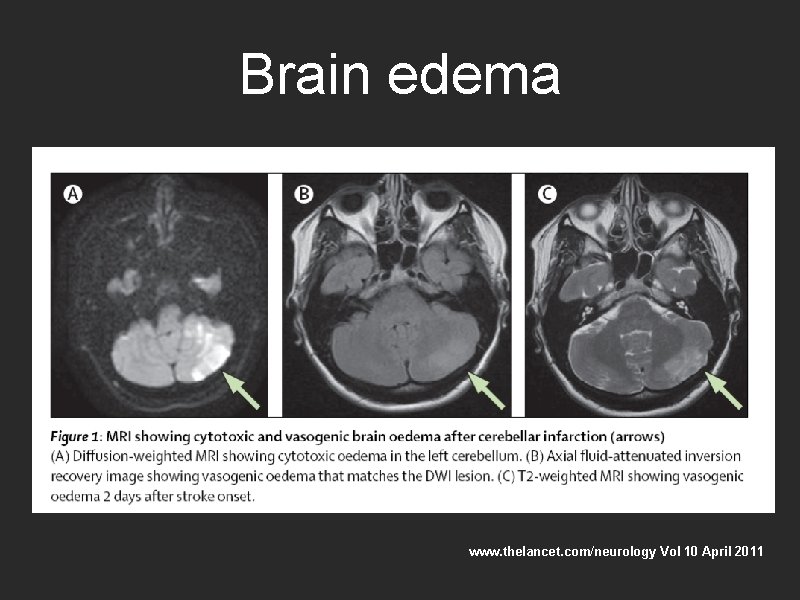
Brain edema www. thelancet. com/neurology Vol 10 April 2011
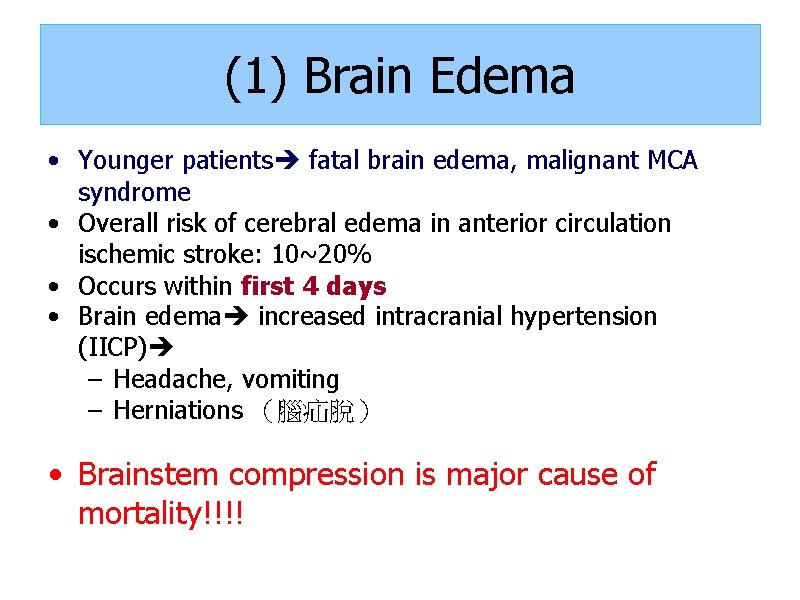
(1) Brain Edema • Younger patients fatal brain edema, malignant MCA syndrome • Overall risk of cerebral edema in anterior circulation ischemic stroke: 10~20% • Occurs within first 4 days • Brain edema increased intracranial hypertension (IICP) – Headache, vomiting – Herniations (腦疝脫) • Brainstem compression is major cause of mortality!!!!
