General and local anesthesia General Anesthesia Components Analgesia
- Slides: 36
General and local anesthesia
General Anesthesia Components : • Analgesia (33) • Consciousness control (hypnosis, induced) • Muscle relaxation • Stability of the autonomic nervous system 1; 2; 4
Complications of Acute Pain b Pulmonary - respiratory muscle spasm - immobility - suppression of cough - abdominal distension from decreased GI motility - atelectasis from impaired ventilation - mucus plugging from suppression of clearing mechanisms - V/Q mismatching and hypoxemia - Pulmonary infections
Complications of Acute Pain Hematologic - increase thrombus formation by increasing blood viscosity - increasing activity of clotting factors - increasing platelet aggregation
Complications of Acute Pain Cardiovascular Acute rise in HR, BP, Cardiac Output = increased cardiac work and oxygen consumption. This could be disastrous for patients with ischemic heart diseases and may lead to myocardial infarction and /or CHF
Complications of Acute Pain b Gastrointestinal - Ileus - Nausea - Vomiting - Decreased bowel motility b Urinary - hypomotility of the urethra and bladder - difficulty with urination
Complications of Acute Pain b Neuroendocrine and Metabolic - increased sympathetic tone & hypothalamic stimulation - increased catecholamine and catabolic hormone secretion - increased metabolism and O 2 consumption
Complications of Acute Pain b Psychological - fear - anxiety - depression - frustration
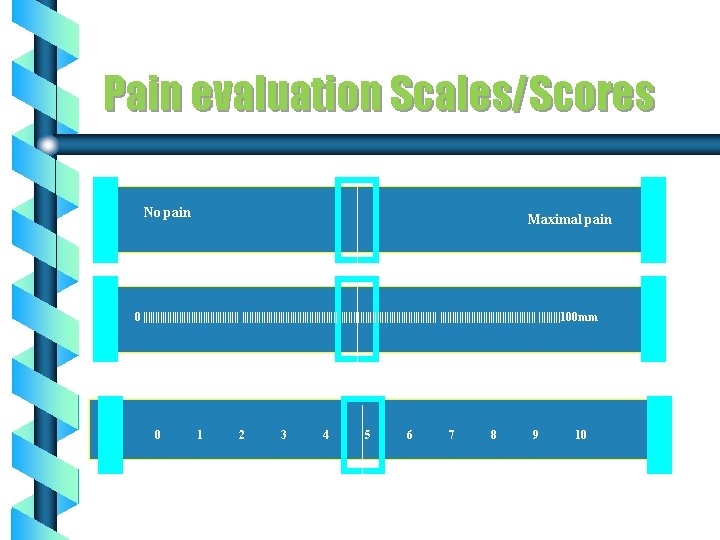
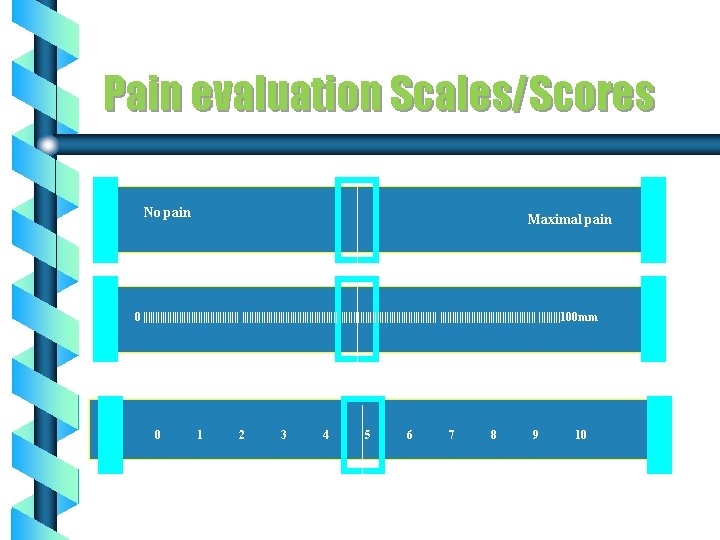
Pain evaluation Scales/Scores No pain Maximal pain 0 |||||||||||||||||||||||||||||||||||||||| |||||100 mm 0 1 2 3 4 5 6 7 8 9 10
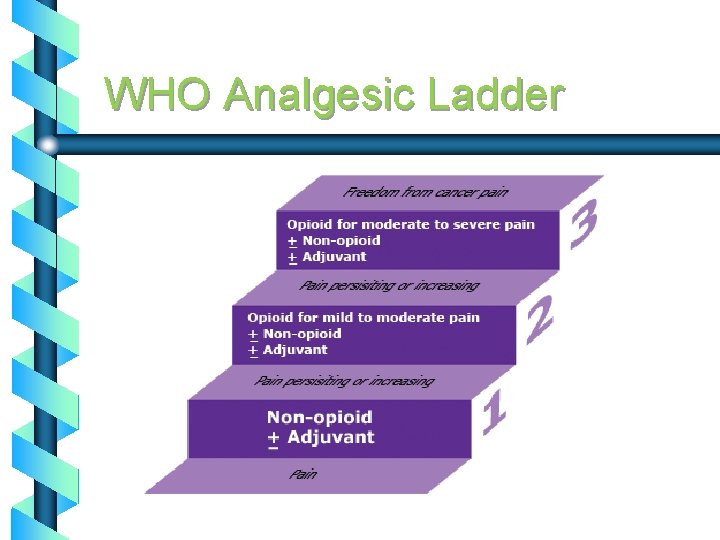
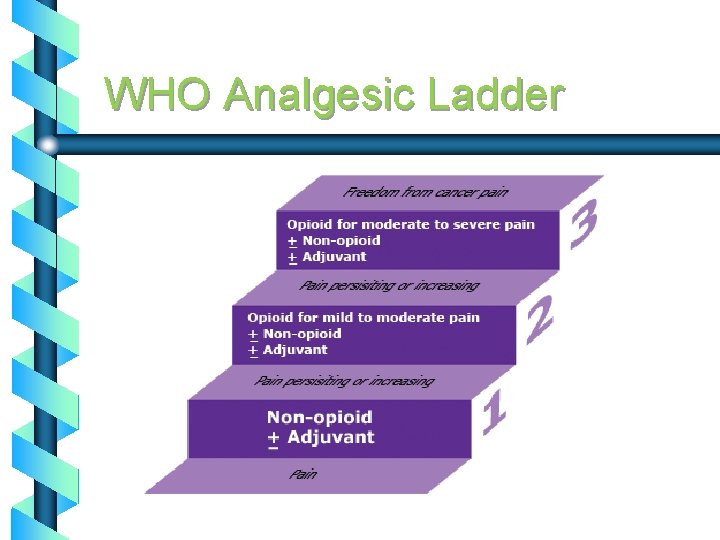
WHO Analgesic Ladder
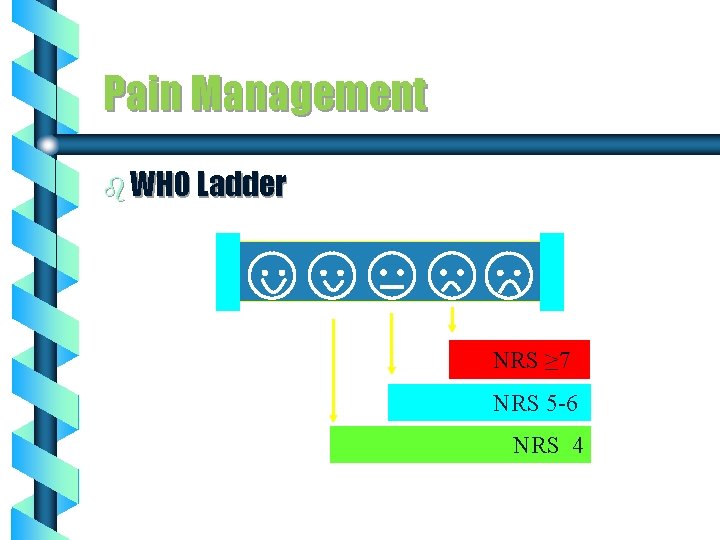
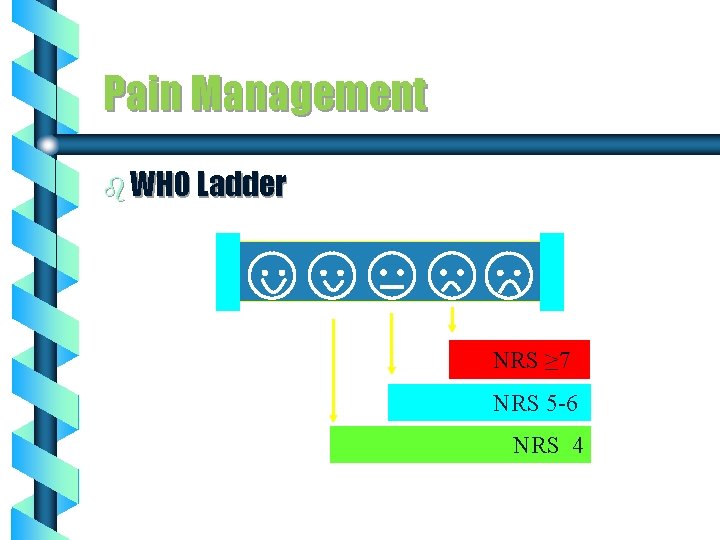
Pain Management b WHO Ladder NRS ≥ 7 NRS 5 -6 NRS 4
ANESTHESIA - Partial or complete loss of sensation with or with out loss of consciousness as result of disease, injury, or administration of an anesthetic agent, usually by injection or inhalation.
