General anesthesia Definition of anesthesia It is a
- Slides: 41
General anesthesia
�Definition of anesthesia It is a reversable blocking of pain feeling in whole body or in a part of it using pharmacology or other methods
Anesthesia- division Local- regional anesthesia, patient is conscious or sedated General- anesthesia interact with whole body, function of central nervous system is depressed: – Intravenous – Inhalation (volatile) – Combined, balanced
TIVA Total Intra Venous Anaesthesia VIMA Volatile Induction and Maintain Anaesthesia
Parts of general anesthesia Hypnosis- pharmacological sleep, reversable lack of consciousness � Analgesia-pain management � Areflexio-lack of reflexes � Relaxatio musculorum- muscle relaxation, pharmacological reversable neuromuscular blockade �
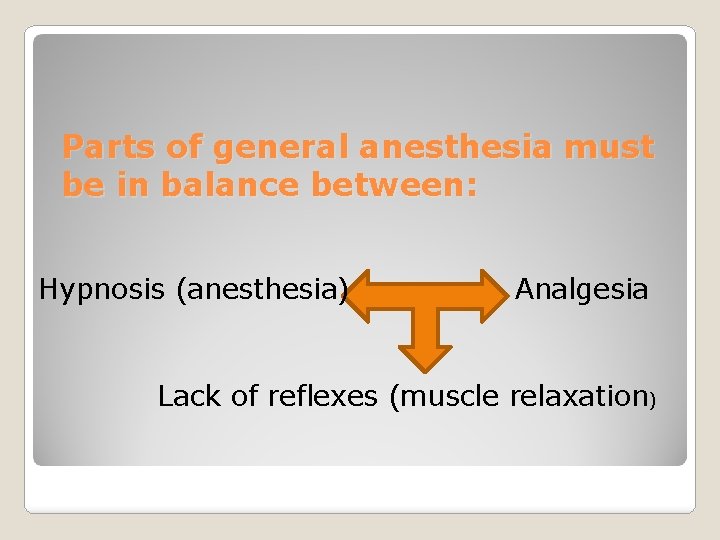
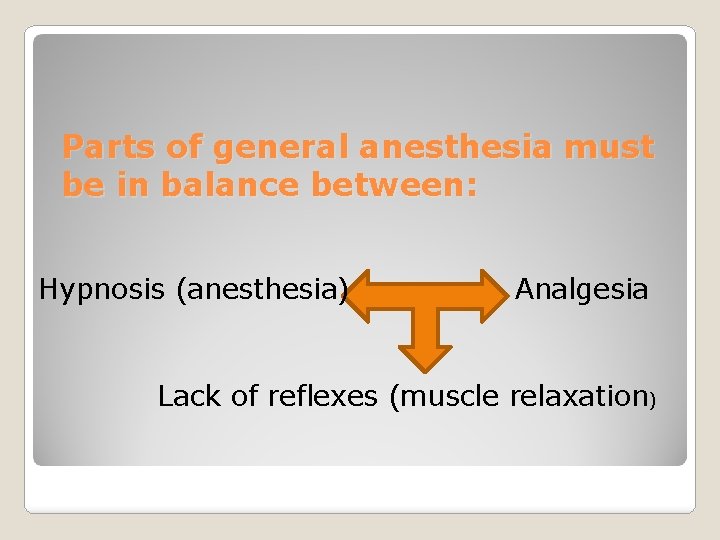
Parts of general anesthesia must be in balance between: Hypnosis (anesthesia) Analgesia Lack of reflexes (muscle relaxation)
�Features � 1 of General anesthesia Lack of consciousness � 2 Pain management � 3 Lack of reflexes � 4 Neuromuscular blockade
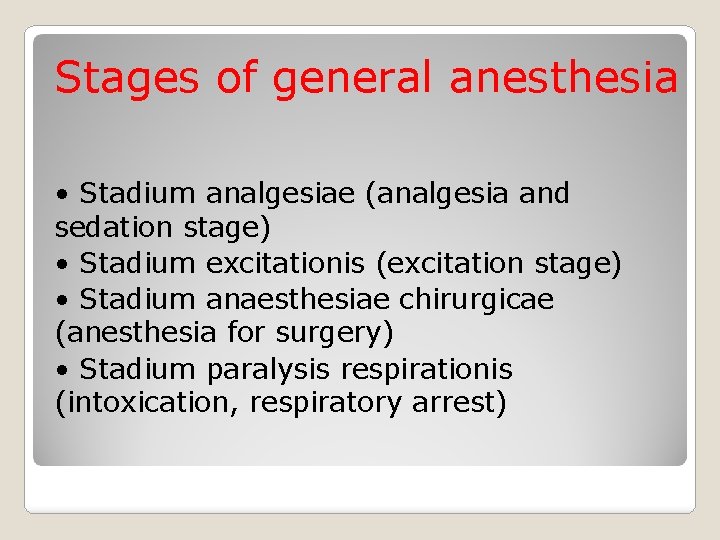
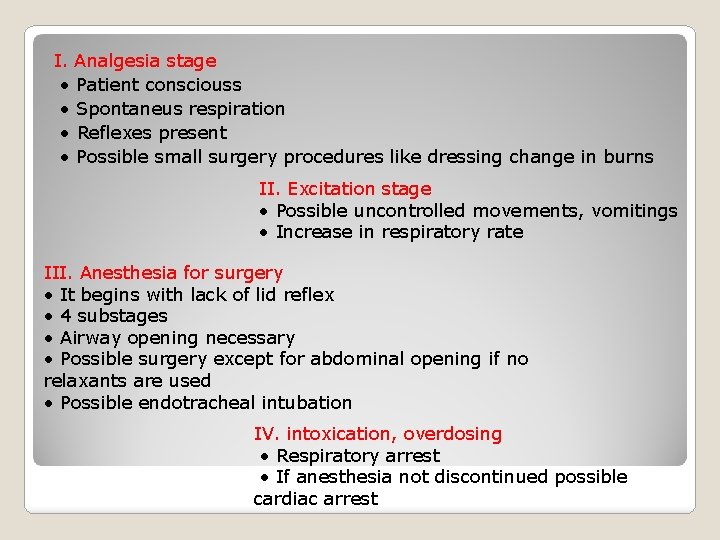
