MULTIPLE SCLEROSIS Multiple Sclerosis A chronic progressive neurologic

















- Slides: 63
MULTIPLE SCLEROSIS
Multiple Sclerosis • A chronic, progressive neurologic disease characterized by scattered demyelination of nerve fibers in the brain and spinal cord.
Multiple Sclerosis • Most common disabling condition in young adults • Most common demyelinating disorder • Progresses to disability in majority of cases • Unpredictable course & variety of signs and symptoms; sometimes mistaken for psychiatric disorder
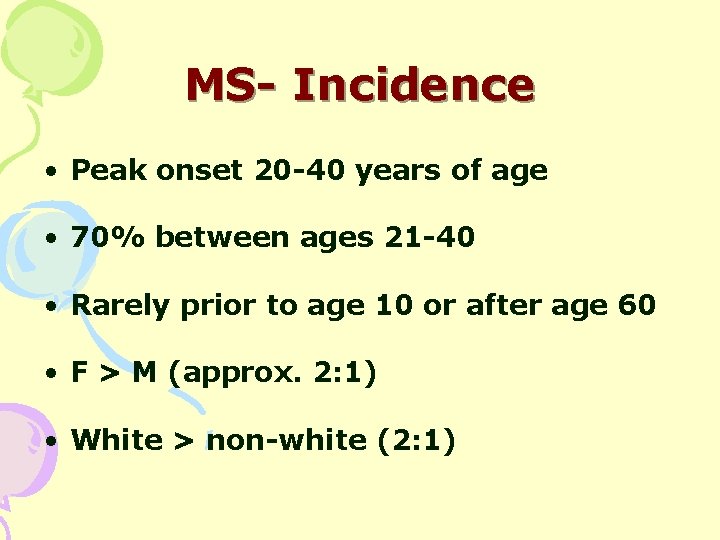
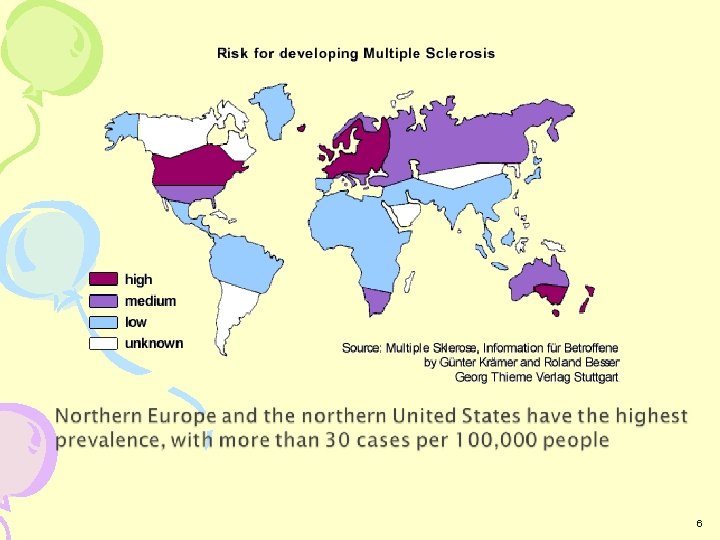
MS- Incidence • Peak onset 20 -40 years of age • 70% between ages 21 -40 • Rarely prior to age 10 or after age 60 • F > M (approx. 2: 1) • White > non-white (2: 1)

6

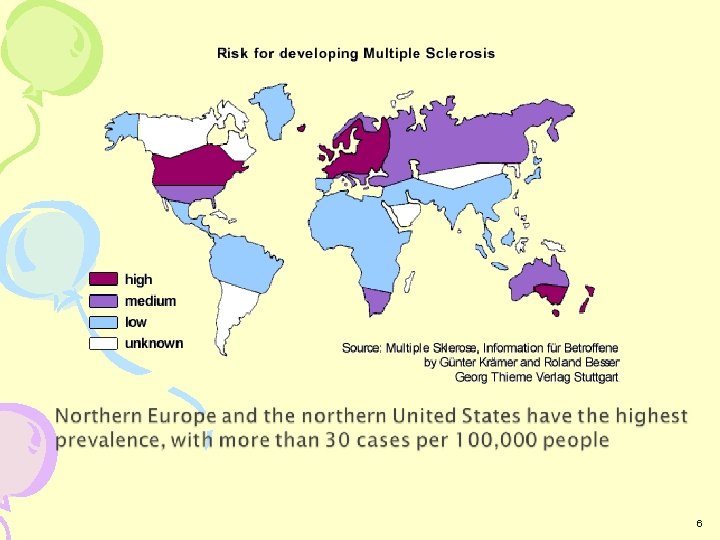
Risk factors • Autoimmune process • Viral infection • Allergic reactions to infection • Familial tendencies. • Cool, temperature climates.
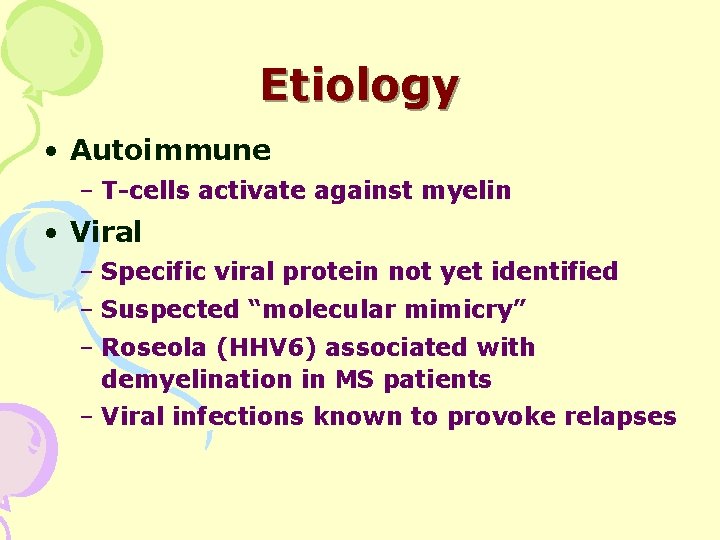
Etiology • Autoimmune – T-cells activate against myelin • Viral – Specific viral protein not yet identified – Suspected “molecular mimicry” – Roseola (HHV 6) associated with demyelination in MS patients – Viral infections known to provoke relapses
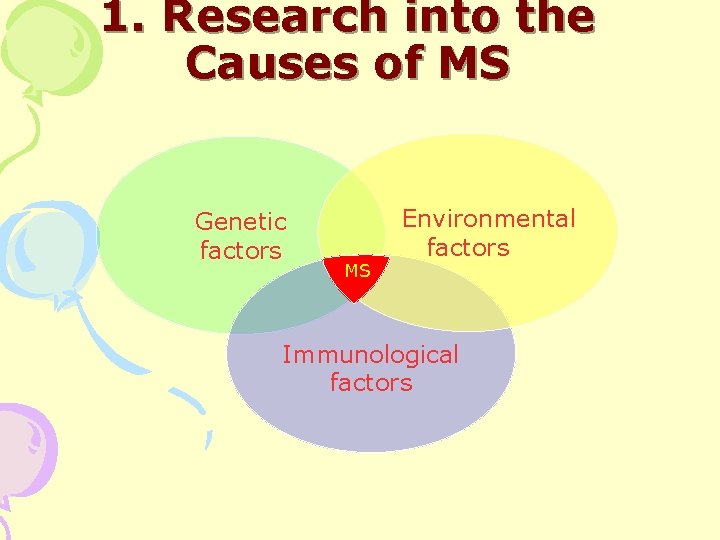
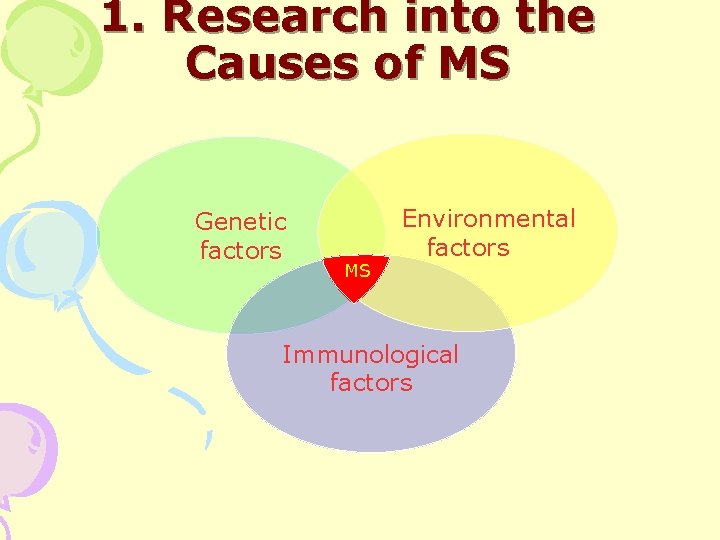
1. Research into the Causes of MS Genetic factors MS Environmental factors Immunological factors
Pathological Hallmarks • Described in late 1800 s by Dr. Charcot • Inflammation and demyelination • Plaques occur anywhere in the CNS – Most frequent: optic nerve, brainstem, cerebellum, spinal cord • Axon sparing within the plaques
