PERIODONTAL FLAP CONTENTS q DEFINITION q CLASSIFICATION q









- Slides: 37

PERIODONTAL FLAP
CONTENTS q DEFINITION q CLASSIFICATION q INDICATIONS q CONTRAINDICATION q FLAP DESIGNS q INCISIONS q ELEVATION OF FLAP q SUTURING TECHNIQUES

q TYPES OF SUTURES q FLAP TECHNIQUES FOR POCKET THERAPY q HEALING OF A PERIODONTAL FLAP
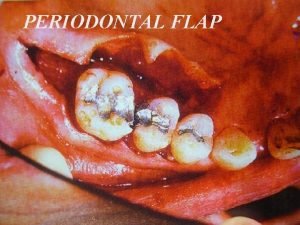
DEFINITION q Periodontal flap is a section of gingiva and / or mucosa surgically separated from the underlying tissue to provide visibility and access to the bone and root surface.
WHY TO RAISE A PERIODONTAL FLAP? q Increase accessibility to root deposits q Eliminate or reduce pocket depth by resection of the pocket wall. q Expose the area to perform regenerative procedures
CONTRAINDICATIONS q When sufficient accessibility can be attained q Prognosis of the tooth in the affected area is very poor q Systemic diseases ( bleeding disorders, history of MI within 6 months) q End stage diseases ( leukemia)
CLASSIFICATION q IT IS BASED UPON………. . q Bone exposure after flap reflection q Placement of the flap after surgery q Management of the papilla
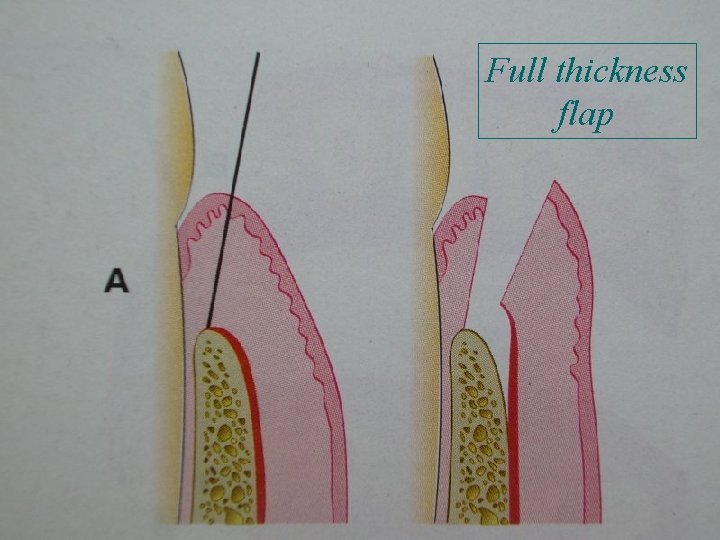
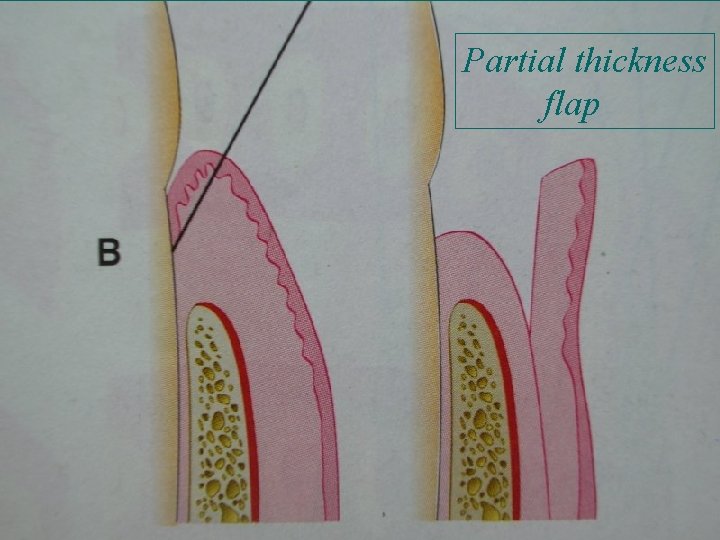