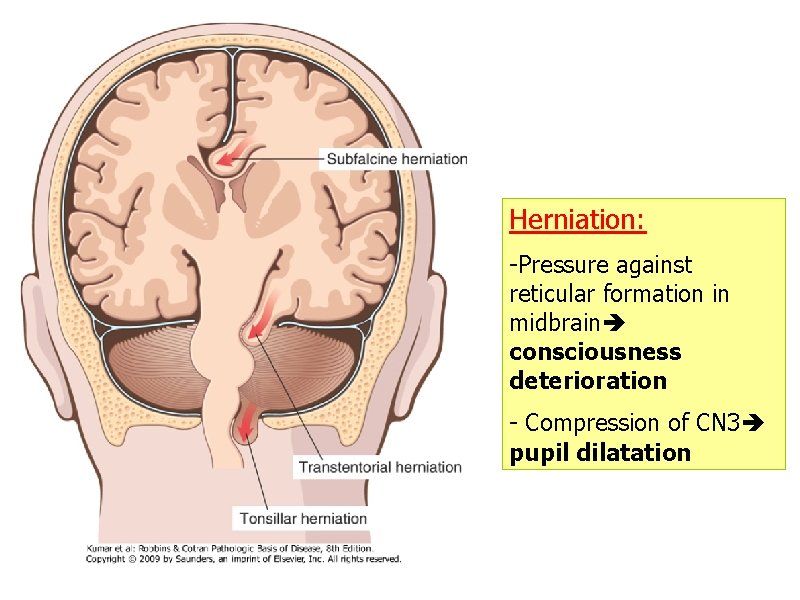
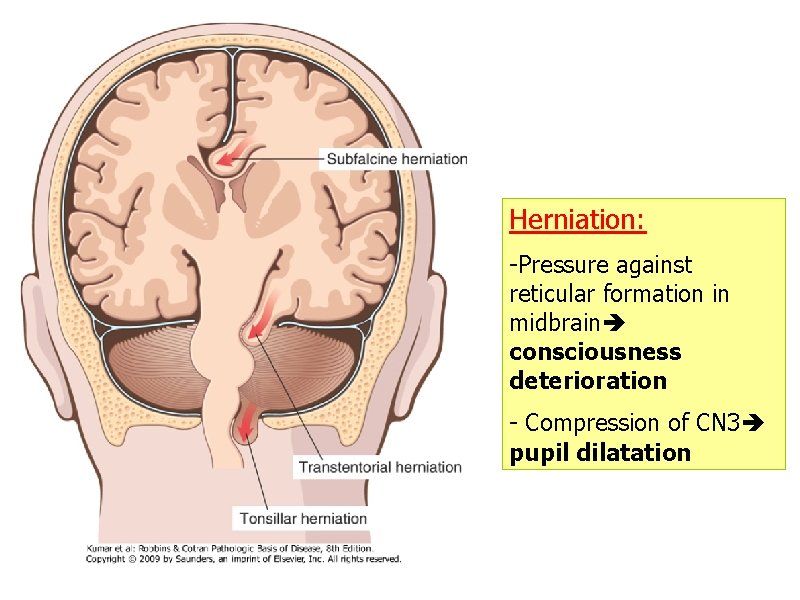
Herniation: -Pressure against reticular formation in midbrain consciousness deterioration - Compression of CN 3 pupil dilatation
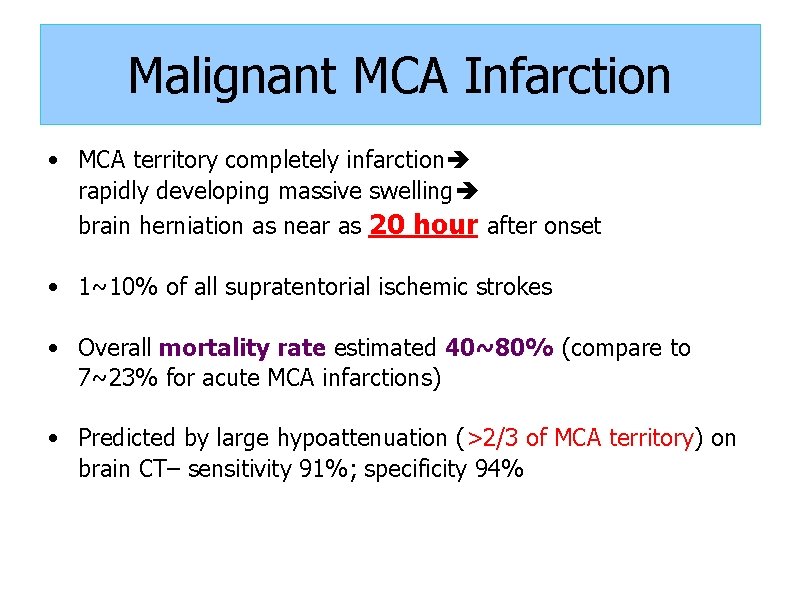
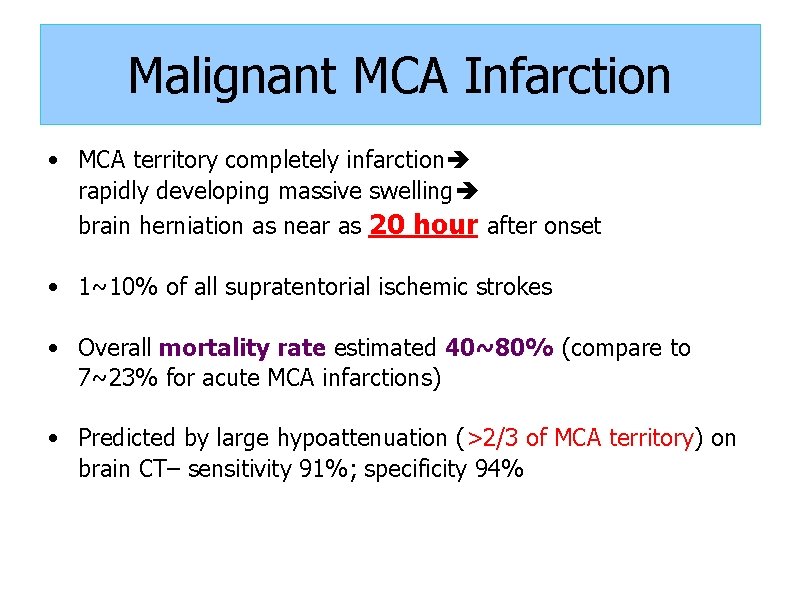
Malignant MCA Infarction • MCA territory completely infarction rapidly developing massive swelling brain herniation as near as 20 hour after onset • 1~10% of all supratentorial ischemic strokes • Overall