ACUTE AORTIC SYNDROME NISHITH PATEL WAIKATO CARDIOTHORACIC UNIT





















- Slides: 55
ACUTE AORTIC SYNDROME NISHITH PATEL WAIKATO CARDIOTHORACIC UNIT
ACUTE AORTIC SYNDROME Nishith Patel 11 th August 2017

Overview • Type A Aortic Dissection • Type A Intramural Haematoma • Type A Penetrating Aortic Ulcer • Evidence • Who and when to operate? • Pre-op management • Surgical Strategies

History On 25 October 1760 George II, then 76, rose at his normal hour of 6 AM, called as usual for his chocolate, and repaired to the closet-stool. The German valet de chambre heard a noise, memorably described as ‘louder than the royal wind', and then a groan; he ran in and found the King lying on the floor, having cut his face in falling. Mr. Andrews, surgeon of the household, was called and bled his Majesty but in vain, as no sign of life was observed from the time of his fall. At necropsy the next day Dr. Nicholls, physician to his late Majesty, found the pericardium distended with a pint of coagulated blood, probably from an orifice in the right ventricle, and a transverse fissure on the inner side of the ascending aorta 3. 75 cm long, through which blood had recently passed in its external coat to form a raised ecchymosis, this appearance being interpreted as an incipient aneurysm of the aorta. Leonard JC. BMJ 1979; 2: 260 -262.

First Repair of Thoracic Aortic Aneurysm - 1955 • De. Bakey and Cooley, Ann Surg 1955: 142: 586 -612.
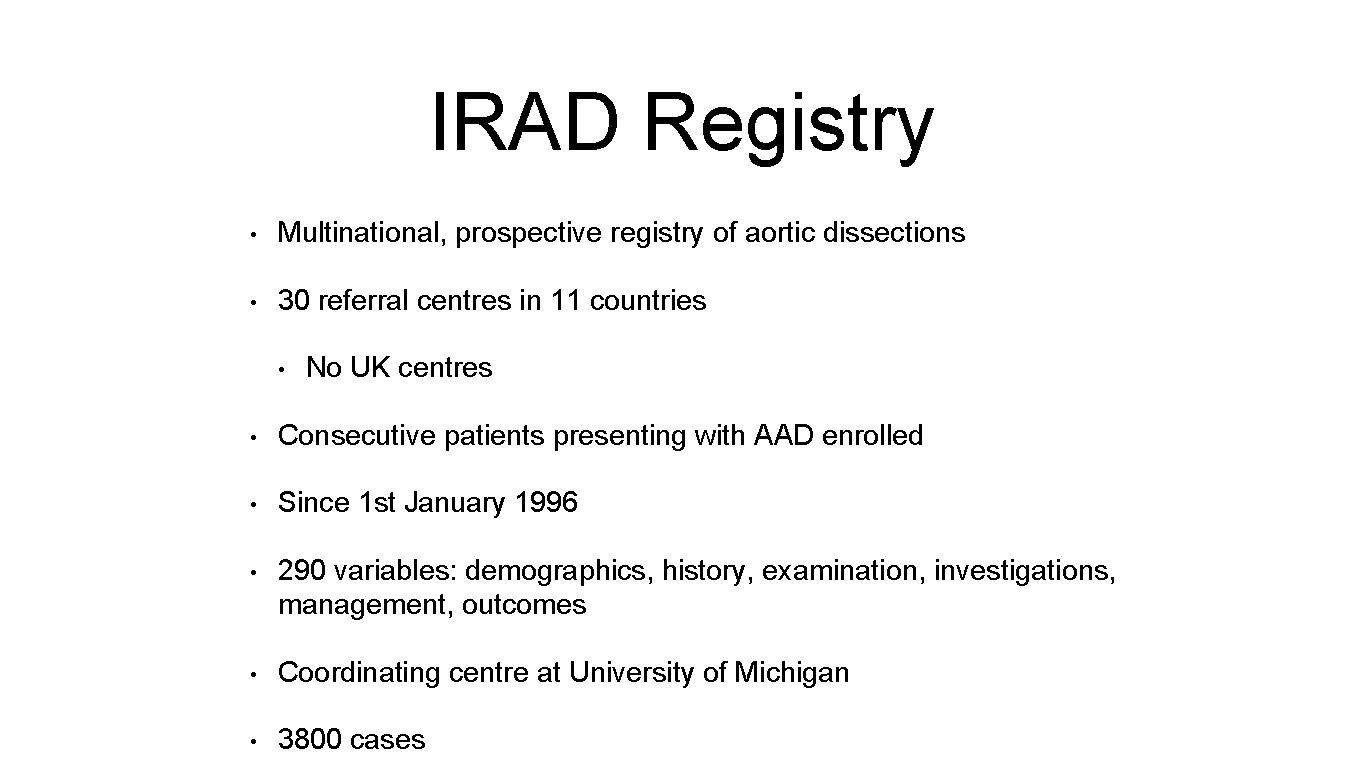
IRAD Registry • Multinational, prospective registry of aortic dissections • 30 referral centres in 11 countries • No UK centres • Consecutive patients presenting with AAD enrolled • Since 1 st January 1996 • 290 variables: demographics, history, examination, investigations, management, outcomes • Coordinating centre at University of Michigan • 3800 cases
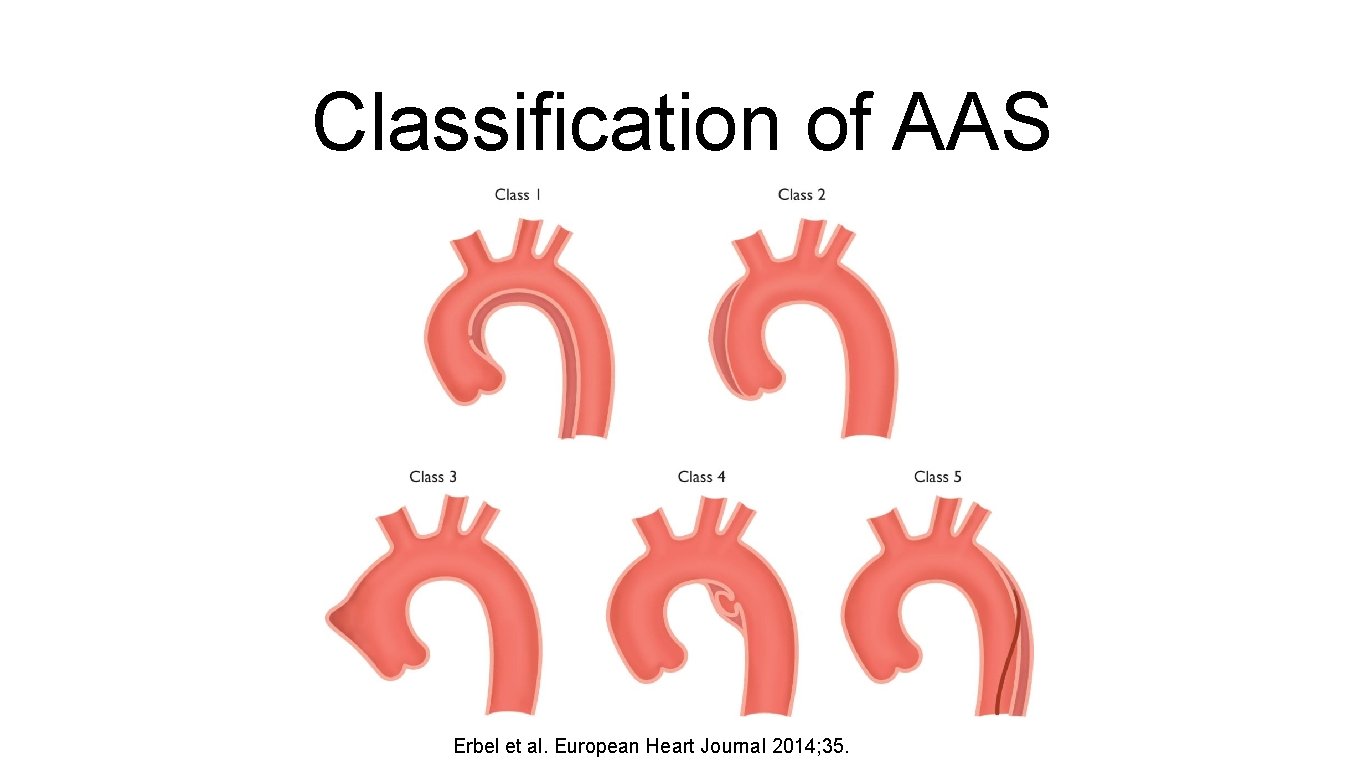
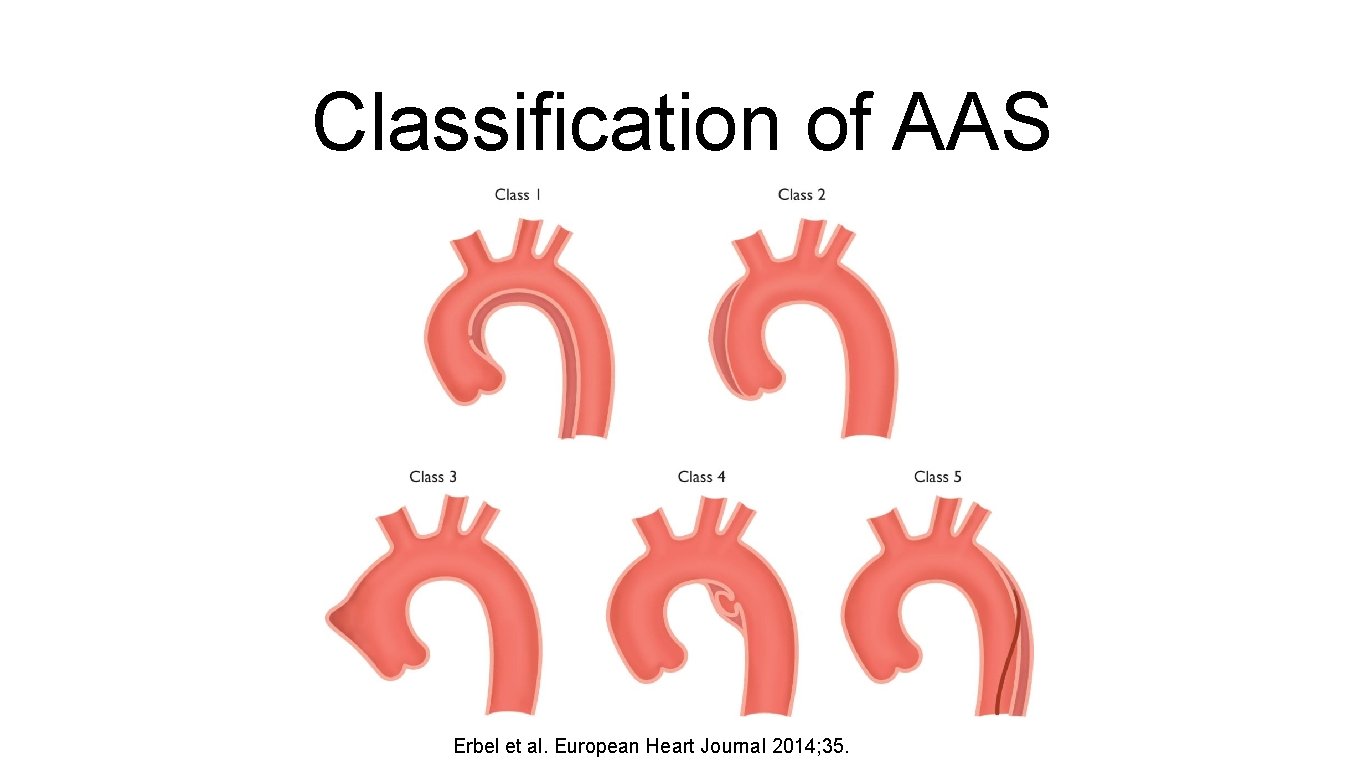
Classification of AAS Erbel et al. European Heart Journal 2014; 35.
Acute Aortic Dissection
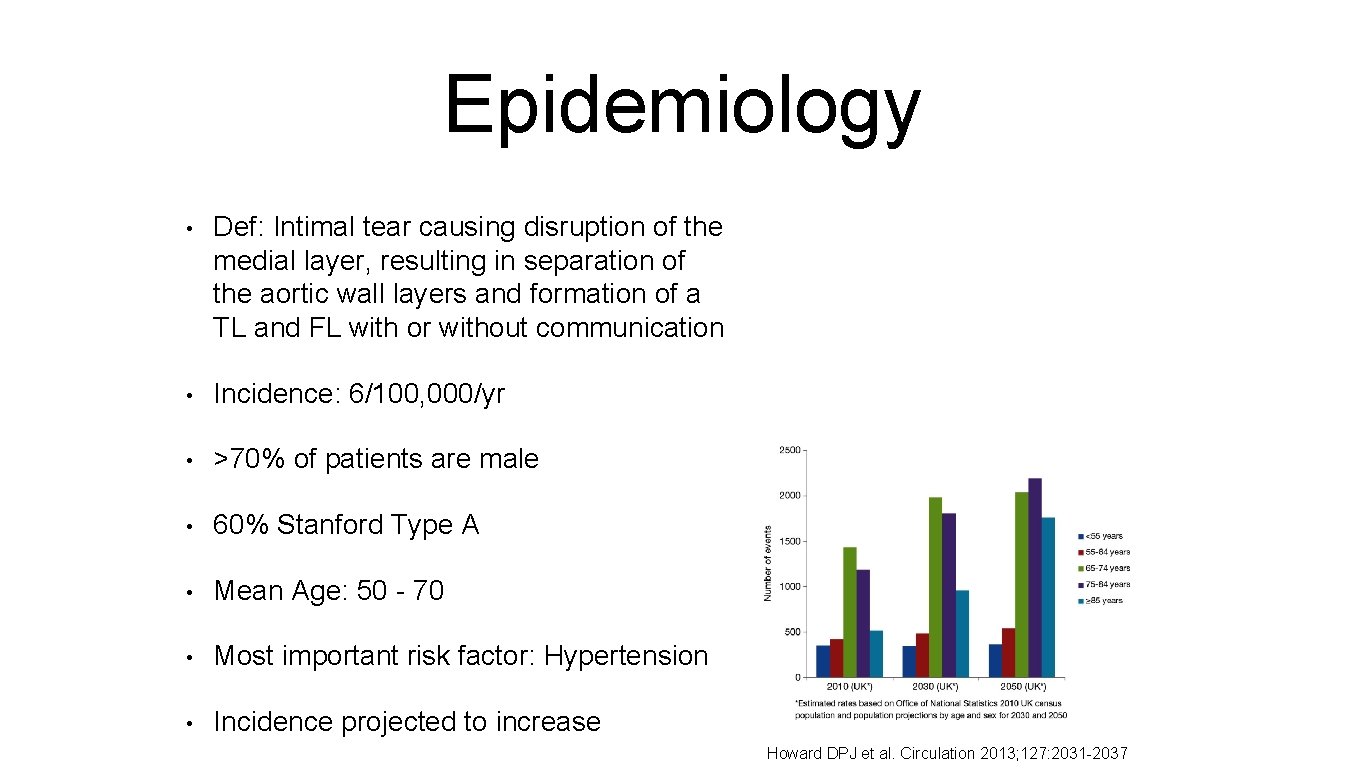
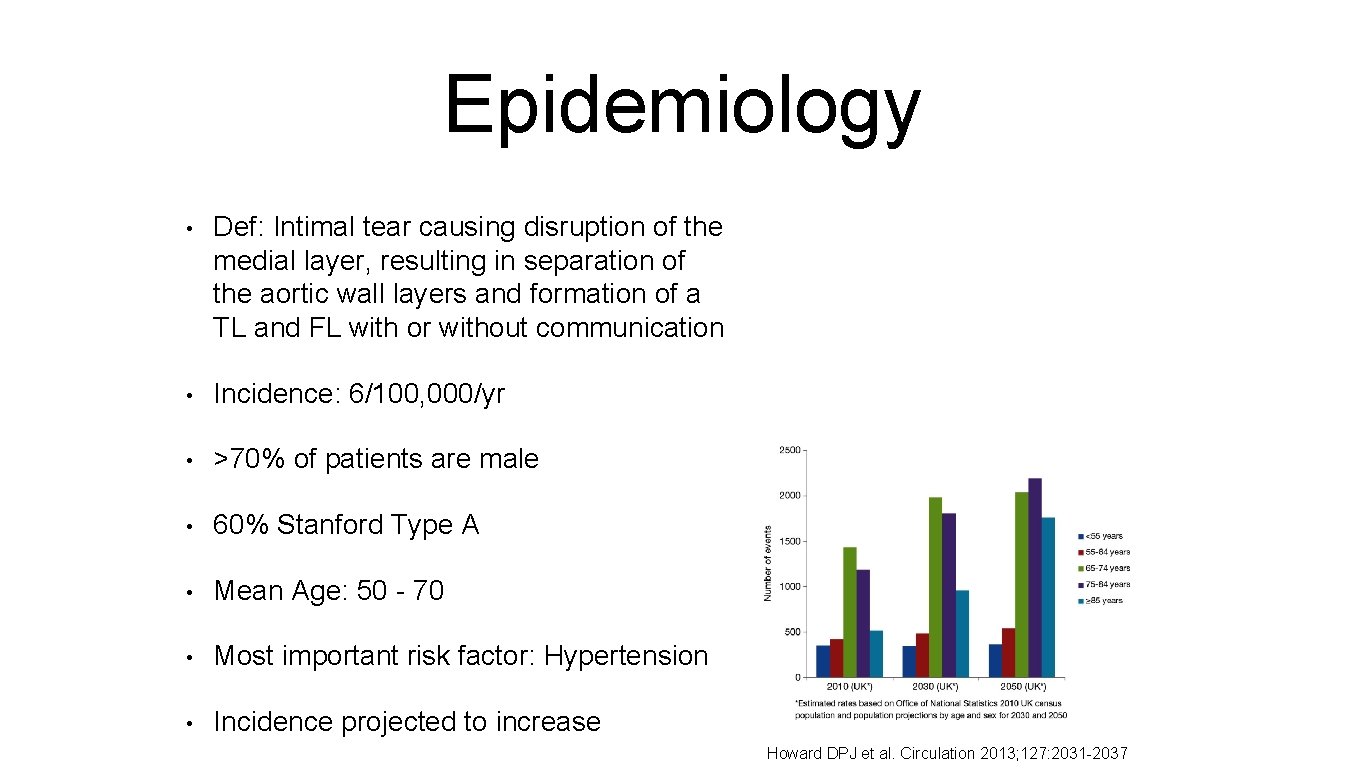
Epidemiology • Def: Intimal tear causing disruption of the medial layer, resulting in separation of the aortic wall layers and formation of a TL and FL with or without communication • Incidence: 6/100, 000/yr • >70% of patients are male • 60% Stanford Type A • Mean Age: 50 - 70 • Most important risk factor: Hypertension • Incidence projected to increase Howard DPJ et al. Circulation 2013; 127: 2031 -2037

Natural History • 50% of patients with Type A Dissection die before reaching hospital. a • For those who survived to hospital admission, the 30 -d mortality rate was 50%. a • Type A dissection, 30 -d mortality b: • • Surgical: 26% • Medical: 58% Type B dissection, 30 -d mortality b: • Surgical: 31% • Medical: 11% a. Howard DPJ et al. Circulation 2013; 127: 2031 -2037 b. Hagan PG et al. JAMA 2000; 283: 897 -903.

