NEUROLOGIC DISORDERS Myasthenia Gravis Parkinsons Disease Multiple Sclerosis
- Slides: 95
NEUROLOGIC DISORDERS Myasthenia Gravis Parkinsons Disease Multiple Sclerosis Amyotrophic Lateral Schlerosis Spinal Cord Injury Intervertebral Disc Herniation Cranial Nerve Problems 2009
Myasthenia Gravis
DEFINITION • problem in neurotransmission • severe fatigue of voluntary muscles • defect of acetylcholine receptor sites § at the myoneuronal junction • theories indicate autoimmune problem • Remissions/exacerbations • Progressive proximal muscle weakness improving with rest
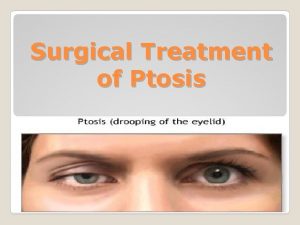
CLINICAL MANIFESTATIONS • Patients indicate abnormal fatigue of the voluntary muscles of the eye, the respiratory tract and the limb muscles • Also have difficulty with speech and swallowing • End up choking with meals • Ptosis, diplopia, dysphagia • MOST ADVANCED: all muscles weakened: no respiratory function, no bladder and bowel function
DIAGNOSTIC TESTS • Tensilon test: – give patient a short acting anticholinesterase (Tensilon or edrophonium chloride) that enhances neurotransmission and results in abrupt, but short term improvement of symptoms • Atropine : antidote for Tensilon • EMG: electromyography:
LABORATORY ASSESSMENT • THYROID FUNCTION STUDIES DONE: thyrotoxicosis seen with MG • Serum protein electrophoresis: for immunologic disorders • Acetylcholine receptor antibodies (ACh. R): important diagnositic criterion 80 -90% of clients with MG have elevated ACh. R • Often have thymoma or hyperplasia of thymus gland
DRUG THERAPY Anticholinesterase medications: – Pyridostigmine bromide (Mestinon), neostigmine bromide (Prostigmin) Increases acetylcholine at the neuromuscular junction – Dosage regulated based on improved strength and less fatigue – MUST BE GIVEN ON TIME to keep stable blood levels • RESULT: pt weakness worse
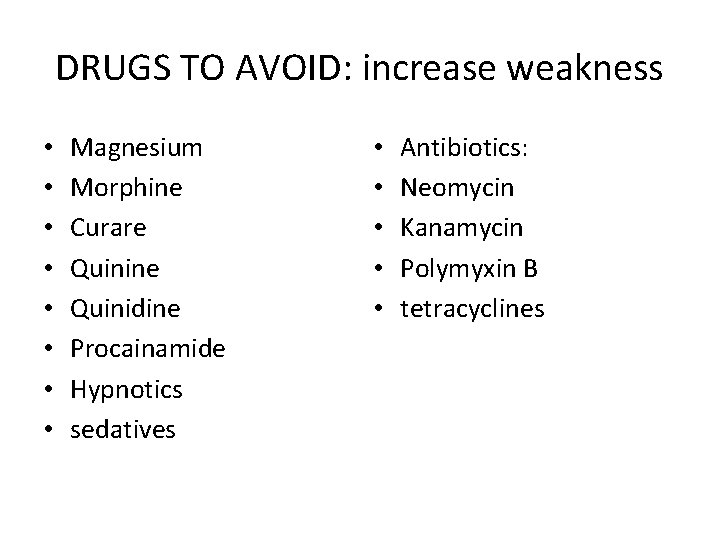
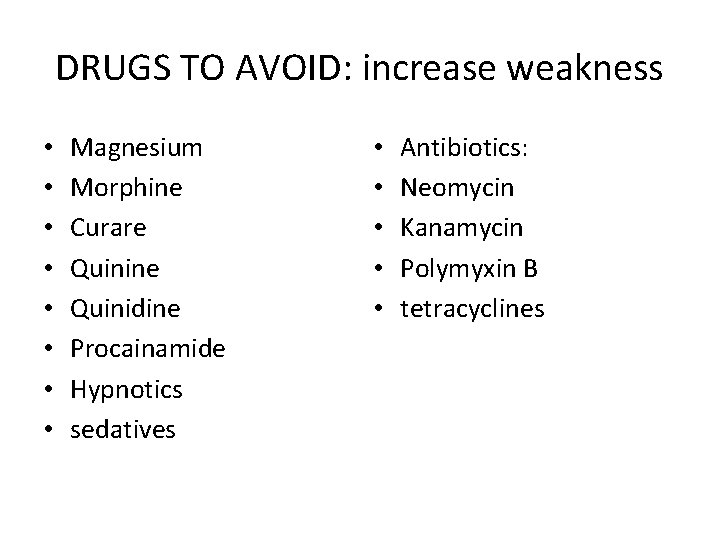
DRUGS TO AVOID: increase weakness • • Magnesium Morphine Curare Quinine Quinidine Procainamide Hypnotics sedatives • • • Antibiotics: Neomycin Kanamycin Polymyxin B tetracyclines
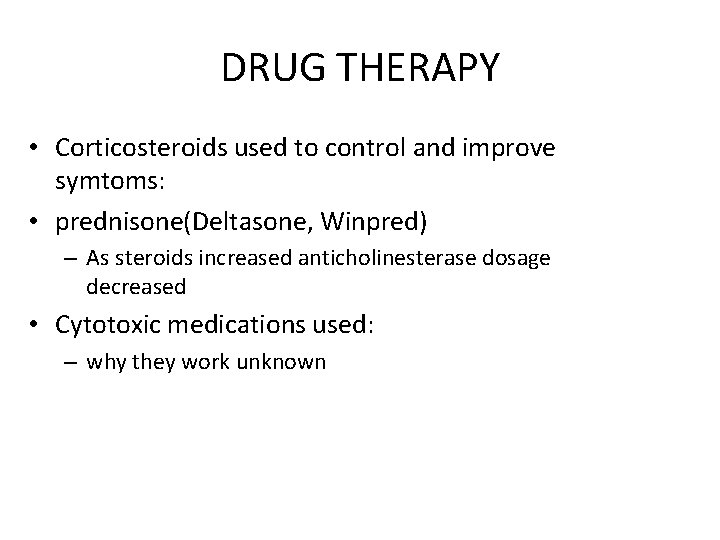
DRUG THERAPY • Corticosteroids used to control and improve symtoms: • prednisone(Deltasone, Winpred) – As steroids increased anticholinesterase dosage decreased • Cytotoxic medications used: – why they work unknown
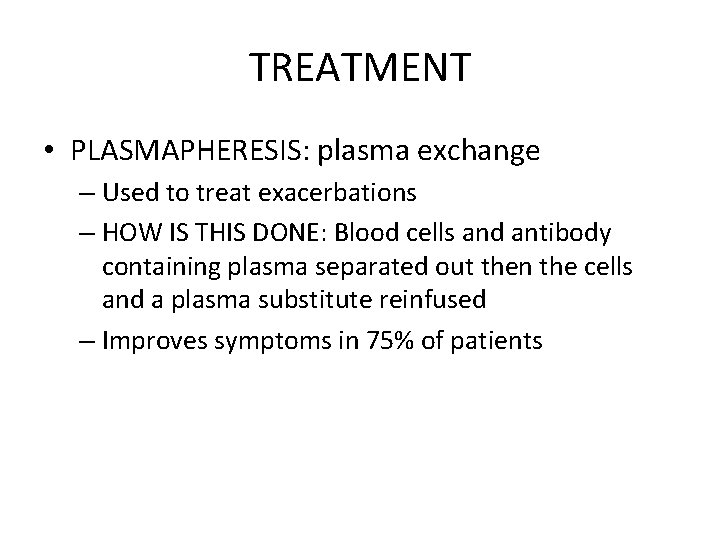
TREATMENT • PLASMAPHERESIS: plasma exchange – Used to treat exacerbations – HOW IS THIS DONE: Blood cells and antibody containing plasma separated out then the cells and a plasma substitute reinfused – Improves symptoms in 75% of patients
TREATMENT CONTINUED • IV immune globulin (IVIG) • Works as well as plasmapheresis during exacerbations
Summary of therapies • Not a cure • Does not stop the production of acetylcholine receptor antibiodies
SURGICAL TREATMENT • Thymectomy continues to be associated with improvement in 50 -92%% of patients • RESULT: – – produces antigen specific immunosuppression Results in clinical improvement Decreases need for medication Takes a year for benefit to be seen because of the long life of circulating T cells
MYASTHENIC CRISIS • SEEN WITH UNDERMEDICATION WITH CHOLINESTERASE INHIBITORS • Severe generalized weakness and respiratory failure • Seen after stress (URI, infection, medication change, surgery, obstetrical delivery, high environmental temperature) • Patient needs ventilatory support • Patient will need help with all ADL • Suctioning, chest PT
