SORMEN ALUEEN PEHMYTKUDOSVAMMAN HOITO Jorma Ryhnen ksikirurgi dos














- Slides: 32
SORMEN ALUEEN PEHMYTKUDOSVAMMAN HOITO Jorma Ryhänen, käsikirurgi, dos. , oyl, OYS
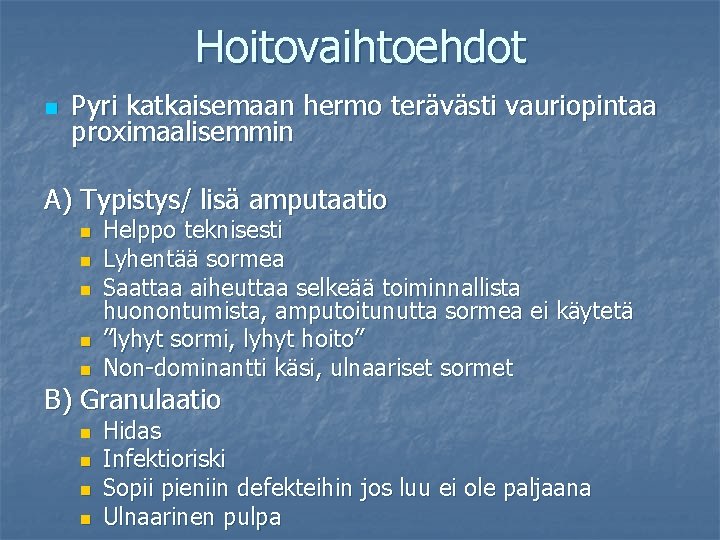
Hoitovaihtoehdot n Pyri katkaisemaan hermo terävästi vauriopintaa proximaalisemmin A) Typistys/ lisä amputaatio n n n Helppo teknisesti Lyhentää sormea Saattaa aiheuttaa selkeää toiminnallista huonontumista, amputoitunutta sormea ei käytetä ”lyhyt sormi, lyhyt hoito” Non-dominantti käsi, ulnaariset sormet B) Granulaatio n n Hidas Infektioriski Sopii pieniin defekteihin jos luu ei ole paljaana Ulnaarinen pulpa
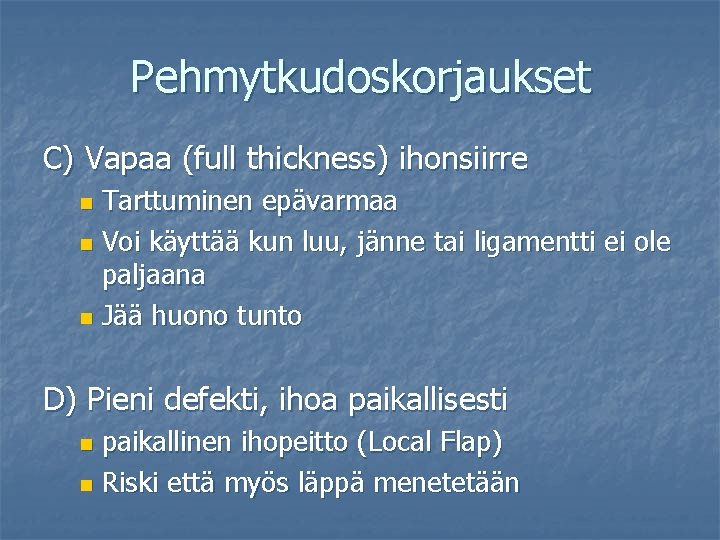
Pehmytkudoskorjaukset C) Vapaa (full thickness) ihonsiirre Tarttuminen epävarmaa n Voi käyttää kun luu, jänne tai ligamentti ei ole paljaana n Jää huono tunto n D) Pieni defekti, ihoa paikallisesti paikallinen ihopeitto (Local Flap) n Riski että myös läppä menetetään n
