General Anesthesia General Anesthesia n Definition of GA
- Slides: 29
General Anesthesia
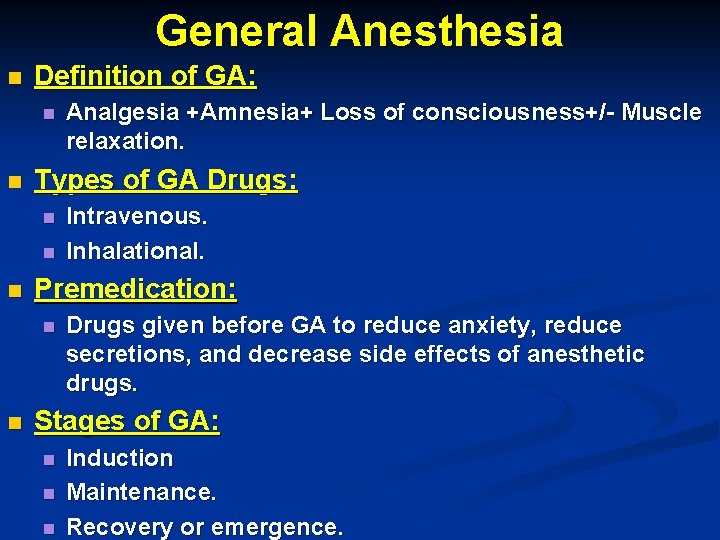
General Anesthesia n Definition of GA: n n Types of GA Drugs: n n n Intravenous. Inhalational. Premedication: n n Analgesia +Amnesia+ Loss of consciousness+/- Muscle relaxation. Drugs given before GA to reduce anxiety, reduce secretions, and decrease side effects of anesthetic drugs. Stages of GA: n n n Induction Maintenance. Recovery or emergence.
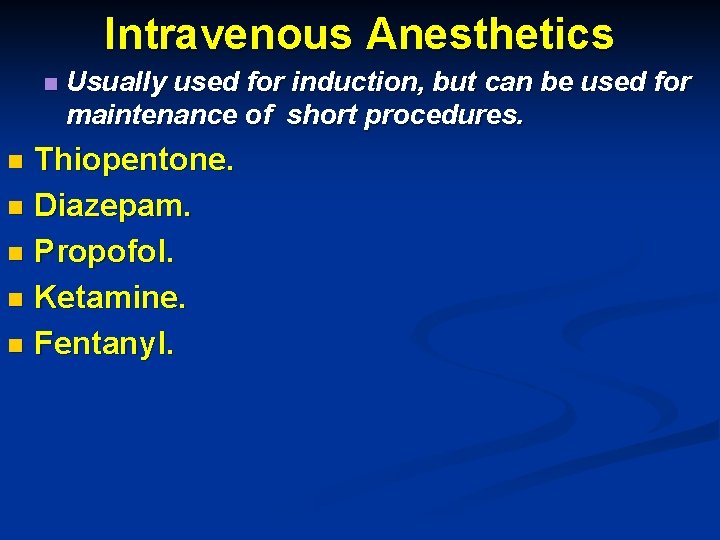
Intravenous Anesthetics n Usually used for induction, but can be used for maintenance of short procedures. Thiopentone. n Diazepam. n Propofol. n Ketamine. n Fentanyl. n
