Measuring Depth of Anesthesia The word anesthesia was


















- Slides: 79

Measuring Depth of Anesthesia
The word "anesthesia" was first used by the Greek philosopher Dioscorides in the first century of the current era to describe the narcotic effect of the plant mandragora. The word reappeared in the 1771 Encyclopaedia Britannica, where it was defined as a "privation of the senses.
Plomley, in 1847, was the first to attempt to define depth of anesthesia. He described three stages: intoxication, excitement (both conscious and unconscious), and the deeper levels of narcosis. In that same year, John Snow described "five degrees of narcotism" for ether anesthesia.
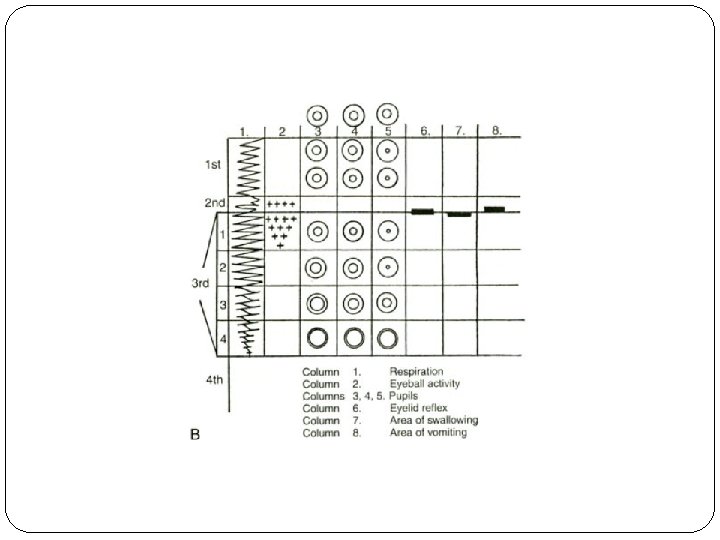
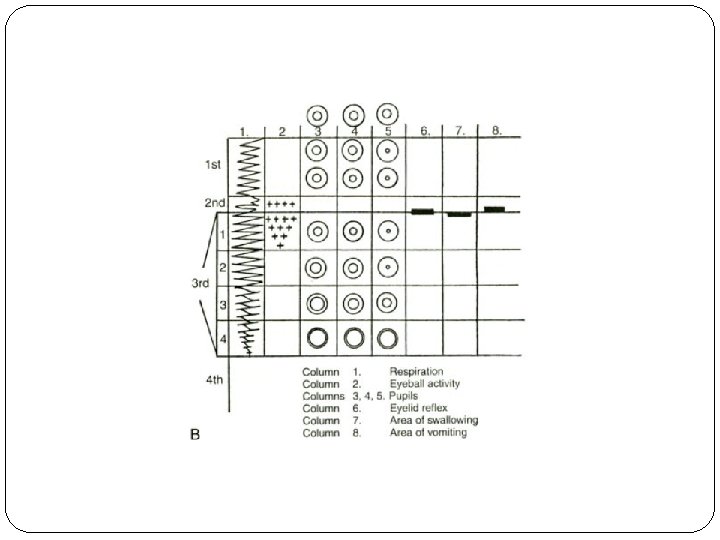
In 1937, Guedel published his classic description of the clinical signs of ether anesthesia. He used clear physical signs involving somatic muscle tone, respiratory patterns, and ocular signs to define four stages.

What Is Anesthesia? The sine qua non of the anesthetized state is unconsciousness, the lack of conscious processing of thoughts. The crux of the difficulty in defining anesthetic depth is that unconsciousness cannot be measured directly.