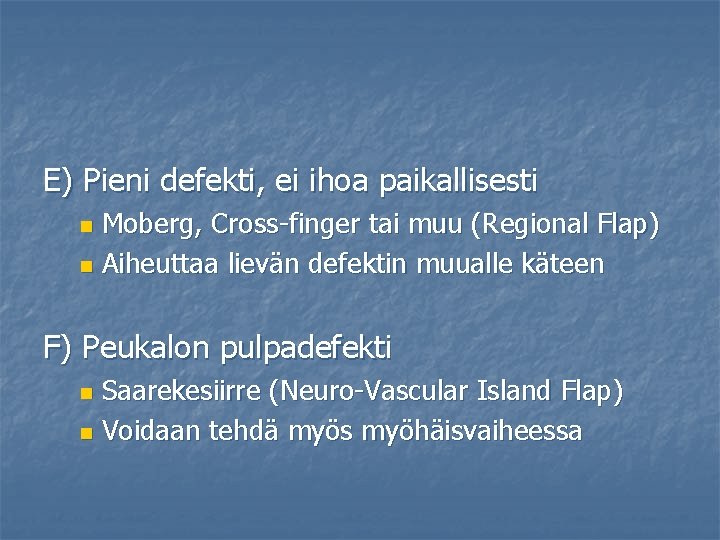
E) Pieni defekti, ei ihoa paikallisesti Moberg, Cross-finger tai muu (Regional Flap) n Aiheuttaa lievän defektin muualle käteen n F) Peukalon pulpadefekti Saarekesiirre (Neuro-Vascular Island Flap) n Voidaan tehdä myös myöhäisvaiheessa n
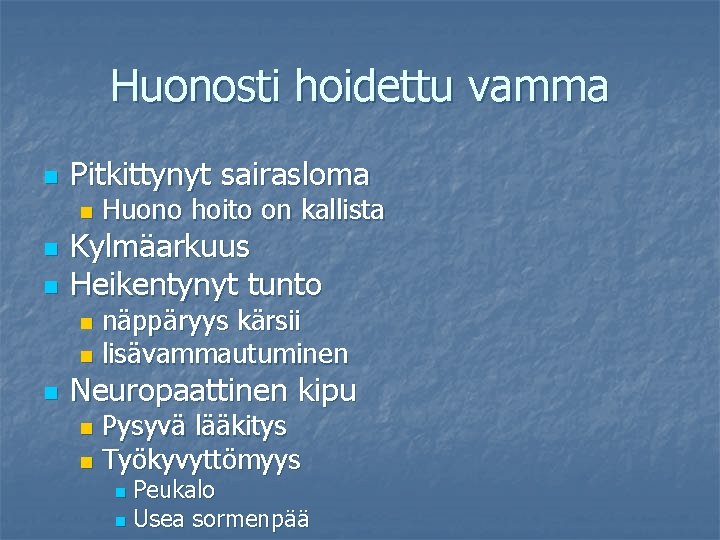
Huonosti hoidettu vamma n Pitkittynyt sairasloma n n n Huono hoito on kallista Kylmäarkuus Heikentynyt tunto näppäryys kärsii n lisävammautuminen n n Neuropaattinen kipu Pysyvä lääkitys n Työkyvyttömyys n Peukalo n Usea sormenpää n

V-Y PLASTIA


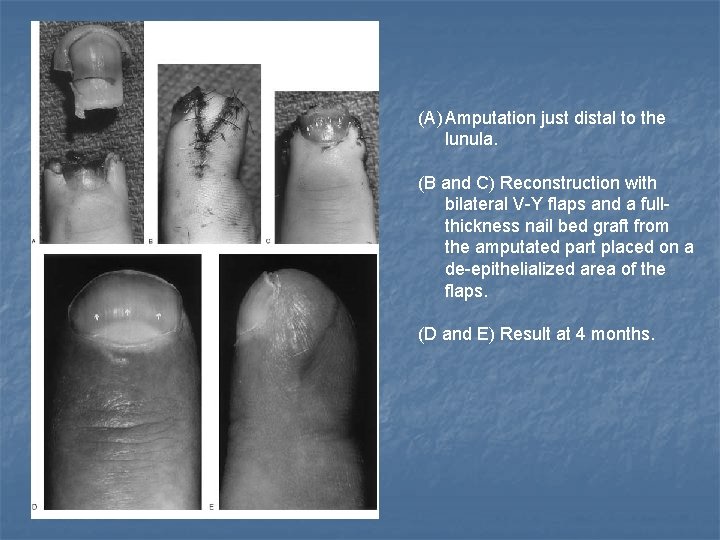
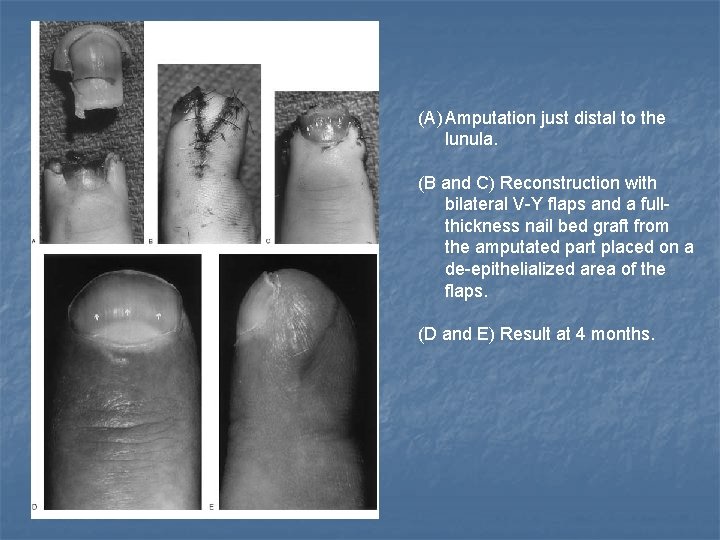
(A) Amputation just distal to the lunula. (B and C) Reconstruction with bilateral V-Y flaps and a fullthickness nail bed graft from the amputated part placed on a de-epithelialized area of the flaps. (D and E) Result at 4 months.