Structure Of Plaques • Outer layers of myelin sheath separate • Degenerative changes in myelin • Infiltration with macrophages • Preservation of axons
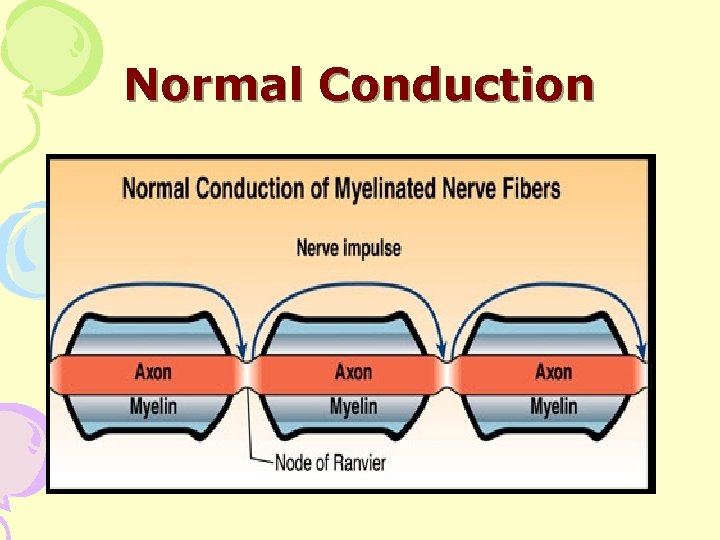
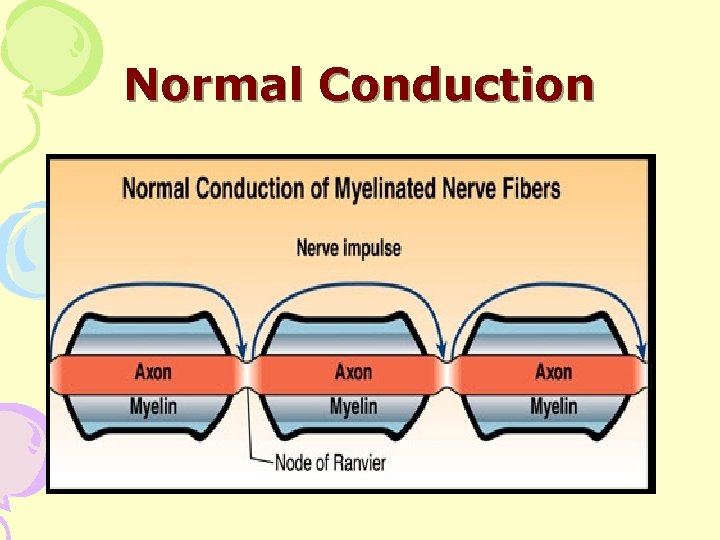
Normal Conduction
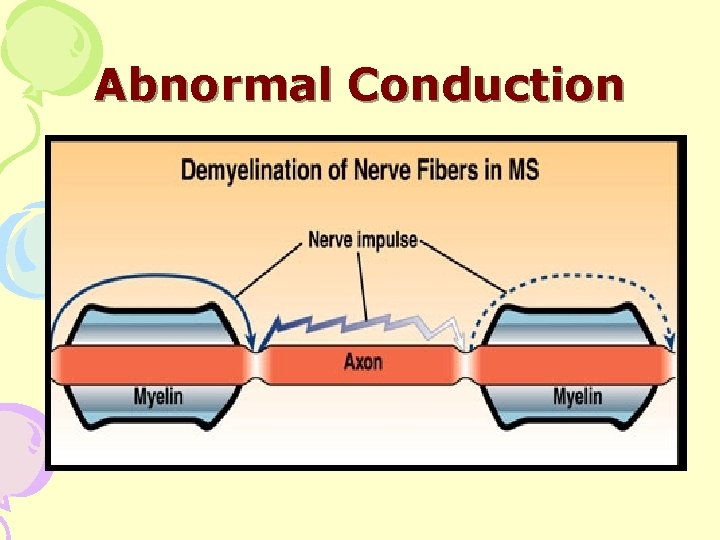
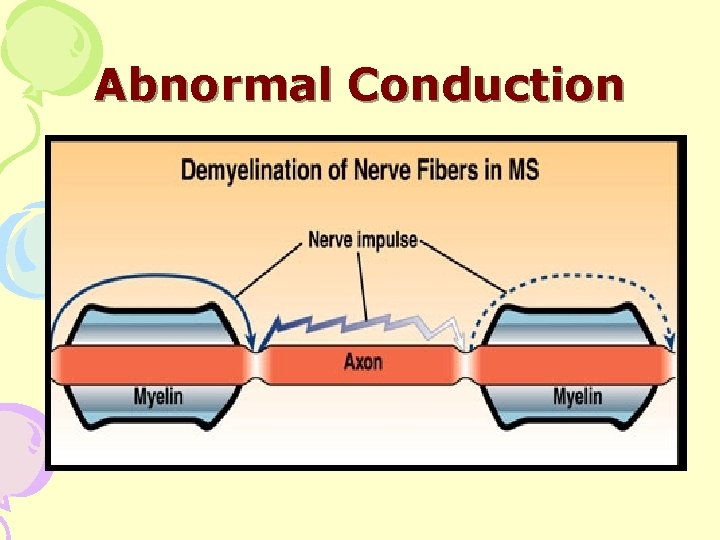
Abnormal Conduction
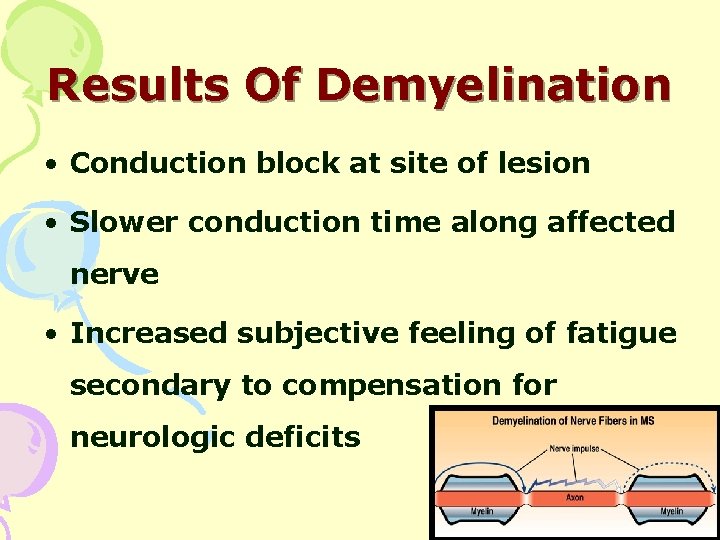
Results Of Demyelination • Conduction block at site of lesion • Slower conduction time along affected nerve • Increased subjective feeling of fatigue secondary to compensation for neurologic deficits
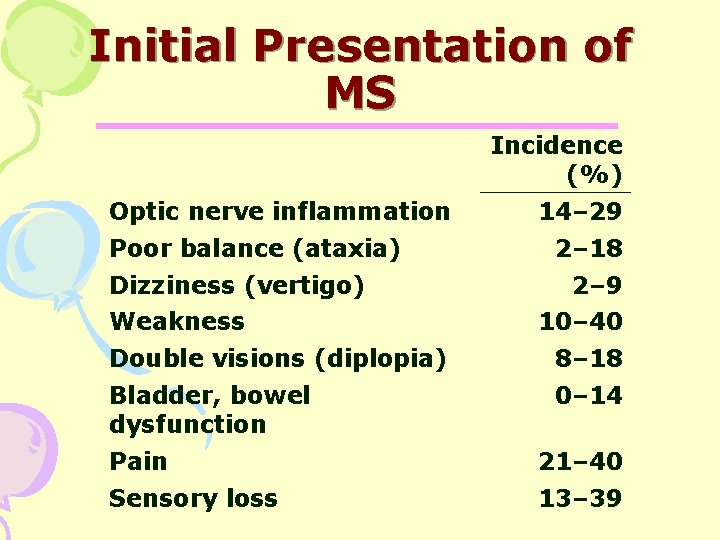
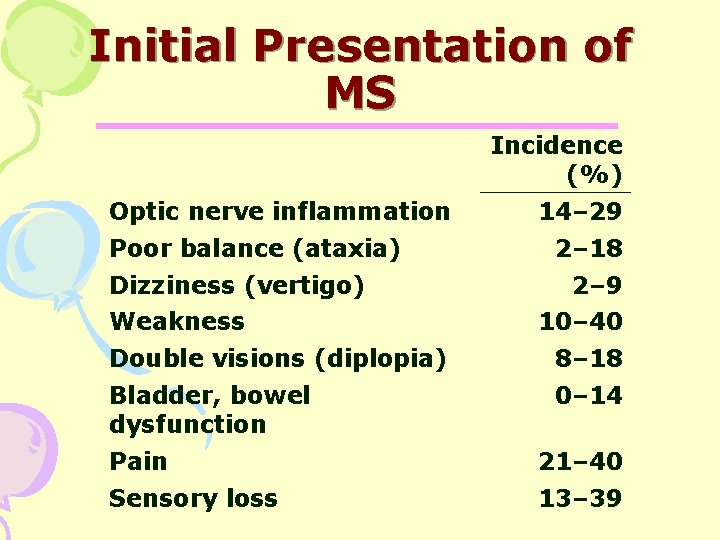
Initial Presentation of MS Incidence (%) Optic nerve inflammation Poor balance (ataxia) Dizziness (vertigo) Weakness 14– 29 2– 18 2– 9 10– 40 Double visions (diplopia) 8– 18 Bladder, bowel dysfunction 0– 14 Pain 21– 40 Sensory loss 13– 39
Initial Symptoms • Double vision / blurred vision • Numbness • Heat intolerance • Motor weakness • Fatigue • Problems with bladder control • Facial Palsy

Signs and Symptoms. • Instability while walking • Poor coordination • Dizziness • Tremors • Spasticity of extremities **All symptoms can be precipitated by heat**
Signs and Symptoms • Slurred speech • Difficulty in chewing and swallowing • Mental changes • cognitive dysfunction • Fecal or urinary incontinence or retention. • Impotence

Classification • Benign Multiple Sclerosis – Mild infrequent sensory exacerbations with full recovery. • Relapsing Remitting Multiple Sclerosis – Episodes of exacerbations and remissions during which not all symptoms resolve completely.
