Chapter 24 Drugs for Neuromuscular Disorders Myasthenia Gravis
- Slides: 28
Chapter 24 Drugs for Neuromuscular Disorders: Myasthenia Gravis, Multiple Sclerosis, and Muscle Spasms Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc.
Myasthenia Gravis (MG) Pathophysiology Autoimmune disorder Lack of nerve impulses and muscle responses at myoneural junction Ø Inadequate secretion of acetylcholine (ACh) Ø Loss of ACh because of an increase in the enzyme acetylcholinesterase Ø Thymus gland Ø Ø Characteristics Ø Ø Muscular weakness and fatigue Respiratory muscle paralysis, ptosis, difficulty chewing and swallowing Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 2
Acetylcholinesterase Inhibitors/Cholinesterase Inhibitors Acetylcholinesterase inhibitors (ACh. E inhibitors) Neostigmine (Prostigmin): short-acting Edrophonium (Tensilon): ultrashort-acting for diagnosing Ø Pyridostigmine (Mestinon): intermediate-acting Ø Ambenonium (Mytelase): long-acting Ø Action • Transmission of neuromuscular impulses by preventing Ø Ø destruction of Ach Ø Use • Control and treat MG Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 3
Patients Not Responding to Acetylcholinesterase Inhibitors Prednisone Plasma exchange Intravenous immune globulin (IVIG) or immunosuppressive drugs Ø Azathioprine (Imuran) Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 4
ACh. E Inhibitors Overdosing and underdosing Ø Ø Ø Similar symptoms Muscle weakness, dyspnea Dysphagia, abdominal cramping Drooling, increases tearing, sweating Bradycardia Myasthenia crisis: underdosed Cholinergic crisis: overdosed Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 5
