Multiple Sclerosis Physicians Overview Defining Multiple Sclerosis An











- Slides: 47
Multiple Sclerosis: Physician’s Overview
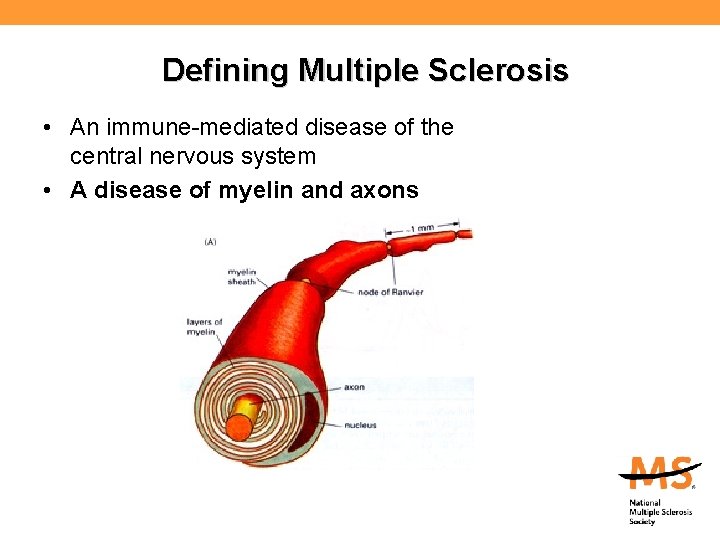
Defining Multiple Sclerosis • An immune-mediated disease of the central nervous system – Immune cells are made throughout the body except in the brain and spinal cord • • • Tonsils Thymus Bone Marrow Spleen Lymphoid tissue of the gut
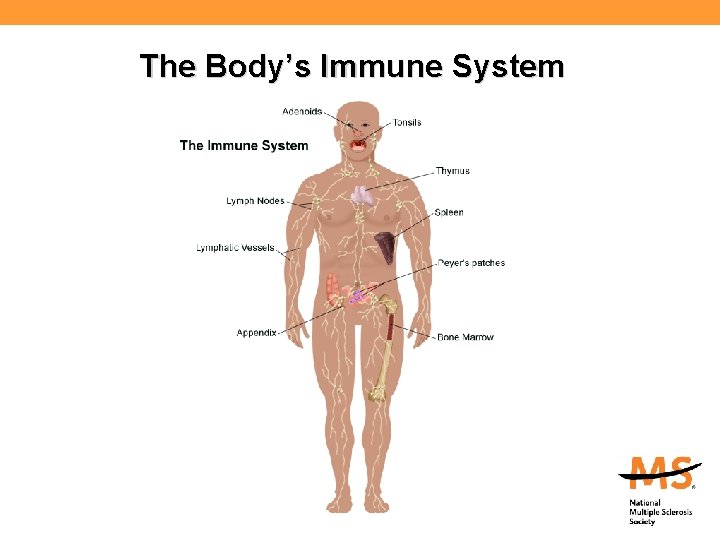
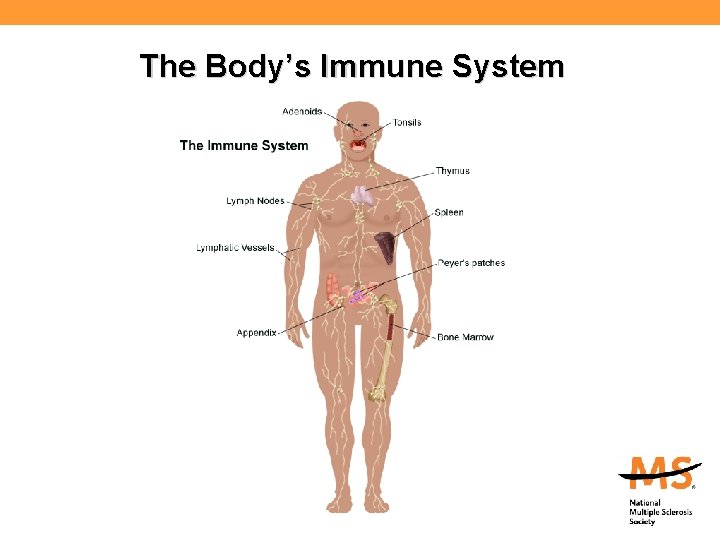
The Body’s Immune System
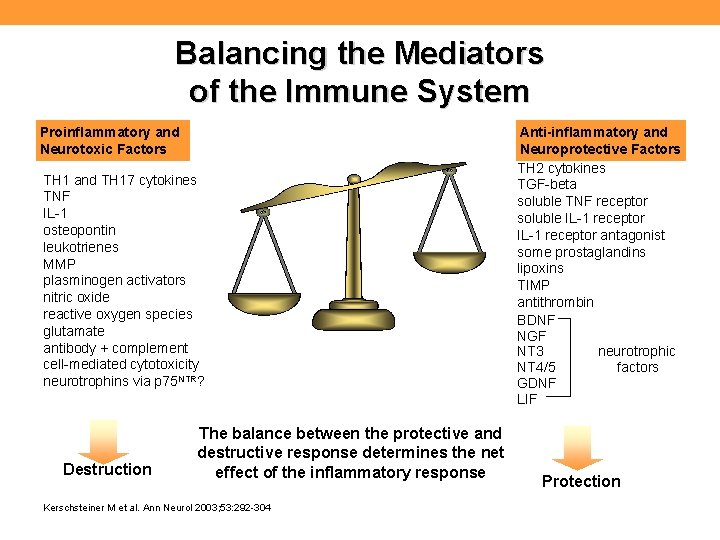
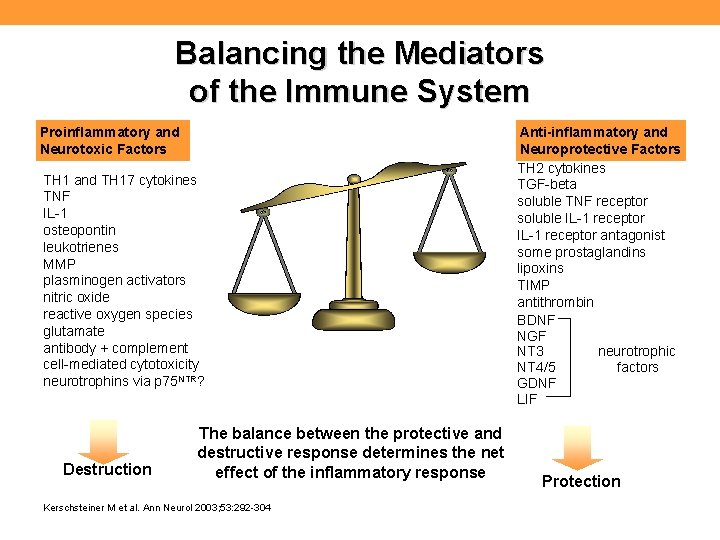
Balancing the Mediators of the Immune System Proinflammatory and Neurotoxic Factors TH 1 and TH 17 cytokines TNF IL-1 osteopontin leukotrienes MMP plasminogen activators nitric oxide reactive oxygen species glutamate antibody + complement cell-mediated cytotoxicity neurotrophins via p 75 NTR? Destruction The balance between the protective and destructive response determines the net effect of the inflammatory response Kerschsteiner M et al. Ann Neurol 2003; 53: 292 -304 Anti-inflammatory and Neuroprotective Factors TH 2 cytokines TGF-beta soluble TNF receptor soluble IL-1 receptor antagonist some prostaglandins lipoxins TIMP antithrombin BDNF NGF NT 3 neurotrophic NT 4/5 factors GDNF LIF Protection
