Pulmonary Medicine Lectures CAP Community Acquired Pneumonia HAP

- Slides: 51
Pulmonary Medicine Lectures CAP – Community Acquired Pneumonia HAP – Hospital Acquired Pneumonia VAP – Ventilator Associated Pneumonia MS V František Sándor, MD, Ph. D, FCCP March, 2020
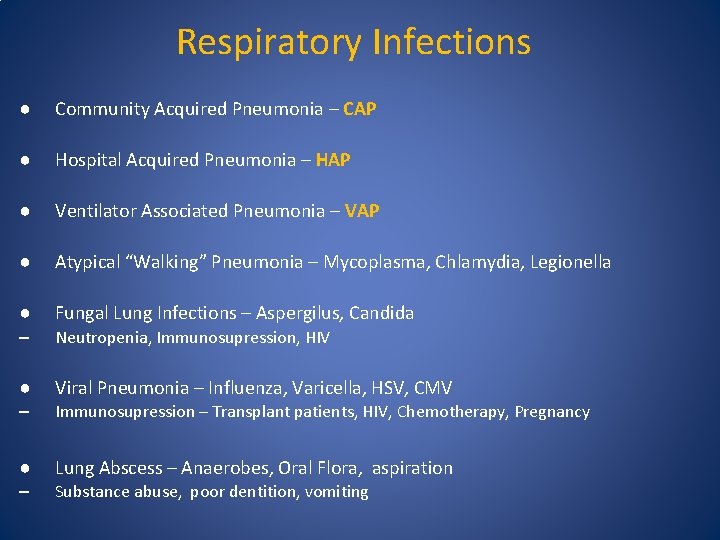
Respiratory Infections ● Community Acquired Pneumonia – CAP ● Hospital Acquired Pneumonia – HAP ● Ventilator Associated Pneumonia – VAP ● Atypical “Walking” Pneumonia – Mycoplasma, Chlamydia, Legionella ● Fungal Lung Infections – Aspergilus, Candida – Neutropenia, Immunosupression, HIV ● Viral Pneumonia – Influenza, Varicella, HSV, CMV – Immunosupression – Transplant patients, HIV, Chemotherapy, Pregnancy ● Lung Abscess – Anaerobes, Oral Flora, aspiration – Substance abuse, poor dentition, vomiting
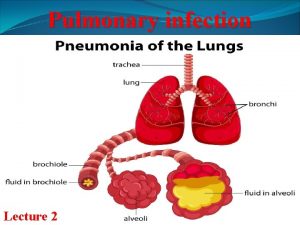
Infectious Pneumonia ● is an infection with a pathogen causing inflammatory condition of the lung parenchyma – affecting primarily respiratory bronchioles, alveoli and lung interstitium. ● is usually caused by infection with bacteria, less commonly other microorganisms (viruses, fungi, parasites)
CAP - Community Acquired Pneumonia Epidemiology • 450 million people worldwide • 7% of the population • 4 million fatalities – third world countries –Very young, very old, malnourished, chronically ill • US – 5. 6 million people – 1. 7 million hospitalizations annually –> 60, 000 deaths annually – 7 th leading cause of death – 5 days - mean hospital stay length – 46% of deaths of all infectious diseases
CAP – Community Acquired Pneumonia • 90% of all pneumonias • Acquired infectiously from normal social contact in the community • Airborne, droplet, close or direct contact • Colonization of oropharyngeal location with facultative pathogen –S. pneumoniae, H. influenzae, –Aspiration –Diminished local and systemic immune surveillance
CAP – Most Common Organisms • Streptococcus pneumoniae (30%) – rusty colored sputum • Hemophilus influenzae (10%) • Mycoplasma pneumoniae (10%) - neck LAP, joint pain, bullous myringitis – middle ear –Atypical “Walking Pneumonia“ • Chlamydia pneumoniae (8%) • Influenza virus (7%) • Legionella species (3%) – confusion, diarrhea, liver damage, abdominal pain • Gram negative Enterobacteriaceae (3%) – Klebsiella – “currant jelly” bloody sputum • Chlamydia psittaci (1%) • Moraxella catarrhalis (0. 5%) • Other pathogens (8 -10%) • In up to 40 -50% cases, no pathogen is identified!!
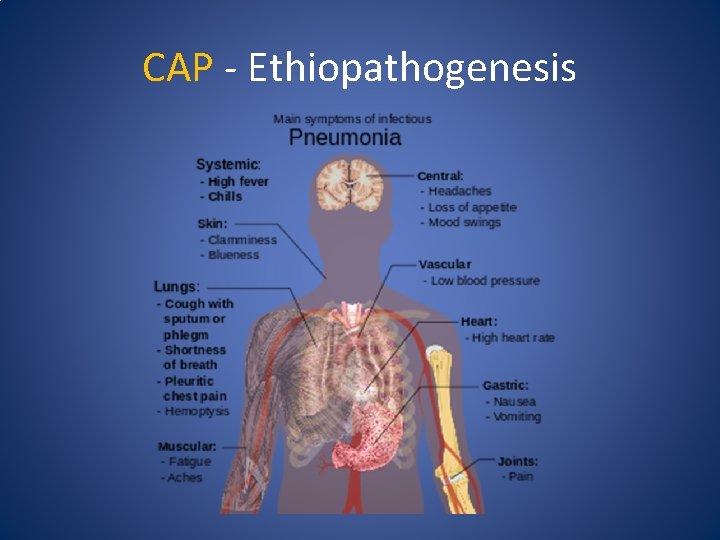
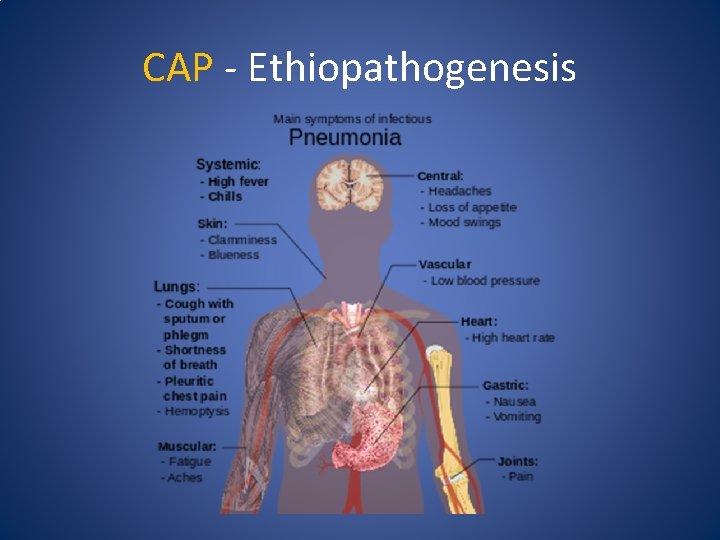
CAP - Ethiopathogenesis
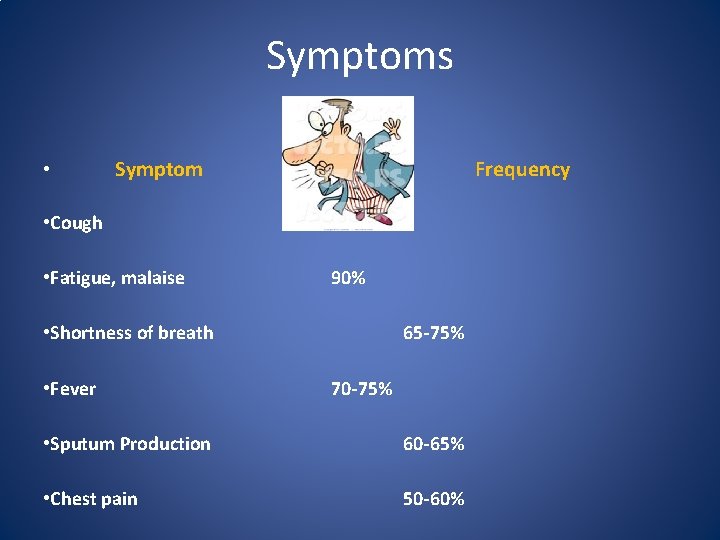
Symptoms • Symptom Frequency • Cough 80 -90% • Fatigue, malaise 90% • Shortness of breath • Fever 65 -75% 70 -75% • Sputum Production 60 -65% • Chest pain 50 -60%
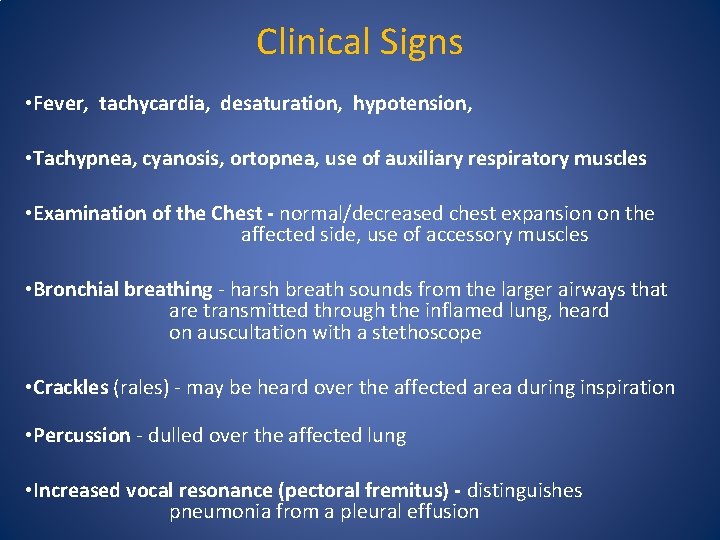