MUUT PAIKALLISET KIELEKKEET
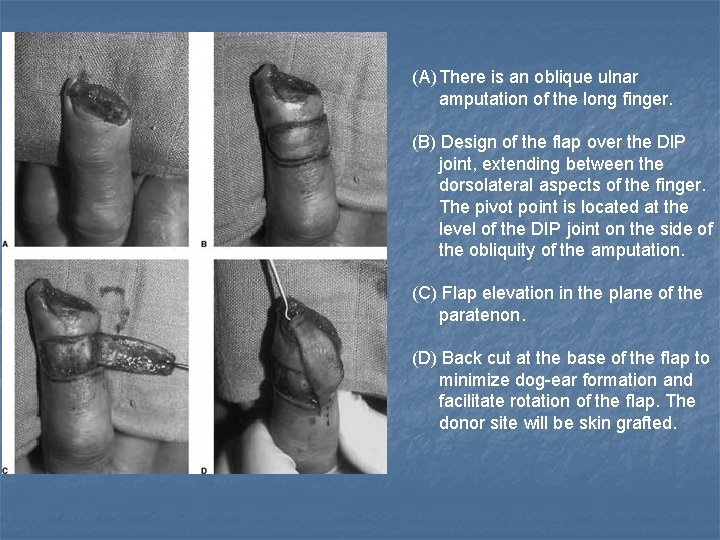
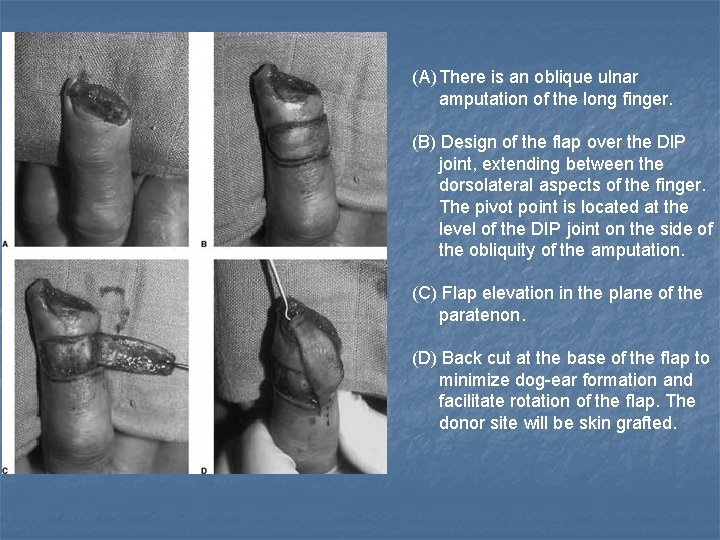
(A) There is an oblique ulnar amputation of the long finger. (B) Design of the flap over the DIP joint, extending between the dorsolateral aspects of the finger. The pivot point is located at the level of the DIP joint on the side of the obliquity of the amputation. (C) Flap elevation in the plane of the paratenon. (D) Back cut at the base of the flap to minimize dog-ear formation and facilitate rotation of the flap. The donor site will be skin grafted.
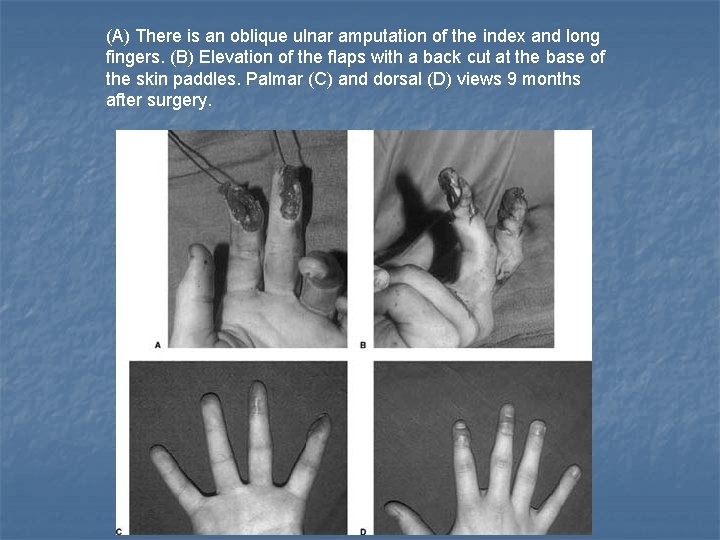
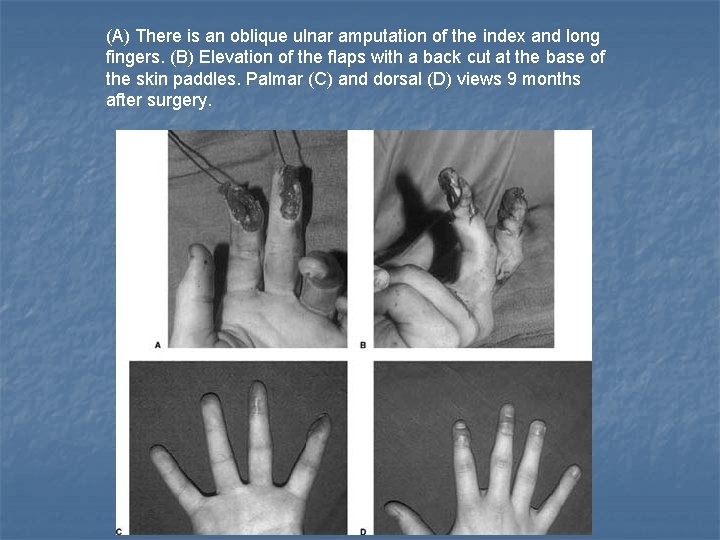
(A) There is an oblique ulnar amputation of the index and long fingers. (B) Elevation of the flaps with a back cut at the base of the skin paddles. Palmar (C) and dorsal (D) views 9 months after surgery.