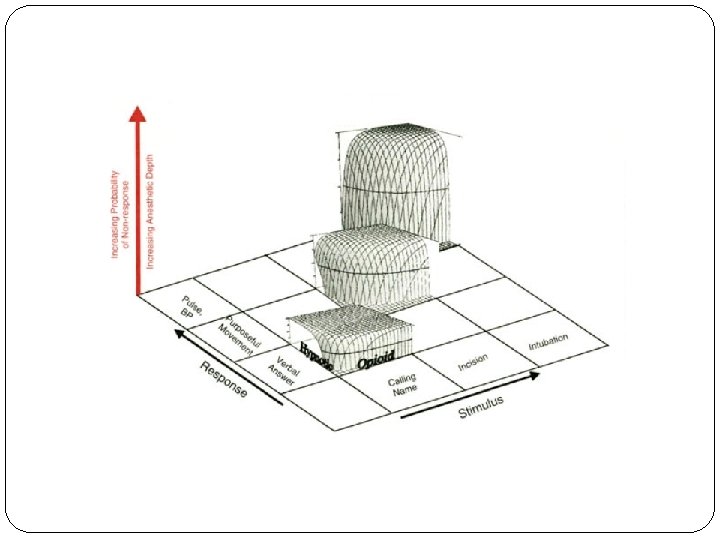
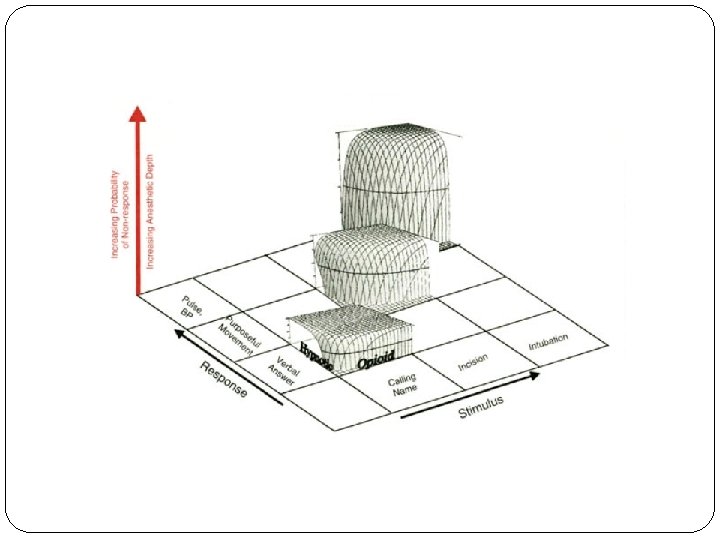
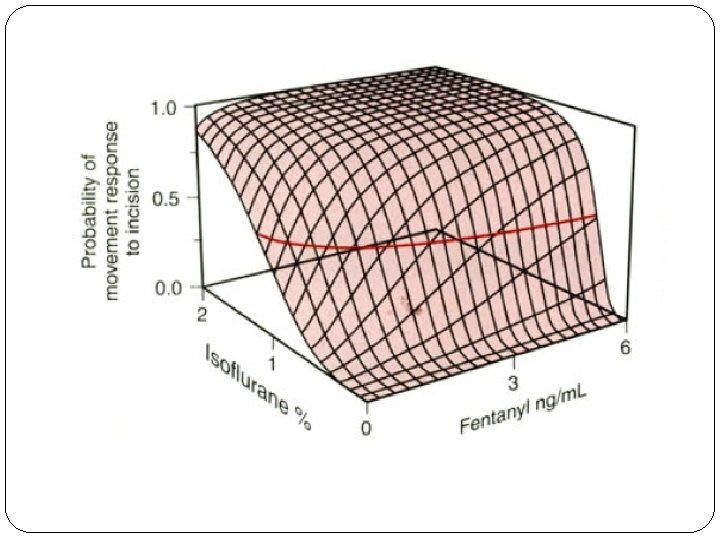
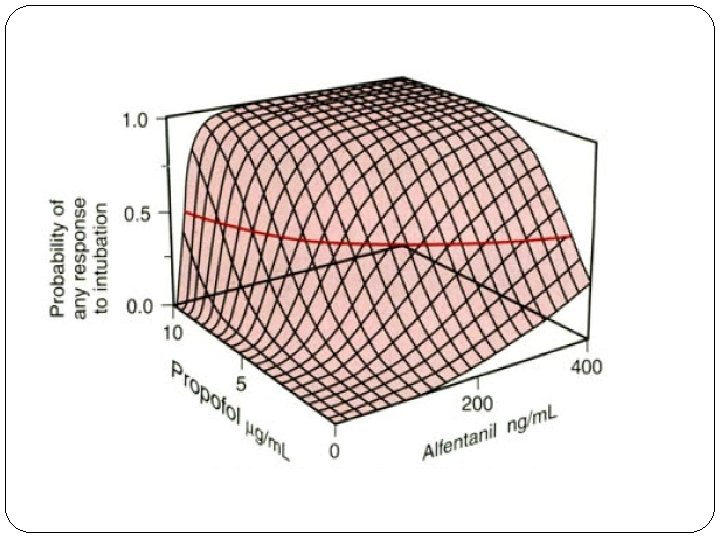
The most important is that for any stimulus response pair, depth of anesthesia is the probability of nonresponse. More generally, depth of anesthesia is the probability of nonresponse to stimulation, calibrated against the strength of the stimulus, the diffi. Culty of suppressing the response, and the druginduced probability of nonresponsiveness.
Anesthetic depth ranges from a 100% probability of an easily suppressed response (verbal answer) to a mild stimulus (e. g. , calling one's name) and readily suppressed responses (e. g. , verbal answer) to a 100%probability of nonresponse to profoundly noxious stimuli (e. g. , intubation) and responses that are difficult to suppress (e. g. , tachycardia).