Clinical Signs • Fever, tachycardia, desaturation, hypotension, • Tachypnea, cyanosis, ortopnea, use of auxiliary respiratory muscles • Examination of the Chest - normal/decreased chest expansion on the affected side, use of accessory muscles • Bronchial breathing - harsh breath sounds from the larger airways that are transmitted through the inflamed lung, heard on auscultation with a stethoscope • Crackles (rales) - may be heard over the affected area during inspiration • Percussion - dulled over the affected lung • Increased vocal resonance (pectoral fremitus) - distinguishes pneumonia from a pleural effusion
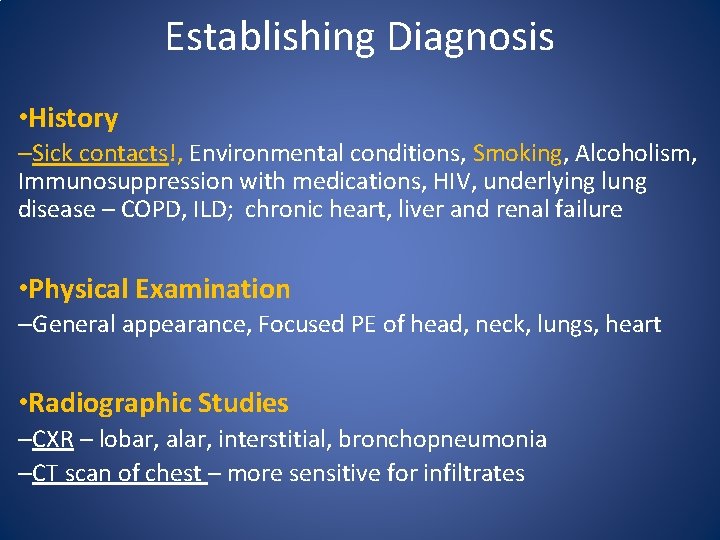
Establishing Diagnosis • History –Sick contacts!, Environmental conditions, Smoking, Alcoholism, Immunosuppression with medications, HIV, underlying lung disease – COPD, ILD; chronic heart, liver and renal failure • Physical Examination –General appearance, Focused PE of head, neck, lungs, heart • Radiographic Studies –CXR – lobar, alar, interstitial, bronchopneumonia –CT scan of chest – more sensitive for infiltrates
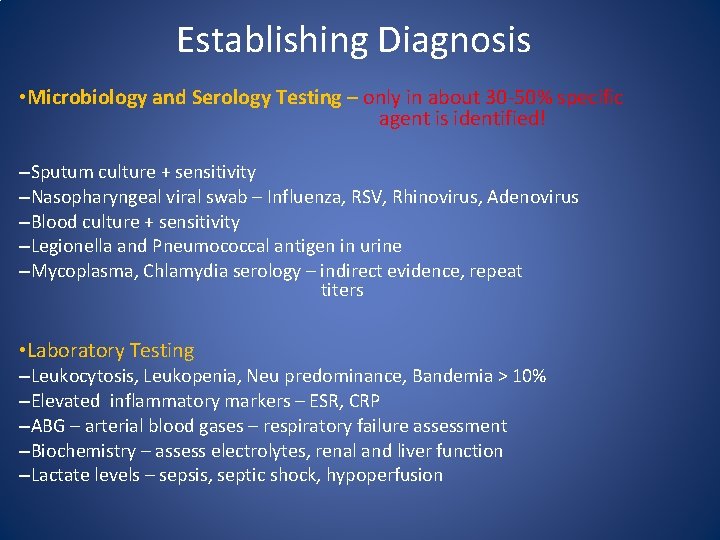
Establishing Diagnosis • Microbiology and Serology Testing – only in about 30 -50% specific agent is identified! –Sputum culture + sensitivity –Nasopharyngeal viral swab – Influenza, RSV, Rhinovirus, Adenovirus –Blood culture + sensitivity –Legionella and Pneumococcal antigen in urine –Mycoplasma, Chlamydia serology – indirect evidence, repeat titers • Laboratory Testing –Leukocytosis, Leukopenia, Neu predominance, Bandemia > 10% –Elevated inflammatory markers – ESR, CRP –ABG – arterial blood gases – respiratory failure assessment –Biochemistry – assess electrolytes, renal and liver function –Lactate levels – sepsis, septic shock, hypoperfusion
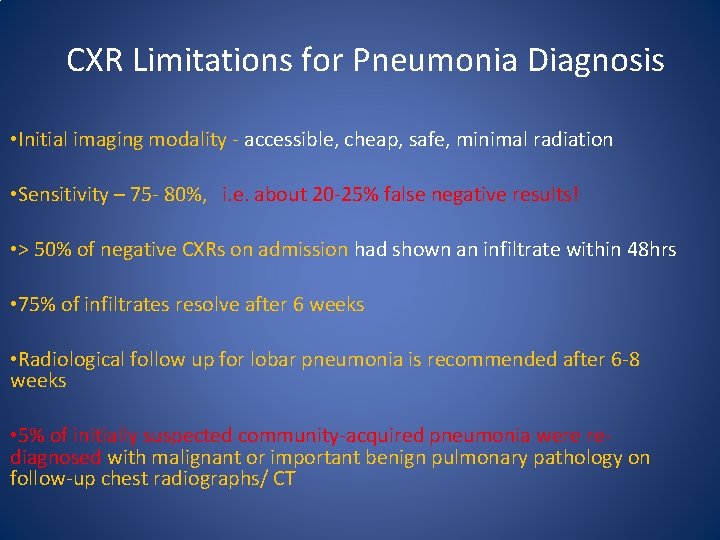
CXR Limitations for Pneumonia Diagnosis • Initial imaging modality - accessible, cheap, safe, minimal radiation • Sensitivity – 75 - 80%, i. e. about 20 -25% false negative results! • > 50% of negative CXRs on admission had shown an infiltrate within 48 hrs • 75% of infiltrates resolve after 6 weeks • Radiological follow up for lobar pneumonia is recommended after 6 -8 weeks • 5% of initially suspected community-acquired pneumonia were rediagnosed with malignant or important benign pulmonary pathology on follow-up chest radiographs/ CT
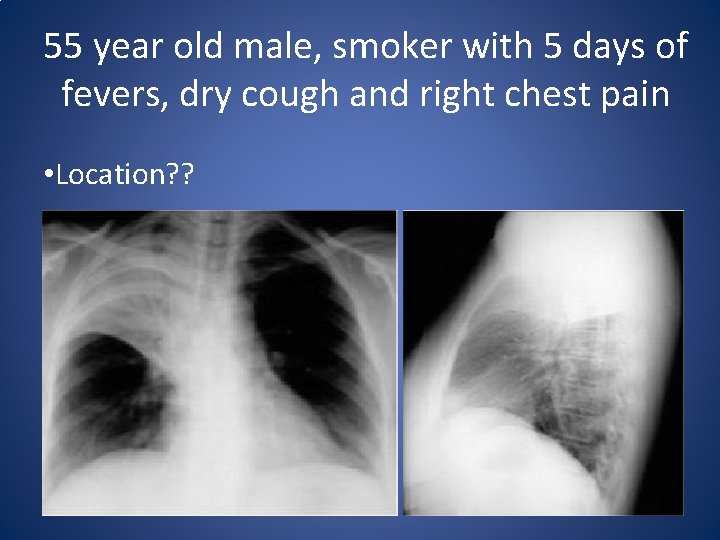
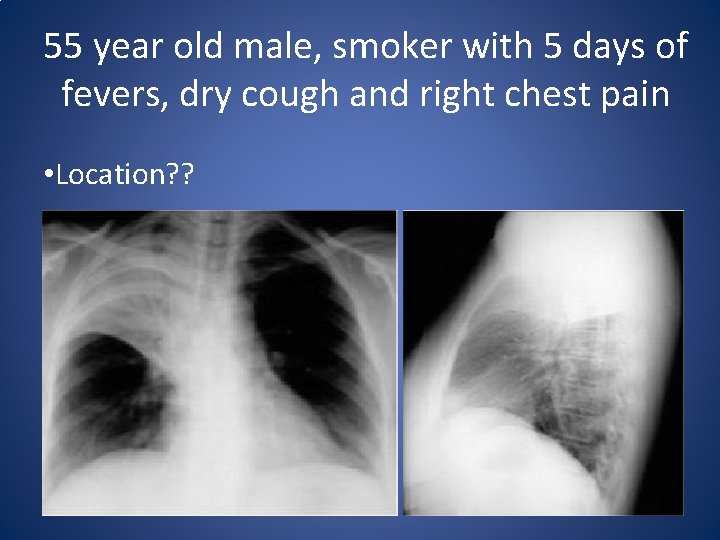
55 year old male, smoker with 5 days of fevers, dry cough and right chest pain • Location? ?
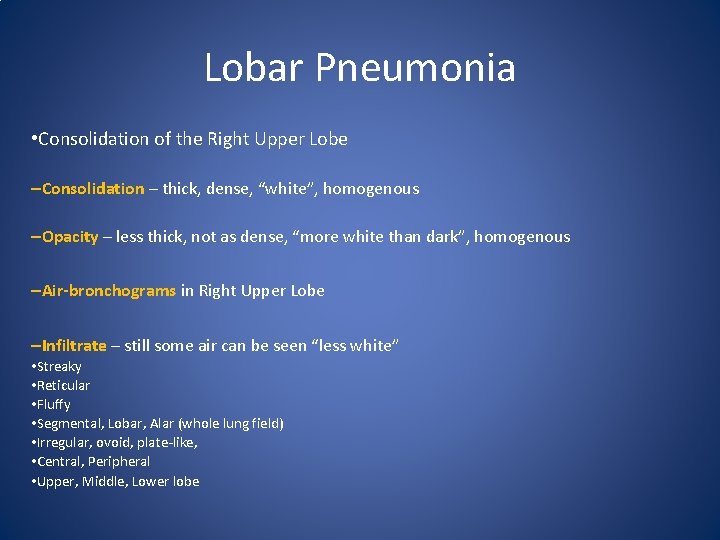
Lobar Pneumonia • Consolidation of the Right Upper Lobe –Consolidation – thick, dense, “white”, homogenous –Opacity – less thick, not as dense, “more white than dark”, homogenous –Air-bronchograms in Right Upper Lobe –Infiltrate – still some air can be seen “less white” • Streaky • Reticular • Fluffy • Segmental, Lobar, Alar (whole lung field) • Irregular, ovoid, plate-like, • Central, Peripheral • Upper, Middle, Lower lobe
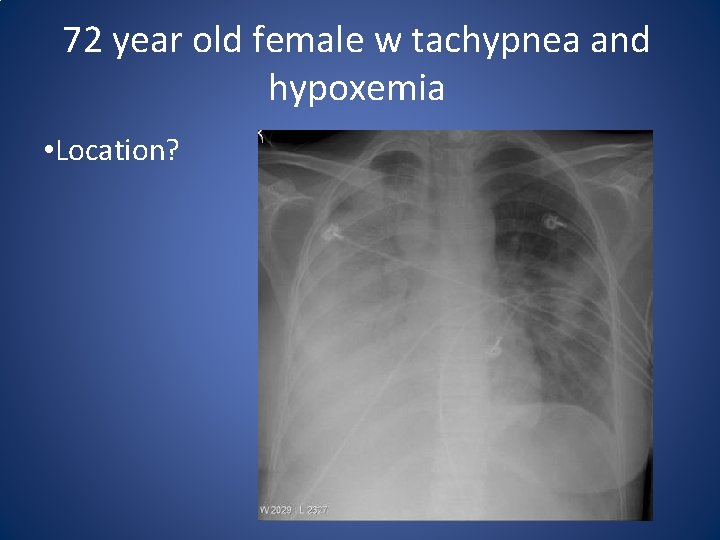
72 year old female w tachypnea and hypoxemia • Location?