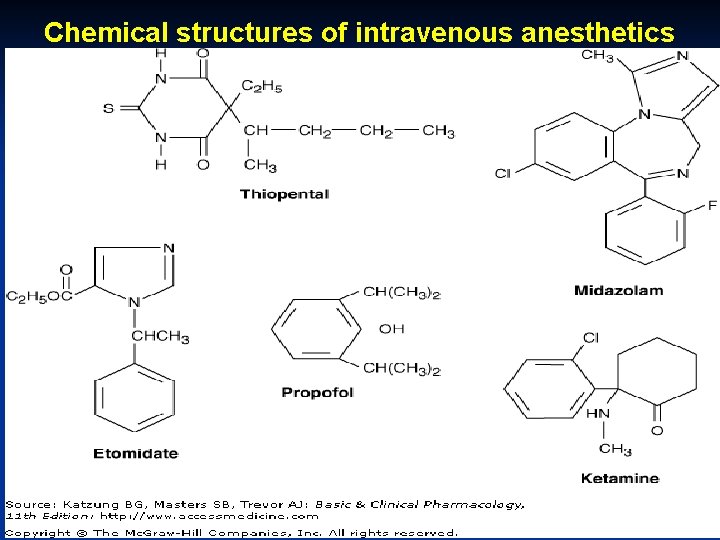
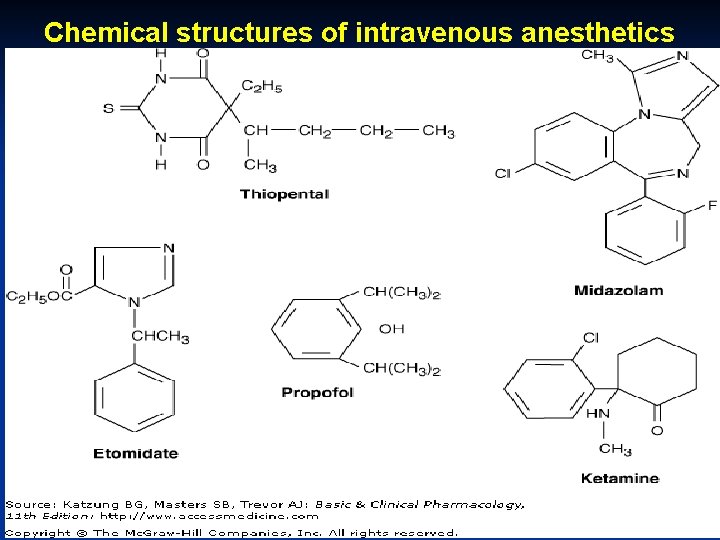
Chemical structures of intravenous anesthetics
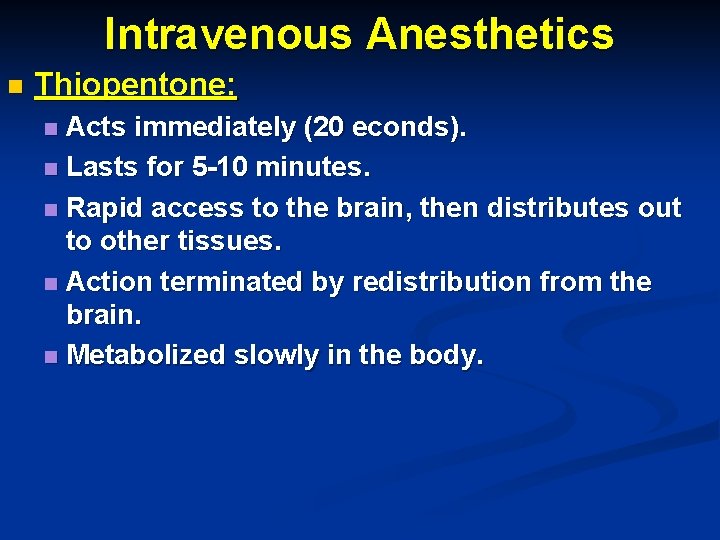
Intravenous Anesthetics n Thiopentone: Acts immediately (20 econds). n Lasts for 5 -10 minutes. n Rapid access to the brain, then distributes out to other tissues. n Action terminated by redistribution from the brain. n Metabolized slowly in the body. n
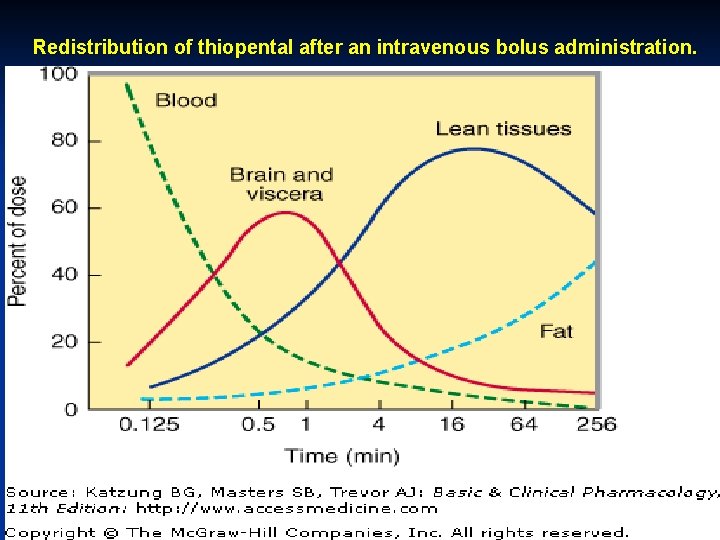
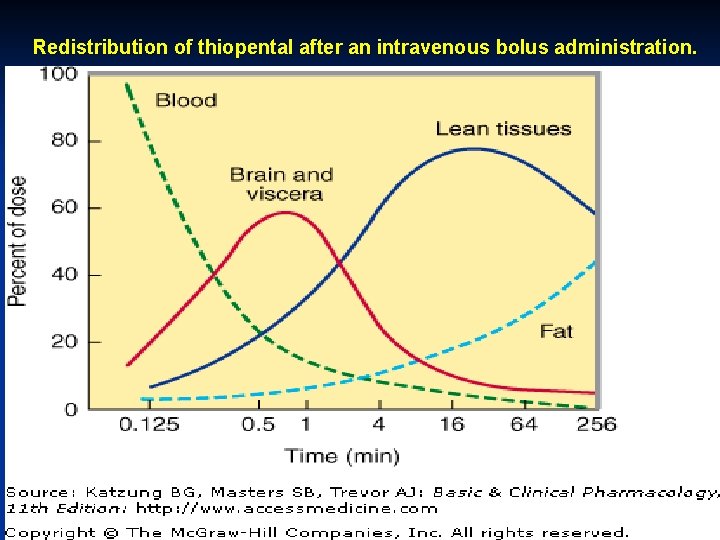
Redistribution of thiopental after an intravenous bolus administration.
