INHALATIONAL ANAESTHETICS PROPERTIES Inhalation anesthetics are one of
- Slides: 24
INHALATIONAL ANAESTHETICS
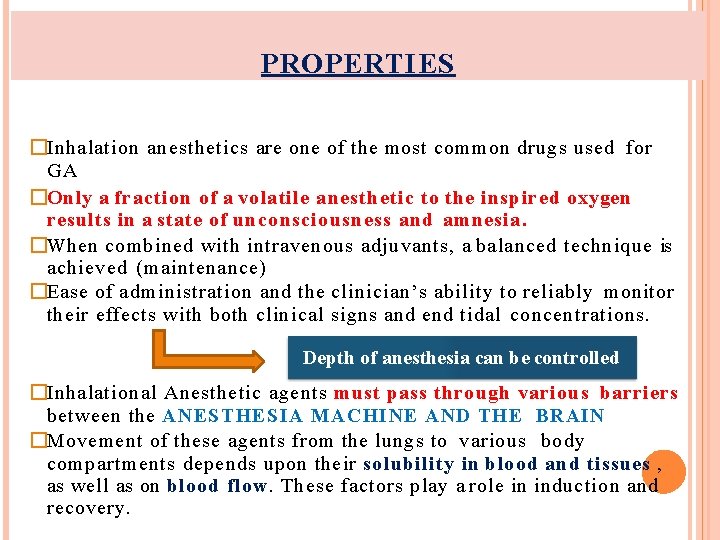
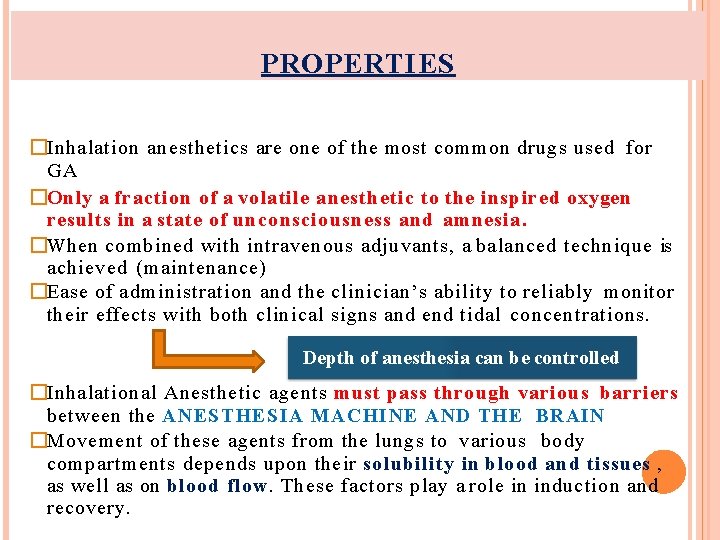
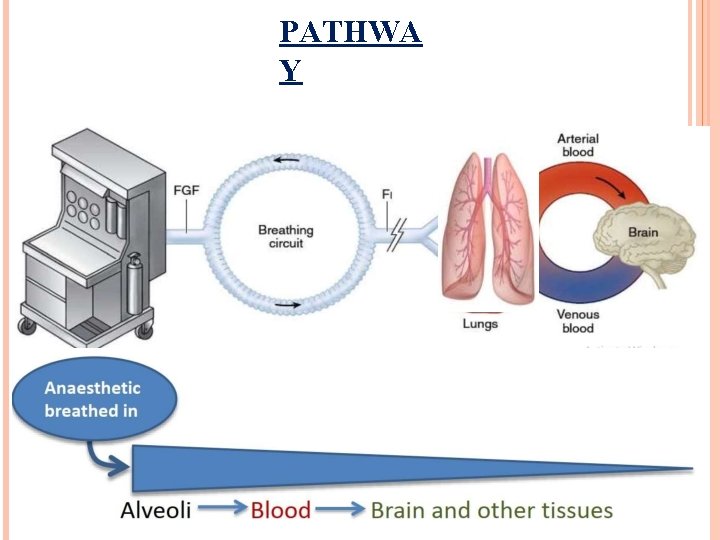
PROPERTIES �Inhalation anesthetics are one of the most common drugs used for GA �Only a fraction of a volatile anesthetic to the inspired oxygen results in a state of unconsciousness and amnesia. �When combined with intravenous adjuvants, a balanced technique is achieved (maintenance) �Ease of administration and the clinician’s ability to reliably monitor their effects with both clinical signs and end tidal concentrations. Depth of anesthesia can be controlled �Inhalational Anesthetic agents must pass through various barriers between the ANESTHESIA MACHINE AND THE BRAIN �Movement of these agents from the lungs to various body compartments depends upon their solubility in blood and tissues , as well as on blood flow. These factors play a role in induction and recovery.
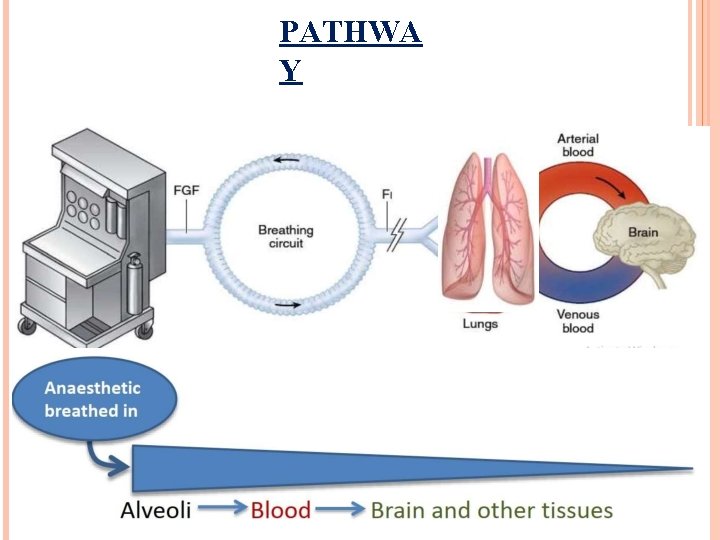
PATHWA Y
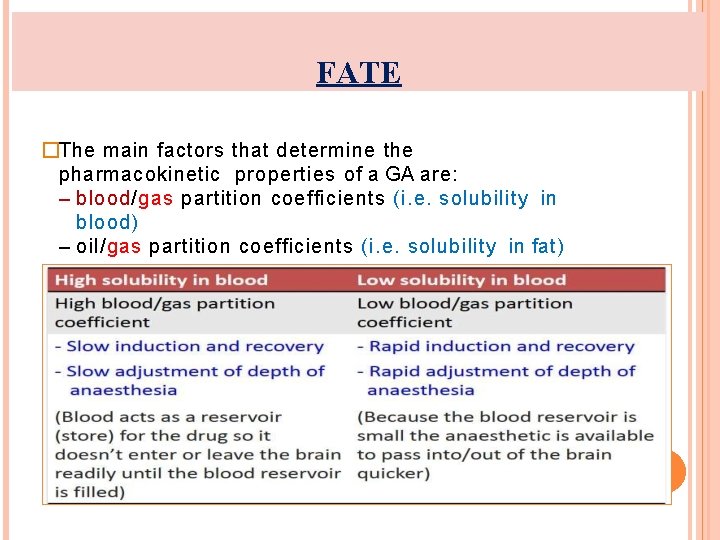
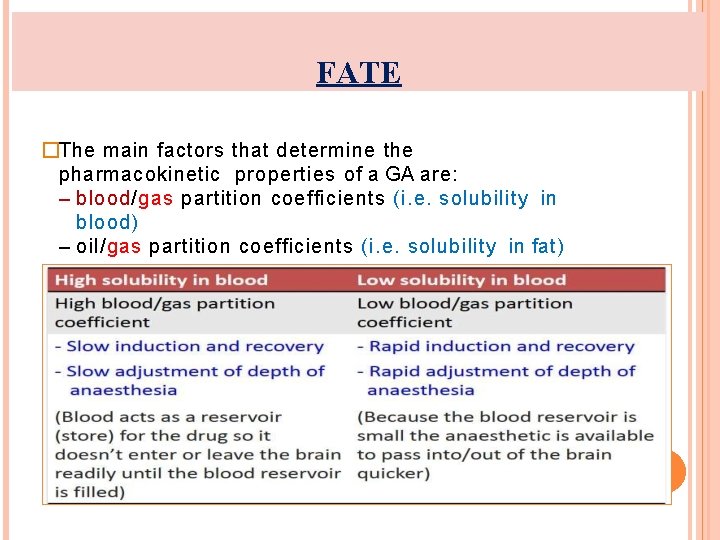
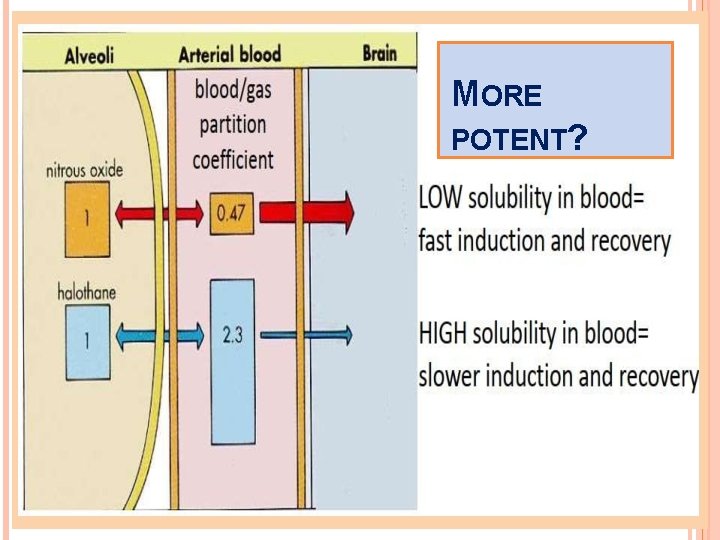
