Portal hypertension DR Walid Elshazly Portal hypertension Portal



















- Slides: 75
Portal hypertension DR/ Walid Elshazly
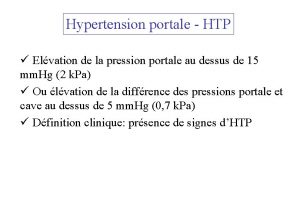
Portal hypertension ® Portal hypertension is an increase in the blood pressure within a system of veins called the portal venous system ® Normal portal pressure is generally defined between 5 and 10 mm Hg.
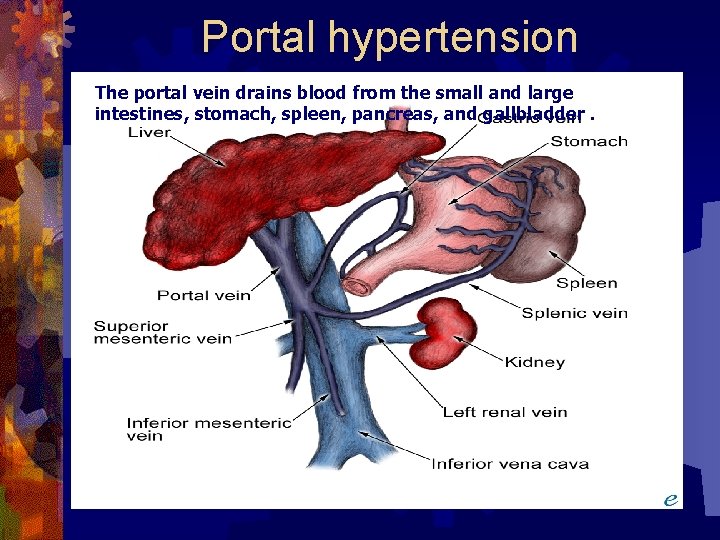
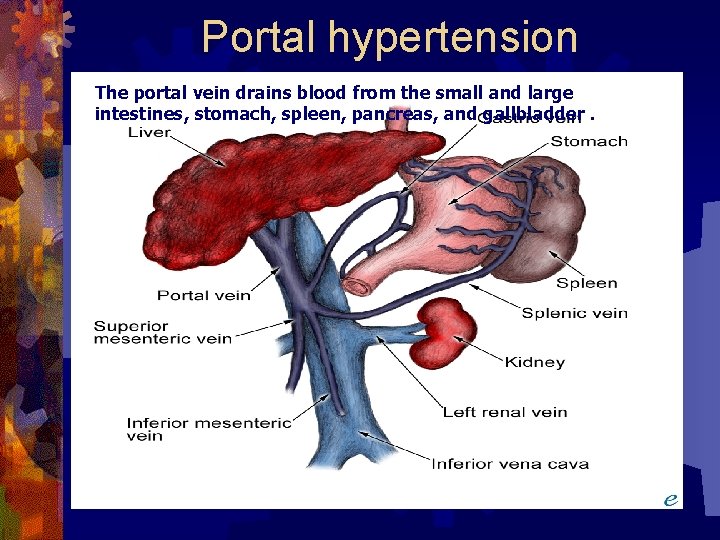
Portal hypertension The portal vein drains blood from the small and large intestines, stomach, spleen, pancreas, and gallbladder.
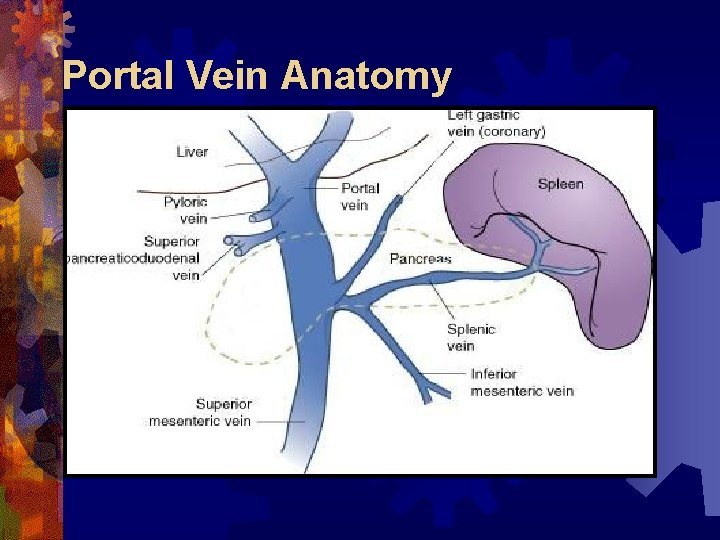
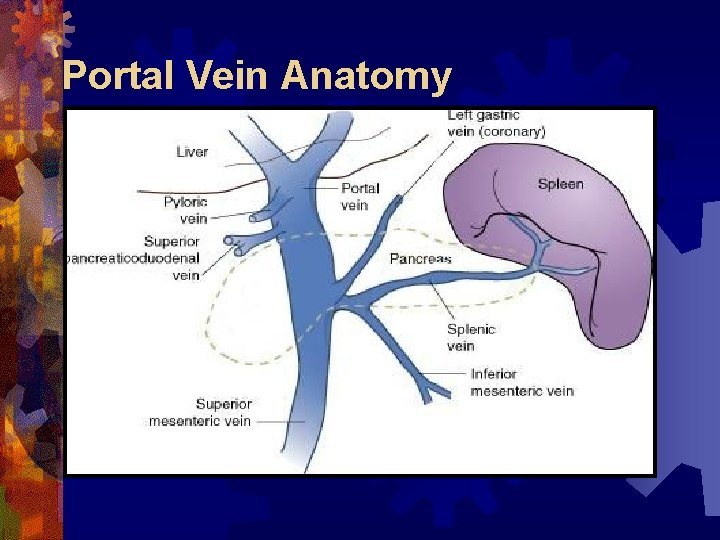
Portal Vein Anatomy

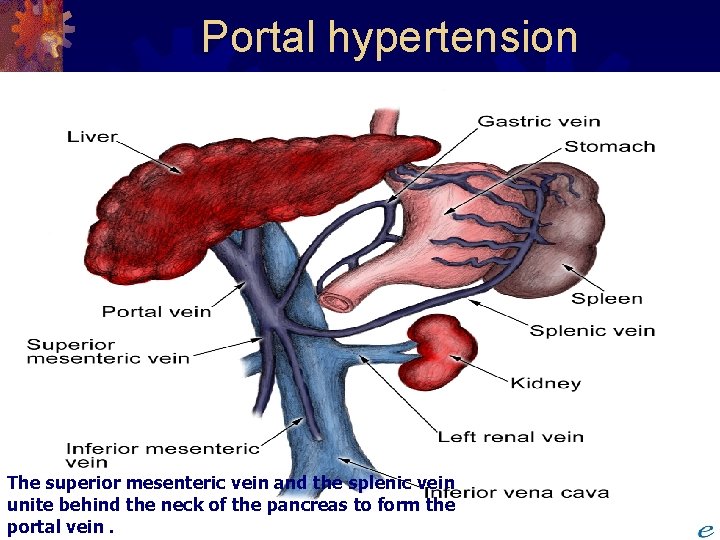
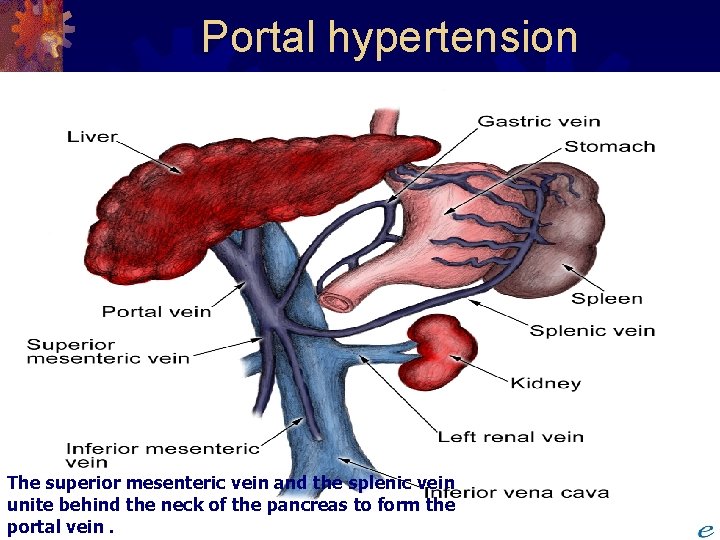
Portal hypertension The superior mesenteric vein and the splenic vein unite behind the neck of the pancreas to form the portal vein.

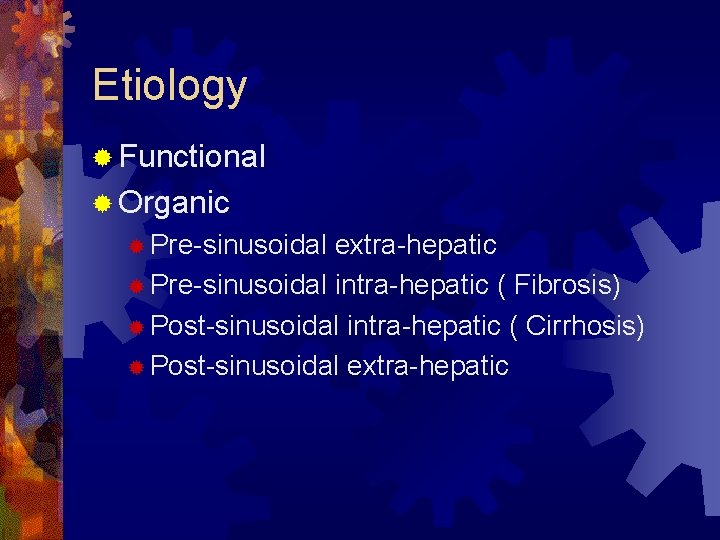
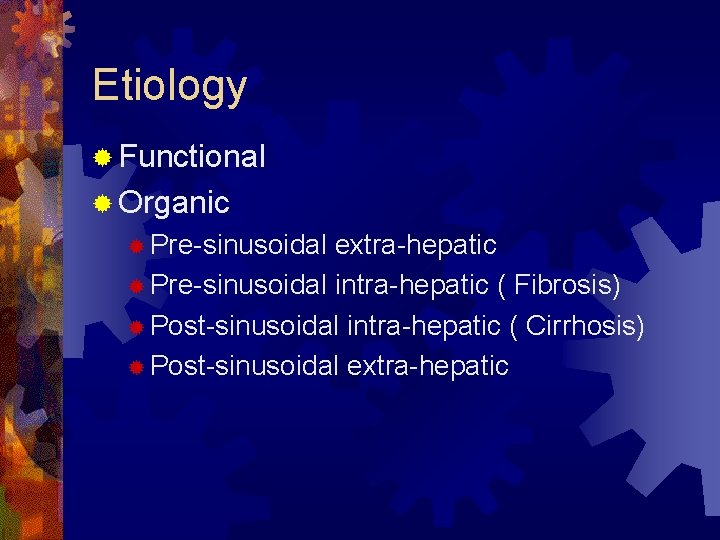
Etiology ® Functional ® Organic ® Pre-sinusoidal extra-hepatic ® Pre-sinusoidal intra-hepatic ( Fibrosis) ® Post-sinusoidal intra-hepatic ( Cirrhosis) ® Post-sinusoidal extra-hepatic
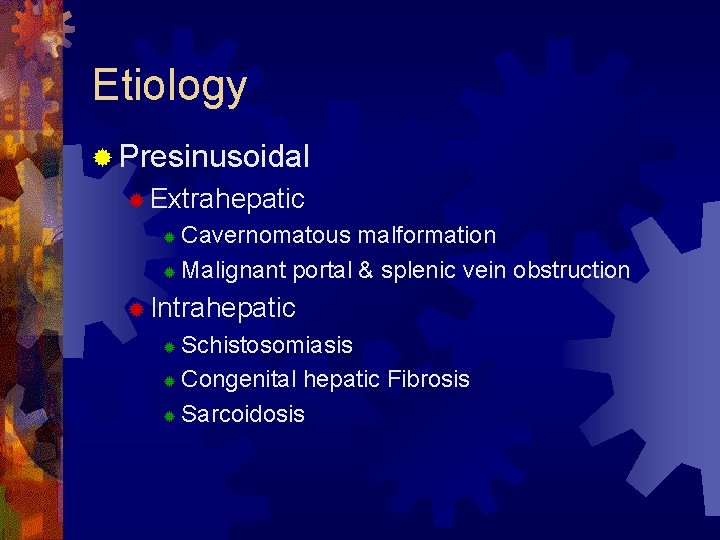
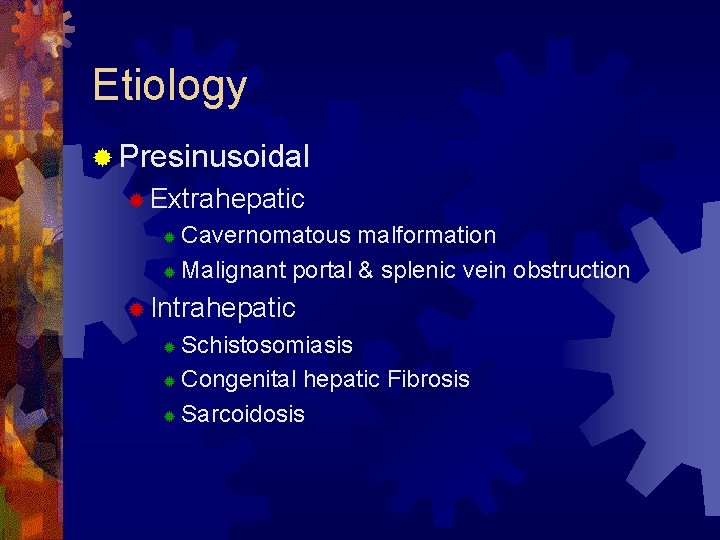
Etiology ® Presinusoidal ® Extrahepatic Cavernomatous malformation ® Malignant portal & splenic vein obstruction ® ® Intrahepatic Schistosomiasis ® Congenital hepatic Fibrosis ® Sarcoidosis ®
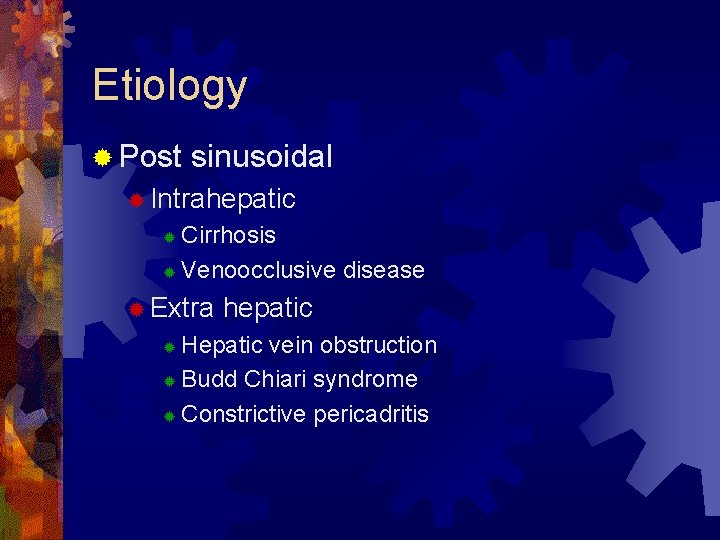
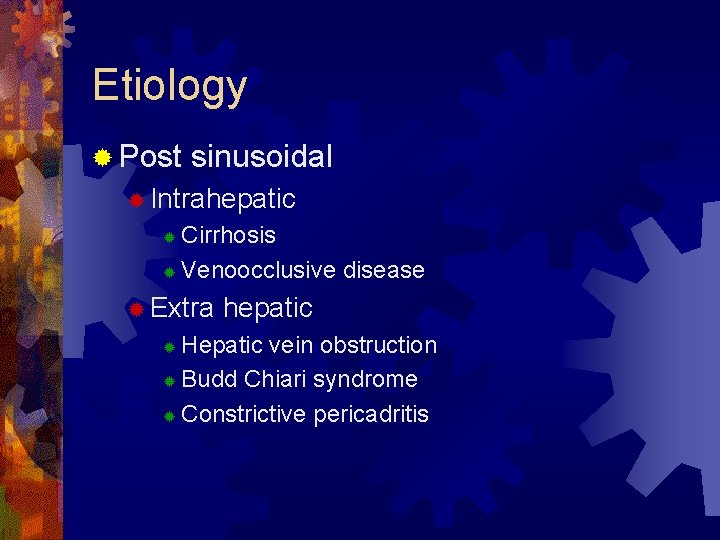
Etiology ® Post sinusoidal ® Intrahepatic Cirrhosis ® Venoocclusive disease ® ® Extra hepatic Hepatic vein obstruction ® Budd Chiari syndrome ® Constrictive pericadritis ®
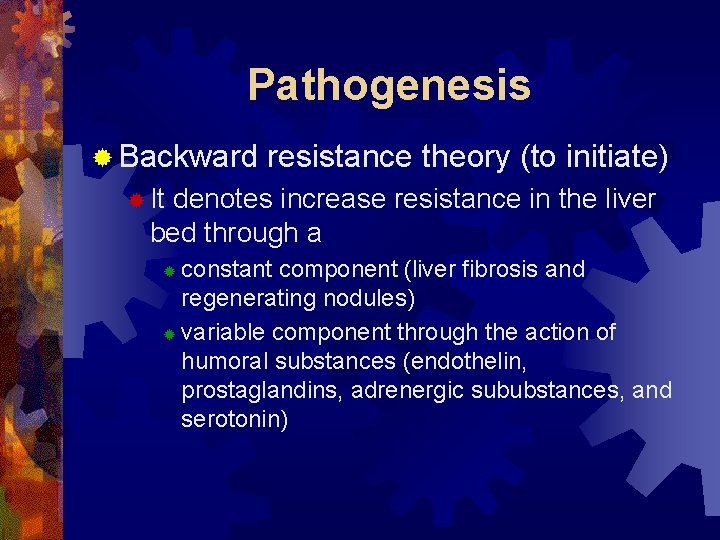
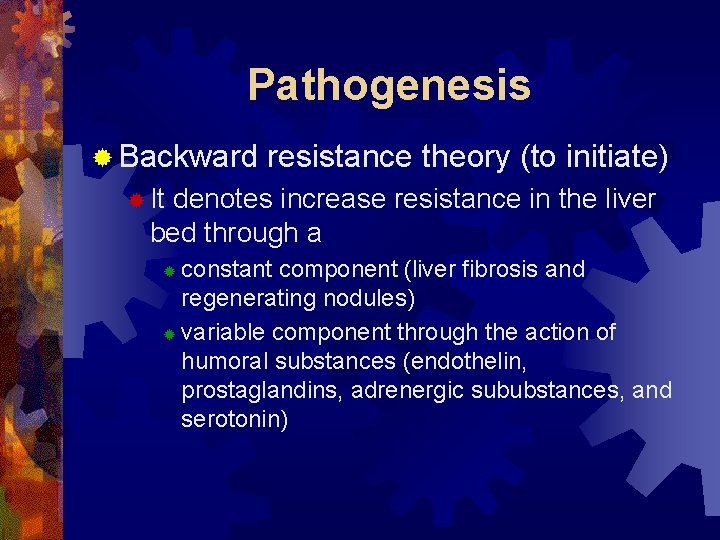