BONE EXPOSURE AFTER FLAP REFLECTION q FULL THICKNESS FLAP All the soft tissue including the periosteum is reflected to expose the underlying bone eg. Resective osseous surgery q PARTIAL THICKNESS FLAP Only the epithelium along with a layer of the connective tissue, but the bone remains covered with a layer of connective tissue and the periosteum Eg. Flap to be positioned apically, operator doesn’t want bone exposure
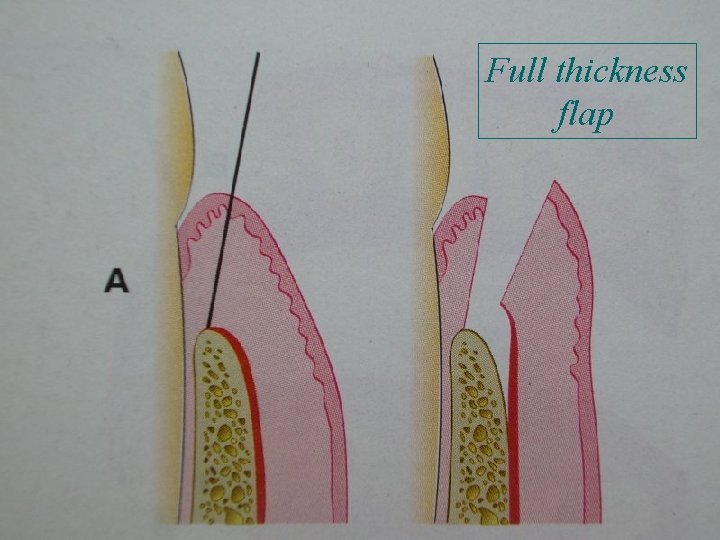
Full thickness flap
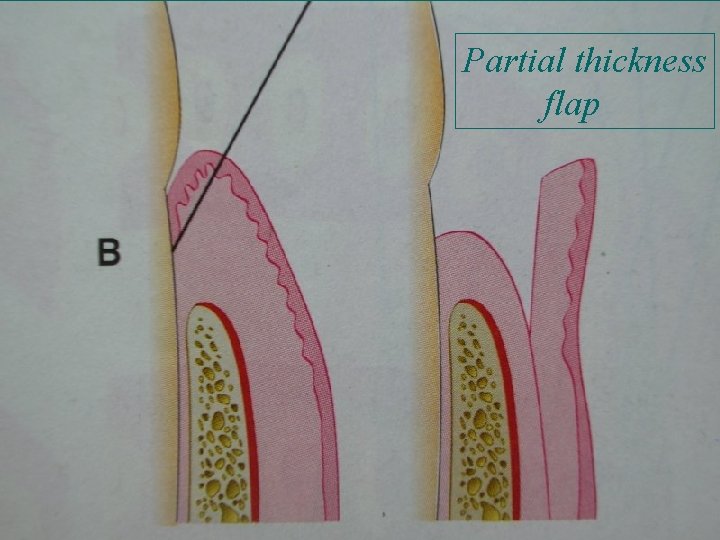
Partial thickness flap
BASED ON THE FLAP PLACEMENT AFTER SURGERY q NON-DISPLACED FLAP These flaps are returned and sutured back to their original position q DISPLACED FLAP They may be apically , coronally, or laterally displaced. Preserves the outer pocket wall and transforms it to the attached gingiva. Palatal flaps cannot be displaced because of absence of attached gingiva.
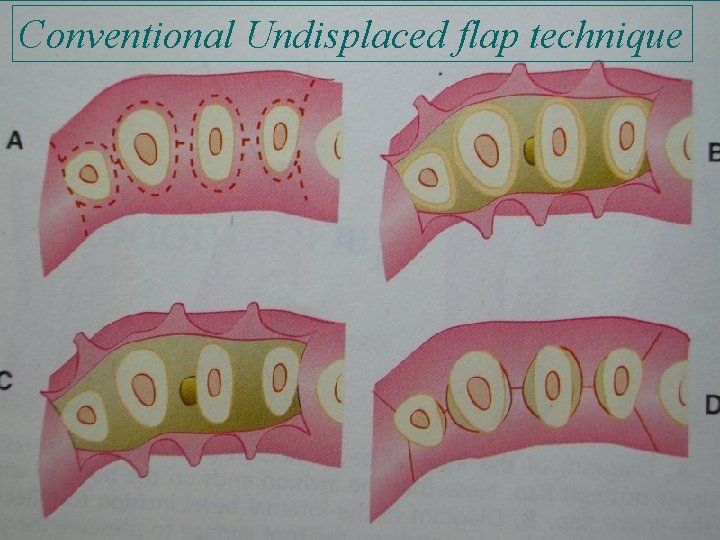
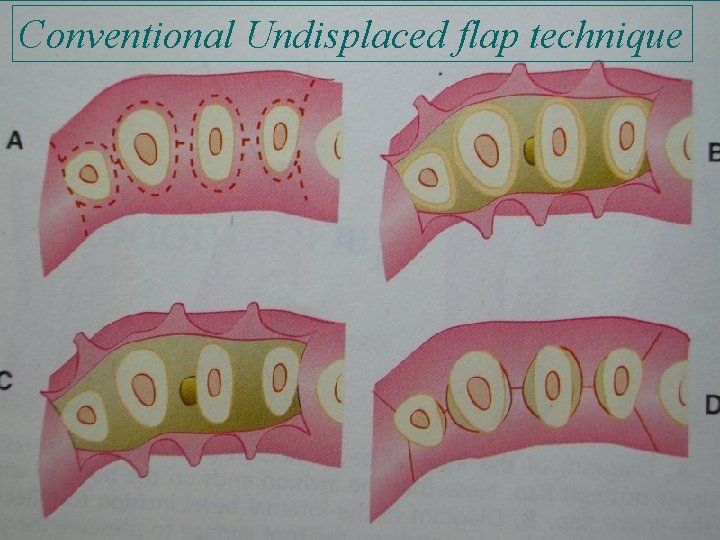
Conventional Undisplaced flap technique

Apically Displaced flap
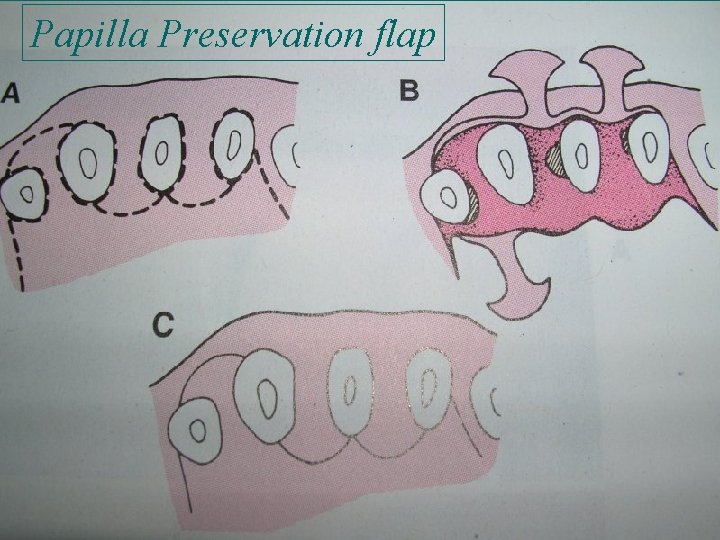
BASED ON THE MANAGEMENT OF PAPILLA q CONVENTIONAL FLAP It includes the- apically displaced flap, undisplaced flap, mod. Widman flap The interdental papilla is split beneath the contact point of the two approximating teeth to raise the buccal and the lingual flap. It is raised when the interdental spaces are very narrow and when the flap is to be displaced.
