Multiple Sclerosis Multiple Sclerosis Inflammatory demyelinating disease of
- Slides: 25
Multiple Sclerosis
Multiple Sclerosis • Inflammatory demyelinating disease of the central nervous system. • Most common cause of neurological disability in young adults.
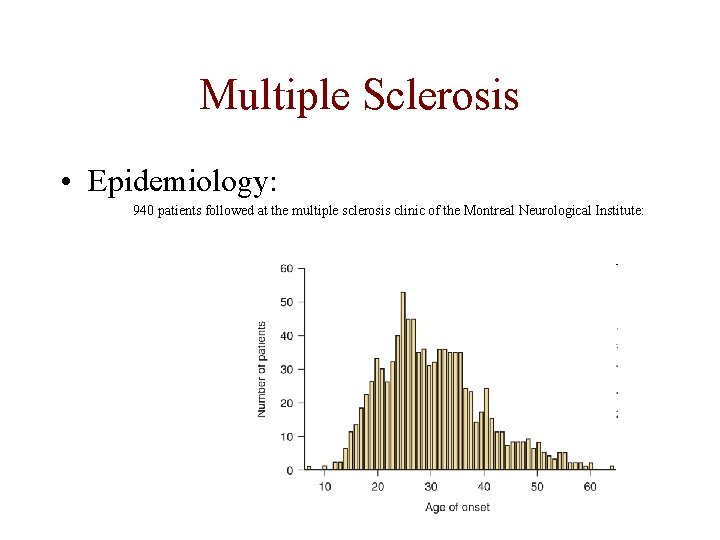
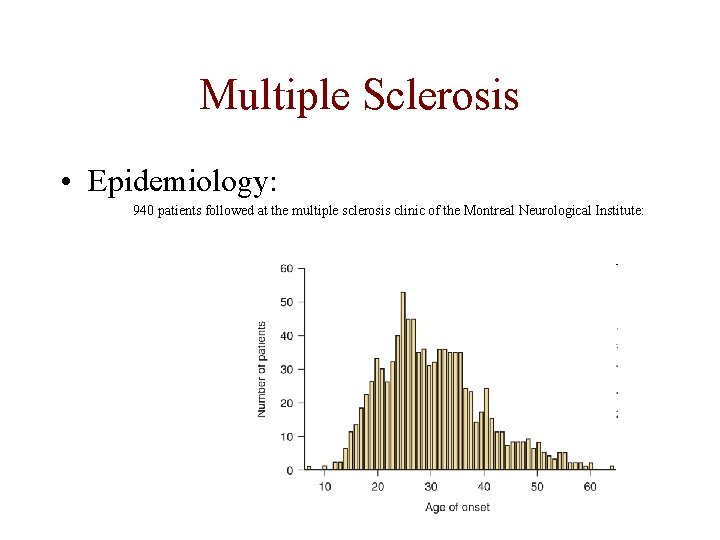
Multiple Sclerosis • Epidemiology: 940 patients followed at the multiple sclerosis clinic of the Montreal Neurological Institute:
Multiple Sclerosis • Epidemiology: • Sex ratio: F: M = 1. 77: 1. 00 • Prevalence ranges from <5 to 60 per 100 000. Higher in Europe and North America. • South Africa: White population: 5 -25/100 000. • Genetics: Sibs 3 -5% risk. Monozygotic twins 20 -38% risk
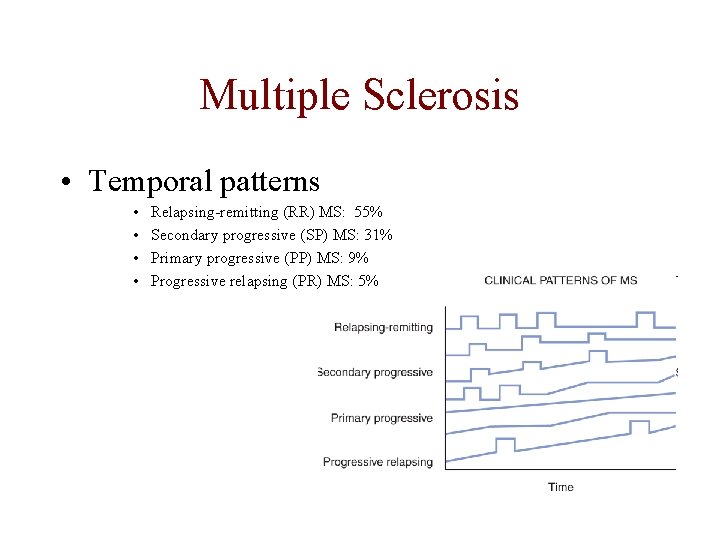
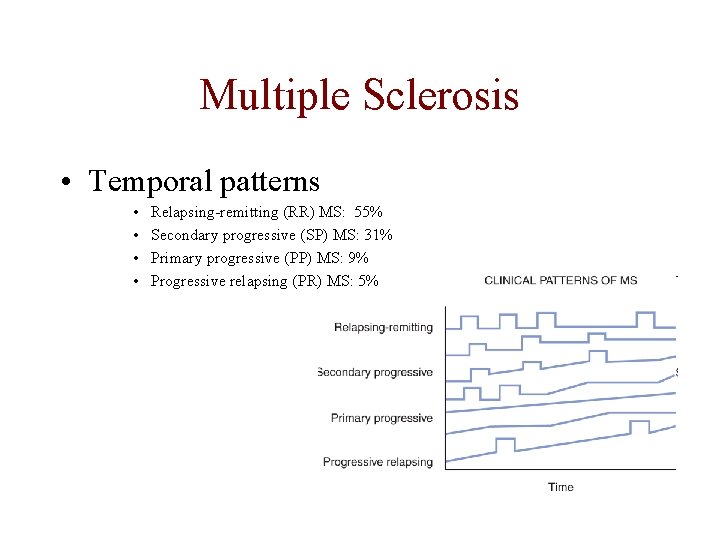
Multiple Sclerosis • Temporal patterns • • Relapsing-remitting (RR) MS: 55% Secondary progressive (SP) MS: 31% Primary progressive (PP) MS: 9% Progressive relapsing (PR) MS: 5%
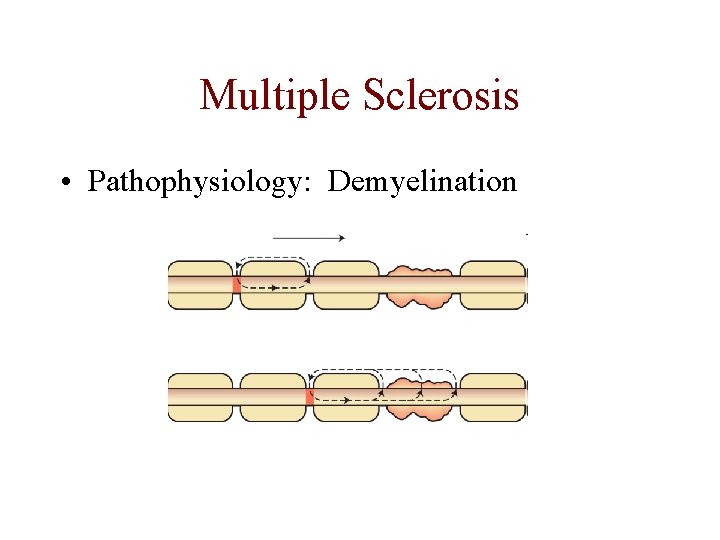
Multiple Sclerosis • Pathophysiology: Demyelination
Multiple Sclerosis • Pathophysiology: – Consequences of demyelination: • • Slowing of conduction Conduction block Uhthoff’s phenomenon – Temperature Mechanical stimulation
Multiple Sclerosis • Pathophysiology: – Axonal injury • Usually occurs later, but also evidence of early loss.
Multiple Sclerosis • Pathophysiology: – Recovery: • Early – Resolution of oedema, cytokines, p. H • Intermediate – Increase in internodal Na channels • Later – Remyelination
Multiple Sclerosis • Pathophysiology: – Immunological disease: • • Complex, not fully elucidated, various patterns. Disruption of perivenular BBB. Migration of T cells (CD 8+CD 4) and macrophages. Macrophages occur in centre of lesion, associated with oligodentrocyte destruction and demyelination. • In periphery of lesion – Remyelination by surviving oligodendrocytes and even oligodendrocyte proliferation. • Plaques: Discreet areas of demyelination, macrophage, and Tcell infiltration, astrocytosis.
