EMPYEMA FELICITY MEIKLE FRACS WAIKATO CARDIOTHORACIC UNIT PLEURA


- Slides: 40
EMPYEMA FELICITY MEIKLE, FRACS WAIKATO CARDIOTHORACIC UNIT
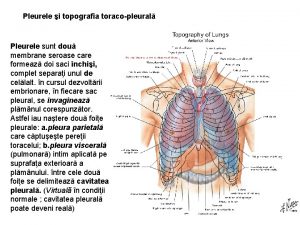
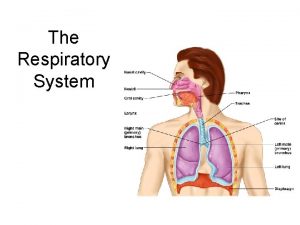
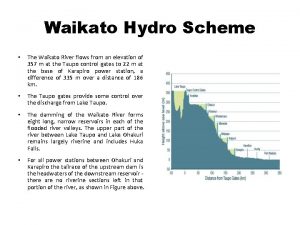
PLEURA • SEROUS MEMBRANE • PLEURAL CAVITY IS POTENTIAL SPACE BETWEEN VISCERAL AND PARIETAL PLEURA • NORMALLY CONTAINS A SMALL AMOUNT OF FLUID • PARIETAL PLEURA VERY SENSITIVE TO PAIN • IMPROVES RESPIRATION AND TRANSMISSION OF FORCES TO LUNGS • HUMANS HAVE SEPARATE PLEURAL CAVITIES
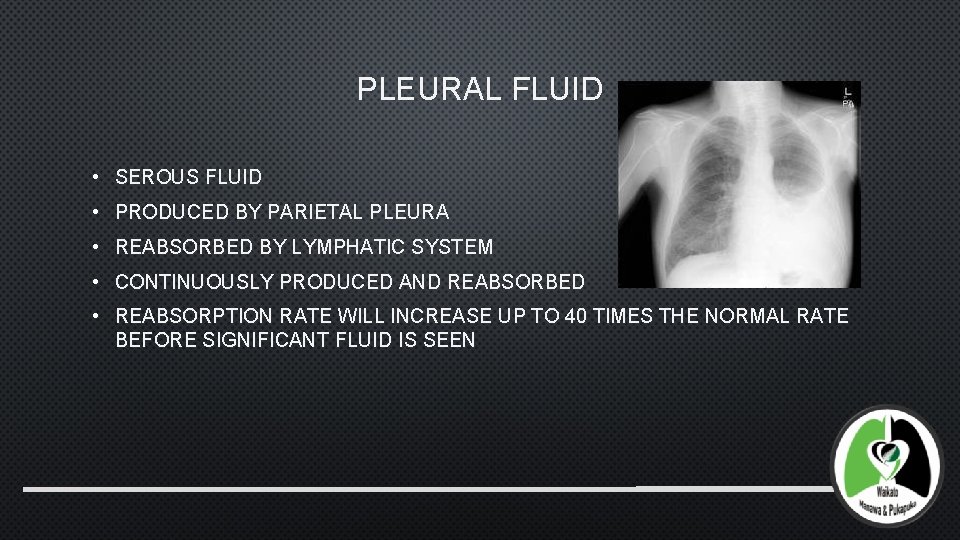
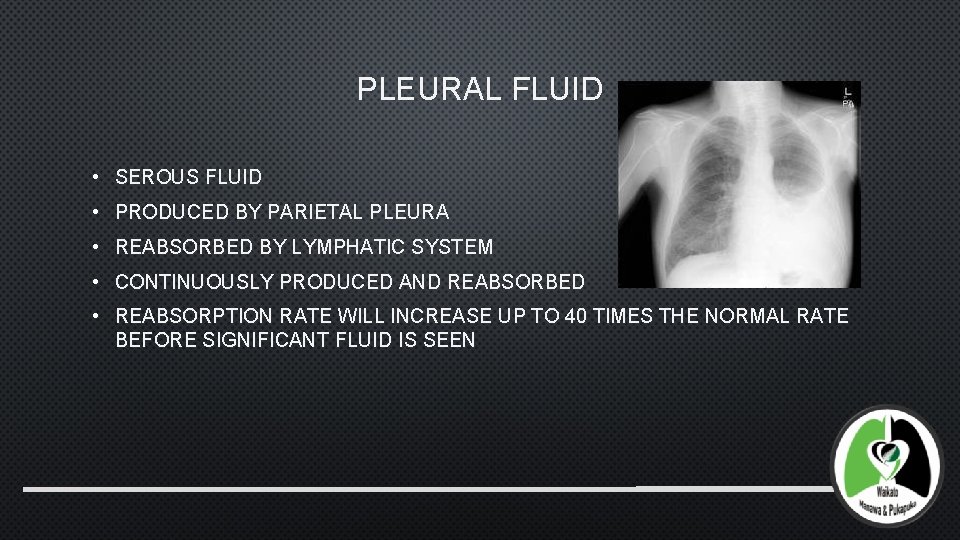
PLEURAL FLUID • SEROUS FLUID • PRODUCED BY PARIETAL PLEURA • REABSORBED BY LYMPHATIC SYSTEM • CONTINUOUSLY PRODUCED AND REABSORBED • REABSORPTION RATE WILL INCREASE UP TO 40 TIMES THE NORMAL RATE BEFORE SIGNIFICANT FLUID IS SEEN
PARAPNEUMONIC EFFUSION • BACTERIAL PNEUMONIA ASSOCIATED WITH PLEURAL EFFUSION (35 -40% OF HOSPITALIZED PNEUMONIA) • PNEUMOCOCCAL – 60% EFFUSION RATE • UNCOMPLICATED – NEGATIVE GRAM STAIN, NO LOCULATIONS, RESOLVE SPONTANEOUSLY • COMPLICATED (20%) – EMPYEMA OR LOCULATED EFFUSIONS, REQUIRE DRAINAGE • LOW PH <7. 2, HIGH LDH >1000 SUGGESTS COMPLICATED EFFUSION
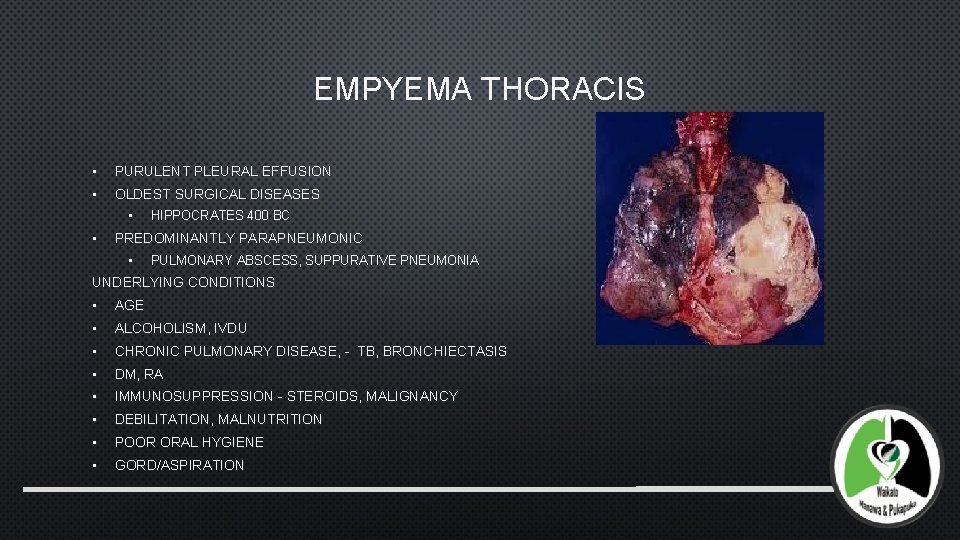
EMPYEMA THORACIS • PURULENT PLEURAL EFFUSION • OLDEST SURGICAL DISEASES • • HIPPOCRATES 400 BC PREDOMINANTLY PARAPNEUMONIC • PULMONARY ABSCESS, SUPPURATIVE PNEUMONIA UNDERLYING CONDITIONS • AGE • ALCOHOLISM, IVDU • CHRONIC PULMONARY DISEASE, - TB, BRONCHIECTASIS • DM, RA • IMMUNOSUPPRESSION - STEROIDS, MALIGNANCY • DEBILITATION, MALNUTRITION • POOR ORAL HYGIENE • GORD/ASPIRATION
OTHER CAUSES - TRAUMA PENETRATING INJURY • 1. 6% INCIDENCE • ORGANIC FOREIGN BODIES BEING CARRIED INTO PLEURAL SPACE HAEMOTHORAX • HAEMOPNEUMOTHORAX MORE LIKELY TO BECOME INFECTED • SECONDARY INFECTION FROM CHEST TUBE – HIGHLIGHTS IMPORTANCE OF STRICT ASEPSIS