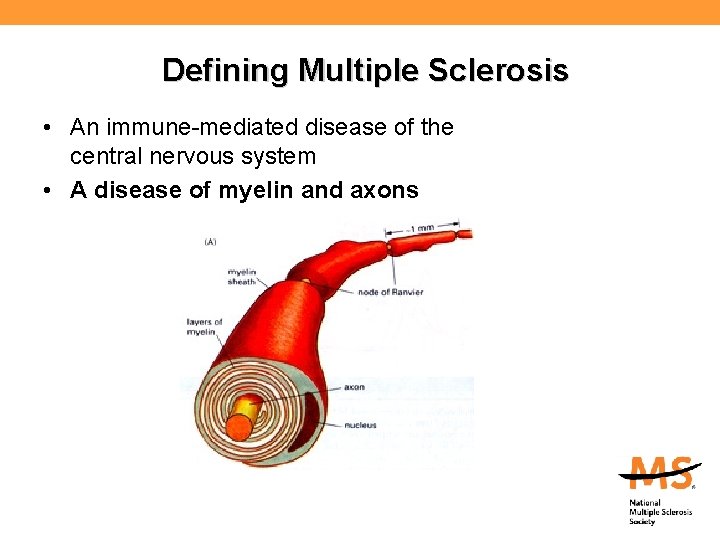
Defining Multiple Sclerosis • An immune-mediated disease of the central nervous system • A disease of myelin and axons

Active Inflammatory Demyelination and Axonal Transection • It has been shown that active inflammation results in both demyelination and axonal transection Arrowheads = areas of active demyelination; Arrow = terminal axon ovoid; Human brain; Red = immunostained for myelin basic protein; Green = immunostained for nonphosphorylated neurofilament; Bar = 45 m. Trapp BD et al. N Engl J Med. 1998; 338: 278 -285. Peterson JW et al. Neurol Clin. 2005; 23: 107 -129.
Multiple Sclerosis • An immune-mediated disease of the central nervous system • A disease of myelin and axons • A disease of people
Who gets MS? • Usually diagnosed between 20 and 50 – Occasionally diagnosed in young children and older adults • More common in women than men (>2 -3: 1) • Most common in those of Northern European ancestry – More common in Caucasians than Hispanics or African Americans; rare among Asians • More common in temperate areas of the world – Environmental factor(s)? – Genetic factor? – Lower vitamin D exposure? – Combination?