Aetiology/Risk Factors • Hypertension (75%) • Genetic • Bicuspid AV • Loeys/Dietz syndrome • • Atherosclerosis • Marfan syndrome • • Ehlers-Danlos Syndrome • Congenital • Coarctation • Turner Syndrome • TOF Inflammatory/Connectiv e tissue disorders PAU • Giant cell arteritis • Takayasu arteritis • Aortitis • Syphilis Trauma/Iatrogenic • Hereditary TAAD • • Cardiac surgery Cardiac cath IABP • Cocaine • Pregnancy

Classification of AAD

Clinical Presentation Symptom/Sign Prevalence (%) Chest Pain 79% Abrupt onset 85% Severe or worst ever pain 90% Hypertensive 40% Normotensive 40% Hypotensive or Shock 20% Pulse Deficit 20% AR Murmur 44% CXR: Widened mediastinum 63% CXR: Abnormal aortic contour 47% CXR: No abnormalities 11% Hagan PG et al. JAMA 2000; 283: 897 -903.
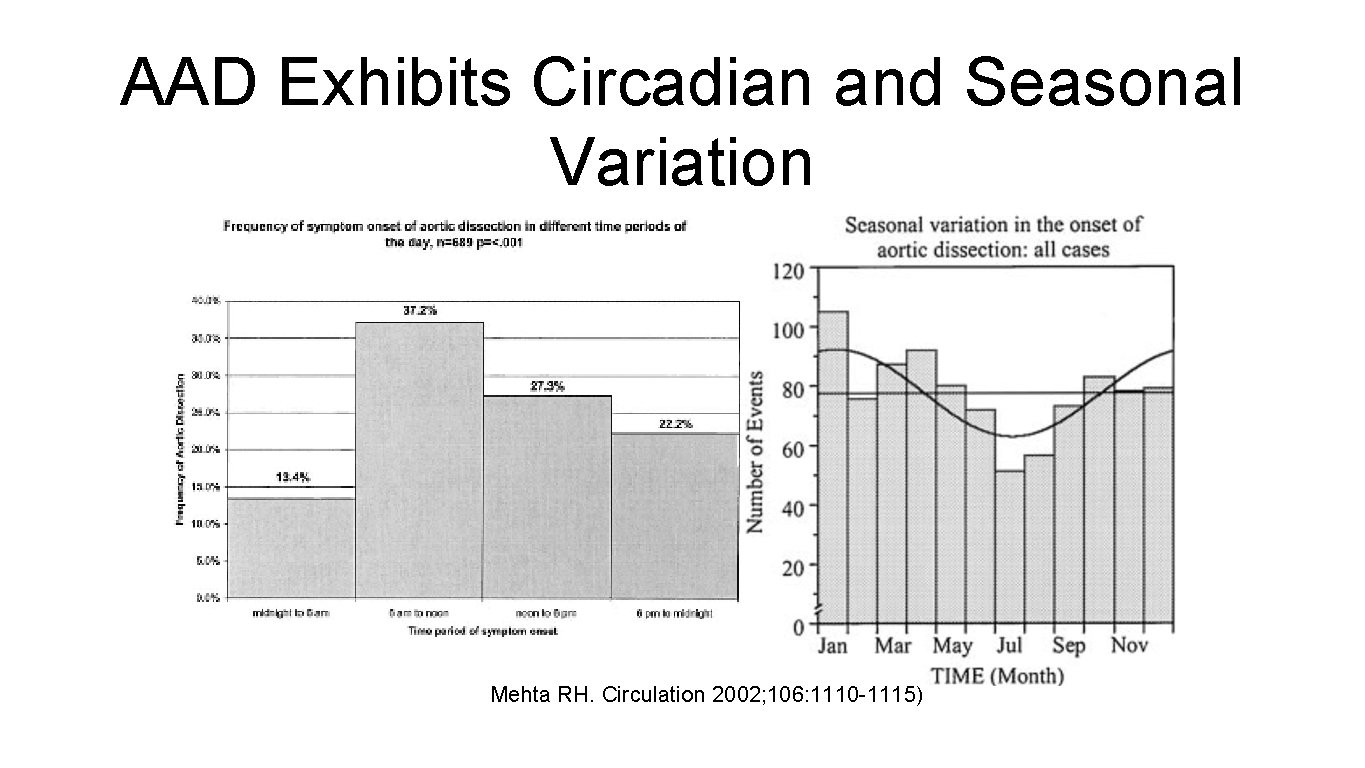
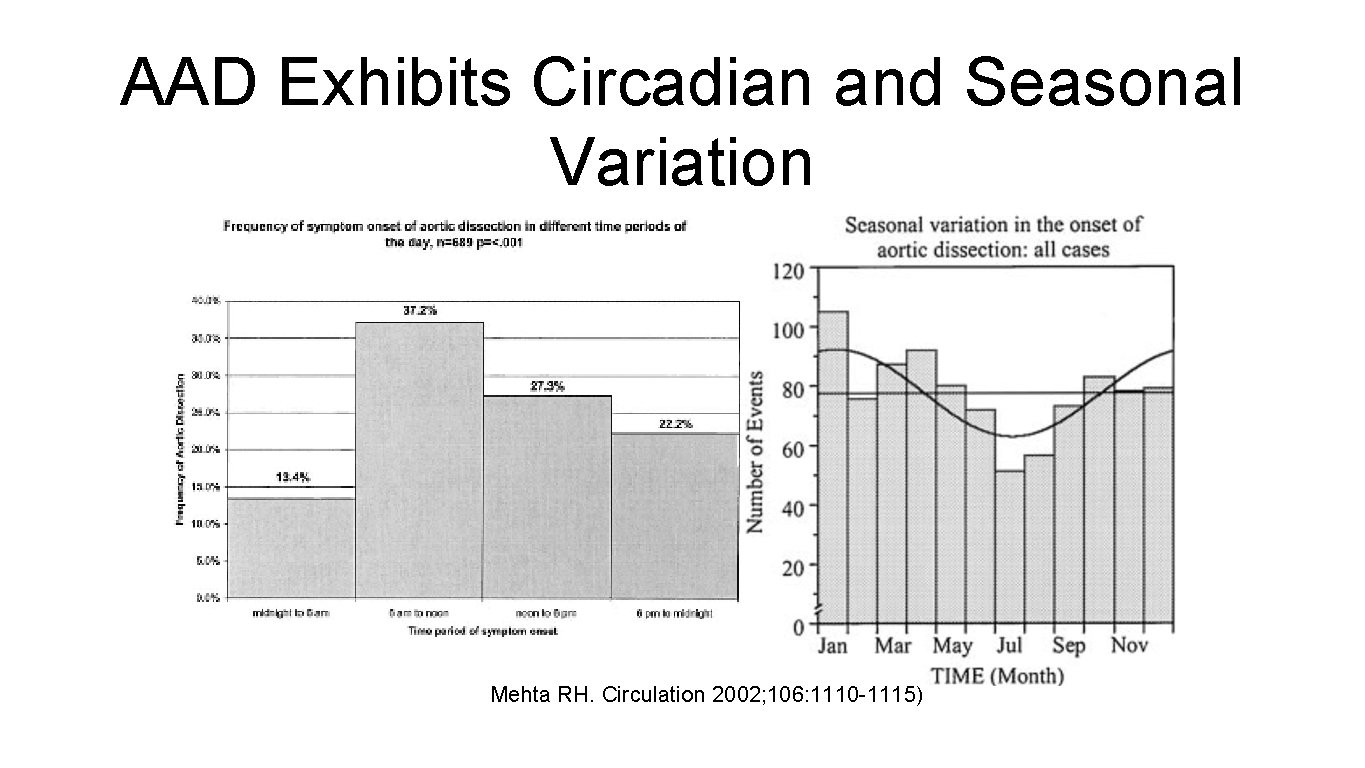
AAD Exhibits Circadian and Seasonal Variation Mehta RH. Circulation 2002; 106: 1110 -1115)
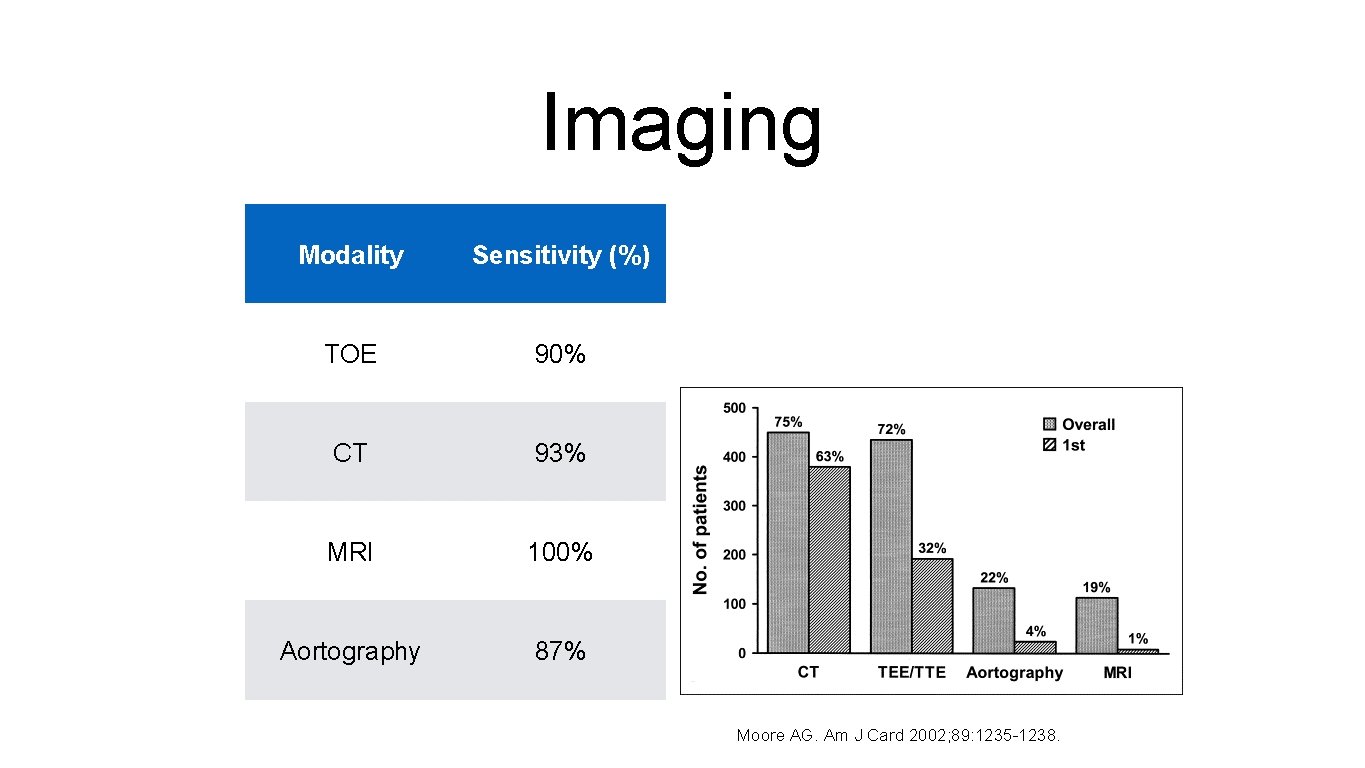
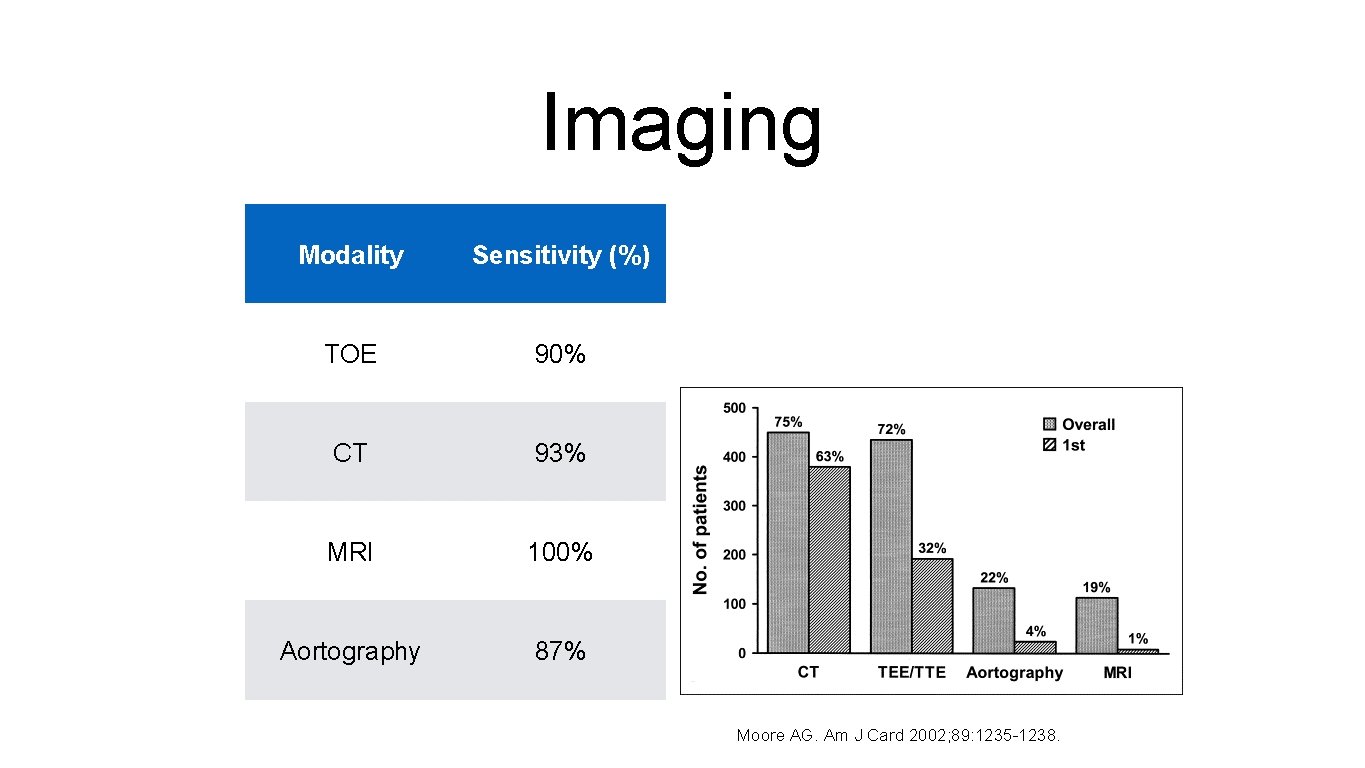
Imaging Modality Sensitivity (%) TOE 90% CT 93% MRI 100% Aortography 87% Moore AG. Am J Card 2002; 89: 1235 -1238.