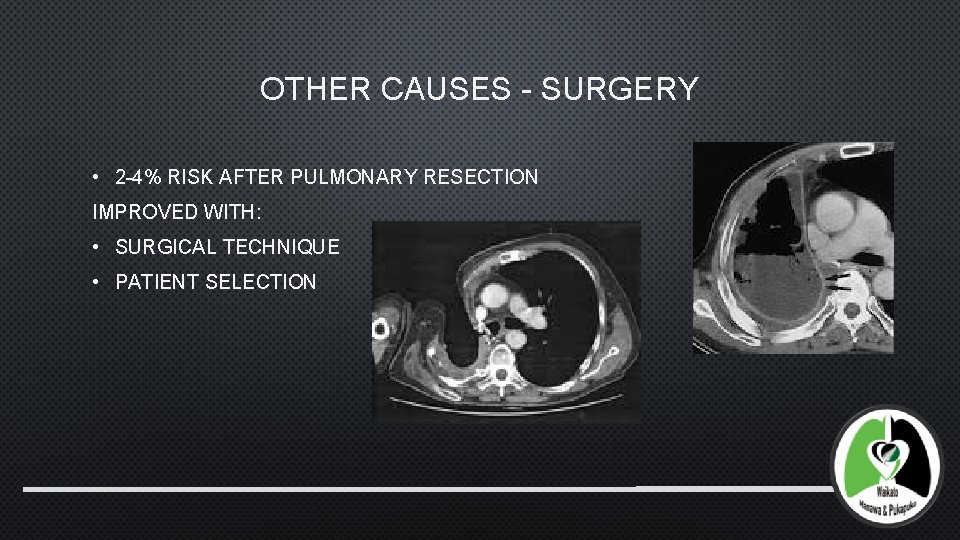
OTHER CAUSES - SURGERY • 2 -4% RISK AFTER PULMONARY RESECTION IMPROVED WITH: • SURGICAL TECHNIQUE • PATIENT SELECTION
OTHER CAUSES • RUPTURE OF OESOPHAGUS • INFECTION FROM POSTERIOR REGION OF THE NECK • CHEST WALL INFECTIONS • THORACIC SPINE • SUBPHRENIC INFECTIONS – TEND TO BE REACTIVE • HAEMATOGENOUS SPREAD IN IMMUNOCOMPROMISED PATIENT
BACTERIOLOGY • PRE ANTIBIOTICS ERA – PNEUMOCOCCI 64%, S. PNEUMONIAE (EHLER 1941) • GREATER LUNG DESTRUCTION MORE ABSCESS FORMATION RECENTLY – • NO INOCULATE FOUND IN 80% • STREPTOCOCCUS SPECIES 30% – S PNEUMONIAE/PYOGENES/MILLERI • STAPH AUREUS ~34% - POST OP/TRAUMA • GRAM -VE – KLEBSIELLA, PSEUDOMONAS, HAEMOPHILUS • ANAEROBES 35% - BACTEROIDES, PEPTOSTREPTOCOCCUS • COMPLEX INOCULATES – ASPIRATION PNEUMONIA
STAGES • 3 STAGES OVER 3 -6 WEEK PERIOD • STAGE 1: EXUDATIVE: 2 -5 DAYS - PLEURAL MEMBRANES SWELL AND DISCHARGE THIN EXUDATE, NEUTROPHILS PRESENT, NO ORGANISMS • INCREASED CAPILLARY PERMEABILITY • STAGE 2: FIBRINOPURULENT: 5 -10 DAYS - HEAVY DEPOSITION OF FIBRIN, PLEURAL FLUID TURBID, LOCULATIONS, NO ORGANISMS • BACTERIAL INFECTION • STAGE 3: ORGANISING: WITHIN 3 -4 WEEKS OVER 2 -3 WEEKS – THICK VISCOUS FLUID, THICK FIBROUS PEEL FORMS, LUNG BECOMES TRAPPED
DIAGNOSIS • SUSPECT EMPYEMA IN PATIENTS WITH ACUTE RESPIRATORY TRACT ILLNESS AND PLEURAL EFFUSION • PERSISTENT FEVER FOLLOWING AB THERAPY SYMPTOMS • DYSPNOEA - 82% • FEVER - 81% • COUGH - 70% • PLEURITIC PAIN 67% • TACHYPNOEA, TACHYCARDIAC • MALAISE, ANOREXIA, WEIGHT-LOSS • SIGNS – REDUCED CHEST WALL MOVEMENT, BREATH SOUNDS AND DULLNESS
BLOODS • LEUKOCYTOSIS • LEFT SHIFT OF NEUTROPHILS • CRP • BLOOD CULTURES • SPUTUM CULTURE
