JUVENILE MYASTHENIA GRAVIS DR JANE NYAWIRA DR JANE


- Slides: 19
JUVENILE MYASTHENIA GRAVIS DR JANE NYAWIRA, DR JANE HASSELL GERTRUDE’S CHILDREN’S HOSPITAL
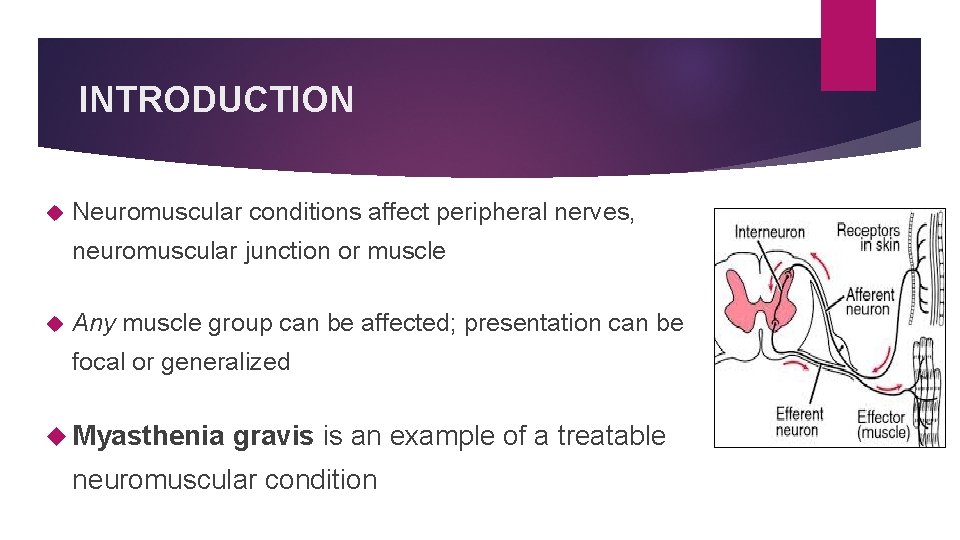
INTRODUCTION Neuromuscular conditions affect peripheral nerves, neuromuscular junction or muscle Any muscle group can be affected; presentation can be focal or generalized Myasthenia gravis is an example of a treatable neuromuscular condition
CASE: 8 -year old girl Presented with acute cough and difficulty in breathing Initially admitted & treated as severe pneumonia, required intubation & mechanical ventilation Subsequent failed exubations x 2 with CO 2 retention – no lung pathology identified Noted to have weak gag, weak cough, inability to swallow
CASE: Examination Alert, following commands Absent cough/gag, bilateral facial weakness and ptosis, diurnal variation noted – better after sleep Mild fluctuating proximal limb weakness, normal tone and reflexes, no additional movements
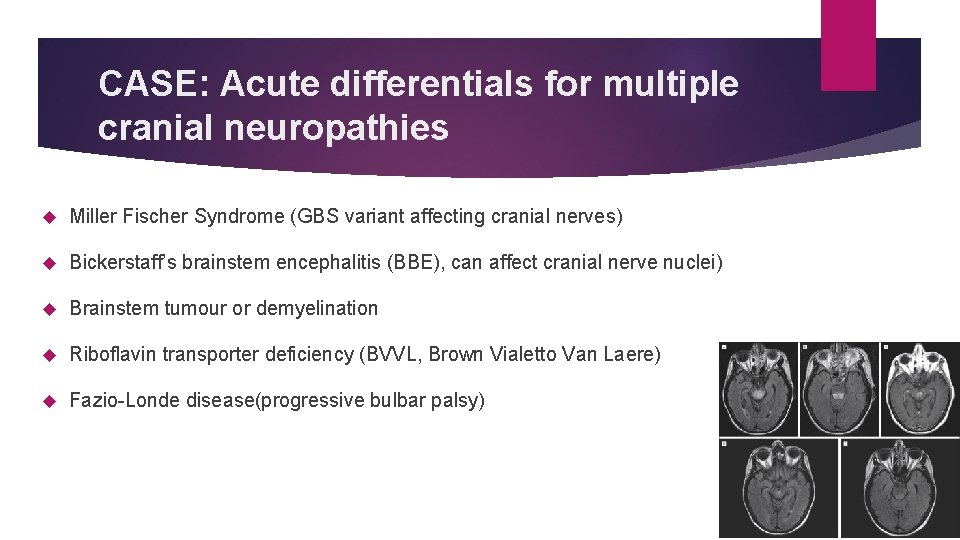
CASE: Acute differentials for multiple cranial neuropathies Miller Fischer Syndrome (GBS variant affecting cranial nerves) Bickerstaff’s brainstem encephalitis (BBE), can affect cranial nerve nuclei) Brainstem tumour or demyelination Riboflavin transporter deficiency (BVVL, Brown Vialetto Van Laere) Fazio-Londe disease(progressive bulbar palsy)
CASE: Assessment MRI brain normal – ruled out Bickerstaff’s encephalitis CSF studies normal – protein not raised so Miller Fischer less likely TFTs, CK, LFTs and lactate normal
CASE: Further history on direct questioning 6 month history of poor cough, difficulty swallowing, slow feeding. Intermittent drooping eyelids, tilting head back to watch TV. Easy fatigability, wobbly walking towards the end of the day. Fall while walking , unable to get up but alert. Treated for “acute wheeze” 2 months prior.