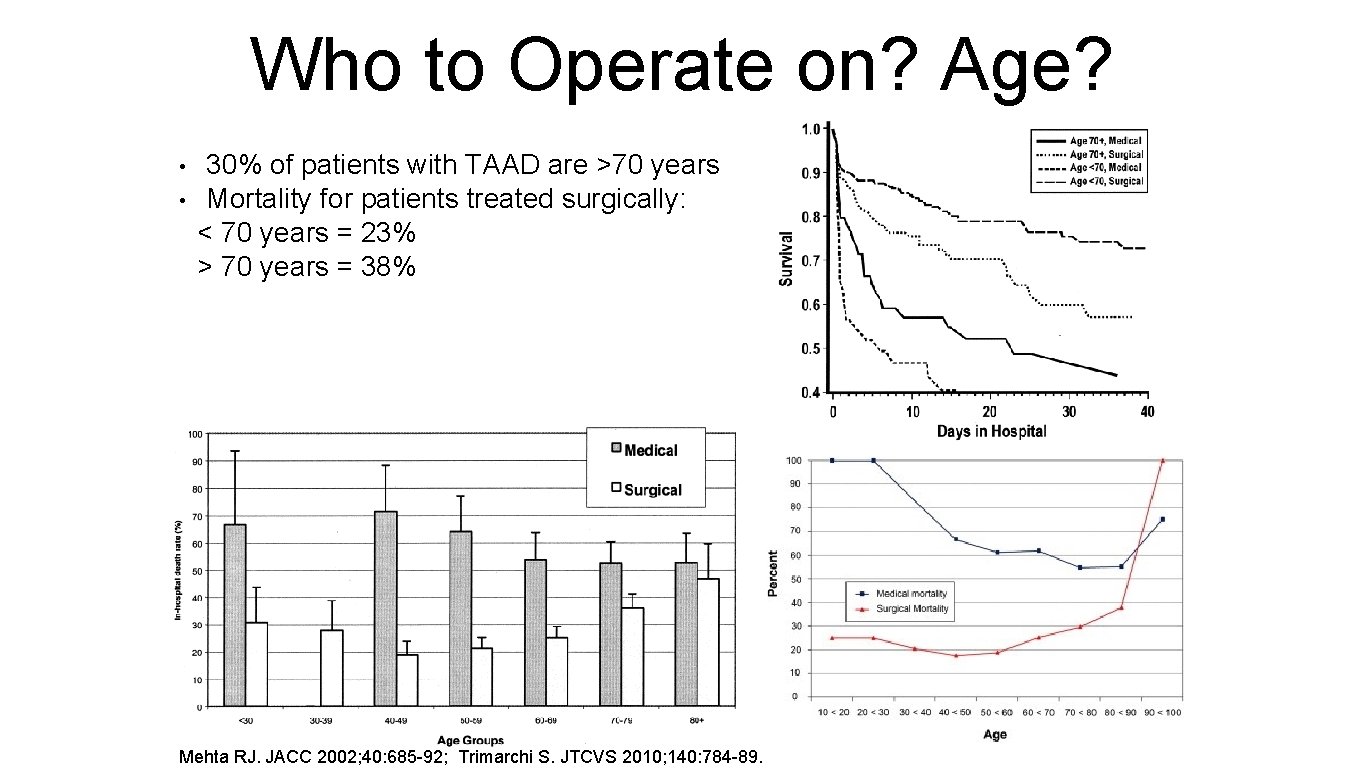
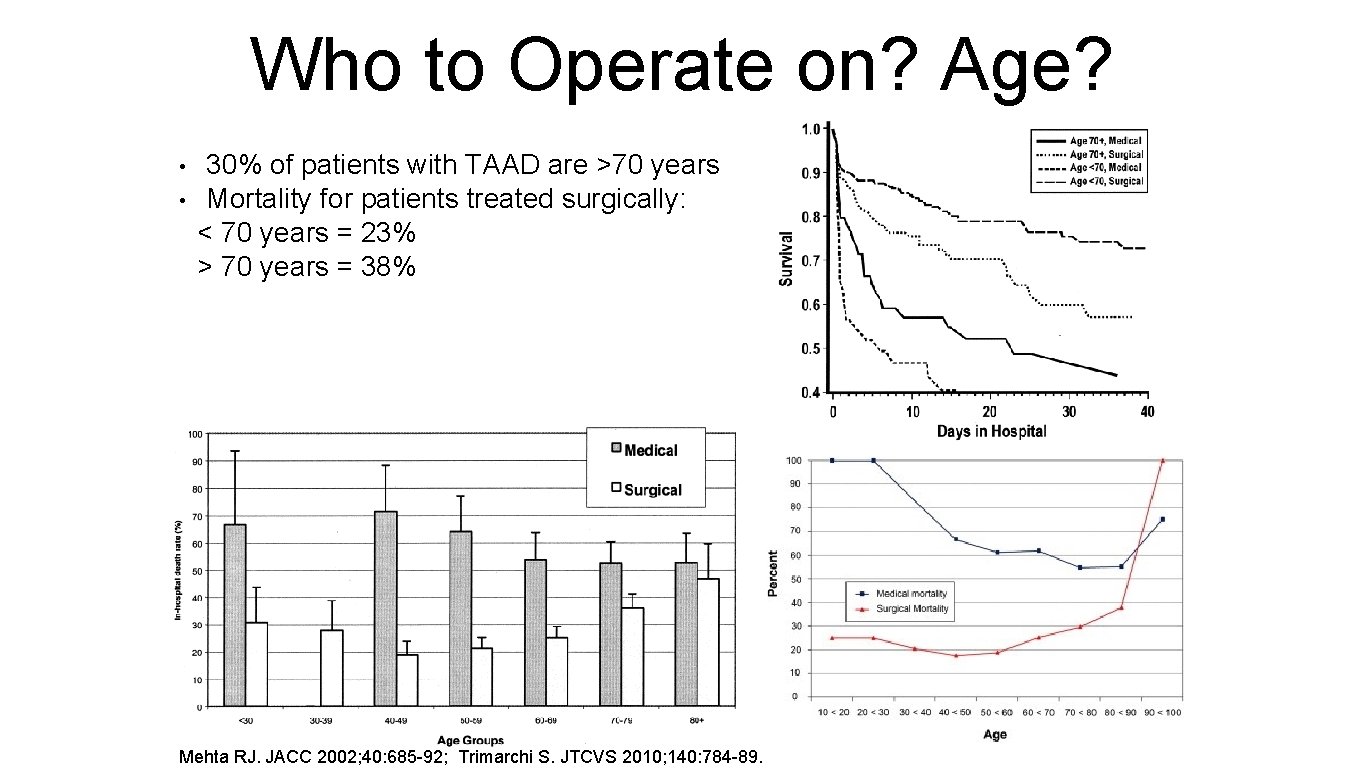
Who to Operate on? Age? • • 30% of patients with TAAD are >70 years Mortality for patients treated surgically: < 70 years = 23% > 70 years = 38% Mehta RJ. JACC 2002; 40: 685 -92; Trimarchi S. JTCVS 2010; 140: 784 -89.
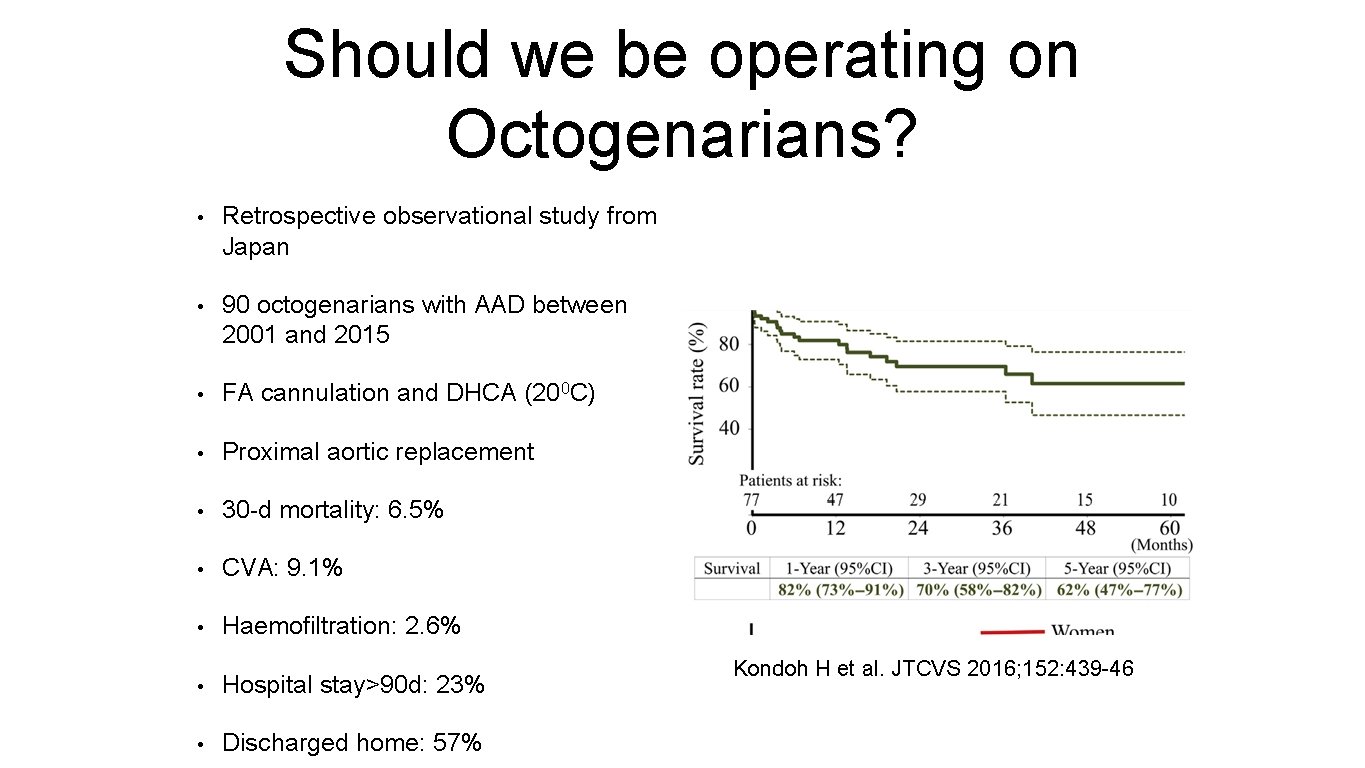
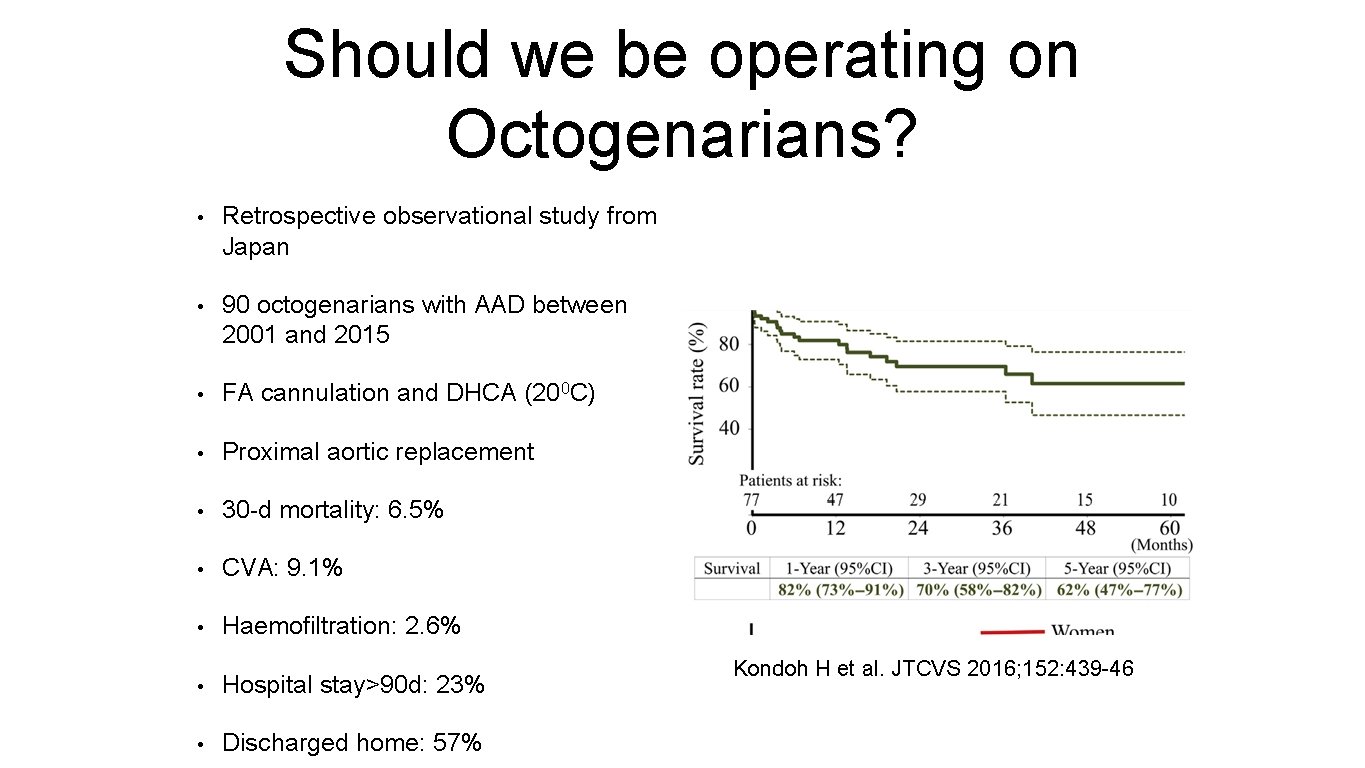
Should we be operating on Octogenarians? • Retrospective observational study from Japan • 90 octogenarians with AAD between 2001 and 2015 • FA cannulation and DHCA (200 C) • Proximal aortic replacement • 30 -d mortality: 6. 5% • CVA: 9. 1% • Haemofiltration: 2. 6% • Hospital stay>90 d: 23% • Discharged home: 57% Kondoh H et al. JTCVS 2016; 152: 439 -46
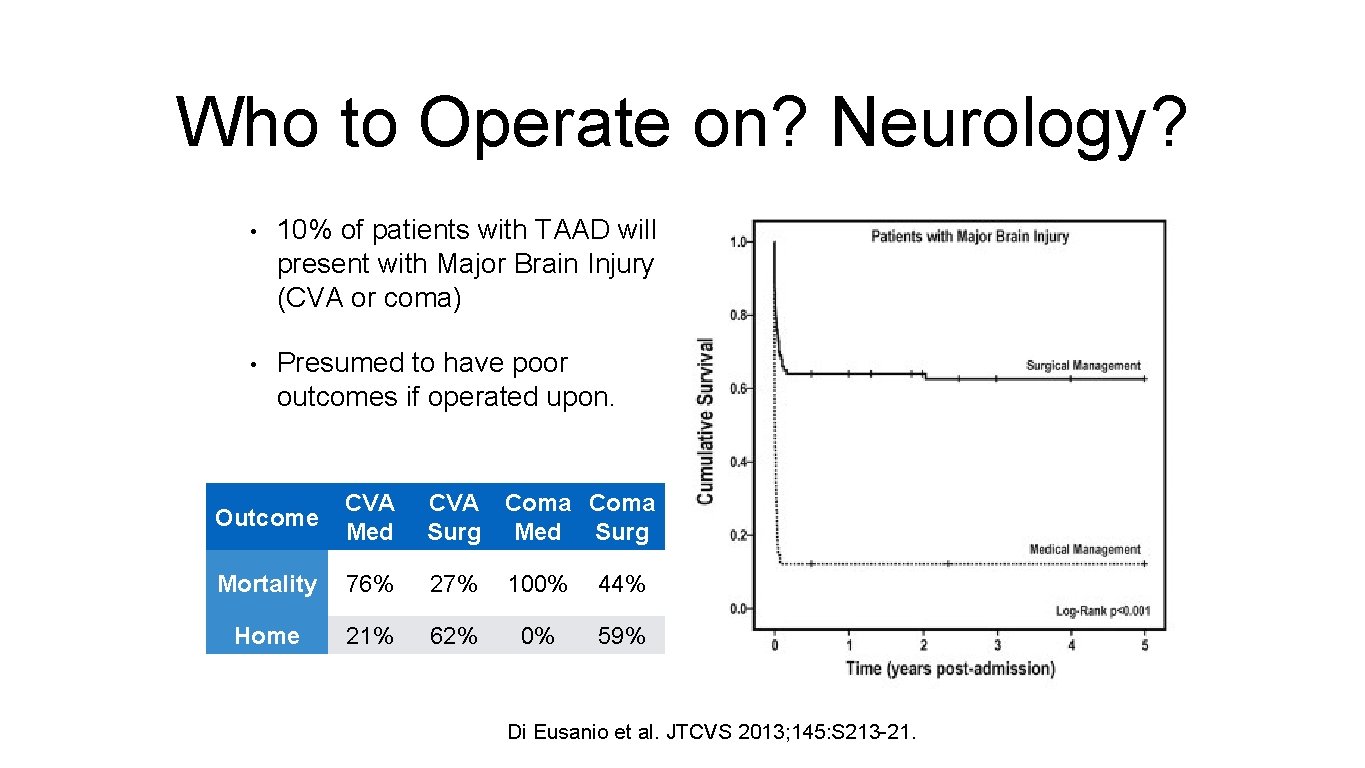
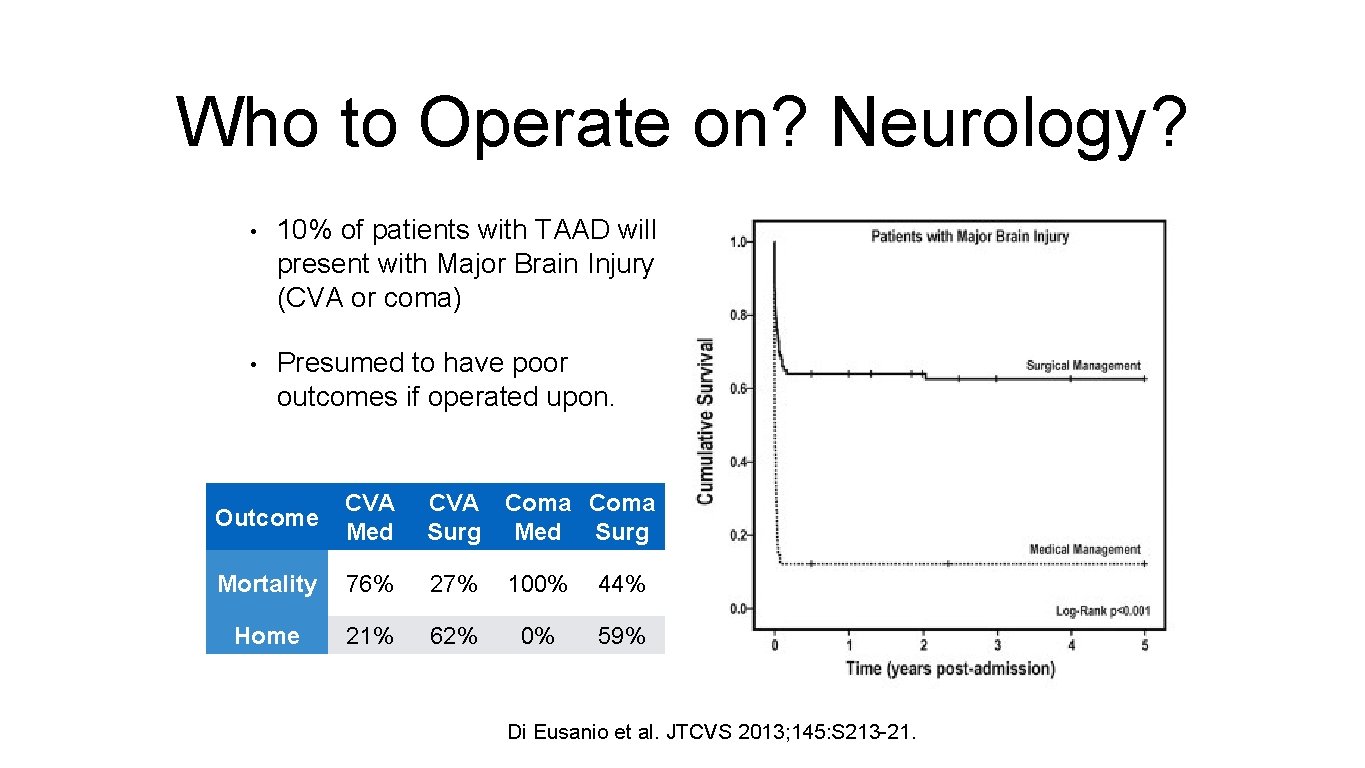
Who to Operate on? Neurology? • 10% of patients with TAAD will present with Major Brain Injury (CVA or coma) • Presumed to have poor outcomes if operated upon. Outcome CVA Med CVA Coma Surg Med Surg Mortality 76% 27% 100% 44% Home 21% 62% 0% 59% Di Eusanio et al. JTCVS 2013; 145: S 213 -21.