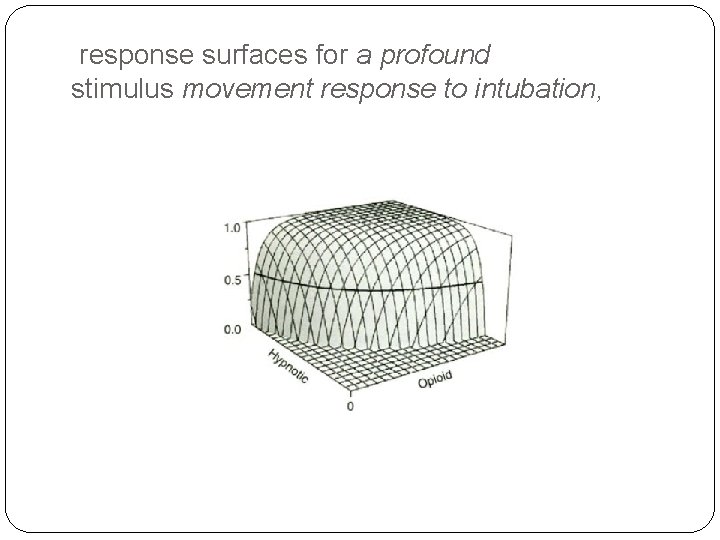
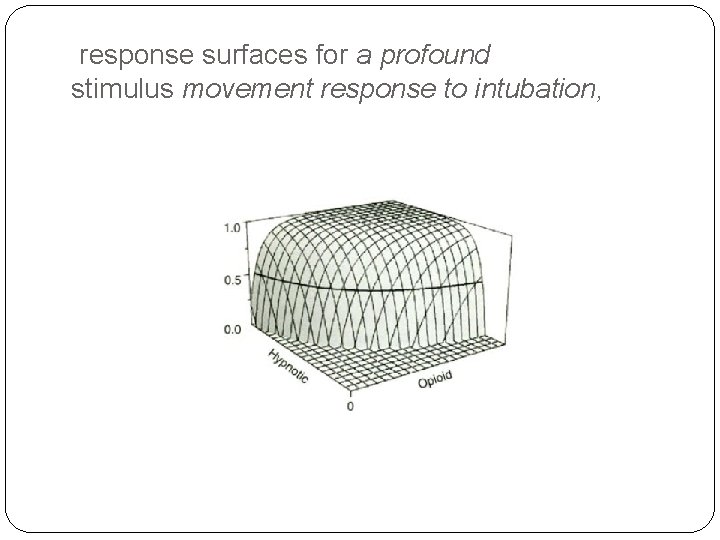
response surfaces for a profound stimulus movement response to intubation,
MEMORY AND AWARENESS Recall, Conscious or Explicit Memory § Detection of Auditory Input, Unconscious or Implicit Memory §
Recall, Conscious or Explicit Memory Ghoneim recently reviewed cases of recall in different anesthetic situations. The incidence of awareness in a non obstetric and noncardiac surgical population approximates 0. 2%. A higher incidence is reported for obstetric general anesthesia, 0. 4%. The incidence in cardiac surgery ranges from 1. 1%to 1. 5%. major trauma cases can have a range of awareness from 11% to 43%.
Intraoperative awareness or recall has occurred with high-dose opioid anesthesia. Two clinical signs possibly predicting the occurrence of recall are movement and autonomic response. The use of muscle relaxants can eliminate the movement response, which leaves only autonomic activity as
Detection of Auditory Input, Unconscious or Implicit Memory Although the patient may not overtly recall a stimulus or an event, auditory input can register in the brain during apparently adequate surgical anesthesia. Auditory and verbal input must be "meaningful" for it to register in the patient's memory. Frequently, hypnosis or other cues may be needed to elicit recall.

Ten volunteers undergoing dental surgery were given thiopental followed by nitrous oxide and diethyl ether. Monitoring the EEG for an irregular slow-wave-high-voltage pattern allowed the anesthetist to maintain a similar depth of anesthesia in all patients. This EEGpattern was considered equivalent to moderate to
During surgery, the anesthetist provided verbal stimulation to the patient in the form of an intraoperative crisis by verbally stating that cyanosis was present and then treated appropriately.
All 10 patients had no spontaneous recall of the simulated intraoperative crisis. Under hypnosis, however, four patients could remember the frightening words in exact detail. An additional four remembered someone speaking to them. All eight became anxious and either emerged spontaneously from their hypnotic trance or refused to continue exploring the event. One subject had activation of the EEGpattern when the intraoperative crisis occurred, but no recall of the event.
Large effects on memory were produced only by propofol and midazolam. Thiopental had mild memory effects, whereas fentanyl had none.
Implications of Explicit, Intraoperative Blacher described a traumatic post- cardiac surgery neurosis involving anxiety and irritability, repeated nightmares, preoccupation with death, and a reluctance to discuss these symptoms. He attributed this postoperative state to patients' being awake and paralyzed during open heart surgery.