Pathogenesis ® Backward resistance theory (to initiate) ® It denotes increase resistance in the liver bed through a constant component (liver fibrosis and regenerating nodules) ® variable component through the action of humoral substances (endothelin, prostaglandins, adrenergic sububstances, and serotonin) ®
Pathogenesis ® Forward flow theory (to maintain) ® It denotes increase in inflow to the liver through the action of humoral substances that cause hyperdynamic and ® hypervolemic circulation (nitric oxide, glucagon and, prostacylin) ®
Mechanism of portal hypertension In Shistosomiasis ® Peri-portal fibrosis ® Portal hyper-volaemia ® Release of vaso-spastic substances ® Angiomatous mass ® Endo- arterial obstruction
Complication of portal hypertension 1. 2. 3. 4. 5. 6. Spleno-megally GIT congestion Ascites Opening of porto-systemic collaterals Hepatocelluar failure Portosystemic encephalopathy
Splenomegally ® Mechanisms ® RES hyper-plasia ® Opening of A/V shunts ® Venous congestion ® hypersplenism
Splenomegally ® Clinical picture ® Pressure manifestations ® Splenic pain ® Hypersplenism ® Psychic trauma
GIT congestion ®Gastric dyspepsia related to type of food ®Haematemesis dt gastropathy which cause sever form of bleeding
Ascites ® etiology of ascites 1. 2. 3. 4. 5. Hormonal factors lead to salt and water retention Hypo-proteinaemia Portal hypertension Lymphorrhoea Disturbed renal function

Ascites ( treatment) ® ® ® Bed rest Diet Albumin infusion Fresh frozen plasma Diuretics Refractory ascites require 1. 2. 3. 4. Therapeutic para-centesis Recirculation therapy Peritoneo-venous shunt Sapheno-peritoneal shunt
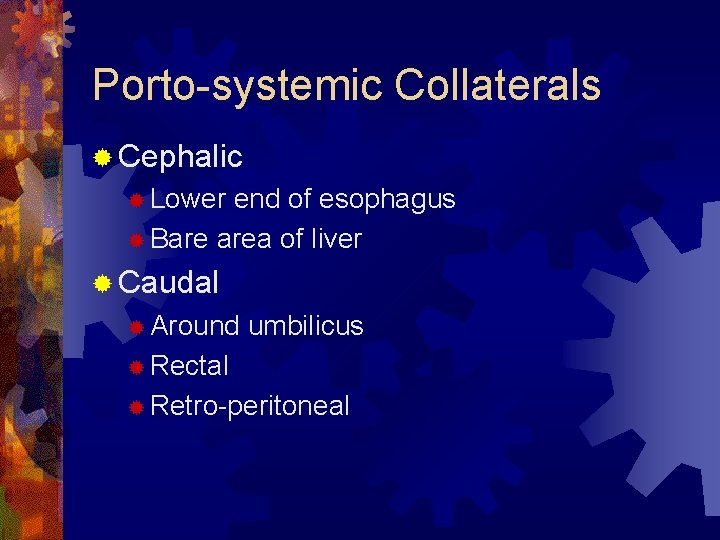
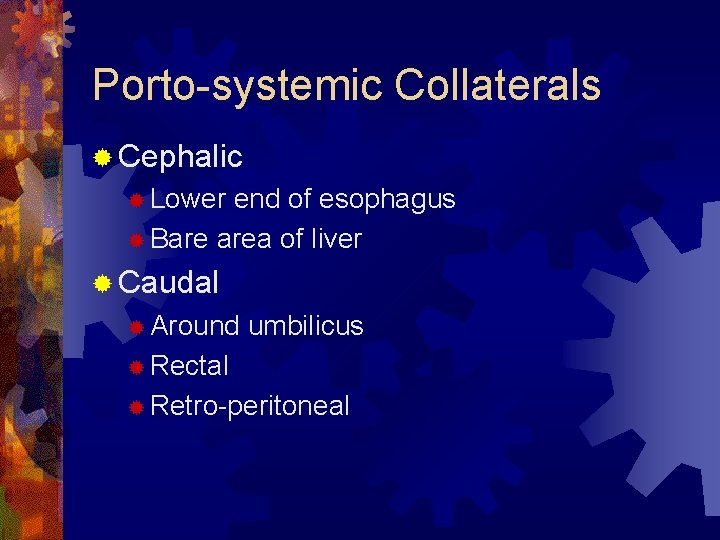
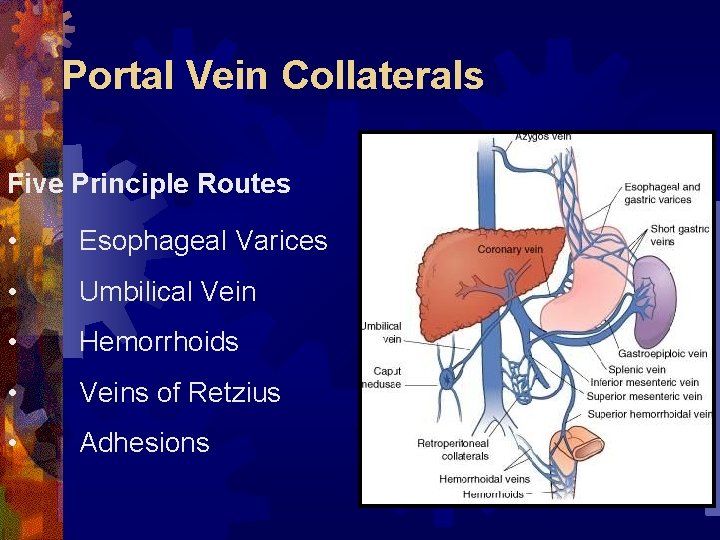