mortality rate estimated 40~80% (compare to 7~23% for acute MCA infarctions) • Predicted by large hypoattenuation (>2/3 of MCA territory) on brain CT– sensitivity 91%; specificity 94%
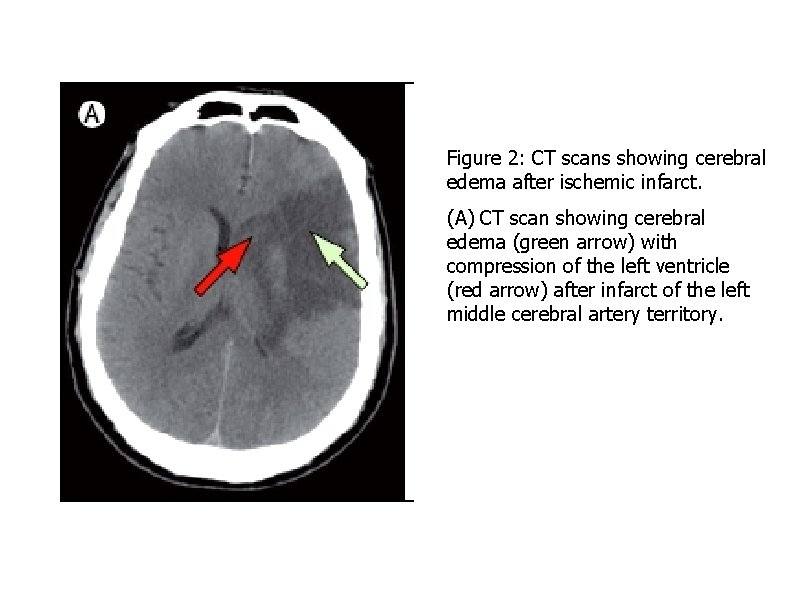
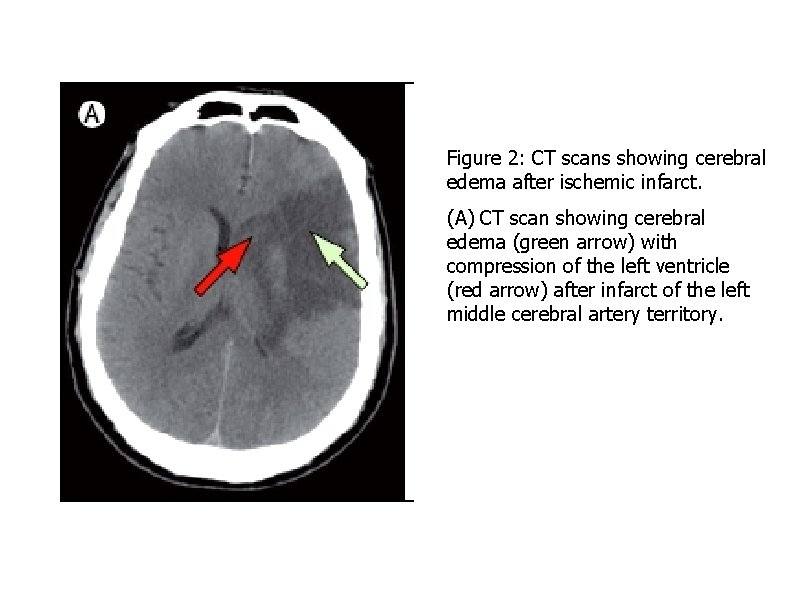
Figure 2: CT scans showing cerebral edema after ischemic infarct. (A) CT scan showing cerebral edema (green arrow) with compression of the left ventricle (red arrow) after infarct of the left middle cerebral artery territory.