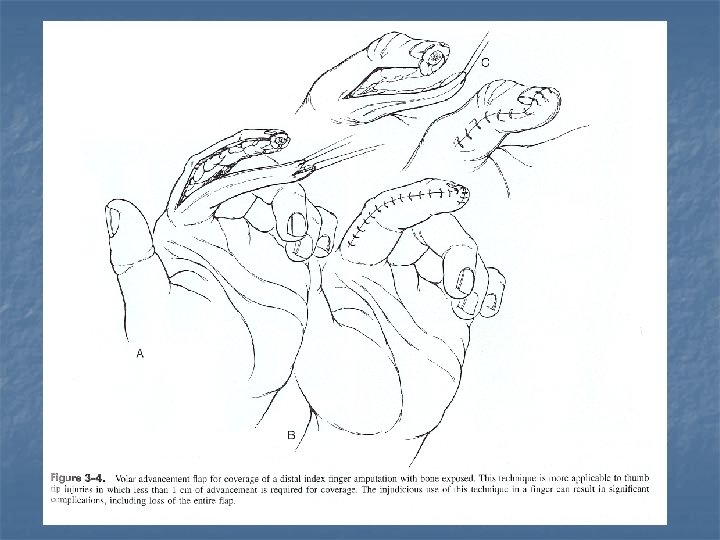
MOBERG FLAP


(A and B) Operative modification of a Moberg flap with a V-Y plasty in a 42 -yearold patient with a thumb defect after a saw injury. (C) Long-term result 16 months after the operation.
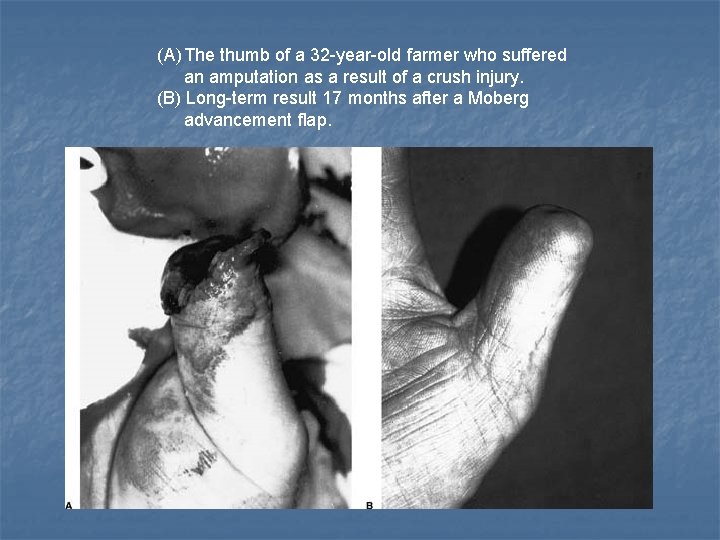
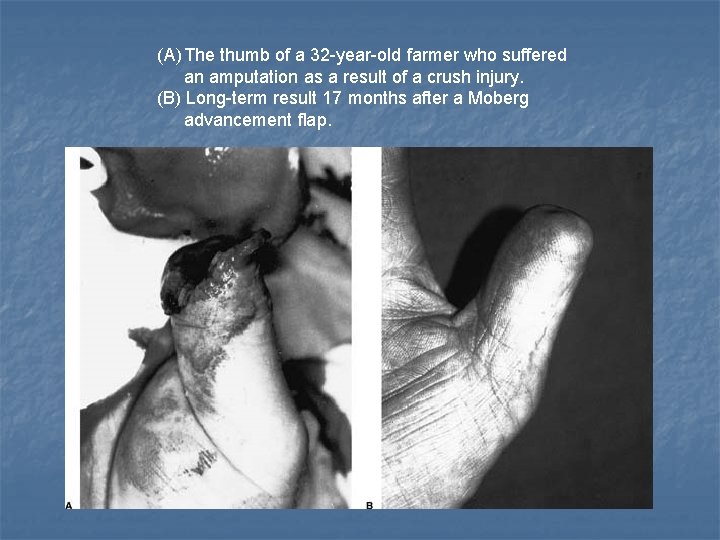
(A) The thumb of a 32 -year-old farmer who suffered an amputation as a result of a crush injury. (B) Long-term result 17 months after a Moberg advancement flap.
