Recurrent pregnancy loss Spontaneous pregnancy loss is the
- Slides: 13
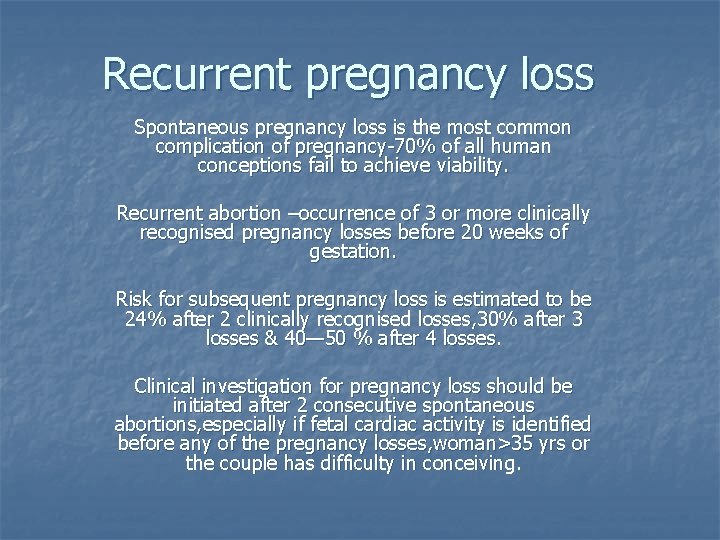
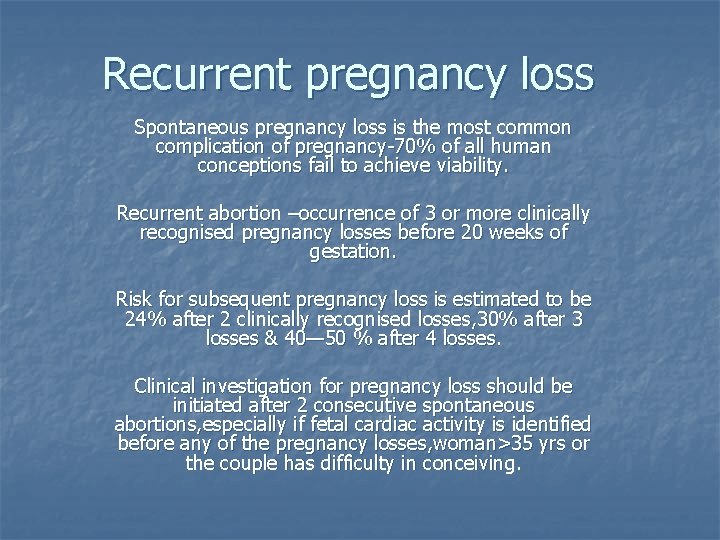
Recurrent pregnancy loss Spontaneous pregnancy loss is the most common complication of pregnancy-70% of all human conceptions fail to achieve viability. Recurrent abortion –occurrence of 3 or more clinically recognised pregnancy losses before 20 weeks of gestation. Risk for subsequent pregnancy loss is estimated to be 24% after 2 clinically recognised losses, 30% after 3 losses & 40— 50 % after 4 losses. Clinical investigation for pregnancy loss should be initiated after 2 consecutive spontaneous abortions, especially if fetal cardiac activity is identified before any of the pregnancy losses, woman>35 yrs or the couple has difficulty in conceiving.
History n n n h/o consanguinity-single gene defects may cause RPL –revealed by a detailed family history. Inherited thrombophilias can cause RPLhyperhomocystinemia, activated protein c resistance, mutations in factor 5 leidein, protein C, S, antithrombin 3 Parental chromosomal abnormalities like balanced translocations can cause RPL-cannot be ruled out by family history or prior term births.
History n n h/o foul smelling vaginal dischargesuggestive of bacterial vaginosis. infection with ureaplasma, prevotella, b-hemolytic streptococcus, mycoplasma, gardenella, chla mydia have been implicated Bacterial vaginosis-recurrent 2 nd trimester loss.
