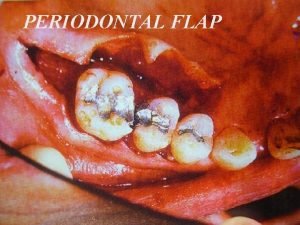
Periodontal Flap Surgery Purpose 1 To gain access


- Slides: 60
Periodontal Flap Surgery
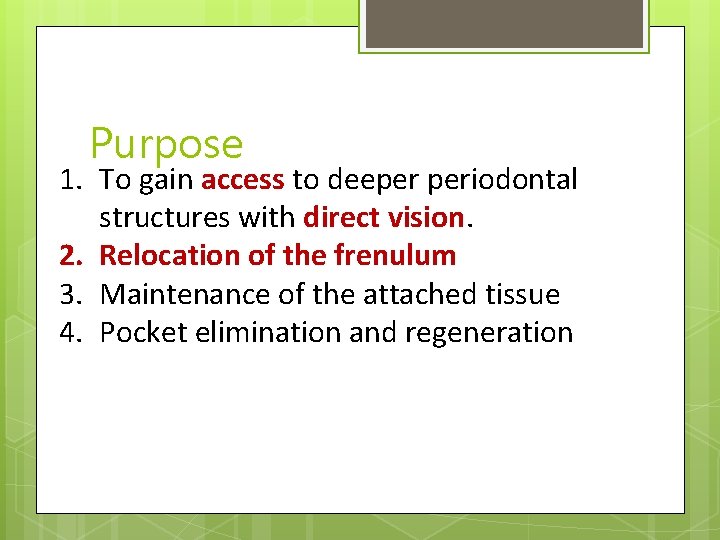
Purpose 1. To gain access to deeper periodontal structures with direct vision. 2. Relocation of the frenulum 3. Maintenance of the attached tissue 4. Pocket elimination and regeneration
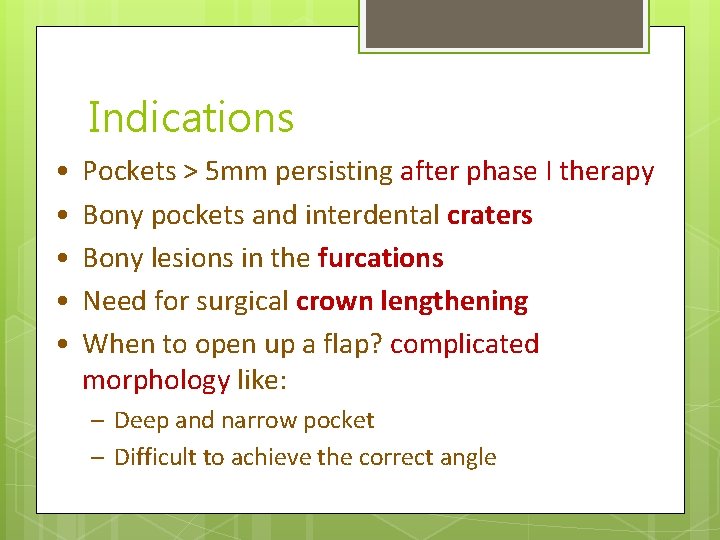
Indications • • • Pockets > 5 mm persisting after phase I therapy Bony pockets and interdental craters Bony lesions in the furcations Need for surgical crown lengthening When to open up a flap? complicated morphology like: – Deep and narrow pocket – Difficult to achieve the correct angle
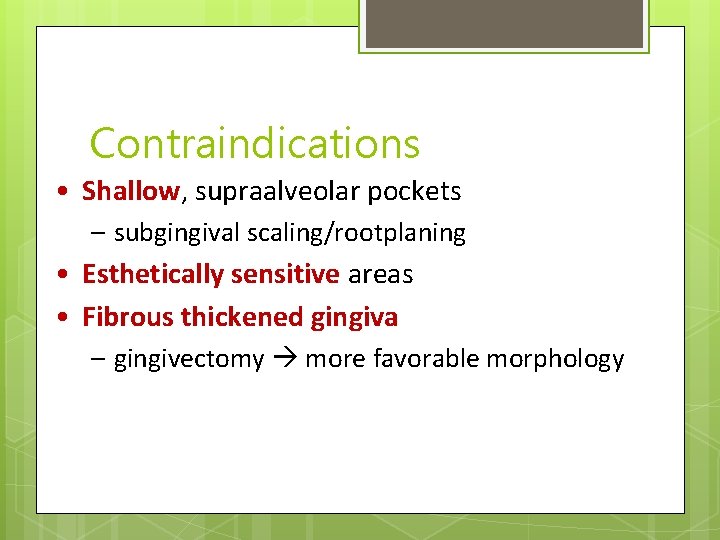
Contraindications • Shallow, supraalveolar pockets – subgingival scaling/rootplaning • Esthetically sensitive areas • Fibrous thickened gingiva – gingivectomy more favorable morphology
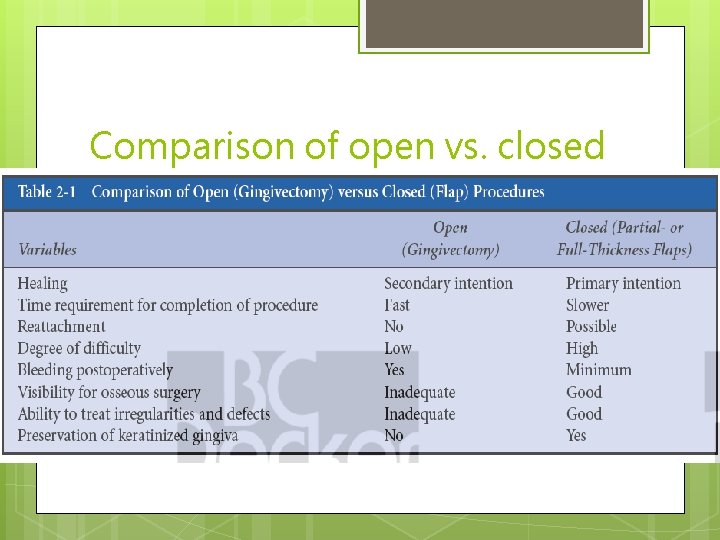
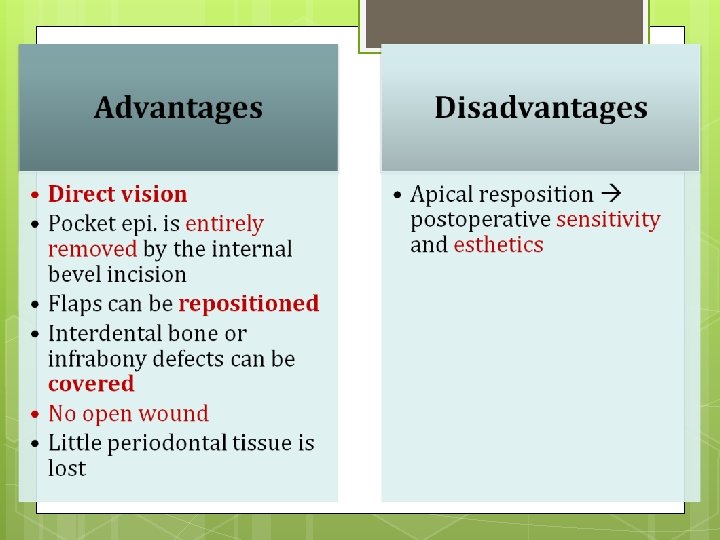
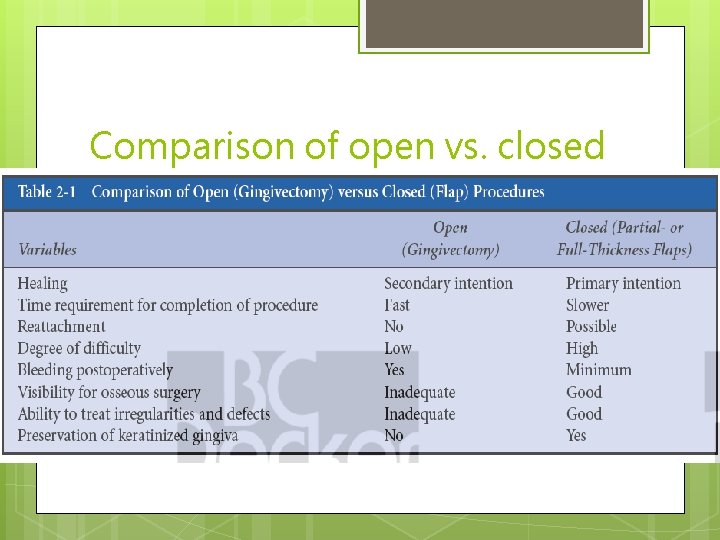
Comparison of open vs. closed
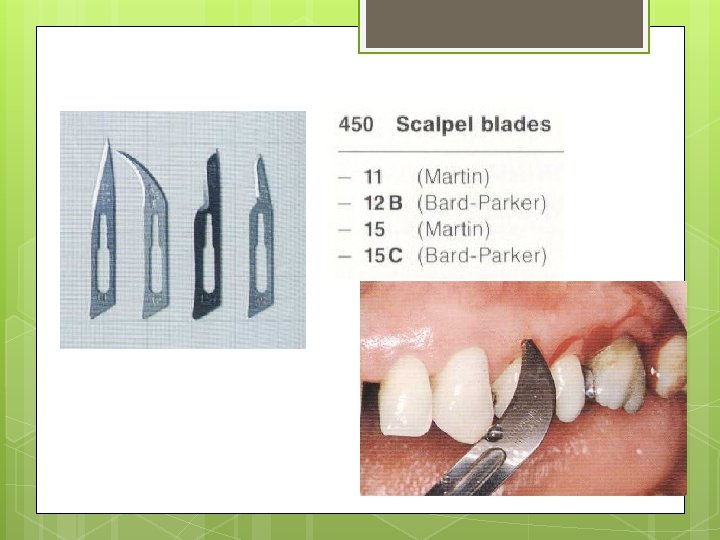
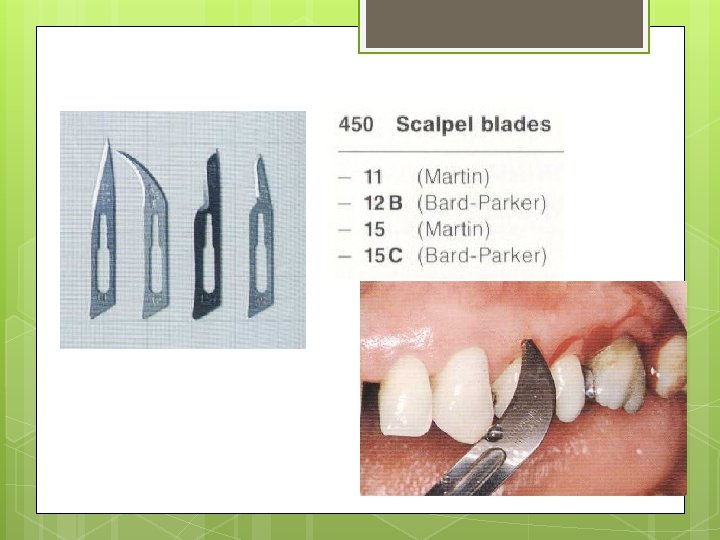
Instruments
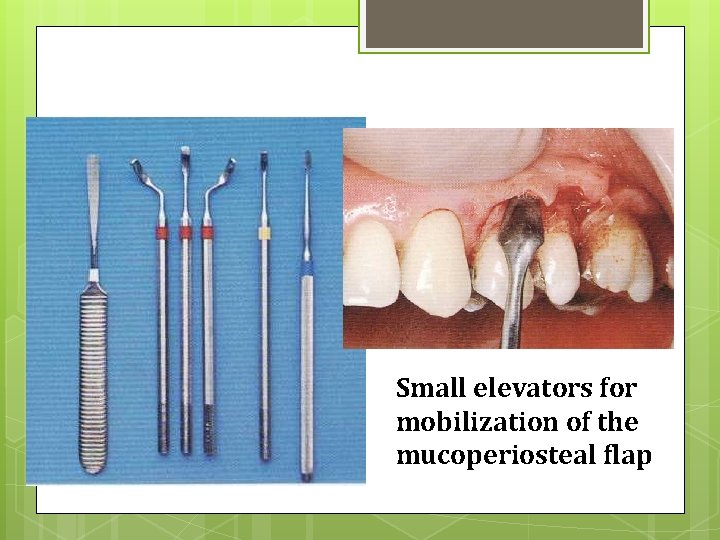
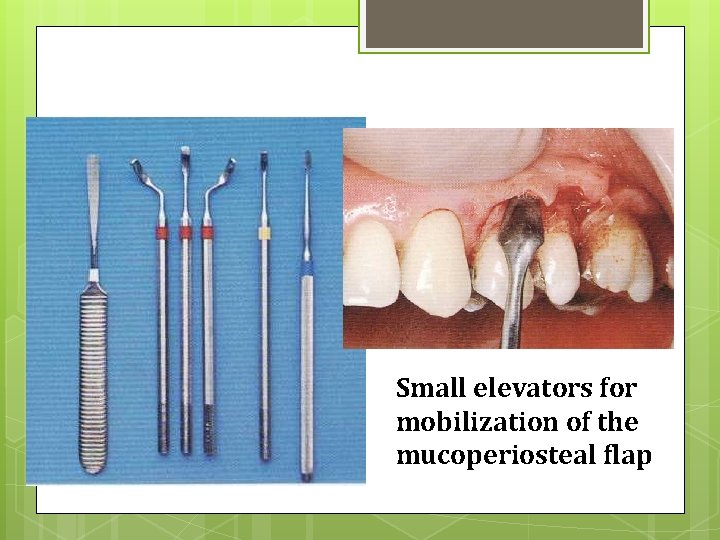
Instruments Small elevators for mobilization of the mucoperiosteal flap
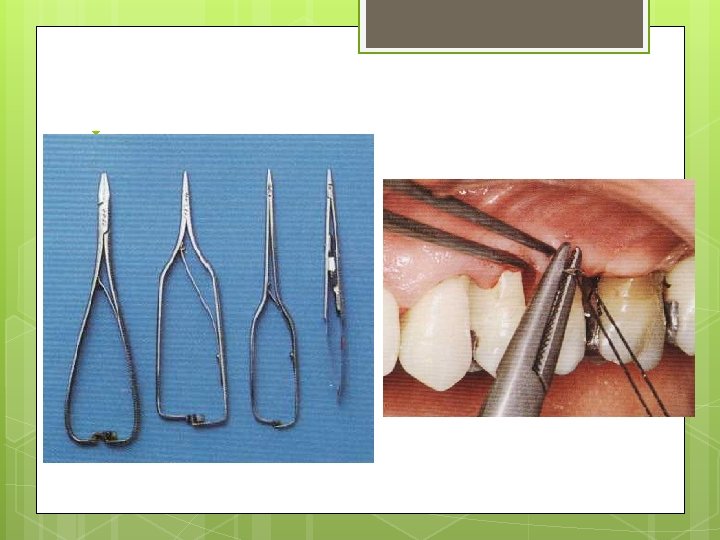
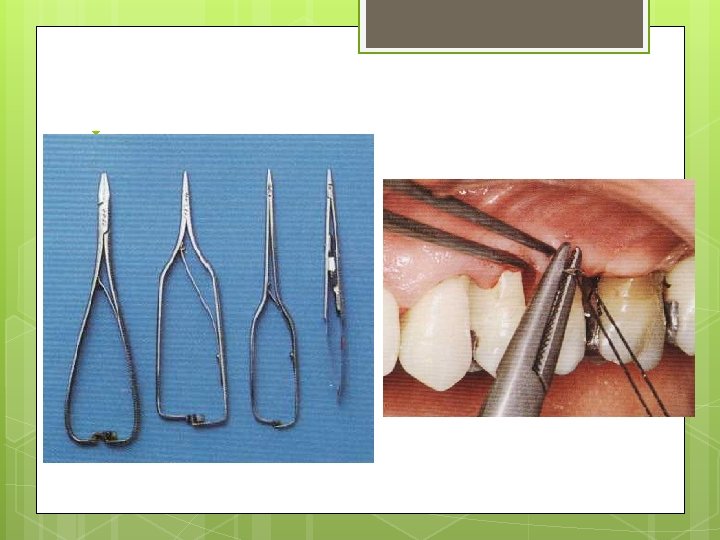
Instruments

• Principles of Flap Design Local flap 1. 2. 3. 4. 5. outlined by a surgical incision carries its own blood supply allows surgical access to underlying tissues can be replaced in the original position can be maintained with sutures and is expected to heal ü Used in oral surgical, periodontic, and endodontic procedures to gain access.