Intravenous Anesthetics n Benzodiazepines: Diazepam ”Valium” n Lorazepam. n Midazolam. n
Intravenous Anesthetics n Propofol. Very rapidly metabolized. n Given by continuous slow IV infusion. n Used for short procedures, and for sedation of patients in ICU. n
Intravenous Anesthetics n Ketamine: IM. n Good for children or in ambulatory conditions. n Causes “Dissociative Anesthesia”: n n Patient remains half awake, can move, free of pain, unaware, muscle tone maintained, BP maintained or elevated. n Causes nightmares and hallucinations: keep in a dark room. n Fentanyl: n Is an opioid-like drug, .
Inhalational Anesthetics n Nitrous Oxide. n Ether. n Halothane n Enflurane. n Isoflurane.
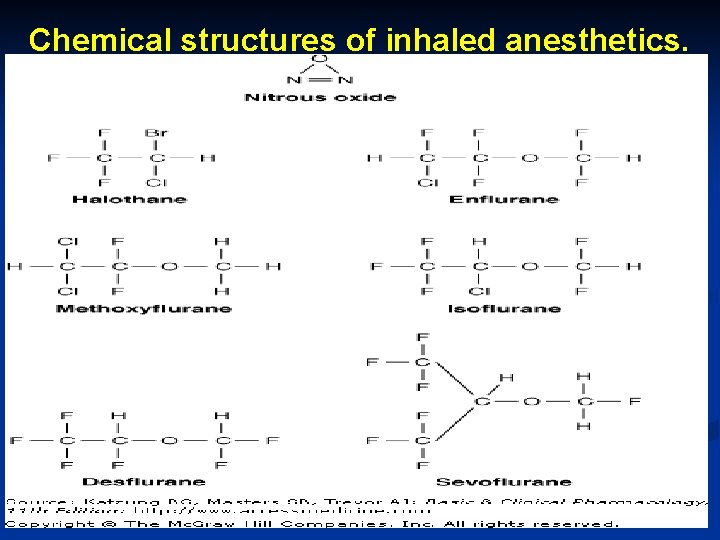
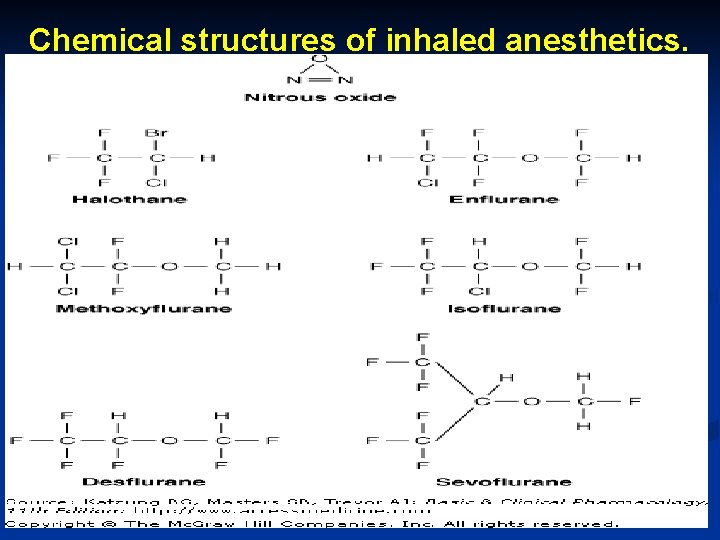
Chemical structures of inhaled anesthetics.