History n HSV, CMV cause direct infection of the n n fetus, placenta-resulting villitis & tissue destruction-pregnancy disruption Aqquired anatomic abnormalitiesintrauterine adhesions, endometriosis, uterine fibroids. endometrium over fibroid/synechiae-inadequately vascularised-abnormal placentationspontaneous pregnancy loss. h/o any purulent discharge pvendometritis, submucous fibroid polyp
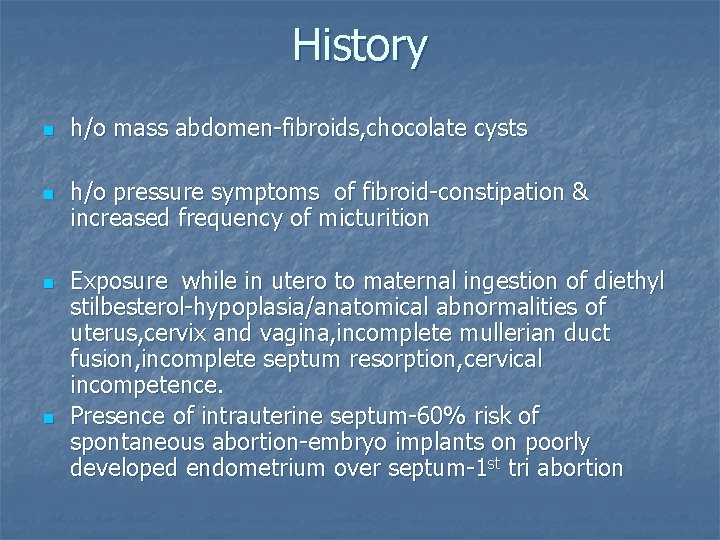
History n n h/o mass abdomen-fibroids, chocolate cysts h/o pressure symptoms of fibroid-constipation & increased frequency of micturition Exposure while in utero to maternal ingestion of diethyl stilbesterol-hypoplasia/anatomical abnormalities of uterus, cervix and vagina, incomplete mullerian duct fusion, incomplete septum