EMPYEMA Empyema An accumulation of thick purulent fluid





- Slides: 23
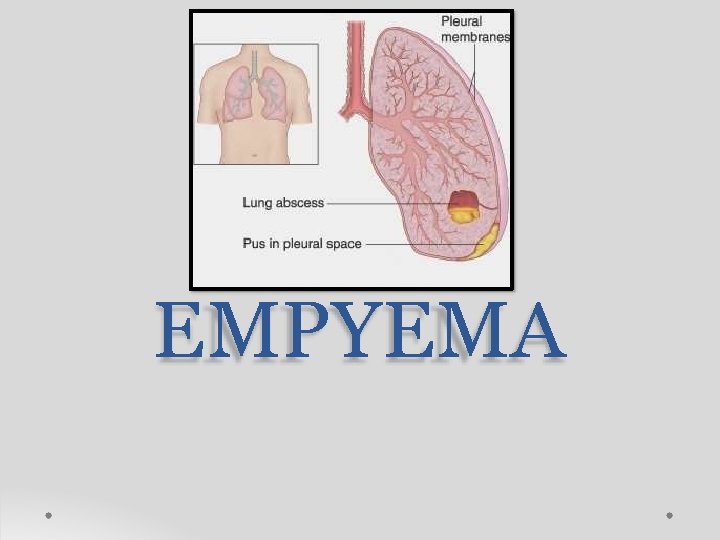
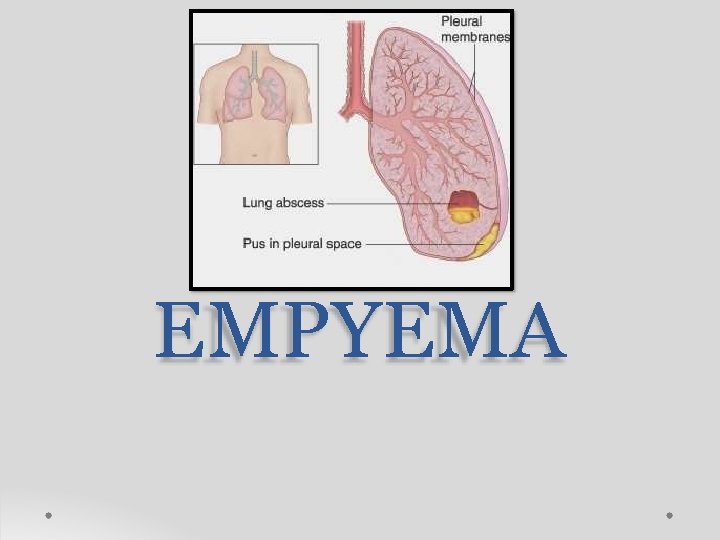
EMPYEMA

Empyema An accumulation of thick, purulent fluid within the pleural space, often with fibrin development
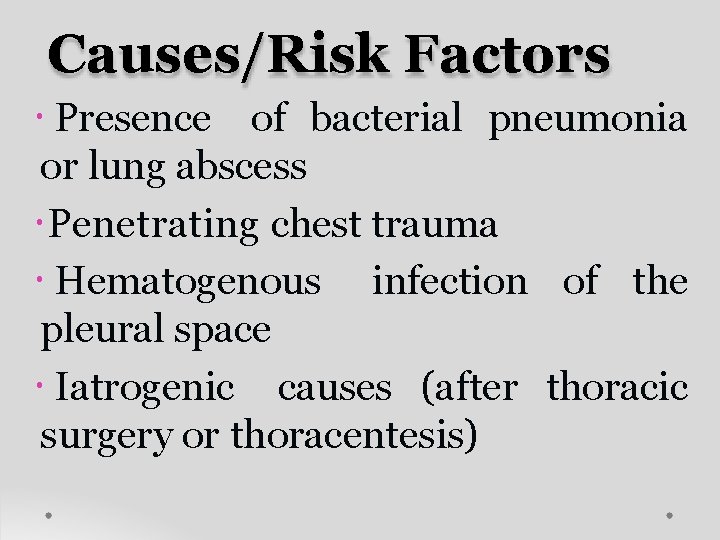
Causes/Risk Factors Presence of bacterial pneumonia or lung abscess Penetrating chest trauma Hematogenous infection of the pleural space Iatrogenic causes (after thoracic surgery or thoracentesis)