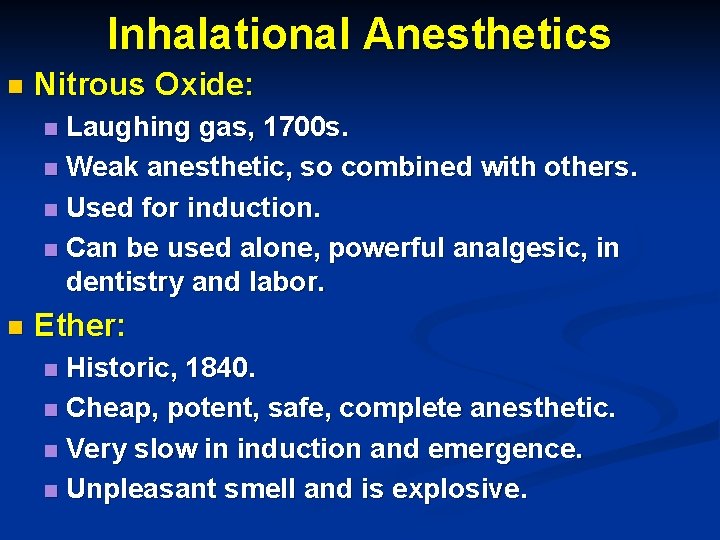
Inhalational Anesthetics n Nitrous Oxide: Laughing gas, 1700 s. n Weak anesthetic, so combined with others. n Used for induction. n Can be used alone, powerful analgesic, in dentistry and labor. n n Ether: Historic, 1840. n Cheap, potent, safe, complete anesthetic. n Very slow in induction and emergence. n Unpleasant smell and is explosive. n
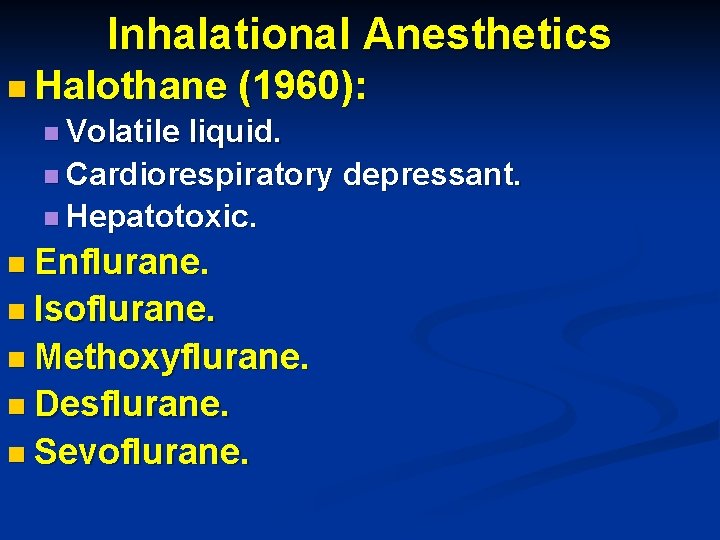
Inhalational Anesthetics n Halothane (1960): n Volatile liquid. n Cardiorespiratory depressant. n Hepatotoxic. n Enflurane. n Isoflurane. n Methoxyflurane. n Desflurane. n Sevoflurane.
Local Anesthesia Block conduction along nerves, mainly carrying pain sensation. n In sufficient concentration, produce complete sensory and motor blockade. n Pain is conducted through fine unmyelinated nerve fibers, so easily blocked with small doses or low concentrations. n
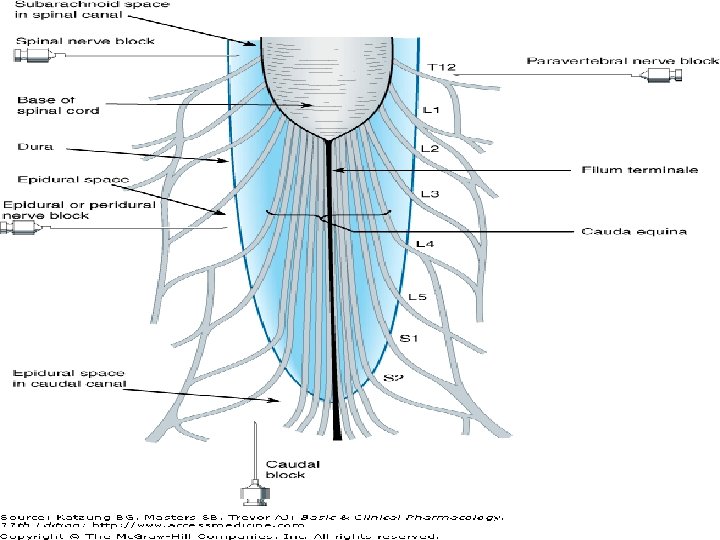
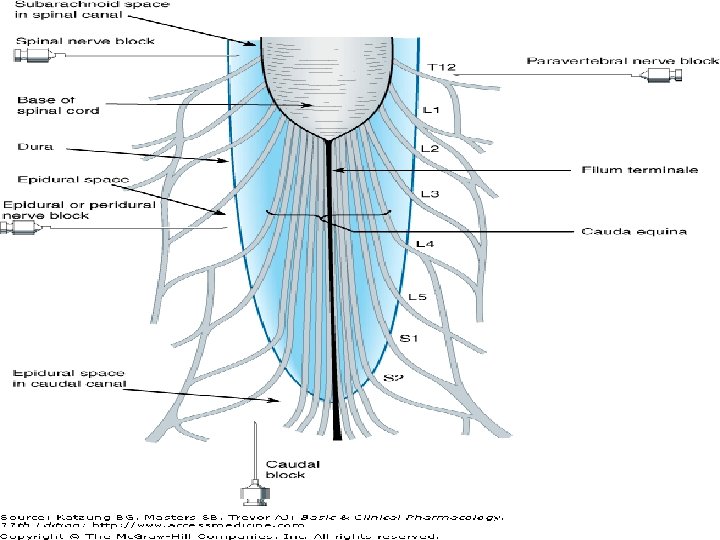