CASE: Progress Clinical diagnosis of Myasthenia Gravis based on history of fluctuating fatigable weakness. Symptom freedom achieved with pyridostigmine (empiric) Physiotherapy & occupational therapy Anticholinesterase antibodies positive CT chest: No thymic enlargement Discharged under Neurologist follow up, returned to school
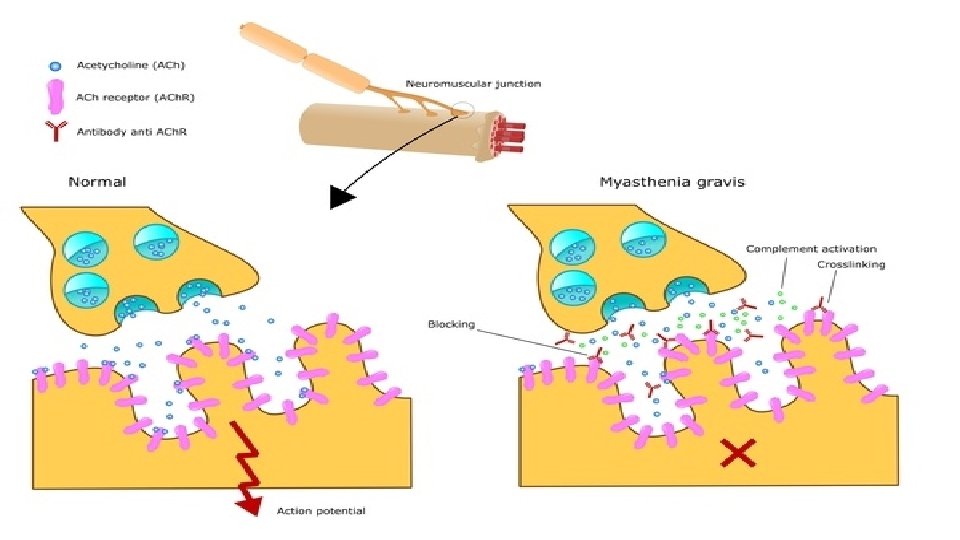
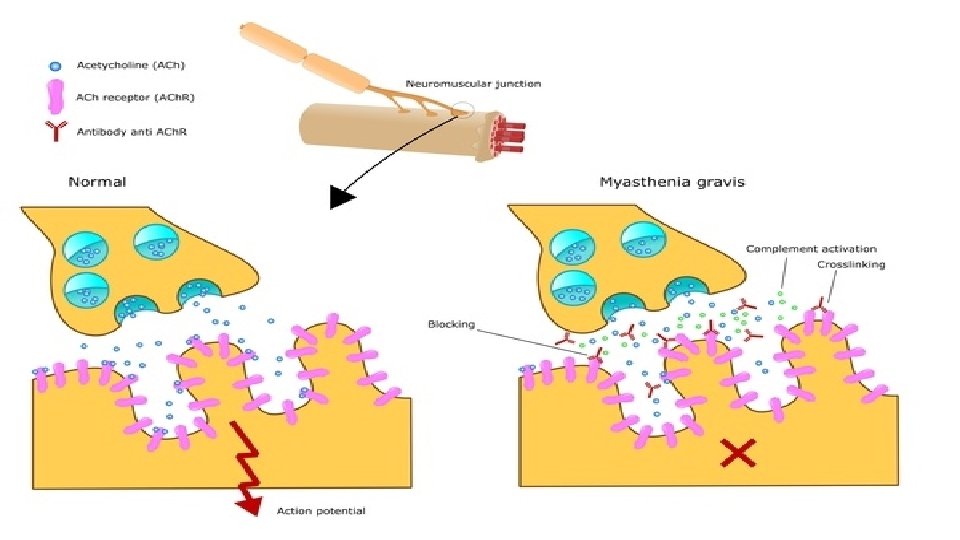
MYASTHENIA GRAVIS (MG) Autoimmune disease. 5 -20 per 100, 000, uncommon in children. Antibodies against postsynaptic membrane of the NMJ interfere with nerve impulse transmission leading to varying muscle weakness & fatigability. Antibodies against nicotinic acetylcholine receptors (ACh. R), specific receptor tyrosine kinase (Mu. SK), or others. muscle-