Stages of general anesthesia • Stadium analgesiae (analgesia and sedation stage) • Stadium excitationis (excitation stage) • Stadium anaesthesiae chirurgicae (anesthesia for surgery) • Stadium paralysis respirationis (intoxication, respiratory arrest)
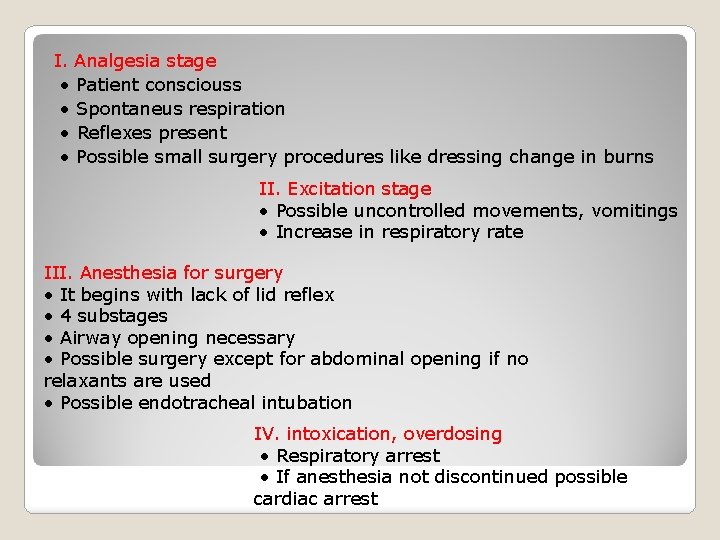
I. Analgesia stage • Patient consciouss • Spontaneus respiration • Reflexes present • Possible small surgery procedures like dressing change in burns II. Excitation stage • Possible uncontrolled movements, vomitings • Increase in respiratory rate III. Anesthesia for surgery • It begins with lack of lid reflex • 4 substages • Airway opening necessary • Possible surgery except for abdominal opening if no relaxants are used • Possible endotracheal intubation IV. intoxication, overdosing • Respiratory arrest • If anesthesia not discontinued possible cardiac arrest
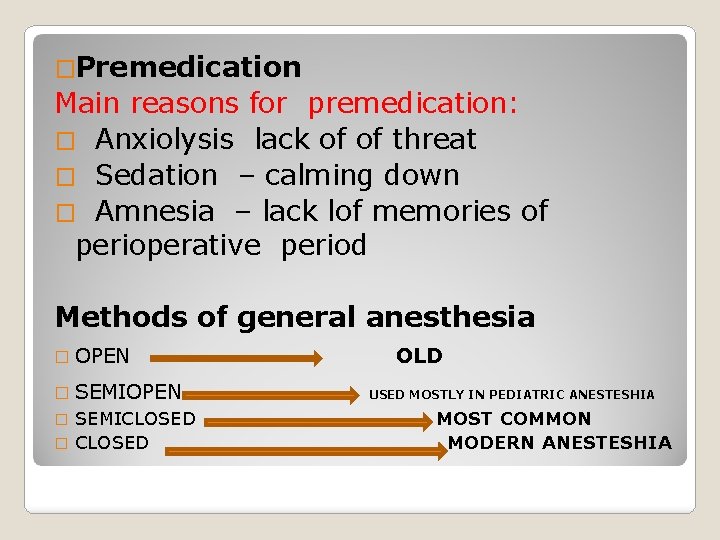
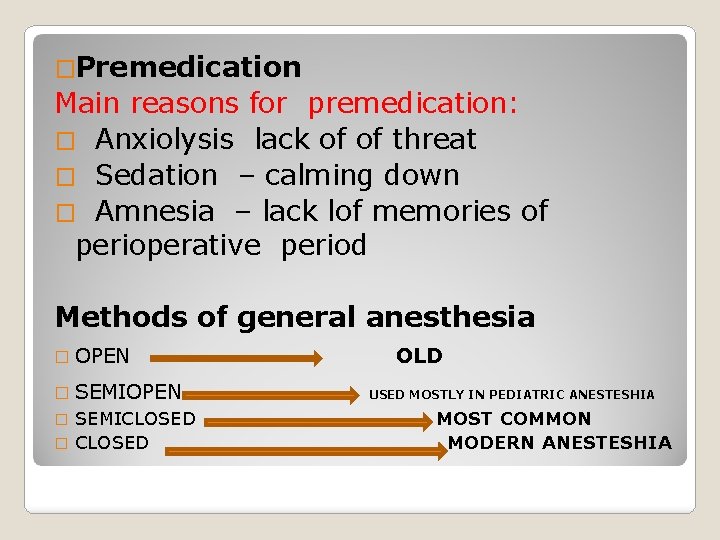
�Premedication Main reasons for premedication: � Anxiolysis lack of of threat � Sedation – calming down � Amnesia – lack lof memories of perioperative period Methods of general anesthesia � OPEN � SEMIOPEN SEMICLOSED � OLD USED MOSTLY IN PEDIATRIC ANESTESHIA MOST COMMON MODERN ANESTESHIA
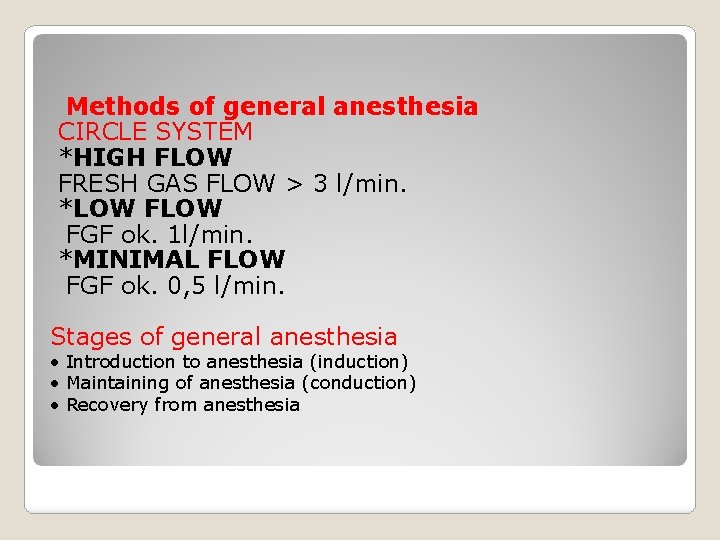