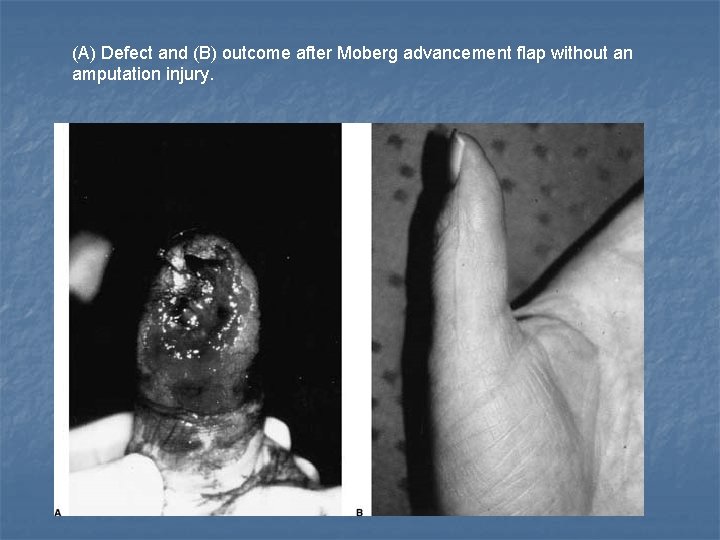
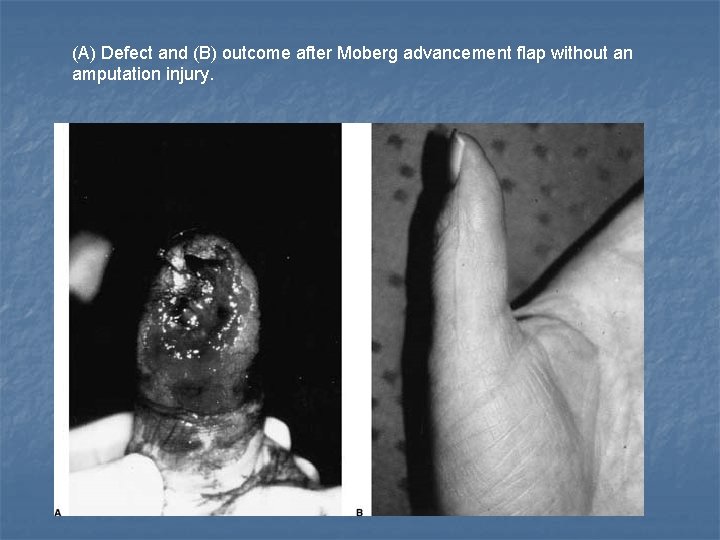
(A) Defect and (B) outcome after Moberg advancement flap without an amputation injury.

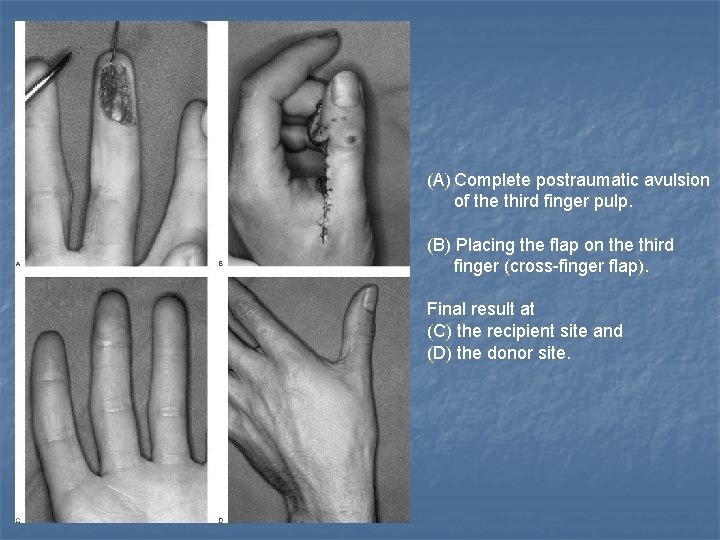
CROSS-FINGER FLAP

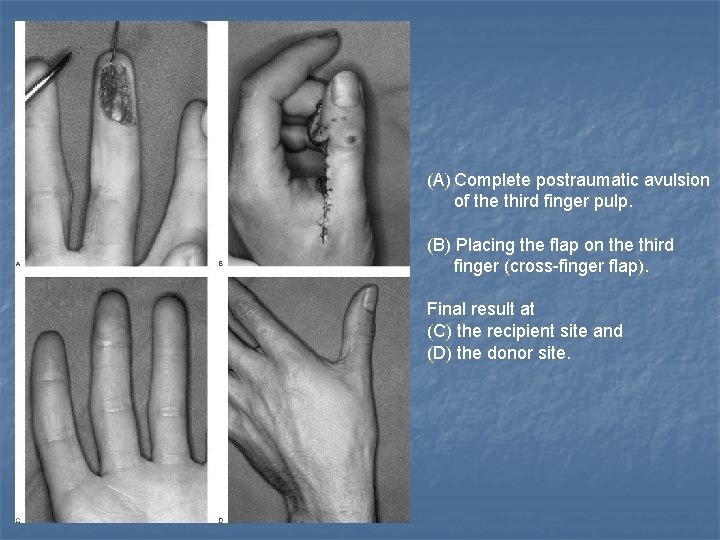
(A) Complete postraumatic avulsion of the third finger pulp. (B) Placing the flap on the third finger (cross-finger flap). Final result at (C) the recipient site and (D) the donor site.