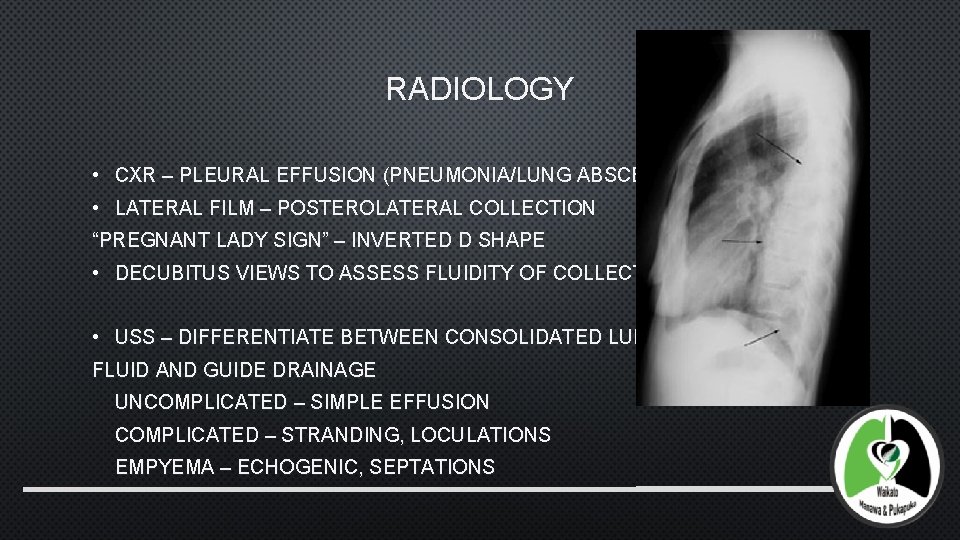
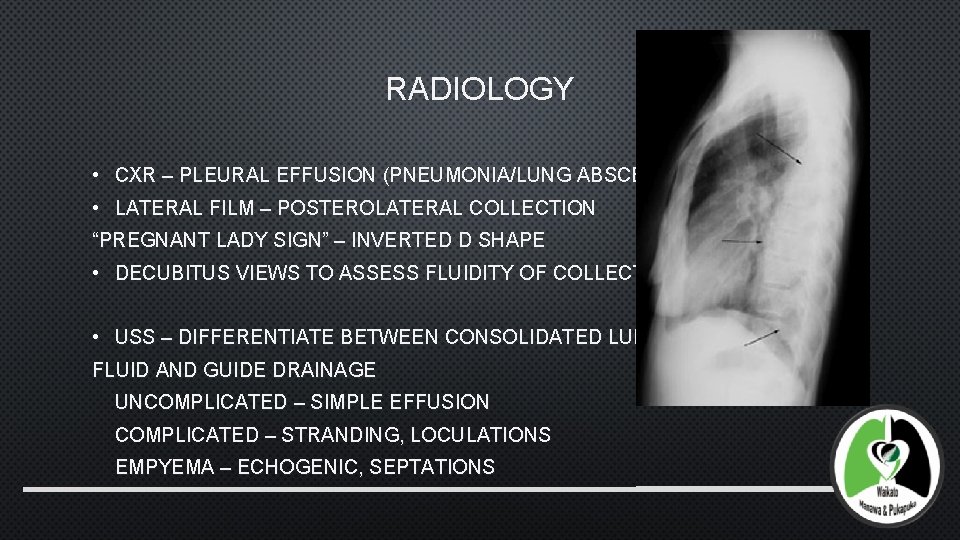
RADIOLOGY • CXR – PLEURAL EFFUSION (PNEUMONIA/LUNG ABSCESS) • LATERAL FILM – POSTEROLATERAL COLLECTION “PREGNANT LADY SIGN” – INVERTED D SHAPE • DECUBITUS VIEWS TO ASSESS FLUIDITY OF COLLECTION • USS – DIFFERENTIATE BETWEEN CONSOLIDATED LUNG AND FLUID AND GUIDE DRAINAGE UNCOMPLICATED – SIMPLE EFFUSION COMPLICATED – STRANDING, LOCULATIONS EMPYEMA – ECHOGENIC, SEPTATIONS
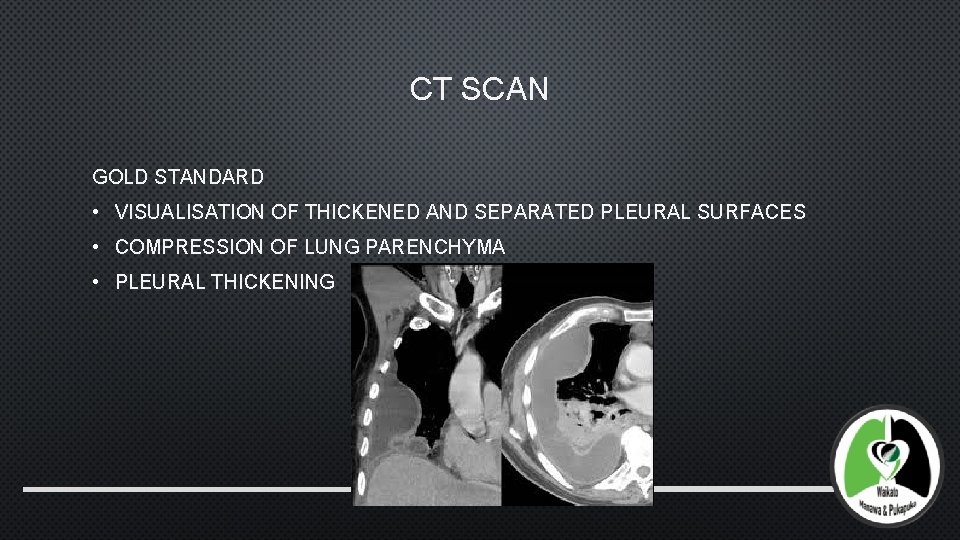
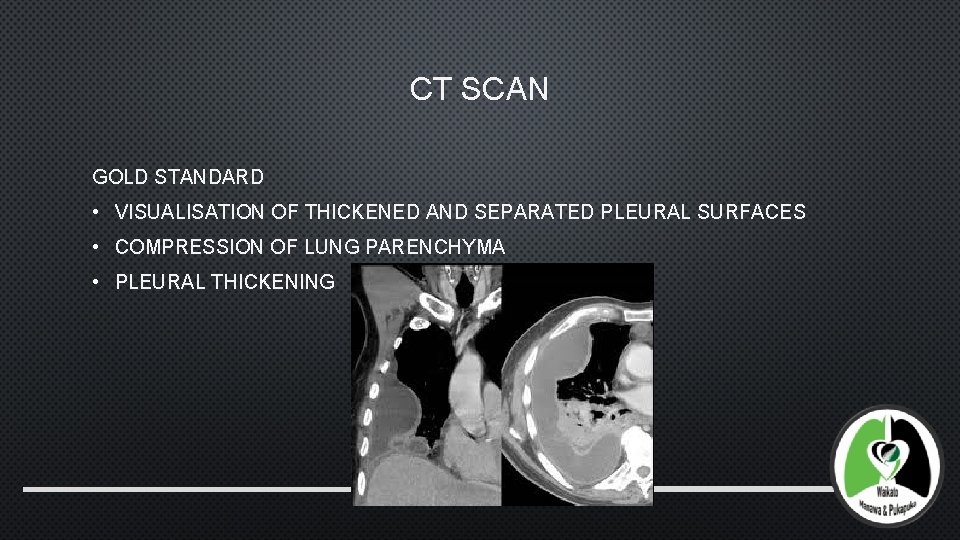
CT SCAN GOLD STANDARD • VISUALISATION OF THICKENED AND SEPARATED PLEURAL SURFACES • COMPRESSION OF LUNG PARENCHYMA • PLEURAL THICKENING
PLEURAL FLUID • CLEAR – UNCOMPLICATED • TURBID – COMPLICATED • PURULENT - ESTABLISHED EMPYEMA INCREASED LEUKOCYTE ACTIVITY AND INCREASED ACID PRODUCTION WITHIN PLEURAL SPACE LEADS TO REDUCED PH AND INCREASED LDH • PH<7. 2, LDH >1000 U/L, GLUCOSE <3. 4 MMOL/L, WCC >50000 CELLS/UL • EFFUSIONS WITH HIGH PH CAN BE MANAGED WITH ANTIBIOTICS AND REPEAT THORACOCENTESIS (SAHN 1989) • IF PH LOW THEN EFFUSION REQUIRES DRAINAGE WITH CHEST TUBE OR SURGERY (VATS)
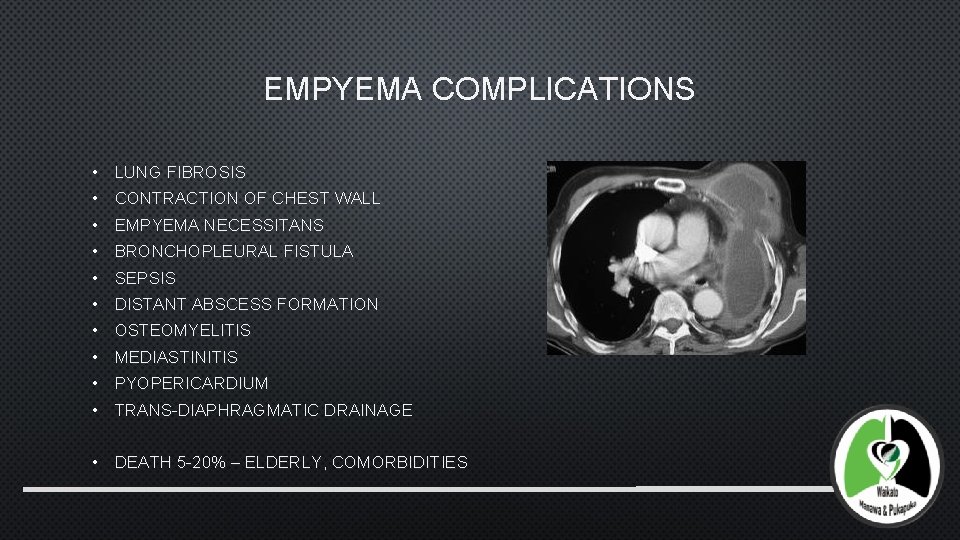
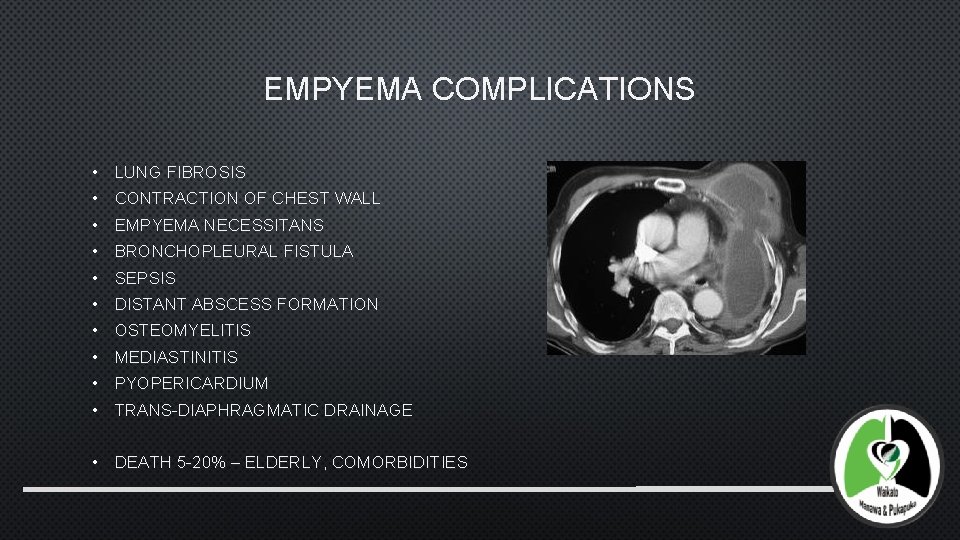
EMPYEMA COMPLICATIONS • LUNG FIBROSIS • CONTRACTION OF CHEST WALL • EMPYEMA NECESSITANS • BRONCHOPLEURAL FISTULA • SEPSIS • DISTANT ABSCESS FORMATION • OSTEOMYELITIS • MEDIASTINITIS • PYOPERICARDIUM • TRANS-DIAPHRAGMATIC DRAINAGE • DEATH 5 -20% – ELDERLY, COMORBIDITIES
MANAGEMENT ACUTE EMPYEMA (STAGE 1 AND 2) • ANTIBIOTICS AND FLUID DRAINAGE • REPEAT THORACOCENTESIS IF TOXICITY IS WELL CONTROLLED • CONTROVERSIAL – ONLY USEFUL IF IMPLEMENTED EARLY ENOUGH • MAY DEVELOP MULTILOCULATED COLLECTIONS THAT ARE DIFFICULT TO DRAIN • VATS DRAINAGE MAY IMPROVE SURVIVAL AND SHORTEN HOSPITAL STAY (FERGUSON 1990) • UNILOCULATION OF SPACE • WASHOUT OF SPACE • BETTER DRAIN PLACEMENT