Principles of Flap Design • Complications A. Flap necrosis B. Flap Dehiscence C. Flap Tearing D. Injury to Local Structures
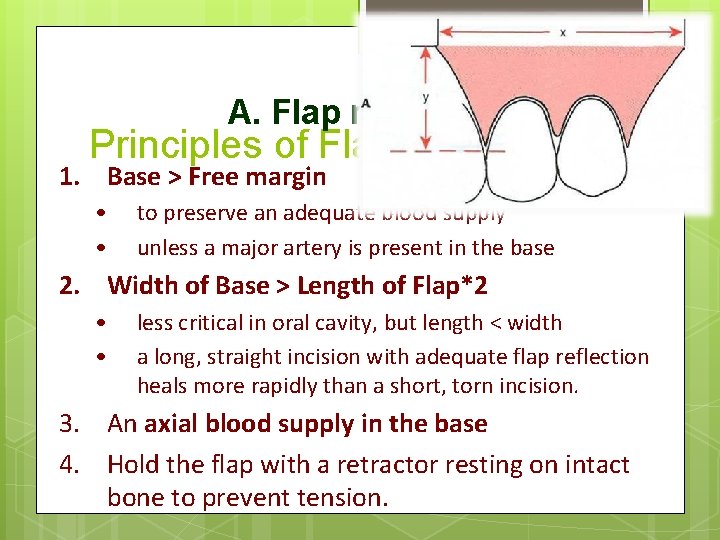
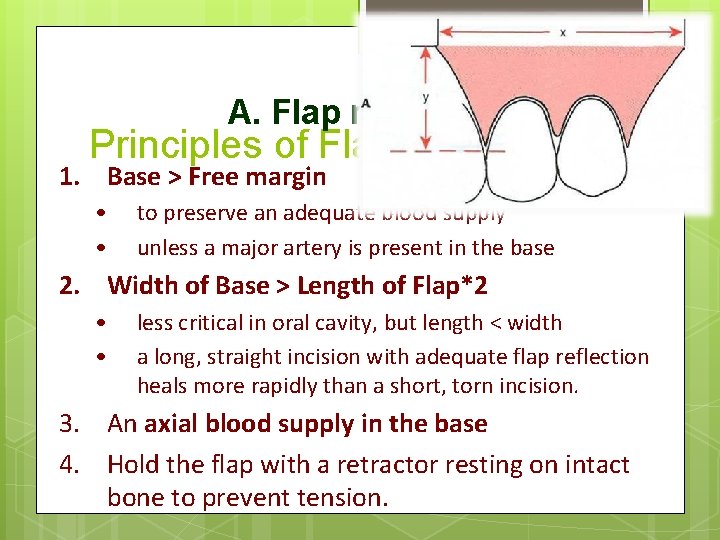
A. Flap necrosis Principles of Flap Design 1. Base > Free margin • • to preserve an adequate blood supply unless a major artery is present in the base 2. Width of Base > Length of Flap*2 • • less critical in oral cavity, but length < width a long, straight incision with adequate flap reflection heals more rapidly than a short, torn incision. 3. An axial blood supply in the base 4. Hold the flap with a retractor resting on intact bone to prevent tension.
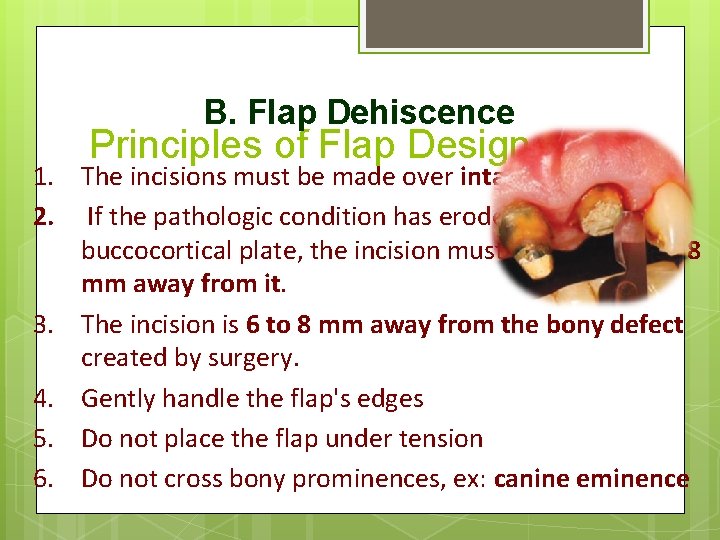
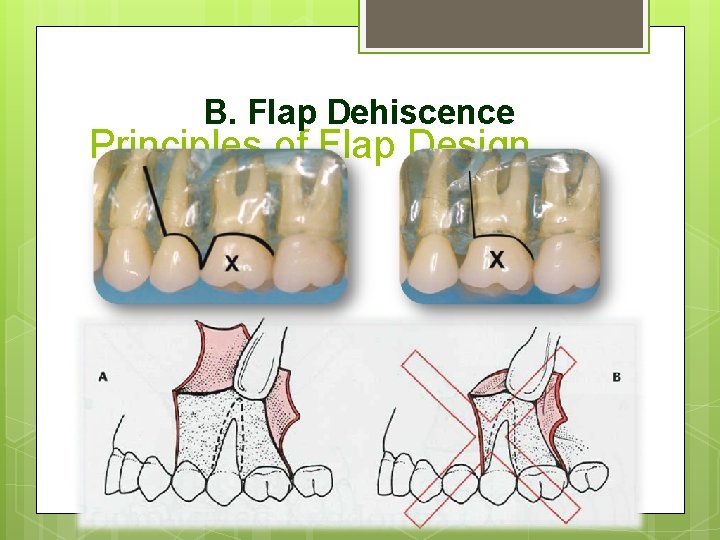
B. Flap Dehiscence Principles of Flap Design 1. The incisions must be made over intact bone 2. If the pathologic condition has eroded the buccocortical plate, the incision must be at least 6 or 8 mm away from it. 3. The incision is 6 to 8 mm away from the bony defect created by surgery. 4. Gently handle the flap's edges 5. Do not place the flap under tension 6. Do not cross bony prominences, ex: canine eminence
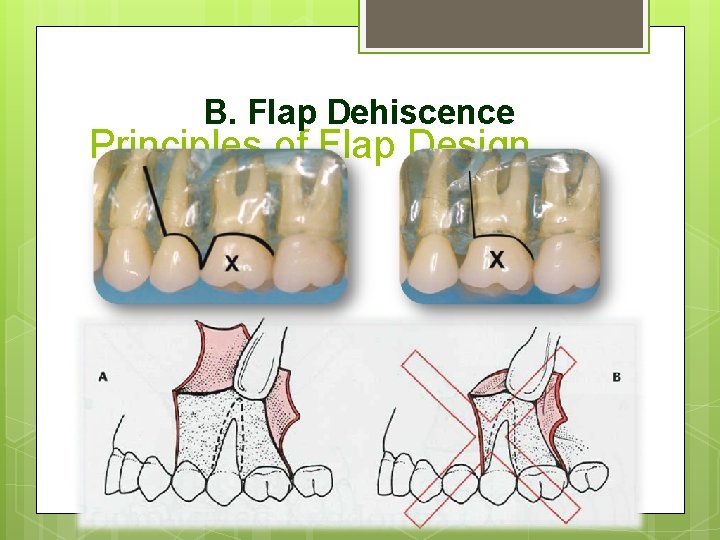
B. Flap Dehiscence Principles of Flap Design
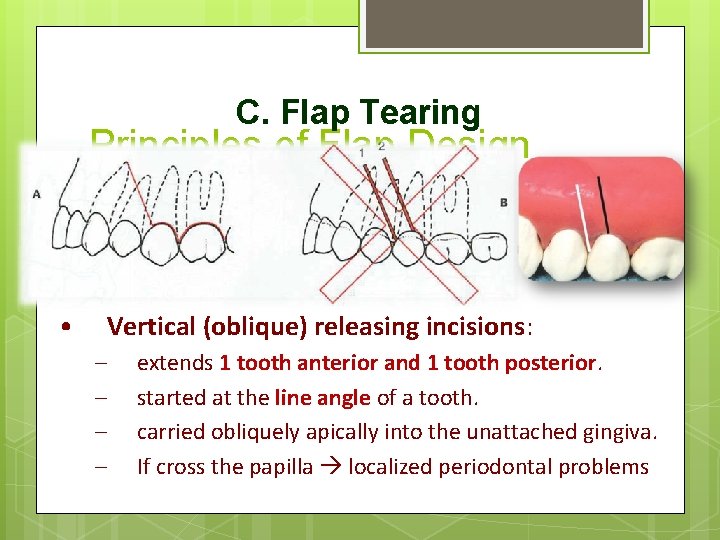
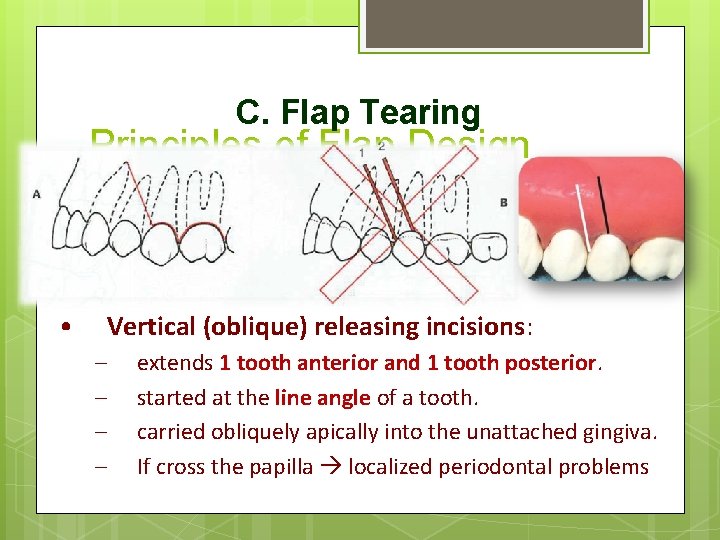
C. Flap Tearing • Principles of Flap Design Envelope flaps – – an incision around the necks of several teeth. extends 2 teeth anterior and 1 tooth posterior. If not provide sufficient access… • Vertical (oblique) releasing incisions: – – extends 1 tooth anterior and 1 tooth posterior. started at the line angle of a tooth. carried obliquely apically into the unattached gingiva. If cross the papilla localized periodontal problems