CHOLINERGIC CRISIS • RESULT OF OVERMEDICATION WITH ANTICHOLINESTERASE DRUGS • Can mimic symptoms of myasthenic crisis • Differentiated via Tensilon test • Pt with Myasthenic Crisis will show immediate improvement following Tensilon administration • Pt with Anticholinergic Crisis will show no improvement and may get worse
TREATMENT OF CHOLINERGIC CRISIS • STOP ALL ANTICHOLINESTRASE MEDICATIONS • Give Atropine sulfate given IV • SE: secretions thickened
NURSING DIAGNOSIS
THYMECTOMY: • REMOVAL OF THYMUS GLAND DONE EARLY IN DISEASE • May take several years for remission to occur if it occurs at all • Review p 1017 Iggy
NURSING CARE • Most pts seen on outpatient basis • Teaching: – – – – use of medications S&S of myasthenic crisis and choinergic crisis How to conserve energy Ways to avoid aspiration Have suction at home Gastrostomy feeding instruction Avoid factors that increase crisis Eye care
PARKINSONS DISEASE
DEFINED Presence of motor dysfunction with 4 cardinal symptoms • resting tremor • akinesia (slowness of body movement) • rigidity • Postural instability NO PREVENTION, NO CURE AGE RANGE: 40 -70, PEAK 60 Michael J. Fox dx at age 30
PATHOPHYSIOLOGY Reduced amount of dopamine • Result: inhibition effect lost • Excitatory effect predominant Reduced norepinephrine in sympathetic NS of the heart: • Orthostatic hypotension
ASSESSMENT: • Initially: one limb involved with mild weakness and arm and hand trembling • Progresses to both limbs involved, slow shuffling gait • Continues to worsen: gait disturbances(slow shuffling, short hesitant steps, propulsive gait • Severe involvement: akinesia, rigidity, CANNOT GET OOD
FURTHER ASSESSMENT: • • • Rigidity of facial muscles: masklike facies Drooling Dysphagia Dysarthria: Rapid slurred speech Echolalia: repetition
ASSESSMENT CONTINUED • PSYCHOSOCIAL • Emotionally labile • Delayed reaction time
DRUGS • ANTIPARKINSON AGENT: monoamine oxidase type b inhibitor: selegiline (Eldepryl, Carbex, Novo-Selegiline): used to protect the neurons, successful in reducing the use of Levodopa until later • Catechol O-methyltransferase (COMT) inhibitors: – Tolcapone (Tasmar) – Entacapone (Comtan) Block breakdown of levodopa in body so more can go to brain and convert to dopamine
DRUGS • DOPAMINE AGONISTS: providing dopamine that is missing – Levodopa (Dopar, L-dopa) and – carbidopa (Sinemet): ANTIPARKINSON AGENT/ANTIVIRAL: • amantadine (Symmetrel): potentiates action of dopamine in CNS, treats tremor; also treats symptoms of “wearing off”
TREATMENT • Meds may need drug holiday - effectiveness after used for long time; admit to hospital to try other drugs • p 693 FOR SURGICAL tx • Stereotactic Pallidotomy/Thalamotomy Deep brain stimulation fetal Tissue transplant
NURSING DIAGNOSIS • Self-care deficit related to slowness of movement and muscle rigidity • Risk for injury related to postural instability and muscular rigidity • Impaired verbal communication related to slowness of movement • Altered nutrition related to poor muscle control
NURSING DIAGNOSIS CONTINUED • Knowledge deficit related to complexity of and fluctuations in treatment regimen • Ineffective coping relate to progressive nature of illness
IMPLEMENTATION Establish routine for personal care Safety in bathing, transferring, walking AROM, PROM Encourage pt to take a deep breath before initiating a conversation, using gestures • Rigidity of facial expression hides pts true feelings • •