Anesthesia The main goal is control of the vital functions of the human body in the framework of the surgery in order to protect the patient from the operative stress
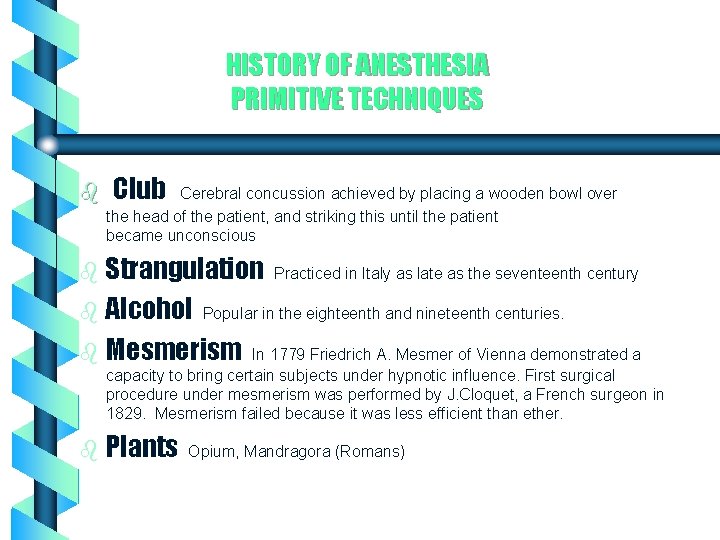
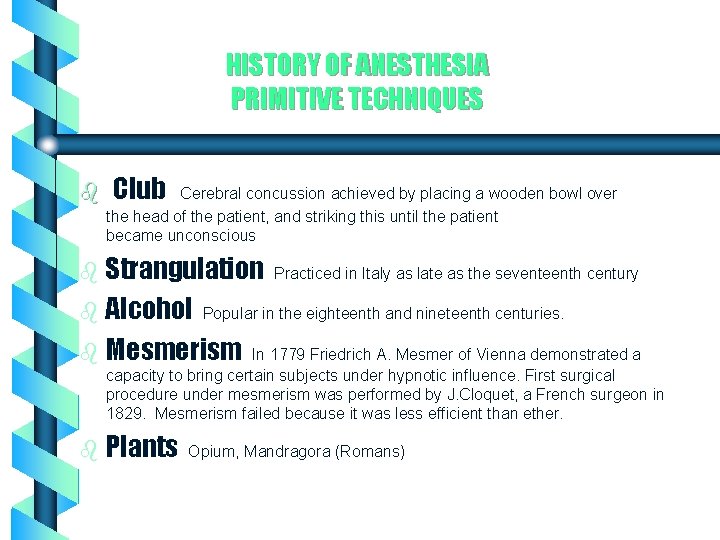
HISTORY OF ANESTHESIA PRIMITIVE TECHNIQUES b Club Cerebral concussion achieved by placing a wooden bowl over the head of the patient, and striking this until the patient became unconscious b Strangulation b Alcohol Practiced in Italy as late as the seventeenth century Popular in the eighteenth and nineteenth centuries. b Mesmerism In 1779 Friedrich A. Mesmer of Vienna demonstrated a capacity to bring certain subjects under hypnotic influence. First surgical procedure under mesmerism was performed by J. Cloquet, a French surgeon in 1829. Mesmerism failed because it was less efficient than ether. b Plants Opium, Mandragora (Romans)
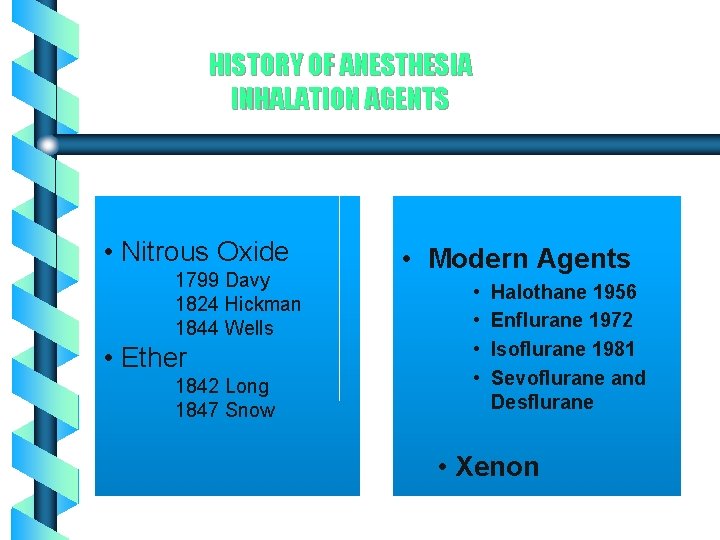
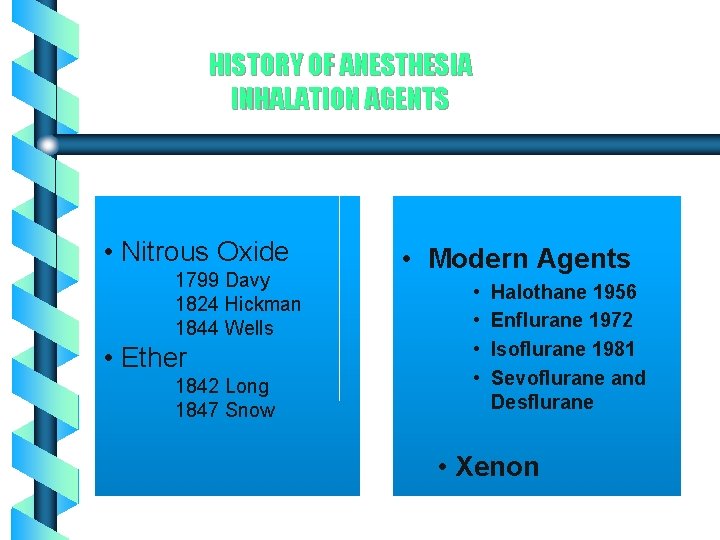