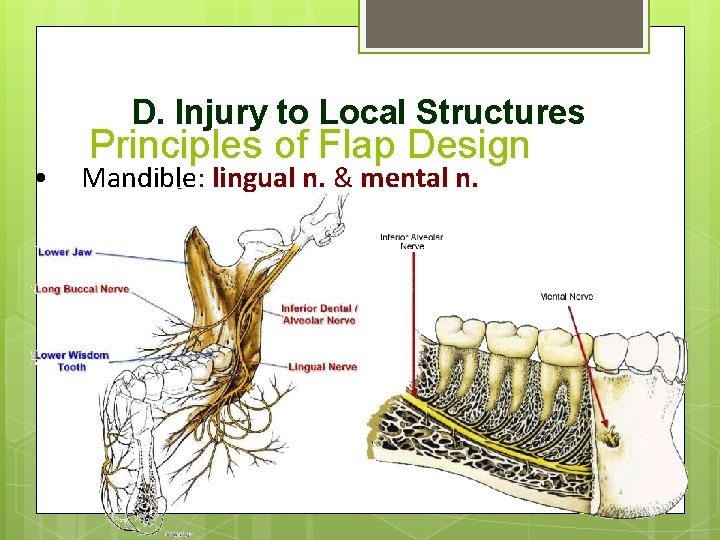
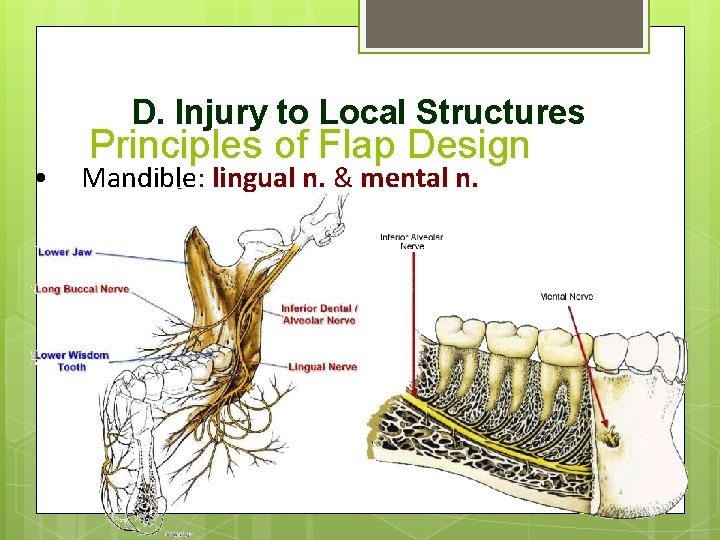
D. Injury to Local Structures • Principles of Flap Design Mandible: lingual n. & mental n.
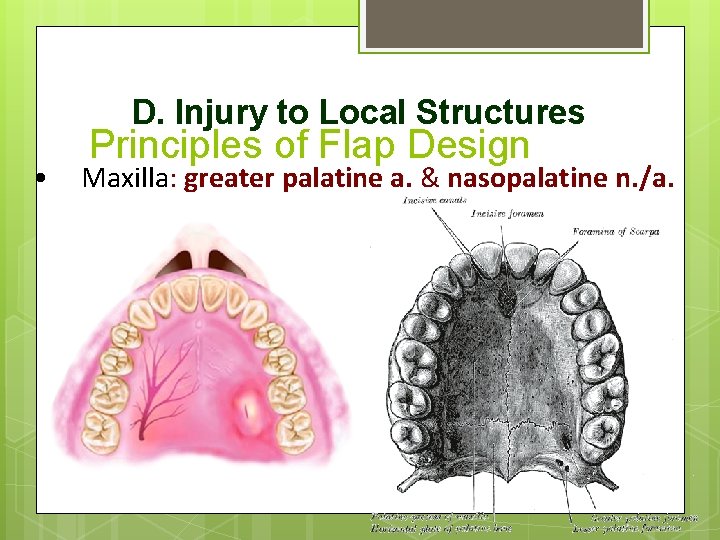
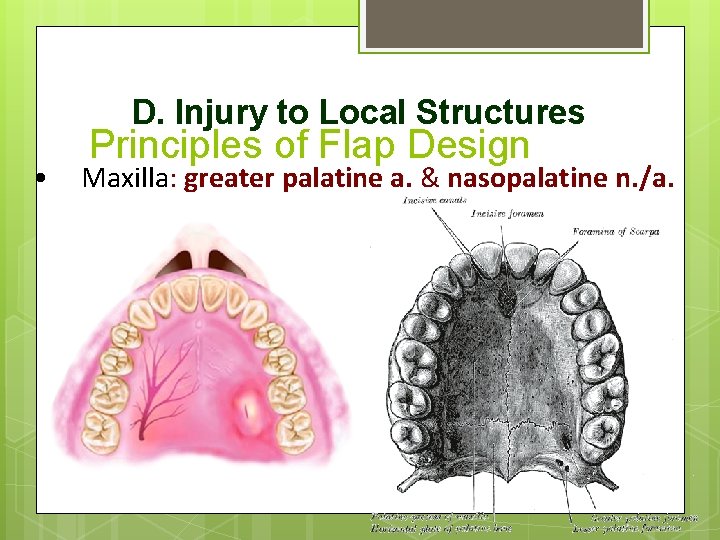
D. Injury to Local Structures • Principles of Flap Design Maxilla: greater palatine a. & nasopalatine n. /a.
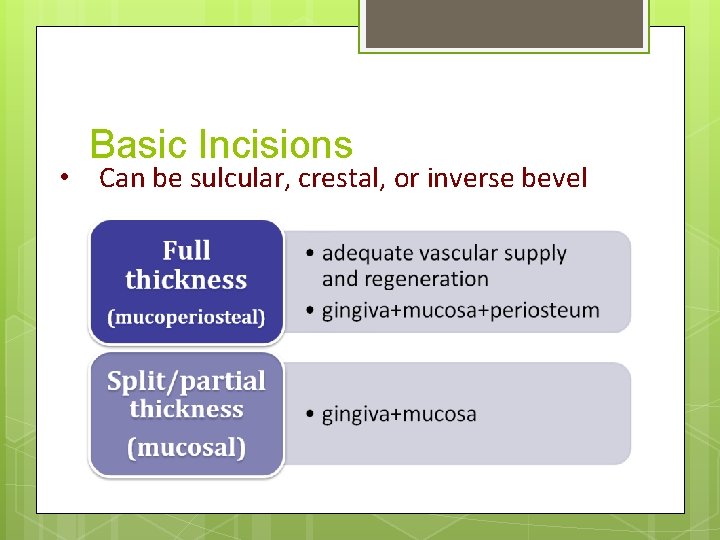
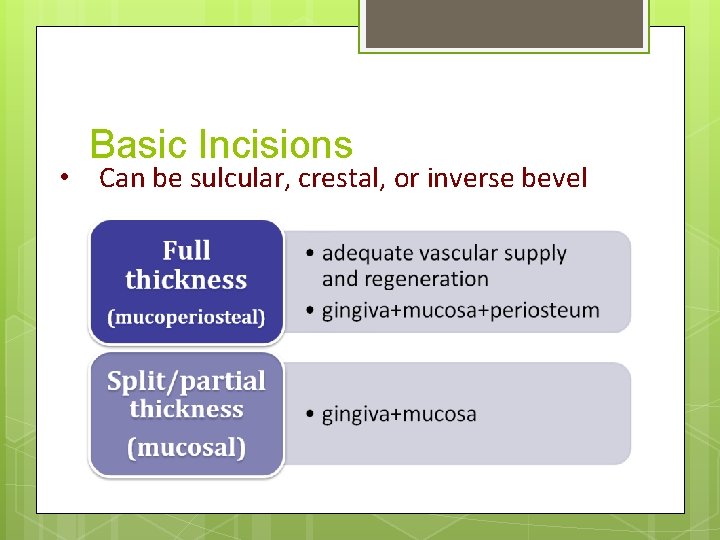
Basic Incisions • Can be sulcular, crestal, or inverse bevel
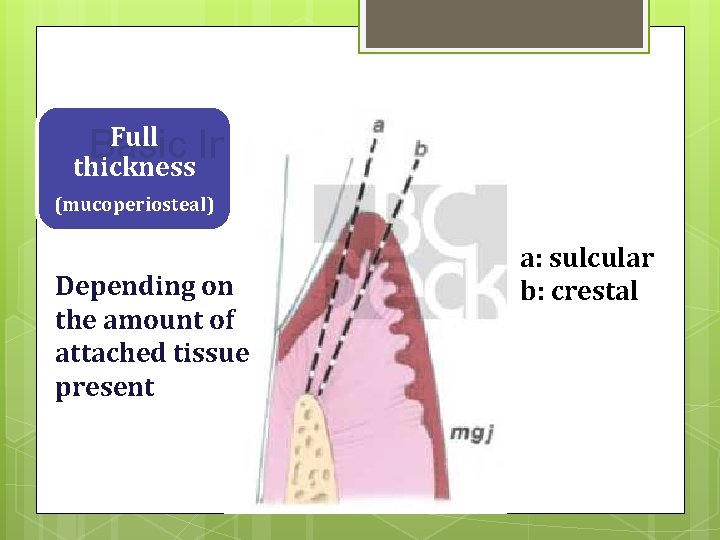
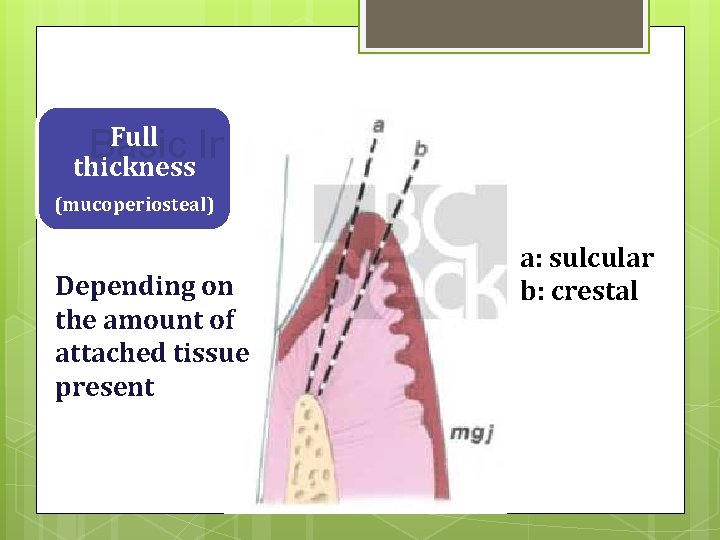
Full Incisions Basic thickness (mucoperiosteal) Depending on the amount of attached tissue present a: sulcular b: crestal
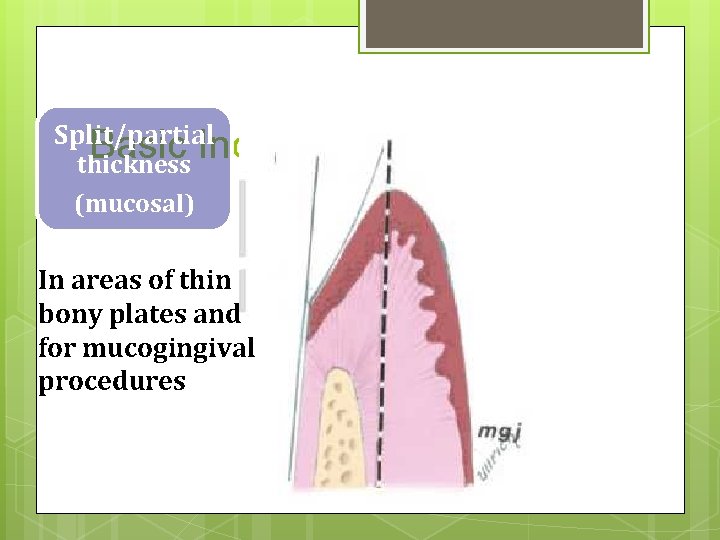
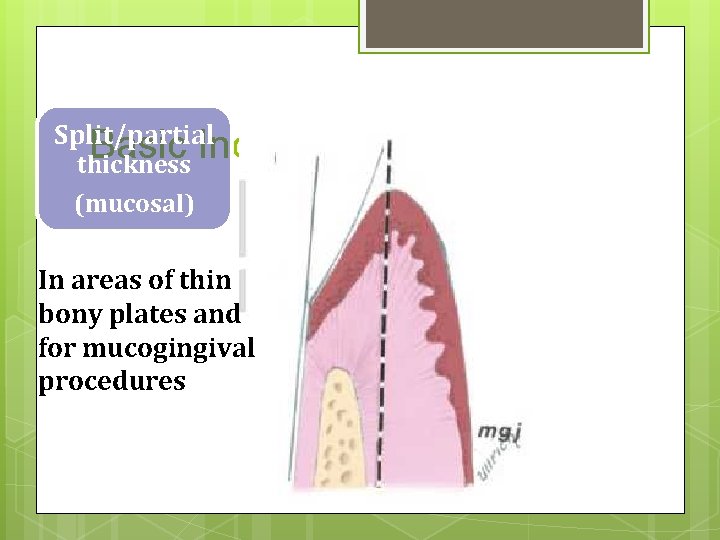
Split/partial Basic Incisions thickness (mucosal) In areas of thin bony plates and for mucogingival procedures
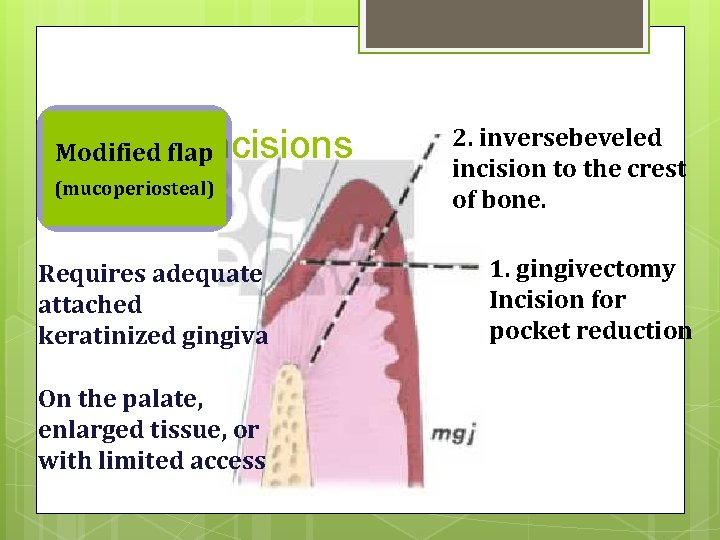
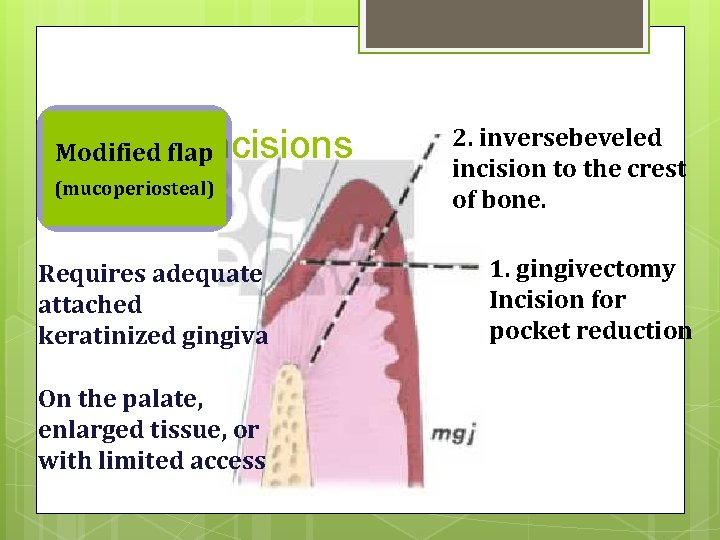
Basicflap. Incisions Modified (mucoperiosteal) Requires adequate attached keratinized gingiva On the palate, enlarged tissue, or with limited access 2. inversebeveled incision to the crest of bone. 1. gingivectomy Incision for pocket reduction
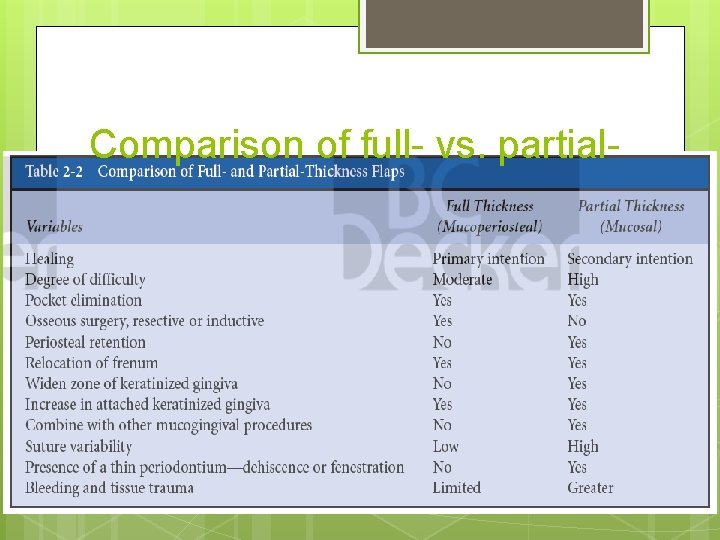
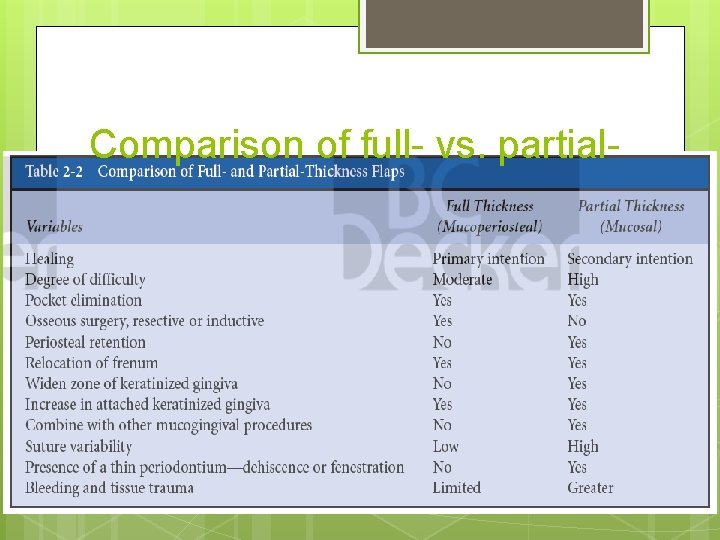