Timing of Surgery • Emergency surgery in all patients • Mortality rate = 1 -2% per hour • In IRAD database, median time from presentation at ED to diagnosis = 4 hrs • Median time from diagnosis to surgery = 4 hrs
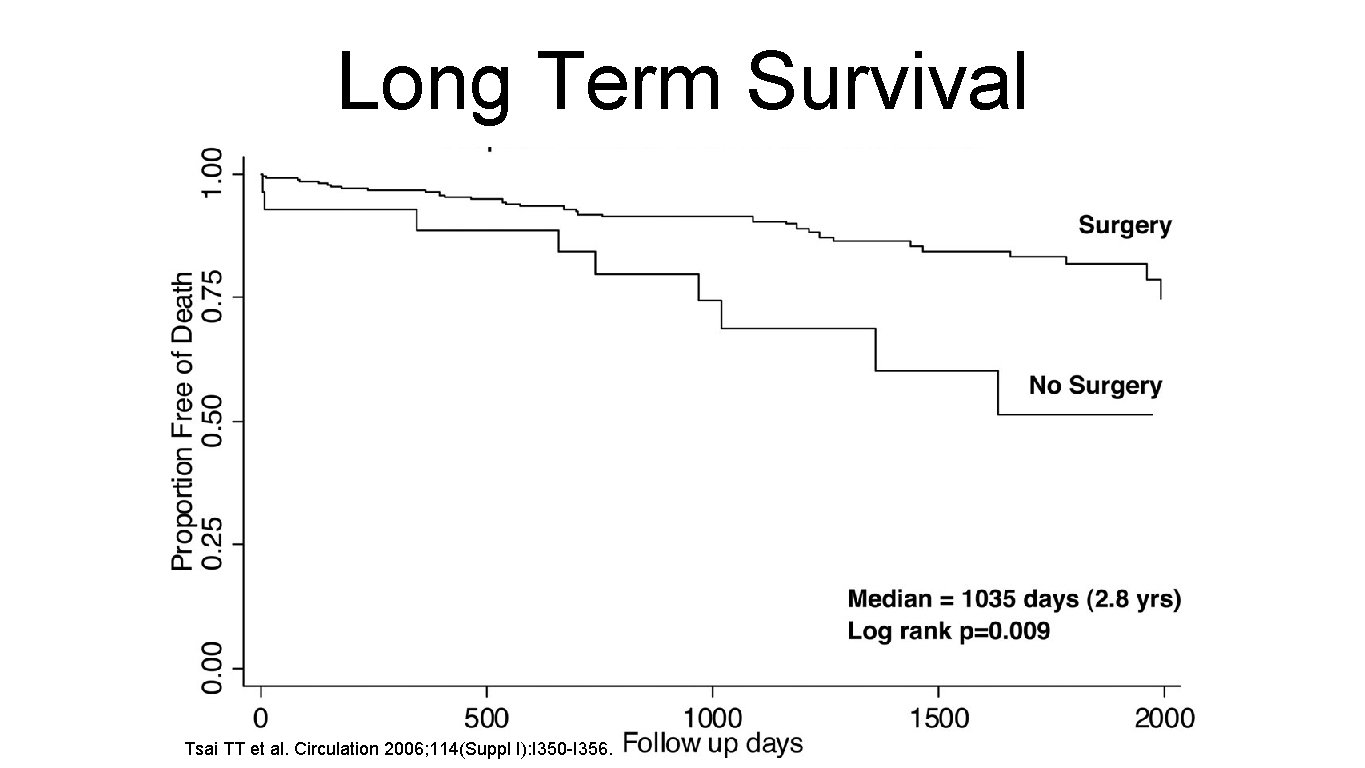
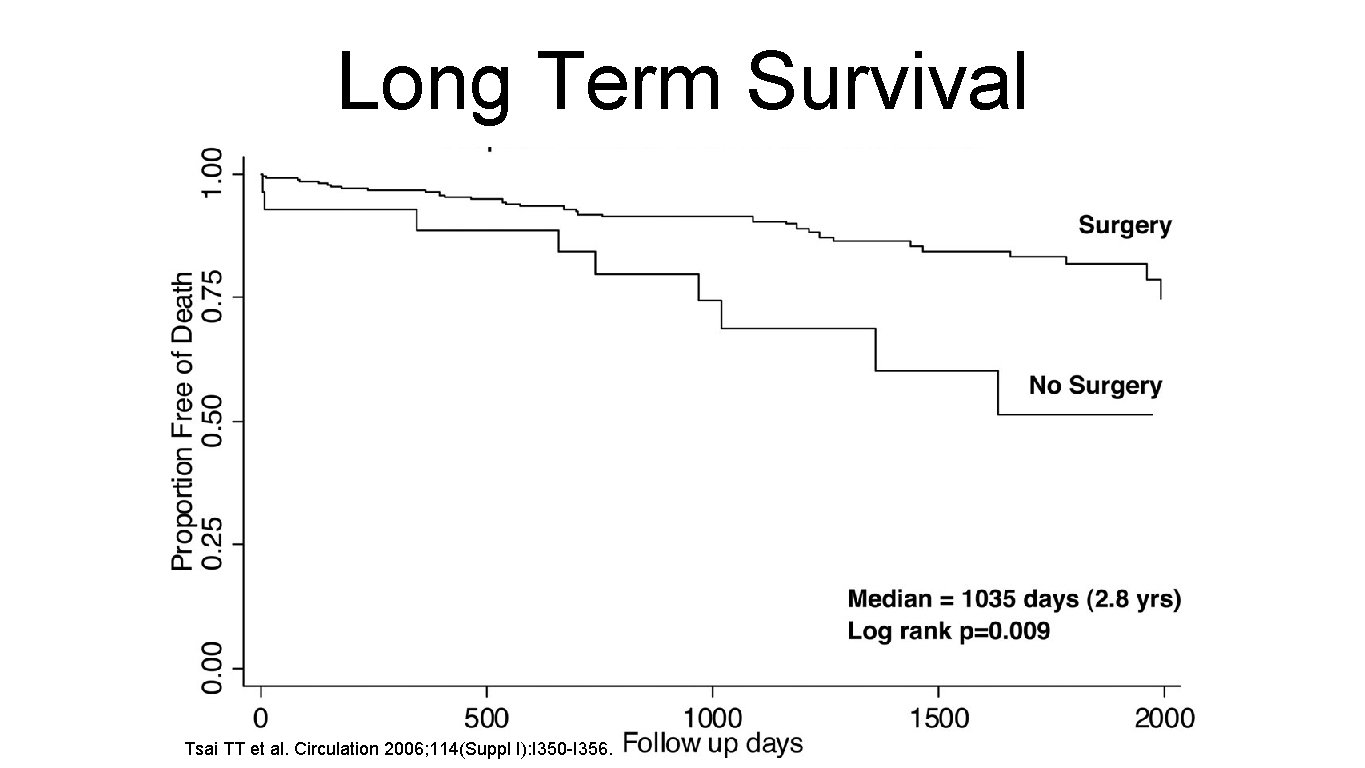
Long Term Survival Tsai TT et al. Circulation 2006; 114(Suppl I): I 350 -I 356.
Aortic Intramural Haematoma
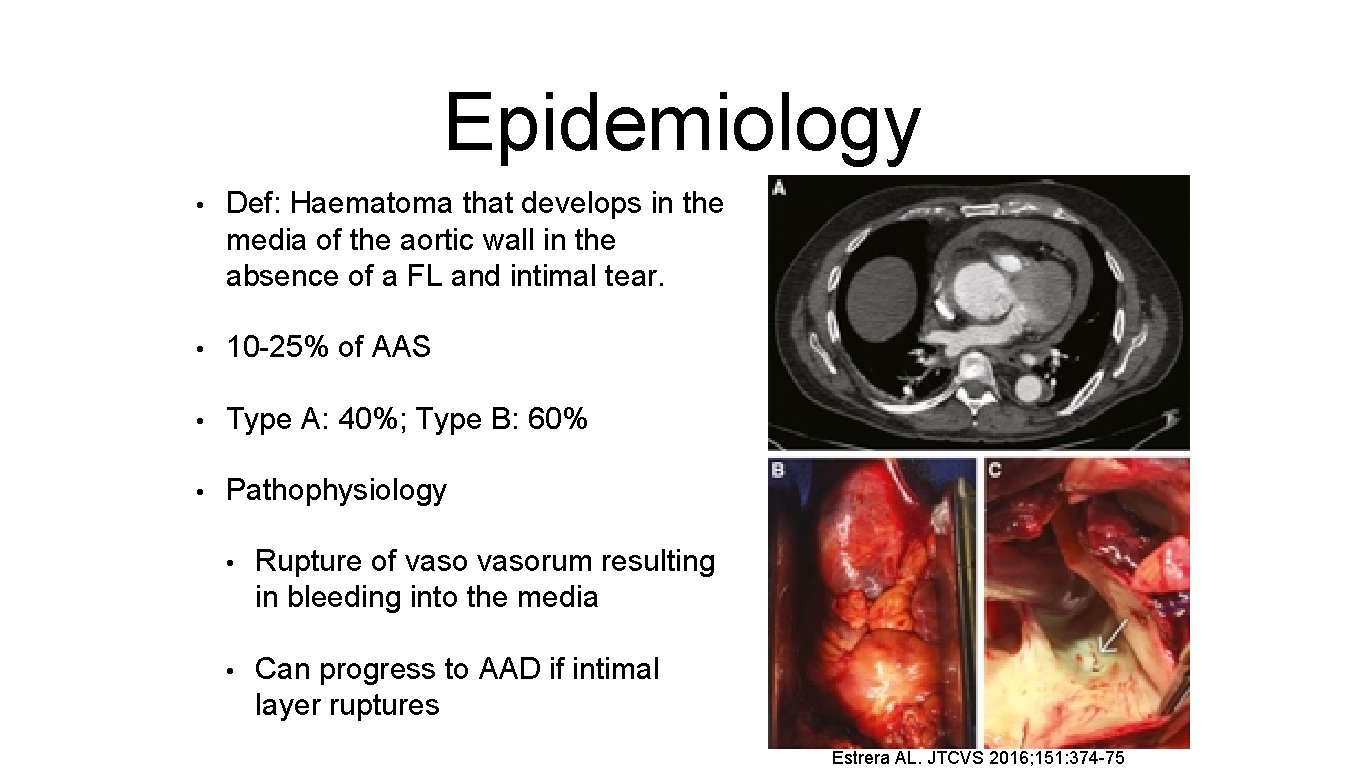
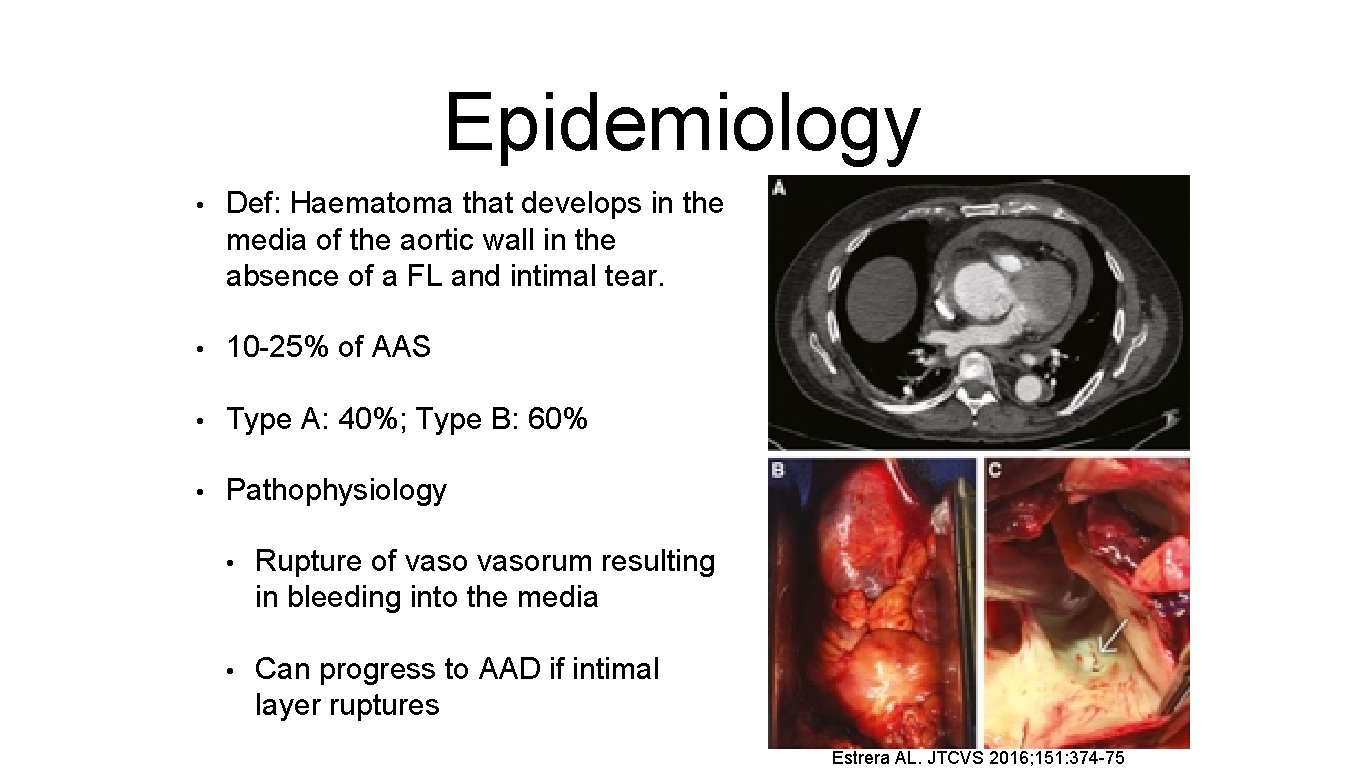
Epidemiology • Def: Haematoma that develops in the media of the aortic wall in the absence of a FL and intimal tear. • 10 -25% of AAS • Type A: 40%; Type B: 60% • Pathophysiology • Rupture of vasorum resulting in bleeding into the media • Can progress to AAD if intimal layer ruptures Estrera AL. JTCVS 2016; 151: 374 -75
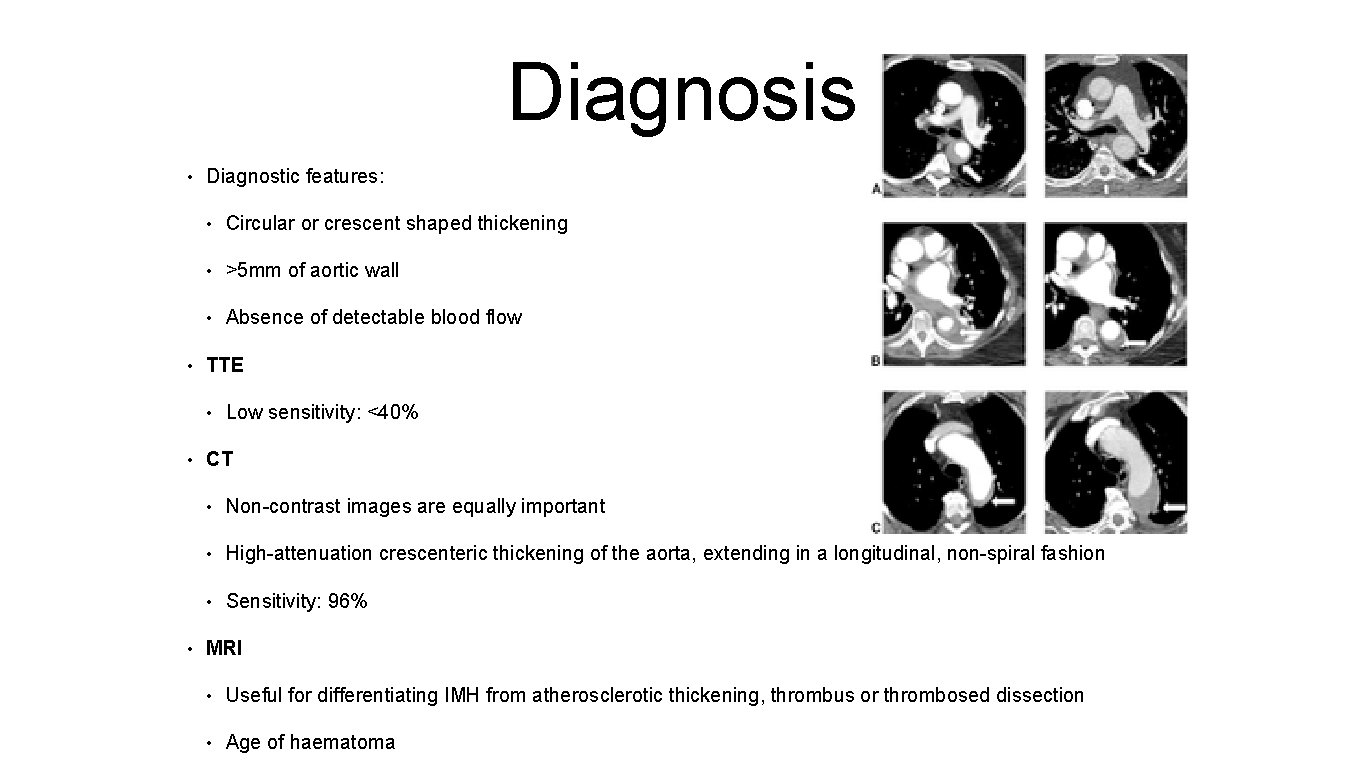
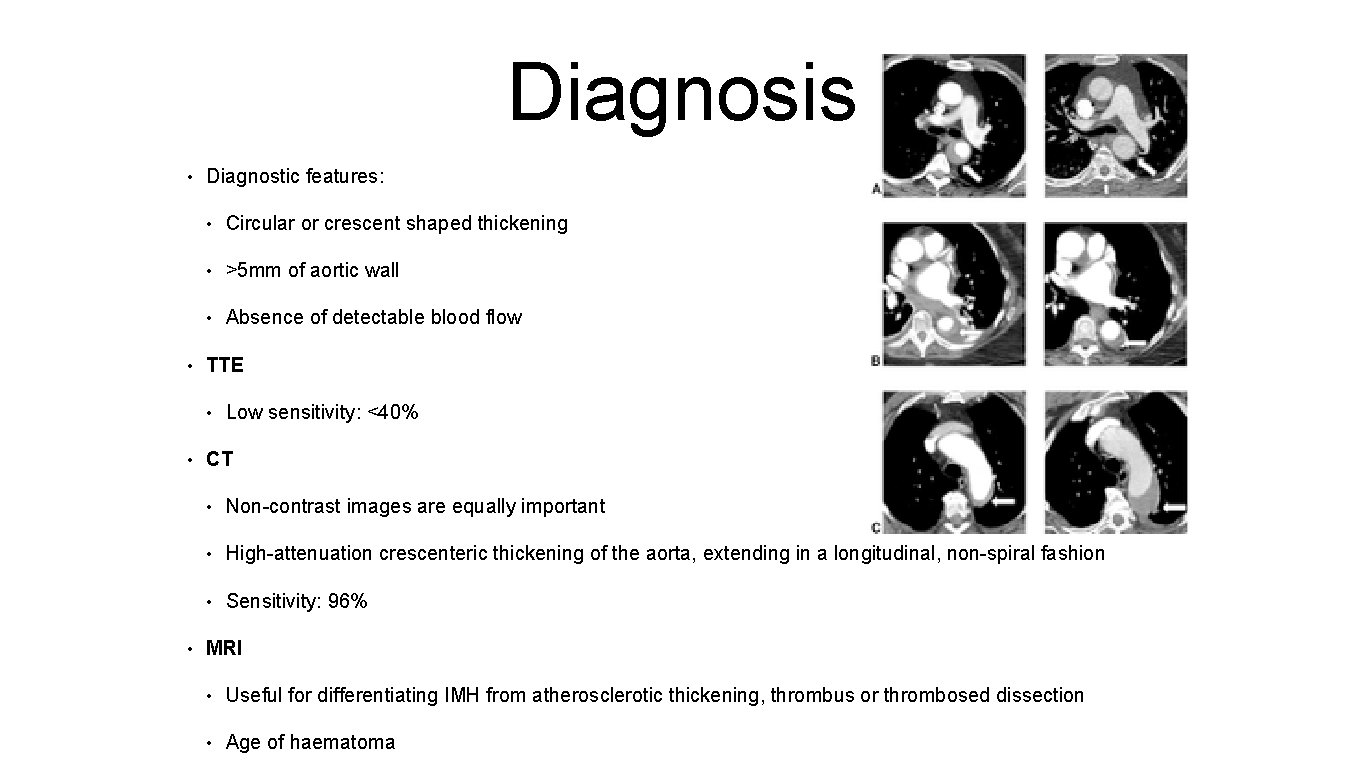
Diagnosis • • Diagnostic features: • Circular or crescent shaped thickening • >5 mm of aortic wall • Absence of detectable blood flow TTE • • • Low sensitivity: <40% CT • Non-contrast images are equally important • High-attenuation crescenteric thickening of the aorta, extending in a longitudinal, non-spiral fashion • Sensitivity: 96% MRI • Useful for differentiating IMH from atherosclerotic thickening, thrombus or thrombosed dissection • Age of haematoma