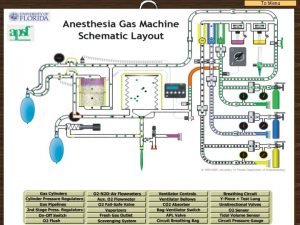
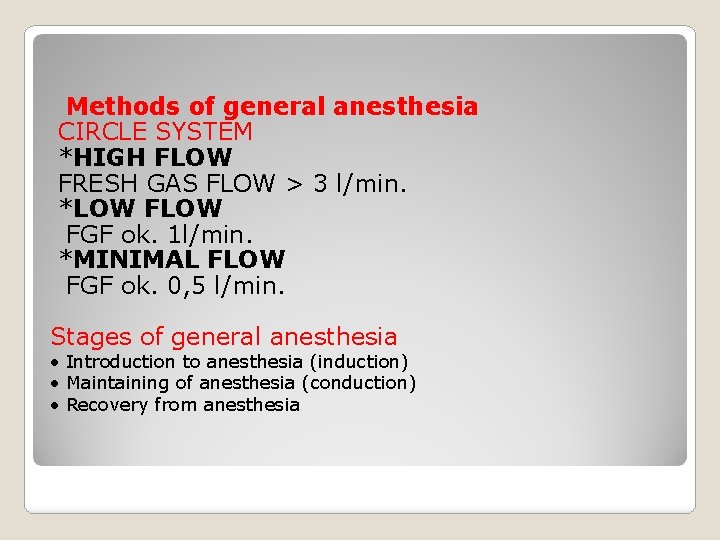
Methods of general anesthesia CIRCLE SYSTEM *HIGH FLOW FRESH GAS FLOW > 3 l/min. *LOW FGF ok. 1 l/min. *MINIMAL FLOW FGF ok. 0, 5 l/min. Stages of general anesthesia • Introduction to anesthesia (induction) • Maintaining of anesthesia (conduction) • Recovery from anesthesia
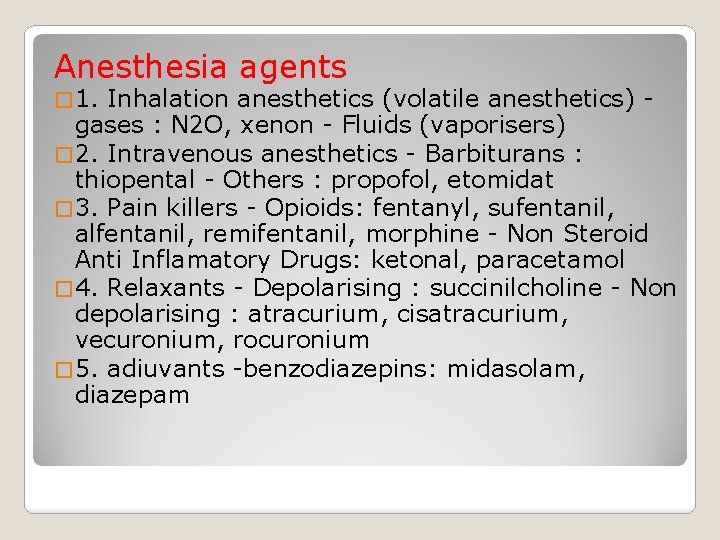
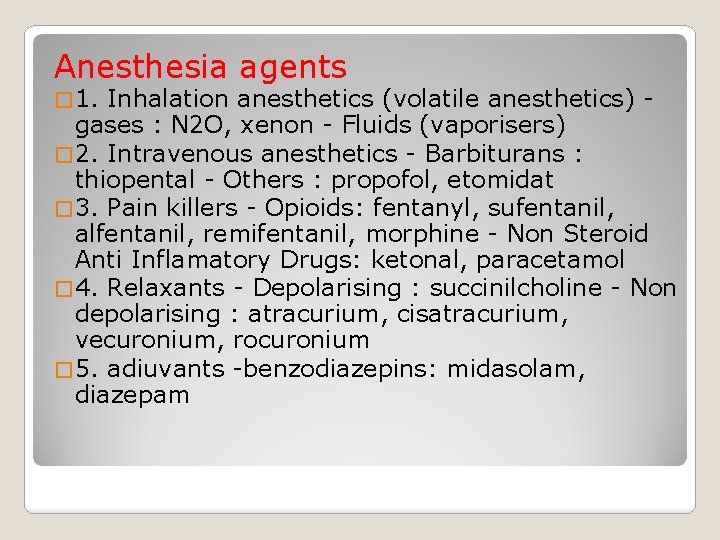
Anesthesia agents � 1. Inhalation anesthetics (volatile anesthetics) gases : N 2 O, xenon - Fluids (vaporisers) � 2. Intravenous anesthetics - Barbiturans : thiopental - Others : propofol, etomidat � 3. Pain killers - Opioids: fentanyl, sufentanil, alfentanil, remifentanil, morphine - Non Steroid Anti Inflamatory Drugs: ketonal, paracetamol � 4. Relaxants - Depolarising : succinilcholine - Non depolarising : atracurium, cisatracurium, vecuronium, rocuronium � 5. adiuvants -benzodiazepins: midasolam, diazepam
Volatile vs intravenous anesthesia
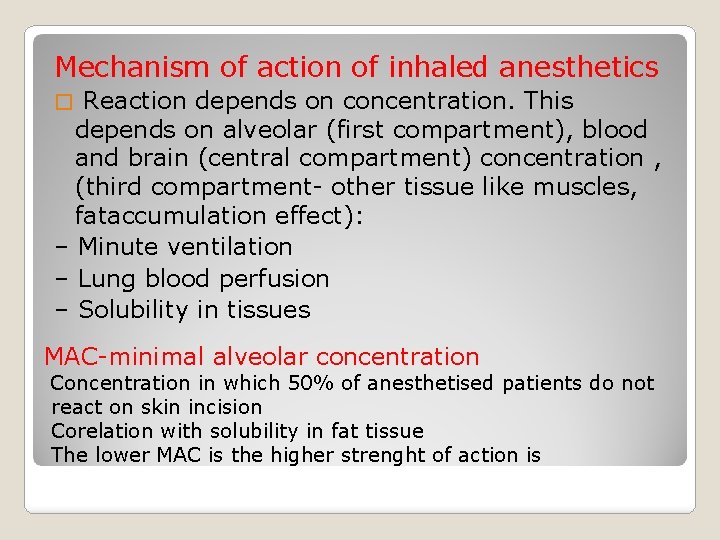
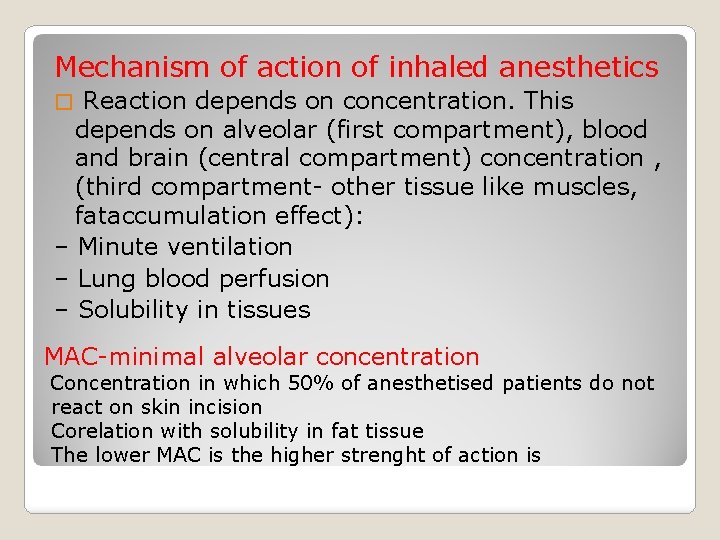