FATE �The main factors that determine the pharmacokinetic properties of a GA are: – blood/gas partition coefficients (i. e. solubility in blood) – oil/gas partition coefficients (i. e. solubility in fat)
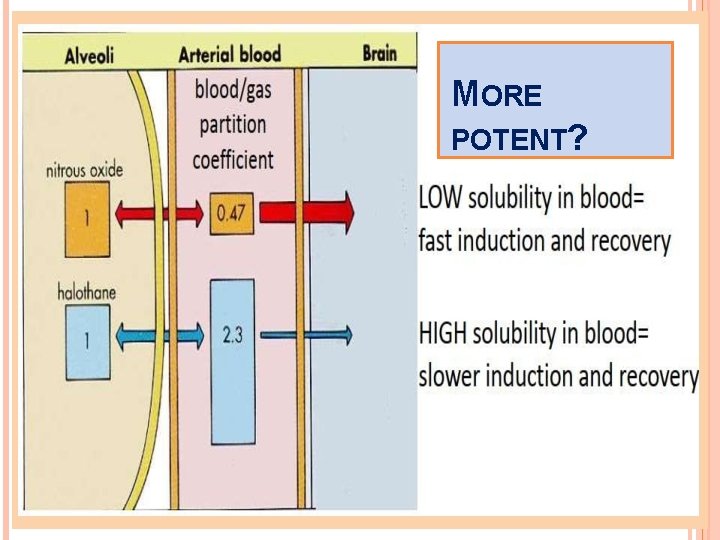
MORE POTENT?
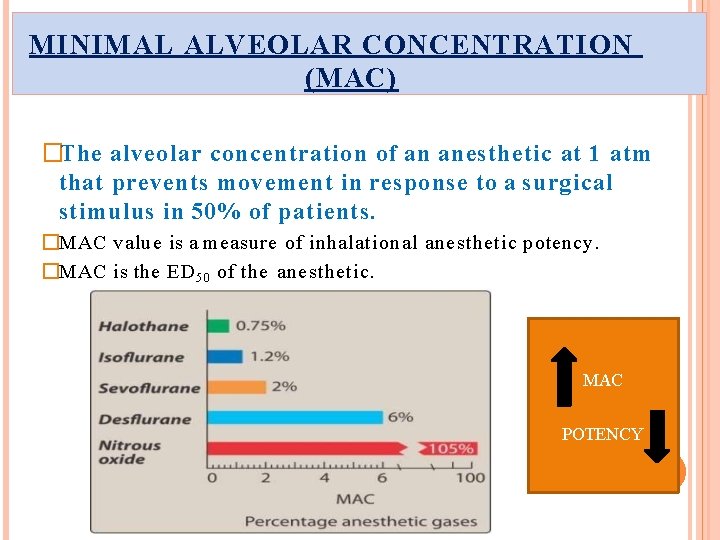
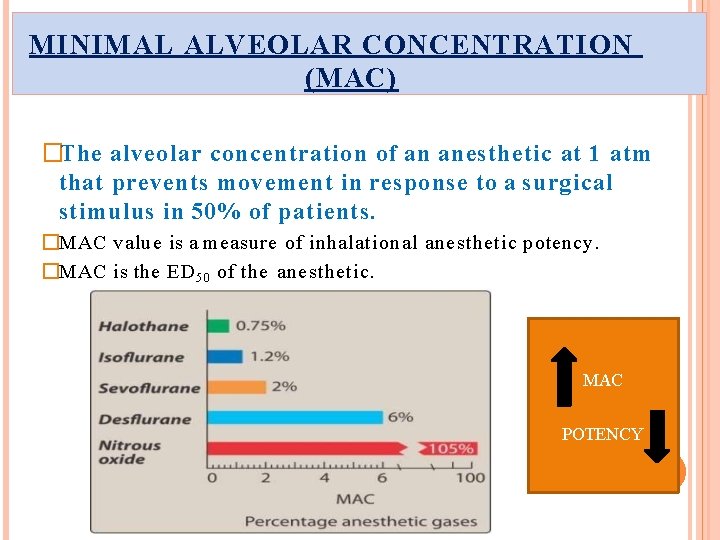
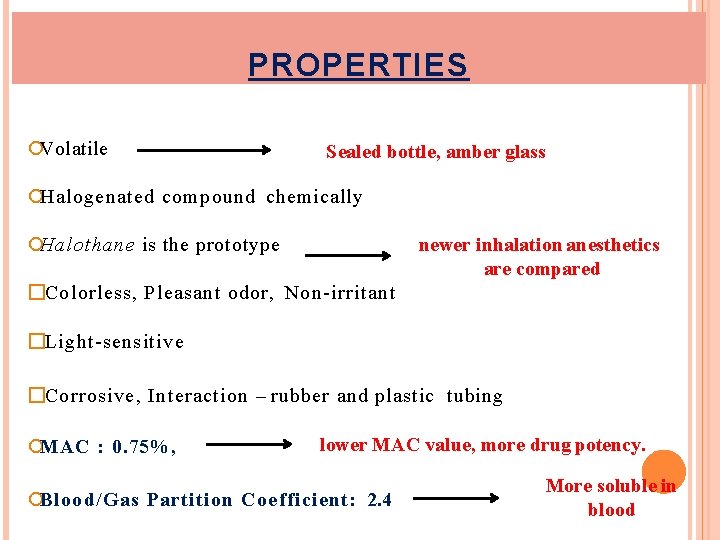
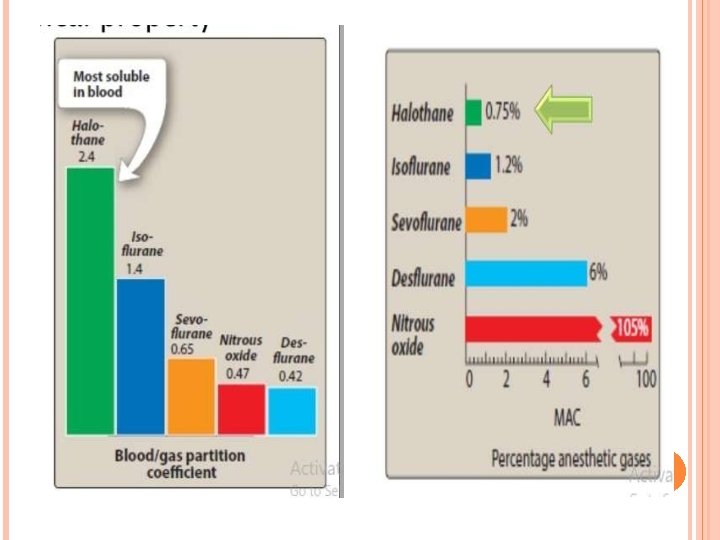
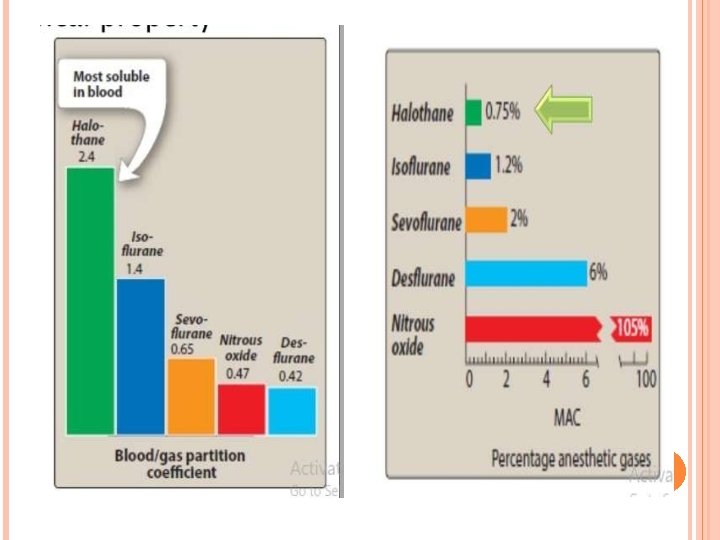
MINIMAL ALVEOLAR CONCENTRATION (MAC) �The alveolar concentration of an anesthetic at 1 atm that prevents movement in response to a surgical stimulus in 50% of patients. �MAC value is a measure of inhalational anesthetic potency. �MAC is the ED 5 0 of the anesthetic. MAC POTENCY
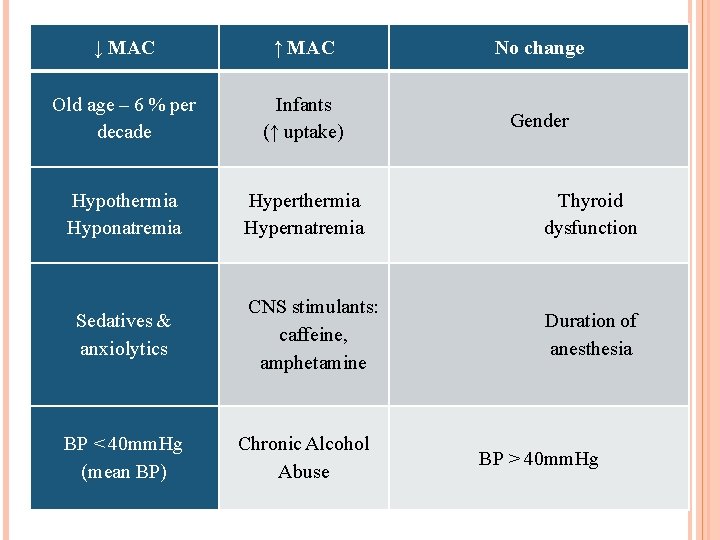
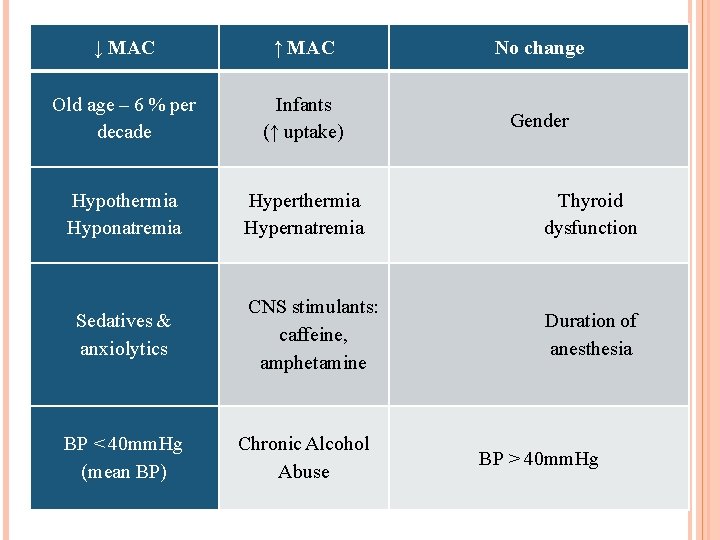
↓ MAC ↑ MAC No change Old age – 6 % per decade Infants (↑ uptake) Gender Hypothermia Hyponatremia Hyperthermia Hypernatremia Thyroid dysfunction CNS stimulants: caffeine, amphetamine Duration of anesthesia Sedatives & anxiolytics BP < 40 mm. Hg (mean BP) Chronic Alcohol Abuse BP > 40 mm. Hg
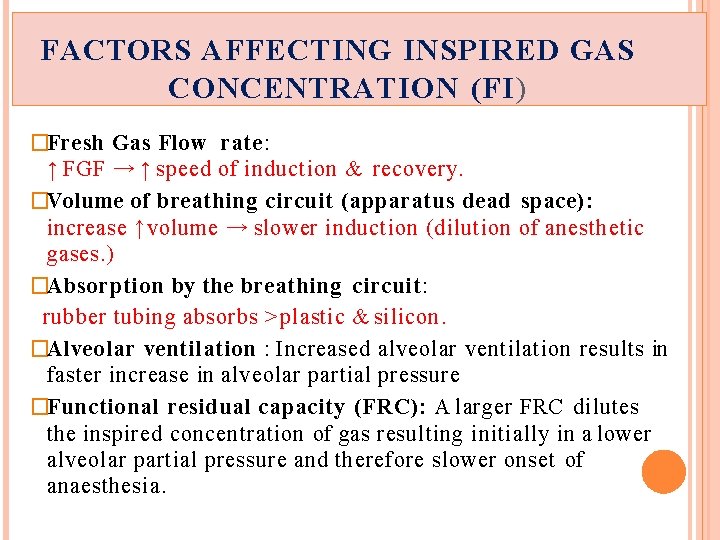
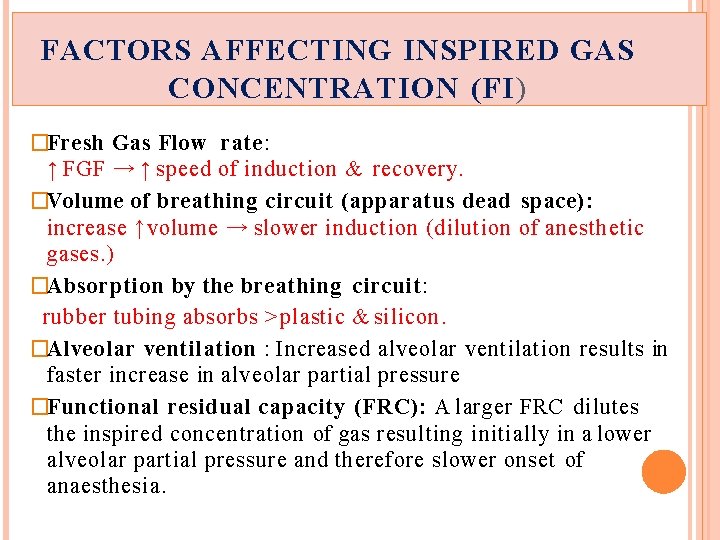