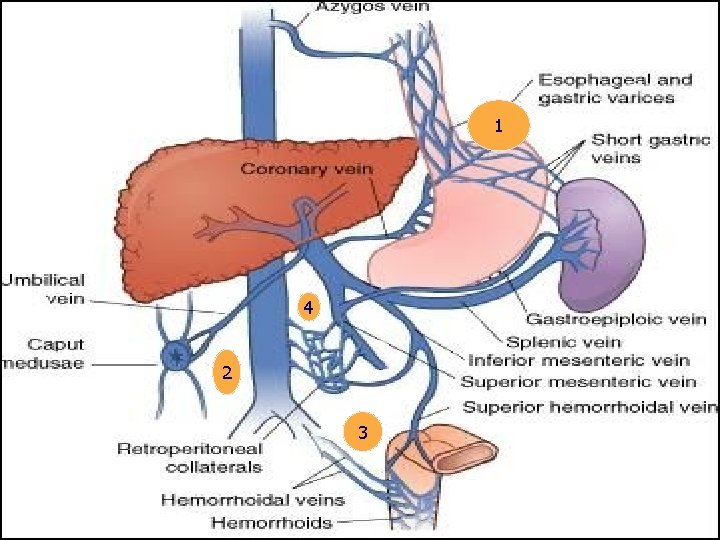
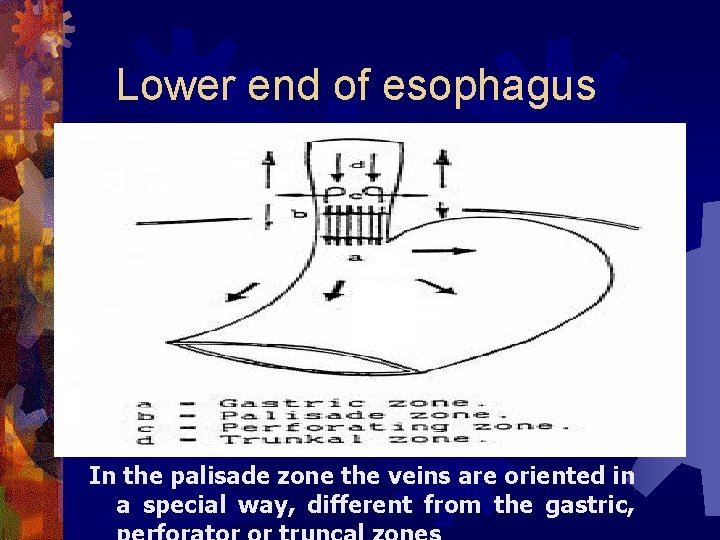
Porto-systemic Collaterals ® Cephalic ® Lower end of esophagus ® Bare area of liver ® Caudal ® Around umbilicus ® Rectal ® Retro-peritoneal
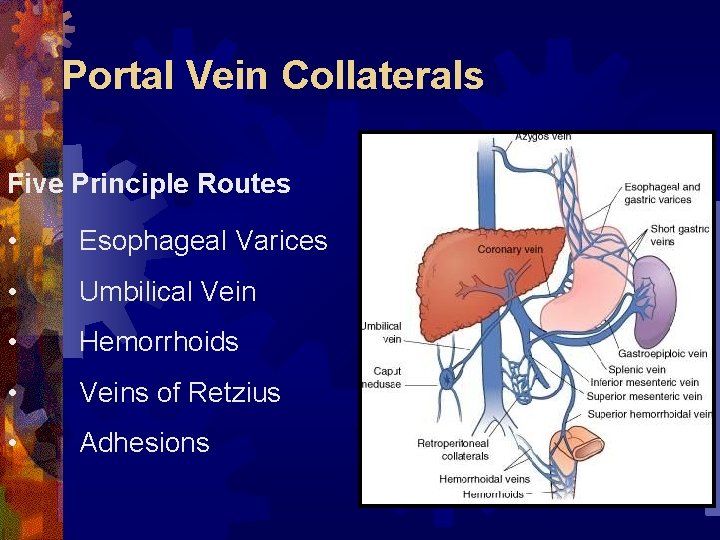
Portal Vein Collaterals Five Principle Routes • Esophageal Varices • Umbilical Vein • Hemorrhoids • Veins of Retzius • Adhesions
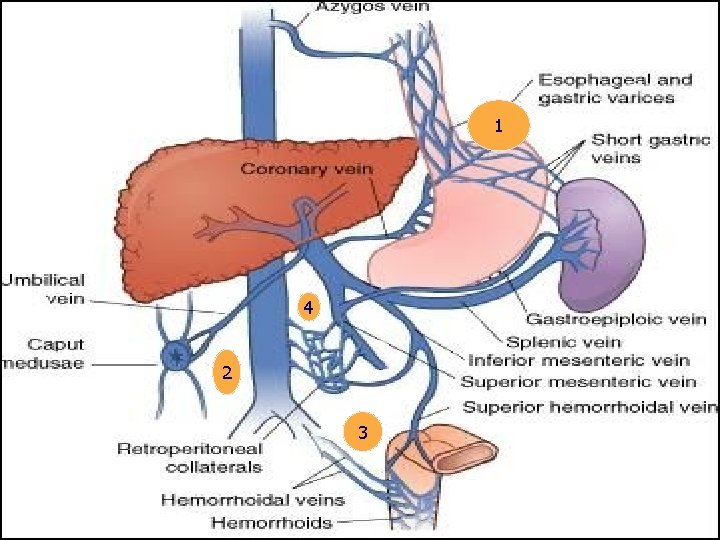
1 4 2 3
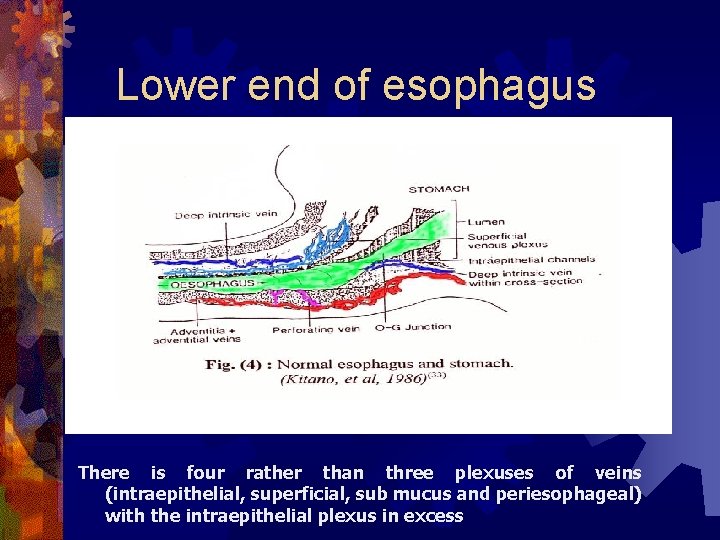
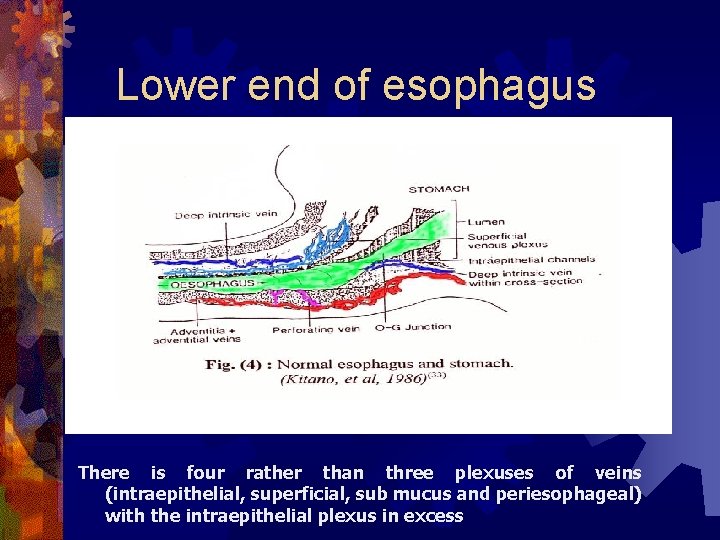
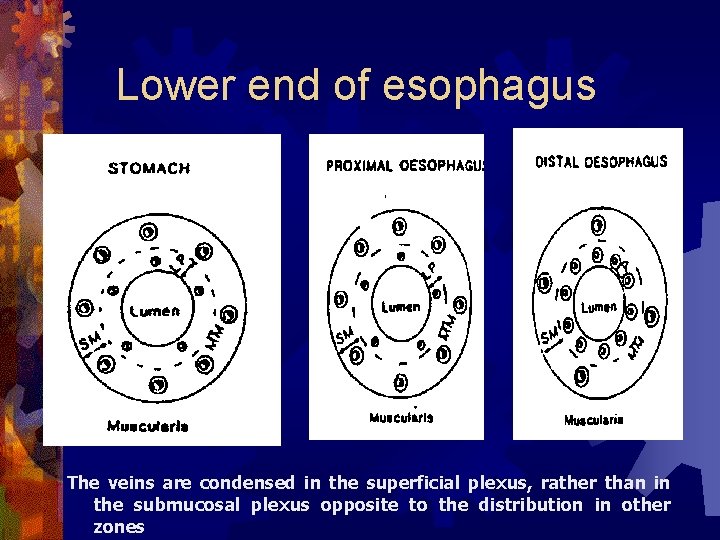
Lower end of esophagus There is four rather than three plexuses of veins (intraepithelial, superficial, sub mucus and periesophageal) with the intraepithelial plexus in excess
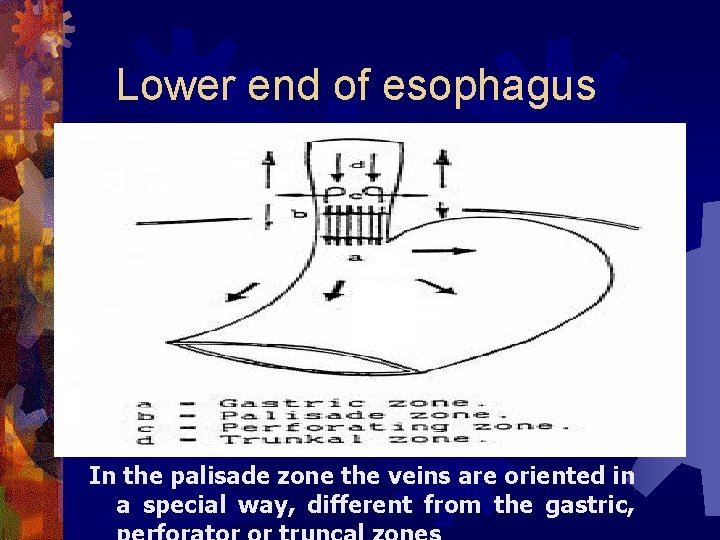
Lower end of esophagus In the palisade zone the veins are oriented in a special way, different from the gastric,
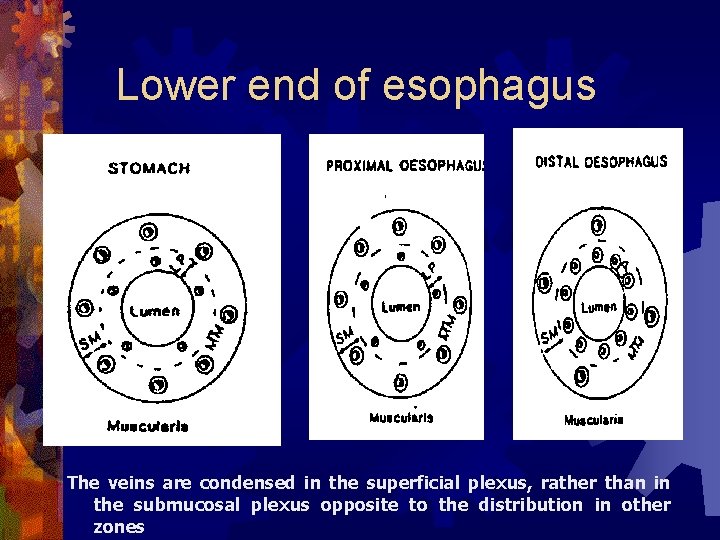
Lower end of esophagus The veins are condensed in the superficial plexus, rather than in the submucosal plexus opposite to the distribution in other zones
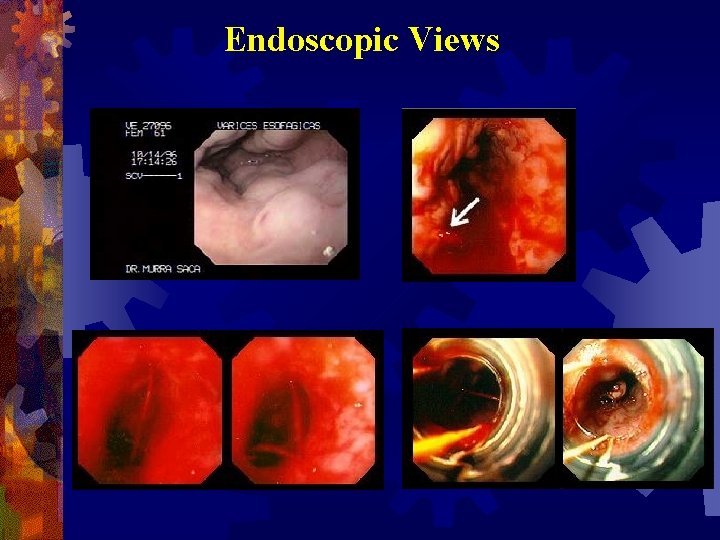
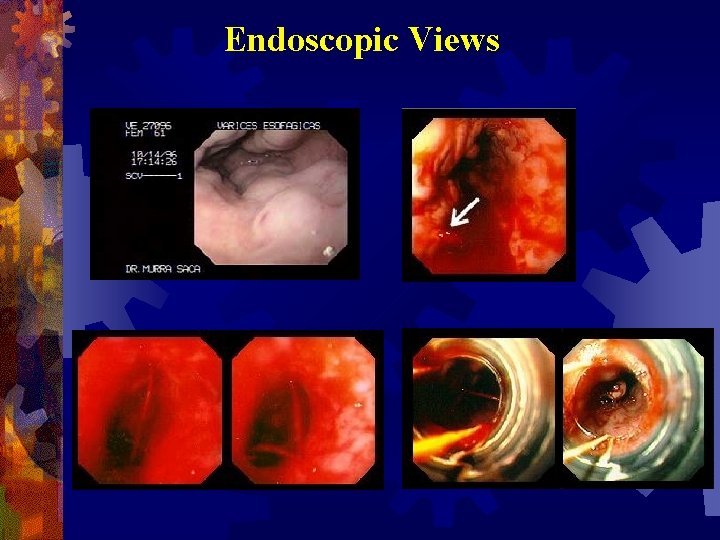
Endoscopic Views
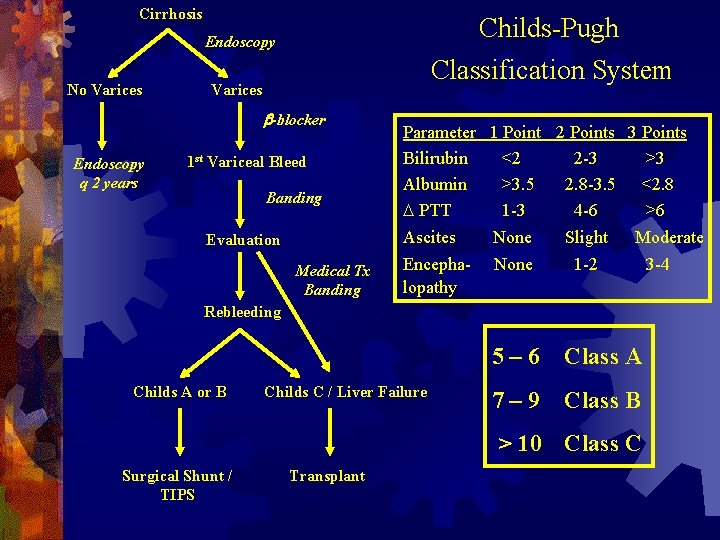
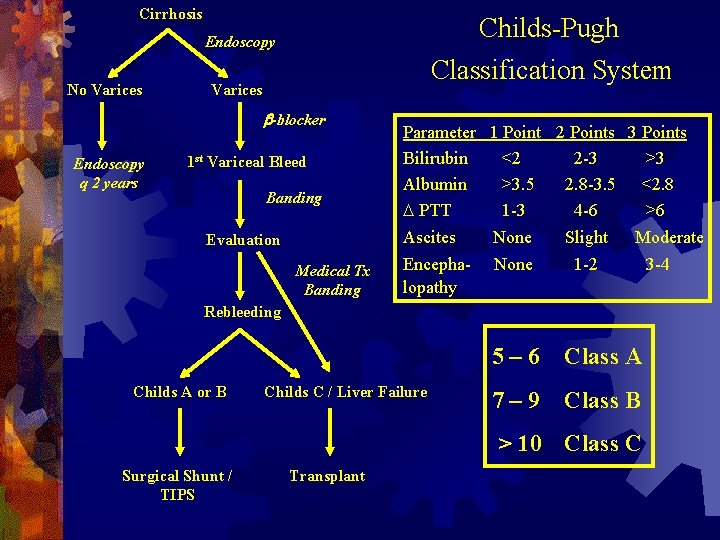
Cirrhosis Childs-Pugh Endoscopy No Varices Classification System Varices b-blocker Endoscopy q 2 years 1 st Variceal Bleed Banding Evaluation Medical Tx Banding Parameter 1 Point 2 Points 3 Points Bilirubin <2 2 -3 >3 Albumin >3. 5 2. 8 -3. 5 <2. 8 D PTT 1 -3 4 -6 >6 Ascites None Slight Moderate Encepha- None 1 -2 3 -4 lopathy Rebleeding Childs A or B Childs C / Liver Failure 5– 6 Class A 7– 9 Class B > 10 Class C Surgical Shunt / TIPS Transplant
Hepato-cellular failure ( etiology) ® Infection ® Bleeding ® Drugs ® Anesthesia ® surgery