Classification • Secondary Chronic Progressive – Relapses become more severe while remissions are less complete, shorter in duration, and eventually non-existent. The course of MS becomes steadily progressive. • Primary Progressive – No relapse. Disease begins with a slow progression of neurologic deficits.
Diagnostic tests • CSF Analysis • Magnetic resonance imaging • Positron Emission Tomography • Evoked Potential Studies

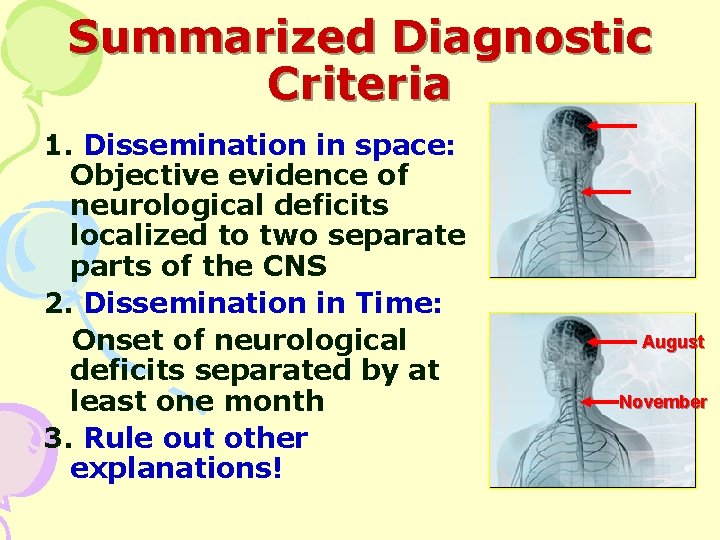
MS Diagnosis Dissemination in space and time
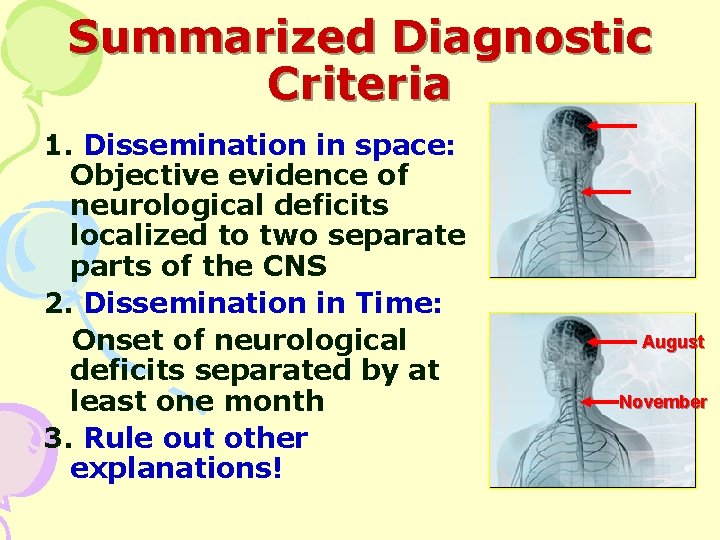
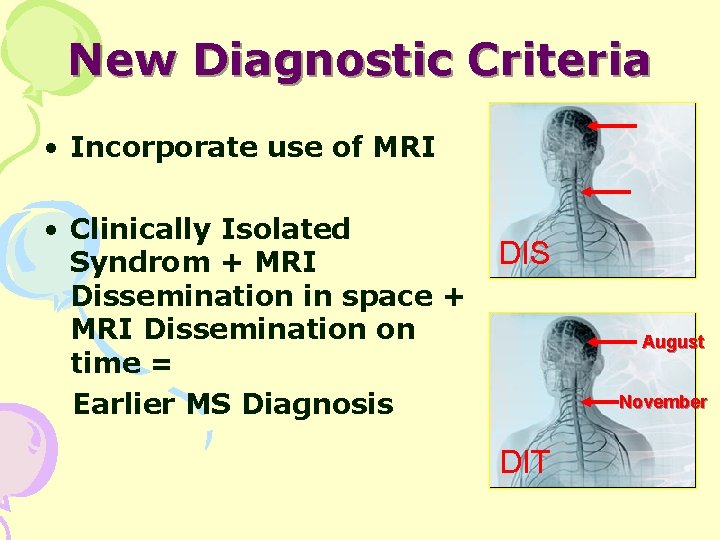
Summarized Diagnostic Criteria 1. Dissemination in space: Objective evidence of neurological deficits localized to two separate parts of the CNS 2. Dissemination in Time: Onset of neurological deficits separated by at least one month 3. Rule out other explanations! August November
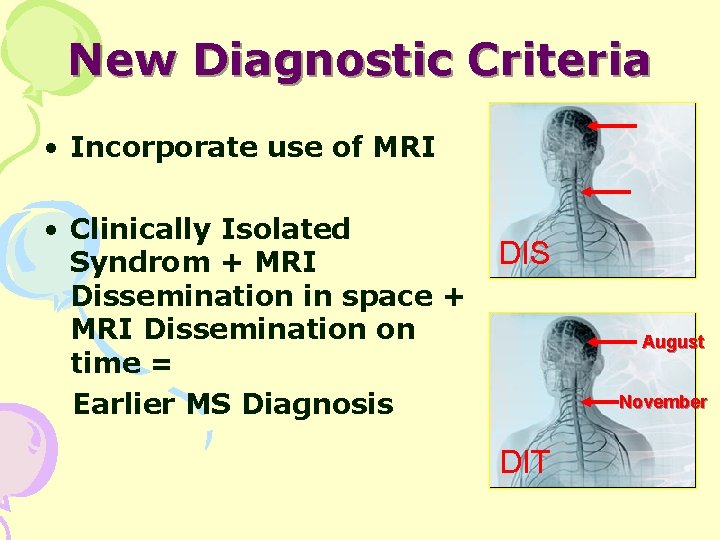
New Diagnostic Criteria • Incorporate use of MRI • Clinically Isolated Syndrom + MRI Dissemination in space + MRI Dissemination on time = Earlier MS Diagnosis DIS August November DIT