FACTORS AFFECTING INSPIRED GAS CONCENTRATION (FI ) �Fresh Gas Flow rate: ↑ FGF → ↑ speed of induction & recovery. �Volume of breathing circuit (apparatus dead space): increase ↑volume → slower induction (dilution of anesthetic gases. ) �Absorption by the breathing circuit: rubber tubing absorbs ˃ plastic & silicon. �Alveolar ventilation : Increased alveolar ventilation results in faster increase in alveolar partial pressure �Functional residual capacity (FRC): A larger FRC dilutes the inspired concentration of gas resulting initially in a lower alveolar partial pressure and therefore slower onset of anaesthesia.
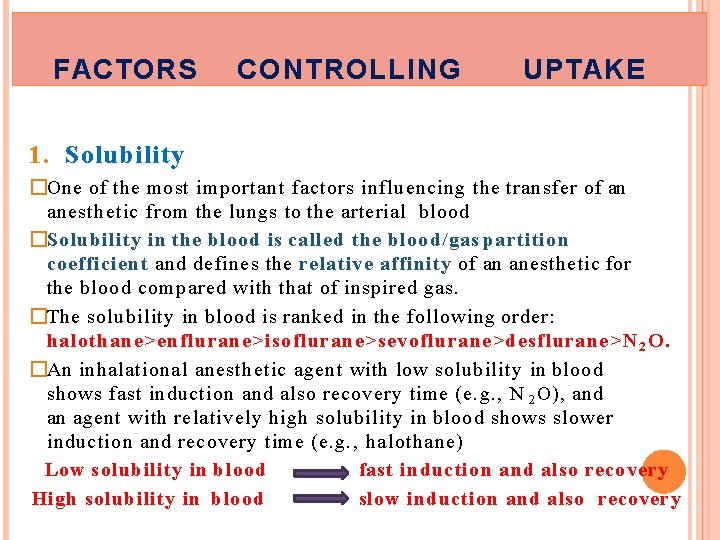
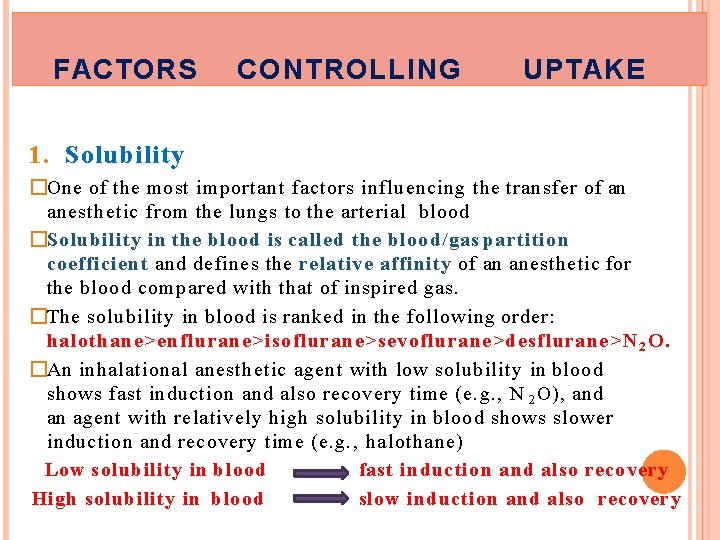
FACTORS CONTROLLING UPTAKE 1. Solubility �One of the most important factors influencing the transfer of an anesthetic from the lungs to the arterial blood �Solubility in the blood is called the blood/gas partition coefficient and defines the relative affinity of an anesthetic for the blood compared with that of inspired gas. �The solubility in blood is ranked in the following order: halothane>enflurane>isoflurane>sevoflurane>desflurane>N 2 O. �An inhalational anesthetic agent with low solubility in blood shows fast induction and also recovery time (e. g. , N 2 O), and an agent with relatively high solubility in blood shows slower induction and recovery time (e. g. , halothane) Low solubility in blood fast induction and also recovery High solubility in blood slow induction and also recovery