Hepato-cellular failure (C/P) ® Weakness ® Jaundice ® Fetor hepaticus ® Palmer erytems ® Spider angioma ® Gynaecomastia ® Loss of axially and pubic hair ® Testicular atrophy ® Acute liver failure
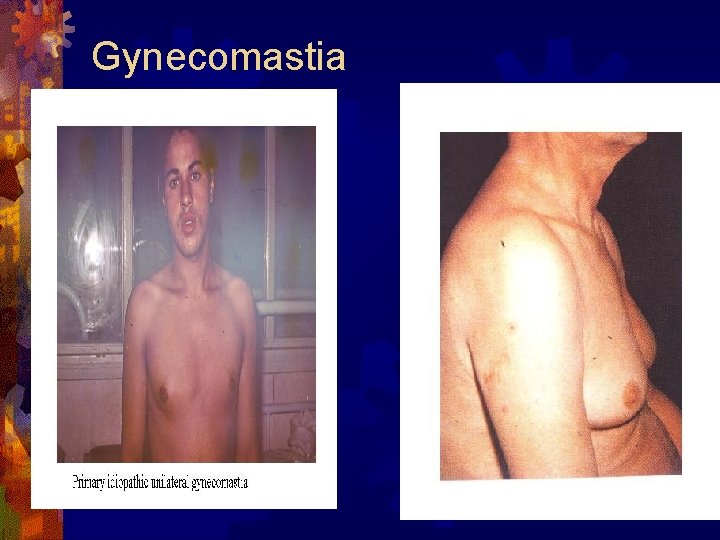
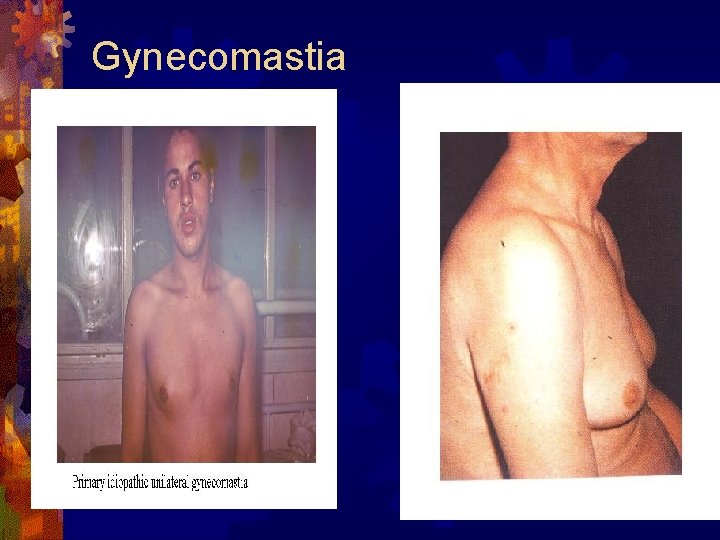
Gynecomastia

Hepato-cellular failure (R) ® Treat precipitating factors ® Diet ® Drugs ® Renal failure ® Correct clotting abnormalites ® If no response ® Exchange transfusion ® Cross circulation between donor and patient ® Extra-corporeal perfusion through pigs liver
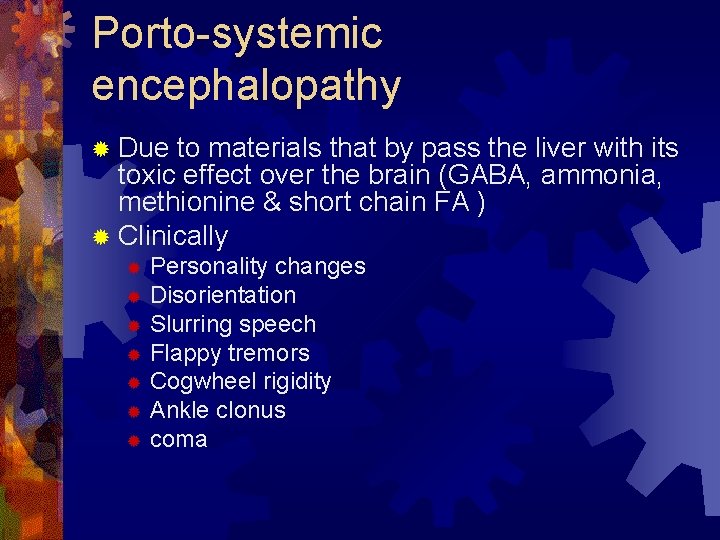
Porto-systemic encephalopathy ® Due to materials that by pass the liver with its toxic effect over the brain (GABA, ammonia, methionine & short chain FA ) ® Clinically Personality changes ® Disorientation ® Slurring speech ® Flappy tremors ® Cogwheel rigidity ® Ankle clonus ® coma ®
Porto-systemic encephalopathy ® Treatment ® Chemical Intestinal antiseptic ® Lactulose ® ® Mechnical ® Liver support ® Nerve cell support glutamic acid
Investigations ® Laboratory ® Stool ® Urine ® CBC ® Kidney function ® Liver function Synthesis (proteins, prothrombin) ® Excretory ( bilirubin, dye excretion) ® Cell insult (SGOT, SGPT, alk phospatase, LDH) ®
Investigations ® Radiological ® U/S ® Doppler ® B swallow ® B enema ® Portography ® CT scan ® MRI ® Radio-isotope ® Instrumental ® Upper endoscopy ® Laparscopic U/S
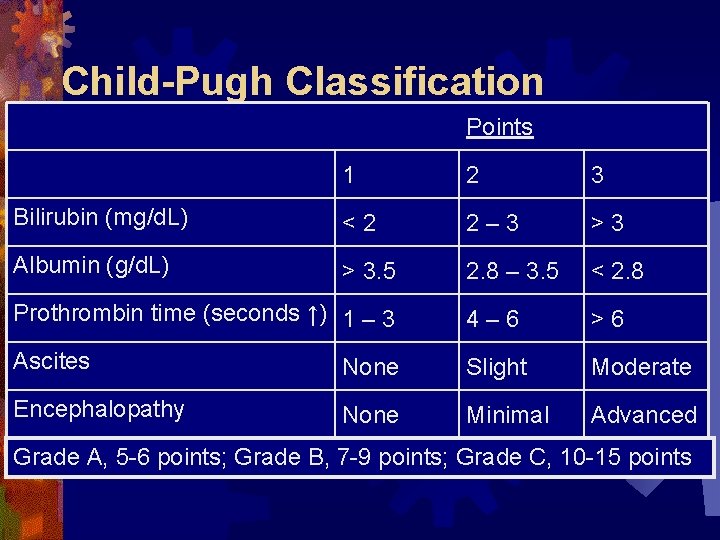
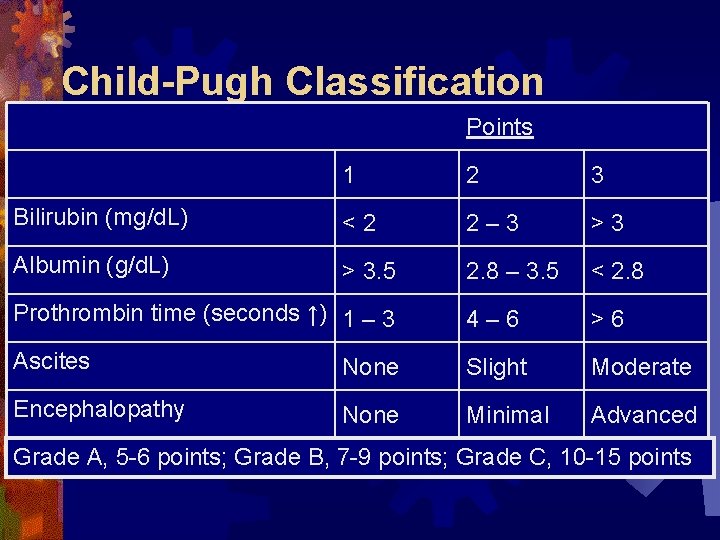
Child-Pugh Classification Points 1 2 3 Bilirubin (mg/d. L) <2 2– 3 >3 Albumin (g/d. L) > 3. 5 2. 8 – 3. 5 < 2. 8 Prothrombin time (seconds ↑) 1 – 3 4– 6 >6 Ascites None Slight Moderate Encephalopathy None Minimal Advanced Grade A, 5 -6 points; Grade B, 7 -9 points; Grade C, 10 -15 points