Local Anesthesia n Methods of Administration: Direct application to skin or mucus membranes. n Intradermal injection. n Local infiltration. n Local nerve block. n Extradural (Epidural) injection. n Subarachnoid (Spinal Block). n Intravenous injection. n
Local Anesthesia n Lidocaine ( Lignocane or Xylocaine): Most commonly used LA, also antiarrhythmic. n Rapid onset. n Duration 1 -2 hours. n Vasodilator, so usually combined with a vasoconstrictor (epinephrine) to reduce absorption and prolong the action. n Various concentrations. n Overdose: Tinnitus, Tremor, Restlessness, Convulsions, Cardiac and Respiratory depression. n
Local Anesthesia n Prilocaine: n Longer acting and less toxic. n Used for dental anesthesia. n Bupivacaine: n Longer acting but more toxic. n Suitable for continuous epidural analgesia in labor.
Local Anesthesia n Cocaine: n First LA, 1860, used for ophthalmic and nose surgery. n Has sympathomometic actions, no need for a vasoconstrictor. n Highly addictive. n Amethocaine Gel: n Used for venipuncture in children, vasodilator.
Skeletal Muscle Relaxants n Neuromuscular Blockers: n Uses: n Facilitate endotracheal intubation. n To relax muscles in surgery. n To enable easy ventilation of the lungs by machine or hand. n Spasmolytics: n Drugs used to relax spastic muscles. n Directly Acting Drugs: n Drugs used in spastic diseases.
Skeletal Muscle Relaxants n Neuromuscular Blockers: n Nondepolarizing Drugs (Tubocurarine) n Depolarizing Drugs (Succinylcholine) n Spasmolytics. n Directly Acting Drugs.
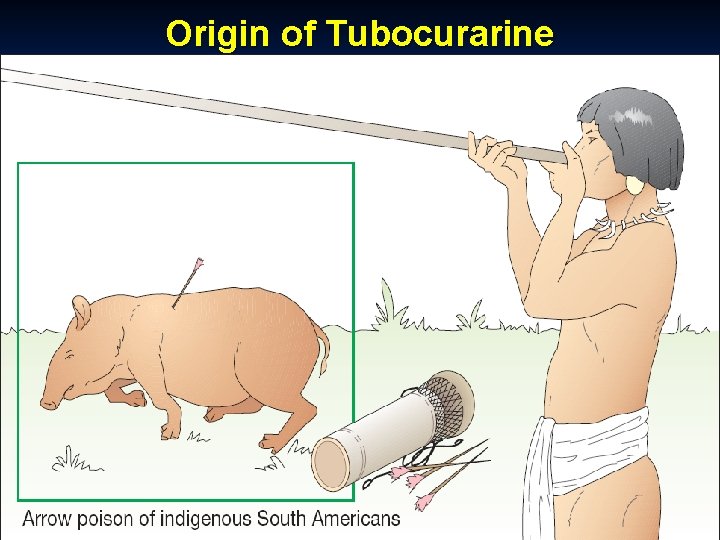
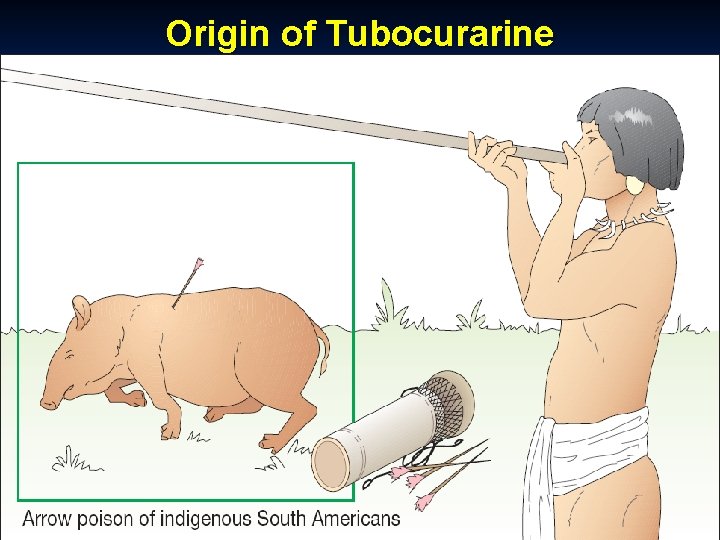
Origin of Tubocurarine
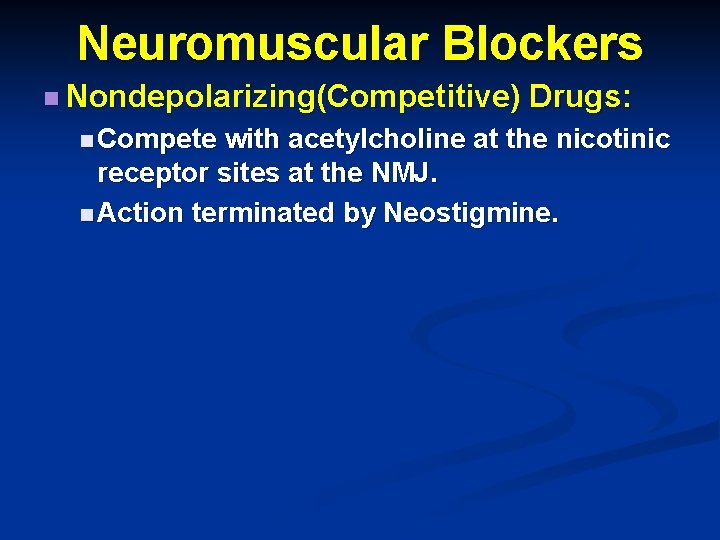
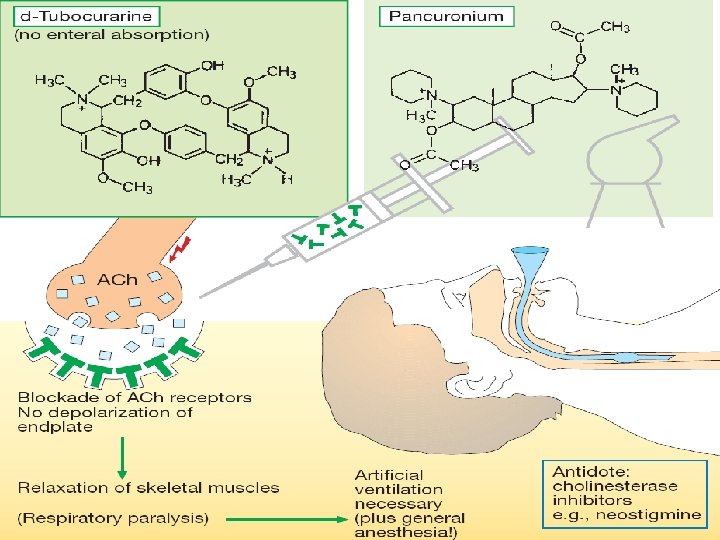
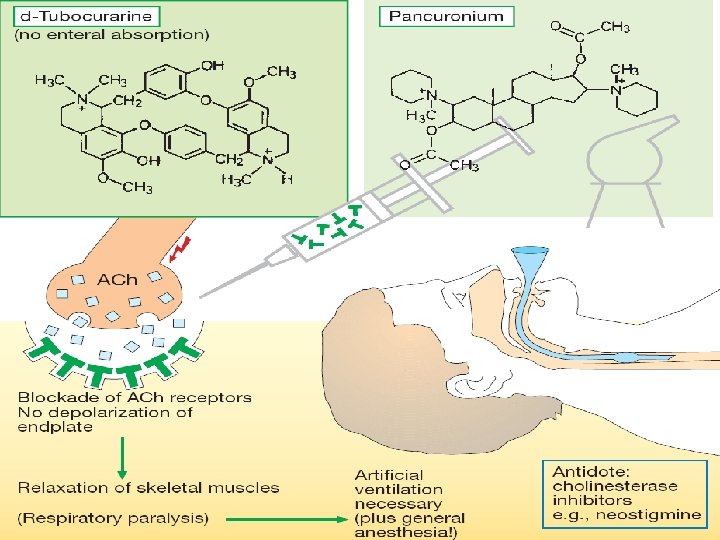
Neuromuscular Blockers n Nondepolarizing(Competitive) Drugs: n Compete with acetylcholine at the nicotinic receptor sites at the NMJ. n Action terminated by Neostigmine.