IMPLEMENTATION Meals thickened liquids, semisolids Eat sitting up Suction Daily wgts Increase fluids/day for constipation Drug flowsheet to document response to medications • Keep patient active as long as possible • • •
MULTIPLE SCLEROSIS AUTOIMMUNE DISORDER
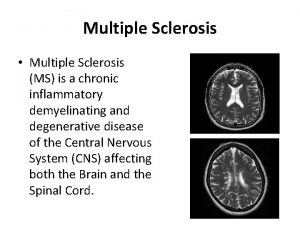
DEFINED • Demyelinating disease affecting nerve fibers of the brain and spinal cord • CAUSE unknown. Thought to be an autoimmune problem with a viral trigger • Lesions scattered through the white matter of the brain around the ventricles; some in grey matter • Inflammatory response triggers phagocytosis with myelin as the target
OLDER DRUG THERAPY • The most widely accepted drug treatment is corticosteroids : • Methylprednisolone(Solumedrol) • Given IV followed by oral prednisone – Steroids decrease the inflammatory response, decrease the edema, improvement of symptoms • Cyclophosphamide (Cytoxan) used for chronic progressive disease to produce temporary remission from 1 -3 years
DEFINITION CONTINUED Edema around lesions Eventually a hard plaque forms Characterized by exacerbations and remissions Progressive from benign with few symptoms to chronic with complete paralysis. • 70% of pts lead active productive lives with long periods of remission • •
DIAGNOSIS • lumbar puncture: CSF shows increase protein, lymphocytes, Ig. G, presence of oligoclonal bands and increased myelin basic protein • EMG: prolonged impulse conduction • MRI: demonstrates white matter lesions (plaques) of brain, brainstem and spinal cord
NEW DRUG THERAPY BIOLOGICAL RESPONSE MODIFIERS: recommended to use one of these three: • Interferon beta -1 a (Avonex) - weekly IM • Interferon beta-1 b recombinant (Betaseron) every other day SQ • PURPOSE AND SIDE EFFECTS OF BOTH – Slows physical disability, decreases physical worsening of disease – Major SE: suicidal tendency, depression • Glatiramer acetate (formerly Copolymer I) (Copaxone) - every other day SQ
SYMPTOMS • • Blurred vision Double vision Dysphagia Facial weakness Numbness Pain Weakness
Symptoms Continued • • paralysis abnormal gait tremor vertigo fecal and urinary incontinence decreased short term memory word finding trouble
Symptoms Continued • • • decreased concentration mood alteration decreased libido for women ejaculatory dysfunction for men overwhelming weakness
DRUGS • Baclofen (Lioresal), Diazepam (Valium), Dantrolene sodium(Dantrium) - for spasticity • Carbamazepine (Tegretol), tricyclic antidepressants (amitriptyline), : paresthesia • propranolol (Inderal), clonazepam (Klonopin) – used for cerebral ataxia • Amantadine hydrochloride (Symmetrel): fatigue • oxybutynin chloride (Ditropan), propantheline bromide (Pro. Banthine) - decreased urinary urgency, incontinence • Bulk additives (Metamucil) - constipation • Colace - improved bowel control • Dulcolax – stimulant • Tizanidine (Sanaflex) antispasmodic for pain
NURSING INTERVENTIONS • Self-care deficit: balance assistance with independence; promote own routine • Urinary retention/incontinence: intermittent catherization, Texas catheter for men • Bowel incontinence: regular routine, high fiber diet, and fluids • Impaired skin integrity related to immobility: skin assessment
NURSING INTERVENTION • Fatigue related to disease process: pace self
AMYOTROPHIC LATERAL SCLEROSIS Lou Gerhig’s Disease