ACCP GUIDELINES • UNCOMPLICATED EFFUSION: <10 MM ON CXR • • ANTIBIOTICS UNCOMPLICATED EFFUSION: >10 MM, PH>7. 2, GLUC >3. 4 • ANTIBIOTICS • THORACOCENTESIS OR INTERCOSTAL DRAIN INSERTION IF LARGE SYMPTOMATIC EFFUSION COMPLICATED EFFUSION: LARGE/LOCULATED EFFUSION PH<7. 2, GLUC<3. 4 • ANTIBIOTICS • THORACOCENTESIS/DRAINAGE • INTRAPLEURAL FIBRINOLYSIS • EARLY SURGICAL INTERVENTION EMPYEMA: PUS • ANTIBIOTICS • DRAINAGE/FIBRINOLYSIS • SURGICAL DECORTICATION
ANTIBIOTIC THERAPY • GUIDED BY LOCAL ANTIBIOTIC RESISTANCE PATTERNS AND POLICIES • COMMON CAUSATIVE ORGANISMS • CAP/HAP/VAP • SEVERITY OF ILLNESS • CAP • • PENICILLIN, CO-AMOXICLAV, CLINDAMYCIN • CEPHALOSPORINS • METRONIDAZOLE HAP • • CONSIDER MRSA IDEALLY SHOULD BE CONTINUED FOR 2 -4 WEEKS
METHODS OF DRAINAGE TUBE THORACOSTOMY (28 -36 FR) • BEWARE OF THE RETRACTED DIAPHRAGM • CAN REVERT TO OPEN SYSTEM BY CUTTING TUBE PIGTAIL CATHETER • OFTEN BLOCK • LESS USEFUL WHEN FLUID THICK • 70 -90% SUCCESS RATE WHEN USED EARLY
VATS • SHOWN TO HAVE REASONABLE SUCCESS RATE (18/18) IN EARLY EMPYEMA (WAKABAYASHI 1991) BENEFITS • DIRECT VISION • BREAK DOWN ALL LOCULATIONS AND EVACUATE PUS • REMOVE FIBRINOUS MEMBRANES • IRRIGATE PLEURAL CAVITY • LUNG RE-EXPANSION • DIRECT DRAINS APPROPRIATELY • MORTALITY 0 -3% IN LARGER STUDIES WITH SUCCESS RATE 80 -97% IN STAGES 2 -3 (LUH 2005, WURNIG 2006, SOLAINI 2007)

STREPTOKINASE? • FIBRINOLYTIC • USED SINCE 1949 • INITIAL PROBLEMS WITH BLEEDING AND ALLERGY DAVIES 1997 • RCT STREPTOKINASE VS SALINE FLUSHES FOR 3 DAYS • 24 PATIENTS • INCREASED FLUID DRAINAGE, GREATER RADIOGRAPHIC IMPROVEMENT WAIT 1997 • COMPARED VATS AND FIBRINOLYTIC THERAPY • VATS IMPROVED EFFICACY, SHORTER HOSPITAL STAY AND LOWER COST