Mechanism of action of inhaled anesthetics Reaction depends on concentration. This depends on alveolar (first compartment), blood and brain (central compartment) concentration , (third compartment- other tissue like muscles, fataccumulation effect): – Minute ventilation – Lung blood perfusion – Solubility in tissues � MAC-minimal alveolar concentration Concentration in which 50% of anesthetised patients do not react on skin incision Corelation with solubility in fat tissue The lower MAC is the higher strenght of action is
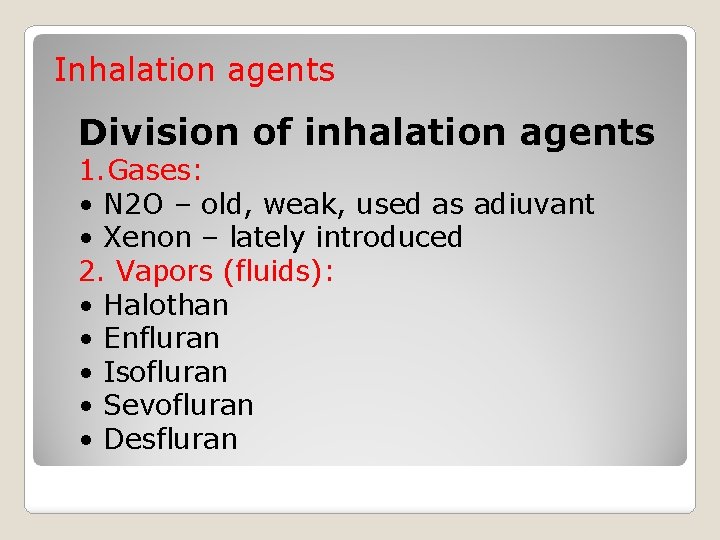
Inhalation agents Division of inhalation agents 1. Gases: • N 2 O – old, weak, used as adiuvant • Xenon – lately introduced 2. Vapors (fluids): • Halothan • Enfluran • Isofluran • Sevofluran • Desfluran
Features of ideal volatile anesthetic Not disturbing smell Fast acting, titrable Low solubility in blood- fast transport to brain � Stable when stored, not reacting with other chemicals � Non- flamable, non- explosive • Low methabolism in body, fast elimination, no accumulative effect �No depressing effect on circulatory and respiratory systems � � �
Nitrous oxide • Old • Weak • Used as adiuvant • Will be removed form medical use up to 2010 Halothan Used for many years with good effect • First non-flamable volatile fluid anesthetic • MAC high • Depression of circulatory system • May destroy liver • Now-a-days used only in pediatric anesthesia •
Isofluran • Disturbing smell • May interact with heart contractivity • Increases relaxation of muscles Desfluran • Very disturbing smell- can not be used for VIMA • Is not methabolised • Very fast acting • May be used for one-day surgery • Expensive, difficult to store (boiling temp. about 20 C) • Modern and widelly used
Sevofluran • Not disturbing smell- may be used for VIMA • Low solubility in blood- fast acting • Does not disturbs airway • May depress circulatory system • Methabolised to Compound A- may be renal toxic (but not confirmed in humans) • May be used in one-day surgery • Modern, and more widely used volatile anesthetic
Intravenous anesthesia
TCI (target controlled infusion) TCI is an infusion system which allows the anaesthetist to select the target blood concentration required for a particular effect � �It allows to control depth of anaesthesia by adjusting the requested target concentration
Instead of setting ml/h or a dose rate (mg/kg/h), the pump can be programmed to target a required blood concentration. � Effect site concentration targeting is now included for certain pharmacokinetic models. � �The pump will automatically calculate how much is needed as induction and maintenance to maintain that concentration.