Amyotrophic Lateral Sclerosis or Lou Gehrig’s disease • Progresive degenerative disease involving the motor system (motor neurons) • Sensory and autonomic systems not involved • No mental status changes
Cause • Excess of glutamate: chemical responsible for relaying messages between the motor neurons • As the motor neurons die the muscle cells they supply undergo atrophic changes leading to paralysis
PROGRESSION OF DISEASE • Muscle weakness and atrophy develop leading to flaccid quadriplegia • Eventually respiratory muscles become affected leading to respiratory compromise, pneumonia and death • No known cure, treatment symptomatic
WHAT DO YOU SEE? • FATIGUE • Fatigue while talking • Muscle weakness/atrophy • Tongue atrophy • Dysphagia (difficulty swallowing) • Weakness hands and arms • Fasciculations (twitching) of face • Nasal quality of speech • Dysarthria (difficulty speaking)
CARE • • Focus on symptoms Monitor respiratory status Prepare to initiate respiratory support Assess complications of immobility
SPINAL CORD INJURY
DEFINED • Fractures, contusions, or compression of the vertebral column with damage to the spinal cord • The injury affects motor and sensory function at the level of injury and below SPINAL CORD INJURIES are classified as complete or incomplete • Complete: total cord transection • Incomplete: partial transection
FOUR TYPES OF INJURIES OCCUR • HYPERFLEXION: compresses vertebral bodies and disrupts ligaments and discs • HYPEREXTENSION: disrupts ligaments and causes vertebral fractures • AXIAL LOADING: application of excessive vertical force and may cause compression fractures • EXCESSIVE ROTATION: tears ligaments and fractures articular surfaces and causes compression fractures
SPINAL SHOCK • With cord damage spinal shock occurs and areflexia (temporary loss of reflex functioning) • Loss of motor sensory, and autonomic activity below the level of injury • Then leads to decrease in blood pressure and bradycardia • The parts of body below the level of the cord injury are paralyzed without sensation or diaphoresis • Lasts days or months after injury
DEFINITIONS OF PARALYSIS • PARAPLEGIA: paralysis of the lower portion of the body; occurs when the injury level is in the thoracic spine or lower • Tetraplegia: formerly quadriplegia is paralysis of the arms, trunk, legs and pelvic portion; occurs when the level of injury is in the cervical spine
EMERGENCY TREATMENT • DO NOT MOVE THE CLIENT until adequate personnel and equipment are available • Keep the neck aligned • Immobilize the head and neck • Maintain a patent airway (with cervical injury edema may cause respiratory difficulty
ADMINISTER DRUGS • High dose corticosteroids: – reduces disability in 8 hrs of injury • Osmotic diuretics: mannitol (Osmitrol) – Decreases edema around spinal cord • Muscle relaxants: baclofen (Lioresal) – Reduces spasticity • Dextran – prevents BP; improves capillary blood flow • dopamine hydrochloride (Intropin) and isoproterenol (Isuprel): inotropic and sympathomimetic agents for severe hypotension
IMMOBILIZATION • Goal: reduce dislocations and stabilize cervical vertebral column HOW? • Skeletal traction (skeletal tongs such as Gardner– Wells tongs or Crutchfield tongs) • Halo traction CARE: weights hang freely, never remove weights, clean tongs, assess for infection
SURGERY • Surgical immobilization via anterior and posterior decompression and fusion with bone grafts • DECOMPRESSION WITH LAMINECTOMY: remove bony fragments that cause compression, remove foreign body causing compression • FUSION: anterior, posterior or anterior/posterior using Harrington rods