resorption, cervical incompetence. Presence of intrauterine septum-60% risk of spontaneous abortion-embryo implants on poorly developed endometrium over septum-1 st tri abortion
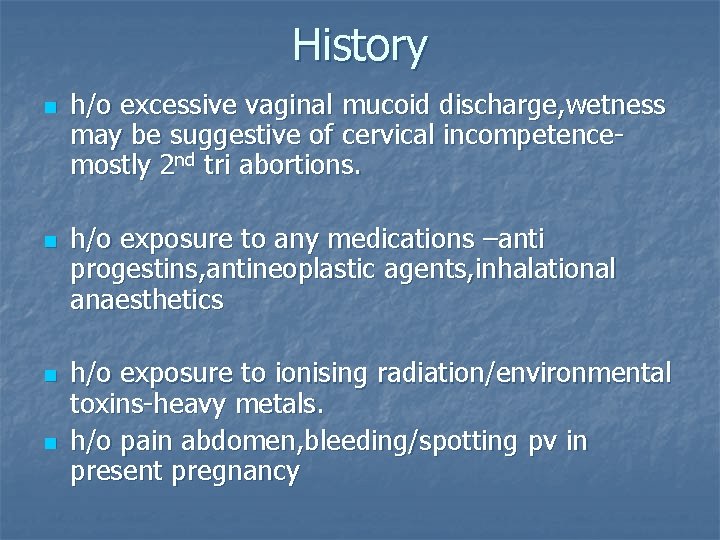
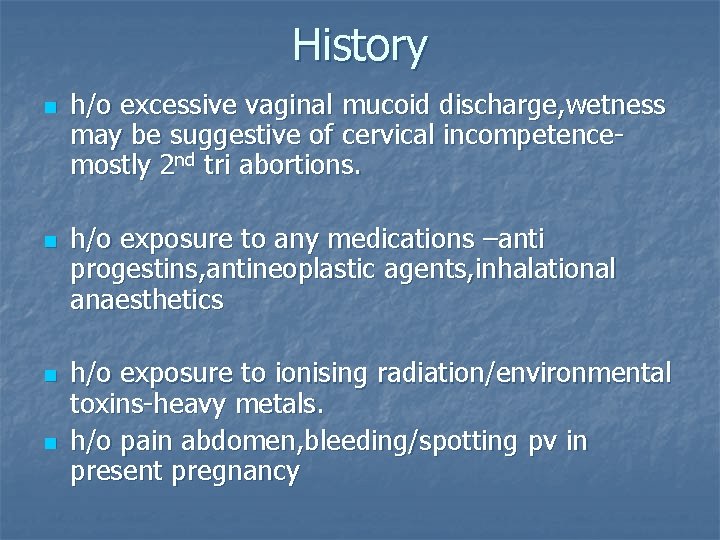
History n n h/o excessive vaginal mucoid discharge, wetness may be suggestive of cervical incompetencemostly 2 nd tri abortions. h/o exposure to any medications –anti progestins, antineoplastic agents, inhalational anaesthetics h/o exposure to ionising radiation/environmental toxins-heavy metals. h/o pain abdomen, bleeding/spotting pv in present pregnancy
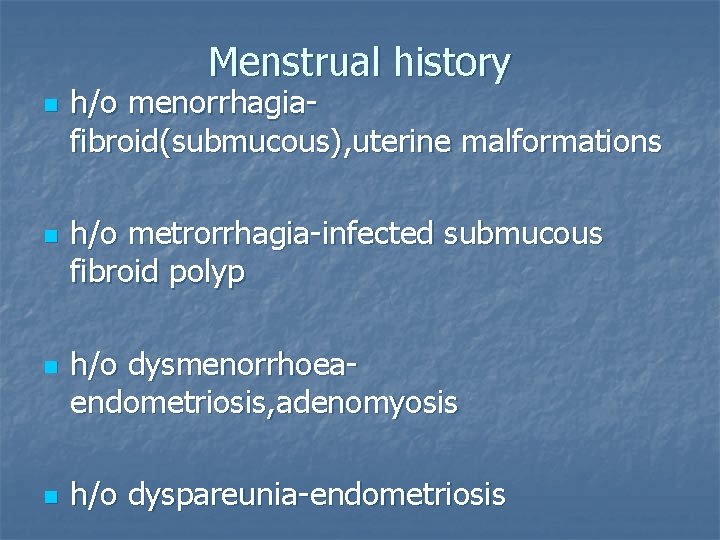
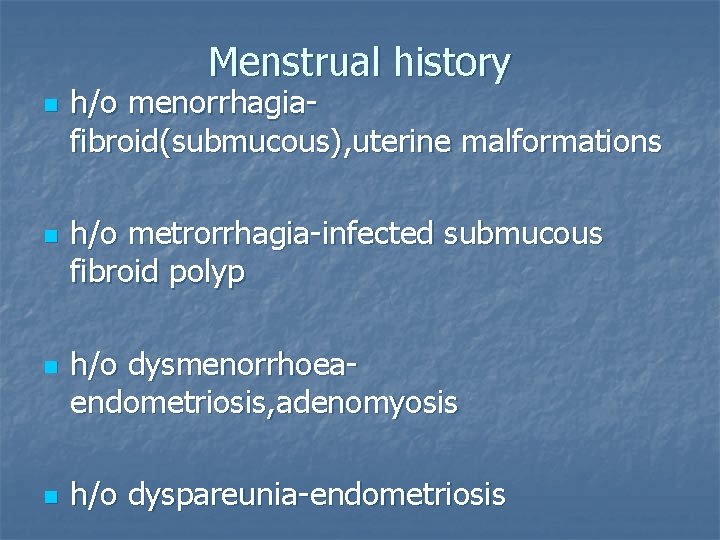