MIST (MANAGEMENT OF INTRAPLEURAL SEPSIS TRIAL) 2005, 2011 I 454 PATIENTS STREPTOKINASE 250000 U BD FOR 3 DAYS VS PLACEBO – NO BENEFIT • PRIMARY END POINT: DEATH&SURGERY = 31% SK VS 27% PLACEBO P 0. 43 • INCREASED SERIOUS ADVERSE EVENTS 7% VS 3% P 0. 08 • NO INCREASED RISK OF BLEEDING DURING SURGERY II DOUBLE BLIND/ DOUBLE DUMMY 193 PATIENTS DNASE 5 MG, T-PA 10 MG BD FOR 3 DAYS • PRIMARY END POINT REDUCTION IN EFFUSION SIZE – TPA/DNASE BETTER THAN PLACEBO OR WITH TPA OR DNASE ALONE • REFERRAL FOR SURGERY LOWER IN TPA/DNASE GROUP THAN PLACEBO. 4%VS 16% P 0. 03 • REDUCED HOSPITAL STAY IN TPA/DNASE GROUP THAN PLACEBO 11. 8 VS 17 DAYS P 0. 006 • MORTALITY RATES SIMILAR 4%(PLACEBO)/8%(T-PA&DNASE)/8%(T-PA)/13%(DNASE) P 0. 46 • PLEURAL THICKENING INCREASES RISK OF FAILURE OF FIBRINOLYTIC THERAPY
OTHER CARE • TREATMENT OF UNDERLYING RESPIRATORY DISEASE • NUTRITION • CHEST PHYSIO • PROMOTE LUNG RE-EXPANSION • PREVENT CHEST WALL COLLAPSE
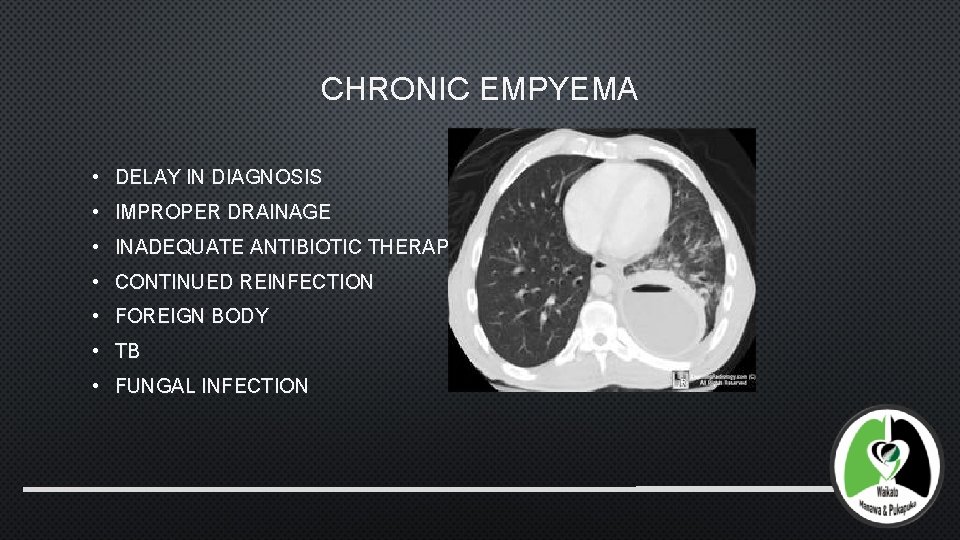
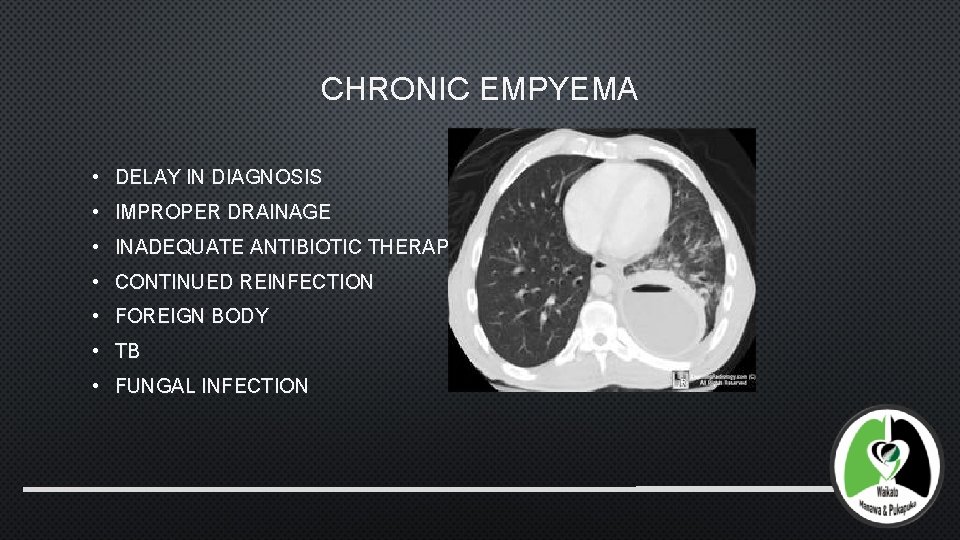
CHRONIC EMPYEMA • DELAY IN DIAGNOSIS • IMPROPER DRAINAGE • INADEQUATE ANTIBIOTIC THERAPY • CONTINUED REINFECTION • FOREIGN BODY • TB • FUNGAL INFECTION
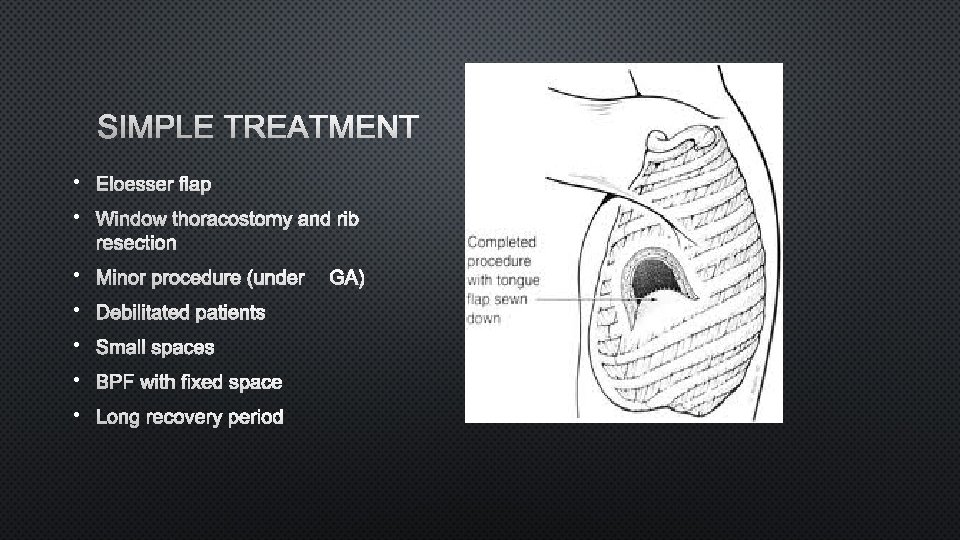
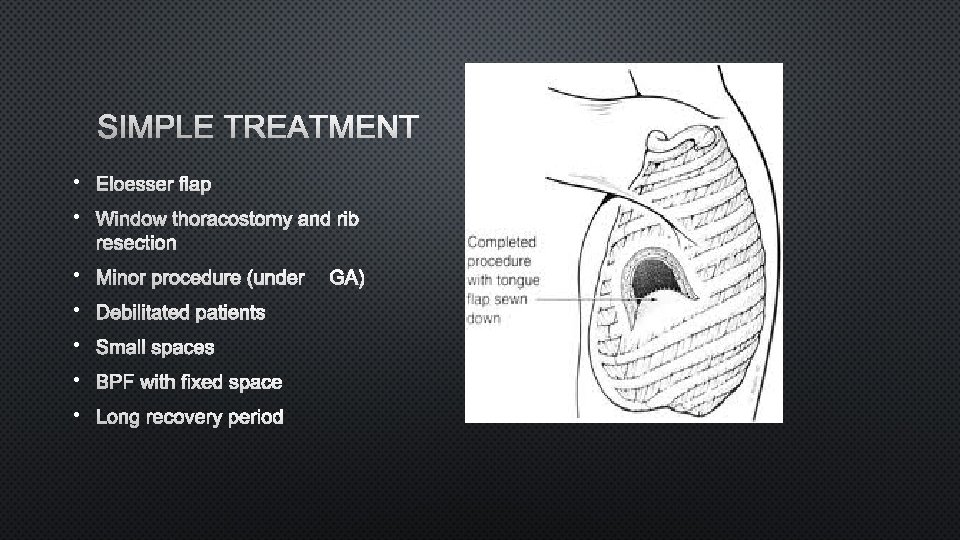
SIMPLE TREATMENT • ELOESSER FLAP • WINDOW THORACOSTOMY AND RIB RESECTION • MINOR PROCEDURE (UNDER GA) • DEBILITATED PATIENTS • SMALL SPACES • BPF WITH FIXED SPACE • LONG RECOVERY PERIOD
SPACE STERILISATION DRAIN SPACE CLAGGETT PROCEDURE • IRRIGATION WITH ANTISEPTICS AND/OR ANTIBIOTIC SOLUTION (MODIFIED) • USEFUL IN POST PNEUMONECTOMY EMPYEMA (IF NO BRONCHOPLEURAL FISTULA) • IRRIGATE WINDOW THORACOSTOMY (CLASSIC)