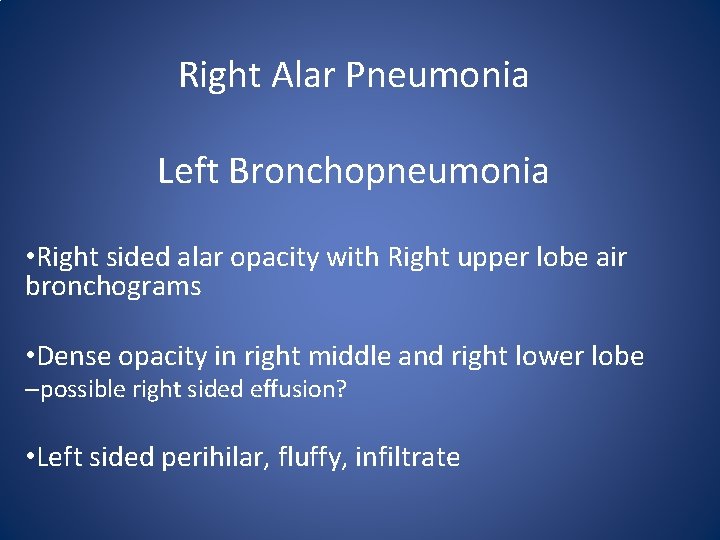
Right Alar Pneumonia Left Bronchopneumonia • Right sided alar opacity with Right upper lobe air bronchograms • Dense opacity in right middle and right lower lobe –possible right sided effusion? • Left sided perihilar, fluffy, infiltrate
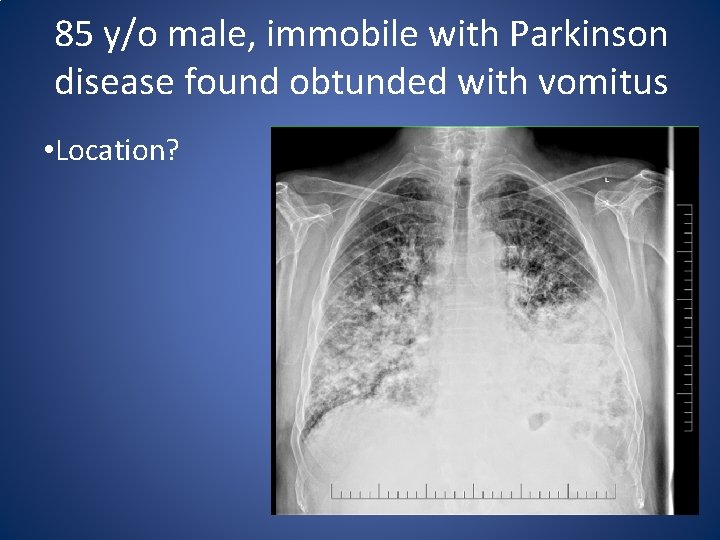
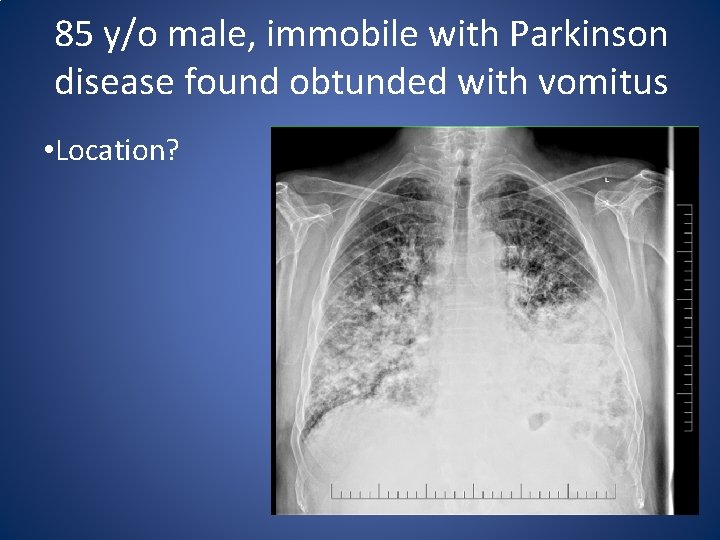
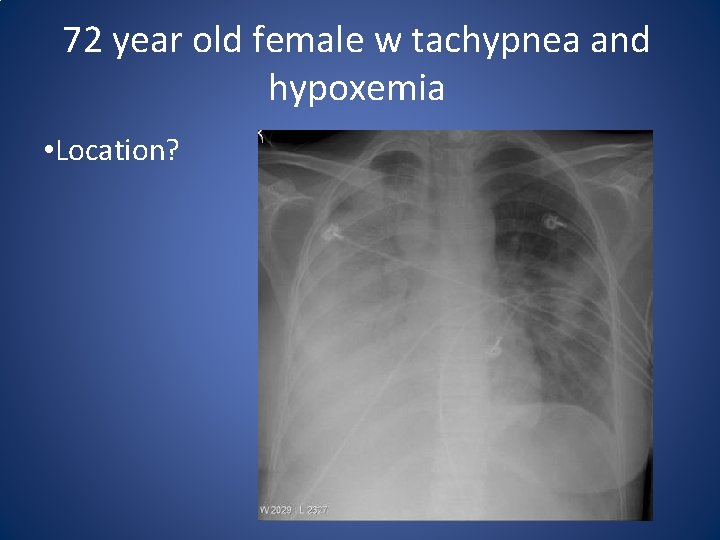
85 y/o male, immobile with Parkinson disease found obtunded with vomitus • Location?
Bilateral Bronchopneumonia • Consider aspiration episode • Extensive bilateral patchy confluent infiltrates • Obscured left hemi-diaphragm suggests aspiration into left lower lobe

35 year old male with positive sick contact having dry cough for 2 weeks • Location?
Segmental Pneumonia • Right middle lobe infiltrate –Obscured right heart border –Right hemi-diaphragm is visible –Right lower lobe is not affected
Chest CT • More sensitive for pneumonia (parenchymal) infiltrates than CXR • Detects infiltrates, ground glass, reticular patterns • Tumors –nodules, mediastinal pathology • Effusions, atelectasis • Underlying structural lung disease (emphysema) • More expensive • Increases radiation burden
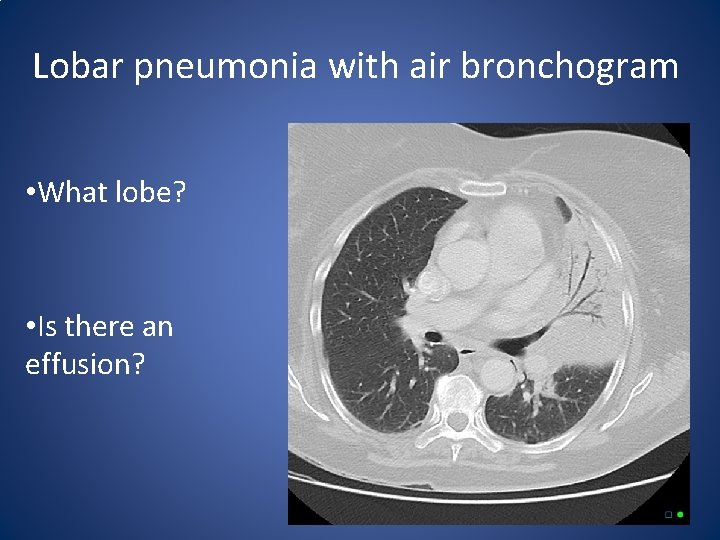
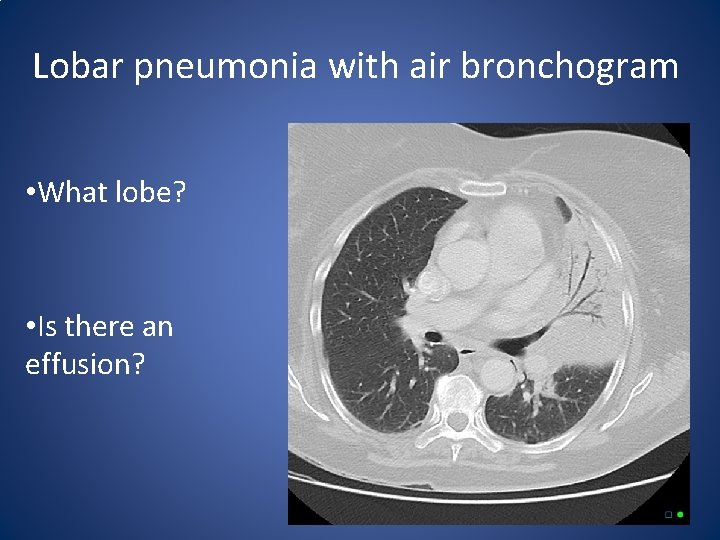
Lobar pneumonia with air bronchogram • What lobe? • Is there an effusion?