HISTORY OF ANESTHESIA INHALATION AGENTS • Nitrous Oxide 1799 Davy 1824 Hickman 1844 Wells • Ether 1842 Long 1847 Snow • Modern Agents • • Halothane 1956 Enflurane 1972 Isoflurane 1981 Sevoflurane and Desflurane • Xenon
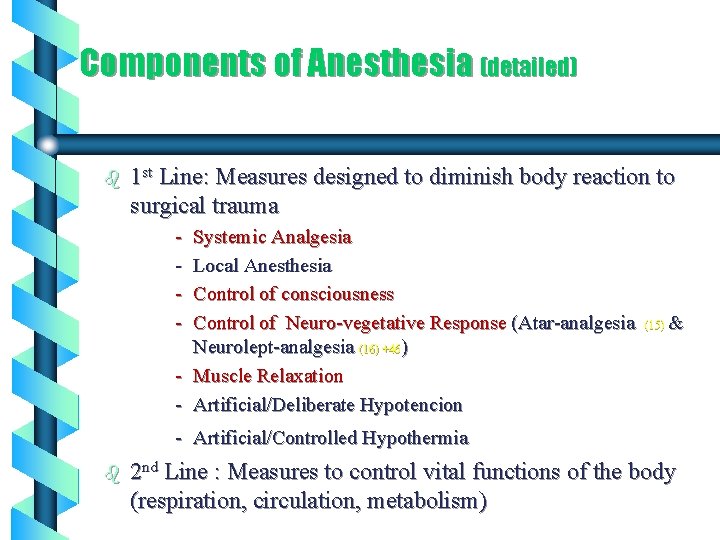
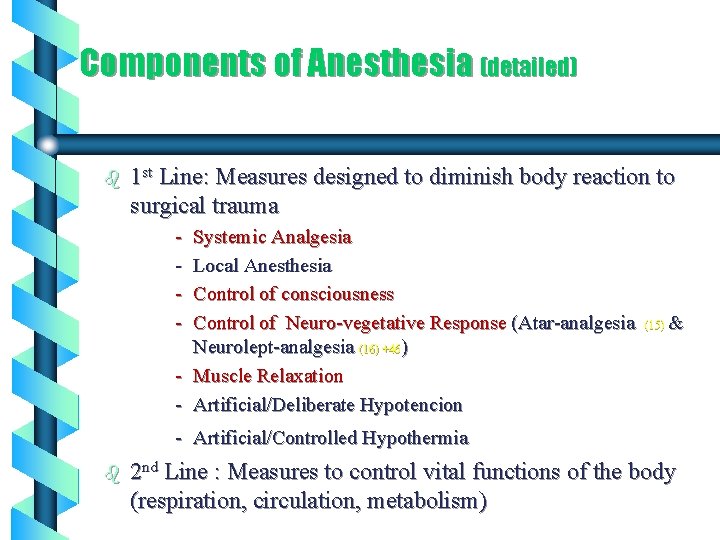
Components of Anesthesia (detailed) b 1 st Line: Measures designed to diminish body reaction to surgical trauma - Systemic Analgesia Local Anesthesia Control of consciousness Control of Neuro-vegetative Response (Atar-analgesia Neurolept-analgesia (16) +46) - Muscle Relaxation - Artificial/Deliberate Hypotencion (15) & - Artificial/Controlled Hypothermia b 2 nd Line : Measures to control vital functions of the body (respiration, circulation, metabolism)
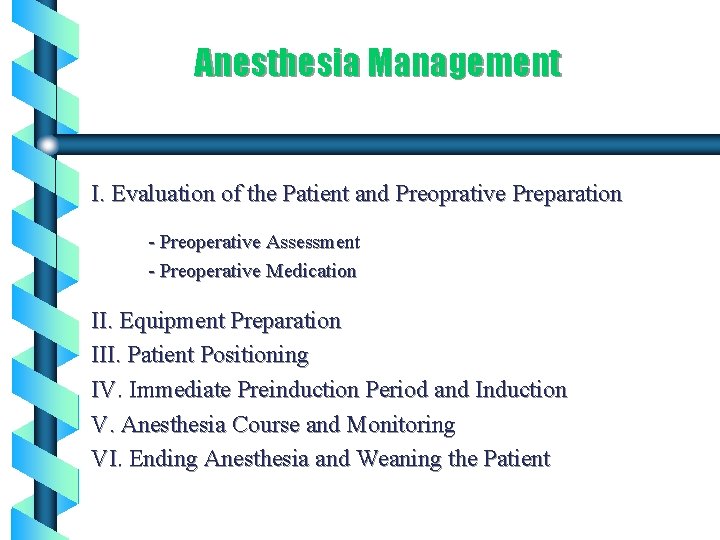
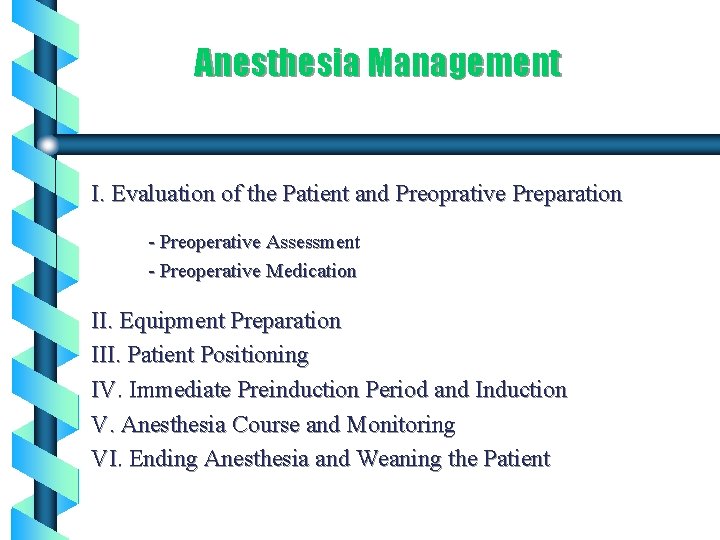