The genetic factor in MS • The risk of getting MS is approximately: – 1/750 for the general population (0. 1%) – 1/40 for those with first-degree relative with MS (3%) – 1/4 for an identical twin (25%) • 20% of people with MS have a blood relative with MS The risk is higher in any family in which there are several family members with the disease (multiplex families)
Diagnosing MS • MS is a clinical diagnosis – Signs and symptoms – Medical history • Paraclinical tests provide support – Magnetic resonance imaging – Spinal fluid – Evoked potentials • Diagnostic criteria: – Dissemination in time and space: evidence that damage has occurred in at least two separate areas of the CNS at different points in time – There must be no other explanation


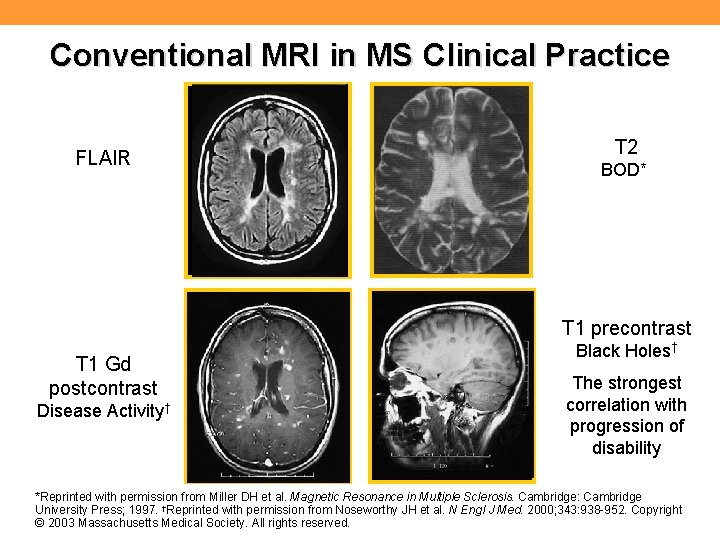
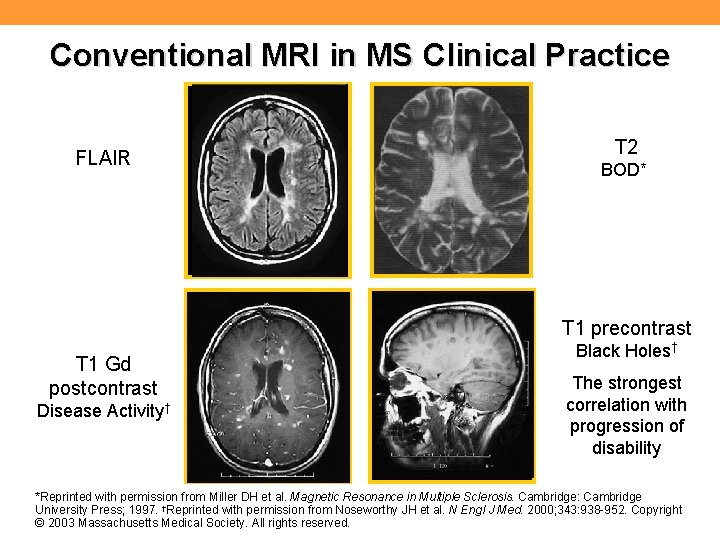
Conventional MRI in MS Clinical Practice FLAIR T 2 BOD* T 1 precontrast T 1 Gd postcontrast Disease Activity† Black Holes† The strongest correlation with progression of disability *Reprinted with permission from Miller DH et al. Magnetic Resonance in Multiple Sclerosis. Cambridge: Cambridge University Press; 1997. †Reprinted with permission from Noseworthy JH et al. N Engl J Med. 2000; 343: 938 -952. Copyright © 2003 Massachusetts Medical Society. All rights reserved.