Comparison of full- vs. partial-
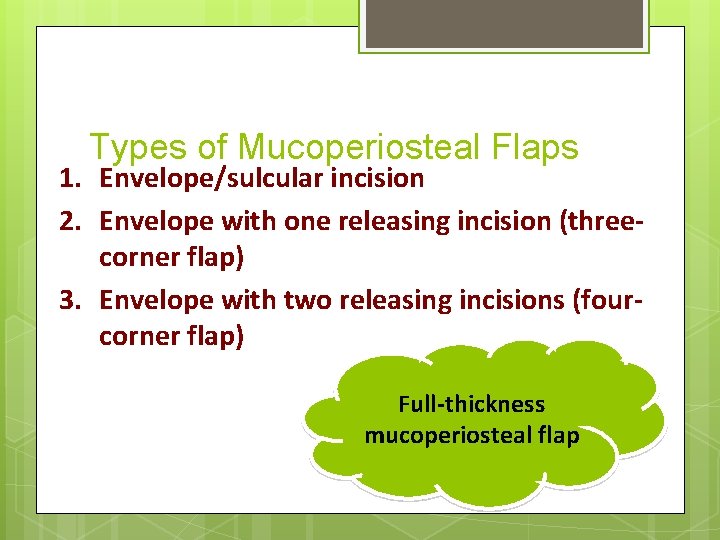
Types of Mucoperiosteal Flaps 1. Envelope/sulcular incision 2. Envelope with one releasing incision (threecorner flap) 3. Envelope with two releasing incisions (fourcorner flap) Full-thickness mucoperiosteal flap
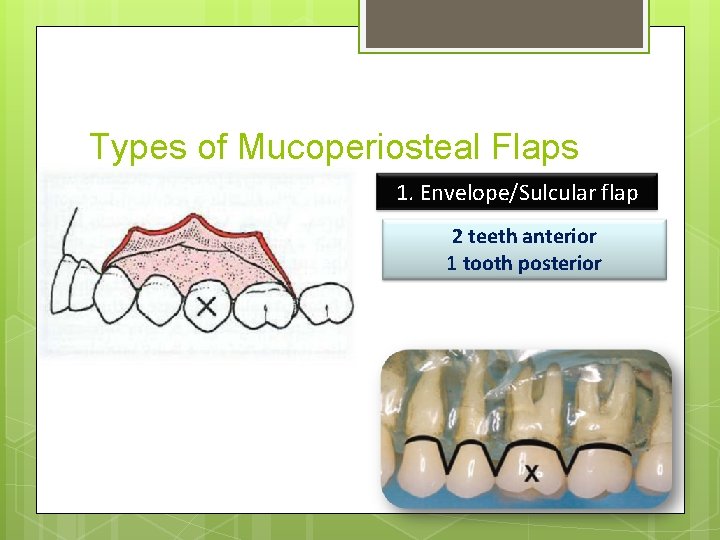
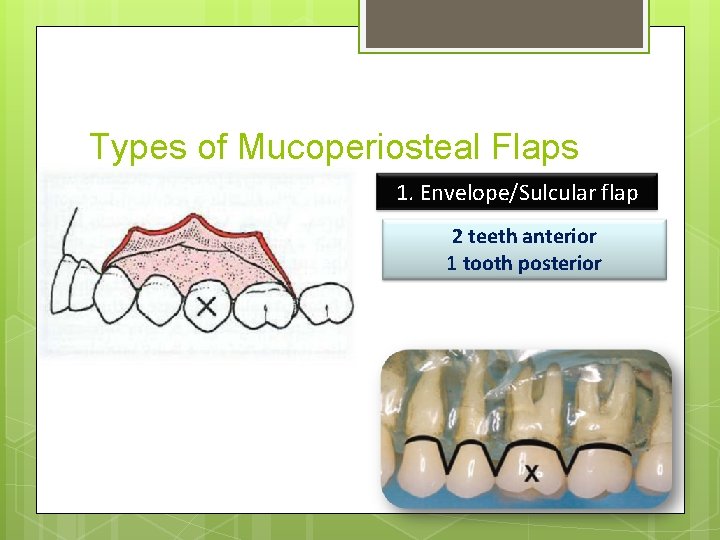
Types of Mucoperiosteal Flaps 1. Envelope/Sulcular flap 2 teeth anterior 1 tooth posterior
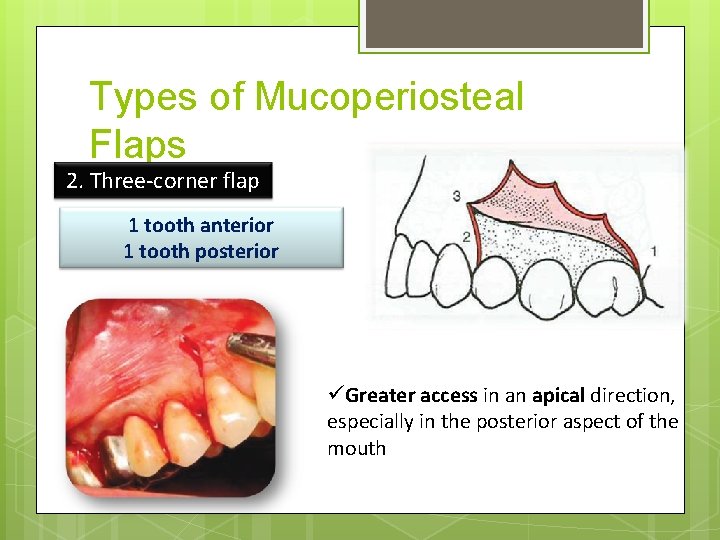
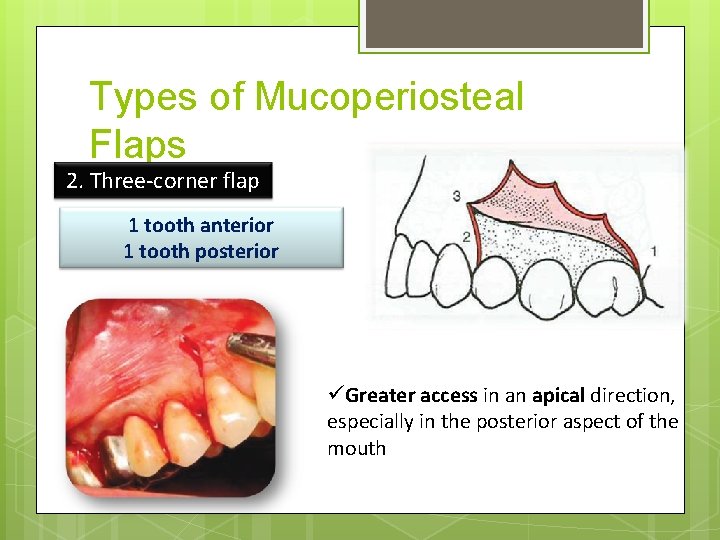
Types of Mucoperiosteal Flaps 2. Three-corner flap 1 tooth anterior 1 tooth posterior üGreater access in an apical direction, especially in the posterior aspect of the mouth
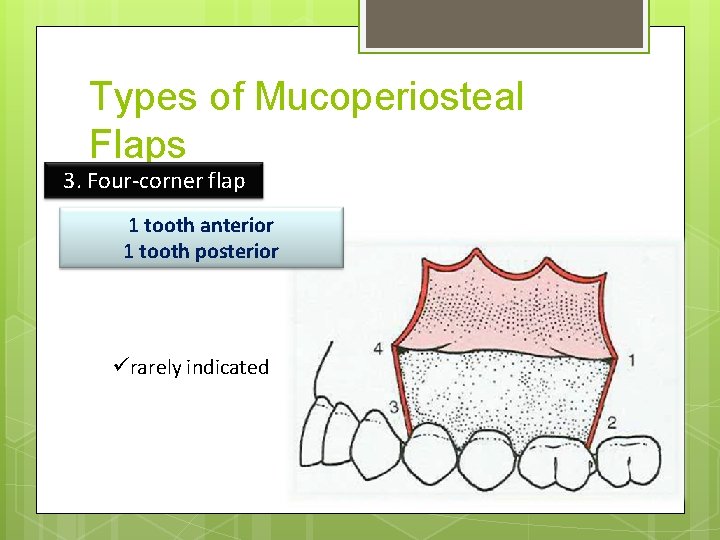
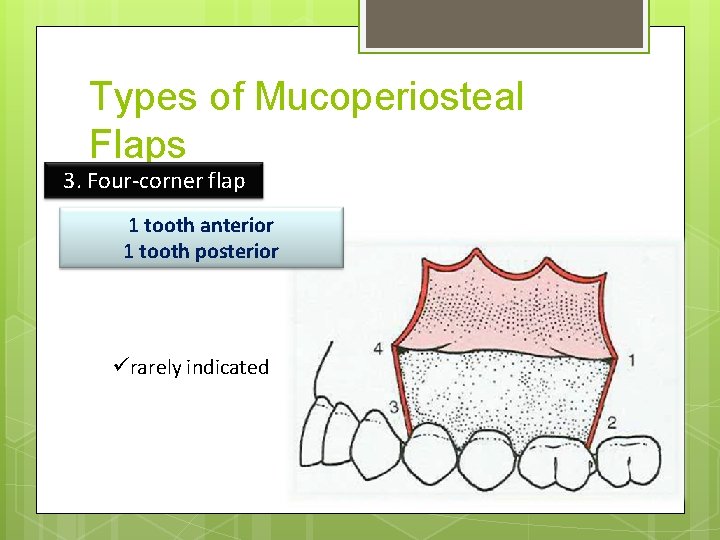
Types of Mucoperiosteal Flaps 3. Four-corner flap 1 tooth anterior 1 tooth posterior ürarely indicated
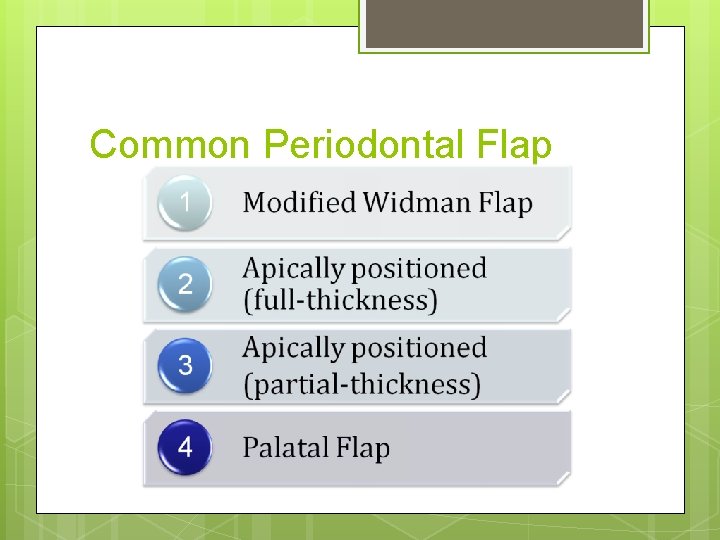
Common Periodontal Flap
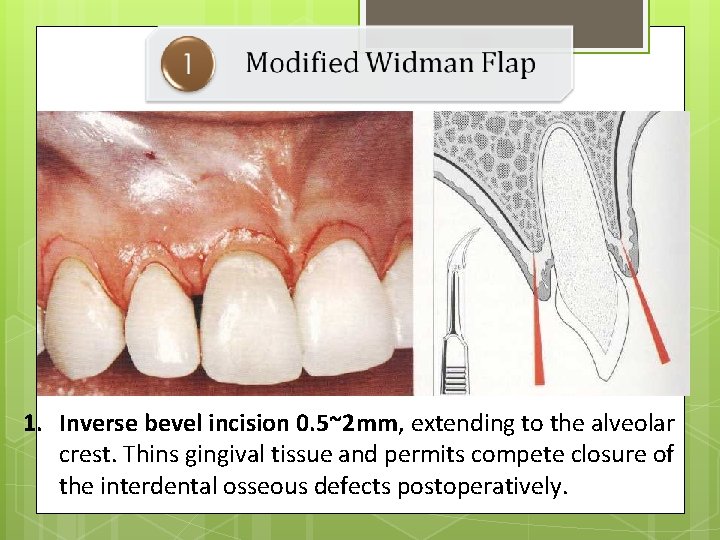
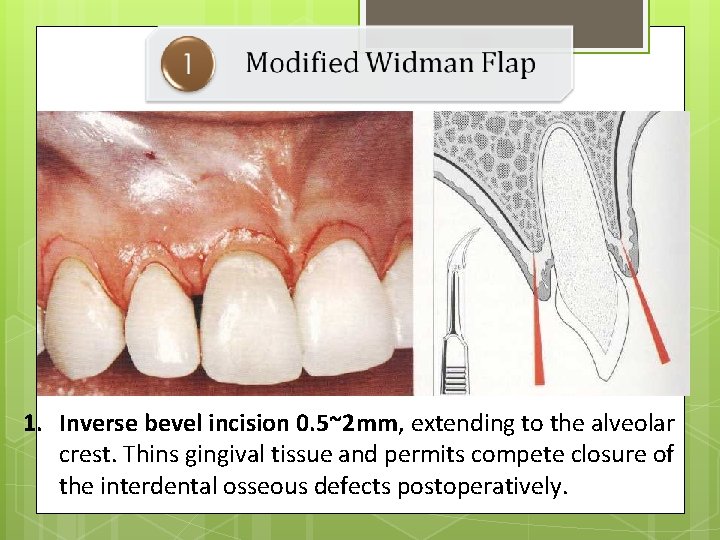
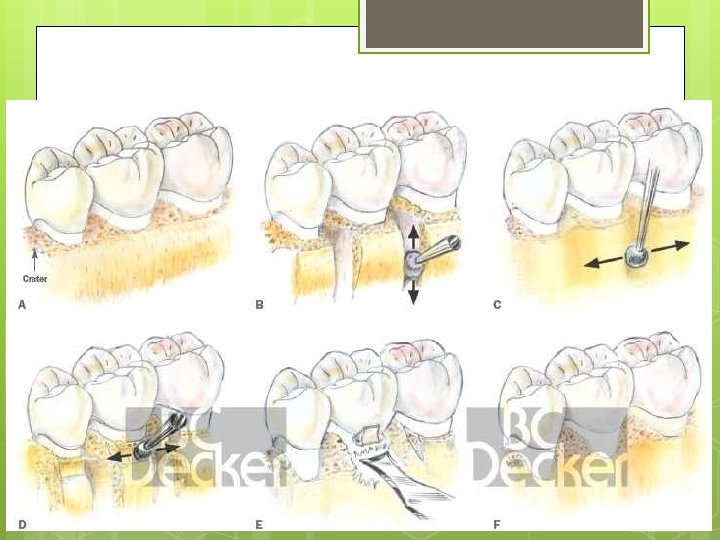
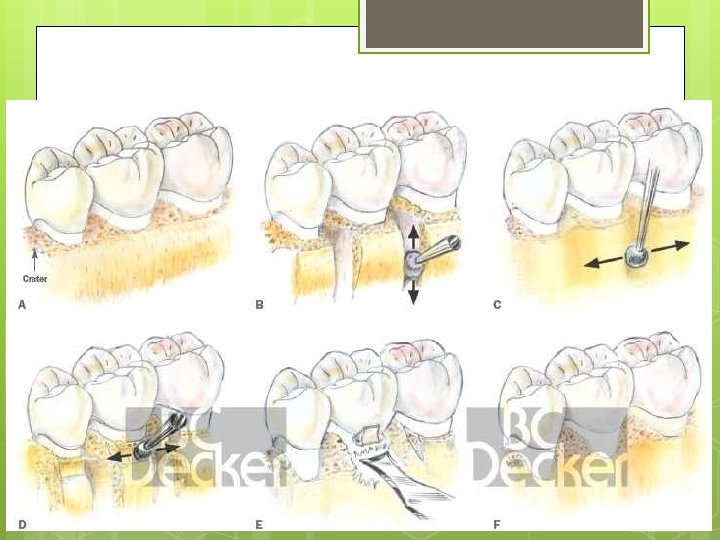
1. Inverse bevel incision 0. 5~2 mm, extending to the alveolar crest. Thins gingival tissue and permits compete closure of the interdental osseous defects postoperatively.