Menstrual history n n h/o menorrhagiafibroid(submucous), uterine malformations h/o metrorrhagia-infected submucous fibroid polyp h/o dysmenorrhoeaendometriosis, adenomyosis h/o dyspareunia-endometriosis
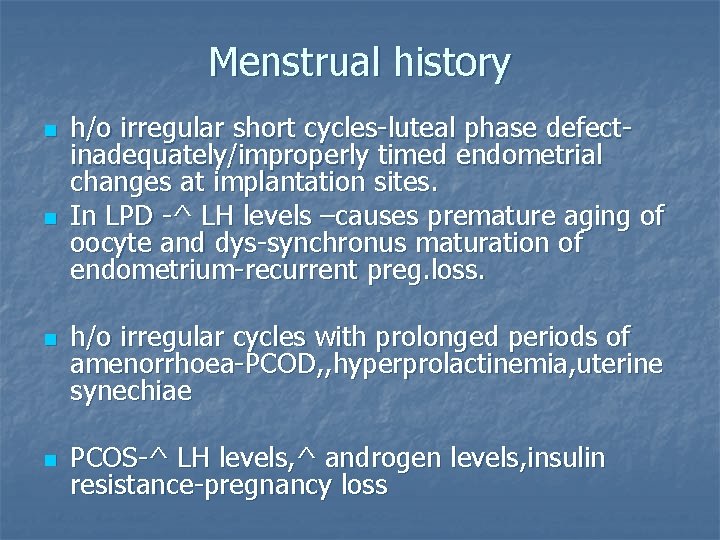
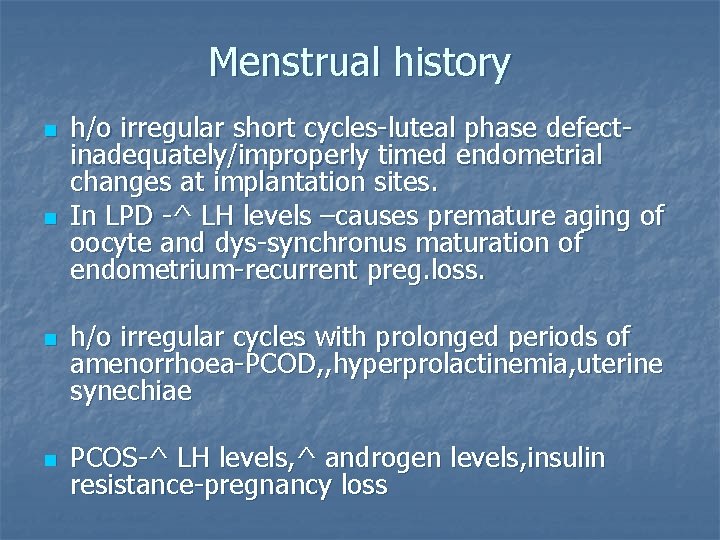
Menstrual history n n h/o irregular short cycles-luteal phase defectinadequately/improperly timed endometrial changes at implantation sites. In LPD -^ LH levels –causes premature aging of oocyte and dys-synchronus maturation of endometrium-recurrent preg. loss. h/o irregular cycles with prolonged periods of amenorrhoea-PCOD, , hyperprolactinemia, uterine synechiae PCOS-^ LH levels, ^ androgen levels, insulin resistance-pregnancy loss
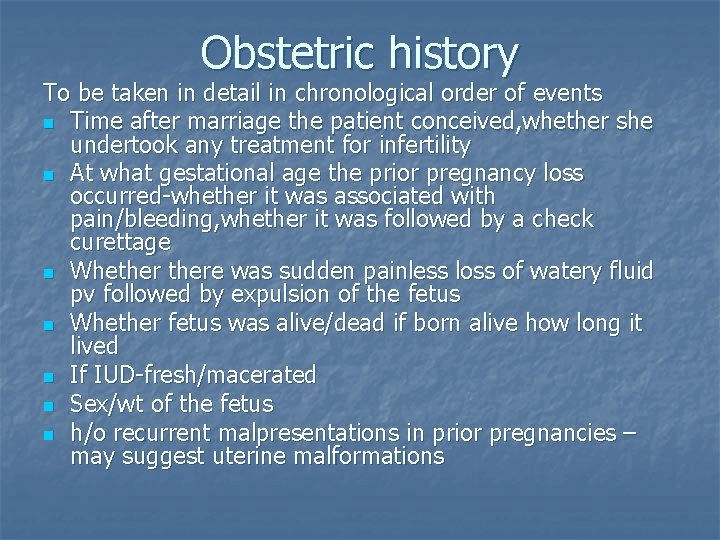
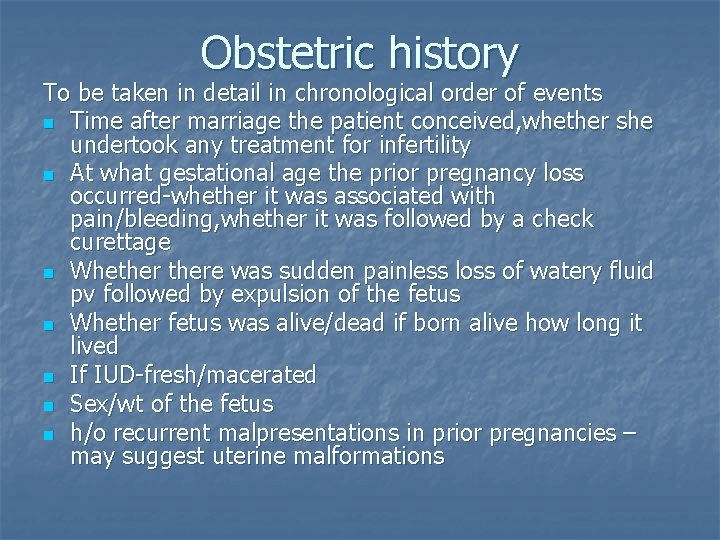