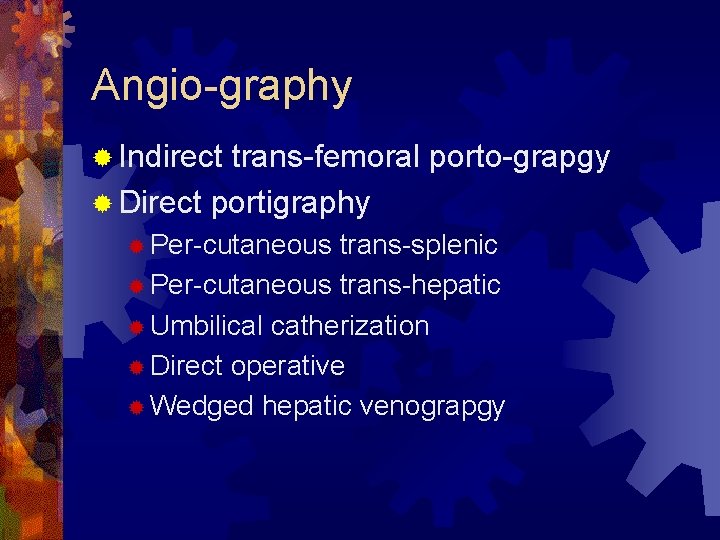
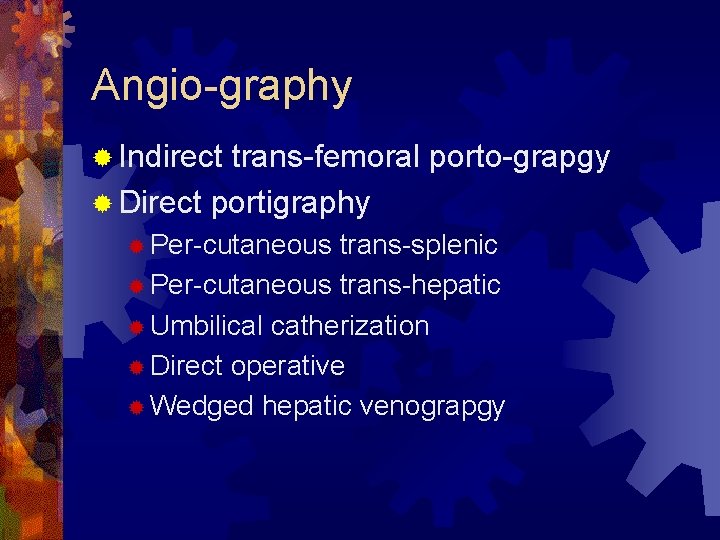
Angio-graphy ® Indirect trans-femoral porto-grapgy ® Direct portigraphy ® Per-cutaneous trans-splenic ® Per-cutaneous trans-hepatic ® Umbilical catherization ® Direct operative ® Wedged hepatic venograpgy
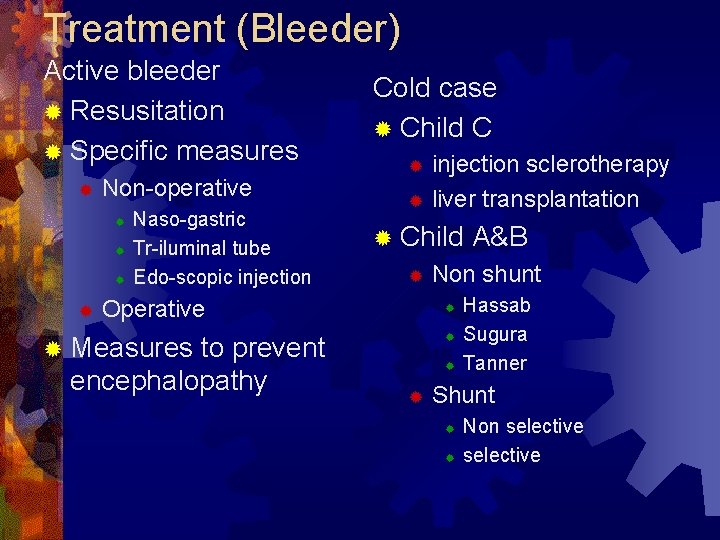
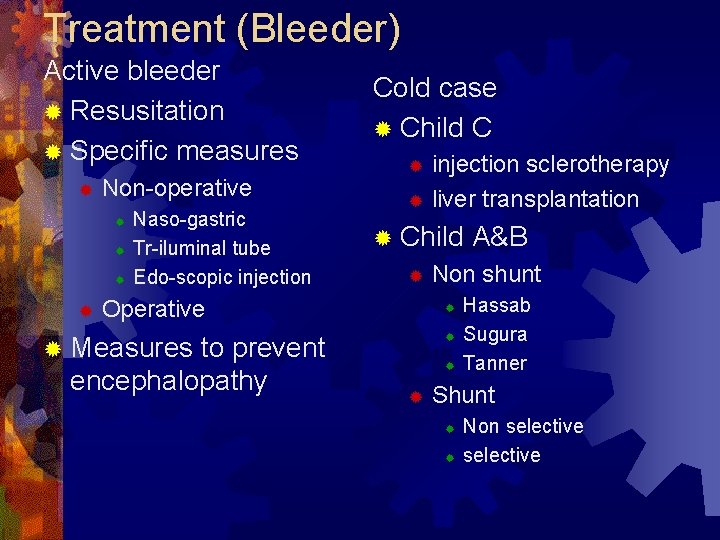
Treatment (Bleeder) Active bleeder ® Resusitation ® Specific measures ® Non-operative ® ® Naso-gastric Tr-iluminal tube Edo-scopic injection Cold case ® Child C injection sclerotherapy ® liver transplantation ® ® Child ® Operative to prevent encephalopathy Non shunt ® ® ® Measures ® ® A&B Hassab Sugura Tanner Shunt ® ® Non selective
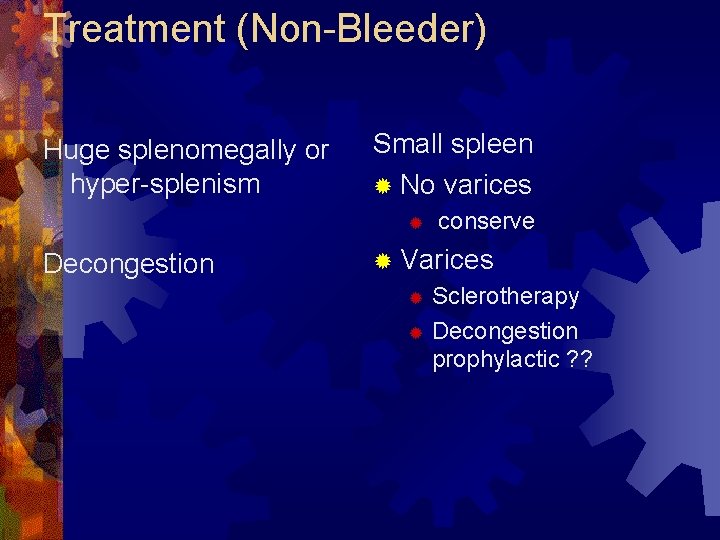
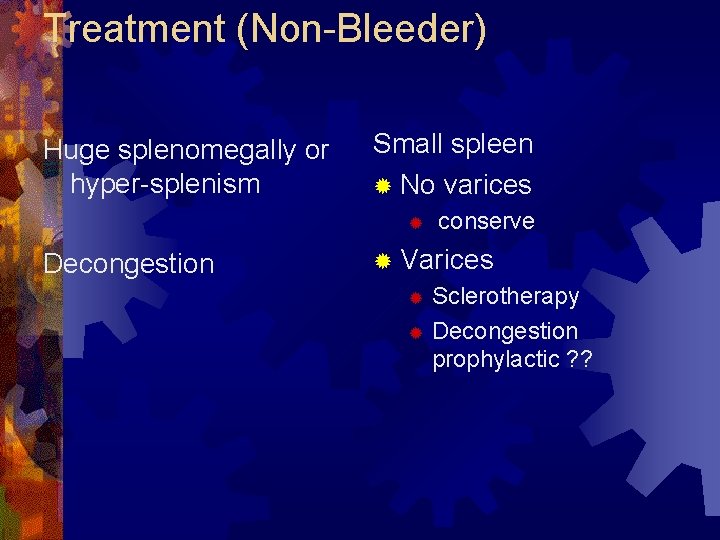
Treatment (Non-Bleeder) Huge splenomegally or hyper-splenism Small spleen ® No varices ® Decongestion conserve ® Varices Sclerotherapy ® Decongestion prophylactic ? ? ®
Treatment (Bleeder) Active bleeder ® Resusitation ® Specific measures ® Non-operative ® ® Naso-gastric Tr-iluminal tube Edo-scopic injection Operative ® Measures to prevent encephalopathy
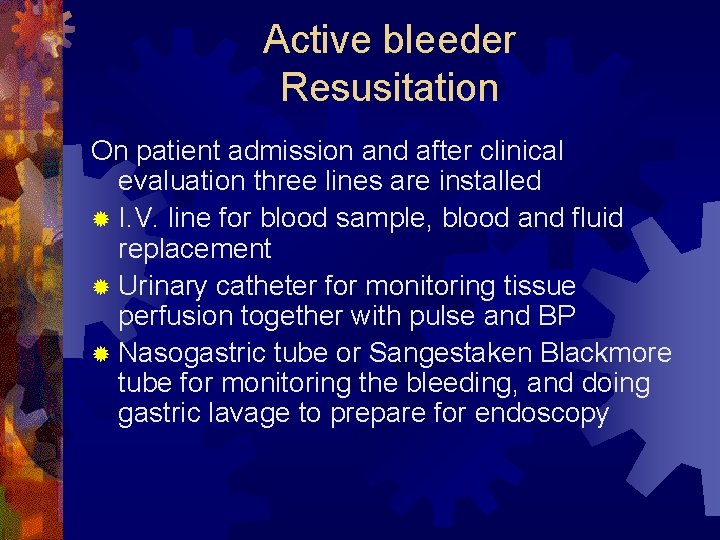
Active bleeder Resusitation On patient admission and after clinical evaluation three lines are installed ® I. V. line for blood sample, blood and fluid replacement ® Urinary catheter for monitoring tissue perfusion together with pulse and BP ® Nasogastric tube or Sangestaken Blackmore tube for monitoring the bleeding, and doing gastric lavage to prepare for endoscopy
Active bleeder Resusitation Resuscitation with transfusion of 1. Colloids (blood) and 2. Crystalloids (Ringer, or lactated Ringer or saline solutions) at the same time with monitoring the blood pressure, pulse and urinary output.