Evoked Potential Testing

Lumbar Puncture

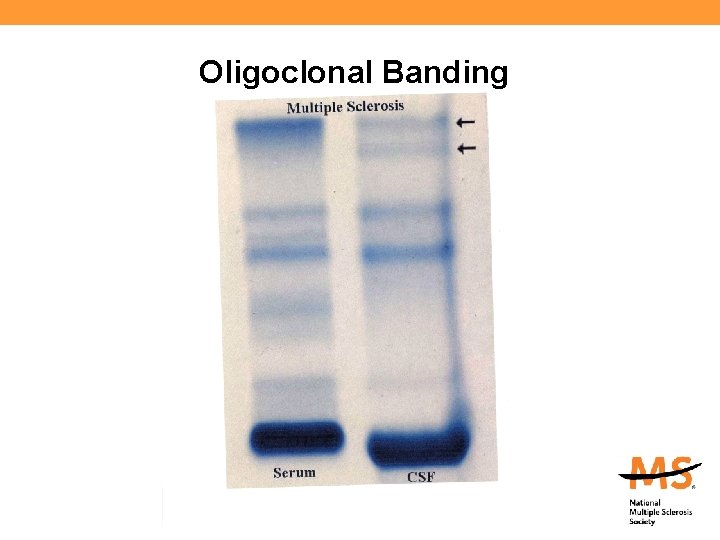
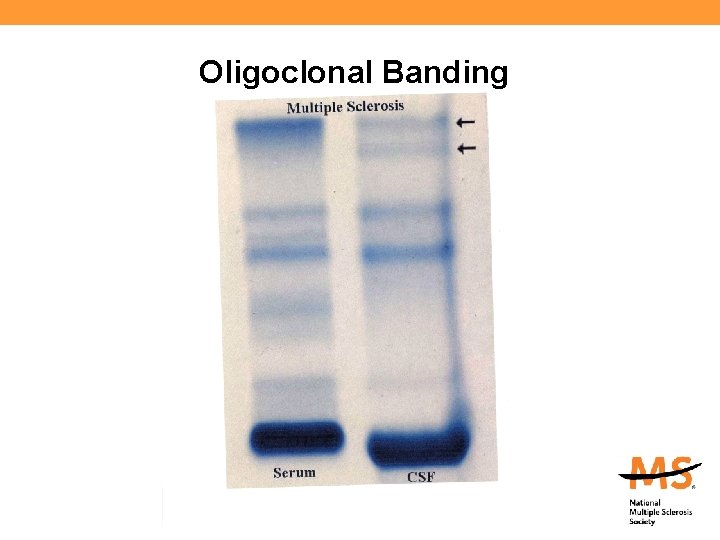
Oligoclonal Banding
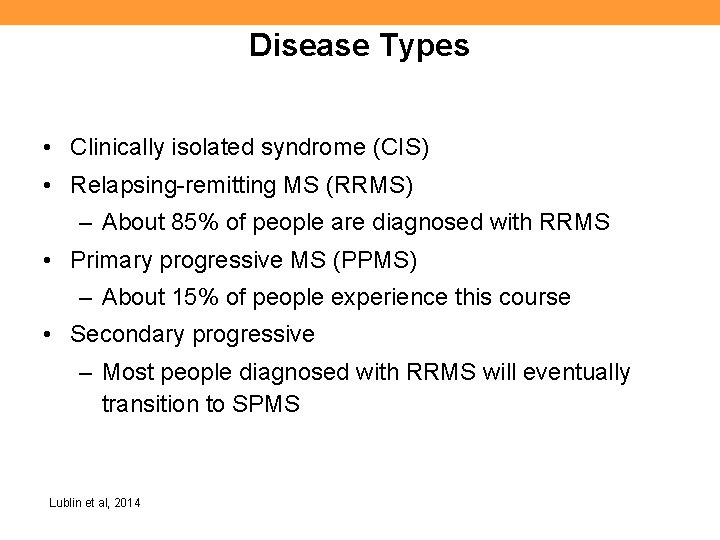
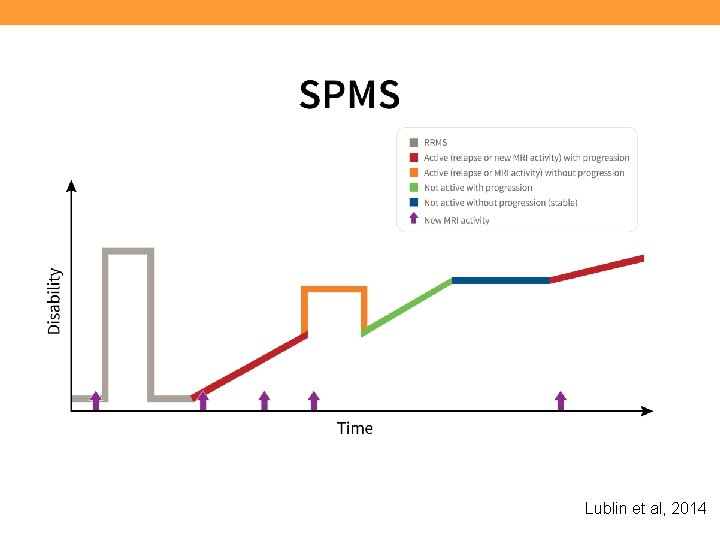
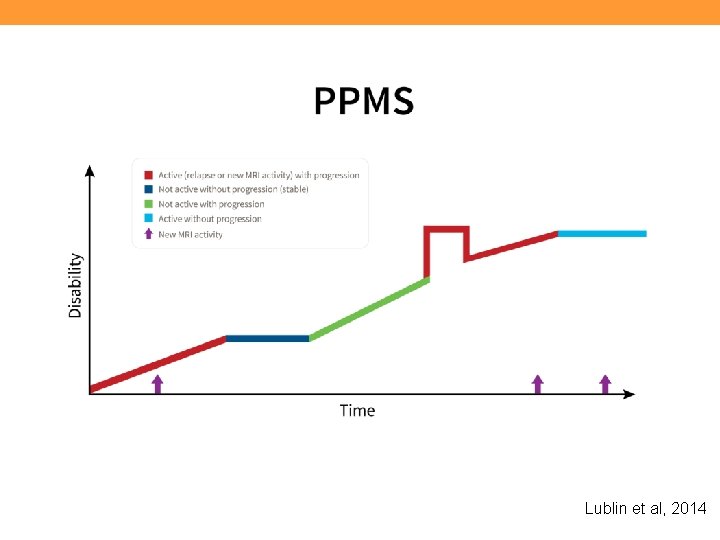
Disease Types • Clinically isolated syndrome (CIS) • Relapsing-remitting MS (RRMS) – About 85% of people are diagnosed with RRMS • Primary progressive MS (PPMS) – About 15% of people experience this course • Secondary progressive – Most people diagnosed with RRMS will eventually transition to SPMS Lublin et al, 2014
Clinically Isolated Syndrome (CIS) • A first neurologic event suggestive of demyelination • Individuals with CIS are at high risk for developing clinically definite MS if the neurologic event is accompanied by multiple, clinically silent (asymptomatic) lesions on MRI typical of MS
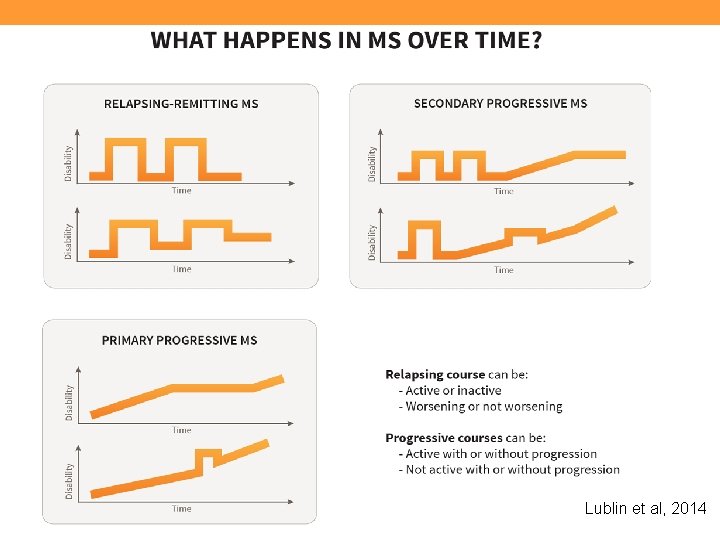
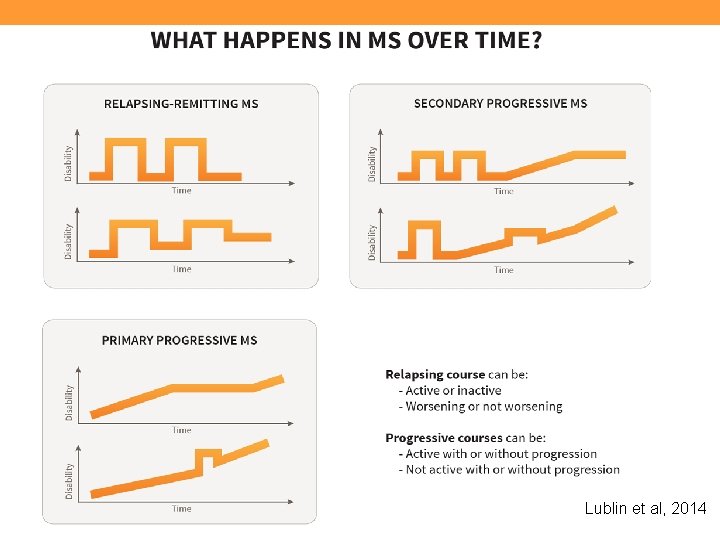
Lublin et al, 2014
Lublin et al, 2014
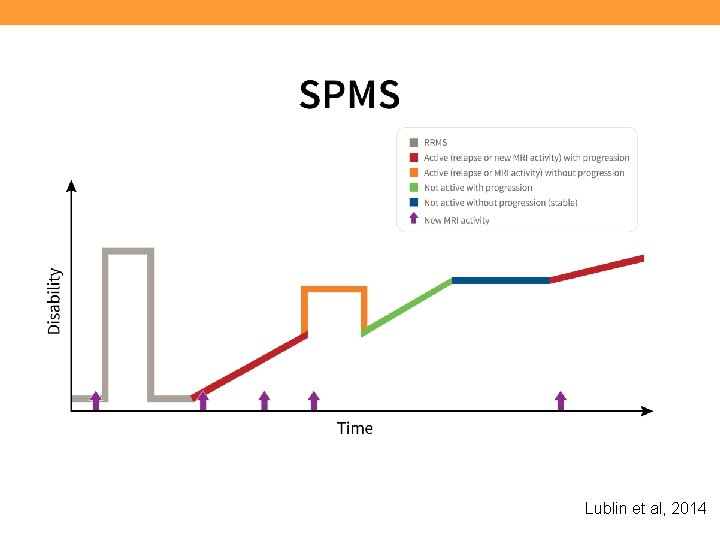
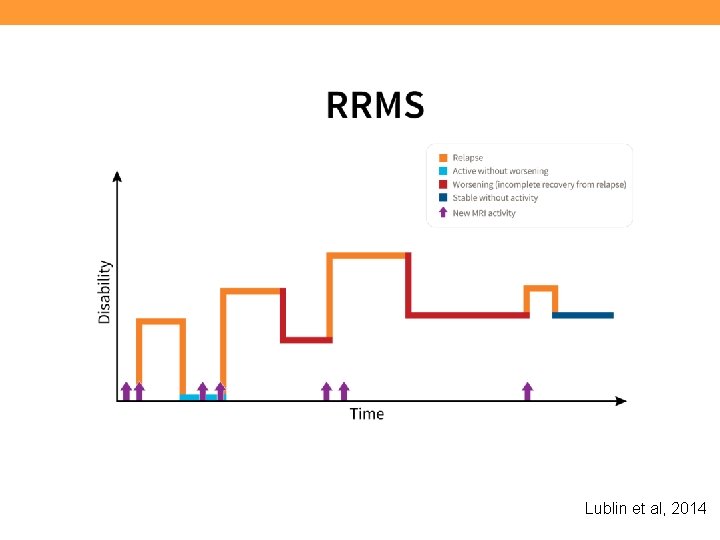
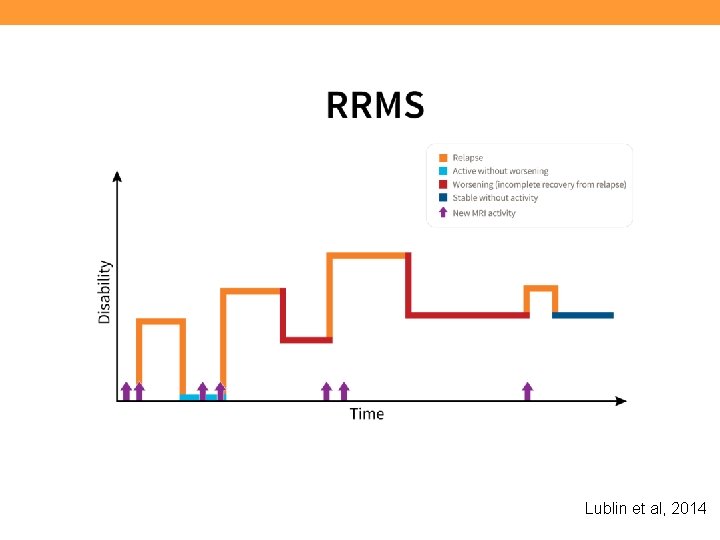