Myasthenia Gravis (Cont. ) Myasthenic crisis Severe muscle weakness • May involve diaphragm and intercostal muscles Ø Triggers: • Inadequate dosing • Infection • Emotional stress • Menses, pregnancy • Surgery, trauma • Hypokalemia, alcohol intake • Medication interactions Ø Improves after edrophonium (Tensilon) and neostigmine (Prostigmin) Ø Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 6
Myasthenia Gravis (Cont. ) Cholinergic crisis Usually occurs within 30 to 60 minutes after taking anticholinergic medications Ø Severe muscle weakness • Possible respiratory paralysis and arrest • Abnormal pupil constriction • Excess salivation • Pallor, sweating, vertigo • GI distress • Bradycardia • Fasciculations Ø Worsens after edrophonium chloride (Tensilon) Ø Triggers • Overdosing Ø Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 7
ACh. E Inhibitors (Cont. ) Side effects GI disturbances (nausea, vomiting, diarrhea, abdominal cramps) Ø Increased salivation Ø Tearing Ø Miosis (constricted pupil of the eye) Ø Blurred vision Ø Bradycardia Ø Hypotension Ø Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 8
Nursing Process: ACh. E Inhibitors Assessment Nursing diagnosis Planning Nursing interventions Ø Ø Patient teaching Cultural considerations Evaluation Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 9
Nursing Process: ACh. E Inhibitors Nursing interventions Administer doses on time. Take drug before meals if possible. Monitor drug effectiveness. Have antidote available for cholinergic crisis. • Atropine Ø Encourage patient to wear medical identification. Ø Ø Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 10