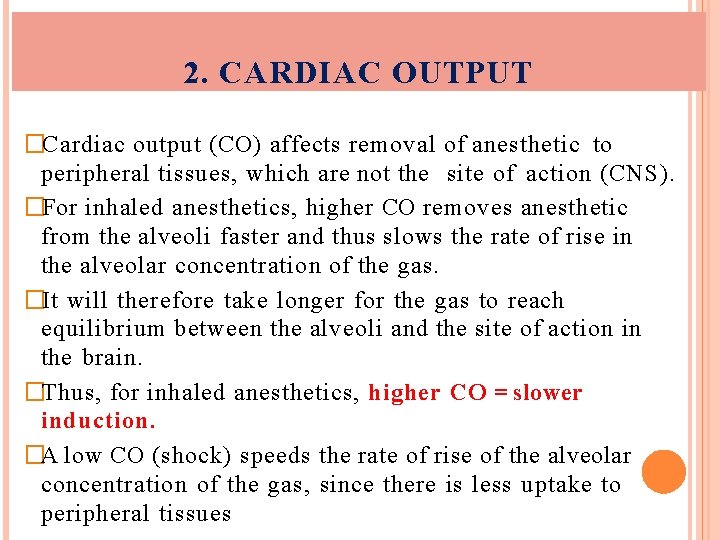
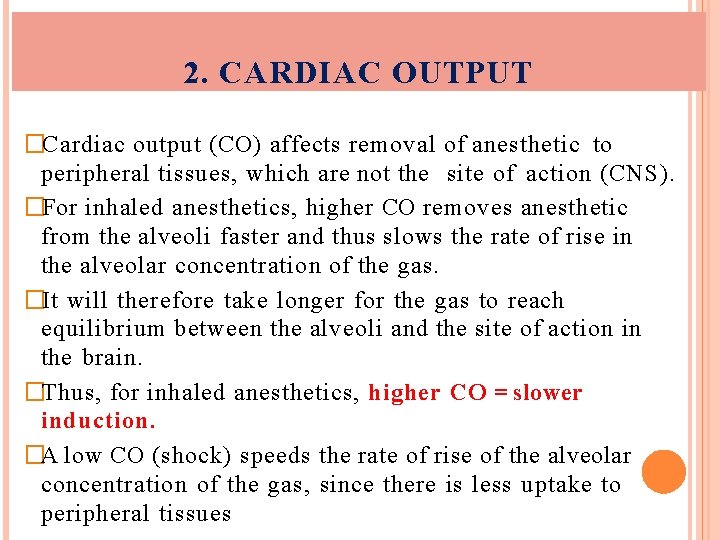
2. CARDIAC OUTPUT �Cardiac output (CO) affects removal of anesthetic to peripheral tissues, which are not the site of action (CNS). �For inhaled anesthetics, higher CO removes anesthetic from the alveoli faster and thus slows the rate of rise in the alveolar concentration of the gas. �It will therefore take longer for the gas to reach equilibrium between the alveoli and the site of action in the brain. �Thus, for inhaled anesthetics, higher CO = slower induction. �A low CO (shock) speeds the rate of rise of the alveolar concentration of the gas, since there is less uptake to peripheral tissues
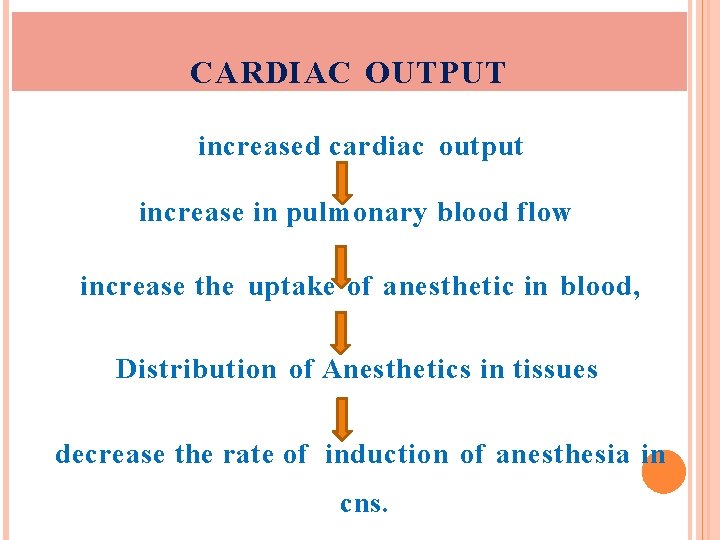
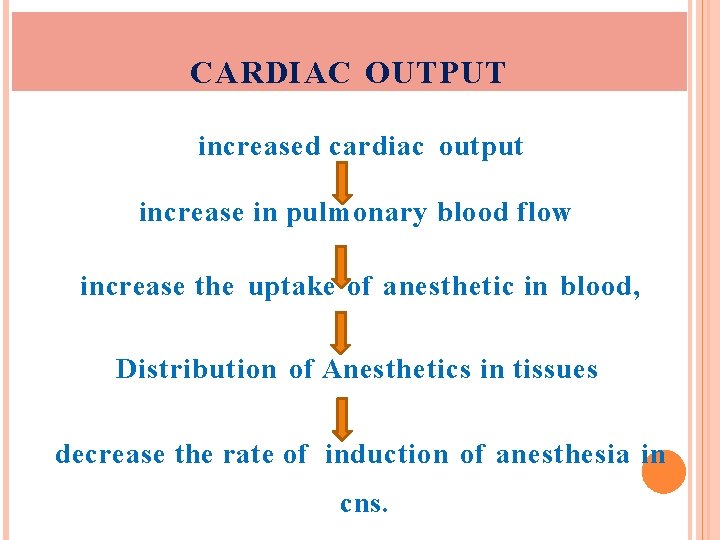
CARDIAC OUTPUT increased cardiac output increase in pulmonary blood flow increase the uptake of anesthetic in blood, Distribution of Anesthetics in tissues decrease the rate of induction of anesthesia in cns.
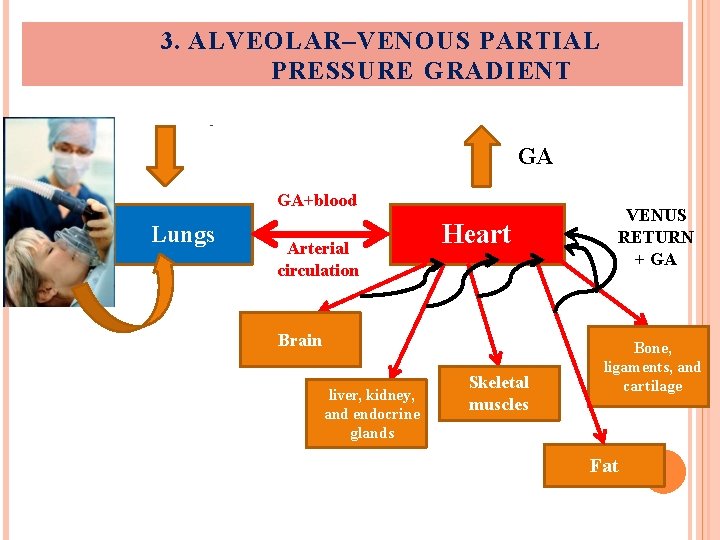
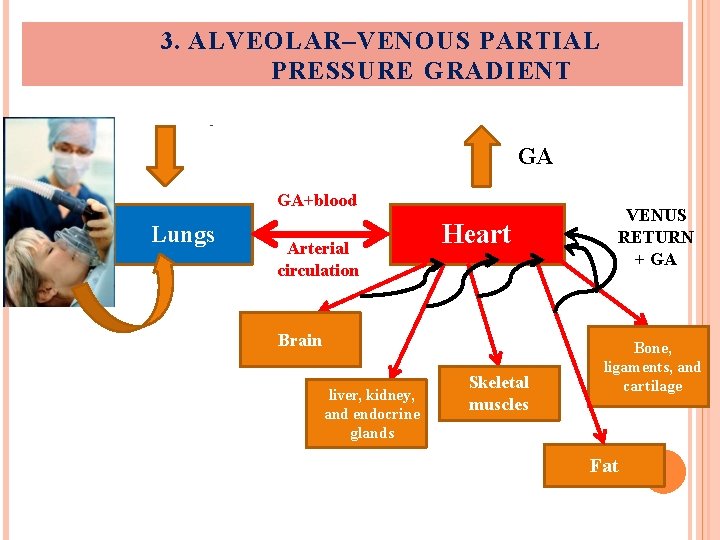
3. ALVEOLAR–VENOUS PARTIAL PRESSURE GRADIENT GA GA+blood Lungs Arterial circulation Heart Brain liver, kidney, and endocrine glands Skeletal muscles VENUS RETURN + GA Bone, ligaments, and cartilage Fat