Natural History • Mortality rates in medically treated patients in European and North American studies are high compared to Asian studies • Progression to dissection and/or rupture • Affects older patients • Patients more likely to present with pericardial effusions Chou AS et al. JTCVS 2016; 151: 361 -73.
IRAD Data • IRAD: 64 cases of Type A IMH • Older patients: mean age 69. 6 (9. 6) • Similar presentation to AAD • Higher incidence of pericardial effusions (61%) • 15. 6% medical mx; 84. 4% surgical mx. • Overall 30 -day mortality: 26. 6% • Medical Mx: 40% • Surgically Mx: 24. 1% Harris KM et al. Circulation 2012; 126(suppl 1): S 91 -96.
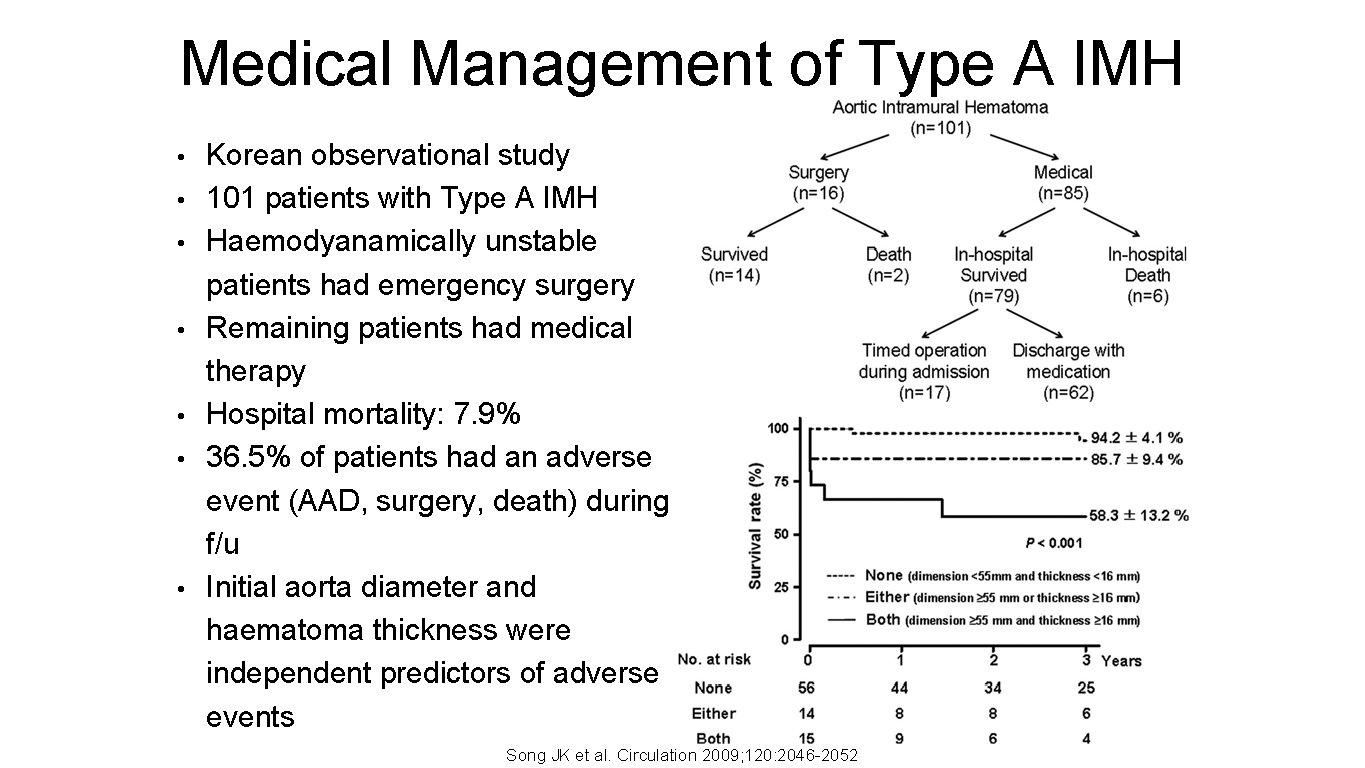
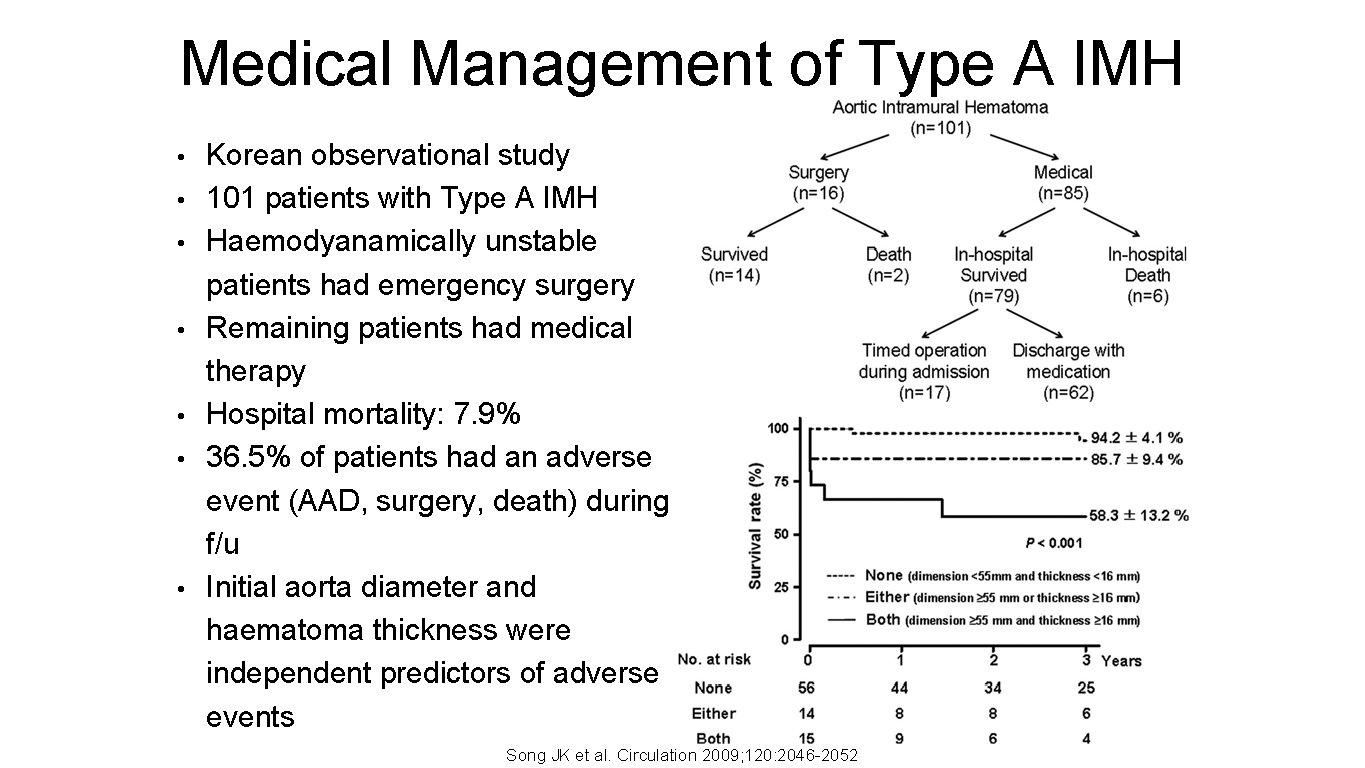
Medical Management of Type A IMH • • Korean observational study 101 patients with Type A IMH Haemodyanamically unstable patients had emergency surgery Remaining patients had medical therapy Hospital mortality: 7. 9% 36. 5% of patients had an adverse event (AAD, surgery, death) during f/u Initial aorta diameter and haematoma thickness were independent predictors of adverse events Song JK et al. Circulation 2009; 120: 2046 -2052
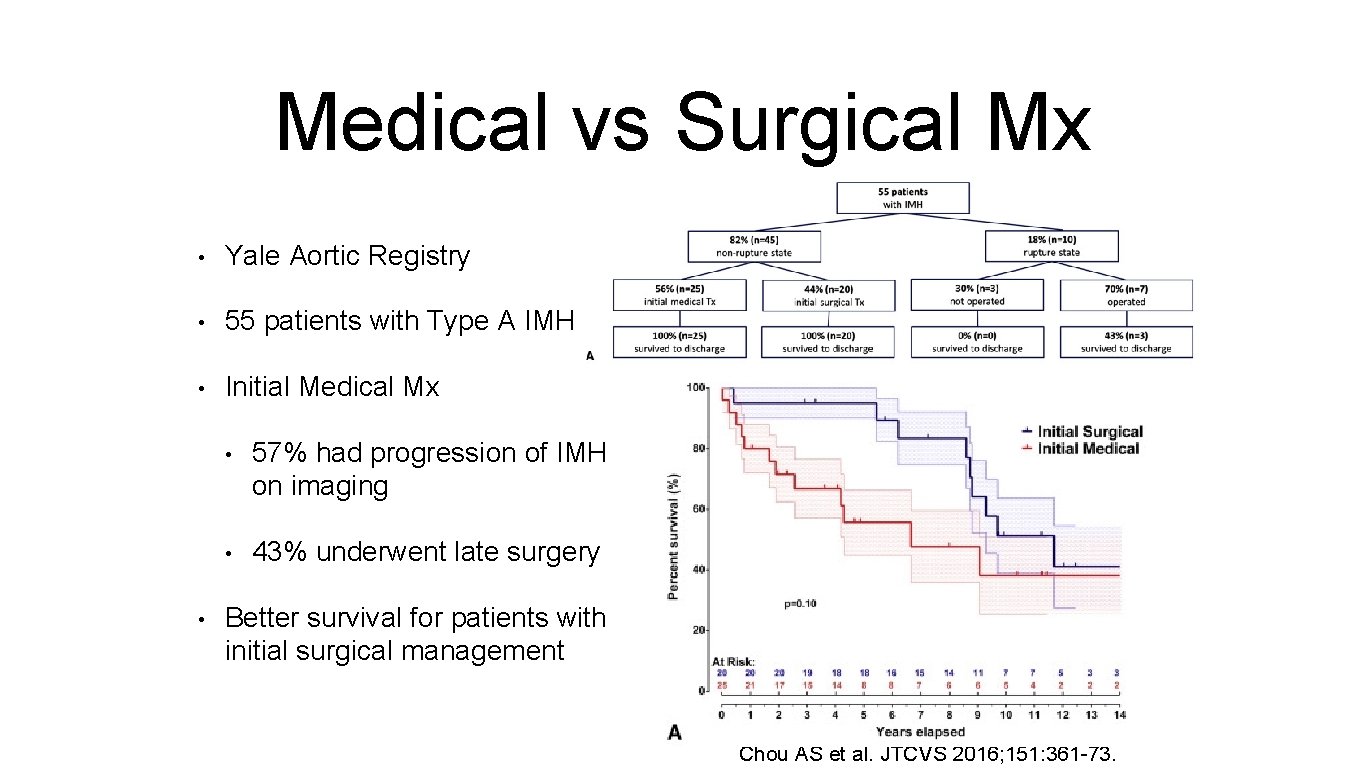
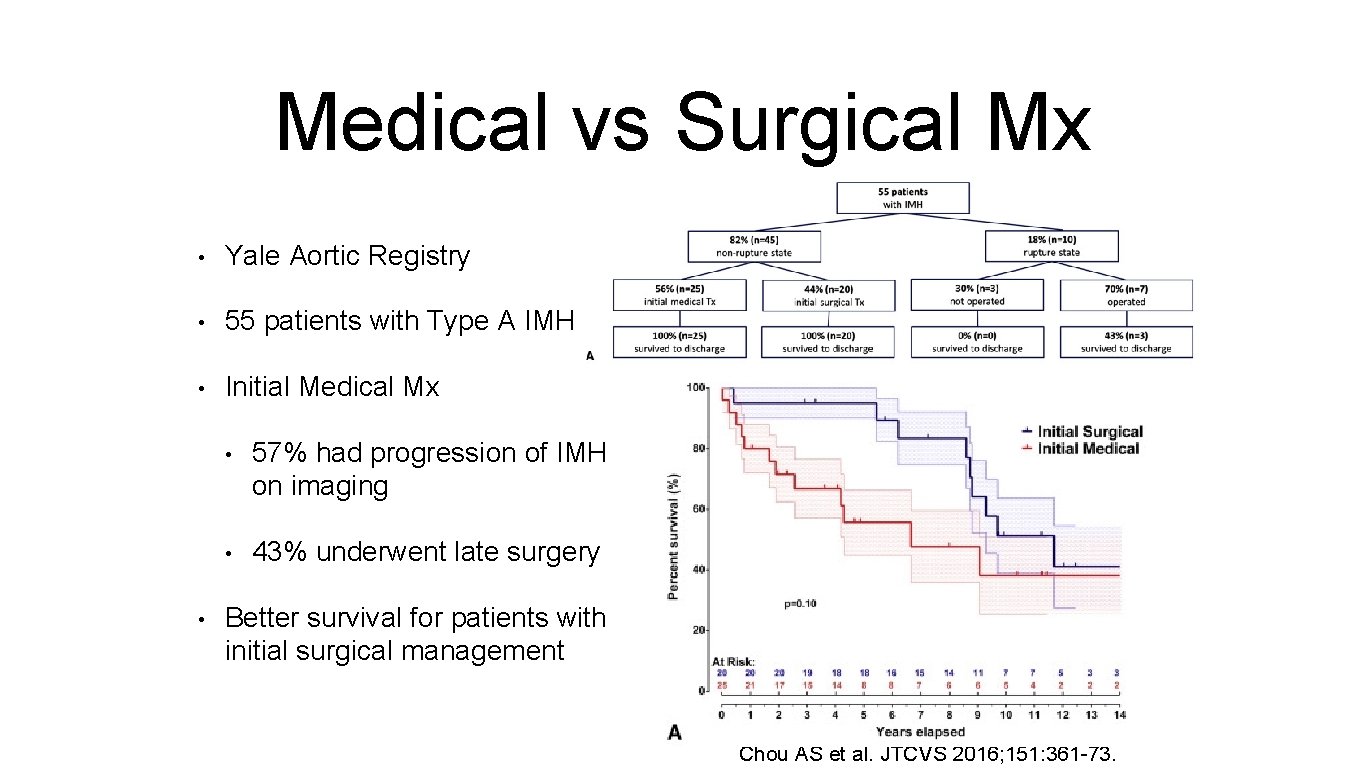
Medical vs Surgical Mx • Yale Aortic Registry • 55 patients with Type A IMH • Initial Medical Mx • • 57% had progression of IMH on imaging • 43% underwent late surgery Better survival for patients with initial surgical management Chou AS et al. JTCVS 2016; 151: 361 -73.
ESC 2014 Guidelines • Emergency surgery: Evidence of rupture • Pericardial effusion • Urgent surgery (<24 hrs): Most Type A IMH • Elderly pt with comorbidities • + Aortic diameter <50 mm and IMH thickness <11 mm • Initial Medical Tx (BP and pain control and imaging)