Multiple Sclerosis (MS) Pathophysiology Autoimmune disorder Attacks myelin sheath of nerve fibers in brain and spinal cord Ø Causes lesions or plaques Ø Ø Characteristics Ø Ø Remissions and exacerbations Weakness Spasticity in extremities Diplopia Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 11
Multiple Sclerosis (Cont. ) Diagnosis Ø Ø Ø No specific diagnostic test Mc. Donald Criteria Laboratory tests that may suggest MS include • Elevated immunoglobulin G (Ig. G) in the cerebrospinal fluid • Increased Ig. G/albumin ratio • Multiple lesions observable through MRI Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 12
Multiple Sclerosis Treatment Acute attack: tapering course of glucocorticoids (prednisone), adrenocorticotropic hormone (ACTH) (H. P. Acthar) Remission-exacerbation: biologic (immune) response modifiers (BRMs) Chronic progressive: immunosuppressant therapy Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 13
Skeletal Muscle Relaxants Spasticity (Centrally acting) Ø Ø Baclofen (Lioresal) Tizanidine (Zanaflex) Spasticity (Direct acting) Ø Dantrolene sodium (Dantrium) Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 14
Skeletal Muscle Relaxants (Cont. ) Centrally acting muscle relaxants Ø Ø Ø Carisoprodol (Soma) Chlorzoxazone (Parafon forte DSC) Methocarbamol (Robaxin) Metaxalone (Skelaxin) Orphenadrine citrate (Norflex) Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 15
Skeletal Muscle Relaxants (Cont. ) Depolarizing muscle relaxants (adjunct to anesthesia) Ø Ø Pancuronium bromide (Pavulon) Succinylcholine (Anectine) Vecuronium (Norcuron) Tubocurarine Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 16