SPACE FILLING PROCEDURES • IDEALLY FILL SPACE WITH LUNG • DECORTICATION “IS SELDOM REQUIRED BECAUSE MOST PATIENTS WITH PARAPNEUMONIC EFFUSIONS ARE TREATED BEFORE THIS STAGE” • REMOVAL OF CONSTRICTING PEEL OVER LUNG • EMPYEMECTOMY – REMOVAL OF VISCERAL AND PARIETAL PLEURA WITH CONTENTS OF EMPYEMA INTACT – NOT GENERALLY NECESSARY
DECORTICATION • TIMING CONTROVERSIAL • 3 MONTHS – MAXIMAL FUNCTIONAL RESPIRATORY RECOVERY • EARLY – LESS BLOODY, NOT AS ADHERENT TO LUNG • PERFORMED BEFORE FIBROSIS EXTENDS INTO LUNG TISSUE – LESS CHANCE OF LUNG INJURY • MAY NEED TO REMOVE LUNG TISSUE AT SAME TIME
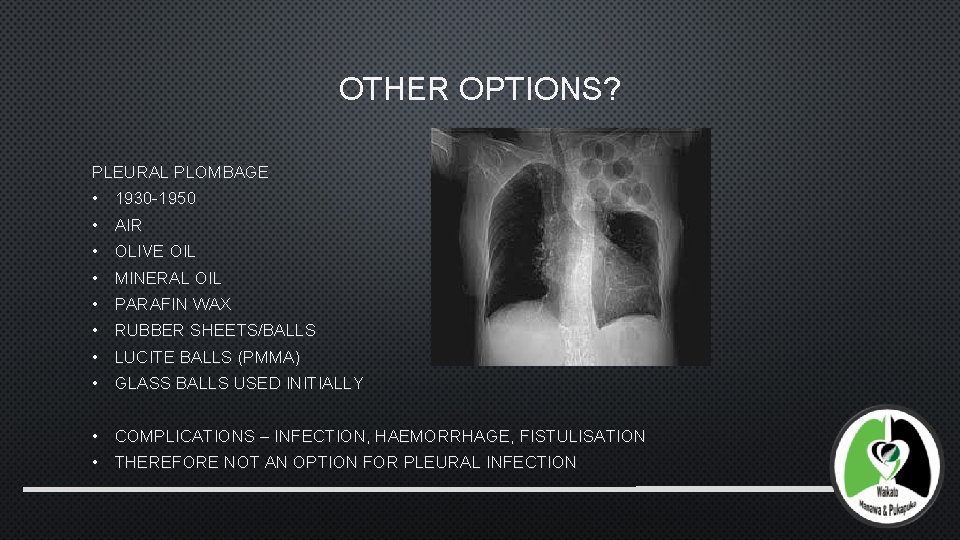
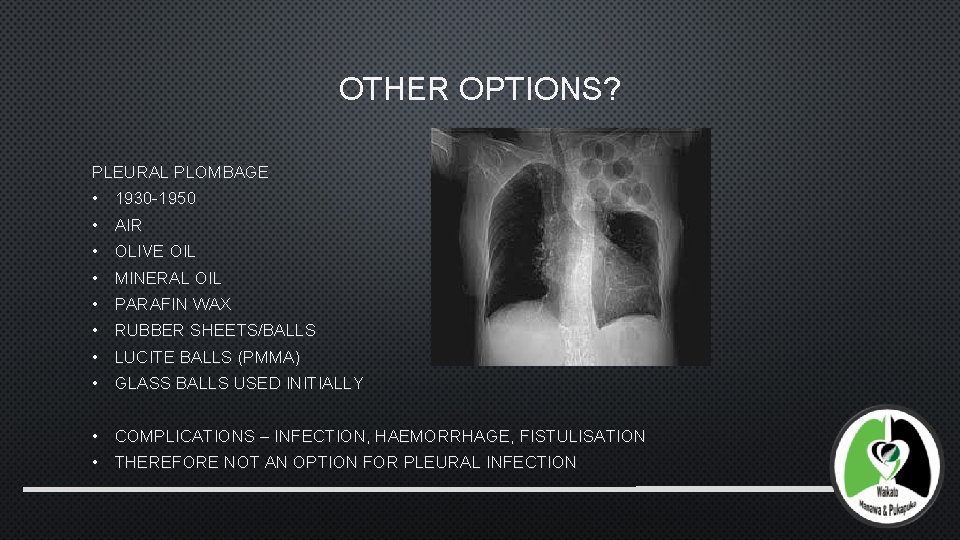
OTHER OPTIONS? PLEURAL PLOMBAGE • 1930 -1950 • AIR • OLIVE OIL • MINERAL OIL • PARAFIN WAX • RUBBER SHEETS/BALLS • LUCITE BALLS (PMMA) • GLASS BALLS USED INITIALLY • COMPLICATIONS – INFECTION, HAEMORRHAGE, FISTULISATION • THEREFORE NOT AN OPTION FOR PLEURAL INFECTION
MUSCLE TRANSPOSITION • OBLITERATING THE SPACE WITH VIABLE TISSUE • REINFORCEMENT OF STUMP (BRONCHOPLEURAL FISTULA) • TYPE OF MUSCLE FLAP TAKEN DEPENDS ON SIZE AND SHAPE AND LOCATION OF CAVITY • LAT DORSI/SERRATUS/PECTORALIS/INTERCOSTAL • OMENTUM • TAKE CARE TO PRESERVE BLOOD SUPPLY, BULK AND INNERVATION
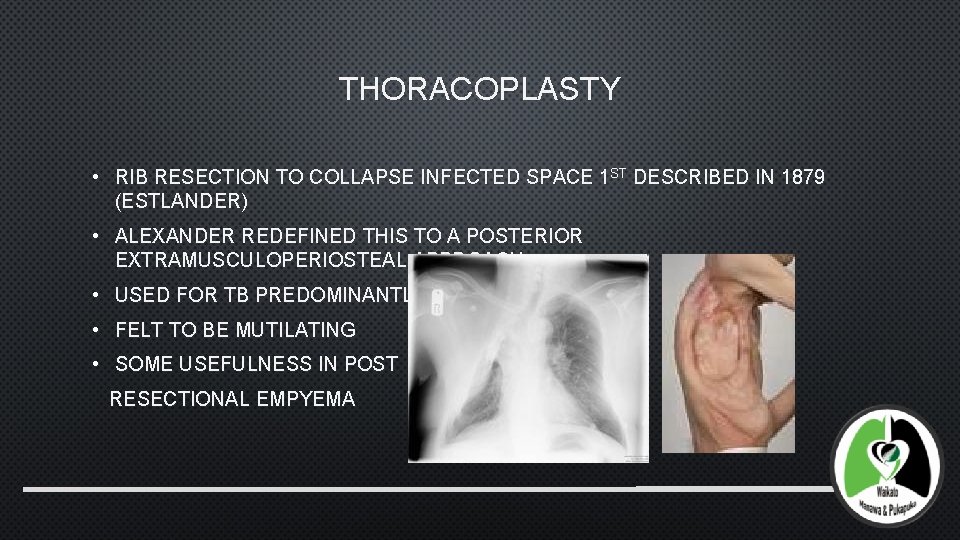
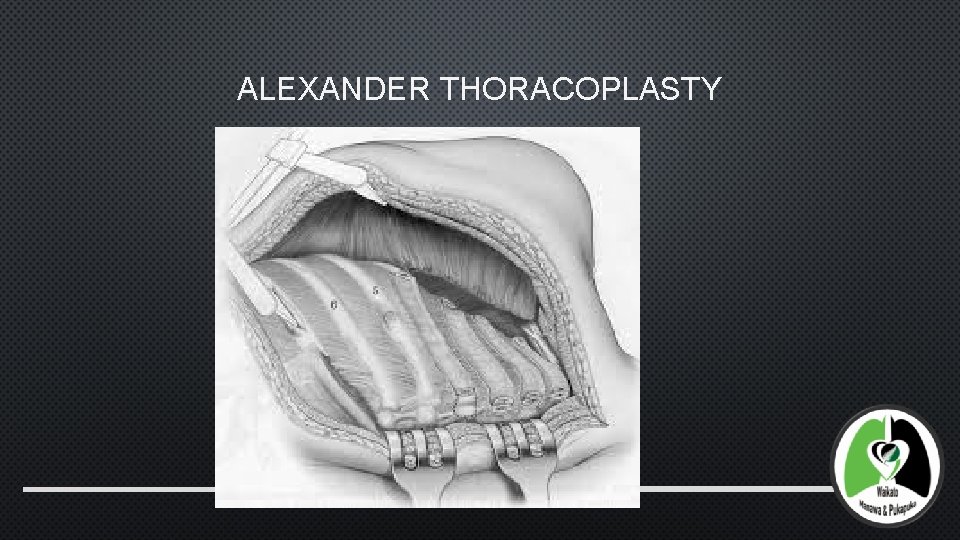
THORACOPLASTY • RIB RESECTION TO COLLAPSE INFECTED SPACE 1 ST DESCRIBED IN 1879 (ESTLANDER) • ALEXANDER REDEFINED THIS TO A POSTERIOR EXTRAMUSCULOPERIOSTEAL APPROACH • USED FOR TB PREDOMINANTLY • FELT TO BE MUTILATING • SOME USEFULNESS IN POST RESECTIONAL EMPYEMA
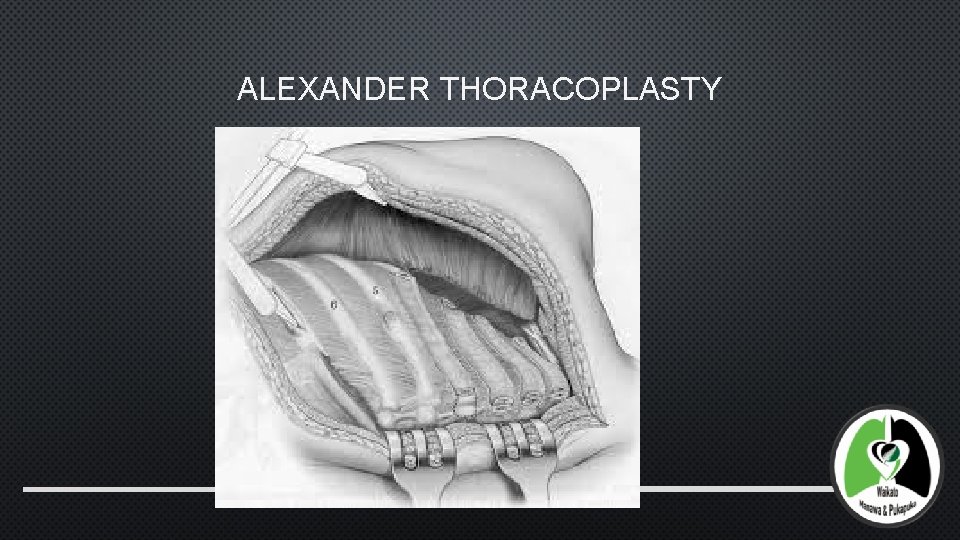
ALEXANDER THORACOPLASTY
SURGICAL CONSIDERATIONS • INFECTION MUST BE TREATED • DRAIN • TUBE/OPEN WINDOW THORACOSTOMY • EXTENT OF THORACOPLASTY • APICAL – EXTRAPLEURAL LYSIS TO ALLOW APEX TO COLLAPSE • DISARTICULATE POSTERIOR RIB ENDS • RESECTION OF SCAPULA TIP IF ENTRAPMENT OCCURS • USED IN CONJUNCTION WITH MUSCLE FLAP/OMENTAL TRANSFER • THORACOPLEUROPLASTY (ANDREWS THORACOPLASTY) • USEFUL FOR POST PNEUMONECTOMY EMPYEMA