Lublin et al, 2014
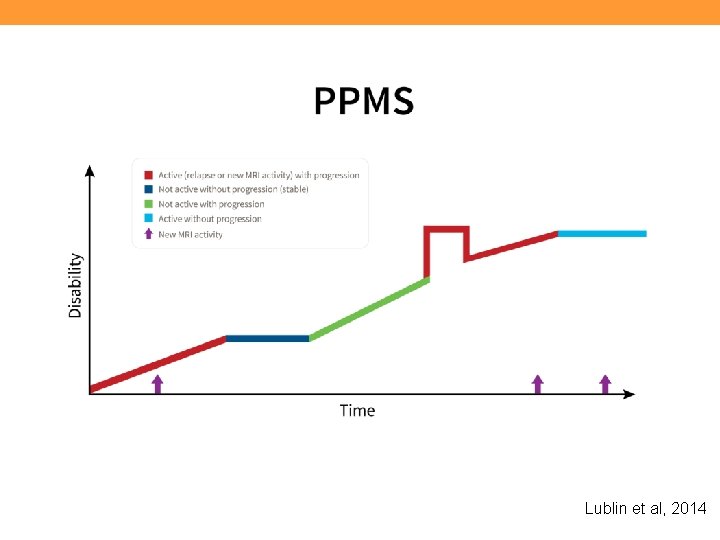
Lublin et al, 2014
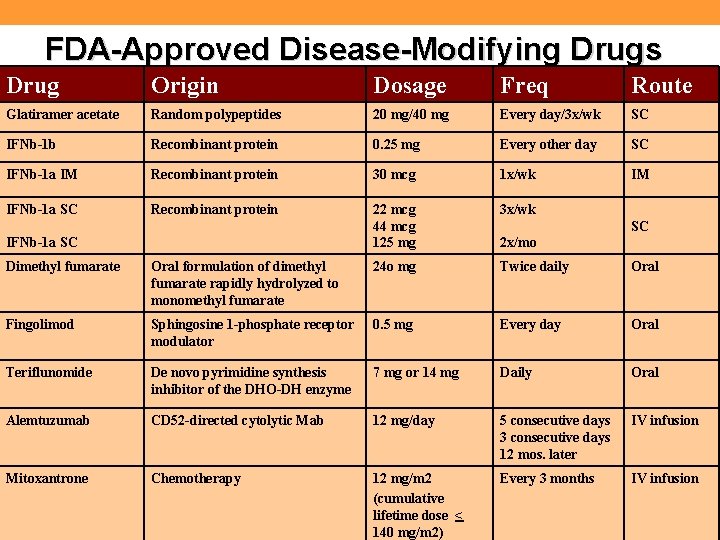
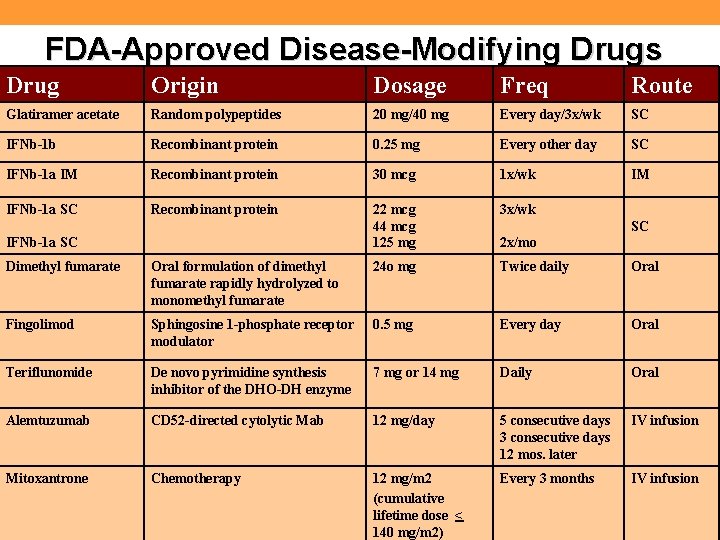
FDA-Approved Disease-Modifying Drugs Drug Origin Dosage Freq Route Glatiramer acetate Random polypeptides 20 mg/40 mg Every day/3 x/wk SC IFNb-1 b Recombinant protein 0. 25 mg Every other day SC IFNb-1 a IM Recombinant protein 30 mcg 1 x/wk IM IFNb-1 a SC Recombinant protein 22 mcg 44 mcg 125 mg 3 x/wk IFNb-1 a SC SC 2 x/mo Dimethyl fumarate Oral formulation of dimethyl fumarate rapidly hydrolyzed to monomethyl fumarate 24 o mg Twice daily Oral Fingolimod Sphingosine 1 -phosphate receptor modulator 0. 5 mg Every day Oral Teriflunomide De novo pyrimidine synthesis inhibitor of the DHO-DH enzyme 7 mg or 14 mg Daily Oral Alemtuzumab CD 52 -directed cytolytic Mab 12 mg/day 5 consecutive days 3 consecutive days 12 mos. later IV infusion Mitoxantrone Chemotherapy 12 mg/m 2 (cumulative lifetime dose < 140 mg/m 2) Every 3 months IV infusion