Penetrating Aortic Ulcer

Epidemiology • Def: ulceration of an aortic atherosclerotic plaque penetrating through the internal elastic lamina into the media. • May lead to IMH, pseudoaneurysm, AD, rupture • 2 -7% of all AAS • Elderly, male, smokers with CAD or COPD • Affects descending aorta commonly • Management as for Type A IMH Chou AS et al. JTCVS 2016; 151: 361 -73.

Penetrating Aortic Ulcer

Operative Strategy
Pre-Operative Strategy • BP Control: IV Labetalol or GTN • Identify any end-organ damage: limbs, CNS, urine output/creatinine, • Impending rupture: pericardial or pleural blood • Feel femoral pulses • Xmatch blood
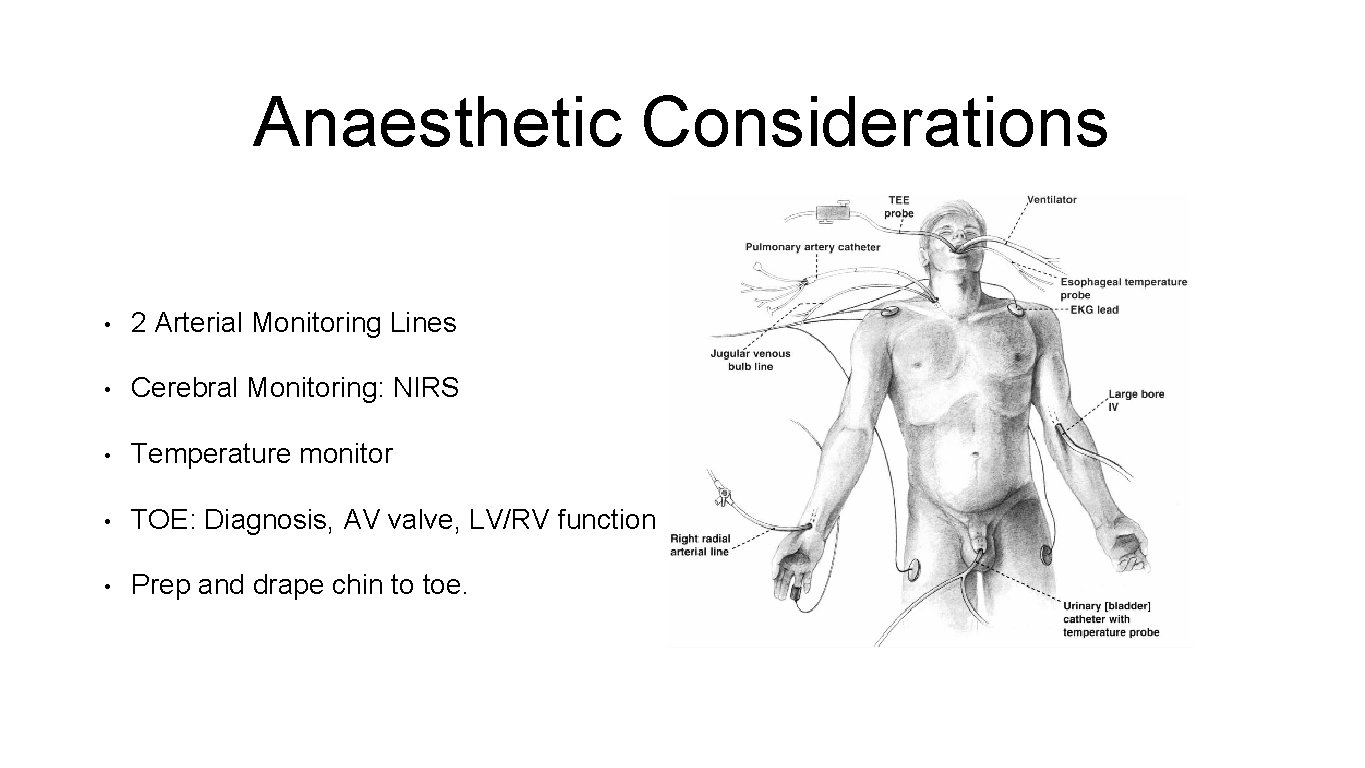
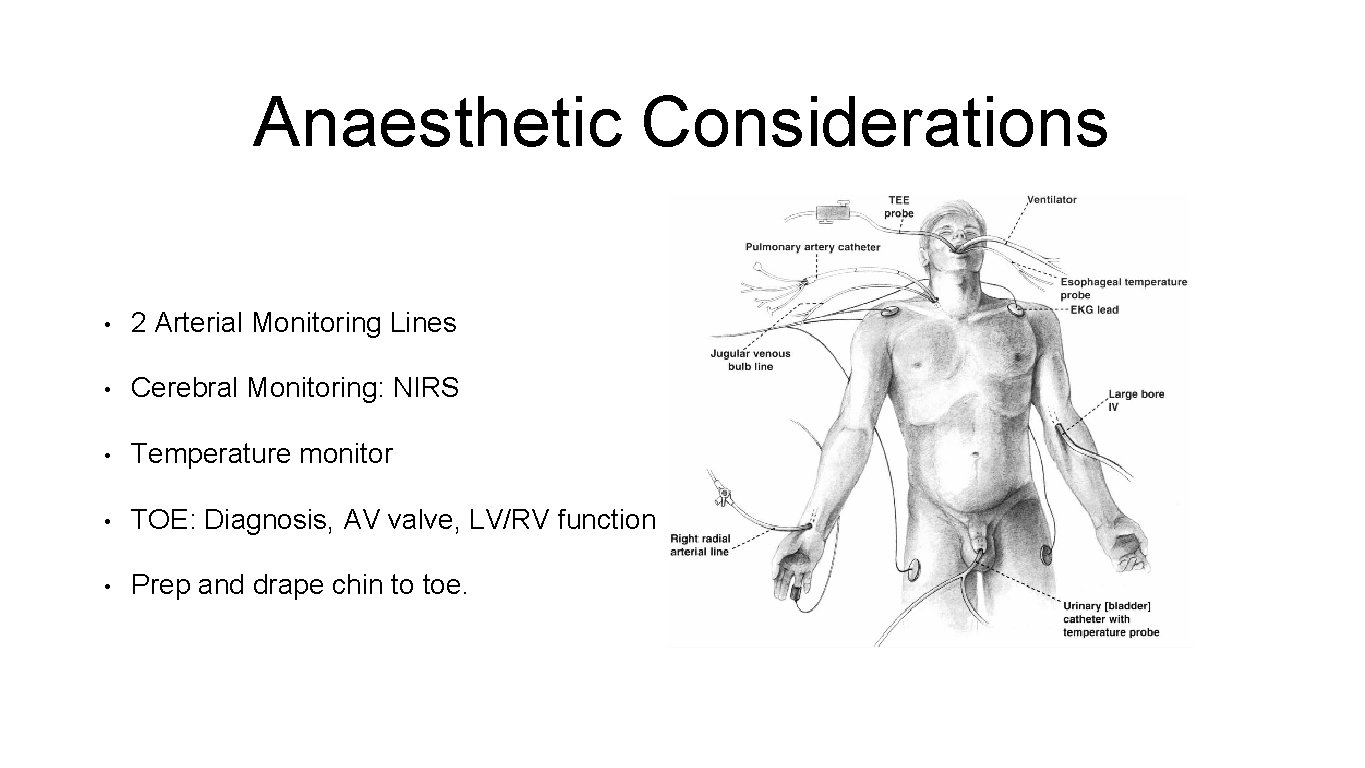
Anaesthetic Considerations • 2 Arterial Monitoring Lines • Cerebral Monitoring: NIRS • Temperature monitor • TOE: Diagnosis, AV valve, LV/RV function • Prep and drape chin to toe.
Operative Strategy • Safe Sternal Entry • CPB - aortic cannulation site • Myocardial protection • Managing the Root/Valve, Ascending Aorta, Arch • Cerebral Protection
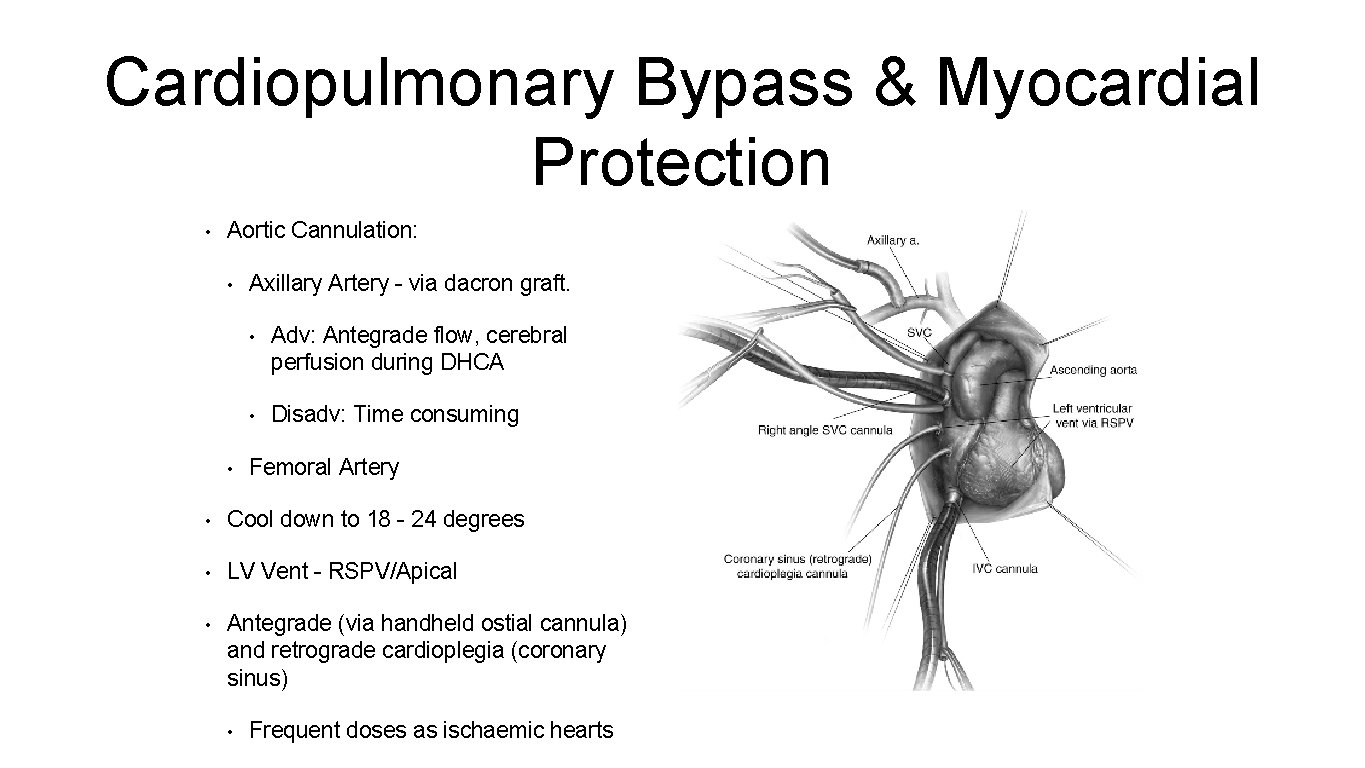
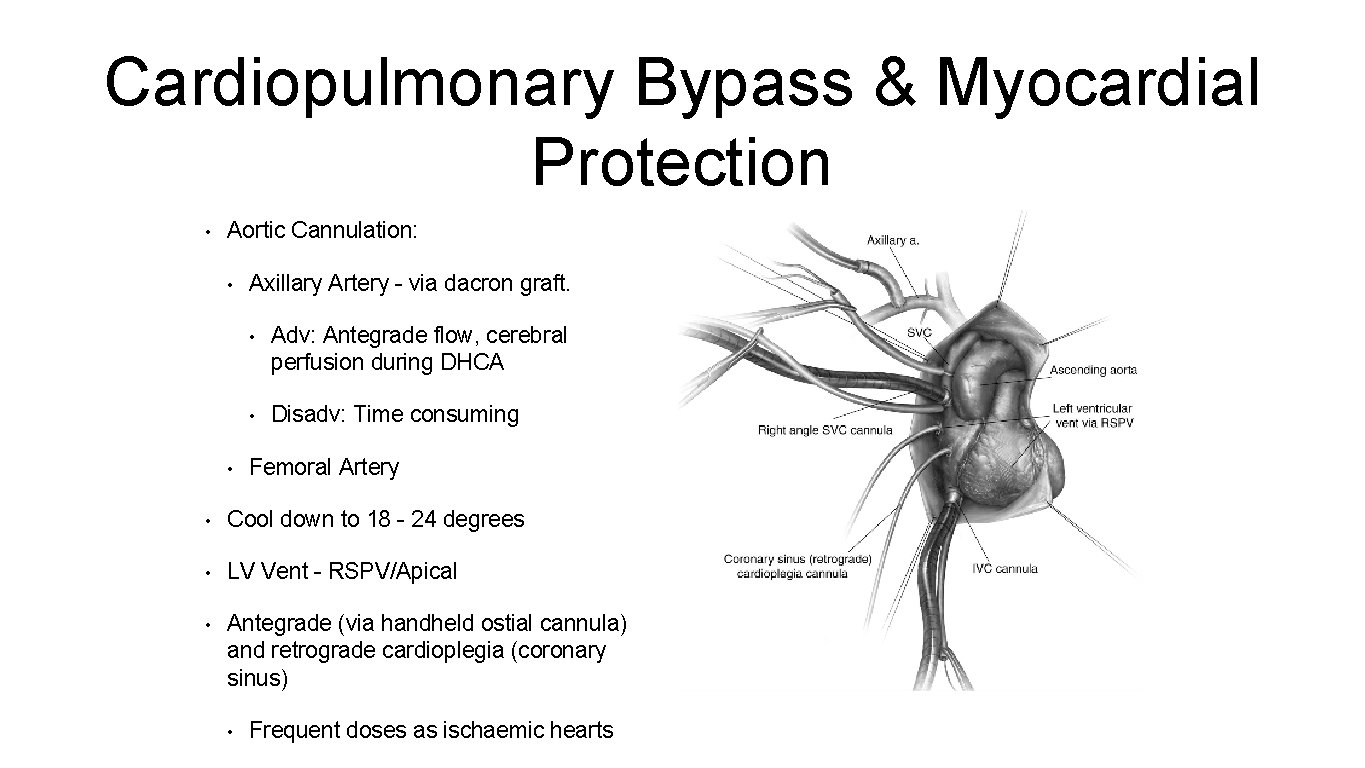
Cardiopulmonary Bypass & Myocardial Protection • Aortic Cannulation: • • Axillary Artery - via dacron graft. • Adv: Antegrade flow, cerebral perfusion during DHCA • Disadv: Time consuming Femoral Artery • Cool down to 18 - 24 degrees • LV Vent - RSPV/Apical • Antegrade (via handheld ostial cannula) and retrograde cardioplegia (coronary sinus) • Frequent doses as ischaemic hearts
Cerebral Protection • HCA – deep vs moderate • HCA + RCP • HCA + ACP • Definitions of HCA • Profound Hypothermia: ≤ 140 C • Deep Hypothermia: 14. 1 – 200 C • Moderate Hypothermia: 20. 1 – 280 C • Mild Hypothermia: 28. 1 - 340 C