IMMOBILIZATION AFTER SURGERY • SOMI JACKET • CTLSO
AUTONOMIC DYSREFLEXIA DEFINED: • Exaggerated sympathetic response that occurs in clients with T 6 injuries or higher • Response seen after spinal shock occurs when stimuli cannot ascend the cord • Stimulus (urge to void) triggers massive vasoconstriction below the injury, vasodilation above the injury, and bradycardia
CAUSES OF AUTONOMIC DYSREFLEXIA MOST COMMON: overdistended bladder • Bowel impaction, rectal exam • UTI, bladder spasms, renal calculi • Pressure sores, ingrown toenail • Burns, blows to body • Tight clothing, tight cast
S & S AUTONOMIC DYSREFLEXIA • • Sudden pounding severe HA Severe hypertension, bradycardia Flushing, sweating above the level of injury Piloerection (goose bumps) Nasal congestion Apprehension Blotching above the level of injury
TX OF AUTONOMIC DYSREFLEXIA SERIOUS MEDICAL EMERGENCY! ACT QUICKLY! DO NOT WAIT! • Identify/remove the stimulus • Reduce the BP • Administer drugs • Teach pt how to deal with it
TX OF AUTONOMIC DYSREFLEXIA • • REQUEST HELP HOB up! Check BP q 5 minutes Do straight cath of bladder; eval bowel Remove tight clothing, check orthotics Check skin, toenails Report to MD if BP still won’t decrease
DRUGS FOR AUTONOMIC DYSREFLEXIA ACUTE PHASE: • Nitropaste (vasodilator) • Arfonad IV (ganglionic blocker to lower BP fast) • Apresoline IV (relaxes arterolar smooth muscle) • Low spinal anesthetic at L 4 if no results with drugs PREVENTION: antihypertensives
BLADDER PROBLEMS • • INCONTINENCE UTI URINARY CALCULI BLADDER SPASMS
SPASTIC BLADDER • Clients have Injury above the sacrum • End up with upper motor neuron spastic bladder • May be able to stimulate voiding by – – – Stroking inner thigh Pullin on pubic hair Pouring warm water over perineum Tapping bladder to stimulate detrusor muscle Taking bethanechol chloride (Urecholine); cholinergic agent which helps contraction of detrusor mucle: take 1 hour before trying to void
FLACCID BLADDER • Clients with lumbosacral injury • Have lower motor neuron flaccid bladder • Able to empty bladder by: – Tightening abdominal muscles – Intermittent cath two or three times daily
TREATMENT OF THE URINARY PROBLEMS • Intermittent catherization : Clean cath • Prevents incontinence, dysreflexia, UTI, calculi CAUTION: never drain more than 700 cc/ leads to hypovolemic shock • increase fluid, water, high acidity fluids, no alcohol, low soda (hi salt), low milk, avoid alkaline fluids
DRUGS FOR ELIMINATION PROBLEMS • oxybutynin (Ditropan) : decreases urinary incontinence • propantheline(Pro Banthine): reduces bladder spasms • ascorbic acid (Vitamin C): increases urine acidity; prevents UTI; works with Mandelamine • methenamine (Mandelamine): urinary tract antisepticto prevent UTI; do not combine with carbonic annhydrase inhibitors, sulfa drugs or diuretics • Imipramine (Tofranil) antidepressant used to tx urinary incontinence (side effect: urinary retention))
BOWEL ELIMINATION PROBLEMS Constipation Loss of bowel control TREATMENT: Bowel Program • Combination of stool softeners, bulk formers, laxatives • High fiber diet, high fluids
Bowel Program • Consitent time • High fluid intake • High fiber diet
DRUGS FOR BOWEL ELIMINATION PROBLEMS docusate sodium(Colace): stool softener senna (Senekot): laxative bisacodyl (Dulcolax): laxative dibucaine (Nupercainal): ointment anesthetic used prior to beginning bowel program to prevent autonomic dysreflexia • psyllium (Metamucil): bulk forming agent • •