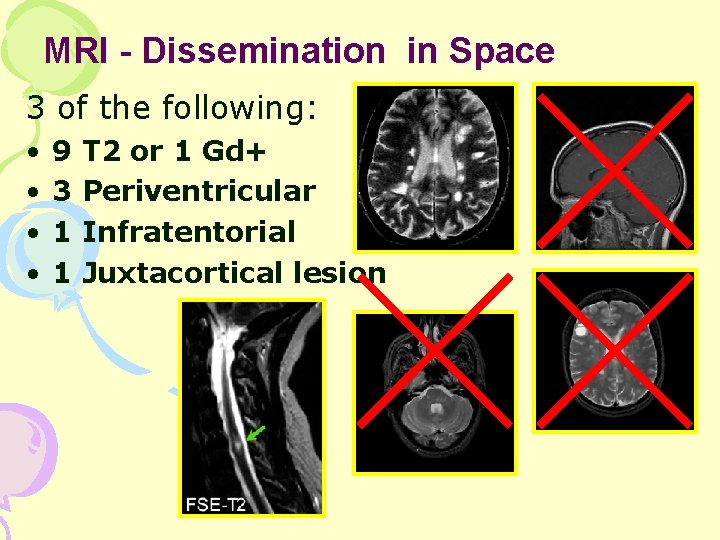
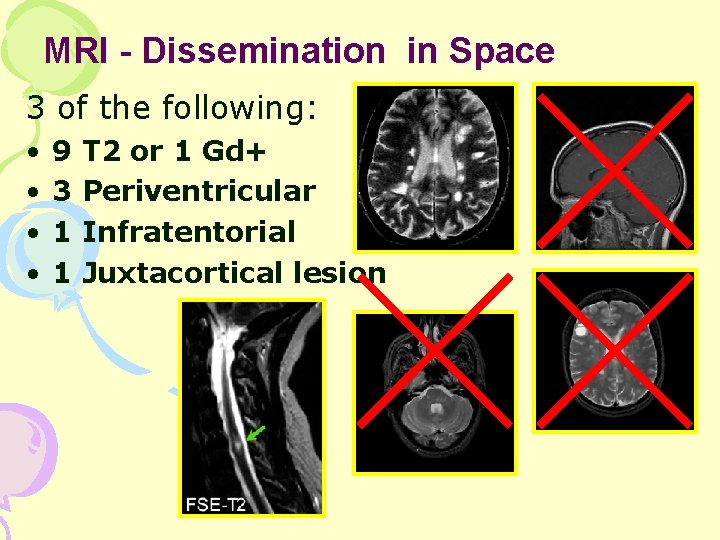
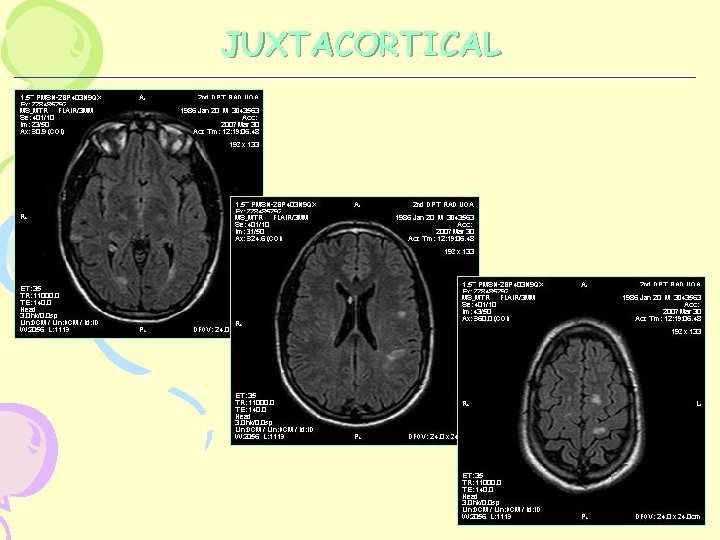
MRI - Dissemination in Space 3 of the following: • • 9 3 1 1 T 2 or 1 Gd+ Periventricular Infratentorial Juxtacortical lesion
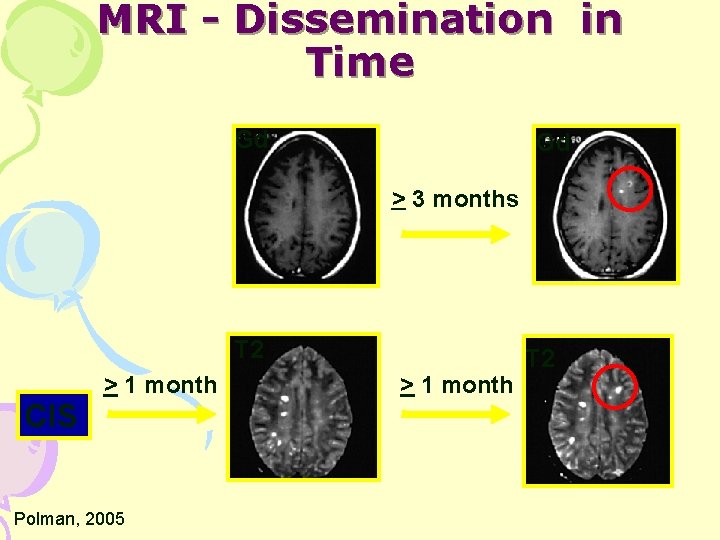
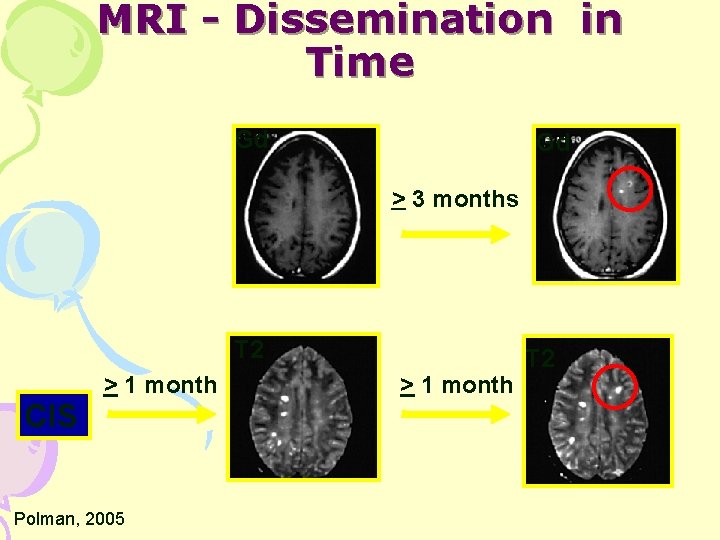
MRI - Dissemination in Time Gd Gd > 3 months T 2 CIS > 1 month Polman, 2005 > 1 month T 2
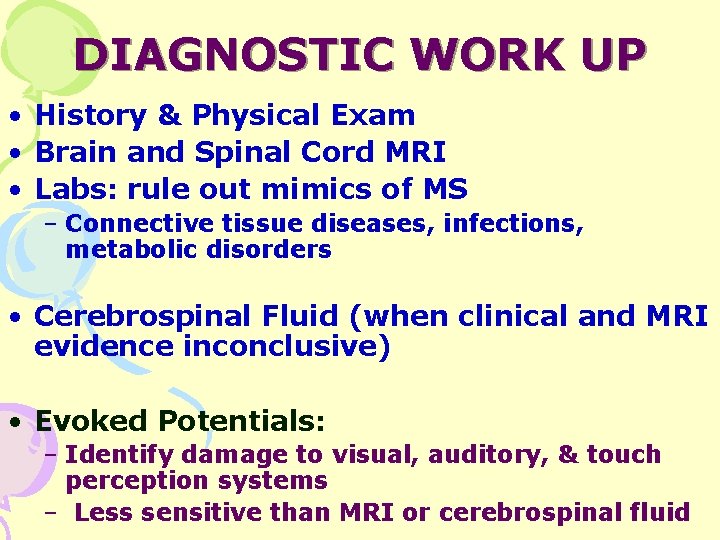
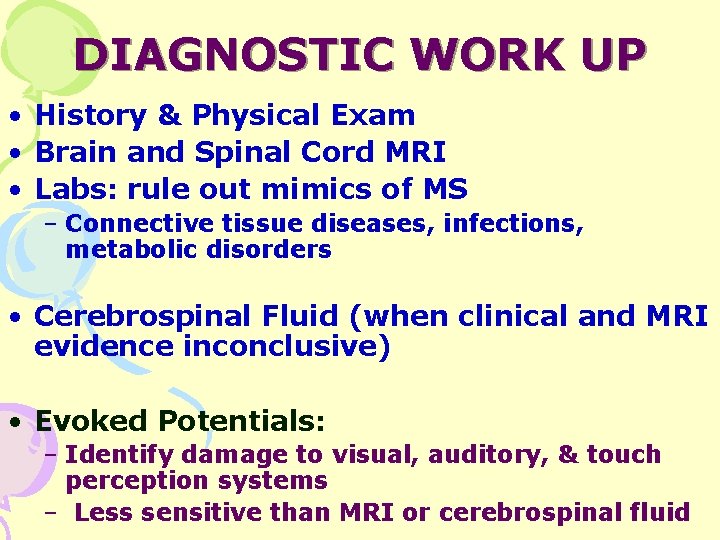
DIAGNOSTIC WORK UP • History & Physical Exam • Brain and Spinal Cord MRI • Labs: rule out mimics of MS – Connective tissue diseases, infections, metabolic disorders • Cerebrospinal Fluid (when clinical and MRI evidence inconclusive) • Evoked Potentials: – Identify damage to visual, auditory, & touch perception systems – Less sensitive than MRI or cerebrospinal fluid
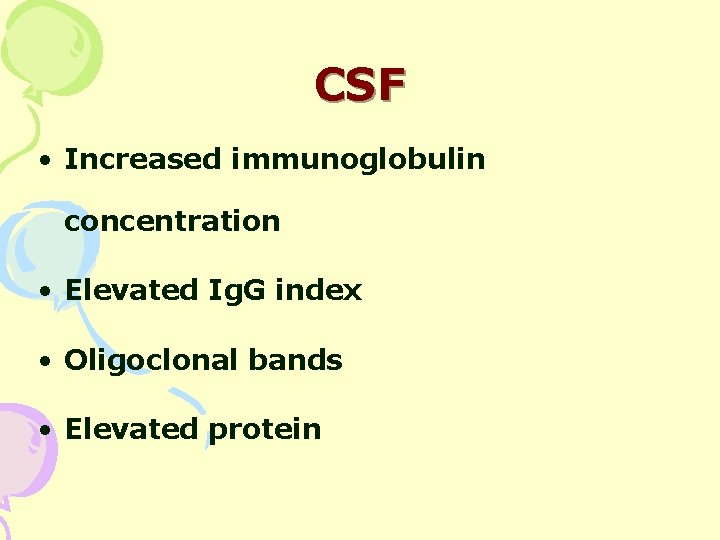
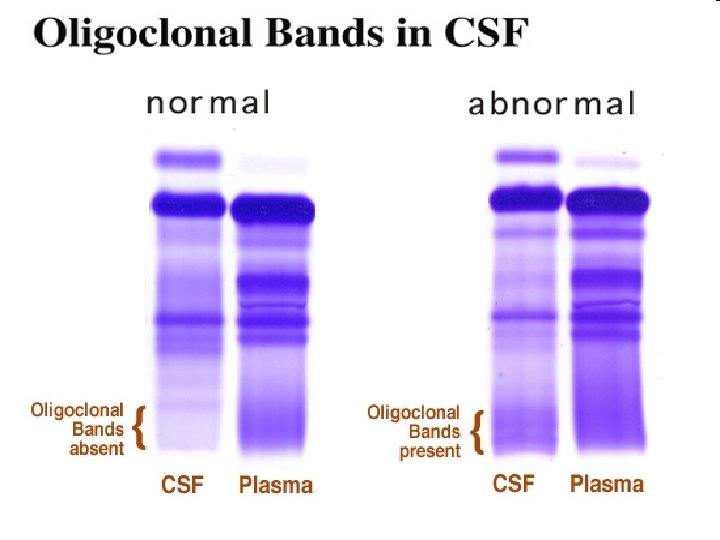