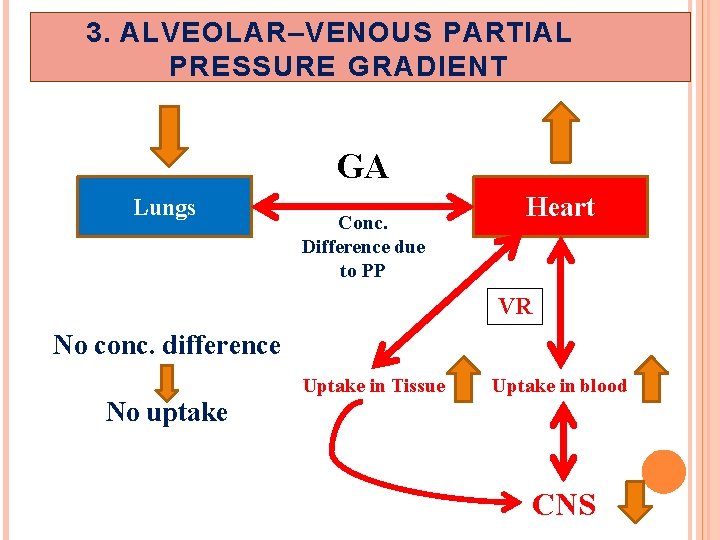
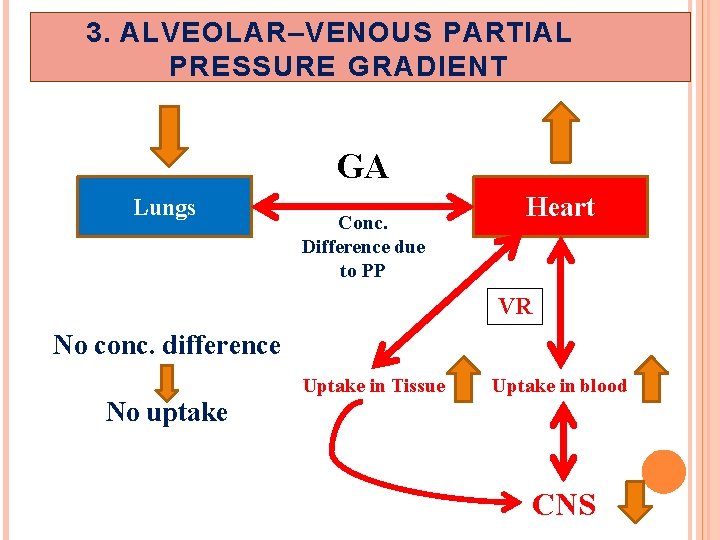
3. ALVEOLAR–VENOUS PARTIAL PRESSURE GRADIENT GA Lungs Conc. Difference due to PP Heart VR No conc. difference No uptake Uptake in Tissue Uptake in blood CNS
3. ALVEOLAR–VENOUS PARTIAL PRESSURE GRADIENT �The arterial circulation distributes the anesthetic to various tissues, and the pressure gradient drives free anesthetic gas into tissues. �As the venous circulation returns blood depleted of anesthetic to the lung, more gas moves into the blood from the lung according to the partial pressure difference. �The greater is the difference in anesthetic concentration between alveolar (arterial) to venous blood, the higher the uptake and the slower the induction. �Over time, the partial pressure in the venous blood closely approximates the partial pressure in the inspired mixture. �That is, no further net anesthetic uptake from the lung occurs.
EFFECT OF DIFFERENT TISSUE TYPES ON ANESTHETIC UPTAKE During maintenance of anesthesia with inhaled anesthetics, the drug continues to be transferred between various tissues at rates dependent on the solubility of the agent, the concentration gradient between