Deciding Which Disease-Modifying Agent Should Be Used—and When • A medical decision taking into account several factors: – Patient’s disease course and prognostic indicators – Benefits vs. risks of each medication – Co-morbidities – Cost vs. benefits for each patient – Patient’s lifestyle and preferences – Patient readiness
Lifestyle and Personal Preferences • • Patient readiness to treat their MS Preconceptions/attitudes about medications Comfort with needles and self-injection Medication side effects Lifestyle Depression, anxiety Cognitive status
Negative Prognostic Indicators • • Frequent, multifocal attacks Heavy MRI burden on initial scans Pyramidal involvement Ataxia Cognitive difficulties 5 year accumulation of disability Spinal progression (primary progressive MS)

The Concept of “Benign” MS Maybe it should be called: “Mild MS”
Relapse Management • Relapse = new symptom or sudden worsening of old symptom lasting at least 24 hours, and usually accompanied by an objective change in neurologi findings • Treatment with corticosteroids recommended if relapse significantly interferes with everyday functioning – 3 -5 day course of high-dose intravenous methylprednisolone with or without oral taper – High-dose oral steroids may also be used • Rehabilitation can help restore function following a relapse

MS Symptom Management • MS symptoms are variable and unpredictable - Fatigue (most common) - Loss of sensation - Decreased visual acuity, diplopia - Bladder and/or bowel dysfunction - Pain - Sexual dysfunction - Paresthesias (tingling, (numbness, burning) - Emotional disturbances (depression, mood swings) - Cognitive difficulties (memory, attention, processing) - Heat sensitivity - Spasticity - Gait, balance, and coordination problems - Speech/swallowing problems - Tremor - Weakness
Managing Weakness • Exercise – The role of progressive resistive exercise • Pharmacological treatment – Dalfampridine • Mobility aids

Mobility vs. Ambulation • The goal of treatment is to promote function, comfort, and independence • Mobility aids conserve energy, enhance safety, and allow people to remain active and involved – – – – Cane Crutches Walker Ankle foot orthosis Manual wheelchairs Motorized scooters Electric wheelchairs • Dalfampridine (Ampyra™) was approved in 2010 to improve walking speed in MS.