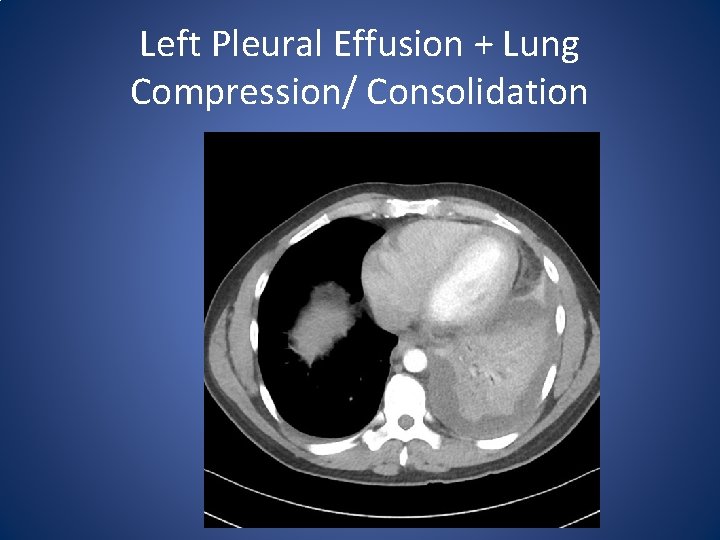
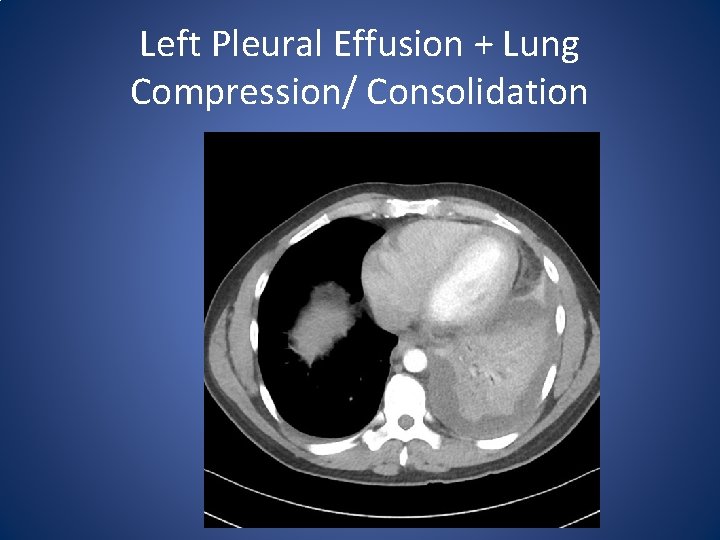
Left Pleural Effusion + Lung Compression/ Consolidation
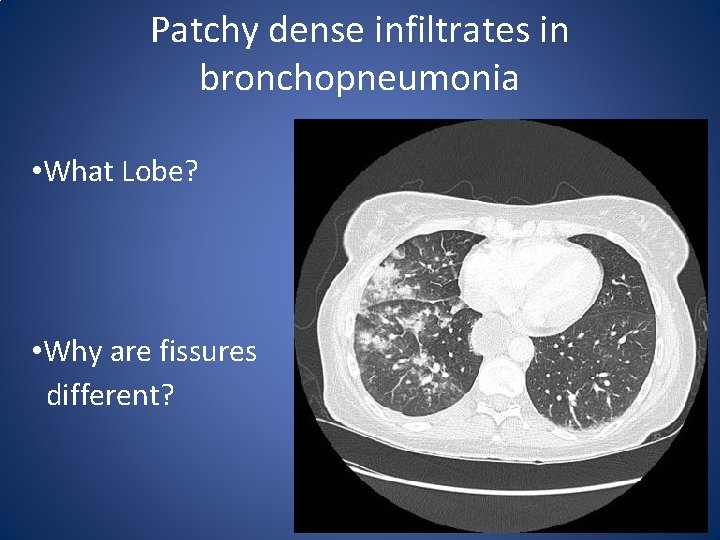
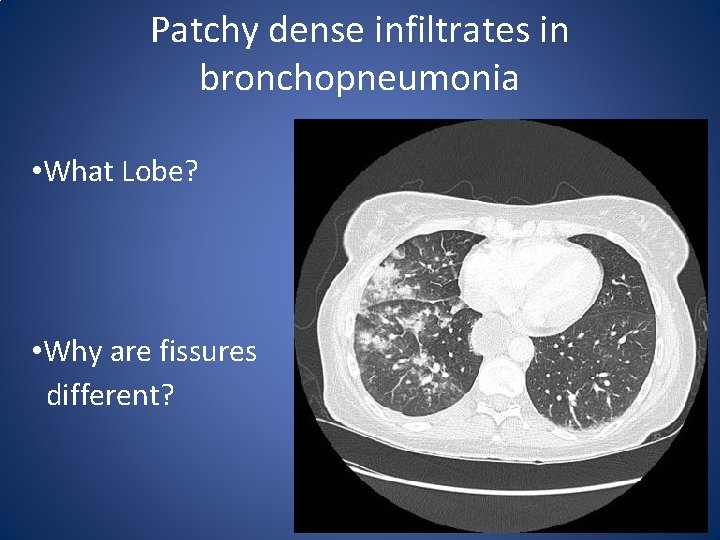
Patchy dense infiltrates in bronchopneumonia • What Lobe? • Why are fissures different?
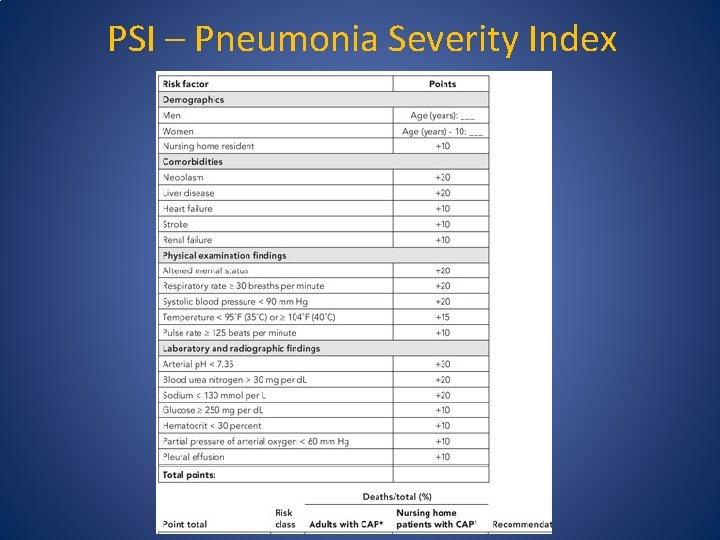
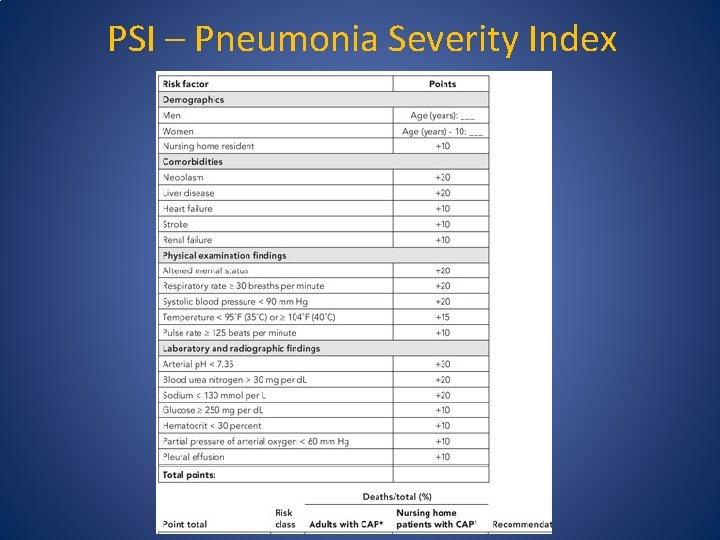
PSI – Pneumonia Severity Index
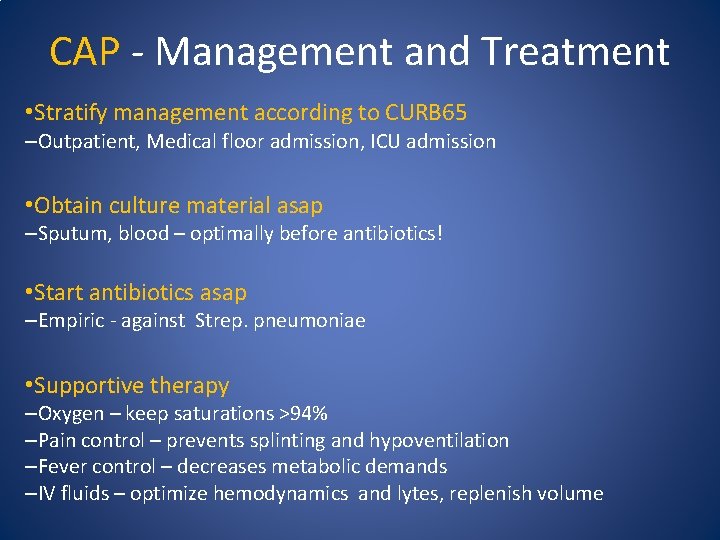
CAP - Management and Treatment • Stratify management according to CURB 65 –Outpatient, Medical floor admission, ICU admission • Obtain culture material asap –Sputum, blood – optimally before antibiotics! • Start antibiotics asap –Empiric - against Strep. pneumoniae • Supportive therapy –Oxygen – keep saturations >94% –Pain control – prevents splinting and hypoventilation –Fever control – decreases metabolic demands –IV fluids – optimize hemodynamics and lytes, replenish volume
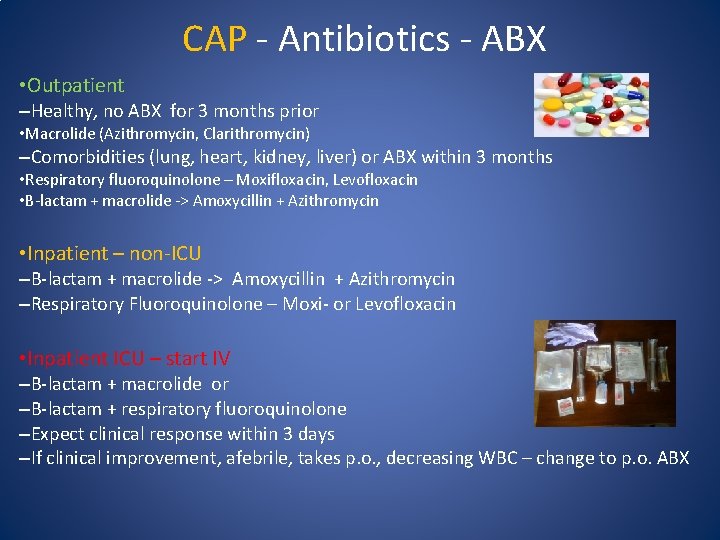
CAP - Antibiotics - ABX • Outpatient –Healthy, no ABX for 3 months prior • Macrolide (Azithromycin, Clarithromycin) –Comorbidities (lung, heart, kidney, liver) or ABX within 3 months • Respiratory fluoroquinolone – Moxifloxacin, Levofloxacin • B-lactam + macrolide -> Amoxycillin + Azithromycin • Inpatient – non-ICU –B-lactam + macrolide -> Amoxycillin + Azithromycin –Respiratory Fluoroquinolone – Moxi- or Levofloxacin • Inpatient ICU – start IV –B-lactam + macrolide or –B-lactam + respiratory fluoroquinolone –Expect clinical response within 3 days –If clinical improvement, afebrile, takes p. o. , decreasing WBC – change to p. o. ABX
Antibiotics – Length of treatment • Mild CAP – 5 -7 days • Severe CAP – 7 -8 days • Severe CAP including Pseudomonas – 14 days