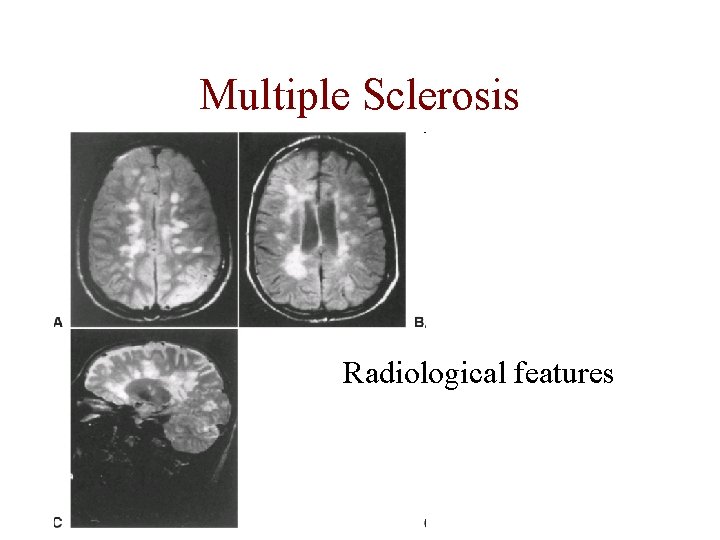
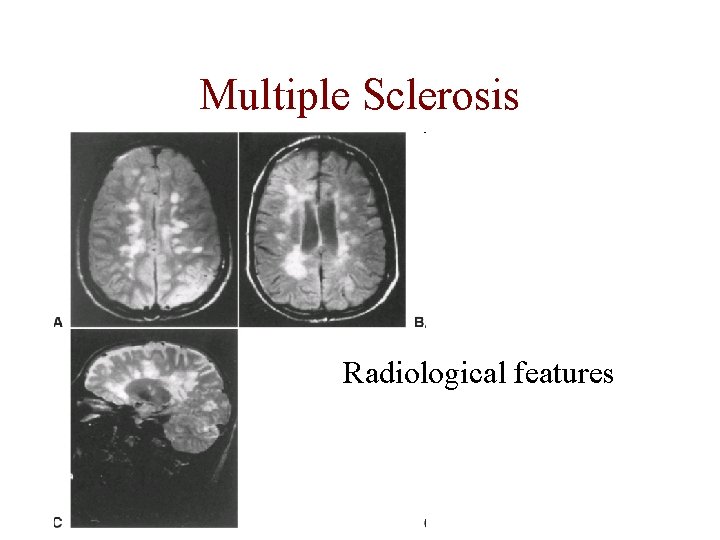
Multiple Sclerosis Radiological features
Multiple Sclerosis • Clinical features: – Cranial nerve deficits: • Optic neuritis – common • Oculomotor involvement: – Isolated nerves: VI>III>IV – Internuclear ophthalmoplegia – Nystagmus • • Trigeminal neuralgia Facial palsy, but Taste not affected. Hemifacial spasma and myokemia Pseudobulbar palsy – common in later stages
Multiple Sclerosis • Clinical features: – Sensory symptoms: • Common • Various patterns • Often paresthesias, dysesthesias and other positive symptoms. • Plaques involving dorsal root entry zones are common – radicular pain or severe loss of proprioception: useless hand with normal power.
Multiple Sclerosis • Clinical features: – Motor features: • • Usually later than sensory Hemiparesis with cerebral or brainstem lesions Acute partial myelitis. Gradually progressive paraparesis characteristic of progressive forms of MS. – Cerebellar features - common
Multiple Sclerosis • Clinical features: – Impairment of Bladder, Bowel, and Sexual Functions: • Urgency and urgency incontinence • Dyssynergic voluntary sphincter activity • With involvement of sacral spinal segments – Hypotonic bladder with overflow incontinence. • Constipation > fecal incontinence • Sexual dysfunction
Multiple Sclerosis • Clinical features: – Cognitive Impairment: • Subtle and underreported. • Subcortical: Abstract conceptualization, recent memory, attention, and speed of information processing – Affective Disorders: • Depression – 50% risk. Higher than with other chronic neurological diseases. – Fatigue
Multiple Sclerosis • Clinical features: – Characteristic positive features: • Lhermitte’s phenomenon - Electric shock radiating down the spine or into the limbs on flexion of the neck. • Uhthoff’s phenomenon – Worsening of existing symptoms • Trigeminal neuralgia, central pain, paraspinal spasms, myokemia, phosphenes and a variety of other paroxysmal neurological symptoms.