A Word about Temperature Sensitivity • Heat sensitivity is common in MS • Sensitivity to cold can also occur • Even a slight elevation in core body temperature can cause temporary worsening of symptoms (called a pseudoexacerbation) • Cooling strategies are beneficial during: – Hot, humid weather – Exercise – Cooking
Treating Bladder Dysfunction • The small (failure to store) bladder – Oxybutynin in various forms – Tolteridine – Trospium chloride – Others • The large (failure to empty) bladder – Stimulating medication – Intermittent self-catheterization
Treating Bladder Dysfunction, cont’d • Dysynergic bladder – Alpha adrenergic agonists • dibenzyline, terazosin (Hytrin), Cardura – Intermittent self-catheterization • Nocturia – DDAVP-desmopressin
Managing Bowel Dysfunction • • Regular bowel regimen High fiber diet; sufficient liquids Bulk formers Stool softeners Mini enemas Suppositories Enemas
Managing Pain • Dysesthesia, paresthesia – Pharmacological: gabapentin (Neurontin), lamotrigine (Lamictal), carbamazepine (Tegretol), amitriptyline (Elavil), pregabalin (Lyrica), others – Mechanical: gloves, counter-irritant – Other: accupuncture, biofeedback • Orthopedic, mechanical
Depression in MS: Diagnosis and Treatment • Symptoms of depression can be confused with symptoms of MS difficult to diagnose. • Depression is under-diagnosed and under-treated in MS. • Best treatment for depression: Psychotherapy + Medication (+ Exercise)
Depression in MS: What Do We Know? • Depression differs from normal grieving. • People with MS are at increased risk; depression is one of the most common symptoms of MS – resulting from changes in the immune system and in the brain, as well as psychosocial challenges • 50+% of people will experience a major depressive episode at some point over the course of the disease. • Suicide is 7. 5 x more common in MS than in general population (Sadovnick et al. , 1991). Feinstein, A. (2007). The clinical neuropsychiatry of multiple sclerosis (2 nd ed. ). Cambridge and New York: Cambridge University Press.
Depression: The Implications People who are depressed: • Carry an additional, painful burden • Can’t participate actively in their own care • Can’t plan/problem-solve effectively • Are difficult to live with Note: Depression is one of the most treatable symptoms of MS
Common Misconceptions about MS and Cognition • Cognitive impairment (CI) is rare in MS. • CI only occurs in late stage MS or severe MS. • MS is a white-matter disease and does not affect: 1) brain volume, 2) gray matter, 3) the cerebral cortex. • If an MS patient can pass a brief mental status exam, everything is OK. • Memory problems reported by MS patients are usually caused by stress, anxiety, and/or depression. • Discussing CI will upset MS patients/families.
Cognition and Other Disease Characteristics • Cognitive function correlates with lesion load and brain atrophy. • Cognitive dysfunction can occur at any time (even as a first symptom) but is more common later on. • Cognitive dysfunction can occur with any disease course, but is more likely in progressive MS. • Being in an exacerbation is a risk factor for cognitive dysfunction. • Depression can worsen cognition, particularly executive functions (Arnett et al. , 1999). La. Rocca N, Kalb R. Multiple Sclerosis: Understanding the Cognitive Challenges. New York: Demos Medical Publishing, 2006.

Cognitive Functions Affected in MS • • • Attention & concentration - working memory Memory - acquisition and retrieval Speed of information processing Executive Functioning Visual/spatial organization Verbal fluency - word finding De. Luca, J. What we know about cognitive changes in multiple sclerosis. In La. Rocca, N & Kalb, R (eds. ) Multiple sclerosis: understanding the cognitive challenges. New York: Demos Medical Publishing, 2006.
Current Treatment Priorities • Better understanding of MS pathogenesis and heterogeneity to guide development of better therapies and monitoring methods • Additional treatment options for relapsing-remitting MS(RRMS) that are more effective, convenient, and/or tolerable • Effective therapies for purely progressive MS • Neuroprotective and repair strategies • More effective treatments for common symptoms such as fatigue, pain, tremor, and cognitive impairment • More effective psychosocial support Cohen J. Arch Neurol. 2009; 66(7): 821 -828
National MS Society Resources for Your Patients • Nationwide network of chapters • Web site (www. national. MSsociety. org) • Access to reliable information and referrals (1 -800 -344 -4867) • Educational programs (in-person, online) • Support programs (self-help groups, peer and professional counseling, friendly visitors) • Consultation (legal, employment, insurance, long-term care) • Financial assistance
National MS Society Resources for You • Professional Resource Center – www. national. MSsociety. org/PRC; healthprof_info@nmss. org – Free Multiple Sclerosis Diagnosis, Disease & Symptom Management app for smart phones – The Use of Disease-Modifying Therapies in Multiple Sclerosis: Principles and Current Evidence – a consensus paper by the Multiple Sclerosis Coalition (http: //ntl. MS/coalition. DMTconsensus) – Literature search services – Clinical consultations with MS specialist physicians – Professional publications – Insurance Appeal template letters – Consultation on insurance and long-term care issues