Anesthesia Management I. Evaluation of the Patient and Preoprative Preparation - Preoperative Assessment - Preoperative Medication II. Equipment Preparation III. Patient Positioning IV. Immediate Preinduction Period and Induction V. Anesthesia Course and Monitoring VI. Ending Anesthesia and Weaning the Patient
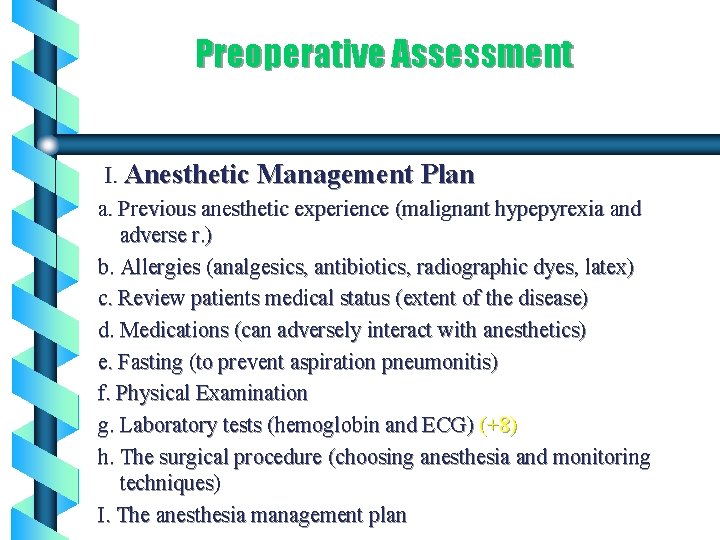
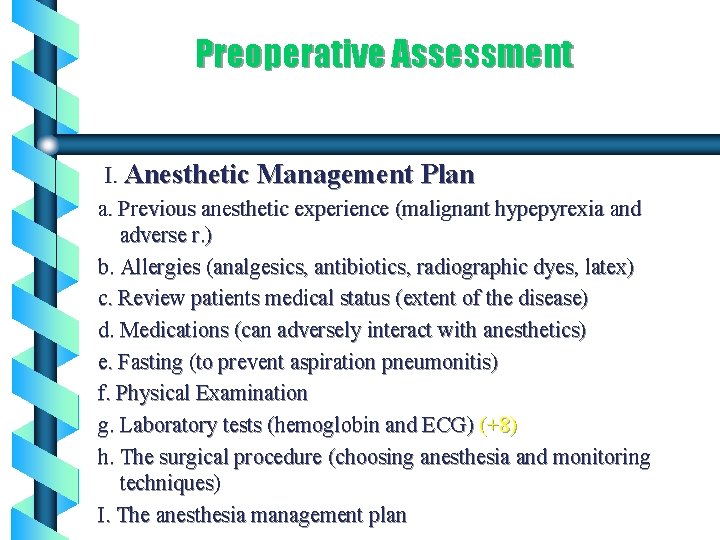
Preoperative Assessment I. Anesthetic Management Plan a. Previous anesthetic experience (malignant hypepyrexia and adverse r. ) b. Allergies (analgesics, antibiotics, radiographic dyes, latex) c. Review patients medical status (extent of the disease) d. Medications (can adversely interact with anesthetics) e. Fasting (to prevent aspiration pneumonitis) f. Physical Examination g. Laboratory tests (hemoglobin and ECG) (+8) h. The surgical procedure (choosing anesthesia and monitoring techniques) I. The anesthesia management plan
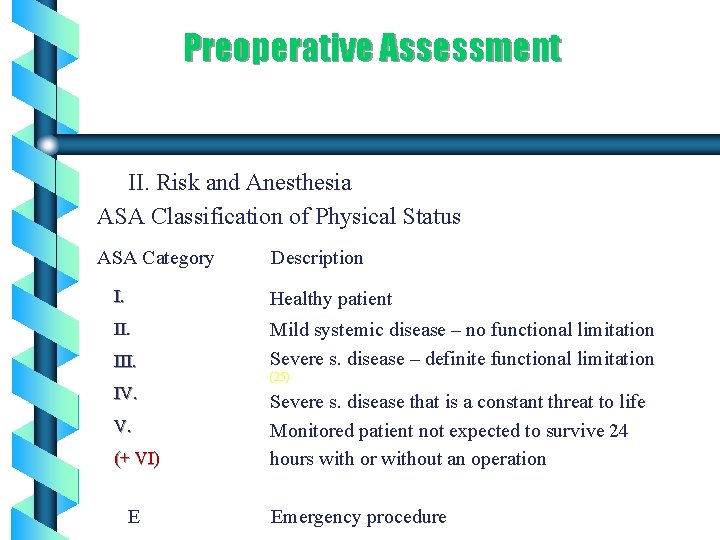
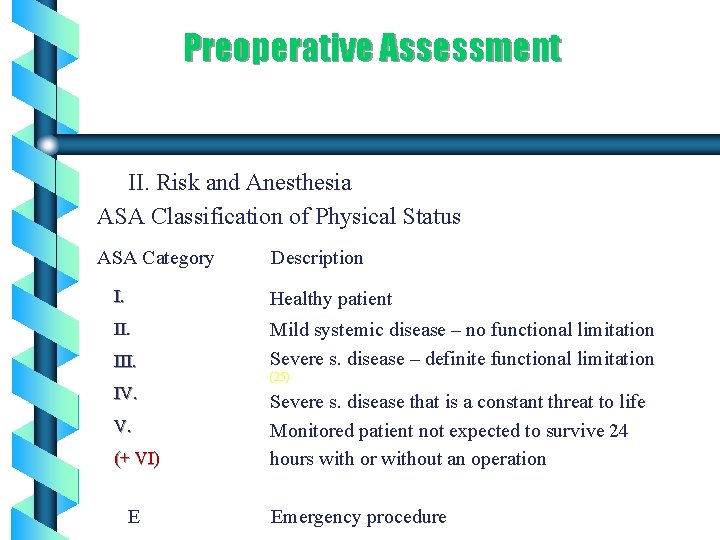