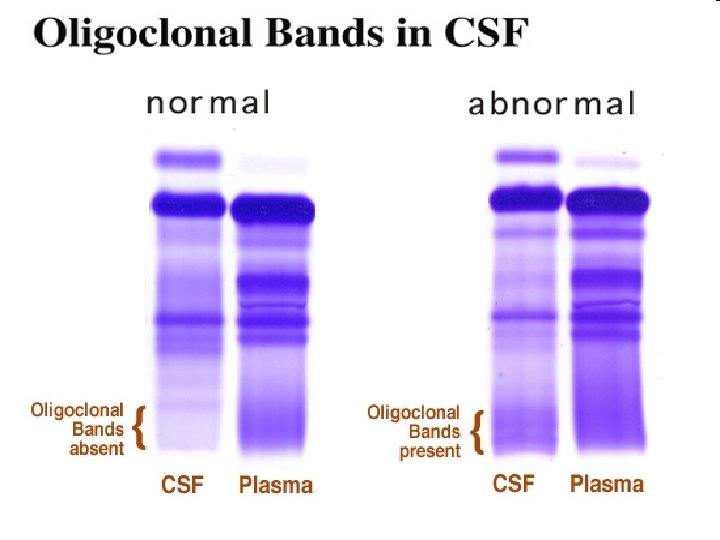
CSF • Increased immunoglobulin concentration • Elevated Ig. G index • Oligoclonal bands • Elevated protein
o
Evoked Potentials • VER (visual evoked response)— 75% abnormal • BAER (brainstem auditory evoked response)— 30% abnormal • SSER (somatosensory evoked response) – 80% abnormal
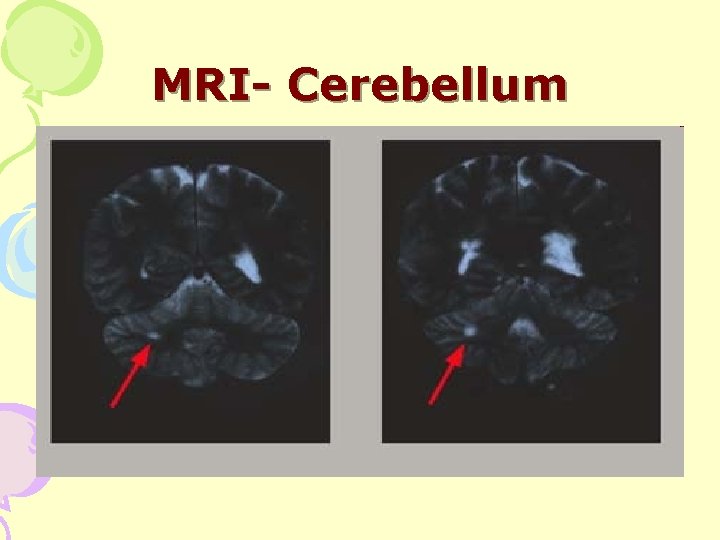
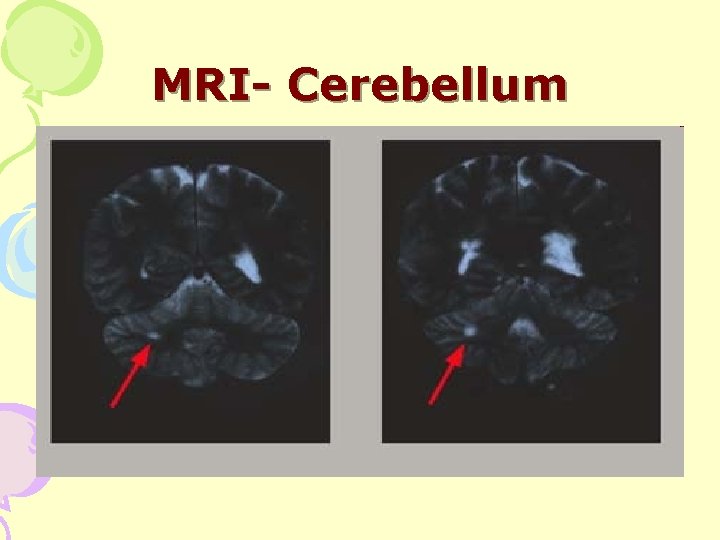
MRI- Cerebellum
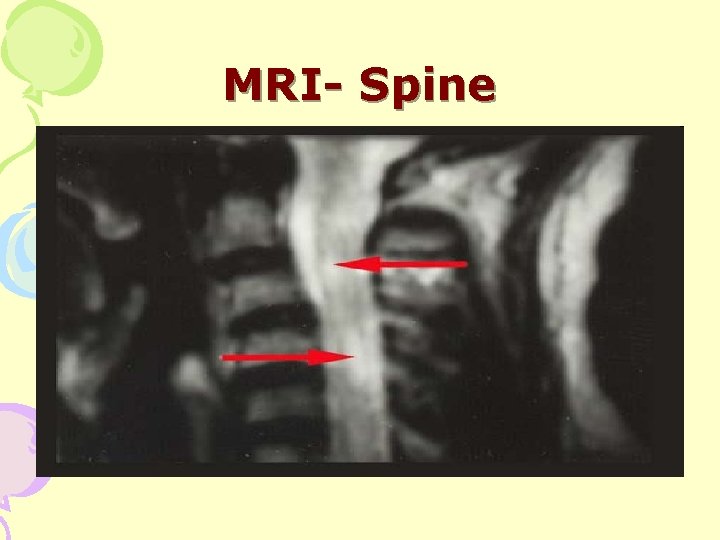
MRI- Spine
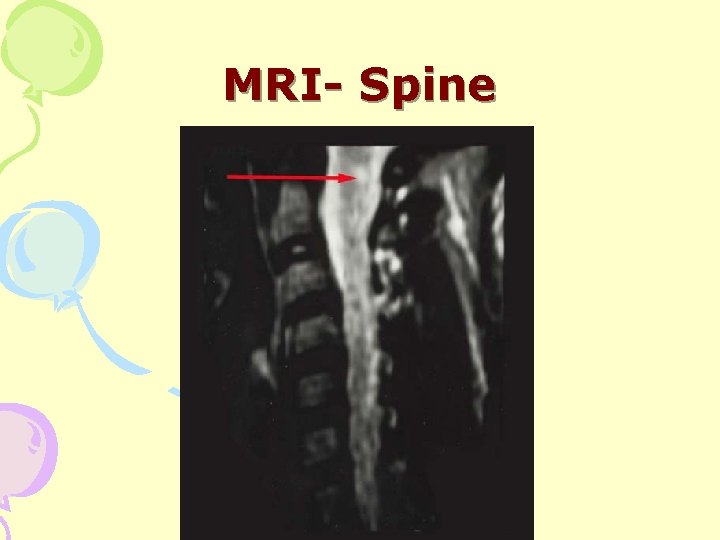
MRI- Spine
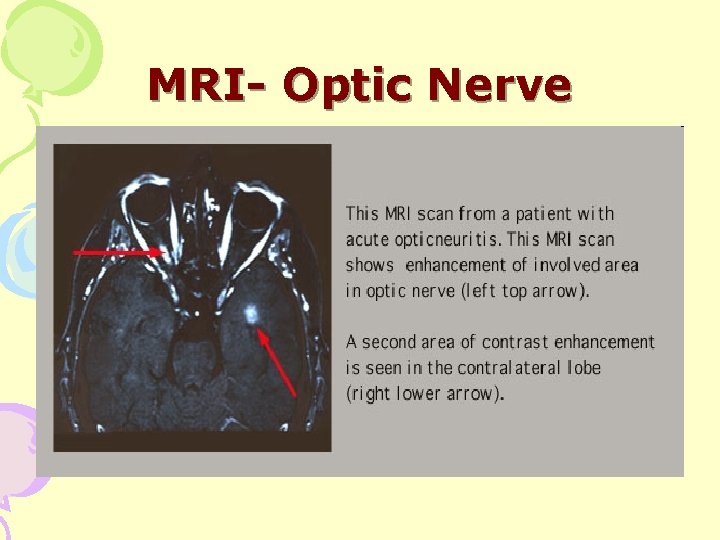
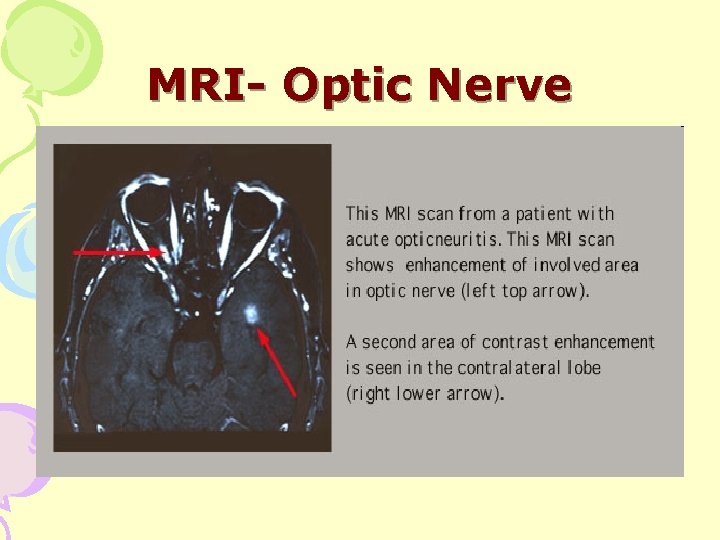
MRI- Optic Nerve

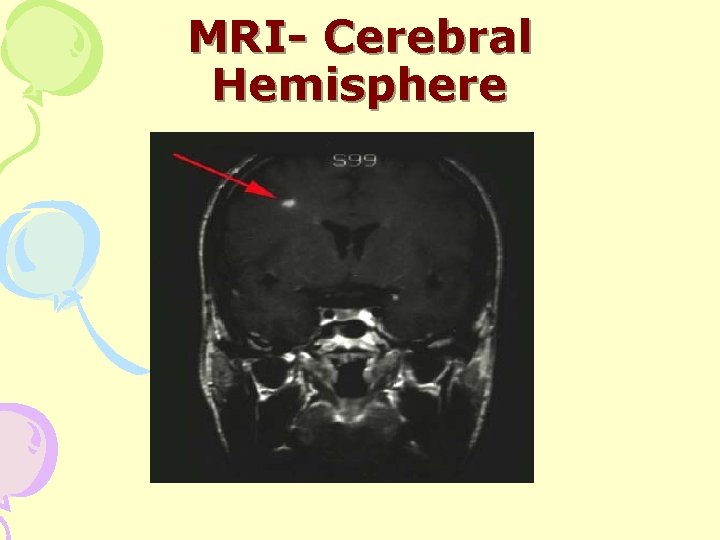
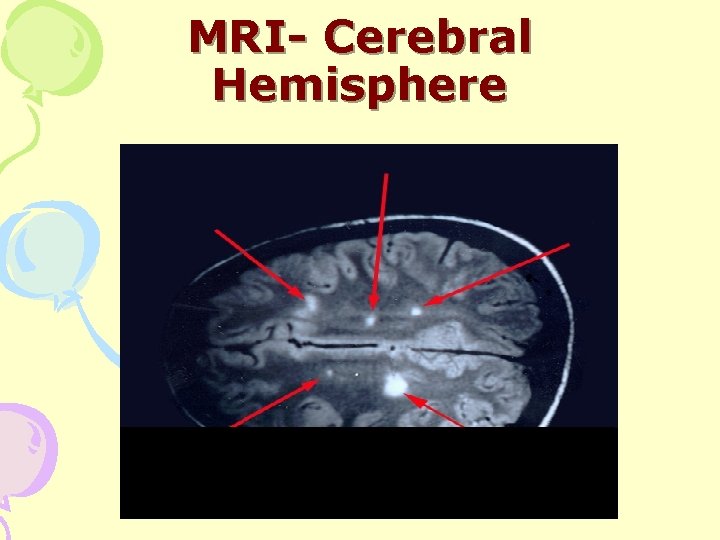
MRI- Cerebral Hemisphere
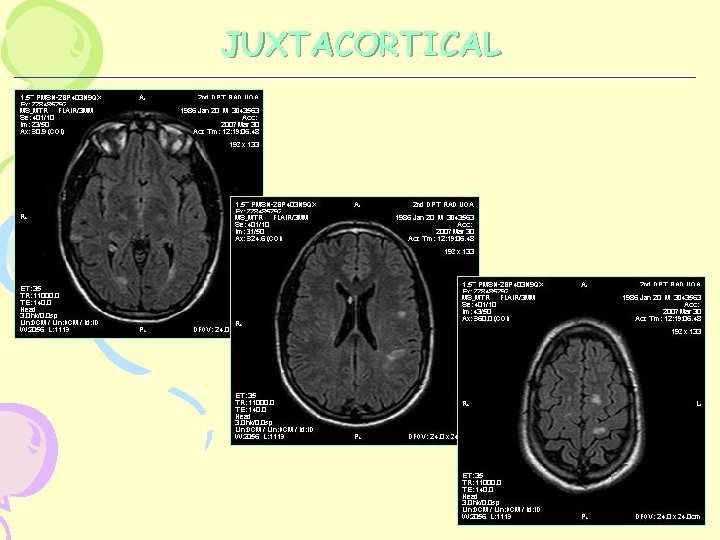
JUXTACORTICAL
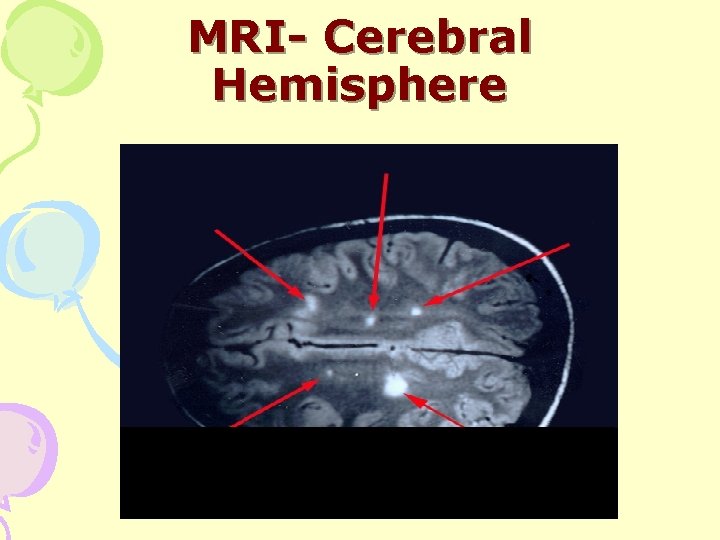
MRI- Cerebral Hemisphere





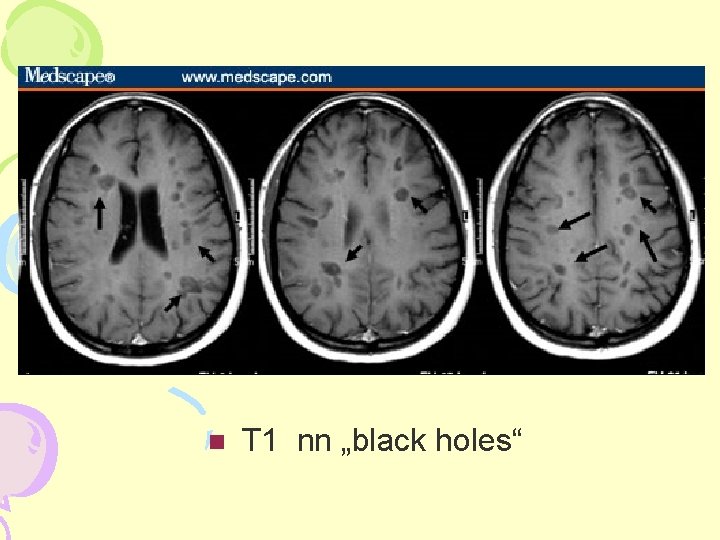
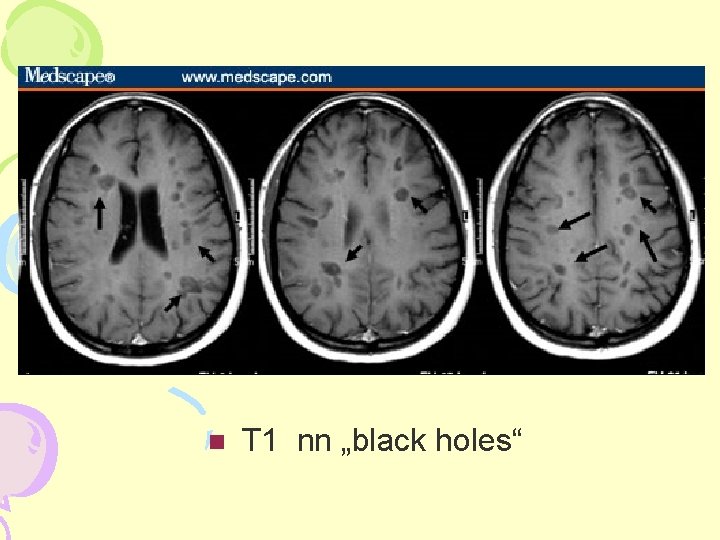
T 1 nn „black holes“

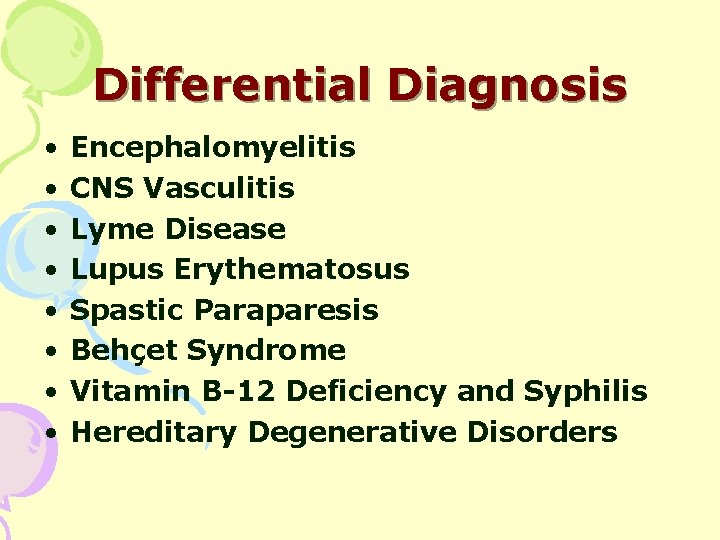