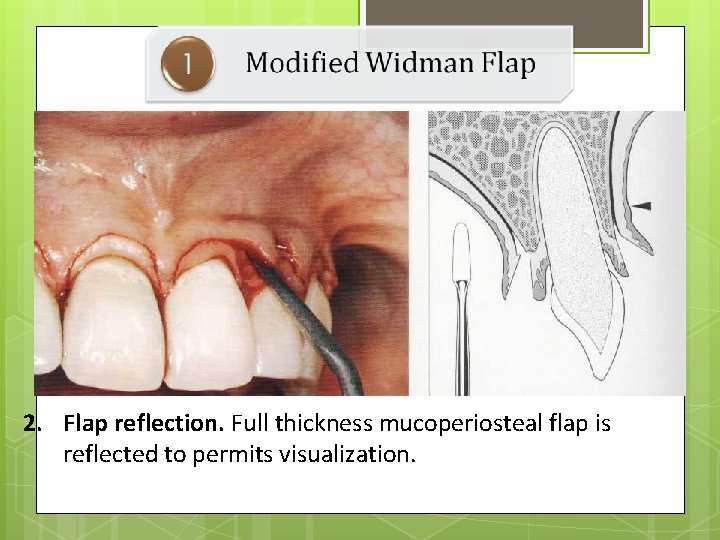
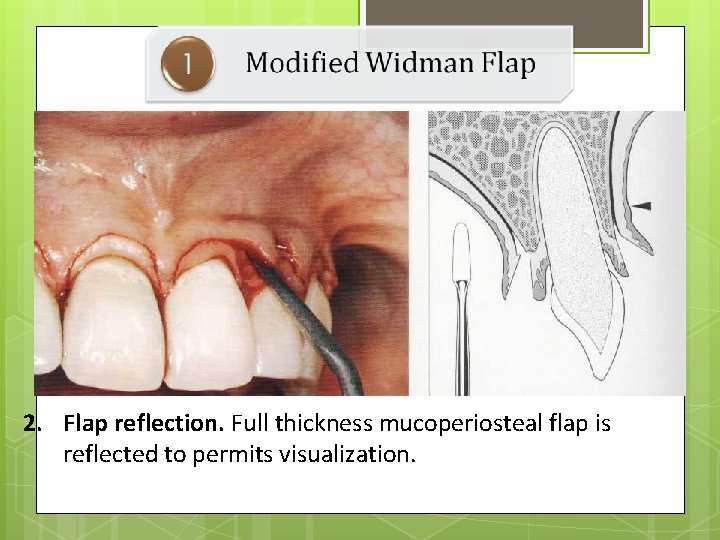
2. Flap reflection. Full thickness mucoperiosteal flap is reflected to permits visualization.
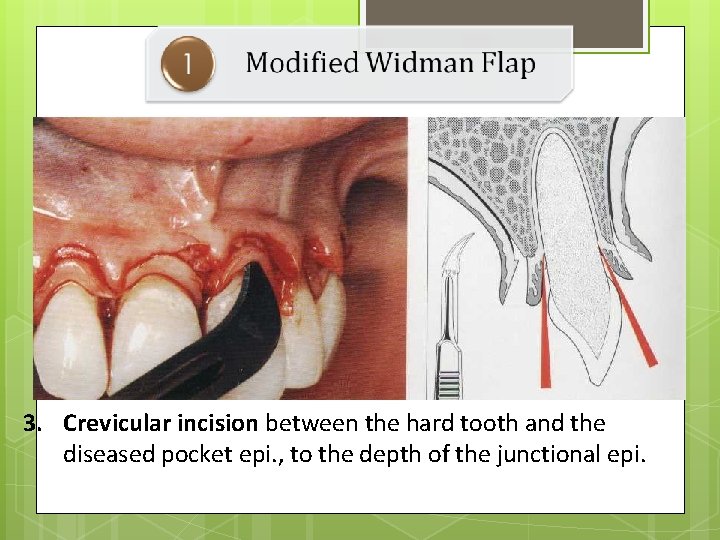
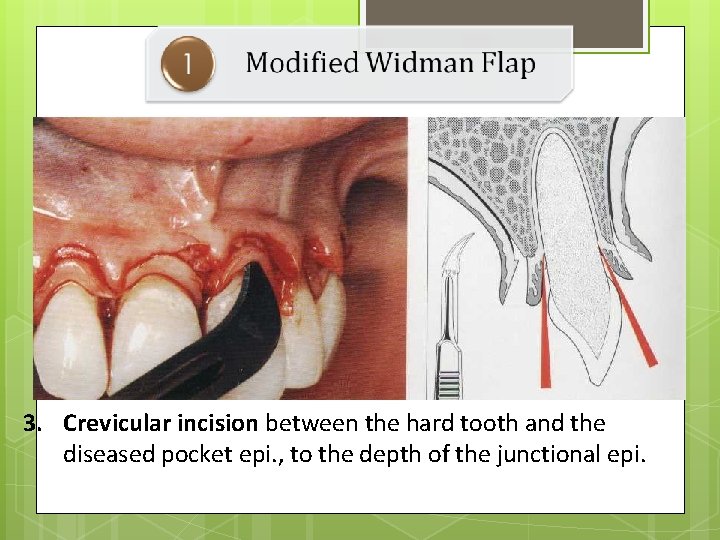
3. Crevicular incision between the hard tooth and the diseased pocket epi. , to the depth of the junctional epi.
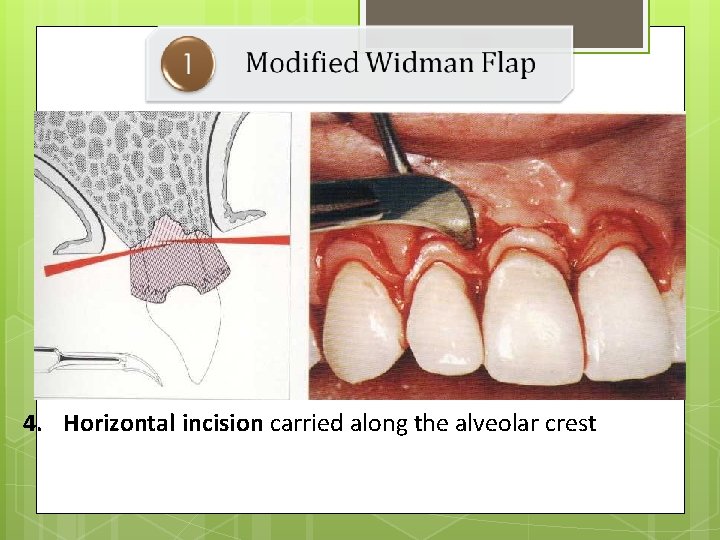
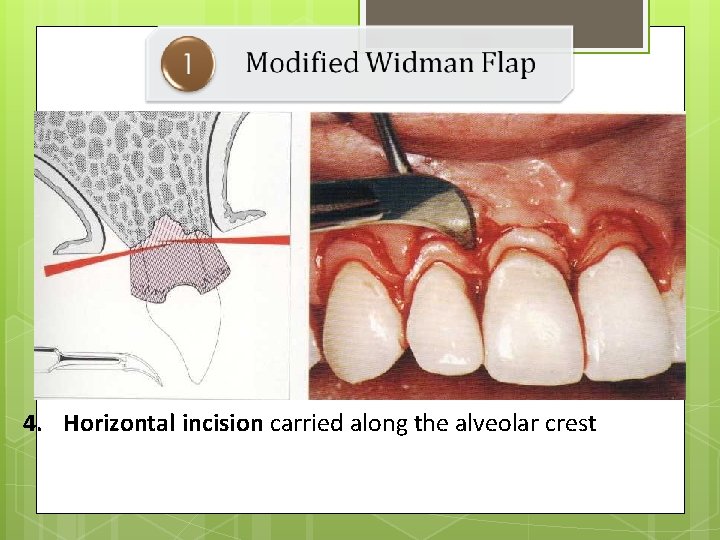
4. Horizontal incision carried along the alveolar crest
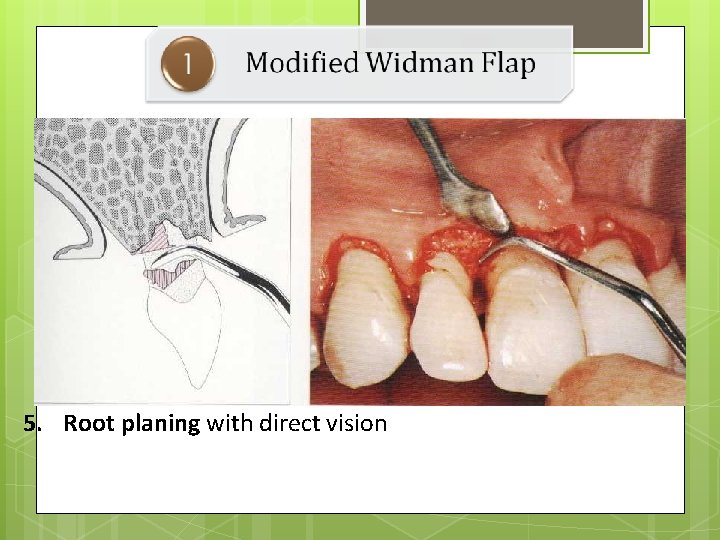
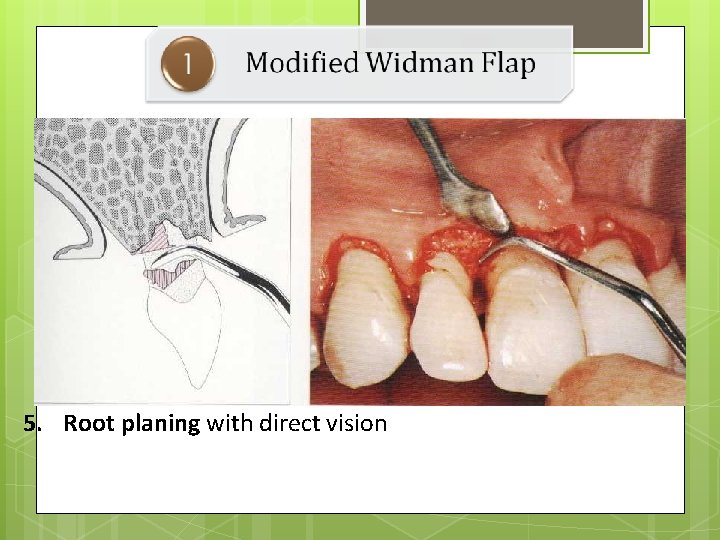
5. Root planing with direct vision
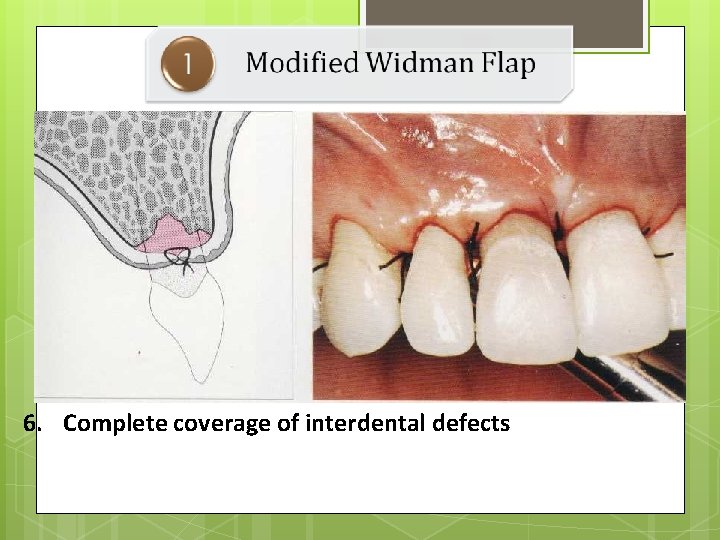
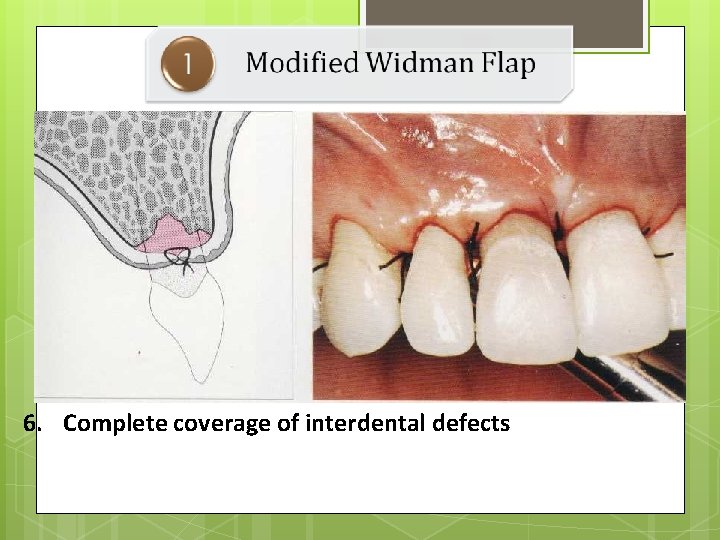
6. Complete coverage of interdental defects
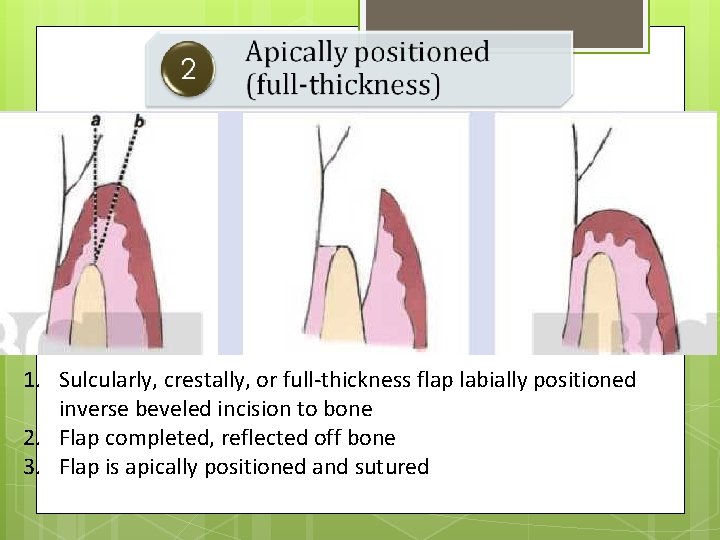
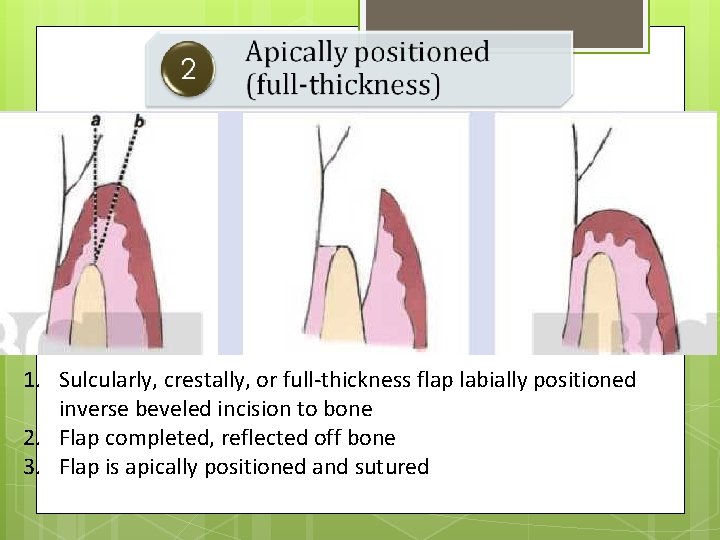
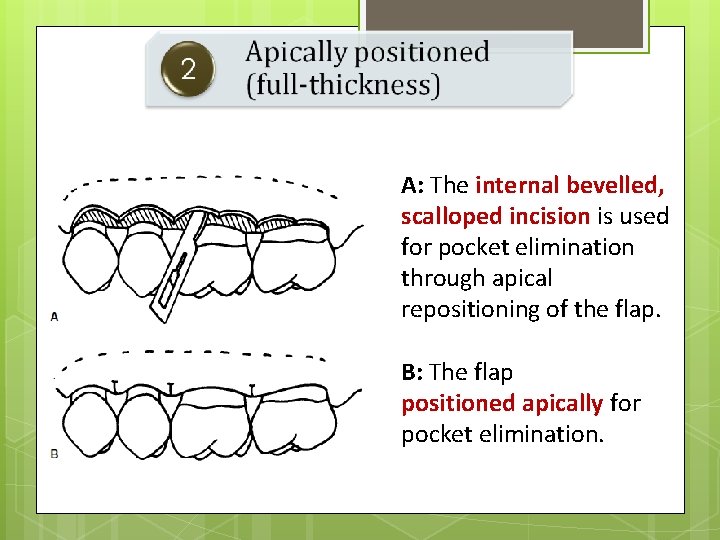
1. Sulcularly, crestally, or full-thickness flap labially positioned inverse beveled incision to bone 2. Flap completed, reflected off bone 3. Flap is apically positioned and sutured
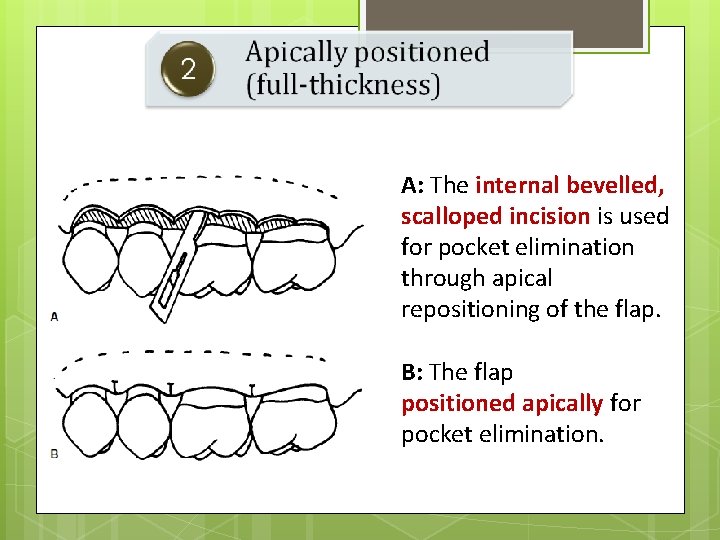
A: The internal bevelled, scalloped incision is used for pocket elimination through apical repositioning of the flap. B: The flap positioned apically for pocket elimination.
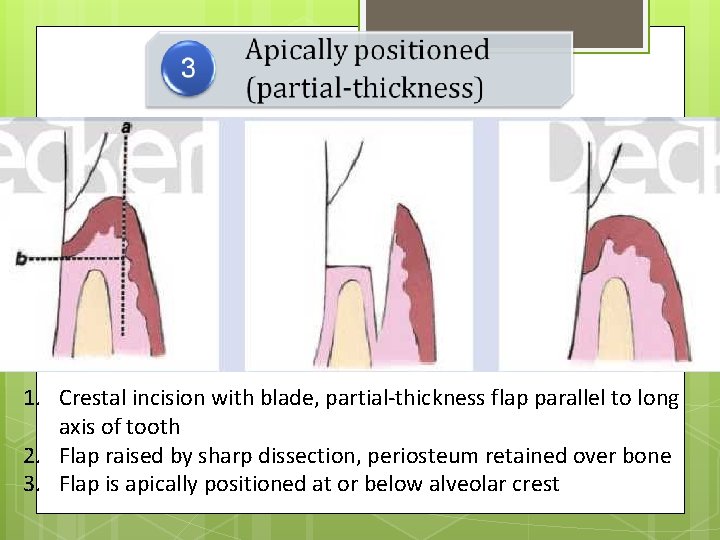
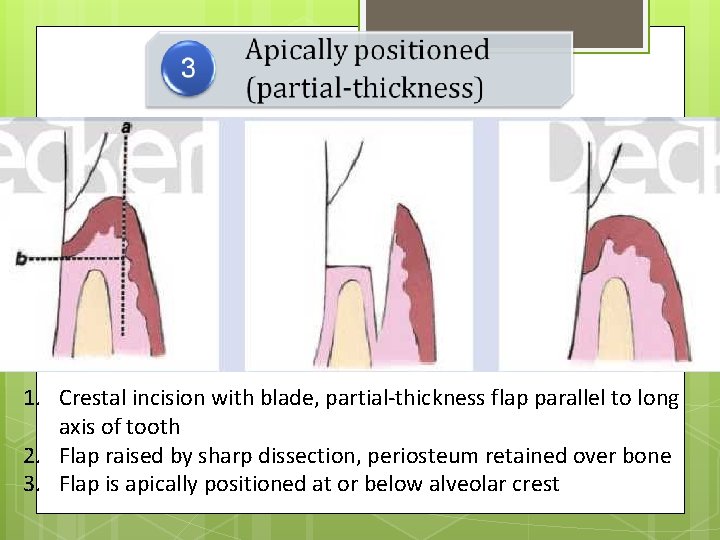
1. Crestal incision with blade, partial-thickness flap parallel to long axis of tooth 2. Flap raised by sharp dissection, periosteum retained over bone 3. Flap is apically positioned at or below alveolar crest
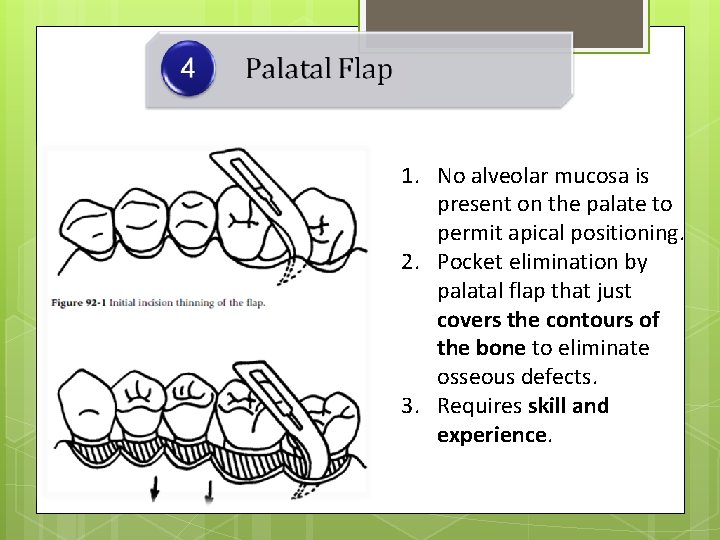
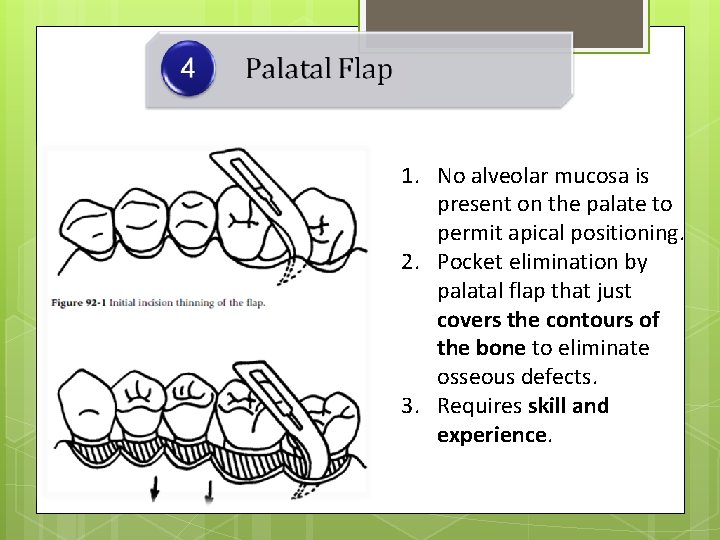
1. No alveolar mucosa is present on the palate to permit apical positioning. 2. Pocket elimination by palatal flap that just covers the contours of the bone to eliminate osseous defects. 3. Requires skill and experience.