Preoperative Assessment II. Risk and Anesthesia ASA Classification of Physical Status ASA Category Description I. Healthy patient II. Mild systemic disease – no functional limitation Severe s. disease – definite functional limitation III. IV. V. (+ VI) E (25) Severe s. disease that is a constant threat to life Monitored patient not expected to survive 24 hours with or without an operation Emergency procedure
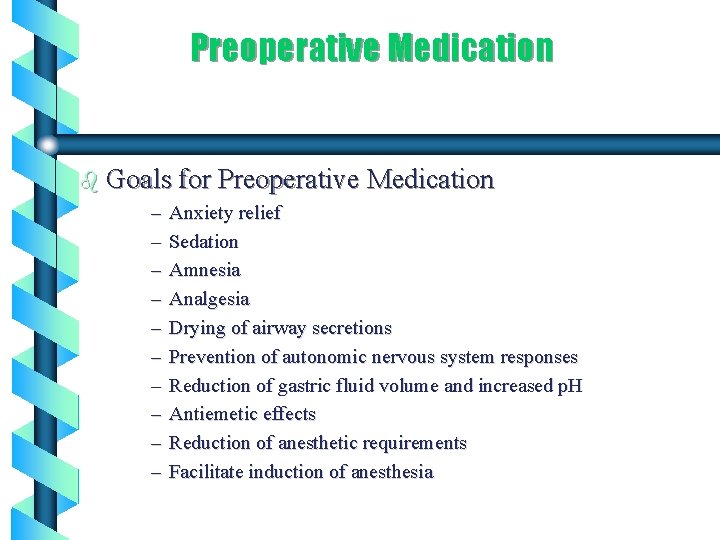
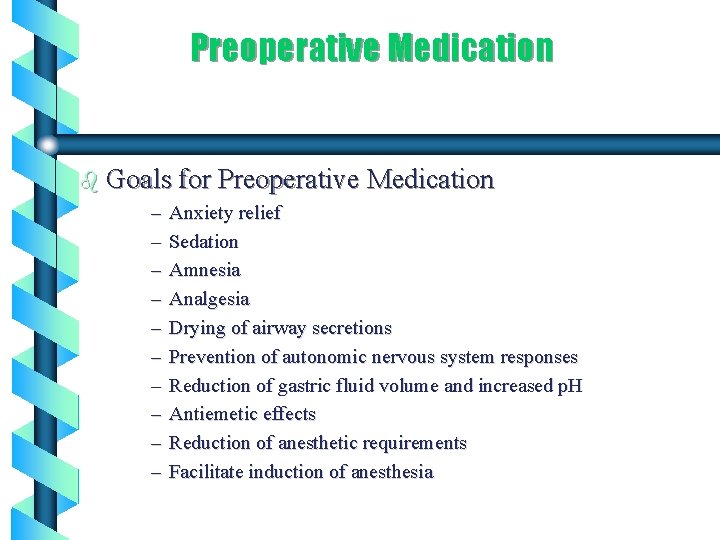
Preoperative Medication b Goals for Preoperative Medication – Anxiety relief – Sedation – Amnesia – Analgesia – Drying of airway secretions – Prevention of autonomic nervous system responses – Reduction of gastric fluid volume and increased p. H – Antiemetic effects – Reduction of anesthetic requirements – Facilitate induction of anesthesia
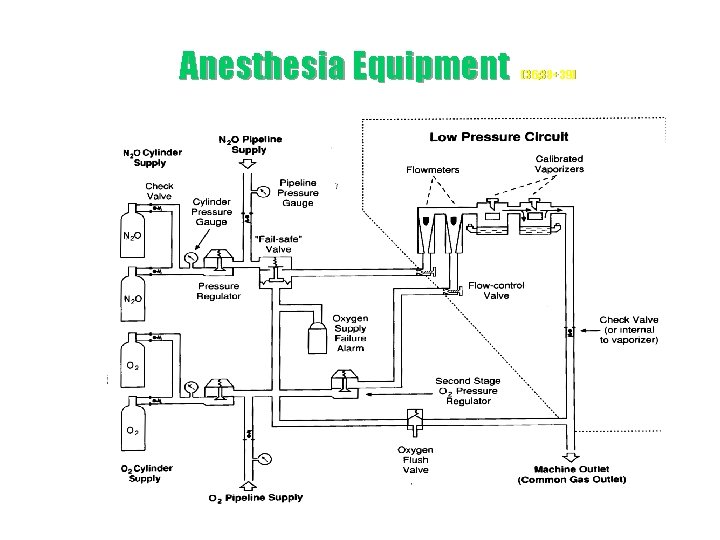
Anesthesia Equipment
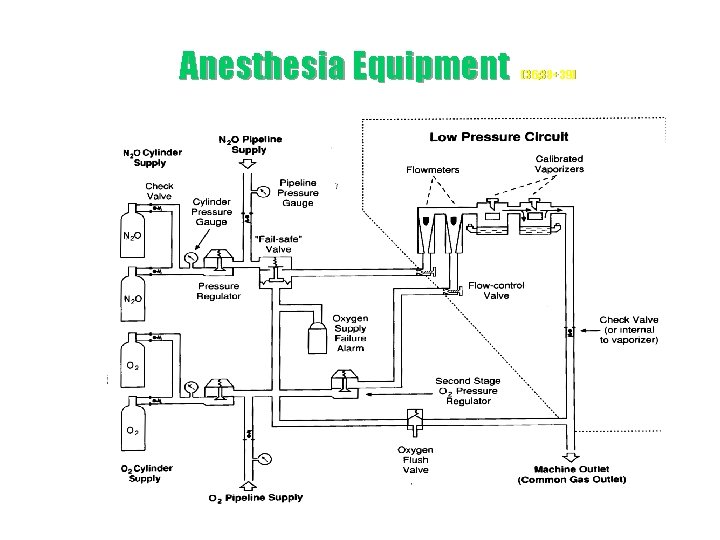
Anesthesia Equipment (36; 38+39)