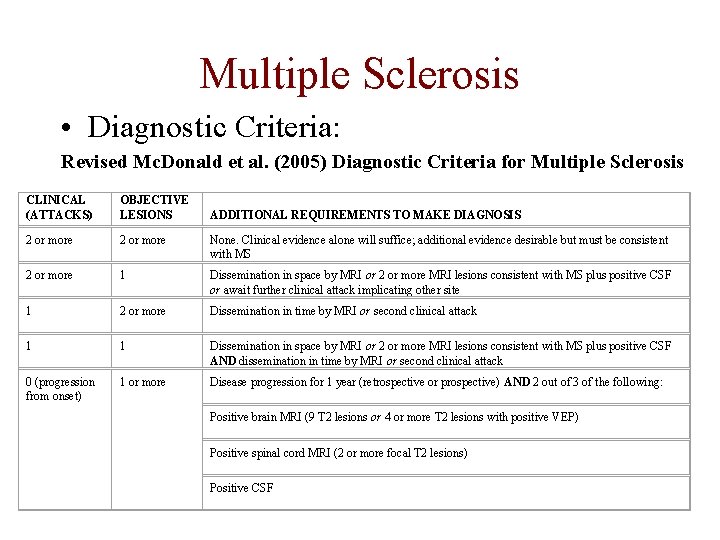
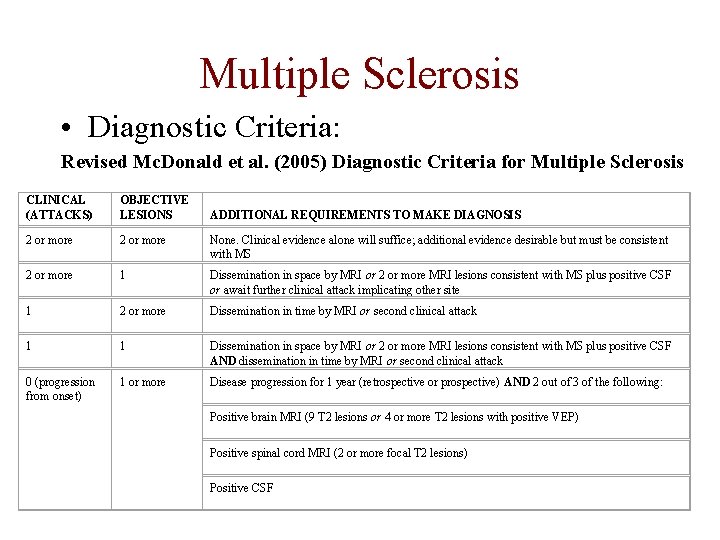
Multiple Sclerosis • Diagnostic Criteria: Revised Mc. Donald et al. (2005) Diagnostic Criteria for Multiple Sclerosis CLINICAL (ATTACKS) OBJECTIVE LESIONS 2 or more None. Clinical evidence alone will suffice; additional evidence desirable but must be consistent with MS 2 or more 1 Dissemination in space by MRI or 2 or more MRI lesions consistent with MS plus positive CSF or await further clinical attack implicating other site 1 2 or more Dissemination in time by MRI or second clinical attack 1 1 Dissemination in space by MRI or 2 or more MRI lesions consistent with MS plus positive CSF AND dissemination in time by MRI or second clinical attack 0 (progression from onset) 1 or more Disease progression for 1 year (retrospective or prospective) AND 2 out of 3 of the following: ADDITIONAL REQUIREMENTS TO MAKE DIAGNOSIS Positive brain MRI (9 T 2 lesions or 4 or more T 2 lesions with positive VEP) Positive spinal cord MRI (2 or more focal T 2 lesions) Positive CSF
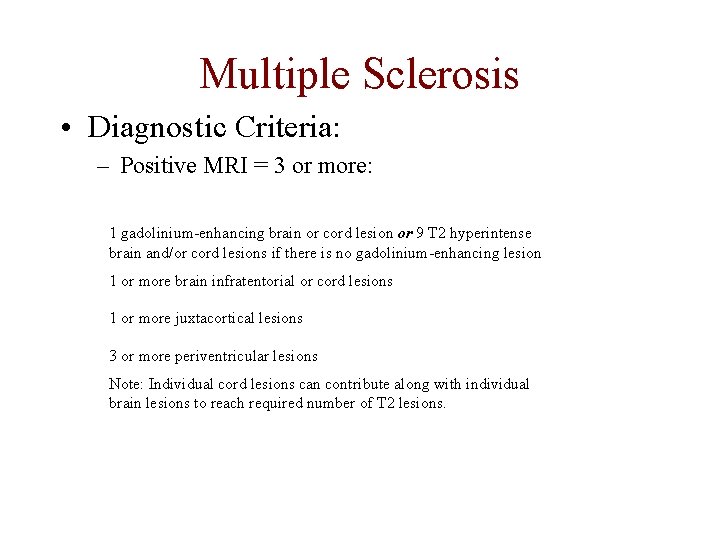
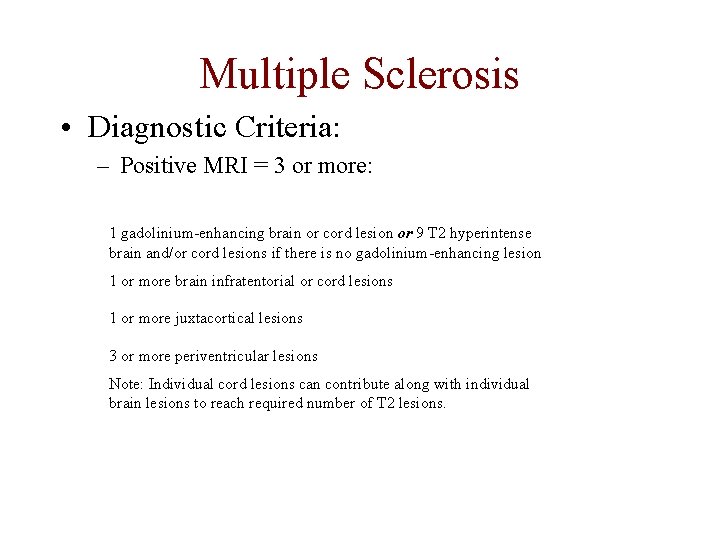
Multiple Sclerosis • Diagnostic Criteria: – Positive MRI = 3 or more: 1 gadolinium-enhancing brain or cord lesion or 9 T 2 hyperintense brain and/or cord lesions if there is no gadolinium-enhancing lesion 1 or more brain infratentorial or cord lesions 1 or more juxtacortical lesions 3 or more periventricular lesions Note: Individual cord lesions can contribute along with individual brain lesions to reach required number of T 2 lesions.