CAP - Prevention ● Smoking cessation – Nicotine patch, lozenge, gum, counseling, clinic visits ● Vaccination – Seasonal Influenza, S. pneumoniae – PPSV 23 and PSV 13 vaccines, Haemophilus influenzae, ● Improve indoor air quality and reduce air pollution ● Treating underlying illnesses – Heart failure, kidney failure, stringent blood sugar control in diabetes, HIV/AIDS retroviral therapy, increase nutrition, optimize asthma/ COPD therapy
Nosocomial Pneumonias ● HAP – Hospital acquired PNA ● VAP – Ventilator Associated PNA
HAP – Epidemiology ● Second most common nosocomial infection ● High morbidity and mortality – 30% ● Increases hospital stay by 7 -9 days ● Increases costs $40, 000 per patient ● 25% of all ICU infections
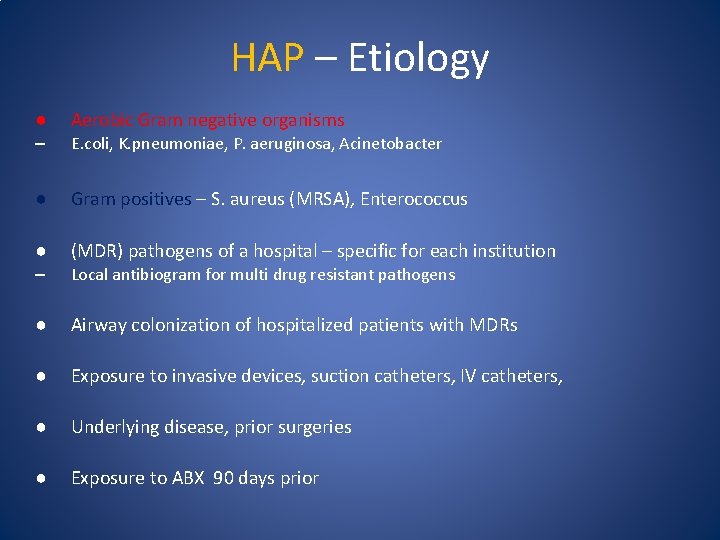
HAP – Etiology ● Aerobic Gram negative organisms – E. coli, K. pneumoniae, P. aeruginosa, Acinetobacter ● Gram positives – S. aureus (MRSA), Enterococcus ● (MDR) pathogens of a hospital – specific for each institution – Local antibiogram for multi drug resistant pathogens ● Airway colonization of hospitalized patients with MDRs ● Exposure to invasive devices, suction catheters, IV catheters, ● Underlying disease, prior surgeries ● Exposure to ABX 90 days prior
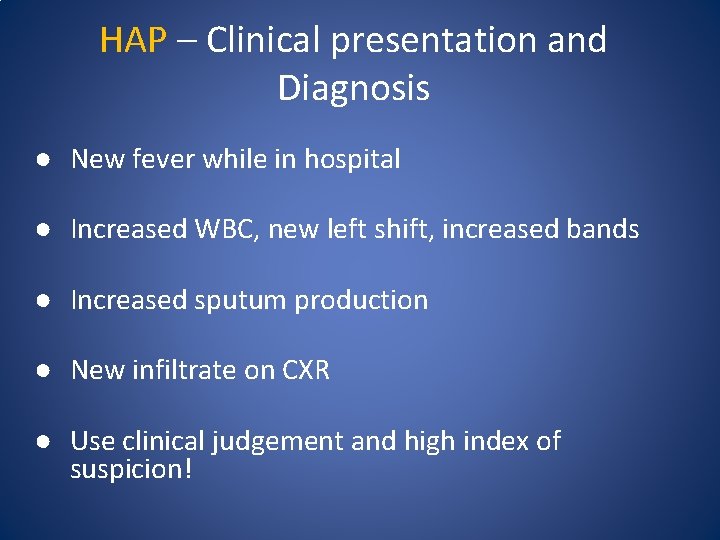
HAP – Clinical presentation and Diagnosis ● New fever while in hospital ● Increased WBC, new left shift, increased bands ● Increased sputum production ● New infiltrate on CXR ● Use clinical judgement and high index of suspicion!
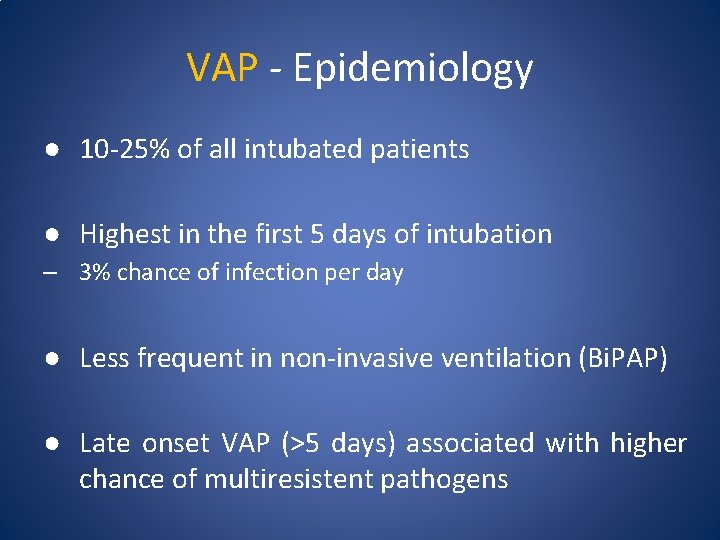
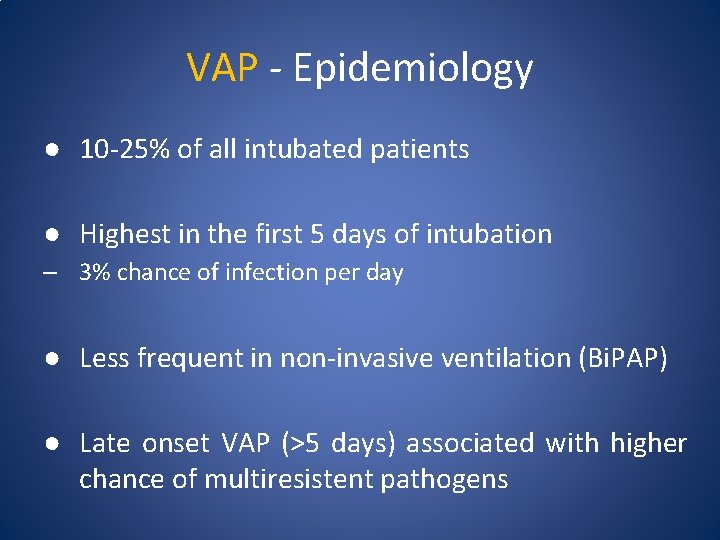
VAP - Epidemiology ● 10 -25% of all intubated patients ● Highest in the first 5 days of intubation – 3% chance of infection per day ● Less frequent in non-invasive ventilation (Bi. PAP) ● Late onset VAP (>5 days) associated with higher chance of multiresistent pathogens
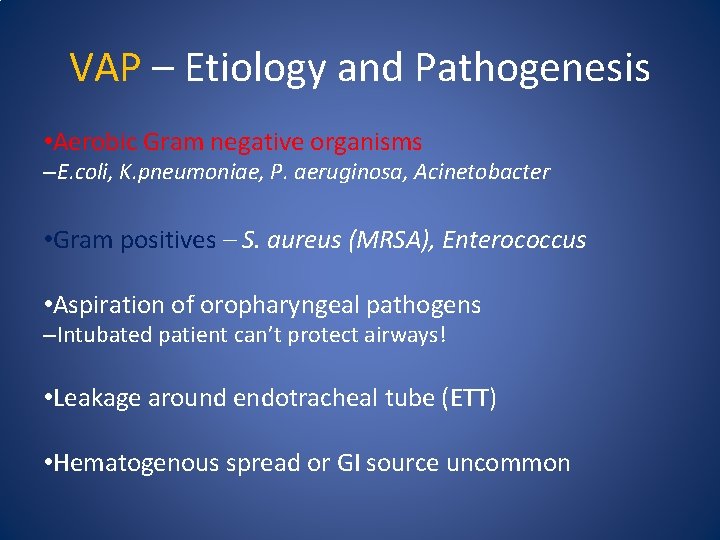
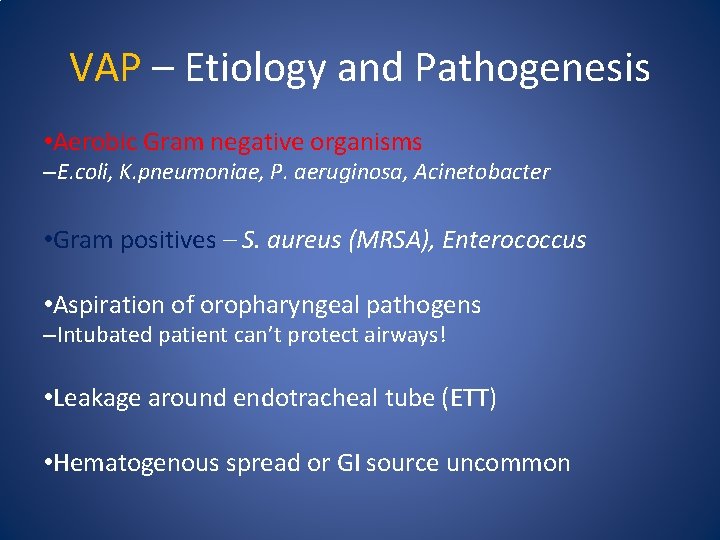