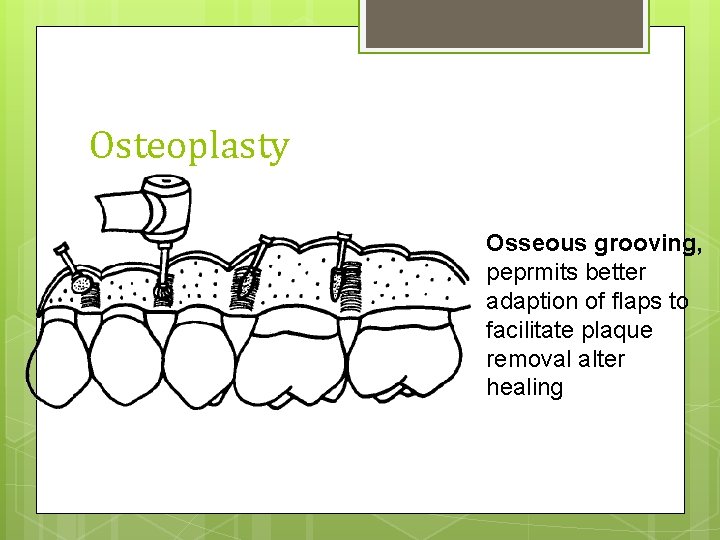
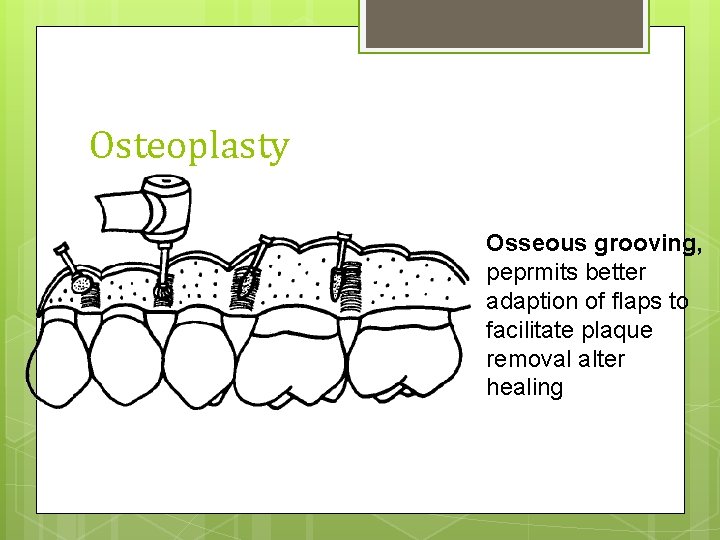
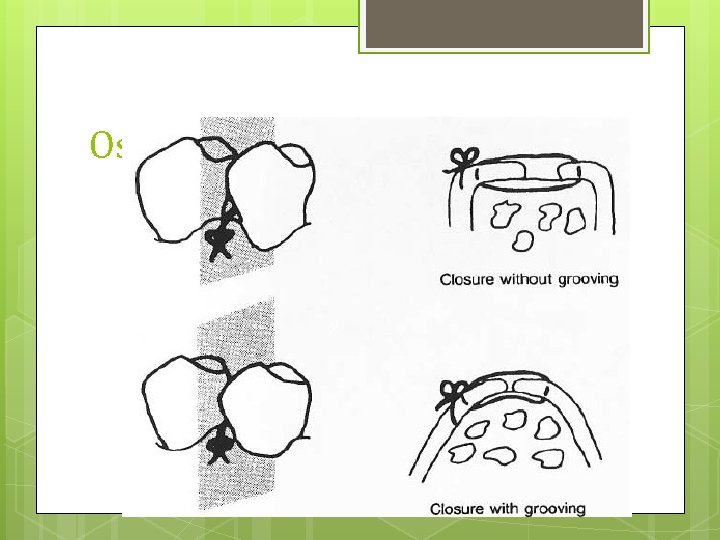
Osteoplasty Osseous grooving, peprmits better adaption of flaps to facilitate plaque removal alter healing
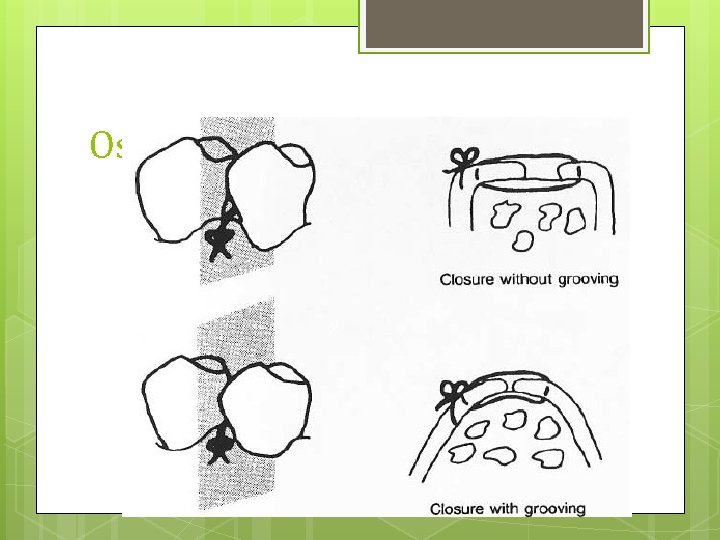
Osteoplasty
Osteoplasty
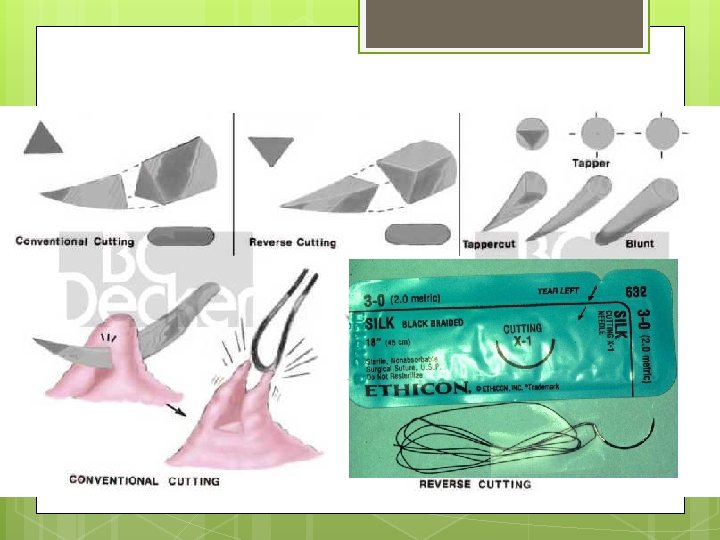
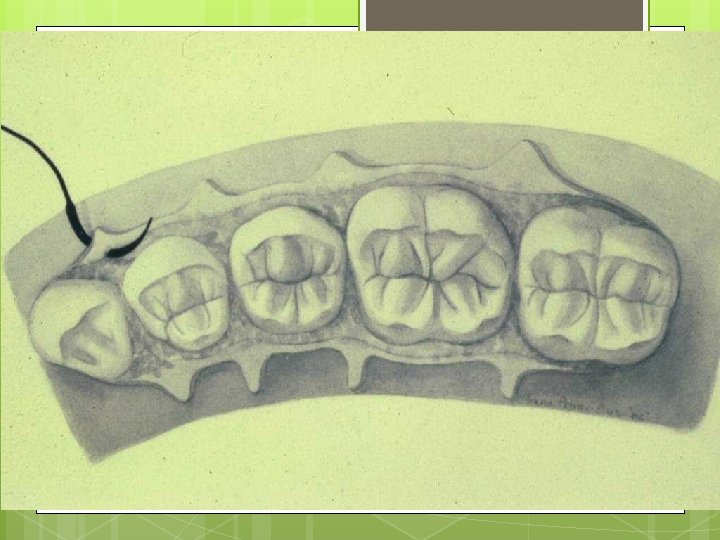
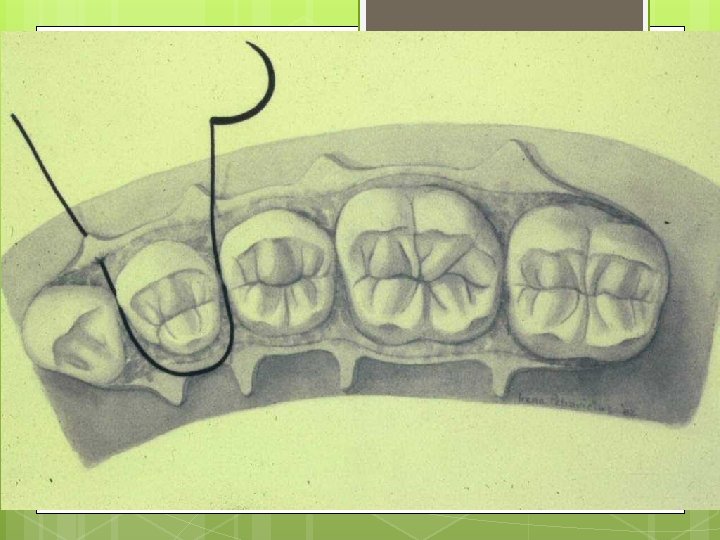
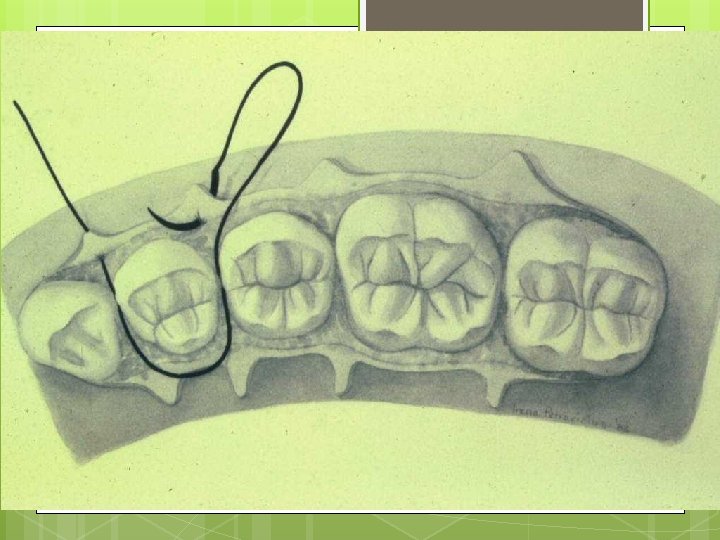
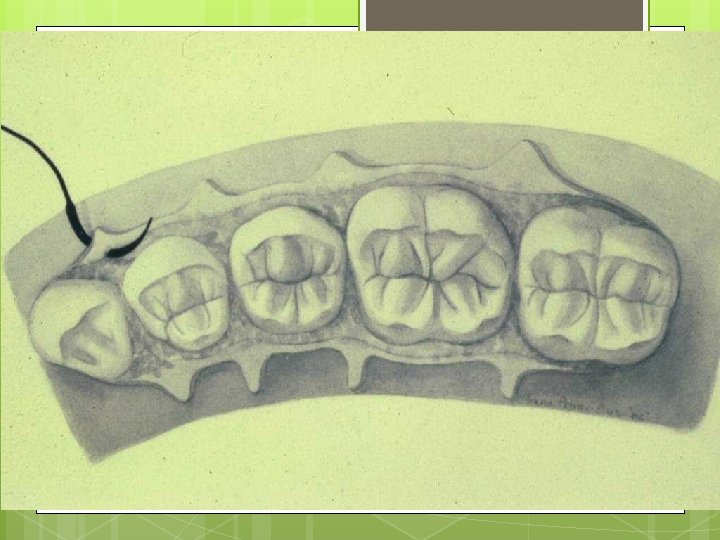
Suturing for Flap Surgery
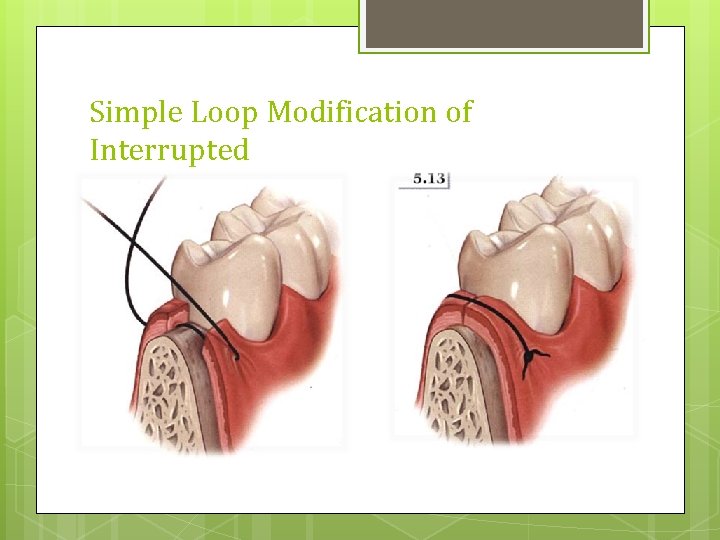
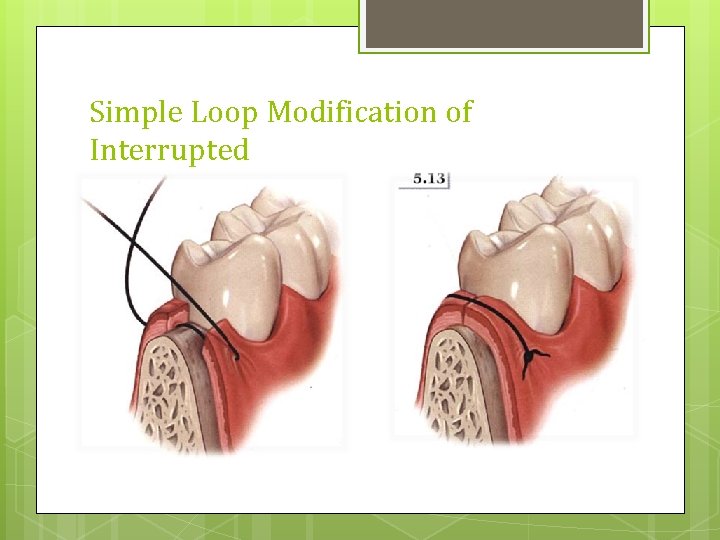
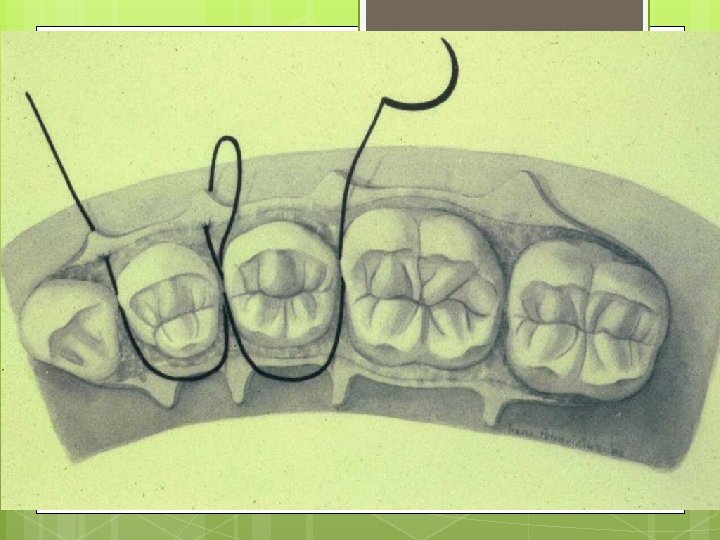
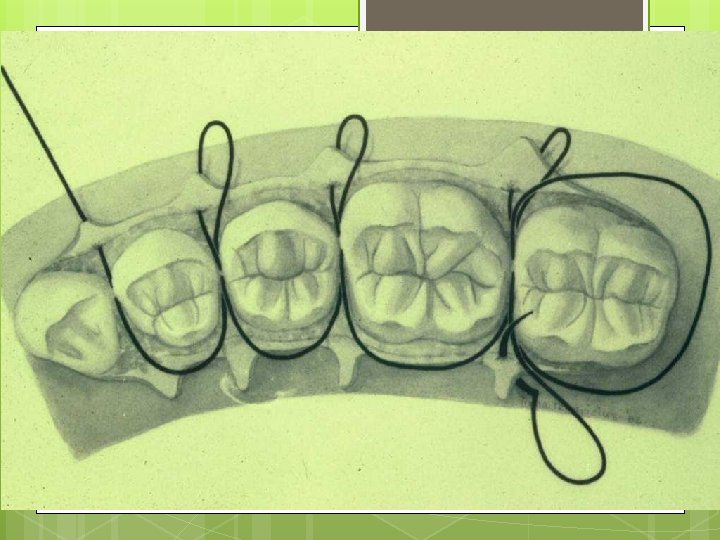
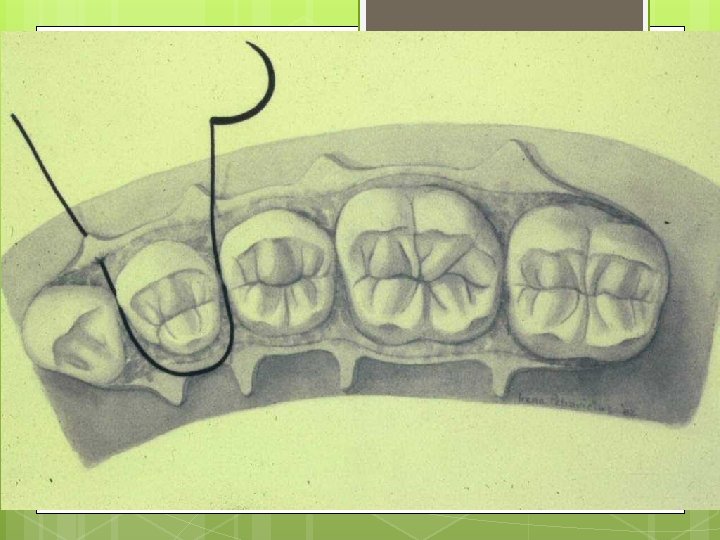
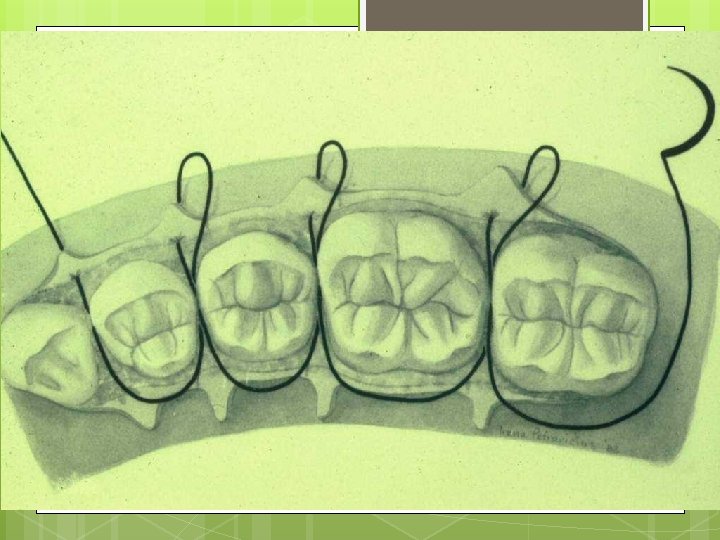
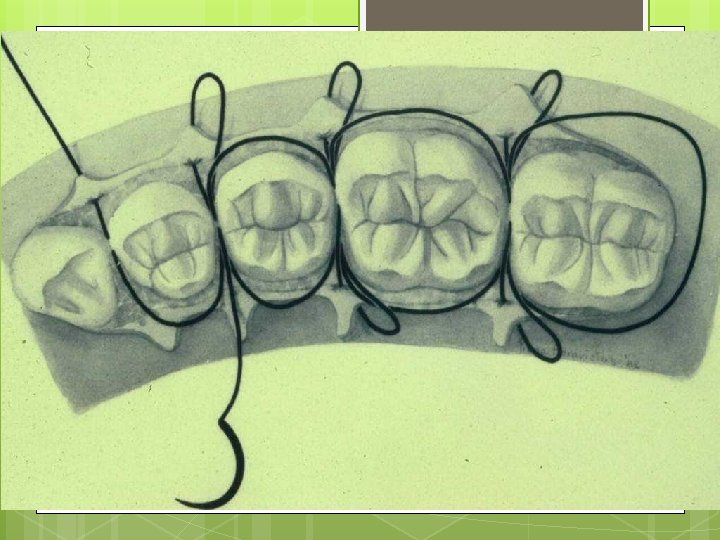
Simple Loop Modification of Interrupted
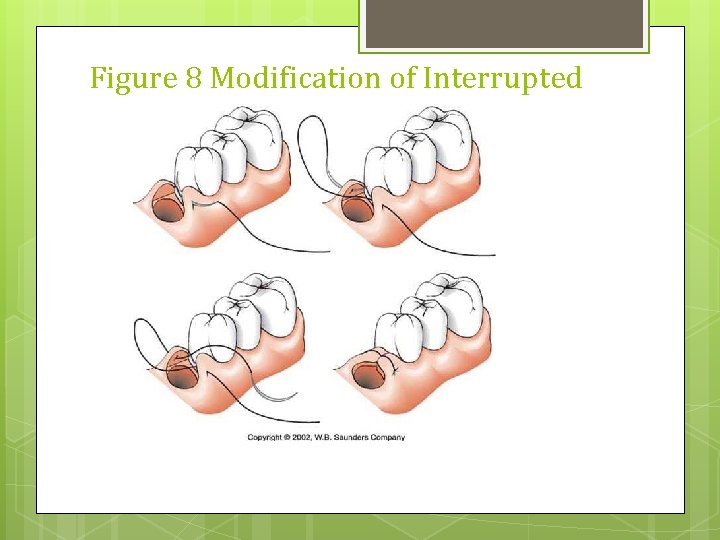
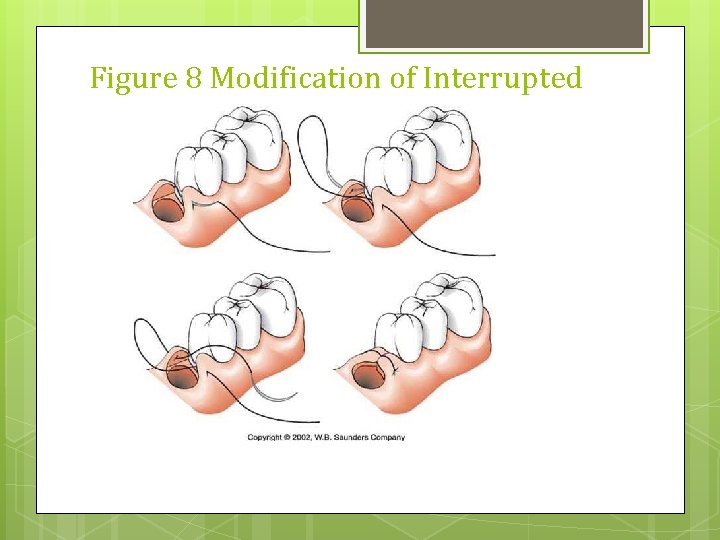
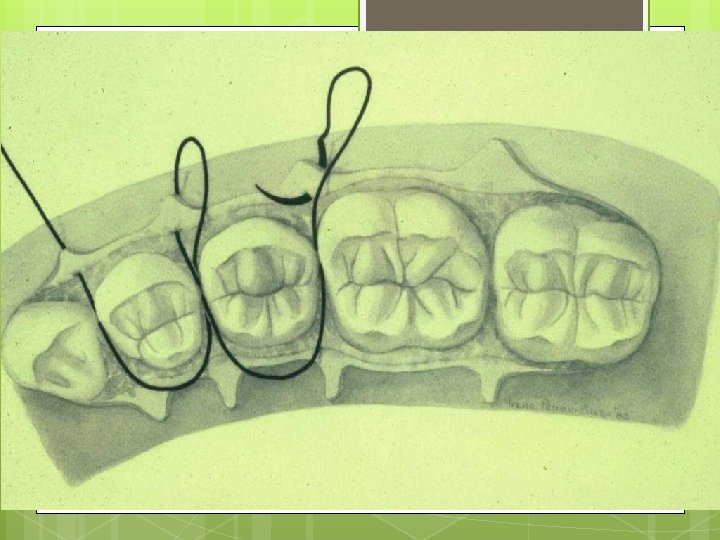
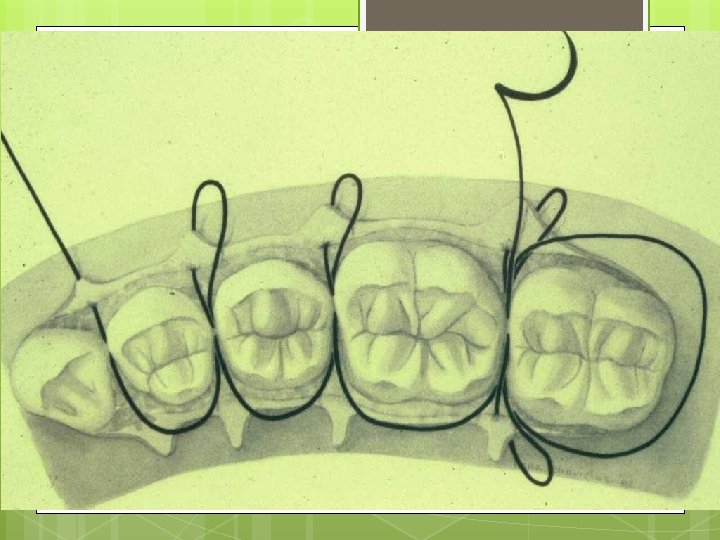
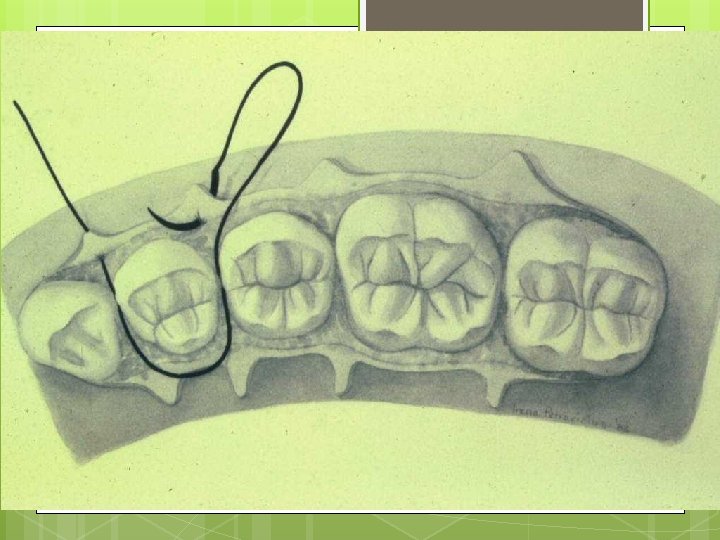
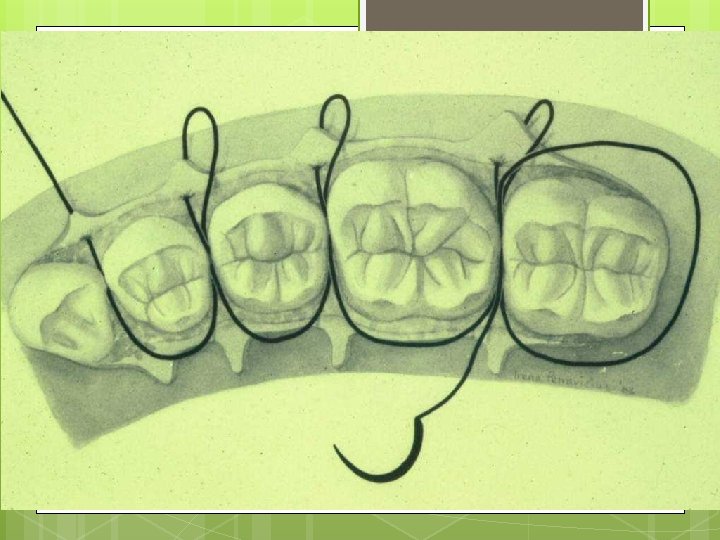
Figure 8 Modification of Interrupted
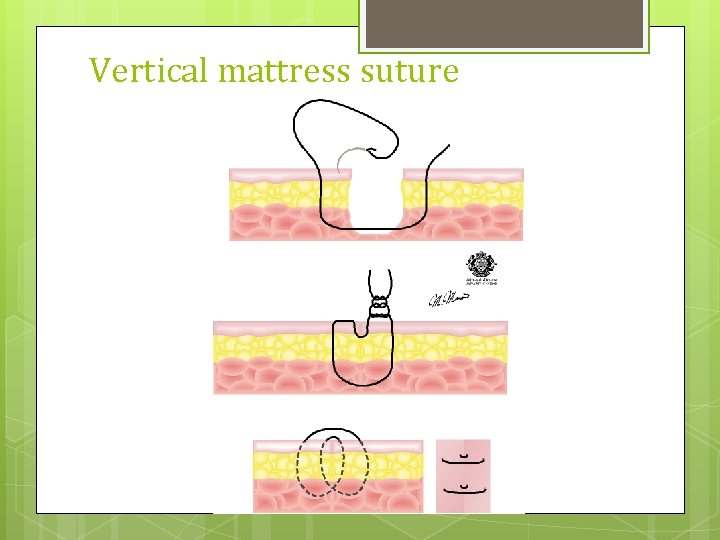
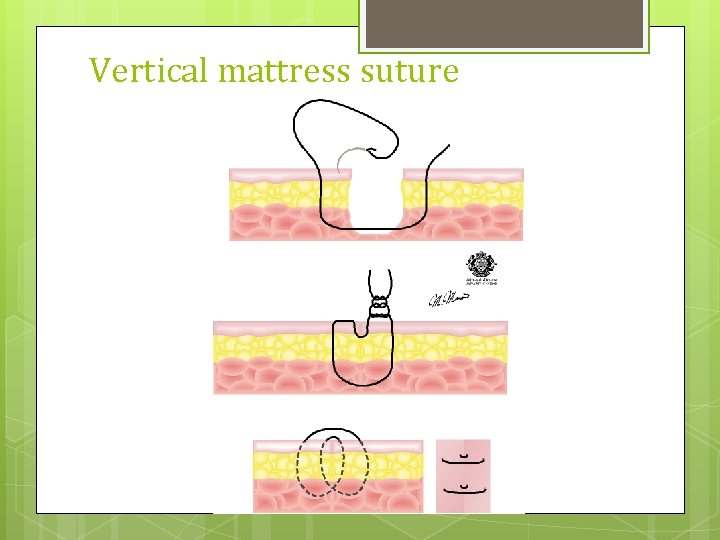
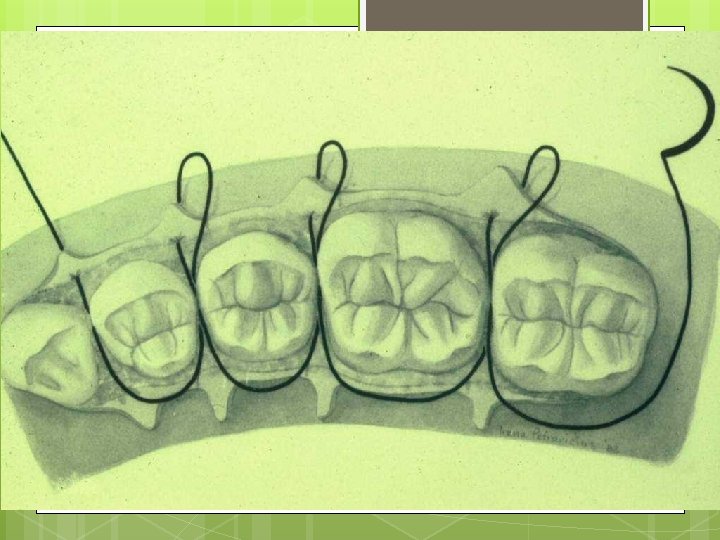
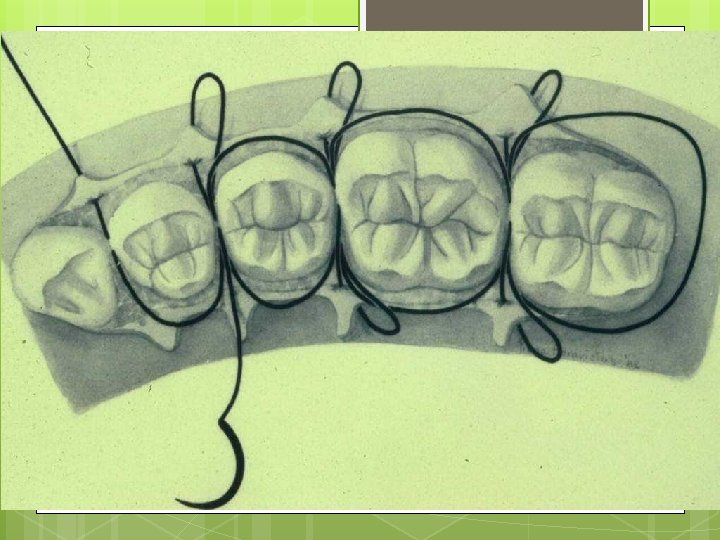
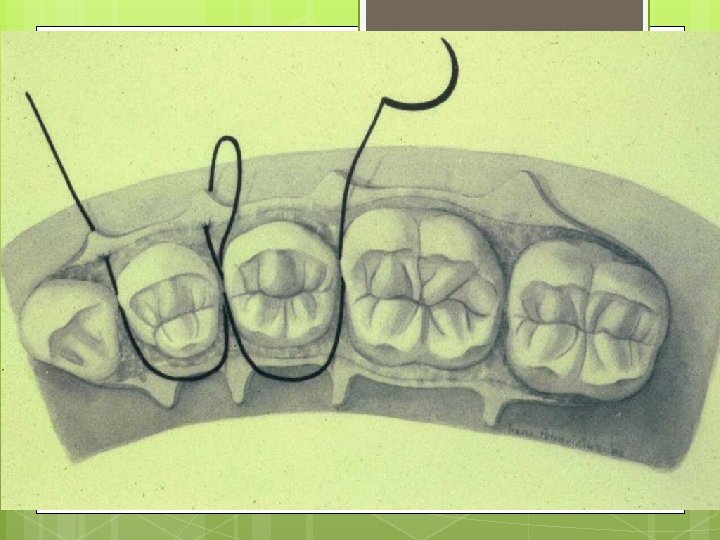
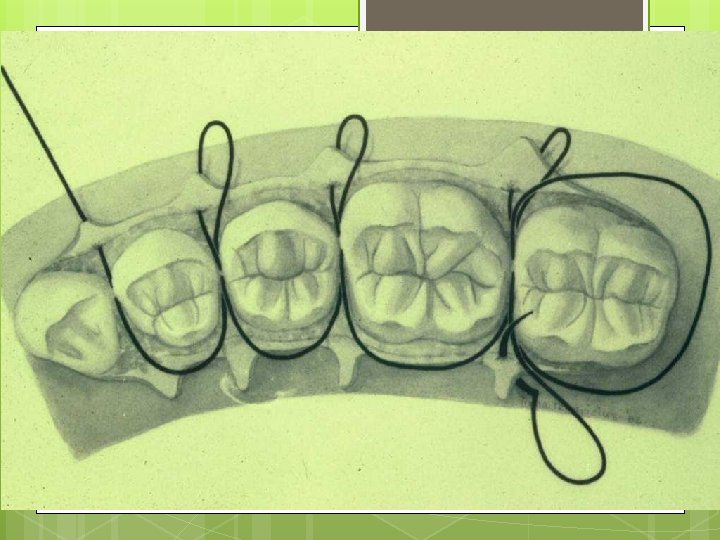
Vertical mattress suture
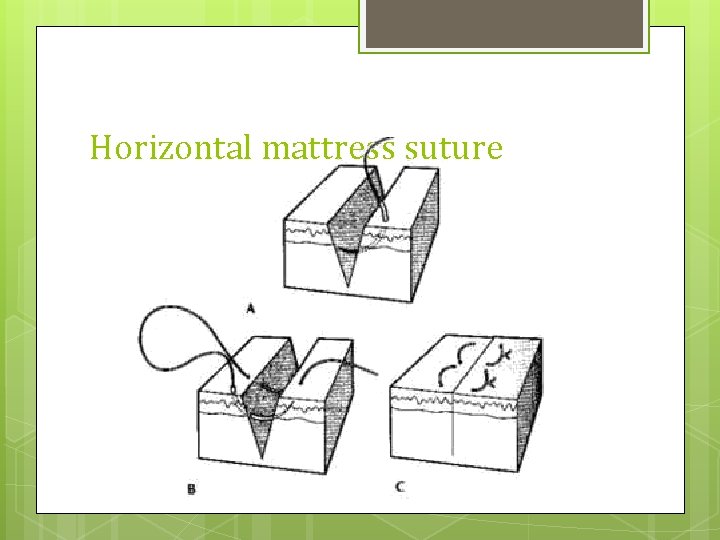
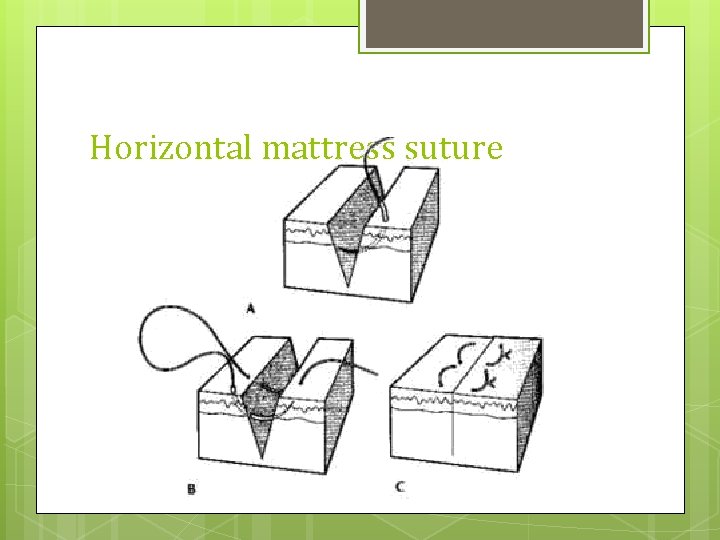
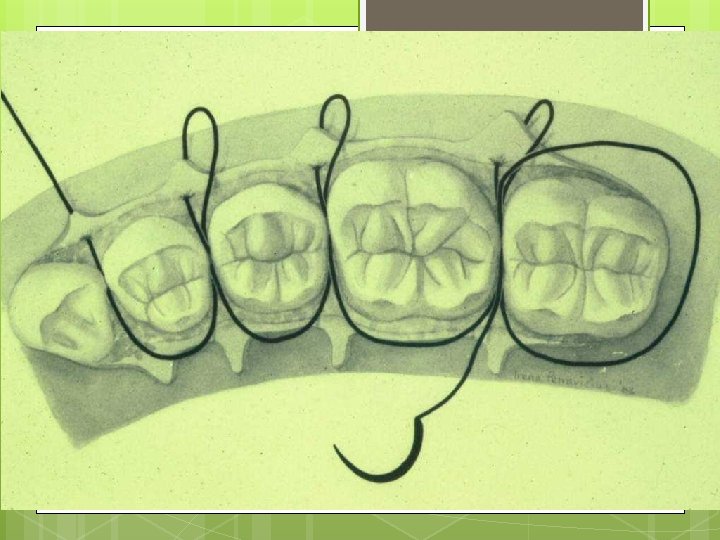
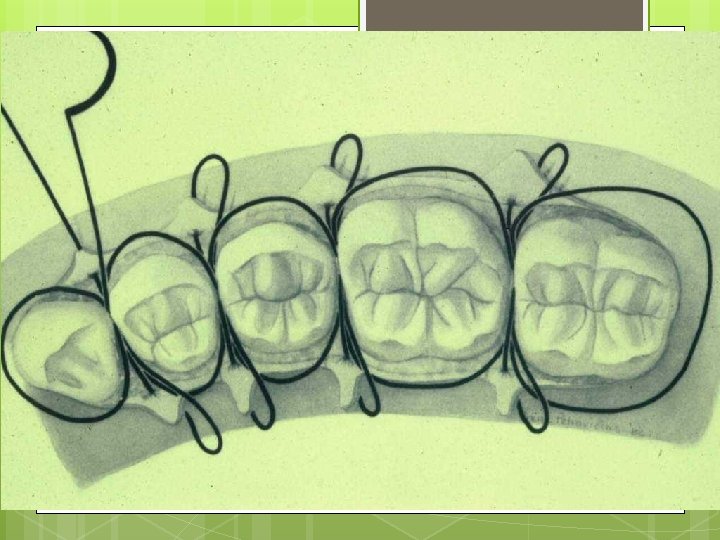
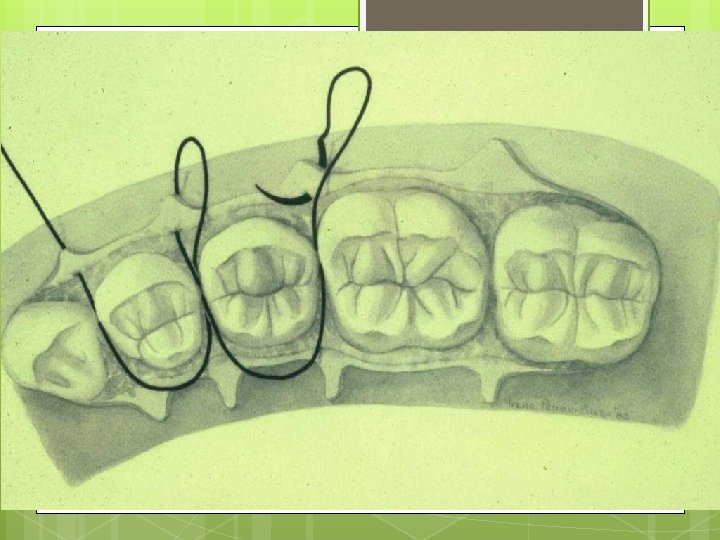
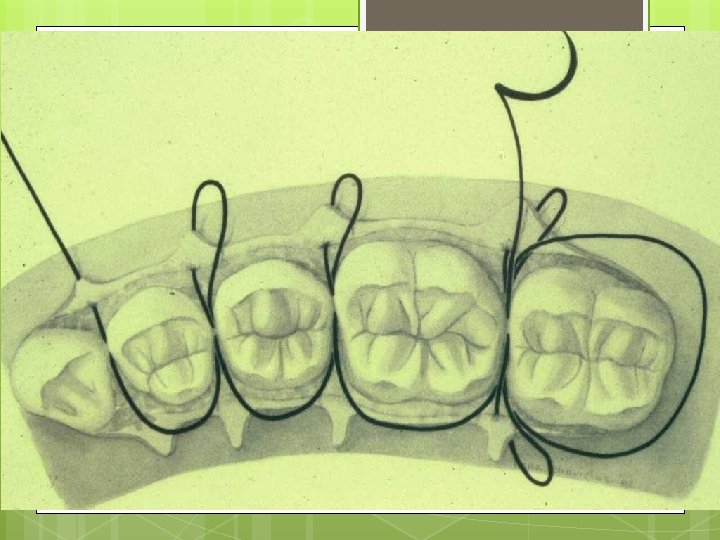
Horizontal mattress suture
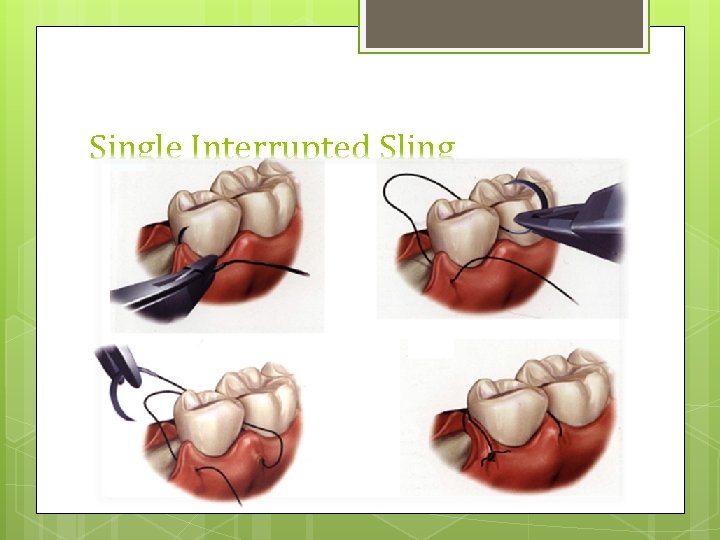
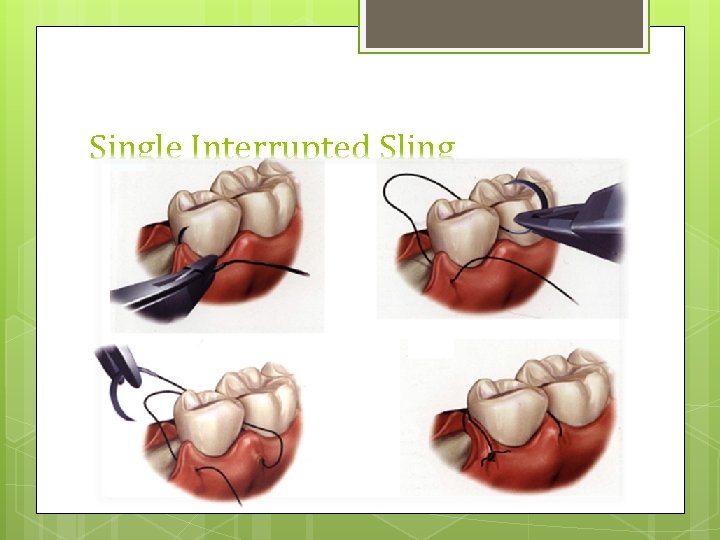
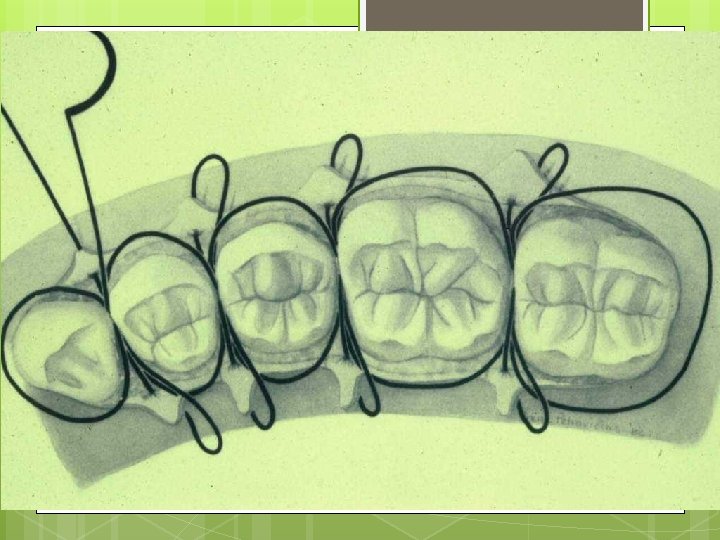