Differential Diagnosis • • Encephalomyelitis CNS Vasculitis Lyme Disease Lupus Erythematosus Spastic Paraparesis Behçet Syndrome Vitamin B-12 Deficiency and Syphilis Hereditary Degenerative Disorders



Standard Therapy • Treatment of Relapses Corticosteroids- Methyl Prednisolone
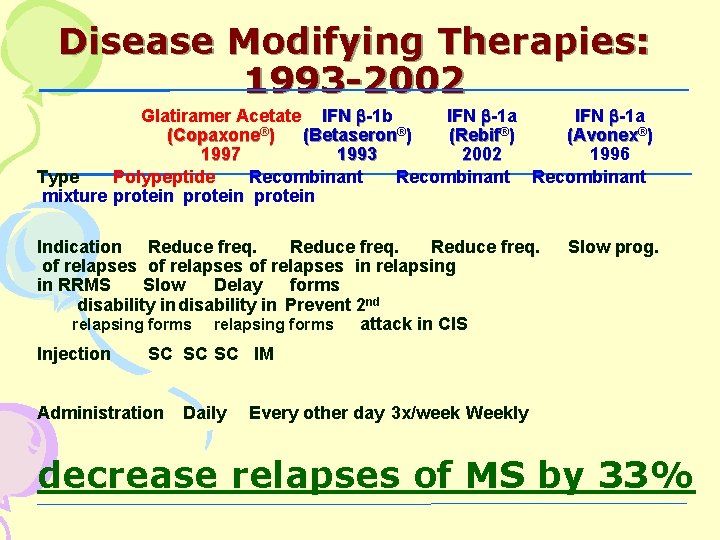
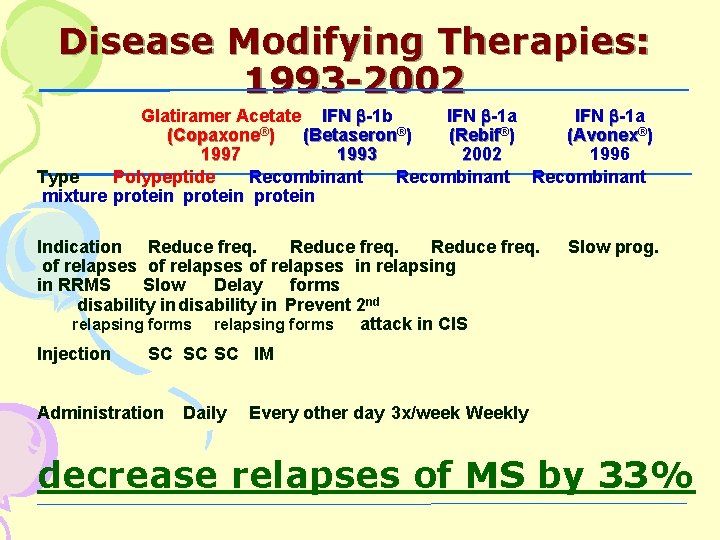
Disease Modifying Therapies: 1993 -2002 Glatiramer Acetate IFN -1 b IFN -1 a ® ® ® (Copaxone ) (Betaseron ) (Rebif ) (Avonex®) 1997 1993 2002 1996 Type Polypeptide Recombinant mixture protein Indication Reduce freq. of relapses in relapsing in RRMS Slow Delay forms disability in Prevent 2 nd relapsing forms attack in CIS Injection Slow prog. SC SC SC IM Administration Daily Every other day 3 x/week Weekly decrease relapses of MS by 33%
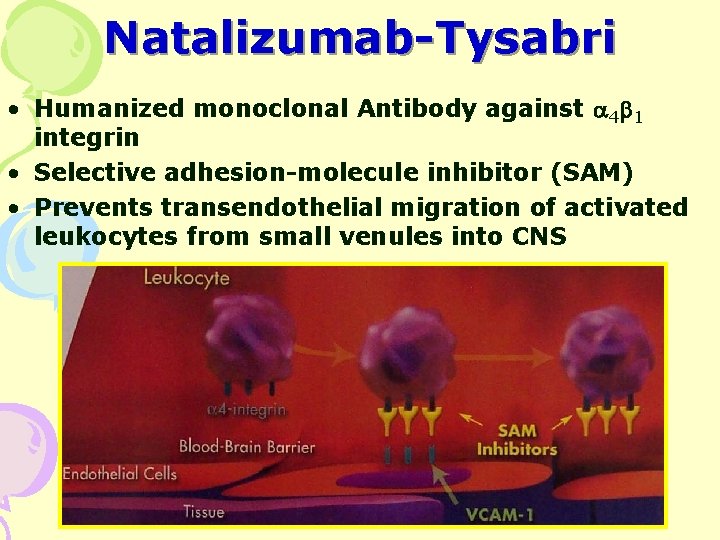
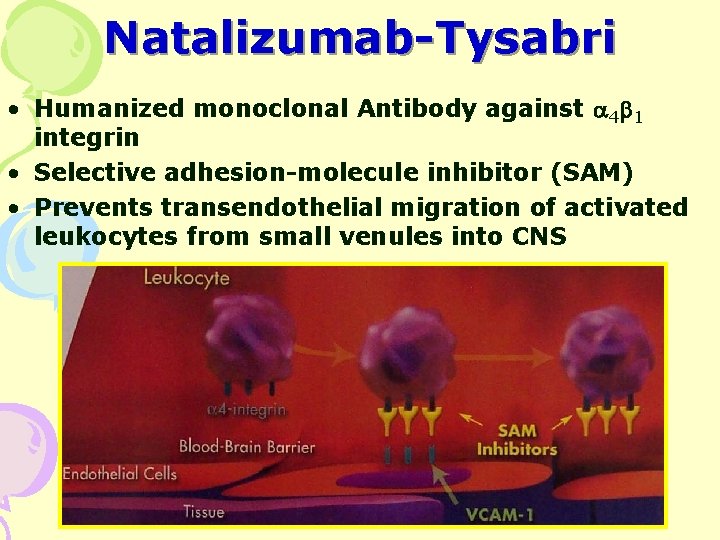
Natalizumab-Tysabri • Humanized monoclonal Antibody against 4 1 integrin • Selective adhesion-molecule inhibitor (SAM) • Prevents transendothelial migration of activated leukocytes from small venules into CNS