ORGANISMS • Staphylococcus aureus, Streptococcus pneumoniae and Streptococcus pyogenes
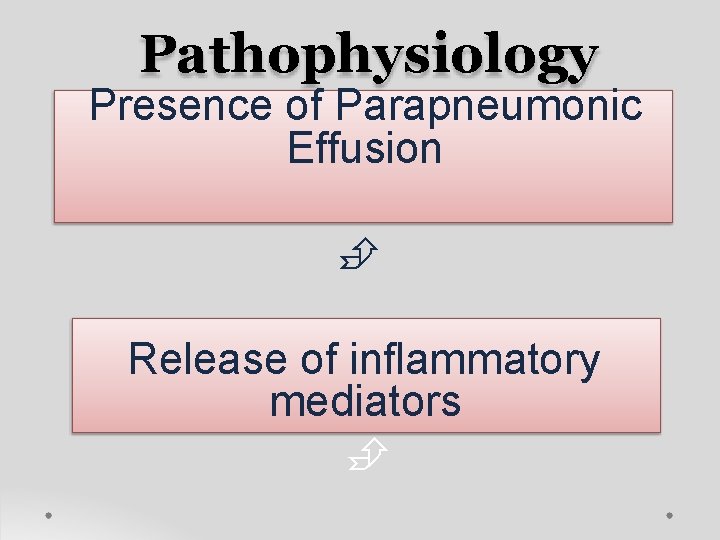
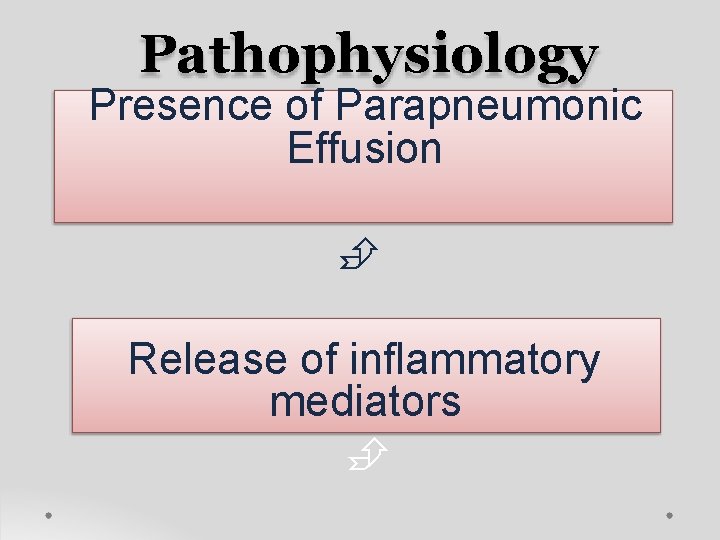
Pathophysiology Presence of Parapneumonic Effusion Release of inflammatory mediators
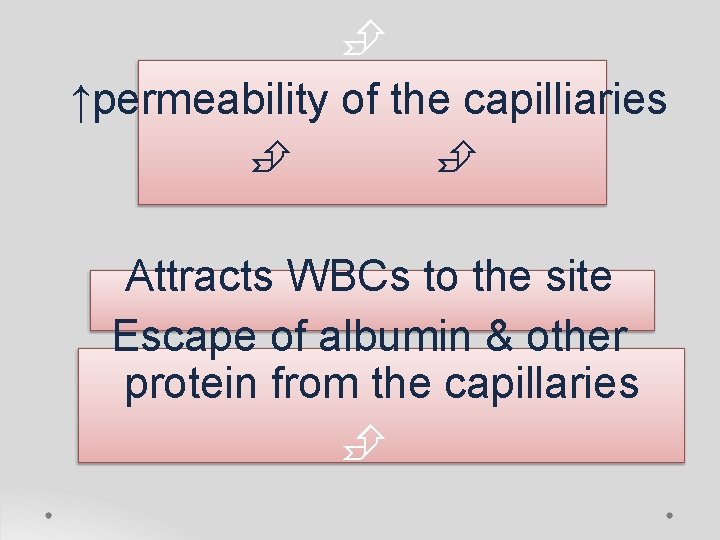
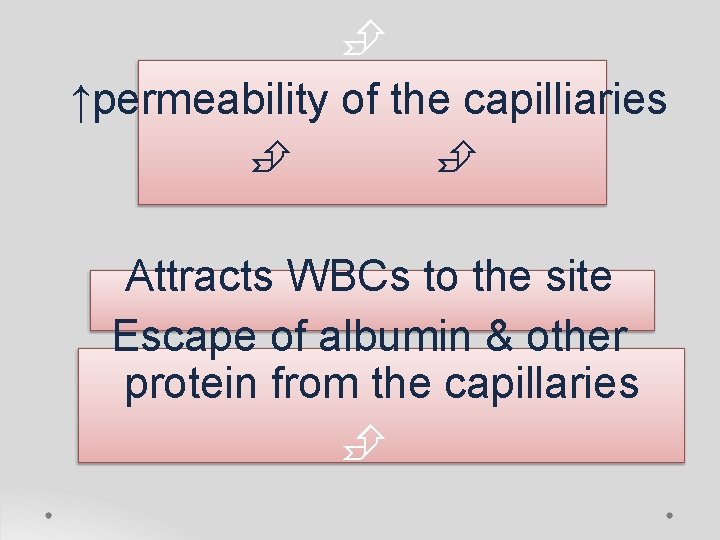
↑permeability of the capilliaries Attracts WBCs to the site Escape of albumin & other protein from the capillaries
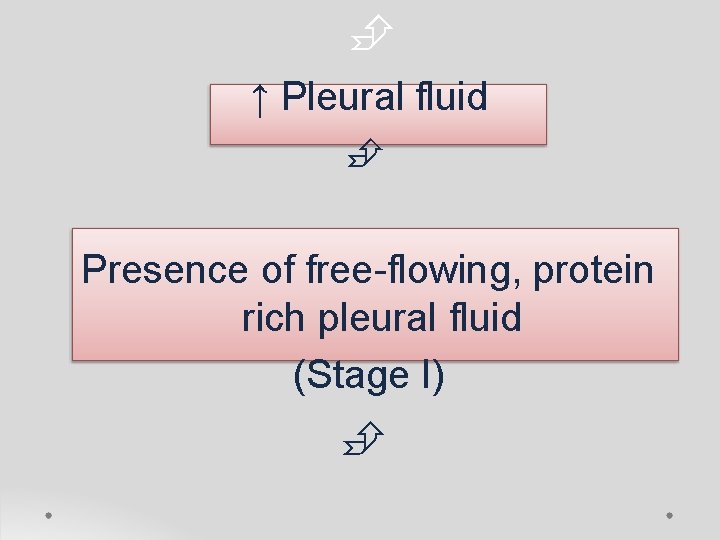
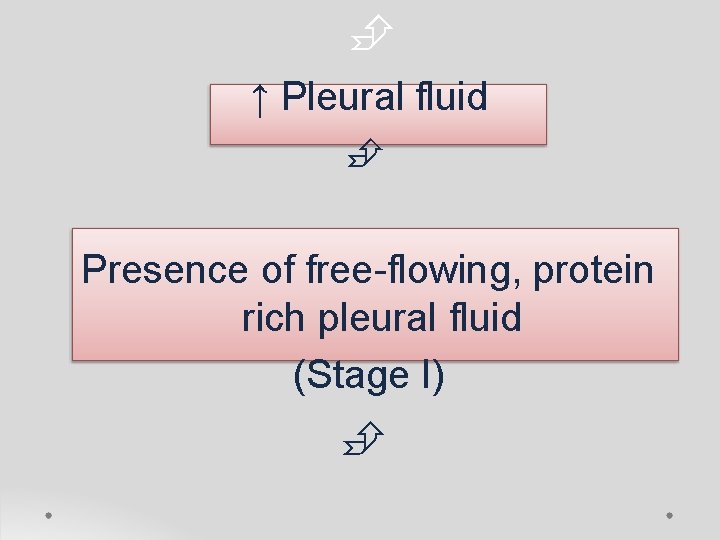