THIOPENTAL �Old, one of the first used intravenous anesthetics �Depressing � effect on circulatory system May be used in patients with ASA 1
Ketamine Only intravenous anesthetic which has good analgesia effect Does not depress circulatory nor respiratory function Used in children, and in emergency and diseaster medicine Gives night mare dreams in adult patients
Propofol Very good anesthetic for induction and maintaince of anesthesia with no accumulation effect � Titrable � May be used in short procedures – titrated do not effect circulatory and respiratory system in important manner � Good for sedation, brain protecting effect � May be used in TCI
�Opioids fentanyl, alfentanil, sufentanil, remifentanil � May be used for induction and maintain of anesthesia in repeated bolus or continuous infusion technique � Sedative effect � In high doses may be used alone for so called opioid anesthesia- formerly used in cardioanesthesia- very stable circulatory effect �
�Compications of use Respiratory depression � Muscle rigidity in high doses �Post-Operative Nausea and Vomitings �Accumulation effect after prolonged administration (except for remifentanil) �
�Remifentanil � T 1/2 3 -5 min �Methabolised by non-specific tissue esterases- methabolism is not altered by renal or liver function �No accumulation effect after prolonged
BENZODIAZEPINES Used in anesthesia: Diazepam Midazolam Used as adiuvants for premedication
MUSCLE RELAXANTS
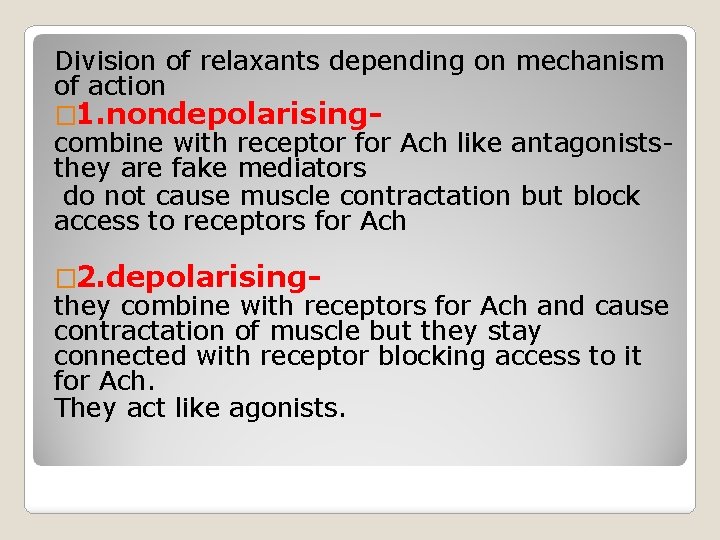
Division of relaxants depending on mechanism of action � 1. nondepolarising- combine with receptor for Ach like antagoniststhey are fake mediators do not cause muscle contractation but block access to receptors for Ach � 2. depolarising- they combine with receptors for Ach and cause contractation of muscle but they stay connected with receptor blocking access to it for Ach. They act like agonists.