OTHER PROBLEMS Mostly related to immobility • RESPIRATORY: pneumonia, PE • MOBILITY: contractures, spasticity, decubitus, burns, bruises, fractures, osteoporosis • CIRCULATORY: DVT/edema, postural hypotension, GI bleed • SEXUAL: males have decreased fertility, females can bear children
INTERVERTEBRAL DISC HERNIATION
DEFINED • Disorder involving impingement of a vertebral disk’s nucleus pulposus on spinal nerve roots causing pain and possible neuromuscular deficit TREATMENT conservative: • with muscle relaxants: cyclobenzaprine hydrochloride (Flexeril) • Nonsteroidal anti-inflammatory drugs (NSAIDS): naproxen (Naprosyn) • Epidural or local steroid injection • Rest, heat, muscle strengthening exercises, pelvic tilts, straight leg raises
MINIMALLY INVASIVE SURGERY (see page 980 of Iggy) ADVANTAGE: ambulatory procedure or shortened hospital stay with less spinal cord complications • Percutaneous lumbar diskectomy • Microdiskectomy • Laser-assisted laparoscopic lumbar diskectomy
SURGERY see p 980 of Iggy • Diskectomy: spinal nerve is lifted to remove the offending portion of the disk • Laminectomy: removal of 1 or more vertebral lamina and the herniated nucleus pulposus • Spinal fusion (arthrodesis): to stabilize area using chips of bone from iliac crest grafted to vertebrae
SURGICAL MANAGEMENT LAMINECTOMY: surgical incision of the lamina to relieve symptoms related to herniated intervertebral disc POST OP CARE: • Neurological and neurovascular assessment, assessment of bowel and bladder function • Assess for c/o severe HA or leakage of CSF • Log roll, proper alignment • Bedrest 24 -48 hours; rise as a unit when getting OOB first time • Paresthesias may not be relieved immediately
AMPUTATION
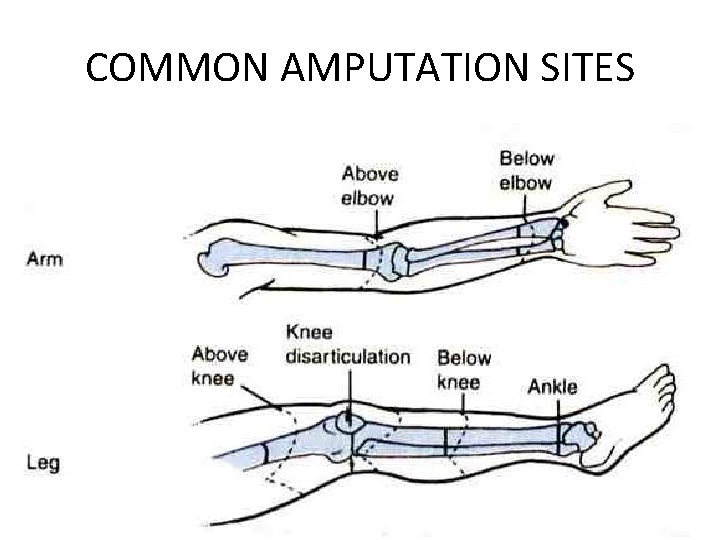
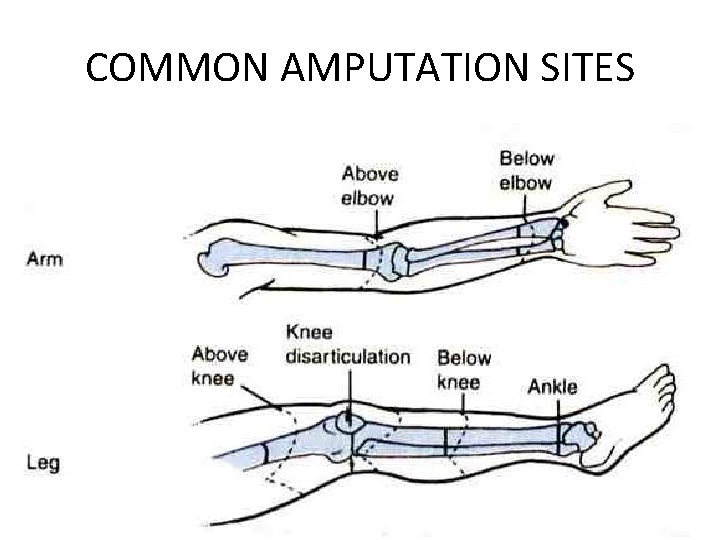
COMMON AMPUTATION SITES
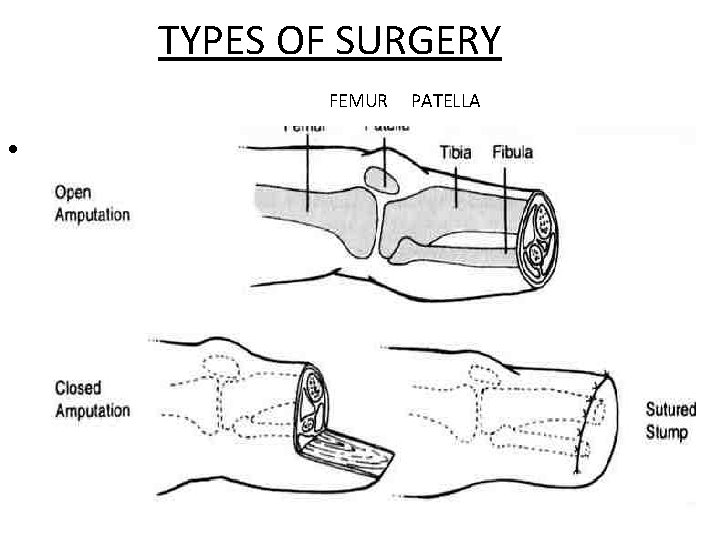
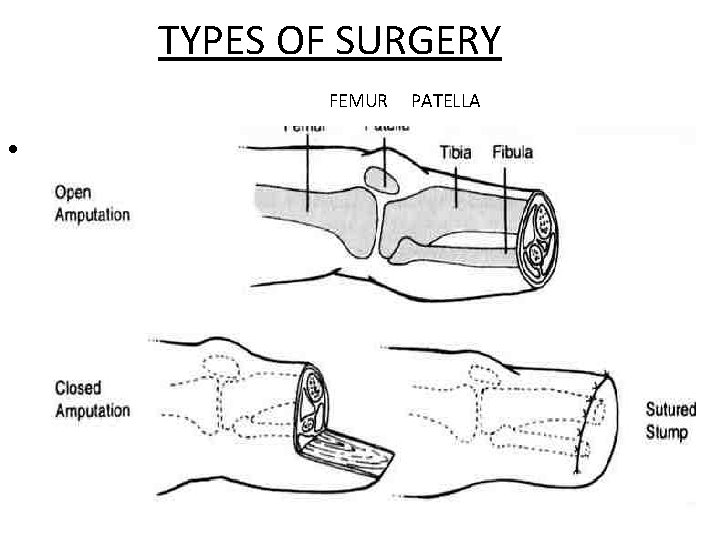
TYPES OF SURGERY FEMUR • femur patella PATELLA
TYPES OF PROSTHESES • TOTAL CONTACT RIGID DRESSING: applied in OR to protect stump swelling • PERMANENT LEG PROSTHESIS: rigid dressing that connects to an adjustable pylon and foot ankle assembly to permit walking; need 3 -4 of these, stump shrinks with healing • SOFT DRESSING: when frequent inspection needed; may have drainage device
COMPLICATIONS • • • Bleeding Infection Skin breakdown PHANTOM LIMB PAIN FLEXION CONTRACTURES
NURSING CARE 1. Proper positioning to minimize contractures 2. Watch use of pillow under stump 3. Lie prone 4. Phantom limb pain 5. Monitor for excessive bleeding 6. Prevent stump edema 7. Assess for infection 8. Assess for hematoma formation 9. Teach stump care 10. Teach use of prosthesis 11. Provide referral to National Amputee Foundation and Amputee Shoe and Glove Exchange
CRANIAL NERVE DISORDERS Trigeminal Neuralgia Bells Palsy Guillan-Barre Syndrome
Trigeminal Neuralgia • DEFINED: chronic disease of the trigeminal nerve causing severe facial pain unknown cause • Pain occurs briefly, intense skin surface pain 100 times/day or a few times a year • Starts peripherally and advances centrally • Some trigger zones initiate pain • TREATED WITH: seizure drugs: carbamazepine (Tegretol); phenytoin (Dilantin) • SURGICAL TREATMENT: removal of blood vessel from posterior trigeminal root or severing nerve root • NURSING DX: risk for imbalanced nutrition; pain