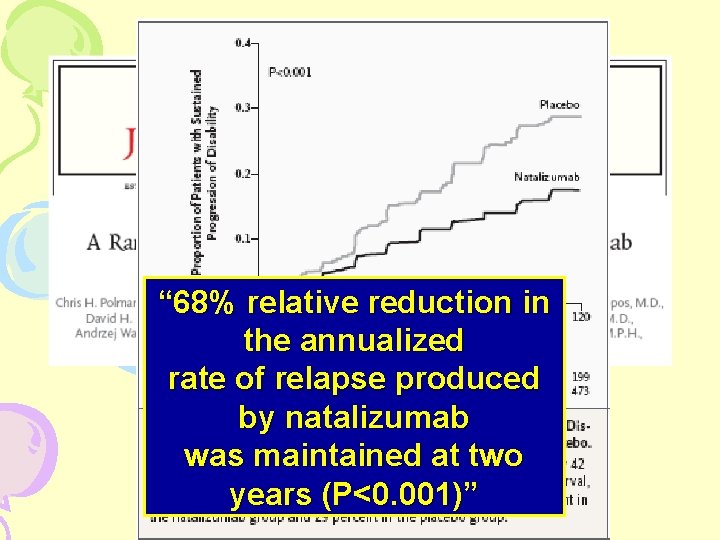
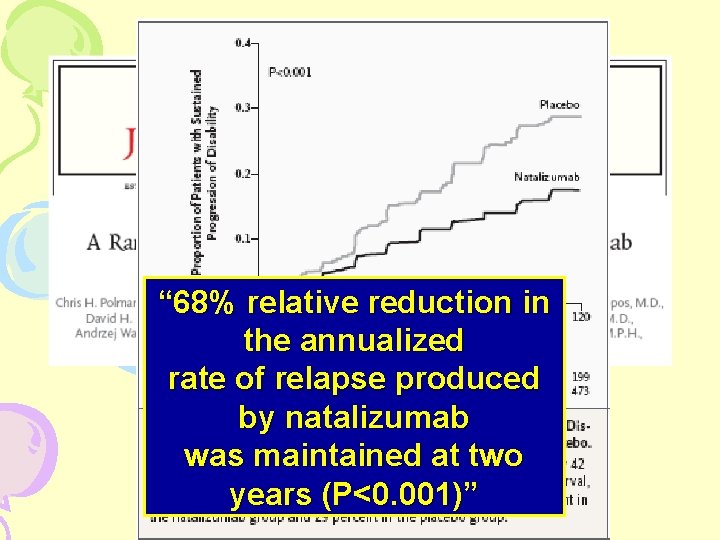
“ 68% relative reduction in the annualized rate of relapse produced by natalizumab was maintained at two years (P<0. 001)”

Newer treatments for RRMS: the return of immunosuppression! • Mitoxantrone • Natalizumab • Oral Treatments (Fingolimod)
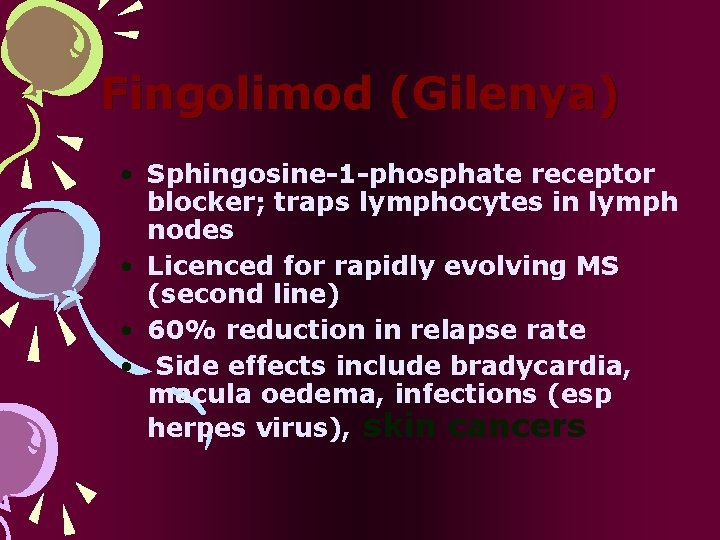
Fingolimod (Gilenya) • Sphingosine-1 -phosphate receptor blocker; traps lymphocytes in lymph nodes • Licenced for rapidly evolving MS (second line) • 60% reduction in relapse rate • Side effects include bradycardia, macula oedema, infections (esp herpes virus), skin cancers
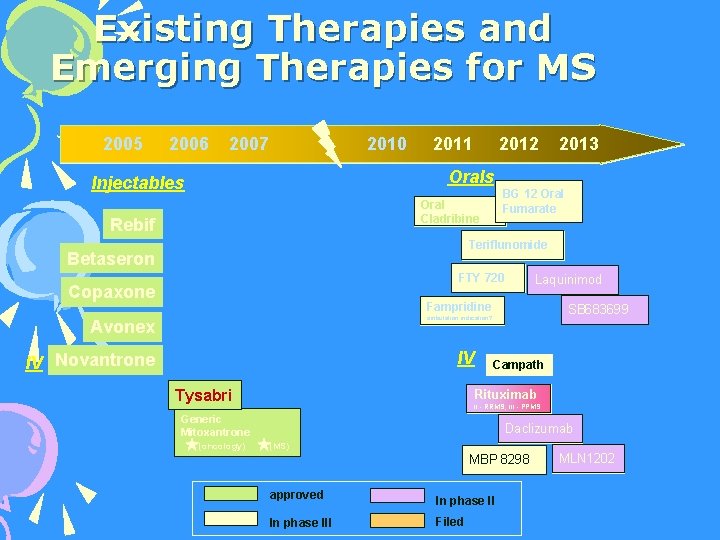
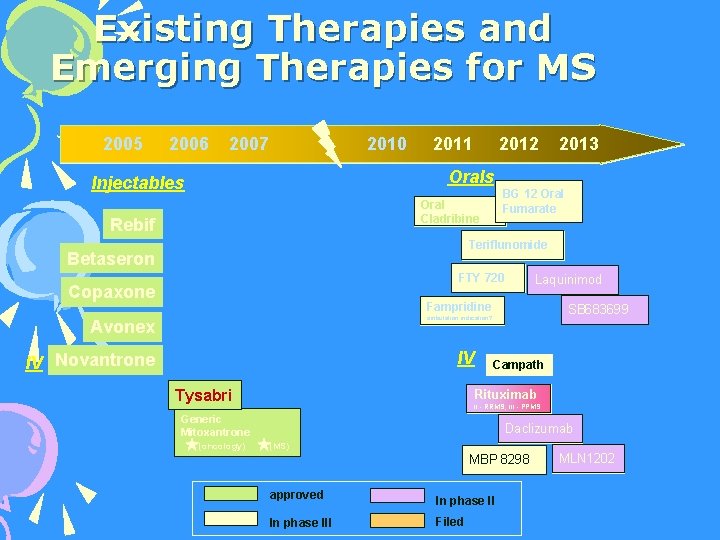
Existing Therapies and Emerging Therapies for MS 2005 2006 2007 2010 2011 2012 2013 Orals Injectables BG 12 Oral Fumarate Oral Cladribine Rebif Teriflunomide Betaseron FTY 720 Copaxone Laquinimod Fampridine SB 683699 ambulation indication? Avonex