Obstetric history To be taken in detail in chronological order of events n Time after marriage the patient conceived, whether she undertook any treatment for infertility n At what gestational age the prior pregnancy loss occurred-whether it was associated with pain/bleeding, whether it was followed by a check curettage n Whethere was sudden painless loss of watery fluid pv followed by expulsion of the fetus n Whether fetus was alive/dead if born alive how long it lived n If IUD-fresh/macerated n Sex/wt of the fetus n h/o recurrent malpresentations in prior pregnancies – may suggest uterine malformations
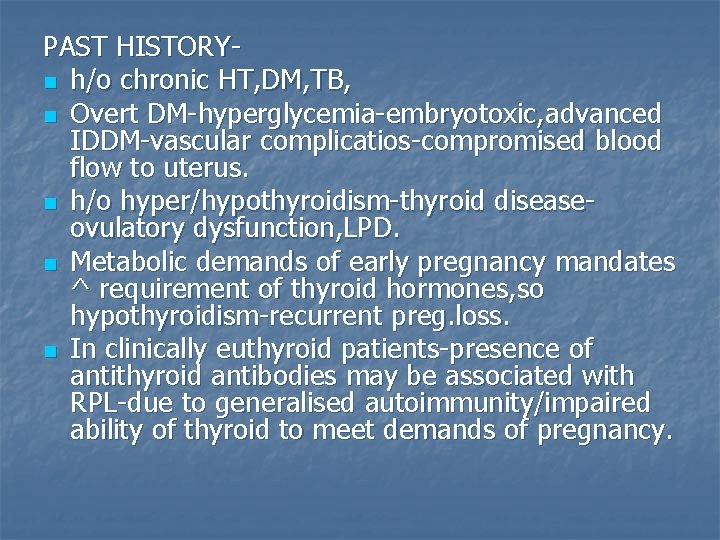
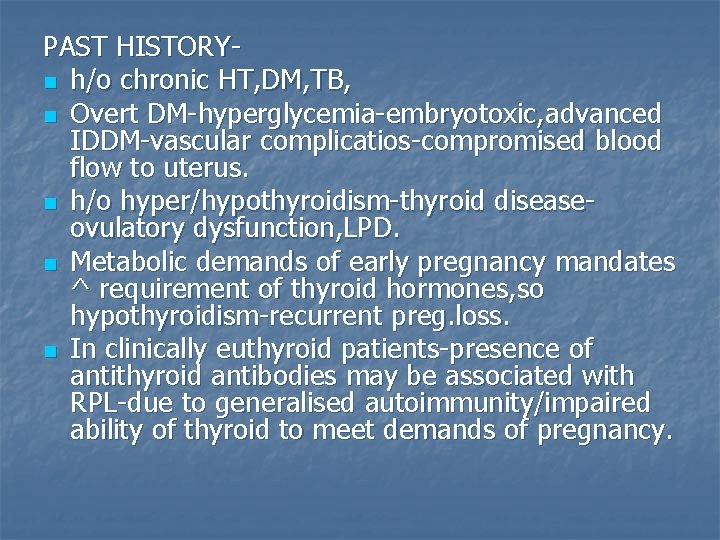