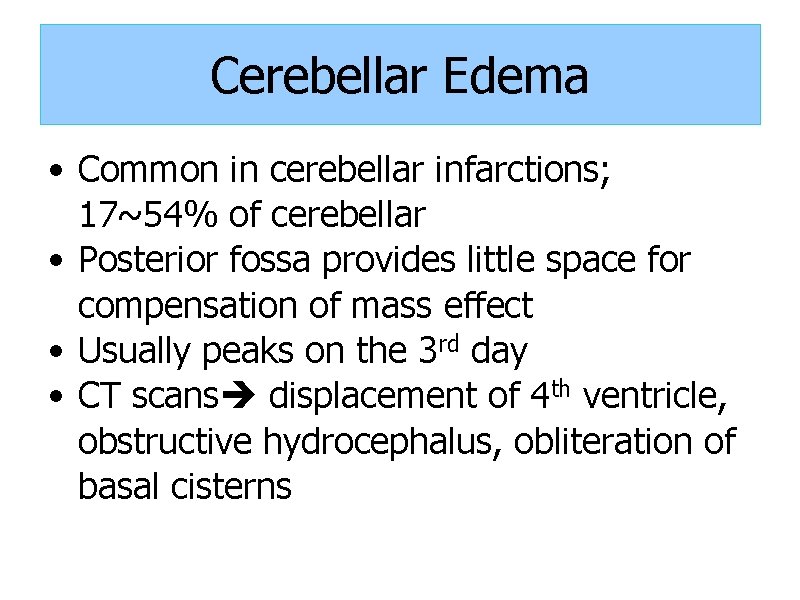
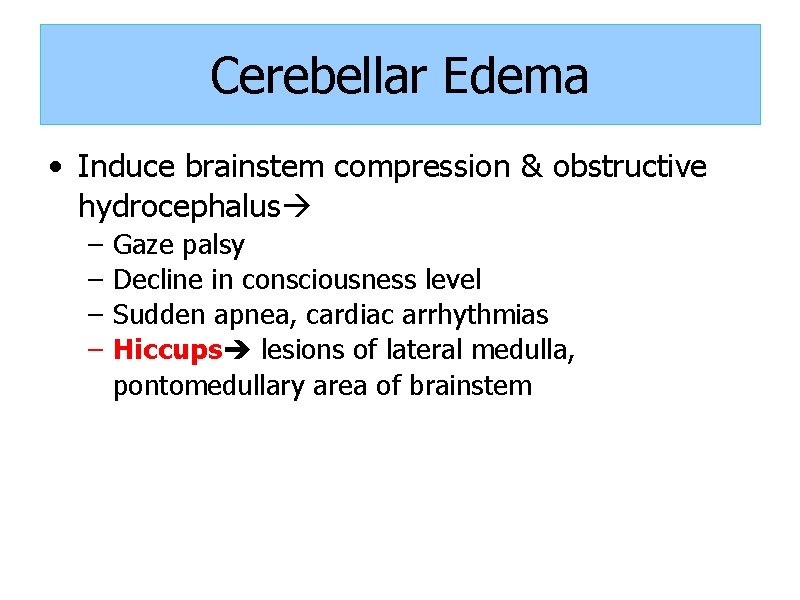
Cerebellar Edema • Common in cerebellar infarctions; 17~54% of cerebellar • Posterior fossa provides little space for compensation of mass effect • Usually peaks on the 3 rd day • CT scans displacement of 4 th ventricle, obstructive hydrocephalus, obliteration of basal cisterns