VAP – Etiology and Pathogenesis • Aerobic Gram negative organisms –E. coli, K. pneumoniae, P. aeruginosa, Acinetobacter • Gram positives – S. aureus (MRSA), Enterococcus • Aspiration of oropharyngeal pathogens –Intubated patient can’t protect airways! • Leakage around endotracheal tube (ETT) • Hematogenous spread or GI source uncommon
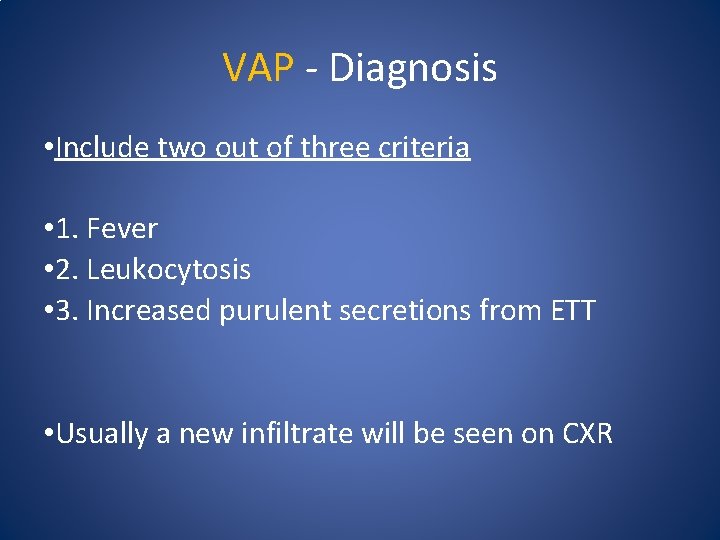
VAP - Diagnosis • Include two out of three criteria • 1. Fever • 2. Leukocytosis • 3. Increased purulent secretions from ETT • Usually a new infiltrate will be seen on CXR
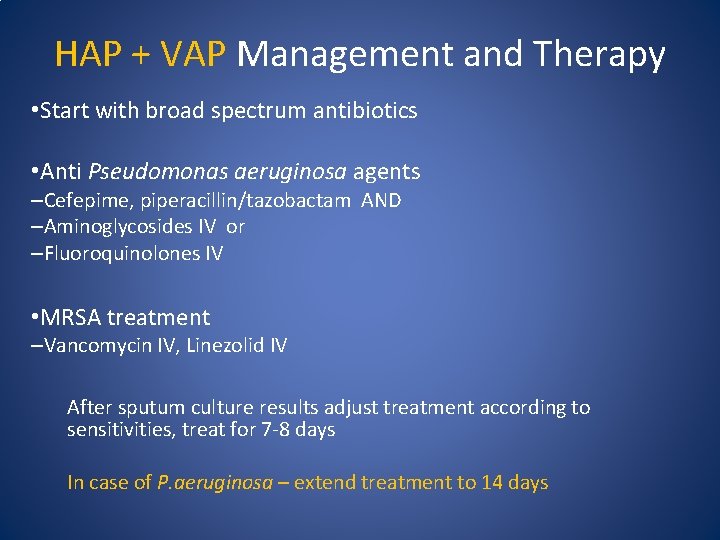
HAP + VAP Management and Therapy • Start with broad spectrum antibiotics • Anti Pseudomonas aeruginosa agents –Cefepime, piperacillin/tazobactam AND –Aminoglycosides IV or –Fluoroquinolones IV • MRSA treatment –Vancomycin IV, Linezolid IV After sputum culture results adjust treatment according to sensitivities, treat for 7 -8 days In case of P. aeruginosa – extend treatment to 14 days
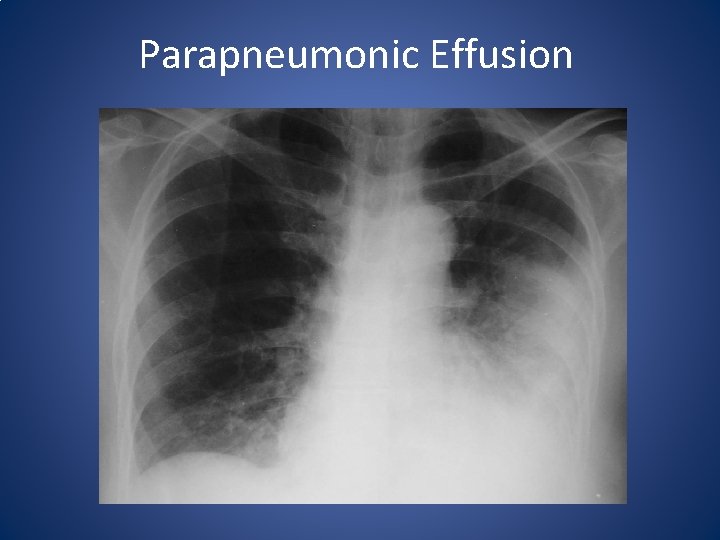
Complications of Pneumonia • Parapneumonic Effusion (Fluidothorax) –Requires thoracenthesis – p. H, LDH, Total protein, Cell #, Cultures, Cytology • Empyema –Requires chest tube drainage – send for Gram stain and cultures! • Circulatory failure –Sepsis, septic shock, MSOF - ICU stay, IV fluids, vasopressors • Respiratory failure (Hypoxemia, Hypercarbia) –ARDS (Adult Respiratory Distress Syndrome) –ICU stay - need for non-invasive or invasive ventilatory support
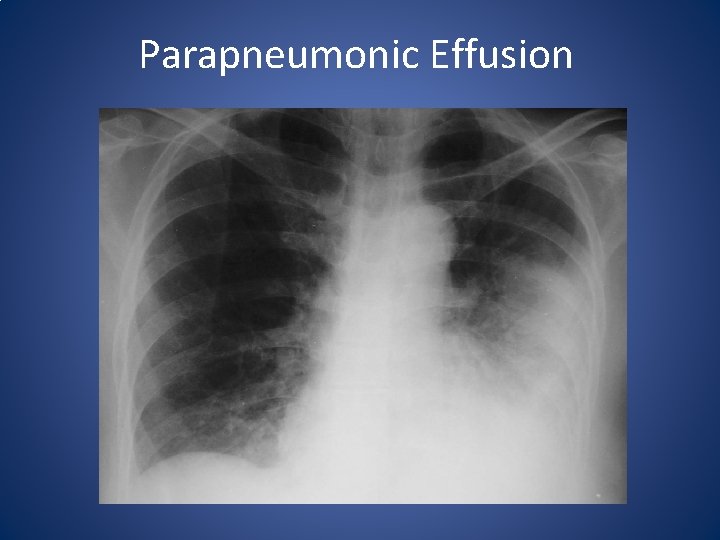
Parapneumonic Effusion
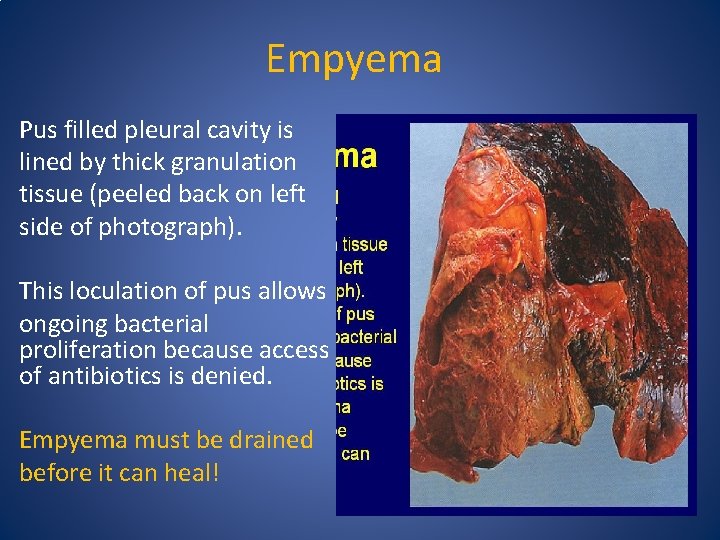
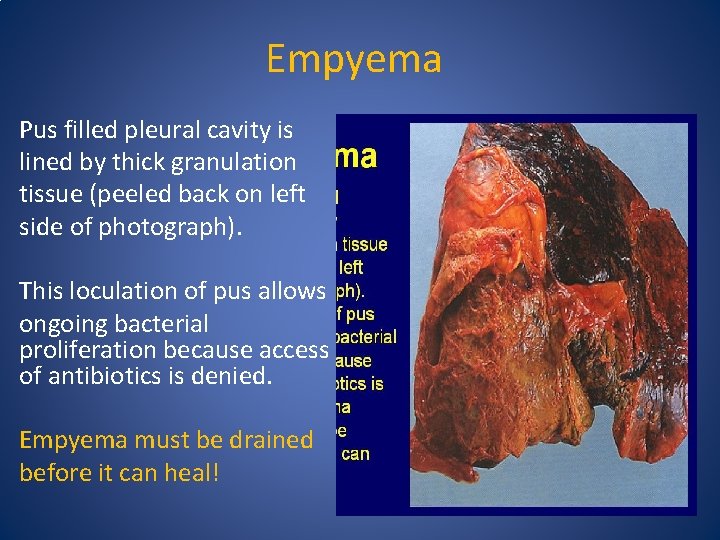
Empyema Pus filled pleural cavity is lined by thick granulation tissue (peeled back on left side of photograph). This loculation of pus allows ongoing bacterial proliferation because access of antibiotics is denied. Empyema must be drained before it can heal!