�Nondepolarising �d-tubocurine agents – oldest deliverate of curarine – �alcuronium �-pancuronium – cheap and still used – �pipercuronium – �vercuronium – �atracurium – �cisatracurium – �mivacurium �-rocuronium
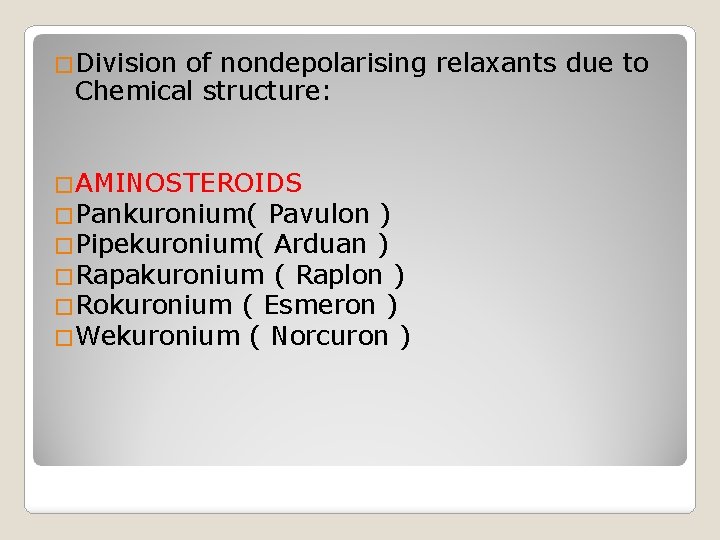
�Division of nondepolarising relaxants due to Chemical structure: �AMINOSTEROIDS �Pankuronium( Pavulon ) �Pipekuronium( Arduan ) �Rapakuronium ( Raplon ) �Rokuronium ( Esmeron ) �Wekuronium ( Norcuron )
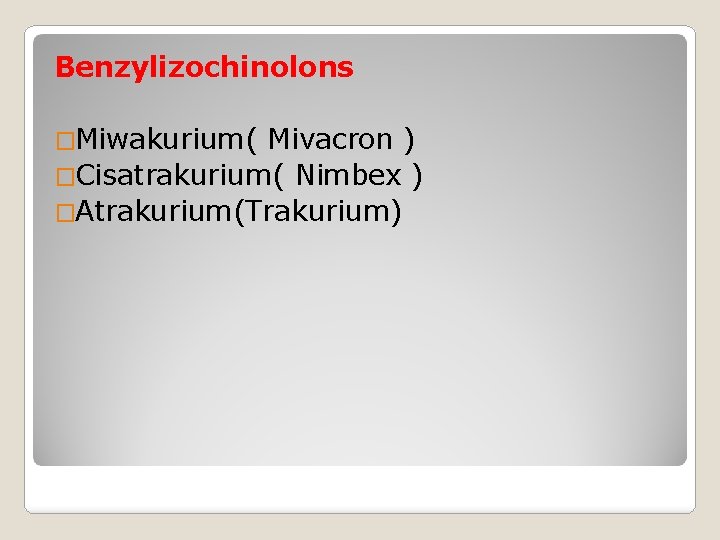
Benzylizochinolons �Miwakurium( Mivacron ) �Cisatrakurium( Nimbex ) �Atrakurium(Trakurium)
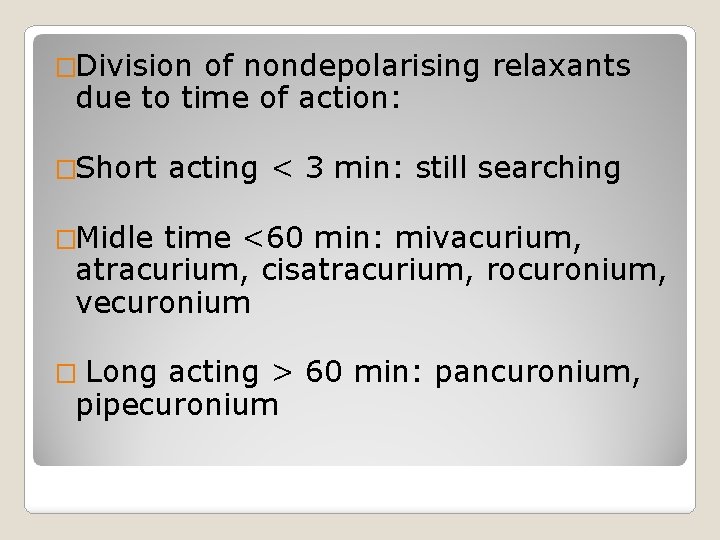
�Division of nondepolarising relaxants due to time of action: �Short acting < 3 min: still searching �Midle time <60 min: mivacurium, atracurium, cisatracurium, rocuronium, vecuronium � Long acting > 60 min: pancuronium, pipecuronium
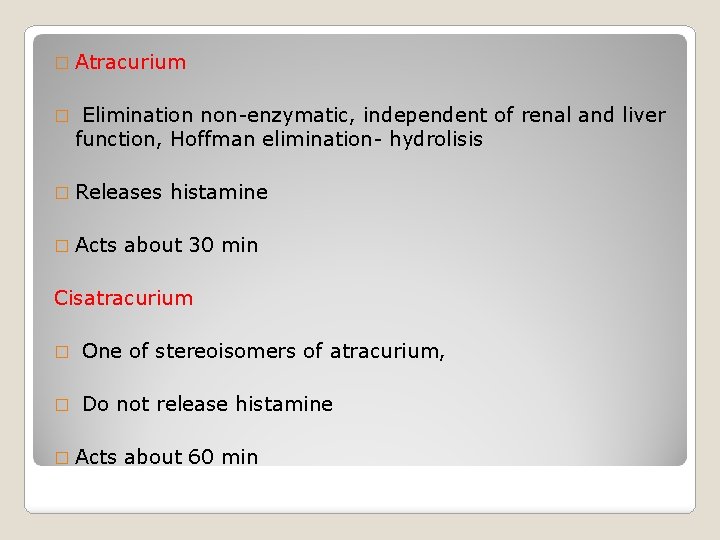
� Atracurium � Elimination non-enzymatic, independent of renal and liver function, Hoffman elimination- hydrolisis � Releases � Acts histamine about 30 min Cisatracurium � One of stereoisomers of atracurium, � Do not release histamine � Acts about 60 min
� Rocuronium Fast acting- time to 100% supresion 60 sec. � Do not release histamine � Acts about 60 min � Is methabolised in liver- disfunction of liver may alter elimination � Mivacurium � Releases histamine � Acts about 15 -20 min – used for short procedures � Methabolised by plasma esterases �
�Reverse of neuromuscular blockade Neostigmine, piridostigmine- blockers of acetylocholinesterase � Must be given toghether with atropine to avoid bradycardia caused by activation of perisympatic system � �Depolarising � Only � It is agents one: chlorsuccinilocholine – methabolised by pseudocholinesterase Causes many complications, has many contraindications – � Indications: Rapid sequence induction: full stomach, suspected difficult intubation because it acts very fast < 30 seconds and short < 3 min
�Complications anesthesia of general Respiratory: residual relaxants/opioids action � �Circulatory �Neurological: residual anesthetics/opioids action �Post-Operative Nausea and Vomitings
Mortality connected with anesthesia � 0, 05 - 4/10000 GA � 2 2 - 16 % of of surgical patients � 80 % is is caused by by human mistakes Major causes of deaths Airway obstruction Difficult and unefficient intubation Insufficient ventillation