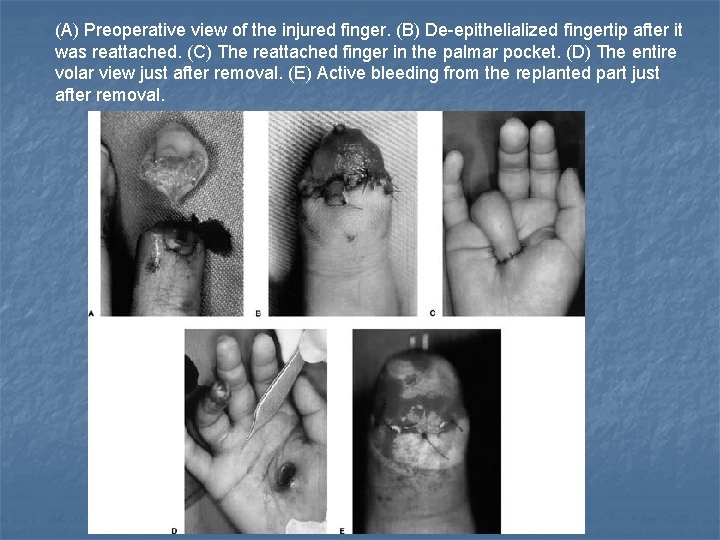
THENAR FLAP

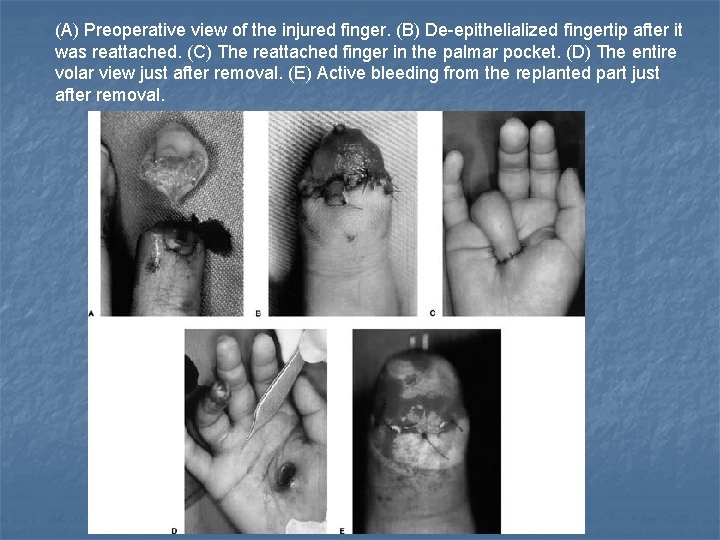
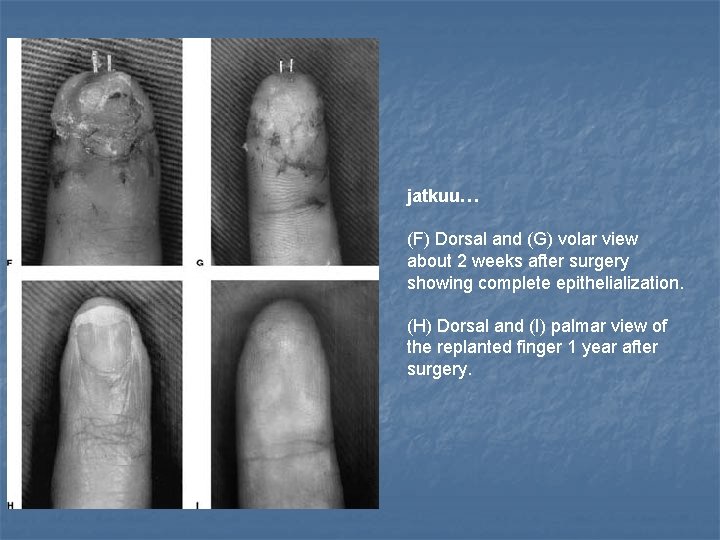
(A) Preoperative view of the injured finger. (B) De-epithelialized fingertip after it was reattached. (C) The reattached finger in the palmar pocket. (D) The entire volar view just after removal. (E) Active bleeding from the replanted part just after removal.
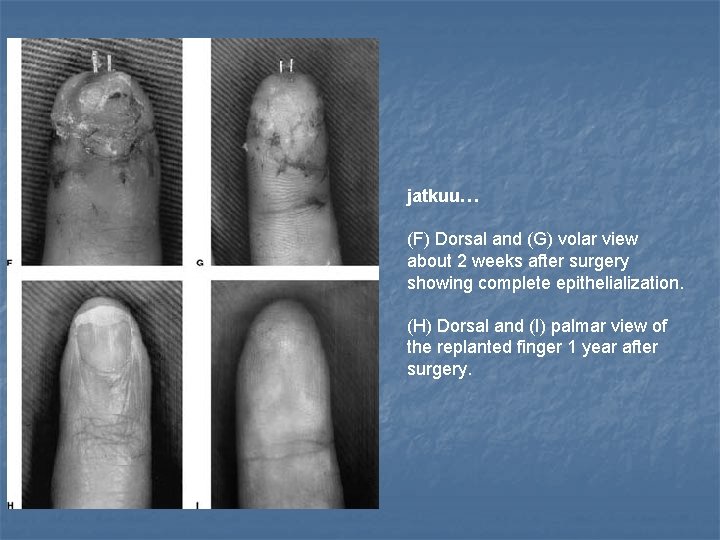
jatkuu… (F) Dorsal and (G) volar view about 2 weeks after surgery showing complete epithelialization. (H) Dorsal and (I) palmar view of the replanted finger 1 year after surgery.