q PAPILLA PRESERVATION FLAP Incorporates the entire papilla in one of the flaps by means of a crevicular incision to sever the connective tissue attachment and a horizontal incision at the base of the papilla leaving it connected to one of the flaps
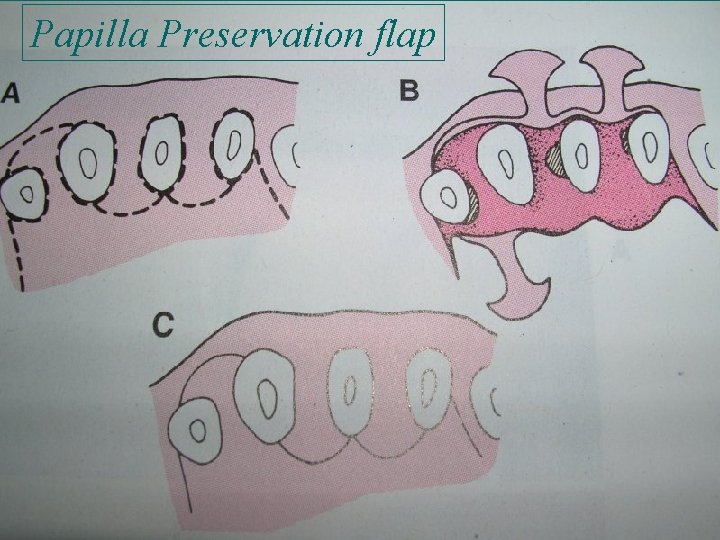
Papilla Preservation flap
FLAP DESIGN q The success of a flap generally depends on two broad criteriaq The base of the flap should be wider which provides a good blood supply to the flap. q When positioned back, it should rest on sound bone. q The design of the flap is solely dependent on the particular requirements of the specific case.

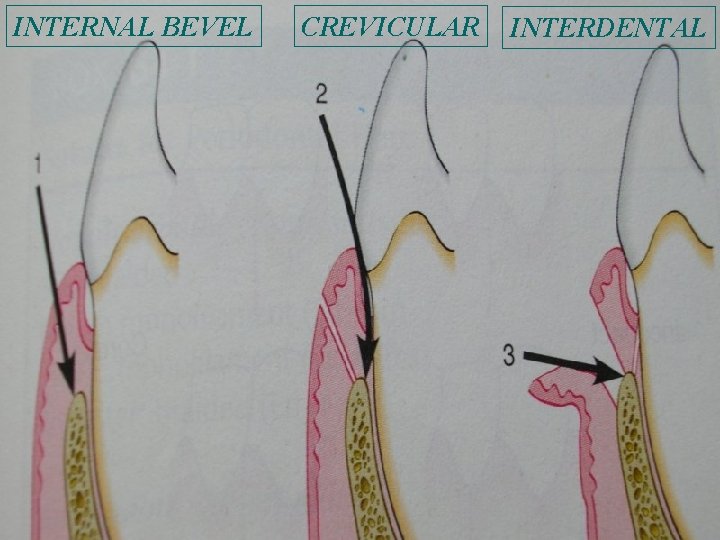
INCISIONS q Two types of incisions – q HORIZONTAL INCISION Internal bevel incision Crevicular incision q VERTICAL INCISION Oblique releasing incision
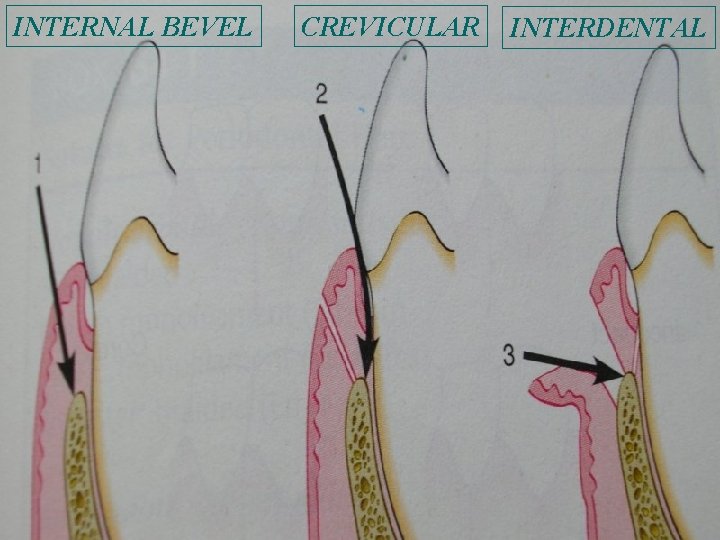