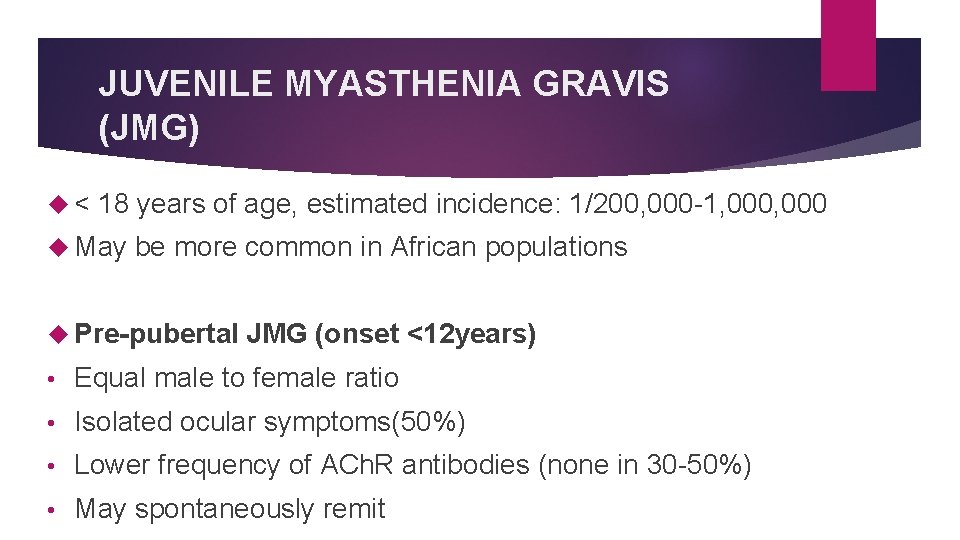
JUVENILE MYASTHENIA GRAVIS (JMG) < 18 years of age, estimated incidence: 1/200, 000 -1, 000 May be more common in African populations Pre-pubertal JMG (onset <12 years) • Equal male to female ratio • Isolated ocular symptoms(50%) • Lower frequency of ACh. R antibodies (none in 30 -50%) • May spontaneously remit
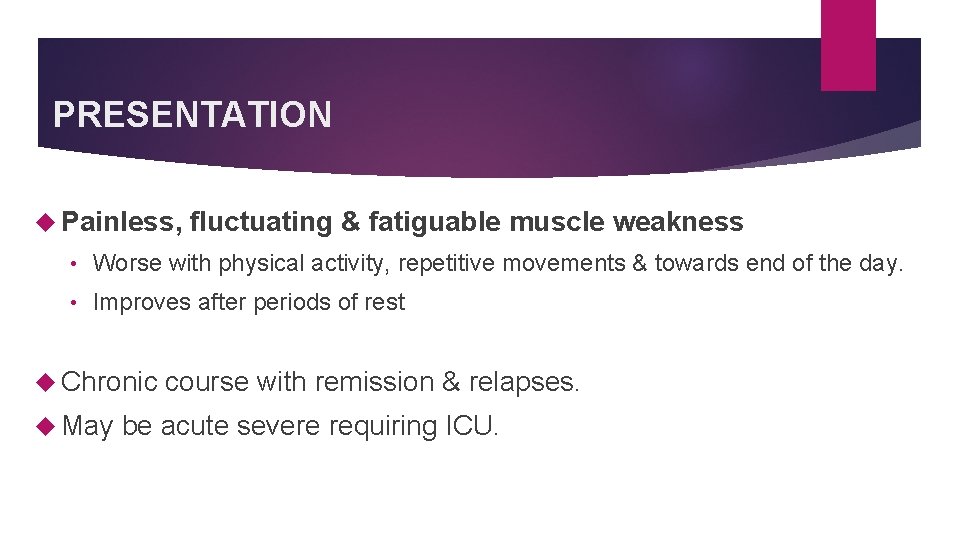
PRESENTATION Painless, fluctuating & fatiguable muscle weakness • Worse with physical activity, repetitive movements & towards end of the day. • Improves after periods of rest Chronic course with remission & relapses. May be acute severe requiring ICU.