Skeletal Muscle Relaxants (Cont. ) Cyclobenzaprine (Flexeril) Action • Relax skeletal muscles Ø Use • Alleviates muscle spasm associated with acute painful Ø musculoskeletal conditions Ø Side effects • Anticholinergic effects • Drowsiness; dizziness • Headache • Fever • Abdominal pain; vomiting; diarrhea; flatulence • Erectile dysfunction Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 17
Nursing Process: Skeletal Muscle Relaxants Assessment Nursing diagnoses Planning Nursing interventions Ø Ø Patient teaching Cultural considerations Evaluation Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 18
Nursing Process: Skeletal Muscle Relaxants (Cont. ) Nursing Interventions Take with food. Monitor liver function. Check vital signs. Advise patient not to drive. Inform patient that most centrally acting muscle relaxants are prescribed for no longer than 3 weeks. Ø Teach patient not to stop abruptly. • Discontinue over 1 week to avoid rebound spasms. Ø Have patient avoid alcohol and other depressants. Ø Ø Ø Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 19
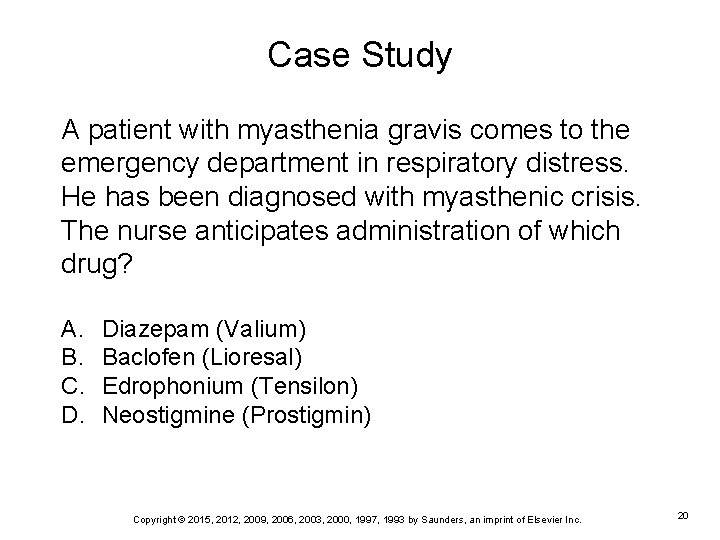
Case Study A patient with myasthenia gravis comes to the emergency department in respiratory distress. He has been diagnosed with myasthenic crisis. The nurse anticipates administration of which drug? A. B. C. D. Diazepam (Valium) Baclofen (Lioresal) Edrophonium (Tensilon) Neostigmine (Prostigmin) Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 20
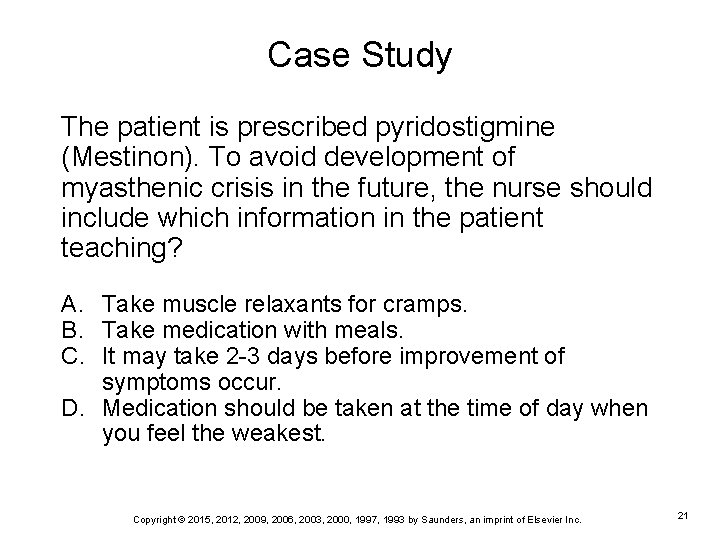