HYPNOTICS, ANALGESICS, AND ANESTHETIC DEPTH
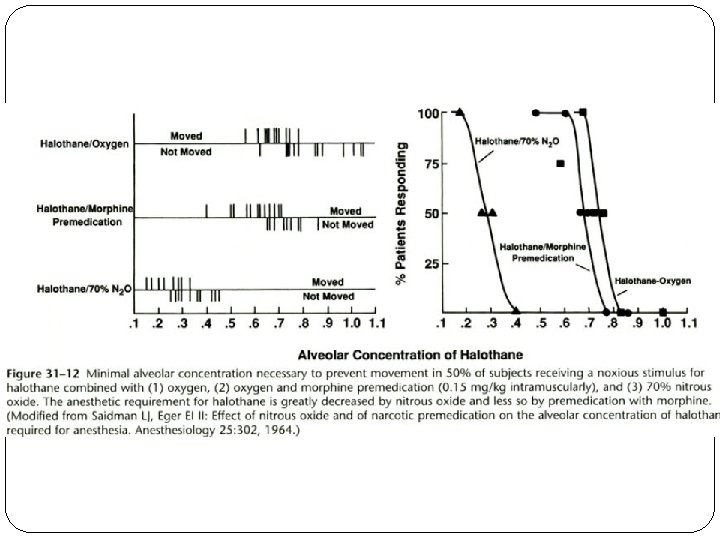
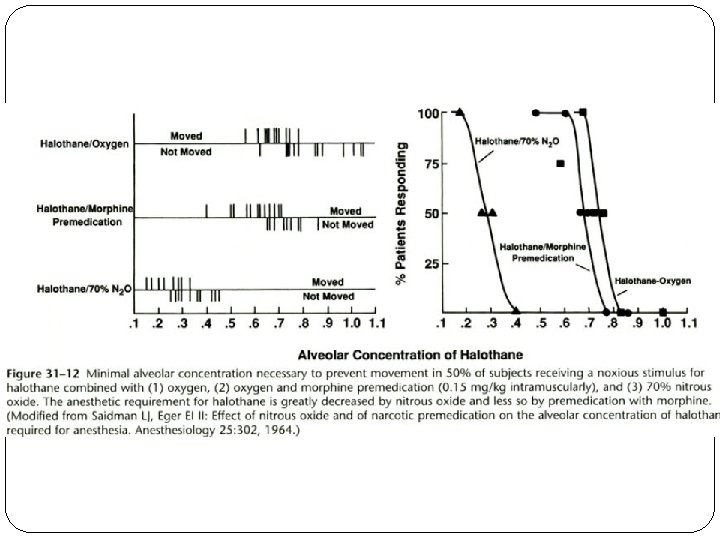
Inhaled Anesthetics Movement Response and the MAC Concept: MAC is the minimum alveolar concentration of inhaled anesthetic required to prevent 50% of subjects from responding to a painful stimulus with "gross purposeful movement. “ For determination of MAC in humans, the standard noxious stimulus has been the initial surgical skin incision.
The MAC concept has been expanded by evaluating other clinical end points and defined stimuli. the MAC of anesthetic that would allow opening of the eyes on verbal command during emergence from anesthesia ("MACawake) Generally, MACawake values are a third to a fourth the MAC values for surgical incision.
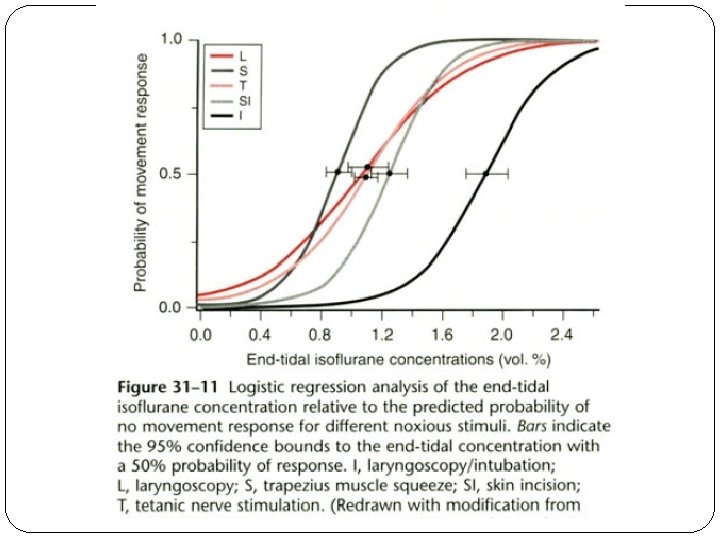
the MAC of inhaled anesthetic that would inhibit movement and coughing during endotracheal intubation ("MACintubation"). Intubation is significantly more stimulating than skin incision, and higher concentrations of inhaled anesthetic are required to eliminate the movement response.

MACBAR: The MAC of anesthetic necessary to prevent an adrenergic response to skin incision, as measured by the concentration of catecholamine in venous blood.
§Because cerebral blood perfusion is large, it is possible to achieve an equilibration among end-tidal, alveolar, arterial, and brain anesthetic partial pressures within 15 minutes of exposure to a constant end-tidal anesthetic concentration. §If the difference between the inspired and end-tidal partial pressures was less than 10% difference between end-tidal and arterial concentrations would be minimal.

Eger and associates proposed that volatile anesthetics cause a lack of movement response to noxious stimuli by action in the spinal cord and create a hypnotic/amnestic loss of consciousness at a supraspinal, cortical site of action.