INTERNAL BEVEL CREVICULAR INTERDENTAL
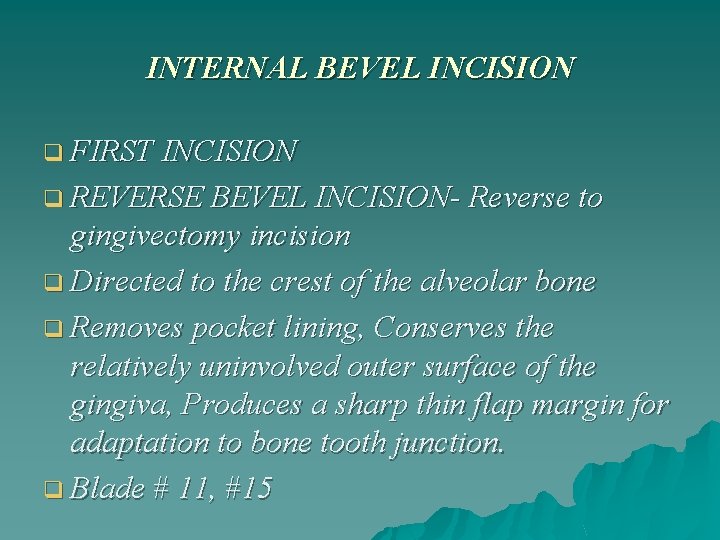
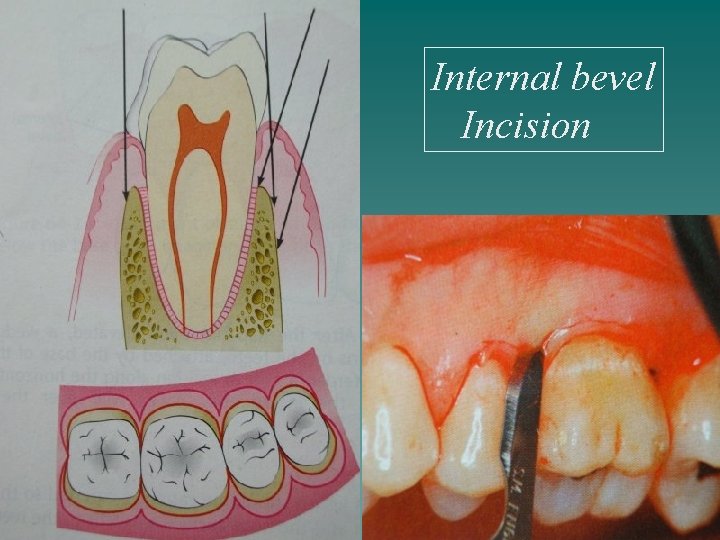
INTERNAL BEVEL INCISION q FIRST INCISION q REVERSE BEVEL INCISION- Reverse to gingivectomy incision q Directed to the crest of the alveolar bone q Removes pocket lining, Conserves the relatively uninvolved outer surface of the gingiva, Produces a sharp thin flap margin for adaptation to bone tooth junction. q Blade # 11, #15
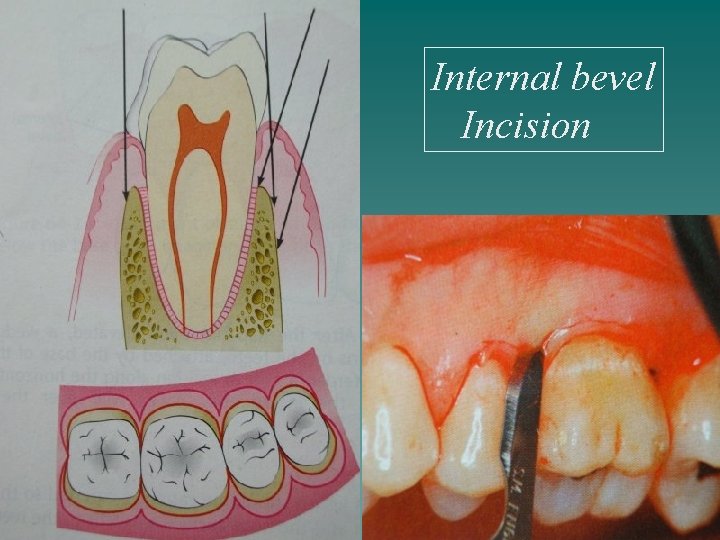
Internal bevel Incision
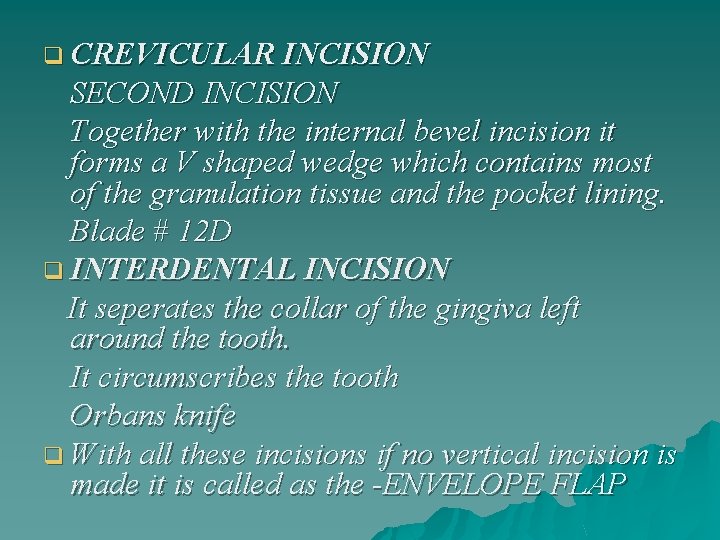
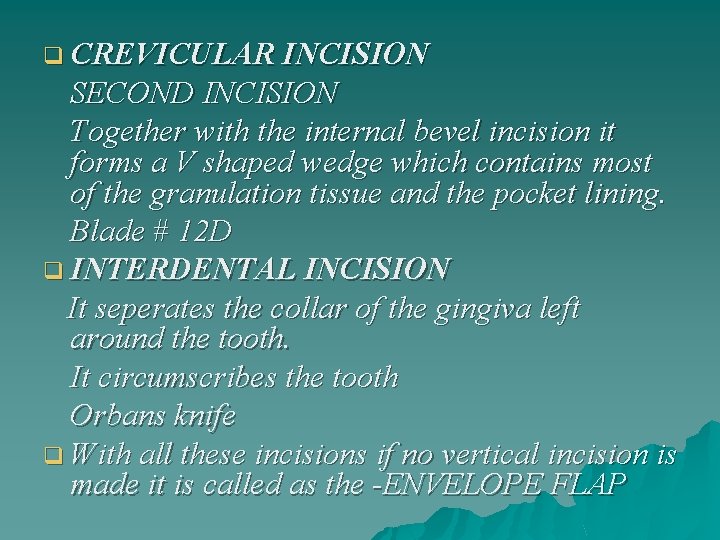
q CREVICULAR INCISION SECOND INCISION Together with the internal bevel incision it forms a V shaped wedge which contains most of the granulation tissue and the pocket lining. Blade # 12 D q INTERDENTAL INCISION It seperates the collar of the