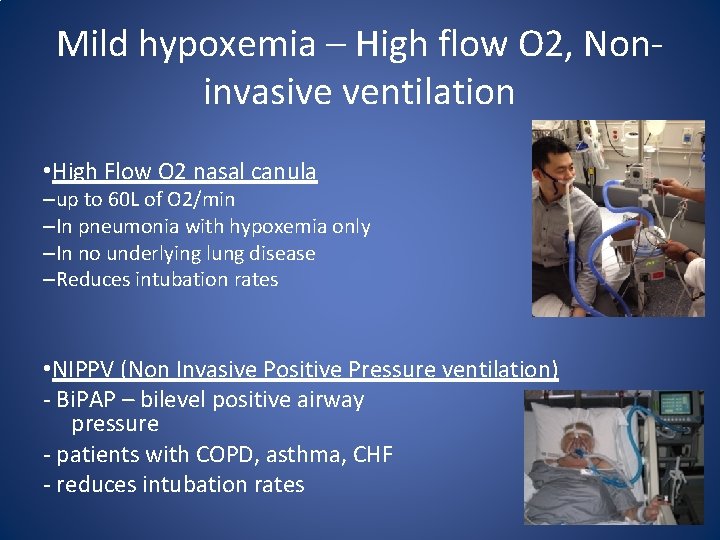
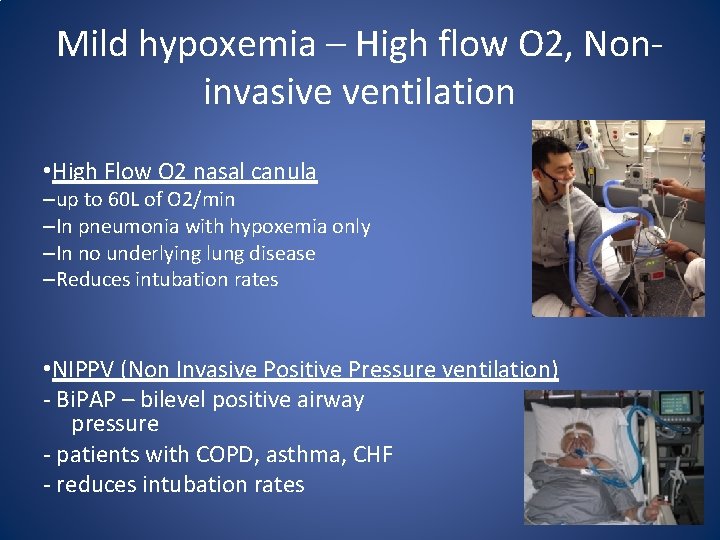
Mild hypoxemia – High flow O 2, Noninvasive ventilation • High Flow O 2 nasal canula –up to 60 L of O 2/min –In pneumonia with hypoxemia only –In no underlying lung disease –Reduces intubation rates • NIPPV (Non Invasive Positive Pressure ventilation) - Bi. PAP – bilevel positive airway pressure - patients with COPD, asthma, CHF - reduces intubation rates
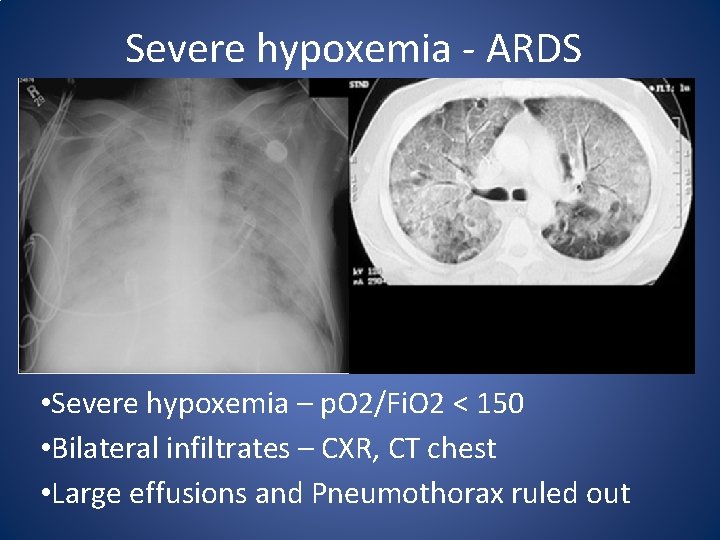
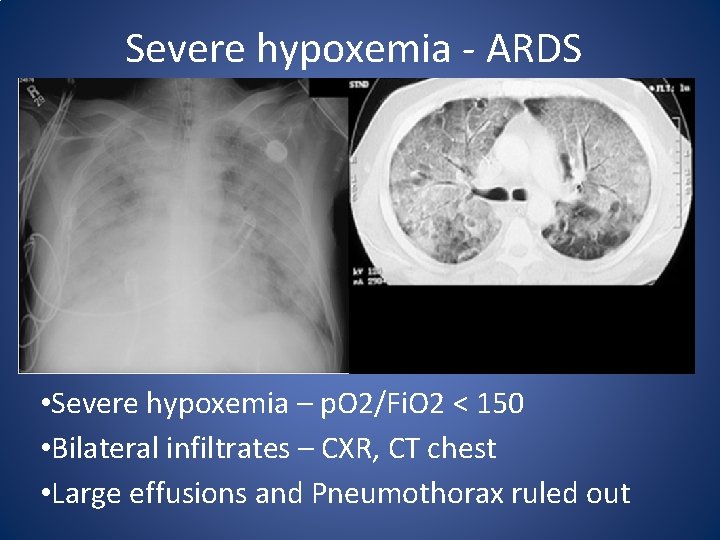
Severe hypoxemia - ARDS • Severe hypoxemia – p. O 2/Fi. O 2 < 150 • Bilateral infiltrates – CXR, CT chest • Large effusions and Pneumothorax ruled out
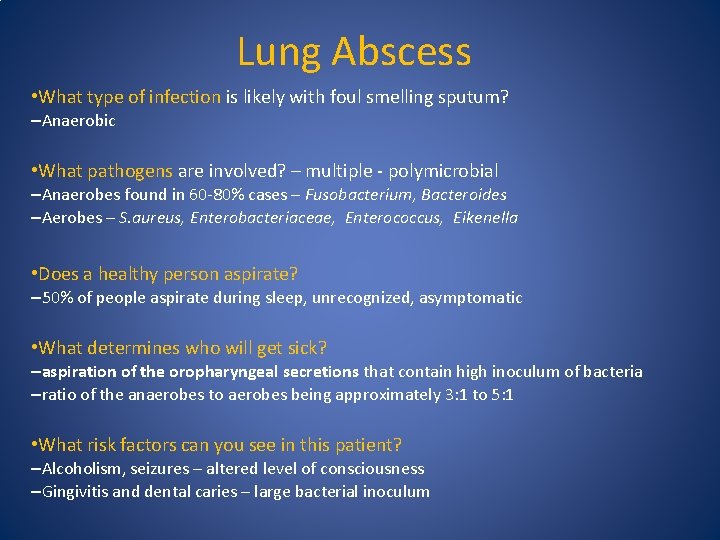
Lung Abscess • What type of infection is likely with foul smelling sputum? –Anaerobic • What pathogens are involved? – multiple - polymicrobial –Anaerobes found in 60 -80% cases – Fusobacterium, Bacteroides –Aerobes – S. aureus, Enterobacteriaceae, Enterococcus, Eikenella • Does a healthy person aspirate? – 50% of people aspirate during sleep, unrecognized, asymptomatic • What determines who will get sick? –aspiration of the oropharyngeal secretions that contain high inoculum of bacteria –ratio of the anaerobes to aerobes being approximately 3: 1 to 5: 1 • What risk factors can you see in this patient? –Alcoholism, seizures – altered level of consciousness –Gingivitis and dental caries – large bacterial inoculum
Lung Abscess – Etiology and Pathogenesis • Mechanical disruption of glottic closure or cardiac sphincter –endotracheal tubes, nasogastric feeding tubes, tracheostomy, –pharyngeal anesthesia • Reduced levels of consciousness –dysfunction of the glottic closure and cough reflex –ethanol abuse, seizures, drug overdose, general anesthesia, CVA, and metabolic encephalopathy • Dysphagia - neurologic disease or esophageal disease. • Periodontal disease and gingivitis –increased anaerobic inoculum, and are frequently encountered in patients with aspiration pneumonia. • In about 10% of lung abscess cases, no risk factors are identified.
Lung Abscess – Clinical Presentation • Sub-acute onset of illness –most do not seek medical attention for three to four weeks since the onset of illness • Cough, low grade fever, anorexia and weight loss –few weeks duration • Large amounts of foul smelling sputum • Lack of foul smell does not exclude lung abscess – 50% of anaerobic infections do not produce a foul smell.
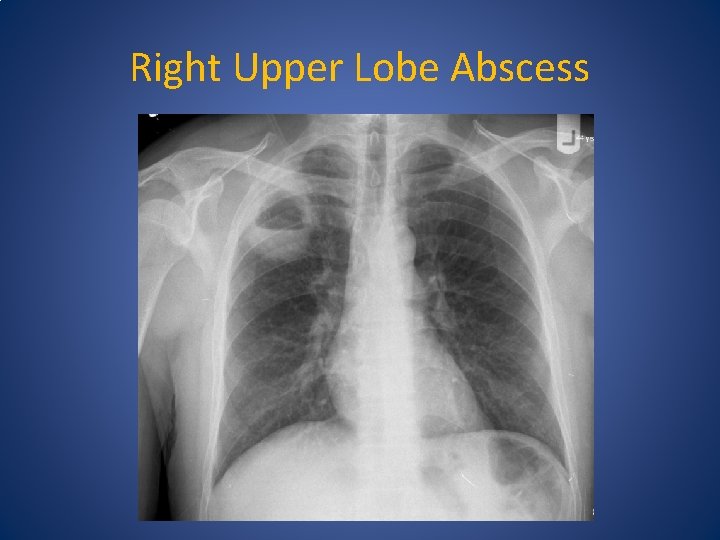
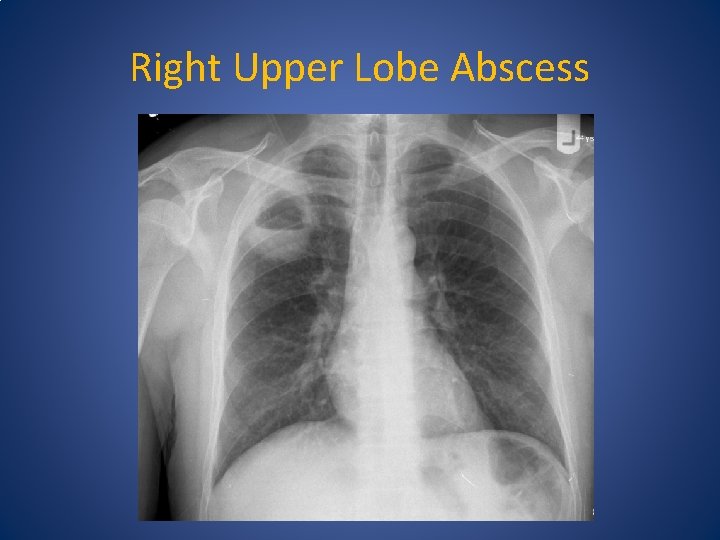
Right Upper Lobe Abscess
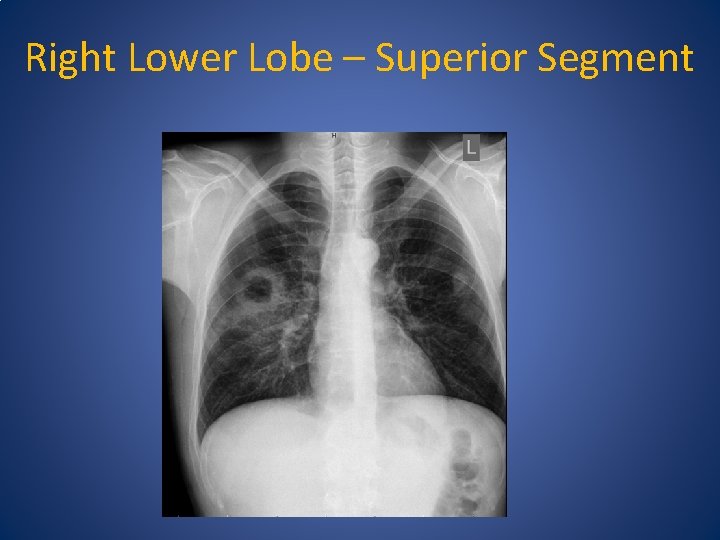
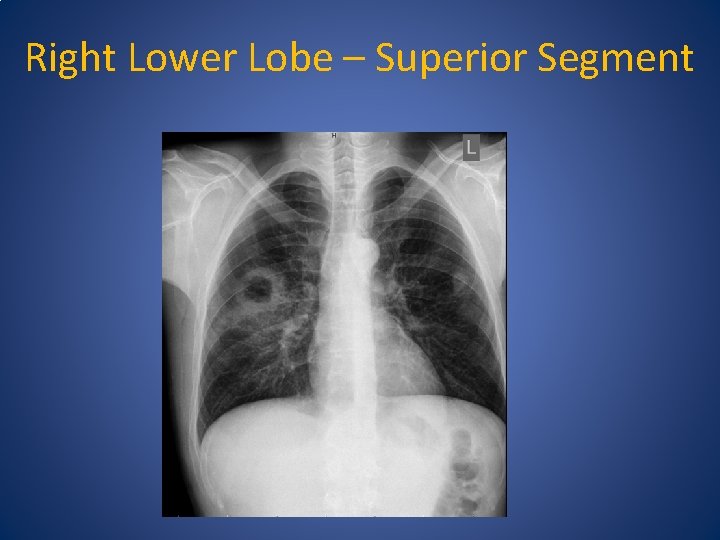
Right Lower Lobe – Superior Segment
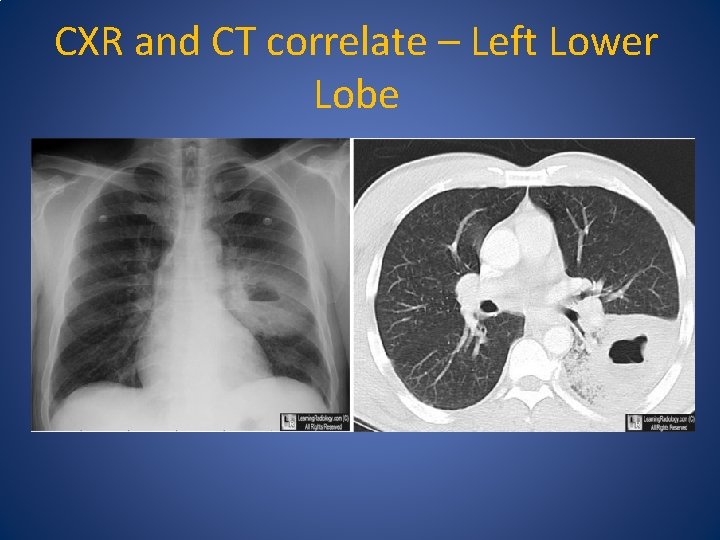
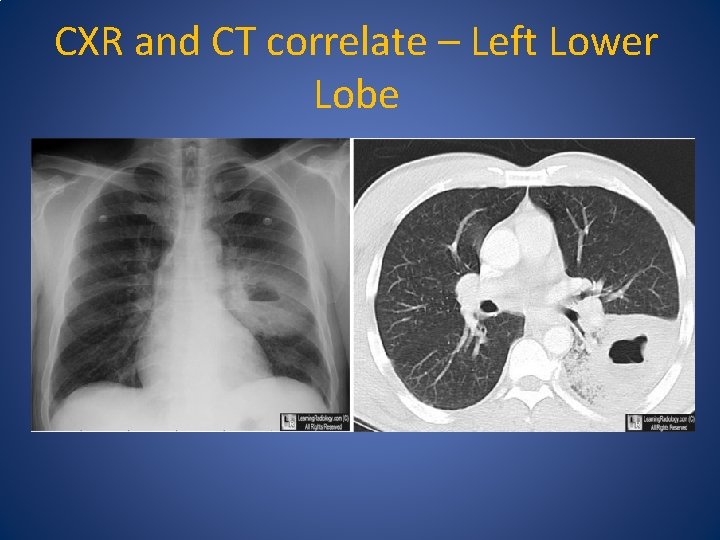
CXR and CT correlate – Left Lower Lobe
Predominant sites for aspiration • Lower lobes –Upright – basilar segments of lower lobes –Supine – superior segments of lower lobes • Gravitational forces –Aspirate goes to the lowest point in the lung • Position of the patient –Supine, left or right lateral decubitus position
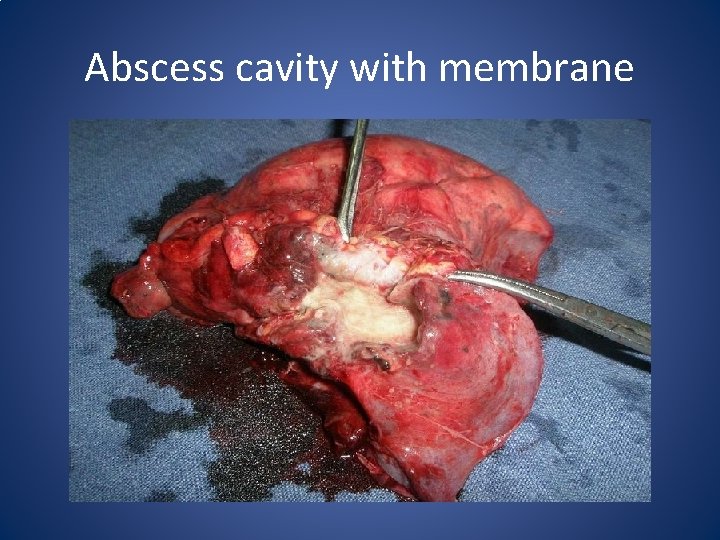