the blood and the tissue, and the tissue blood flow. �Faster flow results in a more rapidly achieved steady state �It is also directly proportional to the capacity of that tissue to store anesthetic (that is, a larger capacity results in a longer time required to achieve steady state) �Capacity, in turn, is directly proportional to the tissue’s volume and the tissue/blood solubility coefficient of the anesthetic molecules.
The higher the blood flow to a region, the faster the delivery of anaesthetic and the more rapid will be equilibration Four major tissue compartments determine the time course of anesthetic uptake: a. Brain, heart, liver, kidney, and endocrine glands: These highly perfused tissues rapidly attain a steady state with the partial pressure of anesthetic in the blood. b. Skeletal muscles: These are poorly perfused during anesthesia prolongs the time required to achieve steady state.
c. Fat: This tissue is also poorly perfused. However, potent volatile general anesthetics are very lipid soluble. Therefore, fat has a large capacity to store anesthetic. This combination of slow delivery to a high-capacity compartment prolongs the time required to achieve steady state in that tissue. d. Bone, ligaments, and cartilage: These are poorly perfused and have a relatively low capacity to store anesthetic. Therefore, these tissues have only a slight impact on the time course of anesthetic distribution in the body.
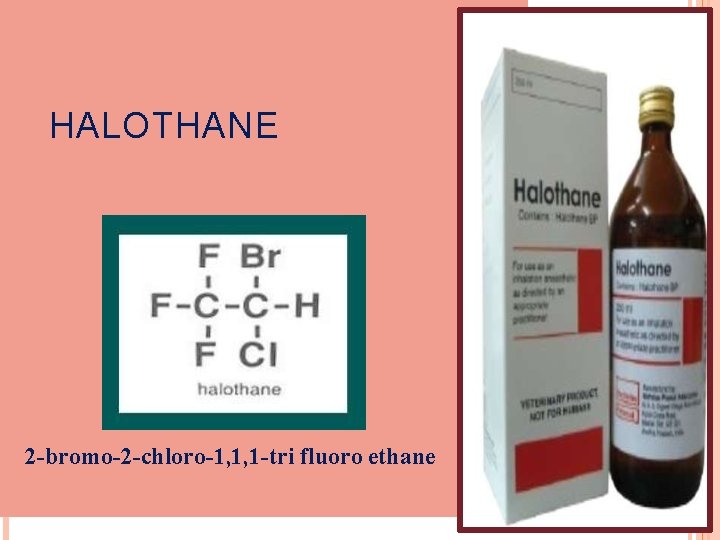
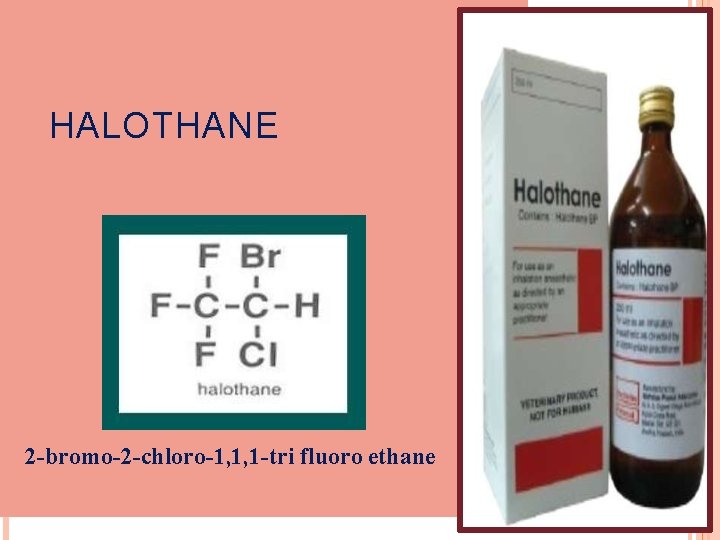
HALOTHANE 2 -bromo-2 -chloro-1, 1, 1 -tri fluoro ethane
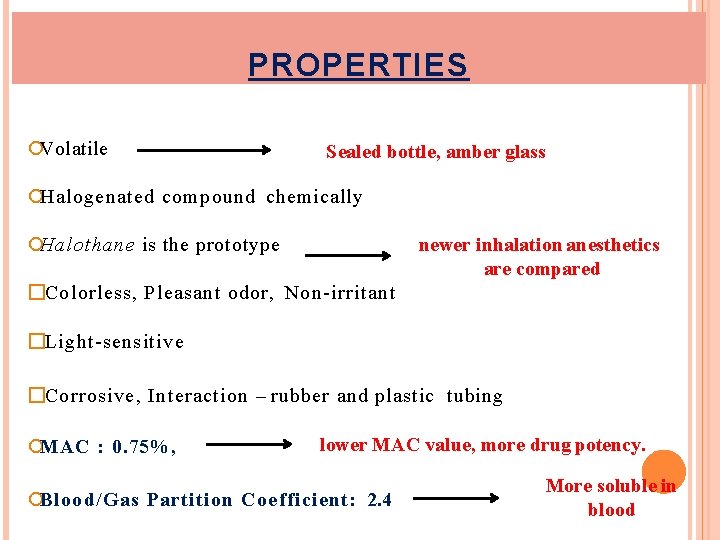
PROPERTIES Volatile Sealed bottle, amber glass Halogenated compound chemically Halothane is the prototype newer inhalation anesthetics are compared �Colorless, Pleasant odor, Non-irritant �Light-sensitive �Corrosive, Interaction – rubber and plastic tubing MAC : 0. 75%, lower MAC value, more drug potency. Blood/Gas Partition Coefficient: 2. 4 More soluble in blood
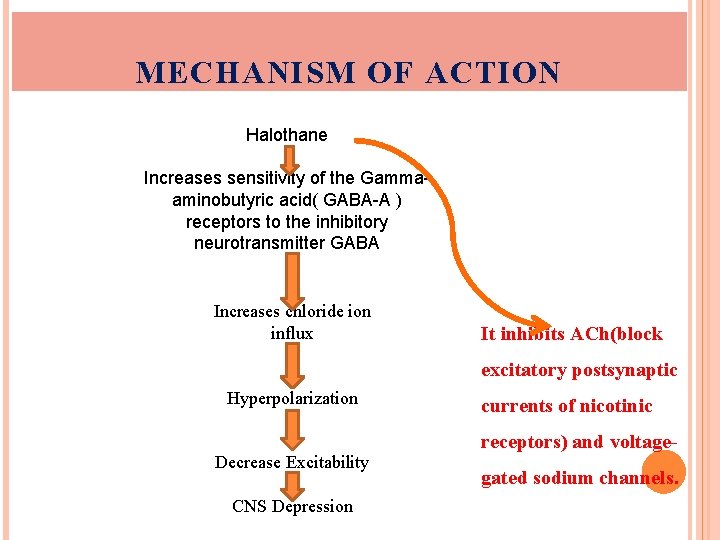
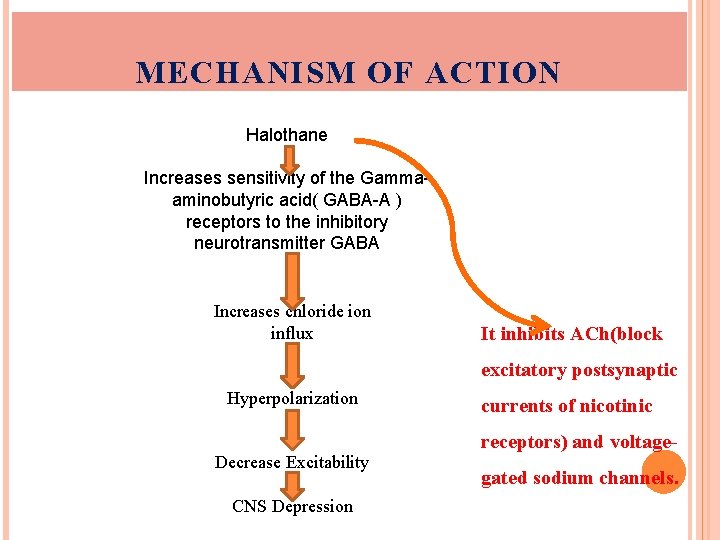
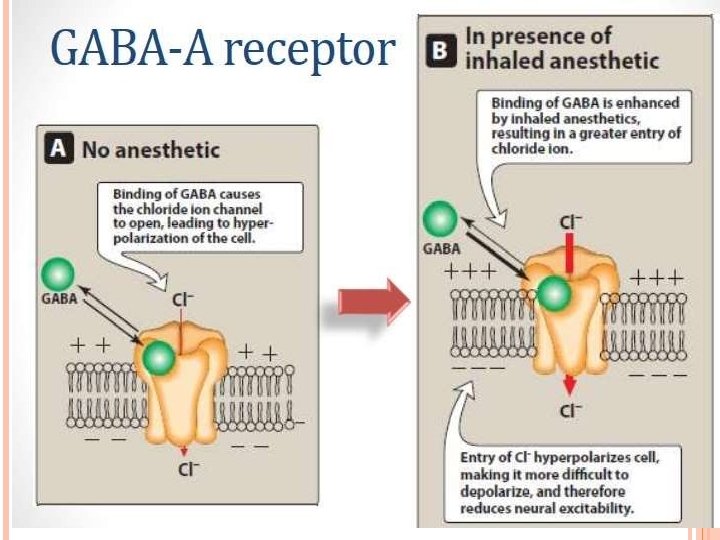
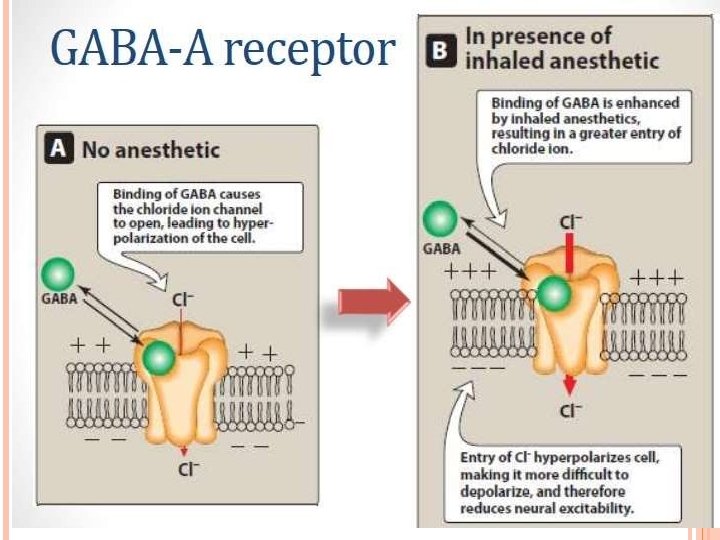
MECHANISM OF ACTION Halothane Increases sensitivity of the Gammaaminobutyric acid( GABA-A ) receptors to the inhibitory neurotransmitter GABA Increases chloride ion influx It inhibits ACh(block Hyperpolarization excitatory postsynaptic Decrease. Excitability receptors) and voltage- Hyperpolarization Decrease Excitability CNSDepression currents of nicotinic gated sodium channels.