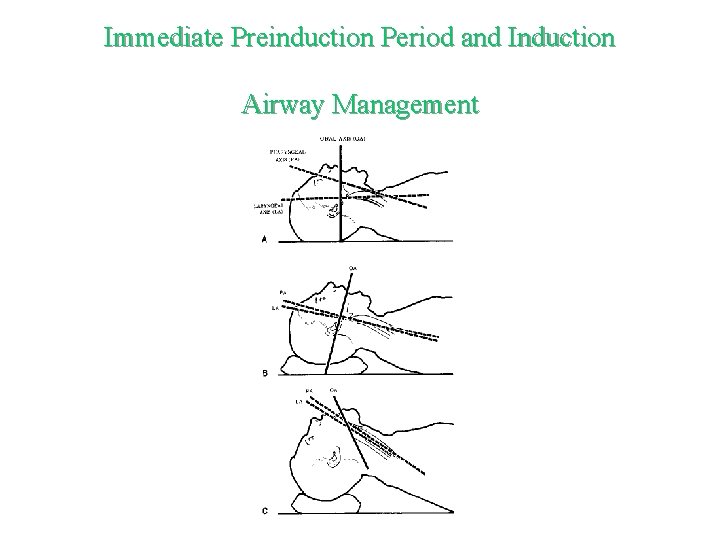
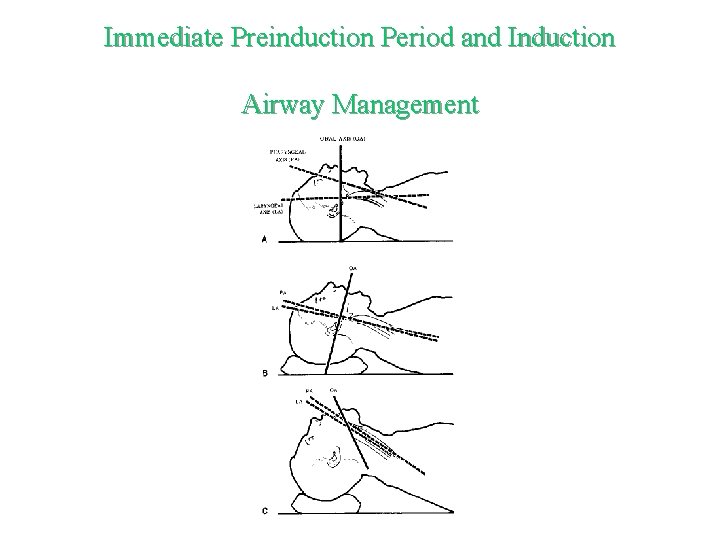
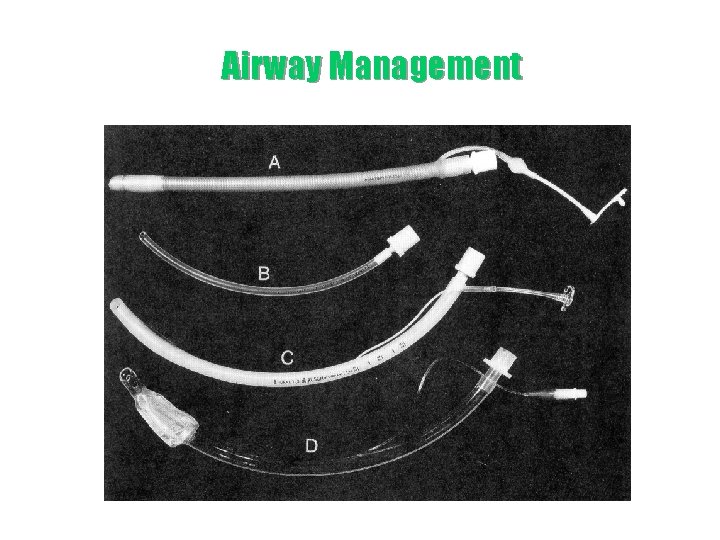
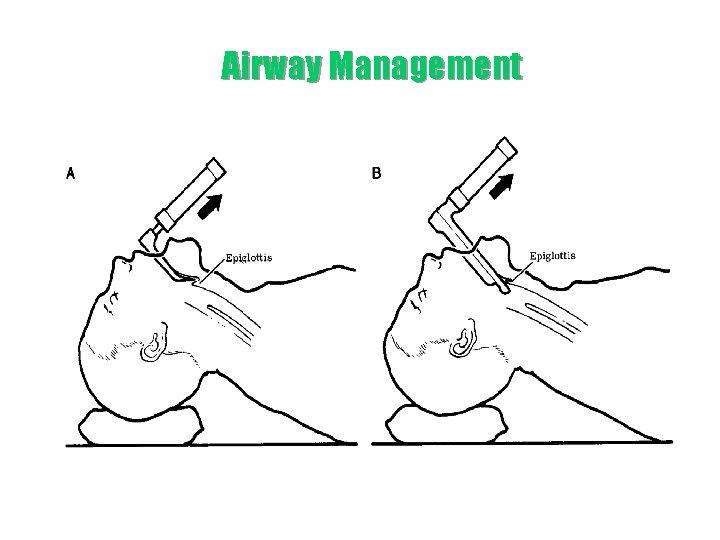
Immediate Preinduction Period and Induction Airway Management
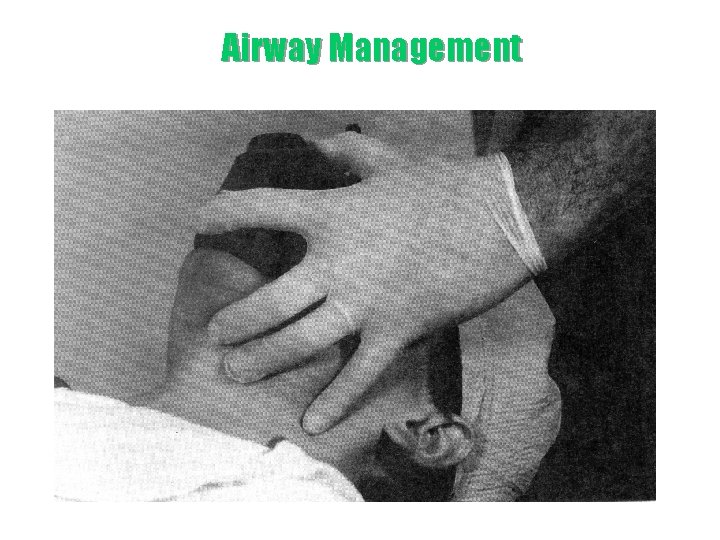
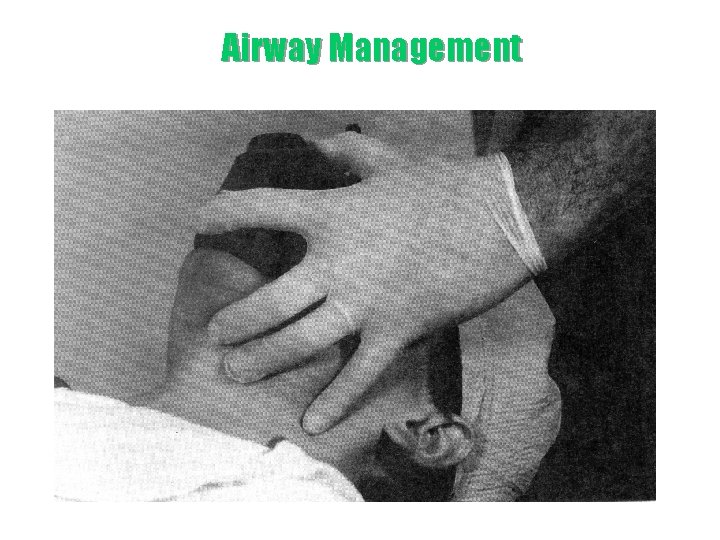
Airway Management
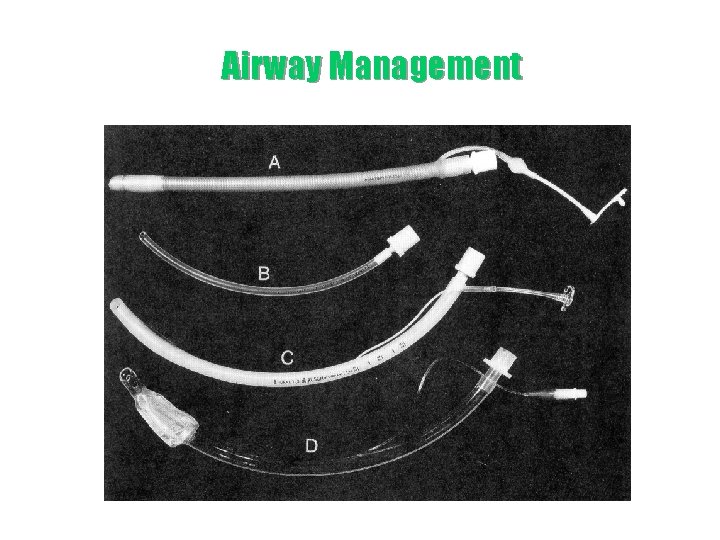
Airway Management
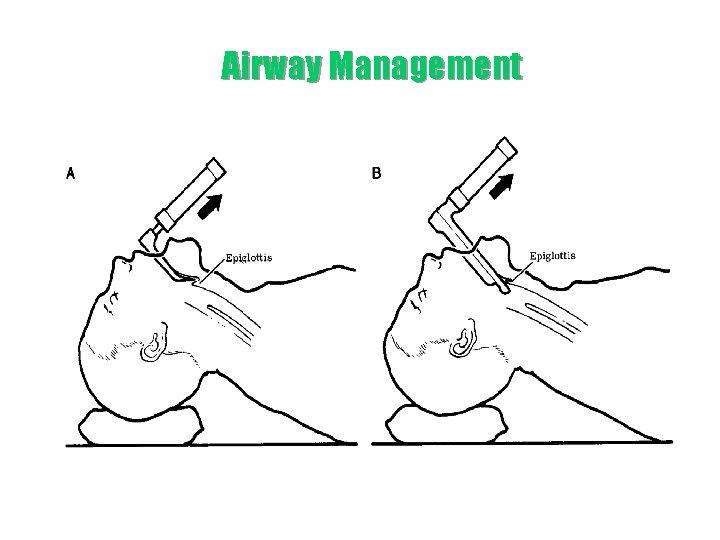
Airway Management
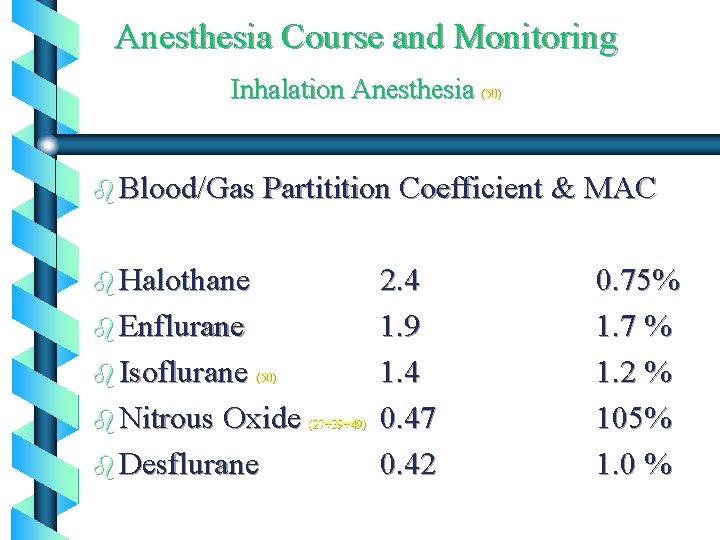
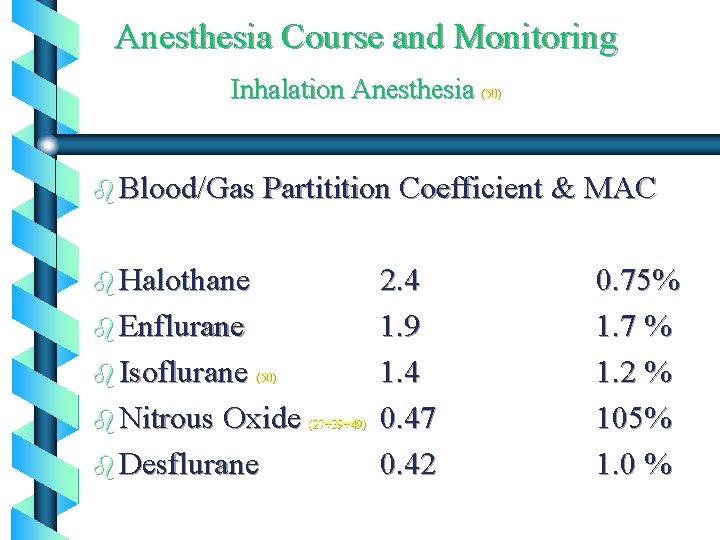
Anesthesia Course and Monitoring Inhalation Anesthesia (50) b Blood/Gas Partitition Coefficient & MAC b Halothane b Enflurane b Isoflurane (50) b Nitrous Oxide (27+39+49) b Desflurane 2. 4 1. 9 1. 4 0. 47 0. 42 0. 75% 1. 7 % 1. 2 % 105% 1. 0 %
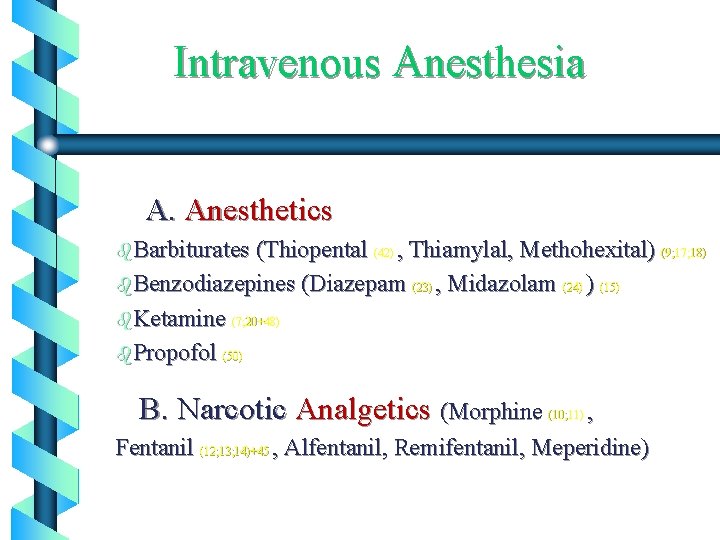
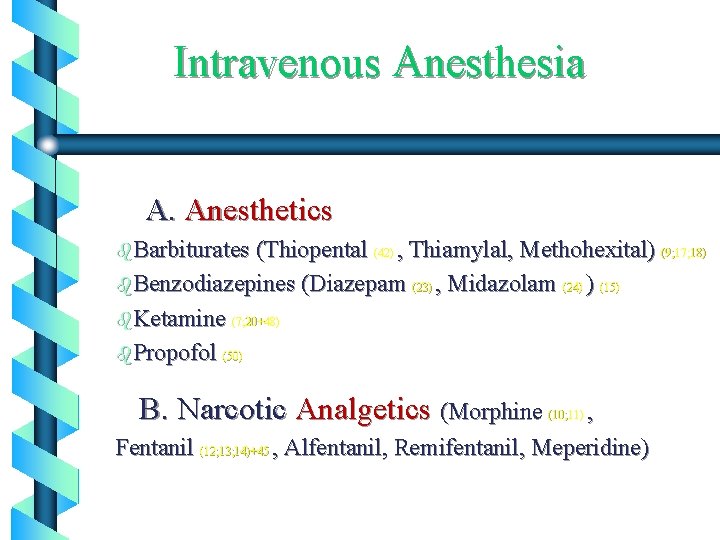