Other Clinical Responses: § Other Clinical Responses other than § § § purposeful movement have been investigated as possible clinical measures of the depth of anesthesia: the rate and volume of ventilation in spontaneously breathing subjects, eye movement, the diameter and reactivity of pupils to light, heart rate, arterialblood pressure, and autonomic signs such as sweating.
It has not been possible, however, to use these clinical signs to generate uniform measures of depth of anesthesia for inhaled anesthetics. Although some clinical signs do correlate with depth of anesthesia for certain inhaled anesthetics, the same cannot be said for other inhaled anesthetics.
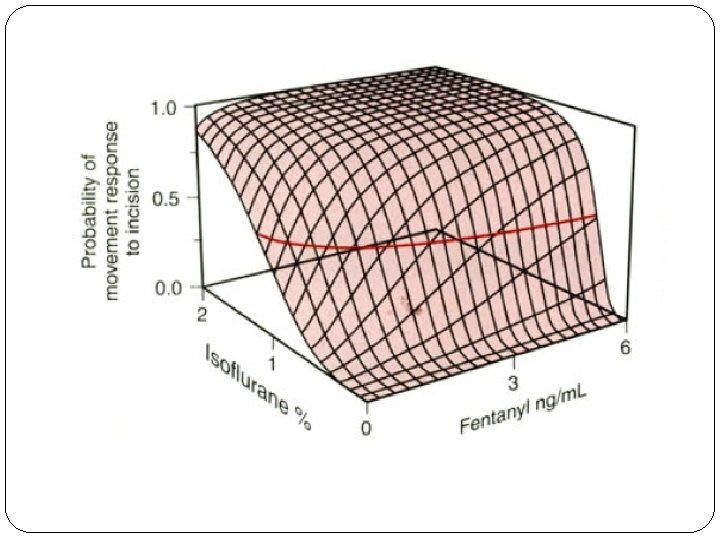
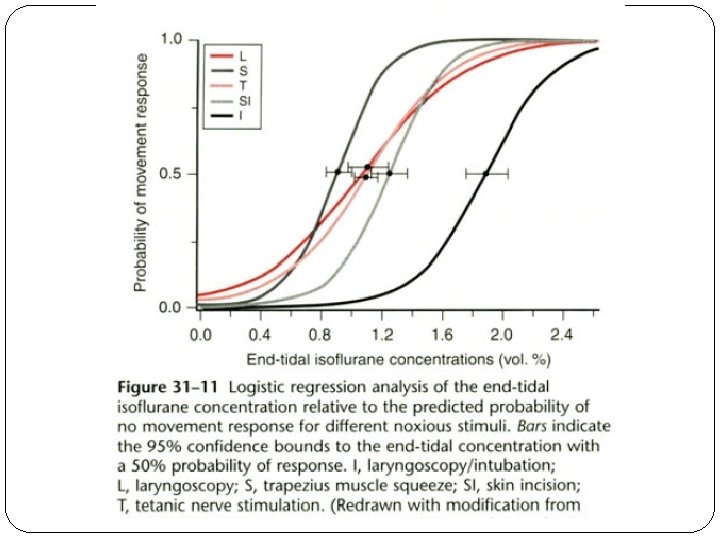
Zbinden and colleagues systematically examined the interaction of isoflurane concentrations with the hemodynamic response to different noxious stimuli.


. When used as a sole agent, even at high concentrations isoflurane is unable to suppress hemodynamic responses to noxious stimuli. the addition of analgesic components, such as nitrous oxide and fentanyl, can prevent the sympathetic stimulation and hemodynamic responses seen with noxious surgical stimuli when inhaled anesthetics are used.

Intravenously Administered (Nonopioid) Anesthetics Assessing Depth during Induction of Anesthesia Assessing Depth during Maintenance of Anesthes
Assessing Depth during Induction of Anesthesia Induction of anesthesia often consists of a rapid intravenous bolus injection of a hypnotic (e. g. , propofol, thiopental, etomidate). Plasma concentrations peak within a half to 1 minute and decline rapidly on redistribution of the drug.
Clinical end points useful in assessing the depth of anesthesia during induction include loss of verbal responsiveness, loss of eyelid reflex, and loss of corneal reflex. Typical stimulation occurring during induction of anesthesia includes laryngoscopy and intubation, which constitute profoundly noxious stimuli. Frequently, response to these two procedures cannot be eliminated completely with just the intravenously administered hypnotic.
Thus, assessment of the depth of anesthesia with the use of clinically relevant noxious stimuli such as laryngoscopy and intubation requires the concurrent administration of other analgesic drugs (opioids or nitrous oxide) to provide reasonable and clinically acceptable hemodynamic control.