↑ Pleural fluid Presence of free-flowing, protein rich pleural fluid (Stage I)
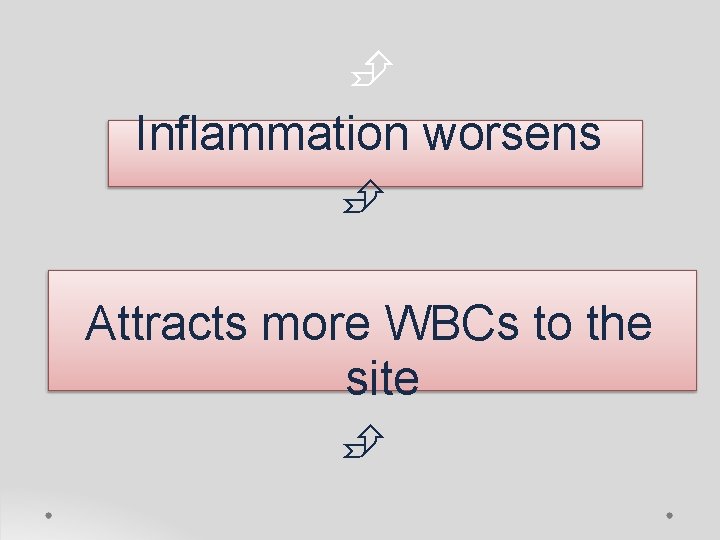
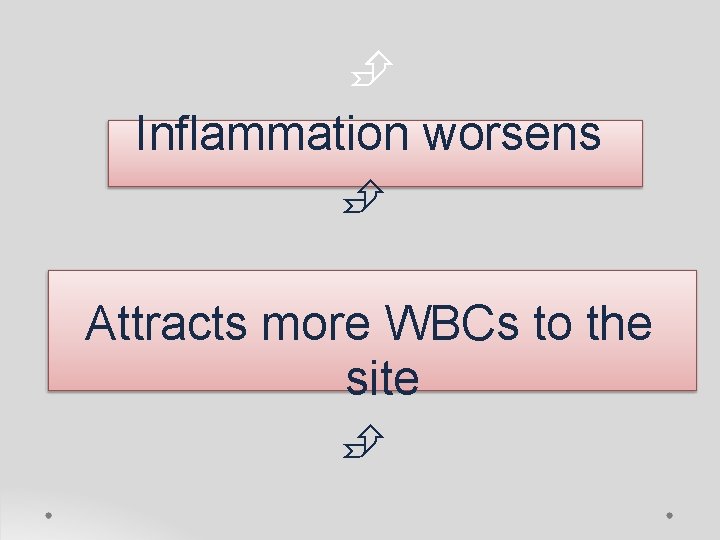
Inflammation worsens Attracts more WBCs to the site
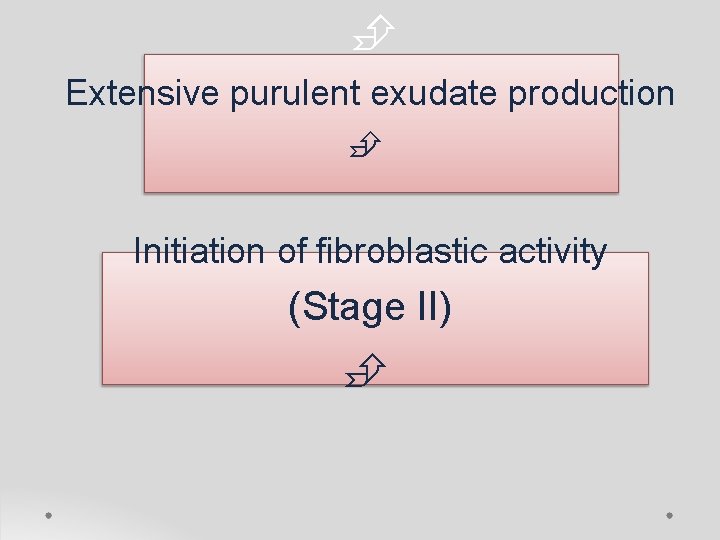
Extensive purulent exudate production Initiation of fibroblastic activity (Stage II)
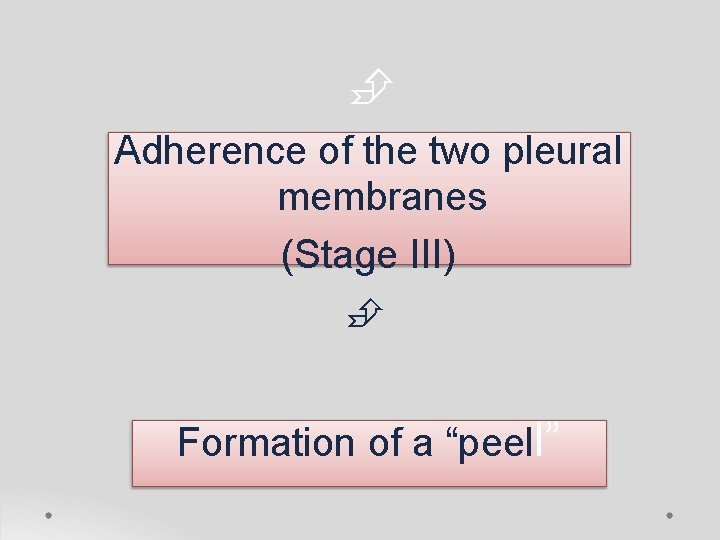
Adherence of the two pleural membranes (Stage III) Formation of a “peell”
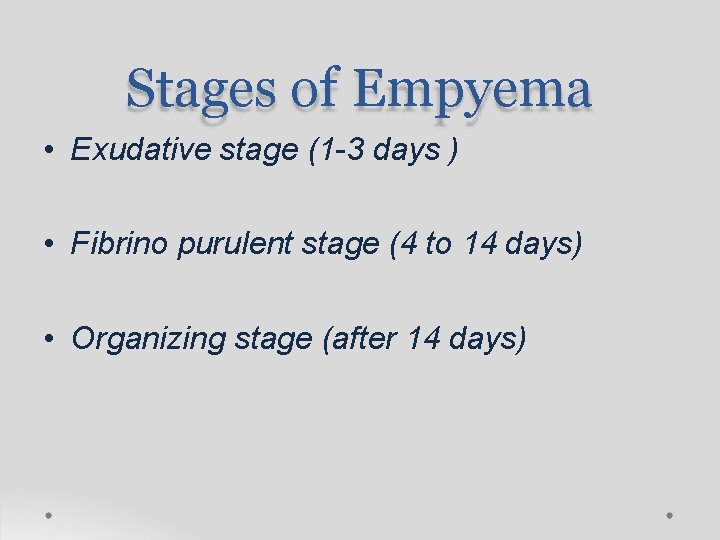
Stages of Empyema • Exudative stage (1 -3 days ) • Fibrino purulent stage (4 to 14 days) • Organizing stage (after 14 days)
Exudative stage (1 -3 days) • Immediate response with outpouring of the fluid. • Low cellular content • It is simple parapneumonic effusion with normal p. H and glucose levels.
Fibrino purulent stage (4 to 14 days) • Large number of poly-morphonuclear leukocytes and fibrin accumulates • Acumulation of neutro-phils and fibrin, effusion becomes purulent and viscous leading to development of empyema.
Organizing stage (after 14 days) • Fibro-blasts grow into exudates on both the visceral and parietal pleural surfaces • Development of an inelastic membrane "the peel". • Most common in S. aureus infection. • Thickened pleural peel can restrict lung movement and it is commonly termed as trapped lung

DIAGNOSIS LAB INVESTIGATIONS • • • CBC count Blood culture Serum LDH Total protein Bacterial, mycobacterial, and fungal cultures
X-RAY • Large pleural effusion can be diagnosed in posteroanterior view • Lateral decubitus view with affected side inferior facilitates recognition of smaller volumes of fluid.