Bell’s Palsy • DEFINED: unilateral paralysis of facial muscles; unknown cause; inflammation of the nerve and viral cause suggested; recover within few weeks/months, some have permanent paralysis • SEE: one sided paralysis of facial muscles and upper eyelid, loss of taste on affected side, increased tearing of eye on affected side • TREATMENT: corticosteroids (decreases edema of nerve tissue) – Prednisone; and antiviral medications • NURSING DX: altered body image; altered nutrition
GUILLAIN BARRE SYNDROME • Autoimmune attack of the peripheral nerve myelin • RESULT: acute rapid demyelination of peripheral nerves and some cranial nerves • PRODUCES: – ***Ascending weakness with dyskinesia (inability to execute voluntary movements) – Weaknss starts in legs and progresses upward for 1 month – ***Hyporeflexia – Paresthesias (numbness and pain) – MAXIMUM WEAKNESS: • neuromuscular respiratory failure and • bulbar muscle weakness (demylelination of glossopharyngeal and vagus nerves leads to inability to swallow or clear secretions)
S & S CONTINUED • VAGUS NERVE DEMYELINATION: – Leads to autonomic dysfunction – Manifested by instability of cardiovascular system – S & S: tachycardia, bradycardia, hypertension, orthostatic hypotension • NO COGNITIVE DYSFUNCTION
SYMPTOMS CONTINUED • PRECIPITATING EVENT: respiratory or GI infection, vaccination, surgery, pregnancy • DURATION OF SYMPTOMS: may take up to two years to recover; some symptoms are permanent due to damage to nerves
TREATMENT • • • MEDICAL EMERGENCY: ICU Rapid progression Neuromuscular respiratory failure May need mechanical ventilation suctioning Prevention of complications of immobility
FOR CARDIOVASCULAR RISKS • EKG • beta blocking agents for tachycardia and hypertension • IV fluid for hypotension
NURSING DIAGNOSIS
 Myasthenia gravis
Myasthenia gravis Wartenberg test
Wartenberg test Pictures of ocular myasthenia gravis
Pictures of ocular myasthenia gravis Myasthenia gravis exercise
Myasthenia gravis exercise Tardyferon allaitement colique
Tardyferon allaitement colique Myasthenia gravis
Myasthenia gravis Myasthenia gravis thymectomy
Myasthenia gravis thymectomy Syringomyelia
Syringomyelia Myasthenia gravis oireet
Myasthenia gravis oireet Acetylcholine crisis
Acetylcholine crisis Myasthenia gravis clinical presentation
Myasthenia gravis clinical presentation Myasthenia gravis eyes
Myasthenia gravis eyes Concept map for disease process
Concept map for disease process Basal ganglia
Basal ganglia Parkinsons disease
Parkinsons disease Cell
Cell Is multiple sclerosis fatal
Is multiple sclerosis fatal Concept map multiple sclerosis
Concept map multiple sclerosis Chapter 17 neurologic emergencies
Chapter 17 neurologic emergencies Lippincott williams & wilkins
Lippincott williams & wilkins Management of patients with neurologic trauma
Management of patients with neurologic trauma Chapter 18 neurologic emergencies
Chapter 18 neurologic emergencies Katharine hepburn parkinsons
Katharine hepburn parkinsons Mb behcet wikipedia
Mb behcet wikipedia Shy drager syndrome
Shy drager syndrome Rectosigmoid junction
Rectosigmoid junction Lymphatic cell types
Lymphatic cell types Vas zita
Vas zita Scleroderma symptoms
Scleroderma symptoms Bharathi viswanathan
Bharathi viswanathan Inhoudsopgave symbool
Inhoudsopgave symbool Miasthenia gravis
Miasthenia gravis Miastenia gravis
Miastenia gravis Translate
Translate Gravis carter
Gravis carter Mythenia
Mythenia Adverbs in latin