gingiva left around the tooth. It circumscribes the tooth Orbans knife q With all these incisions if no vertical incision is made it is called as the -ENVELOPE FLAP
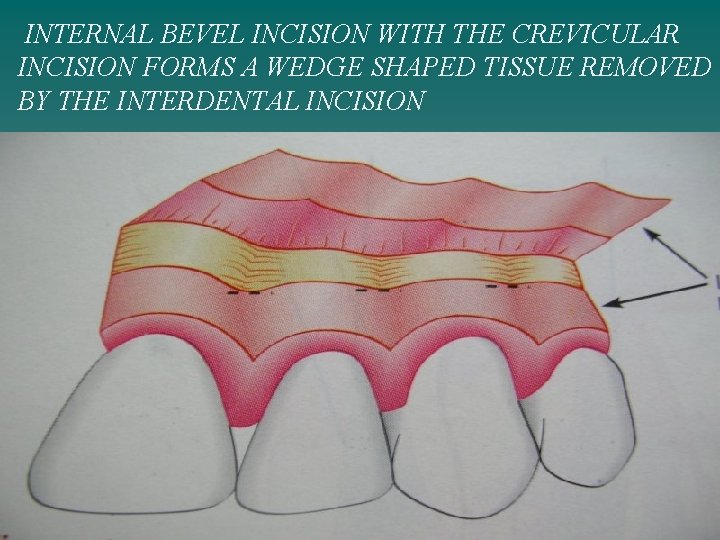
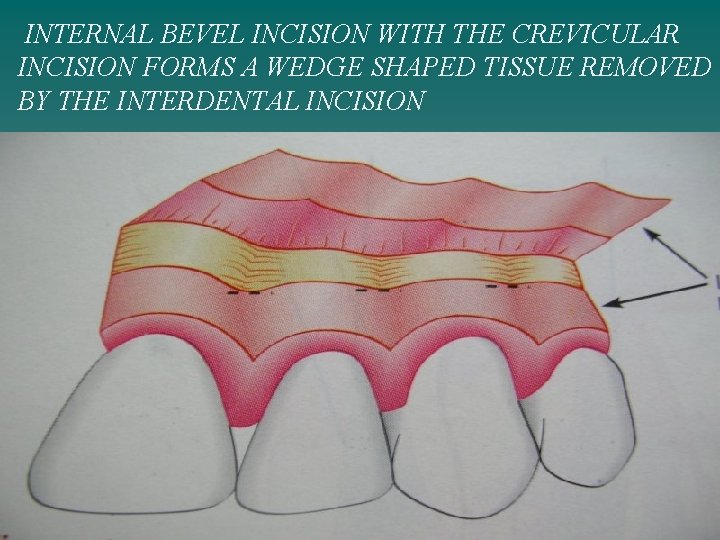
INTERNAL BEVEL INCISION WITH THE CREVICULAR INCISION FORMS A WEDGE SHAPED TISSUE REMOVED BY THE INTERDENTAL INCISION
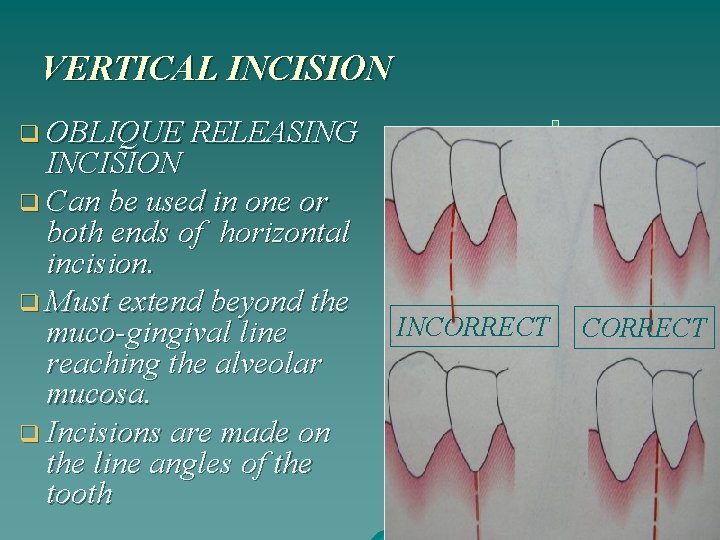
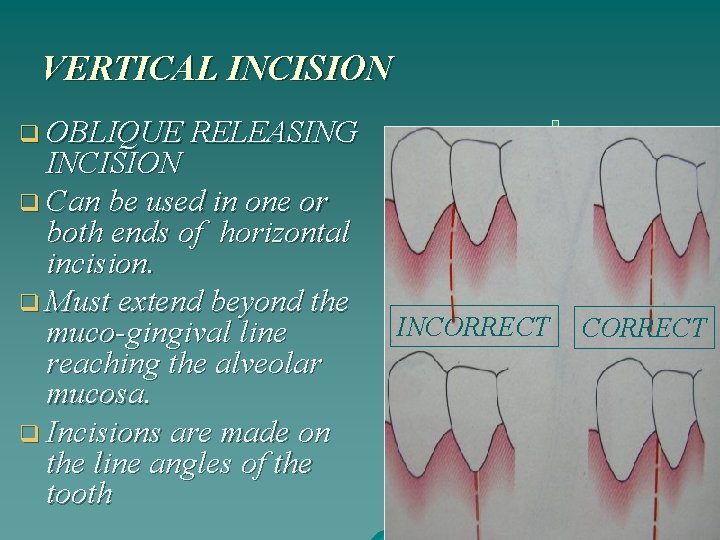
VERTICAL INCISION q OBLIQUE RELEASING INCISION q Can be used in one or both ends of horizontal incision. q Must extend beyond the muco-gingival line reaching the alveolar mucosa. q Incisions are made on the line angles of the tooth INCORRECT
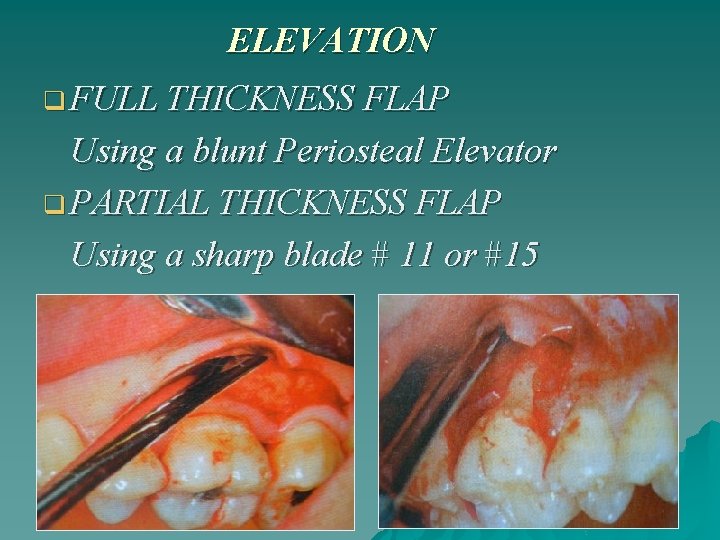
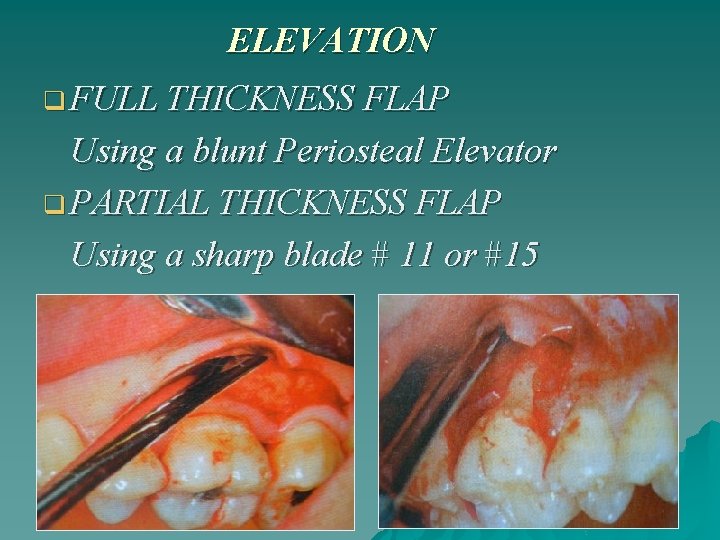
ELEVATION q FULL THICKNESS FLAP Using a blunt Periosteal Elevator q PARTIAL THICKNESS FLAP Using a sharp blade # 11 or #15

SUTURING TECHNIQUES SUTURING MATERIALS q NON-ABSORVABLE q Silk: braided q Nylon: monofilament ( Gore -tex) q Polyester: braided ( Ethibond) q ABSORVABLE q Surgical: Gut q Plain gut: monofilament q Chromic cat gut: monofilament q SYNTHETIC q Polyglycolic: Vicryl, Dexon q Monocryl ( Ethicon) q Polyglyconate: monofilament q
TYPES OF SUTURES q Horizontal mattress suture- in interproximal area of diastema or for wide interdental spaces to adapt interproximal papilla. q Continuous independent sling suture- when there is both a facial and lingual flap involving many teeth. q Anchor suture- closing of a flap mesial or distal to a tooth as in mesial and distal wedge procedures. q Closed anchor suture- to close a flap located in an edentulous area. q Periosteal suture- to hold in place apically displaced flap.