Cerebellar Edema • Induce brainstem compression & obstructive hydrocephalus – – Gaze palsy Decline in consciousness level Sudden apnea, cardiac arrhythmias Hiccups lesions of lateral medulla, pontomedullary area of brainstem
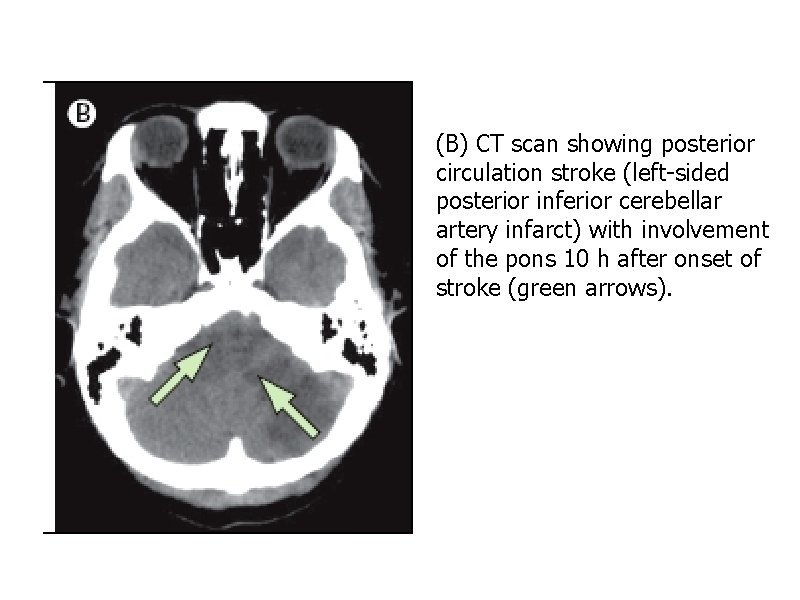
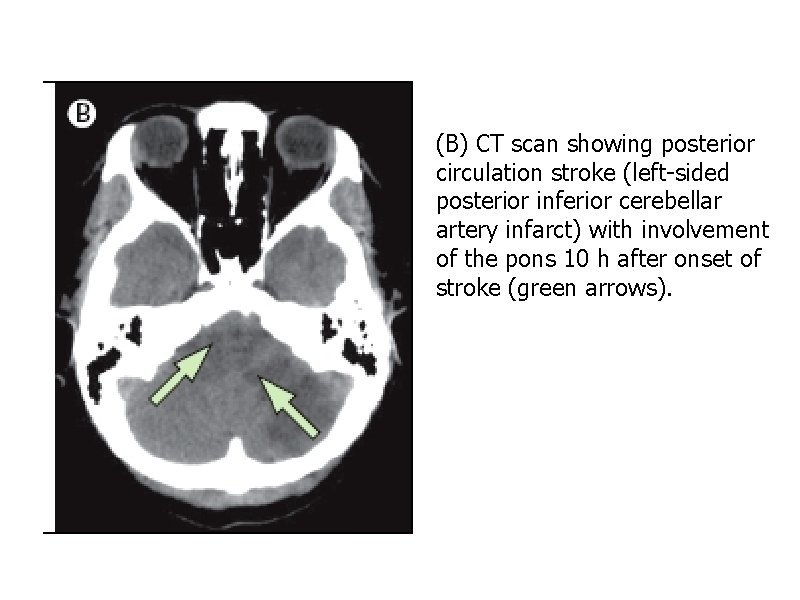
(B) CT scan showing posterior circulation stroke (left-sided posterior inferior cerebellar artery infarct) with involvement of the pons 10 h after onset of stroke (green arrows).