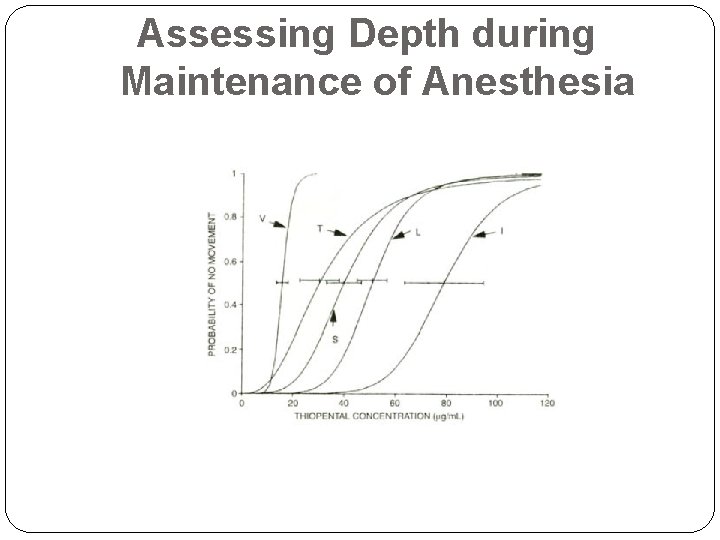
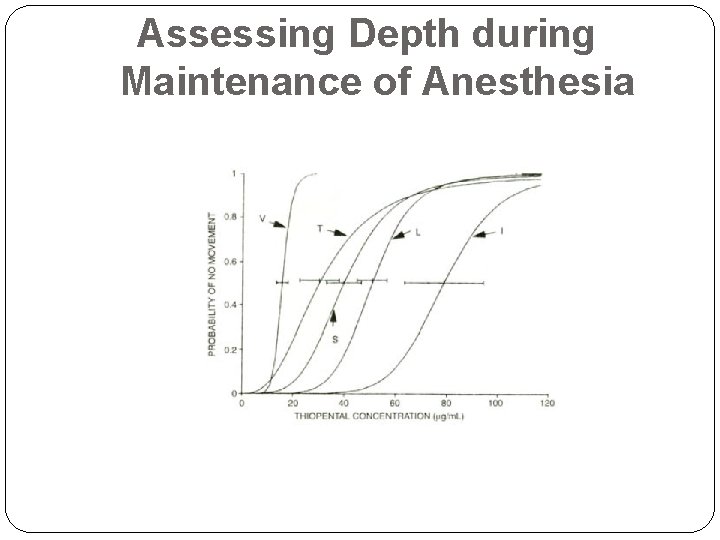
Assessing Depth during Maintenance of Anesthesia
For the patients given 67%nitrous oxide, the plasma concentrations of thiopental necessary to achieve the same surgical end points were as much as 71%lower than those in patients given only thiopental.
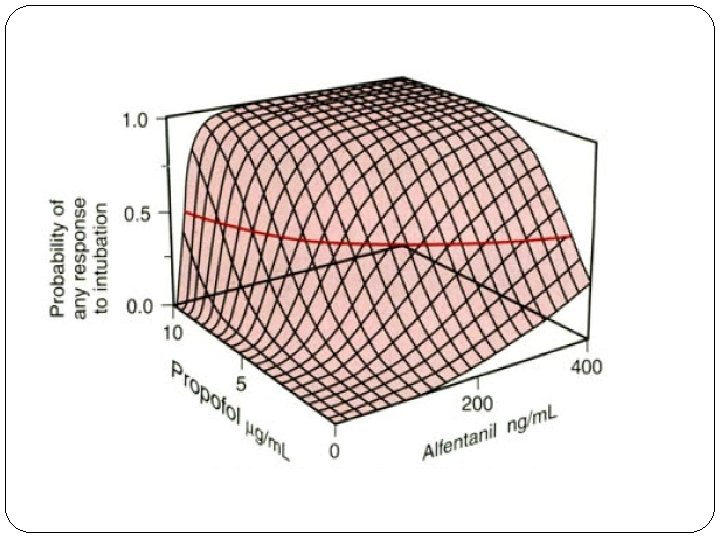
Kazama and coworkers found propofol CPso values for the following defined stimuli: loss of verbal responsiveness, electrical tetanus, laryngoscopy, skin incision, and intubation. With the addition of a steady-state fentanyl , there was only a minimal decrease in the propofol CPso for loss of verbal responsiveness. For the other, more intense noxious stimuli (tetanus, laryngoscopy, skin incision, and intubation), a much greater decrease in propofol CPso occurred.
In clinical practice, intravenously administered anesthetic drugs are frequently combined with other drugs that provide additional analgesia (opioids, nitrous oxide, potent inhaled anesthetics).

large intravenously administered doses of thiopental or propofol are less than effective in eliminating the hemodynamic response to relevant clinical stimuli such as laryngoscopy and intubation. Fentanyl decreases the anesthetic requirement for thiopental or propofol by providing anti nociceptive effects that the intravenous hypnotics do not provide.
Clinically, the hemodynamic response to laryngoscopy, intubation, or skin incision is most commonly used to assess depth of anesthesia. The use of muscle relaxants to ease endotracheal intubation precludes use of the movement response.