o. Sonography or CT imaging o Chest CT imaging to detect : - pleural fluid and image the airways - guide interventional procedures

CLINICAL MANIFESTATIONS o Like bacterial pneumonia o Acute febrile response, pleuritic chest pain, cough, dyspnea, and possibly cyanosis o Abdominal pain, vomiting o Splinting of the affected side 19
TREATMENT • • • 20 Control of the infection Drainage of the pleural fluid Appropriate antibiotic : 10 -14 days / IV Oxygen Oral antibiotics for 1 -3 weeks after discharge if complicated infections (+)
ANTIBIOTICS • Cefuroxime = 150 mg/kg/day (: 3 dose) • Clyndamycin = 25 – 40 mg/kg/day (: 3 dose) Good most patients recover without sequelae Early recognition initiation of definitive therapy reduce morbidity and complications 21
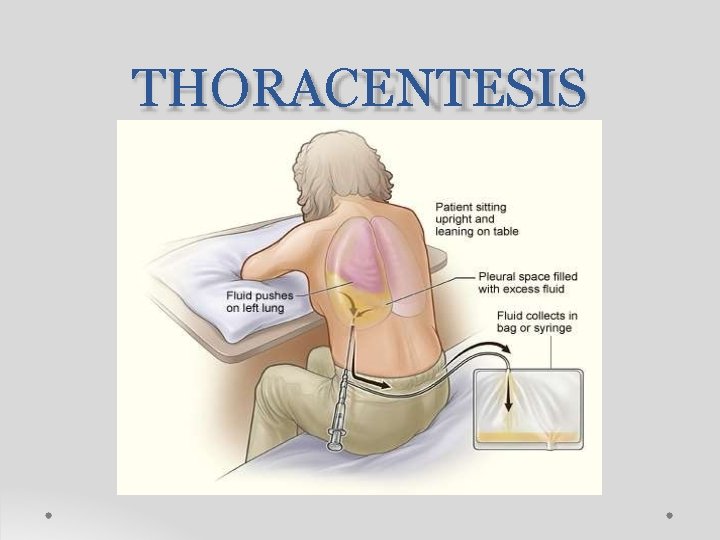
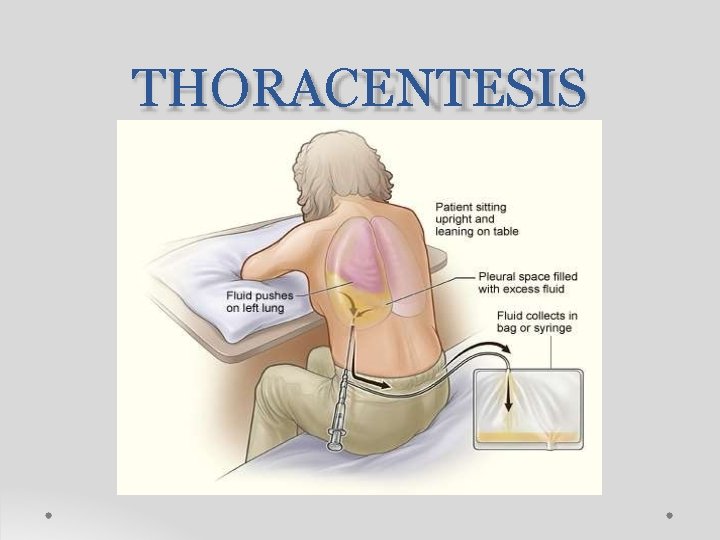
THORACENTESIS

Nursing Diagnosis Impaired Gas Exchange r/t compressed lung Acute Pain r/t infection of the pleura Risk for Activity Intolerance r/t hypoxia secondary to empyema
 Serous fluid
Serous fluid Water balance regulation
Water balance regulation Chapter 26 fluid electrolyte and acid-base balance
Chapter 26 fluid electrolyte and acid-base balance Purulent diseases of lungs and pleura
Purulent diseases of lungs and pleura Morphological pattern of acute inflammation
Morphological pattern of acute inflammation Retrolental flare definition
Retrolental flare definition Seratonin
Seratonin Bindeledd mellom medulla spinalis og cerebrum?
Bindeledd mellom medulla spinalis og cerebrum? Sputum color chart
Sputum color chart Toux moniliforme definition
Toux moniliforme definition Light's criteria
Light's criteria Pleural empyema
Pleural empyema Dr kelechi okoli
Dr kelechi okoli Empyema thoracis
Empyema thoracis Pyothorax vs empyema
Pyothorax vs empyema Chapter 20 lesson 1
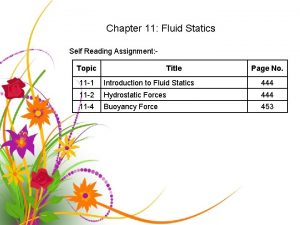
Chapter 20 lesson 1 Fluid statics deals with fluid at rest
Fluid statics deals with fluid at rest Define fluid kinematics
Define fluid kinematics Body fluid compartments
Body fluid compartments Movement of body fluids
Movement of body fluids Synovial membrane
Synovial membrane Interstitial fluid vs extracellular fluid
Interstitial fluid vs extracellular fluid Fluid thrill definition
Fluid thrill definition P1-p2
P1-p2