PAST HISTORYn h/o chronic HT, DM, TB, n Overt DM-hyperglycemia-embryotoxic, advanced IDDM-vascular complicatios-compromised blood flow to uterus. n h/o hyper/hypothyroidism-thyroid diseaseovulatory dysfunction, LPD. n Metabolic demands of early pregnancy mandates ^ requirement of thyroid hormones, so hypothyroidism-recurrent preg. loss. n In clinically euthyroid patients-presence of antithyroid antibodies may be associated with RPL-due to generalised autoimmunity/impaired ability of thyroid to meet demands of pregnancy.
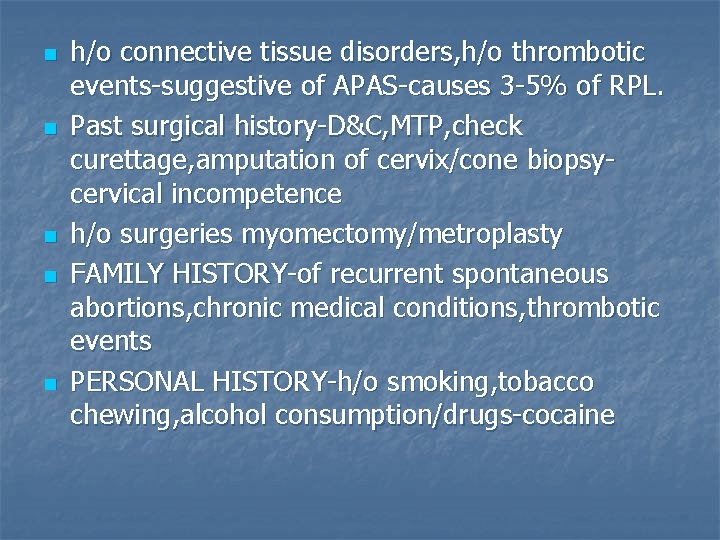
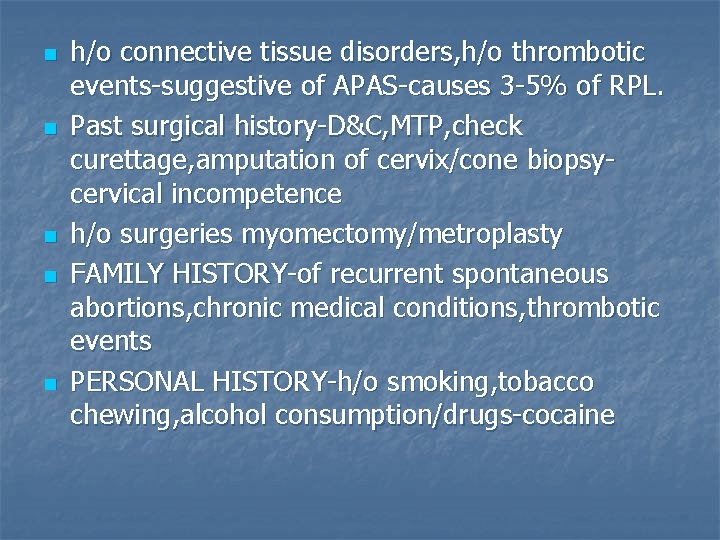
n n n h/o connective tissue disorders, h/o thrombotic events-suggestive of APAS-causes 3 -5% of RPL. Past surgical history-D&C, MTP, check curettage, amputation of cervix/cone biopsycervical incompetence h/o surgeries myomectomy/metroplasty