Case Study The patient is prescribed pyridostigmine (Mestinon). To avoid development of myasthenic crisis in the future, the nurse should include which information in the patient teaching? A. Take muscle relaxants for cramps. B. Take medication with meals. C. It may take 2 -3 days before improvement of symptoms occur. D. Medication should be taken at the time of day when you feel the weakest. Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 21
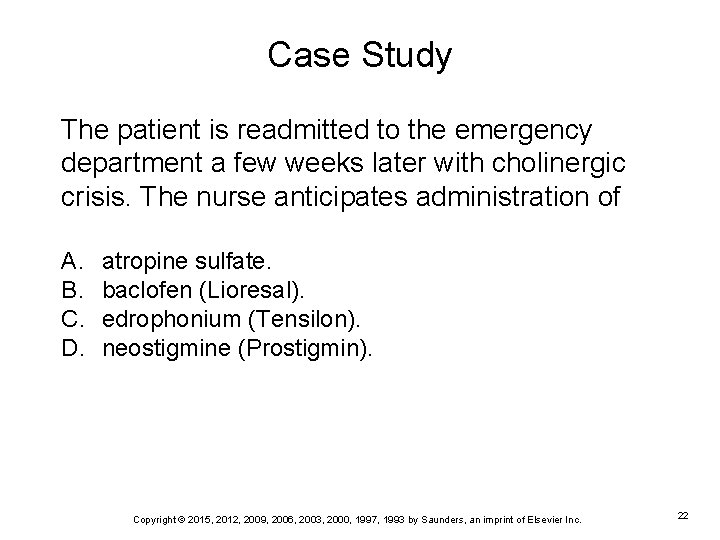
Case Study The patient is readmitted to the emergency department a few weeks later with cholinergic crisis. The nurse anticipates administration of A. B. C. D. atropine sulfate. baclofen (Lioresal). edrophonium (Tensilon). neostigmine (Prostigmin). Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 22
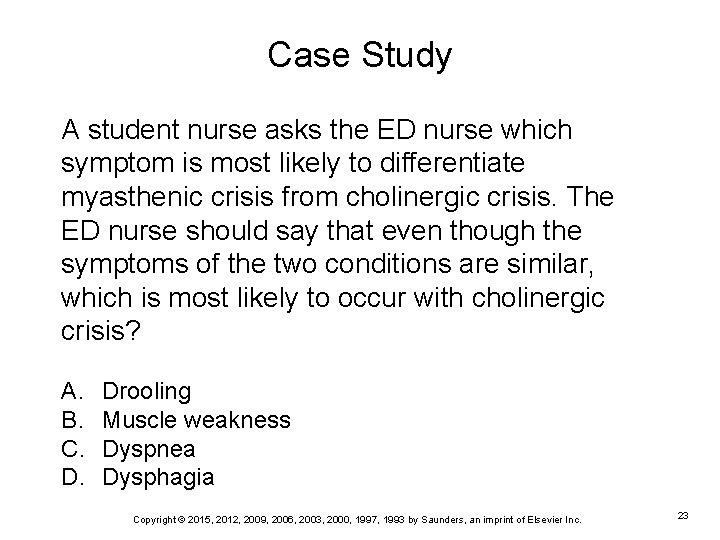
Case Study A student nurse asks the ED nurse which symptom is most likely to differentiate myasthenic crisis from cholinergic crisis. The ED nurse should say that even though the symptoms of the two conditions are similar, which is most likely to occur with cholinergic crisis? A. B. C. D. Drooling Muscle weakness Dyspnea Dysphagia Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 23
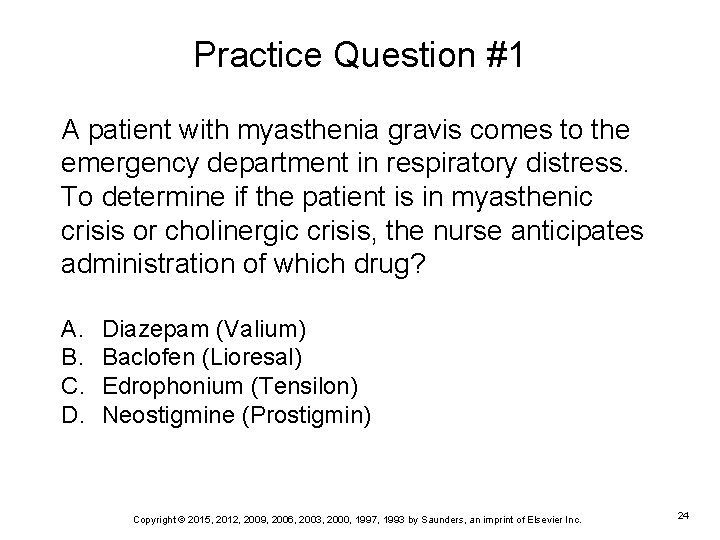
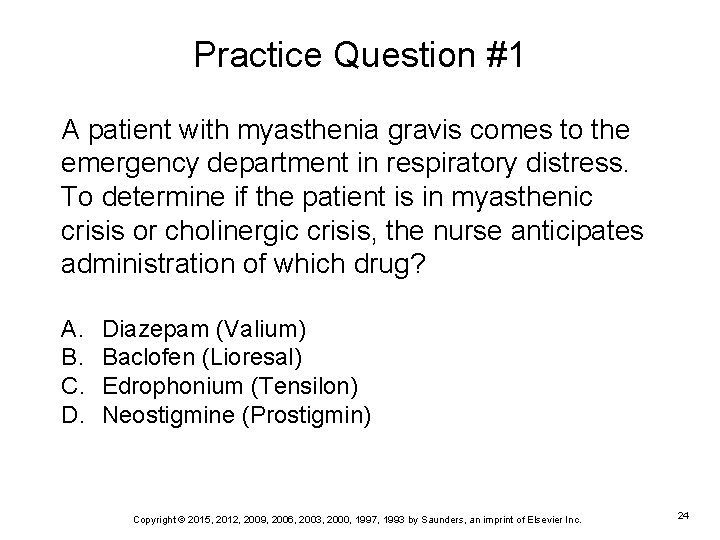
Practice Question #1 A patient with myasthenia gravis comes to the emergency department in respiratory distress. To determine if the patient is in myasthenic crisis or cholinergic crisis, the nurse anticipates administration of which drug? A. B. C. D. Diazepam (Valium) Baclofen (Lioresal) Edrophonium (Tensilon) Neostigmine (Prostigmin) Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 24