�Other causes of mortality and morbidity Anoxia � Haemodynamic instability � Aspiration �Toxity of drugs �mostly inhalation agents �Anaphylaxia and drug interations �
 General anesthesia drugs dosage
General anesthesia drugs dosage Veterinary anesthesia reservoir bag size chart
Veterinary anesthesia reservoir bag size chart General anesthesia drugs chart
General anesthesia drugs chart Oil gas partition coefficient inhaled anesthetics
Oil gas partition coefficient inhaled anesthetics Anesthesia definition
Anesthesia definition Balanced anesthesia definition
Balanced anesthesia definition Diferencia entre gran plano general y plano general
Diferencia entre gran plano general y plano general Where did general lee surrender to general grant?
Where did general lee surrender to general grant? Olv anesthesia
Olv anesthesia Virtual anesthesia machine
Virtual anesthesia machine Fail safe valve anesthesia
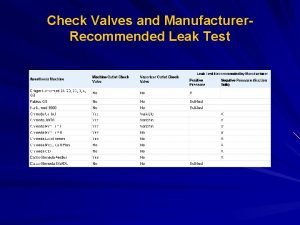
Fail safe valve anesthesia Link 25 system
Link 25 system Structures pierced by spinal needle
Structures pierced by spinal needle Pre anesthesia assessment form
Pre anesthesia assessment form Greater palatine nerve block technique
Greater palatine nerve block technique Facial nerves
Facial nerves Mechanism of local anesthesia
Mechanism of local anesthesia B
B Periodonteum
Periodonteum Types of local anesthesia
Types of local anesthesia Local anesthesia
Local anesthesia Anesthesia airway anatomy
Anesthesia airway anatomy Mac anesthesia minimum alveolar concentration
Mac anesthesia minimum alveolar concentration Minimum alveolar concentration
Minimum alveolar concentration Balanced anesthesia components
Balanced anesthesia components Balanced anesthesia components
Balanced anesthesia components Classification of inhalational agents
Classification of inhalational agents Epidural block level chart
Epidural block level chart Epidural anesthesia
Epidural anesthesia Tuohy needle sizes
Tuohy needle sizes N buccalis
N buccalis Induction anesthesia
Induction anesthesia Negative pressure leak test anesthesia machine
Negative pressure leak test anesthesia machine Btm anesthesia formula
Btm anesthesia formula Anesthesia for cardiac tamponade
Anesthesia for cardiac tamponade Balanced anesthesia components
Balanced anesthesia components Bis scale
Bis scale Anesthesia machine checkout
Anesthesia machine checkout Poynting effect anesthesia
Poynting effect anesthesia Denali anesthesia
Denali anesthesia What is anesthesia
What is anesthesia Ccas anesthesia
Ccas anesthesia