(1) Brain Edema • Treatment- medical – General: close monitor for neurological worsening – Osmotherapy: • Glycerol, mannitol, hyperosmolar saline solutions, corticosteroids, barbiturates; unproven (level 3 C) • May be harmfal in CVST – Hypothermia (32~35℃): • in small RCT (n=25), in addition to decompressive surgery led to better outcome than surgery alone (level 3 C)
(1) Brain Edema • Surgical – Decompressive surgery • Early decompressive hemicraniectomy (<48 hr) improves survival and functional outcome in patients (aged < 60 years) with malignant cerebral artery infarction (level 1 B) • Suboccipital decompressive craniectomy-- recommended as therapy of choice in malignant cerebellar infarction (level 1 B) – External ventricular drainage (EVD)– • for patients with worsening levels of consciousness and obstructive hydrocephalus secondary to cerebellar infarction
(2) Hemorrhagic Transformation • Common; 30~40% of acute ischemic stroke – Symptomatic: • 0. 6% in those with supportive care – Aspirin: small increase in bleeding risk, but nonsignificant • 6% of intravenous alteplase • 7% of intra-arterial fibrinolytics and mechanical embolectomy
(2) Hemorrhagic Transformation • Risk factors of thrombolysis-related ICH – Old age (>65 y/o): • impaired rate of alteplase clearance, high frequency of cardioembolic stroke, age-associated microangiopathy (cerebral amyloid angiopathy or hypertensive microangiopathy) – Larger infarct size mass effect on pre-treatment imaging – High baseline systolic blood pressure – Congestive heart failure – High glucose concentrations/diabetes mellitus • Expands brain edema, increase ICP higher mortality
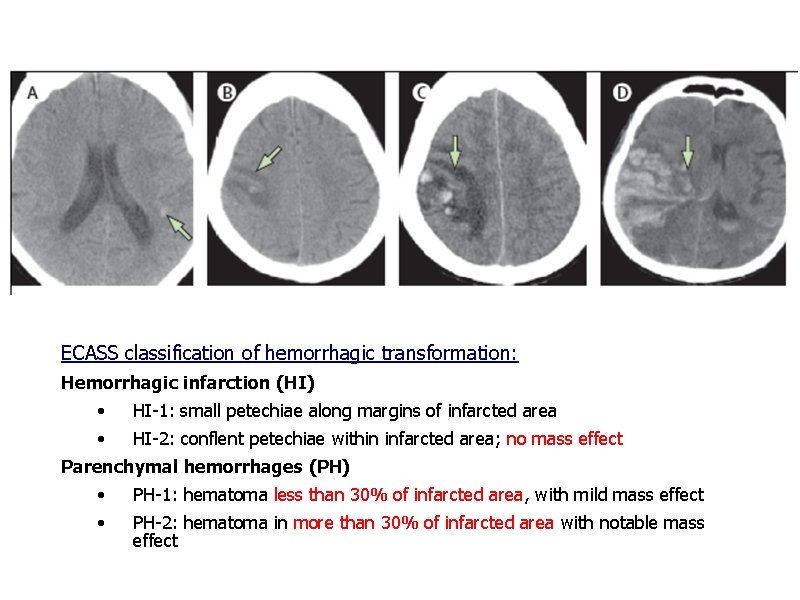
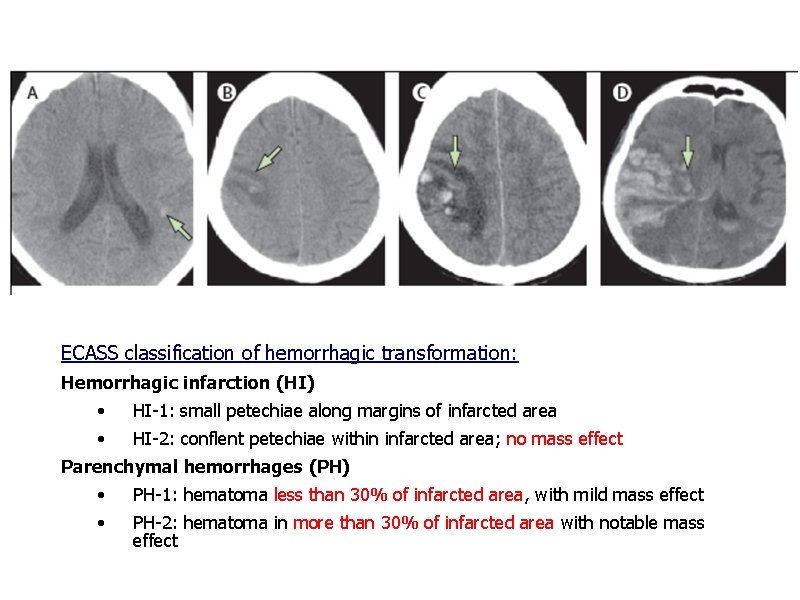
Haemorrhagic transformation ECASS classification of hemorrhagic transformation: Hemorrhagic infarction (HI) • HI-1: small petechiae along margins of infarcted area • HI-2: conflent petechiae within infarcted area; no mass effect Parenchymal hemorrhages (PH) • PH-1: hematoma less than 30% of infarcted area, with mild mass effect • PH-2: hematoma in more than 30% of infarcted area with notable mass effect www. thelancet. com/neurology Vol 10 April 2011
(2) Hemorrhagic Transformation • No intervention to reduce risk of hemorrhagic transformation • Careful selection of suitable patients for thrombolytic therapy • Antithrombotics not recommended for use in first 24 hrs after thrombolytic treatment • Management – Asymptomatic: no specific intervention – Symptomatic • Medical • Surgical
(2) Hemorrhagic Transformation • Medical: – Stop anti-thrombotic medication – Secondary to thrombolytic therapy platelet and cryoprecipitate infusion to correct systemic fibrinolytic state created by alteplase (level 2 BC) – Intravenous vitamin K to reverse effects of warfarin (level 1 B) • Surgical: – Supratentorial: lobar clots >30 m. L and within 1 cm of surface (level 2 B) – Cerebellar hemorrhage > 3 cm (level 1 B)
(2) Hemorrhagic Transformation • Management – Antithrombotic therapy after hemorrhagic transformation • Depends on risk of subsequent arterial or venous thromboembolism, risk of recurrent intracerebral hemorrhage and clinical state of patient • Antiplatelet: – safer choice than warfarin for patients with lower risk of cerebral infarction (eg non-valvular Af), but with higher risk of rebleeding (eg elderly with lobar ICH, possible amyloid angiopathy) • Warfarin: – In patients with high risk of thromboembolism (Level 2 B) – Can be restarted 7~10 days after onset of ICH