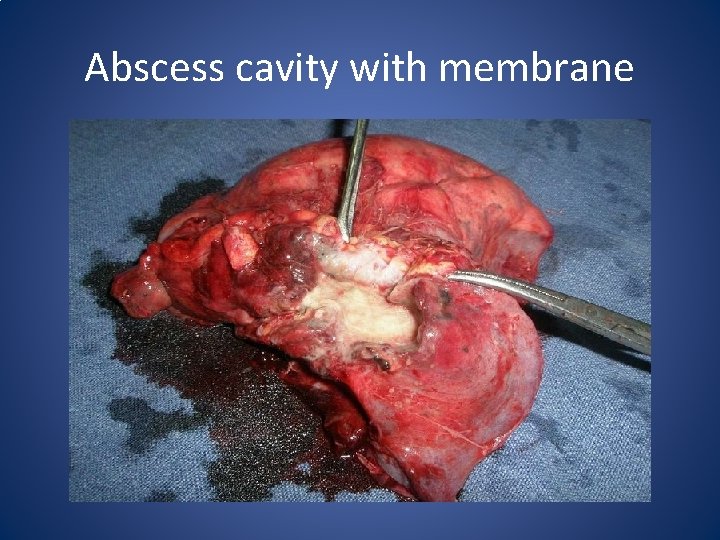
Abscess cavity with membrane
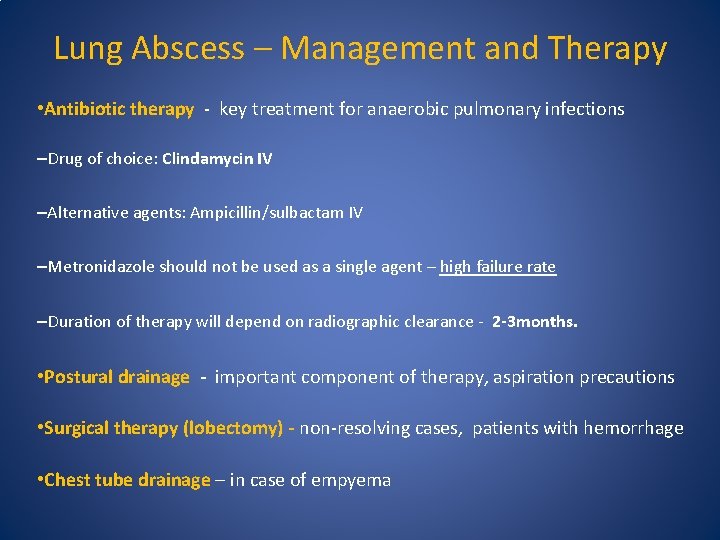
Lung Abscess – Management and Therapy • Antibiotic therapy - key treatment for anaerobic pulmonary infections –Drug of choice: Clindamycin IV –Alternative agents: Ampicillin/sulbactam IV –Metronidazole should not be used as a single agent – high failure rate –Duration of therapy will depend on radiographic clearance - 2 -3 months. • Postural drainage - important component of therapy, aspiration precautions • Surgical therapy (lobectomy) - non-resolving cases, patients with hemorrhage • Chest tube drainage – in case of empyema
 Nuclear medicine lectures
Nuclear medicine lectures Hematology medicine student lectures
Hematology medicine student lectures Soft it beregner
Soft it beregner Cap compas
Cap compas Hap griffin
Hap griffin Hap
Hap Szte hap
Szte hap Hap ci
Hap ci Gmu health informatics
Gmu health informatics Hap python
Hap python Havadan gelir top gibi suda erir hap gibi
Havadan gelir top gibi suda erir hap gibi Hap farber
Hap farber Hap introduction
Hap introduction Hệ hô hấp
Hệ hô hấp Map hap
Map hap Concept of lead time
Concept of lead time Introduction to community medicine
Introduction to community medicine Minus type desk
Minus type desk Cohort study community medicine
Cohort study community medicine Lt lead time
Lt lead time Basic requirements for sound phc
Basic requirements for sound phc Duke medicine grand rounds
Duke medicine grand rounds Types of family in community medicine
Types of family in community medicine Introduction to community medicine
Introduction to community medicine Seqs community medicine
Seqs community medicine Bureau of lectures
Bureau of lectures Jim kurose
Jim kurose Frcr physics lectures
Frcr physics lectures Advanced medicinal chemistry
Advanced medicinal chemistry Software project management lectures
Software project management lectures Pathology lectures for medical students
Pathology lectures for medical students Medical emergency student lectures
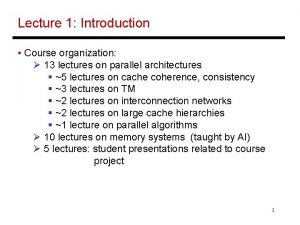
Medical emergency student lectures 13 lectures
13 lectures Oral communication 3 lectures text
Oral communication 3 lectures text What is aerodynamics
What is aerodynamics Theory of translation lectures
Theory of translation lectures Utilities and energy lectures
Utilities and energy lectures Cern summer school lectures
Cern summer school lectures Comsats virtual campus lectures
Comsats virtual campus lectures Rick trebino lectures
Rick trebino lectures Trend lectures
Trend lectures Hegel philosophy of fine art summary
Hegel philosophy of fine art summary Frcr physics lectures
Frcr physics lectures Dr asim lectures
Dr asim lectures Uva powerpoint
Uva powerpoint Molecular biology lectures
Molecular biology lectures Rcog cpd portfolio
Rcog cpd portfolio C programming and numerical analysis an introduction
C programming and numerical analysis an introduction Tamara berg husband
Tamara berg husband Theory of translation lectures
Theory of translation lectures Web engineering lectures ppt
Web engineering lectures ppt Neonatology lectures
Neonatology lectures