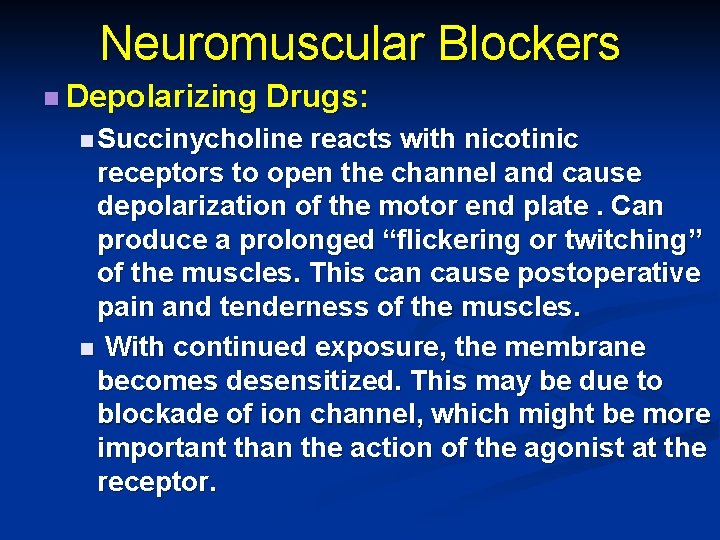
Neuromuscular Blockers n Depolarizing Drugs: n Succinycholine reacts with nicotinic receptors to open the channel and cause depolarization of the motor end plate. Can produce a prolonged “flickering or twitching” of the muscles. This can cause postoperative pain and tenderness of the muscles. n With continued exposure, the membrane becomes desensitized. This may be due to blockade of ion channel, which might be more important than the action of the agonist at the receptor.
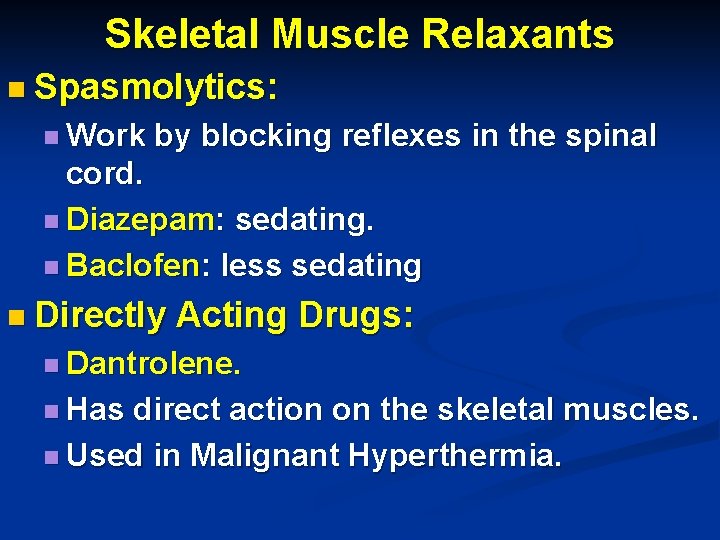
Skeletal Muscle Relaxants n Spasmolytics: n Work by blocking reflexes in the spinal cord. n Diazepam: sedating. n Baclofen: less sedating n Directly Acting Drugs: n Dantrolene. n Has direct action on the skeletal muscles. n Used in Malignant Hyperthermia.