Hypothermia
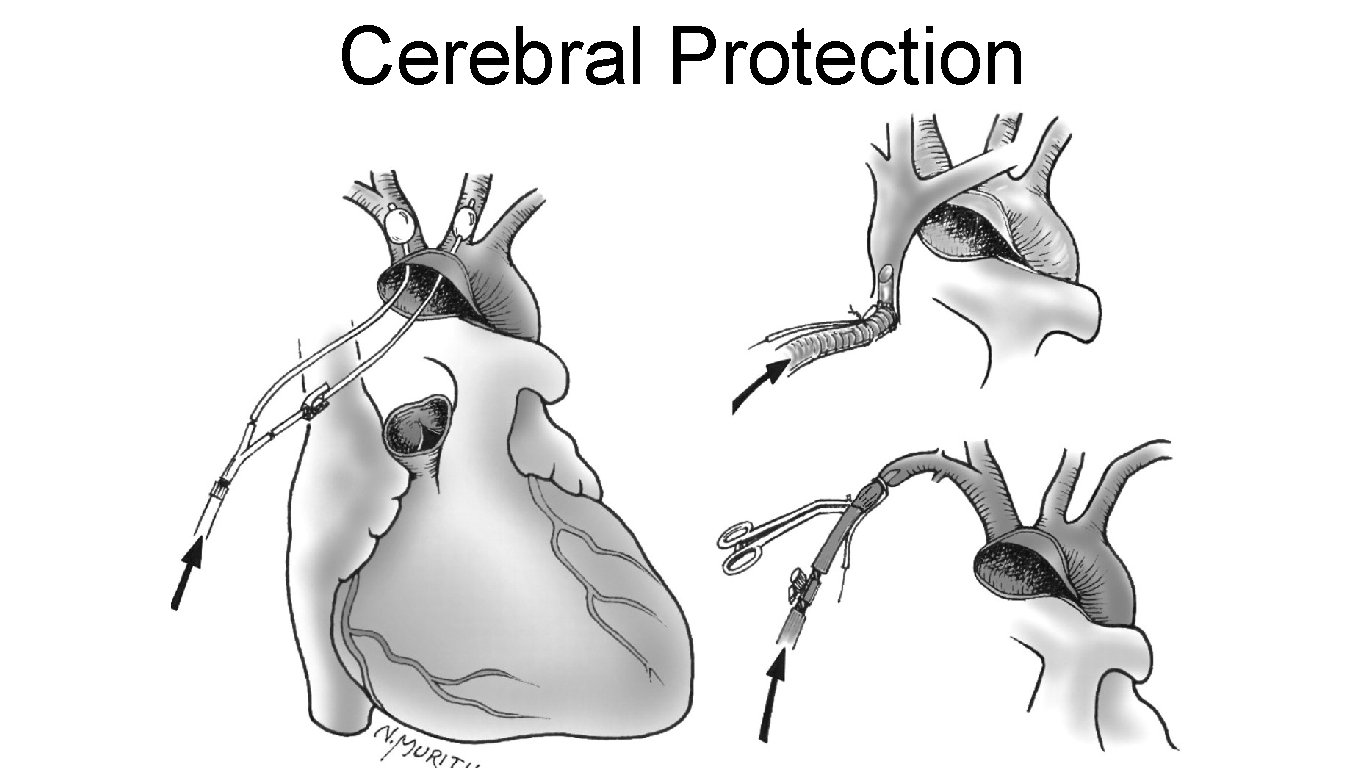
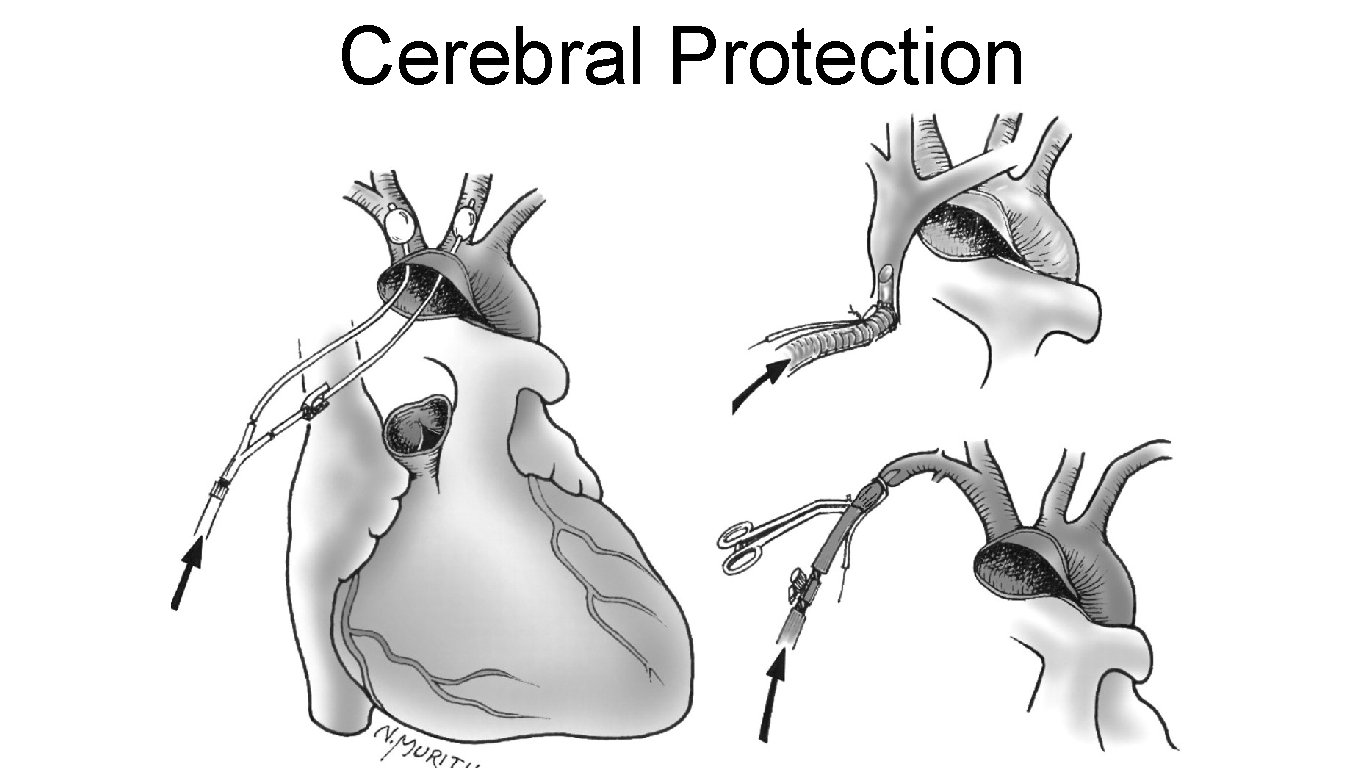
Cerebral Protection
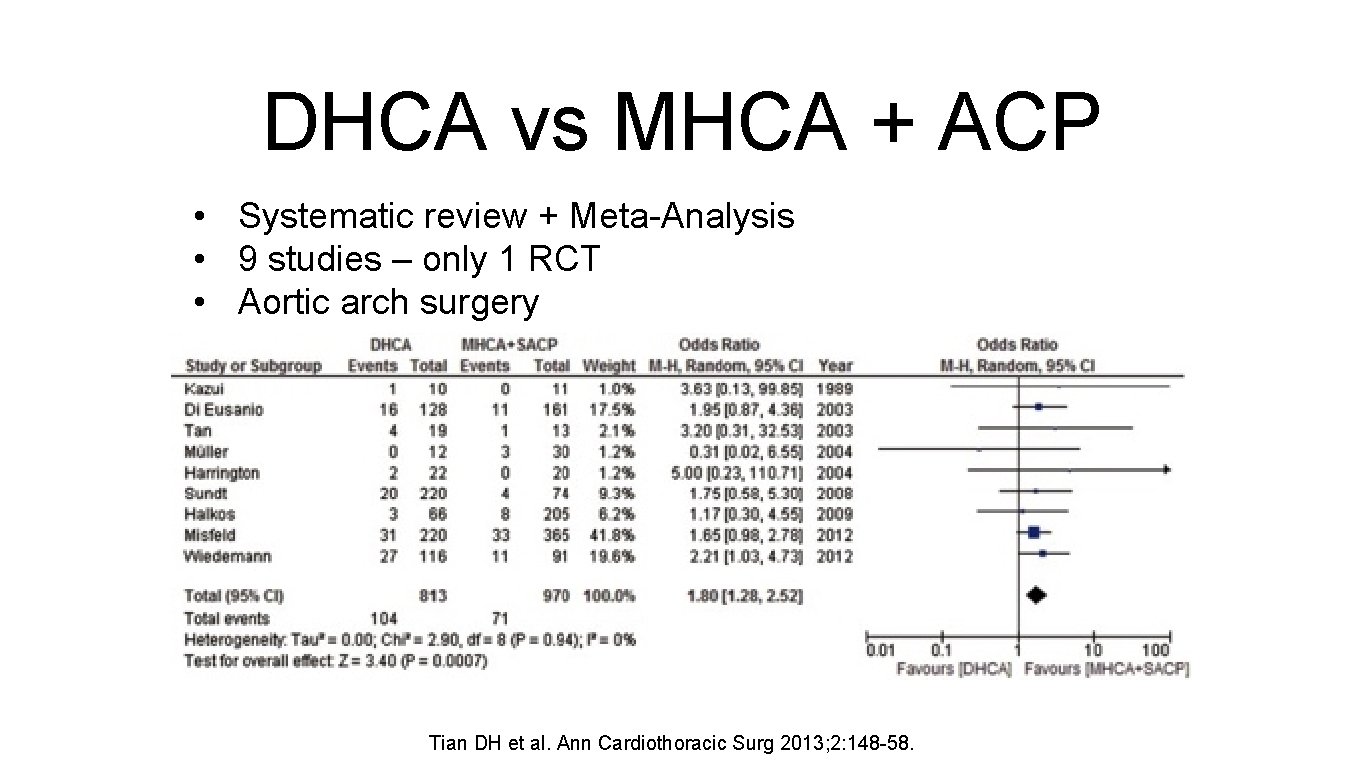
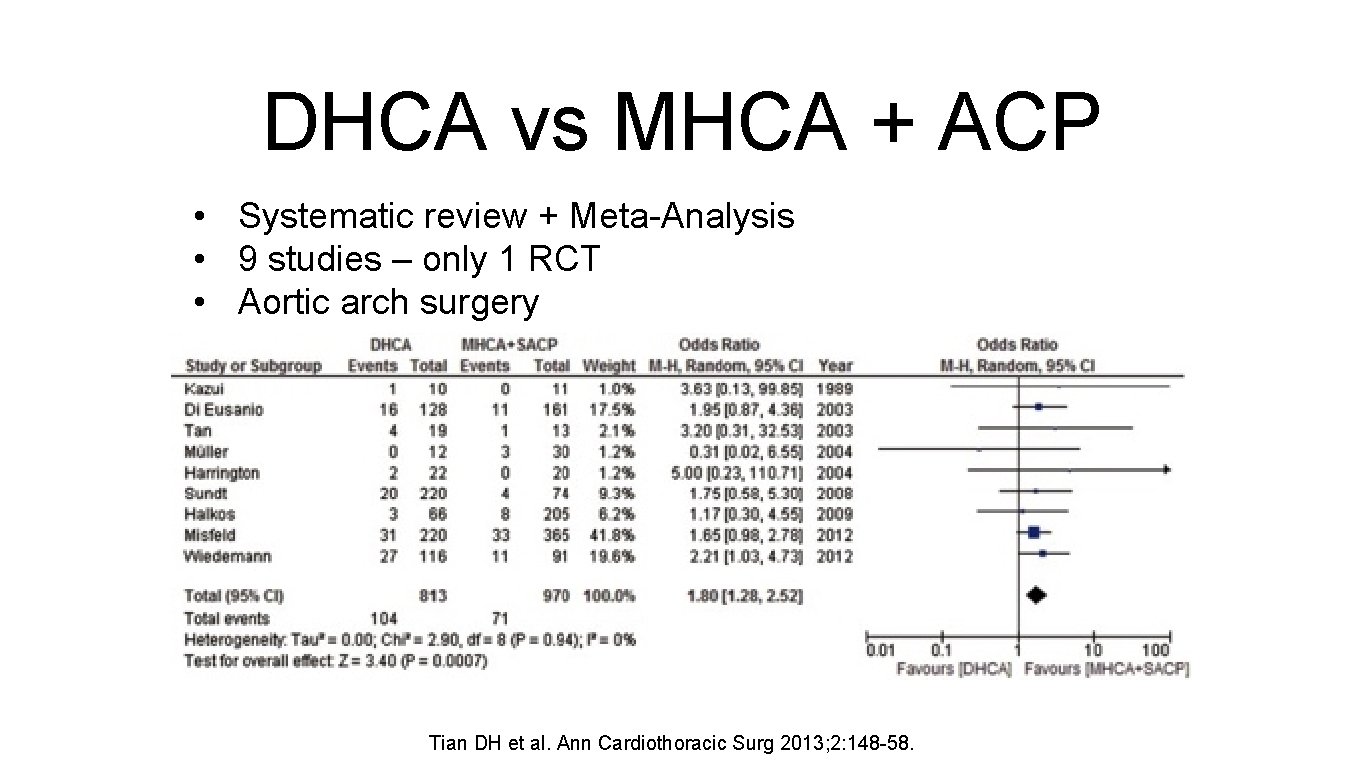
DHCA vs MHCA + ACP • Systematic review + Meta-Analysis • 9 studies – only 1 RCT • Aortic arch surgery Tian DH et al. Ann Cardiothoracic Surg 2013; 2: 148 -58.

Ascending Aorta Only No AR, 70 -85% of cases Morton Bolmon R. Op Tech Thor Card Vasc Surg 2009.
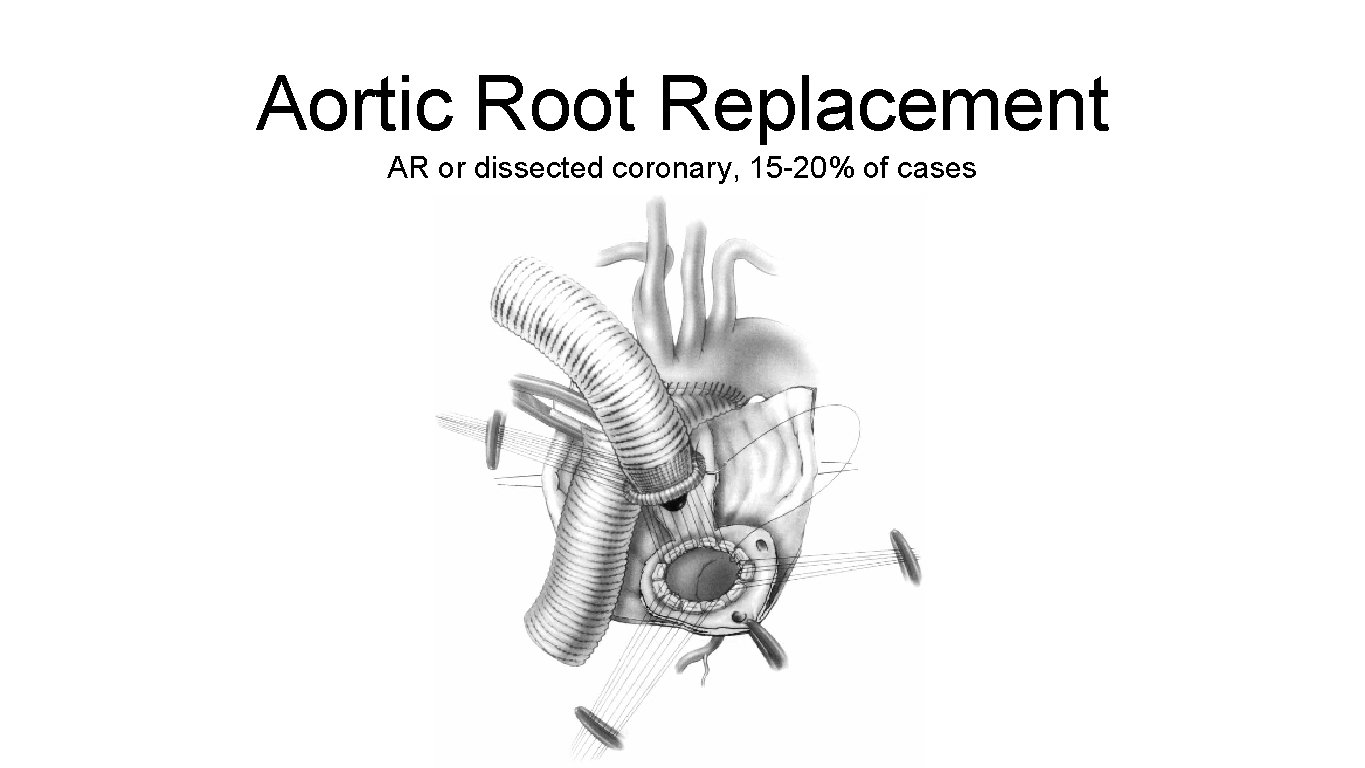
Aortic Root Replacement AR or dissected coronary, 15 -20% of cases

Arch Replacement 5 -10% of cases
Operative Principles • Reinforce dissected tissues with teflon • Always look into the arch for another tear using DHCA • Complete the distal anastomosis using DHCA • Lots of cardioplegia • Protect the brain with ACP
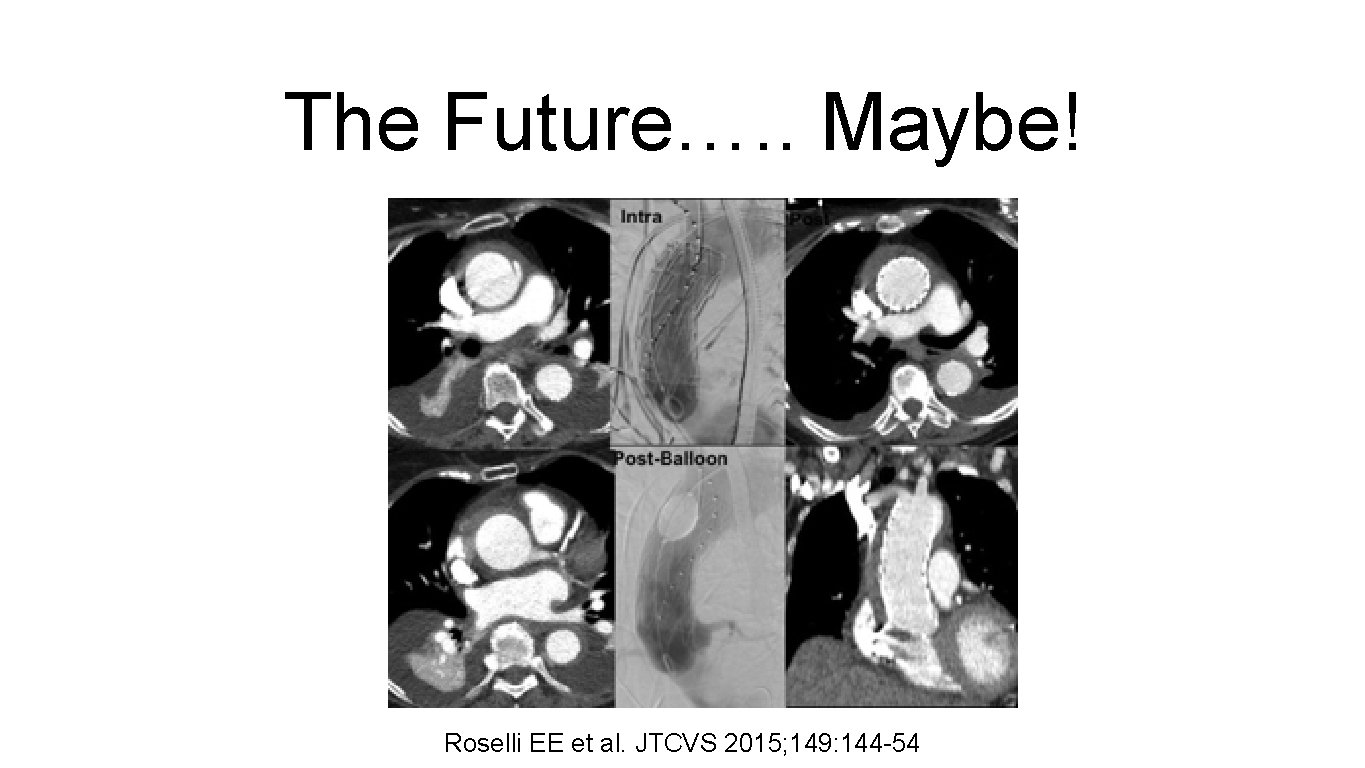
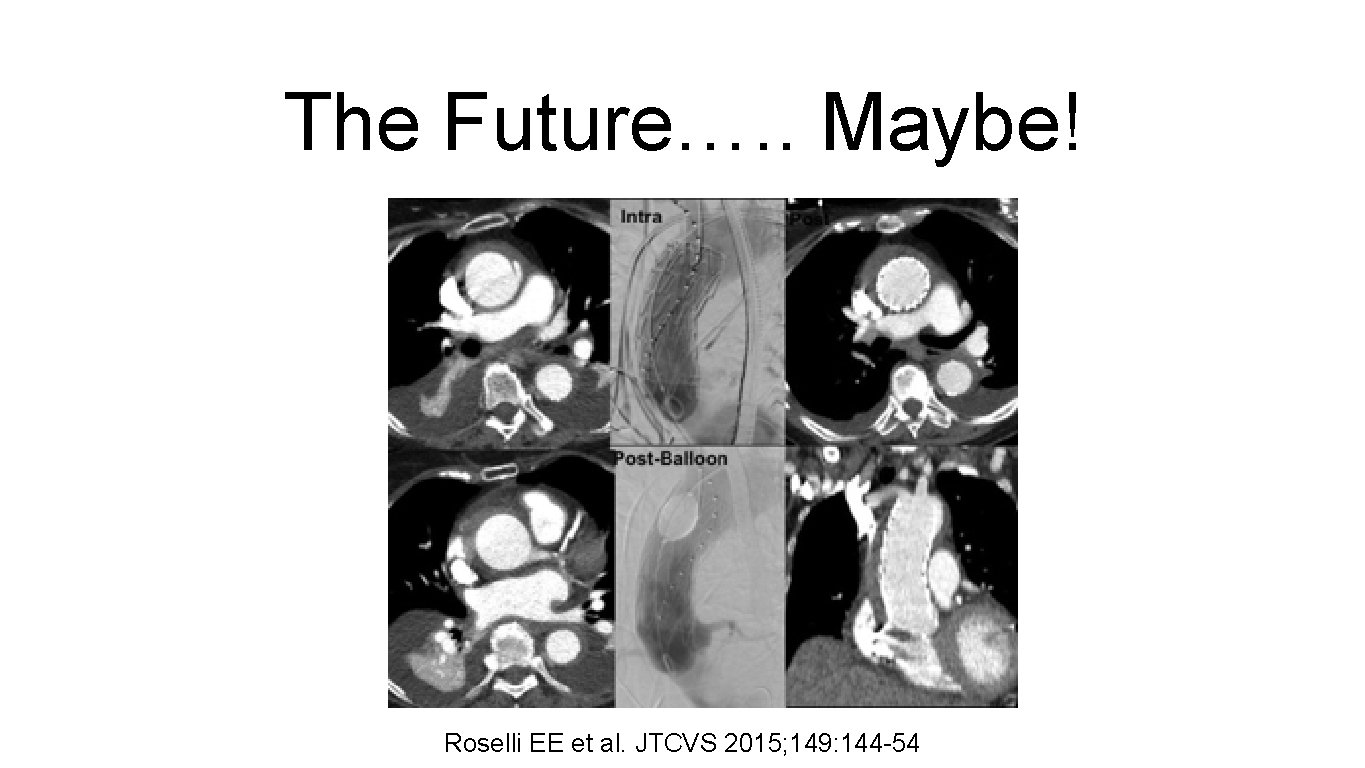
The Future…. . Maybe! Roselli EE et al. JTCVS 2015; 149: 144 -54