Single Interrupted Sling

Reference 1. 2. 3. 4. 5. 6. 7. Contemporary Oral and Maxillofacial Surgery, 4 th Edition, Larry J Peterson, DDS, MS, Edward Ellis, III, DDS, MS, James R Hupp, DMD, JD, FACS and Myron R Tucker, DDS Peterson's principles of oral and maxillofacial surgery, Michael Miloro, G. E. Ghali, Peter Larsen, Peter Waite An atlas of minor oral surgery: principles and practice, David A. Mc. Gowan Manual of minor oral surgery for the general dentist, Karl R. Koerner Critical Decisions in Periodontology, 4 th Edition, WALTER B. HALL, BA, DDS, MSD Color Atlas of Periodontology, Klaus H. & Edith M. Rateitschak Atlas of Cosmetic and Reconstructive Periodontal Surgery 3 rd edition, EDWARD S. COHEN, DMD
 Undisplaced flap surgery
Undisplaced flap surgery Skew flap below knee amputation
Skew flap below knee amputation Principles of periodontal surgery
Principles of periodontal surgery Guided surgery flap
Guided surgery flap Terminal access controller access-control system
Terminal access controller access-control system Terminal access controller access-control system
Terminal access controller access-control system Heliprobe 2 positivo
Heliprobe 2 positivo Rationale of periodontal treatment
Rationale of periodontal treatment Maintenance phase of periodontal therapy
Maintenance phase of periodontal therapy Seccin 7
Seccin 7 Politür nedir
Politür nedir Periodontal ligament injection definition
Periodontal ligament injection definition Periapical granuloma
Periapical granuloma Non-infective
Non-infective Dental case
Dental case Russell periodontal index
Russell periodontal index Gtr indications
Gtr indications Desmodent
Desmodent Interdental septum
Interdental septum Williams sondu nedir
Williams sondu nedir Periodontium definition
Periodontium definition Periodontal disease