Because laryngoscopy and intubation are single events, if clinical depth is inadequate (e. g. , in the event of a profound hemodynamic response), additional intravenous anesthetics, opioids, or maintenance anesthetic drugs are rapidly administered.
When precise hemodynamic control becomes important (as in coronary artery disease), larger doses of opioids are used instead of intravenously administered anesthetics.
Opioids The analgesia produced by these drugs through specific receptor systems within the CNS decreases autonomic, endocrine, and somatic responses to noxious stimulation. Although opioids have been used as sole anesthetics, they create incomplete hypnotic effects at very large doses. Opioids need to be combined with hypnotic drugs to induce the anesthetic state.

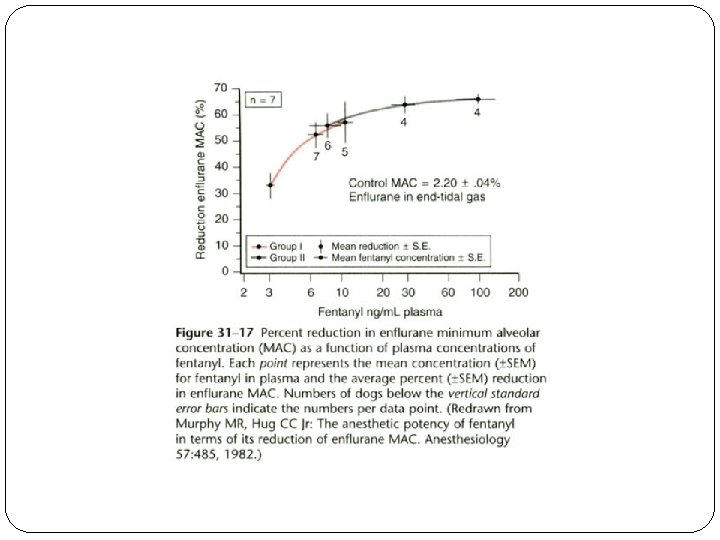
Murphy and Hug found that even high plasma concentrations of fentanyl (20 ng/m. L) did not decrease enflurane MAC beyond 60% to 70% of its initial value (Fig. 31 -17). That is, there was a ceiling to the enfluranesparing effect. Morphine, sufentanil, and alfentanil also decrease enflurane MAC and have a similar ceiling effect in dogs.
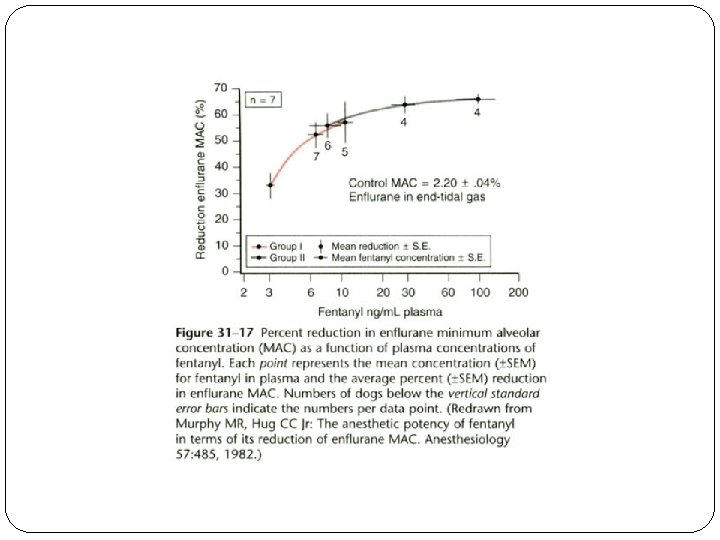
Mc. Ewan and coworkers found very similar results in humans. The maximal MAC reduction was 82% at a steady-state fentanyl plasma concentratio of 10. 6 ng/m. L. Similar MAC reduction results have been obtained with other inhaled anesthetics (desflurane, sevoflurane) and other opioids (alfentanil, sufentanil, remifentanil).


El. ECTROPHYSIOl. OGIC MONITORING
Bispectral Electroencephalographic Monitoring In the 1990 s, Aspect Medical Systems, a medical device company in Natick, Massachusetts, undertook an integrated research effort to develop the EEG as a measure of anesthetic depth. The Aspect EEG monitor quantitates the anesthetic effects on the brain, specifically, the hypnotic component of anesthesia.
The device presents a continuous EEG parameter, the bispectral (BIS) index, which ranges from an awake, no-drugeffect value of 95 to 100 to zero with no detectable EEG activity.
• Successful development of the Aspect BIS EEG monitoring system can be identified with the following concepts:
1. The simultaneous use of multiple EEGsignal-processing approaches captured incremental information that was not captured with traditional approaches based on a single signalprocessing approach.
2. Multiple clinically relevant measures (movement, hemodynamics, drug concentrations, consciousness, recall) in patients and volunteers were gathered with concurrent EEG data.
3. Advanced multivariate statistical data analysis was used to correlate the components of the multiple EEG signalprocessing approaches with the clinical data to create the univariate BIS parameter.