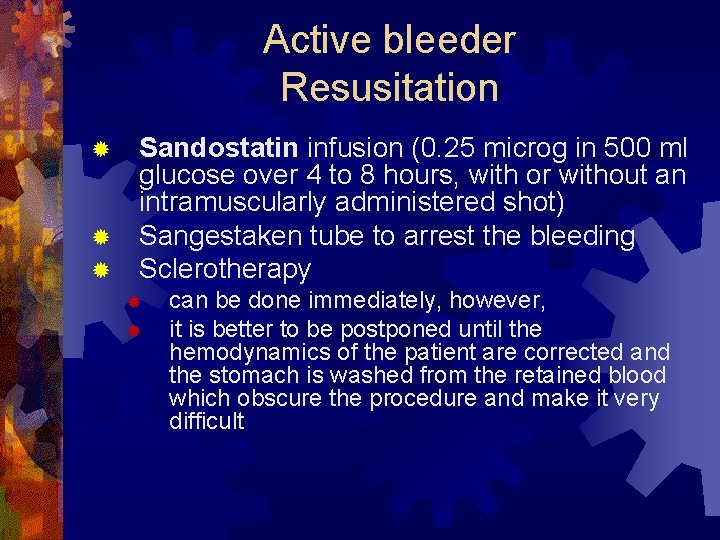
Active bleeder Resusitation Sandostatin infusion (0. 25 microg in 500 ml glucose over 4 to 8 hours, with or without an intramuscularly administered shot) ® Sangestaken tube to arrest the bleeding ® Sclerotherapy ® ® ® can be done immediately, however, it is better to be postponed until the hemodynamics of the patient are corrected and the stomach is washed from the retained blood which obscure the procedure and make it very difficult


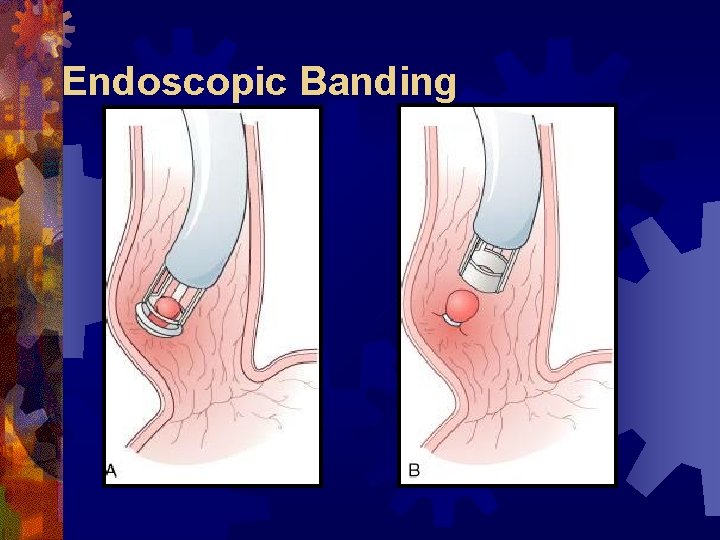
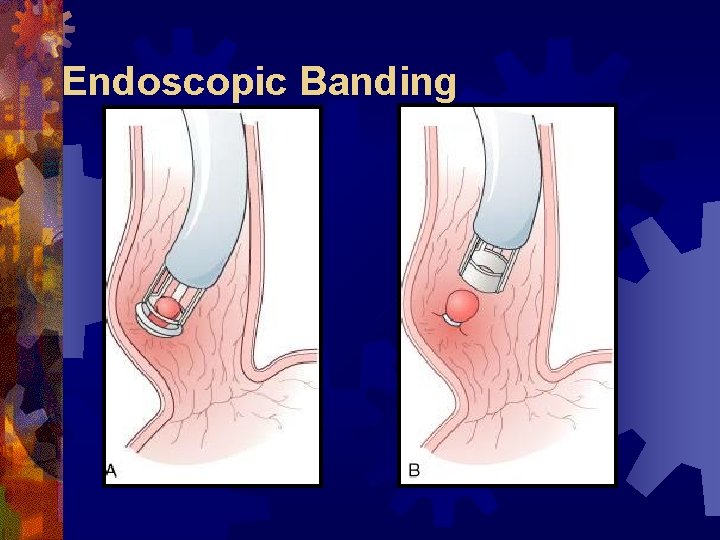
Endoscopic Banding

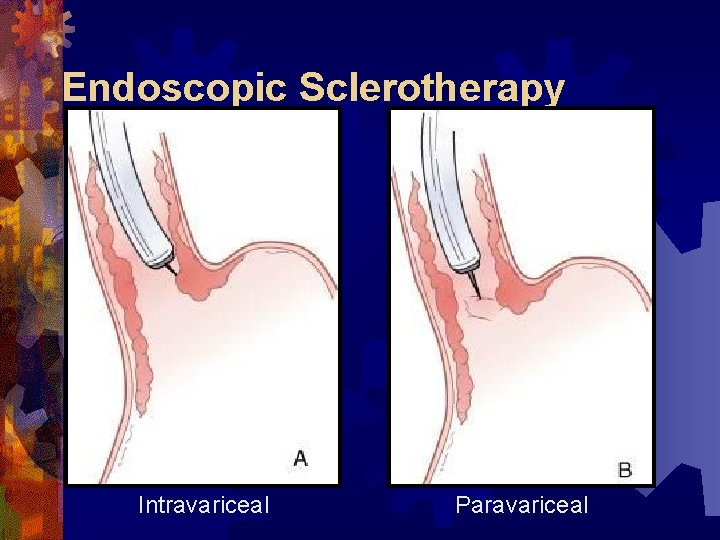
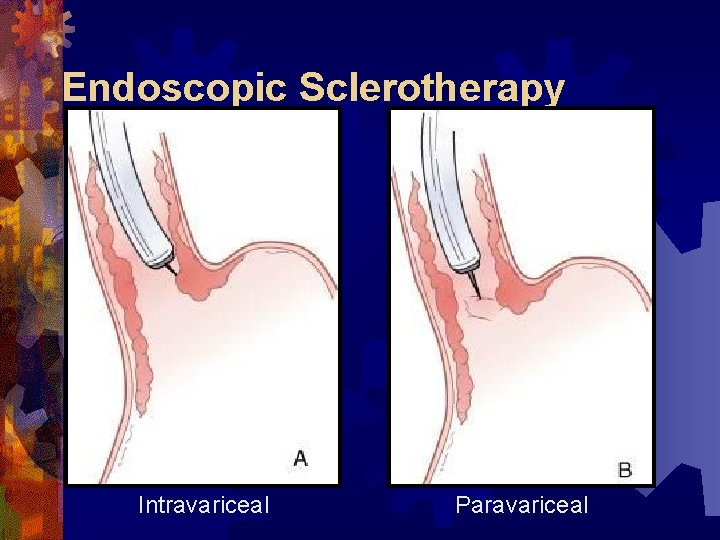
Endoscopic Sclerotherapy Intravariceal Paravariceal
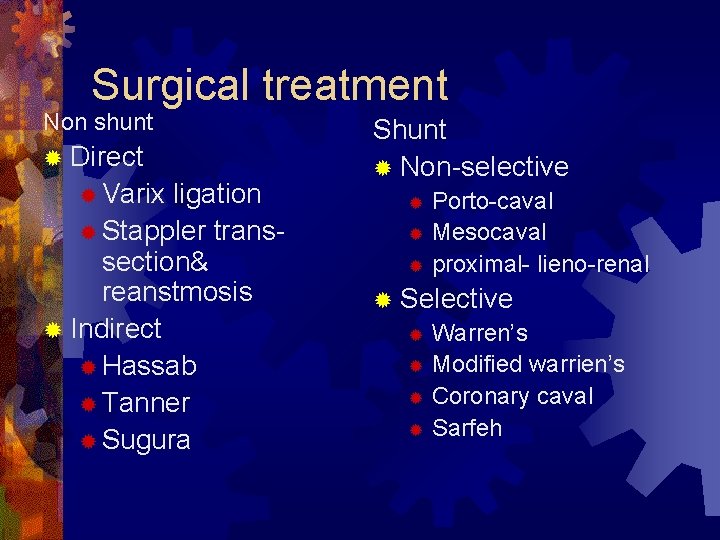
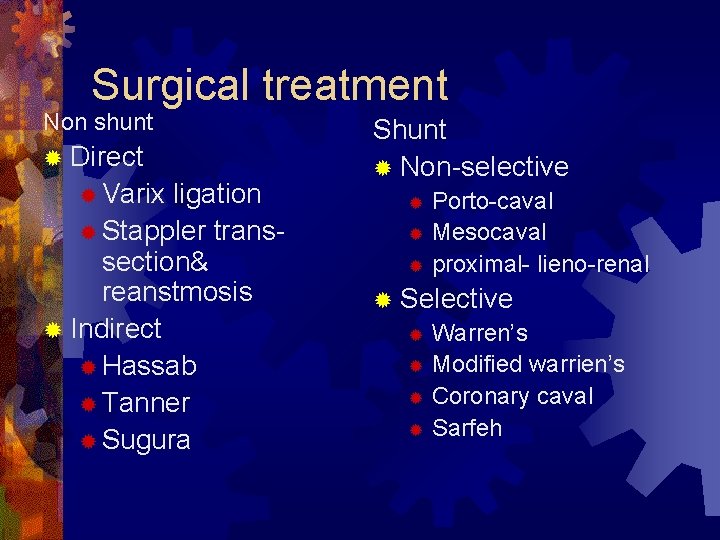
Surgical treatment Non shunt ® Direct ® Varix ligation ® Stappler transsection& reanstmosis ® Indirect ® Hassab ® Tanner ® Sugura Shunt ® Non-selective Porto-caval ® Mesocaval ® proximal- lieno-renal ® ® Selective ® Warren’s ® Modified warrien’s ® Coronary caval ® Sarfeh
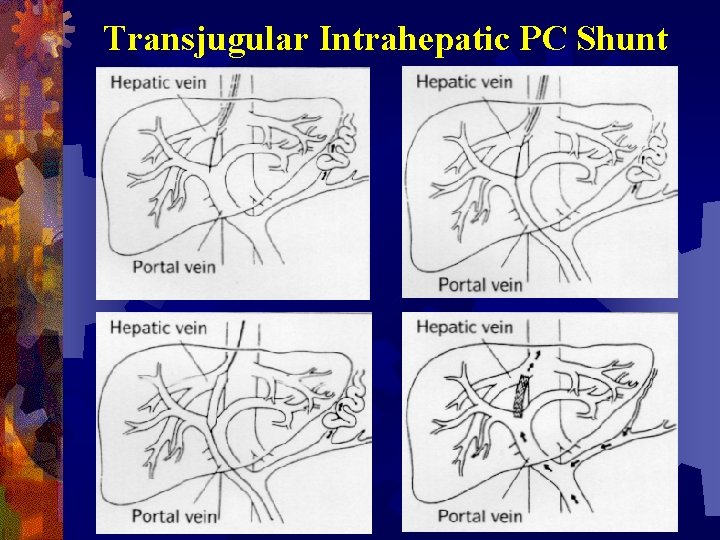
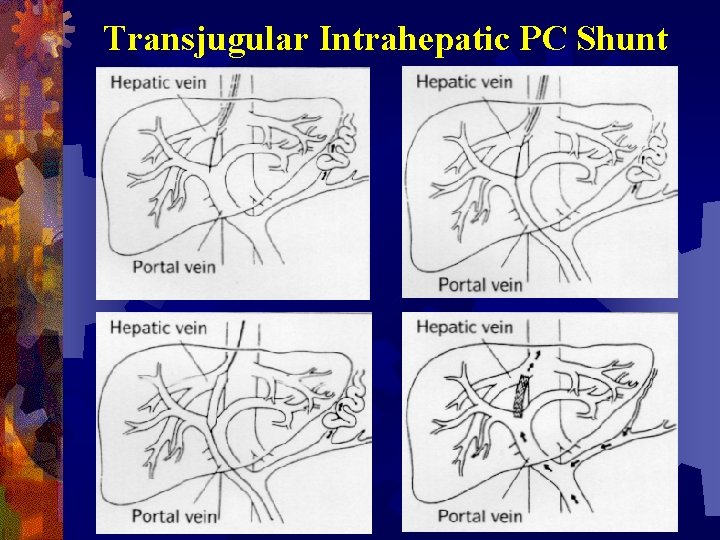
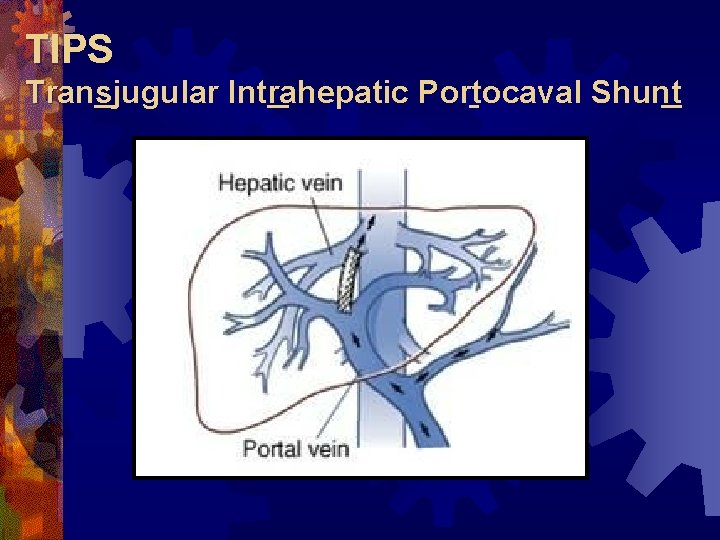
Transjugular Intrahepatic PC Shunt
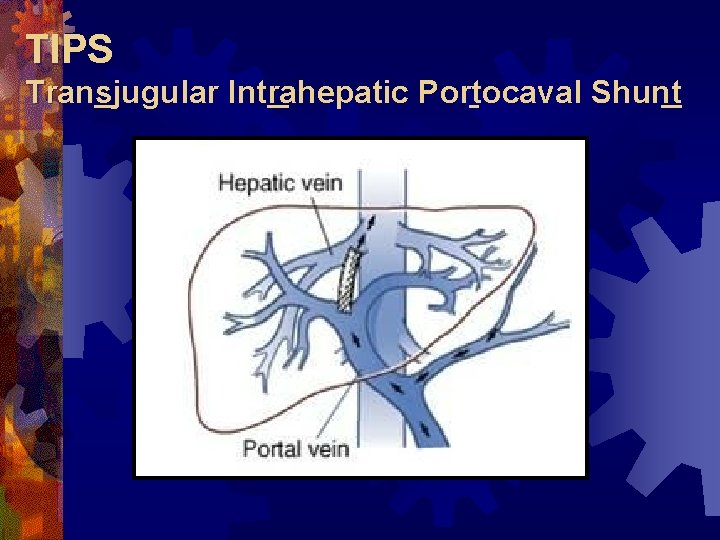
TIPS Transjugular Intrahepatic Portocaval Shunt
TIPS
TIPS
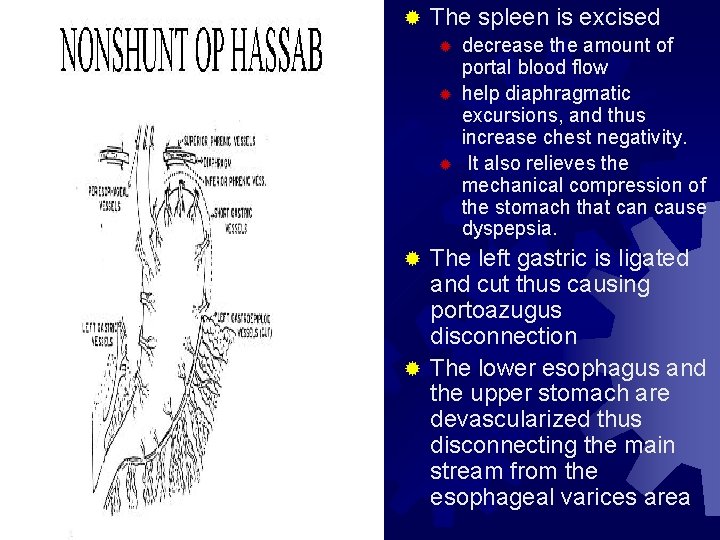