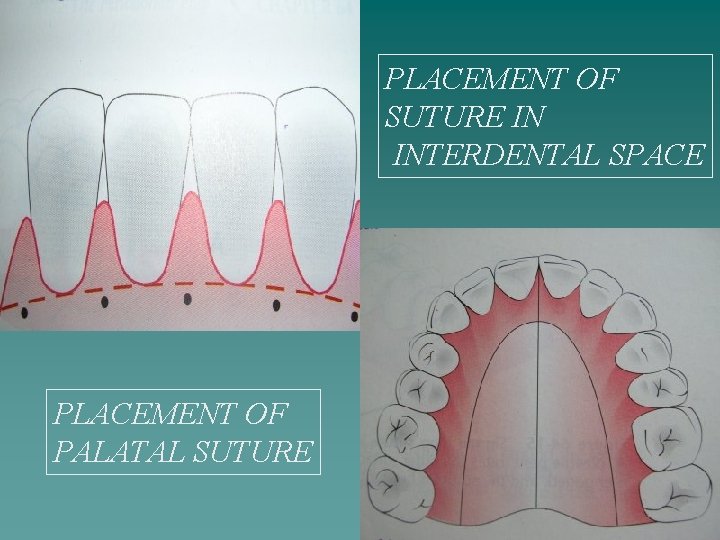
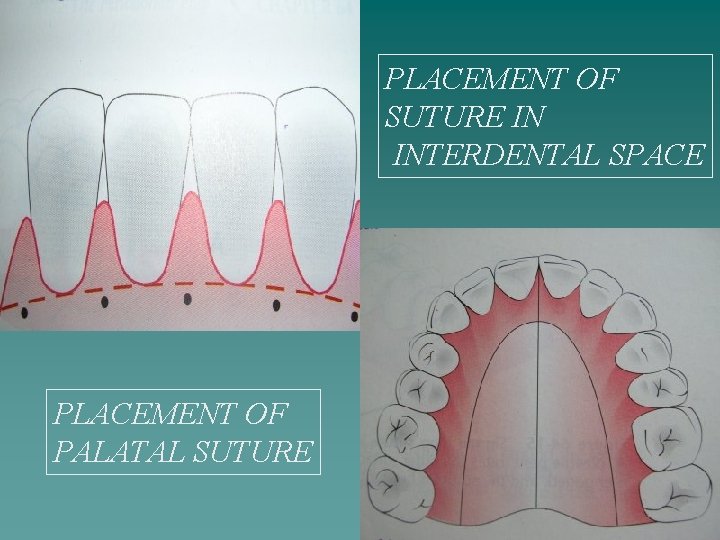
PLACEMENT OF SUTURE IN INTERDENTAL SPACE PLACEMENT OF PALATAL SUTURE

SIMPLE LOOP SUTURE INTERRUPTED FIGURE OF 8 SUTURE SINGLE INTERRUPTED SLING SUTURE
HEALING OF A PERIODONTAL FLAP q UPTO 24 HOURS q The connection between the flap and the tooth is established by a blood clot. q 1 TO 3 DAYS AFTER FLAP SURGERY q Epithelial cells migrate over the border of the flap usually contacting the tooth at this time. , minimum inflamatory response. q I WEEK AFTER SURGERY q Epithelial attachment to the root has been established by means of hemi-desmosomes and basal lamina, the blood clot replaced by granulation tissue.
q 2 WEEKS AFTER SURGERY q Collagen fibres begins to appear parallel to the root surface. The epithelial attachment is still weak. q 1 MONTH AFTER SURGERY q A fully epithelized gingival crevice is generally formed with epithelial attachment and beginning of functional arrangement of supracrestal fibres.
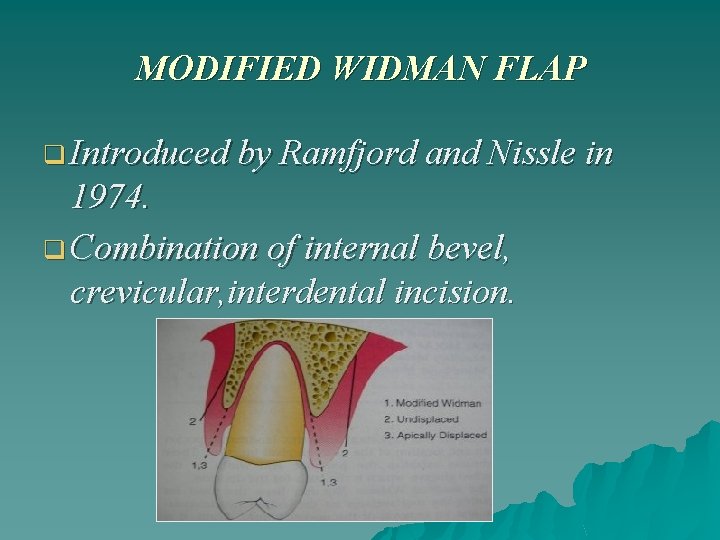
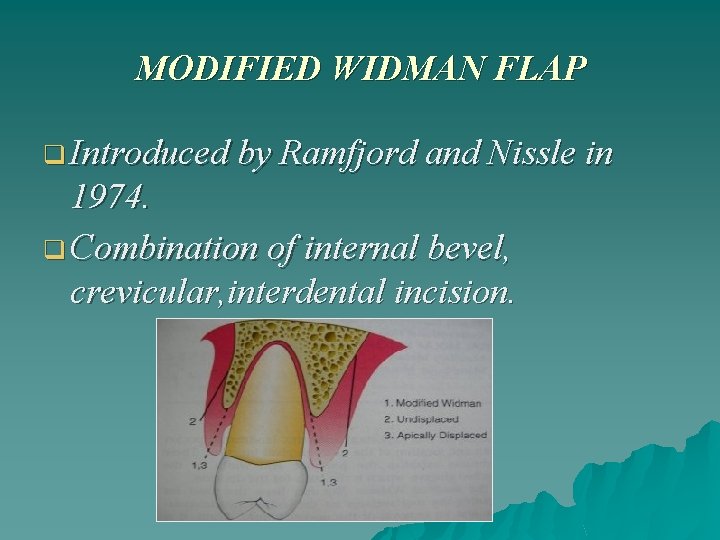
MODIFIED WIDMAN FLAP q Introduced by Ramfjord and Nissle in 1974. q Combination of internal bevel, crevicular, interdental incision.