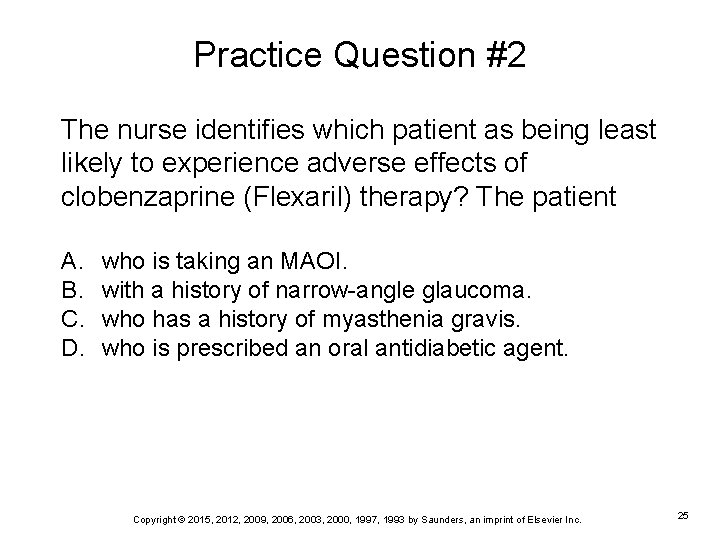
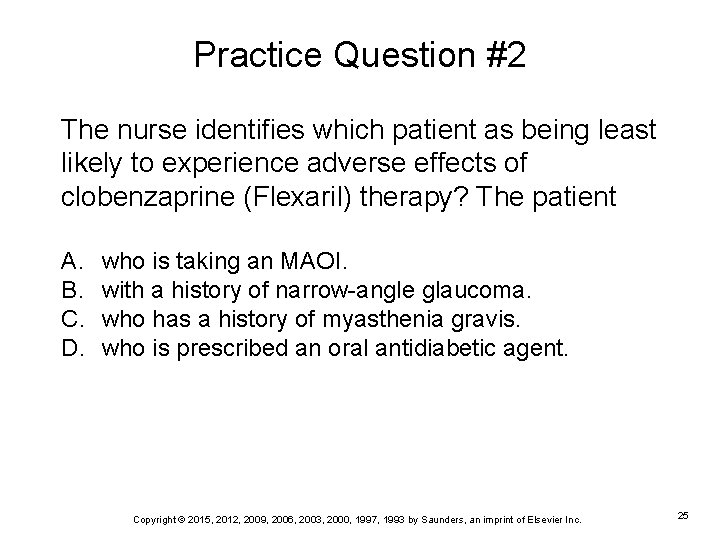
Practice Question #2 The nurse identifies which patient as being least likely to experience adverse effects of clobenzaprine (Flexaril) therapy? The patient A. B. C. D. who is taking an MAOI. with a history of narrow-angle glaucoma. who has a history of myasthenia gravis. who is prescribed an oral antidiabetic agent. Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 25
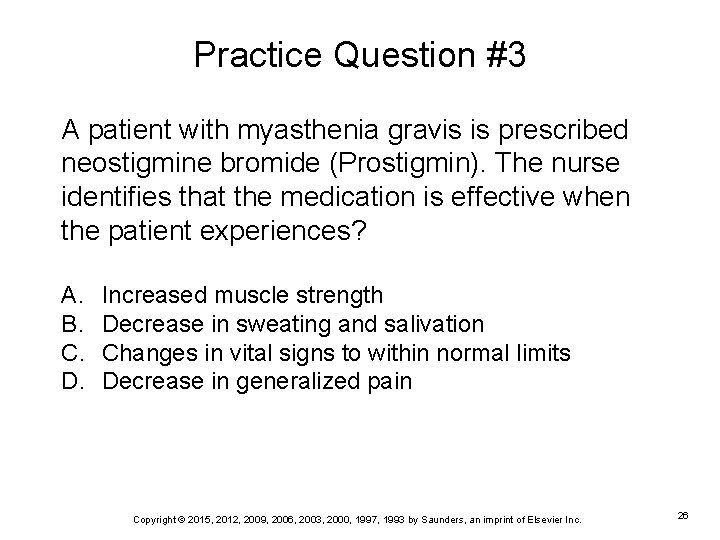
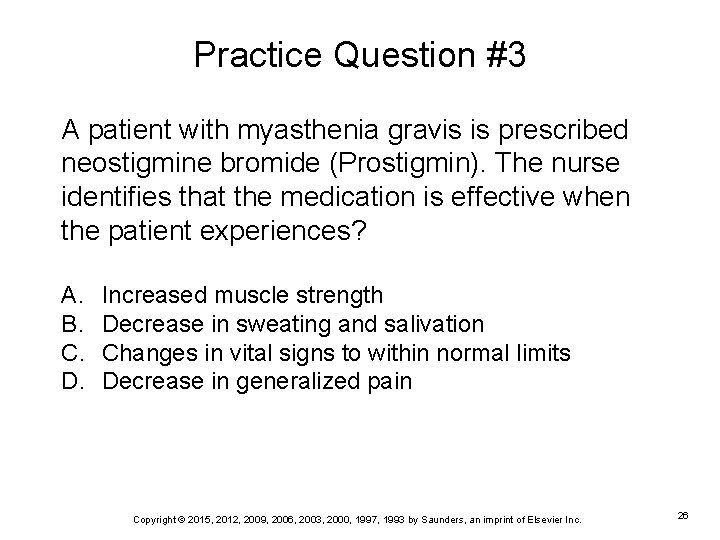
Practice Question #3 A patient with myasthenia gravis is prescribed neostigmine bromide (Prostigmin). The nurse identifies that the medication is effective when the patient experiences? A. B. C. D. Increased muscle strength Decrease in sweating and salivation Changes in vital signs to within normal limits Decrease in generalized pain Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 26
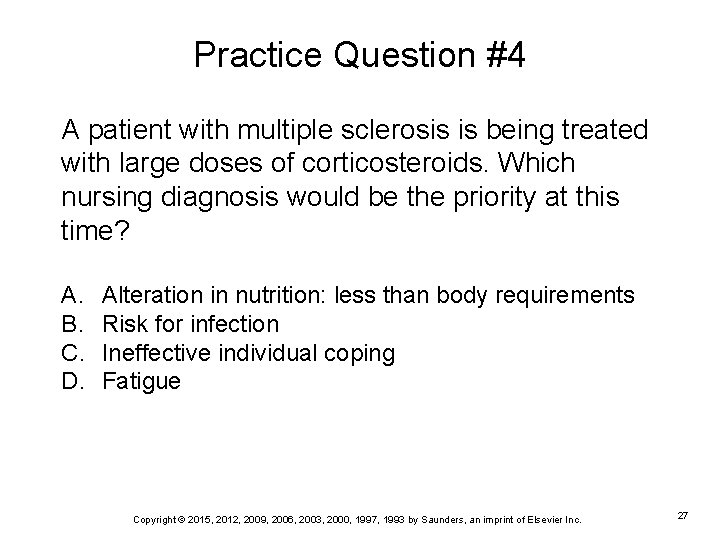
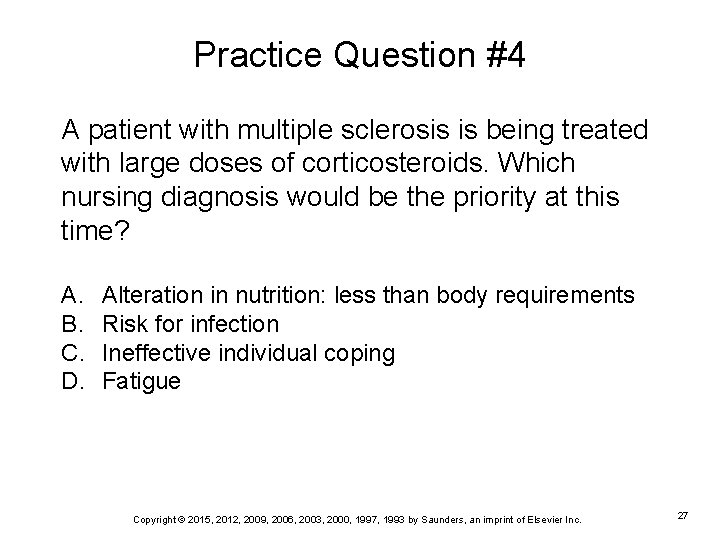
Practice Question #4 A patient with multiple sclerosis is being treated with large doses of corticosteroids. Which nursing diagnosis would be the priority at this time? A. B. C. D. Alteration in nutrition: less than body requirements Risk for infection Ineffective individual coping Fatigue Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 27
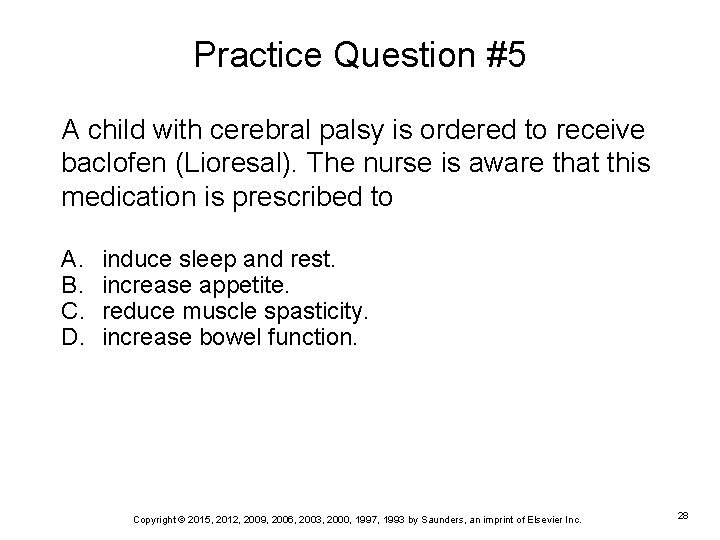
Practice Question #5 A child with cerebral palsy is ordered to receive baclofen (Lioresal). The nurse is aware that this medication is prescribed to A. B. C. D. induce sleep and rest. increase appetite. reduce muscle spasticity. increase bowel function. Copyright © 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc. 28