(3) Seizure • Early seizures: within 1~2 weeks – Frequency: 2~23% – Cellular biochemical dysfunction electrically excitable tissue – Recurrence rate 16% • Delayed: > 2 weeks – Frequency: 3%~67% – Mechanism: gliosis, meningocerebral cicatrices (scar) – Recurrence rate more than 50% • Prognosis: – Recurrent seizure in post-stroke seizures increase disability, vascular cognitive impairment
(3) Seizure • Risk factors: – Venous sinus thrombosis (more than arterial stroke) • In one study, 40% CVST had seizure at presentation, additional 7% within 2 weeks of diagnosis – Large cortical infarcts, multiple infarcts, embolic stroke, hemodynamic and metabolic disturbances
(3) Seizure • Management – No clear guideline for when to initiate anticonvulsant therapy, choice of therapy, or for duration of therapy – Prophylactic use not recommended – Early seizures short-term AED for 3~6 months – Late seizures require long-term treatment
(4) Recurrent Stroke • Risk of early stroke recurrence: 10% at 1 week, 2~4% at 1 month, 5% yearly thereafter • Major risk factors of recurrence: – – – – Old age, previous stroke, diabetes, hypertension, atrial fibrillation, cardiac diseases, smoking, carotid/vertebrobasilar stenosis (large artery atherosclerosis)
(4) Recurrent Stroke • Management – Antiplatelet therapy • First line for non-cardioembolic ischemic stroke or TIA (level 1 A) – Anticoagulation for atrial fibrillation • 68% RRR with warfarin vs 19% with aspirin (level 1 A) – Carotid endarterectomy and endovascular interventions • Early carotid endarterectomy (first 2 weeks) more beneficial (level 1 A) • Carotid angioplasty reserved for those contraindicated to carotid endarterectomy (level 2 B)
(4) Recurrent Stroke – Treatment of hypertension • Controversial – Reduction of elevated cholesterol (level 1 A) – Blood sugar control • Hyperglycemia (> 140 mg/d. L) insulin therapy in acute ischemic stroke (level 2 C)
(5) Sleep disorders • Frequent in initial stages after stroke – 10~50% of stroke patients – Hypersomnia (increased sleep need), excessive daytime sleepiness, insomnia • Bilateral paramedian thalamus, brainstem, large hemispheric stroke with mass effect • Associated with depression, anxiety, sleep-disordered breathing, drugs, post-stroke pain, medical complications (UTI, respiratory infections, nocturia), environmental factors (noise, light)
(5) Sleep-disordered Breathing • Obstructive apnea – Most common form, over 50% of patients – Share same risk factors as stroke: age, obesity, hypertension – Collapse of upper airway – Treat with continuous positive airway pressure breathing • Central apnea= Ondine’s curse • Mixed apnea • 50~72% of stroke patients
Ondine’s curse Ondine is a water nymph and falls in love with a handsome knight, Sir Lawrence, and they are married. One afternoon, she sees Lawrence lying in the arms of another woman. Ondine curses him, “You swore faithfulness to me with every waking breath. As long as you are awake, you shall have your breath, but should you ever fall asleep, then that breath will be taken from you and you will die!"