POST PNEUMONECTOMY EMPYEMA • UNCOMMON • LIFE THREATENING • TREATMENT DEPENDS ON TIMING AND EXTENT OF BPF • DEGREE OF PLEURAL CONTAMINATION • GENERAL CONDITION OF THE PATIENT • CONTROL INFECTION • (CLOSE FISTULA) • STERILISE CLOSED PLEURAL SPACE
BRONCHOPLEURAL FISTULA 4. 5 -20% FOLLOWING PNEUMONECTOMY 0. 5% FOLLOWING LOBECTOMY ETIOLOGY • ENDOBRONCHIAL TB, CONTAMINATION OF PLEURAL SPACE DURING PROCEDURE • DEVASCULARISATION OF BRONCHUS • RIGHT SIDED RESECTION • PREVIOUS RADIOTHERAPY • LONG BRONCHIAL STUMP • CONCOMITANT ILLNESS – DM, STEROIDS, CIRRHOSIS • INFECTION • RESIDUAL TUMOUR AT BRONCHUS • POST PNEUMONECTOMY VENTILATION
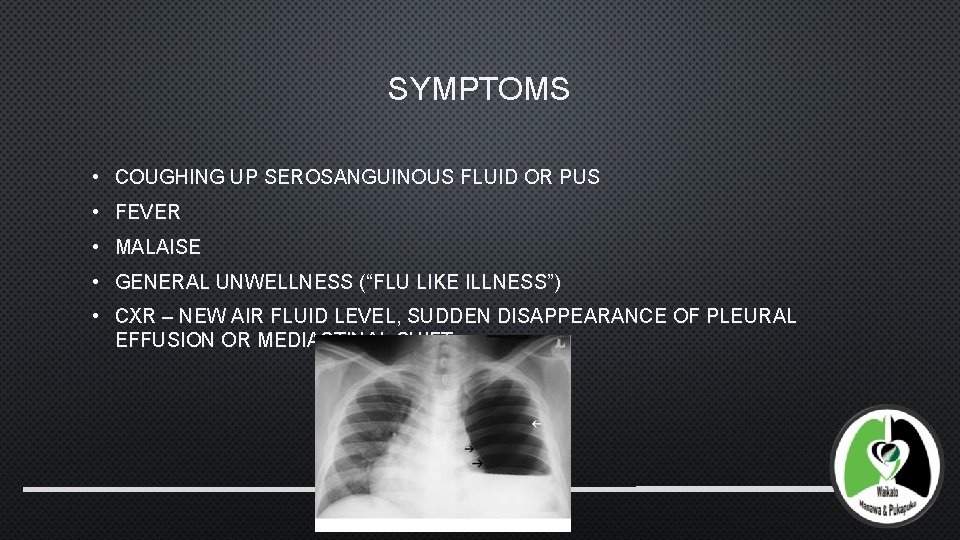
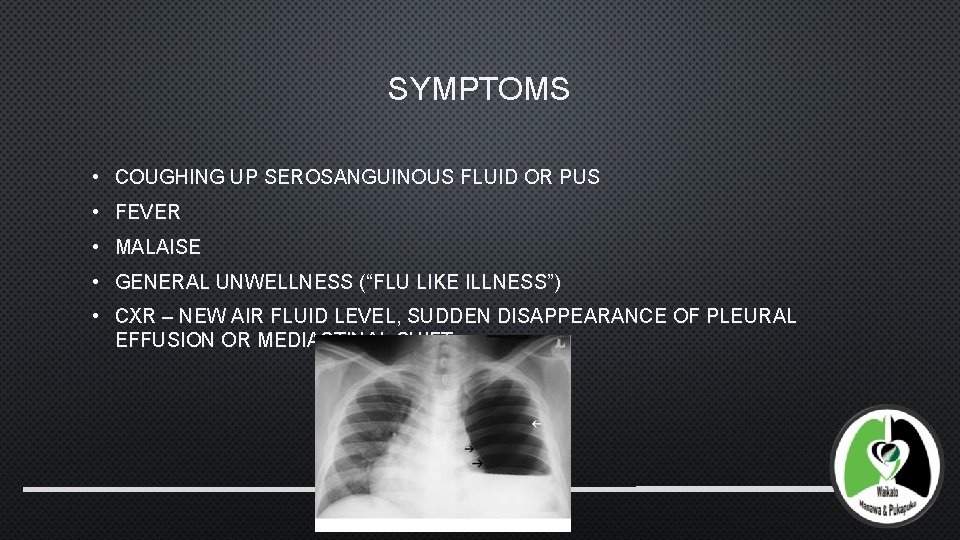
SYMPTOMS • COUGHING UP SEROSANGUINOUS FLUID OR PUS • FEVER • MALAISE • GENERAL UNWELLNESS (“FLU LIKE ILLNESS”) • CXR – NEW AIR FLUID LEVEL, SUDDEN DISAPPEARANCE OF PLEURAL EFFUSION OR MEDIASTINAL SHIFT
EMERGENCY MANAGEMENT OF POST PNEUMONECTOMY BPF • PREVENT SOILING OF REMAINING LUNG • NURSE WITH RESECTED SIDE DOWN, • SELECTIVELY INTUBATE REMAINING LUNG • BRONCHOSCOPY • CLOSURE OF FISTULA/BUTTRESS STUMP • IF INFECTED DRAIN SPACE • OPEN/CLOSED
CONCLUSION • COMPLICATED PNEUMONIA IS COMMON. • MORTALITY CONTINUES TO IMPROVE AS TECHNIQUES FOR DEALING WITH EMPYEMA AND ANTIBIOTIC THERAPY IMPROVES 50% -> 5 -20% • ONGOING BATTLE WITH PHYSICIANS WHO DON’T WANT TO TRAUMATISE PATIENTS WITH LARGE BORE DRAINS AND SO INAPPROPRIATELY RELY ON PIGTAIL DRAINAGE • APPROPRIATE TIMING OF SURGERY IS KEY TO OPTIMAL OUTCOME AND AVOIDANCE OF COMPLICATIONS OR DISFIGURING SURGERY. (ARGUMENTATIVE!) • MAY BE A PLACE FOR FIBRINOLYSIS IN COMORBID/INOPERABLE PATIENTS • THORACOPLASTY RESERVED FOR END OF THE LINE TREATMENT FOR PATIENTS WHO CAN TOLERATE THIS PROCEDURE • BEWARE THE POST PNEUMONECTOMY EMPYEMA – CAN BE SUBTLE.