4. Prospective clinical evaluation of the BIS index was performed at multiple institutions under varying anesthetic and surgical conditions.
5. The BIS index was recognized as measuring the hypnotic components of the anesthetic and was relatively insensitive to the analgesic (e. g. , opioid) components of an anesthetic.
6. Prospective clinical trials demonstrated that BIS monitoringcould improve the outcome of an anesthetic regimen. 7. Simple hardware and sensors were developed and are commercially available to facilitate high-quality signal capture despite the noisy electrical environment of the operating room.

Several factors that will be encountered in clinical anesthesia care can interact with the BIS index: hypothermia decreased the BIS index by 1. 12 units per degree Celsius decline in temperature. Infusion of esmolol can also alter the BIS index. Epidural anesthesia can also decrease the amount of hypnotic anesthetic needed for sedation. Ketamine doses that create unresponsiveness (0. 25 to 0. 5 mg/kg) did not change the BIS index.
Bispectral lndex and Clinical Utility/Outcome The use of BIS monitoring was associated with a significantly reduced incidence of awareness (78%reduction) when compared with historical controls from the same hospitals and investigators.
Mortality was significantly higher if the BIS index was less than 40 in patients older than 40 years. Increasing age and lower BIS values were both independently associated with higher mortality rates.
Clinical Use of the Bispectral Index Clinical use of BIS monitoring involves separating the hypnotic and analgesic components of an anesthetic regimen. The concept entails titration of the hypnotic drug (e. g. , isoflurane, desflurane, sevoflurane, propofol, midazolam) to lower the BISvalue to 40 to 60. This range appears to be therapeutic window associated with a high probability of unconsciousness.
 Total internal reflection in a semicircular glass block
Total internal reflection in a semicircular glass block Anesthesia root word
Anesthesia root word Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Ng-html
Ng-html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Chụp phim tư thế worms-breton
Chụp phim tư thế worms-breton Chúa yêu trần thế
Chúa yêu trần thế Các môn thể thao bắt đầu bằng từ đua
Các môn thể thao bắt đầu bằng từ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tính độ biến thiên đông lượng
Công thức tính độ biến thiên đông lượng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thể thơ truyền thống
Thể thơ truyền thống Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế
Cái miệng nó xinh thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ V cc
V cc Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Tia chieu sa te
Tia chieu sa te Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dạng đột biến một nhiễm là
Dạng đột biến một nhiễm là Số.nguyên tố
Số.nguyên tố Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Khi nào hổ mẹ dạy hổ con săn mồi
Khi nào hổ mẹ dạy hổ con săn mồi Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu Sơ đồ cơ thể người
Sơ đồ cơ thể người Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Double lumen tube sizing
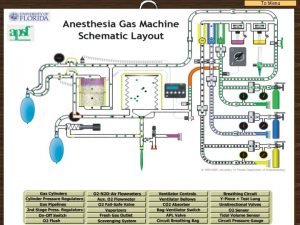
Double lumen tube sizing Virtual anesthesia machine
Virtual anesthesia machine Fail safe valve anesthesia
Fail safe valve anesthesia Yoke block anesthesia machine
Yoke block anesthesia machine Paramedian epidural layers
Paramedian epidural layers Pre anesthesia assessment form
Pre anesthesia assessment form Greater palatine nerve block landmark
Greater palatine nerve block landmark Supraperiosteal definition
Supraperiosteal definition Mechanism of local anesthesia
Mechanism of local anesthesia Mechanism of local anesthesia
Mechanism of local anesthesia Psa nerve block
Psa nerve block Types of local anesthesia
Types of local anesthesia Sanjita das
Sanjita das Anesthesia hose
Anesthesia hose Mac isoflurane
Mac isoflurane Inhalation anesthetics
Inhalation anesthetics Minimum alveolar concentration
Minimum alveolar concentration Classification of inhalational agents
Classification of inhalational agents Balanced anesthesia components
Balanced anesthesia components General anesthesia drugs dosage
General anesthesia drugs dosage Residual blockade
Residual blockade 2nd gas effect
2nd gas effect Spinal anesthesia level chart
Spinal anesthesia level chart Spinal anesthesia
Spinal anesthesia Epidural needle markings
Epidural needle markings N mentalis anesthesia
N mentalis anesthesia Induction anesthesia
Induction anesthesia Positive pressure leak test anesthesia machine
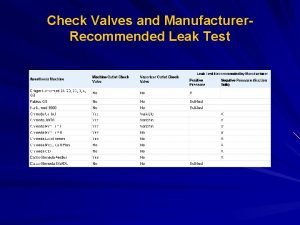
Positive pressure leak test anesthesia machine Anesthesia formula btm
Anesthesia formula btm Midazolum
Midazolum Components of anaesthesia
Components of anaesthesia What is anesthesia
What is anesthesia Anesthesia machine checkout
Anesthesia machine checkout Poynting effect anesthesia
Poynting effect anesthesia Laryngospasm
Laryngospasm What is anesthesia
What is anesthesia