Intravenous Anesthesia A. Anesthetics b. Barbiturates (Thiopental (42) , Thiamylal, Methohexital) (9; 17; 18) b. Benzodiazepines (Diazepam (23) , Midazolam (24) ) (15) b. Ketamine (7; 20+48) b. Propofol (50) B. Narcotic Analgetics (Morphine , Fentanil (12; 13; 14)+45 , Alfentanil, Remifentanil, Meperidine) (10; 11)
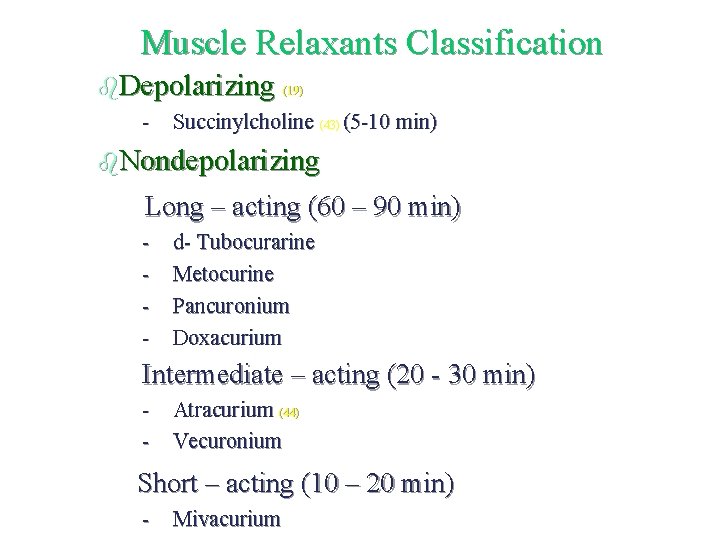
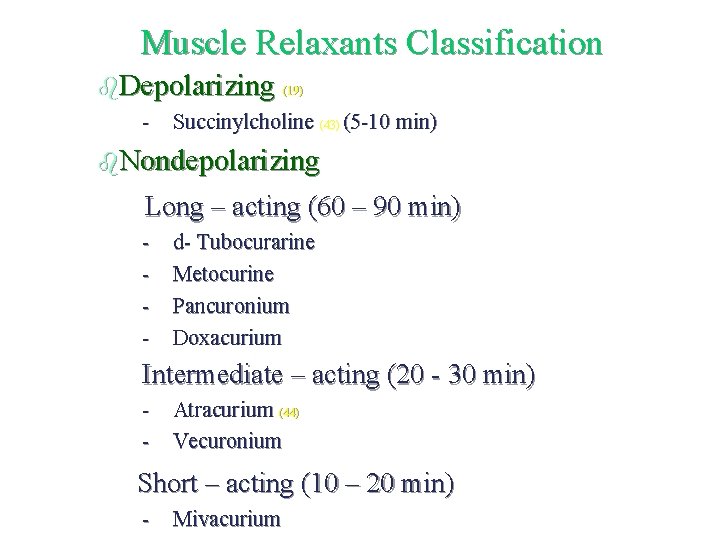
Muscle Relaxants Classification b. Depolarizing (19) - Succinylcholine (43) (5 -10 min) b. Nondepolarizing Long – acting (60 – 90 min) - d- Tubocurarine Metocurine Pancuronium Doxacurium Intermediate – acting (20 - 30 min) - Atracurium (44) - Vecuronium Short – acting (10 – 20 min) - Mivacurium
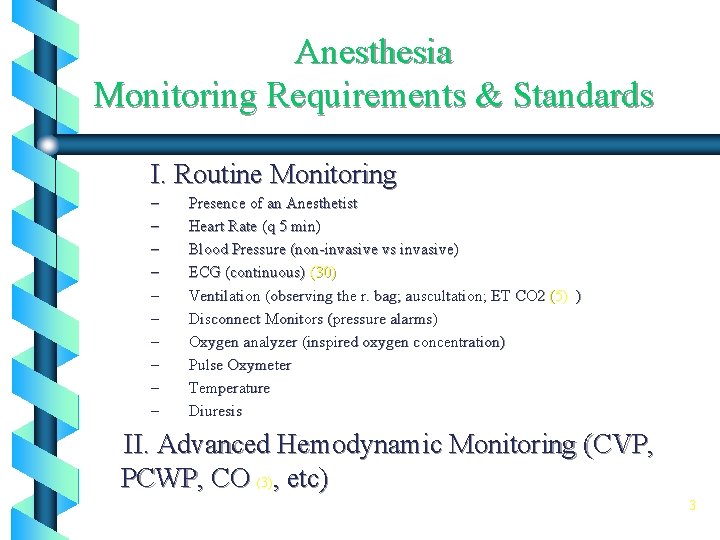
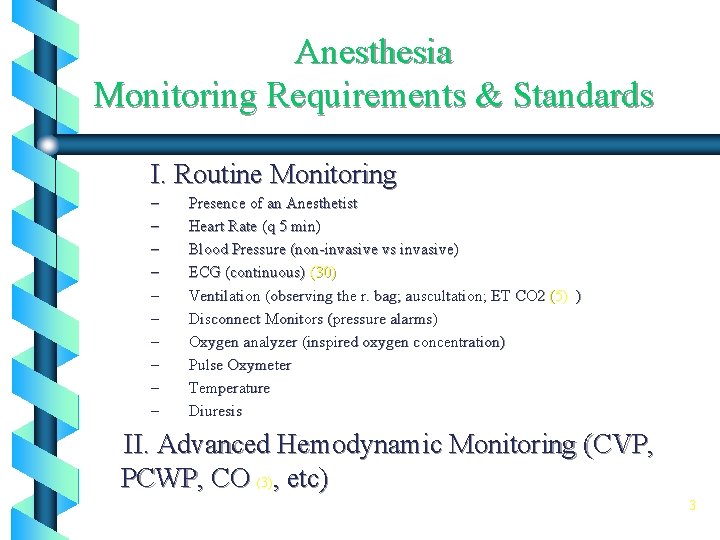
Anesthesia Monitoring Requirements & Standards I. Routine Monitoring – – – – – Presence of an Anesthetist Heart Rate (q 5 min) Blood Pressure (non-invasive vs invasive) ECG (continuous) (30) Ventilation (observing the r. bag; auscultation; ET CO 2 (5) ) Disconnect Monitors (pressure alarms) Oxygen