 Myasthenia gravis oireet
Myasthenia gravis oireet Concept map of assessment
Concept map of assessment Exercise with myasthenia gravis
Exercise with myasthenia gravis Myasthenia gravis thymectomy
Myasthenia gravis thymectomy Myasthenia gravis clinical presentation
Myasthenia gravis clinical presentation Wartenberg test
Wartenberg test Anemia
Anemia Myasthenia gravis definition
Myasthenia gravis definition Myasthenia gravis eyes
Myasthenia gravis eyes What is myasthenia gravis
What is myasthenia gravis Myasthenia gravis
Myasthenia gravis Itk sisekliinik
Itk sisekliinik Hypersenzitivita
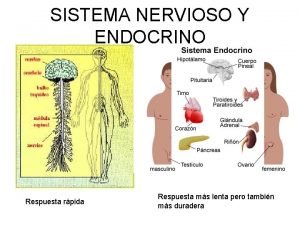
Hypersenzitivita Acondicionamiento neuromuscular dibujos
Acondicionamiento neuromuscular dibujos Pnf techniques definition
Pnf techniques definition Hypocalcemia neuromuscular excitability
Hypocalcemia neuromuscular excitability Sequence of events at neuromuscular junction
Sequence of events at neuromuscular junction Huso neuromuscular
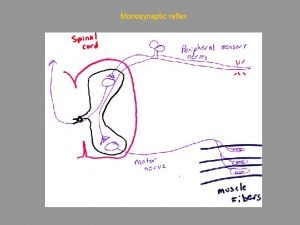
Huso neuromuscular Type of reflex arc
Type of reflex arc Neuromuscular
Neuromuscular Piridostigmine
Piridostigmine Focus figure 9.1: events at the neuromuscular junction
Focus figure 9.1: events at the neuromuscular junction Succinylcholine dose
Succinylcholine dose Neuromuscular junction
Neuromuscular junction Neuromuscular junction
Neuromuscular junction Sistema nervioso para niños
Sistema nervioso para niños Neuromuscular blocking agents
Neuromuscular blocking agents Overview figure
Overview figure Placa neuro muscular
Placa neuro muscular