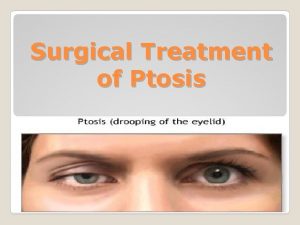
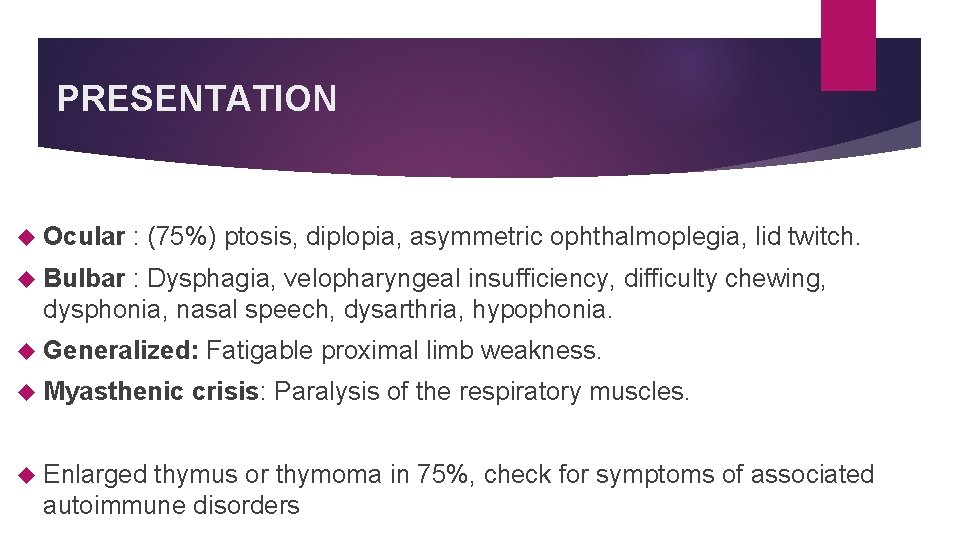
PRESENTATION Ocular : (75%) ptosis, diplopia, asymmetric ophthalmoplegia, lid twitch. Bulbar : Dysphagia, velopharyngeal insufficiency, difficulty chewing, dysphonia, nasal speech, dysarthria, hypophonia. Generalized: Myasthenic Fatigable proximal limb weakness. crisis: Paralysis of the respiratory muscles. Enlarged thymus or thymoma in 75%, check for symptoms of associated autoimmune disorders

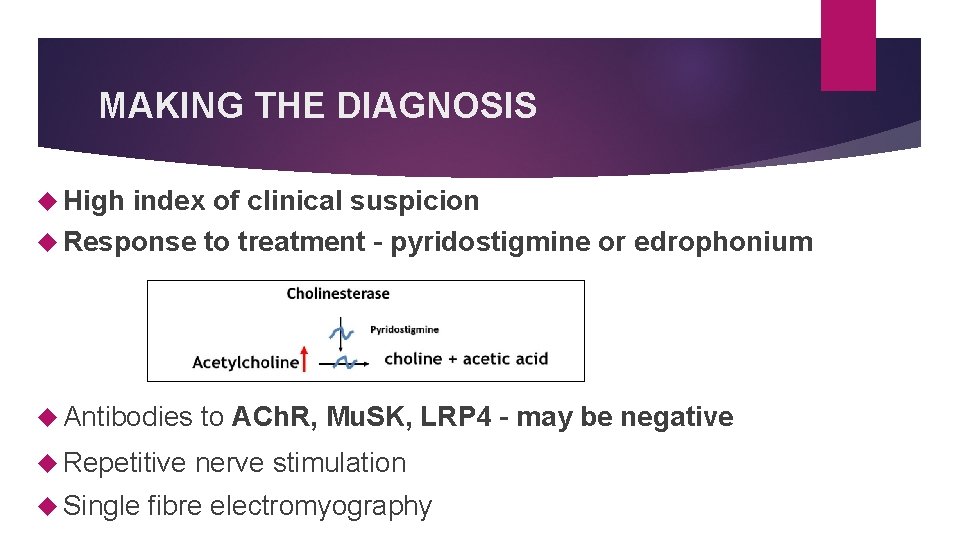
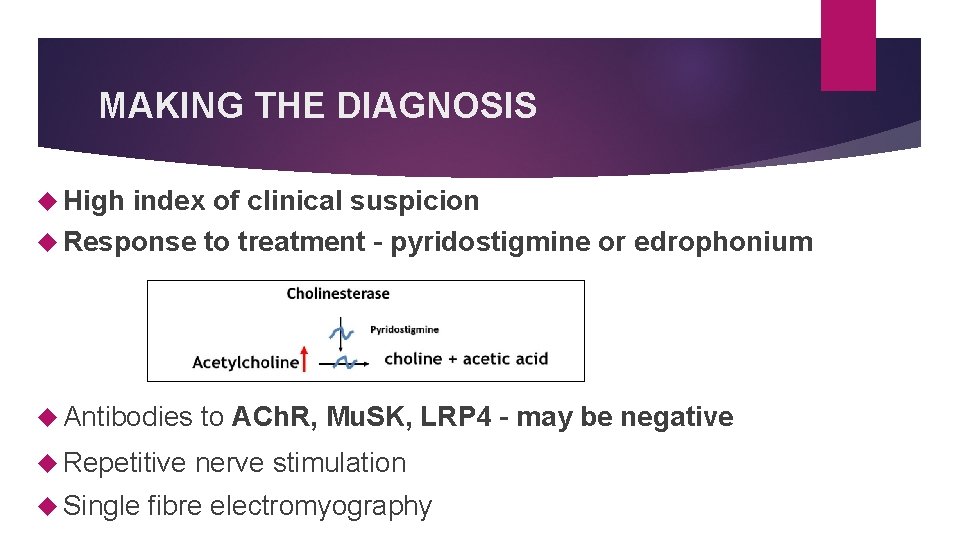
MAKING THE DIAGNOSIS High index of clinical suspicion Response to treatment – pyridostigmine or edrophonium Antibodies to ACh. R, Mu. SK, LRP 4 – may be negative Repetitive nerve stimulation Single fibre electromyography
TREATMENT 1 st line: Acetylcholinesterase inhibitors e. g. Pyridostigmine 2 nd line: If breakthrough symptoms on max dose pyridostigmine, add immune suppression Steroids for acute exacerbations Steroid sparing long-term e. g. azathioprine, mycophenolate mofetil IVIg or plasmapheresis if drug-resistant Acutely may need ventilation Thymectomy cures some

CONCLUSION: JMG is a rare, treatable neuromuscular condition that frequently presents with isolated ocular or bulbar symptoms Important aspects specific to the pediatrics: • Distinct clinical features of prepubertal presentations • Different rates of ACh. R seropositivity • Response to therapy, remission rates Serology may be negative, start empiric pyridostigmine and seek help