IV IV Novantrone Tysabri Campath Rituximab II - RRMS; III - PPMS Generic Mitoxantrone (oncology) Daclizumab (MS) MBP 8298 approved In phase III Filed MLN 1202
Complications • Respiratory failure • Pneumonia • Neurologic deficits: paralysis. • UTI • Sexual dysfunction • Contractures
Factors that influence prognosis • Females • Low rate of relapses per year • Complete recovery from the first attack • Long interval between first and second attack • Low disability at 2 to 5 years from the disease onset
Factors that influence prognosis • Symptoms predominantly from afferent systems (i. e. , . sensory symptoms) • Younger age of onset • Later cerebellar involvement • Involvement of only one CNS system at the time of onset
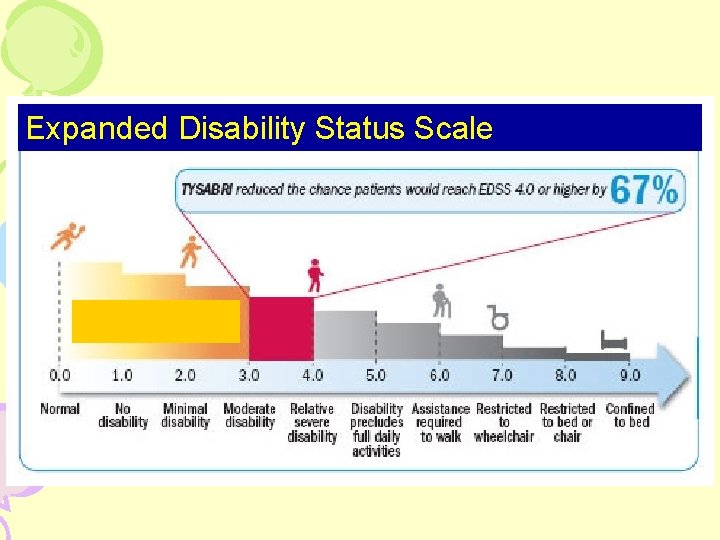
What Happens? • 50% of MS patients will need help walking within 15 years of disease onset • Life Expectancy: – 82. 5% of normal • 58 years old
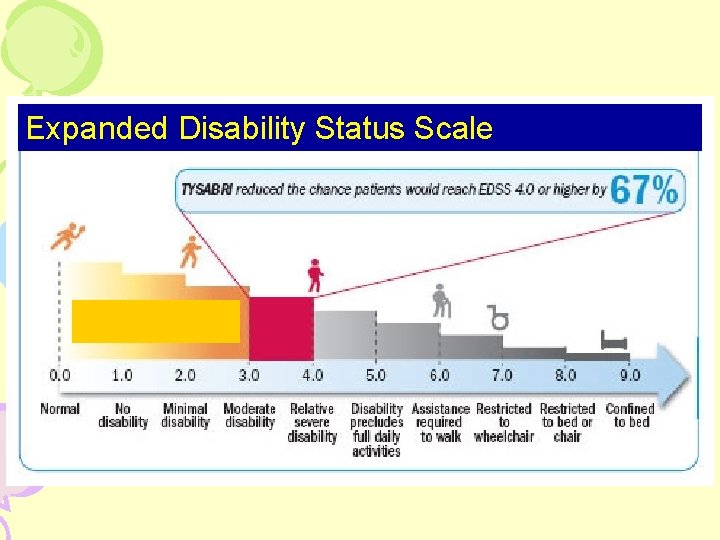
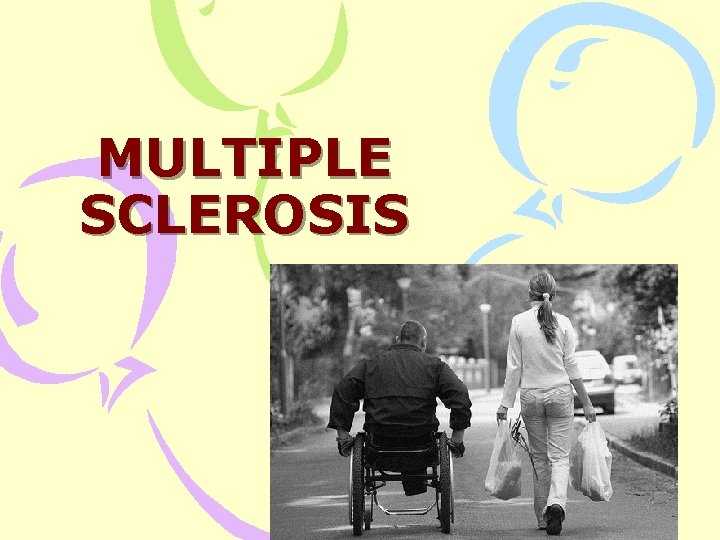
Expanded Disability Status Scale