FAMILY HISTORY-of recurrent spontaneous abortions, chronic medical conditions, thrombotic events PERSONAL HISTORY-h/o smoking, tobacco chewing, alcohol consumption/drugs-cocaine
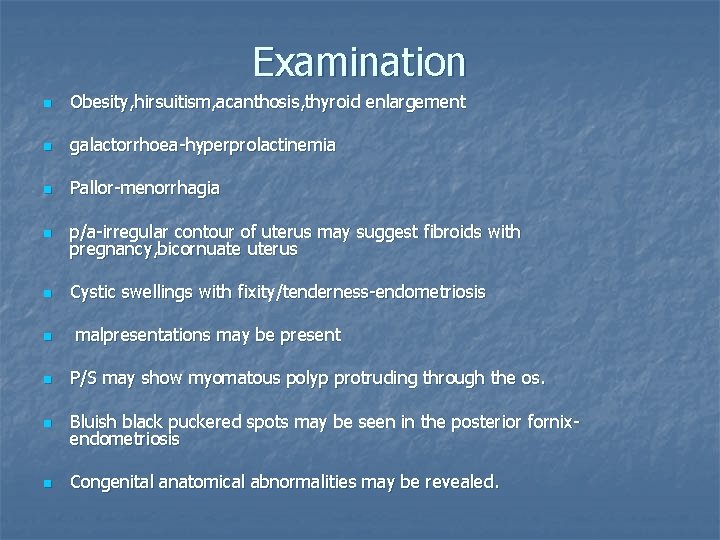
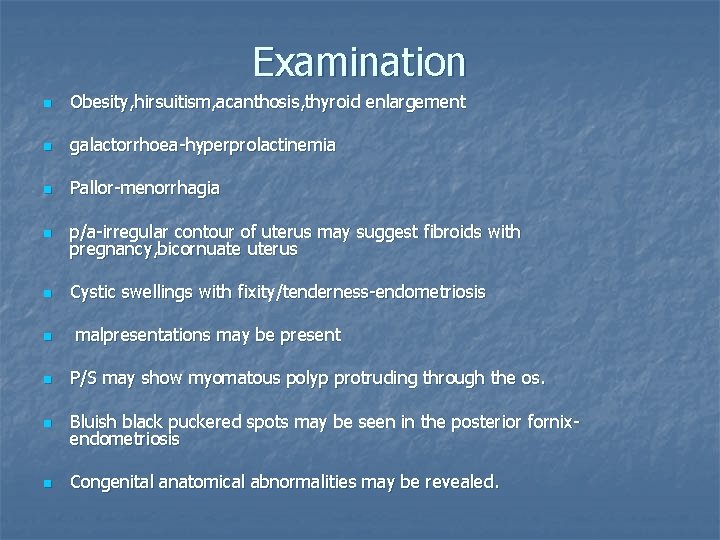
Examination n Obesity, hirsuitism, acanthosis, thyroid enlargement n galactorrhoea-hyperprolactinemia n Pallor-menorrhagia n p/a-irregular contour of uterus may suggest fibroids with pregnancy, bicornuate uterus n Cystic swellings with fixity/tenderness-endometriosis n malpresentations may be present n P/S may show myomatous polyp protruding through the os. n Bluish black puckered spots may be seen in the posterior fornixendometriosis n Congenital anatomical abnormalities may be revealed.