References Finnis, Maria F, and Sandeep Jayawant. “Juvenile myasthenia gravis: a paediatric perspective. ” Autoimmune diseases vol. 2011 (2011): 404101. doi: 10. 4061/2011/404101 Clinical Characteristics of Pediatric Myasthenia: A Surveillance Study. Juliana Vander. Pluym, Jiri Vajsar, Francois Dominique Jacob, Jean K. Mah, Danielle Grenier, Hanna Kolski. Pediatrics Oct 2013, 132 (4) e 939 -e 944; DOI: 10. 1542/peds. 2013 -0814
THANK YOU
 Myasthenia gravis
Myasthenia gravis Myasthenia gravis thymectomy
Myasthenia gravis thymectomy Myasthenia gravis definition
Myasthenia gravis definition Myasthenia gravis oireet
Myasthenia gravis oireet Gravis grave
Gravis grave High frequency antibodies
High frequency antibodies Myasthenia gravis eyes
Myasthenia gravis eyes Concept map of assessment
Concept map of assessment Imunopatologické reakcie
Imunopatologické reakcie Tes wartenberg positif
Tes wartenberg positif Myasthenia gravis.
Myasthenia gravis. Myasthenia gravis exercise
Myasthenia gravis exercise Anmies
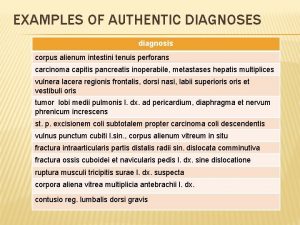
Anmies Fractura ossium nasalium
Fractura ossium nasalium Miasthenia gravis
Miasthenia gravis Gravis carter
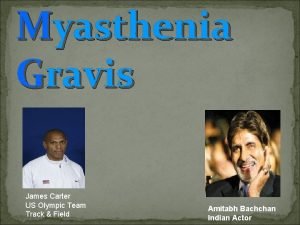
Gravis carter Mythenia gravis
Mythenia gravis Quam comparative latin
Quam comparative latin Haec precor hanc vocem extremam
Haec precor hanc vocem extremam Myathesia gravis
Myathesia gravis