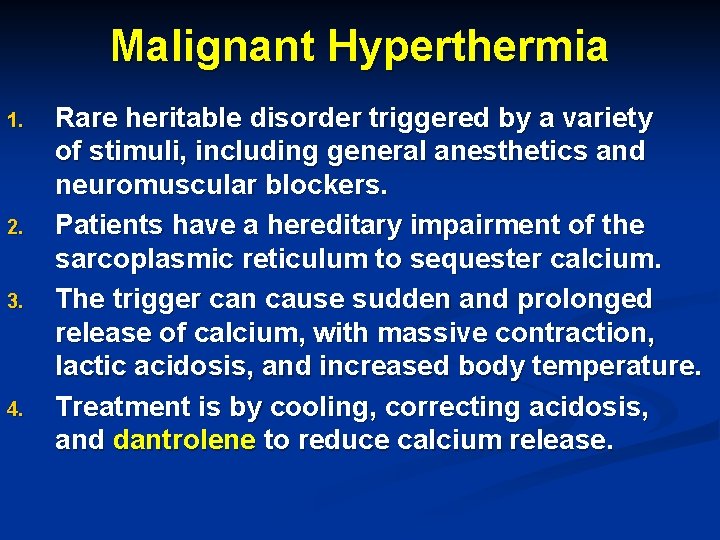
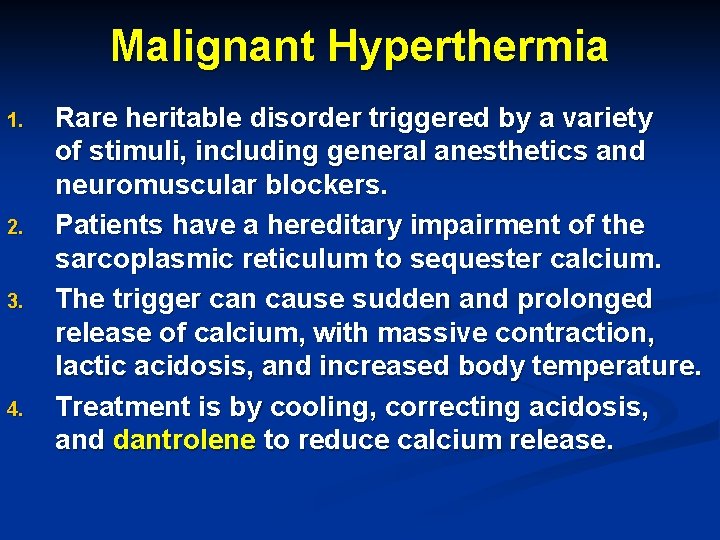
Malignant Hyperthermia 1. 2. 3. 4. Rare heritable disorder triggered by a variety of stimuli, including general anesthetics and neuromuscular blockers. Patients have a hereditary impairment of the sarcoplasmic reticulum to sequester calcium. The trigger can cause sudden and prolonged release of calcium, with massive contraction, lactic acidosis, and increased body temperature. Treatment is by cooling, correcting acidosis, and dantrolene to reduce calcium release.
Malignant Hyperthermia
Botulinum Toxin Produced by Botulinum bacteria. Inhibits acetylcholine release. Food poisoning by this bacteria causes, within 1236 hours, diplopia, dysphagia, dysarthria, and dyspnea. Toxin is used for ophthalmic purposes, local muscle spasms, and in the cosmetic treatment of facial wrinkles around the eyes and mouth, as well as for generalized spastic disorders like cerebral palsy.
 General anesthesia drugs dosage
General anesthesia drugs dosage Do they intubate you for general anesthesia
Do they intubate you for general anesthesia General anesthesia drugs
General anesthesia drugs What is second gas effect
What is second gas effect Remifentanil infusion rate
Remifentanil infusion rate Balanced anesthesia definition
Balanced anesthesia definition Double lumen tube sizing
Double lumen tube sizing Virtual anesthesia machine
Virtual anesthesia machine Fail safe valve anesthesia
Fail safe valve anesthesia Yoke block anesthesia machine
Yoke block anesthesia machine Structure pierced in lumbar puncture
Structure pierced in lumbar puncture Pre anesthesia assessment form
Pre anesthesia assessment form Anterior palatine nerve block
Anterior palatine nerve block Trigeminal
Trigeminal Mechanism of local anesthesia
Mechanism of local anesthesia Mechanism of local anesthesia
Mechanism of local anesthesia Incisive nerve block
Incisive nerve block Types of local anesthesia
Types of local anesthesia Lidocaine max dose
Lidocaine max dose Anesthesia hose
Anesthesia hose Mac anesthesia minimum alveolar concentration
Mac anesthesia minimum alveolar concentration Mac anesthesia minimum alveolar concentration
Mac anesthesia minimum alveolar concentration Balanced anesthesia components
Balanced anesthesia components Classification of inhalational agents
Classification of inhalational agents Dr sanjeewani fonseka channeling
Dr sanjeewani fonseka channeling Spinal anesthesia level chart
Spinal anesthesia level chart Epidural anesthesia drugs
Epidural anesthesia drugs Tuohy needle sizes
Tuohy needle sizes N
N Induction anesthesia
Induction anesthesia