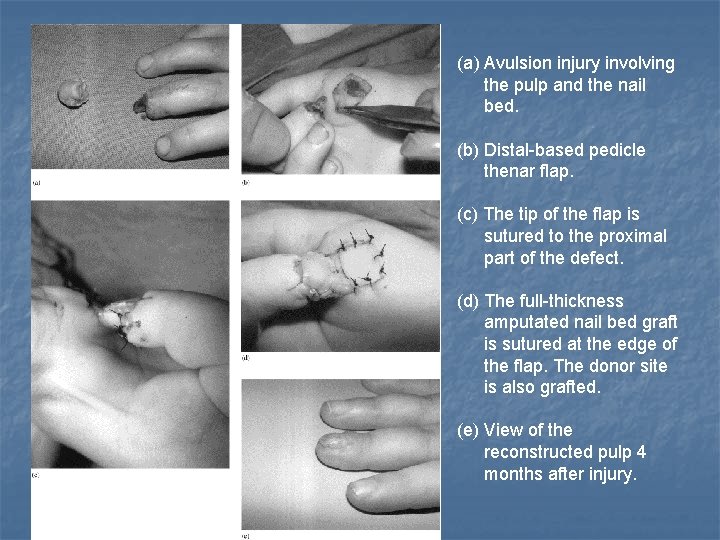
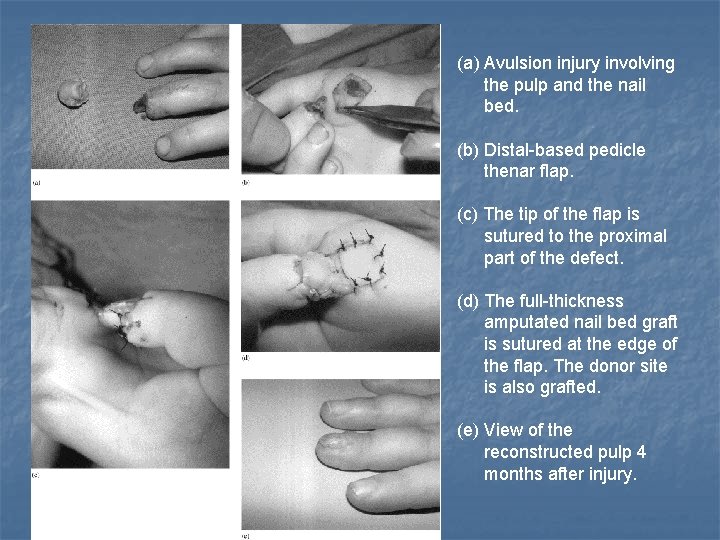
(a) Avulsion injury involving the pulp and the nail bed. (b) Distal-based pedicle thenar flap. (c) The tip of the flap is sutured to the proximal part of the defect. (d) The full-thickness amputated nail bed graft is sutured at the edge of the flap. The donor site is also grafted. (e) View of the reconstructed pulp 4 months after injury.

NEUROVASCULAR ISLAND FLAP

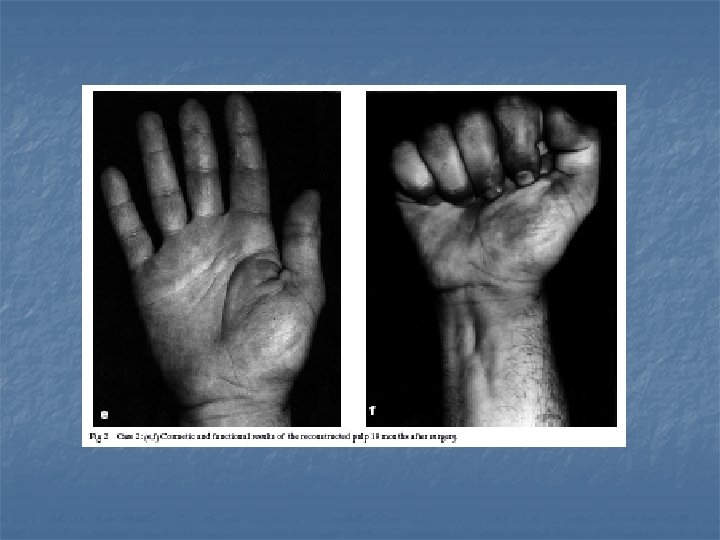
The NVIF is transferred from the ulnar side of the middle finger to the thumb. It covers the thumb from the dorsal nail area to the proximal volar region.
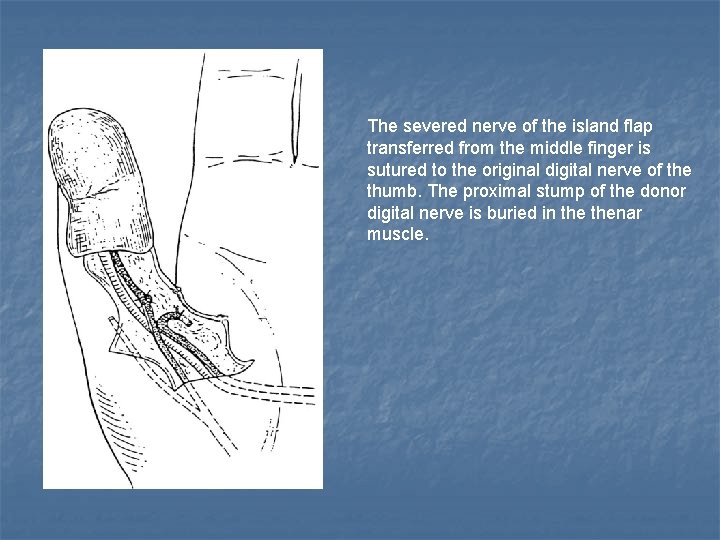
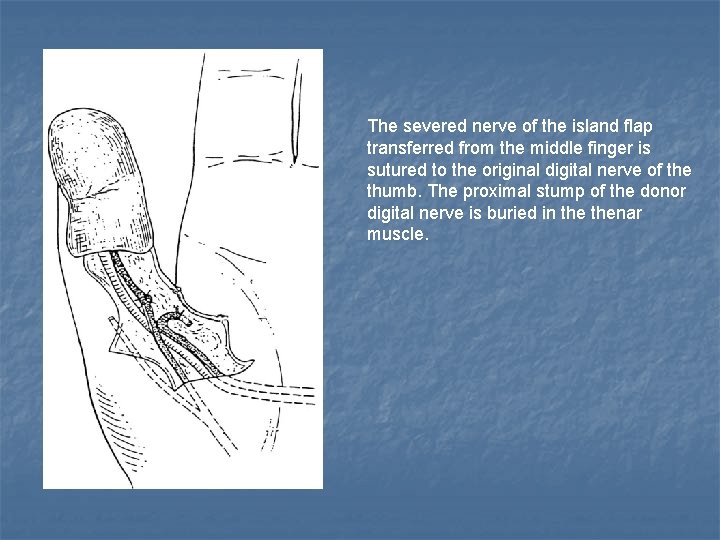
The severed nerve of the island flap transferred from the middle finger is sutured to the original digital nerve of the thumb. The proximal stump of the donor digital nerve is buried in thenar muscle.