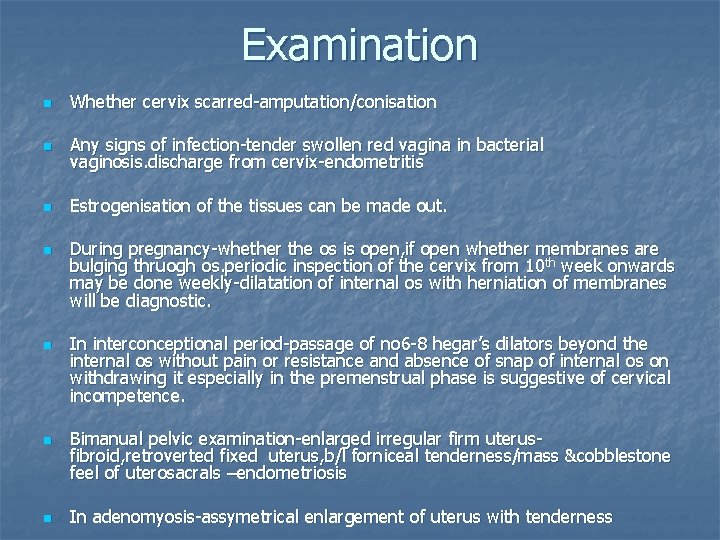
Examination n Whether cervix scarred-amputation/conisation n Any signs of infection-tender swollen red vagina in bacterial vaginosis. discharge from cervix-endometritis n Estrogenisation of the tissues can be made out. n n During pregnancy-whether the os is open, if open whether membranes are bulging thruogh os. periodic inspection of the cervix from 10 th week onwards may be done weekly-dilatation of internal os with herniation of membranes will be diagnostic. In interconceptional period-passage of no 6 -8 hegar’s dilators beyond the internal os without pain or resistance and absence of snap of internal os on withdrawing it especially in the premenstrual phase is suggestive of cervical incompetence. Bimanual pelvic examination-enlarged irregular firm uterusfibroid, retroverted fixed uterus, b/l forniceal tenderness/mass &cobblestone feel of uterosacrals –endometriosis In adenomyosis-assymetrical enlargement of uterus with tenderness
 Spotting differential diagnosis
Spotting differential diagnosis Difference between normal loss and abnormal loss
Difference between normal loss and abnormal loss Nasal vestibulitis treatment
Nasal vestibulitis treatment What are the five elements of hair design
What are the five elements of hair design Lstm colah
Lstm colah Wrist anastomosis
Wrist anastomosis Partial vs complete recurrent laryngeal nerve injury
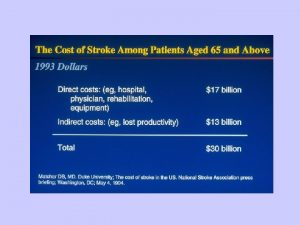
Partial vs complete recurrent laryngeal nerve injury Recurrent stroke causes
Recurrent stroke causes Foot arteries
Foot arteries Coarcitation of aorta
Coarcitation of aorta Coco
Coco Quadrangular membrane larynx
Quadrangular membrane larynx Beahrs triangle
Beahrs triangle Recurrent artery of huebner
Recurrent artery of huebner