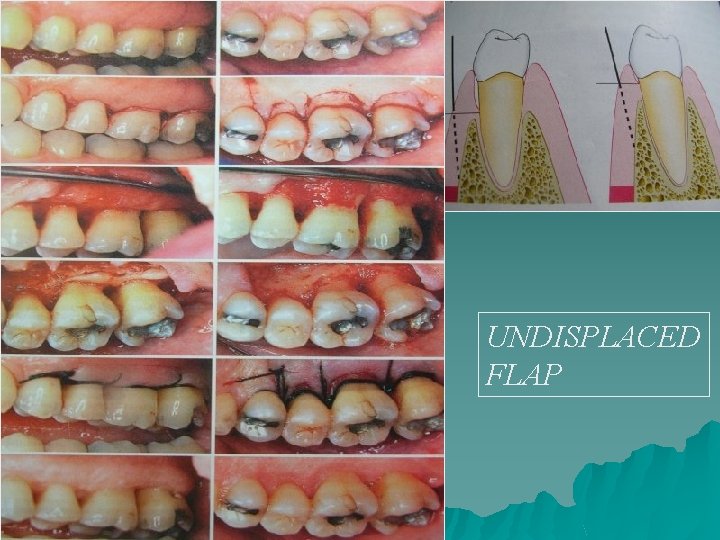
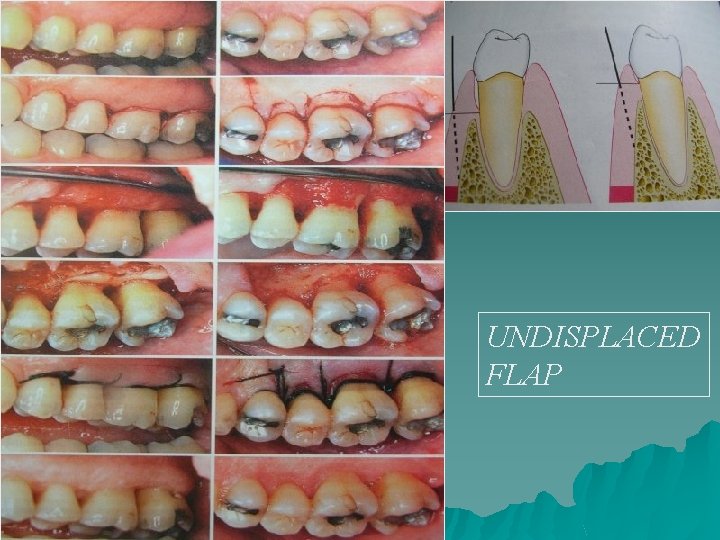
UNDISPLACED FLAP

APICALLY DISPLACED FLAP

PAPILLA PRESERVATION FLAP
CONCLUSION q Raising of a flap is a part and parcel of periodontal therapy, but the choice of flap for a patient is multifactorial and depends on the case variation. q The proper choice of a flap determines the success…. . In therapy

IS THIS WHAT U R DOING FOR ALL THIS TIME……. ? THANK U
 Reverse bevel incision
Reverse bevel incision Long posterior flap of burgess
Long posterior flap of burgess Periodontal instruments classification
Periodontal instruments classification Synonyms of periodontal ligament
Synonyms of periodontal ligament Alveolar bone proper lamina dura
Alveolar bone proper lamina dura Periodontal ligament injection definition
Periodontal ligament injection definition Corrective phase periodontal therapy
Corrective phase periodontal therapy Non displaced flap
Non displaced flap Reverse bevel incision
Reverse bevel incision Periodontal therapy in female patients
Periodontal therapy in female patients Plak boyayıcı ajanlar
Plak boyayıcı ajanlar Periodontal case study
Periodontal case study Iatrogenic factors in periodontal disease
Iatrogenic factors in periodontal disease Russell periodontal index
Russell periodontal index Ligamento periodontal
Ligamento periodontal Enap periodontal adalah
Enap periodontal adalah Rationale of periodontal treatment
Rationale of periodontal treatment Birleşim epiteli
Birleşim epiteli Paranky
Paranky Periodontal response to external forces
Periodontal response to external forces Periodontal treatment of medically compromised patients
Periodontal treatment of medically compromised patients Akut periodontal apse
Akut periodontal apse Tecnica de step back
Tecnica de step back Heliprobe 2 positivo
Heliprobe 2 positivo Periodontal dokuların embriyolojisi
Periodontal dokuların embriyolojisi Diagnosis of periodontal disease
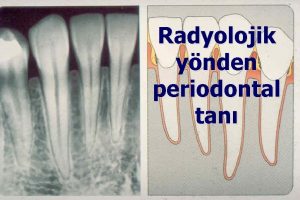
Diagnosis of periodontal disease Periapical granuloma
Periapical granuloma Non corticated
Non corticated Periodontal abscess
Periodontal abscess Periodontal disease
Periodontal disease Kista residual adalah
Kista residual adalah Periodontal charting symbols
Periodontal charting symbols Gtr indications
Gtr indications Principles of periodontal surgery
Principles of periodontal surgery Caruncula sublingualis
Caruncula sublingualis Grupos de fibras del ligamento periodontal
Grupos de fibras del ligamento periodontal Ligamento periodontal
Ligamento periodontal Nabers sondu
Nabers sondu