analyzer (inspired oxygen concentration) Pulse Oxymeter Temperature Diuresis II. Advanced Hemodynamic Monitoring (CVP, PCWP, CO (3), etc) 3
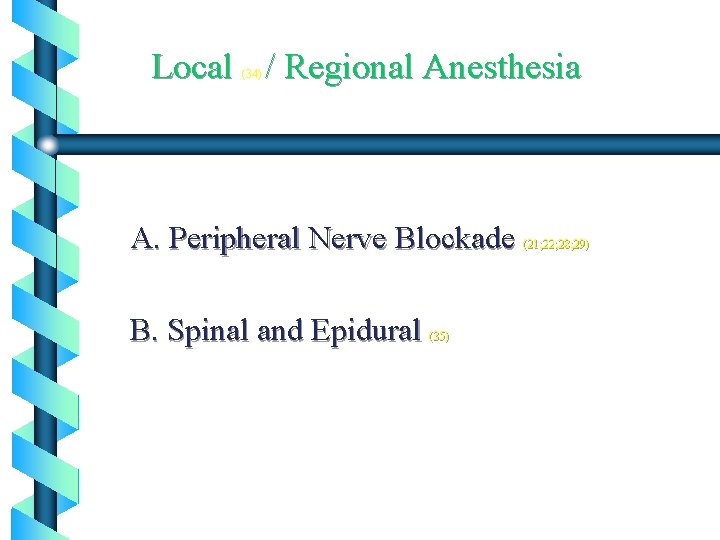
Local / Regional Anesthesia (34) A. Peripheral Nerve Blockade B. Spinal and Epidural (35) (21; 22; 28; 29)
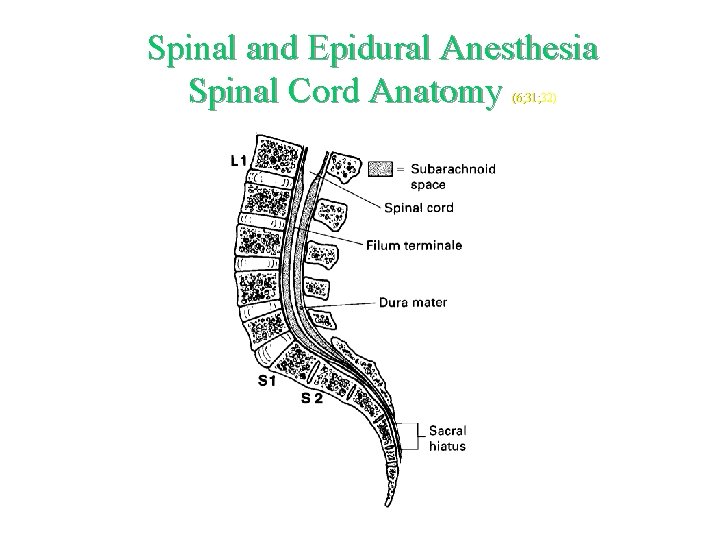
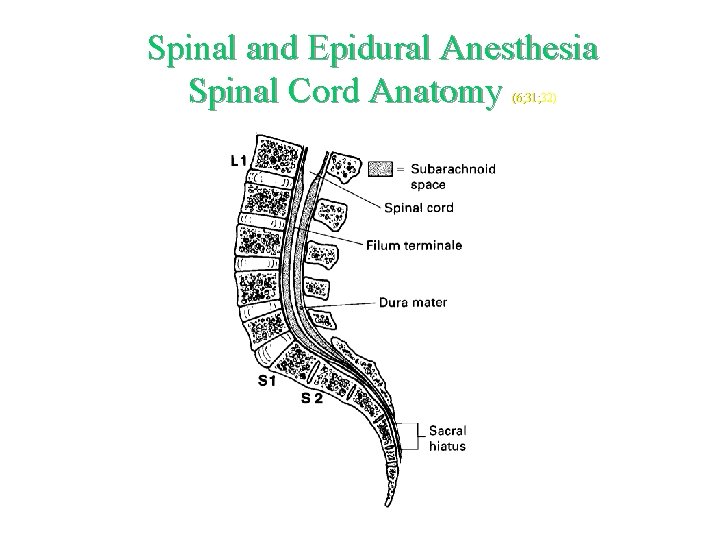
Spinal and Epidural Anesthesia Spinal Cord Anatomy (6; 31; 32)
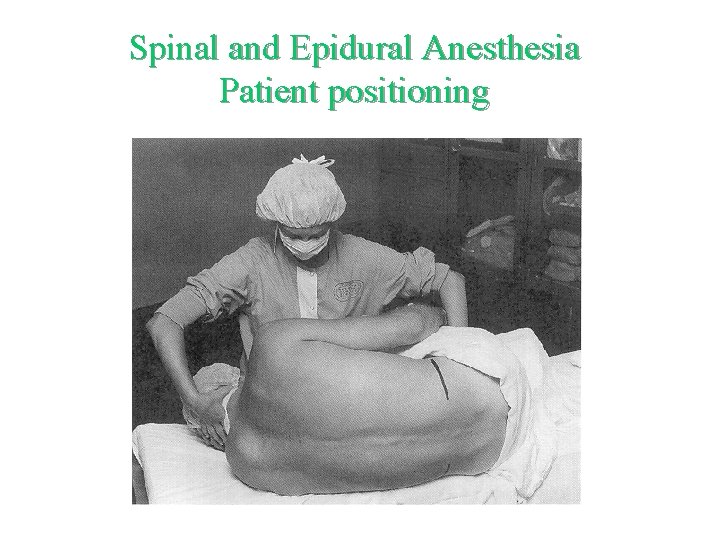
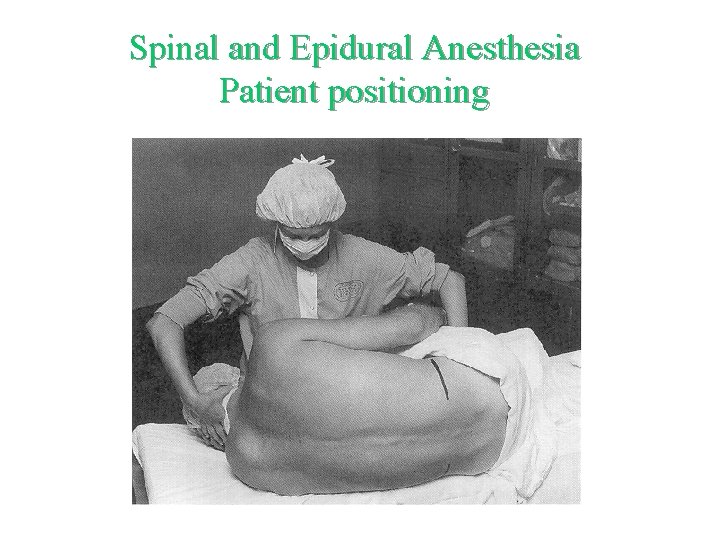
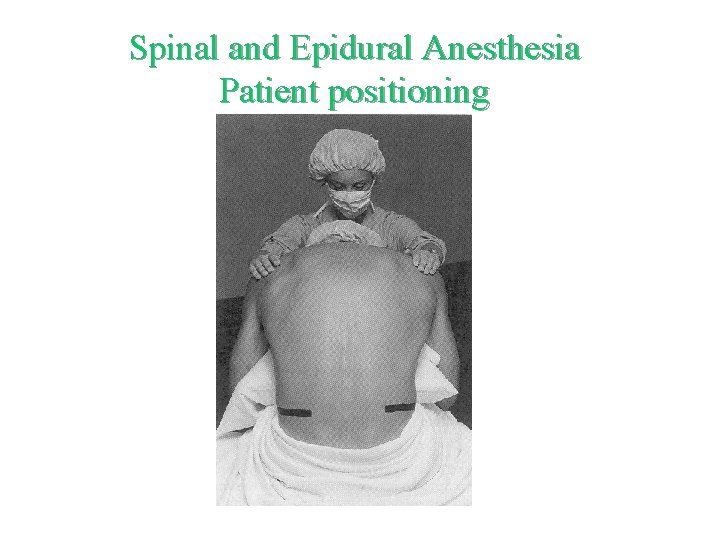
Spinal and Epidural Anesthesia Patient positioning
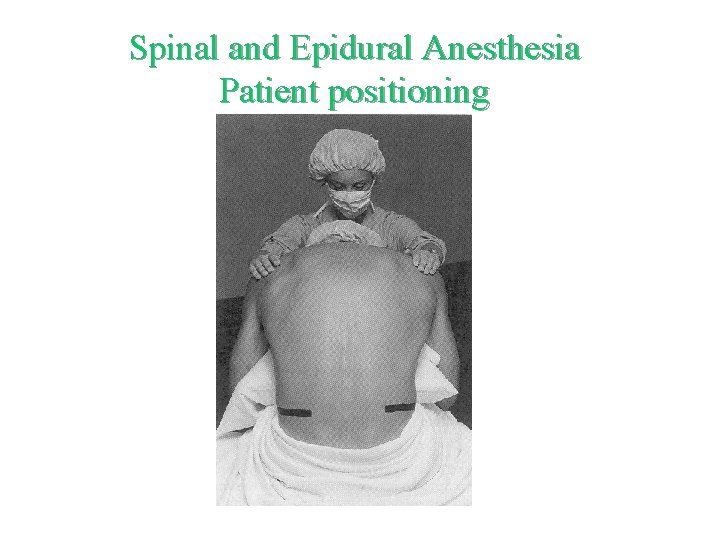
Spinal and Epidural Anesthesia Patient positioning
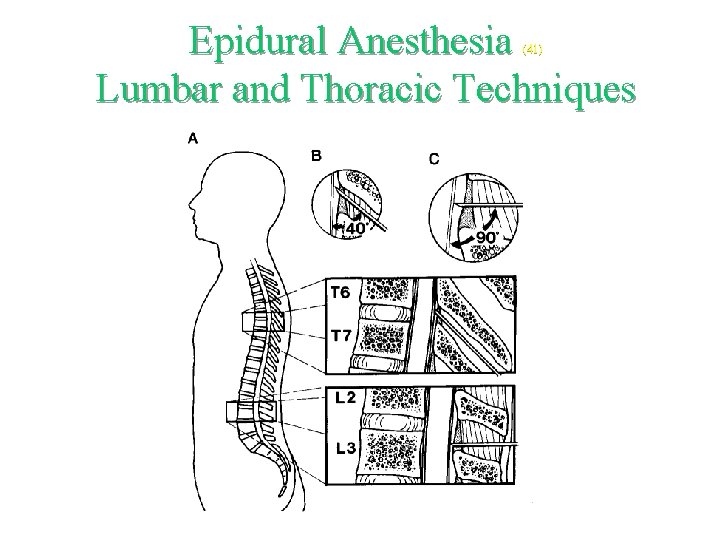
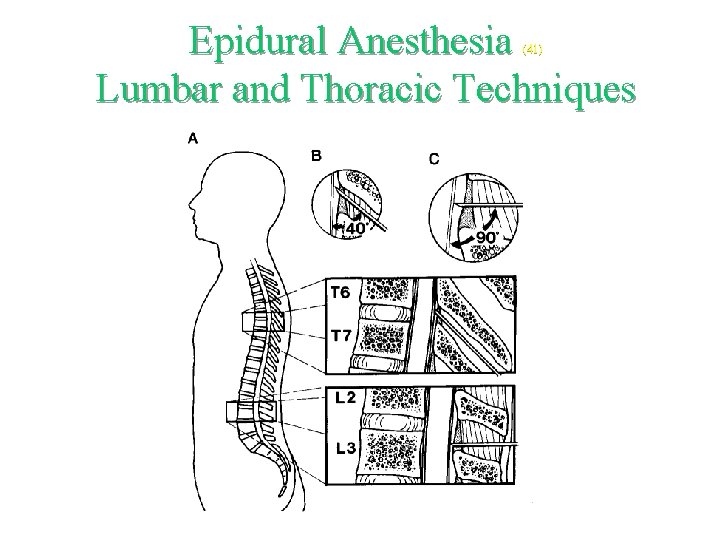
Epidural Anesthesia Lumbar and Thoracic Techniques (41)
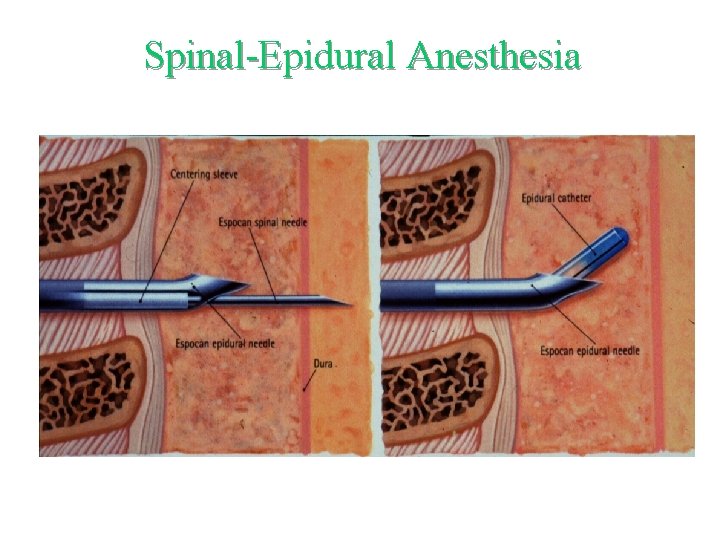
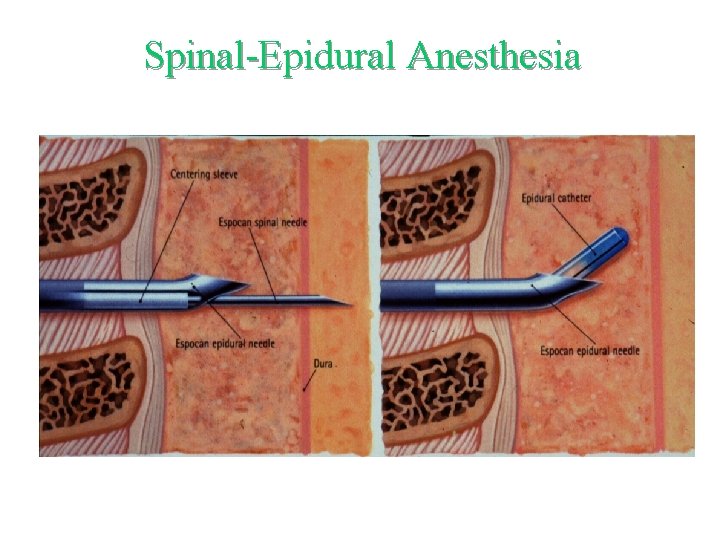
Spinal-Epidural Anesthesia