 Felicity meikle
Felicity meikle Cardiothoracic surgeon salary
Cardiothoracic surgeon salary Vertical
Vertical Pyothorax vs empyema
Pyothorax vs empyema Pleural empyema
Pleural empyema Dr kelechi okoli
Dr kelechi okoli Empyema thoracis
Empyema thoracis Complications of empyema
Complications of empyema Waikato stormwater management guideline
Waikato stormwater management guideline Slidetodoc
Slidetodoc Weka waikato
Weka waikato Waikato dhb ransomware
Waikato dhb ransomware Felicity marmduke
Felicity marmduke Len felicity
Len felicity Felicity goodyear-smith
Felicity goodyear-smith Ohsnet
Ohsnet Direct and indirect speech act
Direct and indirect speech act Felicity conditions
Felicity conditions Recesul costodiafragmatic
Recesul costodiafragmatic Visceral and parietal pleura
Visceral and parietal pleura Costo mediastinal recess
Costo mediastinal recess Pleura
Pleura Mediastinal surface
Mediastinal surface Pleura
Pleura Pleura lungs
Pleura lungs Ligamento de morosow
Ligamento de morosow Crural area
Crural area Lobos dos pulmões
Lobos dos pulmões Double layered pleura
Double layered pleura Pericardium pleura and peritoneum
Pericardium pleura and peritoneum Pleura
Pleura Dome of pleura
Dome of pleura True vocal cord
True vocal cord Pleura megvastagodás
Pleura megvastagodás Surface marking of pleura
Surface marking of pleura Respiratory mucosa
Respiratory mucosa Pleura
Pleura Respirazione toracica
Respirazione toracica Foto rontgen efusi pleura
Foto rontgen efusi pleura Purulent diseases of lungs and pleura
Purulent diseases of lungs and pleura Analisis cairan pleura
Analisis cairan pleura