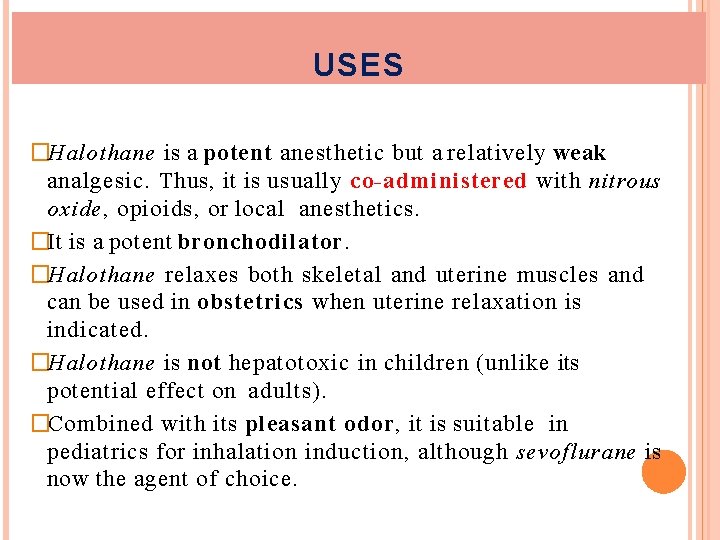
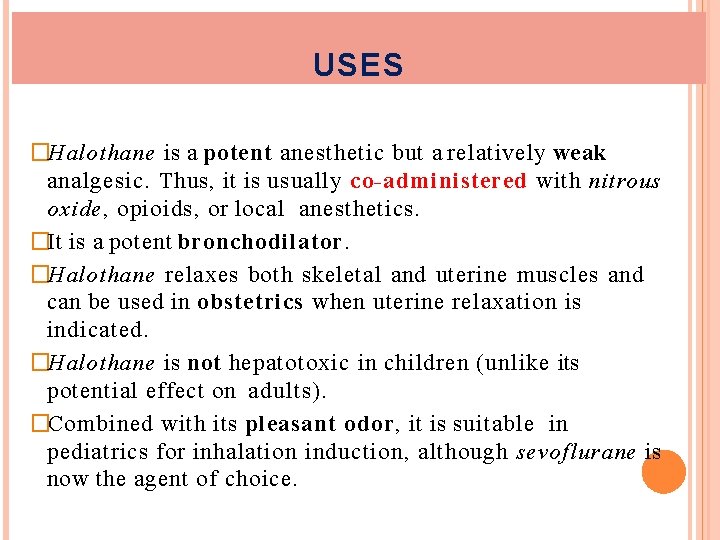
USES �Halothane is a potent anesthetic but a relatively weak analgesic. Thus, it is usually co-administered with nitrous oxide, opioids, or local anesthetics. �It is a potent bronchodilator. �Halothane relaxes both skeletal and uterine muscles and can be used in obstetrics when uterine relaxation is indicated. �Halothane is not hepatotoxic in children (unlike its potential effect on adults). �Combined with its pleasant odor, it is suitable in pediatrics for inhalation induction, although sevoflurane is now the agent of choice.
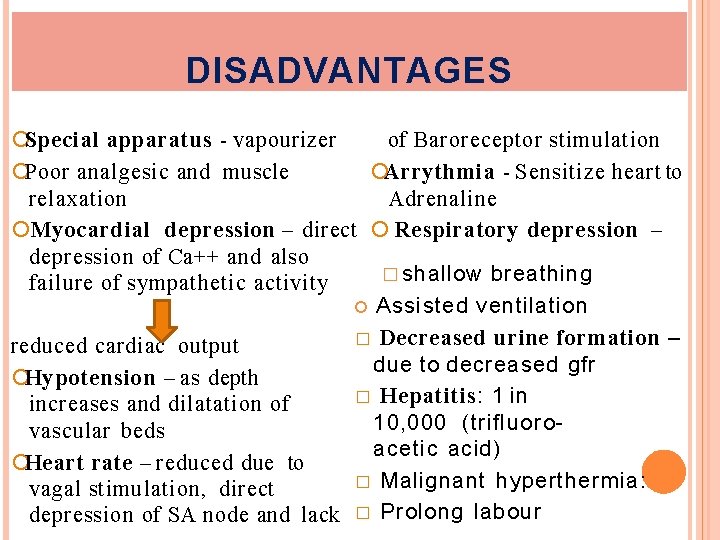
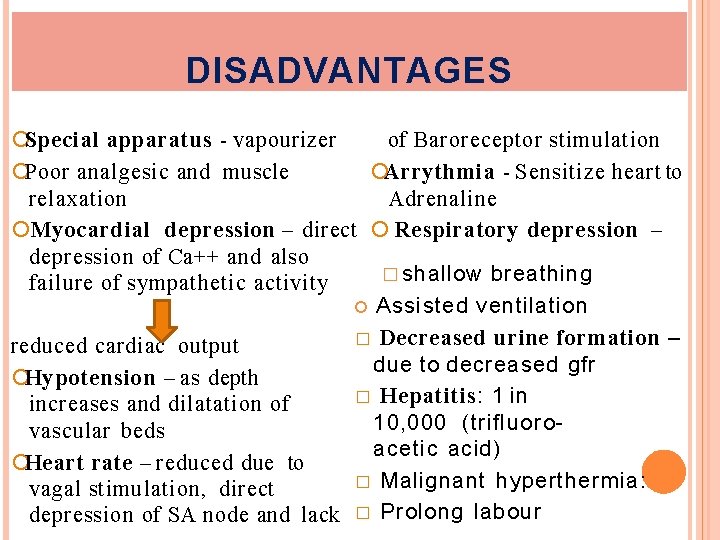
DISADVANTAGES Special apparatus - vapourizer of Baroreceptor stimulation Arrythmia - Sensitize heart to Poor analgesic and muscle Adrenaline relaxation Myocardial depression – direct Respiratory depression – depression of Ca++ and also � shallow breathing failure of sympathetic activity Assisted ventilation � Decreased urine formation – reduced cardiac output due to decreased gfr Hypotension – as depth � Hepatitis: 1 in increases and dilatation of 10, 000 (trifluorovascular beds acetic acid) Heart rate – reduced due to � Malignant hyperthermia: vagal stimulation, direct depression of SA node and lack � Prolong labour
 Mac anesthesia minimum alveolar concentration
Mac anesthesia minimum alveolar concentration Nitric oxide properties
Nitric oxide properties Components of anaesthesia
Components of anaesthesia Insidan region jh
Insidan region jh Mac isoflurane
Mac isoflurane Classification of inhalational agents
Classification of inhalational agents Classification of inhalational agents
Classification of inhalational agents General anesthesia drugs chart
General anesthesia drugs chart Local anesthesia classification
Local anesthesia classification Site:slidetodoc.com
Site:slidetodoc.com Baricity definition
Baricity definition Site:slidetodoc.com
Site:slidetodoc.com What is regional anesthesia
What is regional anesthesia Inhalation route
Inhalation route Order of inhalation
Order of inhalation Definition of oxygen inhalation
Definition of oxygen inhalation Cement hazards
Cement hazards Widowmaker heart attack smoke inhalation
Widowmaker heart attack smoke inhalation O2 inhalation sos
O2 inhalation sos Linctuses are
Linctuses are Chambre d'inhalation cipla
Chambre d'inhalation cipla One empire one god one emperor
One empire one god one emperor One one one little dog run
One one one little dog run One king one law one faith
One king one law one faith Byzantine definition
Byzantine definition