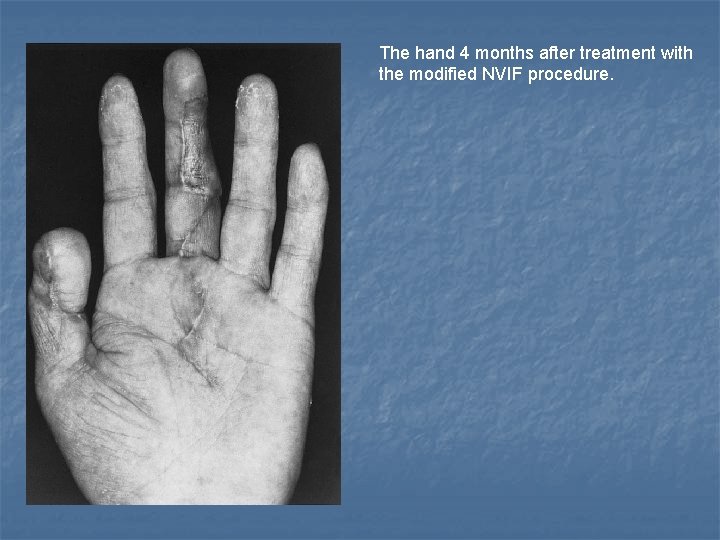
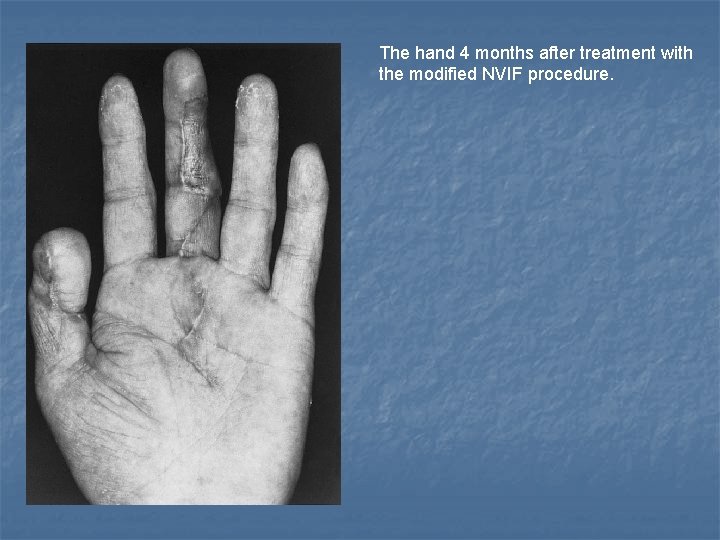
The hand 4 months after treatment with the modified NVIF procedure.

 Marko sunnari
Marko sunnari V-y plastia
V-y plastia Jorma tarhio
Jorma tarhio Jorma takanen
Jorma takanen Jorma nokkala
Jorma nokkala Jorma lempinen
Jorma lempinen Jorma tähkä
Jorma tähkä Sarv head
Sarv head Jorma härkönen
Jorma härkönen Jorma imppola
Jorma imppola Norddrg
Norddrg Jorma imppola
Jorma imppola 2 tyypin diabeteksen lääkehoito
2 tyypin diabeteksen lääkehoito Kipeä niska oulu
Kipeä niska oulu Sinikieliskinkki
Sinikieliskinkki Brickerin diversio
Brickerin diversio Viisaudenhammas niskakipu
Viisaudenhammas niskakipu Vastasyntyneen elvytys käypä hoito
Vastasyntyneen elvytys käypä hoito Kannabinoidireseptorit
Kannabinoidireseptorit Hoito thunder bay
Hoito thunder bay Radikulaatio
Radikulaatio Mortonin neurooma rasitusmurtuma
Mortonin neurooma rasitusmurtuma Karieksen hallinta
Karieksen hallinta Kkk hoito
Kkk hoito Panacod vyöruusu
Panacod vyöruusu Lautuma ennen kuolemaa
Lautuma ennen kuolemaa Tic oireet
Tic oireet Käypä hoito epilepsia
Käypä hoito epilepsia Dystymia hoito
Dystymia hoito Tics-hoito
Tics-hoito Cavilon suihke
Cavilon suihke Käypä hoito hyppääjän polvi
Käypä hoito hyppääjän polvi Lada diabetes oireet
Lada diabetes oireet