Di. Re. CTion trial Distal aortic Repair versus Conservative surgery in Type A Aortic Dissection NIHR HTA Application Round 1 Passed
Background • Type A AAD – Incidence in UK: 4. 3 per 100 000 per year – Operative mortality: 20 -25% – Most patients have surgery restricted to ascending aorta (conservative surgery) • Survivors of surgical repair – Patent false lumen: 60 -70% of patients – Further surgery: 20 -40% of patients – 10 year survival: 40 -50% – Require long term surveillance
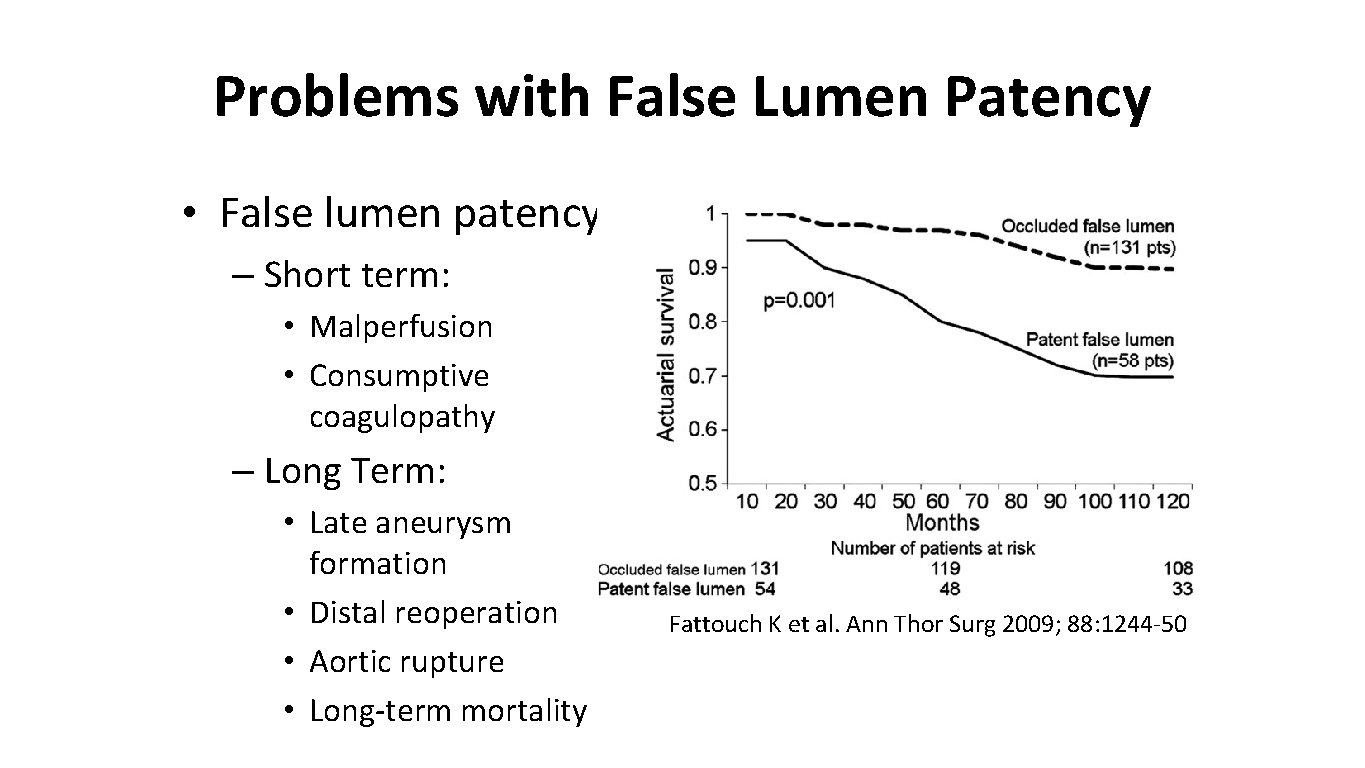
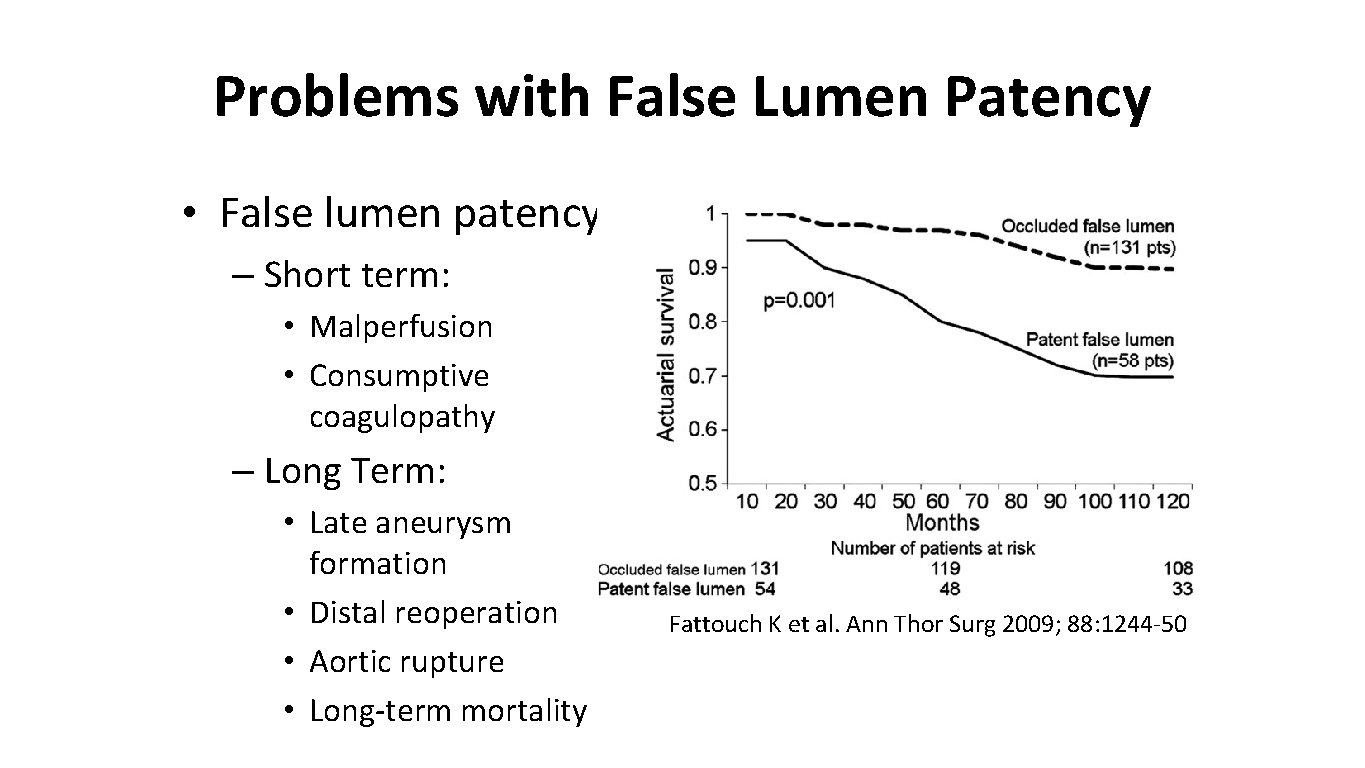
Problems with False Lumen Patency • False lumen patency – Short term: • Malperfusion • Consumptive coagulopathy – Long Term: • Late aneurysm formation • Distal reoperation • Aortic rupture • Long-term mortality Fattouch K et al. Ann Thor Surg 2009; 88: 1244 -50
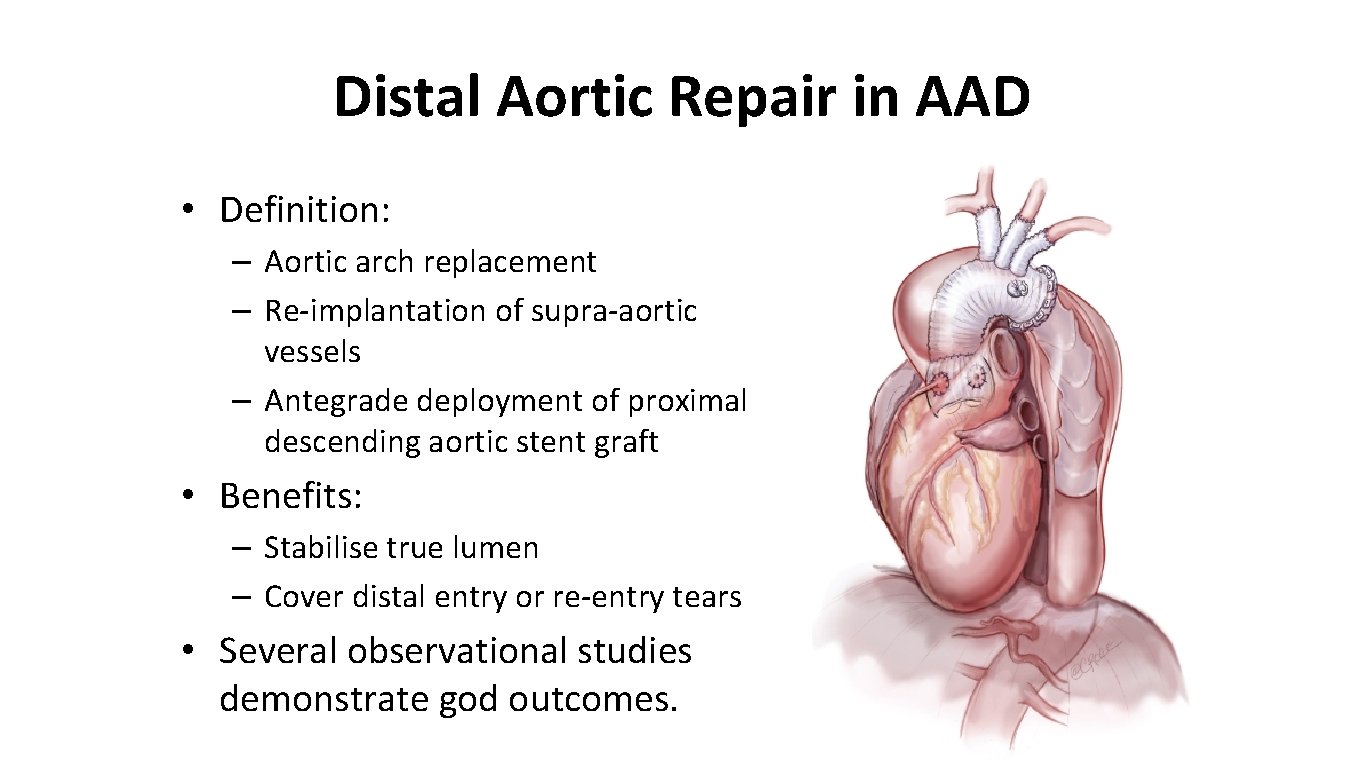
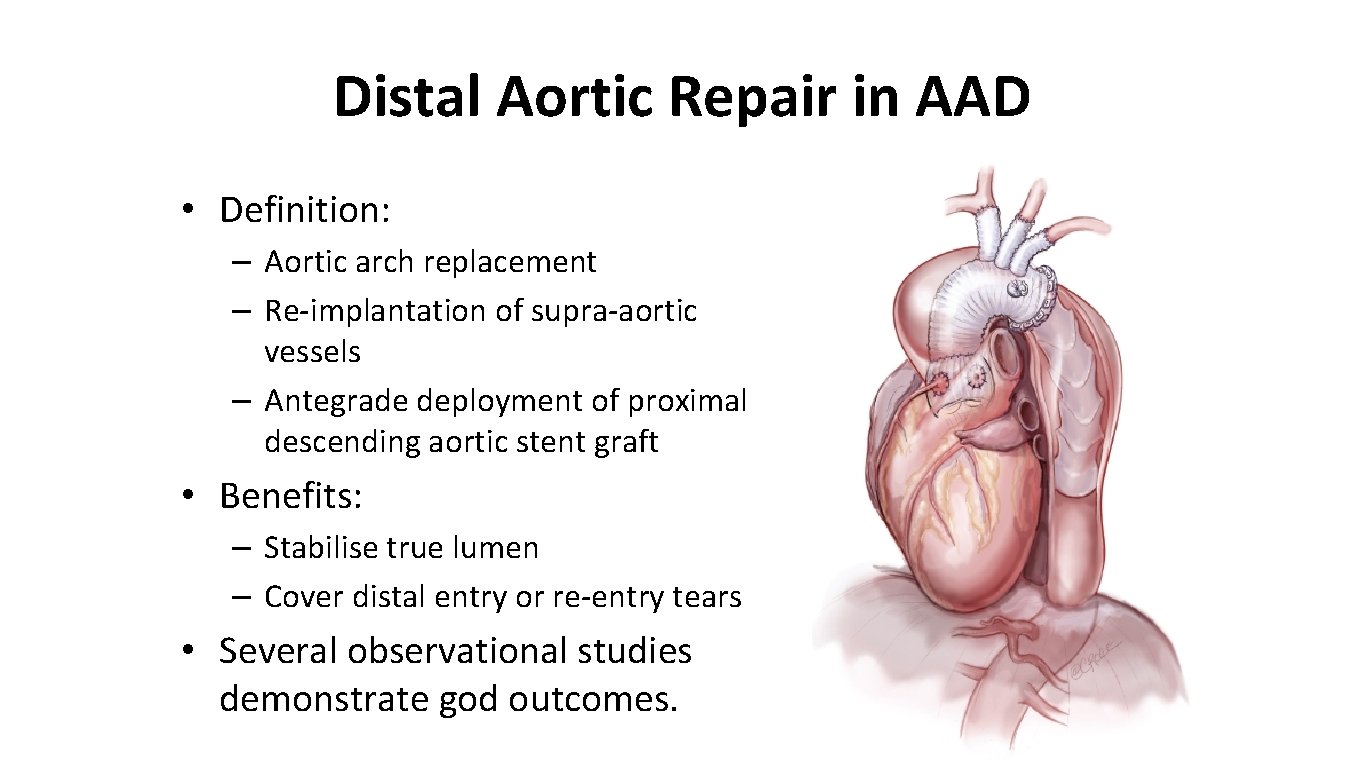
Distal Aortic Repair in AAD • Definition: – Aortic arch replacement – Re-implantation of supra-aortic vessels – Antegrade deployment of proximal descending aortic stent graft • Benefits: – Stabilise true lumen – Cover distal entry or re-entry tears • Several observational studies demonstrate god outcomes.

Comparative Observational Studies 14 observational studies comparing outcomes in a total of 1435 patients undergoing conservative surgery and 786 patients undergoing distal aortic repair Conservative Surgery Distal Aortic Repair 30 -day mortality 3 – 24% 4 – 29% 5 -year mortality 15 – 30% 5 – 10% 10 -year mortality 40 – 50% (patent FL) 10 – 30% (thrombosed FL) Not available Stroke 5 – 7% 3 – 6% Spinal cord injury 0 – 1% 1 – 3% False lumen patency 60 – 70% 0 – 20% Distal Re-operation 20 – 40% 0 – 10%

Research Question • In adult patients presenting with Type A AAD, does the addition of arch repair and distal aortic stent-graft placement: – Reduce long-term mortality – Reduce distal aortic re-intervention – Provide equivalent short-term mortality and morbidity • Compared to conservative surgery

Study Design • Multi-centre RCT with 2 parallel groups (Conservative surgery vs Distal aortic repair) • Inclusion Criteria – Age: 18 -79 years – CT proven Type A AAD extending beyond ascending aorta – Candidate for emergency surgery and either conservative or distal aortic repair feasible – Patient able to give informed consent • Exclusion Criteria: – Age ≥ 80 years – Onset of symptoms prior to 14 days – Patient unable to give informed consent • Registry – Patients falling outside inclusion criteria will be recorded in a study registry
Control and Intervention Groups • Control Group: Conservative Surgery – Supra coronary replacement of the ascending aorta with a synthetic graft • Intervention Group: Distal aortic Repair – Arch Replacement + Placement of Proximal Descending Aortic Stent + Supra coronary replacement of ascending aorta with a synthetic graft • For all patients: – Aortic root procedures as determined by surgeon – Cannulation strategy, anaesthetic monitoring, cerebral and neuro protection according to institutional practice.

Summary • Real surgical emergency • High mortality associated with condition • High mortality if we don't operate • Most patients warrant an operation • Work out a surgical strategy prior to commencing
 Facs
Facs Cardiothoracic surgeon salary
Cardiothoracic surgeon salary Chest physiotherapy assignment
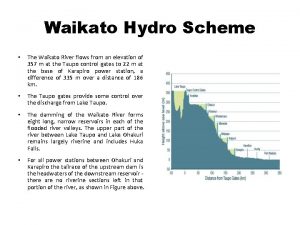
Chest physiotherapy assignment Waikato stormwater management guideline
Waikato stormwater management guideline Waikato kindergarten association
Waikato kindergarten association Weka waikato
Weka waikato Waikato dhb ransomware
Waikato dhb ransomware Acute coronary syndrome
Acute coronary syndrome Acute radiation syndrome
Acute radiation syndrome Mean arterial pressure formula
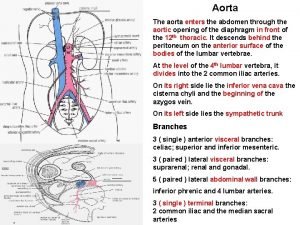
Mean arterial pressure formula Aortic area 1 and 2
Aortic area 1 and 2 Aortic root enlargement
Aortic root enlargement Thoacic
Thoacic Carina respiratory system
Carina respiratory system Dvi aortic valve
Dvi aortic valve Bronchopulmonary segments
Bronchopulmonary segments Major arteries of the ascending aorta and aortic arch
Major arteries of the ascending aorta and aortic arch Iliac vessels anatomy
Iliac vessels anatomy Dvi aortic valve
Dvi aortic valve Branches off aortic arch
Branches off aortic arch Features of aortic stenosis
Features of aortic stenosis Spermatic cord
Spermatic cord Dvi in echo
Dvi in echo Rcc aortic valve
Rcc aortic valve Aortic regurgitation murmur
Aortic regurgitation murmur Aortic valve dimensionless index
Aortic valve dimensionless index Aortic body
Aortic body Truncus arterioso
Truncus arterioso Hila lung
Hila lung Dr m chadi alraies
Dr m chadi alraies Pulmonary aortic window
Pulmonary aortic window Aortic pressure curve
Aortic pressure curve 4th aortic arch derivatives
4th aortic arch derivatives Aortic valve leaflets
Aortic valve leaflets Dobutamine dose
Dobutamine dose The pulmonary semilunar valve
The pulmonary semilunar valve Dicrotic pulse
Dicrotic pulse Great cardiac vein
Great cardiac vein Atrioventricular groove
Atrioventricular groove Aortic disection
Aortic disection Aortic stanosis
Aortic stanosis Aortic pressure
Aortic pressure Aortic bifurcation surface anatomy
Aortic bifurcation surface anatomy Art labeling activity figure 19.26b
Art labeling activity figure 19.26b Type b aortic dissection
Type b aortic dissection Aortic semilunar valve sheep heart
Aortic semilunar valve sheep heart Site:slidetodoc.com
Site:slidetodoc.com Iliac nodes
Iliac nodes Pathophysiology of aortic aneurysm ppt
Pathophysiology of aortic aneurysm ppt /watch?v=0evgft8hgns
/watch?v=0evgft8hgns Structure of the heart
Structure of the heart Good morning blood
Good morning blood Thorasic aortic aneurysm
Thorasic aortic aneurysm Unit 6 review questions
Unit 6 review questions Dr vikas patel
Dr vikas patel Dr vikas patel
Dr vikas patel