Adverbs in latin Myathesia
Myathesia Delayed multiple baseline design
Delayed multiple baseline design Example of mimd
Example of mimd Chapter 14 psychological disorders
Chapter 14 psychological disorders Class a personality disorders
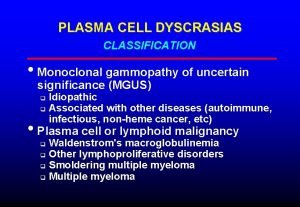
Class a personality disorders Plasma cell dyscrasias classification
Plasma cell dyscrasias classification Section 4-1 mental disorders answers
Section 4-1 mental disorders answers Congenital voice disorders
Congenital voice disorders Health and social care level 3 unit 14
Health and social care level 3 unit 14 Axis 1 and 2 disorders
Axis 1 and 2 disorders Work related musculoskeletal disorders definition
Work related musculoskeletal disorders definition Hemodynamic disorders
Hemodynamic disorders Kate moss anorexia
Kate moss anorexia Chapter 14 psychological disorders
Chapter 14 psychological disorders Unit 14 physiological disorders assignment 1
Unit 14 physiological disorders assignment 1 Icd 10 gatal alergi
Icd 10 gatal alergi Difference between renal and cardiac edema
Difference between renal and cardiac edema Difference between mendelian and chromosomal disorders
Difference between mendelian and chromosomal disorders Chapter 18 psychological disorders
Chapter 18 psychological disorders Looseness of association example
Looseness of association example Mild neurocognitive disorder
Mild neurocognitive disorder Acid base disorders chart
Acid base disorders chart Cluster b disorder
Cluster b disorder Genetic disorders
Genetic disorders Types of dissociative disorders
Types of dissociative disorders Physical disorders and health psychology
Physical disorders and health psychology Chapter 12 schizophrenia spectrum disorders
Chapter 12 schizophrenia spectrum disorders Marsipan criteria
Marsipan criteria Physiological disorders and their care
Physiological disorders and their care Ego dystonic
Ego dystonic Dissociative disorders
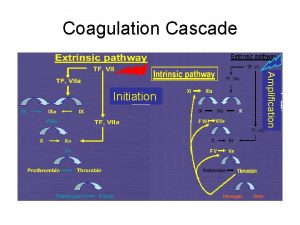
Dissociative disorders Coagulation disorders
Coagulation disorders Nail diseases and disorders milady
Nail diseases and disorders milady Sleep disorders
Sleep disorders Body fluid
Body fluid Mnemonics for personality disorders
Mnemonics for personality disorders Enduring pattern meaning
Enduring pattern meaning Hirschsprung disease nursing management
Hirschsprung disease nursing management Somatoform disorders
Somatoform disorders Strawberry physiological disorders
Strawberry physiological disorders Purine disorders
Purine disorders Pituitary gland disorders
Pituitary gland disorders Brainpop eating disorders
Brainpop eating disorders Inflexible personality
Inflexible personality Hirschberg test
Hirschberg test Lysosomal disorders
Lysosomal disorders Schizoid
Schizoid Neurodevelopmental disorders
Neurodevelopmental disorders Myeloproliferative disorder
Myeloproliferative disorder Neurotic stress-related and somatoform disorders
Neurotic stress-related and somatoform disorders Puberty and autism spectrum disorders
Puberty and autism spectrum disorders Neurocognitive disorder
Neurocognitive disorder Lower limb disorders
Lower limb disorders Dissociative
Dissociative Flinders model of chronic health disorders
Flinders model of chronic health disorders Weird wild wacky personality disorders
Weird wild wacky personality disorders Causes of paraphilic disorders
Causes of paraphilic disorders Secrotal
Secrotal Chapter 14 depressive disorders
Chapter 14 depressive disorders