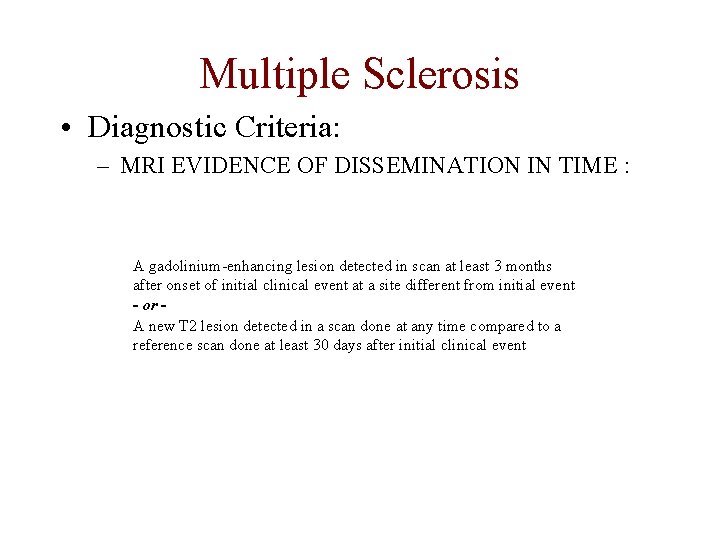
Multiple Sclerosis • Diagnostic Criteria: – MRI EVIDENCE OF DISSEMINATION IN TIME : A gadolinium-enhancing lesion detected in scan at least 3 months after onset of initial clinical event at a site different from initial event - or A new T 2 lesion detected in a scan done at any time compared to a reference scan done at least 30 days after initial clinical event
Multiple Sclerosis • Prognosis: – Poor prognostic indicators: • • • Male Older onset Progressive from start Frequent initial relapses Pyramidal or brainstem rather that optic neuritis or sensory symptoms. – Pure optic neuritis, without brain lesions has good prognosis, only 16 % progress to MS in 5 years. Compared to 51% with 3+ lesions.
Multiple Sclerosis • Treatment: – Acute attacks: Methyl-Prednisolone: 500 mg to 1000 mg daily x 3 -5/7.
Multiple Sclerosis • Treatment: – Disease modifying treatment in RRMS: • • • Interferon beta-1 a (Avonex) 30 ug IMI/w Interferon beta 1 a (Rebif) 22 -44 ug SC 3 x/w Interferon beta-1 b (Betaferon) 8 MIU alt days Glatirimer acetate (Copaxone) 20 mg daily Mitoxanthrone Natalizumab (Tysarbi)
Multiple Sclerosis • Treatment: – Disease modifying treatment in SP and PRMS: • • • Mitoxanthrone Interferon beta-1 b (Betaferon) Cyclophosphamide ? ? Azathioprine ? ? Methotrexate ? ? Monthly – 3 monthly pulses of Solumedrol ? ?
Multiple Sclerosis • Treatment: – Disease modifying treatment in PPMS: • ? ? ?