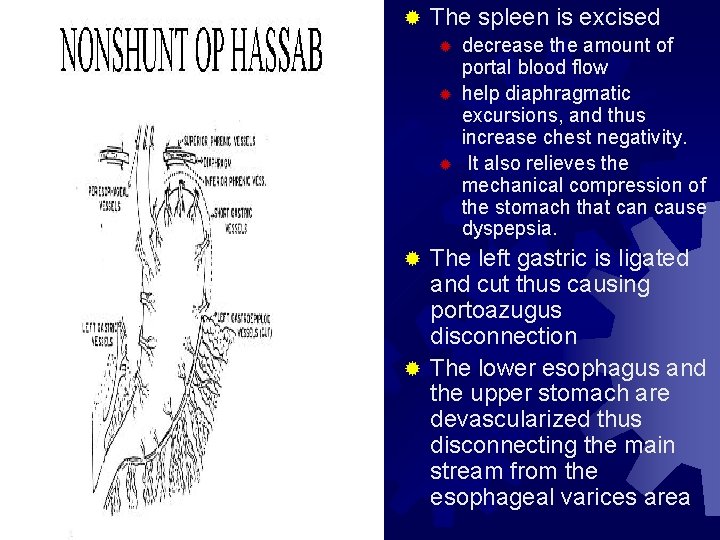
® The spleen is excised ® ® ® decrease the amount of portal blood flow help diaphragmatic excursions, and thus increase chest negativity. It also relieves the mechanical compression of the stomach that can cause dyspepsia. The left gastric is ligated and cut thus causing portoazugus disconnection ® The lower esophagus and the upper stomach are devascularized thus disconnecting the main stream from the esophageal varices area ®
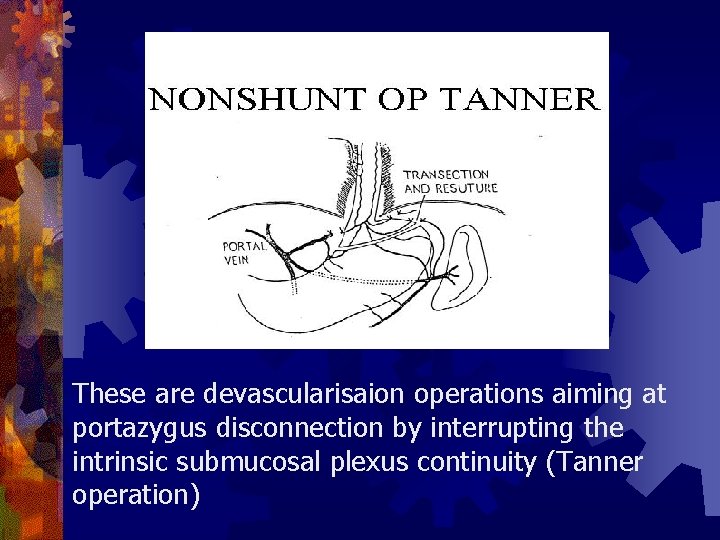
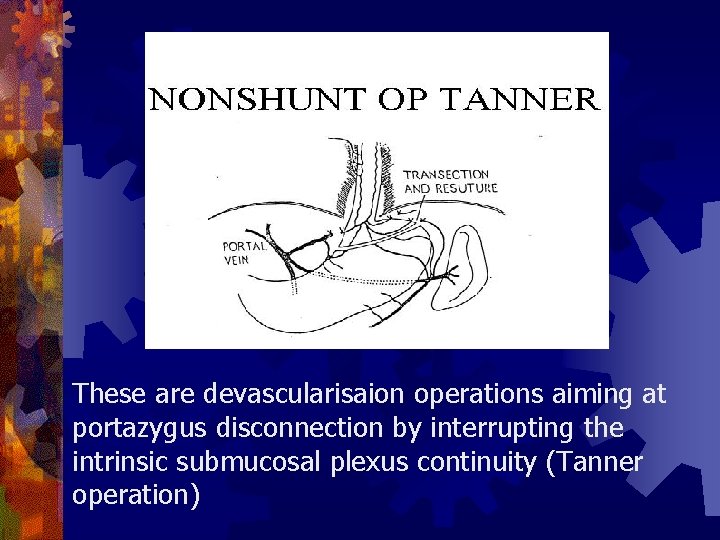
These are devascularisaion operations aiming at portazygus disconnection by interrupting the intrinsic submucosal plexus continuity (Tanner operation)
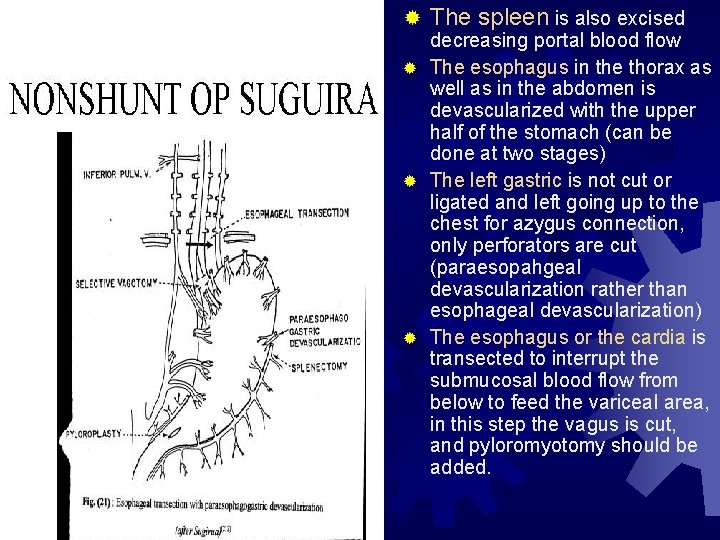
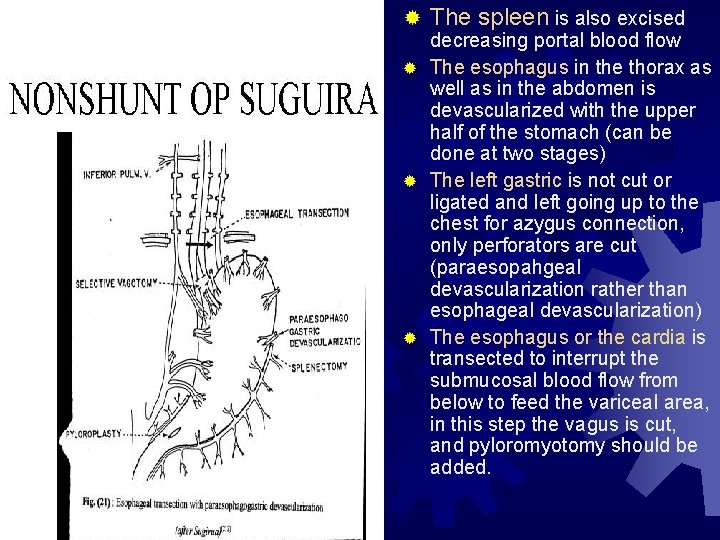
® The spleen is also excised decreasing portal blood flow ® The esophagus in the thorax as well as in the abdomen is devascularized with the upper half of the stomach (can be done at two stages) ® The left gastric is not cut or ligated and left going up to the chest for azygus connection, only perforators are cut (paraesopahgeal devascularization rather than esophageal devascularization) ® The esophagus or the cardia is transected to interrupt the submucosal blood flow from below to feed the variceal area, in this step the vagus is cut, and pyloromyotomy should be added.
