Flap Failure it happens to us all Flap

- Slides: 13
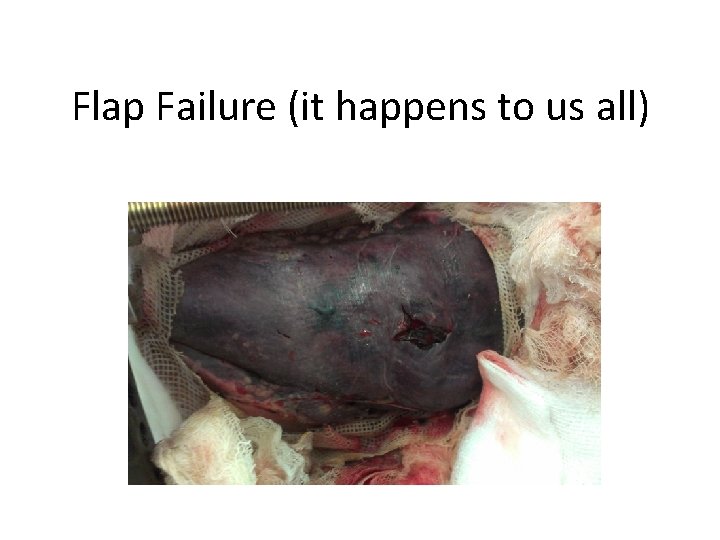
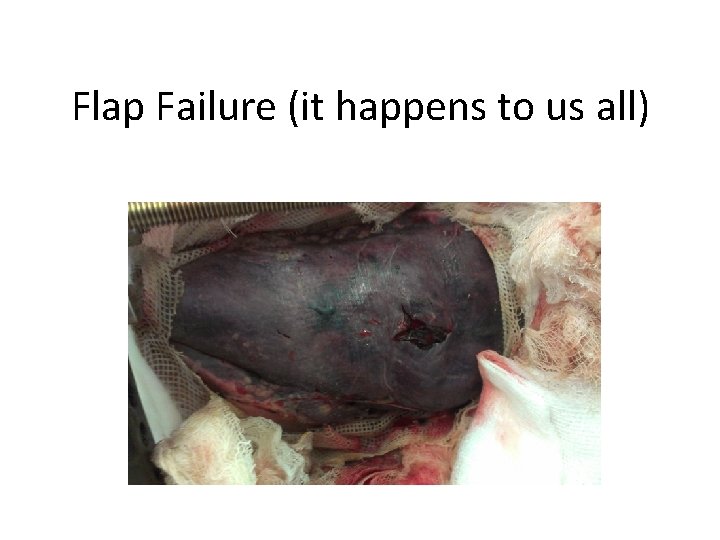
Flap Failure (it happens to us all)
Flap failure How to • Prevent it • Recognise it • Treat it
Prevention of flap failure • Patient factors – Local – General • ‘Surgeon’ factors – Technique – Team – Equipment – Anaesthetic factors – Post-op care – timing
Patient factors • Local – Radiotherapy • Khouri PRS 1998 survey of 23 surgeons and all their flap failures over 6 months 4. 1% failure v 9. 4% • Mullholland PRS 1993 >300 cases with 2/3 in irradiated tissue 3. 5% v 2. 8% but noted higher failure rate with increased time from DXR to surgery • Recommendations – pre DXR or as soon after as possible and anastamosis outside zone if possible – Infection – Inflammation
Surgeon factors • Technique – End to end or end to side? – Practise like your livelihood depended on it • Initial large number in simulated setting to overcome the learning curve • Ongoing practise – at least once a fortnight

Surgeon factors • Technique – Meticulous attention to detail at every stage from choice of flap, size of flap, choice of vessels Size discrepancy Pedicle length Pedicle position – don’t relax too quickly after the anastamosis is finished or your pedicle will become kinked • Don’t be in a rush to finish • Any doubt – REDO IT • • •
Surgeon factors • Team – Define roles – Scrub staff training and cues – Flap time off and on • Equipment • Anaesthetic – What do you need from the anaesthetic team to make sure this is a safe procedure for the patient and the flap
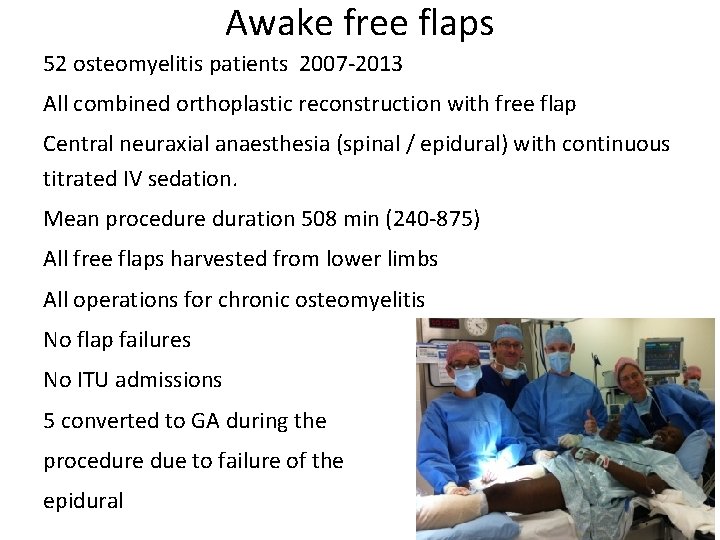
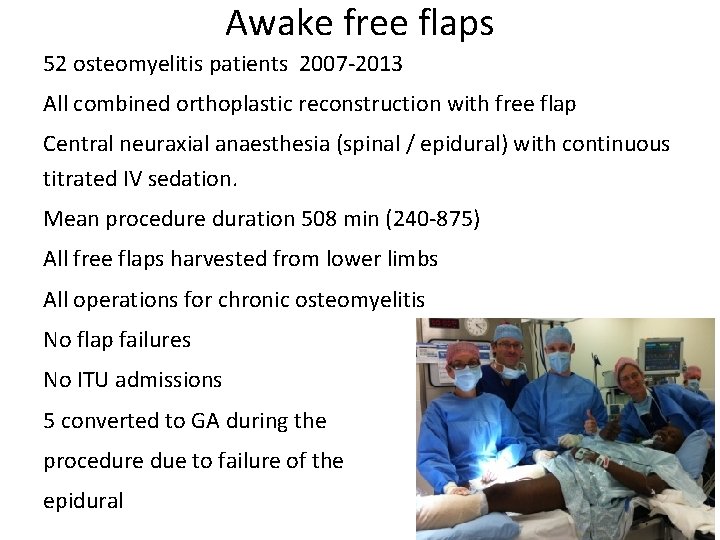
Awake free flaps 52 osteomyelitis patients 2007 -2013 All combined orthoplastic reconstruction with free flap Central neuraxial anaesthesia (spinal / epidural) with continuous titrated IV sedation. Mean procedure duration 508 min (240 -875) All free flaps harvested from lower limbs All operations for chronic osteomyelitis No flap failures No ITU admissions 5 converted to GA during the procedure due to failure of the epidural
‘Surgeon’ Factors • Post-op care – Position of patient in recovery – Creating the perfect environment for a flap • Timing – The earlier the better – If late presentation don’t delay but ensure fearless debridement Fearless debridement
Recognise it • • Team One to one care in PACU No place for denial Use all methods of monitoring available to you and act immediately if any of them show signs of impending failure. – 5% return to theatre of which 50% are salvaged – 3% overall failure rate
Treat it • Return to theatre – Lift flap and check for haematoma – Flow check anastamosis – ANY DOUBT REDO