Periodontal disease Periapical granuloma
Periapical granuloma Nug tedavisi
Nug tedavisi Supra and infrabony pocket
Supra and infrabony pocket Fases de la enfermedad periodontal
Fases de la enfermedad periodontal Plicae digestive system
Plicae digestive system Sharpey fibrilleri
Sharpey fibrilleri Gracey curette classification
Gracey curette classification Periodonto de insercion
Periodonto de insercion Lamina dura
Lamina dura Periodontal abscess
Periodontal abscess Plaque index
Plaque index Kista residual
Kista residual Tecnica step back y crown down
Tecnica step back y crown down Enap periodontics
Enap periodontics Periodontal tendonitis
Periodontal tendonitis Como se divide el periodonto
Como se divide el periodonto Periodontal dressing definition
Periodontal dressing definition Diagnosis of periodontal disease
Diagnosis of periodontal disease Periodontal therapy in female patients
Periodontal therapy in female patients Glickman's concept
Glickman's concept Periodontal cep
Periodontal cep Iatrogenic factors in periodontal disease
Iatrogenic factors in periodontal disease Dental nurse charting
Dental nurse charting Boari flap psoas hitch
Boari flap psoas hitch Impacted molar surgery
Impacted molar surgery Swing check valve symbol
Swing check valve symbol Cross finger flap
Cross finger flap Aft momentum flap
Aft momentum flap Flap design principles
Flap design principles Transposition flap
Transposition flap Reverse bevel incision
Reverse bevel incision Flap dragon std
Flap dragon std 4 flap foldable
4 flap foldable Distacco menisco capsulare
Distacco menisco capsulare Trapezius flap
Trapezius flap Cold abscess stages
Cold abscess stages Papilla preservation flap
Papilla preservation flap Shutter mechanism of inguinal canal
Shutter mechanism of inguinal canal Waterman sluice gate
Waterman sluice gate