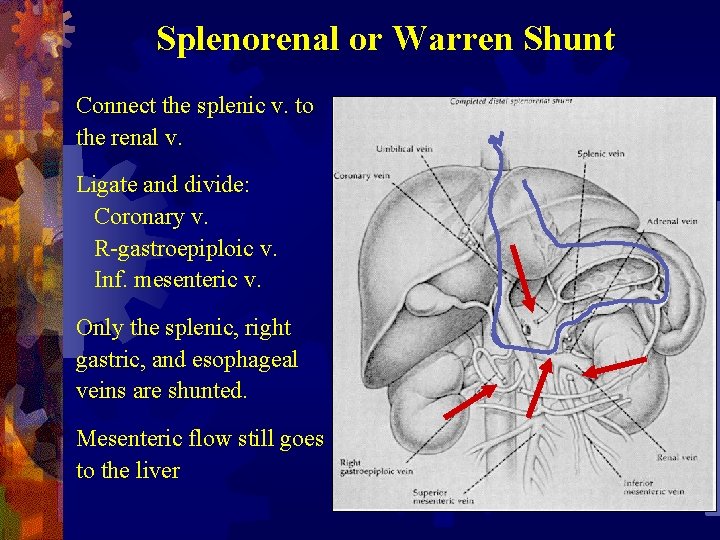
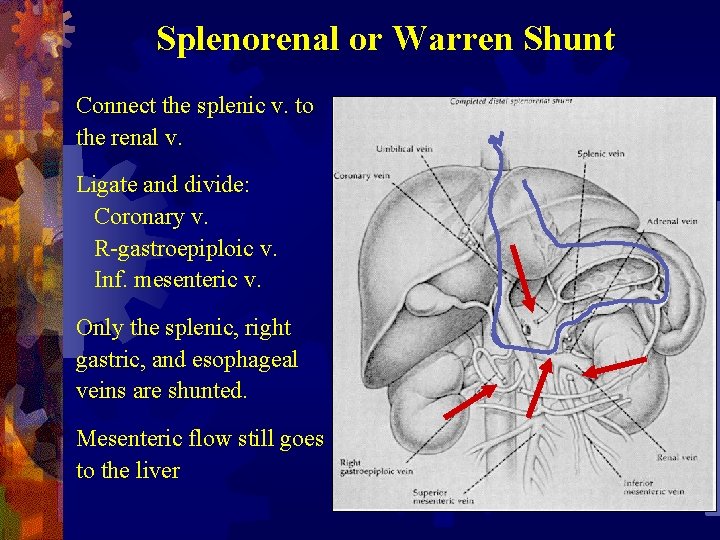
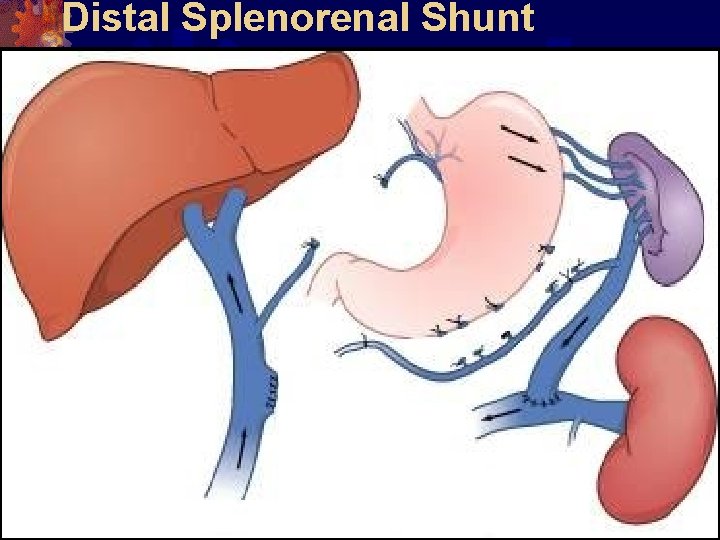
Splenorenal or Warren Shunt Connect the splenic v. to the renal v. Ligate and divide: Coronary v. R-gastroepiploic v. Inf. mesenteric v. Only the splenic, right gastric, and esophageal veins are shunted. Mesenteric flow still goes to the liver
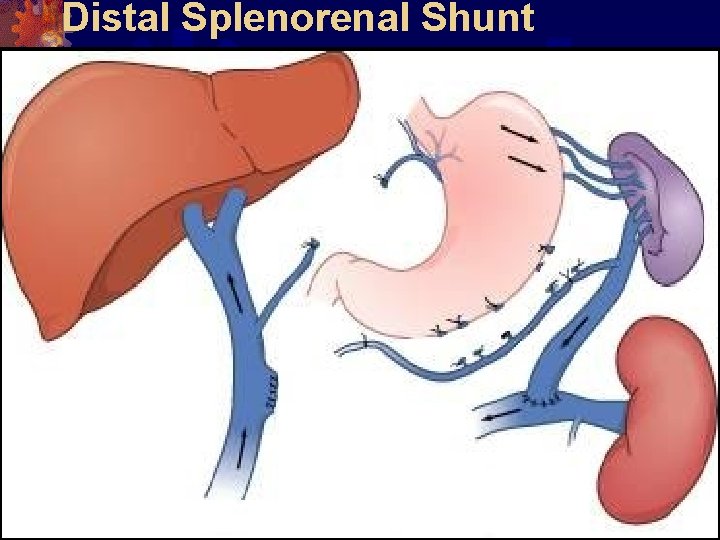
Distal Splenorenal Shunt










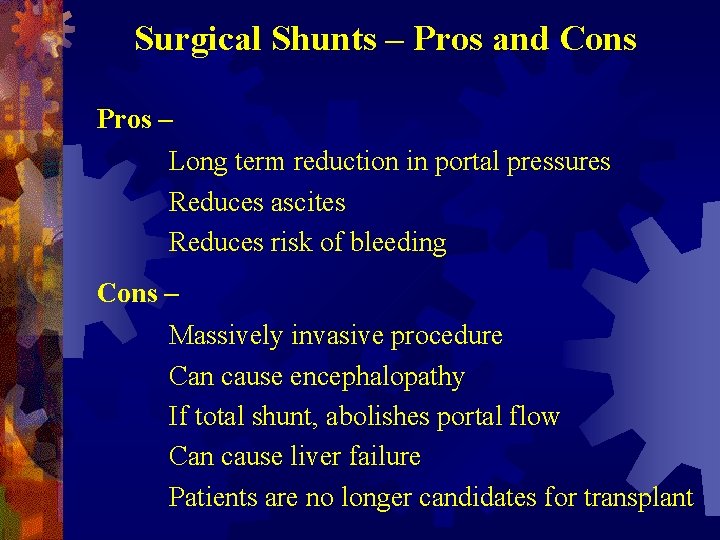
Surgical Shunts – Pros and Cons Pros – Long term reduction in portal pressures Reduces ascites Reduces risk of bleeding Cons – Massively invasive procedure Can cause encephalopathy If total shunt, abolishes portal flow Can cause liver failure Patients are no longer candidates for transplant
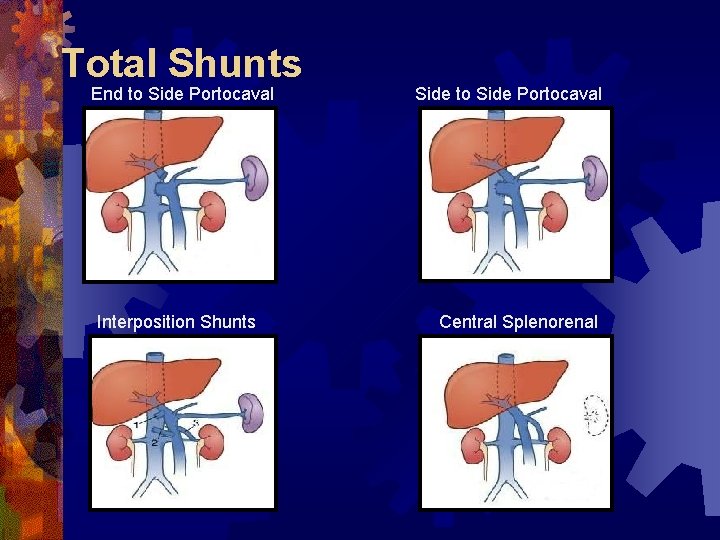
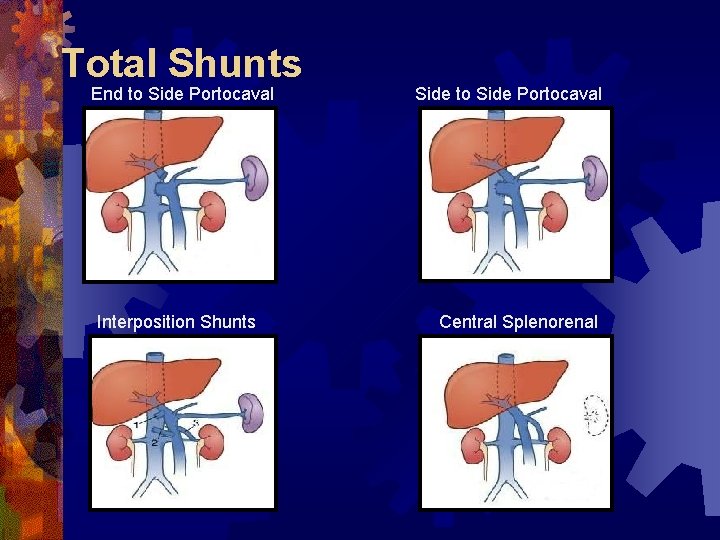
Total Shunts End to Side Portocaval Interposition Shunts Side to Side Portocaval Central Splenorenal
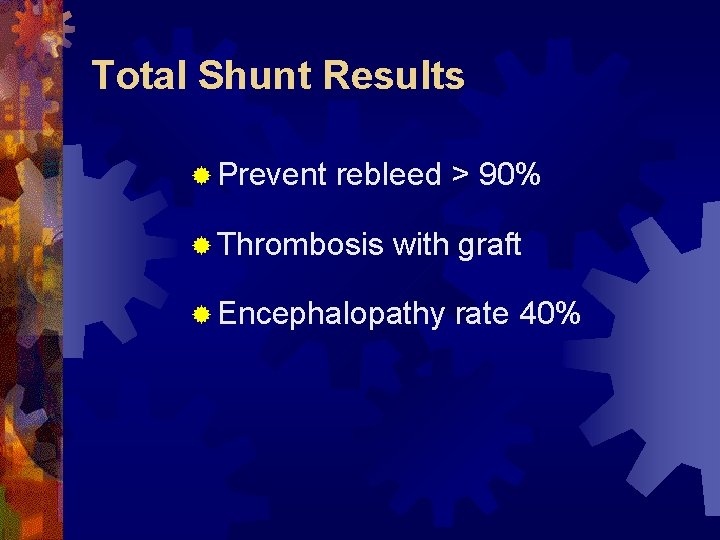
Total Shunt Results ® Prevent rebleed > 90% ® Thrombosis with graft ® Encephalopathy rate 40%


 Building management system definition
Building management system definition Walid radwan
Walid radwan Diadynamic
Diadynamic Walid saadi
Walid saadi Walid radwan
Walid radwan Walid abou jaoude
Walid abou jaoude Complications of hydrocephalus
Complications of hydrocephalus Walid radwan
Walid radwan Seldinger technique
Seldinger technique Walid radwan
Walid radwan Walid radwan
Walid radwan Walid radwan
Walid radwan Dr walid saghir
Dr walid saghir Presinusoidal portal hypertension
Presinusoidal portal hypertension Features of cld
Features of cld Ascites veins
Ascites veins Nursing management of portal hypertension
Nursing management of portal hypertension Symptoms of portal hypertension
Symptoms of portal hypertension Portal hypertension mayo clinic
Portal hypertension mayo clinic Splenomegaly liver cirrhosis
Splenomegaly liver cirrhosis Hypertension
Hypertension Systemic vascular resistance
Systemic vascular resistance Stages of pulmonary hypertension
Stages of pulmonary hypertension Dyslipidemia pathophysiology
Dyslipidemia pathophysiology Hypertension intracrânienne
Hypertension intracrânienne Malignant hypertention
Malignant hypertention Pulmonary hypertension definition
Pulmonary hypertension definition Faa caci asthma
Faa caci asthma Hypertensive emergency vs urgency
Hypertensive emergency vs urgency Causes of secondary hypertension
Causes of secondary hypertension Pulmonary hypertension
Pulmonary hypertension Non pharmacological management of hypertension
Non pharmacological management of hypertension Signe du flot genou
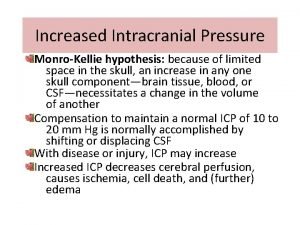
Signe du flot genou Signs of increased intracranial pressure
Signs of increased intracranial pressure Vital signs cpr
Vital signs cpr Case scenario for hypertension
Case scenario for hypertension Pico question examples hypertension
Pico question examples hypertension Gestational hypertension
Gestational hypertension Hypertensive urgency
Hypertensive urgency Conclusion of hypertension
Conclusion of hypertension Malignant hypertension ppt
Malignant hypertension ppt Definition of hypertension
Definition of hypertension Classification of hypertension
Classification of hypertension Medslide
Medslide Dianne zwicke
Dianne zwicke Chief complaint present illness
Chief complaint present illness Bmpr gene
Bmpr gene Hypertension vs hypotension
Hypertension vs hypotension Blood pressure medication dosage chart
Blood pressure medication dosage chart Stage 1 hypertension
Stage 1 hypertension Isolated systolic hypertension
Isolated systolic hypertension Urgency hypertension
Urgency hypertension Health coaches for hypertension control
Health coaches for hypertension control Hypertension
Hypertension Conclusion of hypertension
Conclusion of hypertension Standardized office bp measurement
Standardized office bp measurement Conclusion of hypertension
Conclusion of hypertension Malignant hypertension management
Malignant hypertension management Jnc 8 hypertension classification
Jnc 8 hypertension classification Masked hypertension
Masked hypertension Ttp disease
Ttp disease Hypertension
Hypertension Chd pulmonary hypertension
Chd pulmonary hypertension Conclusion of hypertension
Conclusion of hypertension Cruveilhier sign varicose veins
Cruveilhier sign varicose veins Mitral stenosis pulmonary hypertension
Mitral stenosis pulmonary hypertension Nt pro brain natriuretic peptide
Nt pro brain natriuretic peptide Nursing blood pressure assessment
Nursing blood pressure assessment Modifiable risk factors for hypertension
Modifiable risk factors for hypertension Traitement hypertension
Traitement hypertension Rules of halves in hypertension
Rules of halves in hypertension Jnc7
Jnc7 Sohil rangwala
Sohil rangwala Conclusion of hypertension
Conclusion of hypertension Nervous mechanism for regulation of blood pressure
Nervous mechanism for regulation of blood pressure Definition of hypertension
Definition of hypertension