Ondine’s curse • Respiratory control: – Voluntary: supramedullary respiratory control; cerebral cortex corticospinal tract – Automatic: • Regulates breathing automatically in response to the changes in oxygen and carbon dioxide in the blood • Respiratory center in medulla and pons
Ondine’s curse • Ondine’s curse – impairment of the automatic respiration – no damage to the voluntary respiration • Lateral medullary infarction in distal vertebral artery occlusion • Central apnea during sleep • Progress to fatal respiratory failure need mechanical ventilation
Take home message • Neurological complications occur early after ischemic stroke lead to death within first few days (high mortality rate) • Improved detection and management is important • Neurological complications include: – – – Brain edema Hemorrhagic transformation Post-stroke seizures Recurrent stroke Sleep disorder and sleep-disordered breathing Delirium

 Stroke protocol
Stroke protocol Pathogenesis of stroke ppt
Pathogenesis of stroke ppt Hemorrhagic vs ischemic stroke symptoms
Hemorrhagic vs ischemic stroke symptoms Tenecteplase stroke
Tenecteplase stroke Anterior stroke vs posterior stroke
Anterior stroke vs posterior stroke Acute stroke ready certification
Acute stroke ready certification Cns ischemic response
Cns ischemic response Superadded changes in coronary atherosclerosis
Superadded changes in coronary atherosclerosis Atrail
Atrail Optic ischemic neuropathy
Optic ischemic neuropathy Haemorrhage
Haemorrhage Pathophysiology of ischemic heart disease
Pathophysiology of ischemic heart disease Ischemic bile duct injury
Ischemic bile duct injury Cns ischemic response
Cns ischemic response Ischemic heart disease classification
Ischemic heart disease classification Amy lee plastic surgery
Amy lee plastic surgery Solent msk physiotherapy
Solent msk physiotherapy Haapsalu neurological rehabilitation centre
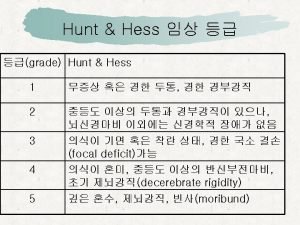
Haapsalu neurological rehabilitation centre Grade wfns
Grade wfns Ao classification system
Ao classification system Abnormal flexion and extension
Abnormal flexion and extension Ryan waters neurosurgeon
Ryan waters neurosurgeon Neurological based behavior
Neurological based behavior Neurological assessment form
Neurological assessment form Papilloedema
Papilloedema Psychomotor considerations language acquisition
Psychomotor considerations language acquisition Is adhd a neurological disorder
Is adhd a neurological disorder Neurological observations glasgow coma scale
Neurological observations glasgow coma scale Neurological examination
Neurological examination Motor function neurological assessment
Motor function neurological assessment Neurological disease
Neurological disease Biosocial theory of crime
Biosocial theory of crime Grades of power cns
Grades of power cns Muscle power neurological examination
Muscle power neurological examination What is focal neurological signs
What is focal neurological signs Joseph berger md neurology
Joseph berger md neurology